From Networks to Cures: How Systems Biology is Powering the Personalized Medicine Revolution
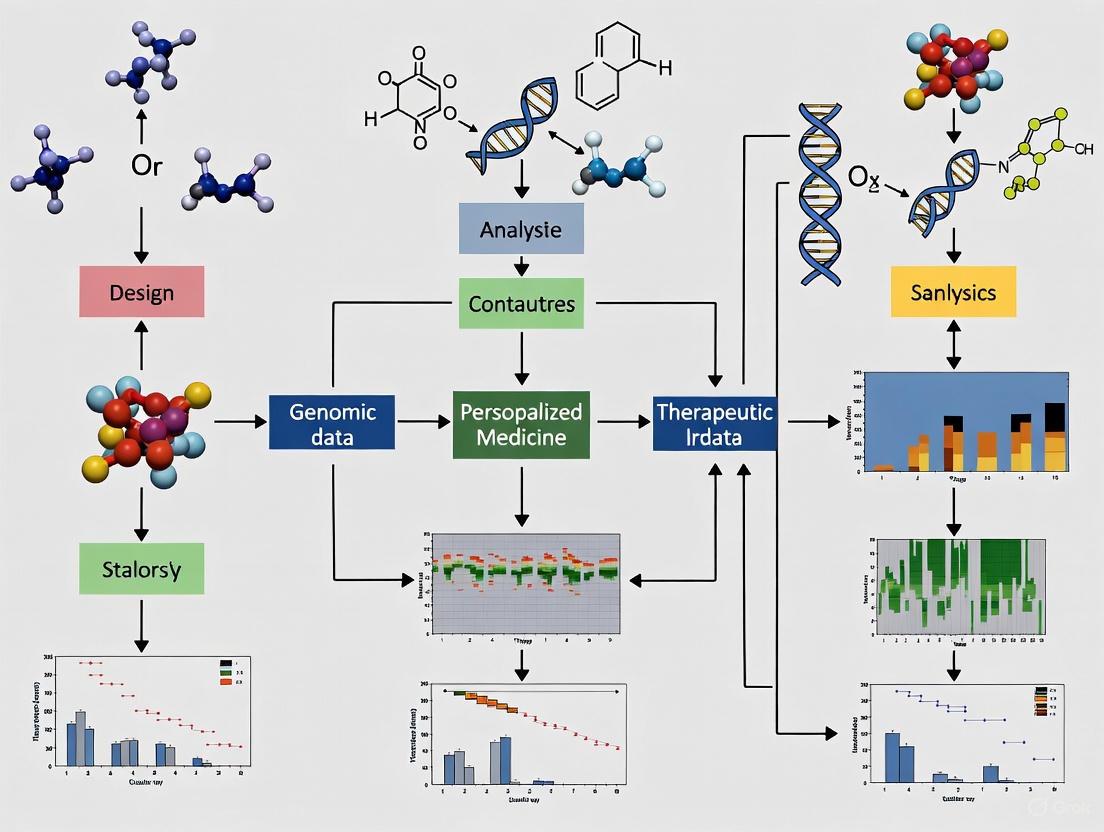
This article explores the transformative role of systems biology in advancing personalized medicine, moving beyond the 'one-size-fits-all' treatment model.
From Networks to Cures: How Systems Biology is Powering the Personalized Medicine Revolution
Abstract
This article explores the transformative role of systems biology in advancing personalized medicine, moving beyond the 'one-size-fits-all' treatment model. Tailored for researchers, scientists, and drug development professionals, it details how integrative approaches—including multi-omics data integration, AI-driven computational modeling, and Quantitative Systems Pharmacology (QSP)—are used to decode complex disease mechanisms and predict individual patient responses. The content covers foundational concepts, key methodologies and their therapeutic applications, strategies to overcome translational and technical challenges, and the frameworks for validating these approaches through industry-academia collaboration and real-world evidence. The synthesis provides a roadmap for leveraging systems biology to develop next-generation, patient-specific diagnostics and therapies.
The Systems View of Biology: Laying the Foundation for Personalized Medicine
For decades, drug discovery has been dominated by a reductionist paradigm that seeks to identify single molecular targets responsible for disease pathology. This "one drug–one target" approach, while successful for infectious diseases and conditions with well-defined molecular etiology, has demonstrated significant limitations when applied to complex multifactorial diseases such as cancer, neurodegenerative disorders, and metabolic syndromes [1]. These diseases involve intricate interactions across gene regulatory networks, protein-protein interactions, and signaling pathways with redundant mechanisms that diminish the efficacy of single-target therapies [2]. The consequences of this limitation are quantifiable: drugs developed through conventional approaches experience clinical trial failure rates of 60–70%, partly due to insufficient understanding of complex biological interactions [1].
The emerging discipline of systems biology has facilitated a fundamental shift toward viewing human physiology and pathology through the lens of interconnected biological networks. This paradigm shift recognizes that diseases manifest from perturbations in complex molecular networks rather than isolated defects in single molecules [3] [4]. Network medicine, which integrates systems biology, network science, and computational approaches, provides a framework for understanding the organizational principles of human pathobiology and has begun to reveal that disease-associated perturbations occur within connected microdomains (disease modules) of molecular interaction networks [4]. This holistic perspective enables researchers to explore drug-disease relationships at a network level, providing insights into how drugs act on multiple targets within biological systems to modulate disease progression [3].
Theoretical Foundations: From Single Targets to Network Therapeutics
Core Principles of Network Pharmacology
Central to the paradigm shift is network pharmacology, an interdisciplinary field that integrates systems biology, bioinformatics, and pharmacology to understand sophisticated interactions among drugs, targets, and disease modules in biological networks [1]. Unlike traditional pharmacology's single-target focus, network pharmacology views diseases as the result of complex molecular interactions, where multiple targets are involved simultaneously [3]. The theoretical foundation was significantly advanced by the proposal of network target theory by Li et al. in 2011, which addressed the limitations of traditional single-target drug discovery by proposing that the disease-associated biological network itself should be viewed as the therapeutic target [3].
This theory posits that diseases emerge from perturbations in complex biological networks, and effective therapeutic interventions should target the disease network as a whole. Network targets include various molecular entities such as proteins, genes, or pathways that are functionally associated with disease mechanisms, and their interactions form a dynamic network that determines disease progression and therapeutic responses [3]. This perspective represents a fundamental departure from traditional approaches by conceptualizing therapeutic intervention as a modulation of network states rather than simple inhibition or activation of individual targets.
Key Conceptual Differences Between Paradigms
Table 1: Comparison of Traditional Pharmacology vs. Network Pharmacology
| Feature | Traditional Pharmacology | Network Pharmacology |
|---|---|---|
| Targeting Approach | Single-target | Multi-target / network-level |
| Disease Suitability | Monogenic or infectious diseases | Complex, multifactorial disorders |
| Model of Action | Linear (receptor-ligand) | Systems/network-based |
| Risk of Side Effects | Higher (off-target effects) | Lower (network-aware prediction) |
| Failure in Clinical Trials | Higher (60-70%) | Lower due to pre-network analysis |
| Technological Tools Used | Molecular biology, pharmacokinetics | Omics data, bioinformatics, graph theory |
| Personalized Therapy | Limited | High potential (precision medicine) |
Methodological Framework: Computational Approaches and Experimental Design
Network Construction and Analysis Protocols
The implementation of network pharmacology follows a systematic workflow that begins with data retrieval and curation from established biological databases. Essential data sources include DrugBank and PubChem for drug-related information, DisGeNET and OMIM for disease-associated genes, and STRING and BioGRID for protein-protein interactions [1]. Following data collection, researchers construct multi-layered biological networks including drug-target, target-disease, and protein-protein interaction maps using tools such as Cytoscape and NetworkX [1].
A critical step in the process involves topological and module analysis using graph-theoretical measures. Key metrics include degree centrality (number of connections), betweenness (influence over information flow), closeness (efficiency in accessing other nodes), and eigenvector centrality (influence based on connections to other influential nodes) [5]. These analyses help identify hub nodes and bottleneck proteins that play disproportionately important roles in network stability and function. Community detection algorithms like MCODE and Louvain are subsequently applied to identify functional modules within the networks, which are then subjected to enrichment analysis using tools such as DAVID and g:Profiler to determine overrepresented pathways and biological processes [1].
Integrating Qualitative and Quantitative Data in Parameter Identification
Systems biology models often face challenges in parameter estimation due to limited quantitative data. A sophisticated approach addresses this limitation by converting qualitative biological observations into inequality constraints on model outputs [6]. For example, qualitative data such as "activating or repressing" or "viable or inviable" can be formalized as inequality constraints, which are then combined with quantitative measurements in a single objective function:
f_tot(x) = f_quant(x) + f_qual(x)
where f_quant(x) represents the sum-of-squares distance from quantitative data points, and f_qual(x) represents penalty terms for violation of qualitative constraints [6]. This approach enables researchers to incorporate diverse data types, such as both quantitative time courses and qualitative phenotypes of mutant strains, to perform automated identification of numerous model parameters simultaneously [6].
Network Analysis Workflow
Predictive Modeling and Validation Frameworks
Advanced machine learning algorithms including support vector machines (SVM), random forests (RF), and graph neural networks (GNN) are trained on specialized datasets to predict novel drug-target interactions [1]. The performance of these models is rigorously evaluated using cross-validation and metrics such as AUC (Area Under the Curve) and accuracy [3]. Promising predictions are subsequently validated through molecular docking simulations and experimental methodologies including surface plasmon resonance (SPR) and quantitative PCR (qPCR) for in vitro validation [1].
A notable example of this approach is found in a 2025 transfer learning model based on network target theory that integrated deep learning techniques with diverse biological molecular networks to predict drug-disease interactions [3]. This model achieved an AUC of 0.9298 and an F1 score of 0.6316 in predicting drug-disease interactions, successfully identifying 88,161 relationships involving 7,940 drugs and 2,986 diseases [3]. Furthermore, the algorithm demonstrated exceptional capability in predicting drug combinations, achieving an F1 score of 0.7746 after fine-tuning, and accurately identified two previously unexplored synergistic drug combinations for distinct cancer types [3].
Advanced Applications in Personalized Medicine
Contextualized Network Modeling for Individual Patient Profiles
A groundbreaking approach developed by Carnegie Mellon University researchers introduces contextualized modeling, a family of ultra-personalized machine learning methods that build individualized gene network models for specific patients [7]. This methodology addresses a fundamental limitation of traditional modeling approaches, which require large patient populations to produce a single model and consequently lump together patients with potentially important biological differences [7].
Contextualized models overcome this limitation by generating individualized network models based on each patient's unique molecular profile, or context. These models consider thousands of contextual factors simultaneously and automatically determine which factors are important for differentiating patients and understanding diseases [7]. In a landmark study, researchers applied this approach to build personalized models for nearly 8,000 tumors across 25 cancer types, identifying previously hidden cancer subtypes and improving survival predictions, particularly for rare cancers [7]. The generative nature of these models enables researchers to produce models on demand for new contexts, including predicting gene behavior in types of tumors they had never previously encountered [7].
Network-Based Drug Repurposing and Combination Therapy
Network pharmacology enables systematic drug repurposing by mapping the network proximity between drug targets and disease modules within molecular interaction networks [4]. The recently recognized extraordinary promiscuity of drugs for multiple protein targets provides a rational basis for this strategy [4]. The potential of this approach has been demonstrated across numerous conditions, from coronary artery disease to Covid-19 [4].
Beyond single-drug repurposing, network approaches facilitate the design of rational combination therapies that simultaneously target multiple nodes in disease networks. Tools from network medicine can investigate the impact of complex combinations of small molecules found in food on the human molecular interaction network, potentially leading to mechanism-based nutritional interventions and food-inspired therapeutics [4]. This approach is particularly valuable for understanding traditional medicine formulations, such as Traditional Chinese Medicine, where multi-component formulae act on multiple targets simultaneously [2] [1].
Table 2: Performance Metrics of Network-Based Prediction Models
| Model Type | Application | Performance Metrics | Key Outcomes |
|---|---|---|---|
| Transfer Learning Model [3] | Drug-disease interaction prediction | AUC: 0.9298, F1 score: 0.6316 | Identified 88,161 drug-disease interactions |
| Fine-tuned Combination Prediction [3] | Synergistic drug combination | F1 score: 0.7746 | Discovered two novel cancer drug combinations |
| Contextualized Network Model [7] | Personalized cancer modeling | Improved survival prediction | Identified hidden thyroid cancer subtype with worse prognosis |
Computational Tools and Biological Databases
Implementing network pharmacology requires specialized computational tools and comprehensive biological databases. The table below summarizes essential resources for constructing and analyzing biological networks.
Table 3: Research Toolkit for Network Pharmacology
| Category | Tool/Database | Functionality |
|---|---|---|
| Drug Information | DrugBank, PubChem, ChEMBL | Drug structures, targets, pharmacokinetics |
| Gene-Disease Associations | DisGeNET, OMIM, GeneCards | Disease-linked genes, mutations, gene function |
| Target Prediction | Swiss Target Prediction, SEA | Predicts protein targets from compound structures |
| Protein-Protein Interactions | STRING, BioGRID, IntAct | Protein interaction networks, functional associations |
| Pathway Analysis | KEGG, Reactome | Pathway mapping, biological process annotation |
| Network Visualization & Analysis | Cytoscape, NetworkX, Gephi | Network construction, visualization, topological analysis |
| Machine Learning Frameworks | DeepPurpose, DeepDTnet | Prediction of drug-target interactions |
Experimental Validation Techniques
While computational predictions form the foundation of network pharmacology, experimental validation remains essential for translational applications. Key validation methodologies include:
- Molecular Docking Simulations: Tools such as AutoDock Vina and Glide predict binding affinities between drug compounds and target proteins [1].
- Surface Plasmon Resonance (SPR): Measures real-time binding kinetics and affinity between molecules [1].
- In Vitro Validation: Includes qPCR for gene expression analysis, cytotoxicity assays for drug efficacy testing [3], and specialized assays for pathway modulation.
- Multi-omics Integration: Approaches such as multi-omics factor analysis (MOFA) integrate genomic, transcriptomic, proteomic, and metabolomic data to create comprehensive, patient-specific models [1].
Personalized Network Therapy
The paradigm shift from single-target drugs to biological network models represents a fundamental transformation in how we understand and treat disease. This approach moves beyond the reductionist view of focusing on individual molecular targets to embrace the complexity of biological systems and their emergent properties. The integration of systems biology with network science and artificial intelligence has enabled the development of predictive models of disease mechanisms and therapeutic interventions that account for the interconnected nature of biological processes [4].
The future of network-based approaches will likely involve even deeper integration of multi-scale biological information, from molecular interactions to organ-level and organism-level networks [4]. Emerging technologies such as total-body PET imaging can provide insights into interorgan communication networks, potentially enabling the creation of whole-organism interactomes for functional and therapeutic analysis [4]. Furthermore, as single-cell technologies advance, we can anticipate the development of cell-type-specific network models that capture the extraordinary heterogeneity of biological systems.
For researchers and drug development professionals, embracing this paradigm shift requires familiarity with both computational and experimental approaches. The successful implementation of network pharmacology depends on interdisciplinary collaboration across systems biology, bioinformatics, pharmacology, and clinical medicine. As these approaches mature, they hold the promise of truly personalized, precision medicine based on comprehensive understanding of individual network perturbations and targeted interventions to restore physiological balance.
Integrative Pharmacology and Systems Therapeutics represent a paradigm shift in biomedical research, moving away from a reductionist focus on single drug targets toward a holistic understanding of drug action within complex biological systems. Integrative Pharmacology is defined as the systematic investigation of drug interactions with biological systems across molecular, cellular, organ, and whole-organism levels, combining traditional pharmacology with signaling pathways, bioinformatic tools, and multi-omics data [8]. This approach aims to improve understanding, diagnosis, and treatment of human diseases by elucidating complete mechanisms of action and predicting therapeutic targets and effects [8].
Systems Therapeutics, in parallel, defines where pharmacologic processes and pathophysiologic processes interact to produce clinical therapeutic responses [9]. It provides a framework for understanding how drugs modulate biological networks rather than isolated targets, with the overarching goal of discovering and verifying novel treatment targets and candidate therapeutics for diseases based on understanding molecular, cellular, and circuit mechanisms [10]. The integration of these two disciplines enables researchers to address the complexity of therapeutic interventions in a more comprehensive manner, ultimately accelerating the development of safer and more effective personalized treatments.
The Framework of Systems Therapeutics
The organizing principle of Systems Therapeutics involves two parallel processes—pharmacologic and pathophysiologic—that interact at different biological levels to produce therapeutic outcomes [9]. A systematic diagram illustrates this framework consisting of two rows of four parallel systems components representing different biologic levels of interaction.
Core Components and Processes
The pharmacologic process begins with a pharmacologic agent (drug) interacting with a pharmacologic response element (e.g., receptor, drug target) [9]. This initial interaction initiates a pharmacologic mechanism via signal transduction, which progresses to a pharmacologic response at the tissue/organ level via pharmacodynamics, and finally translates to a clinical (pharmacologic) effect at the whole-body level [9].
The pathophysiologic process is initiated by an intrinsic operator, a hypothetical endogenous entity originating in a diseased organ's principal cell type that interacts with and influences an etiologic causative factor (e.g., genetic mutation, protein abnormality) via disease preindication [9]. This leads to initiation of a pathogenic pathway via disease initiation, which progresses to a pathophysiologic process at the tissue/organ level via pathogenesis, and finally manifests as a disease manifestation at the clinical level via progression [9].
The therapeutic response is determined by how the clinical (pharmacologic) effect moderates the disease manifestation, regardless of the biologic level at which the pivotal interaction occurs [9].
Diagram Title: Systems Therapeutics Framework
Systems Therapeutics Categories and Examples
The Systems Therapeutics framework defines four distinct categories based on the biological level at which the pivotal interaction between pharmacologic and pathophysiologic processes occurs [9]. Each category represents a different therapeutic strategy with characteristic drug classes and mechanisms.
Table 1: Systems Therapeutics Categories and Examples
| Category | Pivotal Interaction Level | Definition | Therapeutic Approach | Drug Examples | Indications |
|---|---|---|---|---|---|
| Category I | Molecular Level: Elements/Factors | Interaction between pharmacologic response element and etiologic causative factor | Molecular-based therapy targeting primary molecular entities | Ivacaftor (Kalydeco), Imatinib (Gleevec) | Cystic Fibrosis, Chronic Myelogenous Leukemia |
| Category II | Cellular Level: Mechanisms/Pathways | Interaction involving fundamental biochemical mechanism related to disease evolution | Metabolism-based therapy interfering with biochemical mechanisms | Atorvastatin (Lipitor), Adalimumab (Humira) | Hypercholesterolemia, Rheumatoid Arthritis |
| Category III | Tissue/Organ Level: Responses/Processes | Modulation of physiologic function linked to disease evolution | Function-based therapy modulating normal physiologic functions | Irbesartan (Avapro), Tadalafil (Cialis) | Hypertension, Male Erectile Dysfunction |
| Category IV | Clinical Level: Effects/Manifestations | Effect directed at clinical symptoms rather than disease cause | Symptom-based therapy providing symptomatic or palliative treatment | Acetaminophen (Tylenol), Ibuprofen (Advil) | Fever, Pain, Inflammation |
Category I: Molecular-Level Therapeutics
Category I represents the most fundamental level of therapeutic intervention, where drugs interact directly with the etiologic causative factors of disease [9]. This category includes replacement therapies such as enzyme replacement (e.g., idursulfase for Hunter Syndrome) and protein replacement (e.g., recombinant Factor VIII for Hemophilia A), as well as therapies that potentiate defective proteins (e.g., ivacaftor for Cystic Fibrosis) or inhibit abnormal enzymes (e.g., imatinib for Chronic Myelogenous Leukemia) [9]. These interventions target the primary molecular abnormalities responsible for disease pathogenesis, offering potentially transformative treatments for genetic and molecular disorders.
Categories II-IV: Cellular to Clinical Level Therapeutics
Category II interventions target biochemical mechanisms and pathways central to disease evolution, though not necessarily etiologic pathways [9]. Examples include HMG-CoA reductase inhibitors (statins) for hypercholesterolemia, TNF-α inhibitors for rheumatoid arthritis, and xanthine oxidase inhibitors for hyperuricemia and gout [9]. Category III therapeutics operate at the tissue/organ level by modulating normal physiologic functions linked to disease evolution, such as angiotensin II receptor blockers for hypertension and PDE-5 inhibitors for erectile dysfunction [9]. Category IV represents symptom-based therapies that alleviate clinical manifestations without directly targeting disease causes, including antipyretics, analgesics, and antitussives [9].
Methodological Approaches in Integrative Pharmacology
Integrative Experimental Strategies
Integrative Pharmacology employs a hierarchical experimental approach that connects in vitro findings with in vivo outcomes through progressively complex model systems [11]. This methodology acknowledges that isolated molecules and cells in vitro do not necessarily reflect properties they possess in vivo and cannot adequately capture intact tissue, organ, and system functions [12]. The National Institute of General Medical Sciences (NIGMS) defines Integrative and Organ Systems Pharmacology as "pharmacological research using in vivo animal models or substantially intact organ systems that are able to display the integrated responses characteristic of the living organism that result from complex interactions between molecules, cells, and tissues" [12].
The experimental workflow typically progresses from in vitro systems (cell cultures, biochemical assays) to ex vivo models (isolated organs, tissue slices) and finally to in vivo models that recapitulate human clinical conditions [11]. This sequential approach allows researchers to establish connections between in vitro mechanisms and in vivo outcomes while accounting for the complex interactions that emerge at each level of biological organization [12]. Advanced tools such as microdialysis, imaging methods, and multi-omic technologies enhance the collection and interpretation of pharmacological data obtained from these integrated experimental systems [12].
Diagram Title: Integrative Pharmacology Workflow
Systems Biology and Multi-Omic Integration
Integrative Pharmacology leverages systems biology approaches and multi-omic technologies to understand drug actions within biological networks [13] [14]. This involves the application of genomic, transcriptomic, proteomic, metabolomic, epigenomic, and microbiomic data to construct comprehensive models of drug-target interactions and physiological responses [8]. Blood is particularly valuable as a window into health and disease because it bathes all organs and contains molecules secreted by these organs, providing readouts of their behavior [15].
The integrative Personal Omics Profile (iPOP) approach exemplifies this strategy by combining genomic information with longitudinal monitoring of transcriptomes, proteomes, and metabolomes to capture personalized physiological state changes during health and disease transitions [13]. This method has demonstrated utility in detecting early disease onset and monitoring responses to interventions, serving as a proof-of-principle for predictive and preventative medicine [13]. Additional omics profiles such as gut microbiome, microRNA, and immune receptor repertoire provide complementary layers of biological information for personalized health monitoring and therapeutic optimization [13].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Research Reagents and Experimental Materials
| Category | Specific Reagents/Materials | Function/Application | Key Considerations |
|---|---|---|---|
| Model Systems | Genetically engineered mouse models, Primary cell cultures, Human organoids, Tissue engineering scaffolds | Recapitulate human disease conditions for therapeutic testing | Species differences, Genetic stability, Physiological relevance, Ethical considerations |
| Omics Technologies | Whole genome/exome sequencing kits, RNA/DNA extraction kits, Mass spectrometry reagents, Microarray platforms | Comprehensive molecular profiling for systems-level analysis | Data integration challenges, Batch effects, Normalization methods, Computational requirements |
| Drug Delivery Systems | Nanoparticles (polymeric, lipid-based), Stimuli-responsive biomaterials, Implantable devices, Targeting ligands | Enhanced specificity, Localized delivery, Controlled release kinetics | Biocompatibility, Scalability, Release profile characterization, Sterilization requirements |
| Analytical Tools | Microdialysis probes, Biosensors, Wearable monitoring devices, High-resolution imaging agents | Real-time monitoring of physiological and pharmacological parameters | Temporal resolution, Sensitivity limits, Calibration requirements, Signal-to-noise optimization |
| Computational Resources | Network analysis software, PK/PD modeling platforms, AI/ML algorithms, Data integration frameworks | Predictive modeling of drug effects, Network pharmacology analysis, Personalized dosing optimization | Data standardization, Algorithm validation, Computational power, Interoperability challenges |
| PROTAC BRM degrader-1 | PROTAC BRM degrader-1, MF:C57H69N11O8S, MW:1068.3 g/mol | Chemical Reagent | Bench Chemicals |
| Gly-Mal-GGFG-Deruxtecan 2-hydroxypropanamide | Gly-Mal-GGFG-Deruxtecan 2-hydroxypropanamide, MF:C52H55FN10O15, MW:1079.0 g/mol | Chemical Reagent | Bench Chemicals |
Integration with Personalized Medicine and Systems Biology
Integrative Pharmacology and Systems Therapeutics fundamentally contribute to personalized medicine by providing frameworks to understand individual variations in drug response and disease manifestations [13] [15]. The combination of personal genomic information with longitudinal monitoring of molecular components that reflect real-time physiological states enables predictive and preventative medicine approaches [13]. Dr. Lee Hood's concept of P4 medicine—predictive, preventive, personalized, and participatory—exemplifies this integration, representing a shift from symptom-based diagnosis and treatment to continuous health monitoring and early intervention [15].
Systems biology provides the methodological foundation for this integration by enabling comprehensive analysis of biological systems through global profiling of multiple data types [13] [15]. The convergence of high-throughput technologies, computational modeling, and multi-omic data integration allows researchers to examine the interconnected nature of biological systems and their responses to therapeutic interventions [13]. This approach is particularly valuable for understanding complex diseases that involve multiple interacting pathways and systems, such as cancer, neurodegenerative disorders, and metabolic conditions [13] [14].
Artificial intelligence and machine learning are increasingly important in analyzing the complex datasets generated by integrative pharmacological studies [8]. These computational approaches can identify patterns and relationships within multi-omic data, predict drug responses, optimize therapeutic combinations, and guide personalized treatment strategies [8]. The ongoing development of these analytical tools, combined with advances in experimental technologies, continues to enhance the precision and predictive power of Integrative Pharmacology and Systems Therapeutics.
The staggering molecular heterogeneity of human diseases, particularly cancer, demands innovative approaches beyond traditional single-omics methods [16]. Multi-omics integration represents a paradigm shift in biomedical research, enabling the collection and analysis of large-scale datasets across multiple biological layers—including genomics, transcriptomics, proteomics, metabolomics, and epigenomics [17]. This approach provides global insights into biological processes and holds great promise in elucidating the myriad molecular interactions associated with complex human diseases [17] [16].
The clinical imperative for multi-omics integration stems from the limitations of reductionist approaches. Traditional methods reliant on single-omics snapshots or histopathological assessment alone fail to capture cancer's interconnected biological complexity, often yielding incomplete mechanistic insights and suboptimal clinical predictions [16]. Multi-omics profiling systematically integrates diverse molecular data to construct a comprehensive and clinically relevant understanding of disease biology, recovering system-level signals that are often missed by single-modality studies [18] [16]. This framework is transforming precision oncology from reactive population-based approaches to proactive, individualized care [16].
Computational Methods for Multi-Omics Integration
Strategy Spectrum: From Conceptual to Network-Based Integration
The integration of multi-omics data presents significant challenges due to high dimensionality, heterogeneity, and technical variability [17] [16]. Based on data type, quality, and biological questions, researchers employ distinct integration strategies:
Table 1: Multi-Omics Integration Strategies
| Integration Type | Core Methodology | Applications | Tools/Examples |
|---|---|---|---|
| Conceptual Integration | Utilizes existing databases and knowledge bases to associate different omics data by shared concepts or entities | Hypothesis generation, functional annotation | STATegra, OmicsON [19] |
| Statistical Integration | Employs correlation analysis, regression modeling, clustering, or classification to extract patterns and trends | Identifying gene-protein co-expression relationships, drug response prediction | Seurat WNN, Harmony [19] [20] |
| Model-Based Integration | Leverages network models or pharmacokinetic/pharmacodynamic simulations to simulate biological system behavior | Understanding system dynamic regulation mechanisms | Graph neural networks [19] [16] |
| Network & Pathway Integration | Constructs protein-protein interaction networks or metabolic pathways to integrate multi-omics data across different layers | Revealing complex molecular interaction networks, identifying key regulatory hubs | GLUE, MIDAS [19] [20] |
Artificial Intelligence and Novel Computational Frameworks
Artificial intelligence (AI), particularly machine learning (ML) and deep learning (DL), has emerged as the essential scaffold bridging multi-omics data to clinical decisions [16]. Unlike traditional statistics, AI excels at identifying non-linear patterns across high-dimensional spaces, making it uniquely suited for multi-omics integration [16].
Deep Learning Approaches include specialized architectures such as Convolutional Neural Networks (CNNs) that automatically quantify immunohistochemistry staining with pathologist-level accuracy, Graph Neural Networks (GNNs) that model protein-protein interaction networks perturbed by somatic mutations, and multi-modal transformers that fuse MRI radiomics with transcriptomic data to predict disease progression [16]. The SWITCH deep learning method exemplifies innovation in this space, utilizing deep neural networks to learn complex relationships between different omics data types by mapping them to a common latent space where they can be effectively compared and integrated [21].
Single-Cell Multi-Modal Integration represents a particularly advanced frontier. Recent benchmarking efforts have evaluated 40 software packages encompassing 65 integration algorithms for processing RNA and ATAC (high-dimensional), ADT (protein, low-dimensional), and spatial genomics data [20]. In modality-matched integration tasks, Seurat's Weighted Nearest Neighbors (WNN) algorithm demonstrates superior performance for RNA+ATAC and RNA+ADT integration, while in scenarios with partial or complete missing modality matches, deep generative models like MIDAS and GLUE excel at cross-modal imputation and alignment [20].
Universal AI Models represent another groundbreaking approach. Researchers have developed a general AI model that employs a multi-task architecture to jointly predict diverse genomic modalities including chromatin accessibility, transcription factor binding, histone modifications, nascent RNA transcription, and 3D genome structure [22]. This model contains three key components—task-shared local encoders, task-shared global encoders, and task-specific prediction heads—and can be trained using innovative strategies like task scheduling, task weighting, and partial label learning [22].
Multi-Omics Applications in Clinical Research and Therapeutics
Biomarker Discovery and Patient Stratification
Multi-omics integration enables the identification of novel biomarkers and patient stratification approaches that would be impossible with single-omics data alone. By integrating genetic data with insights from other omics technologies, researchers can provide a more comprehensive view of an individual's health profile [23].
Liquid Biopsies exemplify the clinical impact of multi-omics, analyzing biomarkers like cell-free DNA (cfDNA), RNA, proteins, and metabolites non-invasively [23] [16]. Recent improvements have enhanced their sensitivity and specificity, advancing early disease detection and treatment monitoring [23]. While initially focused on oncology, liquid biopsies are expanding into other medical domains, further solidifying their role in personalized medicine through multi-analyte integration [23]. Technologies like ApoStream enable the capture of viable whole cells from liquid biopsies, preserving cellular morphology and enabling downstream multi-omic analysis when traditional biopsies aren't feasible [18].
Cancer Subtyping and Prognosis has been revolutionized by multi-omics approaches. Integrated classifiers report AUCs of 0.81–0.87 for challenging early-detection tasks, significantly outperforming single-modality biomarkers [16]. In breast cancer, multi-omics analysis helps predict patient survival and drug response, while in brain tumors like glioma, integrating MRI radiomics with transcriptomic data enables more accurate progression prediction [19] [16].
Drug Discovery and Therapeutic Optimization
Multi-omics approaches are accelerating drug discovery and enabling more targeted therapeutic strategies across multiple disease areas:
- Target Identification: Multi-omics can identify new drug targets by integrating gene, protein, metabolite, and epigenetic information to construct disease and drug action mechanism networks, allowing prioritized screening of potential targets [19].
- Drug Response Prediction: Analysis of individual variations in drug response helps identify genetic, transcriptional, protein, and metabolic factors affecting efficacy and toxicity [19]. Machine learning models (random forests, SVMs, neural networks) can predict individualized efficacy and safe dosage, advancing precision medicine [19].
- CRISPR and Gene Therapy: Multi-omic data drives the next generation of cell and gene therapy approaches, including CRISPR-based treatments [23]. New solutions like Perturb-seq enable functional genomics at single-cell resolution, allowing unprecedented insight into drug mechanisms of action and genetic disease treatments [24].
Table 2: Multi-Omics Applications in Disease Research
| Disease Area | Multi-Omics Approach | Key Findings/Applications |
|---|---|---|
| Oncology | Integration of genomic, transcriptomic, proteomic, and metabolomic data | Therapy selection, proteogenomic early detection, radiogenomic non-invasive diagnostics [16] |
| Neurodegenerative Disorders | Multi-omics analysis of brain tissue from ASD and Parkinson's patients | Risk gene function analysis, identification of potential therapeutic targets [19] |
| Rare Genetic Diseases | Whole genome sequencing with epigenomic analysis | Rapid diagnosis, identification of structural variants, development of antisense oligonucleotides [24] |
| Metabolic Diseases | Host tissue and microbiome data integration | Revealing how microbes affect host metabolism, immunity, and behavior [19] |
Experimental Workflows and Research Toolkit
Essential Research Reagents and Platforms
Successful multi-omics research requires specialized reagents and platforms designed to handle the complexity of integrating multiple data types from the same biological sample:
- Single-Cell Multi-Omic Profiling: Technologies like Illumina's Single Cell and Perturb-seq solutions support the analysis of transcriptomics alongside protein expression or CRISPR perturbations at single-cell resolution, with scalability from 10,000 to 1,000,000 cells per sample [24].
- Spatial Transcriptomics: Platforms enabling spatial resolution of gene expression within tissue architecture, with newer technologies offering nine times larger capture area and four times higher resolution than previous standards [24].
- 5-Base Methylation Analysis: Solutions allowing simultaneous genetic variant and methylation detection in a single assay, providing insights into how DNA methylation patterns affect gene expression timing in development, cell differentiation, and tumor progression [24].
- Multi-Omic Analysis Software: Integrated platforms like Illumina Connected Multiomics (ICM) provide seamless workflows from sample to insight, allowing researchers without bioinformatics backgrounds to explore and analyze multi-modal datasets [24].
Technical Protocols for Multi-Omics Integration
Protocol 1: Universal AI Model for Multi-Omics Prediction
This protocol outlines the methodology for developing a universal AI model capable of predicting diverse genomic modalities from ATAC-seq and DNA sequence inputs [22]:
- Input Preparation: Process 600kb DNA sequences with corresponding ATAC-seq data. Split into 1kb genomic intervals with 300bp flanking regions on each side.
- Local Feature Extraction: Use task-shared local encoders to extract local sequence features from each 1kb interval, generating local sequence representation vectors.
- Global Dependency Modeling: Process local sequence representations through global encoders containing convolutional layers and seven transformer encoder layers to model long-range dependencies across the entire 600kb region.
- Task-Specific Prediction: Employ task-specific prediction heads for different genomic modalities (TF binding, histone modifications, RNA transcription, 3D structure).
- Training Strategy: Implement three specialized training approaches:
- Task Scheduling: Use curriculum learning to gradually introduce different genomic modalities, starting with tasks relying on local sequence information before progressing to those requiring long-range interactions.
- Task Weighting: Dynamically adjust loss weights for different prediction tasks.
- Partial Label Learning: Handle missing data across modalities efficiently.
- Cross-Species Adaptation: Transfer learning from human to mouse models by retraining with species-specific data.
Protocol 2: Single-Cell Multi-Modal Integration Benchmarking
This protocol describes the comprehensive benchmarking of single-cell multi-modal integration algorithms [20]:
- Data Collection and Curation: Assemble diverse single-cell multi-modal datasets encompassing RNA+ATAC (high-dimensional), RNA+ADT (protein, low-dimensional), and spatial genomics data.
- Task Definition: Establish six benchmark evaluation tasks based on data type and pairing: paired integration, unpaired mosaic integration, unpaired diagonal integration, and spatial multi-omics tasks.
- Algorithm Evaluation Framework: Implement three-dimensional assessment metrics:
- Usability: Test algorithms across different dataset sizes (500 to 500,000 cells) and hardware platforms (CPU/GPU).
- Accuracy: Evaluate biological structure preservation, batch effect removal, cell alignment, and cross-modal generation accuracy using latent space metrics.
- Stability: Assess performance consistency across multiple runs and with varying dataset qualities.
- Performance Comparison: Execute 65 integration algorithms across 40 software packages using standardized preprocessing and evaluation pipelines.
- Web Server Deployment: Create user-friendly web interfaces for result exploration and algorithm selection based on specific data processing needs.
Multi-omics integration represents a transformative approach in biomedical research, moving beyond theoretical methods to demonstrate tangible impact in biomarker discovery, patient stratification, and therapeutic interventions [17]. The field continues to evolve rapidly, with several emerging trends shaping its future trajectory. Spatial and single-cell multi-omics are providing unprecedented resolution for decoding tissue microenvironments and cellular heterogeneity [16]. Federated learning approaches enable privacy-preserving collaboration across institutions, addressing data governance concerns while leveraging diverse datasets [16]. Explainable AI (XAI) techniques like SHAP are making "black box" models more interpretable, clarifying how genomic variants contribute to clinical outcomes and building trust for clinical implementation [16]. Perhaps most promising is the movement toward patient-centric "N-of-1" models and generative AI for synthesizing in silico "digital twins"—patient-specific avatars that simulate treatment response and enable truly personalized therapeutic optimization [16].
Despite remarkable progress, operationalizing multi-omics integration requires confronting ongoing challenges in algorithm transparency, batch effect robustness, ethical equity in data representation, and regulatory alignment [16]. Standardizing methodologies and establishing robust protocols for data integration remain crucial for ensuring reproducibility and reliability [23]. The massive data output of multi-omics studies continues to demand scalable computational tools and collaborative efforts to improve interpretation [23]. Moreover, engaging diverse patient populations is vital to addressing health disparities and ensuring biomarker discoveries are broadly applicable across different ethnic and socioeconomic groups [23]. Looking ahead, collaboration among academia, industry, and regulatory bodies will be essential to drive innovation, establish standards, and create frameworks that support the clinical application of multi-omics [23]. By addressing these challenges, multi-omics research will continue to advance personalized medicine, offering deeper insights into human health and disease and ultimately fulfilling the promise of precision medicine—matching the right treatment to the right patient at the right time.
Systems biology represents a fundamental shift in biological research, moving from a reductionist study of individual components to an integrative analysis of complex systems. This discipline serves as a critical bridge, connecting the abstract world of computational modeling with the empirical reality of molecular biology. By constructing quantitative models that simulate the dynamic behavior of biological networks, systems biology provides a powerful framework for understanding how molecular interactions give rise to cellular and organismal functions. This approach has become indispensable in the era of personalized medicine, where predicting individual patient responses to therapeutics requires a sophisticated understanding of the complex, interconnected pathways that vary between individuals.
The foundational power of systems biology lies in its ability to formalize biological knowledge into computable representations. As noted in research on model similarity, systems biology models establish "a modelling relation between a formal and a natural system: the formal system encodes the natural system, and inferences made in the formal system can be interpreted (decoded) as statements about the natural system" [25]. This encoding/decoding process enables researchers to move beyond qualitative descriptions to quantitative predictions of system behavior, creating a genuine bridge between disciplines that traditionally operated in separate scientific domains.
Within personalized medicine research, this integrative approach is particularly valuable. The unifying paradigm of Integrative and Regenerative Pharmacology (IRP) exemplifies this trend, merging pharmacology, systems biology, and regenerative medicine to develop transformative curative therapeutics rather than merely managing symptoms [8]. This approach leverages the rigorous tools of systems biology—including omics technologies, bioinformatic analyses, and computational modeling—to understand drug mechanisms of action at multiple biological levels and develop targeted interventions capable of restoring physiological structure and function.
Core Methodologies: Combining Computational and Experimental Techniques
Quantitative Modeling Paradigms for Biological Systems
Selecting appropriate modeling paradigms is crucial for generating biologically meaningful insights. Different biological scales and system characteristics demand distinct computational approaches, each with specific strengths and limitations for personalized medicine applications [26]:
Deterministic Modeling using ordinary differential equations (ODEs) works well for systems with high molecular abundances and predictable behaviors, typically at macroscopic scales. These models assume continuous concentration changes and yield identical results for identical parameters, making them suitable for simulating population-level phenomena or dense intracellular networks where stochastic effects average out.
Stochastic Modeling approaches, including stochastic simulation algorithms, capture the random fluctuations inherent in biological systems with low molecular counts. This paradigm is essential for modeling microscopic and mesoscopic systems such as gene regulatory networks, where random molecular collisions and rare events can drive significant physiological outcomes—a critical consideration when modeling individual patient variations in drug response.
Fuzzy Stochastic Methods combine stochastic simulation with fuzzy logic to address both randomness and parameter uncertainty, which is particularly valuable for personalized medicine applications where precise kinetic parameters may be unknown. This approach recognizes that "reaction rates are typically vague and rather uncertain" in biological systems, and this vagueness affects stoichiometry and quantitative relationships in biochemical reactions [26].
Table 1: Modeling Paradigms in Systems Biology
| Modeling Approach | Mathematical Foundation | Ideal Application Scope | Personalized Medicine Relevance |
|---|---|---|---|
| Deterministic | Ordinary Differential Equations | Macroscopic systems with high component density | Population-level drug response trends |
| Stochastic | Stochastic Simulation Algorithm | Sparse systems with low molecular counts | Individual variations in drug metabolism |
| Fuzzy Stochastic | Fuzzy sets + Stochastic processes | Systems with parameter uncertainty | Patient-specific models with limited data |
| Cyclo(CRLLIF) | Cyclo(CRLLIF) Peptide|Research Use Only | Cyclo(CRLLIF) is a cyclic peptide for research. This product is for Research Use Only (RUO). Not for human, veterinary, or therapeutic use. | Bench Chemicals |
| Mpo-IN-7 | Mpo-IN-7, MF:C16H14N2O6, MW:330.29 g/mol | Chemical Reagent | Bench Chemicals |
The choice between these paradigms depends on the system's spatial scale and component density. As [26] demonstrates through scale-density analysis, intracellular and cellular processes (microscopic and mesoscopic systems) with relatively low numbers of biological components are best modeled using stochastic methods, while intercellular and population-wide processes (macroscopic systems) with high component density are more suited to deterministic approaches.
Parameter Identification Using Multimodal Data
A critical methodological challenge in systems biology is parameter identification—determining the numerical values that define how model components interact. Traditional approaches rely heavily on quantitative data, but recent advances demonstrate how qualitative biological observations can be formalized as inequality constraints and combined with quantitative measurements for more robust parameter estimation [6].
This methodology converts qualitative data, such as whether a particular mutant strain is viable or inviable, into mathematical inequalities that constrain model outputs. For example, a qualitative observation that "protein B concentration increases when pathway A is activated" can be formalized as Bactivated > Bbaseline. These constraints are combined with quantitative measurements through an objective function that accounts for both datasets:
ftot(x) = fquant(x) + fqual(x)
where fquant(x) is a standard sum of squares quantifying the fit to quantitative data, and fqual(x) imposes penalties for violations of qualitative constraints [6]. This approach was successfully applied to estimate parameters for a yeast cell cycle model incorporating "both quantitative time courses (561 data points) and qualitative phenotypes of 119 mutant yeast strains (1647 inequalities) to perform automated identification of 153 model parameters" [6], demonstrating its power for complex biological systems.
Table 2: Data Types in Systems Biology Model Development
| Data Type | Examples | Formalization in Models | Parameter Identification Value |
|---|---|---|---|
| Quantitative Time Courses | Concentration measurements, metabolite levels | Numerical data points | Direct parameter estimation through curve fitting |
| Qualitative Phenotypes | Viability/inviability, oscillatory/non-oscillatory | Inequality constraints | Reduced parameter uncertainty |
| Steady-State Dose Response | EC50 values, activation thresholds | Numerical constants | Definition of system sensitivities |
| Network Topology | Protein-protein interactions, pathway maps | Model structure | Constraint of possible parameter spaces |
Model Similarity and Comparison Frameworks
As the number of biological models grows, comparing and integrating models becomes increasingly important. Research has identified six key aspects relevant for assessing model similarity: (1) underlying encoding, (2) references to biological entities, (3) quantitative behavior, (4) qualitative behavior, (5) mathematical equations and parameters, and (6) network structure [25]. Flexible, problem-specific combinations of these aspects can mimic researchers' intuition about model similarity and support complex model searches in databases—a crucial capability for personalized medicine where multiple models may need integration to capture patient-specific biology.
Formally, similarity between two models M1 and M2 with respect to aspect α is defined as:
simα(M1, M2) = σα(Πα(M1), Πα(M2))
where Πα is the projection of a model onto aspect α and σα is a similarity measure for that aspect [25]. This framework enables systematic comparison of models developed by different research groups or for different aspects of the same biological system, facilitating model integration and reuse in personalized medicine applications.
Technical Implementation: From Theory to Practice
Experimental Workflow for Integrative Studies
The following diagram illustrates the core workflow integrating computational and experimental approaches in systems biology:
This iterative process begins with a biological question, develops computational models to formalize hypotheses, designs experiments to test predictions, integrates resulting data to refine models, and ultimately generates insights applicable to personalized therapeutic strategies. The cycle continues until models achieve sufficient predictive power for clinical applications.
Key Research Reagents and Computational Tools
Successful implementation of systems biology approaches requires specific research reagents and computational tools. The following table details essential resources mentioned in recent literature:
Table 3: Essential Research Reagents and Computational Tools
| Resource Type | Specific Examples | Function in Research | Application Context |
|---|---|---|---|
| Genome-Scale Metabolic Models (GEMs) | Yeast9, Tissue-specific GEMs | Predict flux of metabolites in metabolic networks | Analysis of metabolism across tissues and microbial species [27] [28] |
| Model Repositories & Standards | BioModels Database, SBML, CellML | Enable model sharing, reproducibility, and software interoperability | Encoding and exchange of biological models [25] |
| Annotation Databases | BRENDA, ChEBI | Provide semantic annotations linking model components to biological entities | Standardized representation of model components [25] [28] |
| Optimization Algorithms | Differential evolution, scatter search | Solve parameter identification problems with multiple constraints | Estimation of model parameters from experimental data [6] |
| Multi-tissue Physiological Models | Mixed Meal Model (MMM) | Describe interplay between physiological systems | Integration of tissue-specific GEMs for whole-body predictions [27] [28] |
Protocol: Parameter Identification with Mixed Data Types
Based on the methodology described in [6], the following protocol provides a detailed procedure for identifying model parameters using both qualitative and quantitative data:
Step 1: Model Structure Definition
- Formalize the biological network using appropriate mathematical representations (ODEs, Petri nets, etc.)
- Identify unknown parameters requiring estimation
- Define model outputs corresponding to measurable quantities
Step 2: Data Collection and Formalization
- Quantitative data: Collect numerical measurements (e.g., time-course data, dose-response curves)
- Qualitative data: Gather categorical observations (e.g., viability, relative changes, oscillatory behavior)
- Convert qualitative data into inequality constraints: gi(x) < 0
Step 3: Objective Function Formulation
- Construct quantitative objective term: fquant(x) = Σj (yj,model(x) - yj,data)²
- Construct qualitative objective term: fqual(x) = Σi Ci · max(0, gi(x))
- Combine into total objective function: ftot(x) = fquant(x) + fqual(x)
Step 4: Parameter Estimation
- Select appropriate optimization algorithm (differential evolution recommended for nonlinear problems)
- Set problem-specific constants Ci to balance contributions of different constraint types
- Perform constrained optimization to minimize ftot(x)
Step 5: Uncertainty Quantification
- Apply profile likelihood approach to assess parameter identifiability
- Evaluate confidence intervals for parameter estimates
- Validate identified parameters with held-out experimental data
This protocol was successfully applied to estimate parameters for a Raf inhibition model and a yeast cell cycle model, demonstrating its general applicability to biological systems of different complexities [6].
Applications in Personalized Medicine
Virtual Tumors for Predictive Oncology
The creation of "virtual tumours" represents a powerful application of systems biology in personalized cancer treatment. As described by Jasmin Fisher in the 2025 SysMod meeting, these computational models simulate intra- and inter-cellular signaling in various cancer types, including triple-negative breast cancer, non-small cell lung cancer, melanoma, and glioblastoma [28]. These predictive, mechanistically interpretable models enable researchers to "understand and anticipate emergent resistance mechanisms and to design patient-specific treatment strategies to improve outcomes for patients with hard-to-treat cancers" [28].
The virtual tumor approach exemplifies how systems biology bridges computational modeling and molecular biology by creating digital representations of patient-specific tumors that can be manipulated computationally to test therapeutic strategies before clinical implementation. This methodology aligns with the broader vision of Integrative and Regenerative Pharmacology, which aims to develop "transformative curative therapeutics" that restore physiological structure and function rather than merely managing symptoms [8].
Metabolic Modeling for Personalized Therapeutic Design
Systems biology approaches have demonstrated particular success in metabolic disorders and cancer metabolism through the development of personalized metabolic models. One study presented at the 2025 SysMod meeting embedded "GEMs of the liver, skeletal muscle, and adipocyte into the Mixed Meal Model (MMM), a physiology-based computational model describing the interplay between glucose, insulin, triglycerides and non-esterified fatty acids (NEFAs)" [28]. This multi-scale approach enabled researchers to simulate "personalised hybrid multi-tissue Meal Models" that revealed "changes in tissue-specific flux associated with insulin resistance and liver fat accumulation" [28], demonstrating the power of integrated modeling to identify personalized therapeutic targets.
In cancer research, another study employed "genome-scale metabolic models (GSMMs) integrated with single-cell RNA sequencing data from patient-derived xenograft models to investigate the metabolic basis of breast cancer organotropism" [28]. This approach identified "distinct metabolic adaptations in metastatic tissues" and used "flux-based comparisons of primary tumors predisposed to different metastatic destinations" to identify "metabolic signatures predictive of organotropism" [28]. The resulting models enabled simulation of gene manipulation strategies to identify potential metabolic targets for therapeutic intervention.
The following diagram illustrates how multi-scale modeling integrates different biological levels for personalized therapeutic design:
Integrative and Regenerative Pharmacology
The emerging field of Integrative and Regenerative Pharmacology (IRP) represents a comprehensive application of systems biology principles to therapeutic development. IRP "bridges pharmacology, systems biology and regenerative medicine, thereby merging the two earlier fields" and represents "the emerging science of restoring biological structure and function through multi-level, holistic interventions that integrate conventional drugs with target therapies intended to repair, renew, and regenerate rather than merely block or inhibit" [8].
This approach leverages systems biology methodologies to "define the MoA of therapeutic approaches (e.g., stem cell-derived therapies), accelerating the regulatory approval of advanced therapy medicinal products (ATMPs)" [8]. In this framework, "stem cells can be considered as tunable combinatorial drug manufacture and delivery systems, whose products (e.g., secretome) can be adjusted for different clinical applications" [8], demonstrating how systems biology provides the conceptual and computational tools needed to advance regenerative approaches.
The unifying nature of IRP is its primary strength, as it "envisions achieving therapeutic outcomes that are not possible with pharmacology or regenerative medicine alone" [8]. Furthermore, "IRP aspires to develop precise therapeutic interventions using genetic profiling and biomarkers of individuals" as part of personalized and precision medicine, employing "state-of-the-art methodologies (e.g., omics, gene editing) to assist in identifying the signaling pathways and biomolecules that are key in the development of novel regenerative therapeutics" [8].
Future Directions and Implementation Challenges
Addressing Translational Barriers
Despite its significant promise, the application of systems biology approaches in personalized medicine faces substantial implementation challenges. As noted in research on Integrative and Regenerative Pharmacology, these include "investigational obstacles, such as unrepresentative preclinical animal models," "manufacturing issues, such as scalability, automated production methods and technologies," "complex regulatory pathways with different regional requirements," ethical considerations, and economic factors such as "high manufacturing costs and reimbursement" challenges [8].
These translational barriers are particularly significant for clinical implementation, where "long-term follow-up clinical investigation is required to assess regenerative drugs and biologics beyond initial clinical trials" [8]. Addressing these challenges will require "interdisciplinary clinical trial designs that incorporate pharmacology, bioengineering, and medicine" and cooperation "between academia, industry, clinics, and regulatory authorities to establish standardized procedures, guarantee consistency in therapeutic outcomes, and eventually develop curative therapies" [8].
Technological Advancements and Emerging Methodologies
Future advances in systems biology applications for personalized medicine will likely be driven by several technological developments. Artificial intelligence (AI) represents a particularly promising tool, as "AI has the potential to transform regenerative pharmacology by enabling the development of more efficient and targeted therapeutics, predict DDSs effectiveness as well as anticipate cellular response" [8]. However, challenges remain in implementing AI, "namely, the standardization of experimental/clinical datasets and their conversion into accurate and reliable information amenable to further investigation" [8].
Advanced biomaterials also represent a promising direction, particularly "the development of 'smart' biomaterials that can deliver locally bioactive compounds in a temporally controlled manner" [8]. Specifically, "stimuli-responsive biomaterials, which can alter their mechanical characteristics, shape, or drug release profile in response to external or internal triggers, represent transformative therapeutic approaches" [8] that could be optimized using systems biology models.
Community-driven benchmarking initiatives represent another important direction for advancing systems biology applications. As described in the SysMod meeting, one such initiative aimed at "evaluating and comparing O-ABM for biomedical applications" has enlisted "developers from leading tools like BioDynaMo" [28] to establish standardized evaluation frameworks similar to successful efforts in other scientific domains such as CASP (Critical Assessment of Structure Prediction).
As systems biology continues to mature, its role in personalized medicine will expand, ultimately fulfilling the vision that "regeneration today must be computationally informed, biologically precise, and translationally agile" [8]. Through continued development of integrative approaches that bridge computational modeling and molecular biology, systems biology will increasingly enable the development of truly personalized therapeutic strategies that account for the unique biological complexity of each individual patient.
From Data to Therapy: Methodological Approaches and Clinical Applications
The integration of artificial intelligence (AI) and machine learning (ML) with systems biology is fundamentally transforming biomarker discovery, enabling a shift from reactive disease treatment to proactive, personalized medicine. By decoding complex, multi-scale biological networks, these technologies are accelerating the identification of diagnostic, prognostic, and predictive biomarkers. This whitepaper provides an in-depth technical examination of how AI/ML methodologies are being deployed within a systems biology framework to create predictive models of disease and treatment response. It details cutting-edge computational protocols, presents structured comparative data, and outlines the essential toolkit for researchers and drug development professionals, thereby charting the course toward more precise and effective therapeutic interventions.
Systems biology represents a paradigm shift in biomedical research, moving from a reductionist study of individual molecular components to a holistic analysis of complex interactions within biological systems [29] [30]. This approach views biology as an information science, where biological networks capture, transmit, and integrate signals to govern cellular behavior and physiological responses [29]. When applied to personalized medicine, systems biology aims to understand how disease-perturbed networks differ from healthy states, thereby enabling the identification of molecular fingerprints that can guide clinical decisions [29].
The core premise is that diseases are rarely caused by a single gene or protein but rather by perturbations in complex molecular networks [29]. AI and ML serve as the critical computational engine that powers this framework. They provide the capacity to analyze vast, multi-dimensional datasets—genomics, transcriptomics, proteomics, metabolomics, and clinical data—to identify patterns and relationships that are imperceptible to traditional statistical methods [31] [32]. This synergy is crucial for biomarker discovery, as it allows researchers to move beyond single, often inadequate, biomarkers to multi-parameter biomarker panels that offer a more comprehensive view of an individual's health status and likely response to therapy [29] [31].
Biomarker Types and Their Clinical Application in Precision Oncology
Biomarkers are objectively measurable indicators of biological processes, pathological states, or responses to therapeutic intervention [32]. In precision medicine, they are foundational for diagnosis, prognosis, and treatment selection. The table below categorizes key biomarker types and their roles, with a focus on oncology applications.
Table 1: Classification and Clinical Applications of Biomarkers in Precision Oncology
| Biomarker Type | Clinical Role | Example | Application Context |
|---|---|---|---|
| Diagnostic | Identifies the presence or subtype of a disease | MSI (Microsatellite Instability) status in colorectal cancer [33] | Differentiates cancer subtypes for initial diagnosis. |
| Prognostic | Provides information on the likely course of the disease | Deep learning features from histopathology images in colorectal cancer [34] | Forecasts disease aggressiveness and patient outcome independent of therapy. |
| Predictive | Indicates the likelihood of response to a specific therapeutic | MARK3, RBCK1, and HSF1 for regorafenib response in mCRC [33] | Guides therapy selection by predicting efficacy of a targeted drug. |
| Pharmacodynamic | Measures the biological response to a therapeutic intervention | Dynamic changes in transcriptomic profiles during viral infection or T2D onset [13] | Confirms drug engagement and assesses biological effect during treatment. |
The challenge in oncology, particularly for complex diseases like metastatic colorectal cancer (mCRC), is that few validated predictive biomarkers exist. For instance, despite the efficacy of regorafenib in some elderly mCRC patients, no biomarkers are currently available to predict which individuals will benefit, highlighting a critical unmet need that AI-driven systems biology approaches aim to address [33].
AI and Machine Learning Methodologies in Biomarker Discovery
AI and ML algorithms are uniquely suited to handle the high dimensionality, noise, and complexity of biological data. Their application spans the entire biomarker discovery pipeline, from data integration and feature selection to model building and validation.
Key Machine Learning Approaches
ML methodologies can be broadly categorized into supervised and unsupervised learning, each with distinct applications in biomarker research.
Table 2: Machine Learning Methodologies for Different Omics Data Types in Biomarker Discovery
| Omics Data Type | ML Techniques | Typical Applications | Considerations |
|---|---|---|---|
| Transcriptomics | Feature selection (e.g., LASSO); SVM; Random Forest [31] | Identifying gene expression signatures associated with disease subtypes or drug response. | High-dimensional data requires robust feature selection to avoid overfitting. |
| Proteomics | Random Forest; XGBoost [35] | Classifying predictive biomarker potential based on network features and protein properties. | Handles complex, non-linear relationships between protein features and biomarker status. |
| Multi-Omics Integration | Deep Learning (CNNs, RNNs, Transformers) [31] [32] | End-to-end learning from integrated genomic, transcriptomic, and proteomic data for patient stratification. | Requires large sample sizes and significant computational resources; "black box" interpretability challenges. |
| Histopathology Images | Convolutional Neural Networks (CNNs) [34] [31] | Extracting prognostic and predictive features directly from standard histology slides. | Can outperform human observation and established molecular markers [34]. |
The Role of Deep Learning and Large Language Models
Deep learning (DL) architectures, particularly CNNs and Recurrent Neural Networks (RNNs), have proven highly effective for complex data types like imaging and sequential omics data [31]. Transformers and Large Language Models (LLMs) are increasingly being adapted to analyze biological sequences and integrate multi-modal data, enabling precise disease risk stratification and diagnostic determinations by identifying complex non-linear associations [32].
Experimental Protocols and Workflows
The application of AI/ML in biomarker discovery follows rigorous computational and experimental protocols. Below are detailed methodologies for two key approaches: digital patient modeling and machine learning-based biomarker classification.
Protocol 1: In Silico Clinical Trial Using Digital Patient Modeling
This protocol, derived from a study on regorafenib in mCRC, outlines the steps for simulating drug response in a virtual patient population [33].
Objective: To simulate individualized mechanisms of action and identify predictive biomarkers of regorafenib response in elderly mCRC patients.
Methodology:
- Data Acquisition and Curation:
- Patient Transcriptomics: Obtain gene expression data from mCRC biopsies of untreated elderly patients (e.g., from GEO database, TCGA). Include a set of healthy control samples from the same tissue type [33].
- Drug Target Information: Compile a list of known pharmacological protein targets of the drug (e.g., 18 targets for regorafenib from DrugBank) [33].
- Disease Molecular Definition: Manually curate a set of proteins with documented roles in the disease (mCRC), annotated as activation-associated (+1) or inhibition-associated (-1), to form the core knowledge set for modeling [33].
Generation of Individual Differential Expression (IDE) Signatures:
- Normalization: Apply cross-platform normalization (e.g., CuBlock) to all gene expression samples at the probe level [33].
- Protein-level Conversion: Convert probe-level expression to protein-level expression by averaging all probes mapping to the same protein [33].
- Differential Expression Calling: For each patient sample, compare protein expression levels against the distribution in healthy controls. Proteins with expression above the 95th percentile or below the 5th percentile of the healthy distribution are considered upregulated (+1) or downregulated (-1), respectively [33].
- IDE Refinement: Filter the IDE signatures by retaining only proteins that are both differentially expressed at the population level (using Welch’s t-test/DESeq2 with FDR < 0.05) and lie within three interaction links of the core mCRC protein knowledge set in a protein interaction network [33].
Therapeutic Performance Mapping System (TPMS) Modeling:
- Network Construction: Build mathematical models based on the Human Protein Network (HPN), integrating physical interactions, signaling pathways, and gene regulation from curated databases (KEGG, REACTOME, BIOGRID, etc.) [33].
- Signal Propagation: Simulate the drug's effect by introducing the target inhibition stimulus into the HPN. The signal propagates through the network over iterative steps. In each step, nodes integrate weighted inputs from upstream neighbors, transforming the sum via a hyperbolic tangent function to normalize and limit signal magnitude [33].
- Individualized Simulation: Execute the TPMS model for each patient's specific IDE signature to simulate their unique response to the drug stimulus [33].
Biomarker Identification and Validation:
- Analysis: Correlate the simulated network states or protein activity levels with the predicted drug response outcomes to identify proteins associated with both the drug's mechanism of action and treatment efficacy [33].
- Validation: Validate candidate biomarkers (e.g., MARK3, RBCK1, HSF1) in an independent cohort of mCRC patients and cross-reference with previously reported predictive miRNAs [33].
The following diagram illustrates the digital patient modeling workflow:
Protocol 2: Machine Learning Classification of Predictive Biomarkers
This protocol details the methodology for the MarkerPredict tool, which uses ML to classify the potential of proteins as predictive biomarkers [35].
Objective: To develop a hypothesis-generating framework (MarkerPredict) that classifies target-interacting proteins as potential predictive biomarkers for targeted cancer therapeutics.
Methodology:
- Data Compilation and Network Analysis:
- Signaling Networks: Utilize three signed signaling networks: Human Cancer Signaling Network (CSN), SIGNOR, and ReactomeFI [35].
- Motif Identification: Identify all three-nodal network motifs (triangles) using the FANMOD tool. Focus on triangles containing both a known oncotherapeutic target and an interacting protein (neighbor) [35].
- Protein Disorder Annotation: Annotate all proteins using intrinsic disorder databases and prediction methods (DisProt, IUPred, AlphaFold) [35].
Training Set Construction:
- Positive Controls: Annotate neighbor-target pairs where the neighbor is an established predictive biomarker for the drug targeting its pair, using the CIViCmine text-mining database. Manually review for accuracy (Class 1) [35].
- Negative Controls: Construct a set of neighbor-target pairs where the neighbor is not listed as a predictive biomarker in CIViCmine, supplemented by random pairs and proteins absent from CIViCmine [35].
Feature Engineering and Model Training:
- Feature Extraction: For each neighbor-target pair, extract features including network topological properties (e.g., motif type, centrality measures) and protein annotations (e.g., intrinsic disorder scores) [35].
- Model Selection and Training: Train multiple binary classification models, including Random Forest and XGBoost, on network-specific and combined data, and on individual and combined IDP databases. Optimize hyperparameters using competitive random halving [35].
- Validation: Evaluate model performance using Leave-One-Out Cross-Validation (LOOCV), k-fold cross-validation, and a 70:30 train-test split, assessing AUC, accuracy, and F1-score [35].
Classification and Scoring:
- Biomarker Probability Score (BPS): Apply the trained models to classify all potential neighbor-target pairs in the networks. Define a Biomarker Probability Score (BPS) as a normalized summative rank across all models to prioritize candidates for experimental validation [35].
The following diagram illustrates the MarkerPredict classification workflow:
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents, tools, and data resources essential for conducting AI-driven biomarker discovery research within a systems biology framework.
Table 3: Essential Research Reagent Solutions for AI-Driven Biomarker Discovery
| Resource Category | Item | Function and Application |
|---|---|---|
| Data Resources | GEO Database [33] | Public repository for transcriptomic data, used to obtain patient and control samples for analysis. |
| The Cancer Genome Atlas (TCGA) [33] | Source of multi-omics data (e.g., RNA-seq) for model training and validation in oncology. | |
| DrugBank [33] | Curated database of drug and drug target information, essential for defining the molecular stimulus in drug response modeling. | |
| CIViCmine [35] | Text-mining database of clinical interpretations for variants in cancer, used to construct training sets for ML models. | |
| Software & Algorithms | Therapeutic Performance Mapping System (TPMS) [33] | A systems biology platform that uses a neural network-like algorithm to simulate drug mechanisms of action on individual patient molecular profiles. |
| FANMOD [35] | Software tool for network motif detection, used to identify significant three-nodal motifs in signaling networks. | |
| Random Forest / XGBoost [35] [31] | High-performance, interpretable machine learning algorithms used for classifying biomarker potential and analyzing omics data. | |
| Cytoscape [36] [37] | Open-source platform for complex network analysis and visualization, used to map and interpret disease-perturbed networks and interactions. | |
| Laboratory Reagents | High-Throughput Sequencing Kits (RNA-seq, miRNA-seq) [37] | Generate global transcriptomic data from patient samples, forming the primary input for differential expression and IDE signature analysis. |
| Mass Spectrometry Reagents [32] [37] | Enable high-throughput proteomic and metabolomic profiling to measure protein abundance, modifications, and metabolite levels. | |
| Ac-VAD-AFC | Ac-VAD-AFC|Fluorogenic Caspase Substrate| | Ac-VAD-AFC is a fluorogenic caspase-1 substrate for apoptosis research. For Research Use Only. Not for diagnostic or therapeutic use. |
| Fgfr4-IN-18 | Fgfr4-IN-18, MF:C32H35Cl2N9O6, MW:712.6 g/mol | Chemical Reagent |
Challenges and Future Directions
Despite the significant promise, several challenges impede the widespread clinical adoption of AI-driven biomarker discovery.
- Data Heterogeneity and Quality: Inconsistent standardization protocols, batch effects, and data interoperability issues can lead to biased models and misleading conclusions [31] [32]. Ensuring high-quality, harmonized, and ML-ready data is paramount [36].
- Model Interpretability and Trust: Many advanced ML models, particularly deep learning, operate as "black boxes," making it difficult for clinicians to understand and trust the predictions. The development of explainable AI (XAI) methods is critical for clinical translation [34] [31].
- Generalizability and Validation: Models trained on one cohort often fail to generalize to different populations or healthcare settings. Rigorous external validation using independent cohorts and prospective studies is essential to ensure robustness and clinical reliability [31] [32].
- Regulatory and Ethical Hurdles: The dynamic nature of AI models presents challenges for regulatory frameworks. Establishing pathways for FDA and EMA approval of AI-based biomarkers requires adaptive yet stringent validation frameworks [34] [32].
Future directions will likely focus on strengthening integrative multi-omics approaches, conducting large-scale longitudinal cohort studies to capture dynamic biomarker changes, incorporating real-time data from wearable devices, and leveraging edge computing for deployment in low-resource settings [32]. Furthermore, the direct linking of genomic data to functional outcomes, such as the prediction of biosynthetic gene clusters for novel antibiotic discovery, represents an exciting frontier [31].
The confluence of AI, machine learning, and systems biology is ushering in a new era in personalized medicine. By providing the computational power to model the breathtaking complexity of human biology, these technologies are dramatically accelerating the discovery of robust, clinically actionable biomarkers. From in silico clinical trials that simulate drug effects in digital patients to machine learning classifiers that prioritize biomarker candidates from network features, the methodologies outlined herein are transforming biomarker discovery from a slow, candidate-driven process to a rapid, systems-level science. As the field continues to mature by addressing challenges of data quality, model interpretability, and clinical validation, AI-powered biomarker discovery is poised to fulfill the promise of precision medicine, delivering truly personalized healthcare based on the unique molecular makeup of each individual.
Quantitative Systems Pharmacology (QSP) is an advanced discipline that uses computational modeling and experimental data to bridge the gap between biology, pharmacology, and disease processes. By constructing mechanistic mathematical models that simulate the complex interactions between drugs, biological systems, and diseases, QSP provides a robust platform for predicting clinical outcomes and optimizing therapeutic strategies [38]. This approach represents a paradigm shift from traditional pharmacometric methods, moving beyond empirical relationships to capture the underlying biological mechanisms that drive drug response variability across patient populations.
The role of QSP within personalized medicine is transformative. Personalized medicine aims to move beyond one-size-fits-all treatment by tailoring therapy to the unique biology of the disease and the biography of the person with the disease [39]. QSP supports this mission through its ability to simulate virtual patient populations and create digital twins that account for individual variability in genetics, pathophysiology, and biosocial factors [38]. This capability is particularly impactful for rare diseases and pediatric populations where clinical trials are often unfeasible, enabling drug developers to explore personalized therapies with unprecedented precision while bypassing dose levels that would traditionally require live trials [38].
Fundamental Principles of QSP Modeling
Mathematical and Computational Foundations
QSP model development relies heavily on preexisting knowledge and requires a comprehensive understanding of current physiological concepts, often making use of heterogeneous and aggregated datasets from multiple sources [40]. The foundational workflow for QSP model development and application can be delineated into three major elements: (1) defining the model, (2) qualifying the model, and (3) performing simulations [40]. This workflow typically centers around the construction of ordinary differential equation models but may be extended beyond this framework to include more complex mathematical representations.
The development of QSP models presents unique challenges, particularly in determining an optimal model structure while balancing model complexity and uncertainty [40]. Additionally, QSP model calibration is arduous due to data scarcity, especially at the human subject level, which necessitates the use of sophisticated parameter estimation approaches and sensitivity analyses earlier in the modeling workflow compared to traditional population modeling approaches [40]. This rigorous process ensures that resulting models don't simply accept assumptions but identify knowledge gaps and force necessary questions to be asked, ultimately leading to more robust and validated predictive tools [38].
Integration with Systems Biology and Immunology
QSP finds particularly powerful application in systems immunology, where it helps decipher the extraordinary complexity of the mammalian immune system—an intricate network comprising an estimated 1.8 trillion cells that utilize around 4,000 distinct signaling molecules to coordinate its responses [41]. The immune system operates as a dynamic, multiscale, and adaptive network composed of heterogeneous cellular and molecular entities interacting through complex signaling pathways, feedback loops, and regulatory circuits [41]. QSP models in immuno-oncology and inflammatory diseases capture these emergent properties such as robustness, plasticity, memory, and self-organization, which arise from local interactions and global system-level behaviors [41].
Table 1: Key Characteristics of QSP in Drug Development
| Aspect | Traditional Approaches | QSP-Enabled Approach |
|---|---|---|
| Basis | Empirical relationships | Mechanistic understanding |
| Patient Variability | Statistical representation | Biological and physiological sources |
| Trial Design | Physical patient recruitment | Virtual populations and digital twins |
| Animal Testing | Heavy reliance | Reduction, refinement, and replacement |
| Therapeutic Personalization | Limited by trial constraints | Tailored to individual biology and biography |
QSP Workflow: From Model Development to Application
Systematic Model Development Process
The QSP modeling workflow follows a structured approach to ensure predictive reliability and clinical relevance. The initial phase involves systematic literature reviews and aggregation of heterogeneous datasets from multiple sources to inform model structure [40]. This foundational work supports the selection of appropriate structural model equations that mathematically represent the biological system, disease pathophysiology, and drug mechanisms. The model development process must carefully balance mechanistic depth with practical identifiability constraints, as over-parameterization can render models unstable or uninformative.
A critical challenge in QSP model development is parameter estimation amidst data scarcity, particularly for human-specific biological processes [40]. This necessitates the implementation of advanced sensitivity analyses and parameter optimization techniques to ensure models are both biologically plausible and mathematically robust. The subsequent model qualification phase involves rigorous validation against experimental and clinical data to verify predictive performance, with continuous refinement based on emerging evidence [40]. This comprehensive development process ensures that QSP models serve as reliable platforms for generating testable hypotheses and informing clinical decisions.
Virtual Population Generation and Simulation
A powerful application of QSP is the generation of virtual populations and digital twins that enable in silico clinical trials [38]. Using techniques such as virtual population simulations, QSP models can capture the natural biological variability observed in real patient populations, allowing researchers to explore differential treatment responses across diverse demographic, genetic, and pathophysiological profiles [42]. This approach is particularly valuable for studying rare diseases, pediatric populations, and other clinical scenarios where traditional trials are ethically challenging or practically impossible to conduct [38].
The process of virtual population generation involves sophisticated computational methods that ensure each virtual patient embodies a physiologically plausible combination of parameters while collectively representing the heterogeneity of the target population [42]. These virtual cohorts then undergo simulated interventions, with QSP models predicting pharmacokinetic profiles, pharmacodynamic responses, and ultimate clinical outcomes for each individual. This methodology enables researchers to identify biomarkers of response, optimize dosing strategies, and predict subpopulation effects before initiating costly clinical trials, ultimately accelerating the development of personalized therapeutic approaches [41].
Quantitative Applications and Impact
Drug Development Efficiency and Cost Savings
The implementation of QSP in pharmaceutical R&D delivers substantial quantitative benefits in both efficiency and cost reduction. Analyses from industry leaders like Pfizer estimate that Model-Informed Drug Development (MIDD)—enabled by approaches such as QSP, PBPK, and QST modeling—saves companies approximately $5 million and 10 months per development program [38]. These impressive figures represent only part of the value proposition, as QSP additionally helps companies make crucial go/no-go decisions earlier in drug development by eliminating programs with no realistic chance of success, thereby redirecting resources to more promising candidates.
The scalability of QSP models further amplifies these benefits, as each model serves as a knowledge repository that grows more valuable with every application [38]. Learnings from one therapeutic area or modality can often be applied to others, multiplying cost savings and fostering innovation across the R&D portfolio. Furthermore, models developed for an initial reference indication can continue delivering value to subsequent indications, streamlining clinical dosage optimization and strategic decisions throughout a drug's lifecycle [38].
Table 2: Quantitative Benefits of QSP in Drug Development
| Metric | Impact | Application Context |
|---|---|---|
| Cost Savings | $5 million per program | Overall development efficiency [38] |
| Time Savings | 10 months per program | Accelerated development timelines [38] |
| Animal Testing Reduction | Significant reduction | Alignment with FDA's push to reduce, refine, and replace animal testing [38] |
| Regulatory Submissions | Increased leveraging of QSP | Growing regulatory acceptance at FDA and other agencies [38] |
Advancing Personalized Medicine Through Clinical Applications
QSP demonstrates particular strength in advancing personalized medicine across multiple therapeutic domains, with significant applications in immuno-oncology, inflammatory diseases, and rare disorders. In oncology, QSP models have been developed to simulate perturbations to immune activity in the solid tumor microenvironment, whole-patient and spatial dynamics for immuno-oncology, and personalized radiotherapy with integrated scientific modeling [42]. These applications enable researchers to explore combination therapies, identify biomarkers of response, and optimize treatment schedules for individual patients based on their unique tumor biology and immune status.
The integration of machine learning and artificial intelligence techniques with traditional QSP modeling has further enhanced its personalization capabilities [41]. For instance, machine learning-empowered PBPK and QSAR models can predict the pharmacokinetics of drugs and nanoparticles, while AI-driven analysis of multi-omics data (transcriptomics, proteomics, and immune cell profiling) improves diagnostics in autoimmune and inflammatory diseases and predicts individual vaccine responses [41]. These computational advances, combined with the growing availability of high-dimensional biological data, are strengthening the translational bridge from quantitative modeling to clinically actionable insights.
Experimental Protocols and Methodologies
QSP Model Development and Validation Protocol
Objective: To develop and validate a QSP model for simulating drug actions and patient responses in a specific disease context.
Materials and Software Requirements:
- Computational Environment: MATLAB, R, Python, or specialized QSP platforms (e.g., Certara's QSP solutions) [40]
- Data Curation Tools: Systematic literature review databases, data normalization algorithms
- Parameter Estimation Algorithms: Maximum likelihood estimation, Bayesian methods, Markov Chain Monte Carlo (MCMC)
- Sensitivity Analysis Tools: Sobol method, Morris elementary effects, partial rank correlation coefficients
- Validation Metrics: Goodness-of-fit measures, prediction error quantification, visual predictive checks
Methodology:
- Problem Formulation and Scope Definition: Clearly articulate the research questions, clinical decisions, and predictive outcomes the model will address.
- Knowledge Assembly and Data Integration: Conduct systematic literature reviews to identify key pathways, mechanisms, and quantitative parameters. Aggregate heterogeneous datasets from multiple sources, including in vitro studies, animal experiments, and clinical trials [40].
- Model Structure Design: Develop a mechanistic model framework using ordinary differential equations that capture the essential biological processes, drug mechanisms, and disease pathophysiology.
- Parameter Estimation and Optimization: Calibrate model parameters using available data, employing appropriate estimation techniques that account for uncertainty and variability [40].
- Sensitivity and Identifiability Analysis: Perform comprehensive sensitivity analysis to identify parameters that most influence model outputs and assess practical identifiability given available data.
- Model Validation: Test model predictions against experimental data not used during model development, employing both qualitative and quantitative validation metrics [40].
- Virtual Simulation Experiments: Execute simulated interventions, including clinical trials, dose optimization, and combination therapies, using virtual populations representing relevant patient heterogeneity.
Virtual Patient Generation and Simulation Protocol
Objective: To generate virtual patient populations that capture real-world biological variability and simulate their responses to therapeutic interventions.
Materials and Software Requirements:
- Population Generation Tools: Monte Carlo sampling algorithms, Bayesian population methods
- Clinical Data Sources: Electronic health records, clinical trial databases, omics datasets
- Covariate Models: Statistical distributions of demographic, genetic, and physiological parameters
- Simulation Platforms: High-performance computing environments, cloud-based simulation infrastructure
Methodology:
- Covariate Selection and Distribution Fitting: Identify key patient characteristics that influence drug response and fit appropriate statistical distributions to population data.
- Parameter Correlation Structure Definition: Establish relationships between model parameters based on physiological principles and clinical data.
- Virtual Population Generation: Implement sampling algorithms that generate virtual patients with physiologically plausible combinations of parameters while maintaining population-level diversity [42].
- Simulation Design: Define intervention protocols, including dosing regimens, combination therapies, and treatment durations.
- Output Analysis and Interpretation: Implement statistical methods to analyze simulation results, identify response subgroups, and quantify uncertainty in predictions.
- Validation Against Clinical Data: Compare virtual trial outcomes with real-world evidence when available to refine population models and increase predictive accuracy.
Signaling Pathways and Workflow Visualization
QSP Workflow Diagram
QSP Modeling Workflow: This diagram illustrates the systematic process for developing and applying QSP models, from initial problem formulation through clinical decision support.
Virtual Patient Simulation Diagram
Virtual Patient Simulation: This diagram outlines the process for generating virtual patient populations and simulating their responses to therapeutic interventions.
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Computational Tools for QSP
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| Omics Datasets | Parameterize and validate QSP models | Transcriptomics, proteomics, metabolomics data from public repositories and clinical studies [41] |
| Mechanistic QSP Platforms | Implement and simulate QSP models | Certara's QSP Platform, MATLAB with Systems Biology Toolbox, R with packages for differential equations [38] [40] |
| Parameter Estimation Tools | Calibrate model parameters against experimental data | Maximum likelihood estimation software, Bayesian inference tools, Markov Chain Monte Carlo (MCMC) algorithms [40] |
| Sensitivity Analysis Software | Identify influential parameters and assess identifiability | Sobol method implementation, Morris elementary effects, partial rank correlation coefficients [40] |
| Virtual Population Generators | Create in silico patient cohorts with physiological variability | Monte Carlo sampling tools, Bayesian population methods, covariance structure modeling [42] |
| Model Validation Frameworks | Assess predictive performance and credibility | Goodness-of-fit metrics, visual predictive checks, external validation protocols [40] |
| High-Performance Computing | Execute large-scale simulations and virtual trials | Cloud computing infrastructure, parallel processing environments, simulation management systems [38] |
Future Directions and Concluding Perspectives
The future trajectory of QSP points toward increasingly integrative approaches that incorporate more sophisticated representations of human biology, including enhanced spatial resolution, multi-scale interactions, and deeper integration of AI and machine learning methodologies [41]. The growing regulatory acceptance of QSP approaches, as evidenced by increased submissions to agencies like the FDA, suggests these methods are transitioning from emerging technologies to standard tools in drug development [38]. This normalization within the pharmaceutical industry will likely accelerate as best practices for model qualification and validation become more established and widely disseminated.
A critical frontier for QSP is the more comprehensive incorporation of the biosocial dimension of personalized medicine—moving beyond the molecular characterization of disease to include what has been described as the "biography" of the individual [39]. This includes factors such as emotional distress, which has been shown to significantly impact clinical outcomes—for example, reducing median progression-free survival from 15.5 months to 7.9 months in patients with advanced non-small cell lung cancer undergoing treatment with immune checkpoint inhibitors [39]. Future QSP models that successfully integrate these biosocial factors with mechanistic biology will come closer to fulfilling the original promise of personalized medicine: therapy tailored to both the unique biology of the disease and the distinctive characteristics of the person with the disease [39].
Multi-omics integration represents a transformative approach in systems biology that combines diverse biological data layers—including genomics, transcriptomics, epigenomics, proteomics, and metabolomics—to construct comprehensive molecular portraits of disease heterogeneity. This methodology enables the identification of distinct disease subtypes with significant implications for prognosis and treatment selection, moving beyond traditional single-marker approaches toward network-based disease understanding [17]. The fundamental premise is that complex diseases like cancer, neurodegenerative disorders, and cardiovascular conditions manifest through dysregulated biological networks rather than isolated molecular defects, necessitating integrated analytical frameworks to capture their full complexity [8].
Within personalized medicine, multi-omics integration provides the analytical foundation for precision oncology and therapeutic stratification by linking molecular signatures to clinical outcomes. By simultaneously analyzing multiple molecular layers, researchers can identify coordinated alterations across biological pathways that remain invisible when examining individual omics layers separately [43]. This holistic perspective aligns with the core principles of systems biology, which seeks to understand biological systems as integrated networks rather than collections of isolated components [8]. The resulting biomarker signatures offer unprecedented opportunities for patient stratification, therapeutic targeting, and clinical trial design based on molecular subtype-specific vulnerabilities.
Computational Methodologies for Multi-Omics Integration
Technical Approaches and Algorithms
Multi-omics integration employs sophisticated computational strategies that can be broadly categorized into network-based fusion, matrix factorization, and machine learning approaches. Each methodology offers distinct advantages for specific research contexts and data structures, with the choice of algorithm significantly impacting the biological interpretability and clinical applicability of the resulting subtypes [44] [45].
Table 1: Computational Methods for Multi-Omics Integration
| Method Category | Representative Algorithms | Key Characteristics | Best Use Cases |
|---|---|---|---|
| Network-Based Fusion | EMitool, SNF, ANF | Constructs patient similarity networks; preserves global data structure; high computational complexity | Cancer subtyping with survival differences |
| Matrix Factorization | IntNMF, LRAcluster, iClusterPlus | Decomposes data into latent components; distribution-agnostic; sensitive to initialization | Identifying shared structures across omics layers |
| Bayesian Models | iClusterBayes | Statistical inference for joint modeling; mature implementation; resource-intensive | Data with clear probabilistic structures |
| Clustering Ensembles | PINSPlus, CIMLR | Robust against noise; rapid convergence; limited interpretability | Large-scale data processing |
| Pathway-Informed Methods | MKKM with pathway kernels | Incorporates prior biological knowledge; enhanced interpretability; complex implementation | Biologically-driven subtype discovery |
The EMitool (Explainable Multi-omics Integration Tool) exemplifies recent advances in network-based approaches, leveraging a weighted nearest neighbor algorithm to integrate multi-omics data in a transparent, data-driven manner [44]. Unlike "black box" methods, EMitool assigns explicit weights to each omics type by evaluating the predictive power of within-omics and cross-omics similarity, allowing quantitative assessment of each omics layer's contribution to patient subtypes [44] [46]. This explainability addresses a critical limitation in earlier integration methods, which often failed to establish clear links between identified subtypes and their underlying molecular drivers.
The MOVICS (Multi-Omics Integration and Clustering in Cancer Subtyping) R package provides a unified framework implementing ten state-of-the-art clustering algorithms, enabling robust molecular subtyping through consensus approaches [43] [47]. This comprehensive toolkit facilitates method comparison and consensus subtype identification, particularly valuable for heterogeneous diseases like pancreatic cancer and glioma where single-algorithm approaches may yield unstable results [43].
Integration Workflows and Pathway Analysis
Multi-omics integration follows systematic workflows that transform raw molecular measurements into clinically actionable subtypes. The process typically begins with data preprocessing and feature selection, followed by integrated clustering and biological validation [43] [47].
Pathway enrichment analysis transforms molecular signatures into biological insights through methods like Gene Set Enrichment Analysis (GSEA) and Gene Set Variation Analysis (GSVA) [43]. These approaches evaluate whether specific biological pathways show coordinated dysregulation within identified subtypes, connecting computational findings to established biological knowledge. For example, glioma subtyping has revealed distinct pathway activations: CS1 (astrocyte-like) subtypes display glial lineage features and immune-regulatory signaling, CS2 (basal-like/mesenchymal) subtypes exhibit epithelial-mesenchymal transition and stromal activation, while CS3 (proneural-like) subtypes show metabolic reprogramming with immunologically cold microenvironments [47].
Experimental Protocols for Multi-Omics Subtyping
Data Acquisition and Preprocessing
Robust multi-omics subtyping begins with systematic data acquisition from coordinated molecular profiling. The TCGA (The Cancer Genome Atlas) Pan-Cancer Atlas provides comprehensive data for 31 cancer types, including mRNA expression, DNA methylation, miRNA profiles, and somatic mutations [44]. Standardized preprocessing ensures cross-platform comparability, including log-transformation of expression data (TPM values), probe selection for methylation arrays targeting promoter-associated CpG islands, and binary mutation encoding (mutated=1, wild-type=0) [43] [47].
Feature selection prioritizes biologically informative variables while reducing dimensionality. The getElites() function in MOVICS selects top variable features based on median absolute deviation (MAD)—typically 1,500 mRNAs, 1,500 lncRNAs, 200 miRNAs, and 1,500 variable methylation loci [43]. Additionally, univariate Cox regression (p<0.05) identifies prognostically significant features, focusing subsequent analysis on molecular features with potential clinical relevance [47].
Integrative Clustering and Validation
Determining the optimal cluster number represents a critical step in subtype discovery. The getClustNum() function implements multiple metrics including Clustering Prediction Index, Gap Statistics, and Silhouette scores to identify biologically plausible cluster numbers [43]. Following parameter optimization, consensus clustering integrates results from multiple algorithms (SNF, PINSPlus, NEMO, COCA, LRAcluster, ConsensusClustering, IntNMF, CIMLR, MoCluster, and iClusterBayes) to derive robust subtypes [43].
Experimental validation confirms the biological and clinical significance of computationally derived subtypes. This includes survival analysis using Kaplan-Meier curves and log-rank tests to assess prognostic differences, pathological stage enrichment analysis to evaluate clinical correlations, and immune microenvironment characterization using deconvolution algorithms (TIMER, CIBERSORT, xCell, MCP-counter, quanTIseq, EPIC) [44] [43]. For example, in kidney renal clear cell carcinoma (KIRC), EMitool identified three subtypes with significant survival differences (p<0.05) and distinct immune compositions [44].
Table 2: Performance Comparison of Multi-Omics Integration Methods Across 31 Cancer Types
| Integration Method | Cancer Types with Significant Survival Differences | Key Strengths | Notable Limitations |
|---|---|---|---|
| EMitool | 22/31 | Explainable weights for omics contributions, superior subtyping accuracy | Complex implementation |
| SNF | 20/31 | Effective capture of sample relationships, comprehensive integration | High computational complexity, multiple iterations required |
| NEMO | 18/31 | Leverages local neighborhood information, no imputation needed | Requires shared omics measurements |
| iClusterPlus | N/R | Widely used, mature implementation | High computational resource consumption |
| IntNMF | N/R | Distribution-agnostic, adaptable to various data types | Sensitive to initialization, computationally intensive |
Biomarker Discovery and Functional Characterization
Differential expression analysis identifies subtype-specific biomarkers using methods like edgeR with adjusted p-value thresholds (<0.05) and sorting by absolute log2 fold change [43]. Functional validation employs RT-qPCR, western blotting, and immunohistochemistry to confirm protein-level expression differences in candidate biomarkers like A2ML1 in pancreatic cancer [43].
In vitro and in vivo functional experiments elucidate mechanistic roles of identified biomarkers. For example, A2ML1 was shown to promote pancreatic cancer progression through LZTR1 downregulation and subsequent KRAS/MAPK pathway activation, ultimately driving epithelial-mesenchymal transition (EMT) [43]. Such mechanistic insights transform computational predictions into biologically validated therapeutic targets.
Research Reagent Solutions for Multi-Omics Studies
Essential Research Tools and Platforms
Table 3: Essential Research Reagent Solutions for Multi-Omics Integration Studies
| Reagent/Platform | Function | Application Example |
|---|---|---|
| TCGA Pan-Cancer Atlas | Provides standardized multi-omics data across 33 cancer types | Benchmarking integration algorithms across 31 cancer types [44] |
| MOVICS R Package | Implements 10 clustering algorithms with standardized pipeline | Identifying consensus subtypes in pancreatic cancer and glioma [43] [47] |
| COPS R Package | Evaluates clustering stability and prognostic relevance | Comparing data-driven vs. pathway-driven clustering in 7 cancers [45] |
| CIBERSORT/xCell/EPIC | Deconvolutes immune cell populations from transcriptomic data | Characterizing immune microenvironment across subtypes [43] |
| AWS HealthOmics | Cloud-based genomic analysis with scalable computing | Processing whole exome/genome sequencing data [48] |
| Columbia Combined Cancer Panel | Targeted NGS panel querying 586 cancer-related genes | Clinical genomic testing with therapeutic implications [48] |
Signaling Pathways in Multi-Omics Subtyping
Molecular Pathways Underlying Disease Subtypes
Multi-omics subtyping consistently identifies specific signaling pathways that drive disease heterogeneity and therapeutic responses. The KRAS/MAPK pathway emerges as a critical regulator across multiple cancer types, with activation patterns distinguishing aggressive from indolent subtypes [43]. In pancreatic cancer, the A2ML1 gene promotes epithelial-mesenchymal transition through LZTR1 downregulation and subsequent KRAS/MAPK activation, establishing a mechanistically defined subtype with distinct clinical behavior [43].
Immunomodulatory pathways consistently differentiate subtypes with implications for immunotherapy response. Analysis across glioma subtypes revealed discrete immune microenvironments: CS2 (basal-like/mesenchymal) subtypes show elevated PD-L1 expression and T-cell infiltration, suggesting susceptibility to checkpoint blockade, while CS3 (proneural-like) subtypes exhibit metabolically cold microenvironments with hypoxia and OXPHOS activation, potentially requiring alternative therapeutic strategies [47].
Metabolic reprogramming represents another hallmark of distinct molecular subtypes. Glioma subtyping revealed CS3 (proneural-like) tumors with pronounced oxidative phosphorylation (OXPHOS) and hypoxic response signatures, suggesting potential vulnerability to metabolic inhibitors [47]. Similarly, pancreatic cancer subtypes show differential engagement of glycolytic and mitochondrial metabolic pathways, with implications for both prognosis and therapy selection [43].
Applications in Precision Medicine and Therapeutics
Clinical Translation and Therapeutic Implications
Multi-omics integration directly informs personalized treatment strategies by linking molecular subtypes to therapeutic vulnerabilities. In oncology, comprehensive molecular subtyping enables biomarker-guided therapy selection beyond single-gene alterations. For example, glioma subtyping identifies CS2 (basal-like/mesenchymal) patients as potential candidates for checkpoint blockade due to their immunologically active microenvironments, while CS3 (proneural-like) patients might benefit from metabolic inhibitors targeting OXPHOS or hypoxia pathways [47].
Drug sensitivity prediction represents another critical application, connecting molecular subtypes with treatment response patterns. Machine learning approaches applied to multi-omics data have identified subtype-specific drug sensitivities, with ridge regression models demonstrating superior performance in predicting therapeutic responses [43]. Connectivity mapping using platforms like CTRP/PRISM has nominated specific compounds (dabrafenib, irinotecan) for high-risk glioma subtypes defined by multi-omics signatures [47].
The clinical implementation of multi-omics approaches requires infrastructure for genomic data integration within electronic health records. Initiatives like Columbia Precision Medicine Initiative's Clinical Genomics Officer position and the Genomic & Bioinformatics Analysis Resource (GenBAR) represent institutional efforts to bridge computational discovery and clinical application [48]. These platforms facilitate the translation of multi-omics signatures into routine patient care through standardized ordering systems, results dissemination, and data aggregation for ongoing research.
Multi-omics integration represents a paradigm shift in disease subtyping, moving beyond reductionist single-omics approaches toward network-based disease understanding that captures biological complexity. Through methods like EMitool, MOVICS, and COPS, researchers can identify molecularly distinct subtypes with significant prognostic and therapeutic implications, advancing the core mission of personalized medicine to match the right patient with the right treatment at the right time [44] [43] [45].
The future of multi-omics integration lies in enhanced explainability, clinical translation, and temporal dynamics. As these methodologies mature, they will increasingly incorporate single-cell resolution, spatial context, and longitudinal profiling to capture disease evolution and therapeutic resistance mechanisms [47]. By firmly embedding multi-omics integration within systems biology frameworks, researchers can accelerate the development of personalized therapeutic strategies that reflect the true complexity of human disease.
Systems biology, with its holistic focus on the complex interactions within biological systems, is fundamentally reshaping the landscape of personalized medicine. By integrating high-throughput 'omics' technologies—genomics, transcriptomics, proteomics, metabolomics—with advanced computational modeling, systems biology moves beyond the analysis of individual molecules to study the emergent behaviors of biological networks [49] [13]. This approach is particularly powerful in addressing the core challenges of precision oncology and rare genetic diseases, where patient-specific molecular profiling is essential but insufficient on its own. In precision oncology, the goal is to match treatments to the unique molecular alterations found in an individual's tumor, yet the relationship between cancer genotypes and phenotypes is notoriously nonlinear and dynamic [49]. Similarly, for the vast majority of the over 7,000 known rare diseases, which are often driven by monogenic mutations, understanding the network-wide consequences of a single defective protein is critical for developing effective therapies [50] [51]. This whitepaper presents advanced case studies and methodologies that demonstrate how systems biology provides the necessary framework to translate complex molecular data into actionable, personalized therapeutic strategies for these challenging medical conditions.
Case Study 1: Precision Oncology – Overcoming Drug Resistance in NSCLC
Clinical Challenge and Systems Biology Approach
A central challenge in precision oncology is overcoming intrinsic and acquired drug resistance in cancers such as Non-Small Cell Lung Cancer (NSCLC). Resistance to targeted therapies like EGFR inhibitors can arise through multiple mechanisms, including secondary mutations in the target itself (e.g., EGFR T790M), activation of bypass signaling pathways (e.g., amplification of MET or HER2), or feedback network adaptations within the MAPK pathway [49]. A reductionist approach, focusing on single biomarkers, often fails to dissect this complexity. Systems biology addresses this by constructing dynamic network models of intracellular signaling pathways. These models quantitatively simulate how tumor signaling networks process environmental signals and respond to perturbations, such as targeted drug treatments [49]. This allows researchers to move from a static view of mutations to a dynamic understanding of network state and control, enabling the prediction of which drug combinations will most effectively block a tumor's escape routes and induce cell death.
Application of Single-Sample Network Inference
A key technical advancement in this domain is the development of single-sample network inference methods. Unlike traditional methods that infer an aggregate network from a large cohort of samples, these techniques reconstruct a biological network for an individual patient. This is critical for true personalization in a clinical context.
A 2024 study evaluated six such methods—SSN, LIONESS, SWEET, iENA, CSN, and SSPGI—using transcriptomic data from lung and brain cancer cell lines from the Cancer Cell Line Encyclopedia (CCLE) [52]. The performance of these methods in distinguishing NSCLC from SCLC subtypes was quantitatively compared, with key findings summarized in the table below.
Table 1: Performance Comparison of Single-Sample Network Inference Methods in Lung Cancer (NSCLC vs. SCLC)
| Method | Underlying Principle | Subtype-Specific Hubs | Correlation with Other Omics Data | Notes |
|---|---|---|---|---|
| SSN | Differential PCC network with STRING background | High | High | Identified most subtype-specific hubs; showed strong correlation with cell-line specific proteomics/CNV. |
| LIONESS | Linear interpolation on aggregate networks | High | High | Flexible (any aggregate method); strong performance similar to SSN. |
| SWEET | Linear interpolation with sample correlation weighting | Moderate | High | Mitigated potential network size bias between subtypes. |
| iENA | Altered PCC for node/edge-networks | Moderate | Moderate | --- |
| CSN | Stable statistical gene associations | Low | Low | Produces a binary network output. |
| SSPGI | Individual edge-perturbations | Low | Low | --- |
The study concluded that SSN, LIONESS, and SWEET networks correlated better with other omics data (e.g., proteomics, copy number variation) from the same cell line than aggregate networks, confirming they capture sample-specific biology [52]. Furthermore, hub genes in these networks were enriched for known subtype-specific driver genes, validating their biological relevance.
Experimental Protocol for Single-Sample Network Analysis
Protocol Title: Constructing Single-Sample Co-expression Networks from Bulk RNA-seq Data for Tumor Subtyping.
1. Sample Preparation & RNA Sequencing:
- Obtain tumor tissue samples, ensuring standardized processing and storage.
- Extract total RNA and assess quality (e.g., RIN > 7).
- Perform bulk RNA-sequencing on an approved platform (e.g., Illumina) to a sufficient depth (e.g., 30 million paired-end reads). Include a cohort of reference samples representing relevant tumor subtypes.
2. Computational Data Preprocessing:
- Quality Control: Use FastQC to assess sequence quality. Trim adapters and low-quality bases with Trimmomatic.
- Alignment: Align reads to a reference genome (e.g., GRCh38) using a splice-aware aligner like STAR.
- Quantification: Generate gene-level read counts using featureCounts.
3. Single-Sample Network Inference:
- Normalize the count matrix (e.g., using TPM or variance-stabilizing transformation).
- Choose a single-sample network inference method (e.g., SSN, LIONESS). For LIONESS:
- Construct an aggregate co-expression network (e.g., using Pearson Correlation) from all samples.
- Recompute the aggregate network iteratively, each time leaving one sample out.
- Apply the LIONESS equation to estimate the single-sample network for each left-out sample [52].
- Prune the resulting networks using a protein-protein interaction background network (e.g., STRING) to focus on biologically plausible interactions.
4. Downstream Analysis & Validation:
- Calculate node strength (sum of connection weights) for each gene in each single-sample network.
- Perform clustering (e.g., hierarchical clustering) on the node strength matrix to see if samples group by known subtype.
- Identify hub genes (genes with the highest node strength) in subtype-specific networks.
- Validate hubs by enrichment for known drivers from databases like IntOGen/COSMIC.
- Correlate node strength or edge weights with other omics data from the same samples (e.g., proteomics) to confirm biological relevance [52].
Figure 1: Workflow for Single-Sample Network Analysis in Precision Oncology
Case Study 2: Rare Diseases – Menkes Disease and Spinal Muscular Atrophy
Rare Diseases as a Window into Fundamental Biology
Rare genetic diseases, while individually uncommon, collectively affect an estimated 260-450 million people worldwide and represent a vast landscape for discovering fundamental biological mechanisms [51]. The study of these "nature's experiments" has historically provided profound insights, exemplified by Nobel Prize-winning work on cell cycle (cdc genes), secretion (sec genes), and circadian rhythms (period gene), which originated from rare mutations in model organisms [51]. A systems biology approach is particularly suited to rare diseases because it can model the network-wide perturbations caused by a single defective gene, moving from the defective protein to its interactome and resulting pathophysiology.
Menkes Disease: A Systems View of Copper Metabolism
Menkes disease is a rare X-linked recessive disorder caused by mutations in the ATP7A gene, which encodes a copper-transporting P-type ATPase. A systems biology approach moves beyond the single gene to model the interactome of the ATP7A protein. This involves identifying its direct and indirect molecular interactions, which include copper transporters (e.g., CTR1), chaperones (e.g., ATOX1), and downstream copper-dependent enzymes such as lysyl oxidase, cytochrome c oxidase, and superoxide dismutase [51]. By constructing a dynamic model of this network, researchers can simulate how disrupted copper transport leads to systemic deficiencies in these enzymes, causing the observed pathophysiology: connective tissue defects, neurological degeneration, and hypopigmentation. This network view also illuminates the connection between Menkes disease and common neurodegenerative disorders like Parkinson's disease, where copper metabolism is also implicated, demonstrating how rare disease research can inform our understanding of prevalent conditions [51].
Risdiplam for Spinal Muscular Atrophy: Mechanism and Workflow
Spinal Muscular Atrophy (SMA) is a rare neuromuscular disease caused by loss-of-function mutations in the SMN1 gene, leading to insufficient levels of survival motor neuron (SMN) protein. The small molecule Risdiplam was developed to treat SMA by modifying the splicing of the paralogous SMN2 gene, thereby increasing production of functional SMN protein [50]. This exemplifies a systems pharmacology approach that targets a specific network node to restore a critical biological function.
Figure 2: Therapeutic Splicing Modification in Spinal Muscular Atrophy
Experimental Protocol for iPSC-Based Rare Disease Modeling
Protocol Title: Utilizing Induced Pluripotent Stem Cells (iPSCs) for Rare Disease Modeling and Drug Screening.
1. iPSC Generation and Differentiation:
- Biopsy: Obtain patient somatic cells (e.g., skin fibroblasts) via biopsy.
- Reprogramming: Reprogram patient cells into induced pluripotent stem cells (iPSCs) using non-integrating methods (e.g., Sendai virus or episomal vectors expressing Oct4, Sox2, Klf4, c-Myc) [50].
- CRISPR-Corrected Control: Generate an isogenic control line by using CRISPR/Cas9 technology to correct the disease-causing mutation in the patient iPSC line.
- Directed Differentiation: Differentiate both patient and corrected iPSCs into the relevant disease-affected cell type (e.g., motor neurons for SMA) using established, standardized protocols [50].
2. Phenotypic and Molecular Characterization:
- Transcriptomics: Perform RNA-sequencing on differentiated cells from both patient and corrected lines to identify differentially expressed genes and pathways.
- Proteomics/Metabolomics: Analyze protein and metabolite profiles to characterize the downstream consequences of the mutation.
- Functional Assays: Perform cell-type specific functional assays (e.g., electrophysiology for neurons, contractility for muscle cells).
3. Drug Testing and Validation:
- Compound Screening: Treat patient-derived cells with the candidate therapeutic compound (e.g., Risdiplam) across a range of doses.
- Efficacy Assessment: Measure the rescue of molecular and phenotypic endpoints. For SMA, this would include quantifying the increase in full-length SMN2 transcript and SMN protein, and assessing motor neuron survival and function.
- Animal Model Correlation: Test the compound in a parallel rare disease animal model (e.g., SMNΔ7 mouse model for SMA) to validate in vivo efficacy and translational potential [50].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Key Research Reagent Solutions for Systems Biology Studies
| Tool / Reagent | Function / Application | Example Use Case |
|---|---|---|
| CRISPR/Cas9 Systems | Gene editing for creating isogenic control lines and disease models in vitro and in vivo. | Correcting the ATP7A mutation in a Menkes disease iPSC line to create a controlled experimental system [50]. |
| Induced Pluripotent Stem Cells (iPSCs) | Patient-derived pluripotent cells that can be differentiated into any cell type for disease modeling. | Generating motor neurons from an SMA patient to study disease mechanisms and screen drugs like Risdiplam [50]. |
| CCLE Database | A publicly available database of omics data from a large panel of human cancer cell lines. | Providing transcriptomic, proteomic, and CNV data for evaluating single-sample network methods on lung and brain cancers [52]. |
| STRING Database | A knowledgebase of known and predicted protein-protein interactions. | Used as a background network to prune and validate inferred co-expression networks in SSN and other methods [52]. |
| q-bio Modeling Software & Python Notebooks | Computational tools for building deterministic and stochastic mechanistic models of biological processes. | Simulating the dynamics of signaling networks to predict drug response in cancer or the effect of a mutation in a metabolic pathway [53]. |
| MSK-IMPACT (MSKCC) | A targeted sequencing panel for identifying somatic and germline mutations in cancer patients. | Used in clinical workflows at Memorial Sloan Kettering to match patients to targeted therapies or clinical trials based on their tumor's molecular profile [54]. |
| Hsd17B13-IN-77 | Hsd17B13-IN-77, MF:C27H30F2N2O5S2, MW:564.7 g/mol | Chemical Reagent |
| Lacidipine-13C4 | Lacidipine-13C4 Stable Isotope | Lacidipine-13C4 is an isotopically labeled internal standard for LC-MS/MS analysis of lacidipine in pharmacokinetic and metabolism research. For Research Use Only. Not for human or diagnostic use. |
The case studies and methodologies detailed in this whitepaper underscore the transformative role of systems biology in advancing personalized medicine for both cancer and rare diseases. By embracing a holistic, network-oriented perspective, researchers can move from a static list of molecular alterations to a dynamic, predictive understanding of disease pathogenesis and therapeutic response. The development of sophisticated tools like single-sample network inference allows for the creation of patient-specific network models, bringing us closer to the goal of true n-of-1 medicine. Similarly, the integration of iPSC technology and mechanistic modeling provides a powerful platform for deconstructing rare diseases and identifying novel treatment strategies. As these technologies continue to mature and standardization improves [55], the integration of systems biology into clinical research and practice will be paramount for delivering on the promise of personalized healthcare.
The advancement of personalized medicine hinges on the ability to understand and monitor disease at unprecedented resolution. The convergence of liquid biopsy techniques with single-cell analysis technologies, underpinned by the holistic framework of systems biology, is creating a paradigm shift in real-time disease monitoring. Liquid biopsy provides a minimally invasive window into disease dynamics by analyzing tumor-derived components from bodily fluids, bypassing the limitations of traditional tissue biopsies [56]. When combined with single-cell technologies that resolve cellular heterogeneity, these approaches generate rich, multi-dimensional data essential for a systems-level understanding of patient-specific disease mechanisms [57]. This integration is foundational to developing truly personalized diagnostic and therapeutic strategies.
Liquid Biopsy: A Minimally Invasive Window into Disease Dynamics
Core Components and Analytical Targets
Liquid biopsy involves the isolation and analysis of various tumor-derived components from bodily fluids, most commonly blood. These components provide complementary information about the tumor's molecular landscape [56].
- Circulating Tumor Cells (CTCs): Intact viable cells shed from primary and metastatic tumors into the circulation. They offer insights into cellular heterogeneity, phenotype (e.g., epithelial-to-mesenchymal transition), and functional potential for metastasis [58].
- Circulating Tumor DNA (ctDNA): Short fragments of cell-free DNA released from apoptotic or necrotic tumor cells. ctDNA analysis can reveal tumor-specific genetic alterations, including mutations and copy number alterations [56].
- Tumor Extracellular Vesicles (EVs): Membrane-bound particles secreted by cells that carry proteins, nucleic acids, and lipids. They play a role in intercellular communication and preparing metastatic niches [56].
- Other Biomarkers: Additional components include circulating cell-free RNA (cfRNA), including microRNAs, and tumor-educated platelets (TEPs) [56].
The table below summarizes the key analytical targets in liquid biopsy.
Table 1: Core Components Analyzed in Liquid Biopsy
| Component | Description | Primary Analysis Methods | Key Information Obtained |
|---|---|---|---|
| Circulating Tumor Cells (CTCs) | Intact cells from primary or metastatic tumors | Enrichment-free imaging, immunofluorescence, scRNA-seq [58] [59] | Tumor heterogeneity, phenotypic plasticity, metastatic potential |
| Circulating Tumor DNA (ctDNA) | Cell-free DNA fragments from tumor cells | Next-generation sequencing (NGS), PCR-based methods [56] | Somatic mutations, copy number alterations, epigenetic markers |
| Tumor Extracellular Vesicles (EVs) | Membrane-bound vesicles (exosomes, microvesicles) | Ultracentrifugation, nanomembrane ultrafiltration [56] | Proteins, miRNAs, mRNAs, lipid profiles |
Key Methodological Approaches
Liquid biopsy methodologies can be broadly divided into enrichment-based and enrichment-free platforms.
- Enrichment-Based Platforms: These techniques use biophysical properties (e.g., size, density) or biological markers (e.g., surface antigens) to isolate specific cell populations, such as CTCs, from peripheral blood. While effective for enriching rare cells, this targeted approach may miss heterogeneous or phenotypically unusual cell populations [58].
- Enrichment-Free Platforms: These approaches profile all nucleated cells from a blood sample after plating them on slides. Cells are typically stained with immunofluorescent (IF) markers and analyzed via whole slide imaging (WSI). This method offers a comprehensive, unbiased profile of circulating cell heterogeneity, including rare tumor-associated cells and immune cell subpopulations [58].
Single-Cell Analysis: Deconvoluting Cellular Heterogeneity
Single-Cell RNA Sequencing (scRNA-seq)
Single-cell RNA sequencing has revolutionized the study of complex tissues and rare cell populations by allowing transcriptome profiling at the individual cell level.
Workflow Overview: The general workflow for scRNA-seq involves: (1) sample preparation and single-cell suspension; (2) single-cell capture (e.g., using droplet-based microfluidics or plate-based FACS); (3) cell lysis and reverse transcription with cell-specific barcoding; (4) cDNA amplification and library construction; and (5) high-throughput sequencing [57]. A critical advantage in clinical contexts is the compatibility with single-nuclei RNA sequencing (snRNA-seq), which allows the use of snap-frozen archived specimens [57].
Data Analysis Pipeline: Analysis of scRNA-seq data requires specialized bioinformatics tools and pipelines [57]:
- Quality Control (QC): Filtering out low-quality cells based on metrics like library size, number of detected genes, and mitochondrial gene percentage.
- Dimensionality Reduction: Using techniques such as Principal Component Analysis (PCA), t-distributed Stochastic Neighbor Embedding (t-SNE), or Uniform Manifold Approximation and Projection (UMAP) to visualize cell clusters.
- Cell Type Identification & Clustering: Identifying distinct cell populations based on transcriptome profiles.
- Trajectory Inference: Reconstructing cellular developmental pathways or transition states using algorithms that identify intermediate cellular states.
Table 2: Key Single-Cell Sequencing Technologies and Applications
| Technology | Key Feature | Primary Application |
|---|---|---|
| 10x Genomics Chromium | High-throughput droplet-based system | Profiling thousands of cells simultaneously for population analysis [57] |
| Single-Cell Combinatorial Indexed Sequencing (SCI-seq) | Low-cost library construction | Detecting somatic copy number variations (CNVs) across many cells [57] |
| scCOOL-seq | Multi-omics at single-cell level | Simultaneous analysis of chromatin state, CNV, ploidy, and DNA methylation [57] |
| Topographic Single-Cell Sequencing (TSCS) | Spatial information retention | Investigating spatial relationships and tumor cell invasion [57] |
| TSCS | Precise spatial positioning | Analyzing tumor cell invasion and metastasis with spatial context [57] |
| Microwell-seq | High-throughput, low-cost | Large-scale cell atlas construction [57] |
Single-Cell MicroRNA Sequencing
MicroRNAs (miRNAs) are key post-transcriptional regulators, and their profiling at the single-cell level provides insights into regulatory states. However, single-cell miRNA sequencing presents distinct technical challenges due to the small size of miRNAs and adapter dimer formation. A systematic comparison of 19 protocol variants identified key parameters for optimal performance: specific adapter designs (e.g., SB, SB4N, SBNCL) demonstrated high reproducibility and detection rates, with the best protocols detecting a median of 68 miRNAs per single circulating tumor cell (CTC) from lung cancer patients [59].
The Integration of Systems Biology
Systems biology provides the computational and conceptual framework to integrate multi-scale data from liquid biopsies and single-cell analyses. It moves beyond descriptive biology to model the dynamic interactions within biological systems [41].
Computational and AI-Driven Integration
Multi-Omics Data Integration: Combining datasets from genomics, transcriptomics, proteomics, and metabolomics provides a holistic view of the biological state. For example, metagenomic sequencing of the gut microbiome can be linked to host immune responses and metabolic pathways, revealing systemic influences on disease [60].
Artificial Intelligence and Machine Learning: AI/ML algorithms are critical for analyzing high-dimensional data generated by single-cell technologies. Applications include:
- Cell State Classification: Supervised learning to identify and classify cell phenotypes from imaging or transcriptomic data [58].
- Biomarker Discovery: Identifying predictive signatures of disease progression or treatment response from complex datasets [41].
- Deep Learning for Image Analysis: Using self-supervised contrastive learning frameworks to extract robust features from single-cell images, enabling accurate identification and stratification of rare circulating cells without the need for extensive manual labeling [58].
Mechanistic Modeling: Quantitative models simulate the dynamics of biological systems, such as signaling pathways or immune cell interactions. These in silico models can generate testable hypotheses about therapeutic interventions and predict patient-specific responses [41].
Experimental Protocols and Workflows
Detailed Protocol: Enrichment-Free Liquid Biopsy with Deep Learning Analysis
This protocol details the process for identifying and characterizing rare circulating cells from whole blood, incorporating a deep learning-based feature extraction approach for high accuracy and scalability [58].
1. Sample Preparation and Staining:
- Sample Collection: Collect peripheral blood into EDTA or CellSave tubes.
- Nucleated Cell Preparation: Use red blood cell lysis to obtain a nucleated cell fraction.
- Slide Plating: Plate cells as a monolayer on glass slides.
- Immunofluorescence Staining: Stain cells with a panel of antibodies to define cell phenotypes. A typical panel includes [58]:
- DAPI: Nuclear stain (DNA).
- Cytokeratins (CK): Markers for epithelial cells (CTCs).
- Vimentin (VIM): Marker for mesenchymal cells and endothelial cells.
- CD45: Pan-leukocyte marker (white blood cells).
- CD31: Marker for endothelial cells.
2. Whole Slide Imaging (WSI) and Cell Segmentation:
- Image Acquisition: Scan the entire slide using a high-throughput fluorescence microscope.
- Cell Segmentation: Identify and segment all individual nucleated cells. A trained U-Net architecture (e.g., a customized Cellpose model) is used for accurate segmentation, achieving high F1-scores across Intersection-over-Union (IoU) thresholds [58].
3. Feature Extraction via Contrastive Learning:
- Dataset Curation: Create a balanced training dataset by combining sampled rare cells and white blood cells (WBCs) from patient samples. WBCs can be controllably depleted using a pre-trained binary classifier.
- Model Training: Train a self-supervised contrastive learning model on the curated single-cell images. This model learns to project images into a feature space where similar phenotypes are clustered together, without relying on manually engineered features [58].
- Feature Output: The model generates a high-dimensional feature vector for each segmented cell.
4. Downstream Analytical Tasks:
- Classification: A logistic regression classifier can be trained on the learned features to identify known cell phenotypes (e.g., epithelial CTCs, immune-like CTCs, circulating endothelial cells), achieving accuracies over 92% [58].
- Outlier Detection: Algorithms like Isolation Forest are applied in the learned feature space to flag cells with unusual phenotypes for novel cell discovery.
- Clustering: Unsupervised clustering (e.g., using UMAP and HDBSCAN) characterizes unknown cell phenotypes based on their feature representations.
Detailed Protocol: Single-Cell miRNA Sequencing for CTCs
This protocol is optimized for sequencing miRNAs from low-input samples, such as single cells or rare CTCs, based on the performance comparison of multiple methods [59].
1. Protocol Selection:
- Based on comparative studies, ligation-based protocols such as SB and SB_4N are recommended due to their high reproducibility, low adapter dimer formation, and high number of detected miRNAs [59].
2. Library Preparation:
- Cell Lysis: Single cells are lysed in a buffer containing detergents.
- Adapter Ligation:
- 3' Adapter Ligation: A pre-adenylated 3' adapter is ligated to the miRNA using a truncated T4 RNA ligase 2.
- Reverse Transcription: The ligation product is reverse transcribed.
- 5' Adapter Ligation: A 5' adapter is ligated to the cDNA/miRNA hybrid using T4 RNA ligase 1.
- cDNA Amplification: The product is amplified via PCR with primers containing unique molecular identifiers (UMIs) and sequencing adapters.
- Library Purification: Use solid-phase reversible immobilization (SPRI) beads to purify the final library and remove adapter dimers.
3. Quality Control and Sequencing:
- QC: Assess library quality and concentration using a Bioanalyzer or TapeStation and qPCR.
- Sequencing: Pool libraries in equimolar amounts and sequence on a high-throughput platform (e.g., Illumina) to a depth of ~1-2 million reads per cell.
4. Data Analysis:
- Preprocessing: Remove reads shorter than 18 nt and low-quality reads.
- Adapter Trimming: Trim adapter sequences from the reads.
- Alignment: Map reads to the human genome and miRBase.
- Quantification: Count reads aligned to miRNA loci, using UMIs to correct for PCR duplicates.
Table 3: Performance Metrics of Selected Single-Cell miRNA-seq Protocols
| Protocol Name | Adapter Type | Average miRXplore miRNAs Detected (per cell) | Reproducibility (Euclidean Distance) | Key Advantage |
|---|---|---|---|---|
| SB | Standard Ligation | >900 | Highest (Lowest Distance) | High reproducibility and accuracy [59] |
| SB_4N | Ligation with 4N Adapters | >900 | High | Combines high detection with reproducibility [59] |
| SBN_CL | Ligation with Adapter Exchange | >900 | High | Robust performance with mixed adapters [59] |
| 4N | Ligation with 4N Adapters | >900 | Lower | High detection but lower reproducibility [59] |
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Essential Research Reagent Solutions for Single-Cell Liquid Biopsy
| Reagent/Material | Function | Example Application |
|---|---|---|
| CellSave Tubes | Preserves blood samples for CTC analysis | Stabilizes CTCs in whole blood for up to 96 hours post-draw [58] |
| Anti-Cytokeratin Antibodies | Immunofluorescent labeling of epithelial CTCs | Identifying canonical epithelial CTCs in enrichment-free assays [58] |
| Anti-CD45 Antibodies | Immunofluorescent labeling of leukocytes | Distinguishing WBCs from tumor-derived cells (CD45-negative) [58] |
| DAPI (4',6-diamidino-2-phenylindole) | Fluorescent nuclear stain | Identifying and segmenting all nucleated cells [58] |
| miRNA-Seq Library Kits (e.g., SB protocol) | Preparation of sequencing libraries from low-input RNA | Profiling miRNA expression from single CTCs [59] |
| Unique Molecular Identifiers (UMIs) | Barcoding individual RNA molecules | Correcting for PCR amplification bias in sequencing data [59] |
| 10x Genomics Chromium Single Cell 5' Kit | Barcoding single cells for RNA-seq | Profiling the transcriptome of thousands of single cells simultaneously [57] |
| Neuraminidase-IN-18 | Neuraminidase-IN-18|High-Purity Inhibitor | Neuraminidase-IN-18 is a potent research compound targeting viral neuraminidase. This product is for Research Use Only (RUO) and not for human or veterinary diagnosis or therapeutic use. |
| KRAS G12D inhibitor 20 | KRAS G12D inhibitor 20, MF:C18H26N6O, MW:342.4 g/mol | Chemical Reagent |
The synergy between single-cell analysis, liquid biopsies, and systems biology is forging a new path in personalized medicine. These technologies provide an unprecedented, dynamic view of disease biology, enabling real-time monitoring of treatment response, detection of minimal residual disease, and discovery of novel biomarkers. The continued development of robust experimental protocols and powerful computational frameworks for data integration is essential to translate this wealth of information into improved clinical outcomes and truly personalized therapeutic strategies.
Navigating the Hurdles: Technical and Translational Challenges in Systems-Driven Personalization
Systems biology, by investigating the intricate interactions between biological components across multiple scales, provides the essential theoretical foundation for modern personalized medicine. It posits that complex diseases emerge from dysregulated networks rather than isolated molecular defects. This paradigm shift demands a research approach that integrates diverse, high-dimensional data—spanning genomics, transcriptomics, proteomics, metabolomics, and electronic health records (EHRs)—to construct comprehensive models of health and disease [8]. The grand challenge for fields like Integrative and Regenerative Pharmacology (IRP) is to unify pharmacology, systems biology, and regenerative medicine to develop transformative curative therapeutics that restore physiological structure and function, moving beyond mere symptomatic relief [8].
However, the journey from isolated data to integrated insight is fraught with technical obstacles. The promise of multi-omics integration is a comprehensive, holistic view of a patient’s biological status, enabling unprecedented precision in diagnosis, prognosis, and treatment selection [61]. Realizing this promise requires overcoming significant data management hurdles related to both data integration and data security. This technical guide examines these core challenges, details contemporary methodologies for addressing them, and explores their pivotal role in advancing personalized medicine research.
Core Data Integration Challenges
The integration of multi-omics data with clinical EHR information presents a set of complex, interconnected technical challenges that stem from the fundamental nature of the data itself.
Data Heterogeneity and Scale
The various data types involved in systems biology research possess distinct characteristics, formats, and scales, creating a profound heterogeneity problem.
- Diversity of Data Types: Each biological layer provides a different perspective. Genomics (DNA) offers a static blueprint of genetic variation. Transcriptomics (RNA) reveals dynamically changing gene expression levels. Proteomics (proteins) captures the functional effectors of cellular processes, while metabolomics (metabolites) provides a snapshot of ongoing physiological activity [61]. EHR data adds another layer of complexity, containing both structured information (e.g., lab values, ICD codes) and unstructured data (e.g., physician notes) that require natural language processing (NLP) to extract meaningful insights [61].
- The High-Dimensionality Problem: Multi-omics studies typically generate far more features (e.g., >20,000 genes, >500,000 CpG sites, thousands of proteins) than patient samples, a phenomenon known as the "curse of dimensionality" [16]. This creates statistical challenges, increases the risk of identifying spurious correlations, and overwhelms conventional biostatistical methods [16].
Technical and Analytical Hurdles
Beyond heterogeneity, researchers face significant technical barriers in data processing and analysis.
- Data Normalization and Harmonization: Data generated from different platforms, laboratories, and technologies contain technical variations (batch effects) that can obscure true biological signals. Robust normalization techniques (e.g., TPM/FPKM for RNA-seq, intensity normalization for proteomics) and harmonization methods like ComBat are essential prerequisites for integration [61] [16].
- Missing Data: It is common for patient datasets to be incomplete, with some omics layers missing entirely or specific measurements absent. Handling this requires sophisticated imputation methods such as k-nearest neighbors (k-NN) or matrix factorization to estimate missing values without introducing bias [61] [16].
- Computational Infrastructure: The scale of data is staggering; single whole genomes can generate hundreds of gigabytes, and cohort-level multi-omics studies can reach petabyte scales [61] [16]. This demands scalable cloud-based solutions and distributed computing architectures [48] [61].
Table 1: Key Challenges in Multi-Omics and EHR Data Integration
| Challenge Category | Specific Issues | Impact on Research |
|---|---|---|
| Data Heterogeneity | Different formats, scales, and biological contexts across omics layers and EHRs [61] [23] | Obscures unified biological interpretation; requires specialized computational methods |
| Volume and Velocity | Petabyte-scale data streams from NGS, mass spectrometry, and digital pathology [16] | Overwhelms traditional computing infrastructure; demands cloud/distributed solutions |
| Data Veracity | Technical noise, batch effects, and biological confounding factors [16] | Risks false discoveries; necessitates rigorous quality control and normalization |
| Missing Data | Incomplete omics profiles or clinical measurements across patient cohorts [61] | Reduces statistical power and can bias analysis if not handled properly |
Methodologies for Data Integration
To overcome these challenges, the field has developed advanced computational methodologies centered on artificial intelligence (AI) and machine learning (ML).
AI-Powered Integration Strategies
AI acts as a powerful engine for pattern recognition, detecting subtle connections across millions of data points that are invisible to conventional analysis [61]. The choice of integration strategy depends on the research question and data characteristics.
- Early Integration (Feature-Level): This approach merges all raw features from different omics layers into a single, massive dataset before analysis. While it can capture complex, unforeseen interactions between modalities, it is computationally intensive and highly susceptible to the curse of dimensionality [61].
- Intermediate Integration: Here, each omics dataset is first transformed into a more manageable representation, which are then combined. Network-based methods are a prime example, where each omics layer is used to construct biological networks (e.g., gene co-expression, protein-protein interactions) that are subsequently integrated to reveal functional modules driving disease [17] [61].
- Late Integration (Model-Level): This strategy involves building separate predictive models for each data type and then combining their predictions using ensemble methods (e.g., weighted averaging, stacking). It is computationally efficient and robust to missing data, though it may miss subtle cross-omics interactions [61].
State-of-the-Art Machine Learning Techniques
Several sophisticated ML techniques have proven particularly effective for multi-omics integration:
- Autoencoders (AEs) and Variational Autoencoders (VAEs): These unsupervised neural networks compress high-dimensional omics data into a dense, lower-dimensional "latent space." This compression makes integration computationally feasible while preserving key biological patterns, providing a unified representation for combined analysis [61].
- Graph Convolutional Networks (GCNs): GCNs are designed for network-structured data. They model biological systems as graphs (e.g., with genes/proteins as nodes and their interactions as edges), learning from this structure to make predictions about disease progression or drug response [61] [16].
- Multi-Modal Transformers: Leveraging self-attention mechanisms, transformers can weigh the importance of different features and data types, learning which modalities are most critical for specific predictions. This allows them to identify key biomarkers from a sea of noisy data [61] [16].
- Similarity Network Fusion (SNF): This technique creates a patient-similarity network for each omics type and then fuses them into a single, comprehensive network. The process strengthens consistent similarities and removes noise, enabling more accurate disease subtyping [61].
The following diagram illustrates a generalized workflow for integrating multi-omics data with EHRs to generate clinical insights, incorporating the AI methodologies described above.
The Critical Imperative of Data Security
While integrating diverse datasets unlocks scientific potential, the aggregation and storage of sensitive health and omics information creates a significant security burden that cannot be overlooked.
The Evolving Threat Landscape
The healthcare sector faces an increasingly severe cybersecurity crisis.
- Escalating Breach Statistics: As of October 2025, 364 hacking incidents had been reported to the U.S. Department of Health and Human Services, affecting over 33 million Americans [62]. The year 2024 set a grim record with 259 million Americans' protected health information (PHI) reported as hacked, a figure heavily influenced by the UnitedHealth Group/Change Healthcare ransomware attack [62].
- The "Single-Point-of-Failure" Risk: The EHR vendor market is highly consolidated, with Epic and Oracle Health dominating 71.7% of the national inpatient market [63]. This concentration means a successful attack on one of these major vendors could have catastrophic, nationwide implications for patient care, data privacy, and healthcare operations [63].
- Third-Party Vulnerabilities: Over 80% of stolen PHI is not taken from hospitals directly but from third-party vendors, software services, and business associates [62]. Furthermore, 90% of hacked health records were stolen from outside the EHR system itself, often from unencrypted data stores or through stolen credentials that granted access to encrypted data [62].
Foundational Security Frameworks and Best Practices
To mitigate these risks, healthcare and research organizations should adhere to established cybersecurity frameworks and implement core defensive measures.
- Adherence to Security Frameworks: Three key frameworks provide guidance:
- HHS Cybersecurity Performance Goals (CPGs): Voluntary, high-impact practices designed to defend against the most common attack tactics [62].
- Healthcare Industry Cybersecurity Practices (HICP): Outlines top threats and provides best practice recommendations [62].
- NIST Cybersecurity Framework: Offers a taxonomy of high-level cybersecurity outcomes for managing risk [62].
- Core Technical Defenses:
- Multi-Factor Authentication (MFA): A critical layer of defense to prevent unauthorized access, even if passwords are compromised [64]. The lack of MFA was a significant contributor to the Change Healthcare breach [63].
- Advanced Data Encryption: Essential for protecting data both at rest and in transit, ensuring information is useless if stolen [64].
- Comprehensive Monitoring and AI Analytics: AI-powered tools can identify unusual behavior and potential threats in real-time, enabling faster response [64].
- Software Bill of Materials (SBOM): An SBOM provides a formal record of software components and their supply chain relationships, which is critical for identifying and patching vulnerabilities [62].
Table 2: Key Cybersecurity Threats and Defensive Measures in Healthcare Data Management
| Threat Category | Representative Incidents/Statistics | Recommended Defensive Measures |
|---|---|---|
| Ransomware & Data Theft | 70% increase in ransomware attacks over two years; "double-layered extortion" common in 2024-25 [62] [64] | Modern ransomware detection tools, regular secure backups, robust incident response plans [64] |
| Third-Party & Vendor Risk | 80% of stolen PHI taken from third-party vendors [62]; Oracle Health breach (2025) affected 6M patients [63] | Strategic third-party risk management programs, strong contractual security provisions, SBOM monitoring [62] [63] |
| Insider Threats & Human Error | Human error (e.g., phishing) remains a leading cause of breaches [64] | Role-based access controls, activity monitoring, comprehensive and regular employee training [64] |
| Legacy System Vulnerabilities | Many organizations rely on outdated software with inadequate security [64] | Regular risk assessments, patch management programs, system modernization where feasible |
The following diagram outlines a multi-layered security architecture necessary to protect integrated multi-omics and EHR data environments, incorporating the frameworks and defenses listed above.
Experimental Protocols and Research Applications
Detailed Methodologies: From Columbia's Genomic Infrastructure
Real-world implementations provide a blueprint for successful data integration. The Columbia Precision Medicine Initiative (CPMI) offers a detailed case study in building the infrastructure to support precision medicine.
- Objective: To create a cohesive program for implementing genomic medicine and produce infrastructure to support genetic bioinformatic research in anticipation of routine genetic sequencing of patients [48].
- Genomic Data Migration and Harmonization: CPMI assumed oversight of the Genomic & Bioinformatics Analysis Resource (GenBAR), migrating petabytes of genomic data from an on-premises data center to Amazon Web Services (AWS) cloud computing [48]. The bioinformatic tool Analysis Tool for Annotated variants (ATAV) was also migrated to the cloud.
- Pipeline Development: Using AWS HealthOmics and WARP (WDL Analysis Research Pipelines) tools developed by the Broad Institute, the team designed harmonized exome and genome pipelines [48]. As of January 2025, over 1,800 archived whole exome sequencing datasets were reprocessed, aligned to an updated reference sequence (GRCh38), and aggregated in a new joint called file [48].
- Clinical Integration Workflow: In oncology, the group worked with Columbia Pathology to utilize the Columbia Combined Cancer Panel (CCCP), an NGS panel querying 586 genes. They collaborated with NYP partners to facilitate the electronic ordering of genetic tests through EPIC EHR, disseminate results within the medical record, and store clinical genetic data in a way that enables future integration with research platforms [48].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Multi-Omics and EHR Integration
| Tool/Category | Specific Examples | Function in Research |
|---|---|---|
| Cloud Computing Platforms | Amazon Web Services (AWS), Google Cloud, Microsoft Azure | Provides scalable, on-demand computing resources and storage for petabyte-scale multi-omics data [48] [61] |
| Bioinformatic Pipelines | AWS HealthOmics, WARP (WDL Analysis Research Pipelines), Broad Institute's GATK | Standardized, portable workflows for processing and analyzing genomic and transcriptomic data [48] |
| Data Harmonization Tools | Harmony, ComBat | Algorithmic tools that remove technical batch effects and normalize data across different platforms and studies [61] [23] |
| AI/ML Frameworks | PyTorch, TensorFlow, Scikit-learn | Open-source libraries for building and training deep learning models (Autoencoders, GCNs, Transformers) for data integration [61] [16] |
| Federated Learning Systems | Lifebit, NVIDIA CLARA | Enables collaborative model training across institutions without sharing raw patient data, preserving privacy [61] [16] |
The integration of multi-omics data with EHRs represents both a formidable challenge and a tremendous opportunity for advancing personalized medicine. The technical hurdles of data heterogeneity, scale, and security are significant, but not insurmountable. As this guide has detailed, the convergence of AI-powered integration strategies—including network-based intermediate integration, deep learning models like GCNs and transformers, and robust computational pipelines—provides a clear path forward for synthesizing disparate biological data into unified insights.
Concurrently, the escalating cybersecurity threat landscape demands a proactive, layered defense strategy. This must include strict adherence to established frameworks like the HHS CPGs and NIST, widespread implementation of multi-factor authentication and encryption, and diligent third-party risk management. The Columbia Precision Medicine Initiative exemplifies how these technical and operational components can be unified into a functional, scalable infrastructure for modern research.
For systems biology to fully deliver on its promise of personalized medicine, the research community must continue to prioritize both the sophisticated integration of diverse data types and the rigorous protection of the sensitive information entrusted to it. By simultaneously advancing these twin pillars of data management, researchers and clinicians can translate the systems-level understanding of human biology into tangible improvements in patient care, drug development, and health outcomes.
The transition of promising preclinical research into successful clinical trials remains a formidable challenge in biomedical science, with a high rate of failure despite quality basic research. This "translation gap" represents a critical bottleneck in drug development and personalized medicine. Translational medicine, designed to advance the two-way process between basic research and clinical practice, has emerged as a vital discipline to address this challenge [65]. The field aims to eliminate barriers that block the discovery and application of new treatments by integrating multiple disciplines and understanding diverse outcomes.
A quantitative understanding of why translation fails is emerging. Research has identified structural reasons for this "Lost in Translation" phenomenon, including the Butterfly Effect (minute differences between preclinical models producing significantly different outcomes) and the Two Cultures problem (differences in how experiments are designed and analyzed in preclinical versus clinical settings) [66]. Most significantly, the Princess and the Pea problem describes how an initially significant effect size dissipates as research transitions through increasingly complex biological systems due to accumulating variability [66]. This progressive accumulation of noise often renders potentially valuable therapeutic effects undetectable by the time they reach clinical testing.
The Quantitative Basis of Translational Failure
The Accumulation of Variability in Translational Research
The Princess and the Pea problem is fundamentally about the propagation and amplification of variance across experimental systems. As research progresses from molecular studies to cellular systems, animal models, and eventually human trials, each level introduces its own source of variability [66]. The variance of the sum or difference of independent random variables equals the sum of their variances, meaning that variability increases additively with each sequential experimental system.
Monte Carlo simulations using nested sigmoidal dose-response transformations have quantified this effect, demonstrating how adding variability to dose-response parameters substantially increases sample size requirements compared to standard calculations [66]. The widening distribution of results through consecutive experimental levels is visually apparent in simulation data, demonstrating the gradual obscuring of biological signals beneath accumulating noise.
Impact on Study Power and Feasibility
The practical consequence of increasing variability is its dramatic effect on sample size requirements for maintaining statistical power. Simulation studies demonstrate that with each additional experimental level (from molecular to cellular to animal to human systems), the required sample size increases substantially to detect the same underlying biological effect [66].
Table 1: Impact of Variance Accumulation on Sample Size Requirements
| Experimental Level | Variance Level | Sample Size Requirement | Study Feasibility |
|---|---|---|---|
| Molecular studies | Low | Minimal (benchmark) | High |
| Cellular systems | Moderate | 2-3x increase | Moderate |
| Animal models | High | 5-10x increase | Challenging |
| Human trials | Very High | 10-20x+ increase | Potentially impossible |
In extreme cases, realistic degrees of variability in a series of experiments can render clinical trials practically impossible due to impossibly large sample size requirements to detect significant differences between groups [66]. This quantitative framework explains why many promising preclinical findings fail to demonstrate efficacy in human trials.
Systems Biology as an Integrative Framework
Spatial Biology and Tissue Context
Spatial biology has emerged as a transformative discipline in life sciences, enabling researchers to study how cells, molecules, and biological processes are organized and interact within their native tissue environments [67]. By combining spatial transcriptomics, proteomics, metabolomics, and high-plex multi-omics integration with advanced imaging, spatial biology provides unprecedented insights into disease mechanisms, cellular interactions, and tissue architecture [67]. These capabilities are fueling breakthroughs in oncology, neuroscience, immunology, and precision medicine.
The global spatial biology market, projected to reach $6.39 billion by 2035 with a compound annual growth rate of 13.1%, reflects the strategic importance of these technologies in bridging the translation gap [67]. The field is experiencing rapid growth, powered by major market drivers such as rising investments in spatial transcriptomics for precision medicine, the growing importance of functional protein profiling in drug development, and the expanding use of retrospective tissue analysis for biomarker research [67].
AI and Computational Integration
Artificial Intelligence (AI) and Machine Learning (ML) have advanced from speculation to working technologies that can make actual differences in patient care and drug development [68]. The integration of AI is particularly valuable for addressing the variability challenge in translational science through pattern recognition in complex datasets and predictive modeling.
AI applications in translational science now include:
- Predicting pharmacokinetics using machine learning models that achieve comparable accuracy to traditional PBPK modeling with less required data [68]
- Target discovery through computational pipelines that identify novel therapeutic targets like NAMPT in neuroendocrine prostate cancer [68]
- Biomarker identification through analysis of metabolomic data to pinpoint biomarkers associated with specific disease states or treatment responses [68]
- Predicting adverse events using explainable machine learning models that help clinicians anticipate and manage treatment side effects [68]
The integration of model-informed drug development with AI creates a synergistic approach to accelerating pharmaceutical innovation, particularly through hybrid models that improve efficiency and adaptability [68].
Diagram 1: Systems Biology Translation Framework. This workflow illustrates how systems biology integrates multi-omics data with AI to bridge the preclinical-clinical divide.
Practical Methodologies for Translation
Quantitative Variance Assessment
The Monte Carlo simulation approach for quantifying variance spread provides a methodological framework for predicting translational success [66]. The process involves:
Define Dose-Response Transformations: Model biological systems using sigmoidal dose-response functions (Hill equations) with parameters including EC50, slope, maximal response, and minimal response.
Simulate Experimental Levels: Create consecutive levels of dose-response transformations, where the output of one transformation serves as input for the next, simulating the progression from molecular to cellular to animal to human systems.
Introduce Parameter Variability: At each level, add realistic variability to dose-response parameters based on empirical observations from similar experimental systems.
Calculate Sample Size Requirements: For each level of complexity, determine the sample size needed to maintain statistical power (typically 80-90%) for detecting the original effect size.
Assess Translational Feasibility: Use the calculated sample size requirements to evaluate whether pursuing clinical translation is practically feasible given the accumulating variability.
Integrated Translational Study Design
Operationally, addressing the translation gap requires moving away from siloed handovers between discovery and clinical functions in favor of more integrated translational strategies [69]. This organizational shift recognizes that many late-stage failures can be traced to decisions made much earlier in the pipeline due to incomplete understanding of mechanism, weak translational models, or limited predictive data [69].
Effective integrated translational design includes:
- Embedding translational science directly into development workflows by bringing together discovery biologists, pharmacologists, toxicologists and clinical strategists into early collaborative teams
- Implementing stage-gate frameworks with scientific and regulatory reviews to support data-driven decision-making
- Co-locating drug substance and product manufacturing to remove barriers to technology transfer and enable tighter integration of API characterization and early formulation work
- Ensuring access to high-quality, well-characterized patient samples through collaborations with leading biobanks, particularly for rare tissues critical for translational research on rare diseases
Table 2: Key Research Reagent Solutions for Translational Research
| Reagent/Category | Function in Translation | Application Examples |
|---|---|---|
| Spatial Biology Platforms (GeoMx, CosMx) | Enable multi-omic mapping of tissue architecture | Oncology, neuroscience, immunology [67] |
| High-Characterization Patient Samples | Provide biological relevance for translational studies | Biomarker validation, target identification [69] |
| AI-Ready Multi-omic Datasets | Train predictive algorithms for clinical outcome | Patient stratification, drug response prediction [68] |
| Target Engagement Assays | Verify mechanism of action in complex systems | Lead optimization, pharmacodynamic modeling [69] |
| Molecular Signatures | Bridge preclinical and clinical findings | Biomarker development, patient selection [69] |
Emerging Technologies and Approaches
Advanced Computational Methods
Computational drug discovery pipelines are increasingly identifying novel therapeutic targets by integrating diverse data types. For example, the LANTERN framework leverages large language models and transformers for predicting drug-target, protein-protein, and drug-drug interactions at scale, offering a promising path to accelerating therapeutic discovery [70]. These AI breakthroughs in bioinformatics represent a significant advancement in our ability to untangle complex biological relationships.
Digital twin technology is also emerging as a valuable tool for translational research, creating in silico patient simulations that can help predict treatment responses and optimize trial designs before engaging human subjects [68]. Increasing acceptance of AI-generated digital twins through clinical trial applications represents a frontier in reducing translational uncertainty [68].
Operational Excellence in Translation
Beyond technological solutions, operational excellence plays a crucial role in bridging the translation gap. This includes:
- Adapting quality systems to support phase-appropriate governance that meets the needs of early-phase studies while supporting long-term development goals [69]
- Leveraging global capabilities in regions like India, which offers regulatory reforms, improved infrastructure, and a growing clinical research talent base for global trials [69]
- Implementing open science practices as outlined in the updated SPIRIT 2025 and CONSORT 2025 guidelines, which enhance transparency and reproducibility through improved protocol content and results reporting [71] [72]
Diagram 2: Variance Accumulation Across Systems. This diagram illustrates how variability accumulates while effect size remains constant across experimental systems, reducing detectability.
Bridging the translation gap requires a multifaceted approach that addresses both the quantitative challenges of variability accumulation and the operational challenges of integrated drug development. Systems biology contributes to personalized medicine research by providing the conceptual framework and technological tools to navigate this complexity. Through spatial biology, AI integration, quantitative variance modeling, and operational excellence, translational science is evolving from an add-on activity to "one of the most important design features in drug development today" [69].
The future of successful translation lies in recognizing that it is not only about compressing timelines at all costs, but about making smarter, earlier decisions that lead to stronger outcomes. By quantitatively understanding the propagation of variance, strategically implementing systems biology approaches, and creating organizationally integrated translational workflows, researchers can significantly improve the probability that promising preclinical discoveries will successfully translate to clinical benefit for patients.
The advancement of personalized medicine hinges on our ability to decode complex biological systems and translate these insights into targeted therapeutic strategies. Systems biology and Quantitative Systems Pharmacology (QSP) have emerged as critical disciplines in this endeavor, offering a transformative approach to understanding disease mechanisms and predicting patient-specific responses to treatment [73]. Systems biology constructs comprehensive models by integrating data from molecular, cellular, organ, and organism levels, providing a holistic view of biological processes [73]. QSP leverages these models to simulate drug behaviors, optimize development strategies, and ultimately bring safer, more effective therapies to patients faster [73]. The growing complexity of drug development, particularly in the era of personalized medicine, creates an urgent demand for a skilled workforce capable of bridging computational modeling, biological science, and clinical application. This whitepaper outlines the foundational educational frameworks, core competencies, and strategic collaborations required to cultivate the cross-disciplinary talent essential for the next wave of innovation in personalized medicine.
Foundational Educational Frameworks
Established Academic Programs
A cornerstone for building talent is the establishment of dedicated graduate programs. Several universities have developed specialized MSc and PhD programs to equip students with the necessary interdisciplinary skills. These programs blend theoretical foundations with practical, applied learning. The table below summarizes leading programs and their focus areas:
Table 1: Exemplary Graduate Programs in Systems Biology and QSP
| University | Program Name | Key Features & Focus Areas |
|---|---|---|
| University of Manchester | MSc Model-based Drug Development [73] | Integrates real-world industry case studies; combines theoretical teaching with hands-on modeling and data analysis projects. |
| University of Delaware | MSc in Quantitative Systems Pharmacology [73] | Focused on the application of QSP modeling in drug development. |
| Maastricht University | MSc Systems Biology and Bioinformatics [73] | Active role from industrial partners providing real-life case studies and co-supervision. |
| Imperial College London | MSc in Systems and Synthetic Biology [73] | |
| University at Buffalo | MS in Pharmacometrics and Personalised Pharmacotherapy [73] | Includes an elective course on QSP. |
Core Competencies and Skill Sets
The ideal cross-disciplinary scientist in this field possesses a unique blend of knowledge and skills. Educational programs must be designed to instill a core set of competencies:
- Biological and Pharmacological Knowledge: Deep understanding of human physiology, disease pathways, and the mechanisms of drug action, from molecular targets to organism-level effects [8] [74].
- Mathematical and Computational Modeling Proficiency: Skills in developing and working with mathematical models (e.g., ordinary differential equations for QSP) and computational methodologies to represent biological systems and drug interactions [74].
- Data Science and Bioinformatics Acumen: Expertise in managing, processing, and interpreting large-scale biological data (genomics, proteomics, etc.) using bioinformatic tools and workflow systems [75] [48].
- Familiarity with Software and Workflow Management: Proficiency with data-centric workflow systems like Snakemake and Nextflow is reshaping biological data analysis, enabling reproducible, scalable, and FAIR (Findable, Accessible, Interoperable, and Reusable) research [75]. The Playbook Workflow Builder (PWB) is an example of a web-based platform that allows for the interactive construction of bioinformatics workflows without deep technical expertise, democratizing complex analyses [76].
Strategies for Implementation and Collaboration
Industry-Academia Partnership Models
Closing the gap between theoretical knowledge and industry application requires robust, symbiotic partnerships between academia and industry. These collaborations provide invaluable practical experience, access to cutting-edge technologies, and insight into real-world research challenges [73]. Successful models include:
- Co-Designed Academic Curricula: Collaborations where industry experts contribute to curriculum design, provide guest lectures, and co-supervise student projects. This ensures that academic training is aligned with the evolving needs of pharmaceutical research and development [73].
- Specialized Training and Experiential Programs: Competitive internships and industrial placements, such as the summer internships and "sandwich" placements offered by companies like AstraZeneca, allow students to work alongside multidisciplinary project teams on high-impact problems [73].
- Joint Mentorship and Research Programs: Initiatives like Industrial CASE PhDs in the United Kingdom pair students with both an academic supervisor and an industry-based mentor, co-guiding the research project to ensure relevance and rigor [73].
Experimental and Modeling Protocols
A critical function of systems biology and QSP in personalized medicine is the creation of analytical and modeling workflows. The following protocol outlines the general methodology for developing a QSP model, a core process in the field.
Table 2: Key Protocol for QSP Model Development
| Step | Description | Methodological Considerations |
|---|---|---|
| 1. Define Needs Statement | Clearly articulate the biological, clinical, or pharmacological question the model will address. | The scope must be appropriate to ensure model utility and manageable complexity [74]. |
| 2. Literature Mining & Data Extraction | Systematically gather and synthesize prior knowledge and experimental data from published literature and databases. | Artificial Intelligence (AI) and Machine Learning (ML) tools can automate the extraction of PKPD parameters and relationships from vast amounts of text, streamlining this foundational step [74]. |
| 3. Identify System Representations | Select the appropriate mathematical structure (e.g., ODEs, network models) to represent the key biological components and their interactions. | The choice balances biological fidelity with computational tractability [74]. |
| 4. Model Assessment & Validation | Calibrate model parameters and rigorously test model predictions against independent experimental or clinical data. | This step is crucial for establishing model credibility and ensuring reliable predictions [74]. |
| 5. Hypothesis Generation & Testing | Use the validated model to simulate scenarios, optimize dosing regimens, or identify new biomarkers and drug targets. | The model becomes a tool for in-silico experimentation, guiding further research and clinical trial design [74]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Executing research in systems biology and QSP relies on a suite of computational and data resources.
Table 3: Essential Research Reagent Solutions in Computational Biology
| Item / Solution | Function in Research |
|---|---|
| Workflow Systems (e.g., Snakemake, Nextflow) | Automate and manage complex, multi-step computational analyses, ensuring reproducibility, scalability, and portability across different computing environments [75]. |
| Pre-designed Pipelines (e.g., nf-core RNA-seq) | Provide community-vetted, standardized analysis workflows for common data types (e.g., RNA sequencing), allowing researchers to conduct robust analyses without writing code from scratch [75]. |
| Cloud Computing Platforms (e.g., AWS) | Offer scalable computational power and data storage, essential for processing the large-scale genomic and 'omic datasets (petabyte-scale) common in modern research [48]. |
| Bioinformatics Databases (e.g., ATAV, GenBAR) | Centralized platforms for storing, sharing, and interrogating genomic data, facilitating large-scale case/control studies and the integration of research with clinical data [48]. |
| AI/ML Tools for Literature Mining | Natural Language Processing (NLP) and Large Language Models (LLMs) can rapidly extract and synthesize pharmacological parameters and biological relationships from scientific literature, accelerating model development [74]. |
Visualizing the Educational Pathway and Collaborative Ecosystem
The following diagrams map the key relationships in cultivating talent and the collaborative frameworks that support it.
Talent Cultivation Pathway
Collaborative Framework
Cultivating a robust workforce in systems biology and QSP is not merely an educational objective but a strategic imperative for advancing personalized medicine. The journey requires a fundamental shift from traditional, siloed training to integrated, collaborative models that blend deep biological knowledge with advanced quantitative skills. Success depends on a sustained commitment to co-designed curricula, hands-on experiential learning, and strong industry-academia partnerships that provide real-world context [73]. Furthermore, the adoption of tools that promote reproducibility and efficiency, such as data-centric workflow systems and AI-powered data extraction, will empower the next generation of scientists to tackle the complexity of human biology with unprecedented rigor and scale [75] [74]. By aligning educational initiatives with the practical demands of modern drug discovery and development, we can forge a path toward a future where therapies are not only more effective but are precisely tailored to the individual patient, fulfilling the promise of personalized medicine.
The field of Advanced Therapy Medicinal Products (ATMPs) stands at a pivotal juncture in 2025, characterized by remarkable scientific momentum juxtaposed with significant systemic strain. While groundbreaking CRISPR-based therapies and an expanding regulatory landscape create new opportunities, the industry faces a central tension: balancing rapid innovation with the infrastructure required to deliver it at scale [77]. The core challenge lies in the transition from laboratory-scale production to commercial-scale manufacturing, where complexities grow exponentially. As the industry moves beyond early adopter markets, developers are forced to do more with less, and to do it faster, with fewer missteps in a constrained funding environment [77]. This whitepaper examines how systems biology provides the foundational knowledge and analytical frameworks to overcome these standardization and scalability barriers, thereby accelerating the integration of ATMPs into personalized medicine paradigms.
The scalability challenge is quantified by a significant access gap—current manufacturing capacity reaches only approximately 20% of the eligible patient population across the U.S. and Europe [77]. This gap emerges from interrelated factors including cost of goods, reimbursement hurdles, cold chain logistics, treatment scheduling, and patient proximity to qualified treatment sites. The inherent biological complexity of ATMPs, which often involve living cells or genetic material, creates additional hurdles in manufacturing consistency, product characterization, and process control [78]. Within this context, systems biology approaches that model biological complexity as interconnected networks provide essential tools for standardizing critical quality attributes and accelerating process scalability.
Current Barriers to ATMP Standardization and Scalability
Manufacturing and Supply Chain Complexities
ATMP manufacturing faces multidimensional challenges that impact both development timelines and commercial viability. A 2025 survey of ATMP professionals revealed that 90% perceive a shortage of personnel with necessary manufacturing skills, highlighting a critical workforce gap [79]. The table below summarizes the primary areas experiencing talent shortages according to industry respondents:
Table 1: ATMP Industry Talent Shortages Identified in 2025 Survey Data
| Area of Shortage | Percentage of Respondents Identifying | Critical Skill Gaps |
|---|---|---|
| Quality Assurance/Quality Control | 20% | GMP compliance, quality systems, sterility assurance |
| Manufacturing Operations | 17% | Aseptic processing, cell culture techniques |
| Process Development | 16% | Scalable bioprocess design, tech transfer |
| Regulatory Affairs | 10% | ATMP-specific regulatory pathways, CMC documentation |
| Clinical Trials | 8% | ATMP-specific trial design, patient monitoring |
Beyond workforce challenges, manufacturing processes face technical hurdles in scaling out (increasing parallel production capacity) and scaling up (increasing batch size) while maintaining consistent product quality [78]. The autologous nature of many cell therapies introduces additional complexity, as manufacturers must manage patient-specific production chains requiring tight synchronization between apheresis, manufacturing, and reinfusion [77]. Each link in this chain must be meticulously coordinated across geographic, regulatory, and technical boundaries, creating a logistical challenge unprecedented in traditional pharmaceutical manufacturing.
Analytical and Characterization Challenges
The living nature of ATMPs introduces unique characterization difficulties that impede standardization efforts. Unlike small molecule drugs with well-defined chemical structures, ATMPs exhibit inherent biological variability that complicates the establishment of definitive critical quality attributes (CQAs) [78]. Key challenges include:
- Potency Assay Development: Creating robust, clinically relevant potency assays that accurately predict biological function remains challenging for many cell-based products.
- Genetic Stability Monitoring: Ensuring genetic integrity throughout manufacturing processes, particularly for pluripotent stem cell-derived products requiring successive culture expansions.
- Tumorigenicity Risk Assessment: Implementing sensitive methods like digital soft agar assays or cell proliferation characterization tests to detect rare transformed cells in therapeutic products [78].
These analytical challenges are compounded by the transition from Good Laboratory Practice (GLP) to Good Manufacturing Practice (GMP) environments, which requires demonstrating process consistency while accommodating biological variability [78]. Systems biology approaches help address these challenges by providing network-based models of product mechanism of action, enabling more targeted characterization strategies focused on biologically relevant attributes.
The Role of Systems Biology in Addressing ATMP Challenges
Foundational Principles and Methodologies
Systems biology provides a paradigm shift from reductionist approaches to a holistic framework that examines biological systems as integrated networks. This perspective is particularly valuable for ATMP development, where therapeutic effects often emerge from complex interactions between multiple molecular pathways rather than single targets. The core contribution of systems biology to ATMP standardization lies in its ability to:
- Model Biological Networks: Map the complex interactions between genes, proteins, and metabolic pathways that underlie therapeutic mechanisms.
- Identify Critical Quality Attributes: Distinguish biologically significant product characteristics from incidental variations.
- Predict System Behavior: Anticip how modifications in manufacturing processes might impact product safety and efficacy.
These capabilities enable a more systematic approach to quality by design (QbD) in ATMP development, where product and process understanding forms the basis for establishing a flexible yet controlled manufacturing framework. The experimental workflow below illustrates how systems biology approaches can be integrated into ATMP development:
Diagram 1: Systems Biology in ATMP Development
Experimental Protocols for Systems-Based ATMP Characterization
Implementing systems biology approaches requires specific methodological frameworks for data collection and analysis. The following protocols provide guidance for key characterization activities:
Protocol 1: Multi-omics Integration for Critical Quality Attribute Identification
Objective: Identify biologically relevant CQAs through integrated analysis of molecular data.
- Sample Collection: Collect samples at multiple manufacturing timepoints (cell isolation, expansion, final product).
- Multi-omics Profiling: Perform transcriptomic (RNA-seq), proteomic (mass spectrometry), and metabolomic profiling.
- Data Integration: Apply statistical integration methods (MOFA+, mixOmics) to identify correlated features across omics layers.
- Network Analysis: Construct interaction networks using pathway databases (KEGG, Reactome) and prior knowledge.
- CQA Prioritization: Select attributes strongly associated with mechanism of action and predictive of product potency.
Protocol 2: Mechanism of Action Deconvolution for Potency Assay Development
Objective: Develop clinically relevant potency assays based on understanding of biological mechanism.
- Pathway Perturbation: Systematically perturb key pathways (pharmacologically, genetically) in relevant cellular systems.
- Multi-parameter Readouts: Measure functional responses using high-content imaging, cytokine secretion, metabolic flux.
- Causal Network Modeling: Apply causal inference methods (PIDC, LEAP) to reconstruct regulatory networks.
- Key Node Identification: Identify minimal set of network components that predict functional output.
- Assay Development: Translate key node measurements into scalable potency assays.
Enabling Technologies and Technology Gaps
Advanced Analytical and Computational Tools
The effective implementation of systems biology in ATMP development relies on specialized research reagents and computational tools that enable comprehensive characterization of complex biological products. The table below details essential components of the "systems biology toolkit" for ATMP development:
Table 2: Research Reagent Solutions for Systems Biology-Driven ATMP Development
| Tool Category | Specific Examples | Function in ATMP Development |
|---|---|---|
| Multi-omics Platforms | Single-cell RNA sequencing, Spatial transcriptomics, Mass cytometry | Comprehensive molecular profiling of starting materials and final products to identify variability sources |
| Bioinformatics Pipelines | ATAV (Analysis Tool for Annotated Variants), WARP (WDL Analysis Research Pipelines) | Standardized analysis of genomic data, identification of biologically relevant variants [48] |
| Pathway Databases | KEGG, Reactome, WikiPathways | Contextualizing molecular measurements within established biological networks |
| Gene Editing Tools | CRISPR-based screening, Base editing | Functional validation of critical quality attributes through targeted perturbation |
| Bioprocessing Sensors | Metabolite sensors, In-line viability monitors | Real-time monitoring of critical process parameters during manufacturing |
These tools collectively enable a data-rich understanding of ATMP products and processes, facilitating the transition from empirical to knowledge-based manufacturing approaches. Cloud-based bioinformatics infrastructure, such as the Genomic & Bioinformatics Analysis Resource (GenBAR) that manages petabytes of genomic data on Amazon Web Services (AWS), provides the computational backbone for these analyses [48].
Addressing Technical Skill Gaps
The implementation of advanced technologies is hampered by significant skill shortages in the ATMP sector. Survey data indicates particular concerns about the availability and quality of expertise in aseptic processing techniques (identified by 22/40 respondents) and digital and automation skills (identified by 18/40 respondents) [79]. The integration of systems biology approaches further compounds this challenge, requiring cross-disciplinary professionals with expertise in both biological systems and computational analysis.
To address these gaps, organizations should prioritize:
- Cross-training Programs: Developing structured pathways for bioinformaticians to gain manufacturing knowledge and vice versa.
- Academic-Industry Partnerships: Collaborating with initiatives like the iGEM competition that foster systems biology approaches in biomedical innovation [80].
- Digital Skill Integration: Incorporating bioinformatics and data science training into core ATMP manufacturing curricula.
Implementing Quality by Design Through Systems Approaches
Risk-Based Process Characterization
A systems biology-informed QbD approach begins with comprehensive process characterization to identify relationships between critical process parameters (CPPs) and critical quality attributes (CQAs). The following workflow illustrates how systems modeling can guide experimental design for process characterization:
Diagram 2: QbD Implementation via Systems Biology
Standardization Through Predictive Modeling
Predictive models derived from systems biology analyses enable a more flexible approach to standardization—one based on achieving consistent biological outcomes rather than rigid adherence to fixed process parameters. This is particularly valuable for autologous therapies, where starting material variability necessitates some process adaptation. Key applications include:
- Real-Release Testing: Developing reduced-parameter release assays that serve as proxies for comprehensive product characterization.
- In-Process Controls: Establishing intermediate quality checkpoints based on predictive models of final product quality.
- Adaptive Manufacturing: Implementing controlled process adjustments to accommodate biological variability while maintaining consistent quality.
The implementation of these approaches requires robust quality management systems specifically designed for ATMPs in hospital settings, focusing on risk-based procedures, staff training, facility validation, and documentation systems [81].
Future Directions and Implementation Roadmap
Emerging Technologies and Capabilities
The convergence of systems biology with other technological advancements creates new opportunities for addressing ATMP standardization challenges. Emerging solutions include:
- AI-Enhanced Process Optimization: Machine learning algorithms that identify non-intuitive relationships between process parameters and product quality, enabling faster process characterization [82] [78].
- Organoid-Based Potency Testing: More physiologically relevant models for assessing product potency and safety, providing better predictors of clinical performance [78].
- Digital Twin Technology: Virtual replicas of manufacturing processes that enable in silico optimization and troubleshooting before implementation in GMP facilities.
These technologies, combined with advanced analytics, are transforming ATMP manufacturing from a artisanal activity to a knowledge-based enterprise capable of delivering personalized therapies at scale.
Strategic Implementation Framework
Successfully implementing systems biology approaches requires a structured framework:
- Technology Integration: Deploy multi-omics technologies at critical process checkpoints to build comprehensive process-product understanding.
- Workforce Development: Address skill gaps through targeted training in bioinformatics, data science, and systems modeling for ATMP professionals.
- Infrastructure Investment: Establish cloud-based bioinformatics infrastructure similar to Columbia's GenBAR platform to manage and analyze large datasets [48].
- Regulatory Engagement: Proactively communicate systems-based approaches to regulatory agencies, emphasizing how mechanistic understanding supports alternative control strategies.
- Knowledge Management: Implement systems to capture and leverage process and product understanding across the organization and product lifecycle.
As these elements fall into place, the industry moves closer to resolving the fundamental tension between innovation and infrastructure, enabling delivery on the promise of personalized medicine through scalable, standardized ATMP manufacturing processes.
The emergence of personalized therapeutics, propelled by integrative pharmacology and systems biology, represents a paradigm shift in clinical medicine. While these therapies promise more consistent health improvements and greater efficiency by avoiding trial-and-error use of medications, their deployment faces significant economic and accessibility hurdles. This whitepaper examines these challenges through the lens of systems biology, detailing how its principles can inform strategies for cost-effective development and equitable dissemination. Without proactive, systematic intervention, there is a substantial risk that these advanced therapies will worsen existing socioeconomic disparities in health, creating a new health equity gap.
Personalized therapeutics aims to capitalize on an improved understanding of biological heterogeneity, enabling patient selection for medications based on specific physiological, immunological, or genetic markers [83]. This approach moves beyond traditional symptom-focused treatments toward therapies that restore physiological structure and function, often classified under the emerging field of Integrative and Regenerative Pharmacology (IRP) [8]. The motivation stems from recognizing that drug responses are highly variable across populations. The convergence of systems biology, which provides a holistic framework for analyzing biological networks and dynamics [84], with pharmacologic sciences creates the foundational toolkit for this transformation.
However, this promising field faces a critical implementation challenge: if personalized therapeutics are adopted first and preferentially by economically advantaged groups, this advancement could fundamentally worsen socioeconomic disparities in health [83]. This whitepaper examines these challenges and proposes systematic, data-driven solutions grounded in systems biology principles to ensure equitable deployment.
Economic Challenges in Therapy Development
Development and Manufacturing Complexities
The development of Advanced Therapy Medicinal Products (ATMPs), including stem cell-derived therapies, faces significant translational barriers. These include unrepresentative preclinical animal models that raise questions about long-term safety and efficacy, alongside complex manufacturing issues involving scalability, automated production methods, and stringent Good Manufacturing Practice (GMP) requirements [8]. The high costs associated with these complexities ultimately limit accessibility, particularly in low- and middle-income countries.
Upfront Financial Barriers
Despite potential for long-term cost savings through more efficient, targeted treatments, personalized therapeutics represents significant additional up-front costs [83]. These include expenses for designing individualized drugs, testing biomarkers, and developing prospective profiles of disease risks and treatment responses. These costs are magnified when multiple personalized therapies are required per patient, creating substantial financial barriers for healthcare systems and payers.
Table 1: Key Economic Challenges in Personalized Therapy Development
| Challenge Category | Specific Barriers | Potential Impact |
|---|---|---|
| Development & Manufacturing | Scalability issues; Need for GMP compliance; Unrepresentative preclinical models [8] | High production costs; Delayed market entry; Regulatory uncertainties |
| Upfront Financial Outlays | Biomarker testing; Individualized drug design; Multiple therapies per patient [83] | High initial pricing; Limited insurer reimbursement; Restricted R&D portfolios |
| Regulatory & Policy | Complex pathways; Regional requirement variations (e.g., EMEA vs. FDA) [8] | Prolonged development timelines; Increased compliance costs; Market fragmentation |
Accessibility and Equity Concerns
The Risk of Widening Health Disparities
Medical progress often creates or worsens socioeconomic disparities because wealthier, more highly educated individuals typically have preferential access to new technologies and treatments [83]. According to fundamental cause theory, persons of higher socioeconomic status benefit first from new treatments because they possess the resources, knowledge, and power to learn of and act upon new developments. This pattern has historical precedent across epidemiological transitions, from plague responses in 15th century Florence to differential access to HIV/AIDS treatments in the modern era [83].
Personalized therapeutics introduces particular equity concerns because it requires additional upfront investment either for developing individualized drugs or for biomarker testing. Without proactive intervention, this creates a scenario where access is limited to economically advantaged groups, potentially increasing health inequity between both wealthy and less advantaged members of developed nations, and between rich and poor nations [83].
Multidimensional Barriers to Access
Beyond financial constraints, equitable access faces multiple barriers:
- Structural barriers in healthcare systems that limit availability in underserved areas
- Knowledge barriers among providers and patients about new treatment options
- Digital divides affecting access to the technological infrastructure required for personalized medicine approaches
- Geographic disparities in the distribution of specialized medical expertise
Table 2: Accessibility Barriers and Systems Biology-Informed Solutions
| Barrier Type | At-Risk Populations | Systems Biology Mitigation Approaches |
|---|---|---|
| Financial | Uninsured; Underinsured; Low-income countries [83] | Cost-prediction models; Streamlined biomarker identification; In silico trial optimization |
| Structural | Rural communities; Marginalized groups [83] | Portable diagnostic platforms; Decentralized manufacturing models |
| Knowledge | Health literacy challenges; Primary care providers [83] | Decision support systems; Integrated electronic health records |
The Role of Systems Biology in Addressing Challenges
Systems Biology as an Integrative Platform
Systems biology aims at achieving a system-level understanding of living organisms through the integration of genomic, transcriptomic, proteomic, and metabolomic data from a systematic perspective [84]. This approach provides a powerful framework for addressing the challenges of personalized therapy development through:
- Network Analysis: Investigating gene regulation, protein interactions, signaling, and metabolic pathways to identify critical intervention points [84]
- System Dynamics Modeling: Understanding stability, robustness, and transduction ability through system identification methods [84]
- Quantitative Modeling: Using absolutely quantified experimental measurements (e.g., mM, g/L) for direct integration into mechanistic models [85]
The application of systems biology principles enables more efficient target identification, predicts therapeutic outcomes, and characterizes mechanisms of action for regenerative approaches, ultimately accelerating regulatory approval of ATMPs [8].
Data-Driven Optimization for Cost Reduction
Quantitative -omic data empowers bottom-up systems biology approaches that can significantly reduce development costs [85]. By generating high-quality quantitative data with appropriate replicates to capture biological variability, researchers can create predictive models that:
- Identify the most efficient biomarker combinations for patient stratification
- Predict pharmacokinetic and pharmacodynamic profiles in regenerative approaches [8]
- Optimize bioreactor conditions and cell culture media through metabolic modeling
- Reduce failed experiments through in silico testing and simulation
Systems Biology Optimization Workflow
Experimental Protocols and Methodologies
Multi-Omic Data Integration Protocol
Objective: To integrate disparate -omic data types for identifying robust biomarkers and therapeutic targets.
Methodology:
- Sample Collection: Collect biological samples (blood, tissue, etc.) under standardized conditions, noting time of collection to account for circadian variations [86]
- Data Generation:
- Genomics: Whole genome sequencing for genetic variant identification
- Transcriptomics: RNA sequencing to quantify gene expression levels
- Proteomics: Mass spectrometry-based quantification of protein abundances
- Metabolomics: LC-MS/MS for absolute quantification of metabolite concentrations [85]
- Data Integration: Employ reverse-engineering schemes to construct integrated cellular networks through coupling dynamic models and statistical assessments [84]
- Network Analysis: Identify key regulatory nodes and pathways using system identification technologies [84]
Validation: Confirm network predictions using synthetic biology approaches [84] and validate biomarkers in independent patient cohorts.
AI-Enhanced Biomarker Discovery Protocol
Objective: To leverage artificial intelligence for identifying cost-effective biomarker panels.
Methodology:
- Data Preprocessing: Normalize multi-omic data sets and handle missing values using appropriate imputation methods
- Feature Selection: Apply machine learning algorithms (e.g., random forests, neural networks) to identify minimal biomarker sets with maximal predictive power
- Model Training: Train predictive models using cross-validation to avoid overfitting
- Clinical Translation: Develop simplified assay protocols focusing on the identified minimal biomarker set
- Cost-Benefit Analysis: Evaluate the economic impact of implementing the simplified biomarker panel
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Systems Biology-Driven Personalized Therapy
| Reagent/Category | Function in Research | Application in Personalized Therapy |
|---|---|---|
| Absolute Quantification Standards | Enable precise measurement of metabolite/protein concentrations [85] | Accurate biomarker measurement for patient stratification |
| Orthogonal Inducible Promoters | Enable precise control of gene expression in synthetic circuits [84] | Engineered cellular therapies with tunable activity |
| CRISPR/Cas9 Gene Editing Systems | Targeted genome modification for functional validation | Correction of disease-causing mutations in cell therapies |
| Stimuli-Responsive Biomaterials | Temporally controlled delivery of bioactive compounds [8] | Localized, sustained drug release with reduced side effects |
| Single-Cell RNA Sequencing Kits | Characterization of cellular heterogeneity in tissues | Identification of rare cell populations for targeting |
| Isotopic Tracers (13C, 15N) | Enable fluxomics studies of metabolic pathway activity [85] | Understanding drug metabolism variations between patients |
Strategic Framework for Equitable Implementation
Proactive Equity Monitoring
A three-tiered approach should be implemented to prevent worsening health disparities:
- Systematic Surveillance: Collect data on access to and use of personalized therapeutics stratified by socioeconomic status, including information on awareness, understanding, barriers to availability, and reasons for declination [83]
- Provider Feedback: Report to individual providers their rates of use relative to peers to motivate changes in clinical practice [83]
- Targeted Intervention: Identify locations with relative underuse and investigate potential barriers in access or underperforming dissemination practices [83]
Alternative Dissemination Models
Several innovative models should be piloted and evaluated for their effectiveness in promoting equitable access:
- Assistance Programs: Develop free or low-cost programs for uninsured or low-income patients [83]
- Targeted Introduction: Implement focused deployment in medical practices serving low-income patients [83]
- Patient Navigator Programs: Utilize community health workers to facilitate access to treatment [83]
- Cross-Subsidization: Create pricing models where higher margins in affluent markets subsidize costs in underserved areas
Integrated Framework for Equitable Implementation
Personalized therapeutics represents a transformative advancement in clinical medicine with the potential to significantly improve treatment outcomes. However, without systematic attention to economic and accessibility challenges, there is substantial risk of worsening existing health disparities. Systems biology provides powerful tools for addressing these challenges through data-driven optimization, network-based biomarker discovery, and quantitative modeling of therapeutic outcomes.
Future progress requires interdisciplinary collaboration between academia, industry, clinics, and regulatory authorities to establish standardized procedures and ensure consistency in therapeutic outcomes [8]. Particular attention should be paid to developing affordable biomaterials, establishing scalable bioprocesses, and implementing proactive equity monitoring. Through these coordinated efforts, the promise of personalized therapeutics can be realized for all patient populations, regardless of socioeconomic status.
Proving the Paradigm: Validation, Collaboration, and Measuring Impact
The escalating complexity of therapeutic development, particularly for personalized medicine, demands a workforce proficient in Systems Biology (SB) and Quantitative Systems Pharmacology (QSP). These disciplines provide a holistic, model-based framework for understanding complex biological systems and predicting patient-specific responses to therapy [87] [73]. This paradigm shift necessitates a new kind of scientist, one equipped with interdisciplinary skills to bridge the gap between computational modeling and clinical application. Industry-academia partnerships have consequently emerged as a critical engine for cultivating this talent and accelerating the translation of basic research into novel therapies.
These collaborations are foundational to a broader thesis on how systems biology fuels personalized medicine. By integrating multi-scale data—from molecular and cellular levels to organ and organism levels—SB constructs comprehensive models of disease mechanisms [87]. QSP then leverages these models to simulate drug behavior, predict patient responses, and optimize therapeutic strategies, moving beyond the traditional one-size-fits-all approach to enable truly personalized care [87] [8]. The co-design of educational programs and research validation frameworks between industry and academia ensures that the scientific workforce is trained in the precise tools and methodologies needed to realize this potential, creating a direct pipeline from foundational science to patient-specific treatment solutions.
Co-Designing Educational Curricula for a Model-Ready Workforce
Collaborative design of academic curricula is a cornerstone of building a robust talent pipeline. These initiatives integrate real-world industrial challenges into academic training, equipping students with the practical skills required for model-informed drug development.
Models for Collaborative Curriculum Development
Several innovative models demonstrate how industry and academia can intertwine their strengths to enhance education.
- Co-Designed Academic Curricula: This model involves industry experts directly contributing to the development and delivery of MSc and PhD programs. Challenges include a scarcity of faculty with applied experience and the inflexibility of traditional university structures [87] [73]. A prime exemplar is the University of Manchester's MSc in Model-based Drug Development, which integrates real-world case studies, hands-on modeling projects, and guest lectures from practicing scientists [87] [73]. Similarly, Dutch MSc Systems Biology programs at institutions like Maastricht University and Wageningen University actively involve industrial partners in providing case studies and co-supervising research projects [87] [73]. For undergraduate education, a framework proposed by Androulakis (2022) offers actionable syllabi combining mathematical modeling, numerical simulation, and pharmacokinetics/pharmacodynamics (PK/PD) using clinically-relevant problems [87] [73].
- Specialized Experiential Programs: Internships and placements provide invaluable hands-on experience. AstraZeneca, for example, hosts competitive summer internships and long-term "sandwich" placements for undergraduates and postgraduates [87] [73]. These opportunities expose students to high-impact SB/QSP problems, often leading to joint publications and post-graduation employment. Short, challenge-based events like "datathons" and "hackathons" also serve as effective, focused training grounds.
- Mentorship and Career Development: Programs like the Industrial CASE PhDs in the United Kingdom formally pair a student with both an academic supervisor and an industry-based mentor [73]. This co-guidance ensures the research project remains academically rigorous while addressing relevant industry challenges, though it requires clear coordination to define roles and avoid redundancy [87] [73].
Exemplar Programs in Systems Biology and QSP
A growing number of universities have established specialized programs that serve as models for training in SB and QSP, many of which inherently involve industry collaboration.
Table 1: Exemplar Graduate Programs in Systems Biology and Quantitative Systems Pharmacology
| University | Program Name | Key Features | Industry Collaboration Elements |
|---|---|---|---|
| University of Manchester | MSc Bioinformatics and Systems Biology; MSc Model-based Drug Development [87] [73] | Combines theoretical teaching with hands-on modeling projects. | Input from industry experts, guest lectures, real-world case studies. |
| Imperial College London | MSc in Systems and Synthetic Biology [87] [73] | Focuses on the integration of biology with engineering principles. | |
| University of Delaware | MSc in Quantitative Systems Pharmacology [87] [73] | Dedicated QSP program focusing on pharmacometric and modeling approaches. | |
| University at Buffalo | MS in Pharmacometrics and Personalised Pharmacotherapy [87] [73] | Includes an elective course on QSP. | |
| Maastricht University | MSc Systems Biology and Bioinformatics [87] [73] | Industrial partners provide real-life case studies and co-supervise projects. |
Validated Experimental and Computational Workflows
A critical output of industry-academia partnerships is the development and rigorous validation of integrated workflows that combine experimental biology with computational modeling. These workflows are essential for generating reliable, translatable insights in personalized medicine.
An Integrated Workflow for Genomic Validation and Clinical Reporting
The Geno4ME study provides a powerful, real-world example of a fully implemented and validated workflow for integrating whole genome sequencing (WGS) into clinical care, a cornerstone of personalized medicine [88]. This framework can be adapted for validating systems biology models in drug development.
The diagram below outlines the key stages of this process, from participant enrollment to the return of actionable results.
Detailed Methodologies for Workflow Validation
The workflow's reliability is ensured through rigorous, multi-faceted validation protocols:
- WGS Assay Validation for Inherited Disease Genes: The analytical validity of the WGS assay for detecting single nucleotide variants (SNVs), indels, and copy number variants (CNVs) was confirmed using two primary methods. First, orthogonal testing was performed at a commercial reference laboratory (N=188 participants), demonstrating 100% sensitivity and specificity for detecting pathogenic/likely pathogenic (P/LP) variants. Second, concordance was assessed using known positive samples and reference materials (N=61) [88].
- Pharmacogenomics (PGx) Panel Validation: The PGx genotyping for genes including
CYP2C19,CYP2C9,VKORC1, andCYP4F2was validated against data from the CDC Genetic Testing Reference Material (GeT-RM) program, showing 100% concordance [88]. Furthermore, paired blood and saliva samples from 60 participants demonstrated 100% genotyping concordance using the study's WGS method [88]. - Bioinformatic and Clinical Interpretation: Processed sequencing data is analyzed through a curated panel of genes associated with hereditary disease and pharmacogenomics. Variants are classified according to ACMG guidelines, and clinical reports are generated with guideline-based management recommendations (e.g., from the National Comprehensive Cancer Network) [88].
The Scientist's Toolkit: Key Reagents and Materials
The successful execution of integrated workflows relies on a suite of specialized reagents and tools.
Table 2: Essential Research Reagent Solutions for Genomic Studies
| Item | Function/Description |
|---|---|
| Blood and Saliva Collection Kits | Non-invasively collect and stabilize high-quality DNA for subsequent Whole Genome Sequencing [88]. |
| Whole Genome Sequencing (WGS) Platforms | Provide a comprehensive view of an individual's genetic code, enabling the discovery of variants across coding and non-coding regions [48] [88]. |
| Orthogonal Validation Platforms | Independent testing methods (e.g., commercial reference lab panels) used to confirm the accuracy of primary WGS findings and ensure result reliability [88]. |
| Bioinformatic Pipelines (e.g., ATAV, WARP) | Computational tools for aligning sequence data to a reference genome (GRCh38), variant calling, and performing case/control association studies [48] [88]. |
| Curated Gene Panels (ACMG, CPIC) | Expert-defined lists of clinically actionable genes for hereditary disease and pharmacogenomics, which focus analysis and reporting on medically relevant findings [88]. |
Impact and Application in Personalized Medicine
The ultimate validation of these collaborative models and workflows is their tangible impact on patient care and therapeutic development, particularly in advancing personalized medicine.
Quantitative Outcomes in Clinical Implementation
The Geno4ME study demonstrates the profound clinical utility of such validated approaches. In a diverse cohort of 2,017 participants, 21.4% (432 individuals) received one or more medical intervention recommendations based on their genetic results for inherited disease or pharmacogenomics [88]. Crucially, 7.8% (158 participants) were found to have a clinically significant (P/LP) variant associated with an inherited disease, the majority of which were in cancer-associated genes, enabling early detection and prevention strategies [88]. This real-world data underscores how systems biology-driven approaches directly contribute to personalizing healthcare by identifying individual genetic risks.
Driving Innovation in Integrative and Regenerative Pharmacology
The convergence of systems biology with regenerative medicine is creating a new paradigm known as Integrative and Regenerative Pharmacology (IRP) [8]. This field aims to restore physiological structure and function, moving beyond merely managing symptoms. Systems biology methodologies are critical for defining the mechanism of action (MoA) of complex regenerative therapies, such as those involving stem cells, which can be viewed as "tunable combinatorial drug manufacture and delivery systems" [8]. By modeling disease networks, systems biology aids in the discovery of drugs that can simultaneously target multiple levels of biological organization, thereby accelerating the regulatory approval of advanced therapy medicinal products (ATMPs) [8].
Industry-academia partnerships are not merely beneficial but are essential for co-designing the educational frameworks and validating the sophisticated models that underpin modern, personalized drug development. Through collaborative curricula, experiential learning, and rigorous validation of integrated computational-experimental workflows, these alliances cultivate a skilled workforce and generate the robust evidence required to translate systems biology insights into patient-specific therapies. As the field progresses, the continued refinement of these partnerships, supported by shared data platforms and flexible manufacturing technologies, will be paramount in ensuring that the promise of personalized medicine is realized equitably and effectively for all patient populations.
The integration of real-world evidence (RWE) into biomarker development and regulatory science represents a paradigm shift in personalized medicine. Moving beyond traditional clinical trials, RWE provides a dynamic, systems-level understanding of biomarker function across diverse patient populations and clinical settings. This technical guide examines methodologies for leveraging RWE to enhance biomarker validation, supported by emerging regulatory frameworks that recognize the value of real-world data (RWD) for regulatory decision-making. By establishing rigorous standards for RWD collection, study design, and evidence generation, researchers can accelerate the development of robust biomarkers that reliably predict therapeutic responses and disease outcomes in real-world contexts, thereby advancing systems biology approaches to personalized medicine.
The Convergence of RWE and Biomarker Science in Regulatory Contexts
Defining the Framework: RWD and RWE
The U.S. Food and Drug Administration (FDA) defines real-world data (RWD) as data relating to patient health status and/or the delivery of health care routinely collected from a variety of sources, while real-world evidence (RWE) is the clinical evidence about the usage and potential benefits or risks of a medical product derived from analysis of RWD [89]. The FDA has demonstrated a strong commitment to advancing the use of fit-for-purpose RWD to generate RWE that can enhance drug development and strengthen regulatory oversight [89]. This established framework provides the foundation for incorporating RWE into biomarker validation.
RWE is increasingly recognized as having the potential to address gaps in traditional research methodologies, particularly in precision oncology where it can supplement clinical trials, enable conditional reimbursement and accelerated drug access, and innovate trial conduct [90]. Purpose-built RWD repositories may support the extension or refinement of drug indications and facilitate the discovery and validation of new biomarkers [90].
The Expanding Regulatory Acceptance of RWE
Regulatory agencies are increasingly incorporating RWE into their decision-making processes. The FDA's Center for Drug Evaluation and Research (CDER) and Center for Biologics Evaluation and Research (CBER) have applied RWE in various regulatory contexts since 2011, including product approvals, labeling changes, and assessments determining no regulatory action was warranted [89]. This regulatory acceptance forms part of a comprehensive landscape analysis to assess the scope and frequency of RWE use in regulatory determinations across the agency.
The FDA has launched FDA-RWE-ACCELERATE, the first FDA-wide initiative dedicated to advancing the integration of real-world evidence into regulatory decision-making [91]. This initiative brings together experts from across all Centers, strengthens information exchange, and ensures that RWE is applied consistently and effectively throughout the Agency. Additionally, the modernization of the Sentinel System to Sentinel 3.0 is designed to harness advanced data science and analytics to detect safety signals earlier, generate evidence more efficiently, and better inform regulatory decisions [91].
Table 1: FDA-Reported Regulatory Actions Supported by RWE
| Product | Regulatory Action | RWE Use Case | Data Source | Date |
|---|---|---|---|---|
| Aurlumyn (Iloprost) | Approval | Confirmatory evidence | Medical records | Feb 2024 |
| Vimpat (Lacosamide) | Labeling expansion | Safety assessment | PEDSnet data network | Apr 2023 |
| Actemra (Tocilizumab) | Approval | Primary efficacy endpoint | National death records | Dec 2022 |
| Vijoice (Alpelisib) | Approval | Substantial evidence of effectiveness | Medical records | Apr 2022 |
| Prolia (Denosumab) | Boxed Warning | Safety assessment | Medicare claims data | Jan 2024 |
Methodological Framework: RWE for Biomarker Validation
Data Source Considerations for Biomarker Validation
The quality and appropriateness of RWD sources are paramount for biomarker validation. Different data sources offer distinct advantages and limitations for various aspects of biomarker development:
- Electronic Health Records (EHRs): Provide clinical data, treatment patterns, and outcomes across diverse care settings, but often lack structured biomarker data [92]
- Disease Registries: Offer curated, disease-specific data with standardized follow-up, particularly valuable for rare diseases [89]
- Genomic Databases: Enable correlation of molecular biomarkers with clinical outcomes when linked to clinical data [48]
- Claims Data: Provide longitudinal treatment patterns and healthcare utilization, but limited clinical granularity [89]
- Patient-Generated Data: From wearables and mobile devices, offering continuous physiological monitoring [32]
The emerging trend toward multi-modal data fusion addresses the limitations of individual data sources by integrating complementary data types to create a more comprehensive understanding of biomarker performance [32]. This approach is particularly relevant within systems biology frameworks, where biomarkers are understood as components of interconnected biological networks rather than isolated indicators.
Methodological Approaches and Study Designs
Robust study designs are essential for minimizing bias and confounding when using RWE for biomarker validation:
External Control Arms (ECAs): These are advancing clinical research by replacing traditional non-interventional groups with high-quality RWD, particularly valuable in rare diseases where traditional control groups are unattainable [92]. ECAs streamline research processes, improve feasibility, and reduce costs, creating a faster pathway from trial to treatment [92].
Retrospective Cohort Studies: Well-suited for assessing biomarker-disease associations and evaluating biomarker performance across diverse populations [89]. These designs can leverage existing longitudinal data to evaluate how biomarkers predict long-term outcomes.
Non-interventional Studies: Can provide pivotal evidence for biomarker validation, particularly when using registry data with well-documented natural history comparators [89].
Hybrid Trial-RWE Designs: Combine elements of traditional clinical trials with RWD collection to enhance generalizability while maintaining scientific rigor.
Analytical Techniques for RWE-Based Biomarker Validation
Advanced analytical methods are required to address the inherent challenges of RWD:
- Propensity Score Methods: For balancing measured confounders between comparison groups
- Machine Learning Algorithms: To identify complex, non-linear relationships between biomarkers and outcomes [32]
- Natural Language Processing (NLP): For extracting biomarker information from unstructured clinical notes [92]
- Time-to-Event Analyses: To evaluate biomarker performance for predicting long-term outcomes
- Sensitivity Analyses: To assess the robustness of findings to various assumptions and potential unmeasured confounding
Artificial intelligence is transforming biomarker analytics by pinpointing subtle patterns in high-dimensional multi-omic and imaging datasets that conventional methods may miss [93]. Predictive models could ultimately facilitate a paradigm shift within oncology as they go beyond merely identifying biomarkers to actually forecasting future outcomes, enabling more personalized and effective therapies [93].
Experimental Protocols for RWE-Based Biomarker Studies
Protocol 1: Retrospective Biomarker Validation Using EHR Data
Objective: To validate the association between a predictive biomarker and treatment response in real-world populations.
Materials and Methods:
- Cohort Definition: Identify patients with the condition of interest using structured diagnosis codes, medication records, and clinical notes
- Biomarker Assessment: Extract biomarker values from laboratory databases, pathology reports, or genomic test results
- Outcome Ascertainment: Define and validate clinical outcomes through a combination of structured data and chart review
- Statistical Analysis:
- Apply appropriate methods to control for confounding (e.g., propensity score matching/stratification)
- Evaluate biomarker-performance using appropriate statistical measures (sensitivity, specificity, AUC)
- Conduct pre-specified subgroup and sensitivity analyses
Quality Control Measures:
- Implement validation checks for electronic phenotyping algorithms
- Establish blinded adjudication processes for critical outcomes
- Apply standardized approaches for handling missing data
Protocol 2: External Control Arm Construction for Biomarker-Enriched Trials
Objective: To create a well-matched external control group for single-arm trials of biomarker-targeted therapies.
Materials and Methods:
- Source Population Identification: Identify potential controls from RWD sources with similar clinical characteristics to trial participants
- Biomarker Status Imputation: Develop and validate algorithms to infer biomarker status in RWD populations when not directly measured
- Matching Procedure:
- Apply propensity score-based matching on clinically relevant covariates
- Prioritize matching on strong prognostic factors and biomarker status
- Assess balance using standardized differences
- Outcome Comparison: Compare outcomes between trial participants and matched external controls, accounting for residual confounding
Validation Steps:
- Compare characteristics of RWD-derived external controls with historical control groups when available
- Assess transportability of treatment effect estimates from previous randomized trials
- Evaluate consistency of results across different matching algorithms and RWD sources
Table 2: Key Research Reagent Solutions for RWE Biomarker Studies
| Research Tool Category | Specific Examples | Primary Function | Considerations for Use |
|---|---|---|---|
| Data Integration Platforms | ATAV, AWS HealthOmics, WARP pipelines | Genomic data processing and harmonization | Cloud-based scalability, standardized processing [48] |
| Biomarker Assay Technologies | Liquid biopsy, multiplex IHC, spatial transcriptomics | Multi-parameter biomarker measurement | Sensitivity, specificity, standardization requirements [94] |
| AI/Analytical Tools | Natural Language Processing, Machine Learning algorithms | Pattern recognition in complex datasets | Validation requirements, interpretability [93] |
| Biomarker Data Repositories | IRIS Registry, AQUA Registry, CIBMTR registry | Disease-specific clinical and outcome data | Data completeness, representativeness [92] |
| Advanced Disease Models | Organoids, humanized mouse models | Functional validation of biomarker candidates | Biological relevance, throughput capabilities [93] |
Regulatory Considerations and Evidence Standards
Evolving Regulatory Frameworks for RWE
Regulatory agencies are developing more sophisticated approaches to evaluating RWE submissions. The FRAME (Framework for Real-World Evidence Assessment to Mitigate Evidence Uncertainties for Efficacy/Effectiveness) framework represents one such approach for evaluating regulatory and health technology assessment decision-making [95]. Similarly, the APPRAISE tool provides a methodology for appraising potential for bias in real-world evidence studies [95].
These frameworks address key dimensions of RWE quality assessment:
- Data Quality and Relevance: Fitness of RWD for the intended use case
- Study Design Appropriateness: Ability of the design to address the research question
- Bias Mitigation: Approaches to minimize confounding, selection bias, and information bias
- Transparency and Reproducibility: Complete reporting of data sources, methods, and analyses
Standards for RWE Submission in Biomarker Applications
When submitting RWE to support biomarker validation, researchers should address several key considerations:
- Data Provenance: Provide detailed descriptions of RWD sources, including original collection purposes, data curation processes, and quality assurance procedures
- Biomarker Measurement: Document the accuracy, precision, and reproducibility of biomarker assessment methods in real-world settings
- Context of Use: Clearly specify the intended clinical context for the biomarker and ensure the RWE is appropriate for that context
- Evidence Integration: Position the RWE within the totality of evidence supporting the biomarker's clinical utility
Regulatory bodies will increasingly recognize the importance of real-world evidence in evaluating biomarker performance, allowing for a more comprehensive understanding of their clinical utility in diverse populations [94]. This aligns with the broader trend toward standardization initiatives where collaborative efforts among industry stakeholders, academia, and regulatory bodies promote establishment of standardized protocols for biomarker validation [94].
Case Studies in RWE-Driven Biomarker Development
Case Study 1: Oncology Biomarker Validation
Challenge: Traditional clinical trials for rare oncology biomarkers face recruitment challenges and may lack generalizability.
RWE Approach: Use of external control arms from curated EHR-derived datasets to contextualize single-arm trial results. For example, Verana Health's Qdata modules provide research-ready data that can serve as control data, enabling shorter trial timelines and optimized resources [92]. In rare diseases, where traditional control groups are often unattainable, specialized datasets offer a viable alternative by providing a more accurate way to analyze and identify patient populations [92].
Outcome: More efficient biomarker validation with enhanced understanding of biomarker performance in diverse clinical settings.
Case Study 2: Safety Biomarker Identification
Challenge: Identification of biomarkers predictive of adverse drug reactions in real-world populations.
RWE Approach: Leverage large healthcare databases like the FDA Sentinel System to identify potential safety signals, then conduct focused biomarker studies within these populations. The FDA has utilized this approach for multiple products, resulting in safety-related labeling changes [89]. For example, a retrospective cohort study in Sentinel indicated an association between beta blocker use and hypoglycemia in pediatric populations, leading to FDA-approved safety labeling changes to describe this risk [89].
Outcome: Clinically actionable safety biomarkers that reflect medication risks in heterogeneous patient populations.
Future Directions and Emerging Trends
The field of RWE in biomarker development is rapidly evolving, with several emerging trends likely to shape future approaches:
AI-Enhanced Predictive Models: Artificial intelligence is anticipated to play an even bigger role in biomarker analysis, with AI-driven algorithms revolutionizing data processing and analysis [94]. This will enable more sophisticated predictive models that can forecast disease progression and treatment responses based on biomarker profiles [94].
Multi-Omics Integration: The trend toward multi-omics integration is expected to gain momentum, with researchers increasingly leveraging data from genomics, proteomics, metabolomics, and transcriptomics to achieve a holistic understanding of disease mechanisms [94]. This approach will enable identification of comprehensive biomarker signatures that reflect the complexity of diseases [94].
Advanced Biomarker Technologies: Liquid biopsies are poised to become a standard tool in clinical practice, with advances in technologies such as circulating tumor DNA (ctDNA) analysis and exosome profiling increasing sensitivity and specificity [94]. Single-cell analysis technologies are also expected to become more sophisticated and widely adopted [94].
Patient-Centric Approaches: The shift toward patient-centric approaches in clinical research will be more pronounced, with biomarker analysis playing a key role in enhancing patient engagement and outcomes [94]. This includes incorporating patient-reported outcomes into biomarker studies and engaging diverse patient populations to ensure new biomarkers are relevant across different demographics [94].
These advancements align with the broader movement toward Integrative and Regenerative Pharmacology (IRP), which represents the application of pharmacological sciences to accelerate, optimize, and characterize the development, maturation, and function of bioengineered and regenerating tissues [8]. This emerging field bridges pharmacology, systems biology and regenerative medicine, thereby merging conventional drugs with target therapies intended to repair, renew, and regenerate rather than merely block or inhibit [8].
The strategic integration of RWE into biomarker validation represents a transformative approach to advancing personalized medicine. By leveraging diverse real-world data sources, implementing rigorous methodological approaches, and adhering to evolving regulatory standards, researchers can develop robust biomarkers that reliably predict treatment responses and disease outcomes across diverse patient populations. As regulatory frameworks continue to evolve and analytical methodologies advance, RWE will play an increasingly critical role in biomarker development, ultimately accelerating the delivery of personalized therapeutics to patients who stand to benefit most. The convergence of RWE with systems biology approaches promises to unlock new dimensions in understanding disease mechanisms and therapeutic responses, moving beyond single biomarkers to integrated biomarker networks that more comprehensively capture biological complexity.
The pharmaceutical industry faces a persistent challenge of declining efficiency in research and development. Traditional drug discovery and development is an extraordinarily complex and protracted endeavor, requiring 10 to 15 years on average from initial discovery to market approval, with only about 1 in 250 compounds entering preclinical testing ever reaching commercialization [96]. This lengthy timeline, coupled with extremely high attrition rates, has catalyzed a search for more efficient approaches. The emerging discipline of systems biology represents a fundamental paradigm shift from traditional reductionist pharmacology toward a holistic, network-based understanding of biological systems and drug actions [97] [98].
This paradigm shift is particularly crucial within the context of personalized medicine, where the goal is to tailor therapies based on individual patient characteristics rather than population averages. Traditional pharmacology typically focuses on single drug targets and biomarkers, while systems biology aims to integrate multi-scale data from genomic, proteomic, transcriptomic, and metabolomic layers to build comprehensive network models of disease mechanisms and drug responses [99]. This integrative approach provides the foundational framework necessary for predicting how individual variations in molecular networks influence drug efficacy and safety, thereby enabling truly personalized therapeutic strategies [97] [8].
The following analysis examines the comparative efficiency of these two approaches across key dimensions of the drug development pipeline, with particular emphasis on how systems biology methodologies are addressing the critical bottlenecks that have long plagued traditional pharmacological approaches.
Methodological Foundations: Contrasting Approaches
Core Principles of Traditional Pharmacology
Traditional pharmacology operates primarily through a reductionist framework, focusing on linear cause-effect relationships between drugs and their targets. The pharmacokinetic/pharmacodynamic (PK/PD) modeling approach establishes relationships between drug administration, plasma concentration, and biological response, often relying on empirical data fitting rather than mechanistic understanding [98]. This approach typically focuses on a single biomarker as a measure of drug activity and generally does not account for the complex network interactions within biological systems [97]. The traditional drug development workflow follows a sequential, stage-gated process from target identification through clinical trials, with decision points primarily based on statistical analysis of empirical data rather than mechanistic predictions [100].
Core Principles of Systems Biology in Pharmacology
Systems biology approaches drug development through a holistic framework that analyzes cellular regulatory networks as integrated systems. This methodology applies quantitative tools and computational modeling to develop and study the functional capabilities of molecular networks [97] [101]. Rather than focusing on single targets, it employs network analyses to map the topology of biological systems and constructs dynamic models representing biochemical reaction mechanisms from ligand-receptor binding to cell outputs [97]. This approach explicitly accounts for regulatory motifs such as feed-forward and feedback loops that determine system behavior [97]. By integrating multi-omics data, systems biology creates computational models that can simulate experiments, predict outcomes of biological processes, and generate testable hypotheses [101] [99].
Table 1: Fundamental Methodological Differences Between Approaches
| Dimension | Traditional Pharmacology | Systems Biology Approach |
|---|---|---|
| Philosophical Foundation | Reductionist | Holistic |
| Primary Modeling Approach | Empirical PK/PD models | Mechanistic network models |
| Target Perspective | Single targets | Multiple targets within networks |
| Data Utilization | Focused on specific biomarkers | Multi-omics data integration |
| Temporal Resolution | Static snapshots | Dynamic system behavior |
| Validation Strategy | Statistical significance | Mechanistic plausibility + statistical validation |
Quantitative Efficiency Metrics: Comparative Analysis
The efficiency differential between traditional and systems-based approaches manifests across multiple dimensions of the drug development pipeline. Systems biology approaches demonstrate particular advantage in early phases where mechanistic understanding can de-risk subsequent development stages.
Table 2: Efficiency Metrics Comparison in Drug Development
| Development Stage | Traditional Pharmacology | Systems Biology Approach | Efficiency Advantage |
|---|---|---|---|
| Target Identification | 3-6 years [100] | 1-3 years [102] | 40-50% reduction |
| Preclinical Attrition | >99% failure rate [96] | Early de-risking via mechanistic models | Significant improvement predicted |
| Clinical Success Rates | 10-20% from human trials to approval [96] | Improved patient stratification | 2-3 fold improvement potential |
| Personalization Capability | Limited by single biomarkers | Enabled by network response profiling | Transformative improvement |
| Mechanistic Insight | Limited to direct drug-target interactions | Comprehensive network pharmacology | Deeper understanding of efficacy/toxicity |
The integration of systems biology has demonstrated particular value in addressing patient variability, a major contributor to drug development failures. Enhanced Pharmacodynamic (ePD) models that combine systems biology with traditional PD approaches can account for how genomic, epigenomic, and posttranslational characteristics in individual patients alter drug response [97]. For example, simulations of EGFR inhibitor therapy have shown how different genomic profiles (e.g., RASAL1 hypermethylation, RKIP/PEBP polymorphisms) can predict resistance or sensitivity, enabling pre-treatment stratification that significantly improves clinical trial success rates [97].
Experimental Protocols: Methodological Applications
Protocol 1: Constructing Predictive Multi-Scale Networks for Target Identification
Objective: Identify novel drug targets and their network context for complex diseases using multi-omics data integration.
Methodology:
- Data Collection: Acquire matched genomic, transcriptomic, proteomic, and metabolomic datasets from disease and control samples. Utilize high-throughput technologies including RNA sequencing, mass spectrometry-based proteomics, and metabolomic profiling [102].
- Differential Analysis: Identify differentially expressed genes (DEGs) using moderated t-statistics and empirical Bayes approaches (e.g., Limma package in R). Select genes with significant fold-change and p-values [99].
- Network Construction:
- Build protein-protein interaction (PPI) networks using known interaction databases
- Construct gene co-expression networks using Weighted Gene Co-expression Network Analysis (WGCNA) or Context Likelihood of Relatedness algorithm for non-linear correlations [99]
- Integrate multi-omics layers into unified networks using statistical integration methods
- Network Analysis: Identify densely connected modules and hub genes with high connectivity. Annotate modules for functional enrichment using gene ontology and pathway databases.
- Experimental Validation: Perform in vitro or in vivo perturbation experiments (e.g., CRISPR/Cas9 knockouts) on prioritized targets to confirm functional role in disease mechanisms [100].
Protocol 2: Enhanced Pharmacodynamic (ePD) Modeling for Patient Stratification
Objective: Develop mechanistic models that predict individual patient drug response based on genomic and molecular profiling.
Methodology:
- Pathway Mapping: Construct a detailed map of the drug's target pathway, including all key components and regulatory motifs (feedback/feed-forward loops). For example, a comprehensive EGFR signaling map including downstream RAS-RAF-MEK-ERK cascade [97].
- Ordinary Differential Equation (ODE) Development: Translate pathway map into a system of ODEs that quantitatively describes the dynamics of each component. Parameters include reaction rates, synthesis, and degradation constants.
- Genomic Integration: Incorporate patient-specific genomic variations as altered parameters in the ODE model. For example:
- Single nucleotide polymorphisms (SNPs) as modified kinetic constants
- Gene copy number variations as altered protein expression levels
- Epigenetic modifications as changed reaction rates [97]
- Model Calibration: Fit model parameters to in vitro experimental data using optimization algorithms (weighted least squares, maximum likelihood).
- Simulation and Stratification: Simulate drug response for virtual patient populations with different genomic profiles. Cluster patients into response categories based on simulation outcomes [97].
Protocol 3: Phosphoproteomic Signaling Analysis for Mechanism of Action Elucidation
Objective: Characterize drug mechanism of action and identify resistance mechanisms through dynamic signaling network analysis.
Methodology:
- Experimental Design: Treat disease-relevant cell lines with compounds across multiple concentrations and time points. Include appropriate controls and replicates.
- Sample Processing: At each time point, lyse cells and prepare lysates for phosphoproteomic analysis using appropriate protein extraction and quantification methods.
- Phosphoprotein Measurement: Utilize high-content phosphoproteomic technologies such as:
- xMAP technology: Multiplexed bead-based assays measuring up to 30 phosphoproteins simultaneously
- Reverse Phase Protein Arrays (RPPA): High-throughput antibody-based profiling of signaling phosphoproteins
- Mass spectrometry-based phosphoproteomics: Global identification and quantification of phosphorylation sites [98]
- Data Preprocessing: Normalize data, impute missing values, and perform quality control checks.
- Network Inference: Construct dynamic signaling networks using computational methods that infer causal relationships from phosphoproteomic time-series data.
- Drug Signature Analysis: Compare compound-induced signaling changes to reference compounds with known mechanisms to infer MoA and identify potential resistance mechanisms [98].
Visualization of Key Concepts
Systems Biology Drug Development Workflow
EGFR Signaling Pathway with Genomic Variants
The Scientist's Toolkit: Essential Research Reagents and Technologies
Implementation of systems biology approaches requires specialized reagents and technologies that enable comprehensive molecular profiling and computational analysis.
Table 3: Essential Research Reagents and Platforms for Systems Pharmacology
| Reagent/Technology | Function | Application in Drug Development |
|---|---|---|
| CRISPR/Cas9 Gene Editing | Precise genome engineering for target validation | Functional validation of candidate targets in disease-relevant models [100] |
| DNA-Encoded Libraries (DELs) | Ultra-high-throughput screening of compound libraries | Hit identification against validated targets with expanded chemical space [100] |
| xMAP Technology | Multiplexed bead-based phosphoprotein measurement | Signaling network analysis for mechanism of action studies [98] |
| scRNA-seq Platforms | Single-cell RNA sequencing for cellular heterogeneity | Identification of cell subpopulations driving disease or treatment resistance [101] |
| Reverse Phase Protein Arrays (RPPA) | High-throughput antibody-based protein profiling | Quantitative analysis of signaling pathways across patient samples [98] |
| AI/ML Modeling Platforms | Machine learning algorithms for pattern recognition | Predictive modeling of drug response and patient stratification [103] |
Future Perspectives and Integration with Emerging Technologies
The integration of artificial intelligence with systems biology approaches represents the next frontier in drug development efficiency. AI technologies are revolutionizing systems pharmacology by enhancing model generation, parameter estimation, and predictive capabilities [104] [103]. Specific advances include the development of surrogate modeling to reduce computational complexity, virtual patient generation for robust clinical trial simulations, and digital twin technologies that create virtual representations of individual patients for treatment optimization [104]. The emerging concept of Quantitative Systems Pharmacology as a Service (QSPaaS) supported by AI-driven databases and cloud-based platforms promises to make these sophisticated approaches more accessible across the pharmaceutical industry [104].
The convergence of systems biology with regenerative medicine is creating new therapeutic paradigms through Integrative and Regenerative Pharmacology (IRP), which aims to restore physiological structure and function rather than merely managing symptoms [8]. This approach utilizes systems biology methodologies to define the mechanisms of action of advanced therapeutic medicinal products, including stem cell-derived therapies, accelerating their regulatory approval and clinical translation [8]. Furthermore, the development of smart biomaterials that can deliver bioactive compounds in a temporally controlled manner represents another frontier where systems biology approaches are enabling more precise therapeutic interventions [8].
Despite these promising developments, significant challenges remain in the widespread adoption of systems biology approaches. These include computational complexity, high dimensionality, model explainability, data integration barriers, and regulatory acceptance of model-based evidence [104]. Additionally, true multi-omics integration remains in its infancy, with genomic, transcriptomic, proteomic, and metabolomic datasets still suffering from incompatible formats and opaque sharing practices [103]. Addressing these limitations will require continued development of standardized, FAIR-compliant data pipelines and interdisciplinary collaboration across academia, industry, and regulatory agencies.
The comparative analysis reveals that systems biology approaches offer substantial advantages over traditional pharmacology in drug development efficiency, particularly through their ability to generate mechanistic insights, predict clinical outcomes, and enable patient stratification. By integrating multi-omics data into network models that capture the complexity of biological systems, these approaches address fundamental limitations of the reductionist paradigm that has dominated pharmaceutical research. The application of enhanced pharmacodynamic models, phosphoproteomic signaling analysis, and multi-scale network modeling is transforming key stages of the drug development pipeline from target identification to clinical trial design.
Within the context of personalized medicine research, systems biology provides the essential conceptual and methodological framework for understanding how individual variations in molecular networks influence therapeutic responses. This enables a shift from the traditional one-size-fits-all model to precisely targeted interventions based on individual patient characteristics. As these approaches continue to evolve through integration with artificial intelligence, digital twin technologies, and advanced therapeutic modalities, they hold the potential to fundamentally reshape pharmaceutical research and development, ultimately delivering more effective and personalized therapies to patients in a more efficient manner.
The convergence of advanced therapy medicinal products (ATMPs) and companion diagnostics (CDx) represents a frontier in precision oncology, necessitating equally advanced regulatory frameworks. Adaptive pathways, built on principles of iterative development and real-world evidence generation, are emerging as crucial models for facilitating patient access to these innovative therapies while ensuring safety and efficacy. This whitepaper examines the evolution of these regulatory pathways, their application to complex therapeutic areas, and the enabling role of systems biology in driving personalized medicine forward. As AI-based personalised drug and cell therapies advance, new regulatory thinking is required to address the challenges posed by these highly individualized treatments [105].
Conceptual Framework and Definitions
Adaptive pathways, also known as Medicines Adaptive Pathways to Patients (MAPPs) or adaptive licensing, represent a fundamental shift in how regulators evaluate novel therapies. This approach is defined as "a prospectively planned, flexible approach to regulation of drugs and biologics" that employs "iterative phases of evidence gathering to reduce uncertainties followed by regulatory evaluation and license adaptation" [106]. The European Medicines Agency (EMA) emphasizes that adaptive pathways is based on three core principles: (1) iterative development, beginning with a restricted patient population then expanding; (2) confirming benefit-risk balance following conditional approval based on early data; and (3) gathering evidence through real-life use to supplement clinical trial data [107].
This model acknowledges that therapeutic knowledge continues to accumulate after initial approval and that patient access is best served through repeated cycles of "learning-confirming-(re)licensing" rather than single, definitive approval decisions [106]. The approach is particularly suited to treatments in areas of high medical need where collecting data via traditional routes is difficult and where large clinical trials would unnecessarily expose patients unlikely to benefit [107].
Drivers for Regulatory Evolution
Multiple environmental factors are driving the transition toward adaptive regulatory frameworks:
- Patient Expectations: Growing pressure for timely access from increasingly informed and organized patient advocacy groups across multiple disease areas [106].
- Emerging Science: Increasing fragmentation of treatment populations based on molecular characteristics and the need for early disease interception [106].
- Healthcare System Pressures: Rising payer influence on product accessibility amid constrained budgets [106].
- Pharmaceutical Industry Sustainability: Need for more efficient drug development paradigms that de-risk development and ensure sustainability [106].
- Technological Acceleration: Rapid advances in AI-based therapy personalization that outpace traditional regulatory approaches [105].
Table 1: Conventional vs. Adaptive Regulatory Scenarios [106]
| Aspect | Conventional Scenario | Adaptive Licensing Scenario |
|---|---|---|
| Decision Framework | Single gated licensing decision | Life span management |
| Evidence Approach | Prediction based on pre-approval data | Monitoring and continual assessment |
| Study Designs | Primarily RCTs | Entire toolbox of evidence generation |
| Target Populations | Broad populations | Targeted populations |
| Primary Focus | Obtaining marketing authorization | Ensuring appropriate patient access |
| Market Utilization | Open utilization | Targeted utilization |
Companion Diagnostics: Evolution and Current Landscape
Definition and Regulatory Significance
Companion diagnostics (CDx) are defined as "in vitro diagnostic assay or imaging tools that provide information that is essential for the safe and effective use of a corresponding therapeutic product" [108]. The development of trastuzumab with its immunohistochemical assay HercepTest in 1998 marked the first instance where a molecular predictive assay was developed alongside a targeted drug specifically for patient selection [108]. This drug-diagnostics co-development model has proven crucial for targeted therapies that might otherwise demonstrate insufficient activity in unselected patient populations.
Regulatory bodies distinguish between companion diagnostics (CDx), where testing is obligatory for prescription, and complementary diagnostics (cDx), which provide optional additional information on enhanced benefits in subgroups [105]. The coordination between drug and diagnostic approval presents significant regulatory challenges, particularly in regions like the EU with fragmented assessment systems involving separate drug and device regulators [105].
Quantitative Analysis of CDx Growth
Between 1998 and the end of 2024, the FDA approved 217 new molecular entities (NMEs) for oncological and hematological malignancies, with 78 (36%) linked to one or more companion diagnostics [108]. The growth in CDx-linked approvals has been particularly notable after 2010, reflecting the increasing molecular stratification of cancer therapies.
Table 2: FDA-Approved NMEs with Companion Diagnostics (1998-2024) [108]
| Molecular/Therapeutic Class | Total NMEs Approved | NMEs with CDx | Percentage with CDx |
|---|---|---|---|
| Kinase Inhibitors | 80 | 48 | 60% |
| Antibodies | 44 | 17 | 39% |
| Small-molecule Drugs | 31 | 8 | 26% |
| Antibody-Drug Conjugates (ADC) | 12 | 3 | 25% |
| Advanced Therapy Medicinal Products (ATMP) | 12 | 1 | 8% |
| Chemotherapeutics | 20 | 0 | 0% |
| Radiopharmaceuticals | 5 | 0 | 0% |
| Others | 13 | 1 | 8% |
| Total | 217 | 78 | 36% |
For 52 (67%) of the 78 NMEs approved with a CDx assay, both the drug and CDx received approval simultaneously, while in the remaining 26 (33%), CDx was approved later through a supplemental process [108]. This highlights the regulatory challenge of synchronizing therapeutic and diagnostic approval timelines.
Tissue Agnostic Approvals and Regulatory Challenges
The tissue-agnostic approval paradigm represents a significant evolution in oncology drug regulation, where therapies are approved based on molecular biomarkers regardless of tumor origin. Among the 217 NMEs approved by the FDA since 1998, nine (4%) have received tissue-agnostic indications [108]. All these agents were associated with a CDx assay for patient selection during clinical development.
A critical challenge in this paradigm has been the synchronization of drug and diagnostic approvals. For eight of the nine tissue-agnostic drugs, approval of the CDx assay was significantly delayed compared to the drug approval date, with a mean delay of 707 days (range 0-1732 days) [108]. This approval misalignment creates practical challenges for implementing precision medicine in clinical practice.
Advanced Therapy Medicinal Products: Regulatory Complexities
Definition and Classification
Advanced Therapy Medicinal Products (ATMPs) are "medicines for human use that are based on genes, tissues, or cells as well as combinations" [105]. Most ATMPs are developed for cancer therapy, and they include cell therapies, gene therapies, and tissue-engineered products [105]. The field has expanded to include 12 FDA-approved NMEs in oncology and hematology as of 2024, representing 6% of all approvals in these categories [108].
ATMPs present unique regulatory challenges due to their complex nature, frequently individualized manufacturing processes, and often novel mechanisms of action. These therapies currently face substantial waiting times for approval in the US, and even longer timelines in the EU [105].
AI-Enabled Personalization of ATMPs
Emerging AI technologies are enabling new approaches for personalizing ATMP design and development. Realistic short-term advances include applications for personalized design and delivery of cell therapies [105]. With this acceleration in technical capabilities, the limiting step to clinical adoption will likely be the capacity and appropriateness of regulatory frameworks [105].
Several specific AI-enabled personalized oncology approaches have been proposed:
- Clinical Decision Support (CDS) Systems: Provide diagnosis and/or personalized treatment suggestions based on individual patient data [105].
- Precision Diagnostics - Companion Diagnostics (CDx) and Complementary Diagnostics (cDx): Evolving from chemical and genomic biomarkers to include AI-based image analysis and potentially Generalist Medical Artificial Intelligence (GMAI) approaches [105].
- Drug Companion Apps: Digital tools that support patients undergoing cancer treatment and enable monitoring for dose adaptation [105].
The regulatory classification of these AI-based tools varies significantly by jurisdiction, with the EU typically classifying them as at least moderate risk in-vitro diagnostic devices/medical devices, while the US may classify certain types as non-medical devices under specific conditions [105].
The Role of Systems Biology in Personalized Medicine and Regulatory Science
Systems Biology Foundations
Systems biology represents an interdisciplinary field that focuses on complex interactions within biological systems, aiming to understand how these interactions give rise to the function and behavior of living organisms [30]. This holistic approach involves integrating biology, computational modeling, and quantitative analysis to predict how biological systems respond to various stimuli [30]. By utilizing high-throughput technologies like genomics, proteomics, and metabolomics, systems biology provides a more detailed understanding of biological processes in health and disease.
The field is actively transforming healthcare from symptom-based diagnosis and treatment to precision medicine in which patients are treated based on their individual characteristics [13]. Development of high-throughput technologies such as high-throughput sequencing and mass spectrometry has enabled scientists and clinicians to examine genomes, transcriptomes, proteomes, metabolomes, and other omics information in unprecedented detail [13].
Applications in Personalized Medicine
Systems biology contributes to personalized medicine through several key applications:
Disease Mechanism Elucidation: By creating comprehensive models of biological processes, researchers can identify key regulatory networks and pathways involved in disease development [30]. In cancer treatment, systems biology helps identify specific genetic mutations and pathways driving tumor growth, enabling targeted drug development [30].
Biomarker Discovery and Validation: Systems biology facilitates discovery and validation of biomarkers by analyzing large-scale biological datasets [30]. The integrative Personal Omics Profile (iPOP) approach demonstrates how longitudinal monitoring of multiple omics can detect physiological state changes and enable early disease detection [13].
Drug Development and Optimization: By modeling how drugs interact with biological systems at the molecular level, researchers can predict efficacy and potential side effects of new therapies [30]. This approach helps streamline drug development by identifying promising candidates and optimizing dosing regimens.
Precision Medicine and Treatment Personalization: Analyzing a patient's genetic and molecular profile enables healthcare providers to select therapies most likely to be effective with the fewest side effects [30]. Pharmacogenomics, a field within systems biology, examines how genetic variations affect drug responses, allowing personalized dosing and drug selection [30].
Experimental Protocols and Methodologies
Integrative Personal Omics Profiling (iPOP)
The integrative Personal Omics Profile (iPOP) represents a comprehensive approach to personalized health monitoring that combines multiple omics technologies [13]. This methodology enables detailed tracking of an individual's physiological states over time and detection of subtle changes indicative of network perturbation.
Protocol Details:
- Genome Sequencing: Perform whole genome sequencing using multiple platforms (Illumina and Complete Genomics) and whole exome sequencing using multiple capture technologies (Agilent, Roche Nimblegen, and Illumina) to identify genetic predispositions and variants affecting drug response [13].
- Longitudinal Blood Sampling: Collect peripheral blood mononuclear cells (PBMCs) and serum at regular intervals (e.g., monthly) and during health status changes.
- Multi-Omic Analysis:
- Transcriptome: Profile gene expression patterns using RNA sequencing
- Proteome: Analyze protein expression using mass spectrometry
- Metabolome: Characterize metabolite profiles using mass spectrometry
- Data Integration: Combine genomic, transcriptomic, proteomic, and metabolomic data to create comprehensive physiological models.
- Dynamic Monitoring: Identify both trend changes (associated with gradual physiological changes) and spike changes (particular genes and pathways enriched during state transitions) [13].
- Clinical Correlation: Correlate omics findings with clinical parameters and health outcomes.
This approach successfully enabled early detection of Type 2 Diabetes onset in a research participant, allowing condition reversal through proactive interventions like diet change and physical exercise [13].
Companion Diagnostic Validation Protocol
The co-development of therapeutic products and companion diagnostics requires rigorous validation protocols to ensure analytical and clinical validity.
Protocol Details:
- Assay Development Phase:
- Identify biomarker target based on therapeutic mechanism of action
- Develop prototype assay with appropriate sensitivity and specificity parameters
- Establish preliminary cut-off values for positive/negative classification
Analytical Validation:
- Determine analytical sensitivity (limit of detection) and specificity
- Assess assay precision (repeatability and reproducibility)
- Evaluate interference and cross-reactivity potential
- Validate assay performance across intended sample types
Clinical Validation:
- Establish clinical sensitivity and specificity using well-characterized clinical specimens
- Correlate assay results with clinical response outcomes
- Define positive and negative predictive values in intended use population
- Validate assay performance in multicenter studies if applicable
Regulatory Submission Preparation:
- Compile analytical and clinical performance data
- Develop detailed instructions for use
- Establish quality control procedures and acceptance criteria
- Implement clinical trial assay harmonization if used across multiple sites
For tissue-agnostic therapies, additional validation is required across multiple tumor types to ensure consistent performance regardless of tissue origin [108].
Research Reagents and Essential Materials
The following table details key research reagents and materials essential for conducting studies in systems biology and companion diagnostic development for ATMPs.
Table 3: Essential Research Reagents for Systems Biology and CDx Development
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| High-Throughput Sequencing Kits | Whole genome and exome sequencing for genetic variant identification | Illumina sequencing platforms, Complete Genomics platforms, Agilent, Roche Nimblegen capture technologies [13] |
| Mass Spectrometry Reagents | Proteomic and metabolomic profiling to characterize protein and metabolite expression | LC-MS/MS systems, isotope-labeled internal standards, protein digestion kits [13] |
| Immunohistochemistry Assays | Tissue-based companion diagnostics for protein biomarker detection | HercepTest for HER2 detection, automated staining systems, validated antibody panels [108] |
| PCR and Digital PCR Reagents | Molecular companion diagnostics for genetic variant detection | FDA-approved CDx assays for BRAF, EGFR, KRAS mutations; quantitative PCR master mixes; probe-based detection chemistries [108] |
| Flow Cytometry Reagents | Immune monitoring for cell-based therapies and biomarker analysis | Fluorescently-labeled antibodies for immune cell profiling, viability dyes, intracellular staining kits [105] |
| Cell Culture Media and Reagents | ATMP manufacturing and expansion | Serum-free media formulations, cytokine supplements, activation reagents for CAR-T cells [105] |
| Bioinformatic Analysis Tools | Systems biology data integration and modeling | Multi-omics integration platforms, pathway analysis software, computational modeling environments [13] [30] |
Future Directions and Regulatory Considerations
Evolving Regulatory Frameworks
As AI-enabled personalized therapies advance, regulatory frameworks must adapt to address several critical challenges:
- Combination Product Classification: Current provisions for drug-device combinations are inadequate for emerging complex interactions between patient data, AI, and prescription, design, and adaptive dosing of medicines [105].
- Generalist Medical AI Models: GMAI and LLM system validation is challenging as they can invent data and have a near infinite range of inputs and outputs [105].
- Real-World Evidence Integration: Adaptive pathways increasingly incorporate real-world evidence gathered through clinical practice to supplement traditional clinical trial data [107].
- Stakeholder Collaboration: Early involvement of patients and health technology assessment bodies in development discussions is crucial for defining appropriate evidence requirements [107].
Systems Biology-Enabled Regulatory Science
The future of ATMP and companion diagnostic regulation will likely incorporate systems biology approaches in several ways:
- Quantitative Systems Pharmacology: Using computational models to understand drug action and optimize dosing strategies based on individual patient characteristics [30].
- Network-Based Biomarker Identification: Moving beyond single biomarkers to network-based signatures that better capture disease complexity and therapeutic response [13] [30].
- Digital Twins Concept: Creating computational models of individual patients to simulate treatment responses and optimize therapeutic strategies before implementation [105].
- Dynamic Treatment Optimization: Using continuous monitoring and model refinement to adjust therapies in response to changing patient biology [13].
The implementation of these advanced approaches will require ongoing dialogue between researchers, clinicians, regulators, and patients to ensure that regulatory evolution keeps pace with scientific advancement while maintaining appropriate safeguards for patient safety.
Adaptive regulatory pathways for companion diagnostics and ATMPs represent a necessary evolution in how we translate scientific advances into patient benefit. The integration of systems biology approaches provides the foundational methodology for understanding complex biological systems and developing truly personalized therapeutic strategies. As these fields continue to advance, regulatory science must similarly evolve to address the challenges posed by highly individualized therapies, AI-enabled treatment design, and the need for more efficient development pathways. Through continued collaboration across stakeholders and thoughtful implementation of adaptive approaches, we can accelerate the delivery of innovative therapies to patients while ensuring appropriate evaluation of safety and efficacy.
The fundamental challenge in modern healthcare, particularly in oncology and chronic disease management, lies in translating molecular-level understanding into predictable improvements in patient outcomes. Precision oncology, which aims to tailor treatments based on individual tumor molecular characterization, has demonstrated that knowing specific cancer mutations is necessary but insufficient for optimal therapeutic decisions due to the nonlinear and dynamic nature of genotype-phenotype relationships [109]. Systems biology addresses this complexity by studying the collective behavior of molecules within biological processes, enabling researchers to reconstruct system-level behaviors and quantitatively predict responses to perturbations such as targeted therapies [109]. This approach represents a paradigm shift from reductionist methods to a holistic framework that can model the emergent properties of biological systems.
The clinical implementation of this framework relies on sophisticated technological infrastructure. Leading medical institutions have established precision medicine initiatives that focus on creating cohesive programs for implementing genomic medicine and building bioinformatics infrastructure to support genetic research [48]. These initiatives recognize that preparing for routine patient genetic sequencing requires integrating clinical implementation with discovery science, enabling the merger of diverse data types—genomic, transcriptomic, proteomic, radiomic, and exposomic—with clinical phenotypic data to advance phenotype/genotype correlations [48]. This integration provides the foundational evidence for assessing clinical impact through systems biology approaches.
Key Quantitative Metrics for Assessing Clinical Impact
Evaluating the clinical impact of systems biology-driven approaches requires tracking specific, quantifiable metrics across multiple dimensions. The table below organizes the primary success indicators for clinical impact assessment in personalized medicine.
Table 1: Key Quantitative Metrics for Clinical Impact Assessment
| Metric Category | Specific Metric | Measurement Methodology | Clinical Significance |
|---|---|---|---|
| Treatment Efficacy | Objective Response Rate (ORR) | RECIST criteria (solid tumors) or disease-specific response criteria [109] | Direct measure of therapeutic effect on disease burden |
| Pathological Complete Response (pCR) | Histopathological examination of tumor tissue post-therapy [109] | Surrogate endpoint for long-term survival in certain cancers | |
| Patient Survival | Overall Survival (OS) | Time from treatment initiation to death from any cause [109] | Gold standard endpoint for clinical benefit |
| Progression-Free Survival (PFS) | Time from treatment initiation to disease progression or death [109] | Measures disease control while balancing toxicity | |
| Quality of Life | Patient-Reported Outcomes (PROs) | Validated instruments (e.g., EORTC QLQ-C30, PROMIS) [110] | Quantifies treatment impact from patient perspective |
| Treatment Toxicity Management | NCI Common Terminology Criteria for Adverse Events (CTCAE) [109] | Assesses safety profile and tolerability of interventions | |
| Healthcare Utilization | Hospitalization Rates | Electronic Health Record (EHR) analysis of admission frequency [110] [111] | Indicator of disease complications and care efficiency |
| Emergency Department Visits | EHR tracking of unplanned care encounters [110] [111] | Measures disease stability and outpatient management success |
These quantitative metrics provide the evidentiary foundation for evaluating whether systems biology-driven approaches translate into meaningful clinical benefits. The integration of these metrics into standardized assessment frameworks enables robust comparison across therapeutic strategies and patient populations.
Systems Biology Methodologies for Clinical Impact Assessment
Multi-Omic Data Integration and Analysis
The application of systems biology begins with comprehensive molecular characterization through multi-omic data integration. In prostate cancer, for example, large-scale profiling studies have characterized the molecular landscape defined primarily by structural variation in the form of gene fusion events (e.g., TMPRSS2-ERG) and copy number alterations affecting tumor suppressor genes like NKX3-1, PTEN, MAP3K7, and RB1 [112]. The analytical workflow for this integration follows a structured pipeline:
Table 2: Multi-Omic Data Integration Pipeline
| Processing Stage | Key Components | Research Reagent Solutions |
|---|---|---|
| Data Generation | Whole exome/genome sequencing, RNA sequencing, DNA methylation arrays, proteomic profiling [112] | Next-generation sequencing kits (Illumina), DNA extraction kits (Qiagen), microarray platforms (Affymetrix) |
| Computational Processing | Alignment to reference genome (GRCh38), variant calling, quality control metrics [48] | Broad Institute WARP pipelines, Genomic Analysis Toolkit (GATK), Amazon Web Services HealthOmics |
| Data Integration | Joint called variant files, harmonized data resources, cross-platform normalization [48] | Genomic & Bioinformatics Analysis Resource (GenBAR), ATAV analysis platform, cloud computing infrastructure |
| Model Building | Network reconstruction, dynamical modeling, patient-specific biomarker identification [109] | R/Bioconductor packages, Python scientific stack, Boolean network modeling tools |
Multi-Omic Data Integration Workflow
Dynamical Modeling of Signaling Networks
Dynamic systems modeling represents a core methodology in systems biology for predicting therapeutic responses. These models study biological processes at the systems level using statistical methods, network reconstruction, and mathematical modeling to reconstruct the often counterintuitive dynamic behavior of biological systems [109]. The methodology involves several critical components:
Ordinary Differential Equation (ODE) Models simulate the dynamic behavior of signaling networks by representing molecular interactions as rate equations. For example, modeling the EGFR-MAPK pathway can predict resistance mechanisms arising from feedback loops and network adaptations [109]. Boolean Network Models provide a logical framework for simulating large-scale regulatory networks, particularly useful when precise kinetic parameters are unavailable. These have been applied to model androgen receptor signaling in prostate cancer and its evolution toward treatment resistance [112].
Patient-Specific Network Biomarkers represent a key clinical application of these models. Rather than relying on static molecular measurements, these biomarkers use dynamical models of signaling networks calibrated to individual patient data, demonstrating greater prognostic value than conventional biomarkers [109]. The experimental protocol for developing these biomarkers involves: (1) Network topology reconstruction from literature and databases; (2) Parameter estimation using optimization algorithms and experimental data; (3) Model validation through perturbation experiments; and (4) Clinical calibration using patient-derived molecular and outcome data.
Signaling Network with Feedback
Research Reagent Solutions for Systems Biology
Implementing systems biology approaches requires specialized research reagents and computational tools. The table below details essential solutions for conducting systems biology research in clinical contexts.
Table 3: Essential Research Reagent Solutions for Clinical Systems Biology
| Reagent/Tool Category | Specific Examples | Function in Research |
|---|---|---|
| Next-Generation Sequencing | Illumina sequencing kits, Qiagen DNA extraction kits [112] | Generate multi-omic data (genome, transcriptome, epigenome) from clinical specimens |
| Single-Cell Analysis | 10X Genomics Chromium, BD AbSeq antibodies [113] | Resolve cellular heterogeneity in tumors and microenvironment |
| Computational Pipelines | Broad Institute WARP, GATK, ATAV analysis platform [48] | Process and analyze genomic data with clinical-grade reproducibility |
| Network Modeling Software | Boolean network tools, ODE/PDE modeling environments [109] [113] | Construct and simulate dynamical models of biological systems |
| Cloud Computing Infrastructure | Amazon Web Services HealthOmics, GenBAR [48] | Store, process, and integrate large-scale multi-omic datasets |
| Electronic Health Record Integration | Epic Systems, Athenahealth, Meditech Expanse [111] | Link molecular data with clinical phenotypes and outcomes |
Case Studies: Clinical Impact of Systems Biology Approaches
Prostate Cancer: From Molecular Landscape to Adaptive Therapy
Prostate cancer exemplifies the successful application of systems biology in clinical impact assessment. Research has established that the prostate cancer genome is characterized primarily by structural variation, including ETS-family gene fusions (e.g., TMPRSS2-ERG) and copy number alterations affecting tumor suppressor genes (NKX3-1, PTEN, RB1) [112]. This molecular understanding has enabled the development of commercially available molecular diagnostics (Decipher, Oncotype DX, Prolaris) that provide prognostic information beyond standard clinical parameters [112].
A particularly impactful application has been the development of adaptive therapy strategies for metastatic castration-resistant prostate cancer (mCRPC). This approach uses mathematical modeling of tumor evolutionary dynamics to determine treatment scheduling, aiming to maintain sensitive cell populations that suppress resistant clones [112]. Rather than continuous maximum tolerated dosing, adaptive therapy modulates treatment based on PSA levels as a biomarker of tumor burden, demonstrating improved outcomes in clinical studies [112].
The experimental protocol for adaptive therapy involves: (1) Establishing baseline tumor burden through PSA measurement; (2) Initiating therapy until a predefined response threshold is achieved; (3) Withholding treatment until tumor burden reaches a predetermined upper limit; (4) Re-initiating therapy while monitoring for resistance emergence; (5) Iteratively adjusting this cycle based on mathematical models of competitive suppression between sensitive and resistant cell populations.
Oncology: Overcoming Drug Resistance through Network Analysis
In precision oncology, systems biology approaches have proven invaluable for deciphering mechanisms of resistance to targeted therapies and identifying strategies to overcome them. Resistance may emerge through various mechanisms: alterations in the drug target itself (e.g., secondary EGFRT790M mutations in NSCLC), mutations in downstream molecules (e.g., RAS, RAF, PI3K during EGFR inhibitor therapy), or network adaptation mechanisms including feedback loops and activation of parallel bypass pathways [109].
Systems biology has identified combination therapy strategies that target these resistance mechanisms proactively. For example, the dual targeting of a receptor with drugs acting through different mechanisms (trastuzumab with pertuzumab or lapatinib) or combining drugs acting on different molecules along the same pathway (BRAF inhibitor with MEK inhibitor) has demonstrated improved efficacy in randomized controlled trials [109]. These combinations were identified through network analysis that modeled signal transduction pathways and their adaptive responses to perturbation.
The experimental protocol for identifying effective drug combinations involves: (1) Reconstruction of relevant signaling networks from proteomic and phosphoproteomic data; (2) Mathematical modeling of network dynamics under single-agent inhibition; (3) Identification of feedback mechanisms and bypass pathways that maintain network output; (4) In silico screening of combination therapies that disrupt these compensatory mechanisms; (5) Experimental validation in cell line and patient-derived model systems; (6) Clinical translation through biomarker-guided trial designs.
Overcoming Drug Resistance Through Systems Biology
Implementation Framework and Future Directions
The clinical implementation of systems biology approaches requires both technological infrastructure and methodological standardization. Leading institutions have established implementation frameworks that include: (1) Clinical genomics leadership through roles such as Chief Genomics Officer to coordinate implementation across clinical services; (2) Standardized genomic testing platforms such as comprehensive cancer panels (e.g., Columbia Combined Cancer Panel querying 586 genes) integrated into electronic health records; (3) Bioinformatics infrastructure for genomic data sharing and analysis; (4) Education programs to build institutional capacity in precision medicine [48].
Future methodological developments will likely focus on several key areas: novel computational methods that integrate deep learning with ODE or PDE models to provide efficient mechanisms for model fitting and prediction; multi-scale modeling that addresses biological questions through the integration of models and quantitative experiments across spatial and temporal scales; and single-cell modeling to understand stochastic dynamics, gene regulation, and cell response to stimuli [113]. These advancements will enhance the resolution and predictive power of systems biology approaches, further strengthening their role in clinical impact assessment.
The integration of health information technology (HIT) creates additional opportunities for enhancing chronic disease management through electronic health records, telehealth services, mobile health applications, and remote monitoring devices [110]. These technologies enable continuous assessment of patient outcomes beyond traditional clinical trial settings, providing real-world evidence of treatment efficacy and generating rich datasets for refining systems biology models.
Systems biology provides a powerful methodological framework for assessing clinical impact and treatment efficacy in oncology and chronic diseases. By moving beyond static molecular characterization to dynamic, network-level understanding of disease processes, this approach enables more accurate prediction of therapeutic responses and identification of effective combination strategies. The integration of multi-omic data with computational modeling, coupled with robust clinical implementation frameworks, positions systems biology as an essential component of personalized medicine research and practice. As methodological developments continue to enhance our ability to model biological complexity, systems biology approaches will play an increasingly central role in measuring and improving patient outcomes across the spectrum of human disease.
Conclusion
Systems biology is fundamentally reshaping the development and delivery of personalized medicine by providing a holistic, computational framework to understand disease complexity and individual patient variation. The integration of multi-omics data, AI, and QSP models enables a move from reactive, symptomatic treatment to proactive, mechanism-based intervention. While significant challenges in data integration, model translation, and workforce training remain, the path forward is clear. Success depends on sustained collaboration between academia and industry, the evolution of regulatory science, and a focus on making these advanced therapies accessible. The future will be driven by AI-powered predictive medicine, real-time molecular monitoring, and increasingly sophisticated, patient-centric therapeutic strategies that fully realize the promise of precision health.
References
- 1. A Systems-Based Paradigm-DrivenMulti-Target Drug ... [https://www.healthcare-bulletin.co.uk/article/network-pharmacology-a-systems-based-paradigm-drivenmulti-target-drug-discovery-development-3872/]
- 2. Leveraging network pharmacology for drug discovery [https://www.sciencedirect.com/science/article/pii/S259009862500017X]
- 3. Leveraging Network Target Theory for Efficient Prediction of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11923905/]
- 4. Artificial Intelligence and Network Medicine: Path to Precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12410635/]
- 5. A Guide to Conquer the Biological Network Era Using ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2020.00034/full]
- 6. Using both qualitative and quantitative data in parameter ... [https://www.nature.com/articles/s41467-018-06439-z]
- 7. CMU Researchers Build Personalized Models To Advance ... [https://www.cmu.edu/news/stories/archives/2025/may/cmu-researchers-build-personalized-models-to-advance-precision-cancer-care]
- 8. Unifying pharmacology, systems biology, and regenerative ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1729610/full]
- 9. SYSTEMS THERAPEUTICS [https://tri-institute.org/systems-therapeutics/]
- 10. Integrative Systems Pharmacology Program [https://www.nimh.nih.gov/about/organization/dnbbs/molecular-and-cellular-neuroscience-research-branch/integrative-systems-pharmacology-program]
- 11. The Grand Challenge for Integrative and Regenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3108500/]
- 12. Integrative and Organ Systems Pharmacology: A New ... [http://triggered.edina.clockss.org/ServeContent?rft_id=info:doi/10.1124/mi.4.2.1]
- 13. Systems Biology: Personalized Medicine for the Future? [https://pmc.ncbi.nlm.nih.gov/articles/PMC4076046/]
- 14. Systems Pharmacology [https://icahn.mssm.edu/research/systems-biology-center-ny/systems-pharmacology]
- 15. Systems Biology, Personalized Medicine, AI & the Future of ... [https://mindandmatter.substack.com/p/systems-biology-personalized-medicine]
- 16. AI-driven multi-omics integration in precision oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634751/]
- 17. Integrating Multi-Omics Data: Methods and Applications in ... [https://www.sciencedirect.com/science/article/pii/S2215017X25000657]
- 18. Lost in Translation: Turning Multi-omic Chaos into Clinical ... [https://www.precisionformedicine.com/blog/lost-in-translation-turning-multi-omics-chaos-into-clinical-clarity]
- 19. 多组å¦æ•´åˆï¼šå¼€è¾Ÿæ–°ç–—æ³•ä¸Žç”Ÿç‰©æ ‡å¿—ç‰©è¯†åˆ«çš„æ–°å¤©åœ° [https://wap.sciencenet.cn/blog-3516770-1510264.html?mobile=1]
- 20. 刘ç¦æ•™æŽˆå›¢é˜Ÿå¼€å‘å•ç»†èƒžå¤šæ¨¡æ€æ•´åˆç®—法的全é¢åŸºå‡†è¯„ä¼°å¹³å° [https://life.tongji.edu.cn/6f/1f/c12693a356127/page.htm]
- 21. SWITCH深度å¸ç¿’方法é©æ–°å¤šé«”å¸æ•´åˆåŠ©åŠ›ç²¾æº–醫療發展 [https://geneonline.news/switch%E6%B7%B1%E5%BA%A6%E5%AD%B8%E7%BF%92%E6%96%B9%E6%B3%95%E9%9D%A9%E6%96%B0%E5%A4%9A%E9%AB%94%E5%AD%B8%E6%95%B4%E5%90%88%E5%8A%A9%E5%8A%9B%E7%B2%BE%E6%BA%96%E9%86%AB%E7%99%82%E7%99%BC%E5%B1%95/]
- 22. å¼€å‘通用人工智能模型整åˆå¤šç»„å¦æ•°æ®ä¸ŽåŸºå› 组知识以æ示 ... [https://www.ebiotrade.com/newsf/2025-11/20251125085151436.htm]
- 23. 2025 Trends: Multiomics [https://www.genengnews.com/topics/omics/2025-trends-multiomics/]
- 24. å› ç¾Žçº³å…¨æ–°æŠ€æœ¯æŽ¨åŠ¨å¤šç»„å¦ç ”究é©æ–°ï¼ŒåŠ©åŠ›è§£é”更深入的生物 ... [https://www.illumina.com.cn/company/news-center/press-releases/2025/15da9928-16c1-453a-b908-a4469a1fc91c.html]
- 25. Notions of similarity for systems biology models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5862271/]
- 26. Optimal Paradigms for Quantitative Modeling in Systems ... [https://www.mdpi.com/2076-3417/14/22/10696]
- 27. Schedule for SysMod [https://www.iscb.org/cms_addon/conferences/ismbeccb2025/schedule/detailed?track=SysMod]
- 28. 2025 SysMod meeting @ ISMB/ECCB [https://sysmod.info/meetings/sysmod-2025/]
- 29. Systems biology and the discovery of diagnostic biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/mid/NIHMS259366/]
- 30. How is systems biology applied in personalized medicine? [https://synapse.patsnap.com/article/how-is-systems-biology-applied-in-personalized-medicine]
- 31. Machine Learning in Biomarker Discovery for Precision ... [https://esmed.org/machine-learning-in-biomarker-discovery-for-precision-medicine/]
- 32. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 33. Digital patient modeling identifies predictive biomarkers of ... [https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2025.1648559/full]
- 34. AI and the future of biomarker analysis in early R&D [https://www.drugtargetreview.com/article/190428/ai-and-the-future-of-biomarker-analysis-in-early-rd/]
- 35. MarkerPredict: predicting clinically relevant ... [https://www.nature.com/articles/s41540-025-00603-0]
- 36. Advancing Biomedical Data Visualization for ... [https://www.elucidata.io/blog/data-visualization-connecting-the-dots-in-biomedical-research]
- 37. A Primer in Biological Data Analysis and Visualization [https://www.pharmiweb.com/article/a-primer-in-biological-data-analysis-and-visualization]
- 38. QSP Summit 2025: A New Standard in the Future of Drug ... [https://www.certara.com/blog/qsp-summit-2025-a-new-standard-in-the-future-of-drug-development/]
- 39. The imperative of the person in personalized medicine [https://www.nature.com/articles/s43856-025-01218-6]
- 40. A Framework for Quantitative Systems Pharmacology ... [https://pubmed.ncbi.nlm.nih.gov/40111538/]
- 41. Systems immunology: When systems biology meets immunology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12447193/]
- 42. 2025 QSP Symposium [https://pharmacy.buffalo.edu/news-events/events/annual-events/quantitative-systems-pharmacology-symposium/quantitative-systems-pharmacology-symposium-2025.html]
- 43. Multi-omics integration and machine learning uncover ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06711-z]
- 44. EMitool: Explainable Multi-Omics Integration for Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12072579/]
- 45. COPS: A novel platform for multi-omic disease subtype ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1012275]
- 46. Explainable Multi-Omics Integration for Disease Subtyping [https://pubmed.ncbi.nlm.nih.gov/40362506/]
- 47. Comprehensive multi-omics and machine learning ... [https://www.nature.com/articles/s41598-025-09742-0]
- 48. 2025 Columbia Precision Medicine Initiative Newsletter [https://www.precisionmedicine.columbia.edu/news/2025-columbia-precision-medicine-initiative-newsletter]
- 49. Can Systems Biology Advance Clinical Precision Oncology? [https://pmc.ncbi.nlm.nih.gov/articles/PMC8699328/]
- 50. Case studies in rare disease small molecule discovery and ... [https://www.sciencedirect.com/science/article/abs/pii/S0960894X20305734]
- 51. Rare Genetic Diseases: Nature's Experiments on Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7229282/]
- 52. Evaluation of single-sample network inference methods for ... [https://www.nature.com/articles/s41540-024-00340-w]
- 53. Methods in quantitative biology—from analysis of single-cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150428/]
- 54. A case study of Memorial Sloan Kettering Cancer Center's ... [https://www.sciencedirect.com/science/article/abs/pii/S0277953623001466]
- 55. Standardizing experimental protocols [https://www.sciencedirect.com/science/article/abs/pii/S0958166908000773]
- 56. Liquid biopsy – a narrative review with an update on current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333414/]
- 57. Clinical application of singleâ€cell RNA sequencing in disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12576031/]
- 58. Representation learning enables robust single cell ... [https://www.nature.com/articles/s41598-025-20514-8]
- 59. Single-cell microRNA sequencing method comparison and ... [https://www.nature.com/articles/s41467-021-24611-w]
- 60. Systems biology and microbiome innovations for ... [https://www.nature.com/articles/s41540-025-00607-w]
- 61. Integrating Multi-Omics for Precision Medicine: 2025 Guide [https://lifebit.ai/blog/integrating-multi-modal-genomic-and-multi-omics-data-for-precision-medicine/]
- 62. 2025 Cybersecurity Year in Review, Part One: Breaches ... [https://www.aha.org/news/aha-cyber-intel/2025-10-07-2025-cybersecurity-year-review-part-one-breaches-and-defensive-measures]
- 63. Electronic health record market consolidation and implications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394940/]
- 64. Why Healthcare Data Security is Critical in 2025 and Beyond [https://www.onec1.com/blog/why-healthcare-data-security-is-critical-in-2025-and-beyond]
- 65. Quantitative Evaluation of Translational Medicine Based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5350927/]
- 66. A quantitative approach to the spread of variance in ... [https://www.nature.com/articles/s41598-022-09921-3]
- 67. Spatial Biology Market Analysis and Forecast, 2025-2035 [https://www.businesswire.com/news/home/20251124442495/en/Spatial-Biology-Market-Analysis-and-Forecast-2025-2035-Opportunities-in-AI-Bridging-the-Gap-Between-Routine-Pathology-and-Spatial-Omics-Technology-and-Partnerships-Boosting-Spatial-Biology---ResearchAndMarkets.com]
- 68. Artificial Intelligence in Clinical and Translational Science [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580936/]
- 69. Integrating translational and clinical research to advance ... [https://www.ddw-online.com/how-integrating-translational-and-clinical-research-can-advance-drug-development-37444-202510/]
- 70. BIOKDD 2025 highlights AI breakthroughs in bioinformatics [https://www.uab.edu/medicine/news/informatics/biokdd-2025-highlights-ai-breakthroughs-in-bioinformatics]
- 71. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 72. CONSORT 2025 statement: updated guideline for reporting ... [https://www.nature.com/articles/s41591-025-03635-5]
- 73. advancing systems biology and QSP education through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463889/]
- 74. The dawn of a new era: can machine learning and large ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12170689/]
- 75. Streamlining data-intensive biology with workflow systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC8631065/]
- 76. Playbook workflow builder: Interactive construction of ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1012901]
- 77. ATMP Development in 2025: Promise, Pressure, and the ... [https://www.cryoport.com/bio-blog-atmp-development-in-2025-promise-pressure-and-the-push-to-scale/]
- 78. Current challenges and future directions of ATMPs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274769/]
- 79. Skill Needs for ATMP Manufacturing: A Heatmap Tool [https://www.bioprocessintl.com/cell-therapies/skill-needs-for-advanced-therapy-medicinal-product-manufacturing-a-survey-report-and-proposed-skills-heatmap]
- 80. iGEM 2025/2026: Systems Biology in Biomedical ... [https://www.frontiersin.org/research-topics/73776/igem-20252026-systems-biology-in-biomedical-innovations-and-healthcare]
- 81. The clinical quality management system of advanced ... [https://www.sciencedirect.com/science/article/pii/S2329050125000804]
- 82. Advances in personalized medicine: translating genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12106117/]
- 83. Personalized Therapeutics: A Potential Threat to Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3378738/]
- 84. Systems Biology as an Integrated Platform for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3972654/]
- 85. Quantitative -omic data empowers bottom-up systems biology [https://www.sciencedirect.com/science/article/abs/pii/S0958166917302276]
- 86. Expanding our thought horizons in systems biology and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12341958/]
- 87. Bridging academia and industry: advancing systems ... [https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2025.1627214/full]
- 88. Geno4ME Study: implementation of whole genome ... [https://www.nature.com/articles/s41525-025-00508-1]
- 89. FDA use of Real-World Evidence in Regulatory Decision ... [https://www.fda.gov/science-research/real-world-evidence/fda-use-real-world-evidence-regulatory-decision-making]
- 90. Generating and using real-world data: A worthwhile uphill ... [https://www.sciencedirect.com/science/article/pii/S0092867424001788]
- 91. Regulatory Submissions with Real-World Evidence ... [https://www.fda.gov/news-events/speeches-fda-officials/regulatory-submissions-real-world-evidence-successes-challenges-and-lessons-learned-09232025]
- 92. Top 5 Trends in Real-World Data and ... [https://veranahealth.com/top-5-trends-in-real-world-data-and-real-world-evidence-for-2025/]
- 93. Emerging Technologies in Biomarker Discovery You ... [https://blog.crownbio.com/emerging-technologies-in-biomarker-discovery-you-should-know-about]
- 94. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 95. Regulatory and Payer Evaluation of Real-World Evidence [https://www.drugepi.org/dope/rwe-roundtable-2025]
- 96. The Drug Development Timeline: Why It Takes Over 10 Years [https://intuitionlabs.ai/articles/drug-development-timeline-explained]
- 97. Merging Systems Biology with Pharmacodynamics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3405973/]
- 98. Leveraging systems biology approaches in clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4034589/]
- 99. Computational systems biology in disease modeling and ... [https://www.nature.com/articles/s41540-022-00247-4]
- 100. Drug Discovery Workflow - What is it? [https://www.vipergen.com/from-target-to-therapy-a-comprehensive-overview-of-the-drug-discovery-workflow/]
- 101. Perspectives on computational modeling of biological systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11213628/]
- 102. Systems biology in drug discovery and development [https://www.sciencedirect.com/science/article/abs/pii/S1359644613003292]
- 103. Harnessing AI for Precision Medicine and Its Applications ... [https://www.sciencedirect.com/science/article/abs/pii/S0014299925009379]
- 104. Integrating artificial intelligence with quantitative systems ... [https://pubmed.ncbi.nlm.nih.gov/40774584/]
- 105. New regulatory thinking is needed for AI-based ... [https://www.nature.com/articles/s41698-024-00517-w]
- 106. From adaptive licensing to adaptive pathways - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6706805/]
- 107. Adaptive pathways | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/adaptive-pathways]
- 108. An analysis of FDA drug approvals for oncological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12507643/]
- 109. Can Systems Biology Advance Clinical Precision Oncology? - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8699328/]
- 110. Role of health information technology in enhancing chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12161299/]
- 111. Top Digital Solutions for Disease Management in 2025 [https://www.mahalo.health/insights/22-top-disease-management-alternatives-in-2025]
- 112. Systems biology successes and areas for opportunity in prostate cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12372069/]
- 113. Methodological developments in systems biology [https://www.nature.com/collections/chdbdhfibd]