Systems Biology in Biomarker Validation: From Discovery to Clinical Application
This article provides a comprehensive overview of the integration of systems biology into the biomarker validation pipeline for researchers, scientists, and drug development professionals.
Systems Biology in Biomarker Validation: From Discovery to Clinical Application
Abstract
This article provides a comprehensive overview of the integration of systems biology into the biomarker validation pipeline for researchers, scientists, and drug development professionals. It explores the foundational principles of moving beyond single-target approaches to understand complex disease networks. The scope covers methodological frameworks that combine high-throughput omics technologies, in silico modeling, and preclinical studies to develop robust, multi-marker panels. It further addresses critical challenges in optimization and troubleshooting, including specificity, reproducibility, and analytical variability. Finally, the article details rigorous statistical and clinical validation protocols, featuring comparative analyses of real-world algorithms to establish clinical utility and translate biomarker panels into tools for precision medicine.
The Systems Biology Framework: A New Paradigm for Biomarker Discovery
The landscape of disease diagnosis and monitoring is undergoing a fundamental transformation, shifting from reliance on single biomarkers to the implementation of multi-marker panels. This evolution is particularly critical for complex diseases such as pancreatic cancer, neurodegenerative disorders, and autoimmune conditions, where single-target biomarkers often lack sufficient sensitivity and specificity for early detection and accurate prognosis. By integrating diverse molecular information through systems biology approaches, multi-marker panels capture the multifaceted nature of disease pathophysiology, offering significantly improved diagnostic performance. This review synthesizes current evidence supporting the superiority of biomarker panels, details experimental methodologies for their development and validation, and frames these advances within the context of systems biology, providing researchers and drug development professionals with a comprehensive resource for advancing diagnostic innovation.
Traditional diagnostic approaches have predominantly relied on pauci-parameter measurements—often just a single parameter—to decipher specific disease conditions [1]. While simple and historically valuable, this approach presents significant limitations for complex multifactorial diseases. Single-marker tests (SMTs) fundamentally lack the robustness to capture the intricate biological networks perturbed in conditions like cancer, neurodegenerative disorders, and autoimmune diseases [2] [1].
The well-documented flaws of carbohydrate antigen 19-9 (CA19-9) in pancreatic ductal adenocarcinoma (PDAC) exemplify these limitations. As the only FDA-approved serological biomarker for PDAC, CA19-9 demonstrates increasing concentration and sensitivity with advancing disease stage. However, in early stages (e.g., stage I), its levels are often similar to those found in various benign conditions and other malignancies, resulting in unacceptably low specificity for early detection [3]. Furthermore, approximately 6% of Caucasians and 22% of non-Caucasians lack Lewis antigen A necessary to produce CA19-9, leading to false-negative results [3]. Consequently, international guidelines do not recommend CA19-9 as a standalone diagnostic method but rather as a longitudinal marker in patients with detectable levels at baseline [3].
Theoretical and empirical studies confirm that single-marker approaches face inherent constraints. In genetic association studies of rare variants, SMTs struggle with low statistical power and potential violations of established estimator properties [4]. While multi-marker tests (MMTs) were proposed to address these challenges, their performance relative to SMTs depends on specific conditions. For quantitative traits, SMTs can outperform MMTs when causal variants have large effect sizes, while MMTs show advantage with small effect sizes—a common scenario in complex diseases [4]. For binary traits, the power dynamics differ further, highlighting that no uniformly superior test exists for all scenarios [5].
Theoretical Foundation: Advantages of Multi-Marker Strategies
Multi-marker panels address fundamental gaps in single-target approaches by capturing disease heterogeneity, improving statistical power, and representing the interconnected nature of biological systems.
Capturing Disease Heterogeneity and Biological Complexity
Complex diseases like pancreatic cancer, multiple sclerosis, and psychiatric disorders involve dysregulation across multiple biological pathways rather than isolated molecular defects [2] [6]. Multi-protein biomarker tests are particularly suited for measuring disease progression because they can capture the breadth of disease heterogeneity across patient populations and within individual patients as their biology changes in response to disease manifestations, aging, and therapies [6].
The systems biology perspective recognizes that biological information in living systems is captured, transmitted, modulated, and integrated by networks of molecular components and cells [1]. Disease-associated molecular fingerprints result from perturbations to these biological networks, which are better captured by measuring multiple network nodes simultaneously than by assessing individual components in isolation [1]. This approach has revealed that initial molecular network changes often occur well before any detectable clinical signs of disease, creating opportunities for earlier intervention if these multi-component signatures can be detected [1].
Statistical and Diagnostic Performance Advantages
From a statistical perspective, multi-marker panels incorporate various sources of biomolecular and clinical data to guarantee higher robustness and power of separation for clinical tests [2]. The performance advantage depends on the correlation structure among markers and their relationship to causal disease variants [5]. When adjacent markers show high correlation, multi-marker tests tend to demonstrate better performance than single-marker tests [5].
Table 1: Comparative Performance of Single-Marker vs. Multi-Marker Approaches
| Feature | Single-Marker Tests | Multi-Marker Panels |
|---|---|---|
| Biological Coverage | Limited to one pathway or process | Captures multiple disease-relevant pathways simultaneously |
| Statistical Power | Varies by effect size; better for large effects | Generally superior for small effect sizes common in complex diseases |
| Handling Heterogeneity | Poor; misses disease subtypes | Good; can identify and stratify patient subgroups |
| Diagnostic Specificity | Often compromised by non-disease influences | Enhanced through multi-parameter assessment |
| Early Detection Capability | Limited for complex diseases | Improved through network perturbation detection |
Evidence and Case Studies: Performance Across Disease Areas
Pancreatic Ductal Adenocarcinoma (PDAC)
Pancreatic cancer exemplifies the critical need for better diagnostic approaches, with a dismal 5-year survival rate of approximately 10% largely attributable to late diagnosis [3]. At diagnosis, less than 20% of PDAC tumors are eligible for curative resection, highlighting the urgent need for early detection methods [3]. Liquid biopsy—the minimally invasive sampling and analysis of body fluids like blood—offers promising avenues for PDAC detection through analysis of circulating tumor cells (CTCs), circulating cell-free DNA and RNA (cfDNA, cfRNA), extracellular vesicles (EVs), and proteins [3].
While individual liquid biopsy biomarkers may lack sufficient sensitivity or specificity for reliable PDAC detection, combinations in multimarker panels significantly improve diagnostic performance. CTCs specifically demonstrate high specificity for PDAC (>90% in several studies) but present detection challenges in early stages due to low abundance—approximately one CTC among more than a million blood cells—and a short half-life of only 1–2.4 hours [3]. This limitation may be overcome with novel, more sensitive analysis techniques and processing of larger blood volumes [3].
Beyond traditional tumor-derived markers, the prominent desmoplastic stroma characteristic of PDAC provides additional biomarker sources. Circulating host cells, including cancer-associated fibroblasts (CAFs), represent key components of the tumor microenvironment that can detach and enter circulation as possible liquid biopsy biomarkers [3]. The three major CAF types—myofibroblast CAFs (myCAFs), inflammatory CAFs (iCAFs), and antigen-presenting CAFs (apCAFs)—perform distinct functions and may provide complementary information when incorporated into multi-analyte panels [3].
Ovarian Cancer
A retrospective study investigating multimarker combinations for early ovarian cancer detection identified an optimal 4-marker panel comprising CA125, HE4, MMP-7, and CA72-4 [7]. This panel demonstrated significantly improved performance compared to any single marker alone, achieving 83.2% sensitivity for stage I disease at a high specificity of 98% [7].
Critical to their utility in longitudinal screening algorithms, the selected markers exhibited favorable variance characteristics, with within-person coefficient of variation (CV) values lower than between-person CV values: CA125 (15% vs. 49%), HE4 (25% vs. 20%), MMP-7 (25% vs. 35%), and CA72-4 (21% vs. 84%) [7]. This variance profile indicates stable individual baselines in healthy volunteers, enabling the establishment of person-specific reference ranges that enhance early detection capability when deviations occur.
Multiple Sclerosis
In multiple sclerosis, measuring disease progression—the driver of long-term disability—has remained particularly challenging with conventional clinical assessments alone [6]. The future of progression management lies in multi-protein biomarker tests, which can provide quantitative, objective insights into disease biology that imaging and symptom assessment cannot capture [6].
Multi-protein tests are ideal for measuring MS progression because they can capture disease heterogeneity across populations and within individual patients, while offering prognostic power that enables personalized medicine approaches [6]. Development of such panels involves evaluating thousands of proteins as potential biomarkers, examining both statistical associations with progression endpoints and biological relevance to MS pathways and mechanisms [6].
Methodological Framework: Developing and Validating Marker Panels
Experimental Design and Statistical Considerations
Robust development of multi-marker panels requires specialized methodological approaches to address unique statistical challenges. A primary concern is obtaining unbiased estimates of both the biomarker combination rule and the panel's performance, typically evaluated via ROC(t)—the sensitivity corresponding to specificity of 1-t on the receiver operating characteristic curve [8].
Two-stage group sequential designs offer efficiency for biomarker development by allowing early termination for futility, thereby conserving valuable specimens when initial performance is inadequate [8]. In such designs, biomarker data is collected from first-stage samples, the panel is built and evaluated, and if pre-specified performance criteria are met, the study continues to the second stage with remaining samples assayed [8]. Nonparametric conditional resampling algorithms can then use all study data to provide unbiased estimates of the biomarker combination rule and ROC(t) [8].
An additional source of bias arises from using the same data to derive the combination rule and estimate performance, particularly problematic in studies with small sample sizes [8]. The Copas & Corbett (2002) shrinkage correction addresses this bias and can be incorporated into resampling algorithms [8].
Table 2: Key Methodological Considerations in Panel Development
| Development Phase | Key Considerations | Recommended Approaches |
|---|---|---|
| Study Design | Resource optimization; Early futility assessment | Two-stage group sequential design; Conditional unbiased estimation |
| Biomarker Selection | Balancing statistical association with biological plausibility | Integration of correlation data with pathway analysis |
| Statistical Modeling | Over-optimism bias with small sample sizes | Shrinkage corrections; Resampling methods |
| Performance Evaluation | Comprehensive assessment of discriminative ability | ROC(t) estimation; Sensitivity at fixed specificity |
| Validation | Generalizability across populations | Testing in multiple independent cohorts |
Systems Biology Framework
Systems biology approaches view biology as an information science, studying biological systems as a whole and their interactions with the environment [1]. This perspective has particular power in biomarker discovery because it focuses on fundamental disease causes and identifies disease-perturbed molecular networks [1] [9].
The transformation in biology through systems biology enables systems medicine, which uses clinically detectable molecular fingerprints resulting from disease-perturbed biological networks to detect and stratify pathological conditions [1]. These molecular fingerprints can be composed of diverse biomolecules—proteins, DNA, RNA, miRNA, metabolites—and their post-translational modifications, all providing complementary information about network states [1].
In practice, applying systems biology to complex diseases involves several key steps: measuring global biological information, integrating information across different levels, studying dynamic changes in biological systems as they respond to environmental influences, modeling the system through integration of global dynamic data, and iteratively testing and improving models through prediction and comparison [1]. This approach was successfully applied to prion disease, revealing dynamically changing perturbed networks that occur well before clinical signs appear [1].
The Scientist's Toolkit: Research Reagent Solutions
Implementing multi-marker panel research requires specialized reagents and technologies across multiple analytical domains. The following table details essential research tools and their applications in panel development and validation.
Table 3: Essential Research Reagents and Technologies for Multi-Marker Studies
| Reagent/Technology | Function | Application in Panel Development |
|---|---|---|
| Liquid Biopsy Collection Systems | Standardized sample acquisition from blood, saliva, urine | Minimizes pre-analytical variability across multi-center studies |
| Immunoassay Reagents | Quantification of protein biomarkers (e.g., CA125, HE4) | Enables precise measurement of panel components in validation phases |
| Proteomic Analysis Platforms | Simultaneous measurement of thousands of proteins | Facilitates discovery phase biomarker identification |
| Next-Generation Sequencing Kits | Genomic, transcriptomic, and epigenomic analysis | Provides complementary molecular dimensions for comprehensive panels |
| Extracellular Vesicle Isolation Kits | Enrichment of exosomes and microvesicles | Expands analyte repertoire beyond conventional biomarkers |
| Multiplex PCR Reagents | Amplification of multiple nucleic acid targets | Supports genetic and transcriptomic panel components |
| Reference Standard Materials | Calibration and quality control | Ensures reproducibility and comparability across batches and sites |
| Data Integration Software | Systems biology analysis of multi-omic data | Enables network-based biomarker selection and validation |
| Tioxaprofen | Tioxaprofen, CAS:40198-53-6, MF:C18H13Cl2NO3S, MW:394.3 g/mol | Chemical Reagent |
| Talatisamine | Talatisamine, MF:C24H39NO5, MW:421.6 g/mol | Chemical Reagent |
The transition from single-target biomarkers to multi-marker panels represents a paradigm shift in diagnostic development, particularly for complex diseases where multiple biological pathways are perturbed. By capturing disease heterogeneity, leveraging complementary information from diverse analytes, and reflecting the network nature of disease pathophysiology, multi-marker approaches offer substantially improved sensitivity and specificity compared to traditional single-marker tests. The integration of systems biology principles provides a robust framework for discovering and validating these panels, while advanced statistical methods address the unique challenges of development and performance estimation. As measurement technologies continue to advance and computational methods become more sophisticated, multi-marker panels are poised to transform disease detection, monitoring, and ultimately patient outcomes across a spectrum of complex conditions.
In the disciplined approach of modern drug discovery and development, the Mechanism of Disease (MOD) and Mechanism of Action (MOA) provide the essential conceptual framework for understanding disease pathology and therapeutic intervention. The MOD defines the precise biological pathways, molecular networks, and pathophysiological processes that contribute to a disease state [10]. In parallel, the MOA describes the specific biochemical interaction through which a therapeutic entity produces its pharmacological effect, ideally counteracting the MOD [10]. Within biomarker science, these concepts transition from theoretical models to practical tools; biomarkers serve as the measurable indicators that provide an objective window into these mechanisms, bridging the gap between biological theory and clinical application [11] [12]. The integration of MOD and MOA knowledge is therefore critical for the rational development of biomarker panels, moving beyond simple correlation to establish causative links that can reliably predict disease progression or therapeutic response.
Defining the Framework: MOD, MOA, and Biomarker Interrelationships
Formal Definitions and Classifications
- Mechanism of Disease (MOD): A comprehensive description of the network of biological pathways, molecular interactions, and cellular processes that are dysregulated and contribute to the initiation and progression of a pathological condition [10]. The MOD represents the fundamental target for any therapeutic intervention.
- Mechanism of Action (MOA): The specific biochemical interaction through which a drug substance produces its pharmacological effect, typically designed to modulate a key element within the MOD network to restore a state of health [10].
- Biomarker: "A defined characteristic that is measured as an indicator of normal biological processes, pathogenic processes, or responses to an exposure or intervention" [11]. Biomarkers are the empirical observables that are perturbed by the MOD and subsequently modulated by the MOA.
Biomarker Classifications Within the MOD/MOA Context
Biomarkers are categorized based on their specific application in the drug development continuum, each type providing distinct insights into MOD or MOA [11] [12]:
Table: Biomarker Classifications and Their Roles in MOD and MOA
| Biomarker Type | Definition | Role in MOD/MOA Context | Example |
|---|---|---|---|
| Diagnostic | Detects or confirms presence of a disease or condition [11]. | Identifies the manifestation of the MOD in a specific patient. | AMACR for prostate cancer [13]. |
| Monitoring | Measured serially to assess status of a disease or medical condition [11]. | Tracks the activity of the MOD over time or in response to a therapy. | CD4 counts in HIV [11]. |
| Pharmacodynamic/ Response | Indicates a biological response to a therapeutic intervention [11]. | Provides direct evidence of the MOA in action. | HIV viral load under antiretroviral treatment [12]. |
| Predictive | Identifies individuals more likely to experience a favorable or unfavorable effect from a specific therapeutic [11]. | Stratifies patients based on the relevance of a specific MOA to their individual MOD. | Galactomannan for enrolling patients in antifungal trials [12]. |
| Safety | Indicates the potential for or occurrence of toxicity due to an intervention [11]. | Monitors for unintended consequences of the MOA, often related to off-target effects. | Hepatic aminotransferases for liver toxicity [12]. |
A Systems Biology Platform for Integrating MOD and MOA in Biomarker Development
The complexity of human biology and the multifactorial nature of most diseases mean that a "single-target" drug development approach is often insufficient [10]. Systems biology provides an interdisciplinary framework that uses computational and mathematical methods to study complex interactions within biological systems, making it ideally suited for elucidating MOD and MOA [10]. This approach is fundamental for developing robust biomarker panels.
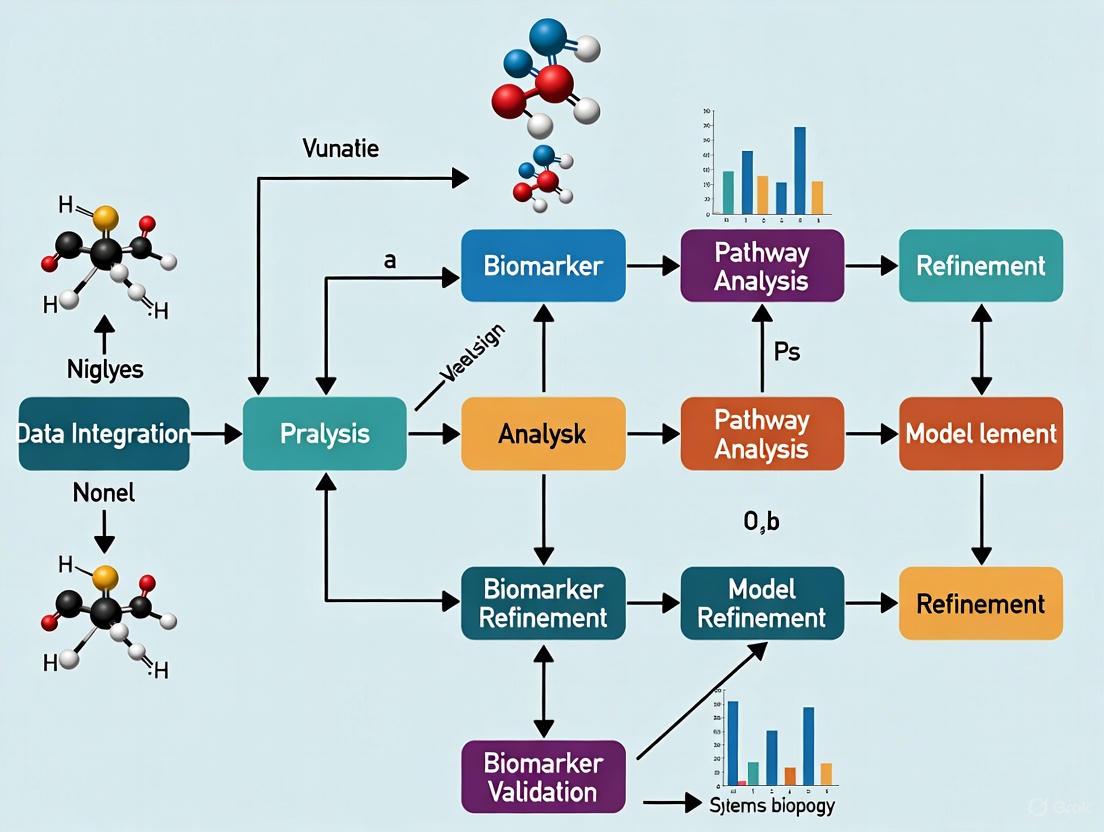
A Stepwise Systems Biology Workflow
The following workflow visualizes the systematic, multi-stage process for developing biomarker panels through the integration of MOD and MOA.
This platform begins with the integration of multi-scale data (genomics, transcriptomics, proteomics, metabolomics) to map the complex network of the MOD [10] [14]. The subsequent identification and design of therapies with a specific MOA are then informed by this network model. Finally, candidate biomarker panels are distilled from the key nodes and pathways that connect the MOD and MOA, enabling the translation of these mechanistic insights into clinical tools for patient stratification and treatment monitoring [10].
Comparative Analysis: Mechanism-Based vs. Traditional Biomarker Discovery
The shift from a traditional, data-centric biomarker discovery pipeline to a mechanism-based approach that is grounded in MOD/MOA understanding represents a significant evolution in the field. The mechanism-based paradigm leverages the growing wealth of functional knowledge and multi-omics data to yield biomarkers with greater biological relevance and clinical utility [15].
Table: Comparison of Traditional and Mechanism-Based Biomarker Discovery
| Aspect | Traditional Approach | Mechanism-Based (MOD/MOA-Driven) Approach |
|---|---|---|
| Core Philosophy | Data-driven; seeks statistically significant differences between sample groups without prior mechanistic hypothesis [15]. | Knowledge-driven; starts with or builds a model of the MOD to inform biomarker selection [10] [15]. |
| Typical Methods | Untargeted mass spectrometry, broad microarrays, followed by targeted ELISA validation [15]. | Pathway analysis, network modeling, multi-omics integration, and systems biology platforms [10] [15]. |
| Primary Output | Lists of differentially expressed biomolecules (genes, proteins, metabolites) [15]. | Contextualized biomarker panels that map onto specific pathways within the MOD/MOA network [16]. |
| Key Strength | Unbiased; can discover novel associations without preconceptions. | Results are more interpretable and biologically plausible, facilitating clinical adoption [15]. |
| Major Challenge | High false-positive rate; poor validation performance due to lack of biological context [15]. | Requires high-quality, multi-scale data and sophisticated computational models [10]. |
| Clinical Translation | Often fails because the biomarker's link to disease pathology is not well understood [15]. | Higher potential for success as biomarkers are inherently linked to core disease mechanisms and drug actions [10]. |
Case Study: Uncovering MOD and Biomarkers in Schizophrenia and Bipolar Disorder
A 2021 study published in Scientific Reports provides a compelling example of a mechanism-based, systems biology approach to biomarker discovery for complex mental disorders [16]. The research aimed to identify the pathways underlying schizophrenia (SCZ) and bipolar disorder (BD) by starting with a curated set of metabolite biomarkers.
Experimental Protocol and Workflow
The methodology followed a structured, multi-stage computational and analytical process, as detailed below.
- Data Collection: The researchers first compiled 46 metabolite biomarkers previously reported in the literature for SCZ and BD (e.g., glutamate, GABA, citrate, myo-inositol) from human blood and serum samples [16].
- Protein Collection: These metabolite biomarkers were then mapped to their related enzymes and proteins using the Human Metabolome Database (HMDB) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway maps, resulting in a set of 610 proteins for SCZ and 495 for BD [16].
- Network Construction: A protein-protein interaction (PPI) network was constructed using the HIPPIE database, creating a large network of 5,595 interactions among 3,184 proteins relevant to the diseases [16].
- Cluster and Pathway Analysis: A graph-clustering algorithm (DPClusO) was applied to this PPI network to identify statistically significant functional modules. These clusters were then analyzed to elucidate the significant pathways underlying the diseases [16].
Key Findings and Outcomes
This mechanism-based analysis revealed that the 28 significant pathways identified for SCZ and BD primarily coalesced into three major biological systems, providing a novel, integrated view of their MOD [16]:
- Energy Metabolism: Dysregulation in pathways such as citrate cycle, glycolysis/gluconeogenesis, and oxidative phosphorylation.
- Neuron System: Alterations in glutamatergic, GABAergic, and cholinergic synapse pathways.
- Stress Response: Involvement of hypoxia response and reactive oxygen species pathways.
This case demonstrates how starting with empirical biomarker data and applying a systems biology workflow can yield a coherent and biologically plausible model of the MOD, moving beyond a simple list of biomarkers to an interconnected network of pathological processes.
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementing a mechanism-based biomarker discovery pipeline requires a suite of specific reagents, databases, and technological platforms.
Table: Essential Research Reagents and Resources for MOD/MOA Biomarker Research
| Category / Item | Specific Examples | Function in Workflow |
|---|---|---|
| Multi-Omics Profiling | Sequencing platforms (e.g., AVITI24), proteomic mass spectrometers, metabolomic NMR/MS [14]. | Generate the high-throughput molecular data required to model the MOD. |
| Knowledge Bases | HIPPIE (PPIs), KEGG (pathways), HMDB (metabolites) [16] [15]. | Provide curated biological knowledge to connect biomarkers into functional pathways and networks. |
| Analysis Software | Cytoscape (network visualization), DPClusO (graph clustering), R/Bioconductor packages [16] [15]. | Enable the construction, analysis, and visualization of complex biological networks. |
| Affinity Reagents | Antibodies, aptamers, somamers for multiplex assays [15]. | Critical for the targeted verification and validation of candidate biomarker panels in biological samples. |
| Clinical Assays | Digital pathology platforms, regulated LIMS (Laboratory Information Management Systems), eQMS (electronic Quality Management Systems) [14]. | Facilitate the translation of discovered biomarkers into clinical-grade, regulated diagnostic tests. |
| 2-C-methyl-D-erythritol 4-phosphate | 2-C-methyl-D-erythritol 4-phosphate, CAS:206440-72-4, MF:C5H13O7P, MW:216.13 g/mol | Chemical Reagent |
| Carteolol | Carteolol Hydrochloride | Carteolol is a non-selective beta-adrenergic antagonist for research applications. This product is For Research Use Only (RUO). Not for human or veterinary use. |
The field of biomarker discovery has undergone a profound transformation, shifting from a traditional focus on single molecules to a comprehensive multi-omics approach that integrates genomics, proteomics, and metabolomics. This paradigm shift is driven by the recognition that complex diseases cannot be adequately understood or diagnosed through single-dimensional biological measurements [2]. The convergence of these omics technologies, framed within systems biology research, enables the development of robust biomarker panels that capture the full complexity of disease mechanisms and heterogeneity [17]. Modern biomarker discovery now leverages high-throughput technologies including next-generation sequencing (NGS), advanced mass spectrometry, and nuclear magnetic resonance (NMR) spectroscopy to generate massive molecular datasets that provide unprecedented insights into disease pathophysiology [18] [19].
The integration of multi-omics data represents more than just technological advancement; it embodies a fundamental change in how researchers approach biological complexity. Where single-omics approaches provided limited, often isolated insights, integrated multi-omics reveals the emergent properties that arise from interactions across molecular layers [17]. This systems-level perspective is particularly valuable for addressing diseases with complex etiology, such as cancer, neurodegenerative disorders, and metabolic conditions, where perturbations at one molecular level create ripple effects across the entire biological network [20]. The resulting biomarker signatures therefore offer superior clinical utility for early diagnosis, prognosis, patient stratification, and therapeutic monitoring compared to traditional single-marker approaches [2] [17].
Comparative Analysis of Omics Technologies
Each omics technology provides unique insights into specific layers of biological organization, with distinct strengths, limitations, and applications in biomarker discovery. The following comparison outlines the fundamental characteristics, analytical outputs, and biomarker applications of the three primary omics technologies.
Table 1: Technology Comparison for Omics Approaches in Biomarker Discovery
| Feature | Genomics | Proteomics | Metabolomics |
|---|---|---|---|
| Analytical Target | DNA sequences and variations [21] | Proteins, polypeptides, and post-translational modifications [2] [22] | Small-molecule metabolites (<1,500 Da) [19] |
| Primary Technologies | Next-generation sequencing (NGS), microarrays [18] [21] | Mass spectrometry (LC-MS, GC-MS), SOMAmer, Olink assays [19] [23] | GC-MS, LC-MS, NMR spectroscopy [19] |
| Key Biomarker Applications | Risk prediction, hereditary markers, companion diagnostics [2] [21] | Diagnostic, prognostic, and therapeutic biomarkers [2] [23] | Diagnostic, prognostic biomarkers, treatment response [2] [19] |
| Temporal Resolution | Static (with exceptions for epigenetic changes) | Medium (minutes to hours) | High (seconds to minutes) [19] |
| Throughput Capability | Very high (whole genomes in days) [18] | Medium to high (thousands of proteins) [23] | High (hundreds of metabolites) [19] |
| Proximity to Functional Phenotype | Low (potential) | Medium (effectors) | High (functional endpoints) [19] |
Table 2: Performance Metrics in Disease-Specific Biomarker Discovery
| Disease Area | Genomics Contribution | Proteomics Contribution | Metabolomics Contribution |
|---|---|---|---|
| Cancer | Somatic mutations, copy number variations, gene fusions [18] [21] | Protein abundance, signaling pathways, tumor microenvironment [17] [21] | Altered energy metabolism (Warburg effect), oncometabolites [19] |
| Neurodegenerative Disorders | APOE ε4 carrier status, risk loci [23] | CSF and plasma tau, neurofilament light, neuroinflammation markers [23] | Energetic metabolism shifts, oxidative stress markers [19] |
| Cardiovascular Diseases | Polygenic risk scores [17] | Inflammatory cytokines, cardiac troponins, NT-proBNP [17] | Lipid species, fatty acids, acylcarnitines [19] [17] |
| Metabolic Disorders | Monogenic diabetes genes, T2D risk variants | Adipokines, inflammatory mediators [22] | Glucose, amino acids, organic acids, ketone bodies [19] |
The complementary nature of these technologies becomes evident when examining their respective positions in the central dogma of biology and their relationship to functional phenotypes. Genomics provides the blueprint of potential risk, identifying hereditary factors and predispositions that may contribute to disease development. Proteomics captures the functional effectors of biological processes, reflecting the actual machinery that executes cellular functions and responds to therapeutic interventions. Metabolomics offers the closest readout of functional phenotype, revealing the dynamic biochemical outputs that result from genomic, transcriptomic, and proteomic activity [19]. This hierarchical relationship means that integrated multi-omics approaches can connect genetic predisposition through protein function to ultimate phenotypic manifestation, providing a comprehensive view of disease mechanisms that is inaccessible to any single omics approach.
Systems Biology Approaches for Multi-Omics Integration
The true power of modern biomarker discovery emerges not from individual omics technologies but from their integration through systems biology approaches. Multi-omics integration methodologies can be categorized into three primary strategies: early, intermediate, and late integration, each with distinct advantages for specific research applications [17].
Early integration, also known as data-level fusion, combines raw data from different omics platforms before statistical analysis. This approach maximizes information preservation but requires sophisticated normalization and scaling to handle different data types and measurement scales. Methods such as principal component analysis (PCA) and canonical correlation analysis (CCA) are commonly employed to manage the computational complexity of early integration strategies [17]. Intermediate integration (feature-level fusion) first identifies important features within each omics layer, then combines these refined signatures for joint analysis. This strategy balances information retention with computational feasibility and is particularly valuable for large-scale studies where early integration might be prohibitive. Network-based methods and pathway analysis often guide feature selection in intermediate integration [17]. Late integration (decision-level fusion) performs separate analyses within each omics layer and combines the resulting predictions using ensemble methods. While potentially missing subtle cross-omics interactions, this approach provides robustness against noise in individual omics layers and allows for modular analysis workflows [17].
Table 3: Multi-Omics Integration Methodologies and Applications
| Integration Method | Key Characteristics | Optimal Use Cases | Common Algorithms/Tools |
|---|---|---|---|
| Early Integration | Combines raw data; maximal information; computationally intensive [17] | Discovery-phase analysis with sufficient sample size and computational resources [17] | PCA, CCA, MOFA [17] [21] |
| Intermediate Integration | Identifies features within layers before integration; balances complexity and information [17] | Large-scale studies; pathway-focused analysis; network biology [17] | mixOmics, network propagation, WGCNA [17] [20] |
| Late Integration | Combines results from separate analyses; robust to noise; modular workflow [17] | Clinical applications; validation studies; heterogeneous data sources [17] | Ensemble methods, weighted voting, meta-learning [17] |
| Network-Based Integration | Incorporates biological interaction knowledge; high interpretability [17] [20] | Mechanism-focused studies; therapeutic target identification [20] | Cytoscape, STRING, graph neural networks [17] [21] |
The integration of multi-omics data faces several significant technical challenges that require specialized computational approaches. Data heterogeneity arises from different data types, scales, distributions, and noise characteristics across omics platforms, necessitating sophisticated normalization strategies such as quantile normalization and z-score standardization [17]. The "curse of dimensionality" – where studies involve thousands of molecular features measured across relatively few samples – requires specialized machine learning approaches including regularization techniques like elastic net regression and sparse partial least squares [17]. Additionally, missing data and batch effects from different measurement platforms must be addressed through advanced imputation methods and batch correction approaches such as ComBat and surrogate variable analysis [17].
Multi-Omics Data Integration Workflow
Machine learning and artificial intelligence have become indispensable for multi-omics integration, with random forests and gradient boosting methods excelling at handling mixed data types and non-linear relationships common in these datasets [18] [17]. Deep learning architectures, particularly autoencoders and multi-modal neural networks, can automatically learn complex patterns across omics layers without requiring explicit integration strategies [17]. For biologically meaningful integration, network approaches model molecular interactions within and between omics layers, with graph neural networks and network propagation algorithms leveraging known biological relationships to guide multi-omics analysis [17] [20]. Tensor factorization techniques naturally handle multi-dimensional omics data by decomposing complex datasets into interpretable components, using methods such as non-negative matrix factorization (NMF) and independent component analysis (ICA) to discover novel biomarker patterns [17].
Experimental Protocols for Biomarker Validation
The validation of biomarker panels discovered through multi-omics approaches requires rigorous experimental methodologies and analytical frameworks. The following section outlines detailed protocols for biomarker verification and validation across different omics technologies, with emphasis on systems biology approaches.
Proteomic Biomarker Validation Protocol
The Global Neurodegeneration Proteomics Consortium (GNPC) has established one of the most comprehensive proteomic biomarker validation frameworks, analyzing approximately 250 million unique protein measurements from over 35,000 biofluid samples [23]. Their large-scale validation protocol involves:
Sample Preparation: Plasma, serum, and cerebrospinal fluid (CSF) samples are collected using standardized protocols across multiple clinical sites. Samples undergo protein extraction and quantification with quality control measures including protein concentration assessment and integrity verification [23].
Multi-Platform Proteomic Profiling: Each sample is analyzed using complementary technologies:
- SOMAmer-based Capture Array (SomaScan versions 3, 4, and 4.1): Measures between 1,300 and 7,000 unique protein aptamers per biosample to ensure broad proteome coverage [23].
- Olink Proximity Extension Assay: Provides complementary protein quantification with high specificity and sensitivity [23].
- Tandem Mass Tag Mass Spectrometry: Applied to a subset of samples (1,975 samples in GNPC V1) for cross-platform validation and identification of protein isoforms and post-translational modifications [23].
Data Harmonization and Quality Control: Data from multiple platforms and cohorts are aggregated and harmonized using the Alzheimer's Disease Data Initiative's AD Workbench, a secure cloud-based environment that satisfies GDPR and HIPAA requirements [23].
Differential Abundance Analysis: Statistical analysis identifies disease-specific differential protein abundance using linear mixed-effects models that account for covariates including age, sex, and technical variables [23].
Transdiagnostic Signature Identification: Machine learning algorithms (including regularized regression and ensemble methods) identify proteomic signatures that transcend traditional diagnostic boundaries, revealing shared pathways across neurodegenerative conditions [23].
Metabolomic Biomarker Workflow
Metabolomic biomarker validation employs both targeted and untargeted approaches, with specific protocols tailored to the analytical technology:
Sample Preparation for Mass Spectrometry:
- Liquid Chromatography-Mass Spectrometry (LC-MS): Proteins are precipitated from biofluids using cold organic solvents (typically methanol or acetonitrile). The supernatant is dried under nitrogen and reconstituted in mobile phase compatible solvents [19].
- Gas Chromatography-Mass Spectrometry (GC-MS): Metabolites undergo derivatization using methoxyamine hydrochloride and N-Methyl-N-(trimethylsilyl)trifluoroacetamide (MSTFA) to increase volatility and thermal stability [19].
Instrumental Analysis:
- LC-MS Analysis: Utilizes reversed-phase chromatography with gradient elution coupled to high-resolution mass spectrometers (Q-TOF or Orbitrap instruments). Electrospray ionization (ESI) is applied in both positive and negative ionization modes to maximize metabolite coverage [19].
- GC-MS Analysis: Employes capillary GC columns with temperature ramping, coupled to electron impact (EI) or chemical ionization (CI) sources. Mass detection typically uses quadrupole or time-of-flight (TOF) analyzers [19].
- NMR Spectroscopy: Requires minimal sample preparation, with biofluids typically diluted in deuterated solvents. 1D ^1H NMR spectra are acquired with water suppression, and 2D experiments (J-resolved, COSY, HSQC) are used for metabolite identification [19].
Data Processing and Metabolite Identification:
- Raw data from MS platforms undergo peak detection, alignment, and normalization using software such as XCMS, MZmine, or Progenesis QI [19].
- Multivariate statistical analysis including principal component analysis (PCA) and partial least squares-discriminant analysis (PLS-DA) identifies differentially abundant metabolites [19].
- Metabolite identification is performed by matching accurate mass, retention time, and fragmentation spectra to authentic standards in databases such as HMDB, MetLin, or NIST [19].
Cross-Omics Validation Framework
Systems biology approaches for validating integrated biomarker panels require specialized computational and statistical frameworks:
Network-Based Integration: Biomarker candidates from individual omics layers are mapped onto biological networks including protein-protein interaction networks, metabolic pathways, and gene regulatory networks using platforms such as Cytoscape, STRING, or custom pipelines like ADOPHIN [20] [21]. This approach identifies topologically important nodes with regulatory significance across multiple molecular layers [20].
Machine Learning Validation: Multi-omics biomarker signatures are validated using nested cross-validation approaches to prevent overfitting. The process includes:
- Feature selection using regularization methods (LASSO, elastic net) to identify the most predictive biomarkers from the high-dimensional multi-omics data [17] [21].
- Model training with algorithms including random forests, support vector machines, or gradient boosting machines optimized for mixed data types [17] [21].
- Performance assessment using receiver operating characteristic (ROC) analysis, calibration curves, and decision curve analysis to evaluate clinical utility [17].
Independent Cohort Validation: Biomarker panels are validated in external cohorts to assess generalizability. The GNPC framework, for example, validates proteomic signatures across 23 independent cohorts comprising over 18,000 participants [23].
Systems Biology Validation Framework
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful implementation of omics technologies for biomarker discovery requires specialized reagents, platforms, and computational tools. The following table summarizes essential resources for multi-omics biomarker research.
Table 4: Essential Research Reagents and Platforms for Omics Biomarker Discovery
| Category | Specific Tools/Platforms | Primary Applications | Key Features |
|---|---|---|---|
| Sequencing Platforms | Illumina NovaSeq X [18], Oxford Nanopore [18] | Whole genome sequencing, targeted gene panels, epigenomics | High-throughput, long-read capabilities, methylation detection [18] |
| Proteomic Technologies | SomaScan [23], Olink [23], LC-MS/MS [19] [23] | High-throughput protein quantification, post-translational modifications | High plex capacity (7,000 proteins), high sensitivity, isoform resolution [23] |
| Metabolomic Platforms | GC-MS [19], LC-MS [19], NMR [19] | Untargeted and targeted metabolite profiling, metabolic pathway analysis | Broad metabolite coverage, structural elucidation, quantitative accuracy [19] |
| Bioinformatics Tools | GATK [21], DESeq2 [21], MaxQuant [21], mixOmics [17] | Variant calling, differential expression, multi-omics integration | Industry-standard pipelines, specialized for omics data types [17] [21] |
| Multi-Omics Integration | MOFA [17], Cytoscape [21], cBioPortal [21] | Data integration, network visualization, interactive exploration | Factor analysis, biological network integration, user-friendly interface [17] [21] |
| Preclinical Models | Patient-derived organoids [24], PDX models [24] | Biomarker validation, therapeutic response assessment | Clinically relevant biology, patient-specific responses [24] |
| Diclobutrazol | Diclobutrazol, CAS:66345-62-8, MF:C15H19Cl2N3O, MW:328.2 g/mol | Chemical Reagent | Bench Chemicals |
| Apricitabine | Apricitabine, CAS:143338-12-9, MF:C8H11N3O3S, MW:229.26 g/mol | Chemical Reagent | Bench Chemicals |
Cloud computing platforms have become essential infrastructure for multi-omics biomarker discovery, with services including Amazon Web Services (AWS), Google Cloud Genomics, and Microsoft Azure providing scalable resources for data storage and analysis [18]. These platforms offer specialized solutions for genomic data analysis while ensuring compliance with regulatory requirements such as HIPAA and GDPR [18]. The implementation of FAIR (Findable, Accessible, Interoperable, Reusable) data principles is particularly important for multi-omics research, facilitating data sharing and method comparison through standardized approaches to data generation, processing, and analysis [17].
Specialized computational tools have been developed specifically for multi-omics integration, with packages such as mixOmics providing statistical frameworks for integration, MOFA (Multi-Omics Factor Analysis) enabling dimensionality reduction across omics layers, and MultiAssayExperiment facilitating data management for complex multi-omics datasets [17]. For network-based integration, platforms including Cytoscape, STRING, and ADOPHIN enable mapping of multi-omics data onto biological networks to identify topologically important nodes with regulatory significance [20] [21].
The integration of genomics, proteomics, and metabolomics through systems biology approaches represents the future of biomarker discovery and validation. While each omics technology provides valuable insights individually, their integration creates synergistic value that far exceeds the sum of their parts. Multi-omics biomarker signatures have demonstrated superior performance across multiple disease areas, with integrated approaches significantly outperforming single-biomarker methods and achieving diagnostic accuracies exceeding 95% in some neurodegenerative disease studies [17] [23]. The transition from single-omics to multi-omics approaches reflects an evolving understanding of disease as a systems-level phenomenon that manifests through coordinated changes across molecular scales.
Despite these advances, significant challenges remain in translating multi-omics biomarker panels into clinically actionable tools. Regulatory agencies are developing specific frameworks for evaluating multi-omics biomarkers, with emphasis on analytical validation, clinical utility, and cost-effectiveness demonstration [17]. The successful clinical implementation of these complex signatures requires careful consideration of workflow integration, staff training, and technology infrastructure [17]. Future directions in the field include the development of single-cell multi-omics technologies that resolve cellular heterogeneity, advanced AI and machine learning algorithms for pattern recognition in high-dimensional data, and streamlined regulatory pathways for biomarker panel qualification [17] [21]. As these technologies mature and integration methodologies become more sophisticated, multi-omics biomarker panels will increasingly guide personalized therapeutic strategies, enhance clinical trial design, and ultimately improve patient outcomes across a broad spectrum of diseases.
Pancreatic Ductal Adenocarcinoma (PDAC) is a devastating malignancy, projected to become the third leading cause of global cancer deaths, with a five-year survival rate below 7% for most patients [25] [26]. The poor prognosis stems primarily from late-stage diagnosis, with only 10-20% of patients presenting with surgically resectable disease at detection [27] [25]. Carbohydrate antigen 19-9 (CA19-9) remains the most widely used serum biomarker but suffers from limited specificity (68-91%) and sensitivity (70-90%), with elevated levels also occurring in various benign conditions such as chronic pancreatitis [27] [25]. Furthermore, CA19-9 is ineffective in Lewis antigen-negative populations, potentially leading to misdiagnosis in up to 30% of PDAC patients [25]. These critical limitations have driven the search for more reliable diagnostic biomarkers, particularly those capable of detecting PDAC at earlier, more treatable stages.
Autoantibodies (AAbs) have emerged as promising biomarker candidates due to their early appearance in disease pathogenesis, stability in serum, and ability to report on underlying cellular perturbations within the tumor microenvironment [25] [28]. The immune system produces AAbs against tumor-associated antigens (TAAs) that arise from aberrant protein expression, mutations, or abnormal post-translational modifications in cancer cells [29]. Cancer-testis (CT) antigens are particularly attractive targets, as they exhibit highly restricted expression in normal adult tissues but are aberrantly expressed in various cancers, potentially triggering detectable humoral immune responses [25]. This case study examines the discovery and validation of a novel autoantibody panel for PDAC detection, contextualized within a systems biology framework for biomarker validation.
Experimental Design and Workflow
Study Populations and Cohort Design
The discovery and validation of the AAb panel followed a multi-phase approach involving independent patient cohorts [25]. The training cohort comprised 94 individuals, including 19 PDAC patients (Stage II-III), 20 chronic pancreatitis (CP) patients, 1 other pancreatic cancer (PC) patient, 13 dyspeptic ulcer (DYS) patients, 7 healthy controls (HCs), plus 18 additional PC and 16 prostate cancer (PRC) samples from collaborating institutions. This diverse training set enabled initial biomarker identification while assessing specificity against confounding conditions.
The validation cohort included 223 samples to rigorously evaluate clinical utility: 98 PDAC (Stage II-III), 65 other pancreatic cancers (Stage II-III), 20 prostate cancers (PRC), 16 colorectal cancers (CRC), and 24 healthy controls. This expansive validation design allowed assessment of diagnostic performance across multiple comparison scenarios: PDAC versus healthy controls, PDAC versus benign pancreatic conditions, and PDAC versus other cancer types [25].
Table 1: Study Cohort Demographics and Clinical Characteristics
| Cohort | PDAC | Chronic Pancreatitis | Other Pancreatic Cancers | Other Cancers | Healthy Controls | Dyspepsia |
|---|---|---|---|---|---|---|
| Training | 19 | 20 | 19 | 16 (prostate) | 7 | 13 |
| Validation | 98 | - | 65 | 36 (20 prostate, 16 colorectal) | 24 | - |
High-Throughput Autoantibody Profiling Technology
CT100+ Protein Microarray Fabrication
The core discovery platform utilized a custom CT100+ protein microarray containing 113 cancer-testis or tumor-associated antigens [25]. These antigen lysates were diluted two-fold with 40% sucrose and printed in a 4-plex format (four replica arrays per slide) on streptavidin-coated hydrogel microarray substrates. Within each array, antigens were printed in technical triplicate to ensure measurement reliability. Following printing, slides were incubated in blocking buffer for one hour at room temperature before serological application.
Serum Processing and Hybridization
Blood samples were collected from all participants and processed under standardized conditions [25]. Serum was isolated by centrifugation at 1500 × g for 15 minutes at 22°C, followed by a second centrifugation at 3500 × g for 15 minutes to remove platelets. The supernatant was aliquoted into polypropylene tubes and stored at -80°C until analysis. For hybridization, serum samples were applied to the microarrays to detect autoantibodies bound to specific antigens, with subsequent detection using fluorescently labeled secondary antibodies.
Biomarker Identification and Validation Workflow
The overall research strategy followed a comprehensive workflow from discovery through validation:
Results: Diagnostic Performance of the Autoantibody Panel
Optimal Autoantibody Panel Identification
Combinatorial ROC curve analysis of the training cohort data identified an optimal seven-autoantibody panel comprising CEACAM1, DPPA2, DPPA3, MAGEA4, SRC, TPBG, and XAGE3 [25] [26]. This combination demonstrated robust diagnostic performance with an area under the curve (AUC) of 85.0%, sensitivity of 82.8%, and specificity of 68.4% for distinguishing PDAC from controls in the training cohort.
Differential expression analysis further identified four additional biomarkers (ALX1, GPA33, LIP1, and SUB1) that were upregulated in PDAC against both diseased and healthy controls [25]. These were incorporated into an expanded 11-AAb panel for subsequent validation studies. The identified AAbs were further validated using public immunohistochemistry datasets and experimentally confirmed using a custom PDAC protein microarray containing the 11 optimal AAb biomarkers.
Validation Performance Across Multiple Comparison Scenarios
The clinical utility of the biomarker panel was rigorously assessed in the independent validation cohort of 223 samples [25]. The results demonstrated consistently strong performance across multiple clinically relevant scenarios:
Table 2: Diagnostic Performance of AAb Panel in Validation Cohort
| Comparison Scenario | AUC | Sensitivity | Specificity | Key Clinical Utility |
|---|---|---|---|---|
| PDAC vs Healthy Controls | 80.9% | - | - | Distinguishing cancer from healthy individuals |
| PDAC vs Other Pancreatic Cancers | 70.3% | - | - | Subtype differentiation within pancreatic malignancies |
| PDAC vs Colorectal Cancer | 84.3% | - | - | Specificity against gastrointestinal cancers |
| PDAC vs Prostate Cancer | 80.2% | - | - | Specificity against non-GI malignancies |
The specific seven-autoantibody combination (CEACAM1-DPPA2-DPPA3-MAGEA4-SRC-TPBG-XAGE3) maintained its performance in the validation cohort with an AUC of 85.0%, confirming the robustness of the initial findings [25] [26].
Comparative Performance Against Existing Biomarkers
When compared to the current clinical standard, CA19-9, the autoantibody panel demonstrated complementary strengths. A separate study developing a serum protein biomarker panel using machine learning approaches reported that while CA19-9 alone achieved an AUROC of 0.952 for detecting PDAC across all stages, this performance dropped to 0.868 for early-stage PDAC [27]. Their machine learning-integrated protein panel (including CA19-9, GDF15, and suPAR as key biomarkers) significantly outperformed CA19-9 alone, achieving AUROCs of 0.992 for all-stage PDAC and 0.976 for early-stage PDAC [27].
Another independent study identified a different three-AAb panel (anti-HEXB, anti-TXLNA, anti-SLAMF6) that achieved AUCs of 0.81 for distinguishing PDAC from normal controls and 0.80 for distinguishing PDAC from benign pancreatic diseases [28]. Notably, when this immunodiagnostic model was combined with CA19-9, the positive rate of PDAC detection increased to 92.91%, suggesting synergistic value in combining autoantibody panels with existing protein biomarkers [28].
Systems Biology Framework for Biomarker Validation
Biological Plausibility and Pathway Analysis
The validation of biomarker panels within a systems biology framework requires establishing biological plausibility beyond statistical associations [2]. The identified autoantibodies in the PDAC panel target antigens with established roles in oncogenic processes. For instance, MAGEA4 belongs to the cancer-testis antigen family with highly restricted expression in normal tissues but aberrant expression in various cancers [25]. SRC is a proto-oncogene involved in multiple signaling pathways regulating cell proliferation, differentiation, and survival. CEACAM1 (carcinoembryonic antigen-related cell adhesion molecule 1) participates in cell adhesion and signaling processes frequently dysregulated in malignancies.
A biological function-based optimization process, as demonstrated in sepsis biomarker development, can strengthen panel validation by ensuring selected biomarkers represent core dysregulated biological processes in the disease [30]. This approach operates on the premise that highly correlated genes involved in the same biological processes share similar discriminatory power, allowing for substitution of poorly performing biomarkers with functionally equivalent alternatives without compromising diagnostic performance.
Integration with Multi-Omics Approaches
Systems biology integrates multiple data types across genomics, transcriptomics, epigenomics, and proteomics to identify optimal biomarker combinations [27] [2]. The rising importance of this approach is reflected in the shift from single-marker to multi-marker panels, which offer higher robustness and separation power for clinical tests [2]. Autoantibody panels represent one component within this multi-omics landscape, with each biomarker class offering distinct advantages:
Table 3: Multi-Omics Biomarker Classes in PDAC Detection
| Biomarker Class | Common Applications | Advantages | Limitations |
|---|---|---|---|
| Genomic (DNA) | Risk prediction, therapy selection | Stable molecules, well-established protocols | Limited dynamic range, may not reflect current disease state |
| Transcriptomic (RNA) | Diagnosis, prognosis, physiological states | Dynamic response, pathway information | Technical variability, sample stability issues |
| Proteomic (Proteins) | Diagnosis, prognosis, treatment monitoring | Direct functional molecules, post-translational modifications | Measurement complexity, dynamic range challenges |
| Autoantibodies (AAbs) | Early detection, diagnosis | Early emergence, persistence, stability, specificity | Variable frequency in patient populations |
Analytical Validation Considerations
The transition from discovery to clinically applicable assays presents technical challenges, particularly when moving between measurement platforms [30]. The biological function-based optimization approach has demonstrated that substituting poorly performing features with biologically equivalent alternatives can maintain diagnostic performance while facilitating platform transition [30]. This principle supports the robustness of the identified AAb panel across different experimental conditions and measurement technologies.
Research Reagent Solutions for AAb Biomarker Studies
The experimental workflow for autoantibody biomarker discovery and validation requires specialized reagents and platforms. The following table outlines key research solutions employed in these studies:
Table 4: Essential Research Reagents for Autoantibody Biomarker Studies
| Research Reagent | Specific Example | Function in Experiment | Application in PDAC AAb Study |
|---|---|---|---|
| Protein Microarray | CT100+ custom microarray [25] | High-throughput AAb profiling | Screening of 113 CT antigens against serum samples |
| Protein Microarray | HuProt Human Proteome Microarray [28] | Comprehensive proteome-wide AAb detection | Identification of 167 candidate TAAbs in discovery phase |
| Antigen Substrates | Recombinant CT antigens [25] | Target for AAb binding | CEACAM1, DPPA2, DPPA3, MAGEA4, SRC, TPBG, XAGE3 |
| Detection Antibodies | HRP-labeled anti-human IgG [28] | Secondary detection of bound AAbs | ELISA validation of identified TAAbs |
| Assay Platform | Luminex xMAP immunoassays [27] | Multiplex protein quantification | Validation of protein biomarkers in parallel studies |
| Sample Processing | Streptavidin-coated hydrogel substrates [25] | Microarray surface chemistry | Fabrication of protein microarrays for AAb screening |
This case study demonstrates that autoantibody panels represent promising diagnostic biomarkers for PDAC, with the identified 7-AAb panel (CEACAM1-DPPA2-DPPA3-MAGEA4-SRC-TPBG-XAGE3) achieving 85.0% AUC in independent validation [25] [26]. The performance across multiple comparison scenarios (PDAC vs. healthy controls: 80.9% AUC; PDAC vs. other cancers: 70.3-84.3% AUC) indicates robust discriminatory capability [25].
The systems biology framework for biomarker validation emphasizes the importance of biological plausibility, multi-omics integration, and analytical robustness [2] [30]. The biological relevance of the target antigens strengthens the case for the clinical potential of this AAb panel. Furthermore, evidence from multiple studies suggests that combining autoantibody signatures with existing biomarkers like CA19-9 can significantly enhance detection rates [28] [31], with one meta-analysis reporting that certain AAb combinations with CA19-9 achieved 100% sensitivity and 92% specificity [31].
Future development of this AAb panel should focus on validation in broader screening populations, including high-risk individuals, and further refinement through integration with other biomarker classes within a comprehensive multi-omics strategy. The transition to clinically applicable assays will benefit from continued optimization based on biological principles to maintain performance while improving feasibility for routine clinical implementation.
Building the Validation Pipeline: Integrating Experimental and Computational Workflows
The validation of biomarker panels is a cornerstone of systems biology research, providing critical insights into disease mechanisms and potential therapeutic targets. Within this framework, high-throughput proteomic technologies are indispensable for the simultaneous identification and quantification of numerous candidate biomarkers. Protein microarrays and mass spectrometry have emerged as two leading platforms, each with distinct operational principles, strengths, and limitations. Protein microarrays, featured as miniaturized, parallel assay systems, enable the high-throughput analysis of thousands of proteins from minute sample volumes [32]. Their design is ideally suited for profiling complex biological systems. Mass spectrometry (MS), conversely, offers antibody-independent quantification of proteins, often with high specificity and the ability to detect post-translational modifications [33] [34]. This guide provides an objective comparison of these platforms, focusing on their performance in biomarker quantification and their role in validating biomarker panels within systems biology.
Protein Microarray Platforms
Protein microarrays are characterized by their high-density format, where hundreds to thousands of proteins or capture agents are immobilized on a solid surface in a miniaturized layout [32] [35]. According to their application and design, they are primarily categorized into three types.
Analytical Microarrays: These arrays use defined capture agents, such as antibodies, immobilized on the surface to detect proteins from a complex sample. They are primarily used for protein expression profiling and biomarker detection [35]. A key advantage is their high sensitivity and suitability for clinical applications, though they can be limited by the availability and quality of specific antibodies [35].
Reverse Phase Protein Arrays (RPPA): In RPPA formats, the samples themselves (such as cell or tissue lysates) are printed onto the array surface. These are then probed with specific antibodies against the target proteins [32] [35]. This method is particularly powerful for signaling pathway analysis and monitoring post-translational modifications (e.g., phosphorylation) from minimal sample material, making it valuable for personalized medicine approaches [32] [35]. Its main limitation is the number of analytes that can be measured, restricted by the availability of specific and validated antibodies [35].
Functional Protein Microarrays: These are constructed with full-length proteins or protein domains and are used to study a wide range of biochemical activities, including protein-protein, protein-lipid, and protein-drug interactions [32] [35]. A prominent subtype is the proteome microarray, which contains most or all of an organism's proteins, enabling unbiased discovery research [32]. For instance, yeast proteome microarrays have been successfully used for a large-scale "Phosphorylome Project," identifying thousands of kinase-substrate relationships [32].
Mass Spectrometry Platforms
Mass spectrometry-based proteomics does not rely on pre-defined capture molecules and can provide absolute quantification of proteins. It is typically divided into discovery and targeted workflows.
Discovery Proteomics (DIA/DDA): These untargeted or data-independent acquisition methods aim to measure as many proteins as possible in a single run. Advanced platforms, such as those using nanoparticle-based enrichment (e.g., Seer Proteograph) or high-abundance protein (HAP) depletion (e.g., Biognosys TrueDiscovery), have significantly increased coverage of the plasma proteome, identifying thousands of proteins [34]. These methods are ideal for initial biomarker discovery but can be challenged by the wide dynamic range of protein concentrations in biofluids like plasma [34].
Targeted Proteomics (e.g., PRM, SRM): Targeted methods, such as Parallel Reaction Monitoring (PRM) or Selected Reaction Monitoring (SRM), focus on precise quantification of a pre-selected set of proteins [33] [36]. These are considered a "gold standard" for verification and validation due to high reliability, reproducibility, and absolute quantification via internal standards [34] [36]. A key application is the multiplexed quantification of specific biomarker panels, such as phosphorylated tau proteins in Alzheimer's disease [33].
Direct Performance Comparison
The table below summarizes a direct comparison of key performance metrics for protein microarray and mass spectrometry platforms, based on data from recent studies.
Table 1: Performance Comparison of Proteomic Platforms
| Performance Metric | Analytical Protein Microarray | Reverse Phase Protein Array (RPA) | Discovery Mass Spectrometry | Targeted Mass Spectrometry |
|---|---|---|---|---|
| Throughput | High | High | Moderate | High for targeted panels |
| Multiplexing Capacity | Hundreds to thousands of targets | Limited by antibody availability | >5,000 proteins per run [34] | Dozens to hundreds of targets |
| Sample Consumption | Low (1-2 µL) [37] | Very low | Moderate | Low to moderate |
| Sensitivity | High (depends on antibody) | High (depends on antibody) | Moderate to High (platform-dependent) | Very High (fmol/mL range) [33] |
| Quantification Type | Relative (fluorescence) | Relative (fluorescence) | Relative or Absolute | Absolute with internal standards [34] |
| Key Advantage | High-throughput, established workflows | Ideal for phospho-signaling analysis | Unbiased, broad proteome coverage | High specificity and accuracy |
| Key Limitation | Dependent on antibody quality/availability | Limited analyte number | Complex data analysis, dynamic range challenges | Requires pre-selection of targets |
A 2024 study directly compared immunoassay-based (a form of analytical microarray) and mass spectrometry-based quantification of phosphorylated tau (p-tau) biomarkers for Alzheimer's disease [33]. The results showed that for p-tau217, mass spectrometry and immunoassays were highly comparable in diagnostic performance, effect sizes, and associations with PET biomarkers [33]. However, for p-tau181 and p-tau231, antibody-free mass spectrometry exhibited slightly lower performance compared to established immunoassays [33]. This underscores that performance can be analyte-specific.
A broader 2025 comparison of eight plasma proteomics platforms further highlights trade-offs. Affinity-based platforms like SomaScan (11K assays) and Olink (5K assays) offer exceptional throughput and sensitivity, measuring thousands of proteins from small samples [34]. Mass spectrometry platforms, while sometimes offering lower coverage, provide unique advantages in specificity (by measuring multiple peptides per protein) and independence from binding reagent availability [34].
Experimental Protocols and Workflows
Protein Microarray Workflow: Serological Biomarker Discovery
A standard protocol for identifying serological biomarkers using a functional proteome microarray is exemplified by work with the vaccinia virus [37].
- Step 1: Microarray Fabrication. The process begins with the PCR amplification of all open reading frames (ORFs) from the pathogen's genome. These ORFs are cloned into an expression system, such as baculovirus, to produce full-length, GST-tagged recombinant proteins. Proteins are then affinity-purified and printed in a high-density format onto nitrocellulose-coated glass slides [37].
- Step 2: Probing and Assay. The microarray is incubated with a diluted serum sample (e.g., from infected or vaccinated individuals). After washing to remove unbound components, target antibodies bound to arrayed antigens are detected using a fluorophore-conjugated secondary antibody (e.g., anti-human IgG) [37].
- Step 3: Data Acquisition and Analysis. The array is scanned with a confocal laser scanner (e.g., GenePix) to generate a quantitative fluorescence image. Signal intensities are extracted, and antigens with significant reactivity are identified by comparing to control sera [37]. This workflow successfully identified a small subset of the vaccinia proteome that was consistently recognized by antibodies from immune individuals [37].
Mass Spectrometry Workflow: Quantification of CSF Biomarkers
A detailed protocol for mass spectrometry-based quantification of biomarkers in cerebrospinal fluid (CSF) was used in a 2024 study comparing p-tau biomarkers [33].
- Step 1: Sample Preparation. A CSF sample (250 µL) is spiked with a known amount of heavy isotope-labeled peptide standards (AQUA peptides) for absolute quantification. Proteins are precipitated using perchloric acid, which leaves tau protein in the supernatant. The supernatant is then processed using solid-phase extraction (SPE) to purify the peptides [33].
- Step 2: Digestion and LC-MS/MS Analysis. The extracted proteins are reconstituted and digested with trypsin overnight at 37°C to generate peptides. The resulting peptides are separated by liquid chromatography (LC) and analyzed by a high-resolution mass spectrometer (e.g., Hybrid Orbitrap) operated in Parallel Reaction Monitoring (PRM) mode for targeted quantification [33].
- Step 3: Data Processing. The LC-MS data is processed using software like Skyline. The quantification is achieved by comparing the peak areas of the native target peptides to the peak areas of their corresponding heavy labeled internal standards. This allows for the precise calculation of the concentration of specific p-tau variants (e.g., p-tau181, p-tau217) [33].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of experiments using these high-throughput platforms requires specific, high-quality reagents and materials. The following table details key solutions used in the featured protocols.
Table 2: Essential Research Reagent Solutions for Biomarker Quantification
| Item | Function | Example Use Case |
|---|---|---|
| Recombinant Proteins | Serve as immobilized antigens or quantitative standards. | Fabrication of functional proteome microarrays for pathogen immunoprofilng [37]. |
| Heavy Isotope-Labeled Peptide Standards (AQUA) | Enable absolute quantification by mass spectrometry; act as internal controls. | Precise measurement of p-tau181, p-tau217, and p-tau231 concentrations in CSF [33]. |
| Specific Antibodies | Act as capture (analytical microarray) or detection (RPA) agents. | Probing reverse-phase protein arrays to analyze cell signaling pathways [32] [35]. |
| Fluorophore-Conjugated Secondary Antibodies | Detect target binding interactions on microarrays via fluorescence. | Visualizing human IgG binding to viral antigens on a proteome microarray [37]. |
| Cell-Free Expression System | Enables on-site protein synthesis for functional microarrays. | Used in NAPPA (Nucleic Acid Programmable Protein Array) to produce proteins directly on the slide [35]. |
| Nitrocellulose-Coated Slides | Provide a high-binding-capacity surface for protein immobilization. | Standard substrate for printing protein microarrays to ensure optimal protein retention [37]. |
| Solid-Phase Extraction (SPE) Plates | Purify and concentrate peptides from complex biological samples prior to MS. | Sample clean-up in the mass spectrometry workflow for CSF biomarkers [33]. |
| Oleandrigenin | Oleandrigenin, CAS:465-15-6, MF:C25H36O6, MW:432.5 g/mol | Chemical Reagent |
| Hydroxynybomycin | Hydroxynybomycin, CAS:63582-81-0, MF:C16H14N2O5, MW:314.29 g/mol | Chemical Reagent |
Both protein microarrays and mass spectrometry are powerful platforms for biomarker quantification, each occupying a complementary niche in the systems biology workflow. The choice between them depends on the specific research question, the required throughput, the need for antibody-independent validation, and the available sample type and volume. Protein microarrays excel in high-throughput, targeted screening of known antigens or antibodies, making them ideal for comprehensive immunoprofiling and signaling network analysis. Mass spectrometry offers unparalleled specificity and the ability to perform unbiased discovery and absolute quantification without antibodies, which is crucial for validating novel biomarker panels.
Within the broader thesis of validating biomarker panels using systems biology, these technologies are not mutually exclusive but are increasingly used in concert. A discovery phase using broad proteome microarrays or discovery MS can identify a candidate biomarker panel, which is then transitioned to a robust, targeted MS or analytical microarray platform for high-throughput validation in larger clinical cohorts [32] [36]. This integrated, multi-platform approach leverages the respective strengths of each technology to build a systems-level understanding of disease pathophysiology and to translate proteomic discoveries into clinically actionable diagnostic tools.
The Role of Selected Reaction Monitoring (SRM) for Targeted Biomarker Validation
In the framework of systems biology, the validation of biomarker panels is a critical step in translating complex molecular discoveries into clinically actionable tools. Selected Reaction Monitoring (SRM), also referred to as Multiple Reaction Monitoring (MRM), is a targeted mass spectrometry technique that has established itself as a cornerstone for precise, sensitive, and reproducible protein quantification in complex biological mixtures [38] [39]. This technique provides the rigorous analytical validation required to confirm the presence and concentration of candidate biomarkers, moving beyond discovery-phase findings to generate highly reliable data suitable for downstream clinical application and drug development.
SRM operates on triple quadrupole mass spectrometers, where it isolates a specific precursor ion from a target peptide in the first quadrupole (Q1), fragments it in the second quadrupole (q2), and monitors one or more predefined fragment ions (transitions) in the third quadrupole (Q3) [39]. This targeted detection method minimizes background interference, resulting in exceptional sensitivity and quantitative accuracy. For systems biology research, which seeks to understand biological systems as integrated networks, SRM offers a powerful method for validating multiplexed biomarker panels across diverse sample types, from plasma and tissue to microsamples [40]. Its ability to absolutely quantify dozens of proteins simultaneously in a single run makes it ideally suited for verifying systems-level hypotheses and validating molecular signatures identified through untargeted omics approaches.
SRM vs. Alternative Targeted MS Techniques
Technical Comparison of SRM and PRM
While SRM is a well-established workhorse for targeted quantification, Parallel Reaction Monitoring (PRM) has emerged as a powerful alternative leveraging high-resolution mass spectrometry. Understanding their distinct technical profiles enables researchers to select the optimal approach for specific biomarker validation projects.
Table 1: Core Technical Comparison of SRM and PRM
| Feature | SRM/MRM | PRM |
|---|---|---|
| Instrumentation | Triple Quadrupole (QQQ) | Orbitrap, Q-TOF |
| Resolution | Unit Resolution | High (HRAM) |
| Fragment Ion Monitoring | Predefined transitions (e.g., 3-5) | Full MS/MS spectrum (all fragments) |
| Selectivity | Moderate | High (less interference) |
| Sensitivity | Very High | High, depending on resolution |
| Throughput | High | Moderate |
| Method Development | Requires transition tuning & optimization | Quick, minimal optimization |
| Data Reusability | No | Yes (retrospective analysis) |
| Best Applications | High-throughput screening, routine quantification of validated panels | Low-abundance targets, PTM analysis, novel biomarker validation |
SRM excels in high-throughput environments where robust, sensitive, and cost-effective quantification of well-characterized targets is required. Its strength lies in monitoring predefined transitions, making it exceptionally fast and sensitive for applications like clinical diagnostics and pharmacokinetic studies [39]. However, this predefined nature means that if interference occurs or better transitions are identified later, the experiment must be re-run.
In contrast, PRM's key advantage is post-acquisition flexibility. By recording the complete fragment ion spectrum, researchers can retrospectively re-analyze data to quantify different peptides, confirm identities with greater confidence, or address new questions without re-acquiring samples [41] [39]. This makes PRM particularly valuable for validating low-abundance biomarkers, analyzing post-translational modifications, and working in complex matrices where interference may be a concern.
Performance and Experimental Data
The performance characteristics of these techniques directly influence experimental design and data quality in biomarker validation.
Table 2: Comparative Performance Metrics in Biomarker Validation
| Performance Metric | SRM/MRM | PRM | Experimental Context |
|---|---|---|---|
| Precision (Typical CV) | <10-15% [38] | Comparable to SRM when optimized [41] | Reproducibility in complex samples |
| Multiplexing Capacity | High (100s of targets) [38] | Moderate (10s-100s of targets) [39] | Number of proteins quantifiable in single run |
| Limit of Quantification | Attomole to low femtomole range | Femtomole range [39] | Sensitivity in standard workflows |
| Dynamic Range | 4-5 orders of magnitude [38] | 4-5 orders of magnitude | Plasma proteome coverage |
| Interference Resistance | Moderate (requires careful transition optimization) | High (HRAM resolves isobaric interference) [39] | Analysis in complex matrices like plasma |
Recent technological advancements continue to push these boundaries. For instance, novel hybrid instruments like the Stellar MS aim to combine the robustness of triple quadrupoles with the enhanced capabilities of advanced ion traps, allowing for extremely rapid and sensitive PRM assays [41]. Such developments are progressively bridging the historical gap between the high throughput of SRM and the superior specificity of PRM.
Experimental Protocols for SRM-Based Biomarker Validation
Sample Preparation and Experimental Workflow
Robust sample preparation is fundamental to successful SRM validation. Variations in pre-analytical steps are a major source of irreproducibility in biomarker studies.
Key Steps in Sample Processing:
- Sample Collection: Depending on the study, samples may include plasma, serum, tissue lysates, or microsamples (e.g., dried blood spots). Consistent collection protocols are critical [40].
- High-Abundancy Protein Depletion: For plasma/serum samples, immunodepletion of top abundant proteins (e.g., albumin, immunoglobulins) is often performed to enhance detection of lower-abundance biomarkers [42].
- Protein Digestion: Proteins are denatured, reduced, alkylated, and digested typically with trypsin to generate peptides. Using stable isotope-labeled standard (SIS) peptides added at this point corrects for variability in digestion efficiency and downstream processing [38].
- Peptide Cleanup: Desalting and cleanup of digested peptides using solid-phase extraction (e.g., C18 tips or columns) removes interfering salts and buffers.
Diagram 1: SRM Biomarker Validation Workflow. SIS: Stable Isotope-labeled Standard.
SRM Assay Development and Statistical Analysis
Developing a robust SRM assay involves selecting the best proteotypic peptides and optimizing mass spectrometric parameters.
Transition Selection and Optimization:
- Peptide Selection: Choose peptides unique to the target protein, typically 7-15 amino acids long, that exhibit good chromatographic behavior and ionization efficiency.
- Transition Optimization: For each peptide, 3-5 optimal precursor-fragment ion pairs (transitions) are empirically selected and optimized for collision energy. This process can be facilitated by tools like Skyline [38].
Statistical Significance Analysis: Proper statistical analysis is crucial to distinguish true biological changes from experimental variation. The process involves:
- Data Normalization: Correcting for technical variation using internal standards.
- Linear Mixed-Effects Models: As implemented in tools like SRMstats, these models appropriately combine quantitative measurements across peptides, transitions, and samples to determine protein-level significance [38]. This approach is more powerful than simple t-tests as it accounts for the hierarchical structure of SRM data.
- False Discovery Rate (FDR) Control: Multiple testing correction is applied to identify proteins that change abundance between conditions while controlling the false positive rate [38].
Successful SRM-based biomarker validation relies on a suite of specialized reagents and computational tools.
Table 3: Key Research Reagent Solutions for SRM Validation
| Tool/Reagent | Function | Application in SRM Workflow |
|---|---|---|
| Stable Isotope-Labeled Standard (SIS) Peptides | Synthetic peptides with heavy isotopes (13C, 15N); serve as internal standards for absolute quantification [38] | Spiked into samples pre-digestion; corrects for sample processing losses and ionization variability |
| Trypsin | Proteolytic enzyme for bottom-up proteomics; cleaves proteins C-terminal to arginine and lysine | Generates measurable peptides from target proteins |
| Immunoaffinity Depletion Columns | Remove high-abundance proteins (e.g., albumin, IgG) from plasma/serum | Enhances detection of low-abundance biomarkers by reducing dynamic range |
| LC-MS Grade Solvents | High-purity solvents (water, acetonitrile, methanol) with minimal contaminants | Ensves consistent chromatographic separation and prevents ion suppression |
| SRM Assay Development Software (e.g., Skyline) | Open-source tool for building transition lists, analyzing data, and quantifying results [38] | Central platform for method design, data visualization, and peak integration |
Integration with Systems Biology and Concluding Perspective
In the context of systems biology, SRM is not an isolated technique but part of an integrated multi-omics workflow. The validated quantitative data generated by SRM strengthens systems models by providing high-confidence protein-level measurements. These datasets can be integrated with transcriptomic, metabolomic, and lipidomic data to build more comprehensive network models of biological systems and disease processes [43]. For instance, SRM-validated protein biomarkers can be correlated with lipidomic profiles to uncover functional pathways dysregulated in disease [44].
The decision to use SRM or an alternative like PRM ultimately depends on the specific goals of the biomarker validation project. SRM remains the gold standard for high-throughput, sensitive quantification of well-characterized biomarker panels in regulated environments. Its robustness, sensitivity, and established workflows make it ideally suited for large-scale verification studies and clinical assay development. PRM, with its superior specificity and data flexibility, is an excellent choice for validating novel biomarkers, analyzing post-translational modifications, or working in particularly complex matrices [39].
Diagram 2: Decision Framework for Selecting SRM vs. PRM in Biomarker Validation.
As mass spectrometry technology continues to advance, the lines between these techniques are blurring with the development of hybrid instruments that combine the best features of both approaches [41]. Nevertheless, SRM maintains its vital role in the systems biology pipeline, providing the rigorous validation needed to transition biomarker candidates from discovery to real-world clinical and pharmaceutical application.
The fields of in silico modeling and bioinformatics are revolutionizing the approach to biological research and therapeutic development. In silico modeling, defined as the use of computer simulations to study biological processes, has evolved from simple network analysis to sophisticated representations of complex diseases [45]. Concurrently, modern bioinformatics provides the computational framework for managing, integrating, and interpreting massive biological datasets generated by high-throughput technologies [45]. These disciplines are particularly transformative for systems biology, which seeks to understand biological systems as integrated networks rather than isolated components [46]. This holistic perspective is essential for addressing complex diseases where single-target approaches have repeatedly failed, driving a paradigm shift toward multi-targeted therapeutic strategies and comprehensive biomarker validation [46].
The validation of biomarker panels represents a critical application where in silico modeling and bioinformatics converge. Where single biomarkers often lack sufficient predictive power for complex diseases, multi-marker panels capturing diverse pathophysiological pathways provide enhanced prognostic capability [47]. The integration of these computational approaches enables researchers to move beyond correlative associations toward mechanistic understanding of disease processes, ultimately accelerating the development of precision medicine through improved patient stratification, drug target identification, and therapeutic optimization [48].
Computational Frameworks for Biomarker Panel Validation
Foundational Methodologies and Approaches
The validation of biomarker panels employs distinct but complementary computational methodologies, each with specific strengths and applications in systems biology research.
Table 1: Computational Frameworks for Biomarker Validation
| Methodology | Core Function | Applications in Biomarker Validation | Representative Tools |
|---|---|---|---|
| Dynamic Systems Modeling | Describes mathematical relationships and interactions between system components over time [45] | Models pathway dynamics and biomarker interactions; simulates intervention effects | Ordinary/partial differential equations; Boolean networks |
| Machine Learning Algorithms | Identifies complex, non-linear patterns in high-dimensional data [48] | Discovers biomarker signatures; predicts disease risk and treatment response | Random Forest; XGBoost; LASSO regression [47] |
| Network Analysis | Maps relationships and dependencies between biological entities [49] | Identifies key regulatory nodes; contextualizes biomarkers within pathways | STRING; Cytoscape; Phenolyzer [49] |
| Multi-Omics Integration | Combines data from genomic, proteomic, metabolomic, and other sources [50] | Develops comprehensive biomarker profiles; reveals cross-platform interactions | Pathway mapping tools; biological network analysis |
Performance Comparison of Computational Approaches
Different computational approaches offer varying strengths in biomarker panel validation, as demonstrated by their performance characteristics in practical applications.
Table 2: Performance Comparison of Modeling Approaches in Biomarker Research
| Model Type | Predictive Accuracy (Example AUC Values) | Data Requirements | Interpretability | Best-Suited Applications |
|---|---|---|---|---|
| Traditional Statistical Models | 0.67-0.80 (Cox model for cardiovascular events) [47] | Moderate | High | Initial biomarker association testing; clinical risk scores |
| Machine Learning (Random Forest) | 0.63-0.80 (varies by outcome) [47] | High | Moderate | Complex biomarker interactions; non-linear relationships |
| Machine Learning (XGBoost) | 0.94-0.98 (high performance in some applications) [47] | Very High | Low | Large, complex datasets with many features |
| Mechanistic Multiscale Models | Qualitative prediction of system behavior [49] | Variable (domain knowledge-dependent) | High | Hypothesis testing; understanding disease mechanisms |
Experimental Protocols for Biomarker Panel Validation
Integrated Workflow for Computational Biomarker Validation
The following diagram illustrates the comprehensive workflow for validating biomarker panels using in silico approaches, from initial data collection through clinical application:
Detailed Methodological Protocols
Data Integration and Preprocessing
The initial phase involves systematic collection and harmonization of diverse data types. For genomic data, this includes whole-genome sequencing and microarray analysis processed through quality control pipelines to remove technical artifacts [45]. Proteomic data from mass spectrometry and protein arrays require normalization and batch effect correction [48]. Clinical data from electronic health records must be structured using standardized ontologies, while natural language processing techniques can extract phenotypic information from unstructured clinical notes [49]. Critical to this phase is the implementation of FAIR principles (Findable, Accessible, Interoperable, and Reusable) to ensure data quality and reproducibility [49].
Biomarker Discovery and Selection
Biomarker identification employs both unsupervised and supervised approaches. Differential expression analysis identifies molecules associated with specific phenotypes or disease states [45]. Network-based methods place candidate biomarkers in biological context by mapping them to protein-protein interaction networks and signaling pathways [45] [49]. For panel development, multivariable regression models identify biomarkers that independently contribute to predictive power, as demonstrated in cardiovascular risk assessment where D-dimer, GDF-15, IL-6, NT-proBNP, and hsTropT were shown to be independently predictive [47]. Regularization techniques like LASSO regression are particularly valuable for selecting the most informative biomarkers from high-dimensional datasets while reducing overfitting [47].
Predictive Model Development
Model construction employs both traditional statistical approaches and machine learning algorithms. Cox proportional hazards models establish baseline associations between biomarkers and clinical outcomes, providing interpretable hazard ratios for individual biomarkers [47]. Machine learning frameworks including Random Forest and XGBoost capture complex, non-linear relationships between multiple biomarkers and outcomes [47]. For dynamic processes, mechanistic models using ordinary differential equations simulate pathway dynamics and intervention effects [45]. Each approach requires careful tuning to optimize performance while maintaining generalizability.
Validation and Experimental Confirmation
Rigorous validation is essential before clinical application. Cross-validation assesses model performance on unseen data, with nested approaches providing unbiased performance estimates for hyperparameter tuning [51]. External validation tests models on completely independent cohorts to evaluate generalizability across populations [48]. For in silico models, experimental corroboration using patient-derived xenografts, organoids, and tumoroids provides critical biological validation of computational predictions [51]. In the cardiovascular domain, biomarker panels must demonstrate improved discrimination (AUC) and reclassification (NRI) beyond established clinical risk scores to warrant clinical adoption [47].
Key Signaling Pathways in Biomarker Research
Multi-Omics Pathway Integration Framework
The following diagram illustrates how biomarkers from different molecular layers integrate into coherent pathological pathways, using cardiovascular disease as an exemplar:
Pathway-Specific Biomarker Applications
Biomarker panels gain predictive power by capturing activity across multiple interconnected biological pathways. In cardiovascular disease, myocardial injury is reflected by hsTropT and NT-proBNP, which indicate cardiomyocyte stress and damage [47]. Inflammatory pathways generate IL-6, a cytokine central to pro-inflammatory signaling that promotes atherosclerosis and cardiac remodeling [47]. Oxidative stress activates GDF-15, a member of the TGF-β superfamily induced in cardiomyocytes under pathological conditions [47]. Finally, coagulation pathways produce D-dimer, a fibrin degradation product that indicates thrombotic activity and stroke risk in atrial fibrillation patients [47]. This multi-pathway approach explains why biomarker panels outperform single biomarkers, as they capture the multidimensional nature of complex disease pathophysiology.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful implementation of in silico biomarker validation requires specialized computational tools, experimental platforms, and analytical resources.
Table 3: Essential Research Tools for In Silico Biomarker Validation
| Tool Category | Specific Tools/Platforms | Primary Function | Application in Biomarker Research |
|---|---|---|---|
| Bioinformatics Databases | GO categories; KEGG pathways; STRING | Biological knowledge bases | Pathway mapping; functional annotation; network construction [45] |
| Variant Effect Prediction | SIFT; PolyPhen; REVEL; SpliceAI | In silico mutation analysis | Predicting functional impact of genetic variants [49] |
| Molecular Structure Modeling | I-TASSER; SWISS-MODEL; COTH | Protein structure prediction | Modeling structural consequences of mutations [49] |
| Multi-Omics Analysis Platforms | PandaOmics; Cytoscape | Integrated data analysis | Target identification; biomarker discovery [49] |
| Experimental Validation Systems | Patient-derived xenografts; organoids; tumoroids | Biological validation | Corroborating computational predictions [51] |
| AI/ML Frameworks | Random Forest; XGBoost; LASSO | Predictive modeling | Developing biomarker-based risk scores [47] |
| 5-Vinyl-2'-deoxyuridine | 5-Vinyl-2'-deoxyuridine, CAS:55520-67-7, MF:C11H14N2O5, MW:254.24 g/mol | Chemical Reagent | Bench Chemicals |
| Traxanox | Traxanox, CAS:58712-69-9, MF:C13H6ClN5O2, MW:299.67 g/mol | Chemical Reagent | Bench Chemicals |
Comparative Performance Data: In Silico vs. Traditional Methods
Quantitative Assessment of Predictive Accuracy
The value of computational biomarker panels is demonstrated through direct comparison with established clinical risk scores across multiple disease domains.
Table 4: Performance Comparison of Biomarker Panels vs. Clinical Risk Scores
| Clinical Context | Established Risk Score (AUC) | Biomarker-Enhanced Model (AUC) | Performance Improvement | Key Biomarkers Incorporated |
|---|---|---|---|---|
| Atrial Fibrillation (Stroke Risk) | CHAâ‚‚DSâ‚‚-VASc: 0.64 [47] | 0.69 [47] | +0.05 (P=0.0003) [47] | D-dimer, GDF-15, IL-6, NT-proBNP, hsTropT [47] |
| Atrial Fibrillation (Major Bleeding) | HAS-BLED: 0.59 [47] | 0.69 [47] | +0.10 (P=0.007) [47] | GDF-15, IGFBP-7, IL-6, hsTropT [47] |
| Heart Failure Hospitalization | Clinical model: 0.77 [47] | 0.80 [47] | +0.03 (P=5.5×10â»Â¹â°) [47] | GDF-15, IGFBP-7, NT-proBNP, hsTropT [47] |
| Composite Cardiovascular Outcome | Clinical model: 0.74 [47] | 0.77 [47] | +0.03 (P=2.6×10â»â¸) [47] | D-dimer, GDF-15, IL-6, NT-proBNP, hsTropT [47] |
Methodological Advantages and Limitations
The integration of in silico approaches with bioinformatics provides distinct advantages over traditional methods. Machine learning models consistently outperform traditional statistical approaches in complex pattern recognition, with XGBoost achieving exceptional AUC values of 0.94-0.98 for some cardiovascular outcomes [47]. Multi-omics integration captures complementary biological information that single-platform approaches miss, providing a more comprehensive view of disease pathophysiology [48] [50]. Network-based analyses contextualize biomarkers within functional pathways, moving beyond correlation to mechanistic understanding [49].
However, these approaches face significant challenges. Data quality and heterogeneity can compromise model performance, requiring sophisticated normalization and batch correction methods [48]. Model interpretability remains problematic for complex algorithms like deep learning, necessitating explainable AI techniques to build clinical trust [51]. Computational requirements can be substantial, particularly for multiscale models simulating biological processes across temporal and spatial scales [51]. Finally, clinical translation requires demonstration of not just statistical improvement but clinical utility and cost-effectiveness [48].
Future Directions and Emerging Applications
The field of in silico biomarker validation continues to evolve with several promising frontiers. Digital twin technology creates virtual patient representations that can simulate individual disease progression and treatment response, enabling truly personalized therapeutic strategies [51]. Single-cell multi-omics provides unprecedented resolution of cellular heterogeneity in complex tissues, revealing rare cell populations that may drive disease processes [50]. Edge computing solutions facilitate deployment of predictive models in low-resource settings, potentially expanding access to precision medicine approaches [48]. Dynamic biomarker monitoring using wearable sensors and liquid biopsies enables real-time tracking of disease activity and treatment response, creating opportunities for adaptive therapeutic interventions [48] [50].
For rare diseases, where traditional research is hampered by small patient populations, in silico approaches offer particularly transformative potential. Virtual cohorts, synthetic control arms, and model-informed drug development can accelerate therapeutic discovery for conditions that affect fewer than 1 in 2,000 people [49]. As these technologies mature, they promise to further bridge the gap between biomarker discovery and clinical application, ultimately fulfilling the promise of precision medicine across the disease spectrum.
The high failure rate of oncology drugs in clinical trials, often due to a lack of efficacy, underscores a critical translational gap in drug development [52]. This challenge extends to the validation of biomarker panels intended for patient stratification and treatment selection. Mouse Clinical Trials (MCTs) utilizing Patient-Derived Xenografts (PDXs) have emerged as a cornerstone preclinical platform that better mirrors human tumor biology, offering a more predictive framework for functionally validating biomarker panels within a systems biology research context [53] [54]. Unlike traditional cell line-derived xenografts (CDX), PDX models are established by directly implanting patient tumor fragments into immunodeficient mice, preserving the original tumor's histological architecture, molecular heterogeneity, and stromal components [54]. When organized into MCTs—which mimic human clinical trials by testing drug candidates across a diverse panel of these models—researchers can evaluate efficacy, identify resistance mechanisms, and most critically, discover and validate predictive biomarkers in a system that closely reflects patient population diversity [53] [55]. This guide provides a comparative analysis of PDX-based MCTs, detailing their application in robust, systems-level biomarker validation.
Comparative Analysis of Preclinical Models for Biomarker Research
The choice of preclinical model significantly impacts the reliability of biomarker validation. The table below compares the key characteristics of major model types, highlighting the relative advantages of PDX-based MCTs.
Table 1: Comparative Analysis of Preclinical Models for Biomarker Validation
| Model Characteristic | Clinical Trials (Human) | Cancer Cell Line-Derived Xenografts (CDX) | Patient-Derived Xenografts (PDX) | Genetically Engineered Mice (GEM) |
|---|---|---|---|---|
| Human Relevance of Tumor | Standard (the reference) | Situational (passage-dependent) [52] | High [54] | High/Variable (model-dependent) [52] |
| Tumor Microenvironment | Functional & Natural | Deficient & Xenogeneic [52] | Xenogeneic (mouse stroma) [52] [53] | Functional & Natural [52] |
| Tumor Heterogeneity | High | Low [52] | Moderate to High [54] | High [52] |
| Immune System Status | Functional | Deficient [52] | Deficient [52] | Functional [52] |
| Experimental Robustness & Throughput | Low | High [52] | High [52] | Moderate/Variable [52] |
| Predictive Value for Clinical Response | The reference | Limited [52] | High [53] [54] | High/Variable [52] |
| Primary Utility in Biomarker Workflows | Final validation | Preliminary triage, toxicity [52] | Biomarker discovery, validation, patient stratification [53] [55] | Pathobiology studies, immunotherapy [52] |
As the table demonstrates, PDX models strike a critical balance between maintaining human tumor relevance and allowing for robust, controlled experimentation. Their ability to preserve the molecular and cellular complexity of the original patient tumor makes them particularly suited for discovering biomarkers that will perform reliably in the clinic [54]. For instance, studies have shown a strong concordance between the response of PDXs to therapies like cetuximab in colorectal cancer and the clinical outcomes of the patients from whom the models were derived, including the predictive value of KRAS mutation status [54]. This fidelity is paramount for functional biomarker validation.
The MCT Workflow: From Study Design to Biomarker Identification
The execution of a Mouse Clinical Trial is a multi-stage process that systematically leads from model selection to biomarker insight. The workflow below outlines the key stages.
Diagram 1: MCT Workflow for Biomarker Discovery.
Detailed Experimental Protocols for Key Phases
Step 1: Study Design and Power Analysis Before initiating an MCT, a power analysis is essential to determine the sample size required for reliable, statistically significant results. This involves:
- Setting Parameters: Typically, power is set at 80% with a significance level (α) of 0.05 [55].
- Endpoint Consideration: The primary endpoint (e.g., Tumor Growth Inhibition (TGI) vs. survival) influences group size. Identifying a novel biomarker requires a larger panel of models to ensure sufficient statistical power for distinguishing responder and non-responder populations [55].
- Statistical Modeling: Using Linear Mixed Models (LMM) to generate power curves that estimate the number of PDX models and animals per model based on expected drug potency [53].
Step 2: PDX Model Selection Model selection is critical for ensuring the MCT recapitulates the targeted patient population. Key parameters include:
- Tumor Indication: Aligning PDX tumor types with the drug's intended indication [55].
- Molecular Characteristics: Selecting models based on genetic mutations, gene/protein expression, and pathway activity relevant to the drug's mechanism of action (e.g., selecting models with high EGFR expression for an EGFR inhibitor) [53].
- Treatment History: Including models derived from patients pre-treated with modern therapies is critical for studying resistance and second-line treatments [56].
- Diversity: Employing a panel of models that captures the heterogeneity of the patient population is essential for identifying broadly applicable biomarkers [55].
Step 4 & 5: Data Collection, Responder Classification, and Multi-Omics Analysis Upon study completion, data is rigorously processed to identify biomarkers.
- Responder Classification: Animals are classified as responders or non-responders based on a threshold for tumor volume reduction, often using a modified version of Response Evaluation Criteria in Solid Tumors (mRECIST) [55].
- Bioinformatics Analysis:
- Differential Gene Expression Analysis (DGEA): Compares gene expression profiles of responders vs. non-responders to identify differentially expressed genes [55].
- Differential Gene Set Enrichment Analysis (DGSE): Identifies functional gene sets or pathways enriched in either group [55].
- Multi-Omics Integration: Combining genomics, transcriptomics, and proteomics data provides a more comprehensive view. Methods like Partial Least-Squares (PLS) regression can identify influential gene networks that predict response [55]. Proteomics is particularly valuable given the frequent lack of correlation between protein and RNA abundance [55].
Quantitative Data from Preclinical Studies
The predictive power of PDX models and MCTs is demonstrated through quantitative data correlating model responses with clinical outcomes. The following table summarizes key performance metrics from published literature and commercial service providers.
Table 2: Quantitative Efficacy and Predictive Performance of PDX Models
| Tumor Type | Therapeutic Agent | Key Biomarker | Concordance with Clinical Response | Reported Data Source |
|---|---|---|---|---|
| Metastatic Colorectal Cancer | Cetuximab (anti-EGFR) | KRAS Wild-Type | ~11% response rate in unselected PDXs, mirroring patient data [54] | Academic Study [54] |
| Ovarian Cancer | Cisplatin | Clinical Histology | Sensitivity/resistance in PDXs matched patient response in most models [54] | Academic Study [54] |
| Small Cell Lung Cancer (SCLC) | Cisplatin + Etoposide | Not Specified | Good correlation between patient and PDX response, with one exception [54] | Academic Study [54] |
| Various Cancers | Diverse Compounds | Multi-Omics Profiles | Advanced metrics (e.g., Exponential Growth Rate - eGR) provide more sensitive efficacy analysis than TGI [53] | Commercial Provider [53] |
| PDX Model Bank | N/A | N/A | >1,000 low-passage PDX models, >50% from metastatic lesions [56] | Commercial Provider [56] |
The Scientist's Toolkit: Essential Reagents and Platforms
Successful execution of MCTs for biomarker validation relies on a suite of specialized reagents, models, and analytical tools.
Table 3: Essential Research Reagent Solutions for PDX MCTs
| Tool Category | Specific Examples | Function in Biomarker Validation |
|---|---|---|
| Animal Models | NOD-SCID Gamma (NSG) mice, SCID-beige mice [54] | Immunodeficient host for successful engraftment and growth of human PDX tumors. |
| PDX Biobanks | Champions Oncology (>1,500 models), CrownBio (>500 live models) [53] [56] | Provide diverse, well-characterized, and clinically annotated PDX models for MCTs. |
| Bioinformatics Software | Linear Mixed Models (LMM), DIABLO multi-omics workflow, Exponential Growth Rate (eGR) algorithms [53] [55] | Analyze complex MCT data, account for variability, and identify robust biomarker signatures. |
| Multi-Omics Platforms | RNA-Seq, Mass Spectrometry-based Proteomics & Phospho-proteomics [55] | Generate comprehensive molecular data (genome, transcriptome, proteome) for integrated biomarker discovery. |
| Data Analysis Portals | NCBI GEO2R, Network Analyst, Gene Set Enrichment Analysis (GSEA) [57] [58] | Publicly available tools for differential expression analysis and pathway enrichment of molecular data. |
| Eulicin | Eulicin, CAS:534-76-9, MF:C24H52N8O2, MW:484.7 g/mol | Chemical Reagent |
Integrated Systems Biology for Biomarker Panel Validation
A systems biology approach is fundamental to moving beyond single, often inadequate, biomarkers to robust, multi-parameter biomarker panels [2] [1]. This philosophy views disease as a perturbation of complex molecular networks and uses high-throughput data to understand these systems-level changes [1]. The relationship between experimental models and clinical translation in a systems biology framework is illustrated below.
Diagram 2: Systems Biology Workflow for Biomarker Validation.
This integrated workflow begins with clinically relevant PDX models. Multi-omics data generated from these models is fed into computational analyses to identify not just individual genes, but entire networks and pathways perturbed by the disease or treatment [58] [1]. For example, a systems biology study of glioblastoma multiforme identified a network hub gene, Matrix Metallopeptidase 9 (MMP9), as a central biomarker and potential therapeutic target by analyzing differentially expressed genes and their protein-protein interaction networks [58]. This network-based understanding leads to biomarker panels with higher diagnostic and predictive power, which are then looped back into the clinic for validation and application, creating an iterative cycle of discovery and refinement.
Navigating the Challenges: Ensuring Specificity, Sensitivity, and Reproducibility
In the pursuit of validating biomarker panels through systems biology, assay precision is not merely a technical detail but a fundamental prerequisite for generating biologically meaningful data. The coefficient of variation (CV), expressed as a percentage, serves as the key metric for precision, quantifying the level of variability in repeated measurements of the same sample [59] [60]. In the context of complex, multi-analyte biomarker panels, controlling analytical variability is paramount; without it, subtle but biologically significant signals emanating from disease-perturbed networks can be easily obscured [2] [1]. This guide establishes why a CV threshold of < 20-30% is a critical benchmark, providing an objective comparison of how different technologies and methodologies perform against this standard to ensure the robustness of systems biology research.
Defining Assay Precision: The Role of the Coefficient of Variation (CV)
The Coefficient of Variation (CV) standardizes the measure of variability relative to the mean of the data, providing a dimensionless and comparable metric for assay precision [60]. It is calculated as:
CV (%) = (Standard Deviation / Mean) x 100 [59]
This measure is particularly useful when comparing the variability of datasets with different units or widely different means [60]. In practice, microbiologists and researchers frequently use two distinct types of CV to describe assay performance, each with specific calculation methods and interpretations [60]:
- Intra-assay CV: Also known as the "within-assay" coefficient of variation, this measures the precision of replicate determinations within a single assay run. It is best calculated using the root mean square approach to provide a more accurate estimate [60].
- Inter-assay CV: This "between-assay" coefficient of variation estimates how precision varies over time, typically measured by running aliquots of the same specimen on different days and calculating the standard deviation of those means [60].
Target values for these metrics are well-established. For intra-assay precision, a CV of ≤ 10% is a common target, while for inter-assay precision, a CV of ≤ 20% is often considered acceptable [60]. It is recommended that if the intra-assay CV exceeds 10% or the inter-assay CV exceeds 20%, the source of variation should be identified and addressed [60].
Industry Standards and Acceptable CV Thresholds
The acceptability of a CV threshold is context-dependent, influenced by the biological system under investigation and the specific assay technology. The following table summarizes common acceptability benchmarks across different experimental fields:
Table 1: Established CV Benchmarks Across Research Fields
| Field/Context | Target Intra-Assay CV | Target Inter-Assay CV | Citation |
|---|---|---|---|
| Laboratory Experiments | < 10% | < 20% | [59] |
| Agricultural Experiments | < 20% | Not Specified | [59] |
| Long-Term Assays | ~7% (Typical) | ~15% (Typical) | [60] |
| Maize Yield Trials | 5-15% (Typical Range) | Not Specified | [60] |
For biomarker validation—a process central to systems biology—maintaining a low CV is non-negotiable. Biomarker panels, which incorporate various sources of biomolecular data to guarantee higher robustness and power of separation for a clinical test, are particularly vulnerable to analytical variability [2]. Imprecise measurements can lead to false positives/negatives and hinder the ability to identify true, disease-relevant molecular fingerprints [1] [61].
Comparative Analysis of Key Experimental Techniques
The choice of experimental platform has profound implications for achievable precision and the type of data generated. The following table provides a high-level comparison of two common techniques used in biomarker research and drug discovery.
Table 2: Technique Comparison: ELISA vs. Flow Cytometry
| Feature | ELISA (Enzyme-Linked Immunosorbent Assay) | Flow Cytometry |
|---|---|---|
| Primary Use | Quantification of soluble analytes (proteins, hormones) | Multi-parameter analysis of single cells |
| Key Strength | High sensitivity for detecting minute quantities; cost-effective for large sample batches [62] | Provides cellular context and can analyze multiple characteristics per cell [62] |
| Key Limitation | Lacks cellular context; fixed parameters per run [62] | High complexity and cost; requires significant expertise [62] |
| Data Output | Concentration of a single analyte | Presence, frequency, and function of specific cell types |
| Precision Consideration | Well-established, robust protocol conducive to low CVs in a controlled setup. | Precision can be affected by complex, multi-step staining procedures and instrument calibration. |
Beyond these core techniques, the broader field of drug discovery is increasingly relying on High-Throughput Screening (HTS). The global HTS market, valued at USD 26.12 billion in 2025, relies on automation and miniaturization to screen thousands of compounds swiftly [63]. A key technology within HTS is cell-based assays, which are projected to hold a 33.4% market share in 2025 because they more accurately replicate complex biological systems compared to traditional biochemical methods [63]. The precision of these automated systems is critical for their value, with quality control procedures like z-factor calculation used to ensure data accuracy and minimize false positives [64].
Experimental Protocols for Determining Assay CV
To objectively assess and compare the precision of any assay, researchers must follow standardized experimental and calculation protocols. Below are detailed methodologies for determining both intra- and inter-assay CV.
Protocol 1: Determining Intra-Assay CV
This protocol evaluates the repeatability of an assay within a single run.
- Sample Preparation: Select N different specimen samples (e.g., patient sera, cell lysates). For each specimen, prepare a set of n replicate aliquots (typically n=2-3). All aliquots for all specimens are processed on the same ELISA plate or assay run [60].
- Assay Execution: Run the entire plate using a standardized, validated protocol. Ensure that all reagents are from the same lot and that the procedure is performed by a single operator within the shortest feasible timeframe.
- Data Calculation - Root Mean Square Method:
- For each specimen i, calculate the mean (i) and standard deviation (s_i) of its n replicates.
- For each specimen, calculate its CV: CVi = (si / i)
- The final intra-assay CV for the run is calculated as the root mean square of the individual CVs: CVintra = √ [ Σ (CVi)² / N ] [60]
Protocol 2: Determining Inter-Assay CV
This protocol evaluates the reproducibility of an assay over time, accounting for day-to-day variability.
- Sample Preparation: Select a single, stable specimen (e.g., a pooled control sample). Prepare n aliquots of this specimen (n can be 2 or more).
- Assay Execution: Run the n aliquots of the same specimen in M separate assay runs on different days (e.g., over 5-10 different days). These runs should incorporate different reagent lots, different operators, and standard instrument calibration to reflect real-world conditions.
- Data Calculation:
- For each day j, calculate the mean (j) of that day's n results.
- Calculate the overall mean () of all the daily means.
- Calculate the standard deviation (s) of the M daily means.
- The inter-assay CV is then calculated as: CV_inter = (s / ) x 100 [60]
Systems Biology Workflow for Biomarker Validation
The following diagram illustrates a generalized systems biology workflow for biomarker discovery and validation, highlighting stages where rigorous assay precision is non-negotiable. Adherence to CV thresholds is especially critical during the technical validation and verification phases to ensure that observed variations are biological rather than analytical.
The Scientist's Toolkit: Essential Reagent Solutions
The precision of any biomarker assay is heavily dependent on the quality and consistency of the core reagents used. The following table details key materials essential for conducting the experiments described in this guide.
Table 3: Key Research Reagent Solutions for Biomarker Assays
| Reagent / Material | Critical Function | Precision Consideration |
|---|---|---|
| High-Affinity Antibodies | Specific capture and detection of target analytes in ELISA and flow cytometry [62]. | Lot-to-lot consistency is paramount for maintaining low inter-assay CV. |
| Stable Calibrators & Controls | Creating standard curves for quantification and monitoring assay performance [60]. | High stability ensures accuracy and reproducibility across runs. |
| Cell-Based Assay Kits | Provide optimized reagents for high-throughput, physiologically relevant screening [63]. | Robust kit formulation minimizes variability in complex cellular models. |
| Liquid Handling Systems | Automated, precise dispensing of samples and reagents in HTS [63]. | Precision at nanoliter scales is crucial for miniaturized assays and low CV. |
In the data-driven paradigm of systems biology, the path from a disease-perturbed molecular network to a clinically useful biomarker panel is built on a foundation of rigorous analytical validation. Adhering to the critical benchmark of CV < 20-30% is not a mere formality but a fundamental requirement to distinguish true biological signal from analytical noise. As this guide has detailed, achieving this requires a holistic strategy: selecting the appropriate technological platform, following standardized experimental protocols for assessing precision, and utilizing high-quality, consistent reagents. By meticulously controlling for analytical variability, researchers can ensure that their biomarker panels are robust, reproducible, and capable of fulfilling their promise in enabling precision medicine.
In the field of systems biology research, the validation of biomarker panels is a critical step toward developing reliable diagnostic tools and therapeutic targets. The integrity of this validation process hinges on the rigorous application of methodologies designed to mitigate bias. Randomized sample assignment and blinded analysis are two cornerstone techniques that protect the validity of experimental findings by minimizing systematic errors and subjective influences. These strategies ensure that the observed outcomes truly reflect the biological phenomena under investigation rather than artifacts of the experimental setup or researcher expectations.
Within clinical and preclinical research, bias can infiltrate at multiple stages—from initial sample selection and group allocation to data analysis and interpretation. Implementing a robust framework for bias mitigation is therefore not merely a procedural formality but a fundamental component of scientific rigor. This guide provides a comparative analysis of the core strategies for randomized assignment and blinded analysis, detailing their protocols, applications, and performance in the specific context of validating biomarker panels.
Foundational Concepts: Randomization and Blinding
Randomized Experimental Design
Randomized experimental design, or random assignment, is a fundamental research methodology involving the random allocation of subjects or samples into different experimental groups. This process ensures that each participant has an equal chance of being assigned to any given group, thereby distributing both known and unknown confounding variables evenly across groups. The primary goal is to create comparable groups at the baseline, so that any differences in outcomes can be more confidently attributed to the experimental intervention rather than pre-existing sample characteristics [65].
In the context of biomarker validation, where patient samples may vary considerably in their clinical and molecular profiles, randomization is crucial for ensuring that the treatment and control groups are biologically comparable. This is a key step toward establishing causal relationships and enhancing the internal validity of an experiment [65].
The Role of Blinding
Blinding is a technique used to prevent the knowledge of group assignments from influencing the behavior or assessments of the participants, researchers, or outcome assessors. In an open-label trial where full blinding is not feasible, it is still recommended to implement blinding during the endpoint evaluation and data analysis phases wherever possible. Maintaining the confidentiality of ongoing results is another practice that helps uphold the integrity of the study's conclusions [66].
Blinding is particularly critical in biomarker studies to prevent conscious or unconscious bias during data collection, processing, and analysis. When analysts are unaware of which samples belong to the case or control groups, their measurements and interpretations are less likely to be swayed by expectations, leading to more objective and reliable data [66] [67].
Randomization Strategies: A Comparative Analysis
Types of Randomization
Several randomization techniques are available to researchers, each with distinct advantages, limitations, and ideal use cases. The choice of technique depends on factors such as sample size, the need to control for covariates, and the overall study design [65].
Table 1: Comparison of Randomization Techniques in Research
| Technique | Key Principle | Advantages | Limitations | Ideal Use Case in Biomarker Research |
|---|---|---|---|---|
| Simple Randomization [65] | Assigns each subject to a group via a random mechanism (e.g., random number generator). | Easy to implement; guarantees equal chance of assignment. | Can lead to imbalanced group sizes, especially with small samples. | Pilot studies or initial biomarker discovery phases with large sample sizes. |
| Block Randomization [65] | Participants are divided into blocks (e.g., of 4 or 6); within each block, assignment is randomized to ensure balance. | Maintains balance in group sizes throughout the enrollment period. | Does not control for covariates unless combined with other methods. | Longitudinal biomarker studies with staggered participant enrollment. |
| Stratified Randomization [65] | Participants are first divided into strata based on key covariates (e.g., age, disease stage); randomization occurs within each stratum. | Controls for known confounders; ensures balance across important covariates. | More complex; requires knowledge of key covariates beforehand. | Validating a biomarker panel where specific patient demographics are known to influence the outcome. |
| Covariate Adaptive Randomization [65] | The random assignment probability is adjusted based on the characteristics of already-enrolled participants to minimize imbalance. | Dynamically maintains balance on multiple covariates. | Computationally intensive; requires real-time covariate data. | Complex biomarker studies with multiple, important confounding variables. |
Experimental Protocol for Stratified Randomization
For biomarker studies, Stratified Randomization is often the most appropriate method as it controls for known confounding variables. Below is a detailed protocol for implementing this technique.
Objective: To randomly assign patient samples to experimental groups while ensuring balanced distribution of specific clinical covariates (e.g., age, sex, disease severity) across all groups. Materials:
- Patient cohort dataset with confirmed biomarker status and covariate information.
- Statistical software (e.g., R, Python, SPSS) or a verified random number generator. Procedure:
- Identify Stratification Variables: Select the key covariates known or suspected to influence the biomarker or primary endpoint (e.g., age groups: <50, 50-65, >65; sex: male, female; disease stage: I, II, III).
- Create Strata: Divide the entire patient cohort into mutually exclusive subgroups (strata) based on every possible combination of the chosen covariates.
- Generate Allocation Sequence: Within each stratum, use a computer-generated random number sequence to assign each participant to an experimental group (e.g., Treatment or Control). Employ block randomization within strata to ensure periodic size balance.
- Conceal the Allocation: Ensure the allocation sequence is concealed from the investigators enrolling participants. This can be done via a centralized, automated system.
- Verify Balance: After assignment, perform a statistical check (e.g., chi-square test, ANOVA) to confirm that the covariates are balanced across the final groups.
The following workflow diagram illustrates the stratified randomization process.
Blinding Strategies for Objective Analysis
Levels of Blinding and Implementation
Blinding can be implemented at various stages of an experiment, and the chosen level should be clearly documented in the study protocol. In open-label trials, where full blinding of participants and caregivers is not possible, focusing on blinding the data analysts becomes paramount [66].
Table 2: Levels of Blinding in Experimental Research
| Blinding Level | Who is Blinded | Key Implementation Strategy | Impact on Bias Mitigation |
|---|---|---|---|
| Single-Blind | Participants OR Investigators | Participants are unaware of their group assignment, or the treating clinicians are unaware. | Reduces placebo effect in participants or performance bias by investigators. |
| Double-Blind | Participants AND Investigators | Both the participants and the research team interacting with them are unaware of group assignments. | Mitigates placebo effect and performance bias; considered a gold standard in clinical trials. |
| Triple-Blind / Analyst-Blind | Participants, Investigators, AND Data Analysts | The allocation code is broken only after the database is locked and the final statistical analysis plan is finalized. | Eliminates confirmation bias during data processing and statistical analysis; highly recommended for biomarker validation. |
Protocol for Blinded Biomarker Analysis
Maintaining blinding during the laboratory and computational analysis of biomarkers is essential for obtaining unbiased results.
Objective: To ensure that all laboratory measurements and computational analyses of biomarker data are performed without knowledge of group assignments. Materials:
- Coded sample identifiers.
- Laboratory Information Management System (LIMS).
- Data analysis software (e.g., R, Python). Procedure:
- Sample Coding: After randomized assignment, replace all group-identifying information (e.g., "Control," "Treatment") with a unique, non-revealing code. This key is held by an independent third party or locked in a secure document until analysis is complete.
- Blinded Laboratory Processing: Technicians performing assays (e.g., ELISA, sequencing, mass spectrometry) receive samples identified only by their code. Standard Operating Procedures (SOPs) are used to minimize technical variation.
- Blinded Data Processing: The raw data output from laboratory instruments is processed and cleaned using the coded identifiers. Any data normalization or transformation is defined in the statistical analysis plan prior to unblinding.
- Blinded Statistical Analysis: The data analyst works with the fully processed, coded dataset to execute the pre-specified analysis plan. This includes generating all primary and secondary endpoint results.
- Unblinding and Final Interpretation: Only after the final analysis dataset and results are finalized and locked is the allocation code broken to interpret the findings in the context of the experimental groups.
The relationship between different bias types and their corresponding mitigation strategies is outlined below.
Performance Comparison of Bias Mitigation Strategies
Empirical data from research studies demonstrates the tangible impact of different bias mitigation strategies on model performance and fairness. The following table summarizes results from a study comparing various mitigation approaches, including random sampling, on key metrics of accuracy and demographic parity [68].
Table 3: Comparative Performance of Bias Mitigation Strategies in Machine Learning
| Mitigation Strategy | Reported Accuracy | Demographic Parity Difference (Sex) | Demographic Parity Difference (Race) | Summary of Effectiveness |
|---|---|---|---|---|
| In-Processing Method | 84.72% | 17.01% | 23.22% | Highest accuracy, but significant residual bias in both demographic categories. |
| Hybrid Method | 84.12% | 17.70% | 20.80% | High accuracy, but bias reduction was not considerable compared to in-processing. |
| SMOTE | 61.27% | 5.40% | 30.57% | Moderate bias reduction for sex, but high racial bias and lowest accuracy. |
| Random Sampling | 79.21% | 5.36% | 11.02% | A balanced approach with the lowest sex-based bias and a moderate reduction in racial bias, while maintaining relatively high accuracy. |
The data indicates that while more complex methods (In-Processing, Hybrid) can achieve high accuracy, they may not adequately address fairness. Random sampling emerged as a robust and balanced strategy, effectively reducing demographic disparities with only a modest trade-off in accuracy [68]. This underscores its value in creating fair and generalizable models, a crucial consideration in biomarker development.
The Scientist's Toolkit for Bias-Aware Research
Implementing these strategies requires a combination of methodological rigor and practical tools. The following table details essential "research reagent solutions" and resources for executing robust, bias-aware experiments.
Table 4: Essential Reagents and Tools for Bias Mitigation Protocols
| Item / Tool | Category | Primary Function in Bias Mitigation |
|---|---|---|
| Statistical Software (R, Python, SPSS) | Software | Generates robust random allocation sequences, performs block and stratified randomization, and conducts blinded statistical analyses. |
| Laboratory Information Management System (LIMS) | Software | Manages sample metadata and implements sample coding protocols to maintain blinding during laboratory processing. |
| Centralized Randomization Service | Protocol | An independent service for allocating participants to groups, ensuring allocation concealment, which is critical for trial integrity. |
| Pre-Specified Statistical Analysis Plan (SAP) | Document | A detailed plan finalized before unblinding data, which prevents data dredging and confirmation bias by pre-defining all analyses. |
| Coded Sample Identifiers | Laboratory Reagent | Physical labels (e.g., barcodes) that replace group names, allowing for blinded sample processing and data collection in the lab. |
Integrated Workflow for Biomarker Validation Studies
Combining randomization and blinding into a single, integrated workflow ensures a comprehensive defense against bias. The following diagram maps the entire process from cohort selection to final unblinding, highlighting how these strategies interlock.
This end-to-end workflow demonstrates that mitigating bias is not a single step but a continuous process embedded throughout the experimental lifecycle. By rigorously applying these strategies, researchers in systems biology and drug development can enhance the reliability and credibility of their validated biomarker panels, accelerating the translation of scientific discovery into clinical application.
The accurate detection of disease-specific signals in complex biological mixtures represents a fundamental challenge in modern biomarker research. The high-dimensional nature of biological samples—containing thousands of proteins, nucleic acids, and metabolites from multiple sources and physiological processes—creates a minefield of potential false positives and confounding variables. Specificity, defined as a test's ability to correctly identify negative cases, becomes exponentially more difficult to achieve as sample complexity increases. Within systems biology, this challenge is addressed through integrated approaches that combine advanced technologies, computational modeling, and multi-analyte profiling to distinguish true pathological signals from biological noise [2] [1].
The transition from single-marker assays to comprehensive biomarker panels reflects an important evolution in diagnostic philosophy. Where single biomarkers often lack the necessary specificity for complex multifactorial diseases, strategically designed panels can capture the nuanced patterns of network perturbations characteristic of pathological states [2]. This approach is particularly valuable for heterogeneous conditions such as neurodegenerative disorders, psychiatric conditions, and complex cancers, where multiple biological pathways are affected simultaneously [1] [69]. By measuring multiple analytes simultaneously and analyzing their relationships through systems biology principles, researchers can achieve the robust specificity required for clinical application despite the challenging matrix effects, concentration dynamic ranges, and biomolecular interactions inherent to complex samples.
Performance Comparison of Detection Platforms
The selection of appropriate analytical platforms significantly influences the specificity achievable in complex mixture analysis. Different technologies offer distinct advantages and limitations in their ability to resolve specific signals amidst biological noise.
Table 1: Comparative Analysis of Biomarker Detection Platforms
| Platform | Multiplexing Capacity | Specificity Mechanisms | Sample Throughput | Key Specificity Challenges |
|---|---|---|---|---|
| xMAP/Luminex | Moderate (Up to 500-plex) | Spectral discrimination of fluorescent microspheres | High (Semi-automated) | Cross-reactivity in antibody-based detection; matrix interference [70] |
| Mass Spectrometry (Targeted) | Low to Moderate (10-100 targets) | Mass/charge separation + MRM transitions | Moderate | Ion suppression; requires prior knowledge of targets [71] |
| ELISA | Low (Typically single-plex) | Antibody-antigen specificity | Low | Cross-reactivity with structurally similar proteins; lot-to-lot antibody variability [70] |
| Full Spectrum Flow Cytometry | High (30+ markers) | Spectral unmixing of full fluorescence signatures | High | Autofluorescence; spillover spreading despite compensation [72] |
| Mass Cytometry (CyTOF) | High (40+ markers) | Metal isotope tagging + time-of-flight detection | Moderate | Cell/nuclear processing complexity; lower analysis speed [72] |
Table 2: Quantitative Performance Comparison for Neurodegenerative Biomarker Detection
| Platform | Target | Reported Specificity | Reported Sensitivity | Sample Type | Key Finding |
|---|---|---|---|---|---|
| xMAP Luminex | Aβ1-42, t-tau, p-tau181 | 88% diagnostic accuracy for AD | Comparable to ELISA | CSF | Demonstrated high accuracy for diagnostic classification between AD and controls [70] |
| ELISA | Aβ1-42, t-tau, p-tau181 | Lower than xMAP in comparative studies | High but with variability | CSF | Higher intra- and inter-assay variability affects specificity [70] |
| Olink Explore | 33-protein ALS signature | AUC: 98.3% | High accuracy for pre-symptomatic detection | Plasma | Machine learning analysis of panel provided exceptional disease discrimination [73] |
Experimental Protocols for Specificity Optimization
Multiplex Immunoassay Comparison Protocol
The precise protocol for comparing xMAP and ELISA platforms, as implemented in the Alzheimer's disease biomarker study, provides a template for specificity validation [70]. CSF samples were obtained via lumbar puncture using 25G Sprotte atraumatic needles following an overnight fast. Samples were immediately frozen on dry ice and stored at -80°C until analysis to prevent protein degradation. For the xMAP analysis, the INNO-BIA AlzBio3 research-use-only kit was used on the Luminex platform, employing monoclonal antibody pairs 4D7A3/3D6 for Aβ1-42, AT120/HT7 for total tau, and AT270/HT7 for p-tau181. The ELISA measurements utilized INNOTEST kits with antibodies 21F12/3D6 for Aβ1-42, AT120/HT7 and BT2 for total tau, and HT7/AT270 for p-tau181. Critical specificity measures included running all assays blinded to clinical information and platform results, using the same sample aliquots for both platforms, and implementing a log-transformation of values to achieve constant variance for proper comparison. The statistical approach employed linear regression using combinations of xMAP measurements to predict corresponding ELISA values, revealing that p-tau181 concentrations by ELISA were better predicted using both t-tau and p-tau181 xMAP values (r=0.96) than p-tau181 alone (r=0.82) [70].
Mass Spectrometry-Based Biomarker Verification
For mass spectrometry approaches, a standardized verification workflow has been developed to maximize specificity in complex samples [71]. The process begins with biomarker discovery using non-targeted "shotgun" proteomics with relative quantitation techniques (e.g., iTRAQ, TMT tagging, or label-free methods) applied to a small number of samples. Following discovery, a critical qualification step filters potential biomarkers using additional patient samples or higher-specificity mass spectrometry. Verification then occurs using targeted approaches like Multiple Reaction Monitoring (MRM) on 10-50 patient samples, focusing on "proteotypic" peptides that act as specific surrogates for parent proteins. The final validation phase employs absolute quantitation on 100-500 samples. Key to maintaining specificity throughout this pipeline is the use of stable isotope-labeled internal standards for each target peptide, which account for matrix effects and ionization efficiency variations. The platform leverages the precise mass resolution and retention time stability of modern LC-MS systems to distinguish target analytes from interfering substances, with specificity further enhanced by monitoring multiple fragment ions per peptide [71].
Visualization of Experimental Workflows
Biomarker Panel Validation Workflow
Specificity Assurance in Complex Mixtures
The Scientist's Toolkit: Essential Research Reagents
Table 3: Research Reagent Solutions for Biomarker Panel Validation
| Reagent/Platform | Function | Specificity Considerations |
|---|---|---|
| INNO-BIA AlzBio3 xMAP Kit | Multiplex quantitation of Aβ1-42, t-tau, p-tau181 | Monoclonal antibody pairs (4D7A3/3D6, AT120/HT7, AT270/HT7) minimize cross-reactivity [70] |
| Olink Explore 3072 Platform | High-throughput proteomics using Proximity Extension Assay | Dual-recognition requirement (pairs of antibodies) reduces false positives [73] |
| Stable Isotope-Labeled Internal Standards | Absolute quantitation in mass spectrometry | Distinguish target analytes from matrix ions; correct for ionization efficiency [71] |
| Proteotypic Peptides | Surrogate markers for proteins in MS-based quantitation | Unique to target protein; avoid shared sequences with other proteins [71] |
| Metal-Labeled Antibodies (CyTOF) | High-parameter single-cell analysis | Minimal spectral overlap compared to fluorophores; enables 40+ parameter panels [72] |
Discussion: Systems Biology Approaches to Specificity Challenges
The integration of systems biology principles represents a paradigm shift in addressing specificity challenges in complex biological mixtures. Rather than relying on single-marker measurements with potentially limited discriminatory power, the field has moved toward network-based analyses that capture the dynamic interactions between multiple biomolecules [2] [1]. This approach recognizes that diseases perturb biological networks in characteristic ways, creating reproducible molecular fingerprints that can be detected through appropriately designed panels. For example, in neurodegenerative diseases, multiple interconnected pathways involving glial activation, synaptic degeneration, and neuronal death create distinct signatures that are more specific than any individual biomarker [1].
Machine learning algorithms further enhance specificity by identifying complex, multi-dimensional patterns that might escape conventional statistical methods. In the ALS biomarker study, a machine learning model applied to a 33-protein signature achieved exceptional diagnostic specificity (AUC 98.3%), demonstrating how computational approaches can integrate information from multiple biomarkers to distinguish disease states with high accuracy [73]. Similarly, two-stage statistical designs with appropriate correction for overfitting, such as the methods developed for Sjögren's Syndrome biomarker panels, help maintain specificity by ensuring that identified panels perform robustly on independent validation samples [8]. These approaches acknowledge that in complex biological systems, specificity emerges not from perfect individual assays, but from the convergent evidence provided by carefully designed panels analyzed through appropriate computational frameworks.
Achieving high specificity in complex biological mixtures requires a multifaceted strategy that integrates appropriate technology selection, rigorous experimental design, sophisticated computational analysis, and systems-level thinking. The comparative data presented in this guide demonstrates that while all platforms face specificity challenges in complex matrices, methodological choices significantly impact outcomes. The emerging consensus favors multiplexed panels over single biomarkers, orthogonal verification across platforms, and the application of systems biology principles that recognize disease as a perturbation of interacting networks rather than isolated molecular events. As validation methodologies continue to evolve—incorporating larger sample sizes, standardized protocols, and advanced computational corrections—the specificity of biomarker panels in complex mixtures will continue to improve, enabling more accurate diagnosis, stratification, and monitoring of complex human diseases.
The journey from biomarker discovery to clinical application is a deliberate process of validation and refinement. In the era of precision medicine, biomarker panels—sets of multiple biomarkers used in combination—are increasingly critical for disease detection, diagnosis, prognosis, and predicting treatment response [61]. The central challenge in developing these panels lies in balancing analytical sophistication with practical implementation: specifically, optimizing the number of biomarkers in a panel to maximize clinical performance while ensuring feasibility for routine clinical use. Clinical utility, a key concept in this optimization, refers to the extent to which a biomarker test improves health outcomes by informing clinical decisions, influencing patient management, or providing prognostic information that directly benefits patients [74] [75]. Demonstrating clinical utility requires evidence that measuring the biomarker leads to better health outcomes through improved decision-making, patient motivation, or direct quality of life benefits [74].
The process of establishing clinical utility follows a phased approach, beginning with proof of statistical association between the biomarker and the clinical state of interest, followed by demonstration that the biomarker adds information beyond established markers [74]. Mid-phase studies examine how often this incremental information might alter physician prescribing decisions, while late-phase studies directly measure the health impact of biomarker-guided strategies through randomized trials or modeling [74]. Within this framework, panel size optimization becomes a critical consideration, as the number of biomarkers directly influences both analytical performance and practical implementation in clinical settings. This guide systematically compares the performance characteristics of small, medium, and large biomarker panels to inform evidence-based selection for research and clinical applications.
Panel Size Comparisons: Performance Metrics Across Scales
Quantitative Performance Across Panel Sizes
The relationship between panel size and clinical performance is not always linear. Careful design can enable medium-sized panels to capture most clinically actionable information while maintaining practical advantages. A 2020 comparative study of solid tumor gene panels demonstrated this balance effectively [76].
Table 1: Detection Rates of Clinically Actionable Variants by Panel Size
| Panel Size | Number of Genes | Total Variants Detected | FDA-Approved Therapy Targets | Off-Label Therapy Targets | Trial-Eligible Variants |
|---|---|---|---|---|---|
| Large | 315 | 2072 | 61 (12.7%) | 89 (18.5%) | 312 (65.0%) |
| Medium | 161 | 1354 (65.3%) | 61 (100%) | 89 (100%) | 312 (100%) |
| Small | 50 | 737 (35.5%) | 54 (88.5%) | 54 (60.7%) | Not reported |
The data reveals a crucial finding: the medium-sized panel detected 100% of patients with clinically actionable variants that were identified by the large panel, despite sequencing only approximately half the number of genes [76]. This demonstrates that carefully selected medium-sized panels can be as effective as large panels for detecting clinically actionable variants while offering practical advantages. The small panel, while covering only 35.5% of total variants, still captured 88.5% of variants with FDA-approved therapies, suggesting that for specific clinical applications with well-defined targets, smaller panels may be sufficient [76].
Diagnostic Accuracy Across Panel Sizes
Different clinical contexts demand varying levels of diagnostic precision. Autoantibody biomarker panels for pancreatic ductal adenocarcinoma (PDAC) detection illustrate how panel size and composition affect diagnostic accuracy across different clinical scenarios.
Table 2: Diagnostic Performance of Autoantibody Panels for PDAC Detection
| Panel Size | Biomarker Composition | Clinical Application | AUC | Sensitivity | Specificity |
|---|---|---|---|---|---|
| 7-marker | CEACAM1, DPPA2, DPPA3, MAGEA4, SRC, TPBG, XAGE3 | PDAC vs. Controls | 85.0% | 82.8% | 68.4% |
| 11-marker | Adds ALX1, GPA33, LIPI, SUB1 to 7-marker panel | PDAC vs. Colorectal Cancer | 84.3% | Not reported | Not reported |
| 11-marker | Same as above | PDAC vs. Prostate Cancer | 80.2% | Not reported | Not reported |
| 11-marker | Same as above | PDAC vs. Healthy Controls | 80.9% | Not reported | Not reported |
The similar performance between the 7-marker and 11-marker panels suggests diminishing returns beyond a certain panel size, while the maintenance of strong discriminatory power across different cancer types indicates robust specificity [25]. This demonstrates that moderately-sized panels can achieve excellent diagnostic performance while potentially offering advantages in clinical workflow integration.
Experimental Approaches for Panel Validation
Statistical Methodologies for Panel Optimization
Robust statistical frameworks are essential for developing and validating biomarker panels. These methodologies help determine optimal panel size and composition while controlling for overfitting and false discovery.
Linear Classifier Development: For ovarian cancer detection, researchers employed a repeated sub-sampling validation procedure to identify optimal marker combinations [77]. Serum samples from 142 stage I ovarian cancer cases and 5 annual samples each from 217 healthy controls were randomly divided into training (60%) and validation (40%) sets. All possible biomarker combinations were exhaustively explored using linear classifiers to identify panels with maximum sensitivity for stage I disease at 98% specificity [77]. The optimal four-marker panel (CA125, HE4, MMP-7, CA72-4) achieved 83.2% sensitivity at 98% specificity, demonstrating that moderate-sized panels can achieve high performance for early cancer detection [77].
Longitudinal Variance Analysis: For biomarkers intended for serial monitoring, evaluating within-person and between-person variability is crucial. The within-person coefficient of variation (CV) should be lower than the between-person CV to establish reliable individual baselines [77]. In the ovarian cancer study, within-person CVs for CA125, HE4, MMP-7, and CA72-4 (15%, 25%, 25%, and 21% respectively) were generally lower than their between-person CVs (49%, 20%, 35%, and 84% respectively), supporting their suitability for longitudinal algorithms [77].
Utility-Based Cut-Point Selection: Rather than relying solely on accuracy metrics like the Youden index, clinical utility-based methods incorporate the consequences of clinical decisions [75]. These methods include:
- Youden-based Clinical Utility (YBCUT): Maximizes the sum of positive and negative clinical utilities
- Product-based Clinical Utility (PBCUT): Maximizes the product of positive and negative clinical utilities
- Union-based Clinical Utility (UBCUT): Minimizes the absolute difference between positive clinical utility and AUC plus negative clinical utility and AUC
- Absolute Difference of Total Clinical Utility (ADTCUT): Minimizes the absolute difference between total clinical utility and twice the AUC [75]
These approaches are particularly valuable when different misclassification errors (false positives vs. false negatives) have substantially different clinical implications.
Experimental Workflow for Panel Development
The following diagram illustrates the comprehensive workflow for developing and validating biomarker panels, integrating multiple experimental and analytical phases:
Research Reagent Solutions for Panel Validation
The following essential materials and methodologies form the foundation of rigorous biomarker panel development:
Table 3: Essential Research Reagents and Platforms for Biomarker Panel Validation
| Category | Specific Examples | Function in Panel Validation |
|---|---|---|
| Sample Collections | Training cohorts (N=94), Validation cohorts (N=223) [25] | Provide biological material for discovery and validation phases |
| Protein Microarrays | CT100+ microarrays (113 CT/tumor antigens) [25] | High-throughput autoantibody profiling for biomarker discovery |
| Immunoassays | Roche Elecsys, Fujirebio HE4, R&D Systems ELISA [77] | Quantitative measurement of individual biomarker concentrations |
| Statistical Platforms | R, STAN, WinBUGS [78] | Advanced modeling for panel optimization and cut-point selection |
| Analytical Frameworks | Linear classifiers, ROC analysis, longitudinal algorithms [77] | Objective assessment of panel performance and clinical utility |
Decision Framework for Panel Selection
Strategic Implementation Guidelines
Choosing the appropriate panel size requires careful consideration of clinical context, technological capabilities, and practical constraints. The following diagram outlines the decision process for selecting optimal panel size based on application requirements:
Context-Specific Panel Selection
When to choose small panels: Small panels (typically ≤50 markers) are ideal for well-characterized cancers with established biomarker pathways, such as EGFR mutations in non-small cell lung cancer or the 7-autoantibody panel for PDAC detection [25] [79]. They offer advantages in settings with rapid turnaround requirements, cost constraints, or limited technical resources. Small panels are particularly suitable when clinical decision-making relies on a few highly validated biomarkers and when the analytical validation of larger panels would be prohibitively expensive or time-consuming [76] [79].
When to choose medium panels: Medium-sized panels (typically 50-200 markers) represent an optimal balance for many clinical applications, as demonstrated by the 161-gene solid tumor panel that maintained 100% detection of clinically actionable variants [76]. These panels are appropriate when covering disease heterogeneity is important but comprehensive genomic profiling is unnecessary. They offer a practical solution for clinical laboratories with standard molecular pathology capabilities while providing sufficient breadth to capture most clinically relevant alterations [76].
When to choose large panels: Large panels (≥200 markers) are reserved for discovery-phase research, complex diagnostic challenges requiring comprehensive profiling, or when identifying rare variants is clinically essential [76] [80]. They necessitate specialized bioinformatics expertise, sophisticated computational infrastructure, and higher cost tolerance. Large panels are particularly valuable in academic medical centers and research institutions where the identification of novel biomarkers or complex molecular patterns contributes to both clinical care and research advancement [76].
Optimizing biomarker panel size requires balancing clinical performance with practical implementation. The evidence consistently demonstrates that carefully designed medium-sized panels can deliver clinical utility equivalent to large panels for many applications while offering advantages in accessibility, cost, and workflow integration. Small panels remain valuable for focused clinical questions with well-defined biomarkers, while large panels maintain their role in discovery research and complex diagnostic scenarios. As systems biology approaches continue to evolve, the integration of multimodal data—genomic, proteomic, and clinical—will further refine our ability to design targeted panels that maximize clinical utility while minimizing unnecessary complexity. The future of biomarker panel optimization lies not in simply maximizing the number of markers, but in strategically selecting the most informative biomarkers for specific clinical contexts.
From Bench to Bedside: Statistical Rigor and Clinical Validation of Biomarker Panels
The validation of biomarker panels represents a critical step in the transition from systems biology research to clinical application. Unlike single-molecule biomarkers, panels that incorporate multiple biomolecular and clinical data points offer higher robustness and power of separation for clinical tests [2]. This is particularly vital for complex, multifactorial diseases, such as psychiatric disorders or many cancers, where a single dysregulated gene, protein, or metabolite is insufficient for accurate diagnosis or prognosis [2]. The performance of these panels is quantitatively assessed using a set of key metrics—Sensitivity, Specificity, the Area Under the Curve (AUC), Positive Predictive Value (PPV), and Negative Predictive Value (NPV). These metrics provide a comprehensive framework for evaluating a test's diagnostic accuracy, guiding researchers and clinicians in selecting optimal cutoffs, and comparing the efficacy of different biomarker strategies [81] [82] [83]. Within systems biology, the discovery and validation of these panels increasingly rely on integrated multi-omic approaches and machine learning to filter biomolecules, pre-validate potential biomarkers, and generate final, clinically useful panels [2] [84].
Defining the Key Metrics
Sensitivity and Specificity
Sensitivity and Specificity are fundamental, interdependent metrics that describe the intrinsic diagnostic accuracy of a test, independent of the population's disease prevalence [82].
- Sensitivity, or the true positive rate, measures a test's ability to correctly identify individuals who have the disease. It is calculated as the proportion of diseased individuals who test positive: Sensitivity = TP / (TP + FN) [82] [83]. A highly sensitive test is crucial for screening and ruling out disease, as it minimizes false negatives.
- Specificity, or the true negative rate, measures a test's ability to correctly identify individuals who do not have the disease. It is calculated as the proportion of non-diseased individuals who test negative: Specificity = TN / (TN + FP) [82] [83]. A highly specific test is preferred for confirmatory testing, as it minimizes false positives.
There is an inherent trade-off between sensitivity and specificity; altering the cutoff value for a positive test typically increases one at the expense of the other [81] [82].
Area Under the Curve (AUC)
The Area Under the Curve (AUC), specifically under the Receiver Operating Characteristic (ROC) curve, is a single metric that summarizes the overall diagnostic performance of a test across all possible cutoff points [82] [83].
The ROC curve is a graphical plot that illustrates the relationship between a test's true positive rate (Sensitivity) and its false positive rate (1 - Specificity) at various threshold settings [81] [83]. The AUC value ranges from 0.5 to 1.0:
- AUC = 0.5: Indicates a test with no discriminatory ability, equivalent to a random guess.
- AUC = 1.0: Represents a perfect test with perfect discrimination.
- AUC ≥ 0.8: Is generally considered satisfactory for a diagnostic test [82].
The AUC is particularly valuable for comparing the diagnostic accuracy of different tests or biomarker panels and for identifying the optimal cutoff point, often chosen as the point on the curve closest to the upper-left corner of the graph [82].
Positive and Negative Predictive Values (PPV and NPV)
While sensitivity and specificity describe the test's performance, Positive Predictive Value (PPV) and Negative Predictive Value (NPV) are probability measures that are critically dependent on the prevalence of the disease in the tested population [82] [81].
- PPV is the probability that a person with a positive test result actually has the disease: PPV = TP / (TP + FP). It answers the clinical question: "Given a positive test, what is the chance the patient has the disease?" [82]
- NPV is the probability that a person with a negative test result truly does not have the disease: NPV = TN / (TN + FN). It answers: "Given a negative test, what is the chance the patient is healthy?" [82]
Table 1: Summary of Key Performance Metrics and Their Clinical Interpretation
| Metric | Definition | Formula | Clinical Interpretation | Dependence on Prevalence |
|---|---|---|---|---|
| Sensitivity | Ability to correctly identify disease | TP / (TP + FN) | Rules out disease; good for screening | No |
| Specificity | Ability to correctly identify health | TN / (TN + FP) | Rules in disease; good for confirmation | No |
| PPV | Probability of disease given a positive test | TP / (TP + FP) | Answers "Chance I am sick after a positive test?" | Yes |
| NPV | Probability of health given a negative test | TN / (TN + FN) | Answers "Chance I am well after a negative test?" | Yes |
| AUC | Overall measure of test performance across all cutoffs | Area under ROC curve | Summarizes test's discriminative power | No |
For a disease with low prevalence, even a test with high sensitivity and specificity can yield a low PPV because most positive results will be false positives [82]. Therefore, understanding the context and population is essential for interpreting PPV and NPV.
Performance Comparison of Biomarker Panels in Clinical Research
The following table summarizes the performance metrics of recently researched biomarker panels across various diseases, illustrating the application of these metrics in practice.
Table 2: Comparative Diagnostic Performance of Recent Biomarker Panels
| Disease / Condition | Biomarker Panel | Sample Type | Sensitivity | Specificity | AUC | Citation |
|---|---|---|---|---|---|---|
| Colorectal Cancer (CRC) | Methylated SDC2 + methylated SFRP1/2 | Liquid Biopsy (ctDNA) | 91.5% | 97.3% | Not specified | [85] |
| Colorectal Cancer (CRC) | Methylated SDC2 + methylated TFPI2 | Liquid Biopsy (ctDNA) | 94.9% | 98.1% | Not specified | [85] |
| Colorectal Cancer (CRC) | Mutational Panel (APC, Bat-26, KRAS, L-DNA, p53) | Liquid Biopsy (ctDNA) | 91.0% | 93.0% | Not specified | [85] |
| Pancreatic Ductal Adenocarcinoma (PDAC) | AAb Panel (CEACAM1, DPPA2, DPPA3...) | Serum | 82.8% | 68.4% | 85.0% | [25] |
| Prostate Cancer (PCa) | Urinary RNA Panel (TTC3, H4C5, EPCAM) | Urine | Not specified | Not specified | 0.92 (Validation) | [86] |
| Atrial Fibrillation (Stroke Prediction) | D-dimer, GDF-15, IL-6, NT-proBNP, hsTropT | Blood | Not specified | Not specified | 0.69 (vs. CHAâ‚‚DSâ‚‚-VASc 0.64) | [47] |
These examples demonstrate how multi-marker panels achieve high diagnostic accuracy. For instance, in colorectal cancer, combining two methylated genes in a panel yielded sensitivities and specificities above 90% [85]. Furthermore, the integration of biomarkers reflecting diverse pathophysiological pathways (e.g., myocardial injury, inflammation, coagulation) can significantly improve risk prediction models for complex conditions like atrial fibrillation, outperforming established clinical risk scores [47].
Experimental Protocols for Biomarker Validation
Workflow for Biomarker Panel Discovery and Validation
The path from biomarker discovery to clinical validation is a multi-stage process that leverages systems biology. The following diagram outlines a typical workflow that integrates in silico, in vitro, and in vivo models.
Key Methodologies in Biomarker Research
The validation of biomarker panels relies on a suite of experimental protocols designed to ensure that the panel is sensitive, specific, and reproducible.
Liquid Biopsy and Circulating Tumor DNA (ctDNA) Analysis: This non-invasive approach analyzes genetic and epigenetic alterations in ctDNA from blood, stool, or urine [85]. The protocol involves sample collection (e.g., blood draw), plasma separation, extraction of cell-free DNA, and targeted analysis using methods like quantitative PCR (qPCR) or next-generation sequencing (NGS) to detect specific mutations or methylation patterns. This method was key in validating high-performance CRC panels like methylated SDC2 and TFPI2 [85].
Autoantibody (AAb) Profiling with Protein Microarrays: This technique is used to identify a humoral immune response against tumor-specific antigens. The protocol involves fabricing microarrays with candidate antigens (e.g., cancer-testis antigens), incubating the arrays with patient serum, and detecting bound autoantibodies with fluorescently labeled secondary antibodies [25]. High-throughput analysis of fluorescence data identifies AAb signatures, as demonstrated in the discovery of a 7-biomarker AAb panel for pancreatic ductal adenocarcinoma [25].
Urinary Biomarker Analysis: For diseases like prostate cancer, urine offers a non-invasive source of biomarkers. The protocol involves collecting urine sediments, extracting RNA, and performing RNA-sequencing or qPCR to quantify candidate biomarkers [86]. This workflow identified a three-RNA panel (TTC3, H4C5, EPCAM) with an AUC of 0.92, significantly outperforming the established PCA3 test [86].
Multiplex Assays for Circulating Protein Biomarkers: Evaluating panels of protein biomarkers requires technologies that can measure multiple analytes simultaneously from a single sample. Methods like Meso Scale Discovery (MSD) electrochemiluminescence assays or customized multiplex ELISA are used [84] [47]. This approach was pivotal in studies that identified a 5-biomarker panel (including NT-proBNP, IL-6, and hsTropT) for predicting cardiovascular events in atrial fibrillation patients [47].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Biomarker Discovery and Validation
| Tool / Reagent | Function in Biomarker Research | Example Application |
|---|---|---|
| Protein Microarrays | High-throughput profiling of autoantibody responses against hundreds of antigens. | Identification of autoantibody signatures in pancreatic cancer [25]. |
| Next-Generation Sequencing (NGS) | Comprehensive genomic and transcriptomic analysis for discovery of mutations and expression changes. | Genomic characterization of patient-derived xenograft (PDX) models; mutation profiling [84]. |
| qPCR / RT-qPCR Assays | Sensitive and quantitative measurement of specific RNA or DNA targets. | Validation of urinary RNA biomarkers for prostate cancer [86]. |
| Meso Scale Discovery (MSD) / ELISA | Multiplex or single-plex quantification of protein biomarkers in solution. | Measuring circulating cytokine and cardiac biomarker levels [84] [47]. |
| Patient-Derived Xenograft (PDX) Models | In vivo models that retain the genomic and phenotypic characteristics of the original patient tumor. | Mouse clinical trials (MCTs) for evaluating drug response and biomarker correlation [84]. |
| Liquid Biopsy Kits | Standardized collection and extraction of cell-free DNA or other analytes from blood and other fluids. | Isolation of ctDNA for detection of colorectal cancer [85]. |
Advanced Statistical and Machine Learning Approaches
Modern biomarker validation extends beyond traditional statistics, incorporating advanced machine learning (ML) models to handle complex, multi-dimensional data. These approaches can identify subtle patterns and interactions within biomarker panels that may not be apparent through conventional means.
For example, in a large study of atrial fibrillation patients, researchers compared traditional Cox regression models with ML models like random forest and XGBoost. The inclusion of a biomarker panel consistently improved predictive accuracy for cardiovascular outcomes. For predicting heart failure hospitalization, the AUC of a combined Cox model increased from 0.77 to 0.80, while an XGBoost model showed an even greater improvement from 0.96 to 0.98 with the addition of biomarkers [47].
Furthermore, new methods for evaluating biomarker performance are emerging. Beyond the traditional sensitivity-specificity ROC curve, researchers are now developing and utilizing accuracy-ROC curves and precision-ROC curves. These multi-parameter ROC curves, when combined with integrated cutoff distribution diagrams, provide a more transparent and comprehensive method for identifying diagnostically optimal cutoff values that balance all relevant performance metrics simultaneously [81].
In the field of systems biology research, the validation of biomarker panels is a critical step in translating scientific discoveries into clinically useful diagnostic tools. Validation ensures that identified biomarkers are not merely statistical artifacts but are reliable, reproducible, and meaningful indicators of biological states or therapeutic responses. The process typically unfolds through phased validation protocols that progress from initial discovery to confirmation in diverse patient populations. These protocols—retrospective, prospective, and multicenter studies—each serve distinct purposes in the validation pathway and contribute unique evidence to establish a biomarker's clinical utility [87].
The evolution toward multimodal biomarker panels, which integrate complementary molecular, protein-based, and inflammatory indicators, has shown considerable promise in enhancing diagnostic accuracy beyond what single markers can achieve [87]. For instance, in prostate cancer detection, a combined model incorporating urinary microRNAs, the free-to-total PSA ratio, and inflammatory markers demonstrated significantly superior diagnostic accuracy (AUC of 0.947) compared to conventional PSA testing alone [87]. Such advancements underscore the importance of rigorous validation strategies that can adequately assess complex biomarker signatures across different study designs and patient populations.
Core Principles of Validation Study Designs
Foundational Concepts and Definitions
In biomarker validation, retrospective studies analyze previously collected data and biospecimens, while prospective studies follow participants forward in time according to a pre-defined protocol. Multicenter studies involve multiple investigative sites to enhance patient recruitment, accelerate study completion, and improve the generalizability of findings [88]. The choice among these designs involves strategic trade-offs between scientific rigor, practical feasibility, resource requirements, and ethical considerations.
A critical distinction exists between validation and verification processes. Validation establishes documented evidence providing a high degree of assurance that a specific process will consistently produce a product meeting predetermined specifications, while verification confirms that specified requirements have been fulfilled for a specific instance or batch [89]. In biomarker research, validation asks "Will this biomarker consistently perform accurately in future clinical applications?" while verification asks "Did this biomarker perform correctly in this specific experimental run?" [89].
Comparative Analysis of Study Design Attributes
Table 1: Key Characteristics of Validation Study Designs
| Design Attribute | Retrospective Study | Prospective Study | Multicenter Study |
|---|---|---|---|
| Time Direction | Backward-looking (analyzes existing data) | Forward-looking (follows participants forward) | Can be either retrospective or prospective in design |
| Typical Duration | Relatively quick | Often lengthy | Varies by design, but typically accelerated through parallel recruitment |
| Cost Considerations | Generally less expensive | Typically more resource-intensive | Higher overall costs but cost-effective per participant |
| Primary Strengths | Efficient for rare conditions; rapid insights | Establishes temporal relationships; minimizes recall bias | Enhanced generalizability; larger sample sizes |
| Key Limitations | Dependent on existing data quality; potential for biases | Resource-intensive; potential for loss to follow-up | Operational complexity; cross-site standardization challenges |
| Level of Evidence | Level 3-4 (observational) | Level 2-3 (depending on design) | Level 2-4 (enhances generalizability of underlying design) |
| Ideal Application | Initial validation; rare diseases; hypothesis generation | Confirmatory validation; establishing causality | Definitive validation; assessing generalizability |
Retrospective Study Designs: Methodology and Applications
Protocol Implementation and Workflow
Retrospective studies represent a pragmatic approach to biomarker validation, particularly valuable during initial validation phases or when investigating rare conditions where prospective enrollment would be impractical. The implementation follows a structured workflow:
Case Ascertainment: Identify appropriate cases and controls using previously collected data. This often involves using billing codes, electronic health record repositories, or previously banked biospecimens [88]. When using diagnosis codes, validation against manual chart review is essential to calculate diagnostic accuracy metrics (sensitivity, specificity, predictive values) [88].
Data Abstraction: Develop a detailed manual of operations that rigorously defines all variables and their sources to optimize data reliability [88]. This includes specifying where data elements are stored in the electronic health record, how laboratory values are measured, and how clinical variables are defined across potential source systems.
Quality Assurance: Implement overlapping data reviews (5-10% of records) when multiple abstractors are involved to evaluate interrater reliability [88]. Regular communication channels, such as video conferences and collective discussions of data issues, help maintain consistency and address emerging concerns during the abstraction process.
Technical Considerations and Bias Mitigation
Retrospective designs are susceptible to several methodological challenges that require specific mitigation strategies:
Selection Bias: Occurs when the study population is not representative of the target population [88]. Mitigation strategies include careful definition of inclusion/exclusion criteria, use of consecutive cases rather than selected cases, and transparent reporting of participant flow.
Ascertainment Bias: Arises from systematic differences in how data are collected or recorded, particularly between cases and controls [88]. Standardized data collection forms, blinded assessment of exposure status, and predefined variable definitions help minimize this bias.
Confounding: Occurs when the relationship between the biomarker and outcome is influenced by a third variable associated with both [88]. Statistical adjustments, matching strategies, and restriction can address confounding in the analysis phase.
Table 2: Data Collection Methods for Retrospective Studies
| Method | Implementation Approach | Advantages | Limitations |
|---|---|---|---|
| Manual Chart Review | Trained abstractors extract data using standardized forms | Can capture nuanced clinical information; adaptable to complex scenarios | Time-consuming; potentially expensive; subject to human error |
| Automated EHR Query | Structured query language (SQL) or other programming languages extract data directly | Efficient for large datasets; reduces human error; cost-effective for repetitive tasks | Limited to structured data fields; may miss contextual information; requires technical expertise |
| Hybrid Approach | Automated extraction supplemented by targeted manual review | Balances efficiency with completeness; allows validation of automated methods | Requires coordination between technical and clinical team members |
Prospective Study Designs: Methodology and Applications
Protocol Implementation and Workflow
Prospective study designs follow participants forward in time to observe outcomes relative to biomarker status, providing stronger evidence for causal relationships and clinical utility. The implementation involves:
Protocol Development: Create a comprehensive study protocol that specifies inclusion/exclusion criteria, sample size justification, biomarker measurement procedures, outcome assessments, and statistical analysis plans. The protocol should establish objective, measurable criteria for success before study initiation [90].
Participant Enrollment and Follow-up: Identify and consent eligible participants, then implement systematic follow-up procedures to capture predetermined endpoints. This often involves scheduled visits, standardized assessments, and protocols for handling missing data.
Biomarker Measurement and Quality Control: Establish standardized procedures for sample collection, processing, storage, and analysis. Implement batch quality control measures and blinded duplicate measurements to assess technical variability.
Technical Considerations and Advanced Methodologies
Prospective designs benefit from several methodological strengths but require careful attention to specific technical aspects:
Temporal Relationship: The forward-moving nature of prospective studies establishes that biomarker measurement precedes outcome assessment, a key requirement for establishing potential causality [91].
Standardized Data Collection: Unlike retrospective studies dependent on existing data, prospective designs allow researchers to define and implement consistent measurement protocols across all participants.
Handling of Evolving Technologies: In rapidly advancing fields like biomarker research, prospective studies must account for potential technological improvements during the study period through protocol-preserved samples or statistical adjustments.
The workflow for prospective validation studies follows a structured sequence from design through analysis, with particular attention to standardization and quality control at each phase:
Multicenter Study Designs: Methodology and Applications
Protocol Implementation and Workflow
Multicenter studies combine elements of both retrospective and prospective designs while introducing additional complexity through involvement of multiple investigative sites. These designs are particularly valuable for validating biomarker panels across diverse populations and clinical settings. Implementation requires:
Site Selection and Investigator Recruitment: Identify coinvestigators at each site who are available, interested, and have appropriate resources [88]. Research networks can facilitate this process by providing infrastructure for identifying coinvestigators and connections to funding opportunities.
Standardization Across Sites: Develop comprehensive manuals of operations, conduct training sessions, and implement regular meetings to ensure consistent case ascertainment, data collection, and variable definitions across all participating sites [88]. This is particularly important as billing practices and clinical workflows may differ across institutions.
Data Management and Quality Assurance: Establish centralized data management systems with built-in quality checks. Implement site audits and overlapping data reviews to identify systematic issues with data entry and maintain data integrity across sites [88].
Technical Considerations and Collaborative Frameworks
Multicenter studies present unique methodological challenges that require specialized approaches:
Cross-site Harmonization: Variations in clinical practices, laboratory methods, and data collection procedures across sites can introduce unwanted variability. Pre-established standard operating procedures, centralized training, and periodic site monitoring help maintain consistency [88].
Statistical Power and Generalizability: While multicenter studies enhance generalizability by including diverse populations, they also require careful attention to sample size calculations that account for potential clustering effects and between-site variability.
Regulatory and Ethical Considerations: Multicenter studies require coordination of institutional review board approvals across sites and establishment of data use agreements that define roles, responsibilities, and data sharing protocols [88].
The organizational structure of multicenter studies involves coordination between central and site-specific teams, with clear communication channels and standardized processes:
Experimental Data and Performance Comparison
Case Study: Urinary Biomarker Panel for Prostate Cancer Detection
A 2025 multicenter study exemplifies the application of phased validation protocols for a multimodal urinary biomarker panel for prostate cancer detection [87]. The research employed a retrospective design across multiple centers involving 307 men divided into three groups: 112 with confirmed prostate cancer, 98 with benign prostatic hyperplasia, and 97 healthy controls [87]. The study measured serum PSA levels, inflammatory markers, and five urinary extracellular vesicle-derived miRNAs to develop and validate an integrated diagnostic model.
The performance of individual biomarkers versus the combined panel demonstrated the superiority of multimodal approaches:
Table 3: Performance Metrics of Individual Biomarkers Versus Combined Panel
| Biomarker | Area Under Curve (AUC) | Sensitivity | Specificity | Clinical Context |
|---|---|---|---|---|
| Standard PSA | 0.70-0.75 (literature estimates) | ~85% | ~20% | Limited specificity in gray zone |
| f/tPSA Ratio | 0.829 | 89% (literature) | 60% (literature) | Improved but suboptimal discrimination |
| miR-21-5p | 0.76 | Not reported | Not reported | Single miRNA marker |
| miR-141-3p | 0.74 | Not reported | Not reported | Single miRNA marker |
| Combined Panel | 0.947 | 92.9% | 88.7% | Integrated model |
| Panel in Gray Zone | 0.92-0.94 | >90% | >85% | Clinically challenging range |
The combined panel integrated miR-21-5p, miR-375, free-to-total PSA ratio, PSA density, and neutrophil-to-lymphocyte ratio, demonstrating significantly enhanced diagnostic accuracy compared to conventional approaches (P < 0.001) [87]. Notably, it exhibited exceptional performance within the diagnostically challenging PSA "gray zone" (4-10 ng/mL), where traditional screening methods often lead to diagnostic uncertainty and unnecessary biopsies.
Comparative Performance Across Study Designs
The evidentiary strength of biomarker validation progresses through sequential study designs, each contributing to different aspects of validation:
Table 4: Evidentiary Progression Across Study Designs
| Validation Phase | Typical Study Design | Primary Research Question | Sample Size Considerations | Regulatory Implications |
|---|---|---|---|---|
| Discovery | Retrospective, single-center | Does the biomarker show promising discrimination? | Limited by available samples | Preliminary evidence only |
| Initial Validation | Retrospective, multicenter | Does the biomarker perform consistently across settings? | Hundreds of participants | Supports further investment |
| Confirmatory | Prospective, single-center | Does the biomarker predict outcomes in a controlled setting? | Adequately powered for primary endpoint | May support limited claims |
| Definitive | Prospective, multicenter | Is the biomarker generalizable to broad populations? | Large-scale, diverse populations | Supports regulatory approval |
Research Reagent Solutions and Essential Materials
The implementation of phased validation protocols requires specific research reagents and technical solutions tailored to each study design. The following toolkit represents essential materials for executing biomarker validation studies:
Table 5: Research Reagent Solutions for Biomarker Validation
| Reagent/Material | Function | Application Context | Technical Considerations |
|---|---|---|---|
| Urinary Extracellular Vesicle Isolation Kits | Isolation of miRNA-containing vesicles from urine | Molecular biomarker studies | Stability in urine; protection against degradation [87] |
| miRNA Quantification Assays | Measurement of specific miRNA expression levels | All study designs | Standardization of collection protocols and RNA isolation methods [87] |
| Multiplex Immunoassay Platforms | Simultaneous measurement of multiple protein biomarkers | Prospective and multicenter studies | Cross-site standardization; batch effect correction |
| Digital Pathology Platforms | AI-driven image interpretation and digital reporting | Retrospective tissue-based studies | Bridge between imaging and molecular biomarker workflows [14] |
| Electronic Data Capture Systems | Standardized data collection across multiple sites | Multicenter studies | HIPAA-compliance; branching logic; field validation [88] |
| Statistical Validation Tools | Open-source web applications for cohort validation | In-silico trial supplement | R-Shiny environments; menu-driven interfaces [92] |
| Liquid Biopsy Technologies | Non-invasive circulating biomarker analysis | Prospective longitudinal studies | Sensitivity/specificity enhancements; real-time monitoring [50] |
Integrated Validation Framework and Future Directions
The strategic integration of retrospective, prospective, and multicenter designs creates a comprehensive validation framework for biomarker panels in systems biology research. This phased approach efficiently balances scientific rigor with practical feasibility, progressing from initial proof-of-concept to definitive generalizable evidence.
Emerging methodologies are enhancing traditional validation approaches. In-silico trials using virtual cohorts present a promising avenue for addressing challenges in clinical research, potentially reducing duration, costs, and ethical implications while providing more detailed information on potential outcomes [92]. The integration of artificial intelligence and machine learning in biomarker analysis enables more sophisticated predictive models that can forecast disease progression and treatment responses based on biomarker profiles [50]. Additionally, multi-omics approaches that leverage data from genomics, proteomics, metabolomics, and transcriptomics are creating more comprehensive biomarker signatures that reflect the complexity of diseases [50] [14].
The future of biomarker validation will increasingly emphasize patient-centric approaches that incorporate patient-reported outcomes and engage diverse populations to enhance the relevance and applicability of biomarkers across different demographics [50]. Furthermore, advances in single-cell analysis technologies will provide deeper insights into tumor microenvironments and facilitate identification of rare cell populations that may drive disease progression or resistance to therapy [50]. These technological innovations, combined with robust phased validation protocols, will accelerate the translation of biomarker discoveries from systems biology research into clinically impactful diagnostic tools that improve patient outcomes.
Hepatocellular carcinoma (HCC) remains a major global health challenge, ranking as the third leading cause of cancer-related mortality worldwide [93]. The prognosis for HCC patients is highly dependent on early detection, with 5-year survival rates exceeding 60% for early-stage diagnosis compared to below 10% for advanced-stage detection [93]. Current international guidelines recommend semi-annual surveillance for at-risk patients using abdominal ultrasound, often combined with the serum biomarker alpha-fetoprotein (AFP). However, the sensitivity of ultrasound for early-stage HCC detection remains suboptimal at approximately 45% when used alone and only 63% when combined with AFP [93]. This limitation has fueled the development of more sophisticated multimarker algorithms that integrate demographic variables with multiple biomarkers to improve early detection capabilities.
The GALAD (Gender, Age, AFP-L3, AFP, and DCP) and GAAD (Gender, Age, AFP, and DCP) systems represent two prominent algorithmic approaches that have shown promise in overcoming the limitations of single-marker strategies. These models leverage the complementary strengths of multiple biomarkers while incorporating demographic risk factors to enhance diagnostic performance. Understanding the comparative performance, methodological considerations, and clinical validation status of these algorithms is crucial for researchers and drug development professionals working in the field of hepatology and cancer biomarker discovery. This analysis examines the lessons learned from HCC detection regarding the validation of biomarker panels through the comparative lens of GAAD versus GALAD, framed within a systems biology research context.
Algorithm Composition and Theoretical Foundations
Component Analysis
The GALAD and GAAD algorithms share common elements but differ in their specific constituent markers and underlying mathematical structures:
GALAD Algorithm Components:
- Demographic variables: Gender (biological sex), age
- Serological biomarkers: AFP, AFP-L3 (Lens culinaris agglutinin-reactive fraction of AFP), DCP (des-gamma-carboxy prothrombin, also known as PIVKA-II)
GAAD Algorithm Components:
- Demographic variables: Gender (biological sex), age
- Serological biomarkers: AFP, DCP/PIVKA-II
The fundamental distinction lies in the inclusion of AFP-L3 in the GALAD score, which is omitted from the GAAD algorithm. This difference stems from research suggesting that the AFP-L3 variable may have a negligible contribution in some populations, as the odds ratio for AFP-L3 barely exceeded 1 in both discovery and validation datasets for GALAD [94]. From a systems biology perspective, these algorithms integrate distinct but overlapping biological pathways: AFP represents an oncofetal glycoprotein, AFP-L3 reflects a fucosylated glycoform associated with malignant transformation, and DCP/PIVKA-II indicates abnormal prothrombin production resulting from impaired vitamin K metabolism in hepatocellular carcinoma [95].
Algorithm Implementation and Workflow
The GAAD algorithm implementation offers two distinct workflow options [94]:
- Manual data entry through a dedicated web portal
- Automated calculation via integration with the NAVIFY Algorithm suite, which automatically retrieves biomarker data from Laboratory Information Systems, Hospital Information Systems, and/or Electronic Medical Records
This dual approach enhances flexibility for both research and clinical environments, facilitating broader implementation across diverse healthcare settings. The GALAD algorithm typically generates a probability score between 0 and 1, while the GAAD algorithm produces a semi-quantitative result based on its specific mathematical formula [94].
Performance Comparison and Meta-Analysis Evidence
Comprehensive Meta-Analysis Findings
A recent systematic review and meta-analysis of 44 studies (n=33,100 patients) provides the most comprehensive comparison of these multimarker panels, examining 37 studies of GALAD, 12 of GAAD, and 11 of the related ASAP score [96] [93]. The pooled analysis revealed remarkably similar performance characteristics between GALAD and GAAD for early-stage HCC detection.
Table 1: Pooled Performance of Multimarker Algorithms for Early-Stage HCC Detection from Meta-Analysis
| Algorithm | Pooled Sensitivity | Pooled Specificity | Number of Studies | AUC Range |
|---|---|---|---|---|
| GALAD | 70.1% - 74.1% | 83.3% - 87.2% | 37 | 0.78 - 0.89 |
| GAAD | 70.1% - 74.1% | 83.3% - 87.2% | 12 | 0.83 - 0.91 |
| ASAP | 70.1% - 74.1% | 83.3% - 87.2% | 11 | 0.83 - 0.89 |
Among studies directly comparing biomarker panels, the meta-analysis found no statistically significant difference in sensitivity for early-stage HCC detection between GALAD and GAAD (relative risk 0.96, 95% CI: 0.80-1.15) [96] [93]. This indicates that both algorithms provide comparable detection capabilities for early-stage disease despite their compositional differences.
Head-to-Head Comparative Studies
Several direct comparative studies provide additional insights into the relative performance of these algorithms across different patient populations:
Table 2: Head-to-Head Comparison of GALAD and GAAD Performance Across Studies
| Study Population | GALAD AUC (Early HCC) | GAAD AUC (Early HCC) | Superior Performer | Key Findings |
|---|---|---|---|---|
| Mixed CLD Etiologies [97] | 0.825 | 0.889 | GAAD | GAAP (similar to GAAD) demonstrated best accuracy for early HCC |
| International Validation [94] | 0.847* | 0.907* | Comparable | Similar performance across disease stages and etiologies |
| Vietnamese Population [98] | N/A | 0.983 | GAAD | GAAD showed 86.7% sensitivity, 98.4% specificity |
*Values approximated from study data
A study enrolling 529 patients (193 with HCC) found that the GAAP score (closely related to GAAD) achieved the best accuracy in detecting early HCC in patients with chronic liver diseases (AUC 0.889), outperforming GALAD (AUC 0.825) and ASAP (AUC 0.839) [97]. The GAAP and GALAD scores were most effective in patients with nonviral etiologies, while GAAP and ASAP performed best in viral hepatitis subgroups [97].
Experimental Protocols and Validation Methodologies
GAAD Algorithm Development and Validation
The development and validation of the GAAD algorithm followed a rigorous prospective design across international centers [94]:
Participant Selection:
- Algorithm Development Cohort: 1,084 participants (309 HCC cases, 40.7% early-stage; 736 controls) recruited from clinics in Germany, Spain, Thailand, and Hong Kong (2014-2016)
- Clinical Validation Cohort: 877 participants (366 HCC cases, 47.6% early-stage; 303 controls) recruited from centers in China, Germany, Thailand, Hong Kong, and Japan (2017-2022)
- Inclusion Criteria: Patients aged ≥18 years with HCC (confirmed radiologically or histologically within 6 months) or chronic liver disease (cirrhosis or non-cirrhotic chronic HBV/HCV, alcohol-associated liver disease, or NASH)
- Exclusion Criteria: Other cancers (except non-melanoma skin cancer), recurrent HCC, previous/current HCC treatment, renal impairment (GFR <60 mL/min/1.73 m²), anti-vitamin K anticoagulant therapy
Sample Processing and Analysis:
- Serum samples collected via blood draw ≥1 day before any procedures involving general anesthesia
- Storage at -70°C before shipment on dry ice to centralized testing facilities
- Analysis performed using Elecsys PIVKA-II and AFP assays on cobas e 601 analyzers over three experimental runs
- GAAD algorithm calculated through web-based tool or automated NAVIFY Algorithm suite integration
Statistical Methods:
- Receiver operating characteristic (ROC) curve analyses to calculate area under the curve (AUC)
- Sensitivity and specificity with 95% confidence intervals calculated using Clopper-Pearson method
- Comparison between methods using one-sided McNemar test
- Establishment of GAAD cutoff score of 2.57 for optimal performance
This validation study demonstrated consistently strong performance, with AUC for differentiation between early-stage HCC and chronic liver disease of 90.7% in the development cohort and 91.4% in the validation cohort, with sensitivity of 71.8% and 70.1% respectively at 90.0% and 93.7% specificity [94].
GALAD Phase 3 Validation Study Protocol
A recent phase 3 biomarker validation study for GALAD followed similarly rigorous methodology [99]:
Study Design:
- Prospective multicenter study of 1,558 patients with cirrhosis followed for median 2.2 years
- Seven participating centers with regular 6-month HCC surveillance per site guidelines
- Blood collected for biomarker research at each follow-up visit and stored in biorepository
- Measurements of AFP, AFP-L3, and DCP performed in a central laboratory (FujiFilm) by staff blinded to clinical data
- Retrospective evaluation of GALAD performance within 12 months before clinical HCC diagnosis
Primary Findings:
- 109 patients developed HCC (76 very early or early stage) with annual incidence rate of 2.4%
- AUC for AFP and GALAD within 12 months before HCC were 0.66 and 0.78 respectively (P<.001)
- At 82% specificity, GALAD showed 62% sensitivity at 12 months before HCC diagnosis versus 41% for AFP (P=.001)
This phase 3 validation confirms that GALAD significantly outperforms AFP alone for early HCC detection in a prospective surveillance setting [99].
Figure 1: Biological Pathways of HCC Biomarkers - This diagram illustrates the distinct biological pathways reflected by the serum biomarkers used in GALAD and GAAD algorithms
Biomarker Integration from a Systems Biology Perspective
The development of multimarker panels like GALAD and GAAD represents a shift from reductionist single-marker approaches to integrated systems biology frameworks. This perspective recognizes that hepatocarcinogenesis involves multiple molecular pathways that manifest in diverse serum biomarker profiles.
Complementary Pathway Coverage
The biomarkers in these algorithms capture complementary aspects of hepatocellular pathophysiology:
AFP: An oncofetal glycoprotein expressed in proliferating hepatocytes, representing dedifferentiation and malignant transformation [95]. It demonstrates modest standalone sensitivity but provides fundamental information about hepatocyte proliferation status.
DCP/PIVKA-II: An abnormal prothrombin molecule resulting from impaired vitamin K metabolism in malignant hepatocytes, which correlates with invasive tumor behavior and angiogenesis [94] [95]. This biomarker operates on a distinct pathway from AFP and can detect HCC cases that might be missed by AFP alone.
AFP-L3: A fucosylated glycoform of AFP that reflects altered glycosylation patterns associated with malignant transformation [95]. This glycosylation change represents a separate biological process from mere AFP overexpression.
From a systems biology standpoint, the GAAD algorithm captures two major pathways of hepatocarcinogenesis (malignant transformation and vitamin K metabolism), while GALAD adds a third dimension (protein glycosylation alterations). However, the comparable performance between the two algorithms suggests potential redundancy in the additional pathway captured by AFP-L3 in some populations, or the need for population-specific optimization.
Algorithm Performance Across Disease Etiologies
The performance of both GALAD and GAAD varies across different underlying liver disease etiologies, reflecting the biological heterogeneity of HCC:
Viral Hepatitis: Both algorithms demonstrate strong performance in HBV and HCV populations, with one study showing GAAD and ASAP performing best for viral hepatitis subgroups [97].
Non-Viral Liver Disease: With the shifting epidemiology of liver disease toward metabolic dysfunction-associated steatotic liver disease (MASLD) and alcohol-related liver disease, performance in non-viral etiologies becomes increasingly important. Both GALAD and GAAD maintain effectiveness in these populations, with one study showing GAAD and GALAD as most effective for nonviral etiologies [97].
This variation in performance across etiologies underscores the biological complexity of HCC and supports a systems approach that acknowledges the different molecular pathways that may predominate in HCC arising from different underlying liver diseases.
Figure 2: Experimental Workflow for Algorithm Validation - This diagram outlines the standardized methodology for developing and validating HCC detection algorithms
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Materials and Platforms for HCC Biomarker Studies
| Category | Specific Products/Platforms | Research Application | Key Features |
|---|---|---|---|
| Immunoassay Systems | Elecsys PIVKA-II and AFP assays on cobas e 601 analyzer | Biomarker quantification | Standardized measurements for algorithm inputs |
| ARCHITECT i2000SR analyzer with AFP and PIVKA-II assays | High-throughput biomarker testing | CE-marked assays for clinical validation studies | |
| Algorithm Platforms | NAVIFY Algorithm Suite | Automated algorithm calculation | Integration with LIS/HIS/EMR for workflow efficiency |
| GAAD Web Tool | Manual data entry and calculation | Research flexibility without system integration | |
| Sample Processing | Standard -70°C freezer systems | Sample preservation | Maintains biomarker stability for longitudinal studies |
| Controlled temperature monitoring systems | Sample quality assurance | Ensures pre-analytical consistency | |
| Reference Materials | Characterized serum panels from well-phenotyped patients | Assay validation | Includes early-stage HCC, cirrhosis, and chronic liver disease |
The comparative analysis of GALAD and GAAD algorithms reveals important lessons for multimarker panel validation in hepatocellular carcinoma detection. Both algorithms demonstrate significantly improved performance over single biomarkers like AFP alone, with pooled sensitivities of 70-74% and specificities of 83-87% for early-stage HCC detection in meta-analyses [96] [93]. The similar performance between these algorithms, despite differences in their constituent biomarkers, suggests that robust HCC detection can be achieved through different combinations of demographic and biomarker data.
From a systems biology perspective, the development and validation of these algorithms highlight several key principles:
- Pathway Complementarity: Effective multimarker panels should capture distinct biological pathways involved in carcinogenesis
- Population Considerations: Algorithm performance varies across different etiologies and geographic populations
- Validation Rigor: Phase 3 prospective studies in intended-use populations are essential for clinical translation
Future research directions should focus on further refinement of these algorithms for specific subpopulations, integration with novel biomarkers including circulating tumor DNA and methylated DNA markers [95] [100], and combination with artificial intelligence-based image analysis for enhanced detection. The ongoing validation and refinement of these multimarker panels represents a paradigm shift in HCC detection that moves beyond single-marker approaches toward integrated systems biology frameworks.
For researchers and drug development professionals, these algorithms offer validated platforms for early HCC detection that can be incorporated into clinical trial designs for high-risk populations, potentially serving as enrichment strategies for HCC prevention trials or as monitoring tools during drug development.
In the realm of modern drug development and personalized medicine, biomarkers have emerged as indispensable tools for optimizing patient care. The clinical validation of biomarkers, particularly within the context of systems biology research, requires a fundamental understanding of two distinct categories: prognostic and predictive biomarkers. According to the FDA-NIH Biomarker Working Group, a prognostic biomarker is used to identify the likelihood of a clinical event, disease recurrence, or progression in patients who already have the disease or medical condition of interest [101]. In contrast, a predictive biomarker identifies individuals who are more likely than similar individuals without the biomarker to experience a favorable or unfavorable effect from exposure to a medical product or environmental agent [101].
This distinction is not merely academic; it fundamentally impacts clinical trial design, therapeutic decision-making, and regulatory approvals. The complexity of multifactorial diseases, especially in areas like oncology and psychiatry, has driven a shift from single-target biomarkers toward comprehensive biomarker panels that integrate various sources of biomolecular and clinical data [2]. Systems biology approaches facilitate the discovery and validation of these panels by leveraging multi-omics data (genomics, proteomics, metabolomics) and computational analyses to achieve a holistic understanding of disease mechanisms [50] [2].
Fundamental Distinctions Between Prognostic and Predictive Biomarkers
Definitions and Clinical Applications
Prognostic and predictive biomarkers serve different clinical purposes and are validated through distinct methodological approaches. The table below summarizes their key characteristics:
Table 1: Key Characteristics of Prognostic and Predictive Biomarkers
| Characteristic | Prognostic Biomarker | Predictive Biomarker |
|---|---|---|
| Primary Function | Provides information on natural disease history and outcome regardless of therapy | Identifies response or lack of response to a specific therapeutic intervention |
| Clinical Question | "What is this patient's likely disease course?" | "Will this patient benefit from this specific treatment?" |
| Validation Requirement | Often identified from observational data in untreated patients | Requires comparison of treatment to control in patients with and without the biomarker |
| Informs | Disease prognosis and stratification | Treatment selection |
| Example | MMP9 expression in glioblastoma multiforme indicates aggressive disease [58] | BRAF V600E mutation predicts response to vemurafenib in melanoma [101] |
Methodological Requirements for Validation
Differentiating between these biomarker types requires specific clinical validation designs. A biomarker's status cannot be determined by studying only patients who have received a particular therapy [101]. The following workflow illustrates the fundamental analytical approach required to distinguish prognostic from predictive biomarkers:
Diagram 1: Clinical Trial Design for Biomarker Validation
As illustrated in Diagram 1, proper classification requires a 2x2 factorial design that compares treatment effects across biomarker-defined subgroups. In this design:
- Prognostic effect: Evident when outcomes differ between biomarker-positive and biomarker-negative groups receiving the same control therapy [101]
- Predictive effect: Present when the treatment effect size differs significantly between biomarker-positive and biomarker-negative groups [101]
Statistical analysis focuses on testing the treatment-by-biomarker interaction, which can be quantitative (differing magnitude of benefit) or qualitative (benefit in one subgroup but not the other) [101].
Experimental Protocols for Biomarker Validation
Systems Biology Approaches for Biomarker Panel Discovery
The validation of biomarker panels using systems biology research involves sophisticated computational and experimental methodologies. Recent advances have demonstrated the power of integrated bioinformatics approaches for novel biomarker discovery, particularly for complex diseases like glioblastoma multiforme (GBM) [58]. The following workflow outlines a comprehensive systems biology protocol for identifying and validating novel biomarker panels:
Diagram 2: Systems Biology Workflow for Biomarker Discovery
This workflow was implemented in a recent study on glioblastoma multiforme, which identified matrix metallopeptidase 9 (MMP9) as a key hub biomarker gene through the following detailed protocol [58]:
Data Retrieval and Preprocessing
- Microarray Data Collection: Researchers retrieved gene expression profile GSE11100 from the Gene Expression Omnibus (GEO) database, containing 22 samples (10 healthy brain regions, 12 malignant regions) [58]
- Platform Specification: Data was generated using the GPL570 Affymetrix Human Genome U133 Plus 2.0 Array [58]
- Quality Control: Implemented using the Network Analyst web server tool to normalize data and remove technical artifacts [58]
Identification of Differentially Expressed Genes (DEGs)
- Statistical Analysis: Applied p-values and false discovery rates (FDR) to identify statistically significant expression changes [58]
- Result: Identified 132 significant DEGs, with 13 upregulated and 29 uniquely downregulated genes showing statistically significant changes [58]
- Visualization: Created heatmaps and performed principal component analysis (PCA) to visualize expression patterns [58]
Protein-Protein Interaction (PPI) Network Construction
- Network Analysis: Built PPI networks specifically focused on DEGs using STRING database and Cytoscape [58]
- Hub Gene Identification: Applied network topology algorithms (degree, betweenness, closeness centrality) to identify MMP9 as the highest-degree hub biomarker, followed by POSTN and HES5 [58]
- Module Analysis: Extracted densely connected subnetwork modules for functional analysis [58]
Functional and Pathway Enrichment
- Enrichment Analysis: Mapped hub genes to KEGG pathways and Gene Ontology (GO) terms, revealing significant enrichment in extracellular matrix organization and signaling pathways [58]
- Transcription Factor Mapping: Identified key transcription factors and kinases regulating the hub biomarker genes [58]
Survival and Clinical Correlation
- Survival Analysis: Performed Kaplan-Meier analysis demonstrating significant association between hub biomarker expression and patient survival [58]
- Therapeutic Association: Mapped known drugs to hub biomarkers, identifying potential therapeutic candidates including marimastat and temozolomide for MMP9 inhibition [58]
Analytical Methods for Differentiating Biomarker Types
The statistical differentiation between prognostic and predictive biomarkers requires specific analytical approaches applied to clinical trial data:
Table 2: Analytical Methods for Biomarker Differentiation
| Method | Application | Interpretation |
|---|---|---|
| Subgroup Analysis | Compare treatment effects in biomarker-positive vs biomarker-negative subgroups | Significant interaction indicates predictive effect |
| Interaction Test | Statistical test for treatment-by-biomarker interaction | p < 0.05 suggests qualitative or quantitative interaction |
| Survival Analysis | Kaplan-Meier curves and Cox proportional hazards models | Parallel curves in control group suggest prognostic effect |
| Multivariable Regression | Models including treatment, biomarker, and interaction terms | Coefficient for interaction term quantifies predictive effect |
The fundamental principle is that prognostic biomarkers show consistent effects across treatment groups (main effect), while predictive biomarkers demonstrate differential effects across subgroups (interaction effect) [101]. This is visually apparent in survival curve patterns where:
- Purely prognostic biomarkers: Show separation between biomarker-positive and biomarker-negative groups within both treatment and control arms, with parallel curves suggesting similar relative treatment benefit regardless of biomarker status [101]
- Purely predictive biomarkers: Demonstrate different treatment effects across biomarker subgroups, with crossing survival curves indicating qualitative interactions [101]
Research Reagent Solutions for Biomarker Validation
The implementation of biomarker discovery and validation protocols requires specific research reagents and platforms. The following table details essential solutions for systems biology-based biomarker research:
Table 3: Essential Research Reagents and Platforms for Biomarker Validation
| Reagent/Platform | Function | Application in Biomarker Research |
|---|---|---|
| Affymetrix Microarray Platforms | Genome-wide gene expression profiling | Identification of differentially expressed genes (e.g., HG-U133 Plus 2.0 Array) [58] |
| Network Analysis Tools | Construction and analysis of biological networks | Protein-protein interaction mapping and hub gene identification [58] |
| STRING Database | Protein-protein interaction data repository | PPI network construction for candidate biomarkers [58] |
| Cytoscape | Network visualization and analysis | Hub biomarker identification and module extraction [58] |
| Multi-omics Integration Platforms | Combined analysis of genomic, proteomic, metabolomic data | Comprehensive biomarker panel development [50] [2] |
| Molecular Docking Software | Computational prediction of drug-biomarker interactions | Screening potential therapeutic agents for hub biomarkers [58] |
| Digital Biomarker Technologies | Sensor-based physiological monitoring | Development of novel digital biomarkers for clinical trials [102] |
| Liquid Biopsy Platforms | Non-invasive biomarker detection from blood | Real-time monitoring of treatment response [50] |
Emerging technologies are further transforming biomarker research. By 2025, enhanced integration of artificial intelligence and machine learning is expected to revolutionize biomarker analysis through sophisticated predictive models and automated data interpretation [50]. Additionally, liquid biopsy technologies with enhanced sensitivity and specificity are poised to become standard tools for non-invasive biomarker assessment across multiple disease areas [50].
Case Studies and Clinical Applications
Exemplary Biomarkers in Oncology
The clinical application of properly validated biomarkers has transformed therapeutic approaches in multiple disease areas:
BRAF V600E in Melanoma: This predictive biomarker identifies patients who will respond favorably to BRAF inhibitors like vemurafenib. Its development was so compelling that definitive clinical trials were performed only in populations enriched for this putative predictive biomarker [101]
MMP9 in Glioblastoma: Research using systems biology approaches identified matrix metallopeptidase 9 (MMP9) as a central hub biomarker in glioblastoma multiforme. Molecular docking studies demonstrated high binding affinities of potential therapeutic agents including carmustine (-6.3 kcal/mol), lomustine (-7.4 kcal/mol), marimastat (-7.7 kcal/mol), and temozolomide (-8.7 kcal/mol) to MMP9 [58]
Microvasculature Imaging Biomarkers: Quantitative high-definition microvessel imaging (HDMI) derives vessel morphological parameters (tortuosity, density, diameter) as imaging biomarkers for thyroid cancer detection, achieving AUC of 0.9005 with 77.78% sensitivity and 94.74% specificity in classifying malignant nodules [103]
Emerging Trends in Biomarker Research
The field of biomarker research continues to evolve with several significant trends:
Multi-omics Integration: Researchers increasingly leverage combined data from genomics, proteomics, metabolomics, and transcriptomics to achieve comprehensive biomarker signatures that reflect disease complexity [50] [2]
Digital Biomarkers: Sensor-derived measurements from wearable devices and digital health technologies are creating new categories of biomarkers for continuous, real-world monitoring of disease progression and treatment response [102]
Patient-Centric Approaches: Incorporation of patient-reported outcomes into biomarker studies provides valuable insights into treatment effectiveness from the patient perspective [50]
The rigorous differentiation between prognostic and predictive biomarkers represents a cornerstone of modern precision medicine. Through the application of systems biology approaches, researchers can now develop comprehensive biomarker panels that more accurately reflect the complexity of human diseases. The experimental protocols and analytical frameworks outlined in this guide provide a roadmap for proper biomarker validation, emphasizing the critical importance of study design and statistical analysis in establishing clinical utility. As biomarker science continues to evolve, integrating multi-omics data, artificial intelligence, and digital health technologies, the potential for biomarkers to transform drug development and clinical practice continues to expand, offering new opportunities for personalized therapeutic interventions.
Conclusion
The integration of systems biology into biomarker validation represents a fundamental shift from a reductionist to a holistic approach, essential for tackling complex human diseases. By synthesizing the key intents, it is clear that successful validation hinges on a multi-faceted strategy: a foundational understanding of disease networks, robust methodological integration of computational and experimental tools, proactive troubleshooting of analytical challenges, and rigorous statistical and clinical validation in diverse cohorts. Future directions will be driven by advances in artificial intelligence for data integration, the standardization of multi-omics workflows, and the broader adoption of in silico trials. This progression will accelerate the development of clinically actionable biomarker panels, ultimately enabling earlier disease detection, more personalized therapeutic strategies, and improved patient outcomes in precision medicine.
References
- 1. Systems biology and the discovery of diagnostic biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/mid/NIHMS259366/]
- 2. Human disease biomarker panels through systems biology [https://pmc.ncbi.nlm.nih.gov/articles/PMC8724340/]
- 3. Multibiomarker panels in liquid biopsy for early detection of ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-024-03166-w]
- 4. Comparison of single-marker and multi-marker tests in rare ... [https://pubmed.ncbi.nlm.nih.gov/28562689/]
- 5. Power of Single- vs. Multi-Marker Tests of Association - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3708310/]
- 6. Capturing the Elusive: Why Multi-Protein Biomarkers Tests ... [https://www.clinicallab.com/capturing-the-elusive-why-multi-protein-biomarkers-tests-are-the-future-of-measuring-ms-progression-28477]
- 7. Validation of a Biomarker Panel and Longitudinal ... [https://www.sciencedirect.com/science/article/pii/S1048891X24021893]
- 8. Unbiased estimation of biomarker panel performance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4974170/]
- 9. Systems biology and the discovery of diagnostic biomarkers [https://pubmed.ncbi.nlm.nih.gov/20534905/]
- 10. Systems biology platform for efficient development and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12341954/]
- 11. Biomarker definitions and their applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5813875/]
- 12. How Biomarkers Can Improve the Drug Development ... [https://www.fda.gov/drugs/biomarker-qualification-program/biomarker-qualification-program-educational-module-series-module-2-how-biomarkers-can-improve-drug]
- 13. Mechanisms of Disease: biomarkers and molecular targets ... [https://www.nature.com/articles/ncpuro0946]
- 14. Insights from Biomarkers & Precision Medicine 2025 [https://www.signifyresearch.net/insights/biomarkers-billions-and-breakthroughs-insights-from-biomarkers-precision-medicine-2025/]
- 15. Mechanism-based biomarker discovery [https://www.sciencedirect.com/science/article/abs/pii/S1359644617301915]
- 16. A system biology approach based on metabolic biomarkers ... [https://www.nature.com/articles/s41598-021-93653-3]
- 17. Multi-Omics Biomarker Integration: A Systems Approach [https://www.motif.bio/blog/multi-omics-biomarker-integration-2025]
- 18. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 19. Metabolomics: Insights for Disease Mechanisms & ... [https://esmed.org/metabolomics-insights-for-disease-mechanisms-biomarkers/]
- 20. Editorial: Systems Biology and Omics Approaches for ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.896818/full]
- 21. Current Bioinformatics Tools in Precision Oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12238682/]
- 22. Current and Future Applications in the Nutritional Sciences [https://www.sciencedirect.com/science/article/pii/S2161831322009413]
- 23. The Global Neurodegeneration Proteomics Consortium [https://pmc.ncbi.nlm.nih.gov/articles/PMC12353841/]
- 24. Preclinical vs. Clinical Biomarkers: Understanding Their ... [https://blog.crownbio.com/preclinical-vs-clinical-biomarkers-understanding-their-distinct-roles-in-drug-development]
- 25. Identification and validation of a novel autoantibody ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1494446/full]
- 26. Identification and validation of a novel autoantibody ... [https://pubmed.ncbi.nlm.nih.gov/39949781/]
- 27. Development of a serum protein biomarker panel for the ... [https://www.nature.com/articles/s41598-025-19631-1]
- 28. A novel autoantibody signatures for enhanced clinical ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-023-03107-1]
- 29. The identification of auto-antibodies in pancreatic cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3130890/]
- 30. A biological function based biomarker panel optimization ... [https://www.nature.com/articles/s41598-019-43779-2]
- 31. A Diagnostic Test Accuracy Review and Meta-Analysis [https://pubmed.ncbi.nlm.nih.gov/40185645/]
- 32. Protein microarrays for systems biology - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7117600/]
- 33. Comparison of immunoassay- with mass spectrometry-derived ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-023-00689-2]
- 34. Current landscape of plasma proteomics from technical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462477/]
- 35. Data Analysis Strategies for Protein Microarrays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5003438/]
- 36. Mass spectrometry based biomarker discovery, verification ... [https://www.sciencedirect.com/science/article/pii/S1574789114000544]
- 37. Protein Microarrays and Biomarkers of Infectious Disease [https://www.mdpi.com/1422-0067/11/12/5165]
- 38. Protein Significance Analysis in Selected Reaction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3322573/]
- 39. PRM vs MRM: A Comparative Guide to Targeted ... [https://www.metwarebio.com/prm-vs-mrm-targeted-ms-comparison/]
- 40. From blood drops to biomarkers: a scoping review of ... [https://clinicalproteomicsjournal.biomedcentral.com/articles/10.1186/s12014-025-09540-w]
- 41. A Novel Hybrid High-Speed Mass Spectrometer Allows ... [https://www.sciencedirect.com/science/article/pii/S1535947625001495]
- 42. Harnessing Mass Spectrometry for Biomarker Discovery in ... [https://blog.crownbio.com/biomarker-and-mass-spectrometry-aml]
- 43. Integrating Proteomics with Metabolomics: A Multi-Omics ... [https://www.metwarebio.com/integrating-proteomics-with-metabolomics-a-multi-omics-strategy-for-systems-biology/]
- 44. Exploring lipidomics in biomarker discovery [https://www.sciencedirect.com/science/article/pii/S0009898125005777?dgcid=rss_sd_all]
- 45. In Silico Models: From Simple Networks to Complex Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC7149665/]
- 46. Systems biology platform for efficient development and ... [https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2023.1229532/full]
- 47. Biomarker panels for improved risk prediction and ... [https://www.nature.com/articles/s41467-025-62218-7]
- 48. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 49. Advancing the frontier of rare disease modeling: a critical ... [https://www.nature.com/articles/s41746-025-02068-1]
- 50. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 51. In Silico Models in Oncology: Validating AI-Driven ... [https://blog.crownbio.com/in-silico-models-in-oncology-validating-ai-driven-predictive-frameworks]
- 52. Preclinical Mouse Cancer Models: A Maze of Opportunities ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4583714/]
- 53. PDX Mouse Clinical Trials [https://www.crownbio.com/pdx-mouse-clinical-trials]
- 54. Patient-derived xenografts: a relevant preclinical model for ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-016-0462-4]
- 55. Ultimate Guide: Designing a Mouse Clinical Trial & Data ... [https://blog.championsoncology.com/blog/the-ultimate-guide-to-designing-a-mouse-clinical-trial-and-data-analysis]
- 56. Mouse Clinical Trials (MCTs) [https://www.championsoncology.com/mouse-clinical-trials?hsLang=en]
- 57. A beginner's guide into curated analyses of open access ... [https://www.nature.com/articles/s41597-023-02338-1]
- 58. System biology approach to identify the novel biomarkers ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1364138/full]
- 59. . Coefficient Example... | Medium of Variation Coefficient of variation [https://finn-stats.medium.com/coefficient-of-variation-cf92d06e4be7]
- 60. - Principles Coefficient of variation [https://influentialpoints.com/Training/coefficient_of_variation-principles-properties-assumptions.htm]
- 61. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 62. ELISA vs. Flow Cytometry: Which is Right for Your ... [https://www.xlbiotec.com/blog/elisa-vs-flow-cytometry-which-is-right-for-your-immunology-study/]
- 63. High Throughput Screening Market Forecast, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/high-throughput-screening-market]
- 64. High Throughput Screening (HTS) Market Size 2025-2029 [https://www.technavio.com/report/high-throughput-screening-market-industry-analysis]
- 65. Impact of Randomization in Experimental Design in Research [https://sawtoothsoftware.com/resources/blog/posts/randomization-in-experimental-designs]
- 66. Considerations for open-label randomized clinical trials [https://pubmed.ncbi.nlm.nih.gov/38618711/]
- 67. in Research: Ensuring Valid Results Bias [https://www.linkedin.com/advice/3/youre-facing-potential-biases-your-research-design-how-w374f]
- 68. GitHub - tfthushaar/ Mitigation - Strategies -for- Sample - Bias ... [https://github.com/tfthushaar/Mitigation-Strategies-for-Sample-Bias]
- 69. Diagnostic Accuracy of Blood-Based Biomarker Panels [https://pmc.ncbi.nlm.nih.gov/articles/PMC8963375/]
- 70. Comparison of xMAP and ELISA assays for detecting CSF ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3660971/]
- 71. Mass spectrometry based biomarker discovery, verification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5528535/]
- 72. Full spectrum flow cytometry and mass ... [https://pubmed.ncbi.nlm.nih.gov/35593221/]
- 73. A plasma proteomics-based candidate biomarker panel ... [https://www.nature.com/articles/s41591-025-03890-6]
- 74. Evaluating the Clinical Utility of a Biomarker - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3138723/]
- 75. an analysis based on population-level parametric distributions ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02656-5]
- 76. Comparison of Large, Medium, and Small Solid Tumor ... [https://pubmed.ncbi.nlm.nih.gov/32770442/]
- 77. Validation of a biomarker panel and longitudinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4915986/]
- 78. A Statistical Challenge: Developing Tests for Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3982897/]
- 79. When to Choose Narrow Panel Testing Over ... [https://www.onclive.com/view/when-to-choose-narrow-panel-testing-over-comprehensive-testing-in-biomarker-analysis]
- 80. Guidelines for benchmarking of optimization-based ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1887-9]
- 81. Interrelationships Among Sensitivity, Precision, Accuracy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11854876/]
- 82. Sensitivity and specificity [https://www.pathologyoutlines.com/topic/chemistrysensitivityspecificity.html]
- 83. Evaluating Risk Prediction with ROC Curves [https://www.publichealth.columbia.edu/research/population-health-methods/evaluating-risk-prediction-roc-curves]
- 84. Biomarker Discovery and Validation Using a Combination ... [https://blog.crownbio.com/biomarker-discovery-and-validation-combining-in-vitro-and-in-vivo-studies]
- 85. Diagnostic value of genetic and epigenetic biomarker panels ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12098509/]
- 86. A sensitive and specific non-invasive urine biomarker ... [https://www.sciencedirect.com/science/article/pii/S2352396425003391]
- 87. Multimodal urinary biomarker panel achieves superior ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613033/]
- 88. Performing a Multicenter Retrospective Study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12164236/]
- 89. Process Validation in Six Sigma: A Complete Guide - SixSigma.us [https://www.6sigma.us/process-improvement/process-validation/]
- 90. Overview of Medical Device Process Validation: IQ, OQ, and PQ – Oriel STAT A MATRIX – ELIQUENT Life Sciences Blog [https://www.orielstat.com/blog/medical-device-process-validation/]
- 91. Study designs [https://www.cebm.ox.ac.uk/resources/ebm-tools/study-designs]
- 92. An open source statistical web application for validation ... [https://www.nature.com/articles/s41598-025-99720-3]
- 93. Performance of GALAD, GAAD, and ASAP for Early HCC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503712/]
- 94. Development and clinical validation of a novel algorithmic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10635602/]
- 95. Leveraging artificial intelligence to validate traditional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575369/]
- 96. Performance of GALAD, GAAD, and ASAP for Early HCC ... [https://pubmed.ncbi.nlm.nih.gov/41063741/]
- 97. Comparison of the GALAD, GAAP, and ASAP Scores for ... [https://www.sciencedirect.com/science/article/pii/S0973688325001070]
- 98. Clinical performance of GAAD score, alpha-fetoprotein, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494999/]
- 99. A Phase 3 Biomarker Validation of GALAD for the Detection of ... [https://pubmed.ncbi.nlm.nih.gov/39293548/]
- 100. Validation of a Multiplex Hypermethylation-based Blood ... [https://www.sciencedirect.com/science/article/abs/pii/S0973688325000787]
- 101. Understanding Prognostic versus Predictive Biomarkers - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK402284/]
- 102. Digital Biomarkers Summit 2025 [https://www.everythingals.org/summit2025]
- 103. Quantitative Biomarkers Derived from a Novel Contrast-Free ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10046818/]