Diseasome and Disease Networks: A Comprehensive Guide for Biomedical Research and Therapeutic Development
This article provides a comprehensive exploration of diseasome and disease network concepts, bridging foundational theory with cutting-edge applications in biomedical research and drug development.
Diseasome and Disease Networks: A Comprehensive Guide for Biomedical Research and Therapeutic Development
Abstract
This article provides a comprehensive exploration of diseasome and disease network concepts, bridging foundational theory with cutting-edge applications in biomedical research and drug development. We examine how network medicine approaches reveal hidden connections between diseases through shared genetic, molecular, and phenotypic pathways. The content covers methodological frameworks for constructing multi-modal disease networks, addresses critical challenges in rare disease research and clinical evidence generation, and validates approaches through case studies in autoimmune disorders, Alzheimer's disease, and heart failure. Designed for researchers, scientists, and drug development professionals, this resource demonstrates how network-based strategies accelerate therapeutic discovery, enhance patient stratification, and optimize clinical trial design across diverse disease areas.
Understanding the Diseasome: Foundations of Network Medicine and Disease Relationships
The diseasome is a conceptual framework within the field of network medicine that represents human diseases as an interconnected network, where nodes represent diseases and edges represent their shared biological or clinical characteristics [1] [2]. This paradigm represents a fundamental shift from traditional reductionist models toward a holistic understanding of disease pathobiology, capturing the complex molecular interrelationships that traditional methods often fail to recognize [2]. The foundational premise of the diseasome is that diseases manifesting similar phenotypic patterns or comorbidities frequently share underlying genetic architectures, molecular pathways, and environmental influences [3] [4].
The construction and analysis of disease networks have been revolutionized by the accumulation of large-scale, multi-modal biomedical data, enabling researchers to move beyond simple, knowledge-based associations to data-driven discoveries of novel disease relationships [5] [3]. By mapping these connections, the diseasome provides a powerful scaffold for uncovering common pathogenic mechanisms, predicting disease progression, optimizing therapeutic strategies, and fundamentally reclassifying human disease based on shared biology rather than symptomatic presentation alone [5] [1].
Theoretical Foundations and Network Principles
Core Architectural Components of a Diseasome Network
In a diseasome network, the basic architectural components are consistent with general network theory. Nodes represent distinct biological entities, which can span multiple scales—from molecular entities like genes, proteins, and metabolites to macroscopic entities like specific diseases or clinical phenotypes [2]. Edges, also called links, represent the functional interconnections between these nodes. The nature of these edges varies based on the network's specific focus and can represent physical protein-protein interactions, transcriptional regulation, enzymatic conversion, shared genetic variants, or phenotypic similarity [3] [2].
The complete set of relevant functional molecular interactions in human tissue is referred to as the human "interactome," which serves as the foundational layer upon which disease-specific networks are built [2]. The structure and dynamics of the interactome are crucial for understanding how localized perturbations can lead to specific disease manifestations and why certain diseases frequently co-occur.
Key Properties of Disease Networks
Disease networks exhibit several key topological properties that provide insights into disease biology. Modularity refers to the tendency of the network to form densely connected groups, or communities, of diseases. These modules often share common etiological, anatomical, or physiological underpinnings, such as immune dysfunction or metabolic disruption [5] [4]. Centrality measures, including degree (number of connections a node has), betweenness (how often a node lies on the shortest path between other nodes), and closeness (how quickly a node can reach all other nodes), help identify diseases that are major hubs within the network, potentially pointing to conditions with widespread systemic effects [5].
The degree distribution of many biological networks has been observed to follow a power-law, indicating a scale-free topology where a few nodes (hubs) have a very high number of connections while most nodes have only a few [5]. This property suggests that the failure of certain hub proteins or pathways may have disproportionately large consequences, leading to disease. Furthermore, the within-network distance (WiND), defined as the mean shortest path length among all links in the network, quantifies the overall closeness and potential functional integration of the entire disease network [5].
Methodological Framework for Diseasome Construction
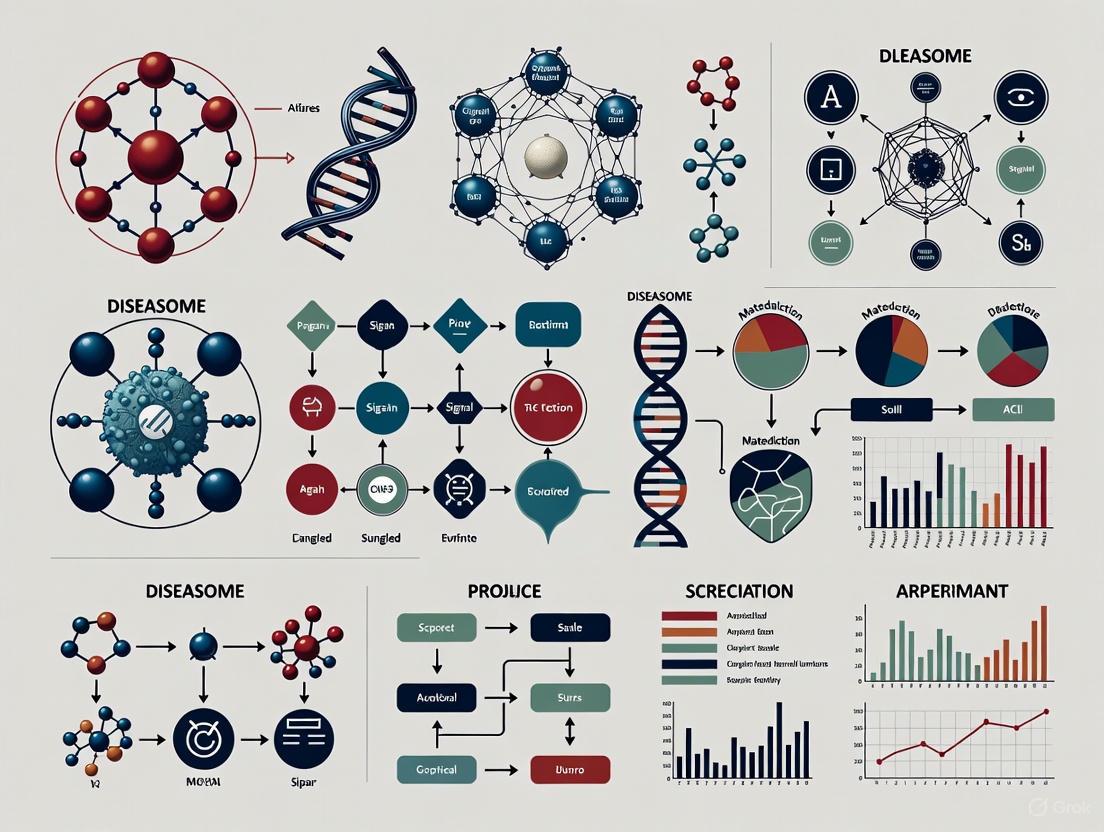
Constructing a comprehensive diseasome requires the integration of multi-scale data through a structured, hierarchical workflow. The following diagram outlines the core procedural stages.
Data Curation and Integration
The initial phase involves the systematic curation of disease terms and associated multi-modal data. A robust methodology, as demonstrated in recent autoimmune disease research, integrates disease terminologies from multiple biomedical ontologies and knowledge bases, including Mondo Disease Ontology (Mondo), Disease Ontology (DO), Medical Subject Headings (MeSH), and the International Classification of Diseases (ICD-11) [5]. Specialized disease databases, such as those from the Autoimmune Association (AA) and the Autoimmune Registry, Inc. (ARI), are also incorporated to ensure comprehensive coverage [5]. This process creates an integrated repository that can encompass hundreds of autoimmune diseases, autoinflammatory diseases, and associated conditions.
Table 1: Key Data Types for Multi-Modal Diseasome Construction
| Data Modality | Data Source Examples | Biological Insight Provided |
|---|---|---|
| Genetic | OMIM, GWAS, PheWAS summary statistics [3] [4] | Shared genetic susceptibility, pleiotropy, genetic correlations. |
| Transcriptomic | Bulk RNA-seq from GEO (e.g., GPL570), single-cell RNA-seq [5] | Gene expression dysregulation, cell-type specific pathways. |
| Phenotypic | Human Phenotype Ontology (HPO), Electronic Health Records (EHRs) [5] [4] | Clinical symptom and sign similarity, comorbidity patterns. |
| Proteomic & Metabolomic | PPI databases, mass spectrometry data, metabolomic profiles [6] [2] | Protein-protein interactions, metabolic pathway alterations. |
Calculation of Disease Similarity
A critical advancement in diseasome construction is the move beyond simple similarity measures to an Ontology-Aware Disease Similarity (OADS) strategy [5]. This approach leverages the hierarchical structure of biomedical ontologies to compute semantic similarity.
For genetic and transcriptomic data, disease-associated genes are mapped to Gene Ontology (GO) biological process terms. The functional similarity between diseases is then computed using methods like the Wang measure, which considers the semantic content of terms and their positions within the ontology graph [5]. For phenotypic data, terms from the Human Phenotype Ontology (HPO) are extracted, and similarity is again calculated using semantic measures [5] [4]. For cellular-level data from single-cell RNA sequencing (scRNA-seq), cell types are annotated using Cell Ontology, and similarity can be calculated with tools like CellSim [5]. The final OADS metric aggregates these cross-ontology similarities, providing a unified, multi-scale measure of disease relatedness.
Network Construction and Analysis
With pairwise disease similarity matrices calculated, disease-disease networks (DDNs) are constructed. A common method involves setting a similarity threshold, such as retaining edges where the similarity score exceeds the 90th percentile and is statistically significant (e.g., p < 0.05, validated through permutation testing) [5]. Networks are typically built and analyzed using Python libraries like NetworkX.
Community detection algorithms, such as the Leiden algorithm, are then applied to partition the network into robust disease modules or communities [5]. The biological significance of these communities is assessed by identifying over-represented phenotypic terms, dysfunctional pathways, and cell types within each cluster, often using Fisher's exact test [5]. Topological analysis further reveals hub diseases and the overall connectivity landscape of the diseasome.
Experimental Protocols for Diseasome Analysis
Protocol 1: Constructing a Shared-SNP Disease-Disease Network (ssDDN)
This protocol details the creation of a genetically-informed diseasome using summary statistics from phenome-wide association studies (PheWAS) [3].
- Data Preparation: Obtain PheWAS summary statistics from a large biobank (e.g., UK Biobank). For binary diseases, ensure a sufficient case count (e.g., >1000 cases) to ensure statistical power. Filter out hyper-specific disease codes and hierarchically related diseases with highly correlated case counts to avoid redundant signals [3].
- Variant Filtering: Restrict the analysis to a unified set of high-quality SNPs, such as HapMap3 SNPs, to ensure consistency. Remove SNPs in regions with complex linkage disequilibrium (LD), like the major histocompatibility complex (MHC) [3].
- Edge Definition: For each pair of diseases, identify the set of shared SNPs that pass a pre-defined genome-wide significance threshold (e.g., p < 5 × 10⁻⁸) in both PheWAS. An edge is established between two diseases if the number or significance of shared SNPs suggests a genetic correlation beyond what is expected by chance [3].
- Network Augmentation (ssDDN+): To enhance interpretability, incorporate quantitative endophenotypes. Calculate genetic correlations between diseases and clinical laboratory measurements (e.g., HDL cholesterol, triglycerides) using methods like Linkage Disequilibrium Score Regression (LDSC). Introduce new edges between diseases that share significant genetic correlations with the same intermediate biomarker [3].
Protocol 2: Building a Phenotype-Based Diseasome via Text Mining
This protocol outlines the generation of a diseasome based on phenotypic similarities derived from the biomedical literature [4].
- Corpus Creation: Build a text corpus from millions of Medline article titles and abstracts.
- Entity Co-occurrence Identification: Use semantic text-mining to identify co-occurrences between disease names (from ontologies like DO) and phenotype names (from HPO and the Mammalian Phenotype Ontology, MP) within the corpus [4].
- Significance Scoring: Score each disease-phenotype co-occurrence using multiple statistical measures, such as Normalized Pointwise Mutual Information (NPMI), T-Score, and Z-Score. Rank the phenotypes associated with each disease by their NPMI score [4].
- Phenotype Set Optimization: Determine the optimal number of top-ranked phenotypes to associate with each disease by evaluating the set's power to identify known disease-associated genes in model organisms or humans. This is typically done by computing the area under the receiver operating characteristic curve (ROCAUC) [4].
- Similarity Calculation and Network Generation: Compute pairwise phenotypic similarity between all diseases using a semantic similarity measure. Construct the network by connecting diseases with a similarity score above a chosen threshold.
Key Analytical Tools and Visualization Platforms
The analysis and visualization of diseasome networks require specialized software tools. The table below summarizes essential platforms for researchers.
Table 2: Essential Software Tools for Diseasome Research
| Tool Name | Type | Primary Function in Diseasome Research |
|---|---|---|
| Cytoscape [7] | Desktop Software | Primary Function: Open-source platform for visualizing complex networks and integrating them with attribute data. Use Case: Visual exploration, custom styling, and plugin-based analysis (e.g., network centrality, clustering) of disease networks. |
| Gephi [8] | Desktop Software | Primary Function: Open-source software for network visualization and manipulation. Use Case: Applying layout algorithms (Force Atlas, Früchterman-Reingold), calculating metrics, and creating publication-ready visualizations of large disease networks. |
| NetworkX [5] | Python Library | Primary Function: A Python package for the creation, manipulation, and study of the structure, dynamics, and functions of complex networks. Use Case: Programmatic construction of disease networks, calculation of topological properties (degree, betweenness), and implementation of network algorithms. |
| powerlaw Library [5] | Python Library | Primary Function: A toolkit for testing if a probability distribution follows a power law. Use Case: Fitting and validating the scale-free properties of a constructed diseasome network. |
The following diagram illustrates a typical workflow integrating these tools for diseasome analysis, from data processing to biological insight.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Resources for Diseasome Studies
| Resource Category | Specific Examples | Function in Diseasome Research |
|---|---|---|
| Biomedical Ontologies | Gene Ontology (GO), Human Phenotype Ontology (HPO), Cell Ontology (CL), Disease Ontology (DO) [5] [4] | Provide standardized, hierarchical vocabularies for consistent annotation of genes, phenotypes, cells, and diseases, enabling semantic similarity calculations. |
| Bioinformatics Software/Packages | Seurat (for scRNA-seq processing) [5], DCGL (for differential co-expression analysis) [5], RDKit (for drug structural similarity) [5], LDSC (for genetic correlation) [3] | Perform critical data processing and analytical steps on raw molecular and clinical data to generate inputs for network construction. |
| Molecular Interaction Databases | Protein-protein interaction databases, PhosphoSite (post-translational modifications), JASPAR (transcription factor binding) [2] | Provide curated knowledge on molecular interactions (edges) to build the foundational human interactome. |
| Biobanks & Cohort Data | UK Biobank [3] [6], Human Phenotype Project (HPP) [6], All of Us [6] | Supply large-scale, deep-phenotyped data linking genetic, molecular, clinical, and lifestyle data from hundreds of thousands of participants, serving as a primary data source. |
The diseasome paradigm, powered by network medicine principles and multi-modal data integration, provides a transformative framework for understanding human disease. By systematically mapping the intricate web of relationships between diseases across genetic, transcriptomic, cellular, and phenotypic scales, it moves beyond organ-centric or symptom-based classifications to a etiology-driven disease taxonomy. The methodologies outlined—from ontology-aware similarity scoring to the construction of genetically-augmented and phenotypically-derived networks—provide researchers with a robust toolkit for uncovering the shared pathobiological pathways that underlie disease comorbidities. As large-scale biobanks and deep phenotyping initiatives continue to grow, the refinement and application of the diseasome will be instrumental in advancing biomarker discovery, identifying novel drug repurposing opportunities, and ultimately paving the way for more personalized and effective therapeutic strategies.
Historical Evolution of Disease Network Concepts and Key Milestones
The concept of the diseasome represents a paradigm shift in how we understand human pathology, moving from a siloed view of diseases to a comprehensive network-based model. In this framework, diseases are not independent entities but interconnected nodes in a vast biological network, where connections represent shared molecular foundations, including common genetic origins, overlapping metabolic pathways, and related environmental influences [9]. This approach is particularly valuable for understanding complex multimorbidities—the co-occurrence of multiple diseases in individuals—which exhibit patterned relationships rather than random associations [3]. The field of network medicine has emerged as the discipline dedicated to studying these disease relationships through network science principles, with the goal of uncovering the fundamental organizational structure of human disease [9].
The theoretical foundation of disease networks rests on several key principles. First, disease-associated proteins have been shown to physically interact more frequently than would be expected by chance, suggesting that diseases manifest from the perturbation of functionally related modules within complex cellular networks [9]. Second, the "disease module" hypothesis proposes that the cellular components associated with a specific disease are localized in specific neighborhoods of molecular networks [9]. Third, pleiotropy (where one genetic variant influences multiple phenotypes) and genetic heterogeneity (where multiple variants lead to the same disease) are not exceptions but fundamental features of the genetic architecture of complex diseases, creating intricate cross-phenotype associations [3].
Historical Evolution and Key Theoretical Milestones
The historical development of disease network concepts can be traced through several pivotal milestones that have progressively shaped our understanding of disease relationships. These developments have transitioned from early database-driven approaches to contemporary data-intensive methodologies that leverage large-scale biomedical data.
Table 1: Key Milestones in Disease Network Research
| Time Period | Key Development | Significance | Primary Data Source |
|---|---|---|---|
| Pre-2000 | Early Disease Nosology | Categorical classification of diseases based on symptoms and affected organs | Clinical observation |
| 2007 | First Diseasome Map | Demonstrated that disease genes form a highly interconnected network | Online Mendelian Inheritance in Man (OMIM) |
| 2010-Present | PheWAS-enabled Networks | Unbiased discovery of disease connections using EHR-linked biobanks | Electronic Health Records, Biobanks |
| 2015-Present | Integration of Endophenotypes | Added quantitative traits as intermediaries in disease networks | Laboratory measurements, Biomarkers |
| 2020-Present | AI and Transformer Models | Generative prediction of disease trajectories across lifespan | Population-scale health registries |
The earliest network approaches relied on manually curated databases to construct networks based on shared disease-associated genes or common symptoms [3] [9]. A seminal 2007 study by Goh et al. introduced the first human "diseasome" map by linking diseases based on shared genes, providing visual proof of the interconnected nature of human diseases [3]. This established the foundation for disease-disease networks (DDNs), where nodes represent diseases and edges represent shared biological factors [3].
The rise of electronic health record (EHR)-linked biobanks in the 2010s enabled a less biased approach to modeling multimorbidity relationships through phenome-wide association studies (PheWAS) [3]. This methodology identified thousands of associations between genetic variants and phenotypes, allowing for the construction of shared-single nucleotide polymorphism DDNs (ssDDNs) where edges represent sets of significant SNPs shared between diseases [3]. More recently, the integration of quantitative endophenotypes (intermediate phenotypes like laboratory measurements) has created augmented networks (ssDDN+) that better explain the genetic architecture connecting diseases, particularly for cardiometabolic disorders [3].
The most recent evolution involves artificial intelligence approaches, particularly transformer models adapted from natural language processing. These models, such as Delphi-2M, treat disease histories as sequences and can predict future disease trajectories by learning patterns from population-scale data [10]. This represents a shift from static network representations to dynamic, predictive models of disease progression.
Fundamental Methodologies in Disease Network Research
Constructing disease networks requires integrating diverse data types through standardized methodologies. The primary data sources include genetic association data from PheWAS, which identifies connections between genetic variants and diseases; clinical laboratory measurements that serve as quantitative endophenotypes; protein-protein interaction networks that provide the physical infrastructure for disease module identification; and structured disease ontologies like the Human Phenotype Ontology (HPO) that enable computational representation of phenotypic relationships [3] [9].
The shared-SNP DDN (ssDDN) construction methodology involves several key steps. First, researchers obtain PheWAS summary statistics from large biobanks (e.g., UK Biobank), typically restricting to HapMap3 SNPs while excluding the major histocompatibility complex region due to its complex linkage disequilibrium structure [3]. For each disease, SNPs surpassing genome-wide significance thresholds (typically p < 5×10^(-8)) are identified. An edge is created between two diseases if they share a predetermined number of significant SNPs (often ≥1), with edge weights potentially reflecting the number of shared SNPs or the strength of genetic correlations [3].
The augmented ssDDN+ methodology extends this approach by incorporating quantitative traits as intermediate nodes. Researchers calculate genetic correlations between diseases and laboratory measurements using methods like linkage disequilibrium score regression (LDSC), which analyzes PheWAS summary-level data while accounting for linkage disequilibrium patterns across the genome [3]. In this enhanced network, connections are established not only through direct SNP sharing but also through shared genetic correlations with biomarkers such as HDL cholesterol and triglycerides, which have been shown to connect multiple cardiometabolic diseases [3].
Key Analytical Techniques
Several network analysis techniques have been specifically adapted for disease network research. Network propagation (also called network diffusion) approaches identify disease-related modules from initial sets of "seed" genes associated with a disease [9]. These methods detect topological modules enriched in seed genes, allowing researchers to filter false positives, predict new disease-associated genes, and relate diseases to specific biological functions [9].
The disease module identification process follows a standardized workflow. Researchers begin with seed genes known to be associated with a disease through genotypic or phenotypic evidence. These seeds are mapped onto molecular networks, and algorithms identify network neighborhoods enriched in these seeds. The resulting modules are then validated for functional coherence and tested for association with relevant biological pathways and processes [9].
Multi-layer network integration has emerged as a powerful approach for combining different data types. Researchers construct networks with different node and edge types (e.g., genes, diseases, phenotypes) and develop integration frameworks to identify conserved patterns across network layers. These integrated networks have proven particularly valuable for identifying robust disease modules and understanding the multidimensional nature of complex diseases [9].
Experimental Protocols and Methodological Standards
Protocol 1: Construction of a Shared-SNP Disease-Disease Network
This protocol details the methodology for constructing a shared-SNP disease-disease network (ssDDN) from biobank-scale data, adapted from studies using UK Biobank data [3].
Sample Processing and Quality Control: Begin with genetic and phenotypic data from a large, EHR-linked biobank. For the UK Biobank, this involves approximately 400,000 British individuals of European ancestry. Perform quality control on genetic data, excluding SNPs with high missingness rates, deviation from Hardy-Weinberg equilibrium, or low minor allele frequency. For phenotypes, map EHR diagnoses to a standardized vocabulary like phecodes, excluding phenotypes with fewer than 1000 cases to ensure sufficient statistical power [3].
Genetic Association Testing: Conduct a PheWAS using appropriate software (e.g., SAIGE for binary traits) that accounts for population stratification, relatedness, and covariates including sex, age, and genetic principal components. For each phecode-labeled phenotype, test associations with millions of imputed SNPs, applying standard genome-wide significance thresholds (p < 5×10^(-8)) [3].
Network Construction and Validation: Create the ssDDN by connecting diseases that share significant SNPs, applying filters to remove spurious connections. Validate the network by checking if known multimorbidities are recovered and through enrichment analysis of shared biological pathways between connected diseases. Perform robustness testing through bootstrap resampling or edge permutation [3].
Protocol 2: Disease Trajectory Prediction with Transformer Models
This protocol outlines the methodology for training transformer models to predict disease progression, based on the Delphi model architecture [10].
Data Preprocessing and Tokenization: Extract longitudinal health records including disease diagnoses (coded as ICD-10 codes), demographic information (sex, age), lifestyle factors (BMI, smoking status, alcohol consumption), and mortality data. Represent each individual's health trajectory as a sequence of tokens, where each token represents a diagnosis at a specific age, plus special tokens for "no event" periods, lifestyle factors, and death. For time representation, replace standard positional encoding with continuous age encoding using sine and cosine basis functions [10].
Model Architecture and Training: Implement a modified GPT-2 architecture with three key extensions: (1) continuous age encoding instead of discrete positional encoding, (2) an additional output head to predict time-to-next token using an exponential waiting time model, and (3) amended causal attention masks that also mask tokens recorded at the same time. Partition data into training (80%), validation (10%), and test (10%) sets. Train the model using standard language modeling objectives but adapted for disease prediction [10].
Model Validation and Interpretation: Validate the model by assessing its calibration and discrimination for predicting diverse disease outcomes across different age groups and demographic subgroups. Use external validation datasets when possible (e.g., Danish registries for the Delphi model). Apply explainable AI methods to interpret predictions and identify clusters of co-morbidities and their time-dependent consequences on future health [10].
Visualization of Disease Network Concepts
Diseasome Network Architecture
The following diagram illustrates the fundamental architecture of disease networks, showing the relationships between different biological scales and disease associations.
Diseasome Network Architecture
ssDDN+ Construction Workflow
This diagram outlines the comprehensive workflow for constructing an augmented shared-SNP disease-disease network with endophenotypes (ssDDN+).
ssDDN+ Construction Workflow
Quantitative Findings and Research Applications
Key Genetic Correlations in Disease Networks
Research using ssDDN+ methodology has revealed specific quantitative relationships between endophenotypes and disease connections. These findings highlight the importance of quantitative biomarkers in explaining shared genetic architecture between complex diseases.
Table 2: Key Endophenotype-Disease Connections in ssDDN+ Networks
| Endophenotype | Most Strongly Connected Diseases | Number of Diseases Connected | Key Genetic Findings |
|---|---|---|---|
| HDL Cholesterol | Type 2 Diabetes, Heart Failure | Greatest number of diseases | Strongest genetic correlation with cardiometabolic diseases |
| Triglycerides | Cardiovascular Disease, Metabolic Syndrome | Substantial number | Adds significant edges to ssDDN+ |
| LDL Cholesterol | Coronary Artery Disease, Atherosclerosis | Multiple connections | Shared loci with vascular diseases |
| Fasting Glucose | Type 2 Diabetes, Metabolic Disorders | Significant connections | Reveals shared metabolic pathways |
Studies have demonstrated that HDL cholesterol connects the greatest number of diseases in augmented networks and shows particularly strong genetic correlations with both type 2 diabetes and heart failure [3]. Triglycerides, another blood lipid with known genetic causes in non-mendelian diseases, also adds a substantial number of edges to the ssDDN+, revealing previously unrecognized connections between metabolic and inflammatory disorders [3].
Performance Metrics for Disease Prediction Models
The evolution of disease network concepts has enabled increasingly sophisticated prediction models. Recent transformer-based approaches like Delphi-2M have demonstrated significant improvements in predicting disease trajectories across diverse conditions.
Table 3: Performance Metrics for Disease Prediction Models
| Model Type | Average AUC | Diseases Covered | Time Horizon | Key Advantages |
|---|---|---|---|---|
| Single-Disease Models | Variable by disease | 1 disease | Short-term | Disease-specific optimization |
| Traditional Multimorbidity Models | 0.65-0.75 | Dozens of diseases | Medium-term | Captures basic comorbidities |
| Delphi-2M Transformer | ~0.76 | >1,000 diseases | Up to 20 years | Comprehensive disease spectrum, generative capabilities |
The Delphi-2M model achieves an average age-stratified area under the receiver operating characteristic curve (AUC) of approximately 0.76 across the spectrum of human disease in internal validation data [10]. This performance is comparable to existing single-disease models but with the advantage of predicting over 1,000 diseases simultaneously based on previous health diagnoses, lifestyle factors, and other relevant data [10].
Successful disease network research requires specific computational resources, data tools, and analytical frameworks. The following table summarizes key resources mentioned in the literature.
Table 4: Essential Research Reagent Solutions for Disease Network Studies
| Resource Category | Specific Tools/Databases | Primary Function | Key Applications |
|---|---|---|---|
| Biobank Data | UK Biobank, Danish Disease Registry | Large-scale genetic and phenotypic data | Network construction, model training, validation |
| Phenotype Ontologies | Human Phenotype Ontology (HPO), ICD-10 | Standardized disease and phenotype coding | Data harmonization, cross-study comparisons |
| Genetic Analysis Tools | SAIGE, Hail, LDSC | Genetic association testing, correlation analysis | PheWAS, genetic correlation estimation |
| Network Analysis Platforms | Cytoscape, NetworkX, igraph | Network construction, visualization, analysis | Module identification, topology analysis |
| AI/ML Frameworks | PyTorch, TensorFlow | Deep learning model implementation | Transformer models, predictive analytics |
The UK Biobank has been particularly instrumental in disease network research, providing PheWAS summary statistics for 400,000 British individuals with 1,403 phecode-labeled phenotypes and 31 quantitative biomarker measurements [3]. The Human Phenotype Ontology (HPO) offers a standardized vocabulary for phenotypic abnormalities with hierarchical relationships, enabling computational analysis of disease phenotypes and their similarities [9].
Specialized computational tools include SAIGE for genetic association testing of binary traits, LDSC for estimating genetic correlations, and network propagation algorithms for identifying disease modules in molecular networks [3] [9]. Recent transformer-based approaches like Delphi-2M require modified GPT architectures with continuous age encoding and additional output heads for time-to-event prediction [10].
Future Directions and Research Challenges
The field of disease network research continues to evolve with several emerging trends and persistent challenges. Multi-omics integration represents a frontier where genetic, transcriptomic, proteomic, and metabolomic data are combined into unified network models to capture the full complexity of disease mechanisms [9]. Temporal network modeling is advancing beyond static representations to dynamic networks that capture how disease relationships evolve over time and across the lifespan [10]. The integration of artificial intelligence with network medicine is producing powerful hybrid approaches that combine the pattern recognition capabilities of deep learning with the biological interpretability of network models [11] [10].
Significant challenges remain in data harmonization across heterogeneous sources, requiring improved ontological frameworks and data standards [9]. Computational scalability continues to be tested as networks grow to incorporate millions of nodes and edges, necessitating more efficient algorithms and computing infrastructure [12]. The field also grapples with translational gaps between network discoveries and clinical applications, particularly in drug development and personalized medicine interventions [3] [9].
Future research directions highlighted in recent literature include developing more sophisticated visualization tools for biological networks that move beyond schematic node-link diagrams to incorporate advanced network analysis techniques [12]. There is also growing interest in fairness and bias mitigation in disease network models, particularly as they increasingly inform clinical decision-making [10]. Finally, researchers are working toward clinical implementation frameworks that can translate network-based risk predictions into actionable interventions for personalized healthcare [11] [10].
The application of graph theory has fundamentally transformed the study of complex biological systems, providing a powerful framework for modeling and analyzing intricate relationships. In biomedical contexts, network medicine has emerged as a distinct discipline that understands human diseases from a network theory perspective [1]. This approach has proven particularly intuitive and powerful for revealing hidden connections among seemingly unrelated biomedical entities, including diseases, physiological processes, signaling pathways, and genes [1]. The structural analysis of disease networks has created significant opportunities in drug repurposing, addressing the high costs and prolonged timelines of traditional drug development by identifying new therapeutic applications for existing compounds [1]. Within this paradigm, network topology—the arrangement of nodes and edges within a network—provides essential insights into the organizational principles of biomedical systems that would remain obscured through reductionist approaches alone.
Core Topological Properties
Network topology describes the arrangement of nodes and edges within a network, with specific properties applying to the network as a whole or to individual components [13]. Understanding these properties is essential for unraveling the complex information contained within biomedical networks.
Fundamental Properties and Definitions
Nodes and Edges: In graph-theoretic modeling, a graph comprises a set of nodes (vertices) representing entities, and links (edges) connecting pairs of nodes [14]. In biomedical contexts, nodes typically represent biological concepts such as genes, proteins, or diseases, while edges represent relationships or interactions between them.
Node Degree: The degree of a node is the number of edges that connect to it, serving as a fundamental parameter that influences other characteristics such as node centrality [13]. The degree distribution of all nodes in a network helps determine whether a network is scale-free [13]. In directed networks, nodes have two degree values: in-degree for edges entering the node and out-degree for edges exiting the node [13].
Shortest Paths: The shortest path represents the minimal distance between any two nodes and models how information flows through networks [13]. This property is particularly relevant in biological networks where signaling pathways and disease propagation follow path-dependent routes.
Clustering Coefficient: This measure quantifies the level of clustering in a graph at the local level, calculated for a given node by counting the number of links between the node's neighbors divided by all their possible links [14]. This results in a value between 0 and 1, which is then averaged across all nodes in a network.
Average Path Length: Also called the "average shortest path," this metric refers to the average distance between any two nodes in the network [14]. The diameter represents the longest distance between any two nodes in the network [14].
Key Network Topologies in Biomedical Contexts
Scale-Free Networks: In scale-free networks, most nodes connect to a low number of neighbors, while a small number of high-degree nodes (hubs) provide high connectivity to the entire network [13]. These networks exhibit a power law distribution in node degrees, where a few nodes have many neighbors while most nodes have only a few [14]. This architecture promotes flexible navigation and less restrictive organic-like growth in comprehensive medical terminologies [14].
Small-World Networks: Networks with small-world properties feature highly clustered neighborhoods while maintaining the ability to move from one node to another in a relatively small number of steps [14]. This combination of strong local clustering and short global separation characterizes many biological systems where functional modules operate efficiently within larger networks.
Transitivity and Clusters: Transitivity relates to the presence of tightly interconnected nodes called clusters or communities—groups of nodes that are more internally connected than they are with the rest of the network [13]. These topological clusters often represent functional modules in biological systems, such as protein complexes or coordinated metabolic pathways.
Experimental Framework for Topological Analysis
The methodology for conducting topological analysis of biomedical terminologies involves specific protocols for data extraction, network modeling, and statistical comparison.
Terminology Selection and Data Extraction
In a landmark study analyzing 16 biomedical terminologies from the UMLS Metathesaurus, researchers selected source vocaburies covering varied domains to form a balanced selection of larger terminologies [14]. To enhance interpretability, they chose source vocabularies familiar to the terminological research community and included related terminology sets for contrastive purposes (ICD9CM and ICD10; SNOMEDCT, SNMI, and RCD) [14]. The extraction process utilized the MetamorphoSys program with the RRF (Rich Release Format) to ensure source transparency—the ability to see terminologies in a format consistent with that obtainable from the terminology's authority [14]. After importing selected tables into a relational database, researchers queried the MRREL table to select links assigned by each terminology, excluding concepts with no associated relationships (isolates) as they don't contribute meaningful information to statistical measures [14].
Network Modeling and Measurements
Each terminology was modeled as a graph where concepts represented nodes and links were assigned between concept pairs appearing in MRREL [14]. To facilitate comparison of large-scale structure, researchers simplified networks by treating all link types equally and disregarding directionality [14]. For each terminology network, the study calculated specific measurements shown in Table 1.
Table 1: Key Topological Measurements in Network Analysis
| Measurement | Description | Calculation Method | Interpretation in Biomedical Context |
|---|---|---|---|
| Average Node Degree | Average number of links per node | (Number of links × 2) / Number of nodes | Measure of graph density; indicates relationship richness in terminologies |
| Node Degree Distribution | Distribution of connectivity across nodes | Scatterplot with node degree (log) vs. frequency (log) | Identifies scale-free properties through power law distribution |
| Average Path Length | Average shortest distance between node pairs | Average of minimum distances between all node pairs | Indicates efficiency of information flow; shorter paths suggest small-world properties |
| Diameter | Longest distance between any two nodes | Maximum of all shortest paths | Reveals maximal conceptual separation in terminology |
| Clustering Coefficient | Level of local clustering | Average of node-level clustering coefficients (0-1) | Quantifies modular organization; higher values indicate strong local connectivity |
Statistical Comparison with Random Controls
To confirm statistically significant differences in topological parameters, the methodology created three random networks per terminology network of equivalent size and density [14]. This controlled comparison allowed researchers to distinguish meaningful topological features from random arrangements, with average path length and diameter measures being particularly stable across randomizations [14].
Quantitative Analysis of Biomedical Terminology Networks
Comprehensive topological analysis of large-scale biomedical terminologies has revealed distinct structural patterns with significant implications for terminology design and maintenance.
Topological Findings from Terminology Analysis
In the study of 16 UMLS terminologies, eight exhibited small-world characteristics of short average path length and strong local clustering, while an overlapping subset of nine displayed power law distribution in node degrees indicative of scale-free architecture [14]. These divergent topologies reflect different design constraints: constraints on node connectivity, common in more synthetic classification systems, help localize the effects of changes and deletions, while small-world and scale-free features, common in comprehensive medical terminologies, promote flexible navigation and organic growth [14].
Table 2: Topological Properties of Selected Biomedical Terminologies
| Terminology | Nodes | Links | Average Node Degree | Average Path Length | Clustering Coefficient | Topological Classification |
|---|---|---|---|---|---|---|
| CPT | 18,622 | 18,621 | 2.00 | 8.88 | 0 | Grid-like |
| NCBI Taxonomy | 247,151 | 246,854 | 2.00 | 26.49 | 0 | Hierarchical |
| Gene Ontology (GO) | 21,234 | 30,105 | 2.84 | 10.51 | 0.001462 | Scale-free |
| Clinical Terms (RCD) | 320,354 | 319,620 | 2.00 | 14.02 | 0.000278 | Small-world |
Implications for Terminology Science
The paradoxical finding that some controlled terminologies are structurally indistinguishable from natural language networks suggests that terminology structure is shaped not only by formal logic-based semantics but by rules analogous to those governing social networks and biological systems [14]. Graph theoretic modeling shows early promise as a framework for describing terminology structure, with deeper understanding of these techniques potentially informing the development of more scalable terminologies and ontologies [14].
Visualization of Network Topologies
Effective visualization of network topologies requires both appropriate graphical representation and adherence to accessibility standards for color contrast.
Basic Network Topology Diagram
Basic Network Concepts: This diagram illustrates the hierarchical relationship between fundamental network topology concepts, showing how local and global properties define network behavior in biomedical contexts.
Disease Network Analysis Workflow
Disease Network Pipeline: This workflow diagram outlines the data science pipeline for disease network construction and analysis, from initial data collection to drug repurposing applications.
Research Reagent Solutions for Network Analysis
Conducting topological analysis of biomedical networks requires specific computational tools and resources.
Table 3: Essential Research Reagents for Network Analysis
| Research Reagent | Function | Application in Network Analysis |
|---|---|---|
| UMLS Metathesaurus | Comprehensive database of biomedical terminologies | Provides standardized source vocabularies for network construction and comparison |
| MetamorphoSys | Customization tool for UMLS subsets | Enables extraction of selected terminologies in RRF format for source-transparent analysis |
| Graph Theory Libraries | Software libraries for network analysis | Calculate key metrics including node degree, path length, and clustering coefficients |
| Random Network Generators | Algorithms for generating control networks | Create equivalent random networks for statistical comparison and validation of topological features |
| Relational Database Systems | Data management and query platforms | Store and process large-scale terminology data for network modeling |
Network topology provides fundamental insights into the structural organization of biomedical knowledge systems, with distinct topological features emerging from different terminology design principles. The identification of scale-free and small-world architectures in comprehensive medical terminologies reveals organizational principles that promote navigability and sustainable growth. As network medicine continues to evolve, topological analysis will play an increasingly critical role in understanding disease relationships, identifying functional modules, and discovering new therapeutic opportunities through drug repurposing. The integration of graph theoretic approaches with traditional terminology science offers promising avenues for developing more scalable and computationally tractable biomedical knowledge resources.
The Spectrum of Autoimmune and Autoinflammatory Diseases as a Model System
The study of autoimmune and autoinflammatory diseases has undergone a paradigm shift with the adoption of the diseasome and disease network concepts. This framework moves beyond examining individual diseases in isolation to instead map the complex web of relationships between clinically distinct disorders. Autoimmune diseases, characterized by aberrant immune responses against self-antigens, provide an ideal model system for exploring this network medicine approach. Contemporary research reveals that these conditions, which affect approximately 3-5% of the global population and display a marked female predominance (approximately 80% of cases), are interconnected through shared genetic susceptibility loci, common environmental triggers, and overlapping immune dysregulation pathways [15] [16]. A 2025 network analysis of 30,334 inflammatory bowel disease (IBD) patients demonstrated that over half (57%) experienced at least one extraintestinal manifestation or associated immune disorder, with mental, musculoskeletal, and genitourinary conditions forming the most frequent disease communities [17]. This interconnectedness provides a powerful foundation for investigating the autoimmune diseasome.
The conceptual advancement of network medicine in autoimmunity represents more than a academic exercise—it offers tangible clinical benefits. By identifying central nodes and connections within the autoimmune network, researchers can pinpoint critical pathogenic hubs that may be amenable to therapeutic intervention. Furthermore, this approach accelerates the identification of novel biomarkers and reveals drug repurposing opportunities based on shared pathways across disease boundaries. The following sections explore the quantitative epidemiology, mechanistic underpinnings, experimental methodologies, and therapeutic innovations that establish the autoimmune spectrum as a premier model for diseasome research.
Quantitative Epidemiology and Disease Associations
The systematic mapping of autoimmune disease relationships requires robust population-level data. Recent studies provide compelling quantitative evidence for the interconnected nature of these conditions, with implications for both clinical management and research prioritization.
Table 1: Epidemiological Burden of Autoimmune Diseases
| Metric | Value | References |
|---|---|---|
| Global population prevalence | 3-5% | [15] |
| U.S. population affected | >50 million (8% of population) | [16] |
| Female predominance | Approximately 80% of cases | [16] [15] |
| Annual increase in global incidence | 19.1% | [16] |
| Patients with one autoimmune disease developing another | ~25% | [16] |
| UK population with autoimmune diseases (2000-2019) | 978,872 of 22 million (∼10% of study population) | [15] |
Network analysis of large patient cohorts reveals distinct clustering patterns within the autoimmune diseasome. A groundbreaking 2025 study applied artificial intelligence to analyze extraintestinal manifestations (EIMs) and associated autoimmune disorders (AIDs) in 30,334 IBD patients, providing unprecedented resolution of disease relationships [17]. The analysis identified distinct disease communities with varying connection densities:
Table 2: Disease Communities in IBD Patients (n=30,334)
| Disease Category | Prevalence in IBD | Preference | Dominant Conditions |
|---|---|---|---|
| Mental/behavioral disorders | 18% | CD > UC | Depression, anxiety |
| Musculoskeletal system disorders | 17% | CD > UC | Arthropathies, ankylosing spondylitis, myalgia |
| Genitourinary conditions | 11% | CD > UC | Calculus of kidney/ureter/bladder, tubulo-interstitial nephritis |
| Cerebrovascular diseases | 10% | No preference | Phlebitis, thrombosis, stroke |
| Circulatory system diseases | 10% | No preference | Cardiac ischemia, pulmonary embolism |
| Respiratory system diseases | 10% | CD > UC | Asthma |
| Skin and subcutaneous tissue diseases | 5% | CD > UC | Psoriasis, pyoderma, erythema nodosum |
| Nervous system diseases | 3% | No preference | Transient cerebral ischemia, multiple sclerosis |
This network-based approach demonstrates that diseases of the musculoskeletal system and connective tissue form particularly robust clusters, with rheumatoid arthritis serving as a central node connected to various IBD subtypes [17]. The identification of these communities enables researchers to hypothesize about shared pathogenic mechanisms and potential therapeutic targets that might transcend traditional diagnostic boundaries.
Shared Mechanisms and Pathways
The clinical interrelatedness observed in autoimmune diseases stems from common biological pathways that drive loss of self-tolerance and sustained inflammation. Understanding these shared mechanisms is fundamental to exploiting the autoimmune diseasome for therapeutic discovery.
Genetic Susceptibility Networks
Genetic studies have identified numerous susceptibility loci that span multiple autoimmune conditions, revealing a shared genetic architecture. The human leukocyte antigen (HLA) region represents the most significant genetic risk factor across numerous autoimmune diseases, with specific alleles conferring susceptibility to conditions including rheumatoid arthritis, type 1 diabetes, and multiple sclerosis [15]. Beyond HLA, genome-wide association studies (GWAS) have identified non-HLA risk loci that demonstrate pleiotropic effects. Notably, polymorphisms in genes such as PTPN22, STAT4, TNFAIP3, and IRF5 have been associated with multiple autoimmune diseases including systemic lupus erythematosus (SLE), rheumatoid arthritis, and type 1 diabetes [18] [15]. These genetic networks form the foundational layer of the autoimmune diseasome, establishing a permissive background upon which environmental triggers act.
Common Environmental Triggers
Environmental factors provide the second hit in autoimmune pathogenesis, often through mechanisms that mirror genetic susceptibility in their pleiotropic effects. The Epstein-Barr virus (EBV) represents a particularly compelling example of a shared environmental trigger. Recent research has demonstrated that EBV can directly commandeer host B cells, reprogramming them to instigate widespread autoimmunity [19]. In SLE, the EBV protein EBNA2 acts as a transcription factor that activates a battery of pro-inflammatory human genes, ultimately resulting in the generation of autoreactive B cells that target nuclear antigens [19]. This mechanism may extend to other autoimmune conditions such as multiple sclerosis, rheumatoid arthritis, and Sjögren's syndrome, where EBV seroprevalence and viral load are frequently elevated [16] [15].
Additional environmental factors including dysbiosis of the gut microbiome, vitamin D deficiency, and smoking have been implicated across the autoimmune spectrum [15]. These triggers appear to converge on common inflammatory pathways, particularly through the activation of innate immune sensors and the disruption of regulatory T cell function. The concept of molecular mimicry, wherein foreign antigens share structural similarities with self-antigens, provides a mechanistic link between infectious triggers and the breakdown of self-tolerance [15].
Convergent Signaling Pathways
At the molecular level, autoimmune diseases share dysregulation in key signaling pathways that control immune cell activation and effector function. The CD28/CTLA-4 pathway, which provides critical costimulatory signals for T cell activation, represents a central node in the autoimmune diseasome [15]. Genetic variations in this pathway influence multiple autoimmune conditions, and therapeutic manipulation of CTLA-4 has demonstrated efficacy in autoimmune models [15]. Similarly, the CD40-CD40L pathway serves as a universal signal for B cell activation, germinal center formation, and autoantibody production across diseases including rheumatoid arthritis and Sjögren's syndrome [15].
The type I interferon (IFN) signature represents another convergent pathway, particularly prominent in SLE and Sjögren's syndrome [16] [20]. In these conditions, sustained IFN production creates a feed-forward loop of immune activation and tissue damage. The JAK-STAT pathway, which transduces signals from multiple cytokine receptors, has emerged as a therapeutic target across autoimmune conditions, with inhibitors showing efficacy in rheumatoid arthritis, psoriatic arthritis, and other immune-mediated diseases [21].
Figure 1: Core Pathways in Autoimmune Diseasome. This diagram illustrates the convergent mechanisms driving autoimmunity, with genetic susceptibility and environmental triggers activating shared inflammatory pathways.
Experimental Approaches and Methodologies
The dissection of the autoimmune diseasome requires sophisticated experimental approaches that can capture the complexity of immune dysregulation across multiple diseases. The integration of high-throughput technologies with bioinformatic analysis has generated powerful methodologies for mapping disease networks.
Network Analysis and Artificial Intelligence
The application of AI-driven network analysis to large patient datasets has emerged as a cornerstone of diseasome research. The 2025 IBD study exemplifies this approach, employing the Louvain algorithm for community detection to identify distinct EIM/AID clusters within a network of 420-467 nodes and 9,116-16,807 edges, depending on the IBD subtype [17]. This method enabled the identification of previously unrecognized disease relationships and temporal patterns. Researchers can access this methodology through an interactive web application that allows for real-time exploration of disease connections, demonstrating how computational tools can transform large-scale clinical data into actionable biological insights.
Advanced Transcriptomic Profiling
Single-cell RNA sequencing (scRNA-seq) has revolutionized the resolution at which immune dysregulation can be characterized in autoimmune diseases. This technology enables the identification of novel cell states and inflammatory trajectories by profiling gene expression at the individual cell level [20]. The experimental workflow typically involves:
- Single-cell suspension preparation from patient tissues (blood, synovial fluid, biopsy specimens)
- Cell encapsulation and barcoding using microfluidic platforms
- Reverse transcription and library preparation with unique molecular identifiers
- High-throughput sequencing and bioinformatic analysis using clustering algorithms
The application of scRNA-seq to autoimmune diseases has revealed previously unappreciated heterogeneity in immune cell populations and identified rare pathogenic subsets that drive tissue inflammation [20]. When combined with spatial transcriptomics, this approach can map immune cells within tissue architecture, providing critical context for understanding mechanisms of tissue damage.
Molecular Imaging Techniques
Positron emission tomography (PET) combined with computed tomography (CT) or magnetic resonance imaging (MRI) enables non-invasive visualization of inflammatory processes across multiple organ systems [20]. Recent advances in tracer development have produced compounds that target specific aspects of immune activation:
Table 3: Molecular Imaging Tracers for Autoimmune Research
| Target | Tracer Examples | Application in Autoimmunity |
|---|---|---|
| Carbohydrate metabolism | 18F-fluorodeoxyglucose (FDG) | Detection of inflammatory lesions in SLE, RA |
| Chemokine receptors | 68Ga-pentixafor (CXCR4) | Tracking immune cell infiltration |
| Fibroblast activation protein | 68Ga-FAPI | Imaging of fibrotic complications |
| Somatostatin receptors | 68Ga-DOTATATE | Detection of granulomatous inflammation |
| Mitochondrial TSPO | 11C-PK11195 | Visualization of microglial activation in neuroinflammation |
These imaging modalities provide a powerful complement to molecular profiling by enabling longitudinal assessment of disease activity and therapeutic response in live organisms.
The Scientist's Toolkit: Essential Research Reagents
Research into the autoimmune diseasome requires a carefully selected set of reagents and tools that enable the dissection of complex immune interactions. The following table summarizes critical reagents and their applications in autoimmune disease research.
Table 4: Essential Research Reagents for Autoimmune Diseasome Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Flow cytometry antibodies | Anti-CD3, CD4, CD8, CD19, CD20, CD38, CD27 | Immune cell phenotyping and subset identification |
| Cytokine detection | IFN-α, IFN-γ, IL-6, IL-17, TNF-α ELISA/MSD | Measurement of inflammatory mediators |
| Autoantibody assays | ANA, anti-dsDNA, anti-CCP, RF | Diagnostic and prognostic biomarker quantification |
| Cell isolation kits | PBMC isolation, CD4+ T cell selection, B cell purification | Sample preparation for functional studies |
| scRNA-seq platforms | 10X Genomics, BD Rhapsody | Single-cell transcriptomic profiling |
| Multiplex imaging reagents | CODEX, GeoMx Digital Spatial Profiler | Spatial analysis of immune cell distribution |
| Animal models | MRL/lpr mice, collagen-induced arthritis, EAE | Preclinical therapeutic testing |
These reagents form the foundation for experimental investigations into autoimmune disease mechanisms. Their selection must be guided by the specific research question and the need for cross-disease comparisons that can reveal shared pathogenic networks.
Emerging Therapeutic Strategies
The diseasome concept has profound implications for therapeutic development in autoimmune diseases, encouraging strategies that target shared mechanisms across multiple conditions. Recent years have witnessed remarkable advances in immune-targeted therapies that exemplify this approach.
Immune Cell Reprogramming
Chimeric antigen receptor (CAR) T-cell therapy, originally developed for oncology, has emerged as a potentially transformative approach for severe, treatment-refractory autoimmune diseases. This strategy involves genetically engineering a patient's own T cells to express synthetic receptors that target specific immune populations. In a groundbreaking application, CD19-directed CAR T-cells induced durable drug-free remission in patients with refractory SLE, achieving rapid elimination of autoantibody-producing B cells and sustained clinical improvement even after B-cell reconstitution [22] [23]. The experimental protocol involves:
- Leukapheresis to collect patient T cells
- T cell activation and genetic modification with viral vectors encoding the CAR construct
- Lymphodepleting chemotherapy to enhance engraftment
- Infusion of CAR T-cells and monitoring for cytokine release syndrome
- Long-term follow-up for efficacy and safety assessment
The success of this approach has sparked an explosion of clinical trials exploring CAR T-cell therapy across a broad spectrum of autoimmune conditions, including multiple sclerosis, myasthenia gravis, and systemic sclerosis [23]. The methodology represents a paradigm shift from continuous immunosuppression toward targeted immune "resetting."
Targeted Biologics and Small Molecules
Beyond cellular therapies, the diseasome concept has informed the development of targeted biologics and small molecules that address shared pathways. The TYK2 pathway, which transduces signals from multiple cytokines including type I IFN, IL-12, and IL-23, has emerged as a compelling target across several autoimmune conditions [21]. Inhibition of TYK2 with agents such as deucravacitinib has demonstrated efficacy in psoriatic arthritis, with emerging evidence supporting potential applications in inflammatory bowel disease and SLE [21].
Similarly, B-cell targeting with agents such as ianalumab has shown significant benefit in Sjögren's disease, reducing disease activity by addressing the underlying autoimmune dysregulation rather than merely alleviating symptoms [21]. These targeted approaches reflect an increasingly precise understanding of the nodes within the autoimmune diseasome that are most amenable to therapeutic intervention.
Figure 2: CAR-T Cell Therapy Workflow. This diagram outlines the key steps in chimeric antigen receptor T-cell therapy, an emerging approach for severe autoimmune diseases.
The spectrum of autoimmune and autoinflammatory diseases provides an exceptionally powerful model system for exploring the diseasome concept and advancing the field of network medicine. The interconnected nature of these conditions, evidenced by shared genetic architecture, common environmental triggers, and convergent inflammatory pathways, offers unprecedented opportunities for mechanistic discovery and therapeutic innovation. The research approaches outlined in this review—from AI-driven network analysis to single-cell transcriptomics and molecular imaging—provide a methodological framework for mapping disease relationships with increasing resolution.
As these technologies continue to evolve, several emerging frontiers promise to further refine our understanding of the autoimmune diseasome. The integration of multi-omic datasets (genomic, epigenomic, transcriptomic, proteomic) will enable more comprehensive mapping of disease networks. Advances in spatial biology will contextualize immune dysregulation within tissue microenvironments. Furthermore, the application of machine learning to large-scale clinical data will identify novel disease associations and predict therapeutic responses.
The ultimate translation of diseasome research will be the development of precision medicine approaches that target shared mechanisms across autoimmune conditions, potentially benefiting multiple patient populations. As noted by Dr. Maximilian Konig of Johns Hopkins University, "We've never been closer to getting to—and we don't like to say it—a potential cure. I think the next 10 years will dramatically change our field forever" [22]. The autoimmune diseasome model provides the conceptual framework needed to realize this transformative potential.
Biomedical ontologies provide a structured, controlled vocabulary for organizing biological and medical knowledge, enabling computational analysis and data integration. The concept of the diseasome—a network representation of human diseases—relies on these formal frameworks to map the complex relationships between diseases based on shared molecular origins, phenotypic manifestations, and underlying genetic architectures [24] [3]. Disease-disease networks (DDNs) constructed from ontological relationships reveal that disorders with common genetic foundations or phenotypic features often cluster together in the human interactome [24] [3]. This network-based perspective is transforming our understanding of disease etiology, moving beyond traditional anatomical or histological classification systems toward a molecularly-defined nosology that can identify novel disease relationships and therapeutic targets [24]. Ontologies like Mondo, Disease Ontology (DO), Medical Subject Headings (MeSH), and the International Classification of Diseases (ICD) provide the essential semantic structure for representing disease concepts and their relationships, forming the computational foundation for diseasome research and network medicine applications in drug discovery and development.
Core Disease Ontology Frameworks
Mondo Disease Ontology
Mondo Disease Ontology (Mondo) is a comprehensive logic-based ontology designed to harmonize disease definitions across multiple biomedical resources [25]. The name "Mondo" originates from the Latin word 'mundus,' meaning 'for the world,' reflecting its global scope and applicability. Mondo addresses the critical challenge of overlapping and sometimes conflicting disease definitions across resources like HPO, OMIM, SNOMED CT, ICD, PhenoDB, MedDRA, MedGen, ORDO, DO, and GARD by providing precise equivalences between disease concepts using semantic web standards [25].
Mondo is constructed semi-automatically by merging multiple disease resources into a coherent ontology. A key innovation is its use of precise 1:1 equivalence axioms connecting to other resources like OMIM, Orphanet, EFO, and DOID, which are validated by OWL reasoning rather than relying on loose cross-references [25]. This ensures safe data propagation across these resources. The ontology is available in three formats: the OWL edition with full equivalence axioms and inter-ontology axiomatization; a simpler .obo version using xrefs; and an equivalent JSON edition [25].
Table: Mondo Disease Ontology Statistical Overview
| Metric | Count |
|---|---|
| Total number of diseases | 25,880 |
| Database cross references | 129,785 |
| Term definitions | 17,946 |
| Exact synonyms | 73,878 |
| Human diseases | 22,919 |
| Cancer (human) | 4,727 |
| Mendelian diseases | 11,601 |
| Rare diseases | 15,857 |
| Non-human diseases | 2,960 |
Table: Mondo Disease Categorization
| Category | Count (classes) |
|---|---|
| Human diseases | 22,919 |
| Cancer | 4,727 |
| Infectious | 1,074 |
| Mendelian | 11,601 |
| Rare | 15,857 |
| Non-human diseases | 2,960 |
| Cancer (non-human) | 215 |
| Infectious (non-human) | 87 |
| Mendelian (non-human) | 1,023 |
Disease Ontology (DO) and DOLite
The Disease Ontology (DO) organizes disease concepts in a directed acyclic graph (DAG), where traversing away from the root moves toward progressively more specific terms [26]. The full DO graph contains substantial complexity—revision 26 included 11,961 terms with up to 16 hierarchical levels—creating challenges for specific applications like gene-disease association studies [26].
To address this, DOLite was developed as a simplified vocabulary derived from DO using statistical methods that group DO terms based on similarity of gene-to-DO mapping profiles [26]. The methodology involves:
- Pre-filtering DO terms: Removing abstract concepts with few gene associations
- Creating a gene-to-DO mapping profile matrix: Documenting evidence of gene-disease relationships
- Calculating distance metrics: Measuring overall similarity (
dist1) and subset similarity (dist2) between DO terms based on their gene associations - Applying compactness-scalable fuzzy clustering: Grouping similar DO terms while constraining results with semantic similarities
This approach significantly reduces redundancy and creates a more tractable ontology for enrichment tests, yielding more interpretable results for gene-disease association analyses [26].
Medical Subject Headings (MeSH)
Medical Subject Headings (MeSH) is a controlled, hierarchically-organized vocabulary produced by the National Library of Medicine for indexing, cataloging, and searching biomedical information [27]. MeSH serves as the subject heading foundation for MEDLINE/PubMed, the NLM Catalog, and other NLM databases, providing a comprehensive terminology for literature retrieval. The taxonomy is regularly updated, with 2025 MeSH files currently in production and available through multiple formats including RDF and an open API [27]. MeSH is part of a larger ecosystem of medical vocabularies that includes RxNorm for drugs, DailyMed for marketed drug information, and the Unified Medical Language System (UMLS) Metathesaurus which integrates over 150 medical vocabulary sources [27].
International Classification of Diseases (ICD)
The International Classification of Diseases (ICD) is a global standard for diagnostic classification maintained by the World Health Organization, widely used for billing, epidemiological tracking, and health statistics [28]. ICD coding presents significant challenges for automation due to the complexity of medical narratives and the hierarchical structure of ICD codes. Recent advances in machine learning for automated ICD coding include:
- Hierarchical modeling: Approaches like Tree-of-Sequences LSTM that capture parent-child relationships in the ICD taxonomy [29]
- Graph neural networks (GNNs): Frameworks like LGG-NRGrasp that model ICD coding as a labeled graph generation problem using adversarial reinforcement learning [29]
- Novel evaluation metrics: The introduction of λ-DCG, a metric tailored specifically for ICD coding tasks that provides more interpretable assessment of coding system quality [28]
These computational approaches must address challenges like over-smoothing in deep networks, structural inconsistencies in medical data, and limited labeled datasets [29].
Table: Comparative Analysis of Disease Ontology Frameworks
| Feature | Mondo | Disease Ontology (DO) | MeSH | ICD |
|---|---|---|---|---|
| Primary Purpose | Harmonize disease definitions across resources | Gene-disease association studies | Literature indexing & retrieval | Billing & epidemiology |
| Structure | Logic-based ontology with equivalence axioms | Directed acyclic graph (DAG) | Hierarchical vocabulary | Hierarchical classification |
| Coverage | 25,880 diseases | 11,961 terms (revision 26) | Comprehensive biomedical topics | Diseases, symptoms, abnormal findings |
| Key Innovation | Precise 1:1 equivalence mappings between resources | DOLite simplified version for statistical testing | Integration with UMLS Metathesaurus | Global standard for health statistics |
| Molecular Focus | High - integrates genetic & phenotypic data | High - designed for gene-disease relationships | Medium - includes genetic terms | Low - primarily clinical descriptions |
Ontology Applications in Diseasome and Disease Network Research
Constructing Disease-Disease Networks
Biomedical ontologies enable the construction of disease-disease networks (DDNs) that reveal shared genetic architecture and molecular relationships between disorders. The shared-SNP DDN (ssDDN) approach uses PheWAS summary statistics to connect diseases based on shared genetic variants, accurately modeling known multimorbidities [3]. An enhanced version, ssDDN+, incorporates genetic correlations with intermediate endophenotypes like clinical laboratory measurements, providing deeper insight into molecular contributors to disease associations [3].
For example, research using UK Biobank data has demonstrated that HDL-C connects the greatest number of diseases in cardiometabolic networks, showing strong genetic relationships with both type 2 diabetes and heart failure [3]. Triglycerides represent another blood lipid biomarker that adds substantial connections to disease networks, revealing shared genetic architecture across seemingly distinct disorders [3].
Disease Network via Shared Genetics & Biomarkers
Phenotype-Based Disease Similarity
Semantic similarity calculations using ontology-annotated phenotype data enable the identification of disease relationships beyond genetic associations. Text-mining approaches applied to MEDLINE abstracts can extract phenotype-disease associations, generating comprehensive disease signatures that cluster disorders with common pathophysiological underpinnings [4].
The methodology involves:
- Identifying co-occurrences: Mining disease-phenotype term co-occurrences in biomedical literature
- Statistical scoring: Applying normalized pointwise mutual information (NPMI), T-Score, Z-Score, and Lexicographer's mutual information to rank associations
- Optimal phenotype cutoff determination: Establishing the ideal number of phenotype annotations per disease (empirically determined to be 21 phenotypes)
- Similarity computation: Using systems like PhenomeNET to calculate phenotypic similarity between human diseases and model organism phenotypes
This approach has demonstrated high accuracy (ROCAUC 0.972 ± 0.008) in matching text-mined disease definitions to established OMIM disease profiles [4].
Network Medicine and Drug Development
Disease progression modeling (DPM) uses mathematical frameworks to characterize disease trajectories, integrating ontological definitions to inform clinical trial design and therapeutic development [30]. DPM applications identified through scoping review include:
- Informing patient selection (56 studies): Identifying patient subtypes based on predicted disease progression
- Enhancing trial designs (35 studies): Using DPM of longitudinal data to increase power or reduce sample size requirements
- Identifying biomarkers and endpoints (34 studies): Developing prognostic models for predicting disease progression
- Characterizing treatment effects (various studies): Informing dose selection and optimization
These applications demonstrate how ontology-structured disease concepts enable more efficient drug development, particularly for rare diseases where traditional trial design faces significant challenges [30].
Experimental Methodologies and Workflows
Gene-Disease Association Enrichment Analysis
DOLite Construction & Enrichment Analysis Workflow
Automated ICD Coding with Graph Neural Networks
The LGG-NRGrasp framework represents a cutting-edge approach to automated ICD coding using graph neural networks [29]. The methodology involves:
- Labeled Graph Generation: Constructing relational graphs from clinical narratives that capture dependencies among diagnostic codes
- Dynamic Architecture: Employing residual propagation and feature augmentation to prevent over-smoothing
- Adversarial Training: Enhancing robustness through domain adaptation techniques
- Reinforcement Learning Integration: Using a parameterized policy (π_θ) for probabilistic decision-making over graph states
This framework specifically addresses challenges like hierarchical ICD code relationships, sparse clinical data, and the need for model interpretability in healthcare settings [29].
Table: Research Reagent Solutions for Diseasome Studies
| Resource | Type | Primary Function | Application in Diseasome Research |
|---|---|---|---|
| Mondo Ontology | Computational Resource | Disease concept harmonization | Integrating multiple disease databases with precise mappings |
| MeSH RDF API | Data Retrieval | Programmatic access to MeSH | Semantic querying of disease-literature relationships |
| PheWAS Summary Statistics | Dataset | Genetic association data | Constructing shared-SNP disease networks (ssDDNs) |
| UK Biobank Data | Biomarker & Genetic Data | Population-scale biomedical data | Augmenting DDNs with biomarker correlations (ssDDN+) |
| PhenomeNET System | Computational Tool | Phenotypic similarity calculation | Cross-species disease phenotype comparison |
| HPO/MP Ontologies | Phenotype Vocabularies | Standardized phenotype descriptions | Annotating diseases with computable phenotypic profiles |
Phenotype-Driven Disease Network Construction
The workflow for constructing phenotype-based disease networks involves [4]:
- Data Extraction: Mining 5 million MEDLINE abstracts for disease-phenotype co-occurrences
- Annotation: Associating over 6,000 Disease Ontology classes with 9,646 phenotype classes from HPO and MP
- Statistical Validation: Using known gene-disease associations from OMIM and MGI to optimize phenotype cutoffs
- Similarity Computation: Applying semantic similarity measures to generate human disease networks
- Network Analysis: Identifying disease clusters based on etiological, anatomical, and physiological relationships
This methodology has demonstrated that diseases with similar signs and symptoms cluster together in the human diseasome, revealing common molecular underpinnings [4].
Biomedical ontologies are evolving from static classification systems toward dynamic frameworks that capture the complex, multi-scale nature of disease. Future development will focus on deeper integration of molecular data, enhanced reasoning capabilities, and more sophisticated network-based analyses. The Mondo initiative exemplifies this trajectory with its logical foundations and precise mapping strategy [25]. As diseasome research advances, ontologies will increasingly incorporate temporal dimensions to model disease progression, treatment responses, and trajectory variations across patient subpopulations [30].
The integration of ontology-structured knowledge with network medicine approaches creates powerful frameworks for identifying drug repurposing opportunities, understanding genetic pleiotropy, and addressing missing heritability in complex diseases [24] [3]. Tools like DOLite demonstrate how domain ontologies can be optimized for specific research applications while maintaining connections to broader knowledge systems [26]. As these resources mature, they will play an increasingly critical role in personalized medicine by enabling more precise disease subtyping, biomarker identification, and therapeutic targeting based on comprehensive molecular and phenotypic profiling.
For researchers exploring the diseasome, the complementary strengths of Mondo (harmonization), DO (gene-disease focus), MeSH (literature integration), and ICD (clinical utility) provide a robust foundation for computational analysis. The experimental methodologies and workflows presented here offer practical approaches for leveraging these resources to uncover the complex network relationships that define human disease.
Building Disease Networks: Methods, Data Integration, and Research Applications
The study of diseasome networks represents a paradigm shift in understanding human disease, moving from isolated examination of single disorders to exploring the complex web of interconnections based on shared molecular and phenotypic foundations. Disease association studies, or diseasome analyses, facilitate the exploration of disease mechanisms and the development of novel therapeutic strategies by constructing and analyzing disease association networks [5]. This approach is particularly valuable for understanding complex disease categories such as autoimmune and autoinflammatory diseases (AIIDs), which are characterized by significant heterogeneity and comorbidities that complicate their mechanistic understanding and classification [5]. The integration of multi-modal data—encompassing genetic, transcriptomic (both bulk and single-cell), and phenotypic layers—provides an unprecedented opportunity to accurately measure disease associations within related disorders and uncover the mechanisms underlying these associations from a cross-scale perspective [5].
Historically, biological network visualization and analysis have faced significant challenges due to the underlying graph data becoming ever larger and more complex [12]. A unified data representation theory has emerged as a critical framework linking network visualization, data ordering, and coarse-graining through an information theoretic approach that quantifies the hidden structure in probabilistic data [31]. The major tenet of this unified framework is that the best representation is selected by the criterion that it is the hardest to be distinguished from the input data, typically measured by minimizing the relative entropy or Kullback-Leibler divergence as a quality function [31]. This theoretical foundation enables researchers to reveal the large-scale structure of complex networks in a comprehensible form, which is particularly important for comprehending the intricate relationships in multi-scale disease networks.
Theoretical Framework and Computational Foundations
Unified Data Representation Theory
The foundational principle of multi-modal data integration rests on a unified data representation theory that elegantly connects network visualization, data ordering, and coarse-graining through information theoretic measures [31]. This approach considers both the input matrix (A) and the approximative representation (B) as probability distributions, where the optimal representation B* is determined by minimizing the relative entropy or Kullback-Leibler divergence according to the equation:
[D(A\|B) = \sum{i,j} a{ij} \log \frac{a{ij}}{b{ij}} - a{} + b{}]
where (a{}) and (b{}) ensure proper normalization of the probability distributions [31]. The relative entropy measures the extra description length when B is used to encode the data described by the original matrix A, with the highest quality representation achieved when the relative entropy approaches zero. This theoretical framework enables meaningful comparison across data modalities by providing a common mathematical foundation for integration.
Ontology-Aware Disease Similarity (OADS)
A critical innovation in modern diseasome research is the development of ontology-aware disease similarity (OADS) strategies that incorporate not only multi-modal data but also the continuous framework of hierarchical biomedical ontologies [5]. The OADS framework leverages structured knowledge representations through several key components:
Gene Ontology (GO) Integration: Disease-associated genes, including genetically associated disease genes obtained from OMIM and dysregulated genes (DCGs), are mapped to GO Biological Process terms. DCGs are weighted by normalized differential co-expression (dC) values, with the top 20 GO terms retained per disease for similarity computation [5].
Cell Ontology Alignment: Single-cell RNA sequencing data are processed through Seurat for quality control, normalization, and clustering, with SingleR-based cell annotation providing cell type identification. Cell ontology similarities are then calculated using the CellSim method [5].
Human Phenotype Ontology (HPO) Utilization: Phenotypic terms extracted from HPO enable standardized comparison of clinical manifestations across diseases. Ontology similarities are calculated using the Wang method, which captures both the semantic content and hierarchical structure of ontological terms [5].
Disease similarity within the OADS framework is computed via FunSimAvg aggregation, which averages bidirectional GO term assignments to provide a comprehensive measure of disease relatedness that transcends individual data modalities [5].
Network Construction and Analysis Pipelines
The construction of robust diseasome networks requires sophisticated computational pipelines that transform multi-modal data into interpretable network structures. The technical workflow typically involves:
Data Curation and Harmonization: Disease terms are curated from multiple sources including Mondo (Monarch Disease Ontology), DO (Disease Ontology), MeSH (Medical Subject Headings), ICD-11 (International Classification of Diseases 11th), and specialized AIID databases [5]. This establishes a comprehensive disease repository that forms the node set of the diseasome network.
Multi-Layered Network Construction: Python and NetworkX libraries are employed to build disease networks with edges representing similarity scores exceeding the 90th percentile with statistical significance (p < 0.05) [5]. This creates multiple network layers corresponding to different data modalities.
Community Detection and Modularity Analysis: Disease modules and communities are detected using hierarchical clustering with Ward's method and the Leiden algorithm at a resolution of 1.0 [5]. These communities represent groups of diseases with shared mechanisms across the integrated data modalities.
Topological Analysis: NetworkX library functions are used to calculate standard centrality measures (degree, betweenness, closeness, eigenvector centrality), clustering coefficient, transitivity, k-core decomposition, network diameter, and shortest path lengths [5]. These metrics identify strategically important diseases within the network.
The power-law characteristics of the resulting networks are evaluated using the powerlaw library to determine if the network displays scale-free properties, which has implications for the robustness and vulnerability of the disease system [5].
Experimental Protocols and Methodologies
Data Acquisition and Preprocessing
Genomic Data Processing
Genetic data acquisition begins with comprehensive curation of disease-associated genes from established databases including OMIM, GWAS catalog, and DISEASES. The differential co-expression analysis is performed using the DCGL package with Z-score normalized dC values, which identifies genes whose co-expression patterns differ significantly between disease and control states [5]. For transcriptomic data, gene expression datasets are curated from Affymetrix U133A platforms (GPL570/96/571) in GEO, filtered by specific criteria including disease/control groups with ≥5 samples each and tissue sources restricted to PBMCs/whole blood/skin to ensure consistency [5]. Quality control includes assessment of RNA integrity, background correction, quantile normalization, and probe summarization using the robust multi-array average (RMA) algorithm.
Single-Cell RNA Sequencing Protocol
Single-cell RNA sequencing data are obtained from five major platforms (GPL24676/18573/16791/11154/20301) through GEO searches with comprehensive disease synonyms [5]. The experimental workflow involves:
Cell Capture and Library Preparation: Cells are captured using microfluidic devices (10X Genomics, Drop-seq, or inDrops) with subsequent reverse transcription, cDNA amplification, and library preparation with unique molecular identifiers (UMIs) to correct for amplification biases.
Sequence Alignment and Quantification: Reads are aligned to a reference genome using STAR or HISAT2, with gene-level quantification performed using featureCounts or similar tools.
Data Processing with Seurat: The Seurat package is employed for quality control filtering (mitochondrial percentage, number of features, counts), normalization using SCTransform, feature selection based on highly variable genes, scaling, principal component analysis, and graph-based clustering [5].
Cell Type Annotation: The SingleR package leverages reference datasets to assign cell type labels to clusters based on correlation with bulk RNA-seq data from pure cell types [5].
Phenotypic Data Extraction
Phenotypic terms are systematically extracted from clinical descriptions in electronic health records, literature sources, and specialized databases, then mapped to standardized terms in the Human Phenotype Ontology (HPO) [5]. This normalization enables computational comparison of disease manifestations across different healthcare systems and documentation practices.
Multi-Modal Similarity Calculation
The calculation of disease similarities across different data modalities follows a structured pipeline with modality-specific processing:
Table 1: Multi-Modal Data Processing Parameters
| Data Modality | Data Sources | Processing Tools | Key Parameters | Output Metrics |
|---|---|---|---|---|
| Genetic | OMIM, GWAS catalog, DISEASES | DCGL package | Z-score normalized dC values, top 20 GO terms | Functional similarity based on shared GO terms |
| Transcriptomic (bulk) | GEO datasets (GPL570/96/571) | limma, DESeq2 | FDR < 0.05, logFC > 1 | Differential expression signatures |
| Transcriptomic (single-cell) | GEO platforms (GPL24676/18573/16791/11154/20301) | Seurat, SingleR | Resolution = 0.8, top 2000 variable features | Cell type abundance differences |
| Phenotypic | HPO, clinical records | Natural language processing | Wang similarity metric | Phenotypic similarity scores |
For each modality, the similarity between two diseases is calculated using the FunSimAvg approach, which averages the maximum semantic similarities for all term pairs between the two diseases [5]. The statistical significance of observed similarities is evaluated through permutation testing, where disease-term mappings are shuffled 500 times while preserving term counts and distributions to generate null distributions [5].
Network Integration and Validation
The integration of multi-modal similarities into a unified diseasome network employs a weighted integration approach where each modality contributes based on data quality and completeness. Cross-modal validation is performed by examining the consistency of disease relationships across independent data layers. The robustness of identified disease communities is assessed through bootstrap resampling and sensitivity analysis of network parameters. Community-specific representative features are identified by counting the frequency of each feature in a given cluster relative to all other clusters, with statistical significance determined using Fisher's exact test [5].
Visualization Methodologies and Technical Specifications
Information-Theoretic Network Layout
Traditional force-directed layout algorithms for biological networks struggle with information shortage problems, as edge weights only provide half the needed data to initialize these techniques [31]. In strong contrast to usual graph layout schemes where nodes are represented by dimensionless points, the information-theoretic approach represents network nodes as probability distributions (ρ(x)) over the background space [31]. For differentiable cases, Gaussian distributions with a width of σ and appropriate normalization are typically used, though non-differentiable cases of homogeneous distribution in spherical regions have also been tested with similar results [31]. The edge weights bij in the representation are defined as the overlaps of the distributions ρi and ρj, creating a natural connection between node positioning and relationship strength.
The numerical optimization can be performed using various approaches: a fast but inefficient greedy optimization; a slow but efficient simulated annealing scheme; or as a reasonable compromise, in the differentiable case of Gaussian distributions, a Newton-Raphson iteration similar to the Kamada-Kawai method with a run-time of O(N²) for N nodes [31]. The optimization starts with an initialization where all nodes are at the same position with the same distribution function (apart from varying normalization to ensure proper statistical weight of nodes), corresponding to the trivial data representation B₀ [31].
Visual Analytics and Design Spaces
The construction of effective visualization design spaces requires systematic analysis of both text and images to articulate why a visualization was created (the research problem it supports) and how it was constructed (the visual design and interactivity) [32]. This nested model for visualization design and analysis deconstructs data visualizations into four layers: the why (domain problem), what (data and specific tasks), how (visual design and interactivity), and the algorithmic implementation [32]. For genomic epidemiology and diseasome applications, this approach has been formalized in the Genomic Epidemiology Visualization Typology (GEViT), which provides a structured way of describing a collection of visualizations that together form an explorable visualization design space [32].
Technical Implementation of Diseasome Visualizations
The implementation of diseasome visualizations requires careful attention to technical specifications, particularly regarding computational efficiency and visual encoding. For large-scale networks, coarse-graining or renormalization techniques enable zooming out from the network by averaging out short-scale details to reduce the network to a manageable size while revealing large-scale patterns [31]. From an implementation perspective, the use of hierarchical clustering and the Leiden algorithm for community detection at a resolution of 1.0 provides a balance between granularity and interpretability [5].
Table 2: Visualization Parameters for Multi-Scale Diseasome Networks
| Visualization Component | Technical Specification | Recommended Tools | Accessibility Considerations |
|---|---|---|---|
| Network Layout | Information-theoretic with Gaussian distributions | Newton-Raphson iteration | Sufficient node-label contrast |
| Community Encoding | Color-based with categorical palette | Leiden algorithm (resolution=1.0) | Colorblind-safe palettes |
| Multi-Scale Representation | Hierarchical coarse-graining | Powerlaw library | Consistent symbolic language |
| Cross-Modal Evidence | Edge bundling and texture | Cytoscape, NetworkX | Multiple redundant encodings |
| Interactive Exploration | Zoom, filter, details-on-demand | D3.js, Plotly | Keyboard navigation support |
Color contrast requirements follow WCAG AA guidelines, with a minimum contrast ratio of 4.5:1 for large text (18pt/24px or 14pt/19px bold) and 7:0:1 for regular text [33] [34]. The specified color palette (#4285F4, #EA4335, #FBBC05, #34A853, #FFFFFF, #F1F3F4, #202124, #5F6368) provides sufficient chromatic variety while maintaining accessibility when properly combined [35] [36] [37]. For text within nodes, the text color (fontcolor) must be explicitly set to have high contrast against the node's background color (fillcolor), typically using black (#202124) on light backgrounds or white (#FFFFFF) on dark backgrounds [38].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools for Diseasome Studies
| Reagent/Tool | Specific Function | Application Context | Implementation Example |
|---|---|---|---|
| DCGL Package | Differential co-expression analysis | Identification of dysregulated gene networks in transcriptomic data | Z-score normalized dC values with top 20 GO terms per disease [5] |
| Seurat Pipeline | Single-cell RNA-seq analysis | Cellular decomposition of disease signatures | QC, normalization, clustering, and cell type annotation [5] |
| SingleR | Automated cell type annotation | Reference-based labeling of single-cell clusters | Correlation with pure cell type transcriptomes [5] |
| RDKit | Chemical similarity computation | Drug repurposing analysis based on structural similarity | SMILES-defined drug similarity for drug-based disease relationships [5] |
| NetworkX Library | Network construction and analysis | Topological characterization of diseasome networks | Centrality measures, community detection, path analysis [5] |
| Powerlaw Library | Scale-free network assessment | Evaluation of network topology characteristics | Fitting degree distribution to power-law model [5] |
| Adjutant R Package | Literature analysis and topic clustering | Systematic review of disease visualization corpus | t-SNE and hdbscan for unsupervised topic clustering [32] |
Technical Implementation Diagrams
Multi-Modal Data Integration Workflow
Ontology-Aware Disease Similarity Framework
Diseasome Network Analysis Pipeline
The integration of genetic, transcriptomic, and phenotypic layers through multi-modal data integration frameworks represents a transformative approach to diseasome research. The ontology-aware disease similarity strategy, coupled with unified data representation theory, enables researchers to move beyond single-dimensional disease classifications toward a comprehensive understanding of disease relationships across biological scales [5] [31]. The experimental protocols and visualization methodologies outlined in this technical guide provide a robust foundation for constructing and analyzing diseasome networks that reveal the complex web of relationships underlying human disease.
Future developments in this field will likely focus on several key areas: the incorporation of additional data modalities such as proteomic, metabolomic, and microbiome data; the development of more sophisticated dynamic network models that capture disease progression over time; and the implementation of advanced visual analytics platforms that support collaborative exploration of complex diseasome networks [12] [32]. As these technical capabilities advance, multi-modal data integration will play an increasingly central role in elucidating disease mechanisms, identifying novel therapeutic targets, and ultimately advancing toward more precise and effective healthcare interventions.
Ontology-Aware Disease Similarity (OADS) Calculations and Algorithms
The systematic exploration of disease associations, known as the "diseasome," provides a powerful framework for uncovering common disease pathogenesis, predicting disease evolution, and optimizing therapeutic strategies [5]. Diseasome research utilizes network biology approaches to construct and analyze disease association networks, revealing unexpected molecular relationships between seemingly distinct pathologies [39]. Within this paradigm, quantifying disease similarity moves beyond symptomatic presentation to incorporate molecular foundations, including shared genetic underpinnings, transcriptomic profiles, and common pathway dysregulations [40].
Ontology-Aware Disease Similarity (OADS) represents an advanced methodological framework that incorporates both multi-modal biological data and the continuous knowledge structures of biomedical ontologies [5]. This approach addresses significant limitations in earlier disease similarity methods that relied on single data types or failed to leverage the rich semantic relationships encoded in hierarchical ontologies. By simultaneously leveraging genetic, transcriptomic, cellular, and phenotypic data within an ontology-informed structure, OADS enables more accurate and biologically meaningful disease relationship mapping, which is particularly valuable for understanding complex disease spectra such as autoimmune and autoinflammatory diseases (AIIDs) [5].
Theoretical Foundations of OADS
Core Mathematical Principles
The OADS framework integrates two fundamental concepts: multi-modal data integration and ontology-aware similarity computation. The methodology utilizes distance metrics between empirical, multivariable statistical distributions derived from high-dimensional -omics data, capable of robust similarity estimation even with dimensionality reaching hundreds of thousands of molecular measurements and sample sizes as low as 40 [39]. This approach captures the intuition that similar diseases demonstrate comparable inter-correlation patterns among molecular quantities, reflected through similar covariance structures across datasets.
The ontology integration employs semantic similarity measures that traverse the directed acyclic graph (DAG) structures of biomedical ontologies. For disease similarity calculations, the framework incorporates the Wang method for Gene Ontology (GO) and Human Phenotype Ontology (HPO), and CellSim for Cell Ontology comparisons [5]. These methods account for both the hierarchical position of terms within ontologies and the depth of their relationships, providing more nuanced similarity measurements than simple term matching.
Biomedical Ontologies in OADS
OADS leverages multiple established biomedical ontologies that provide standardized vocabularies and hierarchical relationships:
- Gene Ontology (GO): Provides structured, controlled vocabularies for gene functions across biological processes, molecular functions, and cellular components [41].
- Cell Ontology: A structured ontology for cell types that provides a standardized representation of cell characteristics [5].
- Human Phenotype Ontology (HPO): Provides standardized vocabulary for phenotypic abnormalities encountered in human disease [40].
- Disease Ontology (DO): Creates a single structure for disease classification that unifies disease representation across varied vocabularies into a relational ontology [40].
These ontologies form the semantic backbone that enables the "awareness" in OADS, allowing the framework to leverage established biological relationships rather than treating each data point in isolation.
Computational Framework and Algorithmic Implementation
Data Integration and Preprocessing
The OADS pipeline begins with comprehensive data curation from multiple sources. The framework aggregates disease terms from Mondo (Monarch Disease Ontology), Disease Ontology (DO), Medical Subject Headings (MeSH), ICD-11, and specialized knowledge bases such as the Autoimmune Association, Autoimmune Registry, Inc., and the Global Autoimmune Institute [5]. This integration creates a comprehensive disease repository encompassing 484 autoimmune diseases, 110 autoinflammatory diseases, and 284 associated diseases.
Molecular data integration includes several modalities:
- Genetic data: Disease-associated genes from OMIM and genetically associated disease genes.
- Transcriptomic data: Both bulk and single-cell RNA-sequencing data from platforms such as Affymetrix U133A and various single-cell platforms.
- Phenotypic data: Phenotypic terms extracted from Human Phenotype Ontology.
- Drug-disease relationships: Sourced from DrugBank, DrugCentral, TTD, PharmGKB, and CTD, filtered to retain SMILES-defined drugs [5].
Similarity Calculation Methodology
The OADS framework implements a multi-layered similarity calculation approach that incorporates both molecular data and ontological relationships:
Molecular Similarity Components:
- Gene-based similarity: Disease genes, including genetically associated disease genes from OMIM and dysregulated genes (DCGs) calculated by DCGL, are mapped to GO Biological Process terms. DCGs are weighted by normalized dC values, retaining top 20 GO terms per disease [5].
- Differential co-expression analysis: Uses the DCGL package with Z-score normalized dC values, retaining top 20 Gene Ontology terms per disease.
- scRNA-seq processing: Data processed through Seurat (QC/normalization/clustering) with SingleR-based cell annotation [5].
Ontology-Aware Similarity Integration: The framework computes disease similarity using the FunSimAvg method, which averages bidirectional GO term assignments [5]. This approach integrates:
- GO term similarity: Calculated using the Wang method, which considers the hierarchical structure of GO.
- Phenotype similarity: HPO terms compared using semantic similarity measures.
- Cell type similarity: CellSim algorithm applied to Cell Ontology terms.
Drug-based Disease Similarity: Drug-disease relationships from five databases are filtered to retain SMILES-defined drugs. Structural similarity between drugs is computed using RDKit, and drug-based disease similarity is derived via FunSimAvg aggregation [5].
Network Construction and Analysis
The OADS framework constructs multi-layered disease association networks supported by cross-scale evidence at genetic, transcriptomic, cellular, and phenotypic levels. Disease networks are built using Python/NetworkX with edges representing similarity scores above the 90th percentile and statistical significance (p < 0.05) [5].
Network analysis includes:
- Community detection: Disease modules/communities detected by hierarchical clustering (Ward's method) and the Leiden algorithm with resolution = 1.0.
- Topological analysis: NetworkX library calculates centrality measures (degree, betweenness, closeness, eigenvector centrality), clustering coefficient, transitivity, k-core, network diameter, and shortest path lengths.
- Power-law evaluation: The network degree distribution is fitted to a power-law model using the powerlaw library to evaluate scale-free properties.
Experimental Protocols and Implementation
Data Curation and Normalization
AIID Classification Score Calculation: To capture both direction and confidence of classification sources, the framework extends the original binary AIID Classification Score (ACS) into a continuous, weighted metric on [-1, +1]. For each disease and each source i, let si denote classification as autoimmune, unclassified or autoinflammatory, and let wi be the source's confidence weight. The normalized ACS is computed as:
Weights are assigned based on coverage, update frequency, and community endorsement: Mondo = 1.0, DO = 0.8, MeSH = 0.7, ICD = 0.7, expert panel lists = 1.0, AA/ARI/GAI = 1.0 [5].
Gene Expression Data Processing:
- Gene expression data are curated from Affymetrix U133A platforms (GPL570/96/571) in GEO, filtered by disease/control groups with ≥5 samples each, and tissue sources (PBMCs/whole blood/skin).
- scRNA-seq data are obtained from five major platforms through GEO searches with disease synonyms.
- Data processing includes quality control, normalization, and clustering through Seurat with SingleR-based cell annotation.
Statistical Validation and Significance Testing
The OADS framework implements rigorous statistical validation:
- Permutation testing: Disease-term mappings are shuffled 500× while preserving term counts/distributions to generate null distributions by recalculating similarities.
- Network significance: Edge inclusion requires similarity scores > 90th percentile and p < 0.05.
- Community feature significance: For each feature, a 2×2 contingency table is constructed, and Fisher's exact test applied to determine representative features of disease communities.
Table 1: Key Data Sources for OADS Implementation
| Data Category | Specific Sources | Application in OADS |
|---|---|---|
| Disease Vocabularies | Mondo, DO, MeSH, ICD-11, MEDIC, UMLS | Disease term standardization and hierarchy |
| Genetic Associations | OMIM, GeneRIF, GAD, CTD | Disease-gene relationships and pathway mapping |
| Transcriptomic Data | GEO datasets (GPL570/96/571), Single-cell platforms | Co-expression patterns and differential expression |
| Phenotypic Data | Human Phenotype Ontology (HPO) | Clinical manifestation similarities |
| Drug Databases | DrugBank, DrugCentral, TTD, PharmGKB, CTD | Therapeutic profile-based similarities |
Applications and Case Studies
Autoimmune and Autoinflammatory Disease Mapping
In a comprehensive study applying OADS to autoimmune and autoinflammatory diseases, network modularity analysis identified 10 robust disease communities and their representative phenotypes and dysfunctional pathways [5]. The research focused on 10 highly concerning AIIDs, including Behçet's disease and Systemic lupus erythematosus, providing insights into information flow from genetic susceptibilities to transcriptional dysregulation, alteration in immune microenvironment, and clinical phenotypes.
A key finding revealed that in systemic sclerosis and psoriasis, dysregulated genes like CCL2 and CCR7 contribute to fibroblast activation and the infiltration of CD4+ T and NK cells through IL-17 signaling pathway and PPAR signaling pathway, leading to skin involvement and arthritis [5]. This demonstrates how OADS can uncover shared mechanistic pathways between clinically distinct conditions.
Disease Comorbidity Pattern Analysis
OADS methodology has been successfully applied to reveal comorbidity patterns in complex diseases. In a study of hospitalized patients with COPD using large-scale administrative health data, network analysis identified 11 central diseases including disorders of glycoprotein metabolism as well as gastritis and duodenitis [42]. The study found that 96.05% of COPD patients had at least one comorbidity, with essential hypertension (40.30%) being the most prevalent.
The comorbidity network construction employed the Salton Cosine Index (SCI) for measuring disease co-occurrence strength:
where Nij represents the number of patients with both disease i and disease j, Ni and N_j represent the number of patients with only disease i or only disease j, respectively [42].
Table 2: OADS Applications in Disease Network Studies
| Application Domain | Key Findings | Reference |
|---|---|---|
| AIID Diseasome | Identified 10 disease communities with shared pathways; revealed CCL2/CCR7 dysregulation in systemic sclerosis and psoriasis | [5] |
| SLE Pathway Mapping | Developed SLE-diseasome with 4400 SLE-relevant functional pathways from 16 datasets and 11 pathway databases | [43] |
| COPD Comorbidities | Discovered 11 central comorbid conditions in COPD patients; identified sex-specific patterns (prostate hyperplasia in males, osteoporosis in females) | [42] |
| Cross-Disease Molecular Similarity | Revealed unexpected similarities between Alzheimer's disease and schizophrenia, asthma and psoriasis via transcriptomic profiling | [39] |
Biomarker Discovery and Drug Repurposing
The OADS framework facilitates biomarker discovery and therapeutic repurposing by identifying shared molecular features across diseases. For example, in Alzheimer's disease research, gene module-trait network analysis uncovered cell type-specific systems and genes relevant to disease progression [41]. The study highlighted astrocytic module 19 (ast_M19), associated with cognitive decline through a subpopulation of stress-response cells.
Similarly, the SLE-diseasome database provides a comprehensive collection of disease-relevant gene signatures developed using a multicohort approach integrating multiple layers of database-derived biological knowledge [43]. This resource enables patient stratification analysis and generation of machine learning models to predict clinical manifestations and drug response.
Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools for OADS Implementation
| Resource Category | Specific Tools/Databases | Function in OADS Pipeline |
|---|---|---|
| Ontology Databases | Gene Ontology, Cell Ontology, Human Phenotype Ontology, Disease Ontology | Semantic similarity computation and hierarchical relationship mapping |
| Bioinformatics Packages | DCGL, Seurat, SingleR, RDKit | Differential co-expression analysis, scRNA-seq processing, drug structure similarity |
| Network Analysis Tools | NetworkX, powerlaw library, Leiden algorithm | Network construction, topological analysis, community detection |
| Molecular Databases | OMIM, GEO, DrugBank, CTD, HMDD, miR2Disease | Source of disease-gene, drug, and molecular interaction data |
| Programming Environments | Python, R | Implementation of analysis pipelines and statistical computations |
The OADS framework represents a significant advancement in computational approaches to disease similarity assessment and diseasome network construction. By integrating multi-modal biological data with the rich semantic structures of biomedical ontologies, OADS enables more comprehensive and biologically meaningful disease relationship mapping than previous single-modality approaches.
Future developments in OADS methodology will likely incorporate additional data modalities, including proteogenomic data [44], and more sophisticated deep learning approaches [45]. As diseasome research evolves, OADS will play an increasingly important role in drug repurposing, patient stratification, and understanding the complex molecular interrelationships between seemingly distinct diseases.
The integration of artificial intelligence methods, particularly multimodal AI approaches that combine various data types, promises to further enhance the precision and predictive power of disease similarity frameworks [45]. These advancements will continue to bridge the gap between molecular insights and clinical applications, ultimately supporting the development of personalized therapeutic strategies.
Correlation networks provide a powerful framework for representing complex relationships among biomedical entities, serving as a foundational tool in the emerging discipline of network medicine. These networks have revolutionized how researchers understand human diseases from a network theory perspective, revealing hidden connections among apparently unconnected biomedical elements such as diseases, genes, proteins, and physiological processes. The intuitive nature of network representations has made them particularly valuable for identifying novel disease relationships and uncovering new therapeutic opportunities, most notably in the field of drug repurposing where existing medications can be applied to new indications [1]. This approach addresses the prolonged timelines and exorbitant costs associated with traditional drug development pipelines.
The construction of robust correlation networks faces a central challenge: transforming correlation matrix data into biologically meaningful networks. While approaches to this problem have been developed across diverse fields including genomics, neuroscience, and climate science, communication between practitioners in different domains has often been limited, leaving significant room for cross-disciplinary pollination [46]. The most widespread method—applying thresholds to correlation values to create unweighted or weighted networks—suffers from multiple methodological problems that can compromise network integrity and interpretability. This technical review examines current methodologies for constructing and analyzing correlation networks, with particular emphasis on their application to diseasome and disease network research.
Correlation Metrics for Network Construction
Fundamental Correlation Measures
The selection of appropriate correlation metrics represents the first critical step in network construction, directly influencing the biological plausibility of resulting network models. Different metrics capture distinct aspects of the relationships between variables, with choice dependent on data characteristics and research objectives.
Table 1: Correlation Metrics for Network Construction
| Metric | Mathematical Basis | Primary Applications | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Pearson Correlation | Linear relationship between continuous variables | Gene co-expression networks; Disease comorbidity networks | Simple interpretation; Computationally efficient | Sensitive to outliers; Only captures linear relationships |
| Partial Correlation | Linear relationship between two variables while controlling for others | Functional brain networks; Protein-protein interaction networks | Controls for indirect effects; Reveals direct relationships | Computationally intensive for high-dimensional data |
| Spectral Coherence | Frequency-specific synchronization | EEG/MEG functional connectivity; Oscillatory neural networks | Frequency-domain analysis; Captures rhythmic coordination | Requires stationary signals; Complex interpretation |
| Weighted Phase Lag Index (wPLI) | Phase synchronization resistant to volume conduction | EEG source connectivity; Neural oscillatory coupling | Reduces false connections from common sources; Robust to artifact | May miss true zero-lag connections |
Pearson correlation measures the linear relationship between two continuous variables, representing the most widely used correlation metric in network construction across diverse fields. Its computational efficiency and straightforward interpretation make it particularly suitable for initial exploratory analyses of large-scale biomedical datasets [46]. In disease network applications, Pearson correlation frequently forms the basis for disease similarity networks, where diseases are connected based on shared genetic signatures, comorbidity patterns, or clinical manifestations.
Partial correlation advances beyond simple bivariate correlation by measuring the relationship between two variables while controlling for the effects of other variables in the dataset. This approach is particularly valuable for distinguishing direct from indirect relationships in complex biological systems, helping to eliminate spurious correlations that may arise from confounding factors [46]. In genomics research, partial correlation networks have proven effective for reconstructing gene regulatory networks by controlling for the effects of transcription factors and other regulatory elements.
For neurophysiological data including EEG and MEG, phase-based synchronization metrics such as spectral coherence and the weighted Phase Lag Index (wPLI) offer advantages for capturing oscillatory coordination between brain regions. These metrics are particularly relevant for constructing functional brain networks in neurological and psychiatric disorders, where altered neural synchronization may underlie pathological states [47]. The wPLI specifically addresses the problem of volume conduction in electrophysiological recordings, providing a more accurate representation of true functional connectivity by reducing false connections arising from common sources.
Advanced Correlation and Covariance Approaches
Beyond basic correlation measures, several advanced techniques have been developed to address specific challenges in network construction from high-dimensional biomedical data.
The graphical lasso (graphical least absolute shrinkage and selection operator) employs L1-regularization to estimate sparse inverse covariance matrices, effectively performing simultaneous network construction and regularization [46]. This approach is particularly valuable for high-dimensional datasets where the number of variables exceeds the number of observations, a common scenario in genomics and transcriptomics research. By promoting sparsity in the inverse covariance matrix, the graphical lasso automatically zeros out weak or spurious connections, resulting in more interpretable network structures.
Covariance selection methods extend beyond correlation to model both direct and indirect dependencies among variables, providing a more comprehensive representation of system architecture [46]. These approaches are particularly relevant for pathway analysis in disease networks, where both direct molecular interactions and indirect functional relationships contribute to disease mechanisms.
Significance Thresholding Methods
Thresholding Approaches and Their Limitations
Network thresholding represents a critical methodological step aimed at eliminating weak or spurious connections from correlation networks to reveal meaningful biological architecture. However, the choice of thresholding approach and specific threshold levels significantly impacts resulting network topology and biological interpretation.
Table 2: Network Thresholding Methods and Properties
| Method | Description | Typical Application Range | Effect on Network Architecture | Biological Interpretation |
|---|---|---|---|---|
| Absolute Thresholding | Retains connections above a fixed correlation value | Correlation 0.1-0.8 (fMRI); Varies by field | Preserves strongest connections; May yield different densities across subjects | Straightforward but may eliminate biologically relevant weak connections |
| Proportional Thresholding | Retains top X% of connections by weight | 2-40% (fMRI); Often ~30% for brain networks | Ensures uniform density across subjects; Facilitates group comparisons | Maintains network sparsity comparable to biological systems |
| Consistency Thresholding | Retains connections with low inter-subject variability | 20-40% density for structural brain networks | Focuses on reproducible connections; Reduces measurement noise | Identifies core conserved architecture; May eliminate subject-specific features |
Absolute thresholding applies a uniform correlation value across all subjects or datasets, retaining only connections exceeding this predetermined cutoff. While methodologically straightforward, this approach fails to account for individual differences in overall connectivity strength, potentially resulting in networks with inconsistent densities across subjects [47]. In functional MRI research, absolute thresholds have varied from 0.1 to 0.8 correlation coefficients, leading to significant challenges in comparing results across studies [47].
Proportional thresholding (also called density-based thresholding) addresses the density variability problem by retaining a fixed percentage of strongest connections in each network [48]. This approach ensures uniform network density across subjects, facilitating group comparisons and statistical analyses. However, proportional thresholding may eliminate meaningful biological information by discarding potentially important weak connections that fall below the density cutoff.
Consistency-based thresholding represents a more sophisticated approach that retains connections demonstrating low inter-subject variability on the assumption that connections with high variability are more likely to represent measurement noise or spurious findings [48]. This method specifically addresses the challenge of distinguishing genuine biological connections from artifacts introduced by the measurement process itself, particularly relevant for techniques with inherent noise such as diffusion MRI tractography.
Experimental Evidence on Thresholding Effects
Empirical investigations have demonstrated the profound impact of threshold selection on network properties and their relationships with biological variables. In a large-scale study of structural brain networks involving 3,153 participants from the UK Biobank Imaging Study, researchers systematically evaluated how thresholding methods affect age-associations in network measures [48].
The experimental protocol applied both proportional and consistency thresholding across a broad range of threshold levels (retaining 10-90% of connections) to whole-brain structural networks constructed using six different diffusion MRI weightings. For each threshold level and weighting combination, researchers computed four common network measures: mean edge weight, characteristic path length, network efficiency, and network clustering coefficient [48].
The key finding revealed that threshold stringency exerted a stronger influence on age-associations than the specific choice of threshold method. More stringent thresholding (retaining 30% or fewer connections) generally resulted in stronger age-associations across five of the six network weightings, except at the highest levels of sparsity (>90% threshold) where crucial biological connections were removed [48]. This pattern suggests that stringent thresholding effectively eliminates noise, enhancing sensitivity to biological effects such as age-related degeneration in white matter connectivity.
Complementary evidence from EEG functional connectivity research demonstrates similar threshold-dependence of network properties. Analysis of 146 resting-state EEG recordings revealed significant changes in global network measures including characteristic path length, clustering coefficient, and small-world index across different threshold levels [47]. These threshold-induced dynamics showed substantial linear trends (R-squared values 0.1-0.97, median 0.62), indicating that threshold selection systematically biases network quantification [47].
Network Construction and Thresholding Workflow
Integrated Protocols for Disease Network Construction
Experimental Protocol for Structural Brain Network Analysis
The UK Biobank imaging study provides a robust protocol for constructing structural brain networks with application to neurodegenerative disease research [48]. This protocol can be adapted for various disease network applications with appropriate modification.
Data Acquisition and Preprocessing:
- Acquire diffusion MRI data using standardized acquisition protocols (e.g., 96-direction diffusion-sensitizing gradient scheme)
- Perform eddy current correction and head motion correction using FSL or similar preprocessing pipelines
- Reconstruct white matter pathways using probabilistic tractography (e.g., FSL's PROBTRACKX with 5000 streamlines per seed voxel)
- Parcellate brain into 85 cortical and subcortical regions using standardized atlases (e.g., Harvard-Oxford atlas)
Network Construction:
- Define network nodes according to brain parcellation regions
- Compute connection weights between nodes using one or more diffusion metrics:
- Streamline count: Number of reconstructed streamlines connecting regions
- Fractional anisotropy (FA): Mean FA along connecting pathways
- Mean diffusivity (MD): Mean MD along connecting pathways
- Neurite density (ICVF): Intra-cellular volume fraction from NODDI
- Orientation dispersion (OD): Neurite orientation dispersion from NODDI
- Construct individual 85×85 structural connectivity matrices for each participant
Thresholding Application:
- Apply consistency thresholding by computing inter-subject variability of each connection and retaining least variable connections
- Apply proportional thresholding by retaining top X% of connections by weight
- Implement both approaches across a range of threshold levels (e.g., 10%-90% in 5% increments)
- Compute network metrics at each threshold level for comparison
Validation and Statistical Analysis:
- Assess criterion validity by correlating network metrics with age across threshold levels
- Compare effect sizes (β coefficients) of age-associations across methods and threshold stringency
- Evaluate reproducibility using split-half validation or bootstrapping approaches
Protocol for EEG Functional Connectivity in Disease States
Research on EEG graph theoretical metrics provides a complementary protocol for functional connectivity analysis in neurological and psychiatric disorders [47].
Data Acquisition and Preprocessing:
- Record resting-state EEG using standardized systems (e.g., 64-channel EEG caps with 500-1000 Hz sampling rate)
- Apply band-pass filtering (e.g., 0.5-70 Hz) and notch filtering (50/60 Hz) to remove line noise
- Perform artifact removal using independent component analysis (ICA) or automated algorithms
- For source-space analysis, compute source reconstruction using inverse modeling (e.g., sLORETA, beamforming)
Functional Connectivity Calculation:
- Compute connectivity matrices using multiple synchronization metrics:
- Weighted phase lag index (wPLI): Phase synchronization resistant to volume conduction
- Imaginary coherence (ImCoh): Complex coherence focusing on non-zero phase lag components
- Spectral coherence: Frequency-domain correlation between signals
- Corrected imaginary phase locking value (ciPLV): Phase-based metric correcting for artificial correlations
- Pairwise phase consistency (PPC): Phase consistency across trials
- Calculate connectivity matrices for standard frequency bands (delta, theta, alpha, beta, gamma)
Thresholding and Graph Analysis:
- Apply proportional thresholding from 10% to 90% in 1% increments
- Compute graph theory metrics at each threshold level:
- Characteristic path length: Average shortest path between node pairs
- Clustering coefficient: Likelihood neighbors connect to each other
- Participiation coefficient: Diversity of inter-modular connections
- Small-world index: Balance between segregation and integration
- Track changes in metrics across threshold levels and identify stability ranges
Statistical Validation:
- Perform linear regression to quantify variance explained by threshold level
- Compute correlation matrices of graph metrics across different thresholds
- Construct edge probability graphs to identify stable connections across thresholds
Visualization and Analysis Tools
The construction and analysis of correlation networks requires specialized software tools that accommodate the unique characteristics of network data and support the implementation of appropriate thresholding methods.
Table 3: Network Visualization and Analysis Tools
| Tool | Primary Application Domain | Key Features | Thresholding Implementation | Strengths for Disease Networks |
|---|---|---|---|---|
| Gephi | General network visualization | Interactive exploration; Force-directed layouts | Plugin architecture for custom thresholding | Intuitive visual analytics; Community detection |
| Cytoscape | Biological network analysis | Extensive app ecosystem; Molecular profiling | Built-in thresholding filters; Advanced filtering options | Biological data integration; Pathway visualization |
| NodeXL | Social network analysis | Excel integration; Social media data import | Edge weight filtering; Automated layout algorithms | Accessibility for non-specialists; Reporting features |
| Graphia | Large-scale biological data | Kernel-based visualization; Correlation networks | Quality thresholding; Data-driven filtering | Handles large datasets; Customizable analysis pipelines |
| Retina | Web-based network sharing | Browser-based; No server requirements | Client-side filtering; Interactive exploration | Collaboration features; Easy sharing of networks |
Gephi serves as a versatile tool for exploratory network analysis, functioning as "Photoshop for graph data" by allowing interactive manipulation of network structures, shapes, and colors to reveal hidden patterns [49]. Its plugin architecture supports implementation of custom thresholding algorithms, while force-directed layouts facilitate intuitive visualization of correlation-based networks.
Cytoscape specializes in biological network analysis, particularly valuable for disease networks through its extensive app ecosystem that enables integration of molecular profiling data, pathway information, and functional annotations [49]. The platform offers built-in thresholding filters and advanced filtering options specifically designed for biological network construction and analysis.
For researchers requiring web-based solutions, Retina provides a free open-source application for sharing network visualizations online without server requirements [49]. This tool enables collaborative exploration of thresholding effects and facilitates sharing of correlation networks across research teams, particularly valuable for multi-center disease network studies.
Application to Diseasome and Disease Network Research
Disease Network Concepts and Methodological Considerations
Network medicine represents a paradigm shift in understanding human disease, conceptualizing disorders not as independent entities but as interconnected elements within a complex "diseasome" network [1]. This perspective reveals that seemingly distinct diseases often share common genetic architectures, molecular pathways, or environmental triggers, explaining frequently observed disease co-occurrence patterns.
The construction of robust disease networks requires careful consideration of several methodological factors specific to biomedical applications. First, the selection of appropriate correlation metrics must align with data types and biological questions—genetic similarity networks may employ different measures than clinical comorbidity networks or protein interaction networks. Second, threshold selection must balance biological plausibility with statistical rigor, as over-thresholding may eliminate meaningful weak connections that represent important disease relationships. Third, validation approaches must incorporate biological criterion validity, assessing whether network properties correlate with established disease biomarkers or clinical outcomes.
Implementation in Drug Repurposing
Correlation-based disease networks have demonstrated particular utility in drug repurposing, where existing medications are applied to new disease indications [1]. By identifying unanticipated connections between seemingly unrelated diseases, network approaches reveal novel therapeutic opportunities that would likely remain undiscovered through conventional reductionist methods.
The implementation typically involves constructing disease similarity networks based on shared genetic variants, protein interactions, or clinical manifestations, then identifying closely connected disease modules that might share therapeutic vulnerabilities. Successful applications of this approach have identified new uses for existing medications across diverse conditions including cancer, inflammatory disorders, and neurological diseases, significantly reducing the time and cost associated with traditional drug development pipelines.
Disease Network Analysis Decision Pipeline
Research Reagent Solutions
The construction and analysis of correlation networks in disease research requires both computational tools and conceptual frameworks. The following essential "research reagents" represent critical components for implementing robust network construction and thresholding methodologies.
Table 4: Essential Research Reagents for Correlation Network Construction
| Reagent Category | Specific Tools/Approaches | Function in Network Construction | Application Notes |
|---|---|---|---|
| Statistical Computing | R (igraph, brainGraph, qgraph); Python (NetworkX, nilearn) | Implementation of correlation metrics and thresholding algorithms | R preferred for reproducibility; Python for scalability |
| Network Visualization | Gephi, Cytoscape, Graphia, Retina | Visual exploration and communication of network structures | Gephi for publication-quality figures; Cytoscape for biological annotation |
| Thresholding Algorithms | Proportional thresholding; Consistency-based methods; Statistical significance testing | Elimination of spurious connections; Noise reduction | Consistency methods preferred for measurement-noisy data |
| Validation Frameworks | Criterion validity analysis; Biological plausibility assessment; Resampling methods | Ensuring network robustness and biological relevance | Age-associations effective for neurological applications |
| Specialized Biomarkers | Diffusion MRI metrics; Genetic similarity measures; Clinical comorbidity indices | Domain-specific correlation calculation | Multiple biomarkers strengthen network validity |
Statistical Computing Environments provide the foundational infrastructure for implementing correlation metrics and thresholding algorithms. The R programming language offers extensive packages specifically designed for network analysis, including igraph for general network manipulation, brainGraph for neuroimaging-specific applications, and qgraph for psychological network construction [50]. Python alternatives including NetworkX and nilearn provide similar functionality with particular strengths in handling large-scale datasets and integration with machine learning pipelines.
Thresholding Algorithms represent methodological reagents for distinguishing meaningful biological connections from measurement noise. Proportional thresholding ensures consistent network density across subjects, facilitating group comparisons in disease studies [48]. Consistency-based methods leverage inter-subject variability to identify reproducible connections, particularly valuable for clinical populations where disease heterogeneity may complicate analysis [48]. Statistical significance testing based on permutation or parametric approaches provides objective criteria for connection retention, though may require modification to address multiple comparison problems in high-dimensional network data.
Validation Frameworks serve as essential quality control reagents for ensuring network robustness and biological relevance. Criterion validity analysis correlates network properties with established biological variables such as age in brain networks [48]. Biological plausibility assessment compares network connections with established anatomical or functional knowledge, while resampling methods including bootstrapping and cross-validation evaluate network stability across different data subsets.
Autoimmune and Autoinflammatory Diseases (AIIDs) represent a broad spectrum of disorders characterized by a loss of immune tolerance and dysregulated inflammation, leading to organ-specific or systemic damage [5] [51]. Historically classified into autoimmune diseases (ADs), involving adaptive immune dysregulation, and autoinflammatory diseases (AIDs), driven by innate immune imbalances, this distinction is increasingly viewed as a spectrum where both components variably contribute to pathogenesis [5]. With over 10% of the population affected by at least one of the 19 common autoimmune diseases, and approximately 25% of AIID patients developing a second autoimmune condition, the comorbidity and heterogeneity present significant challenges for understanding mechanisms and classification [5] [16].
The systematic exploration of disease relationships, known as the "diseasome," provides a network-based approach to unravel this complexity. Diseasome studies aim to construct disease association networks to uncover shared pathogenesis, predict disease progression, and optimize therapeutics [52] [51]. However, AIID diseasome research remains in its nascent stages, with prior studies limited by narrow disease scopes or restricted data types [5]. This case study addresses these gaps by presenting a comprehensive framework that integrates multi-modal data and biomedical ontologies to construct and analyze an AIID association network encompassing 484 ADs and 110 AIDs, offering unprecedented scale and mechanistic insights.
Materials and Methods
Disease Terminology Curation and Repository Construction
We integrated disease terms from seven authoritative sources to build a comprehensive AIID repository:
- General Disease Ontologies: Mondo Disease Ontology (v2024-04-02), Disease Ontology (DO, v2024-03-26), Medical Subject Headings (MeSH, v2023-11-16), and the International Classification of Diseases (ICD-11, 2023).
- Specialized AIID Databases: The Autoimmune Association (AA), Autoimmune Registry, Inc. (ARI), and the Global Autoimmune Institute (GAI) [5] [51].
This integration yielded a final repository containing 484 Autoimmune Diseases (ADs), 110 Autoinflammatory Diseases (AIDs), 14 contested diseases, and 284 diseases associated with existing AIIDs [5].
Multi-Modal Data Acquisition and Processing
To capture disease relationships across biological scales, we curated and processed multiple data types:
- Genetic Data: Disease-associated genes were obtained from OMIM and other genetic databases.
- Transcriptomic Data: Bulk gene expression data were curated from Affymetrix U133A platforms (GPL570/96/571) in the Gene Expression Omnibus (GEO), filtered for disease/control groups with ≥5 samples each from relevant tissues (PBMCs, whole blood, skin) [5] [51]. Single-cell RNA sequencing (scRNA-seq) data were obtained from five major platforms (GPL24676/18573/16791/11154/20301) via GEO searches using disease synonyms.
- Phenotypic Data: Clinical phenotypic terms were extracted from the Human Phenotype Ontology (HPO).
Normalized AIID Classification Score (ACS)
To quantitatively position each disease on the autoimmune-autoinflammatory spectrum, we calculated a normalized AIID Classification Score (ACS~norm~) as a weighted, continuous metric on the interval [-1, +1] [5] [51]. The formula is:
ACS~norm~ = Σ (w~i~ * s~i~) / Σ w~i~ [5] [51]
Where for each source i, s~i~ denotes the classification (autoimmune = +1, unclassified = 0, autoinflammatory = -1) and w~i~ is a pre-defined confidence weight based on the source's coverage, update frequency, and community endorsement (e.g., Mondo=1.0, DO=0.8, MeSH=0.7, ICD=0.7, expert panel lists=1.0) [5] [51].
Ontology-Aware Disease Similarity (OADS) Calculation
A novel Ontology-Aware Disease Similarity (OADS) strategy was developed to compute disease relationships, incorporating both multi-modal data and the hierarchical structure of biomedical ontologies [5] [51].
- Gene Ontology (GO) Similarity: Disease-related genes (from OMIM) and dysregulated genes (from differential co-expression analysis using the DCGL package) were mapped to GO Biological Process terms. The top 20 GO terms per disease were retained, and functional similarity was computed using the Wang method, followed by FunSimAvg aggregation to derive a final disease similarity score [5] [51].
- Cellular-Level Similarity: scRNA-seq data were processed through the Seurat pipeline for quality control, normalization, and clustering. Cell types were annotated using SingleR, and cellular similarities between diseases were calculated using CellSim based on the Cell Ontology [5].
- Phenotypic Similarity: Phenotypic terms from HPO were used to compute similarity between diseases using the Wang method [5].
Network Construction and Modularity Analysis
Disease association networks were constructed in Python using the NetworkX library. Networks were built by connecting diseases with edge similarity scores above the 90th percentile and statistical significance (p < 0.05), determined through permutation testing (500 shuffles) [5] [51]. Disease communities (modules) within the integrated network were identified using a combination of hierarchical clustering (Ward's method) and the Leiden algorithm (resolution=1.0) [5] [51].
Topological and Functional Analysis
Network topological properties—including degree, betweenness centrality, closeness centrality, eigenvector centrality, clustering coefficient, transitivity, k-core, and network diameter—were calculated using NetworkX [5]. The power-law characteristics of the degree distribution were evaluated using the powerlaw library [5]. To identify representative features (pathways, cell types, phenotypes) of each disease community, we performed Fisher's exact test on feature frequency counts, with significance set at p < 0.05 after Benjamini-Hochberg correction [5] [51].
Results
The Integrated AIID Diseasome Network
The integration of multi-modal data through the OADS framework produced a cohesive AIID diseasome network. Topological analysis revealed that the network exhibits properties of a complex biological system, with a degree distribution suggestive of power-law behavior, indicating the presence of highly connected "hub" diseases [5]. The network's Within-Network Distance (WiND), defined as the mean shortest path length among all connected nodes, described the overall closeness and connectivity of the disease relationships [5].
Table 1: Summary of the Constructed AIID Repository
| Category | Number of Diseases | Description |
|---|---|---|
| Autoimmune Diseases (ADs) | 484 | Diseases primarily involving dysregulation of the adaptive immune system. |
| Autoinflammatory Diseases (AIDs) | 110 | Diseases primarily driven by innate immune system dysregulation. |
| Contested Diseases | 14 | Diseases with conflicting or unclear classification. |
| Associated Diseases | 284 | Non-AIIDs with known associations to AIIDs. |
Table 2: Multi-Modal Evidence Layers for Network Construction
| Data Modality | Data Source | Key Metrics/Outputs |
|---|---|---|
| Genetic | OMIM, GWAS studies | Disease-associated genes and variants. |
| Bulk Transcriptomic | Affymetrix U133A (GEO) | Differentially expressed genes (DEGs), differential co-expression (dC). |
| Single-Cell Transcriptomic | Multiple scRNA-seq platforms (GEO) | Cell type proportions, differentially expressed genes per cell type. |
| Phenotypic | Human Phenotype Ontology (HPO) | Clinical symptom and sign profiles. |
| Drug-Based | DrugBank, PharmGKB, CTD | Drug structural similarity, drug-disease associations. |
Disease Communities and Their Characteristic Features
Modularity analysis of the integrated network identified 10 robust disease communities. Each community was enriched for distinct combinations of dysfunctional pathways, cell types, and clinical phenotypes, providing a data-driven re-classification of AIIDs.
Table 3: Characterization of Select AIID Network Communities
| Community | Representative Diseases | Dysregulated Pathways | Key Immune Cells | Representative Phenotypes |
|---|---|---|---|---|
| Community 1 | Systemic Sclerosis, Psoriasis | IL-17 signaling, PPAR signaling | CD4+ T cells, NK cells, Fibroblasts | Skin involvement, Arthritis [5] |
| Community 2 | Behçet's disease, SLE | Type I Interferon signaling, TLR signaling | Plasmacytoid DCs, B cells | Oral ulcers, Photosensitivity [5] |
| Community 3 | Rheumatoid Arthritis, JIA | JAK-STAT signaling, T cell receptor signaling | CD8+ T cells, Macrophages | Synovitis, Joint erosion |
| Community 4 | Crohn's Disease, Ulcerative Colitis | IL-23/Th17 pathway, Autophagy | Th17 cells, Paneth cells | Abdominal pain, Diarrhea |
Cross-Scale Mechanism: From Genetics to Phenotype
The multi-layered network enables the tracing of pathogenic information flow across biological scales. A prime example is the comorbidity between Systemic Sclerosis and Psoriasis within the same network community. The analysis revealed that shared dysregulation of genes such as CCL2 and CCR7 contributes to fibroblast activation and the infiltration of CD4+ T and NK cells through the IL-17 signaling pathway and PPAR signaling pathway, ultimately manifesting in shared clinical phenotypes like skin involvement and arthritis [5].
Experimental Workflow for AIID Diseasome Construction
Cross-Scale Pathogenesis in Sclerosis & Psoriasis
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Resources for AIID Diseasome Studies
| Reagent / Resource | Function / Application | Specific Examples / Notes |
|---|---|---|
| Disease Ontologies | Standardized disease terminology and relationships. | Mondo, Disease Ontology (DO), MeSH, ICD-11 [5] [51]. |
| Gene Expression Data | Profiling transcriptomic dysregulation in diseases. | Affymetrix U133A platforms (GPL570/96/571) from GEO [5]. |
| Single-Cell RNA-seq Platforms | Characterizing cellular heterogeneity and immune cell dynamics. | Platforms GPL24676, GPL18573, GPL16791, GPL11154, GPL20301 [5]. |
| Bioinformatics Software (R/Python) | Data processing, analysis, and network construction. | DCGL (R), Seurat (R), SingleR (R), NetworkX (Python), powerlaw (Python) [5] [51]. |
| Functional Ontologies | Defining and comparing biological processes, phenotypes, and cell types. | Gene Ontology (GO), Human Phenotype Ontology (HPO), Cell Ontology (CL) [5]. |
| Drug-Disease Databases | Informing drug repurposing and therapeutic similarity. | DrugBank, DrugCentral, TTD, PharmGKB, CTD [5]. |
This study establishes a comprehensive, multi-modal diseasome network for Autoimmune and Autoinflammatory Diseases, addressing a significant gap in network medicine. The integration of 484 ADs and 110 AIDs, combined with an ontology-aware similarity framework, provides a more nuanced and accurate map of disease relationships than previously possible.
The identification of 10 robust disease communities offers a data-driven alternative to traditional disease classification, suggesting that shared mechanisms cut across conventional diagnostic boundaries. This is powerfully illustrated by the revealed shared pathways between Systemic Sclerosis and Psoriasis, diseases not typically linked in clinical practice [5]. These findings have direct implications for drug repurposing and the development of targeted therapies that could benefit multiple conditions within a network community.
This AIID diseasome resource serves as a foundational framework for generating new biological hypotheses, understanding the molecular basis of comorbidity, and accelerating translational research. Future work will focus on the dynamic tracking of disease progression within the network and the integration of additional data modalities, such as proteomics and metabolomics, to further refine our understanding of the interconnected landscape of autoimmune and autoinflammatory diseases.
Drug Repurposing and Novel Therapeutic Target Identification Through Network Analysis
The human diseasome is a network representation of the complex relationships between diseases, genes, and their molecular components, forming the foundation of the discipline known as network medicine [53]. This approach conceptualizes human diseases not as independent entities but as interconnected nodes within a large cellular network, where the connectivity between molecular parts translates into relationships between related disorders [53]. Analyzing these networks provides a powerful framework for identifying new therapeutic uses for existing drugs, an approach known as drug repurposing [1]. This methodology offers significant advantages over traditional drug development, reducing both the time to market (from 10-15 years to approximately 6 years) and development costs (from approximately $2.6 billion to around $300 million per drug) by leveraging existing preclinical and clinical safety data [54].
Network-based drug repurposing operates on the principle that drugs located closer to the molecular site of a disease within biological networks tend to be more suitable therapeutic candidates than those lying farther away from the molecular target [54]. The practice has gained substantial momentum with advances in artificial intelligence (AI) and network science, enabling researchers to systematically analyze millions of potential drug-disease combinations to identify the most viable candidates [55] [54]. This technical guide explores the methodologies, experimental protocols, and analytical frameworks for leveraging diseasome networks in drug repurposing and target identification, contextualized within the broader research on human disease networks.
Data Compilation and Curation
Constructing a comprehensive drug-disease network requires integrating multiple data sources to establish robust connections between pharmacological compounds and disease pathologies. A proven methodology involves combining existing textual and machine-readable databases, natural language processing tools, and manual hand curation to create a bipartite network of drugs and diseases [55]. This network structure consists of two distinct node types—drugs and diseases—with edges representing only therapeutic indications between unlike node types.
Table 1: Primary Data Sources for Drug-Disease Network Construction
| Data Category | Specific Sources | Data Content | Application in Network Construction |
|---|---|---|---|
| Machine-Readable Databases | DrugBank, ClinicalTrials.gov | Structured drug-disease indications, targets, mechanisms | Forms the core adjacency matrix for the bipartite network |
| Textual Resources | Scientific literature, clinical guidelines | Unstructured therapeutic relationships | NLP extraction of explicit drug-disease indications |
| Validation Sources | FDA labels, EMA approvals | Verified therapeutic indications | Hand curation and data quality assurance |
The resulting network architecture represents drugs and diseases as interconnected nodes, where a connection between a drug node and a disease node indicates a validated therapeutic indication for that condition. In one implementation, this approach yielded a network comprising 2620 drugs and 1669 diseases, significantly larger and more complete than previous datasets [55]. A critical differentiator of this methodology is its reliance solely on explicit therapeutic drug-disease indications, avoiding associations inferred indirectly from drug function, targets, or structure, which enhances the predictive accuracy of subsequent analyses.
Network Representation
The fundamental structure of the drug-disease network is bipartite, consisting of two disjoint sets of nodes (drugs and diseases) where edges only connect nodes from different sets. This representation captures the complex relationship patterns while maintaining computational tractability for analysis.
Network Analysis Methodologies
Link Prediction Algorithms
Link prediction methods form the computational core of network-based drug repurposing, systematically identifying potential missing therapeutic relationships within the bipartite drug-disease network. These algorithms leverage the existing network structure to predict undiscovered drug-disease associations with high statistical confidence.
Table 2: Link Prediction Algorithms for Bipartite Drug-Disease Networks
| Algorithm Category | Specific Methods | Underlying Principle | Performance Metrics (AUC/Precision) |
|---|---|---|---|
| Similarity-Based | Common Neighbors, Jaccard Coefficient | Network proximity and topological overlap | Moderate (0.75-0.85 AUC) |
| Graph Embedding | node2vec, DeepWalk | Low-dimensional vector representation of nodes | High (>0.90 AUC) |
| Matrix Factorization | Non-negative Matrix Factorization | Dimensionality reduction of adjacency matrix | High (0.85-0.95 AUC) |
| Network Model Fitting | Degree-corrected stochastic block model | Statistical inference of network community structure | Highest (>0.95 AUC) |
Cross-validation tests demonstrate that several link prediction methods, particularly those based on graph embedding and network model fitting, achieve exceptional performance in identifying drug repurposing opportunities, with area under the ROC curve exceeding 0.95 and average precision almost a thousand times better than chance [55]. These methods operate on the principle that the observed network data are inherently incomplete, and that missing edges (therapeutic relationships) can be identified through mathematical regularities and patterns within the existing network structure.
AI and Machine Learning Approaches
Artificial intelligence, particularly machine learning (ML) and deep learning (DL), significantly enhances network-based drug repurposing by enabling the analysis of complex, high-dimensional data relationships that exceed human analytical capacity. Supervised ML algorithms – including Logistic Regression (LR), Support Vector Machine (SVM), Random Forest (RF), and Artificial Neural Networks (ANN) – train on known drug-disease associations to predict new therapeutic indications [54]. These models integrate diverse data modalities, including chemical structures, genomic associations, and clinical outcomes, to identify non-obvious relationships between existing drugs and novel disease applications.
Deep learning architectures further extend these capabilities through multilayer neural networks that automatically extract hierarchical features from raw input data. Convolutional Neural Networks (CNNs) process structural drug information, while Long Short-Term Memory Recurrent Neural Networks (LSTM-RNNs) analyze temporal patterns in disease progression and drug response [54]. These AI-driven approaches excel at identifying complex, non-linear relationships within heterogeneous biological data, enabling the discovery of repurposing opportunities that evade traditional analytical methods.
Experimental Protocols and Validation
Experimental Workflow for Network-Based Drug Repurposing
The systematic identification of drug repurposing candidates through network analysis follows a structured workflow encompassing data integration, network construction, computational analysis, and experimental validation.
Cross-Validation Protocol
Rigorous validation of prediction accuracy employs cross-validation tests where a fraction of known drug-disease edges are systematically removed from the network, and algorithm performance is measured by the ability to correctly identify these removed connections [55]. The standard protocol involves:
- Network Partitioning: Randomly select 10-20% of known therapeutic edges as test cases, removing them from the training network.
- Algorithm Training: Apply link prediction algorithms to the remaining network to learn topological patterns and association rules.
- Prediction Generation: Compute similarity scores or connection probabilities for all possible drug-disease pairs in the test set.
- Performance Quantification: Calculate standard metrics including Area Under the ROC Curve (AUC-ROC), Average Precision (AP), and precision-recall curves to evaluate prediction accuracy.
- Statistical Validation: Compare algorithm performance against random chance baselines and previously published methods to establish significance.
This validation framework ensures that reported performance metrics reflect real-world predictive power and provides a standardized approach for comparing different computational methodologies.
Successful implementation of network-based drug repurposing requires specific computational tools, data resources, and experimental materials for validation studies.
Table 3: Essential Research Resources for Network-Driven Drug Repurposing
| Resource Category | Specific Resources | Function and Application |
|---|---|---|
| Computational Tools | NetworkX, igraph, node2vec | Network construction, analysis, and graph embedding algorithms |
| Data Repositories | DrugBank, ClinicalTrials.gov, DisGeNET | Source data for drug targets, disease associations, and clinical evidence |
| Bioinformatics Platforms | Cytoscape, Gephi, STRING | Network visualization and integration with biological pathway data |
| Experimental Validation | Cell lines (ATCC), animal models, clinical samples | In vitro and in vivo confirmation of predicted drug-disease associations |
| Reporting Standards | SMART Protocols Ontology, MIACA guidelines | Standardized documentation of experimental protocols and results |
Adherence to established reporting standards, such as those defined by the SMART Protocols Ontology, ensures reproducibility and facilitates the integration of findings across research groups [56]. This ontology defines 17 fundamental data elements necessary for experimental protocol documentation, including detailed descriptions of reagents, equipment, workflow steps, and analytical parameters that enable exact reproduction of computational and experimental results.
Case Studies and Clinical Applications
Therapeutic Area Applications
Network-based drug repurposing has demonstrated particular utility in therapeutic areas with high unmet medical need, including oncology, neurodegenerative disorders, and rare diseases [54]. In oncology, diseasome networks have revealed unexpected connections between seemingly distinct cancer types based on shared molecular pathways, enabling the repositioning of targeted therapies across cancer indications. For neurodegenerative diseases, network analysis has identified common pathological mechanisms between neurological and non-neurological conditions, suggesting novel applications for existing drugs.
The COVID-19 pandemic provided a compelling case study in rapid network-based repurposing, where existing drugs including baricitinib (originally approved for rheumatoid arthritis) were identified and validated as effective treatments through analysis of their position within molecular interaction networks relative to SARS-CoV-2 pathogenesis pathways [54]. This demonstration highlights the potential of network methodologies to accelerate therapeutic development during public health emergencies.
Implementation Challenges and Solutions
Despite promising results, several challenges persist in the implementation of network-based drug repurposing. Data quality and completeness remain significant concerns, as missing or erroneous annotations in source databases can propagate through analyses and compromise prediction accuracy. Potential solutions include the implementation of rigorous data curation protocols and the development of algorithms specifically designed to handle network incompleteness.
Biological validation of computational predictions represents another implementation hurdle, as the translation of network-derived hypotheses to clinically relevant therapies requires substantial experimental evidence. The establishment of standardized validation pipelines – incorporating in vitro assays, animal models, and carefully designed clinical trials – provides a framework for efficiently prioritizing and testing the most promising repurposing candidates.
Network analysis provides a powerful, systematic framework for drug repurposing and therapeutic target identification by leveraging the intrinsic connectivity of the human diseasome. The integration of link prediction algorithms, machine learning methods, and experimental validation creates a robust pipeline for discovering novel therapeutic applications of existing drugs, significantly reducing the time and cost associated with traditional drug development.
Future advancements in this field will likely emerge from several key areas: the integration of multi-omics data into expanded network representations, the development of temporal networks that capture disease progression dynamics, and the implementation of explainable AI methods that provide biological insight alongside computational predictions. As these methodologies mature, network-based drug repurposing will increasingly become a cornerstone of pharmaceutical development, enabling the efficient discovery of new therapies for diseases with high unmet need.
Biomarker Discovery and Patient Stratification via Comorbidity Pattern Analysis
The concept of the diseasome, which visualizes human diseases as a complex network of biologically related entities, has fundamentally transformed our understanding of disease mechanisms and interrelationships. Within this framework, comorbidity patterns represent clinically observable manifestations of underlying shared biological pathways connecting distinct medical conditions. The systematic analysis of these patterns provides a powerful approach for identifying novel biomarkers and enabling precise patient stratification in both clinical research and therapeutic development. This technical guide examines current methodologies for leveraging comorbidity pattern analysis to advance biomarker discovery, with particular emphasis on computational approaches, experimental validation, and clinical implementation strategies relevant to researchers and drug development professionals.
The network-based understanding of disease has evolved significantly over the past decade, revealing that seemingly distinct disorders often share common genetic foundations, molecular pathways, and environmental influences [1]. These connections form the basis of the "diseasome network" concept, which provides a systematic framework for mapping relationships between diseases through shared molecular mechanisms. By analyzing comorbidity patterns within this network context, researchers can identify critical nodes and pathways that serve as ideal targets for biomarker development and therapeutic intervention [1]. This approach moves beyond traditional single-disease models to embrace the biological complexity of patient populations, particularly those with multimorbidity presentations.
Theoretical Foundation: Diseasome Networks and Comorbidity Analysis
Diseasome Network Principles and Architecture
Diseasome networks construct mathematical representations of disease relationships based on shared genetic factors, protein interactions, metabolic pathways, and clinical manifestations. In these networks, diseases function as nodes, while edges represent shared biological mechanisms between them. The strength of these connections can be quantified using various similarity measures, including gene overlap coefficients, protein-protein interaction distances, and epidemiological comorbidity indices. Analysis of densely interconnected regions within these networks, often called "disease modules," has revealed that diseases sharing more molecular features tend to exhibit higher comorbidity rates in patient populations [1].
The architectural properties of diseasome networks demonstrate scale-free topology, meaning most diseases have few connections while a minority serve as highly connected hubs. These hub diseases typically involve fundamental cellular processes and pathways, explaining their associations with diverse clinical conditions. From a biomarker perspective, these hubs represent priority targets for discovering master regulatory biomarkers with broad diagnostic and prognostic utility across multiple conditions. The application of network theory to human disease has created unprecedented opportunities for identifying biomarkers that reflect shared pathophysiology rather than isolated diagnostic categories [1].
Comorbidity Patterns as Clinical Signatures of Network Topology
Comorbidity patterns observed in clinical populations represent the practical manifestation of underlying diseasome network topology. Systematic analysis of these patterns using electronic health records and clinical databases enables researchers to identify distinct patient clusters based on their multimorbidity profiles rather than single index diseases. Advanced analytical techniques such as latent class analysis (LCA) enable the identification of these clinically relevant patient subgroups with shared comorbidity patterns [57].
A recent retrospective cross-sectional study on schizophrenia spectrum disorders (SSDs) demonstrates the power of this approach. The study analyzed 3,697 inpatients and identified four distinct comorbidity clusters through LCA based on the 20 most common comorbid conditions: SSDs only (Class 1), High-Risk Metabolic Multisystem Disorders (Class 2), Low-Risk Metabolic Multisystem Disorders (Class 3), and Sleep Disorders (Class 4) [57]. Each cluster exhibited distinctive biomarker profiles, indicating different underlying biological mechanisms despite shared primary psychiatric diagnoses. This clustering approach demonstrates how comorbidity pattern analysis reveals clinically meaningful patient strata with distinctive biomarker signatures [57].
Table 1: Comorbidity Clusters Identified in Schizophrenia Spectrum Disorders
| Cluster | Prevalence | Clinical Characteristics | Key Biomarker Alterations |
|---|---|---|---|
| SSDs Only | 78.0% | No significant somatic comorbidities | Reference class for comparisons |
| High-Risk Metabolic Multisystem Disorders | 1.1% | Complex metabolic dysregulation | ↑ ApoA, ApoB, MPV, RDW-CV, ASO, ALC; ↓ ApoAI, HCT |
| Low-Risk Metabolic Multisystem Disorders | 15.5% | Moderate metabolic involvement | ↑ LDL-C, MPV, WBC, ANC; ↓ HCT |
| Sleep Disorders | 5.5% | Primary sleep disturbances with inflammation | ↑ AISI, NLR, SIRI (inflammatory indices) |
Methodological Approaches: Data to Discovery
Data Acquisition and Preprocessing Pipelines
Robust biomarker discovery begins with comprehensive data acquisition from diverse sources, including electronic health records (EHRs), multi-omics profiling, and digital health technologies. EHR data provide clinical phenotypes and comorbidity information, while multi-omics data (genomics, transcriptomics, proteomics, metabolomics) reveal molecular-level insights. The integration of these disparate data types creates a comprehensive foundation for comorbidity pattern analysis [58] [59].
Critical preprocessing steps include data harmonization, normalization, and batch effect correction to ensure comparability across datasets. For EHR data, this involves standardizing clinical terminologies using common ontologies like ICD-10 for disease classification and structuring temporal clinical data into analyzable formats. For multi-omics data, preprocessing includes quality control, normalization, and transformation to address technical variability. The FAIR principles (Findable, Accessible, Interoperable, Reusable) provide essential guidelines for data management throughout this pipeline [60]. Implementation of these principles ensures that data assets remain available and usable for ongoing and future biomarker discovery efforts.
Computational and Machine Learning Methods
Machine learning (ML) approaches have dramatically enhanced our ability to identify subtle patterns within complex multimorbidity and biomarker data. Both supervised and unsupervised techniques offer distinct advantages for different aspects of comorbidity pattern analysis.
Unsupervised learning methods, particularly latent class analysis (LCA), cluster analysis, and network-based community detection algorithms, enable the discovery of novel patient subgroups based on comorbidity patterns without pre-defined diagnostic categories. The schizophrenia comorbidity study exemplifies this approach, using LCA to identify four distinct patient clusters with different clinical outcomes and biomarker profiles [57]. Similarly, research in critically ill patients has used unsupervised clustering to identify subgroups based on simultaneous pyroptosis and ferroptosis signatures, revealing distinct mortality risks and treatment opportunities [61].
Supervised learning methods, including support vector machines, random forests, and gradient boosting algorithms, enable the development of predictive models for patient stratification based on known comorbidity patterns and biomarker profiles [58]. These approaches are particularly valuable for creating clinical decision support tools that can assign new patients to pre-defined comorbidity clusters based on their biomarker profiles and clinical characteristics.
Table 2: Machine Learning Approaches for Comorbidity Pattern Analysis
| Method Type | Specific Techniques | Applications in Comorbidity Analysis | Considerations |
|---|---|---|---|
| Unsupervised Learning | Latent Class Analysis, K-means Clustering, Hierarchical Clustering | Discovery of novel comorbidity patterns without pre-specified categories | Reveals naturally occurring patient subgroups; requires clinical validation |
| Supervised Learning | Random Forests, SVM, XGBoost, Neural Networks | Prediction of clinical outcomes based on comorbidity-b biomarker profiles | Requires labeled training data; risk of overfitting without proper validation |
| Network Methods | Community Detection, Module Identification, Centrality Analysis | Mapping relationships between comorbid conditions within diseasome networks | Reveals biological pathways connecting comorbid conditions |
| Deep Learning | CNNs, RNNs, Transformers | Analysis of complex multimodal data (imaging, genomics, clinical features) | High computational requirements; limited interpretability without XAI techniques |
Recent advances in explainable AI (XAI) address the "black box" problem often associated with complex ML models. Techniques such as SHAP (Shapley Additive exPlanations) values provide insights into model decision-making processes, revealing which comorbidities and biomarkers contribute most significantly to stratification decisions [62]. This interpretability is essential for clinical adoption and biological validation of ML-derived patient strata.
Experimental Protocols and Validation
Analytical Workflow for Comorbidity-Based Biomarker Discovery
The following diagram illustrates the integrated experimental and computational workflow for biomarker discovery via comorbidity pattern analysis:
Detailed Protocol: Multimodal Biomarker Identification in Comorbidity Clusters
This protocol outlines the steps for identifying and validating biomarker signatures associated with specific comorbidity patterns, based on methodologies successfully employed in recent studies [57] [61].
Patient Cohort Identification and Phenotyping
- Data Source: Extract electronic health records for the target population, including diagnosis codes (ICD-10), medication records, laboratory results, and clinical notes
- Inclusion Criteria: Apply consistent diagnostic criteria (e.g., ICD-10 F20-F29 for schizophrenia spectrum disorders [57]) and ensure complete demographic and clinical information
- Comorbidity Assessment: Systematically identify and catalog all comorbid conditions based on block-level ICD-10 classifications to ensure consistency
- Ethical Considerations: Obtain appropriate institutional review board approval and ensure proper data anonymization to protect patient privacy [57]
Laboratory Biomarker Measurement
The following table details key biomarkers and measurement methodologies for characterizing comorbidity clusters, compiled from recent studies:
Table 3: Essential Biomarker Panels for Comorbidity Pattern Analysis
| Biomarker Category | Specific Biomarkers | Measurement Methodology | Biological Interpretation |
|---|---|---|---|
| Lipid Metabolism | ApoA, ApoB, ApoAI, LDL-C, HDL-C | Immunoassays, colorimetric tests | Cardiovascular risk assessment, metabolic dysregulation |
| Inflammation | IL-1Ra, IL-18, IL-6, IL-10, TNF | Bead-based multiplex immunoassays (Luminex) | Systemic inflammatory state, immune activation |
| Cell Death Signatures | MDA, Catalytic Iron (Fec) | N-methyl-2-phenylindole assay, modified bleomycin assay | Ferroptosis and oxidative stress assessment |
| Hematological Parameters | MPV, RDW-CV, WBC, ALC, NLR | Automated hematology analyzers | Immune status, systemic inflammation |
| Organ Stress | GDF15, CHI3L1 | ELISA, immunoassays | Tissue injury, stress response |
Statistical Analysis and Model Validation
- Comorbidity Pattern Identification: Apply latent class analysis (LCA) to identify naturally occurring comorbidity clusters within the patient population [57]
- Biomarker Comparison: Use linear regression or generalized linear models to compare biomarker levels across comorbidity clusters, adjusting for potential confounders such as age, sex, and medication use
- Multiple Testing Correction: Apply appropriate statistical corrections (e.g., Benjamini-Hochberg false discovery rate) to account for multiple comparisons [57]
- Validation Approach: Employ cross-validation techniques and validate findings in independent patient cohorts to ensure generalizability
- Network Analysis: Construct disease-disease association networks to visualize relationships between comorbid conditions and identify central hub conditions within clusters
Validation in Independent Cohorts and Clinical Trials
Robust validation of comorbidity-based stratification biomarkers requires demonstration of clinical utility in independent populations and prospective clinical trials. The AI-guided re-stratification of the AMARANTH Alzheimer's Disease trial provides a compelling example of this approach. In this study, researchers applied a Predictive Prognostic Model (PPM) trained on ADNI data to stratify patients from the previously unsuccessful AMARANTH trial [63].
The PPM utilized baseline data including β-amyloid, APOE4 status, and medial temporal lobe gray matter density to classify patients as slow or rapid progressors. This AI-guided stratification revealed a significant treatment effect that was obscured in the unstratified analysis: patients classified as slow progressors showed 46% slowing of cognitive decline (measured by CDR-SOB) following treatment with lanabecestat 50 mg compared to placebo [63]. This demonstrates how biomarker-guided patient stratification based on underlying disease progression trajectories can rescue apparently failed clinical trials by identifying responsive patient subgroups.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Essential Research Resources for Comorbidity Biomarker Studies
| Resource Category | Specific Tools/Platforms | Application in Research | Key Features |
|---|---|---|---|
| Data Integration | IntegrAO, NMFProfiler | Integration of incomplete multi-omics datasets | Graph neural networks for classification; identifies biologically relevant signatures |
| Digital Biomarkers | DISCOVER-EEG, DBDP | Processing of digital biomarker data (EEG, wearables) | Automated pipelines; open-source toolkits for standardization |
| Preclinical Models | Patient-derived xenografts (PDX), Organoids | Validation of biomarker signatures | Preserves tumor microenvironment; recapitulates human biology |
| Spatial Biology | Multiplex IHC/IF, Spatial Transcriptomics | Tissue-level context for biomarkers | Maps RNA/protein expression within tissue architecture |
| Analytical Platforms | Luminex, LC-MS, Sequencing | Multiplex biomarker measurement | High-throughput protein/genetic analysis |
Clinical Translation and Implementation
Biomarker Validation and Regulatory Considerations
The translation of comorbidity-based biomarkers from discovery to clinical application requires rigorous validation and adherence to regulatory standards. The biomarker validation pipeline must demonstrate analytical validity (accuracy of measurement), clinical validity (association with clinical endpoints), and clinical utility (improvement in patient outcomes) [60]. This process should follow established frameworks such as the SPIRIT 2025 guidelines for clinical trial protocols, which emphasize comprehensive reporting of biomarker-based stratification methods in trial designs [64].
Regulatory approval of companion diagnostics requires robust evidence from clinical studies. As exemplified by the CRHR1CDx genetic test used in the TAMARIND depression trial, companion diagnostics must demonstrate reliability, reproducibility, and clinical validity for predicting treatment response [62]. Early engagement with regulatory agencies is essential for defining the evidentiary requirements for comorbidity-based stratification biomarkers.
Implementation in Clinical Trial Design
The integration of comorbidity-based biomarkers into clinical trial design enables more precise patient stratification and enhances trial efficiency. Prospective stratification approaches, as implemented in the TAMARIND study, enroll patients based on specific biological profiles rather than broad diagnostic categories [62]. This strategy increases the likelihood of detecting treatment effects by enriching the study population with patients more likely to respond to the investigational therapy.
Beyond patient selection, comorbidity-based biomarkers can inform endpoint selection, dose optimization, and safety monitoring in clinical trials. The successful application of AI-guided stratification in the AMARANTH trial demonstrates how post-hoc analysis using biomarker-based stratification can reveal treatment effects in patient subgroups, potentially rescuing otherwise unsuccessful clinical programs [63].
The analysis of comorbidity patterns within the diseasome network framework provides a powerful approach for biomarker discovery and patient stratification. By leveraging advanced computational methods, multi-omics data, and comprehensive clinical phenotyping, researchers can identify biologically distinct patient subgroups that transcend traditional diagnostic boundaries. These stratification approaches enable more precise therapeutic development and clinical trial design, ultimately advancing the goals of precision medicine.
Future developments in this field will likely include greater integration of real-world data from digital biomarkers and wearables, more sophisticated multi-omics integration methods, and increased application of explainable AI techniques for model interpretation. As these methodologies mature, comorbidity pattern analysis will play an increasingly central role in understanding disease mechanisms, identifying novel therapeutic targets, and matching patients with optimal treatments based on their unique biological and clinical profiles.
Overcoming Challenges: Optimization Strategies for Robust Disease Networks
Addressing Data Heterogeneity and Ontology Resolution Conflicts
The construction of comprehensive disease networks, or diseasomes, represents a paradigm shift in understanding disease relationships from a systemic perspective. However, this approach faces significant challenges from data heterogeneity—the profound differences in how biomedical data is structured, formatted, and semantically represented across diverse sources. In the context of diseasome research, where integrating genetic, clinical, and molecular data is essential, these heterogeneities create substantial barriers to accurate entity matching and ontology resolution. The expanded human disease network (eHDN) exemplifies both the value and challenges of such integration, combining disease-gene associations with protein-protein interaction data to reveal novel disease relationships [65]. When datasets use different schemas, formats, or terminologies to describe the same biological entities, they create resolution conflicts that undermine the reliability of network-based analyses and conclusions. This technical guide examines the taxonomy of data heterogeneity, provides methodologies for addressing ontology conflicts, and presents experimental protocols specifically tailored for diseasome research, enabling researchers to construct more robust and biologically meaningful disease networks.
A Taxonomy of Data Heterogeneity in Diseasome Research
Representation Heterogeneity
Representation heterogeneity encompasses structural and syntactic differences in how data is organized across sources. In diseasome research, this manifests primarily through three distinct subtypes:
Format Heterogeneity: Biomedical data repositories employ diverse syntactic formats, including JSON (for API-based data access), XML (for traditional bioinformatics resources), CSV (for tabular data exports), and specialized formats like BioPAX for pathway data. This structural variation complicates automated parsing and integration pipelines essential for large-scale diseasome construction [66].
Structural (Schema) Heterogeneity: This occurs when datasets describing the same biological entities use different attribute naming conventions, hierarchical organizations, or table structures. For example, one gene expression dataset might use "GeneSymbol" while another uses "Hugo_Symbol" for essentially the same information. Similarly, disease ontologies may nest classification terms differently, creating mismatches in hierarchical relationships [66].
Multimodality: Modern biomedical data integration increasingly incorporates diverse data types—including textual clinical descriptions, genomic sequences, protein structures, and medical images. Aligning entities across these modalities requires specialized models that can jointly embed or compare representations across heterogeneous data sources [66].
Semantic Heterogeneity
Semantic heterogeneity arises when data carries different meanings or interpretations despite structural alignment. This represents perhaps the most challenging aspect of diseasome integration:
Terminological Heterogeneity: The same clinical concept may be described using different terms across datasets (synonymy), while the same term may refer to different concepts depending on context (polysemy). For instance, "T2DM" and "type 2 diabetes mellitus" refer to the same disease, while "depression" could reference a mood disorder or a geological feature without proper contextual cues.
Granularity Mismatches: Diseases may be represented at different levels of specificity across sources—one dataset might use broad categories like "cardiovascular disease" while another specifies "hypertensive heart disease" with precise ICD-10 codes.
Contextual and Quality Variations: Data collected from different experimental conditions, patient populations, or measurement technologies introduces biases that create semantic mismatches in integrated analyses [66].
Table 1: Taxonomy of Data Heterogeneity in Diseasome Research
| Category | Subtype | Description | Example in Diseasome Research |
|---|---|---|---|
| Representation | Format Heterogeneity | Differences in syntactic formats and file structures | JSON vs. XML representations of gene-disease associations |
| Structural Heterogeneity | Variations in attribute naming, hierarchy, and schema | "GeneSymbol" vs. "Hugo_Symbol" attribute names | |
| Multimodality | Incorporation of diverse data types (text, images, sequences) | Linking clinical text descriptions with genomic data | |
| Semantic | Terminological Heterogeneity | Synonymy and polysemy in terminology | "T2DM" vs. "type 2 diabetes mellitus" |
| Granularity Mismatches | Varying levels of specificity in disease classification | "cardiovascular disease" vs. "hypertensive heart disease" | |
| Contextual Variations | Differences arising from experimental conditions or populations | Data from different patient cohorts with varying demographics |
Ontology-Based Resolution Methodologies
Ontology Mapping and Alignment Techniques
Ontology mapping establishes semantic correspondences between concepts across different ontological frameworks, enabling interoperability without requiring complete ontology merging. The process assesses both lexical and semantic similarity among concepts represented in different ontologies through a multi-faceted approach [67]:
Lexical Similarity Measures: These techniques compare concept names, attributes, and relations using string-based algorithms. For disease ontology alignment, this might involve comparing disease names while accounting for syntactic variations, abbreviations, and naming conventions.
Structural Similarity Assessment: This approach examines the hierarchical relationships and positions of concepts within their respective ontology structures. Two diseases with different names but similar parent concepts in their hierarchies may indicate potential matches.
Semantic Similarity Evaluation: Advanced techniques leverage the intended meaning of concepts beyond their lexical representations, using contextual information, relationship networks, and instance data to establish correspondences [67].
Implementation Framework: Combining FIPA CNP and OIP
For dynamic diseasome environments where heterogeneous data sources frequently enter and leave the system, an effective implementation combines the Foundation for Intelligent Physical Agents (FIPA) Contract Net Protocol (CNP) with an Ontology Interaction Protocol (OIP) [67]:
FIPA Contract Net Protocol: Manages the general scenario of agents trading goods or services, structuring complex integration tasks as aggregations of simpler ones through a standardized negotiation framework.
Ontology Interaction Protocol (OIP): Implements the message flow specifically required for solving interoperability problems, including the interaction between customer and supplier agents with ontology-based services that provide resolution capabilities.
This combined approach allows diseasome researchers to maintain flexible integration pipelines that can adapt to new data sources with different ontological representations without requiring complete system redesign.
Similarity Assessment Methodology
The core of ontology resolution lies in accurately assessing similarity between heterogeneous concepts. A comprehensive methodology incorporates multiple dimensions:
Concept Name Comparison: Direct lexical comparison of concept labels using string similarity metrics.
Characteristic Analysis: Comparison of concept attributes and properties to identify overlapping features.
Relation Assessment: Examination of how concepts relate to other concepts within their respective ontologies.
Description Evaluation: Analysis of natural language descriptions associated with concepts to capture contextual meaning [67].
This multi-dimensional approach increases the robustness of similarity assessments, particularly important for disease concepts where clinical descriptions may use varying terminology for the same underlying pathophysiology.
Experimental Protocols for Heterogeneity Resolution
Protocol 1: Constructing an Expanded Human Disease Network (eHDN)
The expanded Human Disease Network protocol demonstrates a concrete approach to addressing heterogeneity by integrating disease-gene associations with protein-protein interaction data [65]:
Step 1: Data Acquisition
- Obtain human disease-gene associations from the Genetic Association Database (GAD) or similar repository
- Acquire protein-protein interaction data from the Human Protein Reference Database (HPRD) or equivalent source
- Filter for high-confidence associations and interactions, removing self-interactions and ambiguous mappings
Step 2: Bipartite Graph Construction
- Construct a bipartite graph representing associations between diseases and disease genes (GAD diseasome)
- Generate the original HDN (oHDN) projection where diseases are connected if they share at least one disease gene
Step 3: Network Expansion
- Identify genes encoding proteins that interact with at least two proteins from disease-associated genes
- Add these genes to the GAD diseasome to create the GAD-HPRD2 diseasome
- Generate the eHDN projection from the expanded diseasome
Step 4: Topological and Functional Analysis
- Calculate network properties including degree distribution, clustering coefficient, and path lengths
- Assess functional properties using Gene Ontology (GO) homogeneity, KEGG pathway homogeneity, and tissue expression patterns
- Compare eHDN with oHDN to validate new connections and identify biologically meaningful expansions [65]
Table 2: Key Research Reagents for Diseasome Construction
| Reagent/Resource | Type | Function in Diseasome Research | Example Source |
|---|---|---|---|
| Genetic Association Database (GAD) | Data Repository | Provides curated disease-gene associations from published literature | [65] |
| Human Protein Reference Database (HPRD) | Data Repository | Offers manually curated protein-protein interaction data | [65] |
| Gene Expression Omnibus (GEO) | Data Repository | Archives functional genomic data for tissue-specific expression analysis | [65] |
| Gene Ontology (GO) | Ontology | Provides standardized vocabulary for gene function annotation | [65] |
| Kyoto Encyclopedia of Genes and Genomes (KEGG) | Knowledge Base | Offers pathway information for functional validation | [65] |
| Significance Analysis of Microarrays (SAM) | Algorithm | Identifies tissue-selective genes for functional characterization | [65] |
Protocol 2: Ontology Mapping for Disease Concept Alignment
This protocol provides a detailed methodology for aligning disease concepts across heterogeneous ontologies:
Step 1: Ontology Preprocessing
- Parse source and target ontologies using appropriate parsers (e.g., OWL API for OWL-formatted ontologies)
- Extract concepts, properties, hierarchies, and definitions
- Normalize lexical representations through tokenization, stemming, and stop-word removal
Step 2: Similarity Computation
- Calculate lexical similarity using string-based metrics (Levenshtein distance, Jaro-Winkler)
- Compute structural similarity based on hierarchical positions and relationship networks
- Determine instance similarity when instance data is available
- Apply machine learning approaches to combine multiple similarity dimensions
Step 3: Mapping Generation
- Establish correspondence candidates based on similarity thresholds
- Apply consistency constraints to ensure mapping coherence
- Validate mappings through domain expert review or automated consistency checking
Step 4: Mapping Implementation
- Implement alignments using appropriate representation languages (e.g., OWL mappings, SPARQL construct queries)
- Integrate mapped ontologies into the diseasome construction pipeline
- Establish maintenance procedures for updating mappings as source ontologies evolve
Protocol 3: Evaluating Resolution Success Metrics
Robust evaluation is essential for assessing the effectiveness of heterogeneity resolution approaches:
Topological Metrics: Compare network properties of integrated diseasomes with ground truth references, measuring degree distribution preservation, clustering coefficients, and connectivity patterns.
Functional Validation: Assess whether integrated data maintains biological meaning through Gene Ontology enrichment analysis, pathway coherence, and tissue-specific expression consistency.
Expert Validation: Engage domain experts to review a subset of integrated entities and relationships, quantifying precision and recall against manual curation.
Downstream Application Testing: Evaluate the integrated diseasome's performance on practical applications such as drug repurposing prediction, disease gene discovery, or comorbidity analysis.
Visualization of Workflows and Relationships
Disease Network Integration Workflow
eHDN Construction Protocol
Addressing data heterogeneity and ontology resolution conflicts is not merely a technical prerequisite but a fundamental requirement for advancing diseasome research and constructing biologically meaningful disease networks. The methodologies and protocols presented in this guide provide a systematic approach to overcoming these challenges, enabling researchers to integrate diverse data sources while preserving semantic meaning and biological context. As the field progresses toward increasingly complex multimodal data integration, the principles of robust ontology alignment, comprehensive similarity assessment, and rigorous validation will remain essential for generating reliable insights into disease mechanisms and relationships. The expanded human disease network exemplifies the substantial benefits of successfully addressing heterogeneity—revealing novel disease connections and potential therapeutic opportunities that would remain hidden in isolated datasets. By implementing these structured approaches, researchers can accelerate the development of more comprehensive, accurate, and clinically actionable disease networks that ultimately enhance our understanding of human disease biology.
Statistical Power Limitations in Rare Disease Network Analysis
Rare disease research faces profound statistical power limitations that impact the validity and generalizability of network analysis findings. This technical review examines how small sample sizes, heterogeneous disease manifestations, and methodological constraints create significant challenges for diseasome and disease network concepts research. We synthesize current evidence on how these limitations affect gene-disease association studies, comorbidity pattern detection, and therapeutic target identification. By evaluating innovative methodological adaptations and computational frameworks, this analysis provides researchers and drug development professionals with strategic approaches to enhance statistical robustness in rare disease investigations while acknowledging inherent constraints in this scientifically crucial field.
The diseasome framework conceptualizes diseases as interconnected nodes within complex biological networks, where shared molecular pathways and genetic architectures reveal previously unrecognized disease relationships. This approach has proven particularly valuable for rare diseases, which collectively affect approximately 6% of the global population yet individually impact small patient populations [68]. The fundamental premise of disease network analysis involves mapping connections between rare genetic disorders through multiple biological scales—from genetic interactions and protein pathways to phenotypic manifestations and clinical comorbidities.
Despite the theoretical power of network medicine, rare disease research confronts unique methodological challenges. Most rare diseases exhibit poorly understood pathophysiology, large variations in disease manifestations, and high unpredictability in clinical progression [69]. These characteristics directly impact the application of diseasome concepts, as the sparse data environment creates significant statistical power limitations that can undermine network inference validity. Furthermore, the monogenic nature of many rare diseases offers deceptive simplicity; while single gene defects may initiate pathology, their effects propagate through complex biological networks, resulting in heterogeneous phenotypic expressions that complicate systematic analysis [70].
The statistical power constraints in rare disease network analysis extend beyond sample size limitations to encompass fundamental methodological trade-offs. Network-based approaches must balance sensitivity against specificity in relationship detection while managing the high-dimensionality of multi-omics data relative to small cohort sizes. These challenges manifest across study designs, from gene-disease association investigations to comorbidity pattern analyses, requiring specialized analytical frameworks that account for the unique data environment of rare diseases.
Methodological Foundations of Disease Network Analysis
Network Construction Principles and Data Integration
Disease network analysis employs sophisticated computational frameworks to integrate multi-modal biological data. The foundational approach involves constructing multiplex networks consisting of multiple layers of gene relationships organized across biological scales. As demonstrated in a comprehensive analysis of 3,771 rare diseases, researchers have successfully built networks encompassing over 20 million gene relationships organized into 46 network layers spanning six major biological scales between genotype and phenotype [70]. This cross-scale integration enables researchers to contextualize individual genetic lesions within broader biological systems.
The critical data dimensions for rare disease network construction include:
- Genetic interactions derived from functional genomic screens
- Transcriptomic relationships representing co-expression patterns across tissues
- Protein-protein interactions mapping physical interactions between gene products
- Pathway memberships identifying shared metabolic and signaling pathways
- Functional annotations leveraging Gene Ontology frameworks
- Phenotypic similarities based on human phenotype ontologies
Network construction employs ontology-aware disease similarity (OADS) strategies that incorporate not only multi-modal data but also continuous biomedical ontologies. This approach uses semantic similarity metrics across Gene Ontology, Cell Ontology, and Human Phenotype Ontology frameworks to quantify disease relationships beyond simple co-occurrence [5]. The resulting networks enable researchers to identify disease modules—subnetworks of interconnected genes and pathways associated with specific pathological manifestations.
Statistical Framework for Network Analysis
The statistical foundation of disease network analysis involves specialized methods adapted for sparse data environments. For genetic association studies, gene- or region-based association tests have been developed to evaluate collective effects of multiple variants within biologically relevant regions. These include burden tests, variance-component tests, and combined omnibus tests that aggregate rare variants to enhance statistical power [71]. These approaches address the limitations of single-variant association tests, which demonstrate inadequate power for rare variants unless sample sizes or effect sizes are substantial.
Comorbidity network analysis employs distinct statistical measures to quantify disease relationships. The Salton Cosine Index (SCI) provides a stable measure of disease co-occurrence strength that remains unaffected by sample size variations, making it particularly valuable for rare disease applications [42]. Statistical significance is determined through permutation testing that generates null distributions by recalculating similarities after shuffling disease-term mappings while preserving term counts and distributions [5]. This approach controls for false positive relationships that might arise from chance co-occurrences in small samples.
Table 1: Statistical Measures for Disease Network Analysis
| Measure | Application | Advantages for Rare Diseases | Limitations |
|---|---|---|---|
| Burden Tests | Gene-based association | Aggregates rare variants to increase power | Sensitive to inclusion of non-causal variants |
| Variance-Component Tests | Gene-based association | Robust to mix of risk and protective variants | Lower power when most variants are causal |
| Salton Cosine Index | Comorbidity networks | Unaffected by sample size | May miss non-linear relationships |
| Ontology-Aware Similarity | Phenotypic networks | Incorporates hierarchical ontological knowledge | Dependent on ontology completeness |
Fundamental Challenges in Statistical Power
Sample Size Limitations and Their Implications
The most fundamental statistical power limitation in rare disease network analysis stems from extremely small patient populations. While clinical trials for common diseases may enroll thousands of participants, studies for rare diseases often struggle to recruit sufficient patients for robust statistical analysis [68]. In practical terms, a clinical trial with 100-150 rare disease patients is considered large, and randomization schemes (e.g., 2:1 allocation) can result in treatment arms with fewer than 50 patients [69]. These sample size constraints directly impact statistical power through multiple mechanisms:
- Reduced ability to detect statistically significant differences between groups, even when apparent treatment effects seem compelling
- Limited power for subgroup analyses, which may contain cohorts of fewer than 30 patients, often necessitating non-parametric statistical tests with lower efficiency
- Inadequate power for multi-dimensional analyses, as symptom heterogeneity in rare diseases may require assessment of multiple endpoints, further compounding power limitations in small trial populations
The impact of small sample sizes extends beyond clinical trials to basic research. In genetic association studies, rare variant analyses require substantial sample sizes to achieve adequate power, as the minor allele frequency directly influences the number of expected carriers in a study population [71]. This challenge is particularly acute for very rare variants (MAF < 0.5%), which may appear in only a handful of patients even in relatively large rare disease cohorts.
Data Sparsity and Heterogeneity Challenges
Rare diseases frequently exhibit incomplete biological characterization that compounds statistical power limitations. Many rare diseases lack well-defined natural history data, International Classification of Diseases codes, and standardized clinical endpoints [69]. This data sparsity creates fundamental challenges for network analysis:
- Poorly characterized disease pathophysiology hinders accurate network node and edge definition
- Large variations in disease manifestations introduce noise that obscures true biological signals
- High disease unpredictability complicates longitudinal modeling and causal inference
The problem of clinical heterogeneity is particularly challenging for rare disease network analysis. Patients with the same rare disease may present with dramatically different symptom profiles, disease trajectories, and treatment responses. This heterogeneity magnifies the difficulties of adequate statistical power in small populations, as measuring treatment benefits may require assessing several endpoints within a single trial [69]. From a network perspective, this heterogeneity manifests as fuzzy disease modules with poorly defined boundaries, reducing the accuracy of network-based predictions.
The lack of established treatments for approximately 95% of rare diseases further complicates statistical analysis [69]. Rare disease clinicians and patients often resort to trial-and-error approaches, resulting in highly variable care pathways. From a health technology assessment perspective, this variability creates substantial challenges for selecting appropriate comparators and quantifying treatment benefits within economic models.
Methodological Adaptations for Power Enhancement
Innovative Study Designs for Rare Diseases
Several methodological adaptations have been developed to enhance statistical power in rare disease research. These innovative study designs address fundamental power limitations while acknowledging practical constraints:
Extreme-phenotype sampling: Enriching study populations with patients at the severe end of the disease spectrum increases the likelihood of detecting genetic associations and treatment effects [71]
Multi-modal data integration: Combining genetic, transcriptomic, proteomic, and phenotypic data provides complementary evidence streams that collectively enhance signal detection [5]
Cross-scale network analysis: Evaluating disease signatures across multiple levels of biological organization (genome, transcriptome, proteome, pathway, function, phenotype) enables cross-validation of findings [70]
External control arms: Using naturalistic or pre-specified historical controls addresses ethical concerns about placebo use in severe rare diseases while providing comparison groups [69]
These adaptive designs specifically address the challenges of rare disease research by maximizing information extraction from limited patient populations. The multiplex network approach exemplifies this strategy, consisting of multiple network layers that represent different scales of biological organization [70]. This framework enables researchers to identify consistent patterns across biological scales, enhancing confidence in findings despite small sample sizes.
Statistical and Computational Innovations
Statistical methodologies have evolved specifically to address power limitations in rare disease research. These innovations include:
Gene-based association tests that aggregate the effects of multiple rare variants within biologically defined units (e.g., genes, pathways) to increase statistical power. These methods include burden tests, variance-component tests, and combined omnibus tests that collectively address the limitations of single-variant analysis [71].
Network-based regularization techniques that leverage the network structure of biological systems to impose constraints on statistical models, reducing effective degrees of freedom and enhancing power for detecting true signals.
Bayesian hierarchical models that incorporate prior knowledge about biological systems to provide more stable effect estimates in small samples.
Table 2: Methodological Adaptations for Power Enhancement in Rare Disease Studies
| Methodology | Application | Power Enhancement Mechanism | Implementation Considerations |
|---|---|---|---|
| Gene-Based Association Tests | Genetic association | Aggregates signals across multiple rare variants | Dependent on accurate variant functional annotation |
| Matching-Adjusted Indirect Comparison | Comparative effectiveness | Adjusts for cross-study differences using propensity score methods | Effective sample size may be very low after matching |
| Multiplex Network Analysis | Cross-scale data integration | Identifies consistent patterns across biological scales | Requires specialized computational infrastructure |
| Ontology-Aware Similarity | Phenotype analysis | Incorporates hierarchical relationships in phenotype data | Dependent on completeness of ontological resources |
Case Studies and Experimental Protocols
Autoimmune and Autoinflammatory Disease Network Analysis
A recent large-scale study demonstrates the application of network approaches to autoimmune and autoinflammatory diseases (AIIDs), providing a protocol for overcoming power limitations through multi-modal data integration. The research curated disease terms from Mondo, Disease Ontology, MeSH, ICD-11, and three specialized AIID knowledge bases, establishing a comprehensive repository including 484 autoimmune diseases, 110 autoinflammatory diseases, and 284 associated diseases [5].
The experimental protocol involved:
- Data integration and harmonization: Leveraging genetic, transcriptomic (bulk and single-cell), and phenotypic data to construct multi-layered AIID association networks
- Ontology-aware similarity calculation: Implementing the OADS strategy that incorporates multi-modal data within continuous biomedical ontologies
- Network modularity analysis: Applying the Leiden algorithm with resolution=1.0 to identify robust disease communities
- Cross-scale validation: Examining information flow from genetic susceptibilities to transcriptional dysregulation, immune microenvironment alterations, and clinical phenotypes
This approach identified 10 robust disease communities with shared phenotypes and dysfunctional pathways, demonstrating how network methods can detect meaningful biological relationships despite the rarity of individual conditions [5]. The study specifically addressed power limitations by aggregating rare conditions into shared pathway modules, effectively increasing sample size for statistical analysis.
COPD Comorbidity Pattern Analysis in Hospitalized Patients
A study of comorbidity patterns in hospitalized COPD patients illustrates adaptive methodologies for analyzing complex disease relationships in large but heterogeneous populations. The research analyzed 2,004,891 COPD inpatients from Sichuan Province, China, constructing comorbidity networks using the Salton Cosine Index to quantify disease co-occurrence strength [42].
The experimental protocol included:
- Data source standardization: Collecting hospital discharge records from all secondary and tertiary hospitals with diagnoses coded according to ICD-10
- Comorbidity identification: Applying chronic condition indicators to differentiate between acute and chronic ICD-10 codes
- Network construction: Calculating SCI values and determining cutoff thresholds based on phi correlation coefficients
- Centrality analysis: Employing PageRank algorithm to identify central diseases within the comorbidity network
- Community detection: Applying the Louvain algorithm to identify tightly connected disease clusters
This study revealed that 96.05% of COPD patients had at least one comorbidity, with essential hypertension being most prevalent (40.30%) [42]. The network analysis identified 11 central diseases and distinct comorbidity patterns across sex and geographic subgroups, demonstrating how large-scale administrative data can overcome power limitations for conditional rare diseases.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Resources for Rare Disease Network Analysis
| Resource Category | Specific Tools/Databases | Function in Rare Disease Research | Key Features |
|---|---|---|---|
| Disease Ontologies | Mondo Disease Ontology, DO, MeSH, ICD-11 | Standardized disease classification and annotation | Harmonizes disease definitions across research communities |
| Gene Interaction Databases | HIPPIE, REACTOME, Gene Ontology | Provides physical and functional gene relationships | Curated protein-protein interactions and pathway memberships |
| Phenotypic Data Resources | Human Phenotype Ontology, Mammalian Phenotype Ontology | Standardized phenotypic annotation | Enables computation of phenotype similarity across diseases |
| Analysis Frameworks | DCGL, Seurat, SingleR, NetworkX | Differential co-expression analysis and network construction | Specialized packages for biological network analysis |
| Multi-Omics Integration Platforms | BC Platforms, CureDuchenne Link | Secure data harmonization and sharing | Enables collaborative analysis while addressing data governance |
Emerging Approaches for Enhanced Statistical Power
The evolving landscape of rare disease network analysis points toward several promising approaches for addressing persistent power limitations. Real-world data (RWD) ecosystems are emerging as crucial resources for augmenting traditional clinical studies. Secure, collaborative data platforms enable the integration of heterogeneous data sources while addressing governance requirements, as demonstrated by initiatives like the CureDuchenne Link global data hub for Duchenne muscular dystrophy research [68].
Advanced computational frameworks that leverage cross-species data integration represent another promising direction. The systematic characterization of network signatures across 3,771 rare diseases has demonstrated that disease module formalism can be generalized beyond physical interaction networks [70]. This approach enables knowledge transfer from model organisms to human rare diseases, effectively expanding the analytical sample size through evolutionary conservation.
Federated learning approaches that enable distributed analysis without centralizing sensitive patient data are particularly relevant for rare disease research. These methods allow statistical models to be trained across multiple institutions while preserving data privacy, collectively enhancing power through increased effective sample sizes.
Statistical power limitations present fundamental but not insurmountable challenges for rare disease network analysis. Through methodological innovations in study design, data integration, and analytical techniques, researchers can enhance power while acknowledging inherent constraints. The diseasome framework provides a powerful conceptual approach for contextualizing individual rare diseases within broader biological networks, enabling knowledge transfer and pattern recognition across conditions.
The continued development of specialized statistical methods, collaborative data platforms, and multi-scale integration frameworks will further enhance our ability to extract meaningful insights from limited patient populations. These advances promise to accelerate therapeutic development and improve outcomes for the millions affected by rare diseases worldwide, ultimately reducing the inequity faced by these underserved patient populations [69].
Alternative Clinical Evidence Generation for Small Patient Populations
The development of therapies for rare diseases and small patient populations represents a significant challenge for researchers and drug development professionals. The conventional drug development paradigm, which relies on large, randomized clinical trials to demonstrate safety and efficacy, becomes difficult or impossible to apply when patient populations are very small [72]. Individually, rare diseases affect small patient groups, but collectively they impact hundreds of millions of people worldwide, with over 10,000 rare diseases identified and approximately more than 90% having no FDA-approved treatment [73]. This vast unmet medical need has driven regulatory agencies and researchers to establish innovative frameworks for evidence generation that can accommodate the statistical and practical challenges inherent in studying small populations.
The concept of the diseasome—which views diseases as interconnected nodes in a network rather than isolated entities—provides a crucial theoretical foundation for these approaches [1]. Disease networks have emerged as an intuitive and powerful way to reveal hidden connections among apparently unconnected biomedical entities such as diseases, physiological processes, signaling pathways, and genes. This network-based perspective enables researchers to leverage information across disease boundaries and develop evidence generation strategies that can function effectively within the constraints of small population research.
Regulatory Frameworks for Alternative Evidence
The FDA Rare Disease Evidence Principles (RDEP)
In response to these challenges, the U.S. Food and Drug Administration has introduced the Rare Disease Evidence Principles (RDEP) to provide greater speed and predictability in the review of therapies intended to treat rare diseases with very small patient populations [72]. This process acknowledges that developing drugs for rare diseases can make it difficult or impossible to generate substantial evidence of safety and efficacy using multiple traditional clinical trials. The RDEP framework ensures that FDA and sponsors are aligned on a flexible, common-sense approach within existing authorities while incorporating confirmatory evidence to give sponsors a clear, rigorous path to bring safe and effective treatments to those who need them most.
To be eligible for the RDEP process, investigative therapies must meet specific criteria: they must address the genetic defect in question and target a very small, rare disease population or subpopulation (generally fewer than 1,000 patients in the United States) facing rapid deterioration in function leading to disability or death, for whom no adequate alternative therapies exist [72]. Sponsor requests for review under this process must be submitted before a pivotal trial begins, allowing for alignment on evidence requirements early in development.
Table 1: FDA Rare Disease Evidence Principles (RDEP) Framework Components
| Component | Description | Eligibility Criteria | Submission Timing |
|---|---|---|---|
| Evidence Standard | One adequate and well-controlled study plus robust confirmatory evidence | Targets very small populations (<1,000 US patients) | Prior to pivotal trial launch |
| Acceptable Confirmatory Evidence Types | Strong mechanistic or biomarker evidence; evidence from relevant non-clinical models; clinical pharmacodynamic data; case reports, expanded access data, or natural history studies | Addresses genetic defect; rapid deterioration; no adequate alternatives | Filed as part of formal meeting request |
| Review Process | Joint implementation by CDER and CBER with patient and expert input | Separate from orphan-drug designation | Work with FDA to define evidence needs early |
Types of Acceptable Alternative Evidence
Under the RDEP process, approval may be based on one adequate and well-controlled study plus robust confirmatory evidence, which represents a significant flexibility compared to traditional requirements [72]. The types of acceptable confirmatory evidence include:
- Strong mechanistic or biomarker evidence: Data demonstrating the biological mechanism of action or validated biomarkers that correlate with clinical outcomes.
- Evidence from relevant non-clinical models: Findings from animal models or in vitro systems that recapitulate key aspects of the human disease.
- Clinical pharmacodynamic data: Information showing the drug's effects on its intended target in human subjects.
- Case reports, expanded access data, or natural history studies: Real-world evidence that provides context for the disease course and treatment effects.
This expanded evidence framework allows drug developers to build a compelling case for effectiveness using multiple complementary data sources rather than relying exclusively on traditional clinical trial endpoints.
Methodological Approaches for Evidence Generation
Primary Research with Stakeholders
Generating robust evidence for small population therapies requires a multifaceted approach that incorporates diverse stakeholder perspectives. At IQVIA, researchers leverage surveys, in-depth interviews, focus groups, and other primary research methods to capture perspectives from all key stakeholders in the rare disease ecosystem [73]. Each group offers a unique lens on the disease, and together they form a 360° view that drives effective strategy.
Table 2: Stakeholder-Based Evidence Generation Methodology
| Stakeholder Group | Research Methods | Key Insights | Strategic Application |
|---|---|---|---|
| Patients & Caregivers | Interviews, surveys, focus groups | Daily challenges, emotional impacts, meaningful outcomes beyond clinical metrics | Identify unmet needs, design patient-centric trials, develop support programs |
| Healthcare Professionals | Surveys, one-on-one interviews | Diagnostic and treatment challenges, gaps in current protocols, referral pathways | Shape physician education, diagnostics, and clinical practice strategies |
| Payers & Market Access Stakeholders | Structured interviews, value assessment surveys | Reimbursement barriers, evidence requirements for coverage decisions | Plan evidence generation and HEOR strategies to address payer concerns |
| Advocacy Groups & KOLs | Advisory boards, collaborative workshops | Collective patient community feedback, clinical trial design recommendations | Ensure holistic, community-informed strategic recommendations |
This stakeholder-centric approach ensures that evidence generation addresses the practical realities of disease management and treatment while identifying outcomes that truly matter to patients and caregivers.
Integrating Clinical Insights with Market Research
Gathering stakeholder input is powerful on its own, but its impact multiplies when combined with clinical insights and data. Studies suggest that approximately 15-30% of trial failures in rare disease are related to issues with endpoints, including poor alignment with disease features, lack of adequate validation, and inadequate capture of important patient-reported outcomes [73]. Bridging primary market research with clinical domain expertise ensures that strategies are both patient-centered and scientifically sound.
This integration might involve analyzing clinical trial results, real-world data, or epidemiological information alongside the primary research. For instance, vast real-world data assets (such as patient registries and electronic health record databases) can complement interview findings by providing hard evidence on disease prevalence, treatment patterns, or outcomes in the real world [73]. If caregivers report that "many patients discontinue therapy after six months due to side effects," researchers can check real-world data to quantify dropout rates and reasons, creating a more comprehensive evidence base.
Data Management and Analysis for Small Populations
The analysis of quantitative research data in small population studies requires careful attention to data management, analysis, and interpretation [74]. On entry into a data set, data must be carefully checked for errors and missing values, and then variables must be defined and coded as part of data management. Quantitative data analysis involves the use of both descriptive and inferential statistics, though the latter must be interpreted with caution in small samples.
Descriptive statistics help summarize the variables in a data set to show what is typical for a sample. Measures of central tendency (mean, median, mode), measures of spread (standard deviation), and parameter estimation measures (confidence intervals) may be calculated [74]. In small populations, careful interpretation of these measures is essential, as outliers can disproportionately influence results. Inferential statistics aid in testing hypotheses about whether a hypothesized effect, relationship, or difference is likely true, producing a value for probability (the P value). However, in small populations, it is particularly important that the P value must be accompanied by a measure of magnitude (effect size) to help interpret how small or large the effect, relationship, or difference is [74].
Disease Networks and Drug Repurposing
Fundamentals of Disease Network Analysis
Over a decade ago, a new discipline called network medicine emerged as an approach to understand human diseases from a network theory point-of-view [1]. Disease networks proved to be an intuitive and powerful way to reveal hidden connections among apparently unconnected biomedical entities such as diseases, physiological processes, signaling pathways, and genes. This approach is particularly valuable for small population research, as it allows for the leveraging of information from more common conditions with shared biological pathways.
The disease network concept has evolved significantly during the last decade, with researchers applying a data science pipeline approach to evaluate their functional units [1]. This analysis has yielded a list of the most commonly used functional units and highlighted the challenges that remain to be solved, providing valuable information for the generation of new prediction models based on disease networks.
Disease Network Analysis for Therapeutic Discovery
Drug Repurposing Through Network Analysis
One of the fields that has benefited most from disease network approaches is the identification of new opportunities for the use of old drugs, known as drug repurposing [1]. The importance of drug repurposing lies in the high costs and the prolonged time from target selection to regulatory approval of traditional drug development. For small patient populations, where commercial incentives may be limited, drug repurposing represents a particularly promising strategy for rapidly delivering treatments to patients.
Primary research can help explore opportunities for drug repurposing, as leveraging existing therapies for multiple rare diseases can accelerate development and funding [73]. By understanding the shared network properties of diseases, researchers can identify existing drugs with established safety profiles that may be effective for rare conditions, significantly shortening the development timeline and reducing costs.
Experimental Design and Endpoint Selection
Endpoint Selection Framework
Stakeholder feedback often highlights the complexities of clinical trial design in rare diseases, particularly around the selection of appropriate endpoints [73]. Studies may struggle or fail if endpoints do not reflect outcomes that are meaningful to patients or are challenging to measure consistently. For example, assessments like the 6-minute walk test (6MWT), commonly used in rare neuromuscular disease trials, can present difficulties in achieving consistency across sites and patient populations.
Incorporating insights from patients, caregivers, and clinicians helps ensure that endpoints are both clinically relevant and feasible (both valid and tractable), ultimately improving the quality and impact of research [73]. This approach aligns with the FDA's patient-focused drug development initiative, which emphasizes the importance of incorporating the patient voice into drug development and evaluation.
Adaptive and Innovative Trial Designs
For small population studies, adaptive trial designs that allow for modifications based on accumulating data are particularly valuable. These designs may include:
- Bayesian approaches: Which incorporate prior knowledge and continuously update probability assessments as new data emerge.
- Platform trials: Which allow for the evaluation of multiple therapies simultaneously within a shared infrastructure.
- N-of-1 trials: Which focus on individual patient responses to treatment and can be particularly useful in ultra-rare diseases.
These innovative designs require close collaboration with regulatory agencies early in the development process but can significantly enhance the efficiency of evidence generation for small populations.
Evidence Integration Workflow for Small Populations
Table 3: Research Reagent Solutions for Small Population Studies
| Resource Category | Specific Tools & Databases | Primary Function | Application in Small Populations |
|---|---|---|---|
| Data Collection & Management | Electronic data capture systems, Patient registries, Natural history databases | Standardized collection of clinical and patient-reported data | Establishes disease baselines, enables historical controls, identifies patients for trials |
| Analytical Tools | Statistical software (R, SAS), Bayesian analysis platforms, Network analysis tools | Data analysis, modeling, and visualization | Supports analysis of small datasets, enables borrowing of information from related conditions |
| Biomarker & Diagnostic Platforms Genomic sequencers, Proteomic analyzers, Metabolic assay kits | Objective measurement of biological processes, patient stratification, treatment response monitoring | Provides mechanistic evidence, supports personalized treatment approaches | |
| Regulatory Guidance Documents | FDA RDEP, EMA guideline on orphan medicines, ICHE19 on personalized medicine | Framework for regulatory submissions, evidence standards, approval pathways | Guides evidence generation strategy, facilitates regulatory alignment, streamlines review |
The generation of robust clinical evidence for small patient populations requires a paradigm shift from traditional drug development approaches. The framework established by the FDA's Rare Disease Evidence Principles provides a flexible yet rigorous pathway for demonstrating substantial evidence of effectiveness using a combination of traditional clinical data and alternative evidence sources [72]. By incorporating disease network concepts [1], stakeholder insights [73], and innovative trial designs, researchers can develop compelling evidence packages that meet regulatory standards while addressing the unique challenges of small population research.
As technology and access to advanced diagnostics continue to evolve, so too do the endpoints and biomarkers used in rare disease research [73]. This ongoing evolution requires that evidence generation strategies remain flexible and adaptive, ensuring that assessments and measures are aligned with the latest scientific understanding and patient-centered priorities. Through these approaches, researchers can accelerate the development of safe and effective treatments for the millions of patients worldwide affected by rare diseases.
The exploration of the diseasome—the complex network of interconnections between diseases—requires sophisticated analytical methods to untangle multifaceted relationships between treatments, genetics, and clinical outcomes. Within this conceptual framework, advanced study designs have emerged as powerful tools for generating robust evidence from real-world data. Self-controlled trials and Bayesian methods represent two particularly transformative approaches, enabling researchers to address confounding challenges and incorporate prior knowledge directly into analytical frameworks. These methodologies are especially valuable in pharmacoepidemiology and drug development, where they facilitate more efficient and nuanced investigation of treatment effects within the interconnected landscape of human disease [75] [76] [1].
This technical guide provides an in-depth examination of these advanced methodologies, detailing their theoretical foundations, implementation protocols, and application within disease network research. By synthesizing recent developments and practical considerations, this resource aims to equip researchers with the knowledge necessary to leverage these approaches in their own investigations of the diseasome.
Self-Controlled Study Designs
Conceptual Foundation and Terminology
Self-controlled study designs represent a paradigm shift from traditional between-person comparisons to within-person analyses. These designs fundamentally compare different time periods within the same individual, effectively using each person as their own control [75]. This approach automatically controls for all time-stable confounders, including genetic factors, socioeconomic status, and baseline health status, regardless of whether these factors are measured or even known to the researcher [75].
The terminology for self-controlled designs has recently been harmonized under the overarching concept of Self-controlled Crossover Observational PharmacoEpidemiologic (SCOPE) studies [75]. Key conceptual elements include:
- Anchor: A point in time relative to which all design features are defined (either exposure or outcome)
- Focal window: Period of hypothesized increased risk
- Referent window: Comparison period representing usual risk
- Transition window: Buffer period excluded from analysis to account for lingering exposure effects or delays
Table 1: Core Terminology in Self-Controlled Designs
| Term | Definition | Alternative Names |
|---|---|---|
| Exposure-anchored | Design features defined relative to exposure dates | Self-controlled case series |
| Outcome-anchored | Design features defined relative to outcome dates | Case-crossover design |
| Focal window | Period of hypothesized increased risk | Risk window, Hazard period |
| Referent window | Period representing usual risk | Control window, Baseline period |
| Transition window | Buffer period excluded from analysis | Wash-out window, Induction period |
Key Design Variants and Methodologies
Self-controlled designs primarily manifest in two principal variants, differentiated by their anchor point and analytical approach.
Outcome-Anchored Designs (Case-Crossover)
The case-crossover design is outcome-anchored, comparing exposure frequency during a period immediately preceding the outcome (focal window) to exposure frequency during one or more reference periods (referent windows) from earlier time points [75]. This design is particularly suitable for investigating transient exposures that trigger acute outcomes, such as medication administration preceding arrhythmias or environmental triggers exacerbating asthma.
Implementation protocol:
- Identify cases experiencing the outcome of interest
- Define focal window based on biological plausibility of exposure-effect relationship
- Select one or more referent windows from the same individual's observation period
- Compare exposure status between focal and referent windows
- Analyze using conditional logistic regression to account for within-person correlation
Exposure-Anchored Designs (Self-Controlled Case Series)
The self-controlled case series (SCCS) design is exposure-anchored, comparing the incidence of outcomes during periods following exposure (focal windows) to outcomes during unexposed or differently exposed periods (referent windows) within the same individual [75]. This method exclusively includes individuals who have experienced both the exposure and outcome of interest.
Implementation protocol:
- Identify individuals who experienced both the exposure and outcome during the study period
- Define the observation period for each individual (often based on age or calendar time)
- Partition observation time into focal, referent, and transition windows relative to exposure dates
- Calculate incidence rates during focal and referent windows
- Analyze using conditional Poisson regression to estimate incidence rate ratios
A recent European study analyzing COVID-19 vaccines and myocarditis demonstrated the application of multiple self-controlled designs, including SCCS and self-controlled risk interval (SCRI) designs, across five databases [77]. This research highlighted how different variants can be applied to the same research question to assess robustness of findings.
Applications in Disease Network Research
Within diseasome research, self-controlled designs offer particular utility for investigating comorbidity relationships and treatment pathways across interconnected conditions. By controlling for fixed genetic and environmental factors, these methods help isolate true biological relationships from spurious correlations in disease networks [1].
For example, researchers might use SCCS to determine whether initiating a medication for one condition acutely increases risk of exacerbation in a comorbid condition—a connection that might represent a previously unrecognized edge in the disease network. The within-person design naturally accounts for the baseline predisposition conferred by shared genetic architecture between comorbid conditions.
Bayesian Methods in Clinical Research
Theoretical Framework
Bayesian methods represent a fundamentally different approach to statistical inference compared to traditional frequentist statistics. While frequentist methods interpret probability as the long-run frequency of an event and rely solely on current trial data, Bayesian statistics interpret probability as a degree of belief and formally incorporate prior knowledge through Bayes' theorem [78] [76].
The mathematical foundation of Bayesian analysis is Bayes' theorem:
[ P(A|B) = \frac{P(B|A) \cdot P(A)}{P(B)} ]
In clinical research contexts, this translates to:
[ \text{Posterior} \propto \text{Likelihood} \times \text{Prior} ]
Where:
- Prior represents pre-existing knowledge about treatment effects before observing trial data
- Likelihood represents the evidence from the current trial data
- Posterior represents the updated knowledge combining both prior beliefs and current evidence
This approach enables sequential learning, where knowledge is continuously updated as new evidence emerges, closely mirroring the cognitive processes of clinical diagnosis and therapeutic decision-making [78].
Implementation in Clinical Trials
Bayesian methods offer particular advantages in adaptive trial designs, where accumulating data informs modifications to trial parameters. These approaches allow for more efficient resource utilization and ethical patient allocation while maintaining statistical rigor [76].
Bayesian Adaptive Design Protocol
Phase II/III seamless design:
- Define prior probability distribution for treatment effect based on preclinical data, early-phase trials, or expert opinion
- Establish pre-specified decision rules for interim analyses based on posterior probabilities
- Enroll initial cohort and collect primary endpoint data
- Conduct interim analysis calculating posterior probability of treatment efficacy
- Apply decision rules:
- If Pr(δ > 0 | data) > 0.95: stop for efficacy
- If Pr(δ > 0 | data) < 0.10: stop for futility
- Otherwise: modify sample size or randomize additional patients
- Repeat steps 4-5 until reaching definitive conclusion or maximum sample size
- Report posterior distribution of treatment effect with credible intervals
A prominent application of Bayesian methods occurred in the pivotal trial for a COVID-19 vaccine, where adaptive elements enabled efficient evaluation during the public health emergency [78].
Incorporating External Data
Bayesian methods provide a formal framework for incorporating external data sources through informative priors. This is particularly valuable in rare diseases where historical controls or natural history data can strengthen inferences from small trials [76].
Power prior approach:
- Identify relevant external data sources (historical trials, registry data)
- Define weighting parameter (0 ≤ a₀ ≤ 1) representing discounting of external data
- Construct power prior: p(θ | D₀, a₀) ∝ L(θ | D₀)^{a₀} × p₀(θ)
- Combine with current trial likelihood: p(θ | D, D₀, a₀) ∝ L(θ | D) × L(θ | D₀)^{a₀} × p₀(θ)
- Analyze posterior distribution to estimate treatment effects
Applications in Disease Network Research and Drug Repurposing
Bayesian approaches are particularly valuable in diseasome research for integrating heterogeneous data types across the disease network. They enable formal combination of genomic, transcriptomic, clinical, and real-world evidence to identify novel drug repurposing opportunities [1].
For example, researchers can use Bayesian hierarchical models to estimate the probability that a drug targeting one disease node might be effective for a connected disease, incorporating evidence from molecular networks, animal models, and observational clinical data. This approach naturally handles the multi-scale, interconnected nature of the diseasome.
Integrated Methodological Applications
Synergies in Complex Research Questions
The combination of self-controlled designs and Bayesian methods offers particularly powerful approaches for addressing complex questions in disease networks. Self-controlled designs minimize confounding by fixed factors, while Bayesian approaches enable formal incorporation of prior evidence about disease relationships.
Application protocol for drug safety surveillance in comorbid populations:
- Identify drug-outcome pairs of interest based on disease network proximity
- Implement SCCS design using real-world data from patients with comorbid conditions
- Develop informative priors for association strength based on pharmacological plausibility
- Analyze using Bayesian SCCS models to estimate posterior probability of association
- Validate findings across multiple data sources using Bayesian meta-analytic approaches
Visualization of Integrated Analytical Framework
Diagram 1: Integrated analytical framework for diseasome research
Table 2: Research Reagent Solutions for Advanced Study Designs
| Reagent/Resource | Function | Application Context |
|---|---|---|
| Common Data Models (CDM) | Standardize structure and terminology across disparate data sources | Multi-database studies using electronic health records [77] |
| Bayesian Computation Software | Implement Markov Chain Monte Carlo sampling for posterior estimation | Complex Bayesian models with non-conjugate priors [78] |
| Contrast Assessment Tools | Verify color contrast ratios for data visualization accessibility | Creating compliant diagrams and research outputs [33] [79] |
| Disease Ontology Resources | Provide standardized disease concepts and relationships | Mapping nodes and edges in disease network analyses [1] |
| Self-Controlled Design Code Repositories | Implement validated algorithms for SCCS and case-crossover designs | Reproducible pharmacoepidemiologic safety studies [75] [77] |
Experimental Protocols and Workflows
Protocol for Comparative Self-Controlled Analysis
Based on a recent multinational study of COVID-19 vaccines and myocarditis, the following protocol outlines a robust approach for comparing multiple self-controlled designs [77]:
Data Standardization
- Convert source data to common data model (e.g., ConcePTION CDM)
- Define common exposure and outcome algorithms across databases
- Establish consistent time-oriented data structure
Cohort Identification
- Include individuals experiencing both exposure and outcome during study period
- Apply consistent eligibility criteria across data partners
- Define clear index dates for each design variant
Parallel Analysis
- Implement standard SCCS with pre-exposure referent periods
- Implement extended SCCS accounting for event-dependent exposures
- Implement SCRI with pre-vaccination control windows
- Implement SCRI with post-vaccination control windows
Sensitivity Analyses
- Vary focal window durations based on biological plausibility
- Adjust for time-varying confounders (age, seasonality)
- Assess impact of transition window duration
Meta-Analysis
- Pool estimates across databases using appropriate random-effects models
- Assess between-design heterogeneity using I² statistics
- Evaluate consistency of conclusions across methodological approaches
Workflow Visualization for Self-Controlled Analysis
Diagram 2: Self-controlled design analysis workflow
Self-controlled trials and Bayesian methods represent sophisticated approaches that address fundamental challenges in modern clinical research and diseasome science. Self-controlled designs elegantly mitigate confounding by between-person differences through within-person comparisons, while Bayesian methods provide a formal framework for accumulating evidence across studies and incorporating prior knowledge. Their integration offers particularly powerful approaches for investigating complex relationships within disease networks, enabling more robust drug repurposing decisions and safety surveillance. As these methodologies continue evolving, they promise to enhance the efficiency and validity of inferences drawn from both experimental and real-world data sources, ultimately advancing understanding of the interconnected nature of human disease.
In the field of diseasome and disease network research, robust statistical validation is paramount for distinguishing true biological signals from spurious correlations. As researchers increasingly model diseases as complex network perturbations, the need for rigorous frameworks to validate these models has grown exponentially. Two powerful methodological approaches have emerged as cornerstones for this task: permutation testing, which provides a non-parametric means of assessing statistical significance, and cross-dataset replication, which establishes generalizability across diverse populations and data sources. This whitepaper provides an in-depth technical examination of these complementary frameworks, detailing their theoretical foundations, implementation protocols, and applications within disease network research to enable researchers and drug development professionals to build more reliable, reproducible findings.
Theoretical Foundations
Permutation Testing Framework
Permutation testing represents a non-parametric statistical approach that empirically generates the null hypothesis distribution by repeatedly shuffling data labels. This method requires no theoretical knowledge of how the test statistic is distributed under the null hypothesis, making it particularly valuable for complex data structures like disease networks where theoretical distributions may be unknown or unreliable [80] [81]. The fundamental strength of permutation testing lies in its ability to provide exact statistical tests that maintain type I error rates at the nominal level, provided the assumption of exchangeability is met—meaning that under the null hypothesis, the joint distribution of observations remains unchanged when group labels are permuted [81].
In the context of diseasome research, permutation testing enables network-level comparisons that incorporate topological features inherent in each individual network, moving beyond simplistic summary metrics or mass-univariate approaches that ignore the complex interconnected nature of biological systems [80]. This approach has been successfully applied across diverse domains, from brain network analyses [80] [81] to genome-wide association studies [82], demonstrating its versatility for complex biological data.
Cross-Validation and Replication Framework
Cross-validation comprises a set of model validation techniques that assess how results from statistical analyses will generalize to independent datasets [83]. By partitioning data into complementary subsets and repeatedly performing analysis on one subset while validating on another, cross-validation provides an estimate of model performance on unseen data, helping to detect issues like overfitting and selection bias [83].
Within the replication hierarchy, cross-validation represents a form of "simulated replication" that can be implemented when direct replication (reproducing exact effects under identical conditions) or conceptual replication (extending effects to new contexts) is not feasible due to practical or methodological constraints [84]. For disease network research, this approach is particularly valuable given the frequent impossibility of replicating studies on extremely rare conditions or large clinical-epidemiological cohorts [84].
Table 1: Hierarchy of Replication Approaches in Disease Network Research
| Replication Type | Definition | Application Context | Strengths | Limitations |
|---|---|---|---|---|
| Direct Replication | Attempts to reproduce exact effects using identical experimental conditions | When identical patient cohorts and measurement protocols are available | Highest form of validation; confirms exact reproducibility | Often infeasible for rare diseases or large biobanks |
| Conceptual Replication | Examines general nature of previously obtained effects in new contexts | Testing disease network principles across different biological systems | Demonstrates broader validity of concepts | Does not confirm exact original findings |
| Simulated Replication (Cross-Validation) | Uses data partitioning to simulate replication within a single dataset | When direct or conceptual replication is not feasible | Computationally efficient; uses existing data fully | Still operates on single dataset; may not capture population differences |
Methodological Approaches
Core Permutation Testing Methodology
The permutation testing framework follows a systematic procedure that can be adapted to various research contexts in disease network analysis:
Calculate Observed Test Statistic: Compute the test statistic of interest (e.g., network similarity measure) for the original data with true group labels [80] [81].
Generate Permuted Datasets: Randomly permute group labels across observations while maintaining data structure, creating numerous pseudo-datasets where the null hypothesis is known to be true [82] [81].
Build Null Distribution: Calculate the test statistic for each permuted dataset, constructing an empirical null distribution [80].
Determine Significance: Compare the observed test statistic to the null distribution, calculating the p-value as the proportion of permuted test statistics that are as extreme as or more extreme than the observed value [82].
For genome-wide association studies, different permutation strategies offer varying advantages: case-control status permutation (column permutation) represents the gold standard, while SNP permutation (row permutation) provides an alternative when raw data are unavailable, and gene permutation maintains linkage disequilibrium but may offer limited specificity improvements [82].
Advanced Permutation Tests for Network Data
Disease network research often requires specialized permutation approaches that account for network topology:
Jaccard Index Permutation Test (PNF-J) This method evaluates consistency in key network nodes (e.g., high-degree hubs or disease-associated proteins) across groups [80] [81]. The implementation involves:
- Identifying key nodes based on nodal characteristics (degree, centrality) using consistent criteria across all networks
- Calculating Jaccard index between all network pairs: J = |A∩B|/|A∪B|
- Computing Jaccard ratio RJ = MJ(Within)/MJ(Between) as test statistic
- Assessing significance through label permutation [80]
Kolmogorov-Smirnov Permutation Test (PNF-KS) This approach compares degree distributions between groups using the Kolmogorov-Smirnov statistic to quantify distance between cumulative distribution functions, with significance assessed through the same permutation framework [81].
Table 2: Permutation Test Selection Guide for Disease Network Research
| Research Question | Recommended Test | Test Statistic | Data Requirements | Key Applications in Disease Networks |
|---|---|---|---|---|
| Consistency of key network elements | Jaccard Index Permutation Test (PNF-J) | Jaccard Ratio (RJ) | Binary node sets identified by specific characteristics | Identifying conserved disease hubs across patient subtypes |
| Overall network topology differences | Kolmogorov-Smirnov Permutation Test (PNF-KS) | K-S statistic | Degree distributions for all nodes | Comparing global network architecture between disease states |
| Pathway over-representation in genomic networks | Hypergeometric Test with Permutation | Enrichment p-value | Gene-pathway mappings and association p-values | Validating disease-associated functional pathways in GWAS |
| Small-scale network comparisons | Case-control status permutation | User-defined network metric | Raw case-control data | Controlled studies with complete data access |
| Large-scale or summary data network comparisons | SNP-based permutation | User-defined network metric | Summary statistics only | Biobank studies with restricted data access |
Cross-Validation Implementation
Cross-validation techniques simulate replication by systematically partitioning data into training and testing sets:
k-Fold Cross-Validation The dataset is randomly partitioned into k equal-sized subsamples (typically k=10). Of these k subsamples, a single subsample is retained as validation data, and the remaining k−1 subsamples are used as training data. The process is repeated k times, with each subsample used exactly once as validation data [83].
Leave-One-Subject-Out Cross-Validation (LOSO) This approach takes k-fold to its logical extreme, where k equals the number of subjects. For each iteration, a single subject is used as the test set and all remaining subjects form the training set. This method is particularly valuable in clinical diagnostic applications where the model will ultimately predict outcomes for new individuals [84].
Stratified Variants Stratified cross-validation ensures that partitions maintain approximately equal proportions of important characteristics (e.g., disease subtypes, demographic factors), preventing biased performance estimates [83].
Experimental Protocols
Integrated Validation Framework for Disease Phenotyping
Recent advances in computational phenotyping demonstrate how permutation testing and cross-validation can be integrated into a comprehensive validation framework. A study defining 313 diseases in the UK Biobank implemented a multi-layered validation approach incorporating [85]:
Data Source Concordance: Assessing consistency of phenotype definitions across multiple electronic health record sources and medical ontologies (Read v2, CTV3, ICD-10, OPCS-4)
Epidemiological Validation: Comparing age-sex incidence and prevalence patterns against established epidemiological knowledge
External Population Comparison: Validating against a representative UK EHR dataset to assess generalizability beyond the biobank population
Risk Factor Validation: Confirming established modifiable risk factor associations
Genetic Validation: Assessing genetic correlations with external genome-wide association studies
This comprehensive approach establishes validation profiles that improve phenotype generalizability despite inherent demographic biases in biobank data [85].
In Vivo V3 Framework for Digital Measures
The adaptation of the clinical V3 Framework (Verification, Analytical Validation, and Clinical Validation) for preclinical research provides another robust validation structure for digital measures in disease network research [86]:
Verification: Ensuring digital technologies accurately capture and store raw data from biological systems
Analytical Validation: Assessing precision and accuracy of algorithms that transform raw data into meaningful biological metrics
Clinical Validation: Confirming that digital measures accurately reflect relevant biological or functional states in model systems
This structured approach enhances the reliability and applicability of digital measures in preclinical research, supporting more robust and translatable drug discovery processes [86].
Visualization of Methodological Workflows
Permutation Testing Workflow
Cross-Validation Workflow
The Scientist's Toolkit
Essential Research Reagent Solutions
Table 3: Key Computational Tools for Validation Frameworks
| Tool Category | Specific Tools/Platforms | Primary Function | Application in Disease Network Research |
|---|---|---|---|
| Statistical Computing | R, Python (Scikit-learn), MATLAB | Implementation of permutation tests and cross-validation schemes | Flexible coding environment for custom validation workflows |
| Specialized Validation Packages | PredPsych, GeneTrail, axe-core | Domain-specific validation implementations | Accessible tools for psychologists (PredPsych) [84] or genomic researchers (GeneTrail) [82] |
| Accessibility Validation | axe-core, W3C ACT Rules | Color contrast validation for visualizations | Ensuring accessibility of network diagrams and data visualizations [33] [87] |
| Color Palette Tools | Coolors | Color palette generation with contrast checking | Creating accessible color schemes for network visualizations [88] |
| Biobank Analysis Platforms | UK Biobank, All of Us, FinnGen | Large-scale integrated data resources | Applying validation frameworks to real-world disease network data [85] |
Permutation testing and cross-dataset replication represent complementary pillars of rigorous validation in diseasome and disease network research. The permutation framework provides robust non-parametric significance testing that accommodates complex network structures, while cross-validation and replication approaches ensure findings generalize beyond specific datasets. As disease network research continues to evolve, integrating these validation approaches into standardized computational frameworks—such as the multi-layered phenotyping validation [85] and in vivo V3 framework [86]—will be essential for building reproducible, translatable knowledge about disease mechanisms and therapeutic strategies. By adopting these comprehensive validation frameworks, researchers and drug development professionals can enhance the reliability of their findings and accelerate the translation of network-based discoveries into clinical applications.
The diseasome concept frames human diseases not as independent entities, but as interconnected nodes in a complex network, where links represent shared molecular foundations, such as genes, proteins, or metabolic pathways [1]. This paradigm shift enables a systems-level understanding of disease etiology, revealing unexpected relationships between seemingly distinct pathologies and opening new avenues for drug repurposing and the identification of novel therapeutic targets [1]. The field of network medicine has emerged over the last decade to exploit these connections, using network theory to reveal hidden relationships among diseases, physiological processes, and genes [1].
Multi-layer network integration represents a sophisticated computational framework that expands upon this concept by formally bridging disparate data types. It moves beyond single-layer networks to construct a unified model where each layer—such as genomic, transcriptomic, proteomic, and clinical imaging data—captures a unique dimension of biological organization [89]. The integration of these layers creates a more comprehensive representation of disease pathophysiology, linking molecular signatures directly to phenotypic manifestations observed in clinical settings [89]. This approach is particularly transformative in oncology, where tumor heterogeneity and complexity demand a multi-faceted analytical strategy [89]. By mapping the intricate connections across biological scales, multi-layer networks provide a powerful scaffold for understanding disease mechanisms and advancing personalized medicine.
Data Modalities for Integration
Constructing a multi-layer network requires the harmonization of diverse data modalities, each providing a unique and complementary view of the disease state. These modalities can be broadly categorized into molecular multi-omics data and clinical/imaging data.
Multi-Omics Data
Multi-omics data provides a deep, molecular-level characterization of a patient's disease, typically derived from tissue or blood samples [89].
Table 1: Core Multi-Omics Data Types
| Data Type | Description | Key Technologies | Insight Gained |
|---|---|---|---|
| Genomics | DNA sequence and variation | Whole Genome Sequencing, SNP Arrays | Identifies inherited and somatic mutations, structural variants, and disease-associated genetic risk loci. |
| Transcriptomics | RNA expression levels | RNA-Seq, Microarrays | Reveals gene activity, alternative splicing events, and expression subtypes; links genotype to molecular phenotype. |
| Epigenomics | Heritable, non-sequence-based regulatory modifications | ChIP-Seq, ATAC-Seq, Bisulfite Sequencing | Maps DNA methylation, histone modifications, and chromatin accessibility, informing on gene regulation mechanisms. |
| Proteomics | Protein identity, quantity, and modification | Mass Spectrometry, RPPA | Characterizes the functional effector molecules, signaling pathway activity, and post-translational regulation. |
| Metabolomics | Profiles of small-molecule metabolites | Mass Spectrometry, NMR | Provides a snapshot of cellular physiology and biochemical activity, downstream of genomic and proteomic influences. |
Large-scale consortia like The Cancer Genome Atlas (TCGA) have been instrumental in generating comprehensive, matched multi-omics datasets for thousands of patients, serving as a foundational resource for the research community [89].
Clinical and Medical Imaging Data
Clinical and imaging data capture the macroscopic, phenotypic manifestation of disease, offering a non-invasive window into tumor characteristics and patient health status [89].
Table 2: Clinical and Medical Imaging Data Types
| Data Type | Description | Key Modalities | Insight Gained |
|---|---|---|---|
| Medical Imaging | Non-invasive visualization of internal anatomy and function | MRI, CT, PET, Histopathology | Provides spatial context, revealing tumor size, location, shape, texture (radiomics), and metabolic activity. |
| Clinical Phenotypes | Structured patient information | Electronic Health Records (EHRs) | Documents patient demographics, medical history, lab results, treatment regimens, and overall survival. |
| Radiogenomics | A subfield linking imaging features to genomic data | Correlative Analysis | Establishes non-invasive biomarkers, predicting molecular subtypes from imaging features alone [89]. |
Initiatives like The Cancer Imaging Archive (TCIA) often partner with TCGA to provide co-registered imaging and omics data, enabling true multimodal analysis [89].
Methodologies for Multi-Layer Network Fusion
The core challenge in multi-layer network integration is the computational fusion of heterogeneous, high-dimensional data. Artificial Intelligence (AI) provides the primary strategies for this task, which can be categorized into three main paradigms [89].
Early Fusion (Feature-Level Fusion)
In early fusion, raw or pre-processed features from different modalities (e.g., gene expression values and radiomic features from an MRI) are concatenated into a single, unified feature vector at the input stage. This combined vector is then fed into a machine learning or deep learning model.
Diagram 1: Early fusion architecture for multi-layer networks.
Advantages:
- Allows the model to learn complex, non-linear interactions between features of different modalities from the very beginning [89].
- Can capture subtle, cross-modal correlations that might be lost in later stages of processing.
Disadvantages:
- Highly susceptible to overfitting due to the high dimensionality of the combined feature space [89].
- Requires all modalities to be available for every patient and can be sensitive to misalignment between data types.
Protocol:
- Feature Extraction: Independently extract features for each modality. For omics data, this may involve normalized expression values or pathway enrichment scores. For images, this involves extracting radiomic features (e.g., texture, shape) using tools like PyRadiomics.
- Normalization: Standardize features from each modality (e.g., Z-score normalization) to ensure they are on a comparable scale.
- Concatenation: Combine the normalized feature vectors from all modalities into a single, long vector for each subject.
- Model Training: Train a predictive model (e.g., a Support Vector Machine or fully connected Deep Neural Network) on the concatenated feature set.
Late Fusion (Decision-Level Fusion)
Late fusion takes a modular approach. Separate, modality-specific models are trained independently on their respective data types. Their predictions are then combined at the final decision stage.
Diagram 2: Late fusion with independent model predictions.
Advantages:
- Robustness: The failure or absence of one modality does not necessarily break the entire system, as other models can still contribute [89].
- Interpretability: It is often easier to understand the contribution of each individual data type to the final prediction.
- Allows the use of state-of-the-art, modality-specific models (e.g., Convolutional Neural Networks for images, Graph Neural Networks for networks).
Disadvantages:
- Cannot model complex, low-level interactions between different data modalities.
Protocol:
- Model Specialization: Train a dedicated classifier for each data modality (e.g., a CNN for medical images, a classifier for genomic data).
- Prediction Generation: Use each specialized model to generate a set of predictions or probability scores for each patient.
- Fusion: Combine these predictions using a meta-classifier (e.g., a logistic regression model) or a simpler method like weighted averaging or voting to produce the final integrated output.
Hybrid Fusion
Hybrid fusion strategies seek to leverage the strengths of both early and late fusion by integrating information at multiple levels of the model architecture. This often involves using intermediate representations from different modalities.
Diagram 3: Hybrid fusion with cross-modal attention.
Advantages:
- Balances the capacity for learning complex feature interactions with the robustness and interpretability of modular designs.
- Can achieve state-of-the-art predictive performance by capturing a more complete picture of the data [89].
Disadvantages:
- Architecturally complex and can be computationally intensive to design and train.
Protocol:
- Modality-Specific Encoding: Pass each data type through a dedicated neural network to generate a high-level embedding (e.g., using a CNN for images, an autoencoder for omics data).
- Intermediate Fusion: Fuse these embeddings using a technique like a cross-modal attention mechanism, which allows the model to dynamically weigh the importance of features from one modality when processing another [89].
- Joint Learning: The fused representation is then passed through additional layers for the final prediction task, allowing joint learning across modalities.
Experimental Protocol for Multi-Layer Network Analysis
The following provides a detailed, step-by-step protocol for a typical multi-layer network study integrating transcriptomic data and medical images for cancer prognosis prediction, following best practices from the literature [89].
Table 3: Key Research Reagent Solutions
| Category | Item / Software | Function |
|---|---|---|
| Data Resources | The Cancer Genome Atlas (TCGA) | Provides standardized, matched multi-omics data (genomics, transcriptomics) for large patient cohorts. |
| The Cancer Imaging Archive (TCIA) | Provides curated medical imaging data (MRI, CT) often linked to TCGA patients. | |
| Programming Languages | Python (v3.8+) / R (v4.0+) | Core languages for data manipulation, statistical analysis, and machine learning implementation. |
| Key Python Libraries | PyTorch / TensorFlow | Deep learning frameworks for building and training complex fusion models (CNNs, Transformers). |
| Scikit-learn | Provides tools for data pre-processing, classical machine learning models, and model evaluation. | |
| NumPy, Pandas | Foundational libraries for numerical computation and data manipulation. | |
| OpenCV, PyRadiomics | Used for medical image processing and radiomic feature extraction. | |
| Scanpy (Python) / Seurat (R) | Specialized tools for the analysis and pre-processing of single-cell and bulk transcriptomics data. |
Step 1: Data Acquisition and Curation
- Objective: Assemble a curated cohort with matched molecular and clinical imaging data.
- Procedure:
- Identify a patient cohort from a public repository like TCGA and its linked imaging data in TCIA [89].
- Download the relevant clinical data, including overall survival time and vital status.
- Download the corresponding transcriptomic data (e.g., RNA-Seq FPKM values).
- Download the associated medical images (e.g., pre-treatment MRI scans).
Step 2: Data Preprocessing
- Objective: Clean, normalize, and extract relevant features from each data modality to prepare them for integration.
- Procedure:
- Clinical Data: Handle missing values. Use survival time and status as the target outcome for a Cox proportional-hazards model.
- Transcriptomic Data:
- Apply log2(FPKM + 1) transformation.
- Perform gene-level normalization (e.g., Z-score standardization).
- Filter for the top ~5,000 most variable genes or a pre-defined gene signature relevant to the cancer type.
- Medical Imaging Data:
- Image Preprocessing: Re-sample all images to a uniform voxel spacing. Apply intensity normalization (e.g., Z-score across all voxels).
- Tumor Segmentation: Manually or automatically delineate the 3D tumor volume using software like 3D Slicer. This requires expert radiologist input for accuracy.
- Radiomic Feature Extraction: Use a standardized software platform like PyRadiomics to extract a set of quantitative features from the segmented tumor volume. This typically includes shape, first-order statistics, and texture features.
Step 3: Network Construction and Model Implementation
- Objective: Build a multi-layer network and train a predictive model using a hybrid fusion approach.
- Procedure:
- Define Network Layers: Construct two core network layers:
- Gene Co-expression Network: Create a patient-by-gene matrix from the processed transcriptomic data.
- Radiomic Feature Network: Create a patient-by-radiomic feature matrix.
- Implement a Hybrid Fusion Model:
- Inputs: The processed gene expression vector and radiomic feature vector for a single patient.
- Architecture:
- Modality-Specific Branches: Use two separate fully connected neural networks to process each input vector into a lower-dimensional embedding (e.g., 128-dimensional).
- Fusion Layer: Concatenate these two embeddings into a single, unified representation.
- Output Layer: Feed the concatenated vector into a final output layer configured for a Cox proportional-hazards loss function to predict survival risk.
- Model Training:
- Split the data into training (70%), validation (15%), and test (15%) sets, ensuring patient independence.
- Train the model on the training set, using the validation set for early stopping to prevent overfitting.
- Optimize the model using the Adam optimizer.
- Define Network Layers: Construct two core network layers:
Step 4: Model Validation and Interpretation
- Objective: Evaluate the model's performance and interpret the biological and clinical insights it generates.
- Procedure:
- Performance Evaluation: On the held-out test set, evaluate the model using the Concordance Index (C-Index) to assess its ability to rank patients by their risk.
- Statistical Comparison: Compare the C-Index of the multi-modal model against unimodal benchmarks (e.g., a model using only genomics or only imaging) using a paired t-test.
- Interpretability Analysis: Apply techniques like SHAP (SHapley Additive exPlanations) to the trained model to determine which specific genes and radiomic features were most influential in predicting high-risk patients. This can generate biologically testable hypotheses.
Multi-layer network integration represents a paradigm shift in biomedical research, moving the field closer to the core principles of the diseasome by formally connecting molecular mechanisms to clinical phenotypes. While significant challenges remain—particularly in data standardization, computational scalability, and clinical translation—the fusion of multi-omics and medical imaging data through advanced AI is poised to redefine precision oncology. Future progress will depend on the development of more interpretable and robust fusion models, larger multi-modal datasets, and, crucially, frameworks that foster collaboration between computational scientists, biologists, and clinicians to ensure these powerful tools deliver tangible improvements in patient care.
Validating Network Insights: Case Studies and Comparative Analysis Across Diseases
The drug development landscape for Alzheimer's disease (AD) is undergoing a significant transformation, characterized by a dynamic pipeline and a strategic pivot toward network-based therapeutic discovery. This shift is increasingly informed by the diseasome and disease network concepts, which recognize AD not as a consequence of single gene defects but as a pathophysiological state arising from perturbations across a complex, interconnected cellular network. The 2025 pipeline reflects this evolution, with 182 active clinical trials assessing 138 drugs across diverse biological targets [90] [91]. This analysis provides an in-depth examination of the current AD drug development pipeline, detailing the quantitative landscape, exploring the application of network medicine in target discovery, and presenting standardized experimental protocols for validating novel network-derived targets.
Current State of the AD Drug Development Pipeline
The AD drug development pipeline has expanded significantly, demonstrating renewed momentum in the field. The following table summarizes the core quantitative data for the 2025 pipeline.
Table 1: 2025 Alzheimer's Disease Drug Development Pipeline at a Glance
| Metric | Count | Details/Significance |
|---|---|---|
| Total Active Trials | 182 | Spanning Phase 1, 2, and 3 [91] |
| Unique Drugs in Development | 138 | Includes both novel and repurposed agents [90] [91] |
| Phase 1 Trials | 48 | Notable increase from 27 in 2024, indicating growing early-stage innovation [91] |
| Disease-Targeted Therapies (DTTs) | 74% of pipeline | Therapies intending to alter underlying disease pathology [90] [91] |
| Repurposed Agents | 46 drugs (33% of pipeline) | Potential for reduced development time and lower risk profiles [90] [91] |
| Clinical Trial Sites | 2,227 in North America; 2,302 globally | Reflects the extensive, worldwide effort in AD clinical research [91] |
Therapeutic Modalities and Target Mechanisms
The pipeline is characterized by its mechanistic diversity, moving beyond traditional, single-target approaches. The Common Alzheimer's Disease Research Ontology (CADRO) categorizes targets into over 15 distinct biological processes [90].
Table 2: Key Therapeutic Targets and Representative Agents in the AD Pipeline
| CADRO Target Category | Representative Agents / Drug Classes | Therapeutic Purpose |
|---|---|---|
| Amyloid Beta (Aβ) | Lecanemab (Leqembi), Donanemab, Aducanumab (Aduhelm) | DTT (Biologic) [92] |
| Tau Protein | Posdinemab (Fast Track designated), Tau aggregation inhibitors | DTT (Biologic & Small Molecule) [92] |
| Inflammation | Undisclosed anti-inflammatory agents | DTT [90] [92] |
| Synaptic Plasticity/Neuroprotection | AXS-05 (dextromethorphan & bupropion) | Symptomatic (Neuropsychiatric Symptoms) [92] |
| Metabolism & Bioenergetics | Semaglutide (repurposed GLP-1 receptor agonist) | DTT (Repurposed Agent) [92] [91] |
| APOE, Lipids, & Lipoprotein Receptors | Various early-stage candidates | DTT [90] |
| Multitarget | Combinations and agents with multiple mechanisms | DTT & Symptomatic [90] |
Network Medicine in AD Target Discovery
The "diseasome" concept posits that diseases are interconnected via shared genetic and molecular components, and that a disease phenotype manifests from a network of pathobiological processes [52]. Applying this conceptual framework to AD involves mapping the complex interactions between genetic variants, molecular pathways, and cell types to identify critical "key driver" nodes whose perturbation can alter the entire disease network state.
Predictive Network Modeling for Key Driver Identification
A pivotal study employed an integrative, multi-omics approach to build robust, cell type-specific predictive network models of AD [93]. The methodology delineated below provides a template for applying diseasome principles to AD target discovery.
Table 3: Experimental Protocol for Predictive Network Analysis & Key Driver Validation
| Stage | Protocol Details | Application in AD Research |
|---|---|---|
| 1. Data Input & Deconvolution | - Input: Bulk-tissue RNA-seq data from post-mortem brain regions (e.g., from AMP-AD consortium). | |
| - Deconvolution Method: Population-specific expression analysis (PSEA) to derive neuron-specific gene expression signals from bulk tissue data [93]. | Isolates cell-type specific signals, crucial for discerning neuronal contributions to the AD diseasome from other brain cell types. | |
| 2. Network Construction | - Algorithm: Predictive network modeling, integrating Bayesian networks with bottom-up causality inference. |
- Priors: Incorporation of genetic variation (e.g., SNPs) as causal anchors to resolve network directionality.
- Process: Constructs causal network models from deconvoluted gene expression and clinical/pathological traits [93]. | Infers causal, rather than merely correlative, relationships within the AD molecular network. Replicated independently across cohorts (e.g., MAYO, ROSMAP) for robustness. | | 3. Key Driver Analysis & Prioritization | - Identification: Agnostic scanning of the network for genes predicted to modulate network states associated with AD pathology.
- Prioritization: Selection of key drivers that replicate across independent cohort networks [93]. | A study identified 19 top-priority neuronal key drivers, including JMJD6, NSF, and RBM4 [93]. | | 4. Experimental Validation | - Model System: Human induced pluripotent stem cell (iPSC)-derived neurons [93].
- Perturbation: shRNA-mediated knockdown of predicted key driver genes.
- Phenotypic Assays: Measurement of Aβ38, Aβ40, Aβ42, total tau, and phosphorylated tau (p231-tau) peptides [93].
- Network Confirmation: RNA sequencing post-knockdown to verify downstream transcriptional changes predicted by the network model [93]. | Confirms the functional role of key drivers in AD-relevant pathology. Knockdown of 10/19 targets (e.g., JMJD6) significantly altered Aβ and/or p-tau levels, validating the network predictions [93]. |
This workflow successfully identified JMJD6 as a key driver capable of modulating both amyloid and tau pathology, positioning it as a high-priority target with relevance to multiple core features of the AD diseasome [93].
Diagram 1: Network-driven target discovery workflow.
The Scientist's Toolkit: Essential Reagents for Network Validation
Table 4: Key Research Reagent Solutions for AD Network Validation Studies
| Reagent / Material | Function in Experimental Protocol |
|---|---|
| Human iPSC Lines | Provides a physiologically relevant, human-derived neuronal model for functional validation of key drivers [93]. |
| shRNA or CRISPR-Cas9 Systems | Enables targeted knockdown or knockout of predicted key driver genes in iPSC-derived neurons to assess phenotypic consequences [93]. |
| ELISA/Kits for Aβ Peptides (Aβ38, 40, 42) | Quantifies changes in amyloid pathology following key driver perturbation [93]. |
| Immunoassays for Tau & p-tau (e.g., p231-tau) | Measures tau pathology and hyperphosphorylation, a key AD hallmark, in response to target modulation [93]. |
| RNA Sequencing Library Prep Kits | Facilitates whole-transcriptome analysis to confirm downstream network effects and identify regulated pathways post-knockdown [93]. |
| Cell Type-Specific Biomarker Panels | Used for deconvolution algorithms and to validate the cellular identity of iPSC-derived neurons (e.g., neuronal markers) [93]. |
Analysis of Signaling Pathways and Network Biology
The validation of key drivers like JMJD6, which influences both Aβ and tau, suggests these nodes may reside at critical integrative points within the AD diseasome. Follow-up RNA sequencing after key driver knockdown revealed that these validated targets are potential upstream regulators of master regulatory proteins like REST and VGF, connecting them to broader neuroprotective and stress response pathways [93].
Diagram 2: Key drivers as integrators in the AD diseasome.
The Alzheimer's disease drug development pipeline is more robust and diverse than ever, reflecting a field in transition. The integration of diseasome and network medicine principles is driving a new wave of discovery, moving the focus from isolated targets to critical nodes within a complex disease network. The successful identification and validation of key drivers like JMJD6 through integrative computational and experimental workflows exemplify the power of this approach [93]. Future success will likely depend on continued innovation in several key areas: the development of multi-target therapies or combination treatments that address the network-based nature of AD; the enhanced use of biomarkers for patient stratification and target engagement; and the strategic repurposing of drugs to accelerate the availability of new treatment options [90] [92] [91]. As these trends converge, the potential to deliver transformative therapies that meaningfully alter the course of Alzheimer's disease is increasingly within reach.
This technical guide explores the application of network analysis to elucidate complex comorbidity patterns in Chronic Obstructive Pulmonary Disease populations. By moving beyond traditional binary associations, this approach reveals the intricate web of interconnections among concomitant chronic conditions through the construction and analysis of disease networks. Framed within the broader context of diseasome research, this whitepaper synthesizes methodologies, findings, and clinical implications from large-scale studies, providing researchers and drug development professionals with advanced analytical frameworks for understanding COPD multimorbidity. The integration of administrative health data with network science principles offers unprecedented opportunities for identifying central disease hubs, detecting clinically relevant clusters, and uncovering sex-specific patterns that inform patient-centered care and therapeutic development.
The human diseasome represents a network-based framework for understanding disease relationships, where conditions are linked through shared genetic components, molecular pathways, or phenotypic manifestations [53]. This conceptual model has evolved into the discipline of network medicine, which investigates how cellular network perturbations manifest as human diseases [1] [65]. Within this paradigm, chronic obstructive pulmonary disease serves as an ideal model for study due to its high multimorbidity burden and systemic manifestations that extend beyond pulmonary pathology.
COPD ranks as the fourth leading cause of death globally, with the World Health Organization reporting approximately 3.5 million deaths attributable to COPD in 2021 alone [42]. In China, COPD has been the third leading cause of death since 1990, with incidence and mortality rates expected to continue rising over the next 25 years [42]. The clinical complexity of COPD is magnified by its frequent association with multiple concomitant conditions, with studies indicating that 81-96% of COPD patients have at least one comorbidity [42] [94]. These comorbidities significantly impact health status, quality of life, and mortality risk in COPD patients, creating an urgent need for comprehensive approaches to understand their interrelationships.
Methodological Framework for COPD Comorbidity Network Analysis
Large-scale administrative health data form the foundation for robust comorbidity network analysis. Key sources include:
- Hospital discharge records from regional healthcare systems [42]
- Insurance claims databases (Medicare, Medicaid, commercial insurers) [95]
- Electronic health records from primary care databases [96]
- Linked data systems combining multiple sources [97]
Patient identification typically relies on ICD coding systems (ICD-9 or ICD-10) with specific codes for COPD (e.g., ICD-10 codes J41-J44) [42]. Study populations often range from thousands to millions of patients, such as the 2,004,891 COPD inpatients studied in Sichuan Province, China [42]. To ensure analytical robustness, chronic conditions are typically identified using established classification systems, and rare diseases are excluded by applying prevalence thresholds (e.g., ≥1%) [42].
Network Construction Techniques
Comorbidity networks represent diseases as nodes and their co-occurrence strengths as edges. The Salton Cosine Index is frequently employed to calculate association strength due to its independence from sample size [42]:
Where N። represents patients with both diseases i and j, and Nᵢ and Nⱼ represent patients with only disease i or j, respectively.
Statistical significance is determined through correlation measures and multiple testing corrections. The phi correlation coefficient is calculated for disease pairs [42]:
A minimum patient count threshold (e.g., N። > N_minimum) is applied to ensure clinical relevance, and disease pairs are ranked by SCI to determine a cutoff for significant associations [42].
Network Analysis and Community Detection
Once constructed, comorbidity networks undergo topological analysis using various centrality measures:
- Degree centrality: Number of direct connections a disease node has
- Weighted degree: Strength of a node's connections
- Betweenness centrality: Bridge potential between disease clusters
- Eigenvector centrality: Influence based on connection quality
- PageRank algorithm: Iterative importance scoring [42]
Community detection algorithms, particularly the Louvain method, identify clusters of highly interconnected diseases. This algorithm optimizes modularity to partition networks into communities with dense internal connections and sparser external links [42]. Additional analyses include subgroup stratification by sex, age, geographic region, and healthcare utilization patterns to reveal population-specific comorbidity patterns.
The following diagram illustrates the comprehensive workflow for COPD comorbidity network analysis:
Key Research Findings from Large-Scale Studies
Prevalence and Central Comorbidities
Multiple large-scale studies have consistently demonstrated the substantial comorbidity burden among COPD patients. A study of 2,004,891 COPD inpatients in China found that 96.05% had at least one comorbidity, with essential (primary) hypertension being the most prevalent (40.30%) [42]. Network analysis identified 11 central diseases including disorders of glycoprotein metabolism and gastritis/duodenitis, indicating their important bridging roles in the comorbidity network [42].
In the United States, analysis of approximately 11.7 million insured individuals with COPD in 2021 showed varying prevalence and outcomes by insurance type. COPD-related acute inpatient hospitalizations totaled 1.8 million nationwide, with the largest share (86.4%) among Medicare beneficiaries [95]. All-cause mortality for individuals with COPD covered by Medicare (11.5%) was more than double that of Medicaid recipients (5.1%), highlighting significant disparities in outcomes across populations [95].
Table 1: COPD Comorbidity Prevalence and Patterns in Large Studies
| Study Population | Sample Size | Key Comorbidities | Prevalence/Findings |
|---|---|---|---|
| Sichuan Province, China (2015-2019) [42] | 2,004,891 inpatients | Essential hypertension | 40.30% |
| ≥1 comorbidity | 96.05% | ||
| Disorders of glycoprotein metabolism | Central hub disease | ||
| U.S. Insured Population (2021) [95] | ~11.7 million | All-cause mortality (Medicare) | 11.5% |
| All-cause mortality (Medicaid) | 5.1% | ||
| COPD-related hospitalizations | 1.8 million nationwide | ||
| EpiChron Cohort, Spain (2015) [96] | 28,608 COPD patients | Cardio-metabolic diseases | Common cluster |
| Behavioral risk disorders | Sex-specific patterns |
Sex-Specific Patterns
Network analyses have revealed significant sex differences in COPD comorbidity patterns. In the Sichuan study, male networks featured prominent connections with hyperplasia of the prostate, while female networks showed stronger associations with osteoporosis without pathological fracture [42]. These findings reflect both biological differences and potentially sex-specific disease manifestations and progressions.
The EpiChron Cohort study in Spain further elaborated on sex-specific patterns, identifying that multimorbidity networks were mainly influenced by the index disease and also by sex in COPD patients [96]. The study detected common clusters (e.g., cardio-metabolic, cardiovascular, cancer, and neuro-psychiatric) and others specific and clinically relevant in COPD patients, with behavioral risk disorders systematically associated with psychiatric diseases in women and cancer in men [96].
Geographic and Socioeconomic Variations
Substantial geographic variation in COPD prevalence and burden has been observed at state and regional levels. In the U.S., COPD prevalence varied among states, ranging from 44 (Utah) to 143 (West Virginia) per 1000 insured individuals [95]. Similarly, COPD-related hospitalization rates varied significantly, ranging from 97 (Idaho) to 200 (District of Columbia) per 1000 individuals with COPD [95].
The Sichuan study compared urban and rural patients, finding that urban patients demonstrated higher comorbidity prevalence and exhibited more complex comorbidity relationships compared to rural patients [42]. These differences may reflect variations in environmental exposures, healthcare access, diagnostic practices, or socioeconomic factors.
Experimental Protocols for COPD Comorbidity Network Analysis
Data Preprocessing and Comorbidity Identification
- Data Extraction: Collect hospital discharge records, insurance claims, or EHR data spanning a defined period (typically 1-5 years) [42] [95]
- Patient Identification: Select patients with COPD diagnosis codes (ICD-9: 490-492, 496; ICD-10: J41-J44) [42] [94]
- Comorbidity Identification: Extract all additional chronic diagnoses using established classification systems (e.g., Chronic Condition Indicator) [42]
- Prevalence Filtering: Apply prevalence threshold (e.g., ≥1%) to exclude rare conditions using Z-test with Bonferroni correction [42]
- Data Stratification: Divide study population into subgroups based on sex, age, geographic region, or other relevant factors [42]
Network Construction and Analysis Protocol
Association Calculation: Compute Salton Cosine Index for all disease pairs [42]:
Significance Testing: Calculate phi correlation coefficients and apply statistical testing (t-test) to identify significant associations [42]:
Threshold Determination: Rank disease pairs by SCI and determine cutoff based on top q pairs, where q equals the number of disease pairs satisfying N። > N_minimum [42]
Network Visualization: Construct undirected, weighted comorbidity network using visualization software (e.g., Cytoscape) [94]
Centrality Analysis: Calculate multiple centrality measures (degree, weighted degree, betweenness, eigenvector, PageRank) to identify key diseases [42]
Community Detection: Apply Louvain algorithm to detect disease clusters with dense interconnections [42]
The following diagram illustrates the molecular comorbidity analysis approach that integrates biological network data:
Validation and Robustness Testing
- Subgroup Analysis: Validate findings across population subgroups (sex, age, region) [42]
- Temporal Validation: Split data into training and validation sets across different time periods [94]
- Statistical Testing: Apply false discovery rate correction (e.g., FDR ≤ 10⁻⁷) for multiple comparisons [94]
- Cluster Validation: Use partitioning around medoids (PAM) method to validate disease clusters in independent datasets [94]
- Clinical Correlation: Examine association between network features and clinical outcomes (hospitalizations, mortality) [94] [95]
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Resources for COPD Comorbidity Network Analysis
| Resource Category | Specific Tools/Databases | Function/Purpose |
|---|---|---|
| Data Sources | Hospital Discharge Records [42] | Provides diagnostic data for large patient populations |
| Medicare/Medicaid Claims Data [95] | Offers comprehensive healthcare utilization data | |
| Electronic Health Records [96] | Contains detailed clinical patient information | |
| Analytical Tools | R Programming Language [94] | Statistical computing and network analysis |
| Python [94] | Custom script development for network construction | |
| Cytoscape [94] | Network visualization and analysis | |
| Biological Databases | DisGeNET [98] | Disease-gene associations |
| HPRD (Human Protein Reference Database) [65] | Protein-protein interaction data | |
| Reactome [98] | Biological pathway information | |
| Comparative Toxicogenomics Database [98] | Chemical-gene/protein interactions | |
| Methodological Algorithms | Louvain Algorithm [42] | Community detection in networks |
| PageRank Algorithm [42] | Node centrality measurement | |
| Salton Cosine Index [42] | Disease association strength calculation |
Integration with Molecular Networks and Biological Pathways
Advanced network medicine approaches integrate clinical comorbidity patterns with molecular-level data to uncover shared pathogenic mechanisms. The expanded human disease network combines disease-gene associations with protein-protein interaction information, establishing new connections between diseases [65]. For COPD, this approach has revealed that all major comorbidities are related at the molecular level, sharing genes, proteins, and biological pathways with COPD itself [98].
The Molecular Comorbidity Index quantifies the strength of association between diseases at the molecular level [98]:
Where proteins_dis1→dis2 represents proteins associated with disease 1 that interact with proteins associated with disease 2.
Studies applying this approach have identified known biological pathways involved in COPD comorbidities, such as inflammation, endothelial dysfunction, and apoptosis [98]. More importantly, they have revealed previously overlooked pathways including hemostasis in COPD multimorbidities beyond cardiovascular disorders, and cell cycle pathway in the association of COPD with depression [98]. The tobacco smoke exposome targets an average of 69% of identified proteins participating in COPD multimorbidities, providing mechanistic insights into how smoking contributes to multiple co-occurring conditions [98].
Clinical and Therapeutic Implications
Patient Stratification and Personalized Medicine
Network analysis enables phenotype discovery in COPD based on comorbidity patterns rather than just respiratory parameters. Studies have identified distinct patient clusters with characteristic comorbidity profiles, such as the "behavioral risk disorder" cluster associating mental health conditions with substance abuse in COPD patients [96]. These classifications facilitate tailored interventions for specific patient subgroups and more precise prognostic assessments.
The identification of central hub diseases in comorbidity networks highlights potential leverage points for intervention. Disorders of glycoprotein metabolism and gastritis/duodenitis emerged as central nodes in the Sichuan study, suggesting they may play important roles in disease progression or represent shared pathological mechanisms [42]. Targeting these central conditions may have disproportionate benefits for overall disease management.
Drug Development and Repurposing Opportunities
The diseasome approach provides a powerful framework for drug repurposing by revealing molecular connections between seemingly unrelated conditions [1]. For instance, the discovery that the ADRB2 gene associates COPD with cardiovascular diseases, diabetes, lung cancer, and obesity [98] suggests potential for therapeutics targeting this pathway across multiple conditions. The extensive sharing of biological pathways among COPD comorbidities indicates that single interventions might effectively address multiple conditions simultaneously.
Network analysis also supports adverse event prediction by highlighting drugs that target proteins involved in multiple disease pathways. The integration of the tobacco exposome with comorbidity networks identifies specific chemical compounds that target proteins shared across COPD comorbidities, suggesting both potential mechanisms of comorbidity development and opportunities for protective interventions [98].
Network analysis of COPD comorbidity patterns represents a paradigm shift from traditional single-disease models to a more comprehensive, systems-level understanding of multimorbidity. The application of diseasome concepts to large hospital populations has revealed previously unrecognized disease relationships, sex-specific patterns, and geographic variations that inform both clinical practice and research priorities.
Future developments in this field will likely include:
- Temporal network analysis to understand the evolution of comorbidity patterns over time
- Integration of multi-omics data (genomics, proteomics, metabolomics) with clinical comorbidity networks
- Machine learning applications for dynamic risk prediction based on evolving comorbidity patterns
- Clinical trial designs that account for specific comorbidity clusters rather than excluding multimorbid patients
- Global comparative studies examining COPD comorbidity networks across diverse populations and healthcare systems
As network medicine continues to evolve, its application to COPD and other complex chronic conditions promises to advance our understanding of disease mechanisms, improve patient stratification, and identify novel therapeutic approaches that address the multifaceted nature of multimorbidity.
The diseasome framework conceptualizes human diseases as an interconnected network, where shared molecular pathways and clinical manifestations reveal fundamental biological relationships. Within this framework, heart failure (HF) represents a paradigm of complex multimorbidity, with over 85% of patients presenting with at least two additional chronic conditions [99]. The application of network medicine to HF comorbidity research represents a shift from traditional reductionist approaches toward a systems-level methodology that can capture the intricate web of relationships between HF and its concomitant conditions. This approach hypothesizes that diseases sharing molecular characteristics likely display phenotypic similarities, and that perturbations in one region of the biological network may manifest as multiple, clinically related conditions [99] [1]. The construction of comorbidity networks allows researchers to visualize these relationships graphically, with nodes representing diseases and edges depicting statistical or biological associations between them, creating a powerful tool for understanding the complex clinical landscape of heart failure [99] [100].
Heart failure subtypes, particularly HF with preserved ejection fraction (HFpEF) and HF with reduced ejection fraction (HFrEF), exhibit distinct comorbidity patterns that reflect potentially different underlying pathophysiological mechanisms. Evidence suggests that HFpEF patients demonstrate higher rates of non-cardiac comorbidities, including neoplastic, osteologic, and rheumatoid disorders, while HFrEF patients more frequently present with primarily cardiovascular conditions [99] [100]. These differential comorbidity profiles not only influence clinical presentation and disease trajectory but also hold implications for understanding the genetic and molecular foundations of HF heterogeneity. The systematic mapping of these subtype-specific relationships through comorbidity networks provides a foundation for advancing precision medicine in cardiology, potentially leading to improved patient stratification, targeted therapeutic interventions, and novel insights into disease mechanisms [100] [101].
Methodological Framework for Constructing HF Comorbidity Networks
Data Source Selection and Preprocessing
The construction of robust heart failure comorbidity networks requires careful selection and processing of data sources that comprehensively capture disease phenotypes across large patient populations. Electronic Health Records (EHRs) and administrative claims databases serve as the primary data sources due to their breadth of clinical information and population-scale coverage [99] [101]. The initial step involves accurate identification of HF patients using standardized criteria, typically combining diagnosis codes (e.g., ICD-9 or ICD-10) with clinical parameters. For example, one established protocol defines HF as two or more HF-relevant diagnosis codes OR at least one HF-relevant diagnosis plus objective evidence such as elevated NT-proBNP, recorded NYHA class, or echocardiographic parameters [100]. HF subtyping is then performed based on left ventricular ejection fraction (LVEF) measurements: HFpEF (LVEF ≥50%), HFmrEF (LVEF 40-49%), and HFrEF (LVEF ≤40%) [100].
Once the cohort is established, comorbidity data extraction requires mapping clinical diagnoses to a standardized disease ontology. Commonly used ontologies include PheCodes, ICD, MeSH, and HPO, with selection dependent on the research question and desired level of granularity [99]. Sensitivity analyses have demonstrated that ontology choice significantly influences network topology, necessitating careful consideration of this methodological aspect [99]. Preprocessing typically involves representing comorbidities as binary features (present/absent) for each patient, though some approaches incorporate temporal aspects or disease severity metrics. For conditions with high missing data rates, sophisticated imputation methods such as Multiple Imputation by Chained Equations (MICE) or missForest have been employed, with studies showing these approaches minimize imputation error and prediction difference when applied to laboratory data [101].
Network Construction and Statistical Measures
Comorbidity network construction formalizes disease relationships as a mathematical graph G = (V, E), where V represents diseases (nodes) and E represents statistical associations between them (edges) [99]. The edges can be undirected, directed, weighted, or unweighted, capturing different aspects of disease relationships. Most commonly, comorbidity networks use weighted edges based on statistical association measures that quantify whether two conditions co-occur more frequently than expected by chance given their individual prevalences [99] [100].
Several statistical approaches exist for determining significant comorbidities, each with distinct advantages. The observed-to-expected ratio calculates the ratio between observed co-occurrence and the expected frequency under the independence assumption. Fisher's exact test is frequently employed to assess statistical significance of co-occurrence, with Benjamini-Hochberg correction controlling for multiple testing [100]. The ϕ-correlation coefficient measures association between binary variables and can be interpreted similarly to Pearson correlation [100]. Some advanced implementations scale ϕ-correlation values by dividing by mean correlation values for each disease to account for bias, using these scaled values as edge weights [100]. Network sparsity is typically controlled by applying significance thresholds (e.g., p < 0.0001) and retaining only positive correlations, resulting in a more interpretable network structure [100].
Table 1: Statistical Measures for Comorbidity Network Edge Definition
| Measure | Formula | Application | Advantages |
|---|---|---|---|
| Observed-to-Expected Ratio | O/E = (Nab × N) / (Na × N_b) | Estimates disease pair co-occurrence frequency relative to chance | Intuitive interpretation; accounts for disease prevalence |
| ϕ-Correlation Coefficient | ϕ = (Nab × N¬a¬b - Na¬b × N¬ab) / √(Na × N¬a × Nb × N¬b) | Measures association between binary disease variables | Comparable across disease pairs; familiar interpretation |
| Fisher's Exact Test | p = ( (Na! × N¬a! × Nb! × N¬b!) ) / ( N! × Nab! × Na¬b! × N¬ab! × N¬a¬b! ) | Determines statistical significance of co-occurrence | Appropriate for small sample sizes; exact p-value |
After edge definition, key network topology metrics characterize structural properties: Degree centrality measures the number of connections per node; Betweenness centrality quantifies how often a node lies on the shortest path between other nodes; Closeness centrality calculates the average distance from a node to all other nodes [99]. These metrics help identify diseases that play strategically important roles in the comorbidity network, potentially serving as hubs or bridges between different disease clusters.
Subtype-Specific Comorbidity Patterns in Heart Failure
Distinct Comorbidity Profiles in HFpEF vs. HFrEF
Comprehensive analyses of heart failure subtypes have revealed fundamentally different comorbidity patterns between HFpEF and HFrEF patients. Studies examining 569 comorbidities across thousands of patients found that HFpEF patients exhibit more diverse comorbidity profiles, encompassing a broader range of non-cardiovascular conditions including neoplastic, osteologic, and rheumatoid disorders [100]. In contrast, HFrEF patients demonstrate a more concentrated pattern of cardiovascular comorbidities such as coronary artery disease and prior myocardial infarction [99] [100]. These distinctions are not merely quantitative but represent qualitative differences in disease pathophysiology, suggesting that HFpEF may emerge as a systemic disorder with multifactorial triggers, while HFrEF more often follows direct cardiac injury.
Multiple correspondence analysis has confirmed significant variance between HFpEF and HFrEF comorbidity profiles, with each subtype showing greater similarity to HF with mid-range ejection fraction (HFmrEF) than to each other [100]. This pattern persists after adjusting for age and sex differences, suggesting inherent pathophysiological distinctions. The clinical implications are substantial, as the comorbidity burden in HFpEF appears more strongly associated with non-cardiovascular hospitalizations and mortality, explaining in part the differential treatment response between HF subtypes [99] [100]. Specifically, clinical trials have demonstrated that HFrEF patients respond more consistently to neurohormonal blockade, while HFpEF patients show limited benefit, potentially because their dominant drivers originate outside the traditional cardiovascular pathways.
Sex and Age Stratification in Comorbidity Networks
Beyond the fundamental HFpEF-HFrEF division, comorbidity networks further stratify by sex and age, revealing additional layers of clinical heterogeneity. Research has demonstrated that males with ischemic heart disease exhibit more complex comorbidity networks than females, with not only different connection densities but also qualitatively distinct disease relationships [99]. For instance, in HF-specific networks, conditions such as arthritis appear among the 10 most highly connected nodes exclusively in women, while peripheral vascular disorders demonstrate high connectivity only in male networks [99]. These sex-specific patterns persist after adjustment for demographic variables, suggesting potential biological mechanisms driving differential disease expression.
Age stratification similarly reveals evolving comorbidity relationships across the lifespan. Older HF patients demonstrate higher prevalence of multimorbidity with distinct cluster patterns, often characterized by intertwining cardiovascular, metabolic, and geriatric conditions [101]. The temporal sequence of comorbidity development provides additional insights, with network approaches incorporating timing information to distinguish potential causal relationships from secondary complications [99]. For example, hypertension and diabetes typically precede HF diagnosis, while renal dysfunction often follows HF onset, creating directed edges in temporal comorbidity networks that may reflect pathophysiological sequences rather than mere associations.
Table 2: Subtype-Specific Comorbidity Patterns in Heart Failure
| HF Subtype | Highly Prevalent Comorbidities | Distinctive Comorbidity Features | Molecular Pathways Implicated |
|---|---|---|---|
| HFpEF | Hypertension, Atrial Fibrillation, Anemia, Obesity, Diabetes, COPD, Neoplastic Disorders | Higher non-cardiovascular burden; More diverse comorbidity profiles; Stronger association with inflammatory conditions | Fibrosis (COL3A1, LOX, SMAD9), Hypertrophy (GATA5), Oxidative Stress (NOS1), ER Stress (ATF6) |
| HFrEF | Coronary Artery Disease, Myocardial Infarction, Valvular Heart Disease, Hypertension | Primarily cardiovascular comorbidities; Higher prevalence of ischemic etiology; More uniform comorbidity profiles | Neurohormonal Activation, Myocyte Injury, Mitochondrial Dysfunction, Calcium Handling |
| Sex-Specific Patterns | Female: Arthritis, Thyroid Disorders, Depression; Male: Peripheral Vascular Disease, COPD, Gout | Different network connectivity patterns; Sex-specific comorbidity hubs; Differential drug responses | Sex Hormone Signaling, Immune Response Modulation, Metabolic Regulation |
Advanced Analytical Techniques
Machine Learning for Patient Stratification
Contemporary approaches to HF comorbidity research increasingly leverage machine learning algorithms to identify patient subgroups based on multidimensional comorbidity profiles. Unsupervised methods such as cluster analysis applied to EHR data from 3,745 HF patients revealed four distinct multimorbidity clusters with significant differences in clinical outcomes, particularly unplanned hospitalizations [101]. These data-driven clusters frequently cross traditional HF subtype boundaries, suggesting that comorbidity patterns may represent orthogonal stratification axes to ejection fraction-based classification.
Supervised learning approaches have demonstrated remarkable accuracy in distinguishing HF subtypes based solely on comorbidity profiles. Random forest classifiers and regularized logistic regression (elastic net) trained on 569 PheCodes achieved high discriminatory performance (AUROC >0.8) in separating HFpEF from HFrEF patients, confirming that comorbidity profiles contain substantial signal for subtype classification [100]. Feature importance metrics from these models help identify the most discriminative comorbidities, providing clinical insights beyond statistical associations. For example, neoplastic and rheumatoid conditions typically rank higher in HFpEF classification, while prior coronary interventions feature more prominently in HFrEF discrimination [100].
The integration of graph neural networks (GNNs) represents a methodological advance that directly incorporates network structure into predictive modeling. Recent research has developed novel architectures combining GNNs with Transformer models to process EHR data represented as temporal concept graphs [102]. This approach outperformed traditional models in predicting drug response, achieving best RMSE of 0.0043 across five medication classes, and identified four patient subgroups with differential characteristics and outcomes [102]. The GNN framework naturally accommodates the graph-like structure of comorbidity networks, enabling capture of higher-order disease interactions that may be missed by conventional statistical models.
Knowledge Graphs and Large Language Models
The construction of heart failure knowledge graphs represents a paradigm shift from traditional comorbidity networks toward semantically rich, integrated knowledge representations. These graphs unify comorbidities, treatments, biomarkers, and molecular entities within a formal schema, enabling complex reasoning about disease mechanisms and therapeutic strategies [103]. Recent methodological innovations employ large language models (LLMs) with prompt engineering to automate knowledge extraction from clinical texts and medical literature, significantly reducing annotation time while maintaining accuracy [103].
The TwoStepChat approach to knowledge graph construction divides the information extraction process into sequential phases: named entity recognition, relation extraction, and entity disambiguation [103]. This method has demonstrated superior performance compared to vanilla prompts and fine-tuned BERT-based baselines, particularly for out-of-distribution entities not seen during training [103]. The resulting knowledge graphs support advanced applications including clinical decision support, treatment recommendation, and mechanistic hypothesis generation by integrating comorbidity patterns with molecular-level information from databases like DisGeNET and UniProtKB [99] [100].
Experimental Protocols and Research Reagents
Detailed Methodologies for Key Experiments
Protocol 1: Construction of HF Comorbidity Networks from EHR Data
This protocol outlines the step-by-step process for building comprehensive comorbidity networks from electronic health records, based on established methodologies [100] [101]:
Cohort Identification: Extract patient cohorts using validated HF phenotyping algorithms combining structured (ICD codes) and unstructured (clinical notes) data. Inclusion criteria typically include: (1) two or more HF-relevant diagnosis codes; (2) elevated NT-proBNP (>120 ng/ml); (3) recorded NYHA functional class; (4) echocardiographic E/e' >15; or (5) documented loop diuretic use.
HF Subtyping: Categorize patients into HFpEF (LVEF ≥50%), HFmrEF (LVEF 40-49%), and HFrEF (LVEF ≤40%) based on echocardiographic or MRI measurements. Exclude patients with inheritable cardiomyopathies or heart transplant history.
Comorbidity Processing: Map all clinical diagnoses to a standardized ontology (e.g., PheCodes). Represent each comorbidity as a binary variable (present/absent) for each patient. Apply prevalence filters (typically >2% cohort frequency) to reduce noise.
Network Construction: Calculate pairwise disease associations using Fisher's exact test with Benjamini-Hochberg correction (p<0.0001 threshold). Compute ϕ-correlation coefficients for significant pairs and scale by mean correlation values per disease to generate edge weights.
Validation: Perform robustness checks through bootstrap resampling and compare network topology metrics (degree distribution, clustering coefficient, betweenness centrality) against random networks.
Protocol 2: Multi-Layer Network Integration for Gene Discovery
This protocol describes the integration of comorbidity networks with molecular data to identify novel gene candidates [100]:
Heterogeneous Network Construction: Create a multi-layer network integrating: (1) comorbidity network (disease-disease); (2) disease-gene associations from DisGeNET (confidence score >0.29); (3) protein-protein interactions from STRING database.
Network Propagation: Apply random walk with restart algorithm to prioritize genes based on network proximity to known HF genes and comorbidity patterns. Use restarts probability of 0.7 and run until convergence (L1-norm < 1e-6).
Experimental Validation: Compare prioritized genes against transcriptomic signatures from murine HFpEF models (e.g., high-fat diet + L-NAME administration). Perform pathway enrichment analysis using g:Profiler with significance threshold of FDR < 0.05.
Literature Mining: Triangulate findings through automated literature extraction using LLMs with manually curated prompts to identify supporting evidence from published studies.
Research Reagent Solutions
Table 3: Essential Research Resources for HF Comorbidity Network Studies
| Resource Category | Specific Tools/Databases | Primary Function | Key Features |
|---|---|---|---|
| Data Sources | EHR Systems (Mayo Clinic UDP, Heidelberg University Hospital RDW) | Provide longitudinal clinical data for network construction | Structured and unstructured data; Large patient cohorts; Standardized terminologies |
| Disease Ontologies | PheCodes, ICD-10, MeSH, HPO, DO | Standardize disease concepts and enable interoperability | Mapping between coding systems; Hierarchical organization; Clinical validity |
| Molecular Databases | DisGeNET, Malacards, UniProtKB, ClinVar, STRING | Annotate disease-gene and protein-protein relationships | Confidence scores; Multiple evidence types; Cross-database integration |
| Analytical Tools | igraph R package, Python IterativeImputer, GNN/Transformer architectures | Network construction, analysis, and machine learning | Network metrics; Missing data imputation; Graph-based deep learning |
| Validation Resources | Murine HFpEF models, Transcriptomic datasets, LLMs (ChatGPT) | Experimental corroboration of computational predictions | Physiological relevance; Molecular profiling; Literature mining |
Clinical and Therapeutic Implications
The mapping of heart failure comorbidity networks extends beyond academic interest to deliver concrete clinical value, particularly in drug repurposing and clinical trial design. Network-based approaches have identified novel therapeutic opportunities by revealing shared pathways between seemingly distinct conditions [1]. For example, comorbidity networks highlighting the strong association between HF and metabolic disorders have spurred investigation of antidiabetic medications (e.g., SGLT2 inhibitors) in HF populations, leading to practice-changing therapeutic advances [99]. The network proximity between disease modules has emerged as a powerful predictor of drug efficacy, with medications more likely to be effective for conditions located close to their primary indications in the disease network [1].
From a clinical management perspective, comorbidity networks enable risk stratification beyond conventional cardiovascular predictors. Studies have demonstrated that specific comorbidity clusters identified through network analysis show differential prognosis regarding unplanned hospital admissions, all-cause mortality, and treatment complications [101]. This refined risk assessment facilitates targeted interventions for high-risk multimorbidity patterns, potentially improving outcomes through personalized care pathways. Additionally, the identification of central "hub" comorbidities within networks suggests strategic intervention points where treatment might yield disproportionate benefits across multiple connected conditions [99] [100].
The integration of comorbidity networks with genetic data further enables precision medicine approaches by linking clinical presentation to underlying molecular mechanisms. Multi-layer networks have successfully prioritized novel candidate genes for HFpEF by propagating information from comorbidity patterns through protein-protein interaction networks [100]. Experimental validation in murine models has confirmed the relevance of predicted genes involved in fibrosis (COL3A1, LOX, SMAD9), hypertrophy (GATA5, MYH7), and oxidative stress (NOS1, GSST1) [100]. These findings not only advance biological understanding but also identify potential therapeutic targets for a condition with currently limited treatment options.
The paradigm of drug development is undergoing a fundamental shift, moving from a traditional single-target approach to a network-based perspective that acknowledges the profound complexity of biological systems. The diseasome concept—which visualizes diseases as nodes in a complex network interconnected through shared genetic, molecular, and pathophysiological pathways—provides a powerful framework for understanding disease etiology and therapeutic intervention [104] [105]. This approach recognizes that diseases often co-occur or share underlying network perturbations, suggesting that therapeutic strategies should target these disturbed networks rather than isolated components [104].
Network pharmacology has emerged as a key discipline leveraging this paradigm, investigating how drugs, with their inherent multi-target potential, can restore balance to diseased biological networks ("diseasomes") [104]. This is particularly relevant for complex, multifactorial diseases like neurocognitive disorders and cardiomyopathies, where single-target therapies have largely proven inadequate [104] [105]. In 2025, the translation of these principles from theoretical concepts to clinical reality is evidenced by several novel drug approvals that exemplify network-informed development strategies, from target identification through clinical validation. This review analyzes these successes and provides the methodological details needed to implement such approaches.
Network-Based Methodologies: From Concept to Clinical Candidate
Experimental Protocols for Diseasome Construction and Analysis
Protocol 1: Construction of a Disease-Centric Diseasome Network
- Objective: To map the genetic and functional interconnectivity between a focal disease and other pathological conditions to identify potential repurposing candidates and comorbidity patterns.
- Input Data: A comprehensive set of disease-gene associations from curated databases (e.g., OMIM, DisGeNET) [105] [5].
- Procedure:
- Data Curation: Compile a non-redundant set of known disease-gene associations. For a focused analysis, extract all associations containing at least one gene linked to the disease of interest (e.g., cardiomyopathy) [105].
- Bipartite Network Formation: Construct a bipartite network where the two node types are diseases and genes. An edge connects a disease to a gene if a known association exists.
- Projection to Diseasome: Project the bipartite network onto a disease-disease network (the diseasome). In this projected network, two diseases are connected if they share at least one common gene. The strength of the connection can be weighted by the number of shared genes or the functional similarity of those genes [105] [5].
- Topological Analysis: Calculate network statistics (degree, betweenness centrality, closeness centrality) to identify diseases that are central hubs or act as bridges between disease communities. Compare the observed number of disease links to random networks (e.g., via z-score) to confirm non-random connectivity [105].
- Validation: Evaluate the functional coherence of the diseasome using Pathway Homogeneity (PH) and Gene Ontology Homogeneity (GH) analyses, comparing the real network's functional clustering against randomized controls [105].
Protocol 2: Candidate Gene Prediction via Network Proximity (DIAMOnD Algorithm)
- Objective: To systematically identify novel candidate disease genes by exploiting the topology of the human protein-protein interaction (PPI) network.
- Input Data: A set of known "seed" genes for a disease and a comprehensive human interactome (e.g., from HuRI, BioPlex) [105].
- Procedure:
- Seed Definition: Define the initial set of seed genes with high-confidence associations to the disease.
- Iterative Network Expansion: The DIAMOnD algorithm iteratively explores the interactome neighborhood of the seed genes. In each step, it identifies the gene with the most significant number of connections to the current module, assessed using a hypergeometric test [105].
- Prioritization and Culling: Continue the iterative process to generate a ranked list of candidate genes. A key step is to set a biologically relevant boundary for expansion. This is achieved by quantifying the biological relevance of newly predicted genes through pathway enrichment analysis. Only candidate genes that show significant enrichment in pathways relevant to the seed genes are considered true hits [105].
- Orthologous Validation: Screen prioritized candidate genes by verifying if their orthologs in model organisms (e.g., mice) produce a phenotype relevant to the human disease, providing functional validation [105].
Protocol 3: Drug Repurposing via Network Proximity and Similarity (DTI-Prox Workflow)
- Objective: To identify novel drug-disease pairs and elucidate their mechanisms of action by analyzing their proximity within integrated biological networks.
- Input Data: Disease-specific genes and drug targets from curated databases [106].
- Procedure:
- Network Integration: Construct an integrated network by merging PPI data and other molecular interactions. Expand this network to include two layers of neighbor nodes and edges to account for indirect interactions [106].
- Proximity Analysis: Calculate the network proximity between drug targets and disease-associated genes. This can be measured using the shortest path length between the drug target and disease gene sets within the network.
- Node Similarity Assessment: Augment proximity data with node similarity metrics (e.g., Jaccard similarity) to evaluate the functional resemblance between network nodes, revealing meaningful drug-gene connections [106].
- Statistical Validation: Generate a null distribution by randomly shuffling drug and disease node labels within the network. Calculate an empirical p-value to determine if the observed proximity/similarity scores are significantly higher than expected by chance [106].
- Pathway Enrichment: Perform pathway enrichment analysis on the genes involved in significant drug-target pairs to explicate the functional relationships and shared biological processes [106].
Visualizing Network Workflows
The following diagrams, generated using Graphviz DOT language, illustrate the core logical workflows and relationships described in the experimental protocols.
Diagram 1: Core Methodologies for Network-Based Drug Discovery. (A) Workflow for building a disease-centric diseasome network to uncover disease relationships and repurposing opportunities. (B) The DTI-Prox workflow for identifying and validating novel drug-disease pairs through network proximity and functional similarity analysis [105] [106] [5].
Diagram 2: DIAMOnD Algorithm for Candidate Gene Identification. This workflow details the process of predicting novel disease-associated genes by iteratively exploring the network neighborhood of known seed genes in the human interactome, followed by rigorous biological filtering and validation [105].
2025 Success Stories: Network-Informed Approvals in Practice
The application of network-based strategies is reflected in the 2025 FDA novel drug approvals, with several agents demonstrating the principle of targeting complex disease networks rather than single molecular entities.
Table 1: Select 2025 Novel Drug Approvals Exemplifying Network-Based Development Principles
| Drug Name | Active Ingredient | Approval Date | FDA-approved Use | Network Pharmacology Rationale |
|---|---|---|---|---|
| Jascayd [107] | Nerandomilast | 10/7/2025 | Idiopathic Pulmonary Fibrosis (IPF) | Represents the success of AI-driven, network-informed target discovery; ISM001-055, an AI-designed TNIK inhibitor for IPF, showed positive Phase IIa results, validating this approach [108]. |
| Komzifti [107] | Ziftomenib | 11/13/2025 | Relapsed/Refractory NPM1-mutant AML | Targets a specific genetic driver (NPM1 mutation) within the complex network of AML pathogenesis, a paradigm enabled by understanding cancer as a network of genetic lesions. |
| Voyxact & Vanrafia [107] | Sibeprenlimab-szsi & Atrasentan | 11/25/2025 & 4/2/2025 | Proteinuria in IgA Nephropathy | Both drugs aim to reduce proteinuria by intervening at different nodes (Sibeprenlimab: targeting APRIL; Atrasentan: endothelin receptor) within the dysregulated immune and inflammatory network of the disease. |
| Lynzosyfic [107] | Linvoseltamab-gcpt | 7/2/2025 | Relapsed/Refractory Multiple Myeloma | A bispecific antibody engaging multiple nodes in the immune network (T-cells via CD3 and myeloma cells via BCMA) to redirect immune cytotoxicity against the cancer. |
| Ekterly [107] | Sebetralstat | 7/3/2025 | Acute attacks of Hereditary Angioedema | Targets the plasma kallikrein node within the intricate contact system and inflammatory bradykinin generation network. |
| Hyrnuo & Hernexeos [107] | Sevabertinib & Zongertinib | 11/19/2025 & 8/8/2025 | HER2-mutant NSCLC | Both drugs target different facets of the HER2 signaling network in lung cancer, demonstrating how understanding oncogenic network signaling leads to targeted therapies. |
The approval of drugs like Jascayd (nerandomilast) is a direct clinical validation of network and AI-driven discovery platforms. Insilico Medicine's platform, for instance, used a generative AI approach to identify a novel target (TNK) for idiopathic pulmonary fibrosis and design a candidate molecule, which demonstrated positive Phase IIa results [108]. This exemplifies the "target-to-design" pipeline, compressing the traditional discovery timeline by leveraging AI to navigate the complex disease network of IPF [108].
Furthermore, the high number of repurposed agents in the 2025 Alzheimer's disease pipeline (33%) underscores a practical application of the diseasome concept. By recognizing shared pathways between diseases, researchers can identify existing drugs with potential efficacy in new indications, a process greatly accelerated by network proximity analysis as formalized in the DTI-Prox workflow [90] [106].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Implementing network-based drug discovery requires a suite of computational and data resources. The following table details key reagents and their applications.
Table 2: Key Research Reagent Solutions for Network Pharmacology
| Reagent / Resource | Type | Primary Function in Research | Example Use Case |
|---|---|---|---|
| Human Interactome (e.g., HuRI, BioPlex) [105] | Data Resource | A comprehensive map of protein-protein interactions; serves as the foundational network for proximity and module detection algorithms. | Used as the input network for the DIAMOnD algorithm to predict new candidate disease genes [105]. |
| Disease-Gene Associations (e.g., OMIM, DisGeNET) [105] [5] | Data Resource | Curated databases linking genes to diseases; used to define seed genes and validate predictions. | Essential for constructing the initial bipartite disease-gene network during diseasome construction [105]. |
| Gene Ontology (GO) & Pathway Databases (e.g., KEGG, Reactome) [106] [5] | Data Resource | Provide functional context for gene sets; used for enrichment analysis to validate the biological relevance of predicted drug-target pairs or disease modules. | Pathway enrichment analysis in the DTI-Prox workflow to explicate functional relationships between drugs and disease genes [106]. |
| CTEP Agents List [109] | Research Tool | A repository of agents available under NCI's CTEP IND for pre-clinical and clinical research, facilitating investigator-initiated trials for repurposing. | Allows researchers to propose clinical trials for anti-cancer drug repurposing based on new network-derived hypotheses [109]. |
| AI Drug Discovery Platforms (e.g., Exscientia, Insilico Medicine) [108] | Integrated Platform | Leverage generative AI, knowledge graphs, and phenotypic screening on integrated data to design and optimize novel drug candidates de novo. | Insilico's platform identified a novel TNIK inhibitor for IPF from target discovery to clinical candidate in 18 months [108]. |
| Common Terminology Criteria for Adverse Events (CTCAE) [109] | Standardized Taxonomy | Provides a standardized lexicon for reporting adverse events in clinical trials, enabling systematic safety analysis across different network-targeting therapies. | Used in the safety reporting of CTEP-supported network trials to ensure consistent data collection [109]. |
Discussion and Future Directions
The novel drug approvals of 2025 provide compelling evidence that network-informed therapeutic development is maturing into a robust and productive paradigm. The successes span from AI-driven de novo drug design to the rational repurposing of existing agents based on shared network pathology. The methodologies underpinning these successes—such as diseasome construction, network proximity analysis, and functional module detection—are now well-defined and accessible to the research community.
Future progress will depend on several key factors. First, the continued development and integration of multi-omics data (genomic, transcriptomic, proteomic, metabolomic) into network models will create more comprehensive and cell-type-specific diseasomes, improving prediction accuracy [104] [5]. Second, the application of more sophisticated AI and graph neural networks will enhance our ability to mine these complex networks for non-obvious therapeutic relationships [108]. Finally, as the field evolves, regulatory frameworks will need to adapt to evaluate the safety and efficacy of multi-target therapies and AI-designed drugs, potentially relying on advanced biomarkers and computational evidence [110] [108].
In conclusion, the integration of diseasome concepts and network pharmacology tools is no longer a speculative endeavor but a tangible and successful strategy for addressing the complexity of human disease. The 2025 approvals mark a significant milestone, heralding a new era of rational, systematic, and effective therapeutic development.
The growing availability of multi-modal biological data presents unprecedented opportunities to map the complex pathways linking genetic variation to clinical disease manifestations. Cross-scale validation has emerged as a critical framework for integrating genomic, transcriptomic, proteomic, and phenomic data to establish causal relationships between genetic susceptibility loci and their phenotypic consequences. This technical guide examines methodologies for connecting genetic discoveries across biological scales, with emphasis on computational approaches that leverage large-scale biobank data, address phenotype misclassification in electronic health records, and generate testable biological hypotheses through network-based analyses. We provide detailed experimental protocols, visualization frameworks, and reagent solutions to equip researchers with practical tools for implementing robust cross-scale validation in diseasome and disease network research.
Cross-scale validation represents a paradigm shift in complex disease genetics, moving beyond genome-wide association studies (GWAS) to establish mechanistic connections between statistical associations and biological reality. This approach addresses the fundamental challenge in post-GWAS research: determining how genetic variants detected in association studies functionally influence disease risk through effects on molecular intermediates and ultimately clinical endpoints.
The diseasome concept provides a theoretical framework for cross-scale investigations, positing that diseases are interconnected through shared genetic architectures and biological pathways rather than existing as isolated entities [5]. Systematic characterization of pleiotropy—where individual genetic loci influence multiple disorders—reveals shared pathophysiological pathways and opportunities for therapeutic development [111]. For example, analyses of UK Biobank data have identified 339 distinct disease association profiles across 3,025 genome-wide independent loci, demonstrating the extensive pleiotropy underlying human disease [111].
Cross-scale validation strengthens causal inference in disease genomics by integrating evidence across multiple biological layers, addressing the limitations of single-scale analyses that often yield statistically robust but mechanistically obscure associations.
Methodological Framework: Connecting Genetic Variants to Clinical Phenotypes
Core Analytical Approaches for Cross-Scale Integration
Table 1: Core Methodologies for Cross-Scale Validation
| Method | Primary Function | Data Inputs | Key Outputs |
|---|---|---|---|
| Transcriptome-Wide Association Study (TWAS) | Tests association between genetically predicted gene expression and traits | GWAS summary statistics, eQTL reference panels | Genes whose predicted expression associates with disease risk [112] |
| Proteome-Wide Association Study (PWAS) | Identifies proteins whose genetically predicted levels associate with disease | GWAS summary statistics, pQTL reference panels | Putative causal proteins and their disease associations [112] [113] |
| Phenome-Wide Association Study (PheWAS) | Tests genetic variant associations across multiple phenotypes | Genetic variant data, EHR-derived phenotype data | Pleiotropy patterns, variant-phenotype associations [114] [112] |
| Mendelian Randomization | Estimates causal relationships between exposures and outcomes | Genetic variants associated with exposure, outcome GWAS data | Causal effect estimates between molecular traits and diseases [115] |
| Ontology-Aware Disease Similarity (OADS) | Quantifies disease relationships using hierarchical ontologies | Multi-modal data, biomedical ontologies (GO, HPO, Cell Ontology) | Disease similarity networks, functional communities [5] |
Addressing Electronic Health Record Phenotype Misclassification
A critical challenge in cross-scale validation involves accurately defining clinical endpoints from electronic health records (EHR). EHR-derived phenotypes are subject to misclassification, with positive predictive values typically ranging between 56% and 89% for different phenotypes [114]. This misclassification introduces bias in odds ratio estimates and reduces statistical power in genetic association analyses.
Genotype-Stratified Validation Sampling: To address this limitation, we recommend a genotype-stratified case-control sampling strategy for phenotype validation [114]. This approach involves:
- Selecting subjects for gold-standard phenotype validation (via chart review) based on both EHR-derived phenotype status (S) and genotype data (X)
- Applying expectation-maximization algorithms to derive maximum-likelihood estimates for odds ratio parameters using combined validated and error-prone EHR-derived phenotype data
- Correcting bias in association parameter estimates, particularly important for variants with low minor allele frequency
This validation strategy maintains nominal type I error rates while increasing power for detecting associations compared to sampling based only on EHR-derived phenotypes [114].
Experimental Protocols for Cross-Scale Validation
Multi-Omic Integration Protocol for Gene Discovery
The following protocol details an integrative approach for identifying susceptibility genes underlying complex traits, demonstrated through COVID-19 hospitalization research [112]:
Step 1: Transcriptome-Wide Association Study (TWAS)
- Obtain GWAS summary statistics for the trait of interest (e.g., COVID-19 hospitalization: 7,885 cases, 961,804 controls)
- Use reference expression quantitative trait loci (eQTL) panels from relevant tissues (GTEx v8: 17,382 samples across 52 tissues)
- Test predicted expression of 22,207 genes for association using FUSION or similar software
- Apply significance threshold of p < 2.3E-6 for single-tissue analysis
- Perform multi-tissue analysis to improve statistical power
Step 2: Splicing TWAS (spTWAS)
- Test 131,376 splice sites of predicted alternative-splicing expression across tissues
- Identify splice variants associated with the trait (significance threshold: p < 3.7E-07)
- Compare signals between gene expression and splicing analyses
Step 3: Proteome-Wide Association Study (PWAS)
- Utilize protein quantitative trait loci (pQTL) reference data (e.g., INTERVAL study: N=3,301; 1,031 plasma proteins)
- Test association between genetically predicted protein abundance and trait
- Apply significance threshold of p < 4.85E-5
Step 4: Functional Validation and Annotation
- Perform gene set enrichment analysis (GSEA) to identify overrepresented pathways
- Conduct phenome-wide association scans (PheWAS) to map clinical manifestations
- Implement laboratory-wide association scans (LabWAS) to identify biomarker associations
This protocol identified 27 genes related to inflammation and coagulation pathways whose genetically predicted expression was associated with COVID-19 hospitalization, highlighting putative causal genes impacting disease severity through host inflammatory response [112].
Cross-Ancestry Fine-Mapping Protocol
The following protocol enables improved fine-mapping resolution by leveraging genetic data across diverse ancestral backgrounds, as applied in preeclampsia research [113]:
Step 1: Cross-Ancestry Meta-Analysis
- Collect GWAS summary statistics from multiple ancestral groups (e.g., European, East Asian)
- Perform meta-analysis using METAL software, retaining SNPs with minor allele frequency > 0.01 and heterogeneity p-value > 0.05
- Apply genomic control to correct for residual population stratification
Step 2: Probabilistic Fine-Mapping
- Implement multi-ancestry sum of single effects model (MESuSiE) using PLINK 2.0 and R
- Consider SNPs with posterior inclusion probability (PIP) > 0.5 as significant
- Identify credible sets of putative causal variants for each risk locus
Step 3: Candidate Gene Prioritization
- Perform eQTL mapping using FUMA platform with false discovery rate threshold of 0.05
- Conduct transcriptome-wide association study (TWAS) using FUSION (FDR-corrected p < 0.05)
- Apply GCTA-mBAT-combo method for gene-based association testing (FDR-corrected p < 0.05)
- Calculate polygenic priority score (PoPS) to prioritize causal genes
This approach identified six novel susceptibility genes for preeclampsia (NPPA, SWAP70, NPR3, FGF5, REPIN1, and ACAA1) and their protective directions of effect [113].
Visualization of Cross-Scale Workflows
The following Graphviz diagrams illustrate key workflows and relationships in cross-scale validation.
Multi-Omic Data Integration Workflow
Diseasome Network Analysis Framework
EHR Phenotype Validation Strategy
Table 2: Key Research Reagent Solutions for Cross-Scale Validation
| Resource | Type | Primary Function | Application Context |
|---|---|---|---|
| UK Biobank | Data Resource | Provides genetic and routine healthcare data from 500,000 participants | Large-scale genetic association studies, pleiotropy analysis [111] |
| GTEx (v8) | Reference Data | eQTL information from 52 tissues and 2 cell lines (17,382 samples) | TWAS, gene expression imputation [112] [113] |
| FUMA | Software Platform | Functional mapping and annotation of genetic variants | eQTL mapping, gene prioritization [113] |
| PathIN | Web Tool | Pathway network visualization and analysis | Post-enrichment pathway analysis, network medicine [116] |
| Cytoscape | Software Platform | Complex network visualization and analysis | Diseasome network construction, modularity analysis [7] |
| QIAGEN IPA | Analysis Platform | Pathway analysis using expert-curated knowledge base | Biological interpretation of multi-omics data [117] |
| METAL | Software Tool | Meta-analysis of GWAS across studies | Cross-ancestry genetic analysis [113] [115] |
| MESuSiE | Statistical Method | Probabilistic fine-mapping across ancestries | Causal variant identification [113] |
Case Studies in Cross-Scale Validation
Autoimmune and Autoinflammatory Disease Diseasome
A comprehensive diseasome study of autoimmune and autoinflammatory diseases (AIIDs) demonstrates the power of cross-scale integration [5]. Researchers curated 484 autoimmune diseases and 110 autoinflammatory diseases, then integrated genetic, transcriptomic (bulk and single-cell), and phenotypic data to construct multi-layered association networks. The ontology-aware disease similarity (OADS) strategy incorporated hierarchical biomedical ontologies (Gene Ontology, Cell Ontology, Human Phenotype Ontology) to quantify disease relationships.
Network modularity analysis identified 10 robust disease communities with shared pathways and phenotypes. For example, in systemic sclerosis and psoriasis, dysregulated genes CCL2 and CCR7 were found to contribute to fibroblast activation and immune cell infiltration through IL-17 and PPAR signaling pathways, explaining shared clinical manifestations including skin involvement and arthritis [5].
COVID-19 Hospitalization Genetics
Integrative genomic analyses of COVID-19 hospitalization illustrate cross-validation from genetic variants to clinical outcomes [112]. The study integrated GWAS of COVID-19 hospitalization (7,885 cases, 961,804 controls) with mRNA expression, splicing, and protein levels (n=18,502), identifying 27 genes related to inflammation and coagulation pathways.
PheWAS and LabWAS in the Vanderbilt Biobank (n=85,460) characterized clinical symptoms and biomarkers associated with these genes. For example, genetically predicted ABO expression was associated with circulatory system phenotypes including deep vein thrombosis and pulmonary embolism, while IFNAR2 was associated with migraine and throat pain [112]. Cross-ancestry replication confirmed consistent effects across diverse populations.
Cross-scale validation provides a robust framework for bridging genetic discoveries to clinical applications in diseasome research. By integrating evidence across genomic, transcriptomic, proteomic, and phenomic levels while addressing methodological challenges such as EHR phenotype misclassification, researchers can strengthen causal inference and identify biologically meaningful disease relationships. The methodologies, protocols, and resources presented in this technical guide offer a comprehensive toolkit for implementing cross-scale approaches to elucidate the functional mechanisms linking genetic susceptibility to clinical disease manifestations.
The human diseasome is a network representation of the relationships between known disorders, based on shared genetic components and molecular pathways. This approach, central to the emerging discipline of network medicine, allows researchers to understand human diseases not as independent entities but as interconnected modules within a larger cellular network [52]. Advances in genome-scale molecular biology have elevated our knowledge of human biology's basic components, while the importance of cellular networks between these components is increasingly appreciated [52]. Built upon these technological and conceptual advances, network medicine seeks to understand human diseases from a network perspective, centered on the concept and applications of the human diseasome and the human disease network [52].
Community detection algorithms play a pivotal role in deciphering the diseasome by identifying densely connected groups of diseases that share underlying mechanistic links. These algorithms help reveal how connectivity between molecular parts translates into relationships between related disorders on a global scale [52]. For complex conditions like cardiomyopathies, which show significant co-morbidity with other diseases including brain, cancer, and metabolic disorders, community detection within molecular interaction networks represents a crucial step toward deciphering the molecular mechanisms underlying these complex conditions [105]. The molecular interaction network in the localized disease neighborhood provides a systematic framework for investigating genetic interplay between diseases and uncovering the molecular players underlying these associations [105].
Theoretical Framework: Network-Based Disease Clustering
Constructing the Diseasome Network
The foundation of disease community detection begins with constructing a comprehensive diseasome network from genetic association data. This process involves several systematic steps that transform raw genetic data into a projected disease network suitable for community detection analysis.
The initial step involves extracting a non-redundant set of disease phenotypes and their associated genes from publicly available datasets. Following data extraction, each disease is categorized by merging similar diseases using fuzzy matching techniques to reduce redundancy and create distinct disease-gene associations [105]. This bipartite network structure forms the foundation for projection—diseases become nodes, and shared genetic components form the edges between them. The resulting disease-projected network, termed a "cardiomyopathy-centric diseasome" in one case study, contained 146 diseases with 1,193 distinct links based on common genes [105].
Table: Cardiomyopathy-Centric Diseasome Network Statistics
| Network Metric | Value | Interpretation |
|---|---|---|
| Total Diseases | 146 | Diseases sharing genetic links with cardiomyopathies |
| Total Links | 1,193 | Connections based on shared genes |
| Cardiovascular System Associations | 28.7% | Largest disease category |
| Musculoskeletal Associations | 13.7% | Second largest category |
| Neoplasms Associations | 12.2% | Significant non-cardiovascular link |
| Metabolic Disorders Associations | 10.0% | Another major association category |
| Degree Distribution | Heavy-tailed | Most diseases link to few others, while key diseases have high connectivity |
Network Properties and Statistical Validation
Evaluating diseasome network properties provides insights into the global organization of human diseases and their genetic relationships. Statistical analysis of the cardiomyopathy-centric diseasome revealed that cardiovascular diseases occupied 28.7% of the total associations, followed by musculoskeletal and congenital disorders (each 13.7%), neoplasms (12.2%), and metabolic disorders (10.0%) [105]. Surprisingly, neoplasms demonstrated significant links to cardiomyopathies, dominated by the RAF1 gene (41% of associations) [105].
Network statistics including degree, betweenness, closeness centrality, degree distribution, and gene distribution provide quantitative measures of network structure and function [105]. The degree distribution follows a heavy-tailed pattern where most diseases connect to only a few others, while intended cardiovascular diseases such as Dilated Cardiomyopathy (DCM) and Hypertrophic Cardiomyopathy (HCM) exhibit high connectivity (k=96 and k=63 respectively) [105]. Comparison with random control networks through reshuffling genes of each disease in 10,000 trials demonstrated that the cardiomyopathic-centric diseasome has significantly higher disease links (z-score=6.652, p-value=1.44e-11) than random expectation [105].
Functional analysis using pathway homogeneity and gene ontology homogeneity distributions revealed that disease-associated genes cluster functionally. Diseases with higher numbers of similar functional genes tend to have fewer disease associations, suggesting functional specificity in genetic relationships [105]. This property can be exploited to predict new disease genes and identify mechanistically linked disease clusters.
Methodological Approaches and Experimental Protocols
Community Detection Algorithm Implementation
The DIseAse MOdule Detection (DIAMOnD) algorithm represents a powerful method for identifying disease modules and predicting candidate genes within the human interactome [105]. This algorithm explores the topological neighborhood of seed genes (known disease-associated genes) in the human protein-protein interaction network and identifies new genes based on significant connectivity to these seed genes.
The DIAMOnD algorithm operates through a systematic process of network expansion. Beginning with a set of seed genes known to be associated with a particular disease, the algorithm iteratively identifies new genes in the human interactome that show statistically significant connectivity to the growing disease module. The statistical significance is determined through p-value calculations that measure whether a node's connectivity to the disease module exceeds what would be expected by random chance [105]. This process continues iteratively, with the algorithm systematically expanding the disease module by adding the most significantly connected genes at each step.
To establish appropriate boundaries for network expansion, researchers must quantify the biological relevance of newly predicted genes using molecular pathway data [105]. This involves tabulating molecular pathways enriched in pathway enrichment analyses of seed genes for individual diseases, then identifying which DIAMOnD genes show enrichment with these same pathways. These genes are considered true hits for candidate genes. In cardiomyopathy research, this approach identified approximately 601, 508, and 31 DIAMOnD genes with clear biological associations for HCM, DCM, and ACM respectively [105].
Experimental Validation Workflow
Following computational prediction, candidate genes require rigorous validation through integrative systems analysis. This multi-step process combines molecular pathway analysis, model organism phenotype data, and tissue-specific transcriptomic information to screen and ascertain prominent candidates.
The validation workflow begins with pathway enrichment analysis of both seed genes and DIAMOnD-predicted candidate genes. Molecular pathways significantly enriched in both sets provide evidence of biological relevance [105]. Next, researchers map candidate genes to ortholog genes in model organism databases—for cardiomyopathy research, mouse knockout data showing abnormal heart phenotypes served as a crucial filter [105]. This step identified 53, 45, and 2 mapped candidate genes in HCM, DCM, and ACM, respectively [105].
Further validation involves analyzing tissue-specific transcriptomic data from repositories like the European Nucleotide Archive to associate cardiomyopathy-centric candidate genes with other disease phenotypes [105]. For comprehensive validation, researchers should compare results across multiple independent interactome datasets (such as HuRI and BioPlex3) to ensure robustness of findings [105].
Table: Essential Research Reagents and Computational Resources for Diseasome Analysis
| Resource Category | Specific Examples | Function in Analysis |
|---|---|---|
| Protein-Protein Interaction Networks | Human Interactome, HuRI, BioPlex3 [105] | Provides the foundational network structure for community detection algorithms |
| Disease-Gene Association Databases | OMIM, DisGeNET, ClinVar [105] | Sources for seed genes and established disease-gene relationships |
| Pathway Analysis Tools | Enrichr, DAVID, KEGG [105] | Identifies significantly enriched molecular pathways in gene sets |
| Model Organism Phenotype Databases | Mouse Genome Informatics (MGI), International Mouse Phenotyping Consortium [105] | Provides ortholog mapping and phenotypic validation of candidate genes |
| Transcriptomic Data Repositories | European Nucleotide Archive, GEO, GTEx [105] | Sources for tissue-specific gene expression validation |
| Network Analysis Software | Cytoscape, NetworkX, igraph [118] | Platforms for implementing community detection algorithms and visualizing diseasome networks |
| Statistical Computing Environments | R, Python with specialized packages | Provides computational framework for significance testing and algorithm implementation |
Technical Considerations for Accessible Network Visualizations
Creating accessible visualizations of diseasome networks is essential for effective research communication and collaboration. Color choices require particular attention—when designing charts or graphs, researchers should be mindful of colors used, contrast against backgrounds, and how color conveys meaning [119]. For adjacent data elements like bars or pie wedges, using a solid border color helps separate and add visual distinction between pieces [119].
Color contrast requirements differ based on element type. Regular text should have a contrast ratio of at least 4.5:1 against the background color, while graphical objects like bars in a bar graph or sections of a pie chart should aim for a contrast ratio of 3:1 against the background and against each other [119] [120]. Since color alone cannot convey meaning to users with color vision deficiencies, researchers should incorporate additional visual indicators such as patterns, shapes, or text labels to ensure comprehension [119]. These patterns should be kept simple and clear to avoid visual clutter [119].
Accessible design practices for network visualizations include providing keyboard navigation support, ensuring compatibility with screen readers through proper ARIA labels, offering multiple color schemes (including colorblind-friendly modes), and providing text alternatives for complex graphics [118]. For animations and interactive elements, researchers should allow users to turn off movements that could be distracting or disorienting, particularly for those with vestibular disorders [119] [118].
Applications in Disease Research and Drug Development
Community detection algorithms in diseasome networks have significant practical applications in drug development and therapeutic innovation. By revealing shared genetic architecture between distinct diseases, these approaches enable drug repurposing opportunities and identify potential side-effect profiles [105]. The cardiomyopathy-centric diseasome study revealed unexpected connections between heart conditions and neoplasms, dominated by the RAF1 gene, suggesting shared pathways that could inform cardiotoxicity screening in oncology drug development [105].
The identification of modifier genes through community detection and DIAMOnD analysis provides targets for biomarker development and explains variability in drug responses [105]. These genes influence disease expressivity and severity by changing the phenotypic outcome of variants at other loci [105]. In cardiomyopathy research, candidate genes like NOS3, MMP2, and SIRT1 emerged through integrative systems analysis of molecular pathways, heart-specific mouse knockout data, and disease tissue-specific transcriptomic data [105].
Network medicine approaches also facilitate understanding of disease comorbidities by revealing shared molecular pathways between conditions. The genetic connectivity observed between cardiomyopathies and metabolic disorders, for example, provides mechanistic insights into why these conditions frequently co-occur in patient populations [105]. Similarly, links between cardiovascular and nervous system disorders in the diseasome network suggest potential genetic pleiotropy that could inform personalized treatment approaches for patients with multiple chronic conditions.
Conclusion
The diseasome framework represents a paradigm shift in biomedical research, moving beyond single-disease models to embrace the complex interconnectedness of human pathology. Through multi-modal data integration and sophisticated network analysis, researchers can now uncover hidden disease relationships, identify novel therapeutic opportunities, and develop more targeted treatment strategies. The validation of these approaches across diverse conditions—from autoimmune diseases to Alzheimer's and heart failure—demonstrates their transformative potential. As network medicine continues to evolve, future directions will likely focus on dynamic network modeling that incorporates temporal disease progression, enhanced multi-omics integration, and the development of standardized frameworks for clinical implementation. These advances promise to accelerate personalized medicine approaches and deliver more effective therapeutic interventions for complex diseases, ultimately bridging the gap between molecular understanding and clinical application in drug development.
References
- 1. Disease networks and their contribution to ... [https://www.sciencedirect.com/science/article/pii/S1532046419301248]
- 2. The Emerging Paradigm of Network Medicine in the Study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3425394/]
- 3. Uncovering genetic associations in the human diseasome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10963079/]
- 4. Analysis of the human diseasome using phenotype ... [https://www.nature.com/articles/srep10888]
- 5. Disease association study of Autoimmune and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1575490/full]
- 6. Deep phenotyping of health–disease continuum in the ... [https://www.nature.com/articles/s41591-025-03790-9]
- 7. Cytoscape: An Open Source Platform for Complex Network ... [https://cytoscape.org/]
- 8. Gephi - The Open Graph Viz Platform [https://gephi.org/]
- 9. Network-Based Methods for Approaching Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9222217/]
- 10. Learning the natural history of human disease with ... [https://www.nature.com/articles/s41586-025-09529-3]
- 11. NIDDK 75th Anniversary 1950-2025 [https://www.niddk.nih.gov/about-niddk/75th-anniversary]
- 12. An introduction to and survey of biological network ... [https://www.sciencedirect.com/science/article/pii/S0097849324002504]
- 13. Graph theory: network topology [https://www.ebi.ac.uk/training/online/courses/network-analysis-of-protein-interaction-data-an-introduction/introduction-to-graph-theory/graph-theory-network-topology/]
- 14. Topological Analysis of Large-scale Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2213477/]
- 15. Evolving understanding of autoimmune mechanisms and ... [https://www.nature.com/articles/s41392-024-01952-8]
- 16. The Rise of Autoimmune Diseases [https://sjogrens.org/blog/2025/the-rise-of-autoimmune-diseases]
- 17. Network analysis of extraintestinal manifestations and ... [https://www.nature.com/articles/s41746-025-01504-6]
- 18. Gene Network Analysis of Small Molecules with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3577986/]
- 19. Stanford Medicine scientists tie lupus to a virus nearly all of us ... [https://med.stanford.edu/news/all-news/2025/11/lupus-epstein-barr.html]
- 20. Advanced methods and novel biomarkers in autoimmune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10326284/]
- 21. Breakthrough Autoimmune Findings at ACR 2025 [https://www.autoimmuneinstitute.org/research_updates/breakthrough-autoimmune-findings-at-acr-2025/]
- 22. Scientists explore new frontier in autoimmune disease ... [https://www.pbs.org/newshour/health/scientists-explore-new-frontier-in-autoimmune-disease-treatment-by-resetting-rogue-cells]
- 23. Innovations in immunotherapy for autoimmune diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485509/]
- 24. A network-based analysis of disease modules from ... [https://pubmed.ncbi.nlm.nih.gov/34428165/]
- 25. Mondo Disease Ontology - Monarch Initiative [http://mondo.monarchinitiative.org/]
- 26. statistical methods to adapt a general-purpose ontology for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2687947/]
- 27. Medical Subject Headings - Home Page [https://www.nlm.nih.gov/mesh/meshhome.html]
- 28. Performance metric choice and use of the ICD hierarchy [https://pubmed.ncbi.nlm.nih.gov/38432534/]
- 29. Breaking barriers in ICD classification with a robust graph ... [https://www.nature.com/articles/s41598-025-10590-1]
- 30. The Potential of Disease Progression Modeling to Advance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11739755/]
- 31. A unified data representation theory for network ... [https://www.nature.com/articles/srep13786]
- 32. A systematic method for surveying data visualizations ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6513170/]
- 33. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 34. Text color must provide high contrast with its background [https://docs.acquia.com/web-governance/text-color-must-provide-high-contrast-its-background]
- 35. Google New Color Palette [https://www.color-hex.com/color-palette/51381]
- 36. Google Logo 4 Colors #4285f4, #ea4335, #fbbc05, #34a853 [https://colorswall.com/palette/170959]
- 37. Color palette - Hex #4285f4 - Partner Marketing Hub - Google [https://partnermarketinghub.withgoogle.com/brands/google-photos/visual-identity/color-palette/]
- 38. contrast-color() - CSS - MDN Web Docs [https://developer.mozilla.org/en-US/docs/Web/CSS/Reference/Values/color_value/contrast-color]
- 39. A data driven approach reveals disease similarity on a ... [https://www.nature.com/articles/s41540-019-0117-0]
- 40. Computational Methods for Identifying Similar Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC6838934/]
- 41. Gene module-trait network analysis uncovers cell type specific ... [https://pubmed.ncbi.nlm.nih.gov/41189021/]
- 42. Disease network analysis to reveal comorbidity patterns in ... [https://www.nature.com/articles/s41598-025-12580-9]
- 43. SLE-DISEASOME: A WIDE SPECTRUM DATABASE OF ... [https://www.jrheum.org/content/52/Suppl_1/76]
- 44. Proteogenomic Approaches for Diseasome Studies [https://pubmed.ncbi.nlm.nih.gov/39436606/]
- 45. Applying artificial intelligence to rare diseases - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12007257/]
- 46. Introduction to correlation networks: Interdisciplinary ... [https://www.sciencedirect.com/science/article/pii/S0370157325001784]
- 47. The thresholding problem and variability in the EEG graph ... [https://www.nature.com/articles/s41598-022-22079-2]
- 48. The effect of network thresholding and weighting on structural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7085460/]
- 49. 16 network visualization tools that you should know! [https://medium.com/@vespinozag/16-network-visualization-tools-that-you-should-know-2c26957b707e]
- 50. 5 Network Visualization | Network Analysis [https://inarwhal.github.io/NetworkAnalysisR-book/ch5-Network-Visualization-R.html]
- 51. Disease association study of Autoimmune and ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12174166/]
- 52. Exploring the human diseasome: the human disease network [https://pubmed.ncbi.nlm.nih.gov/23063808/]
- 53. Exploring the human diseasome: The human disease ... [https://pure.korea.ac.kr/en/publications/exploring-the-human-diseasome-the-human-disease-network/]
- 54. AΙ-Driven Drug Repurposing: Applications and Challenges [https://pmc.ncbi.nlm.nih.gov/articles/PMC12641654/]
- 55. Drug-disease networks and drug repurposing [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013595]
- 56. A guideline for reporting experimental protocols in life sciences [https://pmc.ncbi.nlm.nih.gov/articles/PMC5978404/]
- 57. Comorbidity patterns and immune-metabolic differences in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12276266/]
- 58. Machine Learning in Biomarker Discovery for Precision ... [https://esmed.org/machine-learning-in-biomarker-discovery-for-precision-medicine/]
- 59. The Future of Clinical Trials: Incorporating 'Omics for ... [https://blog.crownbio.com/the-future-of-clinical-trials-incorporating-omics-for-enhanced-stratification]
- 60. Biomarker discovery pipeline: 3 Critical Steps 2025 [https://lifebit.ai/blog/biomarker-discovery-pipeline/]
- 61. Potential of biomarker-based enrichment strategies to ... [https://www.nature.com/articles/s41418-025-01545-0]
- 62. How AI Is Transforming Patient Stratification [https://www.clinicalleader.com/doc/how-ai-is-transforming-patient-stratification-0001]
- 63. AI-guided patient stratification improves outcomes and ... [https://www.nature.com/articles/s41467-025-61355-3]
- 64. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 65. The expanded human disease network combining protein– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3137500/]
- 66. Heterogeneity in Entity Matching: A Survey and ... [https://arxiv.org/html/2508.08076v1]
- 67. Ontology-based Services to help solving the heterogeneity ... [https://www.sciencedirect.com/science/article/abs/pii/S1567422305000797]
- 68. Can real-world data power faster breakthroughs in rare ... [https://www.bcplatforms.com/resources/can-real-world-data-power-faster-breakthroughs-in-rare-diseases]
- 69. HTA Evidence in Rare Diseases: Just Rare or Also Special? [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534280/]
- 70. Network analysis reveals rare disease signatures across ... [https://www.nature.com/articles/s41467-021-26674-1]
- 71. Rare-Variant Association Analysis: Study Designs and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4085641/]
- 72. FDA Advances Rare Disease Drug Development with New ... [https://www.fda.gov/news-events/press-announcements/fda-advances-rare-disease-drug-development-new-evidence-principles]
- 73. From Insight to Action: Translating Primary Research into ... [https://www.iqvia.com/blogs/2025/11/from-insight-to-action]
- 74. An Overview of the Fundamentals of Data Management ... [https://www.sciencedirect.com/science/article/pii/S0749208123000293]
- 75. Core Concepts: Self‐Controlled Designs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11729261/]
- 76. The growing role of Bayesian methods in clinical trial ... [https://www.sciencedirect.com/science/article/pii/S1357303925000799]
- 77. A comparison of four self-controlled study designs in an ... [https://www.sciencedirect.com/science/article/pii/S0264410X2400330X]
- 78. A Tutorial on Modern Bayesian Methods in Clinical Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC10117244/]
- 79. Contrast requirements for WCAG 2.2 Level AA [https://www.makethingsaccessible.com/guides/contrast-requirements-for-wcag-2-2-level-aa/]
- 80. Frontiers | A permutation testing framework to compare groups of ... [https://www.frontiersin.org/articles/10.3389/fncom.2013.00171/full]
- 81. A permutation testing framework to compare groups of brain networks - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3839047/]
- 82. Systematic permutation testing in GWAS pathway analyses: identification of genetic networks in dilated cardiomyopathy and ulcerative colitis | BMC Genomics | Full Text [https://bmcgenomics.biomedcentral.com/articles/10.1186/1471-2164-15-622]
- 83. Cross-validation (statistics) [https://en.wikipedia.org/wiki/Cross-validation_(statistics)]
- 84. Cross-Validation Approaches for Replicability in Psychology [https://pmc.ncbi.nlm.nih.gov/articles/PMC6043802/]
- 85. A computational framework for defining and validating ... [https://www.nature.com/articles/s41598-025-05838-9]
- 86. Validation framework for in vivo digital measures - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11751004/]
- 87. Elements must meet minimum color contrast ratio thresholds [https://dequeuniversity.com/rules/axe/4.8/color-contrast]
- 88. Coolors - The super fast color palettes generator! [https://coolors.co/]
- 89. Integrating Multi-Omics and Medical Imaging in Artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12650882/]
- 90. Alzheimer's disease drug development pipeline: 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131090/]
- 91. Annual Alzheimer's Clinical Trials Pipeline Report Shows ... [https://www.unlv.edu/news/release/annual-alzheimers-clinical-trials-pipeline-report-shows-increased-reason-optimism]
- 92. Alzheimer's Disease pipeline [https://www.delveinsight.com/blog/alzheimers-disease-pipeline]
- 93. Predictive network analysis identifies JMJD6 and other ... [https://www.nature.com/articles/s42003-023-04791-5]
- 94. COPD Hospitalization Risk Increased with Distinct Patterns of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4419951/]
- 95. Variation in Prevalence and Burden of Chronic Obstructive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12147828/]
- 96. Multimorbidity networks of chronic obstructive pulmonary ... [https://www.sciencedirect.com/science/article/abs/pii/S0047637420301883]
- 97. Referral compliance and subsequent hospital admissions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512944/]
- 98. Network medicine analysis of COPD multimorbidities [https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-014-0111-4]
- 99. Disease Network-Based Approaches to Study Comorbidity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11671564/]
- 100. A network medicine approach to study comorbidities in heart ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-023-02922-7]
- 101. Identifying subgroups in heart failure patients with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11020914/]
- 102. Stratifying heart failure patients with graph neural network and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11258417/]
- 103. Knowledge graph construction for heart failure using large ... [https://www.frontiersin.org/journals/computational-neuroscience/articles/10.3389/fncom.2024.1389475/full]
- 104. Network pharmacology to elucidate the role of ... [https://www.sciencedirect.com/science/article/abs/pii/S0944711325006701]
- 105. Integrative network analysis interweaves the missing links ... [https://www.nature.com/articles/s41598-022-24246-x]
- 106. Network based approach for drug target identification in ... [https://www.nature.com/articles/s41598-024-83178-w]
- 107. Novel Drug Approvals for 2025 [https://www.fda.gov/drugs/novel-drug-approvals-fda/novel-drug-approvals-2025]
- 108. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 109. CTEP Trial Development and Conduct - NCI [https://dctd.cancer.gov/research/ctep-trials/trial-development]
- 110. 2025 New Drug Approvals: Key FDA and EMA ... [https://www.tribecaknowledge.com/blog/2025-new-drug-approvals-key-fda-and-ema-approvals-and-emerging-trends?hs_amp=true]
- 111. Identifying cross-disease components of genetic risk across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6974401/]
- 112. Integrative genomic analyses identify susceptibility genes ... [https://www.nature.com/articles/s41467-021-24824-z]
- 113. Cross-ancestry genome-wide association study identifies new ... [https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-025-07534-y]
- 114. Phenotype validation in electronic health records based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5891135/]
- 115. Cross-ancestry analyses of Chinese and European ... [https://www.sciencedirect.com/science/article/pii/S2666979X25000667]
- 116. PathIN: an integrated tool for the visualization of pathway ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9798270/]
- 117. QIAGEN Ingenuity Pathway Analysis (IPA) [https://digitalinsights.qiagen.com/products-overview/discovery-insights-portfolio/analysis-and-visualization/qiagen-ipa/]
- 118. How to build accessible graph visualization tools [https://cambridge-intelligence.com/build-accessible-data-visualization-apps-with-keylines/]
- 119. Data Visualizations, Charts, and Graphs - Digital Accessibility [https://accessibility.huit.harvard.edu/data-viz-charts-graphs]
- 120. Understanding Success Criterion 1.4.11: Non-text Contrast [https://www.w3.org/WAI/WCAG21/Understanding/non-text-contrast.html]