Deconstructing Heterogeneity in Autism: A Roadmap for Biomarker Discovery and Precision Medicine
The profound heterogeneity of Autism Spectrum Disorder (ASD) presents a central challenge for biomarker discovery and the development of targeted therapies.
Deconstructing Heterogeneity in Autism: A Roadmap for Biomarker Discovery and Precision Medicine
Abstract
The profound heterogeneity of Autism Spectrum Disorder (ASD) presents a central challenge for biomarker discovery and the development of targeted therapies. This article synthesizes the latest research to provide a comprehensive framework for navigating this complexity. We first explore the foundational genetic, environmental, and neurobiological sources of heterogeneity, highlighting recent breakthroughs in identifying biologically distinct subtypes. We then detail advanced methodological approaches, from multi-omics integration to AI-driven analysis, that are essential for parsing this diversity. The discussion critically addresses persistent troubleshooting challenges, including statistical limitations and biomarker reliability, and provides actionable optimization strategies. Finally, we evaluate validation frameworks and comparative analyses that are translating research findings into clinically relevant tools, paving the way for a new era of precision medicine in autism for researchers and drug development professionals.
The Roots of Diversity: Unpacking the Genetic, Environmental, and Biological Sources of Heterogeneity
FAQs: Core Concepts and Research Frameworks
FAQ 1: What are the primary sources of heterogeneity in ASD that impact biomarker discovery? Heterogeneity in Autism Spectrum Disorder (ASD) arises from several interconnected factors that pose significant challenges for identifying universal biomarkers. Key sources include:
- Genetic Heterogeneity: Over 1,200 genes have been associated with ASD, but no single gene accounts for more than 1-2% of cases. Individuals present with diverse genetic variants, including de novo mutations, copy number variants, and single base mutations [1].
- Clinical and Developmental Heterogeneity: Individuals with ASD exhibit a wide range of symptom severity, co-occurring conditions (such as intellectual disability, ADHD, anxiety, and epilepsy), and distinct developmental trajectories [1] [2]. Recent research identifies different socioemotional and behavioural trajectories, with some individuals showing difficulties in early childhood and others developing more pronounced challenges in late childhood or adolescence [2].
- Etiological Heterogeneity: ASD results from the complex interplay of genetic susceptibilities and environmental factors. These include prenatal/perinatal influences like maternal immune activation, inflammation, and exposure to certain medications [3] [1].
FAQ 2: Are there distinct biological subtypes of ASD? Emerging evidence from multi-omics studies and genetic research suggests that biologically distinct subtypes of ASD exist. While clinical subtyping has limited predictive value, research is focusing on identifying homogeneous biological subgroups.
- Genetic Stratification: Recent large-scale genetic studies have demonstrated that the polygenic architecture of ASD can be broken down into at least two genetically correlated factors. One factor is associated with earlier diagnosis and lower social-communication abilities in early childhood, while the other is linked to later diagnosis and increased mental health challenges in adolescence [2].
- Omics-driven Stratification: High-throughput omics methods (genomics, transcriptomics, proteomics) are being used to deconstruct heterogeneity. These approaches aim to identify molecular subtypes with shared pathological pathways, such as those involving immune dysregulation, oxidative stress, and synaptic function [1].
FAQ 3: What are the most promising experimental approaches to control for heterogeneity in cohort studies? To manage heterogeneity and increase the likelihood of robust biomarker discovery, researchers should consider:
- Stratification by Biological Signature: Instead of grouping by behavioral scores alone, stratify participants based on underlying biological markers identified through omics, EEG, or eye-tracking [4].
- Developmental Trajectory Mapping: Incorporate longitudinal designs to track participants and group them based on their developmental and behavioral trajectories over time, not just cross-sectional data [2].
- Focus on Convergent Mechanisms: Investigate common pathological pathways that may be shared across different genetic backgrounds, such as inflammation, oxidative stress, mitochondrial dysfunction, and synaptic pathology [1].
- Multimodal Data Integration: Combine data from multiple sources (genetics, neuroimaging, electrophysiology, behavioral assays) to define more coherent subgroups [4].
Troubleshooting Common Experimental Challenges
Challenge 1: Inconsistent or Unreplicable Biomarker Signals
- Problem: A biomarker candidate shows promise in an initial cohort but fails to validate in a subsequent study, likely due to undetected heterogeneity within the sample.
- Solution:
- Increase Sample Characterization: Extend phenotyping beyond standard diagnostic criteria to include detailed clinical co-morbidities, family history, and cognitive profiles.
- Apply Pre-Validation Stratification: Before biomarker validation, use unsupervised learning methods (e.g., clustering on multi-omics data) to identify putative subgroups. Validate the biomarker within each subgroup separately [1].
- Utilize Emerging Biomarker Panels: Leverage recently discovered biomarker panels that have demonstrated high accuracy. For instance, one AI-driven platform has identified an mRNA biomarker panel with reported >90% sensitivity and specificity in detecting ASD and its subtypes [5].
Challenge 2: Integrating Multimodal Data from Genetic, Environmental, and Clinical Sources
- Problem: Data from various platforms (e.g., genomics, proteomics, exposome) are siloed, making it difficult to model their complex interactions in relation to ASD outcomes.
- Solution:
- Adopt a Multi-Omics Framework: Use integrative analysis pipelines that can simultaneously model information from different molecular layers (genes, transcripts, proteins) to identify key convergent pathways [1].
- Incorporate Temporal Environmental Data: For environmental factors, utilize novel platforms like temporal exposome sequencing, which can measure over 150 million biochemical data points from a single strand of hair to model how environmental exposures interact with biology over time [6].
- Apply Quantitative AI Platforms: Employ AI platforms designed to agnostically discover and model the non-linear dynamics between biology, behavior, and environmental circumstances [5].
Challenge 3: Differentiating ASD-Specific Pathways from Those Linked to General Neurodevelopmental Delays
- Problem: A identified pathological mechanism (e.g., synaptic dysfunction) may not be specific to ASD but common across multiple neurodevelopmental conditions.
- Solution:
- Include Relevant Control Groups: Ensure study designs include control groups with other neurodevelopmental disorders (e.g., ADHD, intellectual disability) to test for specificity.
- Investigate Genetic Correlations: Calculate genetic correlations between your ASD-related findings and other traits. The polygenic factor for later-diagnosed ASD shows higher genetic correlations with ADHD and mental health conditions, suggesting a shared etiology, which is less pronounced for the early-diagnosed factor [2].
- Focus on Core ASD Pathophysiology: Prioritize mechanisms directly linked to the core characteristics of ASD, such as genes enriched in pathways for "social behavior," "cognition," and "synapse organization" as identified in the SFARI gene database analysis [1].
Data Presentation: Performance of Key Diagnostic Tools
Table 1: Performance Metrics of Standardized ASD Diagnostic Instruments. This table summarizes the aggregated sensitivity and specificity of common tools as reported in a recent meta-analysis [7].
| Diagnostic Tool | Full Name | Sensitivity (95% CI) | Specificity (95% CI) | Primary Use Context |
|---|---|---|---|---|
| ADOS | Autism Diagnostic Observation Schedule | 87% (79–92%) | 75% (73–78%) | Gold-standard observational assessment |
| ADI-R | Autism Diagnostic Interview-Revised | 77% (56–90%) | 68% (52–81%) | Comprehensive parent interview |
| CARS | Childhood Autism Rating Scale | 89% (78–95%) | 79% (65–88%) | Clinician-rated observational and historical tool |
Table 2: Key Research Reagent Solutions for Investigating ASD Etiology. This table outlines essential materials and their applications in contemporary ASD research.
| Research Reagent / Tool | Function / Application | Key Utility in ASD Research |
|---|---|---|
| SFARI Gene Database | Curated database of ASD-associated genes. | Categorizing genetic risk; pathway and network analysis of ASD susceptibility genes [1]. |
| Multi-Omics Assay Panels | High-throughput measurement of molecular features (e.g., transcriptomics, proteomics). | Unbiased profiling for biomarker discovery and stratification of ASD heterogeneity [1]. |
| Temporal Exposome Sequencing | Platform for measuring environmental exposures and biological responses over time from hair samples. | Investigating the dynamic interplay between environmental factors and an individual's biology in ASD etiology [6]. |
| EEG & Eye-Tracking Paradigms | Non-invasive tools for measuring neurocognitive and visual processing. | Providing scalable, objective biomarkers for stratification and predicting intervention outcomes [4]. |
| AI-Driven Biomarker Platforms | Computational platforms for agnostic discovery of diagnostic and prognostic biomarkers. | Identifying complex, non-linear biomarker patterns from multimodal datasets to diagnose ASD and its subtypes [5]. |
Experimental Protocols for Key Methodologies
Protocol 1: Multi-Omics Integration for Biomarker Discovery and Stratification
Objective: To identify molecularly defined subtypes of ASD and discover subtype-specific biomarkers by integrating genomic, transcriptomic, and proteomic data.
Methodology:
- Sample Collection: Obtain biospecimens (e.g., blood, induced pluripotent stem cell-derived neurons) from a well-characterized ASD cohort and matched controls. Phenotypic data must include DSM-5/ICD-11 criteria, co-occurring conditions, and cognitive scores [8] [7].
- Data Generation:
- Genomics: Perform whole-genome or exome sequencing to identify single nucleotide variants (SNVs) and copy number variants (CNVs). Cross-reference findings with the SFARI gene database [1].
- Transcriptomics: Conduct RNA sequencing (RNA-seq) on relevant tissues to profile gene expression patterns.
- Proteomics and Metabolomics: Use mass spectrometry-based platforms to quantify protein and metabolite levels.
- Data Integration and Analysis:
- Pathway Convergence Analysis: Use Gene Ontology (GO) and pathway enrichment analysis on genetic and transcriptomic data to identify overrepresented biological processes (e.g., synaptic transmission, histone modification, immune response) [1].
- Unsupervised Clustering: Apply computational clustering algorithms (e.g., k-means, hierarchical clustering) to the integrated multi-omics data to identify data-driven subgroups of participants.
- Biomarker Identification: Use machine learning models (e.g., random forest, support vector machines) to identify a minimal panel of molecular features (e.g., mRNA, proteins) that can distinguish ASD subgroups from each other and from controls [1] [5].
Protocol 2: Validating Stratification Biomarkers in an Independent Cohort
Objective: To confirm that the biomarker panel identified in Protocol 1 can reliably stratify a new, independent cohort of individuals with ASD.
Methodology:
- Cohort Recruitment: Recruit a new, independent validation cohort following the same inclusion criteria and sample collection procedures as the discovery cohort.
- Targeted Assay Development: Develop a targeted, cost-effective assay (e.g., qPCR, multiplex immunoassay) to measure only the key biomarkers from the discovered panel.
- Blinded Testing: Apply the targeted assay to the validation cohort in a blinded manner.
- Outcome Correlation: Statistically test whether the predefined biomarker signatures predict the previously established subgroups and, more importantly, correlate with distinct clinical outcomes (e.g., developmental trajectory, treatment response, severity of co-occurring conditions) [4].
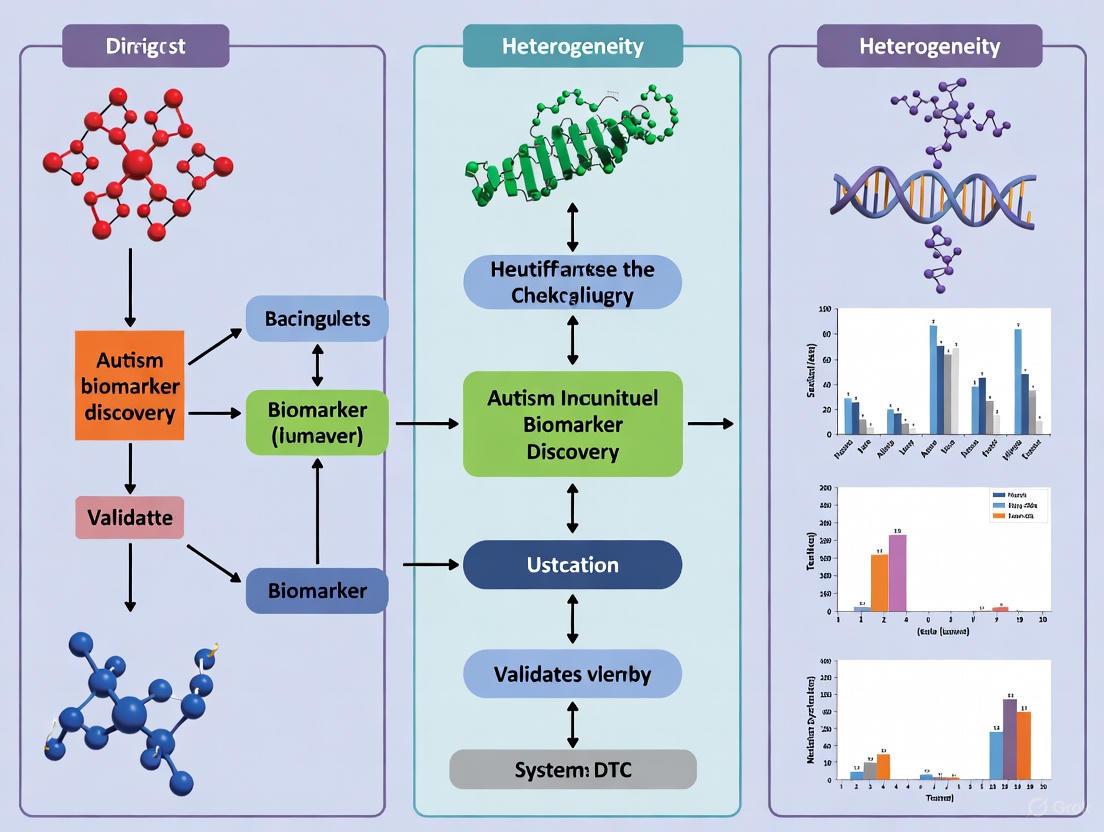
Pathway and Workflow Visualizations
Autism spectrum disorder (ASD) is not a single condition but a collection of neurodevelopmental conditions with highly heterogeneous manifestations. For researchers, this heterogeneity has been a significant obstacle, making it difficult to identify consistent biomarkers and develop targeted therapies. A groundbreaking study published in Nature Genetics in July 2025 has transformed this challenge into an opportunity by establishing a data-driven framework for decomposing autism into biologically distinct subtypes [9] [10]. This research, analyzing data from over 5,000 children in the SPARK cohort, has identified four clinically and biologically distinct subtypes of autism, each with unique genetic profiles, developmental trajectories, and co-occurring conditions [9] [11]. This article provides a technical resource for researchers and drug development professionals navigating this new paradigm, offering troubleshooting guidance, methodological protocols, and analytical frameworks for advancing precision medicine in autism.
Subtype Classification & Clinical Profiles
The research team from Princeton University and the Simons Foundation employed a "person-centered" computational approach, analyzing more than 230 traits in each individual to group participants based on their complete phenotypic profiles rather than isolated characteristics [9]. This methodology represents a significant shift from traditional trait-centered approaches and has revealed four distinct autism subtypes with clear clinical presentations.
Table 1: Clinical Profiles of Autism Subtypes
| Subtype Name | Prevalence | Core Clinical Features | Developmental Milestones | Common Co-occurring Conditions |
|---|---|---|---|---|
| Social and Behavioral Challenges | 37% | Pronounced social difficulties, repetitive behaviors, communication challenges | Typically reached on time, similar to children without autism | High rates of ADHD, anxiety, depression, OCD [9] [11] |
| Mixed ASD with Developmental Delay | 19% | Developmental delays, variable social and repetitive behaviors | Significant delays in early milestones (walking, talking) | Typically absence of anxiety, depression, or disruptive behaviors [9] [12] |
| Moderate Challenges | 34% | Milder core autism traits across all domains | Typically reached on time | Generally absence of co-occurring psychiatric conditions [9] [11] |
| Broadly Affected | 10% | Severe challenges across all domains: social, communication, repetitive behaviors | Significant developmental delays | High levels of anxiety, depression, mood dysregulation, often intellectual disability [9] [12] |
The identification of these subtypes provides researchers with a critical framework for stratifying study populations, potentially reducing variance in biomarker studies and increasing statistical power for detecting subtype-specific biological signals.
Distinct Genetic Architectures
Each autism subtype demonstrates a unique genetic signature, revealing distinct biological narratives underlying what was previously considered a single disorder. These genetic differences explain the varied clinical presentations and developmental trajectories observed across subtypes.
Table 2: Genetic Profiles of Autism Subtypes
| Subtype Name | Key Genetic Features | Primary Genetic Pathways Affected | Developmental Timing of Genetic Expression |
|---|---|---|---|
| Social and Behavioral Challenges | Strong influence of common variants linked to psychiatric traits; polygenic risk for ADHD/depression [11] [13] | Genes active in social/emotional processing; neuronal signaling [9] | Predominantly postnatal gene activity [9] [10] |
| Mixed ASD with Developmental Delay | Mix of rare inherited variants and some de novo mutations [9] [11] | Chromatin organization, transcriptional regulation [10] | Predominantly prenatal gene activity [9] |
| Moderate Challenges | Less pronounced genetic burden across variants studied | Not specified in available literature | Not specified in available literature |
| Broadly Affected | Highest burden of damaging de novo mutations; genes linked to fragile X syndrome [11] [13] | Brain development, synaptic function [9] | Primarily prenatal with broad developmental impact [9] |
Figure 1: Relationship between genetic profiles and clinical presentations in autism subtypes. DD = Developmental Delay.
Essential Research Reagents & Methodological Toolkit
To implement similar stratification approaches in your research, specific reagents, datasets, and computational tools are required. The following table outlines critical resources for replicating and extending this work.
Table 3: Essential Research Reagents & Resources
| Resource Category | Specific Resource | Application in Subtype Research | Technical Specifications |
|---|---|---|---|
| Cohort Data | SPARK dataset (Simons Foundation) [10] | Primary source of phenotypic and genotypic data | >5,000 participants; 230+ phenotypic traits; whole exome/genome sequencing |
| Computational Tools | General Finite Mixture Modeling [10] | Integration of diverse data types and subtype classification | Handles categorical, continuous, and spectrum data simultaneously |
| Genetic Analysis | Whole exome/genome sequencing | Identification of de novo and rare inherited variants | Standard sequencing protocols with family trios when possible |
| Phenotypic Assessment | Standardized autism trait questionnaires | Quantification of core and associated features | Covers social, behavioral, developmental, psychiatric domains |
| Pathway Analysis | Gene set enrichment tools | Linking genetic variants to biological processes | Standard bioinformatics pipelines (e.g., GO, KEGG analysis) |
Experimental Protocols for Subtype Validation
Protocol: Person-Centered Phenotypic Stratification
Purpose: To classify autism research participants into biologically meaningful subtypes using phenotypic data.
Workflow:
- Data Collection: Assemble comprehensive phenotypic data for each participant, including:
- Core autism traits (social communication, restricted/repetitive behaviors)
- Developmental milestones (age at walking, talking)
- Co-occurring conditions (ADHD, anxiety, mood disorders)
- Cognitive and adaptive functioning measures [9]
Data Integration: Apply general finite mixture modeling to handle diverse data types (binary, categorical, continuous) within a unified framework [10].
Subtype Assignment: Calculate probability of subtype membership for each individual based on complete phenotypic profile.
Validation: Confirm subtype stability using cross-validation techniques and replicate findings in independent cohorts [9].
Troubleshooting:
- Missing Data: Implement multiple imputation techniques for incomplete records.
- Model Convergence: Adjust model parameters and increase iterations for complex datasets.
- Cohort Effects: Validate findings across diverse populations to ensure generalizability.
Figure 2: Workflow for phenotypic stratification and biological validation in autism subtyping research.
Protocol: Genetic Validation of Subtypes
Purpose: To identify distinct genetic patterns associated with each autism subtype.
Workflow:
- Genetic Data Processing:
- Process whole exome/genome sequencing data using standard quality control pipelines
- Identify rare inherited variants, de novo mutations, and copy number variations [9]
Variant Burden Analysis:
- Calculate variant burden within each predetermined phenotypic subtype
- Compare burden across subtypes using appropriate statistical tests (e.g., regression models)
Pathway Enrichment Analysis:
- Conduct gene set enrichment analysis for each subtype separately
- Identify biological pathways specifically dysregulated in each subtype [10]
Developmental Timing Analysis:
- Utilize gene expression data across developmental periods (prenatal, postnatal)
- Determine temporal windows of maximal gene expression for subtype-specific genes [9]
Troubleshooting:
- Population Stratification: Include principal components or genetic ancestry measures as covariates.
- Multiple Testing: Apply appropriate correction methods (e.g., Bonferroni, FDR) for genetic analyses.
- Functional Validation: Plan downstream experimental validation of key pathways in model systems.
Integration of Multimodal Biomarkers
Beyond genetics, researchers are exploring multimodal biomarker approaches to refine autism subtyping. A 2025 study demonstrated that integrating neuroimaging and epigenetic data significantly improves ASD classification accuracy compared to either modality alone [14].
Key Biomarker Integration Protocol:
Neuroimaging Data: Acquire structural and functional MRI scans, focusing on thalamocortical connectivity patterns that show hyperconnectivity in ASD [14].
Epigenetic Profiling: Analyze DNA methylation patterns in candidate genes (OXTR, AVPR1A) from saliva or blood samples [14].
Machine Learning Application: Implement eXtreme Gradient Boosting (XGBoost) or similar algorithms to integrate multimodal data streams for classification [14].
Technical Consideration: When building integrated models, ensure sufficient sample size (N=105+ for medium-large effect sizes) and account for multiple comparisons across data modalities.
Frequently Asked Questions (Researcher Focused)
Q1: How can I apply this subtyping framework to my existing autism research cohort?
A: Begin by collecting comprehensive phenotypic data similar to the SPARK study domains. If genetic data is available, analyze it separately within phenotypic subgroups rather than across the entire cohort. For smaller cohorts, consider collaborative efforts to achieve sufficient sample size for robust subgroup identification [13].
Q2: What are the limitations of current autism subtyping approaches?
A: Key limitations include:
- Limited ancestral diversity in current datasets (primarily European ancestry) [13]
- Potential dynamic nature of traits across development
- Need for validation in independent cohorts
- Integration of environmental factors alongside genetic data [15]
Q3: How does this subtyping approach impact biomarker discovery?
A: Subtyping addresses heterogeneity that has plagued previous biomarker studies. By analyzing biomarkers within more homogeneous subgroups, researchers can achieve:
- Increased statistical power for detecting subtype-specific signals
- More precise correlation between biological measures and clinical presentations
- Development of targeted intervention approaches [14] [16]
Q4: What is the clinical translational potential of these findings?
A: These subtypes show promise for:
- More accurate prognostic predictions
- Tailored intervention planning based on subtype profiles
- Genetic counseling guidance for families
- Stratification for clinical trials [12]
Future Research Directions
The identification of autism subtypes opens numerous avenues for future investigation. Priority areas include:
Expanding Ancestral Diversity: Current findings require validation in ancestrally diverse populations, as genetic variants can differ across ancestral groups [13].
Longitudinal Tracking: Understanding how subtypes evolve across the lifespan will be crucial for developmental trajectory mapping.
Non-Coding Genome Exploration: Investigating the 98% of the genome beyond protein-coding regions may reveal additional regulatory mechanisms [10].
Therapeutic Development: Subtype-specific pathways offer targets for precision medicine approaches in autism treatment.
Environmental Interaction Analysis: Examining how environmental factors interact with genetic profiles within subtypes may reveal modifiable risk factors [15].
This technical resource provides a foundation for researchers to implement subtype-aware approaches in their autism research, potentially accelerating the discovery of biologically meaningful biomarkers and targeted interventions for specific autism subtypes.
FAQs: Core Concepts and Definitions
Q1: What is meant by the "genetic architecture" of autism, and why is it important for biomarker discovery?
The genetic architecture of autism refers to the complete spectrum of genetic factors that contribute to the condition, ranging from rare, high-penetrance mutations to common, small-effect genetic variants that collectively form a polygenic liability [17]. Understanding this architecture is fundamental to biomarker discovery because the vast genotypic and phenotypic heterogeneity of autism means that no single genetic marker can serve as a universal biomarker [18]. Research must account for this complexity to identify meaningful biological subgroups.
Q2: How do high-penetrance mutations differ from polygenic liability?
- High-Penetrance Mutations: These are rare genetic variants (e.g., copy number variants or protein-disrupting variants in genes like CHD8, SHANK3, or SCN2A) that have a large effect on disease risk, often on their own. They are frequently associated with syndromic forms of autism and other conditions like intellectual disability or epilepsy [17] [19].
- Polygenic Liability: This refers to the combined effect of hundreds or thousands of common genetic variants, each with a very small individual effect on autism risk. Most autism cases are influenced by this type of inherited polygenic background [17] [19]. The additive effect of these variants can push an individual over a diagnostic threshold [20].
Q3: What is a polygenic risk score (PRS), and what are its current limitations in autism research?
A Polygenic Risk Score (PRS) is a single value that summarizes an individual's genetic loading for a trait, calculated as a weighted sum of the number of risk alleles they carry [21]. Key limitations include:
- Incomplete Information: Current PRS capture only a fraction of the known heritability, as they are based on an incomplete list of genetic variants from genome-wide association studies (GWAS) [21].
- Ancestry Bias: The predictive accuracy of PRS is currently much higher for individuals of European ancestry because most GWAS data comes from this population. Scores are not directly transferable across diverse ancestral groups, risking health disparities [21].
- Limited Discriminatory Power: For complex disorders like autism, the discriminative ability of PRS at an individual level is still low and not sufficient for standalone diagnostic prediction [21].
Q4: My genetic data shows no known high-penetrance mutations. Does this rule out a genetic cause?
No. The absence of a known high-penetrance mutation does not rule out a genetic cause. Most autistic individuals do not have an identifiable rare causal mutation [20]. Their autism is likely influenced by a combination of:
- A polygenic load of common variants [17] [20].
- Rare variants not captured by current clinical testing.
- Potential interactions between genetic factors and the environment [17].
Q5: How can the heterogeneity in the genetic architecture of autism be leveraged in research?
Instead of treating autism as a single disorder, researchers can stratify or subgroup study participants based on shared biological pathways. For example, a 2025 study identified two genetically distinct factors within autism's polygenic architecture that are correlated with different developmental trajectories and ages at diagnosis [2]. This "stratification" approach can reduce noise and increase the power to discover biomarkers and elucidate pathophysiology [22].
Troubleshooting Common Experimental Challenges
Table 1: Troubleshooting Guide for Genetic and Biomarker Studies
| Challenge | Potential Root Cause | Suggested Solution |
|---|---|---|
| Low predictive accuracy of Polygenic Risk Scores (PRS) | Incomplete GWAS data; effect sizes estimated with error; ancestry mismatch between discovery and target cohorts [21]. | Use the largest available, ancestry-matched GWAS summary statistics for score construction. For non-European cohorts, prioritize methods like XP-BLUP that leverage trans-ethnic information [21]. |
| Failure to replicate a biomarker finding | High clinical heterogeneity in the replication cohort; biomarker not specific to autism but to a co-occurring condition; developmental stage differences [18] [22]. | Apply stringent, biologically informed sub-phenotyping (e.g., by age at diagnosis, cognitive profile) [2] [22]. Use multivariate analysis/machine learning with a panel of biomarkers instead of a single marker [23]. |
| Inability to distinguish causal from correlative epigenetic changes | Epigenetic markers (e.g., DNA methylation) are influenced by genetics, environment, and tissue type, making causality difficult to establish [20]. | Integrate epigenomic data with genomic data (e.g., methylation quantitative trait locus analysis). Use longitudinal designs and multi-omics approaches (proteomics, metabolomics) to triangulate evidence [20]. |
| Unexpected variability in phenotypic expression among carriers of the same rare variant | Incomplete penetrance and variable expressivity, modulated by the individual's polygenic background and environmental factors [17] [19]. | Quantify and adjust for the carrier's background PRS for autism and related neurodevelopmental conditions. Deeply phenotype to identify sub-threshold traits. |
Detailed Experimental Protocols
Protocol 1: Differentiating Autism Subgroups by Polygenic Factors and Developmental Trajectories
This protocol is based on a 2025 study that dissected the heterogeneity of autism by linking polygenic architecture to behavioral trajectories [2].
1. Objective: To identify distinct genetic profiles associated with different developmental pathways and ages at autism diagnosis.
2. Materials and Reagents:
- Cohort Data: Longitudinal birth cohort data with repeated measures of socioemotional/behavioral development (e.g., Strengths and Difficulties Questionnaire, SDQ) and recorded age at autism diagnosis [2].
- Genotyping Data: Genome-wide genotyping data for autistic individuals within the cohorts.
3. Methodology:
- Step 1: Identify Behavioral Trajectories. Use Growth Mixture Modeling (GMM) on longitudinal SDQ scores to identify latent subgroups (e.g., "early childhood emergent" vs. "late childhood emergent" trajectories) among autistic individuals [2].
- Step 2: Test Association with Diagnosis Age. Validate the identified trajectories by testing their association with the recorded age at autism diagnosis using chi-square tests or regression [2].
- Step 3: Calculate Polygenic Risk Scores. Using large-scale autism GWAS summary statistics, compute PRS for all individuals.
- Step 4: Deconstruct Polygenic Architecture. Apply genetic factor analysis to the GWAS data to determine if the autism polygenic architecture can be broken down into independent factors. Test the genetic correlation (
rg) between these factors [2]. - Step 5: Correlate Genetic Factors with Trajectories. Test the association between the identified polygenic factors and the behavioral trajectories. The 2025 study found one factor linked to earlier diagnosis and another to later diagnosis and adolescent socioemotional difficulties [2].
- Step 6: Estimate Genetic Correlations with Co-occurring Conditions. Calculate the genetic correlations (
rg) between the identified autism polygenic factors and other traits like ADHD and mental health conditions using LD Score regression [2].
Protocol 2: Integrating Neuroimaging and Epigenetic Data for Classification
This protocol details a multimodal approach to improve the classification of autism, as demonstrated in a 2025 study [23].
1. Objective: To build a machine learning model that integrates brain imaging and epigenetic data with behavioral measures to classify autism.
2. Materials and Reagents:
- Participants: Autistic and typically developing control individuals.
- Behavioral Measure: The Adolescent-Adult Sensory Profile (AASP) questionnaire [23].
- MRI Scanner: 3T MRI scanner for structural and resting-state functional MRI (rs-fMRI) [23].
- Biological Samples: Saliva or blood for DNA extraction and epigenetic analysis.
- Software: FreeSurfer for structural MRI analysis; CONN toolbox or SPM for rs-fMRI preprocessing and seed-to-voxel analysis; a machine learning library (e.g., in R or Python) with the XGBoost algorithm [23].
3. Methodology:
- Step 1: Acquire Behavioral Baseline. Administer the AASP to all participants to establish a baseline of sensory-related behaviors [23].
- Step 2: Acquire and Preprocess Brain Imaging Data.
- Acquire high-resolution T1-weighted structural images and T2-weighted rs-fMRI scans.
- Process structural data with FreeSurfer's
recon-allpipeline to obtain cortical and subcortical volumes. - Preprocess rs-fMRI data (realignment, slice-timing correction, normalization, smoothing). Perform seed-to-voxel analysis with the bilateral thalamus as the seed to compute thalamo-cortical resting-state functional connectivity (rs-FC) [23].
- Step 3: Acquire and Process Epigenetic Data.
- Extract DNA from saliva.
- Perform bisulfite conversion and DNA methylation analysis for candidate genes (e.g.,
AVPR1A,OXTR) via pyrosequencing or array-based methods. Calculate methylation values at specific CpG sites [23].
- Step 4: Model Development and Comparison.
- Build three classification models using the XGBoost algorithm:
- Neuroimaging-Epigenetic Model: Input features include AASP scores, thalamo-cortical rs-FC, brain volumes, and DNA methylation values.
- Neuroimaging Model: Input features include AASP scores and brain data.
- Epigenetic Model: Input features include AASP scores and DNA methylation data [23].
- Compare the predictive accuracy of the three models to determine if the integrated model outperforms the others.
- Build three classification models using the XGBoost algorithm:
Signaling Pathways and Experimental Workflows
Diagram 1: Genetic Architecture and Biomarker Discovery Logic
Diagram 2: Multi-Omics Integration Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
| Item | Function/Application in Research | Example/Notes |
|---|---|---|
| GWAS Summary Statistics | Used as a reference to calculate Polygenic Risk Scores (PRS) in a study cohort. | Sourced from large consortia like the Autism Sequencing Consortium (ASC) or the Psychiatric Genomics Consortium (PGC). Must be ancestry-matched [21]. |
| Genotyping Array | Provides genome-wide data on common single nucleotide polymorphisms (SNPs) from participant DNA. | Arrays like Illumina Global Screening or Infinium PsychArray. Essential for PRS calculation and imputation [2]. |
| Whole Exome/Genome Sequencing | Identifies rare, high-penetrance coding and non-coding variants. | Used to find novel or known pathogenic mutations not covered by genotyping arrays [17] [19]. |
| Bisulfite Conversion Kit | Treats DNA to differentiate methylated from unmethylated cytosine residues for epigenetic studies. | Critical for DNA methylation analysis (methylomics) of candidate genes (e.g., AVPR1A, OXTR) or epigenome-wide studies [23] [20]. |
| Longitudinal Behavioral Measures | Tracks developmental trajectories to link with genetic data. | The Strengths and Difficulties Questionnaire (SDQ) was used to identify latent classes linked to age of diagnosis [2]. The Adolescent-Adult Sensory Profile (AASP) provides a behavioral baseline for multimodal studies [23]. |
| 3T MRI Scanner with rs-fMRI Protocol | Acquires structural and functional brain imaging data to identify neural correlates of genetic risk. | Used to measure thalamo-cortical functional connectivity, a potential intermediate phenotype [23]. |
Autism Spectrum Disorder (ASD) is characterized by vast etiological and phenotypic heterogeneity, which presents a significant challenge for identifying reliable biomarkers [18]. The integration of environmental risk factors into research models is crucial for dissecting this heterogeneity. Key mechanisms include Maternal Immune Activation (MIA), direct exposure to environmental toxicants, and subsequent immune dysregulation [24]. These factors can converge on shared biological pathways, such as chronic neuroinflammation and oxidative stress, which may represent measurable biomarker signatures for specific ASD subgroups [24] [25]. This guide provides technical support for researchers aiming to incorporate these elements into their biomarker discovery pipelines.
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary environmental mechanisms I should focus on for ASD biomarker discovery? The most evidence-supported mechanisms involve prenatal and early-life exposures that disrupt immune and metabolic pathways. Maternal Immune Activation (MIA) is a primary model, where maternal inflammation leads to elevated pro-inflammatory cytokines (e.g., IL-6, IL-17A, TNF-α) in the fetal environment, altering brain development [24]. Concurrently, exposure to environmental toxicants (e.g., air pollutants, heavy metals, persistent organic pollutants) can induce oxidative stress, mitochondrial dysfunction, and exacerbate neuroinflammation [24] [26]. The interaction between these insults and genetic susceptibility is a critical area for stratified biomarker identification.
FAQ 2: How does immune dysregulation manifest in study participants with ASD, and what should I measure? Immune dysregulation in ASD can be systemic and central. In blood samples, studies consistently show upregulation of pro-inflammatory genes (e.g., IL-1β, IFN-γ) and elevated plasma levels of cytokines such as TNF-α, particularly in younger children [27] [25]. Metabolomic analyses often reveal concomitant changes, including alterations in amino acid metabolism (e.g., increased phenylalanine) and lipid metabolism [25]. A multi-omics approach that correlates transcriptomic, metabolomic, and epigenetic data is recommended to capture this complexity.
FAQ 3: My study population is highly heterogeneous. How can I account for this in my experimental design? Heterogeneity is a core feature of ASD. To address this, employ stratification strategies based on potential biological subtypes rather than relying solely on behavioral diagnoses [28]. For instance, you can subgroup participants based on their:
- Immune profile: e.g., high vs. normal TNF-α or IL-6 levels [27].
- Metabolic profile: e.g., specific shifts in amino acid or lipid metabolism [25].
- Sensory phenotypes: which may correlate with thalamo-cortical connectivity and epigenetic markers like AVPR1A methylation [23]. Using machine learning algorithms on multimodal data can help identify these data-driven subgroups [23].
FAQ 4: What are the key signaling pathways involved, and which are the most promising therapeutic targets? Key pathways involve neuroimmune interactions and their impact on synaptic function. Prominent pathways include:
- Cytokine Signaling (IL-6, IL-17A, TNF-α): These cytokines can cross the placenta and activate fetal microglia, leading to chronic neuroinflammation and aberrant synaptic pruning [24].
- AVPR1A and OXTR Epigenetic Regulation: DNA methylation of genes encoding vasopressin and oxytocin receptors is linked to sensory and social behavioral phenotypes [23].
- P2X7 Receptor Signaling: This pathway mediates MIA effects through mitochondrial dysfunction and oxidative stress [24]. Therapeutic targets emerging from these pathways include cytokine blockers, immunomodulatory interventions, and metabolic supplements [24] [25].
Troubleshooting Guides
Issue 1: Inconsistent or Weak Signal in Immune Biomarker Assays
Potential Causes and Solutions:
- Cause: Participant Age Variability. Immune profiles, especially cytokine levels, can change dramatically with development. For example, TNF-α is significantly higher in children with ASD under 5 years old compared to older children and controls [27].
- Solution: Implement strict age-based stratification in your analysis. Treat age as a continuous covariate in statistical models.
- Cause: Sample Timing and Handling. Cytokine levels are sensitive to circadian rhythms, recent infections, and sample processing delays.
- Solution: Standardize sample collection time of day. Screen for recent illnesses. Use standardized protocols for serum/plasma separation and freeze samples at -80°C promptly.
- Cause: Low Specificity of a Single Biomarker. No single immune marker is universal for ASD [18].
- Solution: Move towards a panel-based approach. Combine multiple cytokines (e.g., IL-6, TNF-α) with metabolic markers (e.g., phenylalanine) or epigenetic marks to improve sensitivity and specificity [25].
Issue 2: Modeling the Effects of Environmental Toxicants in Experimental Systems
Potential Causes and Solutions:
- Cause: Unrealistic Dosage. Using a single, high-dose exposure does not mimic the chronic, low-level human exposure scenario.
- Solution: Employ low-dose, chronic exposure paradigms in animal or in vitro models. Refer to epidemiological data to inform environmentally relevant concentrations [26].
- Cause: Ignoring Co-Exposures. Humans are exposed to mixtures of toxicants, which can have synergistic effects.
- Solution: Where feasible, design experiments that test combinations of prevalent toxicants (e.g., air pollution PM2.5 and heavy metals) to better model real-world conditions [24].
- Cause: Lack of Mechanistic Link to Neurodevelopment.
Quantitative Data Tables
Table 1: Key Immune and Metabolic Biomarkers Reported in ASD Research
| Biomarker Category | Specific Marker | Direction of Change in ASD | Associated Phenotype / Note | Key Reference |
|---|---|---|---|---|
| Cytokines | TNF-α | Significantly Elevated | Particularly in children <5 years; not correlated with symptom severity | [27] |
| IL-6 | Trend of Elevation | More pronounced in males; key mediator in MIA models | [27] [24] | |
| IL-1β, IFN-γ | Upregulated (Gene Expression) | Part of activated immune response signature in blood | [25] | |
| Metabolites | Phenylalanine | Increased | Suggests alterations in amino acid metabolism | [25] |
| Citrulline | Increased | Implicated in immune and metabolic dysregulation | [25] | |
| Epigenetic Marks | AVPR1A DNA Methylation | Hypomethylation | Associated with sensory phenotypes and thalamo-cortical connectivity | [23] |
| Brain Connectivity | Thalamo-Cortical rs-FC | Hyperconnectivity | Correlated with sensory abnormalities; a potential neuroimaging biomarker | [23] |
Table 2: Common Environmental Toxicants and Their Documented Immunotoxic Effects
| Toxicant Class | Examples | Key Immunotoxic Effects Relevant to ASD | Evidence Level |
|---|---|---|---|
| Persistent Organic Pollutants | TCDD (Dioxin), PCBs | Reduced lymphocyte response to mitogens; impaired host response to viral infection (influenza); decreased vaccine antibody potency in children | [29] [26] |
| Heavy Metals | Lead (Pb), Cadmium (Cd) | Decreased NK cell number/function; increased inflammatory indicators; reduced vaccine antibody response | [26] |
| Air Pollutants | PM2.5 | Associated with increased pro-inflammatory cytokines (IL-8, TNF-α); may modulate innate immunity and increase infection susceptibility | [26] |
| Polycyclic Aromatic Hydrocarbons (PAHs) | Benzo[a]pyrene | Agonists for the AhR receptor; linked to altered immune function in children exposed during development | [29] |
Experimental Protocols & Workflows
Protocol 1: Multi-Omic Profiling for Immune-Metabolic Subtyping
This protocol is adapted from recent studies that integrate transcriptomic and metabolomic data to characterize biological subtypes in ASD [25].
1. Sample Collection:
- Collect peripheral blood from fasting participants. For the transcriptomic cohort, draw blood into PAXgene Blood RNA tubes. For the metabolomic cohort, collect blood in EDTA tubes for plasma separation.
2. Transcriptomic Processing (RNA Sequencing):
- RNA Extraction & QC: Isolate total RNA using a standardized kit. Assess RNA integrity (RIN > 8.0 recommended).
- Library Prep & Sequencing: Perform ribosomal RNA depletion, followed by library preparation and sequencing on an Illumina platform to a depth of at least 30 million paired-end reads.
- Bioinformatic Analysis:
- Alignment & Quantification: Align reads to a reference genome (e.g., GRCh38) using STAR and quantify gene-level counts with featureCounts.
- Differential Expression: Identify Differentially Expressed Genes (DEGs) using DESeq2 (FDR-adjusted p-value < 0.05).
- Weighted Gene Co-expression Network Analysis (WGCNA): Construct co-expression modules to identify groups of genes with highly correlated expression patterns across samples. Relate key modules to clinical traits.
3. Metabolomic Processing (Mass Spectrometry):
- Metabolite Extraction: Precipitate proteins from plasma with cold methanol, then centrifuge and collect the supernatant.
- LC-MS Analysis: Analyze extracts using a high-resolution LC-MS system (e.g., UHPLC-QTOF-MS) in both positive and negative ionization modes.
- Data Analysis: Use software like XCMS for peak picking, alignment, and annotation. Perform statistical analysis in MetaboAnalyst to identify Differentially expressed Metabolites (DMs).
4. Data Integration:
- Perform pathway enrichment analysis (KEGG, GO) on both DEG and DM lists to identify convergent biological pathways (e.g., "antigen processing and presentation," "linoleic acid metabolism").
- Use multi-omics factor analysis (MOFA) or similar tools to integrate the two datasets and identify latent factors that drive variation across both molecular layers.
Protocol 2: Assessing Maternal Immune Activation (MIA) in Animal Models
This protocol outlines key steps for establishing and validating a poly(I:C)-induced MIA model, a widely used paradigm to study neurodevelopmental effects [24].
1. Animal Model Setup:
- Use timed-pregnant rodents (e.g., C57BL/6 mice).
- Administer a single dose of poly(I:C) (e.g., 20 mg/kg, i.p.) to the dam at a critical gestational time point (e.g., E12.5) to mimic viral infection. Control dams receive saline.
2. Measuring Maternal Immune Response:
- Collect maternal blood and/or placental tissue 3-6 hours post-injection.
- Assay: Measure key pro-inflammatory cytokines (IL-6, IL-17A, TNF-α) using ELISA or a multiplex bead-based assay.
3. Evaluating Offspring Phenotypes:
- Behavior: Test adult offspring for ASD-relevant behaviors (e.g., social interaction in the three-chamber test, repetitive behaviors like marble burying, anxiety in the elevated plus maze).
- Molecular: In postnatal offspring, analyze brain tissue for:
- Microglial Activation: IBA1 immunohistochemistry and morphological analysis.
- Cytokine Levels: Measure in brain homogenates (e.g., prefrontal cortex, amygdala).
- Synaptic Markers: Assess protein levels of pre- and post-synaptic markers (e.g., PSD-95, VGLUT1) via Western blot.
- Neurophysiology: Use ex vivo slice electrophysiology to examine excitatory/inhibitory balance in relevant circuits.
Signaling Pathways and Workflow Diagrams
MIA and Environmental Toxicant Convergence Pathway
Diagram Title: Converging Pathways of MIA and Toxicants on Neurodevelopment
Multi-Omic Biomarker Discovery Workflow
Diagram Title: Multi-Omic Workflow for ASD Biomarker Discovery
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Assays for Investigating Immune Dysregulation
| Item / Reagent | Function / Application | Example / Note |
|---|---|---|
| Multiplex Cytokine Assay Kits | Simultaneously quantify multiple cytokines (e.g., IL-6, TNF-α, IL-17A) from serum/plasma or tissue homogenates. | Luminex xMAP technology or MSD electrochemiluminescence assays. Ideal for low-volume samples. |
| ELISA Kits | Quantify a single, specific protein target with high sensitivity. | Used for validating specific findings from multiplex panels (e.g., specific IL-6 or TNF-α ELISA). |
| PAXgene Blood RNA Tubes | Stabilize intracellular RNA at the point of collection, ensuring an accurate transcriptomic profile. | Critical for RNA-seq studies from whole blood. |
| DNA Methylation Kits | Extract and bisulfite-convert DNA for epigenetic analysis. | Enables analysis of candidate genes (e.g., OXTR, AVPR1A) or genome-wide profiling (EPIC array). |
| LC-MS Grade Solvents | High-purity solvents for metabolomic sample preparation and liquid chromatography-mass spectrometry. | Essential for minimizing background noise and ensuring reproducible metabolite identification. |
| Poly(I:C) | A synthetic double-stranded RNA used to simulate viral infection and induce MIA in animal models. | Available in various molecular weights; high-molecular-weight is typically used for robust immune activation. |
| Antibodies for IHC/IF | Visualize and quantify specific cell types and proteins in brain tissue (e.g., IBA1 for microglia, PSD-95 for synapses). | Validate neuroinflammatory and neurodevelopmental findings from molecular data. |
Frequently Asked Questions (FAQs)
Q1: How can researchers account for heterogeneity in autism when studying epigenetic biomarkers?
The heterogeneity of Autism Spectrum Disorder (ASD) means that a single biomarker is unlikely to apply to all individuals. Recent research has identified four clinically and biologically distinct subtypes of autism, each with different genetic profiles and developmental trajectories [9]. When designing experiments, it is crucial to stratify participants into these or similar subgroups to ensure meaningful results. The subtypes are:
- Social and Behavioral Challenges (37% of participants): Core autism traits with typical developmental milestones but frequent co-occurring conditions like ADHD and anxiety [9].
- Mixed ASD with Developmental Delay (19% of participants): Later achievement of developmental milestones (e.g., walking, talking), without signs of anxiety or depression [9].
- Moderate Challenges (34% of participants): Milder core autism behaviors, typical developmental milestones, and generally no co-occurring psychiatric conditions [9].
- Broadly Affected (10% of participants): The most severe and wide-ranging challenges, including developmental delays, social difficulties, and co-occurring psychiatric conditions [9].
These subgroups are associated with distinct genetic patterns. For example, the "Broadly Affected" subgroup showed the highest proportion of damaging de novo mutations, while only the "Mixed ASD with Developmental Delay" group was more likely to carry rare inherited genetic variants [9]. Using a stratified, "person-centered" approach that considers over 230 traits, rather than searching for genetic links to single traits, is essential for revealing meaningful biological mechanisms [9].
Q2: What is the relationship between epigenetic age (DNAmAge) and brain age in the context of neurological health?
DNAmPhenoAge, one measure of epigenetic age derived from whole blood, has been identified as a significant mediator between chronological age and global brain age, which is estimated from structural MRI [30]. This means that the effect of a person's chronological age on their brain structure is partially explained by their epigenetic age.
Advanced DNAmPhenoAge is specifically related to accelerated aging in brain regions higher on the sensorimotor-to-association (S-A) axis [30]. This axis describes cortical organization, where higher-order association cortices (involved in complex cognitive functions) are the last to develop, exhibit prolonged plasticity, and are the first to show age-related atrophy [30]. This relationship persists even after controlling for cardiovascular health, holistic health factors, and socioeconomic status [30].
Q3: Can early-life stress or trauma lead to measurable epigenetic changes that affect brain structure?
Yes, childhood trauma can leave lasting biological marks, often referred to as epigenetic "scars." A multi-epigenome-wide analysis identified four DNA methylation sites consistently associated with child maltreatment: ATE1, SERPINB9P1, CHST11, and FOXP1 [31].
Of particular significance is FOXP1, a gene that acts as a "master switch" for genes involved in brain development. Hypermethylation of FOXP1 was linked to changes in gray matter volume in key brain regions [31]:
- Orbitofrontal cortex: Involved in emotional regulation.
- Cingulate gyrus: Involved in memory retrieval and emotional processing.
- Occipital fusiform gyrus: Involved in social cognition.
This provides a direct biological link between early adverse experiences, epigenetic alterations, and subsequent changes in brain development.
Q4: What are some key epigenetic mechanisms regulating brain development and plasticity?
The primary epigenetic mechanisms that choreograph brain development and enable lifelong plasticity are [32]:
- DNA Methylation: The covalent addition of a methyl group to cytosine bases, typically at CpG dinucleotides. It is catalyzed by DNA methyltransferases (DNMTs) and can be actively removed by Ten-eleven translocation (TET) enzymes. In the brain, neuronal activity can promote rapid changes in DNA methylation at genes regulating plasticity [32].
- Chromatin Modifications: This involves post-translational modifications to the histone proteins around which DNA is wrapped. These include acetylation, methylation, phosphorylation, and ubiquitination. These modifications, such as histone acetylation or H3K4me3, can create more open ("active") or compact ("repressive") chromatin states, thereby fine-tuning gene expression [32].
- Non-Coding RNAs: RNA molecules that do not code for proteins but can regulate gene expression by influencing transcription, splicing, and mRNA degradation [32].
Troubleshooting Guides
Issue 1: High Background or Non-Specific Signal in Immunofluorescence
| Possible Cause | Recommended Solution | Additional Notes |
|---|---|---|
| Inadequate blocking | Perform a blocking step with a 2-5% solution of Bovine Serum Albumin (BSA) or a 5-10% solution of serum from the species in which the secondary antibody was raised [33]. | Using the Image-iT FX Signal Enhancer as a pre-blocking step can further reduce non-specific labeling [33]. |
| Secondary antibody cross-reactivity | Ensure the species of the secondary antibody is not the same as the species of the sample tissue [33]. | Titrate the antibody to the lowest concentration that provides adequate signal [33]. |
| Low abundance target | Use a signal amplification method, such as Tyramide Signal Amplification (TSA) [33]. | For fluorophores that bleach quickly, use antifade mounting reagents like SlowFade Diamond or ProLong Diamond [33]. |
Issue 2: Loss of Lipophilic Tracer or Dye Signal During Permeabilization
| Possible Cause | Recommended Solution | Additional Notes |
|---|---|---|
| Use of detergent or alcohol-based permeabilization | Use a dye that covalently attaches to proteins in the membrane, such as CellTracker CM-DiI [33]. | Standard lipophilic dyes (e.g., DiI) reside in lipids, which are stripped away by detergents like Triton X-100 or methanol fixation [33]. |
| Use of non-fixable dextran | Ensure the dextran used is the fixable form (contains a primary amine) [33]. | The concentration of the tracer can be increased up to 10 mg/mL for a stronger signal [33]. |
Issue 3: Challenges in Transducing Neuronal Cells
- Problem: Neurons are more difficult to transduce than many other cell types.
- Solutions:
- Increase viral titer: Use a higher number of viral particles per cell [33].
- Optimize timing: For primary neurons, transduce them at the time of plating rather than on established cultures [33].
- Adjust expectations: The onset of expression is often slower in neurons, with peak expression typically occurring 2-3 days post-transduction rather than 16 hours [33].
Experimental Protocols & Data Presentation
Table 1: Key DNA Methylation Age (DNAmAge) Clocks and Their Relation to Brain Structure
Table summarizing epigenetic age estimation methods from whole blood and their association with neuroimaging-derived brain age metrics, as used in recent studies [30].
| DNAmAge Clock | Description | Key Finding in Neuroimaging Study |
|---|---|---|
| PhenoAge | Trained on clinical chemistry markers to capture physiological dysregulation. | Mediates the relationship between chronological age and global BrainAge; associated with advanced BrainAge in higher-order association cortices [30]. |
| Hannum | Based on 71 CpG sites in whole blood, highly correlated with chronological age. | Specific findings not highlighted as primary mediator in the cited path analysis [30]. |
| Horvath | Multi-tissue clock, trained on 353 CpG sites across multiple tissues. | Specific findings not highlighted as primary mediator in the cited path analysis [30]. |
| SkinBlood | Optimized for use in blood and skin samples. | Specific findings not highlighted as primary mediator in the cited path analysis [30]. |
Table 2: Research Reagent Solutions for Key Methodologies
Essential materials and their functions for investigating neurobiological and epigenetic correlates.
| Reagent / Material | Primary Function | Application Notes |
|---|---|---|
| Illumina Infinium MethylationEPIC BeadChip | Genome-wide DNA methylation profiling from biological samples (e.g., whole blood, saliva) [30] [23]. | Used for estimating DNAmAge and for epigenome-wide association studies (EWAS) in neurological and psychiatric research [30] [23]. |
| Covalently-bound Lipophilic Tracers (e.g., CellTracker CM-DiI) | Neuronal tracing and membrane labeling that is retained after fixation and permeabilization [33]. | Crucial for experiments requiring intracellular antibody labeling, which involves detergents that strip standard lipophilic dyes [33]. |
| Tyramide Signal Amplification (TSA) Kits | Enzyme-mediated signal amplification for detecting low-abundance targets in immunoassays [33]. | Increases detection sensitivity by depositing multiple fluorophore-labeled tyramide radicals at the site of antibody binding [33]. |
| Antifade Mounting Reagents (e.g., SlowFade Diamond) | Preserves fluorescence and reduces photobleaching in fixed cell and tissue preparations [33]. | Essential for imaging fluorophores that are prone to rapid bleaching, allowing for longer imaging sessions and better signal-to-noise ratio [33]. |
| NeuroTrace Nissl Stains | Fluorescently labels Nissl substance (ribosomal RNA) in neuronal cell bodies [33]. | While not entirely neuron-specific, it selectively stains neurons based on high protein synthesis; concentration may need optimization (20- to 300-fold dilution) to reduce glial staining [33]. |
Protocol 1: Path Analysis for Mediating Effects of Epigenetic Age on Brain Age
Objective: To formally test whether epigenetic age (DNAmAge) mediates the relationship between chronological age and global brain age (BrainAge), while controlling for confounders.
Methodology [30]:
- Data Collection:
- BrainAge: Estimate global BrainAge from T1-weighted structural MRI using a validated pipeline (e.g., volBrain) [30].
- DNAmAge: Calculate multiple epigenetic age estimates (e.g., PhenoAge, Hannum, Horvath) from whole blood DNA using the Illumina MethylationEPIC array and the online DNA Methylation Age Calculator [30].
- Covariates: Collect data on self-reported sex, race, cardiovascular health (BMI, HbA1c, pulse pressure), holistic health (PROMIS-57 subscores), and socioeconomic status (education level, household income) [30].
- Statistical Analysis:
- Use a mediation analysis framework with a statistical package like Pingouin in Python.
- Model Specification:
- Independent Variable (X): Chronological Age.
- Mediator (M): DNAmAge (test each clock separately).
- Dependent Variable (Y): Global BrainAge.
- Include all covariates as nuisance variables.
- Assess the significance of the indirect effect (Path a*b) using bias-corrected bootstrapped confidence intervals (e.g., 10,000 iterations) [30].
- The indirect effect is significant if the confidence interval does not cross zero.
Protocol 2: Integrating Sensory Behavior, Neuroimaging, and Epigenetics in ASD
Objective: To classify ASD by integrating sensory behavioral profiles, thalamo-cortical connectivity, and epigenetic markers, thereby addressing heterogeneity.
Methodology [23]:
- Participant Characterization:
- Recruit individuals with ASD and typically developing (TD) controls.
- Assess sensory-related behavior using the Adolescent-Adult Sensory Profile (AASP) questionnaire, which characterizes four patterns: Low Registration, Sensitivity, Sensation Seeking, and Avoidance [23].
- Multimodal Data Acquisition:
- Brain Factors: Acquire structural and resting-state functional MRI (rs-fMRI). Preprocess data using standard pipelines (e.g., FreeSurfer for structure, SPM/CONN for function). Calculate thalamo-cortical resting-state functional connectivity (rs-FC) using the bilateral thalamus as a seed [23].
- Epigenetic Factors: Collect saliva samples. Extract DNA and perform methylation analysis for candidate genes implicated in social behavior and sensory processing (e.g., OXTR, AVPR1A, AVPR1B) [23].
- Machine Learning Classification:
- Use the eXtreme Gradient Boosting (XGBoost) algorithm to build and compare different models:
- Model 1: Neuroimaging-Epigenetic Model (AASP + rs-FC + DNA methylation).
- Model 2: Neuroimaging Model (AASP + rs-FC).
- Model 3: Epigenetic Model (AASP + DNA methylation).
- Use the sensory behavior (AASP) as the default baseline for all models.
- Evaluate model performance to determine which combination of factors provides the most accurate classification of ASD. The study hypothesized that the integrated neuroimaging-epigenetic model would be superior [23].
- Use the eXtreme Gradient Boosting (XGBoost) algorithm to build and compare different models:
Methodological Visualizations
Diagram 1: Analytical Workflow for Integrated ASD Biomarker Discovery
Diagram 2: Epigenetic & Neurobiological Pathways of Early-Life Stress
Advanced Tools for Deconstruction: Multi-Omics, AI, and Person-Centered Approaches
Autism Spectrum Disorder (ASD) is fundamentally heterogeneous, encompassing diverse etiologies, clinical presentations, and developmental trajectories. This heterogeneity has persistently challenged traditional reductionist approaches that seek single biomarkers or unified explanations. Research now emphasizes integrating multiple levels of analysis—genetic, epigenetic, neural systems, behavior, and environmental factors—to advance toward precision medicine [34] [35]. The field is transitioning from viewing autism as a single disorder to recognizing "autisms," requiring models that accommodate both categorical subtypes and continuous dimensions of difference [34].
This technical support guide provides troubleshooting resources for researchers implementing integrative approaches to ASD biomarker discovery. It addresses methodological challenges in combining disparate data types, offers standardized protocols for cross-domain integration, and provides frameworks for interpreting complex, multi-level results within a person-centered research paradigm.
Frequently Asked Questions: Troubleshooting Integrative Research
Q1: Our research group is struggling with integrating neuroimaging and epigenetic data. What analytical approaches can handle this multi-modal complexity?
A1: Machine learning frameworks, particularly eXtreme Gradient Boosting (XGBoost), have demonstrated efficacy for neuroimaging-epigenetic integration. One successful protocol combined thalamo-cortical resting-state functional connectivity (rs-FC) measures with DNA methylation values of arginine vasopressin receptor (AVPR) genes, using sensory-related behavior as a baseline reference [14]. This approach identified thalamo-cortical hyperconnectivity and AVPR1A epigenetic modification as significant contributing factors. For optimal results:
- Ensure consistent participant characterization across modalities
- Use standardized pre-processing pipelines for each data type before integration
- Implement cross-validation to prevent overfitting in multi-modal models
- Apply SHapley Additive exPlanations (SHAP) for model interpretability [36]
Q2: How can we address the challenge of small sample sizes in subgroup identification within heterogeneous ASD populations?
A2: Small samples severely limit subgroup detection in ASD heterogeneity. Pursue these strategies:
- Leverage existing large-scale datasets (ABIDE, Simons Foundation Powering Autism Research)
- Employ federated learning approaches that analyze data across multiple sites without sharing raw data
- Utilize data augmentation techniques specific to your data types
- Apply unsupervised clustering algorithms (K-means, hierarchical clustering) to identify data-driven subgroups before validation in larger samples [34]
Current research indicates that sample sizes exceeding 100 participants provide more reliable subgroup identification, with ideal studies including 500+ participants for robust stratification [34].
Q3: What are the best practices for validating biomarker panels across different ASD subpopulations?
A3: Effective validation requires a multi-stage approach:
- Internal validation: Use bootstrapping or cross-validation within your discovery sample
- External validation: Test biomarkers in independent cohorts with different demographic characteristics
- Clinical validation: Assess whether biomarkers predict treatment response or developmental trajectories
- Biological validation: Examine whether identified biomarkers converge on coherent biological pathways
For proteomic biomarkers, one study established a 12-protein panel that identified ASD with AUC = 0.879±0.057, specificity of 0.853±0.108, and sensitivity of 0.832±0.114, with four proteins correlating with ADOS severity scores [37]. This demonstrates the potential of multi-analyte panels over single biomarkers.
Q4: How can we effectively incorporate motor and sensory measures into ASD biomarker studies when most diagnostic instruments focus on social-communication symptoms?
A4: Motor differences are present in 50-85% of autistic individuals and represent a promising domain for biomarker development [38]. Implementation strategies include:
- Supplement standard diagnostic instruments with standardized motor assessments (Peabody Developmental Motor Scales, Movement Assessment Battery for Children)
- Incorporate technological measures (wearable sensors, motion capture) to quantify subtle motor patterns invisible to naked eye observation
- Assess sensory processing using standardized tools like the Adolescent-Adult Sensory Profile (AASP), which characterizes four patterns: Low Registration, Sensitivity, Sensation Seeking, and Avoidance [14]
- Design studies that collect longitudinal motor data to capture developmental trajectories
Q5: What statistical methods best account for the multiple comorbidities and concomitant medical conditions in ASD research?
A5: The Advanced Integrative Model (AIM) reframes "comorbidities" as Concomitant Medical Problems to Diagnosis (CMPD) that may directly influence ASD symptoms [39]. Analytical approaches include:
- Structural Equation Modeling (SEM) to test causal pathways between CMPD and core ASD symptoms
- Multivariate pattern analysis to identify clusters of co-occurring medical conditions
- Network analysis to map interactions between different biological systems
- Control for CMPD that may confound biomarker signals rather than treating them as nuisance variables
Research shows that treating medical conditions such as gastrointestinal issues, immune dysfunction, and mitochondrial disorders sometimes improves core ASD symptoms, indicating their potential relevance to underlying mechanisms [39].
Quantitative Data Synthesis: Biomarker Findings Across Modalities
Table 1: Multi-Level Biomarker Findings in Autism Research
| Domain | Specific Biomarker | Finding Direction | Effect Size/Performance | Reference |
|---|---|---|---|---|
| Neuroimaging | Thalamo-cortical rs-FC | Hyperconnectivity in ASD | Key feature in classification model | [14] |
| Epigenetic | AVPR1A methylation | Significant contributor to classification | Improved model accuracy in combined approach | [14] |
| Proteomic | 12-protein serum panel | Differentiated ASD vs. TD | AUC = 0.879±0.057, Specificity = 0.853±0.108 | [37] |
| Genetic | De novo mutations | Associated with lower IQ and higher epilepsy rates | Distinct subtype with more severe presentation | [35] |
| Sensory | AASP scores | Elevated Avoidance, Low Registration, Sensitivity | Significant group differences (p<0.0001) | [14] |
Table 2: Methodological Comparison of Integrative Approaches
| Approach | Data Types Integrated | Analytical Method | Strengths | Limitations |
|---|---|---|---|---|
| Neuroimaging-Epigenetic | rs-fMRI, structural MRI, DNA methylation | XGBoost machine learning | Accounts for brain-epigenetic interactions | Requires large sample sizes |
| Genomic-ML | Gene expression, SNPs | SHAP explainable AI | Identifies key genetic features | Limited to known genetic variants |
| Proteomic-ML | Serum protein levels | SOMAScan assay + ML | High predictive accuracy | Need for independent validation |
| Motor-Digital | Wearable sensor data, clinical assessment | Digital phenotyping | Objective, continuous measurement | Emerging technology, less standardized |
Experimental Protocols for Integrative Biomarker Discovery
Protocol: Multi-Modal Data Collection for Neuroimaging-Epigenetic Integration
This protocol outlines procedures for collecting matched neuroimaging and epigenetic data for integrative biomarker discovery [14].
Materials:
- 3T MRI scanner with phased-array head coil
- DNA collection kits (saliva or blood)
- Sensory and behavioral assessment tools (AASP, ADOS-2, IQ measures)
- Data management system for multi-modal data linkage
Procedure:
- Participant Characterization:
- Confirm ASD diagnosis using DSM-5 criteria and ADOS-2
- Assess full-scale IQ using Wechsler Intelligence Scales
- Administer Adolescent-Adult Sensory Profile (AASP) questionnaire
- Screen for exclusion criteria (brain injury, major physical illness, substance abuse)
DNA Collection and Methylation Analysis:
- Collect saliva samples using standardized kits
- Extract DNA following manufacturer protocols
- Perform bisulfite conversion on extracted DNA
- Analyze methylation of candidate genes (OXTR, AVPR1A, AVPR1B) using targeted approaches or epigenome-wide arrays
- Normalize methylation data using standard bioinformatics pipelines
Neuroimaging Data Acquisition:
- Acquire high-resolution T1-weighted structural images (parameters: TR=6.38ms, TE=1.99ms, FA=11°, FoV=256mm, voxel size=1×1×1mm³)
- Collect resting-state fMRI using T2*-weighted gradient-echo EPI sequence
- Implement quality control procedures during acquisition
Data Integration and Analysis:
- Preprocess structural images (segmentation, normalization)
- Process functional data (slice-time correction, motion correction, normalization, smoothing)
- Extract thalamo-cortical functional connectivity measures
- Combine neuroimaging and epigenetic features in XGBoost model with sensory behavior as baseline
- Validate model performance using cross-validation
Troubleshooting:
- Motion artifacts in fMRI: Implement rigorous motion correction and consider framewise exclusion
- Batch effects in epigenetic data: Include control samples across batches and apply correction methods
- Missing data: Use multiple imputation techniques appropriate for the data type
Protocol: Serum Proteomic Biomarker Panel Identification
This protocol details the process for identifying serum protein biomarkers for ASD using proteomic analysis [37].
Materials:
- Serum collection tubes (SST)
- SomaLogic SOMAScan assay 1.3K platform
- Clinical assessment tools (ADOS-2, ABAS-II)
- Statistical software (R, Python) with machine learning libraries
Procedure:
- Participant Recruitment and Characterization:
- Recruit age-matched ASD and typically developing (TD) participants (male-only or include sex as biological variable)
- Establish ASD diagnosis with ADOS-2 and clinical judgment
- Exclude participants with genetic, metabolic, or other concurrent physical/neurological disorders
- Collect demographic and clinical data (age, ethnicity, comorbidities, medication use)
Sample Collection and Processing:
- Collect blood samples following standard phlebotomy procedures
- Allow blood to clot for 30 minutes at room temperature
- Centrifuge at 1,000-2,000 × g for 10 minutes at 4°C
- Aliquot serum and store at -80°C until analysis
- Avoid freeze-thaw cycles
Proteomic Analysis:
- Process serum samples using SomaLogic SOMAScan platform
- Measure 1,125 proteins simultaneously using aptamer-based technology
- Follow standard hybridization, washing, and elution procedures
- Normalize data using adaptive normalization by maximum likelihood
Statistical Analysis and Biomarker Identification:
- Perform differential expression analysis (ASD vs. TD) with false discovery rate correction
- Apply multiple machine learning algorithms (random forest, support vector machines, logistic regression)
- Identify optimal protein panel through feature selection methods
- Validate panel using cross-validation and calculate AUC, sensitivity, specificity
- Correlate protein levels with ADOS severity scores (ASD group only)
Troubleshooting:
- High background signal: Check reagent quality and washing steps
- Batch effects: Randomize samples across processing batches
- Overfitting: Use appropriate cross-validation and independent test sets
Signaling Pathways and Workflow Visualizations
Diagram 1: Multi-Modal Data Integration Workflow for ASD Biomarker Discovery
Diagram 2: Modeling Approaches for ASD Heterogeneity
Research Reagent Solutions for Integrative Studies
Table 3: Essential Research Materials for Multi-Modal ASD Biomarker Studies
| Category | Specific Tool/Reagent | Application in ASD Research | Key Features |
|---|---|---|---|
| Genetic/Epigenetic | DNA methylation arrays (Illumina EPIC) | Genome-wide methylation analysis | Coverage of >850,000 CpG sites |
| Targeted bisulfite sequencing kits | Candidate gene methylation analysis | High sensitivity for specific loci | |
| Proteomic | SomaLogic SOMAScan platform | Multiplexed protein biomarker discovery | Simultaneous measurement of 1,100+ proteins |
| Multiplex immunoassays (Luminex) | Cytokine/chemokine profiling | Quantification of immune markers | |
| Neuroimaging | 3T MRI with high-resolution capabilities | Structural and functional brain imaging | Submillimeter resolution for cortical features |
| Resting-state fMRI sequences | Functional connectivity analysis | Identifies network-level alterations | |
| Behavioral | ADOS-2 | Diagnostic confirmation and severity assessment | Gold-standard diagnostic tool |
| Adolescent-Adult Sensory Profile | Sensory processing characterization | Measures four sensory patterns | |
| Data Integration | XGBoost algorithm | Multi-modal data integration | Handles mixed data types, provides feature importance |
| SHAP (SHapley Additive exPlanations) | Model interpretability | Quantifies feature contribution to predictions |
Overcoming reductionism in autism biomarker research requires systematic approaches that embrace rather than control for heterogeneity. By implementing the protocols, troubleshooting guides, and integrative frameworks provided in this technical support resource, researchers can advance toward person-centered biomarker discovery that respects the multifaceted nature of autism. The future of ASD research lies in developing biomarkers that not only improve early detection but also guide personalized intervention strategies matched to individual biological and behavioral profiles.
Autism Spectrum Disorder (ASD) is characterized by significant heterogeneity in its etiology, phenotype, and outcomes, posing substantial challenges for biomarker discovery and therapeutic development. Genetic variation is considered a principal factor in this heterogeneity, with potentially thousands of genes involved, each accounting for less than 1% of cases individually [40]. This diversity makes finding consistent diagnostic biomarkers particularly challenging.
However, emerging research demonstrates that despite this genetic heterogeneity, common underlying mechanisms can be uncovered through integrated multi-omics approaches. By combining proteomic and metabolomic profiling, researchers have identified that children with ASD—whether carrying known risk genes or not—show remarkably similar plasma proteomic and metabolomic characteristics that effectively distinguish them from neurotypical controls [40]. This article provides technical guidance for implementing these approaches to uncover common biological pathways in ASD.
Key Experimental Protocols and Methodologies
Plasma Proteomic Profiling Using SWATH-MS
Protocol Overview: The sequential window acquisition of all theoretical fragment ions mass spectrometry (SWATH-MS) technique enables comprehensive protein quantification from plasma samples. This data-independent acquisition method creates a permanent digital record of all detectable analytes in a sample, allowing retrospective data analysis without additional experiments [40].
Detailed Methodology:
- Sample Preparation: Collect plasma samples via venipuncture using EDTA tubes. Process within 2 hours of collection through centrifugation at 3000× g for 15 minutes at 4°C. Aliquot and store at -80°C until analysis.
- Protein Digestion: Dilute plasma samples 1:10 with 50 mM ammonium bicarbonate. Reduce with 10 mM dithiothreitol at 60°C for 30 minutes, then alkylate with 20 mM iodoacetamide at room temperature for 30 minutes in the dark. Digest with trypsin (1:20 enzyme-to-protein ratio) overnight at 37°C.
- SWATH-MS Analysis: Separate peptides using nanoflow liquid chromatography (nanoLC) with a C18 reverse-phase column (75 μm × 150 mm, 3 μm particle size). Perform MS analysis using a TripleTOF 6600+ system with a DuoSpray ion source. Acquire data in two phases: first create a spectral library using information-dependent acquisition (IDA), then perform SWATH-MS acquisition using 100 variable windows across the 400-1250 m/z range.
- Data Processing: Process SWATH-MS data using software such as PeakView or OpenSWATH. Align retention times, extract ion chromatograms, and identify proteins by matching against the spectral library. Normalize protein intensities using total area sum normalization [40].
Critical Parameters:
- Maintain consistent sample processing times to minimize pre-analytical variability
- Include quality control pools by combining aliquots from all samples
- Monitor instrument performance using retention time standards
- Implement randomized sample acquisition orders to avoid batch effects
Metabolomic Profiling Using HPLC-MS
Protocol Overview: High-performance liquid chromatography-mass spectrometry (HPLC-MS) enables comprehensive metabolomic profiling from plasma samples, capturing diverse classes of metabolites including amino acids, lipids, vitamins, and neurotransmitters [40].
Detailed Methodology:
- Sample Preparation: Thaw plasma samples on ice. Precipitate proteins by adding 300 μL of cold methanol to 100 μL of plasma. Vortex vigorously for 30 seconds, then incubate at -20°C for 1 hour. Centrifuge at 14,000× g for 15 minutes at 4°C. Transfer supernatant to a new tube and evaporate to dryness under nitrogen stream. Reconstitute in 100 μL of 0.1% formic acid in water for analysis.
- HPLC Conditions: Use a reversed-phase C18 column (2.1 × 100 mm, 1.8 μm particle size) maintained at 40°C. Employ a binary gradient with mobile phase A (0.1% formic acid in water) and mobile phase B (0.1% formic acid in acetonitrile). Use a flow rate of 0.3 mL/min with the following gradient: 0-2 minutes 2% B, 2-15 minutes 2-95% B, 15-18 minutes 95% B, 18-18.1 minutes 95-2% B, 18.1-22 minutes 2% B for re-equilibration.
- MS Analysis: Operate mass spectrometer in both positive and negative electrospray ionization modes. Use scan ranges of 50-1000 m/z for full scans. Set source parameters: gas temperature 300°C, gas flow 8 L/min, nebulizer pressure 35 psi, sheath gas temperature 350°C, sheath gas flow 11 L/min, capillary voltage 3500 V (positive) or 3000 V (negative).
- Data Processing: Convert raw data to mzML format. Perform peak picking, alignment, and integration using XCMS or similar software. Annotate metabolites using databases such as HMDB, METLIN, or MassBank with mass accuracy < 10 ppm [40] [41].
Critical Parameters:
- Analyze samples in randomized order with quality control samples every 5-10 injections
- Include process blanks to identify background contamination
- Use internal standards for quality control and retention time alignment
- Maintain consistent sample preparation timing to minimize degradation
Multi-Omics Data Integration Approaches
Protocol Overview: Integration of proteomic and metabolomic data requires specialized computational approaches to identify cross-omics relationships and biological pathways that would remain hidden in single-omics analyses [42].
Detailed Methodology:
- Data Preprocessing: Normalize each omics dataset separately using appropriate methods (e.g., quantile normalization for proteomics, probabilistic quotient normalization for metabolomics). Perform missing value imputation using k-nearest neighbors or similar algorithms. Apply log-transformation and Pareto scaling to normalize distributions.
- Multi-Omics Integration: Use one of three main approaches:
- Early Integration: Combine normalized proteomic and metabolomic features into a single matrix before analysis. Apply multivariate statistical methods such as PCA or OPLS-DA to the combined dataset.
- Intermediate Integration: Use methods such as MOFA+ (Multi-Omics Factor Analysis) to identify latent factors that capture common variation across both omics layers. This approach models each omics dataset as a function of shared and specific factors.
- Late Integration: Analyze each omics dataset separately, then combine results through correlation networks or pathway enrichment analysis [42] [43].
- Pathway Analysis: Map differentially expressed proteins and metabolites to biological pathways using databases such as KEGG or Reactome. Identify enriched pathways using hypergeometric tests or gene set enrichment analysis (GSEA).
- Network Analysis: Construct correlation networks between proteins and metabolites. Identify hub nodes with high connectivity that may represent key regulatory points in ASD-associated pathways [44].
Critical Parameters:
- Address batch effects using ComBat or similar algorithms before integration
- Validate integration results through permutation testing
- Use multiple integration methods to confirm robust findings
- Implement appropriate multiple testing correction (e.g., Benjamini-Hochberg FDR)
Technical Support Center: Troubleshooting Guides and FAQs
Sample Quality and Preparation Issues
FAQ: How can I minimize pre-analytical variability in plasma samples for multi-omics studies?
Answer: Pre-analytical variability significantly impacts multi-omics data quality. Implement these standardized procedures:
- Use consistent blood collection tubes (EDTA) across all samples
- Process samples within 2 hours of collection
- Employ standardized centrifugation protocols (3000× g for 15 minutes at 4°C)
- Aliquot samples immediately after processing to avoid freeze-thaw cycles
- Document exact processing times and include as covariates in statistical models
- Use protease and phosphatase inhibitors for proteomic analyses
- For metabolomics, immediately quench enzymatic activity by placing samples on ice [40] [45]
Troubleshooting Table: Common Sample Preparation Issues
| Problem | Potential Cause | Solution |
|---|---|---|
| High missing values in proteomics data | Protein degradation during processing | Verify inhibitor cocktail effectiveness; reduce processing time |
| Poor chromatographic separation | Column contamination or deterioration | Implement guard columns; perform regular column cleaning |
| Inconsistent metabolite detection | Incomplete protein precipitation | Optimize methanol:plasma ratio; verify precipitation temperature |
| Batch effects in integrated data | Different processing dates or personnel | Randomize sample processing order; include technical replicates |
Data Acquisition and Instrumentation
FAQ: What quality control measures should I implement for SWATH-MS acquisition?
Answer: Robust quality control is essential for reproducible SWATH-MS data:
- Create a spectral library from pooled quality control (QC) samples
- Inject QC samples every 5-10 experimental samples to monitor instrument performance
- Use internal retention time standards to ensure chromatographic alignment
- Monitor peak intensity, retention time stability, and mass accuracy across QC injections
- Establish acceptance criteria for key parameters (e.g., <10% CV for internal standards)
- Include standard proteins at known concentrations to assess quantification accuracy [40]
FAQ: How can I improve metabolite identification confidence in HPLC-MS?
Answer: Enhance metabolite annotation through these approaches:
- Analyze samples in both positive and negative ionization modes
- Use authentic chemical standards when available to verify retention times
- Implement tandem MS (MS/MS) with collision energy ramping for structural information
- Leverage multiple databases (HMDB, METLIN, MassBank) for annotation
- Apply tiered confidence levels (Level 1: confirmed with standard, Level 2: putative annotation by MS/MS, Level 3: putative by mass only)
- Calculate confidence scores incorporating mass accuracy, isotopic pattern, and fragmentation data [40] [45]
Data Integration and Computational Challenges
FAQ: Which multi-omics integration method is most appropriate for ASD biomarker discovery?
Answer: Method selection depends on your research question and data structure:
Table: Multi-Omics Integration Method Selection Guide
| Method | Best Use Case | Advantages | Limitations |
|---|---|---|---|
| MOFA+ | Exploratory analysis of shared variation | Identifies latent factors; handles missing data | Unsupervised; may not directly link to phenotype |
| DIABLO | Supervised biomarker discovery | Maximizes separation of predefined groups | Requires careful tuning of parameters |
| Similarity Network Fusion (SNF) | Identifying patient subgroups | Robust to noise; preserves data types | Computationally intensive for large datasets |
| Multiple Co-Inertia Analysis (MCIA) | Visualizing omics relationships | Intuitive visualization of sample patterns | May not capture complex non-linear relationships |
For ASD biomarker studies where the goal is distinguishing cases from controls, DIABLO often provides the most direct approach. For discovering novel ASD subgroups without pre-defined labels, MOFA+ or SNF are more appropriate [42] [43].
FAQ: How can I address the high dimensionality challenge in multi-omics data?
Answer: High-dimensional data (many features, few samples) requires specialized approaches:
- Apply feature selection methods before integration (e.g., variance-based filtering)
- Use regularization techniques (LASSO, elastic net) to prevent overfitting
- Implement cross-validation with appropriate folds (nested CV for parameter tuning)
- Apply dimension reduction methods (PCA, UMAP) separately to each omics layer before integration
- Utilize ensemble methods that combine multiple feature selection approaches
- Validate findings in independent cohorts when possible [42] [43]
Troubleshooting Table: Common Data Integration Challenges
| Problem | Potential Cause | Solution |
|---|---|---|
| Poor integration performance | High technical noise in individual datasets | Improve preprocessing; apply more stringent quality control |
| Batch effects persisting after correction | Non-linear batch effects | Use non-linear correction methods (e.g., Combat with non-parametric adjustment) |
| Missing data patterns biasing results | Systematic differences in detection limits | Implement missing-not-at-random imputation methods |
| Overfitting in predictive models | High feature-to-sample ratio | Apply stronger regularization; use nested cross-validation |
Key Signaling Pathways and Experimental Workflows
ASD-Associated Pathways Identified Through Multi-Omics
Research integrating proteomics and metabolomics in ASD has consistently implicated several key biological pathways despite genetic heterogeneity. These include complement activation and immune response pathways, amino acid metabolism (particularly tryptophan and glutamate metabolism), glycerophospholipid metabolism, and synaptic signaling pathways [40] [41] [45].
Integrative analyses have revealed that L-glutamic acid and malate dehydrogenase may play particularly important roles in ASD pathophysiology, potentially serving as key nodes connecting multiple disrupted pathways [40]. Additionally, gut-brain axis signaling has emerged as a significant mechanism, with microbial metabolites such as neurotransmitters (glutamate, DOPAC) and immune modulators capable of crossing the blood-brain barrier and influencing neurodevelopment [41].
Multi-Omics Pathway Integration in ASD
Experimental Workflow for ASD Multi-Omics Studies
A robust workflow for ASD multi-omics studies incorporates sample collection, multi-omics data generation, computational integration, and validation phases. The following diagram illustrates this comprehensive approach:
ASD Multi-Omics Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Research Reagents for ASD Multi-Omics Studies
| Reagent/Material | Function | Application Notes |
|---|---|---|
| EDTA blood collection tubes | Plasma preparation; prevents coagulation | Maintain consistent tube lot; process within 2 hours |
| Protease inhibitor cocktails | Preserves protein integrity during processing | Use broad-spectrum formulations; add immediately after collection |
| Mass spectrometry grade solvents | HPLC-MS mobile phases; sample preparation | Use low-UV absorbing acetonitrile and methanol |
| Trypsin (sequencing grade) | Protein digestion for proteomics | Optimize enzyme-to-protein ratio; verify digestion efficiency |
| Stable isotope internal standards | Metabolite quantification normalization | Include for key pathway metabolites (amino acids, neurotransmitters) |
| Quality control reference plasma | Monitoring analytical performance | Use pooled samples from study participants or commercial sources |
| Retention time calibration kits | LC-MS system performance monitoring | Inject at beginning and end of sequence; monitor drift |
| Protein standards (BSA, etc.) | Quantification calibration | Use for absolute quantification when targeted approaches needed |
The integration of proteomics and metabolomics provides a powerful strategy for addressing heterogeneity in ASD research. By focusing on functional readouts of cellular processes rather than genetic variation alone, these approaches can identify common biological mechanisms across genetically diverse ASD individuals. The methodologies and troubleshooting guides presented here offer practical frameworks for implementing these approaches in ongoing ASD biomarker discovery efforts.
Future directions in the field include the incorporation of single-cell multi-omics technologies, spatial omics approaches to understand tissue microenvironment contributions, and longitudinal sampling to capture dynamic changes in proteomic and metabolomic profiles. Additionally, the integration of electronic health records with multi-omics data through artificial intelligence approaches promises to further advance personalized biomarker discovery in ASD [46] [43].
Harnessing Machine Learning for Subtype Identification and Outcome Prediction
Frequently Asked Questions (FAQs) & Troubleshooting Guides
This technical support center is designed for researchers and scientists tackling the challenge of heterogeneity in autism spectrum disorder (ASD) through machine learning (ML). Below you will find answers to common experimental questions and guides for troubleshooting specific issues.
FAQ 1: What are the primary data-driven strategies for addressing heterogeneity in autism research?
Answer: The most effective strategy is to move from a trait-centered to a person-centered approach, which models the full spectrum of co-occurring traits in an individual to define biologically distinct subgroups. This is a foundational step for meaningful biomarker discovery.
- Recommended Approach: Use a person-centered, data-driven subtyping framework. This involves collecting extensive phenotypic and genotypic data and using computational models to group individuals based on their full clinical profile, rather than analyzing single traits in isolation [10] [9].
- Evidence from Recent Research: A seminal 2025 study analyzed over 230 traits in more than 5,000 autistic individuals from the SPARK cohort. Using a general finite mixture model, researchers identified four clinically and biologically distinct subtypes of autism [10] [9]. The traits, group prevalence, and distinct biological narratives of these subtypes are summarized in the table below.
Table 1: Data-Driven Autism Subtypes Identified via Person-Centered Machine Learning
| Subtype Name | Prevalence | Key Clinical Traits | Underlying Biology & Genetic Insights |
|---|---|---|---|
| Social & Behavioral Challenges | ~37% | Core ASD traits (social challenges, repetitive behaviors); co-occurring conditions (ADHD, anxiety, depression); no developmental delays [10] [9]. | Impacted genes are mostly active after birth; aligns with later age of diagnosis and absence of developmental delays [9]. |
| Mixed ASD with Developmental Delay | ~19% | Reaches developmental milestones (e.g., walking, talking) later than peers; generally does not show anxiety or depression [10] [9]. | Impacted genes are mostly active prenatally; higher likelihood of carrying rare inherited genetic variants [9]. |
| Moderate Challenges | ~34% | Core ASD-related behaviors present but to a lesser degree; no developmental delays; generally no co-occurring psychiatric conditions [10] [9]. | - |
| Broadly Affected | ~10% | Widespread challenges: developmental delays, social/communication difficulties, repetitive behaviors, and co-occurring psychiatric conditions [10] [9]. | Shows the highest proportion of damaging de novo mutations (not inherited from parents) [9]. |
The workflow for this person-centered subtyping approach is detailed in the diagram below.
FAQ 2: Our model for predicting adaptive behavior trajectories is underperforming. What key predictors should we prioritize?
Answer: Underperformance often stems from incomplete feature selection. Beyond standard clinical measures, prioritize sociodemographic variables and detailed parental reports collected at intake.
- Troubleshooting Guide:
- Problem: The model fails to capture the true variability in outcomes.
- Solution: Integrate high-impact, non-obvious predictors that have been empirically validated.
- Evidence-Based Protocol: A 2025 clinical cohort study (N=1225) used latent class growth mixture modeling (LCGMM) to identify two distinct adaptive behavior trajectories. A subsequent random forest model predicted trajectory membership with 77% accuracy. The strongest predictors are listed below [47].
Table 2: Key Predictors of Adaptive Behavior Trajectories in Autism
| Predictor Category | Specific Variables | Function in the Model |
|---|---|---|
| Sociodemographic | Socioeconomic Status (SES); Paternal Age at Child's Birth | Provides context on environmental and familial factors influencing development [47]. |
| Developmental History | History of Developmental Regression; Age at Milestone Achievement | Captures critical early-life developmental patterns and potential regressions [47] [48]. |
| Baseline Clinical Presentation | Baseline Autism Symptom Severity; Presence of ADHD Symptoms | Quantifies the initial intensity of core and co-occurring symptoms [47]. |
| Parent-Reported Concerns | Parent Concerns about Development; Parent Concerns about Mood; Child Temperament | Incorporates valuable qualitative insights from caregivers into the quantitative model [47]. |
Note on Interventions: A critical finding was that the cumulative hours of applied behavioral analysis (ABA) and other developmental therapies were not a significant predictor in the model, indicating that increased therapy hours alone did not predict greater improvement [47].
FAQ 3: How can we effectively integrate multimodal data to improve ASD classification accuracy?
Answer: Superior classification is achieved by building models that combine behavioral data with underlying neuroimaging and epigenetic biomarkers, as this directly targets the biological roots of heterogeneity.
- Experimental Protocol: A 2025 study provides a clear methodology for creating a neuroimaging-epigenetic model [14]:
- Data Collection:
- Behavioral: Administer the Adolescent-Adult Sensory Profile (AASP) questionnaire.
- Neuroimaging: Acquire structural and resting-state functional MRI (rs-fMRI) scans. Focus on calculating thalamo-cortical resting-state functional connectivity (rs-FC).
- Epigenetic: Collect saliva samples to compute DNA methylation values of specific genes (e.g., arginine vasopressin receptor 1A, or
AVPR1A).
- Model Building & Comparison: Build and compare three separate models using the XGBoost algorithm [14]:
- A neuroimaging-epigenetic model (behavior, brain, and epigenetic factors).
- A neuroimaging model (behavior and brain factors).
- An epigenetic model (behavior and epigenetic factors).
- Validation: The study demonstrated that the integrated neuroimaging-epigenetic model outperformed the other two, with thalamo-cortical hyperconnectivity and
AVPR1Aepigenetic modification being significant contributing factors [14].
- Data Collection:
The logical relationship and workflow for this multimodal approach is as follows:
FAQ 4: We are getting poor performance from our predictive model for intellectual disability (ID). How can we improve it?
Answer: Poor performance likely results from using predictors in isolation. A model that combines different classes of genetic variants with developmental milestones shows the most clinically relevant, individual-level predictions.
- Troubleshooting Steps:
- Check Data Integration: Ensure your model is not relying on a single type of predictor (e.g., only polygenic scores).
- Feature Selection: Incorporate a blend of genetic and early developmental features.
- Validated Methodology: A 2025 prognostic study (N=5633) developed a model to predict ID in autistic children. The model integrated five key classes of predictors, achieving an area under the receiver operating characteristic curve (AUROC) of 0.65. While modest, this model provided clinically useful predictions, correctly identifying 10% of ID cases with a positive predictive value (PPV) of 55% [48].
Table 3: Predictors for Intellectual Disability (ID) in Autism
| Predictor Category | Specific Variables | Function in the Model |
|---|---|---|
| Developmental Milestones | Motor, Language, and Toileting Milestones; Occurrence of Language Regression | Provides a direct measure of early developmental progress and potential red flags [48]. |
| Polygenic Scores (PGS) | PGS for Cognitive Ability; PGS for Autism | Captures the aggregate contribution of many common genetic variants to an individual's liability [48]. |
| Rare Genetic Variants | Rare Copy Number Variants (CNVs); De novo Loss-of-Function & Missense variants impacting constrained genes | Accounts for the impact of large-effect, often spontaneous, genetic mutations [48]. |
A key finding was that the ability to stratify ID risk using genetic variants was up to 2-fold higher in individuals with delayed milestones compared to those with typical development, highlighting the power of combined models [48].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Resources for Autism ML Biomarker Discovery Research
| Item / Resource | Function / Application | Example from Literature |
|---|---|---|
| SPARK Cohort Data | A large-scale cohort providing extensive phenotypic and genotypic data for over 150,000 autistic individuals and family members; essential for training and validating models on a representative scale [10] [9]. | Used as the primary data source for identifying the four autism subtypes and for developing the ID prediction model [10] [48]. |
| General Finite Mixture Model | A type of computational model that can handle different data types (yes/no, categorical, continuous) and integrate them into a single probability for each individual, enabling person-centered subtyping [10]. | The core algorithm used to define the four autism subgroups based on shared phenotypic profiles [10] [9]. |
| XGBoost Algorithm | An efficient and powerful machine learning algorithm based on gradient boosting, well-suited for classification tasks and handling complex, mixed data types [14] [49]. | Used to compare the performance of neuroimaging, epigenetic, and combined models for ASD classification [14]. |
| Latent Class Growth Mixture Modeling (LCGMM) | A statistical technique used to identify unobserved (latent) subgroups within a population that share similar longitudinal trajectories [47]. | Used to identify the "Less Impairment/Improving" and "Higher Impairment/Stable" adaptive behavior trajectories from VABS-3 scores [47]. |
| AVPR1A DNA Methylation Analysis | An epigenetic marker measured from saliva; its modification (e.g., hypomethylation) has been associated with sensory characteristics and serves as a biomarker in integrated models [14]. | A significant contributing factor in the neuroimaging-epigenetic model for ASD classification [14]. |
Autism spectrum disorder (ASD) is characterized by remarkable heterogeneity in both its genetic underpinnings and clinical manifestations. Research has identified hundreds of genes associated with autism, with heritability estimates of approximately 80% based on family studies [17]. This genetic complexity is matched by diverse phenotypic presentations, ranging from social communication differences to restricted/repetitive behaviors and varying co-occurring conditions [50]. The central challenge in biomarker discovery lies in identifying convergent biological pathways beneath this overwhelming diversity.
This technical support resource addresses the methodological challenges of identifying shared mechanisms across autism's genetic heterogeneity. We provide troubleshooting guidance, experimental protocols, and analytical frameworks to help researchers navigate the complexities of autism biomarker discovery, enabling the transition from heterogeneous data to biologically meaningful subgroups and convergent pathways.
Foundational Concepts: Mapping the Heterogeneity Landscape
Genetic Architecture of Autism
- Polygenic Liability: Most autism cases involve common inherited genes with low individual effects that exert additive effects in a polygenic manner. These common polygenetic influences are thought to be more specific to autism's core features [17].
- Rare Variants: Rare inherited and spontaneous genetic mutations (e.g., copy number variants, protein-disrupting variants) are identified in a subgroup of autistic individuals. These include deletions/duplications at 16p11.2 and 15q12, and alterations in genes such as CHD8, PTEN, SCN2A, and SHANK3 [17].
- Gene-Environment Interactions: Environmental factors account for approximately 40% of variance in twin studies. These include advanced parental age, maternal autoimmune disease, obesity, diabetes, infection during pregnancy, fetal exposures to air pollutants or pesticides, and perinatal factors like prematurity [17].
Data-Driven Subtyping Approaches
Recent large-scale studies have employed person-centered computational approaches to decompose phenotypic heterogeneity. One seminal study analyzed 239 phenotypic features across 5,392 individuals from the SPARK cohort, identifying four clinically and biologically distinct subtypes [51] [9] [13].
Table 1: Clinically Relevant Autism Subtypes and Their Characteristics
| Subtype Name | Approximate Prevalence | Core Clinical Features | Genetic Correlates |
|---|---|---|---|
| Social/Behavioral Challenges | 37% | Core autism traits without developmental delays; high rates of ADHD, anxiety, depression | Highest ADHD and depression polygenic scores; mutations in genes active later in childhood [51] [9] |
| Mixed ASD with Developmental Delay | 19% | Developmental delays, some social challenges and repetitive behaviors; fewer co-occurring psychiatric conditions | Higher burden of rare inherited variants [9] |
| Moderate Challenges | 34% | Milder core autism traits across all domains; fewer co-occurring conditions | Not specified in results |
| Broadly Affected | 10% | Significant challenges across all domains: developmental delays, social communication difficulties, repetitive behaviors, and co-occurring psychiatric conditions | Highest proportion of damaging de novo mutations; genes associated with fragile X syndrome [9] [13] |
Troubleshooting Guides & FAQs
FAQ 1: How can we identify meaningful biological subgroups within genetically heterogeneous autism populations?
Challenge: With hundreds of associated genes and diverse presentations, traditional case-control designs lack the resolution to identify biologically coherent subgroups.
Solution: Implement person-centered computational approaches that group individuals based on their complete phenotypic profiles rather than individual traits.
- Recommended Approach: Apply generative mixture modeling (e.g., General Finite Mixture Models) to broad phenotypic data encompassing core autism features, associated behaviors, and developmental trajectories [51].
- Technical Considerations:
- Utilize item-level data from standardized instruments (e.g., SCQ, RBS-R, CBCL) rather than only composite scores [51].
- Accommodate heterogeneous data types (continuous, binary, categorical) within the modeling framework [51].
- Validate identified classes in independent cohorts and link them to genetic data [51].
Troubleshooting Checklist:
- Are phenotypic measures sufficiently comprehensive (≥200 features ideal)?
- Does the model accommodate different data types without excessive transformation?
- Have identified classes been replicated in an independent cohort?
- Do classes show differential enrichment for specific genetic variants?
FAQ 2: What experimental and analytical approaches can reveal convergent pathways across distinct genetic mutations?
Challenge: Different genetic mutations often converge on common biological pathways, but identifying these pathways requires specialized approaches.
Solution: Implement multi-omics integration and pathway enrichment analyses focused on biological systems rather than individual genes.
Proteomics Workflow:
- Analyze proteins encoded by multiple ASD-associated genes (≥60 genes recommended) [17]
- Identify protein-protein interaction networks using co-immunoprecipitation or proximity-based labeling
- Conduct pathway enrichment analysis to identify shared biological processes
- Validate network alterations using mutant forms of proteins
Key Convergent Pathways Identified in Recent Research:
Table 2: Analytical Approaches for Identifying Convergent Pathways
| Method | Application | Key Output | Technical Considerations |
|---|---|---|---|
| Proteomics Network Analysis | Identify protein interactions across ASD genes | Protein clusters representing functional modules | Requires high-quality antibodies; cross-validate with multiple methods |
| Transcriptomics | Measure gene expression patterns across brain regions | Differentially expressed gene sets | Consider developmental timing; use appropriate cell-type specific markers |
| Methylomics | Profile epigenetic modifications genome-wide | Differentially methylated regions | Tissue-specific effects require relevant tissue samples (e.g., brain) |
| Multi-omics Integration | Combine genetic, epigenetic, transcriptomic data | Unified biological models | Computational intensive; requires specialized integration algorithms |
FAQ 3: How should we handle the confounding effects of co-occurring conditions in autism biomarker studies?
Challenge: Co-occurring conditions (e.g., ADHD, anxiety, intellectual disability) are present in most autistic individuals and can confound biomarker identification.
Solution: Strategically account for co-occurring conditions through study design and statistical analysis.
Design Phase:
- Explicitly measure and characterize co-occurring conditions using standardized instruments
- Consider stratified sampling based on specific co-occurring conditions
- Include comparison groups with similar co-occurring conditions but without autism
Analytical Phase:
- Use multivariate models that include co-occurring conditions as covariates
- Implement latent class analysis to identify subgroups with similar co-occurring condition profiles
- Test for interaction effects between autism genetic risk scores and co-occurring conditions
Critical Consideration: Some co-occurring conditions may represent integral components of specific autism subtypes rather than confounders [51]. For example, ADHD symptoms are central to the "Social/Behavioral Challenges" subtype, while intellectual disability characterizes the "Broadly Affected" subtype.
Experimental Protocols
Protocol: Multi-omics Integration for Pathway Convergence
Objective: Identify biological pathways converged upon by distinct genetic variants associated with autism.
Materials:
- Genomic DNA, RNA, and protein samples from relevant tissue or cell models
- Whole exome/genome sequencing reagents
- RNA sequencing library preparation kit
- Proteomics profiling platform (e.g., mass spectrometry)
- Multi-omics integration computational pipeline
Procedure:
- Genetic Profiling:
- Perform whole exome sequencing to identify rare and common variants
- Calculate polygenic risk scores for autism and related neurodevelopmental conditions
- Annotate variants for functional impact using combined annotation-dependent depletion (CADD) scores
Transcriptomic Analysis:
- Extract high-quality RNA (RIN > 8)
- Prepare stranded RNA-seq libraries
- Sequence to minimum depth of 30 million reads per sample
- Perform differential expression analysis comparing ASD to controls
- Conduct weighted gene co-expression network analysis (WGCNA)
Proteomic Profiling:
- Prepare protein lysates under denaturing conditions
- Perform tryptic digestion and peptide purification
- Analyze using LC-MS/MS with appropriate controls
- Identify differentially expressed proteins (fold change > 1.5, FDR < 0.05)
Data Integration:
- Use multi-omics factor analysis (MOFA) to identify latent factors
- Perform pathway enrichment analysis on identified factors
- Validate key pathways in independent cohort or model system
Troubleshooting: If technical variability dominates biological signal in integration, apply batch correction and normalize using housekeeping genes/proteins. If convergence is not detected, expand analysis to include protein-protein interaction databases and chromatin accessibility data.
Protocol: Validation of Biomarkers in Preclinical Models
Objective: Validate candidate biomarkers identified in human studies in preclinical models with defined genetic alterations.
Materials:
- Genetically engineered mouse models with ASD-associated mutations
- Wild-type control animals
- Equipment for behavioral testing
- Tissue collection supplies for molecular analyses
Procedure:
- Behavioral Characterization:
- Conduct social approach tests (e.g., three-chamber social interaction)
- Assess repetitive behaviors through grooming and marble burying
- Evaluate learning and memory using Morris water maze or fear conditioning
Molecular Validation:
- Collect brain tissue at multiple developmental timepoints
- Analyze expression of candidate biomarkers using qPCR, Western blot, or immunohistochemistry
- Assess functional relevance through electrophysiology or calcium imaging
Interventional Studies:
- Test whether modulating identified pathways rescues behavioral phenotypes
- Assess biomarker response to intervention
Expected Outcomes: Successful validation shows correlation between biomarker levels and behavioral phenotypes, rescue of biomarkers with effective interventions, and consistency across models with mutations in the same pathway.
Visualization of Pathways and Workflows
Pathway Convergence in Autism Heterogeneity
Multi-Omics Integration Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Convergence Studies
| Category | Specific Reagents/Tools | Function/Application | Key Considerations |
|---|---|---|---|
| Genomic Profiling | Whole exome sequencing kits; Illumina Infinium Global Screening Arrays; CRISPR/Cas9 gene editing systems | Identify genetic variants; validate functional impact of mutations | Ensure coverage of known ASD risk genes; include population-matched controls |
| Transcriptomics | RNA extraction kits (e.g., Qiagen RNeasy); ribosomal RNA depletion kits; single-cell RNA-seq platforms | Measure gene expression patterns; identify co-expression networks | Prioritize brain-relevant tissues; consider developmental timing |
| Epigenetic Analysis | Bisulfite conversion kits; methylated DNA immunoprecipitation (MeDIP) reagents; chromatin immunoprecipitation (ChIP) kits | Profile DNA methylation; analyze histone modifications | Account for tissue-specific epigenetic patterns; use appropriate controls |
| Proteomic Tools | Mass spectrometry systems; proximity ligation assay reagents; protein-protein interaction databases | Identify protein networks; validate interactions | Consider post-translational modifications; use multiple validation methods |
| Cell & Animal Models | iPSC differentiation kits; genetically engineered mouse models; organoid culture systems | Validate candidate mechanisms in controlled systems | Ensure relevance to human biology; characterize models thoroughly |
| Computational Tools | MOFA+; WGCNA; GWAS analysis tools; pathway enrichment software | Integrate multi-omics data; identify convergent pathways | Use version-controlled pipelines; document parameters thoroughly |
Autism Spectrum Disorder (ASD) is characterized by profound etiological and phenotypic heterogeneity, presenting a significant challenge for therapeutic development. Recent breakthroughs in defining biologically distinct subtypes and identifying novel neural circuits are paving the way for precision medicine approaches. This technical support guide addresses key experimental challenges in this evolving landscape, providing troubleshooting guidance and detailed protocols to advance your research from gene discovery to pathway-targeted interventions.
## Frequently Asked Questions & Troubleshooting Guides
### FAQ 1: How can we account for biological heterogeneity when testing new therapeutics?
Issue: A therapeutic shows efficacy in only a subset of pre-clinical models or patient-derived cells, likely due to uncharacterized biological heterogeneity.
Solution: Implement a subtyping framework prior to therapeutic testing to stratify subjects based on underlying biology rather than surface-level symptoms.
- Recommended Approach: Adopt the data-driven subtyping model that identifies four biologically distinct autism subtypes [9]. This framework links specific genetic profiles to clinical presentations.
- Experimental Protocol: Subtype Stratification Prior to Intervention
- Data Collection: For each subject, collect comprehensive phenotypic data encompassing at least 230 traits, including social interaction metrics, repetitive behaviors, developmental milestones, and co-occurring psychiatric conditions [9].
- Computational Analysis: Use a machine-learning algorithm (e.g., the "person-centered" approach described by Princeton University and Simons Foundation researchers) to cluster subjects based on their trait combinations [9].
- Genetic Profiling: Within each cluster, analyze genetic data for subtype-specific signatures:
- Therapeutic Assignment: Assign subjects to targeted therapeutic arms based on their stratified subtype and associated biological pathways.
Troubleshooting Tip: If the required computational resources for full subtyping are unavailable, begin by screening for the specific genetic variants most strongly associated with each subtype (see Table 1) to create a simplified stratification key.
### FAQ 2: What are the key considerations for validating a novel neural circuit target?
Issue: A newly identified neural circuit shows correlation with autism-like behaviors, but a causal relationship is unproven, making it a risky therapeutic target.
Solution: Establish causality using a multi-method approach to modulate the circuit and measure behavioral outcomes.
- Recommended Approach: Follow the experimental workflow established for the reticular thalamic nucleus (RTN), which demonstrated that hyperactivity in this region drives ASD-related behaviors [52].
- Experimental Protocol: Establishing Neural Circuit Causality
- Baseline Recording: In an established animal model (e.g., Cntnap2 KO mice), record neural activity (e.g., via electrophysiology or calcium imaging) from the target brain region (e.g., the RTN) during behavioral assays and in response to sensory stimuli [52].
- Pharmacological Suppression: Administer a compound known to suppress activity in the target region (e.g., the experimental seizure drug Z944 for the RTN). Re-measure neural activity and behavioral outcomes [52].
- Genetic Neuromodulation (Key Step for Causality): Use a chemogenetic approach (e.g., DREADDs) to selectively suppress neuronal activity in the target circuit. Assess for reversal of behavioral deficits [52].
- Overexpression Mimicry (Gold Standard for Causality): In wild-type subjects, use neuromodulation tools (e.g., DREADDs) to artificially increase activity in the target circuit. Assess for the induction of core behavioral deficits [52].
Troubleshooting Tip: If behavioral rescue is incomplete, the circuit may be part of a larger network. Use region-specific neuronal tracing and whole-brain imaging to identify and characterize connected networks for potential co-targeting.
### FAQ 3: How do we design an in vitro system to test a therapy for a specific genetic form of ASD?
Issue: There is a need to model a monogenic form of ASD (e.g., SHANK3 haploinsufficiency) for medium-throughput drug screening, but animal models are too low-throughput.
Solution: Generate patient-derived organoids ("mini-brains") that recapitulate key pathological features of the disorder.
- Recommended Approach: As demonstrated for MEF2C haploinsufficiency syndrome, create a human cell-derived platform that mirrors disease-specific neurobiology [53].
- Experimental Protocol: Patient-Derived Organoid Generation & Screening
- Cell Line Generation: Derive induced pluripotent stem cells (iPSCs) from fibroblasts or blood samples of patients with the specific genetic mutation (e.g., SHANK3 haploinsufficiency) and isogenic controls [53].
- Organoid Differentiation: Differentiate iPSCs into cerebral organoids using a established protocol, supporting development for several months to capture key developmental stages [53].
- Phenotypic Validation: Characterify the organoids to confirm they display expected disease phenotypes. For SHANK3, this could include:
- Therapeutic Testing: Treat organoids with candidate compounds (e.g., NitroSynapsin, which has been tested in other autism-related organoid models). Re-measure phenotypic readouts to assess rescue [53].
Troubleshooting Tip: If organoid variability is high, increase the sample size (number of organoids per line) and ensure consistent size and morphology selection for assays. Consider using single-cell RNA sequencing to confirm cell type composition and expression profiles.
### Table 1: Biologically Distinct Autism Subtypes and Associated Genetics
This table summarizes the four data-driven autism subtypes, their clinical profiles, and distinct genetic underpinnings, providing a framework for stratified therapeutic development [9].
| Subtype | Prevalence | Core Clinical Presentation | Co-occurring Conditions | Genetic Correlates |
|---|---|---|---|---|
| Social & Behavioral Challenges | ~37% | Core autism traits, typical developmental milestones | ADHD, anxiety, depression, OCD | Genes active later in childhood |
| Mixed ASD with Developmental Delay | ~19% | Developmental delays, variable social/repetitive behaviors | Typically absent | Rare inherited variants |
| Moderate Challenges | ~34% | Milder core autism traits, typical developmental milestones | Typically absent | Not specified |
| Broadly Affected | ~10% | Significant developmental delays, severe social/repetitive difficulties | Anxiety, depression, mood dysregulation | Highest burden of damaging de novo mutations |
### Table 2: Promising Therapeutic Modalities for Monogenic ASD
This table outlines emerging therapeutic approaches beyond traditional small molecules, highlighting their mechanisms and current status [55] [56].
| Therapeutic Modality | Mechanism of Action | Example Target | Development Stage |
|---|---|---|---|
| Gene Replacement Therapy | Delivers functional gene copy via viral vector (e.g., AAV9) | SHANK3 (JAG201 therapy) | Clinical trials planned for 2025 [56] |
| Antisense Oligonucleotides (ASOs) | Binds mRNA to modulate splicing/expression | SMN2 (for SMA; proof-of-concept) | Approved for other disorders; in research for ASD [56] |
| Small Molecule (e.g., Z944) | Suppresses hyperactive neural circuits | Reticular Thalamic Nucleus (T-type calcium channel) | Preclinical (mouse models) [52] |
| CRISPR-based Gene Editing | Corrects disease-causing mutations at DNA or RNA level | Rett syndrome, Phelan-McDermid models | Preclinical research [56] |
## Experimental Protocols & Workflows
### Protocol 1: Multi-modal Target Validation for the Reticular Thalamic Nucleus
This detailed protocol is derived from the Stanford study that validated the RTN as a novel therapeutic target [52].
Objective: To establish a causal link between reticular thalamic nucleus (RTN) hyperactivity and autism-like behaviors using pharmacological and chemogenetic tools in a mouse model.
Materials:
- Animals: Cntnap2 knockout mice (autism model) and wild-type controls.
- Drugs: Experimental seizure drug Z944 (T-type calcium channel blocker).
- Viral Vectors: AAVs encoding inhibitory DREADDs (hM4Di) and a fluorescent reporter under a cell-type specific promoter (e.g., for RTN neurons).
- Compounds: Clozapine-N-oxide (CNO) to activate DREADDs.
- Equipment: Stereotaxic surgical setup, in vivo electrophysiology rig, behavioral testing apparatus.
Procedure:
- Stereotaxic Surgery: Inject AAV-DREADD or AAV-control virus bilaterally into the RTN of Cntnap2 KO and WT mice. Allow 3-4 weeks for expression.
- Baseline Behavioral & Electrophysiological Phenotyping:
- Subject all mice to a behavioral battery: social interaction test (e.g., three-chamber test), seizure monitoring, open field test for repetitive behavior and hyperactivity, and sensory responsiveness assays.
- Simultaneously, record extracellular neural activity from the RTN in a subset of mice during these tasks.
- Pharmacological Intervention:
- Administer Z944 or vehicle to Cntnap2 KO mice.
- Repeat the behavioral battery and neural recording 1-2 hours post-injection.
- Chemogenetic Intervention:
- Administer CNO to DREADD-expressing and control mice.
- Repeat the behavioral battery and neural recording.
- Causality Test (Mimicry):
- In WT mice expressing excitatory DREADDs (hM3Dq) in the RTN, administer CNO to artificially induce hyperactivity.
- Perform the behavioral battery to determine if RTN hyperactivation is sufficient to produce ASD-like behaviors.
Analysis:
- Compare behavioral scores and neural firing rates (both spontaneous and evoked) between groups (KO vs. WT, drug vs. vehicle, CNO vs. baseline) using appropriate statistical tests (e.g., two-way ANOVA). Successful validation is achieved if both suppression of RTN activity rescues behaviors in KO mice and its artificial induction causes behaviors in WT mice.
### Protocol 2: Analyzing Epigenetic-Neural Interactions in Human Subjects
This protocol is based on the integrated biomarker study that combined sensory behavior, brain imaging, and epigenetic measures [23].
Objective: To investigate how epigenetic modifications (e.g., DNA methylation) and brain function (thalamo-cortical connectivity) interact to contribute to ASD.
Materials:
- Participants: Individuals with ASD and typically developing controls.
- Behavioral Tool: Adolescent-Adult Sensory Profile (AASP) questionnaire.
- Epigenetics: Saliva collection kits, DNA extraction kit, bisulfite conversion kit, pyrosequencer or equivalent for DNA methylation analysis.
- Neuroimaging: 3T MRI scanner, T1-weighted sequence (structural), T2*-weighted EPI sequence (resting-state fMRI).
Procedure:
- Phenotyping: All participants complete the AASP questionnaire to establish a baseline sensory behavior profile [23].
- Saliva Collection & DNA Methylation Analysis:
- Collect saliva samples and extract genomic DNA.
- Perform bisulfite conversion on DNA.
- Quantify DNA methylation levels at candidate gene regions (e.g., AVPR1A, OXTR) via pyrosequencing or targeted bisulfite sequencing. Calculate percentage methylation at specific CpG sites.
- MRI Data Acquisition:
- Acquire high-resolution T1-weighted structural images.
- Acquire resting-state fMRI data (e.g., 220 volumes, TR=2000ms) while participants fixate on a cross.
- fMRI Preprocessing & Analysis:
- Preprocess data using standard pipelines (e.g., in CONN or SPM): realignment, slice-time correction, normalization, smoothing.
- Perform seed-based functional connectivity analysis. Use the bilateral thalamus as the seed region. Extract the mean BOLD time series from the seed and correlate it with every voxel in the brain. Convert correlation coefficients to Fisher's z-scores.
- Integrated Statistical Modeling:
- Use a machine learning algorithm (e.g., XGBoost) to build a classification model for ASD.
- Input features should include AASP scores (baseline), thalamo-cortical functional connectivity values, and DNA methylation percentages.
- Compare model performance (e.g., accuracy, AUC) against models using only behavioral/imaging or behavioral/epigenetic data.
Analysis:
- The model will identify the most important features for classification. A key finding may be that a model integrating all three data types (neuroimaging-epigenetic) outperforms simpler models, with thalamo-cortical hyperconnectivity and AVPR1A hypomethylation being significant contributing factors [23].
## Signaling Pathways & Experimental Workflows
### Diagram 1: Reticular Thalamic Nucleus (RTN) Hyperactivity in ASD
This diagram illustrates the neural circuit and mechanism identified in the Stanford study, showing how RTN hyperactivity drives ASD-related behaviors and serves as a therapeutic target [52].
### Diagram 2: Integrated Biomarker Discovery Workflow
This diagram outlines the multi-modal experimental and computational workflow for discovering integrated biomarkers in ASD, as implemented in recent research [23] [9].
### Diagram 3: Gene Therapy Workflow for Monogenic ASD
This diagram visualizes the key steps in developing and testing an AAV-based gene replacement therapy for a monogenic form of autism, such as SHANK3 haploinsufficiency [56].
## The Scientist's Toolkit: Research Reagent Solutions
### Table 3: Essential Research Reagents for Featured Experiments
This table details key reagents, their functions, and application contexts based on the protocols and studies cited in this guide.
| Reagent / Tool | Function / Mechanism | Example Application Context |
|---|---|---|
| DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) | Chemogenetic tool for remote control of neuronal activity using inert ligand (CNO). | Causally linking RTN hyperactivity to behaviors [52]. |
| AAV9 (Adeno-Associated Virus serotype 9) | A viral vector with high tropism for neurons in the central nervous system, used for gene delivery. | Delivering SHANK3 minigene in JAG201 gene therapy [56]. |
| AASP (Adolescent-Adult Sensory Profile) Questionnaire | A self-report tool quantifying behavioral responses to sensory stimuli across four patterns. | Establishing baseline sensory phenotype in integrated biomarker studies [23]. |
| Bisulfite Conversion Kit | Chemical treatment that converts unmethylated cytosine to uracil, allowing methylation quantification. | Preparing DNA for pyrosequencing of AVPR1A/OXTR promoter regions [23]. |
| Z944 | An experimental T-type calcium channel blocker. | Suppressing RTN hyperactivity and reversing ASD-like behaviors in mice [52]. |
| Patient-Derived iPSCs | Induced Pluripotent Stem Cells; can be differentiated into any cell type, including neurons. | Generating "mini-brain" organoids to model ASD and test drugs in vitro [53]. |
| CNO (Clozapine-N-oxide) | The inert ligand that activates DREADDs. | Used in chemogenetic experiments to modulate neuronal circuits [52]. |
Navigating Research Pitfalls: Statistical Challenges and Biomarker Translation
Context: This troubleshooting guide is framed within the ongoing challenge of heterogeneity in autism spectrum disorder (ASD) research. The persistent lack of validated diagnostic biomarkers is largely attributed to the vast clinical and biological diversity within the autistic population, which group-mean comparisons often obscure [57] [58] [28]. This guide aims to equip researchers with strategies to move beyond the "on average" fallacy.
Frequently Asked Questions & Troubleshooting
Q1: Our case-control study found a statistically significant average difference in a brain imaging metric between ASD and TD groups. Why is this finding criticized as potentially misleading for biomarker development?
A1: This is a classic manifestation of the "on average" fallacy in a heterogeneous condition like ASD. A significant mean difference does not imply the biomarker is characteristic of all, or even most, individuals within the ASD group. Research indicates that in many ASD studies, a substantial proportion (e.g., 45-63%) of autistic participants fall within one standard deviation of the control group mean for various cognitive, EEG, and MRI measures [28]. Your significant p-value may be driven by a subgroup, while the metric is not informative for many others. This reduces the potential diagnostic utility and reflects the group's heterogeneity.
Q2: How can I design an experiment to account for heterogeneity from the start, rather than just acknowledging it as a limitation?
A2: Shift from a purely group-comparison framework to a stratification or subgrouping design [58] [28].
- Pre-planned Stratification: Do not just recruit an "ASD" group. Actively recruit to ensure representation across key dimensions of heterogeneity (e.g., language ability, cognitive function, sensory profiles, co-occurring conditions) [35]. Plan to analyze data within these strata.
- Dimensional Measures: Incorporate continuous measures of core autistic traits and related features (e.g., anxiety, adaptive function) as covariates or for clustering analyses, rather than relying solely on categorical diagnosis [35] [28].
- Cross-Disorder Designs: Include comparison groups with other neurodevelopmental conditions (e.g., ADHD, dyslexia). This helps determine if a putative biomarker is specific to ASD or relates to transdiagnostic mechanisms [59] [28].
Q3: We see high variability in our biomarker measurements within the ASD group. Is this just noise, or could it be meaningful data?
A3: In ASD research, within-group variability is often the signal, not the noise. This variability likely reflects biologically meaningful subgroups [57] [35]. Instead of only reporting the mean and variance, employ unsupervised machine learning techniques (e.g., clustering on multimodal data) to see if distinct data-driven subgroups emerge [59] [60]. The consistency of your biomarker within these emergent clusters is more informative than its value relative to the whole-group average.
Q4: What are the best analytical methods to identify subgroups without pre-existing biases?
A4: A combination of data-driven and hypothesis-driven approaches is recommended.
- Unsupervised Learning: Use algorithms like k-means, hierarchical clustering, or Gaussian mixture models on multimodal data (genetic, neuroimaging, behavioral) to identify data-driven subgroups [59] [60].
- Supervised Learning for Validation: Once subgroups are hypothesized, use supervised models (e.g., SVMs, random forests) to test how well they predict external outcomes (e.g., treatment response, trajectory) [59].
- Network & Systems Approaches: Move beyond single biomarkers. Analyze interactions between biological systems (e.g., brain connectivity, gene co-expression networks) to identify dysfunctional patterns that may define subgroups [28].
Q5: How do I interpret a "null" result in a well-powered ASD biomarker study?
A5: A null finding of no mean group difference is a critically important result. It strongly suggests that the measured variable is not a universal biomarker for ASD as currently defined. This reinforces the heterogeneity hypothesis and should prompt investigation into whether the variable is relevant for a specific subset (e.g., those with a certain genetic background or cognitive profile) [35] [28]. Report such results to help the field refine its hypotheses.
Experimental Protocols for Heterogeneity-Aware Research
Protocol 1: Multimodal Data Acquisition for Subtyping
- Objective: To collect integrated data layers for identifying biologically coherent ASD subgroups.
- Methodology:
- Participant Characterization: Deep phenotyping using standardized tools (ADOS-2, ADI-R) plus measures of IQ, language, adaptive function (Vineland-3), and co-occurring conditions [35].
- Neuroimaging: Acquire structural and resting-state functional MRI. For EEG, use high-density systems (e.g., 128-channel) following the 10-20 system, recording during rest and task paradigms (e.g., face processing for N170) [59].
- Molecular Data: Collect DNA for whole-genome or whole-exome sequencing to identify rare and common variants [35]. Consider metabolomic or proteomic profiling from blood plasma [61].
- Data Integration: All data should be processed through standardized pipelines (e.g., EEGLAB/MNE for EEG, fMRIprep for MRI) and stored in a common format (BIDS) for integrated analysis [59].
Protocol 2: Machine Learning Pipeline for Biomarker Evaluation
- Objective: To assess the diagnostic and stratification utility of candidate biomarkers.
- Methodology:
- Feature Engineering: From processed data, extract relevant features (e.g., spectral power bands from EEG, functional connectivity matrices from fMRI, polygenic risk scores) [59].
- Model Training & Validation:
- For diagnostic classification: Train a model (e.g., Support Vector Machine, Random Forest) to distinguish ASD from TD using nested cross-validation. Report accuracy, sensitivity, specificity [59] [60].
- For stratification: Apply clustering algorithms to the ASD group's feature data. Validate cluster stability and clinical relevance by testing for differences in external measures (e.g., symptom severity, treatment outcome) across clusters.
- Interpretability: Use SHAP or LIME to interpret model decisions and identify which features drive classification or define clusters [59].
Table 1: Evidence of Heterogeneity in ASD Biomarker Research
| Evidence Type | Key Finding | Implication for "Average" | Source |
|---|---|---|---|
| Effect Size Distribution | 45-63% of autistic individuals fall within 1 SD of TD mean on various cognitive/EEG/MRI measures. | A significant group mean difference masks that the measure is not atypical for most individuals. | [28] |
| Temporal Trend | Effect sizes in case-control studies have decreased by up to 80% over 20 years. | Broadening diagnostic criteria increases heterogeneity, diluting mean differences. | [28] |
| Genetic Stratification | Individuals with de novo mutations have lower average IQ and higher epilepsy rates than those without. | Genetic subgroups have distinct average profiles; a grand mean is uninformative. | [35] |
| ML Performance | Machine learning models using multimodal data can achieve 82-99.2% classification accuracy. | Combining features to capture individual patterns outperforms reliance on single mean differences. | [59] |
Visualizations: Pathways and Workflows
Title: Overcoming the Average Fallacy with a Stratification Workflow
Title: Machine Learning Pipeline for Biomarker Discovery
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials & Tools for Heterogeneity-Focused ASD Research
| Item / Solution | Function & Relevance | Example/Note |
|---|---|---|
| High-Density EEG System | Captures detailed brain electrical activity. Critical for extracting spectral power, connectivity, and event-related potential (ERP) features like the N170 for ML analysis [59]. | Systems with 64-128 channels using the 10-20 placement system. |
| Standardized Analysis Pipelines (EEG) | Ensures reproducible preprocessing and feature extraction from complex EEG data, enabling large-scale comparisons. | EEGLAB, MNE-Python, FieldTrip [59]. |
| Multimodal Data Integration Platforms | Allows storage, management, and co-analysis of diverse data types (genetic, imaging, clinical) from large cohorts. | Brain Imaging Data Structure (BIDS), COINS, XNAT. |
| Clustering & ML Software Libraries | Provides algorithms for unsupervised subgroup discovery and supervised predictive modeling. | Scikit-learn (Python), Caret (R), PyTorch/TensorFlow for deep learning [59] [60]. |
| Genetic Sequencing Services | Identifies rare variants (de novo, CNVs) and common polymorphisms to define genetic subgroups linked to different phenotypic profiles [35]. | Whole-exome sequencing, whole-genome sequencing. |
| Deep Phenotyping Battery | A set of validated assessments to capture the multidimensional heterogeneity (cognition, language, behavior, adaptive function) for use as clustering variables or outcomes [35] [28]. | Includes IQ tests (WAIS/WISC), Vineland Adaptive Behavior Scales, specific psychiatric interviews. |
| Biosample Collection Kits | Standardized collection of biological material for molecular biomarker discovery (e.g., metabolomics, proteomics). | Blood collection tubes (PAXgene for RNA, EDTA for plasma), saliva kits. |
Troubleshooting Guides
Troubleshooting Guide 1: Addressing Small Sample Sizes
| Problem | Potential Causes | Solutions & Methodologies | Key Considerations |
|---|---|---|---|
| Low Statistical Power | - Inadequate sample size for effect size [62]- Limited access to clinical cohorts- High cost of data collection | - Perform a priori sample size calculation using tools like G*Power [62]- Use Cohen's standardized effect sizes (small d=0.2, medium d=0.5, large d=0.8) for estimation [62]- Conduct pilot studies to estimate variance and effect size [62] | - Small samples increase false negatives and challenge reproducibility [63] [62] |
| Irreproducible Gene Set Analysis | - High dimensionality of genomic data [63]- Arbitrary sample size selection [63] | - Use m replicate datasets of size 2×n via random sampling without replacement [63]- Apply multiple gene set analysis methods (PAGE, GAGE, ROAST, FRY, GSEA) for comparison [63] | - Results become more reproducible as sample size increases [63]- For >85% reproducibility, ≥20 samples per group often needed [63] |
| Limited Generalizability | - Narrow participant selection- Homogeneous samples | - Implement data harmonization across multiple sites [64]- Use computational methods to combine datasets from different sources [64] | - Multi-site collaborations essential for adequate sample sizes [64] |
Troubleshooting Guide 2: Overcoming Replication Issues
| Problem | Potential Causes | Solutions & Methodologies | Key Considerations |
|---|---|---|---|
| Low Biomarker Specificity | - Biomarkers associated with multiple neuropsychiatric conditions [18]- Pleiotropic genetic effects [18] | - Cross-disorder validation: Test biomarkers against other conditions (e.g., ADHD, anxiety) [18] [28]- Apply multivariable models that evaluate multiple biomarkers together [65] | - Elevated whole-blood serotonin exemplifies non-specific biomarkers also found in other conditions [18] |
| Heterogeneous Patient Populations | - Vast genotypic and phenotypic diversity in ASD [18] [28]- Variable penetrance and pleiotropy [18] | - Subgroup stratification using machine learning (e.g., XGBoost) with multimodal data [23]- Genotype-first approaches to study phenotypic variability [18] | - In 16p11.2 duplication studies, only a minority met ASD criteria despite known association [18] |
| Technical Variability | - Differences in assay protocols- Laboratory-specific effects | - Validate against held-out data and replicate in separate cohorts [64]- Assess test-retest reliability (target: >85%) [64] | - Even with significant biomarkers, most autistic people do not show atypicality on group-level metrics [28] |
Troubleshooting Guide 3: Improving Standardization
| Problem | Potential Causes | Solutions & Methodologies | Key Considerations |
|---|---|---|---|
| Preanalytical Variability | - Lack of standardized protocols for sample collection and processing [66]- Differences in sample handling | - Develop Standardized Operating Procedures (SOPs) for sample processing [66]- Create standardized preanalytical guidelines for blood-based biomarkers [66] | - Preanalytical processing is the largest source of variability in laboratory testing [66] |
| Site-Specific Effects in Neuroimaging | - Different MRI machines and vendors [64]- Variations in scan sequences and processing [64] | - Prospective harmonization of data collection before study begins [64]- Use computational harmonization methods for existing data [64] | - Site-specific effects can make data difficult to compare across studies [64] |
| Lack of Analytical Standardization | - Different statistical approaches across labs [67] [65]- Variable analytical pipelines | - Use multivariable models rather than univariate tests alone [65]- Implement Gene Set Enrichment Analysis (GSEA) for genomic biomarkers [65] | - Multivariable models provide more real-life estimates and decrease false positives from chance [65] |
Frequently Asked Questions (FAQs)
How can I determine the appropriate sample size for my autism biomarker study?
Perform a priori sample size calculation using statistical software like G*Power or OpenEpi. The process requires you to specify: (1) the statistical analysis to be applied, (2) acceptable precision levels, (3) study power (typically 80%), (4) confidence level (typically 95%), and (5) the magnitude of practical significance differences (effect size). For unknown effect sizes, use Cohen's conventions: small (d=0.2), medium (d=0.5), or large (d=0.8). For example, detecting a medium effect size with 80% power typically requires 128 total participants (64 per group) for a two-group comparison [62].
What are the most effective strategies for improving reproducibility in genomic biomarker studies?
Increase sample size systematically and use multiple gene set analysis methods. Research shows that gene set analysis results become more reproducible as sample size increases. To achieve >85% reproducibility of findings identified with large samples (e.g., 48 controls and 48 cases), you typically need at least 20 samples per group. Use methods like PAGE, GAGE, Camera, ROAST, and GSEA in parallel, as they show different reproducibility rates across sample sizes. For initial discovery, use replicate dataset generation by randomly selecting n samples from larger pools multiple times to validate findings [63].
How can we address the challenge of heterogeneity in autism biomarker research?
Employ multimodal data integration and subgroup stratification. Instead of seeking universal biomarkers, use machine learning approaches that combine neuroimaging, epigenetic, and behavioral data to identify more homogeneous subgroups. For example, studies integrating sensory profiles with brain imaging (thalamo-cortical connectivity) and epigenetic markers (AVPR1A methylation) have shown better classification accuracy than single-modality approaches. Focus on identifying biomarkers for specific clinical purposes (diagnostic, prognostic, predictive) rather than seeking one-size-fits-all solutions [18] [23] [28].
What standardization procedures are critical for biomarker studies?
Develop standardized protocols for preanalytical processing, data collection, and analysis. For blood-based biomarkers, establish standardized operating procedures for sample collection, processing, and storage. For neuroimaging, implement prospective harmonization of MRI protocols across sites or use computational harmonization methods for existing data. Analytically, use multivariable models rather than univariate tests alone, as they better account for interactions between biomarkers and decrease false positive rates. Report detailed methodological information to enable cross-validation across cohorts and laboratories [64] [66] [65].
How can we improve the clinical translation of autism biomarkers?
Validate biomarkers for specific contexts of use rather than general diagnosis. Develop biomarkers with clear clinical applications: likelihood (early detection), diagnostic, prognostic, or predictive (treatment response). Follow the FDA-NIH BEST Resource guidelines, which emphasize "fit-for-purpose" validation. Use machine learning approaches that integrate minimal modalities for simplicity and interpretability. Most importantly, ensure diverse training data that captures the heterogeneity of the autistic population to avoid biased models [64] [28].
Experimental Protocols & Workflows
Protocol 1: Multimodal Biomarker Integration for ASD Subgroup Identification
This protocol outlines the methodology from a recent study that successfully integrated sensory behavior, brain imaging, and epigenetic factors to classify ASD with improved accuracy [23].
Sample Requirements: Minimum 105 participants (based on power analysis for 30 predictors, effect size f²=0.3, α=0.05, power=0.8) [23]
Methodology:
- Behavioral Assessment: Administer Adolescent-Adult Sensory Profile (AASP) questionnaire characterizing four sensory patterns: Low Registration, Sensitivity, Sensation Seeking, and Avoidance [23]
- Brain Imaging Acquisition:
- Acquire structural MRI using T1-weighted parameters: TR=6.38ms, TE=1.99ms, flip angle=11°, voxel size=1×1×1mm³
- Acquire resting-state fMRI using T2*-weighted EPI: TR=2000ms, TE=24ms, flip angle=80°, voxel size=3×3mm², 180 volumes [23]
- Epigenetic Analysis:
- Collect saliva samples for DNA methylation analysis
- Compute DNA methylation values of OXTR, AVPR1A, and AVPR1B genes [23]
- Data Processing:
- Process structural MRI with FreeSurfer for cortical and subcortical segmentation
- Preprocess fMRI data using SPM12-based CONN toolbox, including realignment, slice-timing correction, noise reduction, normalization, and band-pass filtering (0.01-0.08Hz)
- Calculate thalamo-cortical functional connectivity using seed-to-voxel analysis with bilateral thalamus as ROIs [23]
- Machine Learning Classification:
- Apply eXtreme Gradient Boosting (XGBoost) algorithm
- Compare three models: neuroimaging-epigenetic model, neuroimaging-only model, and epigenetic-only model
- Use sensory behavior measures as default baseline [23]
Protocol 2: Cross-Site Neuroimaging Data Harmonization
This protocol provides methodology for harmonizing neuroimaging data across multiple clinical sites to increase sample size and generalizability [64].
Workflow:
- Prospective Harmonization (before data collection):
- Standardize MRI scanner platforms and sequences across sites
- Implement identical acquisition parameters and procedures
- Establish common participant positioning protocols
- Use standardized phantoms for quality control [64]
Retrospective Harmonization (for existing data):
- Apply computational methods to remove site-specific technical variance
- Use batch effect correction algorithms
- Implement ComBat or similar harmonization tools
- Preserve biological variability while removing methodological artifacts [64]
Quality Control:
- Regular phantom scans across sites
- Monitoring of signal-to-noise ratio and contrast-to-noise ratio
- Assessment of temporal stability
- Visual inspection for artifacts [64]
Research Reagent Solutions
| Item | Function/Application | Example Use in ASD Biomarker Research |
|---|---|---|
| Adolescent-Adult Sensory Profile (AASP) | Self-report questionnaire characterizing four sensory processing patterns: Low Registration, Sensitivity, Sensation Seeking, and Avoidance [23] | Provides behavioral baseline for multimodal biomarker integration; characterizes sensory abnormalities included in DSM-5 ASD criteria [23] |
| FreeSurfer Software | Automated structural MRI processing for cortical and subcortical segmentation and parcellation [23] | Quantifies brain structural characteristics (cortical thickness, subcortical volume) as potential ASD biomarkers [23] |
| CONN Toolbox | Functional connectivity software for resting-state fMRI preprocessing and analysis [23] | Calculates thalamo-cortical functional connectivity; identifies hyperconnectivity patterns associated with ASD [23] |
| DNA Methylation Analysis Kits | Quantify epigenetic modifications in candidate genes (OXTR, AVPR1A, AVPR1B) from saliva or blood samples [23] | Measures epigenetic biomarkers associated with ASD; AVPR1A hypomethylation identified as significant contributor in classification models [23] |
| XGBoost Algorithm | Machine learning method for classification and regression using gradient boosting framework [23] | Integrates multimodal data (behavior, brain, epigenetics) for ASD classification; identifies significant feature contributions [23] |
| Gene Set Enrichment Analysis (GSEA) | Statistical method for interpreting gene expression data by evaluating coordinated changes in predefined gene sets [65] | Identifies pathways associated with biological processes in genomic biomarker discovery; helps prioritize biomarkers for validation [65] |
Autism Spectrum Disorder (ASD) is characterized by significant heterogeneity in etiology, presentation, and outcomes, creating substantial challenges for biomarker development [14] [35]. This variability means that no single biomarker can capture the full spectrum of the condition, requiring researchers to confront heterogeneity through sophisticated study designs and multimodal approaches [68] [35]. The saying in the field that "if you've met one child with autism... you've met one child with autism" underscores this diversity [68]. Research indicates that different genetic profiles, such as those with de novo mutations versus common variants, present with different clinical features including varying IQ levels and epilepsy comorbidity, further illustrating the biological complexity researchers must account for [35]. Successfully addressing these challenges is crucial for developing reliable biomarkers that can improve diagnosis, enable earlier intervention, and facilitate more targeted treatments for ASD [68].
Troubleshooting Guide: Common Experimental Issues and Solutions
FAQ: Addressing Key Experimental Challenges
Q: How can I improve the specificity of a candidate biomarker to ensure it is not affected by general neurodevelopmental differences? A: To enhance specificity, strategically incorporate comparison groups that account for broader neurodevelopmental conditions. During analysis, employ statistical methods like receiver operating characteristic (ROC) curves to calculate relative true and false positive rates, comparing your biomarker's performance against these control groups [69]. This approach helps determine whether your biomarker is specific to ASD rather than general neurodevelopmental disruption.
Q: Our team is finding inconsistent biomarker results across our cohort. How can we address heterogeneity-related variability? A: Inconsistent results often reflect the inherent biological heterogeneity of ASD. Instead of treating your cohort as a single group, implement subgrouping strategies based on objective measures such as cognitive ability (IQ), language profiles, or genetic markers [35]. Additionally, adopt multimodal approaches that combine different biomarker types (e.g., neuroimaging and epigenetic markers), as integrated models have demonstrated superior classification accuracy compared to single-method approaches [14].
Q: What is the most critical factor in preventing pre-analytical errors in biomarker studies? A: Temperature regulation during sample handling is paramount, particularly for nucleic acids and proteins. Implement standardized protocols for immediate flash freezing, controlled thawing, and maintaining consistent cold chain logistics [70]. Studies indicate that pre-analytical errors account for approximately 70% of laboratory diagnostic mistakes, with temperature sensitivity being a major factor [70].
Q: How can we reduce human error in biomarker data processing? A: Implement automation solutions for repetitive tasks such as sample homogenization and preparation. One clinical genomics lab reported an 88% decrease in manual errors after automating their next-generation sequencing sample preparation workflow [70]. Additionally, establish clear standard operating procedures (SOPs) and implement double-checking systems for critical steps [70].
Q: Our epigenetic biomarkers show variability between sample batches. How can we improve reproducibility? A: Focus on contamination control and standardized sample preparation. Use automated homogenization systems with single-use consumables to eliminate cross-sample contamination [70]. For epigenetic work specifically, ensure consistent DNA methylation protocols by using validated reagents and implementing rigorous quality control checkpoints at each processing stage [14] [70].
Common Laboratory Errors and Rectification Strategies
Table 1: Frequent Laboratory Issues Impacting Biomarker Data Reliability
| Error Category | Specific Issue | Impact on Data | Rectification Strategy |
|---|---|---|---|
| Sample Handling | Temperature fluctuations during storage/processing | Biomarker degradation (proteins/nucleic acids) | Implement standardized cold chain protocols; use automated temperature monitoring [70] |
| Sample Processing | Inconsistent homogenization techniques | Introduces variability; affects downstream analysis | Adopt automated homogenization systems (e.g., Omni LH 96) [70] |
| Data Management | Manual data entry and transcription errors | Incorrect data associations and conclusions | Implement barcode systems; use electronic lab notebooks; one institution reduced slide mislabeling by 85% with barcoding [70] |
| Procedure Complexity | Multi-step protocol variability | Batch-to-batch inconsistencies; irreproducible results | Break complex procedures into managed steps; implement competency assessments [70] |
| Workplace Factors | Cognitive fatigue during extended procedures | Decreased cognitive function (up to 70%) affecting precision | Implement structured break schedules; manage cognitive load [70] |
Experimental Protocols for Robust Autism Biomarker Discovery
Multimodal Biomarker Integration Protocol
Objective: To develop a classification model for ASD that integrates neuroimaging and epigenetic biomarkers to address heterogeneity [14].
Materials:
- 3T MRI scanner with structural and resting-state functional MRI capabilities
- DNA methylation analysis reagents (e.g., bisulfite conversion kits)
- Saliva collection kits for epigenetic analysis
- Adolescent-Adult Sensory Profile (AASP) questionnaire [14]
Methodology:
- Participant Recruitment and Characterization:
- Recruit participants meeting DSM-5 criteria for ASD and age/IQ-matched typically developing controls
- Administer AASP questionnaire to characterize sensory-related behaviors
- Collect demographic and clinical data including age, sex, and full-scale IQ [14]
Neuroimaging Data Acquisition:
- Acquire high-resolution T1-weighted structural MR data using parameters: repetition time (TR) = 6.38 ms, echo time (TE) = 1.99 ms, flip angle (FA) = 11°, field of view (FoV) = 256 mm, matrix = 256 × 256, slice number = 172, voxel dimension = 1 × 1 × 1 mm³ [14]
- Acquire blood-oxygen-level-dependent (BOLD) contrast resting-state fMRI scans using T2-weighted gradient-echo planar imaging sequence
- Process structural data to measure cortical and subcortical volume
- Calculate thalamo-cortical resting-state functional connectivity (rs-FC) from fMRI data [14]
Epigenetic Analysis:
- Collect saliva samples from all participants
- Extract genomic DNA using standardized protocols
- Perform DNA methylation analysis for target genes (OXTR, AVPR1A, AVPR1B)
- Compute DNA methylation values using appropriate bioinformatics pipelines [14]
Data Integration and Machine Learning:
- Develop three separate models using the XGBoost algorithm [16]:
- Neuroimaging-epigenetic model (integrating behavior, brain, and epigenetic factors)
- Neuroimaging model (behavior and brain factors only)
- Epigenetic model (behavior and epigenetic factors only)
- Use sensory-related behavior measures as the default baseline
- Compare model performance to test the hypothesis that the integrated neuroimaging-epigenetic model outperforms single-modality models [14]
- Develop three separate models using the XGBoost algorithm [16]:
Expected Outcomes: This protocol should yield a classification model with superior accuracy, with thalamo-cortical hyperconnectivity and AVPR1A epigenetic modification expected to be significant contributing factors [14].
Prospective-Specimen-Collection, Retrospective-Blinded-Evaluation (PRoBE) Design
Objective: To eliminate common biases in biomarker research through a rigorous study design appropriate for diagnostic, screening, and prognostic markers [71].
Materials:
- Biological specimen collection and storage infrastructure
- Clinical data management system
- Blinded laboratory analysis capabilities
Methodology:
- Cohort Definition:
- Define target population and clinical setting for intended biomarker use
- Establish inclusion/exclusion criteria representing heterogeneous ASD population
- Enroll subjects from multiple institutions to ensure generalizability [71]
Prospective Specimen Collection:
- Collect and store biological specimens before outcome ascertainment
- Collect pertinent clinical data using standardized protocols
- Ensure specimen collection occurs in absence of knowledge about patient outcome [71]
Outcome Ascertainment:
- Define outcome of interest (e.g., ASD diagnosis, symptom severity)
- Implement rigorous procedures for outcome measurement
- Categorize subjects as case patients (ASD) or control subjects (typically developing) after outcome data available [71]
Retrospective Blinded Evaluation:
- Randomly select case patients and control subjects from cohort
- Retrieve specimens from storage
- Perform biomarker assays blinded to case-control status [71]
Analysis:
- Calculate true positive rate (TPR) and false positive rate (FPR)
- Evaluate whether biomarker meets pre-specified performance criteria
- Assess performance in relevant subgroups to address heterogeneity [71]
Quality Control Considerations: This design eliminates common biases by prospectively collecting specimens from a well-defined cohort before outcome status is known, then performing blinded biomarker analysis on randomly selected cases and controls [71].
Essential Research Reagent Solutions
Table 2: Key Research Reagents and Materials for Autism Biomarker Discovery
| Reagent/Material | Specific Function | Application Notes |
|---|---|---|
| DNA Methylation Analysis Kits | Bisulfite conversion of DNA for epigenetic analysis | Critical for analyzing methylation patterns in OXTR, AVPR1A genes; use validated kits for consistency [14] [72] |
| Saliva Collection Kits | Non-invasive DNA collection for epigenetic studies | Preserve sample integrity for methylation analysis; maintain cold chain during storage/transport [14] [70] |
| MRI Contrast Agents | Enhance structural and functional imaging resolution | Essential for detailed volumetric and connectivity analyses; use standardized protocols across sites [14] |
| EEG Electrode Systems | Record electrical brain activity in real-time | 128-electrode systems for high-density recording; enables study of neural processing patterns in ASD [68] |
| Automated Homogenization Systems | Standardize sample preparation | Systems like Omni LH 96 reduce contamination and variability; particularly valuable for high-throughput workflows [70] |
| Quality Control Biomarkers | Monitor assay performance and sample quality | Include internal controls for methylation assays; verify sample integrity pre-analysis [70] |
Visualizing Experimental Workflows and Conceptual Relationships
Multimodal Biomarker Integration Workflow
PRoBE Study Design Implementation
Biomarker Validation Pathway
The Researcher's Troubleshooting Guide
This guide addresses common experimental challenges in autism biomarker discovery, framed within the new paradigm of stratification.
FAQ: Why is my candidate biomarker not replicating across different cohorts?
- Issue: A promising biomarker fails to validate in a new, independent sample of participants.
- Diagnosis: This is a classic symptom of ASD heterogeneity. Your initial cohort likely represented a specific biological subgroup, and the new cohort contains a different mix of subtypes, diluting the effect [73] [57].
- Solution: Shift from case-control designs to stratification approaches. Re-analyze your data using unsupervised machine learning (e.g., clustering) to identify data-driven subgroups within your cohort. Test if your biomarker is robust within one or more of these specific subgroups [74].
FAQ: How can I account for the overwhelming genetic heterogeneity in ASD?
- Issue: Thousands of genes are associated with ASD, making it difficult to find common biological pathways [40].
- Diagnosis: Focusing solely on genetic etiology may obscure convergent downstream mechanisms.
- Solution: Implement multi-omics integration. As demonstrated in one study, plasma proteomic and metabolomic profiles can reveal common pathways—such as inflammation, immune response, and amino acid metabolism—even across children with and without identified de novo mutations [40]. The table below summarizes key findings from such an approach.
Table 1: Common Pathways Identified Despite Genetic Heterogeneity
| Analysis Level | Common Identified Mechanisms | Potential Biomarker Examples |
|---|---|---|
| Proteomics | Complement system, inflammation & immunity, cell adhesion [40] | Differentially expressed proteins distinguishing ASD from controls [40] |
| Metabolomics | Amino acid, vitamin, glycerophospholipid, and glutamate metabolic pathways [40] | L-glutamic acid, malate dehydrogenase [40] |
FAQ: My neuroimaging results are inconsistent with the literature. What steps should I take?
- Issue: Significant brain structural or functional findings from one study do not align with those from another.
- Diagnosis: Group-averaging in neuroimaging can mask the distinct neural subtypes that exist within ASD [74].
- Solution: Employ a neurosubtyping framework. Use techniques like clustering on brain imaging data to parse the heterogeneous study population into more homogeneous neurosubtypes [74]. The following workflow illustrates this process.
Experimental Protocols for Stratification Biomarker Discovery
Here are detailed methodologies for key experiments cited in the troubleshooting guide.
Protocol 1: Integrating Neuroimaging and Epigenetics for Classification
This protocol is based on a study that successfully classified ASD by integrating brain and epigenetic factors with sensory behaviors [23].
- Participant Characterization: Recruit participants with ASD and typically developing (TD) controls, matched for age and IQ. Diagnoses should be confirmed using standardized tools like the DSM-5 and DISCO [23].
- Behavioral Assessment: Administer the Adolescent/Adult Sensory Profile (AASP) questionnaire to characterize sensory processing patterns (Low Registration, Sensitivity, Seeking, Avoiding) as a behavioral baseline [23].
- Brain Data Acquisition & Preprocessing:
- Acquisition: Acquire high-resolution T1-weighted structural and resting-state functional MRI (rs-fMRI) scans on a 3T scanner [23].
- Structural Processing: Process T1 images using FreeSurfer for subcortical segmentation and cortical parcellation [23].
- Functional Processing: Preprocess rs-fMRI data (realignment, slice-timing correction, normalization, smoothing). Perform seed-to-voxel analysis using the bilateral thalamus as the seed region to compute thalamo-cortical resting-state functional connectivity (rs-FC) [23].
- Epigenetic Data Collection:
- Sample Collection: Collect saliva from participants.
- DNA Methylation Analysis: Extract DNA and perform methylation analysis for candidate genes (e.g., OXTR, AVPR1A, AVPR1B) [23].
- Machine Learning Classification:
- Model Building: Use the XGBoost algorithm to build three models: a Neuroimaging model (AASP + brain factors), an Epigenetic model (AASP + epigenetic factors), and a combined Neuroimaging-Epigenetic model [23].
- Evaluation: Compare the predictive accuracy of the three models. The study found that the combined model outperformed the others, with thalamo-cortical hyperconnectivity and AVPR1A methylation being significant contributors [23].
Protocol 2: A Multi-Omics Approach to Find Common Pathways
This protocol outlines how to discover shared biological mechanisms across genetically heterogeneous ASD groups [40].
- Cohort Formation and Genetic Testing: Create three groups: ASD with a identified risk gene (ASDM), ASD without an identified risk gene (ASDnM), and healthy controls (CTR). Identify de novo mutations via whole-exome sequencing [40].
- Plasma Proteomics:
- Sample Prep & Analysis: Isolate plasma from blood samples. Analyze using techniques like SWATH mass spectrometry for high-throughput protein identification and quantification [40].
- Data Analysis: Perform multivariate statistical analysis (PCA, PLS-DA) to visualize group clustering. Identify Differentially Expressed Proteins (DEPs) between the combined ASD group and controls [40].
- Plasma Metabolomics:
- Integrated Pathway Analysis: Input the lists of DEPs and differential metabolites into pathway analysis tools (e.g., KEGG, MetaboAnalyst) to identify significantly enriched biological pathways common to both ASDM and ASDnM groups [40].
The Scientist's Toolkit
Table 2: Key Research Reagent Solutions
| Item / Reagent | Function in Research |
|---|---|
| Adolescent/Adult Sensory Profile (AASP) | A self-report questionnaire to quantify behavioral responses to sensory stimuli, providing a crucial behavioral baseline for stratification [23]. |
| Verasonics Vantage Research Ultrasound | A programmable ultrasound platform used in novel techniques like quantitative High-Definition Microvessel Imaging to quantify in vivo microvascular morphology [75]. |
| SWATH Mass Spectrometry | A data-independent acquisition (DIA) proteomics method for comprehensive identification and quantification of thousands of proteins from plasma samples [40]. |
| DNA Methylation Assay Kits | Used to measure epigenetic modifications (e.g., on OXTR, AVPR1A genes) from saliva or blood, linking molecular changes to brain and behavior [23]. |
Conceptual Roadmap for Stratification Research
The future of ASD biomarker discovery lies in integrating multiple data types to move beyond simple diagnoses and into biologically informed subtypes. The following diagram maps the logical relationship between data types, analytical frameworks, and the ultimate goal of precision medicine.
FAQs: Addressing Heterogeneity in Autism Biomarker Discovery
Q1: How can I design a study to account for the significant heterogeneity in Autism Spectrum Disorder (ASD)?
A person-centered approach that groups individuals based on their combinations of traits is recommended over searching for genetic links to single traits. A recent large-scale study analyzed over 230 traits per individual—from social interactions to developmental milestones—to identify biologically distinct subtypes [9]. This method allows you to connect different clinical presentations to distinct underlying genetic profiles, which is foundational for precision medicine [9].
Q2: What is an intensive longitudinal design and why is it useful for clinical psychology research?
Intensive longitudinal designs assess within-person, dynamic processes in naturalistic contexts in near real-time [76]. They are powerful for capturing how symptoms and behaviors fluctuate over time. When implementing these designs, you must plan for specific considerations such as statistical power, sample size, participant attrition, optimal sampling frequency, and the psychometric properties of frequent measurements [76].
Q3: How can I integrate different data types, like brain imaging and genetics, to improve biomarker discovery?
Combine multiple data modalities within a machine-learning framework. One study created a neuroimaging-epigenetic model that integrated brain structural/functional data with DNA methylation markers, using sensory-related behavior as a baseline [14]. This model outperformed models using only neuroimaging or epigenetic data. Thalamo-cortical resting-state connectivity and arginine vasopressin receptor (AVPR1A) epigenetic modification were identified as significant contributing factors [14].
Q4: What are some key biomarkers currently being investigated for ASD?
Research is exploring a wide variety of biomarkers, which can be categorized as follows [16]:
- Biochemical & Hormonal: Elevated serum serotonin, decreased oxytocin.
- Immunological: Abnormal immune system responses.
- Metabolic: Oxidative stress, amino acid metabolism imbalances, mitochondrial dysfunction.
- Epigenetic: DNA methylation patterns, histone modifications.
Q5: What statistical methods are appropriate for analyzing longitudinal data?
For data where participants are followed over multiple time points, several analytical frameworks are available [77]:
- Multilevel Growth Models (HLM): Ideal for analyzing whether and how change occurs over time, and for assessing the impact of covariates at different levels (e.g., within-student and between-school effects).
- Survival Models: Used to analyze the timing of when a specific event occurs.
- Cross-Lagged Models: Useful for addressing issues of causality in longitudinal research by examining reciprocal relationships over time.
Experimental Protocols & Methodologies
Protocol 1: A Machine Learning Workflow for Biomarker Integration
This protocol is adapted from a study that successfully classified ASD by integrating neuroimaging and epigenetic data with behavioral baselines [14].
- Participant Recruitment & Phenotyping: Recruit participants with ASD and typically developing (TD) controls. Administer standardized behavioral assessments. The cited study used the Adolescent-Adult Sensory Profile (AASP) questionnaire and ensured clinicians confirmed diagnoses [14].
- Data Acquisition:
- Neuroimaging: Acquire structural and resting-state functional MRI (rs-fMRI) scans. Key is to measure thalamo-cortical resting-state functional connectivity (rs-FC) [14].
- Epigenetic Data Collection: Collect saliva samples. Isolate DNA and perform analysis for DNA methylation of candidate genes like
OXTRandAVPR1A[14].
- Data Processing & Feature Extraction:
- Process rs-fMRI data to calculate rs-FC between the thalamus and cortical regions (e.g., prefrontal cortex, superior temporal gyrus).
- Process genetic data to compute DNA methylation values for the target genes.
- Model Development & Testing: Use a machine learning algorithm (e.g., XGBoost) to build and test different models:
- A neuroimaging-epigenetic model (combining all data).
- A neuroimaging-only model.
- An epigenetic-only model. Compare their predictive accuracies to determine if the integrated model provides a superior classification of ASD [14].
Protocol 2: Implementing an Intensive Longitudinal Design
This protocol outlines key steps for setting up a robust intensive longitudinal study, based on best practices for clinical psychology research [76].
- Power and Sample Size Planning: Conduct a power analysis that accounts for the number of repeated measurements and the expected attrition rate. Use specialized software or packages (e.g., the
pwrpackage in R) designed for multilevel and intensive longitudinal designs [76] [14]. - Sampling Design: Decide on the frequency and duration of assessments (e.g., daily diaries, multiple measurements per day) based on the research question and the dynamic nature of the constructs being measured.
- Participant Engagement & Retention: Implement strategies to predict and mitigate attrition. This can include:
- Compensating participants fairly for their time.
- Sending regular reminders.
- Maintaining communication about the study's progress.
- Data Quality and Analysis:
- Plan for assessing data quality upon collection.
- Examine the psychometric properties of your measures in the context of frequent administration.
- Pre-specify your analytical plan, which will likely involve multilevel growth models or similar techniques to handle nested data [77].
Data Presentation
Table 1: Data-Driven Subtypes of Autism and Their Characteristics
This table summarizes the four clinically and biologically distinct subtypes of autism identified in a 2025 study, providing a framework for reducing heterogeneity in research [9].
| Subtype Name | Approximate Prevalence | Key Clinical Traits | Genetic Profile |
|---|---|---|---|
| Social and Behavioral Challenges | 37% | Core autism traits; typical developmental milestones; often has co-occurring conditions (ADHD, anxiety, depression) [9]. | Mutations in genes active later in childhood [9]. |
| Mixed ASD with Developmental Delay | 19% | Later achievement of developmental milestones (e.g., walking, talking); generally lacks co-occurring anxiety/depression [9]. | High proportion of rare, inherited genetic variants [9]. |
| Moderate Challenges | 34% | Milder core autism traits; reaches developmental milestones on a typical track; few co-occurring psychiatric conditions [9]. | Information missing from source. |
| Broadly Affected | 10% | Severe, wide-ranging challenges including developmental delays, social difficulties, and co-occurring psychiatric conditions [9]. | Highest proportion of damaging de novo (non-inherited) mutations [9]. |
Table 2: Categories of Biomarkers in Autism Research
This table lists key categories of biomarkers under investigation for the early diagnosis and understanding of ASD [16].
| Biomarker Category | Example Molecules/Factors | Proposed Role in ASD |
|---|---|---|
| Biochemical & Hormonal | Serotonin (5-HT), Oxytocin | Elevated serum serotonin; decreased oxytocin levels linked to social challenges [16]. |
| Immunological | Cytokines, Immunoglobulins | Associated with abnormal immune system responses and inflammation [16]. |
| Metabolic | Markers of Oxidative Stress, Amino Acids | Implicated in oxidative stress, imbalances in amino acid metabolism, and mitochondrial dysfunction [16]. |
| Epigenetic | DNA Methylation (e.g., of OXTR, AVPR1A), Histone Modifications |
Altered gene expression patterns in brain-related pathways without changing the underlying DNA sequence [14] [16]. |
Diagrams
The Scientist's Toolkit
Table 3: Research Reagent Solutions for Key Experiments
| Item | Function/Application |
|---|---|
| Adolescent-Adult Sensory Profile (AASP) | A self-report questionnaire used to characterize behavioral abnormalities in response to sensory inputs, providing a key behavioral baseline for studies [14]. |
| DNA Methylation Analysis Kits | Used to process saliva or other tissue samples to compute DNA methylation values for candidate genes (e.g., OXTR, AVPR1A) [14] [16]. |
| Resting-state fMRI (rs-fMRI) | A functional neuroimaging technique to measure blood-oxygen-level-dependent (BOLD) contrast at rest, used to calculate thalamo-cortical functional connectivity [14]. |
| Multilevel Growth Model Software (HLM/R packages) | Statistical software and packages capable of performing multilevel growth modeling (hierarchical linear modeling) to analyze longitudinal data with nested structures [77]. |
| XGBoost Algorithm | A machine learning algorithm based on gradient boosting, useful for classification and identifying meaningful features from complex, integrated datasets [14]. |
From Bench to Bedside: Validating Subtypes and Comparative Clinical Translation
Validating and Replicating Phenotypic Classes in Independent Cohorts
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary methodological consideration when attempting to validate phenotypic classes in a new cohort?
The foremost consideration is ensuring phenotypic compatibility between your discovery and validation cohorts. The initial study identified classes using 239 item-level and composite features from standard diagnostic questionnaires, including the Social Communication Questionnaire-Lifetime (SCQ), Repetitive Behavior Scale-Revised (RBS-R), and Child Behavior Checklist (CBCL) [78] [79]. When applying this model to an independent cohort like the Simons Simplex Collection (SSC), you must map a comparable set of features—the study successfully replicated its findings using 108 matched features available in both the SPARK and SSC cohorts [78]. A generative mixture model trained on the original data can then be applied to the new dataset to test for class stability and clinical relevance.
FAQ 2: Our replication attempt yielded different class proportions. Does this indicate a failure?
Not necessarily. Differences in class proportions between cohorts can arise from legitimate variations in recruitment strategies, demographic compositions, or clinical assessment methods. The key metric of successful replication is the preservation of the core phenotypic profile of each class—the specific pattern of strengths and difficulties across the seven core categories (e.g., limited social communication, developmental delay, anxiety/mood) [78] [79]. For example, the "Mixed ASD with DD" class should consistently show strong enrichment in developmental delays and lower levels of ADHD and anxiety, regardless of its relative size in the population [9].
FAQ 3: Beyond behavioral phenotypes, what external clinical data can validate the biological meaningfulness of the classes?
External medical history, not used in the original model training, provides powerful orthogonal validation. You should analyze enrichment patterns of clinically diagnosed co-occurring conditions. For instance, the "Broadly Affected" class was significantly enriched in almost all measured co-occurring conditions, while the "Social/Behavioral" class showed specific enrichment for ADHD, anxiety, and major depression [78] [9]. Additional validating factors include the age of diagnosis (earlier in classes with developmental delays), levels of cognitive impairment and language ability, and the average number of interventions per child [78].
FAQ 4: What genetic evidence supports the distinctness of these phenotypic classes?
The classes exhibit distinct underlying genetic architectures. Analyses reveal:
- Variant Type Burden: The "Broadly Affected" class carries the highest burden of damaging de novo mutations, while the "Mixed ASD with DD" class is uniquely enriched for rare inherited variants [9].
- Polygenic Scores: Patterns in common genetic variation, measured by polygenic scores, align with the phenotypic and diagnostic traits of the different classes [79].
- Biological Pathways: The sets of genes disrupted by mutations in each class point to divergent biological pathways and processes [9].
- Developmental Timing: Genes affected in the "Social and Behavioral Challenges" subtype (which has later diagnosis and no developmental delays) become active later in childhood, suggesting a post-natal biological mechanism [9].
Troubleshooting Guides
Problem: Poor class separation or low model confidence in the replication cohort.
- Potential Cause 1: Incomplete Feature Matching.
- Solution: Conduct a thorough audit of the phenotypic instruments used in your validation cohort. Create a detailed crosswalk to map items to the 239 original features. If direct matches are unavailable, consult with clinical experts to determine if composite scores or proxy items are valid substitutes.
- Potential Cause 2: Cohort-Specific Biases.
- Solution: Compare the basic demographics (e.g., age, sex distribution, intellectual ability) of your cohort against the original SPARK cohort. If significant biases are found, consider stratification or covariate adjustment in your analysis. The original study found the classes were robust across sex and age distributions, providing a baseline for comparison [78].
- Potential Cause 3: Inappropriate Model Application.
- Solution: Instead of just applying the pre-trained model, try independently training a new generative finite mixture model (GFMM) on your cohort's data. Then, compare the emergent class profiles and their enrichment patterns to those from the original study to see if the same patterns arise organically [78].
Problem: One class replicates well, but others are indistinct or absent.
- Potential Cause: Recruitment or Ascertainment Bias.
- Solution: Certain cohorts may be systematically over- or under-enriched for specific subtypes. For example, a cohort recruited from psychiatric services might over-represent the "Social/Behavioral" class, while a cohort focused on developmental pediatrics might over-represent the "Mixed ASD with DD" class. Acknowledge this as a limitation and report the class profiles that are present with high confidence.
Experimental Protocols
Protocol 1: Cross-Cohort Phenotypic Validation
Objective: To validate the four autism phenotypic classes in an independent cohort. Materials:
- Dataset from independent cohort (e.g., Simons Simplex Collection) with phenotypic data.
- Pre-trained Generative Finite Mixture Model (GFMM) from the original study [78].
- Statistical software (e.g., R, Python).
Methodology:
- Data Harmonization: Identify and extract a set of phenotypic features in your validation cohort that directly correspond to the 108 features used in the successful replication study [78].
- Model Application: Apply the pre-trained GFMM to the harmonized dataset to assign each individual a probabilistic class membership.
- Profile Validation: For each assigned class, calculate the mean scores across the seven phenotypic categories (limited social communication, restricted behavior, attention, disruptive behavior, anxiety/mood, developmental delay, self-injury). Compare these profiles to the original patterns using statistical tests (e.g., Cohen's d for effect size).
- External Clinical Validation: Using data not included in the model, test for expected enrichments in co-occurring conditions, cognitive impairment, and age of diagnosis, as detailed in the table of clinical attributes below.
Protocol 2: Genetic Validation of Phenotypic Classes
Objective: To test for distinct genetic patterns across the validated phenotypic classes. Materials:
- Genomic data (e.g., whole exome or genome sequencing) for individuals in the validation cohort.
- Annotation databases for de novo and rare inherited variants.
- Polygenic score calculations for relevant psychiatric traits.
Methodology:
- Variant Burden Analysis: For each phenotypic class, calculate the burden of:
- Likely Gene Disrupting (LGD) de novo mutations.
- Rare inherited variants (e.g., <1% frequency in control populations).
- Compare burden rates between classes using regression models, controlling for relevant covariates like ancestry.
- Polygenic Score Analysis: Calculate polygenic scores for traits like educational attainment, ADHD, and schizophrenia. Test for differences in the distribution of these scores across the phenotypic classes [79].
- Pathway Enrichment: For genes harboring damaging mutations within a specific class, perform gene set enrichment analysis to identify overrepresented biological pathways (e.g., synaptic function, chromatin remodeling) [9].
Data Presentation
Table 1: Clinical and Demographic Profiles of the Four Autism Phenotypic Classes
| Phenotypic Class | Prevalence in SPARK | Core Phenotypic Features | Enriched Co-occurring Conditions | Age of Diagnosis & Intervention |
|---|---|---|---|---|
| Social/Behavioral | 37% (n=1,976) | High core autism traits; No developmental delays; Elevated disruptive behavior, attention, and anxiety. | ADHD, Anxiety, Major Depression, OCD [9] | Later diagnosis; High number of interventions [78] |
| Mixed ASD with Developmental Delay (DD) | 19% (n=1,002) | Nuanced social/restricted behavior profile; Strong enrichment of developmental delays. | Language Delay, Intellectual Disability, Motor Disorders [78] | Early diagnosis; Lower levels of ADHD/anxiety [78] |
| Moderate Challenges | 34% (n=1,860) | Consistently lower scores across all seven difficulty categories. | Generally does not experience co-occurring psychiatric conditions [9] | Later diagnosis; Lowest number of interventions [78] |
| Broadly Affected | 10% (n=554) | Consistently high scores across all seven difficulty categories. | Wide range, including intellectual disability, language delay, ADHD, anxiety [78] | Early diagnosis; Highest number of interventions [78] |
Table 2: Genetic Correlates of the Four Autism Phenotypic Classes
| Phenotypic Class | De Novo Mutation Burden | Rare Inherited Variant Burden | Distinct Biological Features |
|---|---|---|---|
| Social/Behavioral | --- | --- | Mutations in genes active later in childhood, aligning with later clinical presentation [9] |
| Mixed ASD with DD | Not Enriched | Enriched [9] | Associated with specific, yet-to-be-defined inherited pathways |
| Moderate Challenges | Information Not Specified in Search Results | Information Not Specified in Search Results | Information Not Specified in Search Results |
| Broadly Affected | Highest Proportion [9] | Not Enriched | Divergent biological processes and pathways affected |
Research Reagent Solutions
Table 3: Essential Materials and Tools for Replication Studies
| Item Name | Function/Description | Example from Source Study |
|---|---|---|
| Social Communication Questionnaire (SCQ) | Diagnostic questionnaire assessing social and communication skills. | One of three core questionnaires used to define the 239 phenotypic features [78]. |
| Repetitive Behavior Scale-Revised (RBS-R) | Diagnostic questionnaire quantifying repetitive and stereotyped behaviors. | One of three core questionnaires used to define the 239 phenotypic features [78]. |
| Child Behavior Checklist (CBCL) | A comprehensive checklist assessing a wide range of behavioral and emotional problems. | One of three core questionnaires used to define the 239 phenotypic features [78]. |
| Generative Finite Mixture Model (GFMM) | A computational model that identifies latent classes from heterogeneous data types without strong statistical assumptions. | The core algorithm used to decompose phenotypic heterogeneity and identify the four classes [78] [79]. |
| Simons Simplex Collection (SSC) | An independent, deeply phenotyped autism cohort used for replication and validation. | Used to successfully replicate the four-class model, confirming its generalizability [78]. |
Experimental Workflow and Validation Diagrams
Diagram 1: Workflow for validating and replicating phenotypic classes.
Diagram 2: Multi-modal validation framework for phenotypic classes.
Linking Subtypes to Distinct Genetic Programs and Developmental Trajectories
Foundational Concepts: Understanding Heterogeneity in Autism
What are the core subtypes of autism identified in recent research? Recent large-scale studies have established that autism spectrum disorder (ASD) comprises biologically distinct subtypes. An analysis of over 5,000 children identified four clinically and biologically distinct subtypes [9]:
- Social and Behavioral Challenges (37%): Core autism traits (social challenges, repetitive behaviors) with typical developmental milestone achievement. High rates of co-occurring conditions like ADHD, anxiety, and depression [9].
- Mixed ASD with Developmental Delay (19%): Delayed achievement of developmental milestones (e.g., walking, talking). Generally does not show signs of anxiety, depression, or disruptive behaviors [9].
- Moderate Challenges (34%): Core autism-related behaviors present but less pronounced. Developmental milestones are typically met on time, and co-occurring psychiatric conditions are uncommon [9].
- Broadly Affected (10%): The most severe subtype, characterized by wide-ranging challenges including developmental delays, significant social and communication difficulties, repetitive behaviors, and co-occurring psychiatric conditions [9].
How do developmental trajectories relate to age at diagnosis? Research confirms that autistic individuals follow different socioemotional and behavioural trajectories, which are strongly linked to the age at which they are diagnosed. Analyses of longitudinal birth cohort data consistently identify two primary latent trajectories [2] [80]:
- Early Childhood Emergent Trajectory: Characterized by significant socioemotional and behavioural difficulties in early childhood that remain stable or modestly improve into adolescence. Associated with an earlier autism diagnosis [2].
- Late Childhood Emergent Trajectory: Characterized by fewer difficulties in early childhood, but a significant increase in socioemotional and behavioural challenges during late childhood and adolescence. Associated with a later autism diagnosis and a higher likelihood of co-occurring mental health conditions such as ADHD and depression [2] [80].
Methodologies & Experimental Protocols
What integrated methodological approaches are effective for biomarker discovery in heterogeneous autism? Converging evidence suggests that single-method approaches are insufficient. The most promising strategies integrate multiple data modalities [23] [9] [81].
Protocol: Multi-Modal Data Integration for Subtype Stratification
- Objective: To identify biologically distinct ASD subtypes by integrating deep phenotypic data with genetic information [9].
- Procedure:
- Phenotypic Profiling: Collect data on a broad range of over 230 traits per individual, including social interactions, repetitive behaviors, developmental milestones, and co-occurring psychiatric conditions [9].
- Computational Clustering: Apply a "person-centered" computational model (e.g., group-based latent trajectory modeling) to cluster individuals based on their combinations of traits, rather than searching for links to single traits [2] [9].
- Genetic Association: Link the identified clinical subtypes to distinct genetic profiles (e.g., burden of damaging de novo mutations, rare inherited variants) and disrupted biological pathways using whole-exome or genome sequencing data [9].
- Troubleshooting: If clusters are not genetically distinct, ensure the phenotypic data is sufficiently granular and explore alternative clustering algorithms or a different number of subgroups.
Protocol: Neuroimaging-Epigenetic Machine Learning Model
- Objective: To improve ASD classification accuracy by combining brain imaging and epigenetic data, using sensory behavior as a baseline [23].
- Procedure:
- Baseline Behavioral Measure: Administer a standardized sensory behavior questionnaire (e.g., Adolescent-Adult Sensory Profile) [23].
- Brain Imaging: Acquire structural and resting-state functional MRI (rs-fMRI) scans. Preprocess data and calculate thalamo-cortical resting-state functional connectivity (rs-FC) [23].
- Epigenetic Analysis: Extract DNA from saliva or blood. Perform DNA methylation analysis for candidate genes (e.g., AVPR1A, OXTR) using methods like bisulfite sequencing [23].
- Model Building and Validation: Use a machine learning algorithm (e.g., XGBoost) to build and compare three models: a neuroimaging model, an epigenetic model, and a combined neuroimaging-epigenetic model. Validate model performance on a held-out test set [23].
Experimental Workflow: Integrated Biomarker Discovery
The following diagram illustrates the key steps for a multi-modal biomarker discovery pipeline.
What are the key genetic programs and pathways linked to specific subtypes? The distinct subtypes are driven by differences in their underlying genetic programs and the timing of genetic effects on brain development [9] [82].
Table 1: Genetic Programs and Developmental Timelines by Subtype
| Subtype | Key Genetic Findings | Affected Biological Pathways | Developmental Timeline |
|---|---|---|---|
| Broadly Affected | Highest burden of damaging de novo mutations [9] | Disruption in multiple early neurodevelopmental pathways [9] | Genetic effects are predominant in prenatal and early postnatal periods [9] |
| Mixed ASD with Developmental Delay | Enriched for rare inherited genetic variants [9] | Distinct from the de novo driven pathways in the "Broadly Affected" group [9] | Early developmental delays evident [9] |
| Social & Behavioral Challenges | Mutations in genes active later in childhood [9] | Pathways influencing circuit refinement and plasticity [9] [82] | Biological mechanisms may emerge postnatally; diagnosis often later [9] |
| Earlier vs. Later Diagnosis (General) | Two genetically correlated (rg ~0.38) polygenic factors [2] | Earlier-diagnosis factor: social-communication; Later-diagnosis factor: overlaps with ADHD/depression [2] [80] | Earlier: difficulties manifest in early childhood; Later: difficulties emerge in adolescence [2] |
Signaling Pathway: GABA Neuron Remodeling
Several autism-associated genes converge on the process of experience-dependent neuron remodeling, particularly affecting GABAergic neurons, but via distinct temporal trajectories [82].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Reagents for Featured Experiments
| Item | Function/Application | Specific Example |
|---|---|---|
| Adolescent-Adult Sensory Profile (AASP) | A self-report questionnaire used to establish a baseline of sensory-related behavioral abnormalities, a core feature of ASD [23]. | Standardized tool for quantifying low registration, sensitivity, sensation seeking, and avoidance across sensory domains [23]. |
| DNA Methylation Analysis Kit | For quantifying epigenetic modifications (e.g., at OXTR, AVPR1A genes) from saliva or other biospecimens [23]. | Bisulfite conversion kits followed by pyrosequencing or array-based methylation profiling (e.g., Illumina EPIC array) [23]. |
| MRI Scanner (3T) | For acquiring high-resolution structural (T1-weighted) and resting-state functional MRI (rs-fMRI) data to measure brain volume and thalamo-cortical connectivity [23]. | Scanner with standard head coil; parameters: TR=2000ms, TE=24ms for rs-fMRI; 1mm³ voxels for structural scans [23]. |
| C. elegans Model System | An intact, behavior-generating circuit to screen conserved autism genes for roles in experience-dependent neuron remodeling and circuit plasticity [82]. | Strains with loss-of-function mutations in orthologs of human ASD genes (e.g., unc-44/ANK2, set-4/KMT5B) [82]. |
| Computational Analysis Tools | Software for genetic analysis, clustering, and machine learning modeling to integrate multi-modal data and define subtypes. | FreeSurfer (neuroimaging processing) [23], CONN (functional connectivity) [23], XGBoost (machine learning) [23], growth mixture models (trajectory analysis) [2]. |
Troubleshooting Guide: Addressing Common Experimental Challenges
FAQ: Our biomarker discovery study is underpowered. What is the impact of heterogeneity on sample size? Disease heterogeneity profoundly impacts statistical power and sample size requirements. Simulation studies show that identifying biomarkers for heterogeneous diseases requires more than double the sample size compared to homogeneous diseases [83]. This is because a biomarker with high sensitivity for one subtype may have low overall sensitivity if that subtype is not well-represented in the sample. Ensure your study is designed with sufficient power to detect signals within subtypes, not just across the entire heterogeneous cohort [83] [9].
FAQ: We have identified potential biomarker candidates, but they fail to validate in independent cohorts. How can we improve robustness? This is a common challenge due to cross-cohort variability and the biological complexity of autism. To improve robustness:
- Integrate Functional Relevance: Move beyond purely expression-based discovery. Integrate your findings with data on gene essentiality (e.g., from RNAi screens) or known biological pathways to prioritize candidates with a direct link to disease mechanisms [81].
- Adopt Two-Stage Designs: Implement a two-stage screening process. Use a moderate number of samples in the first stage to pre-screen and eliminate poor candidates, then validate the top candidates in the remaining, larger sample set. This can achieve nearly the same power as a single-stage design at a significantly reduced cost and with reduced risk of false positives [83].
- Stratify by Subtype: Do not analyze your cohort as a single group. Validate your biomarkers within the specific data-driven subtypes (e.g., the four subtypes defined by Troyanskaya et al.) to which they are most relevant [9].
FAQ: How do we account for the effect of development itself in our models? The genetic programs underlying autism are not static and unfold across a developmental timeline [9] [82].
- Incorporate Longitudinal Data: Where possible, use longitudinal study designs that track participants over time, rather than relying solely on cross-sectional data [2] [84].
- Model Developmental Trajectories: Use statistical models like growth mixture models or latent growth curve models to identify distinct developmental trajectories, rather than simply comparing group means at a single time point [2].
- Consider Gene Expression Timing: When interpreting genetic findings, consider the developmental timepoint at which the implicated genes are most active. This can provide clues about when the primary neurobiological disruption occurs [9].
Comparative Analysis of Subtype-Specific Clinical Outcomes and Intervention Needs
Autism spectrum disorder (ASD) is perhaps one of the most important medical disorders of our era because of the number of people it affects, with current estimates indicating approximately 2% of children in the United States are affected. [85] The extensive "spectrum" of presentations has proven particularly challenging for clinical research, as the diagnosis of ASD is based exclusively on observing behaviors by trained or untrained individuals without proven biological measurements. [85] [86] This heterogeneity has significantly impeded progress in understanding underlying biological mechanisms and developing effective, targeted interventions. [87]
The limitations of behaviorally-defined subtypes were formally acknowledged in the most recent diagnostic taxonomy for ASD (DSM-5), which discarded these subtypes because they demonstrated poor reliability and limited utility for treatment selection or prognosis determination. [87] As noted by the Autism Biomarkers Consortium for Clinical Trials (ABC-CT), clinical research remains reliant upon standardized but intrinsically subjective clinician and caregiver/self-report measures, creating an urgent need for objective, quantitative, and reliable biomarkers to advance clinical research. [87]
Recent research has begun to address this challenge through computational approaches that identify biologically distinct subtypes of autism. A landmark study by Princeton University and the Simons Foundation analyzed data from over 5,000 children in the SPARK autism cohort, using a computational model to group individuals based on their combinations of more than 230 traits. [9] This "person-centered" approach, which considered a broad range of characteristics from social interactions to repetitive behaviors to developmental milestones, revealed four clinically and biologically distinct subtypes of autism with different genetic profiles and developmental trajectories. [9]
FAQ: Addressing Key Questions in Subtype-Specific Research
Q1: What are the primary sources of heterogeneity in autism spectrum disorder that complicate biomarker discovery? ASD heterogeneity stems from multiple sources including: (1) diverse behavioral manifestations across social communication, repetitive behaviors, and restricted interests; (2) varying associated features such as intellectual disability; (3) numerous comorbidities including epilepsy and attention-deficit/hyperactivity disorder; and (4) myriad genetic, epigenetic, and environmental factors contributing to etiology. [87] This heterogeneity means that myriad upstream molecular pathways can lead to the disruption of network function observed in ASD, making it challenging to identify unified biological mechanisms. [87]
Q2: How can researchers effectively stratify autism populations into meaningful subgroups for clinical trials? Robust stratification requires integrating multiple data types. The Princeton/Simons Foundation study successfully identified subtypes by analyzing over 230 traits in each individual, including social interactions, repetitive behaviors, and developmental milestones, then linking these clinical profiles to distinct genetic patterns. [9] Their data-driven framework defined four clinically relevant subtypes with different genetic profiles and developmental trajectories. Eye-tracking biomarkers like the GeoPref Test offer another stratification method, identifying an ASD subgroup with strong visual preference for geometric images who exhibit distinct clinical profiles. [88]
Q3: What methodological considerations are crucial for ensuring reliable biomarker measurement across multisite studies? The Autism Biomarkers Consortium for Clinical Trials (ABC-CT) has established that effective multisite research requires: (1) standardized protocols for data collection; (2) harmonization of candidate biomarkers across sites; (3) incorporation of replication samples; (4) rigorous quality control procedures; (5) deep phenotyping of participants; and (6) accounting for developmental changes by constraining age ranges or using statistical controls. [87] Methodological factors such as stimulus presentation, experimental design, and variation in hardware/software must be carefully controlled as they can significantly influence biomarker measurements. [87]
Q4: How can researchers address the challenge of developmental change when studying biomarkers in neurodevelopmental disorders? The ABC-CT constrained their study population to children aged 6-11 years to limit age-related confounds while focusing on an age group where biomarker data could be acquired reliably. [87] Additionally, understanding the timing of genetic disruptions' effects on brain development is crucial - researchers found that in one ASD subtype, mutations were found in genes that become active later in childhood, suggesting biological mechanisms may emerge after birth for these children. [9] Longitudinal designs that include multiple sampling points are essential for assessing test-retest reliability and developmental stability of biomarkers. [87]
Troubleshooting Common Experimental Challenges
Challenge: Insufficient Statistical Power for Subtype Identification
Problem: Many biomarker studies have limited sample sizes that prevent robust identification of subgroups within the autism spectrum.
Solution: Leverage large, deeply phenotyped cohorts and collaborative networks. The Princeton study analyzed data from over 5,000 children in the SPARK cohort, providing sufficient power to detect distinct subtypes. [9] The ABC-CT enrolled 280 children with ASD and 119 with typical development, constraining age range from 6-11 years to limit developmental confounds while maintaining statistical power for analyses. [87]
Implementation Considerations:
- Utilize existing large-scale datasets like SPARK or ABC-CT
- Establish multi-site collaborations with standardized protocols
- Constrain age ranges to reduce developmental variability while maintaining clinical relevance
- Ensure inclusion of participants across the full range of intellectual ability (e.g., IQ 60-150) to enhance generalizability
Challenge: Technical Variability in Biomarker Measurements
Problem: Factors such as stimulus presentation, experimental design, and hardware/software variations can introduce significant measurement variability.
Solution: Implement rigorous standardization and quality control procedures across sites. The ABC-CT established a technical and data infrastructure enabling collaborating sites to work together as a single unit. [87] For eye-tracking measures, they used standardized instructions to parents, consistent calibration procedures (five-point calibration using animated cartoon ducks with sounds), and manufacturer-reported accuracy parameters (0.5 degrees). [88]
Implementation Considerations:
- Develop detailed standard operating procedures for all data collection protocols
- Implement regular cross-site training and quality assurance checks
- Use identical or technically matched equipment across sites
- Establish predefined quality thresholds for data inclusion
- Incorporate control tasks to assess data quality
Challenge: Integrating Multimodal Data for Comprehensive Subtyping
Problem: Individual biomarker modalities often capture only specific aspects of ASD heterogeneity, limiting their utility for comprehensive subtyping.
Solution: Adopt a multi-method framework that integrates complementary biomarkers. A 2025 study demonstrated that a neuroimaging-epigenetic model outperformed models using either modality alone when sensory-related behavior was the default baseline. [23] The researchers used machine learning algorithms to integrate brain structural and functional characteristics (cortical and subcortical volume, thalamo-cortical resting-state functional connectivity) with epigenetic measures (DNA methylation values of oxytocin receptor and arginine vasopressin receptor genes). [23]
Implementation Considerations:
- Plan for complementary data collection (e.g., EEG, eye-tracking, genetics, clinical measures)
- Develop computational pipelines for integrated data analysis
- Use machine learning approaches capable of handling high-dimensional, multimodal data
- Ensure temporal alignment of different biomarker assessments
- Address missing data patterns across modalities
Experimental Protocols for Key Biomarker Modalities
Protocol: GeoPref Eye-Tracking Test for ASD Subtyping
Purpose: To identify an ASD subgroup with heightened visual attention toward non-social geometric stimuli, characterized by poor clinical profiles and distinct developmental trajectories. [88]
Apparatus and Setup:
- Eye-gaze data collection using Tobii T120 eye tracker (60 Hz sampling rate; 1280 × 1024 resolution)
- Standardized instructions provided to parents to ensure only toddler's gaze is tracked
- Five-point calibration using animated cartoon ducks with sounds
- Calibration accuracy threshold: 0.5 degrees based on manufacturer-reported parameters
Stimuli and Procedure:
- Stimulus: "The GeoPref Test" (62.22 seconds duration)
- Two rectangular areas of interest (525 × 363 pixels) containing dynamic geometric (DGI) or social images (DSI)
- Side of stimulus presentation varied across subjects to control for spatial biases
- Data processed using Tobii Studio with Tobii Fixation Filter (velocity threshold: 35 ms/window)
Data Analysis:
- Export total fixation duration, fixation count within each AOI, and fixation duration within each AOI
- Calculate percent fixation duration per AOI by dividing total fixation duration within AOI by fixation duration across entire video
- Calculate saccades/sec within each AOI using N-1 total fixations/total fixation duration
- Apply 69% fixation threshold to distinguish ASD toddlers who strongly prefer geometric (ASDGeo) vs. social images (ASDSoc)
Validation Parameters:
- Specificity: 98% (95% CI: 96-99%)
- Sensitivity: 17% (increasing to 33% when saccades included)
- Positive Predictive Value: 81%
- Negative Predictive Value: 65%
- Test-retest reliability: high reliability up to 24 months post-initial test
Figure 1: GeoPref Test Experimental Workflow
Protocol: Multimodal Neuroimaging-Epigenetic Assessment
Purpose: To develop an integrated biomarker model that combines brain and epigenetic factors to improve ASD classification accuracy, particularly in relation to atypical sensory behaviors. [23]
Participant Characterization:
- Total N = 106 participants (34 ASD, 72 controls)
- ASD group meets DSM-5 diagnostic criteria with DISCO assessment
- Exclusion: major physical illness, brain injury, FSIQ < 70, substance abuse
- Sensory assessment: Adolescent-Adult Sensory Profile (AASP) questionnaire
MRI Data Acquisition:
- Scanner: 3T PET/MR scanner (Signa; GE) with 8-channel head coil
- T1-weighted structural parameters: TR = 6.38 ms, TE = 1.99 ms, FA = 11°, FoV = 256 mm, matrix = 256 × 256, voxel dimension = 1 × 1 × 1 mm³
- Rs-fMRI parameters: TR = 2000 ms, TE = 24 ms, FA = 80°, FoV = 192 × 192 mm², voxel dimension = 3 × 3 mm²
Structural Data Preprocessing:
- Software: FreeSurfer version 6.2
- Procedures: brain extraction, bias field correction, motion correction, Talairach transformation, intensity normalization, subcortical segmentation, cortical parcellation
- Quality control: manual inspection and correction of automated reconstructions
Functional Data Preprocessing and Analysis:
- Software: SPM12-based CONN version 21 toolbox
- Preprocessing: discard first 10 volumes, realignment, slice-timing correction, head movement correction, anatomical component-based noise correction, band-pass filtering (0.01-0.08 Hz)
- Seed-to-voxel analysis: bilateral thalamus as seed regions
- Statistical thresholds: voxel-wise p < 0.001 uncorrected, cluster-level p < 0.05 FWE correction
Epigenetic Analysis:
- DNA methylation analysis of OXTR, AVPR1A, AVPR1B from saliva samples
- Computation of DNA methylation values
Statistical Analysis:
- Machine learning: eXtreme Gradient Boosting (XGBoost) algorithm
- Model comparison: neuroimaging-epigenetic model vs. neuroimaging model vs. epigenetic model
- Primary findings: thalamo-cortical hyperconnectivity and AVPR1A epigenetic modification as significant contributing factors
Figure 2: Multimodal Assessment Integration Workflow
Quantitative Data Synthesis for Subtype Comparisons
Table 1: Clinically-Defined Autism Subtypes and Associated Characteristics
| Subtype | Prevalence | Developmental Milestones | Common Co-occurring Conditions | Genetic Features |
|---|---|---|---|---|
| Social and Behavioral Challenges | 37% | Typically reached at similar pace to children without autism | ADHD, anxiety, depression, OCD | Mutations in genes active later in childhood |
| Mixed ASD with Developmental Delay | 19% | Reached later than children without autism | Usually absent anxiety, depression, or disruptive behaviors | Higher likelihood of carrying rare inherited genetic variants |
| Moderate Challenges | 34% | Typically reached at similar pace to children without autism | Generally absent co-occurring psychiatric conditions | Not specified |
| Broadly Affected | 10% | Significant developmental delays | Anxiety, depression, mood dysregulation | Highest proportion of damaging de novo mutations |
Data derived from Princeton/Simons Foundation study of over 5,000 children [9]
Table 2: Performance Metrics of Biomarker Modalities for ASD Identification
| Biomarker Modality | Specificity | Sensitivity | PPV | NPV | Subtype Application |
|---|---|---|---|---|---|
| GeoPref Eye-Tracking (Fixation) | 98% | 17% | 81% | 65% | ASD with strong non-social preference |
| GeoPref Eye-Tracking (with Saccades) | 98% | 33% | 81% | 65% | ASD with strong non-social preference |
| Neuroimaging-Epigenetic Model | Not specified | Superior to single modality | Not specified | Not specified | General ASD classification |
| Functional Connectivity | 100% | 82% | Not specified | Not specified | Presymptomatic detection |
| Cortical Surface Area | 95% | 88% | Not specified | Not specified | Presymptomatic detection |
PPV = Positive Predictive Value; NPV = Negative Predictive Value [23] [85] [88]
Table 3: Key Genetic and Biological Features Across Subtypes
| Subtype | Genetic Profile | Biological Pathways | Developmental Trajectory |
|---|---|---|---|
| Social and Behavioral Challenges | Mutations in genes active later in childhood | Not specified | Later clinical presentation, biological mechanisms may emerge after birth |
| Mixed ASD with Developmental Delay | Rare inherited genetic variants | Distinct from Broadly Affected despite similar clinical presentation | Developmental delays evident early |
| Broadly Affected | Highest de novo mutation burden | Divergent biological processes | Wide-ranging challenges across domains |
Data from Princeton/Simons Foundation study [9]
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Reagents and Resources for Autism Biomarker Research
| Resource Category | Specific Tools/Measures | Research Application | Key Considerations |
|---|---|---|---|
| Diagnostic Characterization | Autism Diagnostic Observation Schedule (ADOS), Autism Diagnostic Interview-Revised (ADI-R), DSM-5 criteria | Gold-standard diagnostic confirmation | Required for participant phenotyping across studies |
| Cognitive Assessment | Wechsler Adult Intelligence Scale (WAIS), Differential Ability Scales (DAS-2nd Edition), Mullen Scales of Early Learning | Intellectual functioning assessment | Critical for stratifying by cognitive ability; DAS used in ABC-CT with IQ range 60-150 |
| Eye-Tracking Hardware | Tobii T120 eye tracker (60 Hz sampling rate) | Visual attention measurement | Manufacturer-reported accuracy of 0.5 degrees; standardized calibration essential |
| Eye-Tracking Stimuli | GeoPref Test (dynamic social vs. geometric images) | ASD subgroup identification | 62.22 second duration; side presentation counterbalanced |
| MRI Acquisition | 3T PET/MR scanner with 8-channel head coil | Brain structure and function | Specific parameters for structural (T1-weighted) and functional (BOLD) sequences |
| Genetic/Epigenetic Analysis | DNA methylation analysis of OXTR, AVPR1A, AVPR1B | Epigenetic biomarker discovery | Saliva samples for DNA collection; methylation value computation |
| Computational Tools | eXtreme Gradient Boosting (XGBoost) algorithm, FreeSurfer v6.2, CONN v21 toolbox | Data analysis and integration | Machine learning for multimodal data integration |
| Large-Scale Datasets | SPARK cohort (Simons Foundation), ABC-CT repository | Validation and replication | Sample sizes in thousands needed for robust subgroup identification |
The validation of biologically-defined autism subtypes represents a transformative step toward precision medicine for neurodevelopmental conditions. [9] The identification of distinct subtypes with unique genetic profiles, developmental trajectories, and clinical presentations enables a more targeted approach to both research and clinical practice. As noted by the Princeton researchers, "This opens the door to countless new scientific and clinical discoveries." [9]
For researchers navigating the challenges of autism heterogeneity, the key recommendations emerging from recent studies include:
- Adopt person-centered approaches that consider broad trait combinations rather than single traits
- Integrate multimodal data including genetic, neuroimaging, behavioral, and epigenetic measures
- Prioritize replication and validation in large, diverse samples with deep phenotyping
- Account for developmental timing in both assessment and interpretation of findings
- Develop subtype-specific assessment batteries that target the most relevant domains for each subgroup
The ability to define biologically meaningful autism subtypes is foundational to realizing the vision of precision medicine for neurodevelopmental conditions. [9] As these approaches continue to mature, they hold promise for enabling earlier identification, more targeted interventions, and improved outcomes across the autism spectrum.
Autism Spectrum Disorder (ASD) is defined by significant genotypic and phenotypic heterogeneity, making the discovery of reliable biomarkers exceptionally challenging [18]. The condition's vast complexity necessitates a move beyond traditional diagnostic categories to identify biologically meaningful subgroups [9] [28]. A precision medicine approach aims to use biomarkers for early detection, diagnosis, prognosis, and prediction of treatment response [89] [28]. However, for heterogeneous conditions like ASD, a single universal biomarker is unlikely; instead, stratification biomarkers that apply to specific subgroups are essential [28]. This technical support center is designed to assist researchers navigating the methodological pitfalls in evaluating the clinical utility of biomarkers within this complex landscape.
Frequently Asked Questions (FAQs)
Q1: My ELISA results show a weak or no signal when testing a novel protein biomarker candidate. What could be the cause? A: Weak signals in immunoassays can stem from multiple pre-analytical and analytical factors. Common issues include: reagents not being at room temperature at assay start, incorrect storage of kit components, use of expired reagents, incorrect preparation of dilutions, or the capture antibody not properly binding to the plate [90]. For novel biomarkers, ensure the assay has been optimally developed and validated for your specific target and sample matrix.
Q2: What is the fundamental difference between a prognostic and a predictive biomarker, and why does it matter for trial design? A: A prognostic biomarker is a baseline measurement that provides information about a patient's probable long-term outcome, regardless of a specific treatment (e.g., likelihood of recurrence with standard care). A predictive biomarker indicates whether a patient is likely or unlikely to benefit from a specific therapy [89]. This distinction is critical: prognostic markers guide whether to treat aggressively, while predictive markers guide which treatment to use. Evaluating a predictive biomarker's utility requires a randomized trial comparing outcomes between marker-positive and marker-negative groups on both the new and standard therapies [89].
Q3: How can I validate a gene-expression classifier derived from a small retrospective cohort? A: The key principle is that data used for evaluation must be distinct from data used for classifier development [89]. If the dataset is large enough, split it into separate training and test sets. For smaller datasets, use complete cross-validation performed correctly. Crucially, provide unbiased estimates of the classifier's predictive accuracy within strata defined by standard prognostic factors. The objective is to estimate clinical validity (correlation with an endpoint) before embarking on prospective trials for clinical utility [89].
Q4: Machine learning models for biomarker discovery show high accuracy during training but fail in independent cohorts. What steps can improve generalizability? A: This often indicates overfitting. Strategies include:
- External Validation: Always test the final model on a completely independent, ideally prospectively collected, dataset [91].
- Rigorous Cross-Validation: Use leave-one-out or repeated k-fold cross-validation during development to get realistic performance estimates [91].
- Feature Selection Discipline: Avoid using the entire dataset for both feature selection and performance estimation.
- Address Batch Effects: Ensure technical variability (e.g., from different labs or sequencing runs) is accounted for.
- Consider Biological Heterogeneity: In ASD, ensure your training and validation cohorts cover the phenotypic spectrum you intend the biomarker to apply to [18] [28].
Q5: Are liquid biopsies reliable for biomarker testing in cancer, and what are their limitations? A: Liquid biopsies (analyzing circulating tumor DNA) are highly specific but not as sensitive as tissue biopsies [92]. If a biomarker is detected in blood, it is likely present. However, a negative result does not rule it out, especially if tumor burden is low or the patient is responding well to treatment [92]. They are very accurate for point mutations (e.g., EGFR) but less so for complex alterations like gene fusions [92]. They complement, but do not yet replace, tissue-based testing in many scenarios.
Troubleshooting Guides
Issue 1: High Background or Non-Specific Signal in Immunoassays
| Possible Cause | Recommended Solution |
|---|---|
| Insufficient washing of plate wells. | Follow recommended washing procedures meticulously. Increase soak time of wash buffer by 30-second increments. After washing, invert plate and tap forcefully on absorbent tissue to remove residual fluid [90]. |
| Contamination between wells. | Always use a fresh plate sealer during incubations; do not reuse sealers [90]. |
| Substrate exposure to light prior to use. | Store substrate in the dark and limit light exposure during the assay [90]. |
| Non-optimized assay conditions for a novel antibody pair. | Titrate both capture and detection antibodies to find the optimal signal-to-noise ratio. Re-optimize blocking conditions and incubation times [90]. |
Issue 2: Inconsistent Biomarker Measurements Across Study Sites
| Possible Cause | Recommended Solution |
|---|---|
| Lack of standardized SOPs for sample collection, processing, and storage. | Develop and distribute detailed, step-by-step SOPs. Conduct mandatory training for all site personnel [70]. |
| Inconsistent sample handling temperatures. | Standardize protocols for flash-freezing, thawing, and maintaining cold chain logistics. Use temperature loggers during shipment [70]. |
| Variable sample preparation techniques (e.g., homogenization). | Implement automated sample prep systems (e.g., Omni LH 96 homogenizer) to reduce human-induced variability and cross-contamination [70]. |
| Equipment calibration drift. | Implement regular calibration and maintenance schedules for all critical equipment (pipettes, analyzers) across sites [70]. |
Issue 3: Poor Replicate Data (High Intra-Assay Variability)
| Possible Cause | Recommended Solution |
|---|---|
| Pipetting errors. | Check pipette calibration and operator technique. Use electronic pipettes for critical dilution steps [90]. |
| Inconsistent washing (as above). | Ensure automated plate washers are calibrated so tips do not scratch well bottoms and deliver consistent volumes [90]. |
| Edge effects on microplates. | Avoid stacking plates during incubation. Ensure even temperature in incubators by not overcrowding and placing plates in the center [90]. |
| Sample carryover or contamination. | Use fresh pipette tips for each sample and reagent. Consider using single-use consumables in automated systems [70]. |
Table 1: Definitions and Purposes of Key Biomarker Types
| Biomarker Type | Definition | Primary Clinical Purpose | Example Context |
|---|---|---|---|
| Diagnostic | Distinguishes subjects with a disease/condition from those without. | Aiding in objective and reliable diagnosis [28]. | Differentiating ASD from other neurodevelopmental conditions [18]. |
| Prognostic | A baseline measurement that provides information about the patient's probable long-term outcome (e.g., disease recurrence, progression). | Predicting the "natural" course to guide treatment intensity [89] [28]. | Oncotype DX score predicting risk of breast cancer recurrence [89]. |
| Predictive | A baseline measurement that indicates likelihood of benefit from a specific therapeutic intervention. | Predicting treatment response to select the right therapy [89] [28]. | EGFR mutation predicting response to EGFR inhibitors in lung cancer [92]. |
| Stratification | A biomarker that defines a subgroup within a heterogeneous condition. | Enabling subgroup-specific diagnosis, prognosis, or treatment prediction [28]. | Identifying the four biologically distinct ASD subtypes (e.g., Broadly Affected, Social/Behavioral) [9]. |
Table 2: Key Metrics for Biomarker Test Validation
| Metric | Formula/Description | Interpretation |
|---|---|---|
| Analytical Validity | Accuracy, reproducibility, and robustness of the test measurement itself. | Fitness for purpose at the assay level [89]. |
| Clinical Validity | Correlation between the test result and a clinical endpoint (e.g., diagnosis, survival). | Does the test measure a clinically relevant state? Can be established retrospectively [89]. |
| Clinical Utility | Evidence that using the test to guide decision-making improves patient outcomes. | The highest bar for validation, generally requiring prospective trials [89]. |
| Sensitivity | True Positives / (True Positives + False Negatives) | Ability to correctly identify individuals with the trait/condition. |
| Specificity | True Negatives / (True Negatives + False Positives) | Ability to correctly identify individuals without the trait/condition [89] [18]. |
| Positive Predictive Value (PPV) | True Positives / (True Positives + False Positives) | Probability that a positive test result is a true positive. Depends on prevalence. |
| Negative Predictive Value (NPV) | True Negatives / (True Negatives + False Negatives) | Probability that a negative test result is a true negative. Depends on prevalence [89]. |
Detailed Experimental Protocols
Protocol 1: Developing and Validating a Predictive Biomarker Classifier Using Machine Learning
Based on the MarkerPredict framework for oncology, adaptable to ASD subgroup discovery [91].
Objective: To identify protein/gene biomarkers predictive of response to a targeted therapy or membership in a clinical subtype.
Materials:
- Data: Network databases (e.g., Human Cancer Signaling Network, SIGNOR, ReactomeFI). Intrinsically Disordered Protein (IDP) databases (DisProt, AlphaFold pLLDT scores, IUPred). Literature-mined biomarker database (e.g., CIViCmine).
- Software: FANMOD for network motif analysis; Python/R with scikit-learn/XGBoost for machine learning.
Methodology:
- Network & Data Curation: Download signed protein-protein interaction networks. Compile lists of therapeutic targets and proteins annotated as IDPs.
- Motif Identification: Use FANMOD to identify all three-node network motifs (triangles). Isolate triangles that contain both a target and an IDP ("IDP-target pairs"). This step hypothesizes close regulatory relationships [91].
- Training Set Construction:
- Positive Set (Class 1): Neighbour-target pairs where the neighbour is a literature-validated predictive biomarker for the target's drug [91].
- Negative Set (Class 0): Random protein pairs not in the positive set, or neighbours not listed in the biomarker database.
- Feature Engineering: For each neighbour-target pair, extract features: network topological properties (degree, centrality), motif participation counts, and protein disorder scores from multiple databases.
- Model Training & Validation: Train multiple classifiers (e.g., Random Forest, XGBoost). Optimize hyperparameters via competitive random halving or grid search. Perform Leave-One-Out-Cross-Validation (LOOCV) and/or 70:30 train-test splits to obtain robust accuracy, AUC, and F1-score estimates [91].
- Ranking & Scoring: Generate a Biomarker Probability Score (BPS) by normalizing and summing rank probabilities across all trained models. Apply the final model to score all possible neighbour-target pairs in the network for novel predictions.
Protocol 2: Integrated Multi-Modal Biomarker Study for ASD Subtyping
Based on the study integrating sensory behavior, brain imaging, and epigenetics [23].
Objective: To classify ASD vs. typically developing controls and identify contributing biomarkers by integrating behavioral, neuroimaging, and epigenetic data.
Materials:
- Participants: Precisely characterized cohorts (e.g., ASD meeting DSM-5 criteria, matched typically developing controls). Minimum sample size calculated a priori (e.g., N=105 for 30 predictors, effect size f²=0.3, power=0.8) [23].
- Assessments: Behavioral questionnaire (e.g., Adolescent-Adult Sensory Profile - AASP). Full-scale IQ test.
- Neuroimaging: 3T MRI scanner. T1-weighted structural and resting-state fMRI sequences.
- Epigenetics: Saliva or blood collection kits. DNA extraction and bisulfite conversion kits. Pyrosequencing or array-based methylation assay.
Methodology:
- Data Acquisition:
- Behavior: Administer AASP to derive four sensory processing patterns (Low Registration, Sensitivity, Sensation Seeking, Avoidance) [23].
- Brain Structure: Acquire high-resolution T1 MRI. Process with FreeSurfer to extract cortical thickness, surface area, and subcortical volumes.
- Brain Function: Acquire resting-state fMRI. Preprocess (realign, normalize, smooth, filter). Perform seed-based functional connectivity analysis (e.g., using thalamus as seed) to generate individual connectivity maps [23].
- Epigenetics: Extract DNA from saliva. Perform bisulfite conversion. Quantify DNA methylation levels at specific CpG sites of candidate genes (e.g., OXTR, AVPR1A) via pyrosequencing.
- Feature Extraction: From the above, create a feature vector for each subject including AASP scores, structural brain volumes, thalamo-cortical connectivity values (Fisher's z-scores), and DNA methylation beta values.
- Model Development: Use a machine learning algorithm (e.g., XGBoost). Develop three nested models:
- Model A (Baseline): AASP behavioral scores only.
- Model B (Neuroimaging): AASP + brain structural/functional features.
- Model C (Epigenetic): AASP + DNA methylation features.
- Model D (Integrated): AASP + brain + epigenetic features [23].
- Analysis: Train classifiers to distinguish ASD from controls. Compare predictive accuracy (e.g., AUC) between models to test if integrated data outperforms single-modality data. Use SHAP or permutation importance to identify top contributing features (biomarkers) to the classification.
Visualizations: Diagrams and Workflows
Diagram Title: Logic Flow for Biomarker Clinical Interpretation
Diagram Title: Machine Learning Workflow for Predictive Biomarker Discovery
Diagram Title: Integrated Framework for Addressing ASD Heterogeneity
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Reagents and Solutions for Featured Biomarker Research
| Item | Function/Brief Explanation | Primary Use Case/Protocol |
|---|---|---|
| Next-Generation Sequencing (NGS) Panel | A comprehensive genomic test that simultaneously sequences multiple genes for mutations, fusions, and amplifications. | Lung cancer biomarker testing; ideal test includes EGFR, ALK, ROS1, RET, NTRK, MET, BRAF, KRAS, etc. [92]. |
| Liquid Biopsy Kit | Reagents for isolating and analyzing circulating tumor DNA (ctDNA) from blood plasma. | Non-invasive monitoring of tumor biomarkers, especially for point mutations, when tissue is unavailable [92]. |
| Anti-PD-L1 Antibody (Clone for IHC) | Primary antibody for immunohistochemistry (IHC) to detect PD-L1 protein expression on tumor cells. | Determining eligibility for immunotherapy in cancers like lung cancer; not part of NGS but a crucial companion diagnostic [92]. |
| DNA Methylation Assay Kit (e.g., Pyrosequencing) | Kit for bisulfite conversion of DNA and quantitative analysis of methylation at specific CpG sites. | Measuring epigenetic biomarkers, such as OXTR or AVPR1A methylation levels in ASD research [23]. |
| ELISA Antibody Pair (Capture/Detection) | Matched set of monoclonal antibodies targeting different epitopes on the same protein analyte. | Developing in-house quantitative immunoassays for novel protein biomarkers [90]. |
| Automated Homogenizer (e.g., Omni LH 96) | Instrument for standardized, high-throughput disruption of tissue or cell samples. | Ensuring consistent sample preparation for downstream nucleic acid or protein biomarker analysis, minimizing contamination [70]. |
| Resting-State fMRI Acquisition Sequence | A specific MRI pulse sequence optimized for capturing low-frequency blood-oxygen-level-dependent (BOLD) signals at rest. | Acquiring functional brain connectivity data for neuroimaging biomarker discovery in ASD and psychiatry [23]. |
| XGBoost or scikit-learn Library | Open-source software libraries implementing powerful machine learning algorithms. | Developing and validating classifiers for biomarker discovery and patient stratification from complex datasets [91] [23]. |
| Network Biology Databases (SIGNOR, Reactome) | Curated databases of protein-protein interactions and signaling pathways. | Providing the network infrastructure for systems-level biomarker discovery, as in the MarkerPredict method [91]. |
| Adolescent-Adult Sensory Profile (AASP) | A standardized, self-report questionnaire assessing behavioral responses to sensory experiences. | Quantifying sensory processing patterns as a behavioral biomarker or baseline measure in ASD studies [23]. |
Autism Spectrum Disorder (ASD) is characterized by significant genotypic and phenotypic heterogeneity, which presents a substantial challenge for biomarker discovery and clinical adoption [18]. The vast heterogeneity of the condition necessitates a vigorous search for biological markers capable of aiding in diagnosis, identifying more homogeneous subgroups for biological study, individualizing treatment, and measuring treatment response [18]. This technical support center addresses the key methodological and ethical considerations in this evolving field, providing researchers with practical guidance for conducting rigorous, inclusive biomarker research that respects neurodiversity while advancing scientific understanding.
Frequently Asked Questions (FAQs)
Q1: What are the primary challenges in developing biomarkers for ASD?
- Heterogeneity: ASD involves hundreds of genetic and genomic disorders, with no single molecular marker defining the diagnosis [18]. The condition spans the entire range of IQ and language function with variable profiles of strengths and deficits [18].
- Sensitivity and Specificity: Many proposed biomarkers display low sensitivity and fail to identify the majority of studied samples. They often associate with neuropsychiatric conditions other than ASD, compromising specificity [18].
- Clinical Relevance: Biomarkers must perform well for individual patients in terms of accuracy, stability over time, precision, cost-effectiveness, and clinical viability [18].
Q2: How can we address ethical concerns in early neurodevelopmental research?
- Community Engagement: Conduct research in partnership with autistic people and their families to anticipate early interventions that serve the community's interests [93].
- Respectful Terminology: Avoid ableist language such as "high/low functioning" that may contribute to stigmatization [94].
- Inclusive Research Teams: Include neurodivergent research team members when researching neurodiversity to center research on the target population [94].
Q3: What emerging technologies show promise for ASD biomarker discovery?
- AI and Machine Learning: Can pinpoint subtle biomarker patterns in high-dimensional multi-omic and imaging datasets that conventional methods may miss [95] [96].
- Multi-Omic Profiling: Provides an effective, holistic approach to biomarker discovery by combining genomic, epigenomic, and proteomic data [96].
- Advanced Models: Organoids and humanized systems better mimic human biology and drug responses compared to conventional models [96].
Q4: How can researchers ensure their biomarker findings are reproducible?
- Adequate Sample Sizes: Increasing sample size steadily increases prediction accuracy, providing an efficient strategy to improve biomarkers [97].
- Cross-Validation: Be aware that models may perform well in cross-validation on available data but not generalize to external datasets [97].
- Multi-Site Validation: Test biomarkers across different acquisition sites and populations to assess generalizability [97].
Troubleshooting Common Experimental Challenges
Problem: Low predictive accuracy of neuroimaging biomarkers
- Potential Cause: Model overfitting or insufficient sample size [97].
- Solution: Increase sample size and utilize rigorous cross-validation techniques. Functional MRI may provide better prediction than anatomical MRI [97].
Problem: Difficulty integrating multiple data modalities
- Potential Cause: Technical variability between platforms and measurements [96].
- Solution: Implement AI-driven approaches that can integrate multi-modal data including genomic, proteomic, transcriptomic, and histopathology data [95].
Problem: Ethical concerns regarding early identification and intervention
- Potential Cause: Framing of research goals without community input [93].
- Solution: Adopt participatory research methods that include autistic people in research design and interpretation [94]. Focus on creating favorable conditions in the social environment alongside biological interventions [28].
Problem: Lack of specificity in candidate biomarkers
- Potential Cause: Shared biological mechanisms across neurodevelopmental conditions [18].
- Solution: Implement cross-condition designs to understand which mechanisms are transdiagnostic or specific for particular autistic sub-populations [28].
Experimental Protocols for Biomarker Discovery
Protocol 1: Multi-Modal Biomarker Integration Using Machine Learning
Purpose: To classify ASD by integrating neuroimaging and epigenetic biomarkers with behavioral measures [23].
Methodology:
- Participant Characterization: Recruit participants meeting DSM-5 criteria for ASD and typically developing controls. Assess using standardized measures (AASP for sensory profiles, WAIS for IQ) [23].
- Neuroimaging Acquisition: Acquire structural and resting-state functional MRI data using standardized parameters (e.g., TR = 2000 ms, TE = 24 ms, FA = 80°, FoV = 192 × 192 mm²) [23].
- Epigenetic Analysis: Collect saliva samples and compute DNA methylation values of candidate genes (OXTR, AVPR1A, AVPR1B) using appropriate assays [23].
- Data Integration: Apply machine learning algorithms (e.g., XGBoost) to build predictive models comparing:
- Neuroimaging-epigenetic model (behavior, brain, and epigenetic factors)
- Neuroimaging model (behavior and brain factors)
- Epigenetic model (behavior and epigenetic factors) [23]
Analysis: Evaluate model performance using accuracy metrics and identify significant contributing factors through feature importance analysis [23].
Protocol 2: Prospective Longitudinal Study of Infant Siblings
Purpose: To map early changes in brain and cognitive development that precede the emergence of diagnostic symptoms [93].
Methodology:
- Cohort Establishment: Recruit infants with an older sibling with ASD ("infant sibs"), who have ~20% chance of meeting autism criteria at age 3 [93].
- Multi-Timepoint Assessment: Assess participants at several timepoints from early infancy until age 2-3 years using:
- Eye-tracking measures of social attention
- EEG and/or fNIRS to measure brain function
- Behavioral measures of social and non-social development [93]
- Outcome Characterization: At age 2-3 years, conduct multidimensional assessment to characterize developmental outcome [93].
- Data Analysis: Link early developmental data to later dimensional and diagnostic outcomes to identify predictive biomarkers [93].
Research Workflow: Integrative Biomarker Discovery
The following diagram illustrates the recommended workflow for integrative biomarker discovery that incorporates ethical considerations and neurodiversity perspectives:
Integrative Biomarker Discovery Workflow
Research Reagent Solutions
Table: Essential Research Materials for Autism Biomarker Discovery
| Research Reagent | Function/Application | Example Use Cases |
|---|---|---|
| DNA Methylation Assays [23] | Measures epigenetic modifications in candidate genes | Quantifying OXTR and AVPR1A methylation patterns in saliva samples [23] |
| fMRI Processing Tools (e.g., FreeSurfer, CONN) [23] | Processes structural and functional MRI data | Cortical parcellation, thalamo-cortical functional connectivity analysis [23] |
| Eye-Tracking Technology [18] | Measures visual attention patterns | Assessing reduced attention to eyes and faces in infants [18] [93] |
| AI/Machine Learning Platforms (e.g., XGBoost) [23] | Integrates multi-modal data for prediction | Classifying ASD using combined behavioral, brain, and epigenetic factors [23] |
| Organoid Models [96] | Recapitulates complex human tissue architectures | Functional biomarker screening and exploration of resistance mechanisms [96] |
| Multi-Omic Profiling Tools [96] | Provides holistic view of molecular processes | Integrating genomic, epigenomic, and proteomic data to reveal novel biomarkers [96] |
Key Methodological Considerations
Statistical Power and Sample Size
- Challenge: Most biomarker studies involve small sample sizes or samples of convenience, limiting replicability and generalizability [18].
- Recommendation: Population-based studies involving biological or neuropsychological variables are needed to achieve greater coverage of the phenotypic spectrum as well as statistical power [18]. For multiple regression with ~30 predictors, a minimum sample size of N=105 is recommended to detect a medium-to-large effect size (f²=0.3) with 80% power [23].
Multi-Modal Data Integration
- Evidence: Studies demonstrate that integrated neuroimaging-epigenetic models outperform models using either modality alone in predicting ASD classification [23].
- Implementation: Utilize machine learning algorithms capable of handling high-dimensional data and identifying complex interactions between different data types [23] [96].
Generalizability Testing
- Challenge: Biomarkers developed on one dataset may not generalize to external samples due to dataset shifts [97].
- Solution: Implement rigorous external validation using completely independent cohorts, including different acquisition sites and populations [97].
The path to clinical adoption of autism biomarkers requires navigating both technical challenges and ethical considerations. Success will depend on developing biomarkers that are not only scientifically robust but also clinically viable, cost-effective, and aligned with the needs and perspectives of the autistic community [18] [93]. By integrating multi-modal data sources, adopting inclusive research practices, and maintaining rigorous validation standards, researchers can advance the field toward biomarkers that genuinely improve support and outcomes for autistic individuals while respecting neurodiversity.
Conclusion
The journey to unravel autism's heterogeneity is fundamentally transforming the landscape of biomarker discovery. The paradigm is decisively shifting from seeking a single, universal biomarker to stratifying ASD into biologically and clinically meaningful subtypes, each with distinct genetic underpinnings, developmental timelines, and intervention needs. The integration of large-scale phenotypic data with multi-omics and advanced computational methods is proving indispensable for this deconstruction. Future research must prioritize large-scale validation, the development of dynamic models that capture brain-body-environment interactions, and close collaboration with the autistic community. By embracing this nuanced, precision-based framework, the field is poised to deliver on the promise of objective diagnostics, prognostication, and mechanism-based therapies that significantly improve the lives of autistic individuals.
References
- 1. : pathogenesis, Autism , and... spectrum disorder biomarker [https://pmc.ncbi.nlm.nih.gov/articles/PMC10908366/]
- 2. Polygenic and developmental profiles of autism differ by ... [https://www.nature.com/articles/s41586-025-09542-6]
- 3. Autism Spectrum Disorder as a Multifactorial Disorder [https://pubmed.ncbi.nlm.nih.gov/40650268/]
- 4. Frontiers | Stratification and Predictive Biomarkers in Autism and... [https://www.frontiersin.org/research-topics/74675/stratification-and-predictive-biomarkers-in-autism-and-other-neurodevelopmental-disorders-advancing-eeg-and-eye-tracking-approaches-to-optimize-intervention-strategies]
- 5. Ignite Biomedical and Liquid Biosciences Announce the ... [https://www.biospace.com/press-releases/ignite-biomedical-and-liquid-biosciences-announce-the-discovery-of-biomarkers-for-the-diagnosis-and-treatment-of-autism-spectrum-disorder]
- 6. LinusBio and The BRAIN Foundation Partner to Advance… [https://www.linusbio.com/news/linusbio-and-the-brain-foundation-partner-to-advance-biomarker-supported-autism-diagnosis-and-early-intervention]
- 7. Screening and diagnostic tools for autism spectrum disorder [https://pmc.ncbi.nlm.nih.gov/articles/PMC10951453/]
- 8. Criteria and tools used in an autism assessment [https://www.autism.org.uk/advice-and-guidance/topics/diagnosis/assessment-and-diagnosis/criteria-and-tools-used-in-an-autism-assessment]
- 9. Major autism study uncovers biologically distinct subtypes, ... [https://www.princeton.edu/news/2025/07/09/major-autism-study-uncovers-biologically-distinct-subtypes-paving-way-precision]
- 10. New Study Reveals Subclasses of Autism by Linking Traits ... [https://www.simonsfoundation.org/2025/07/09/new-study-reveals-subclasses-of-autism-by-linking-traits-to-genetics/]
- 11. New Autism Study Uncovers Four Biological Subtypes [https://www.psychiatrist.com/news/new-autism-study-uncovers-four-biological-subtypes/]
- 12. New study identifies biologically distinct autism subtypes, ... [https://www.autismspeaks.org/science-news/study-identifies-autism-subtypes]
- 13. New Autism Subtypes Identified Based on Genes, ... [https://www.brainfacts.org/diseases-and-disorders/childhood-disorders/2025/new-autism-subtypes-identified-based-on-genes-individual-traits-111125]
- 14. Dissecting the heterogeneity of autism spectrum disorder ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402529/]
- 15. Genetic and environmental influences in autism [https://www.jci.org/articles/view/201157]
- 16. Review Early detection of autism with the help of biomarkers [https://www.sciencedirect.com/science/article/pii/S2950588725000746]
- 17. Genetic and environmental influences in autism [https://pmc.ncbi.nlm.nih.gov/articles/PMC12618061/]
- 18. Biomarkers in Autism Spectrum Disorder - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6526849/]
- 19. Genetic Advances in Autism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8531042/]
- 20. Biomarkers start telling us a story: Autism pathophysiology ... [https://autism.org/biomarkers-and-pathophysiology/]
- 21. Polygenic risk scores: from research tools to clinical instruments [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-020-00742-5]
- 22. Current Progress and Challenges in the Search for Autism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3774962/]
- 23. Dissecting the heterogeneity of autism spectrum disorder ... [https://www.nature.com/articles/s41398-025-03566-2]
- 24. Neurodevelopmental Impact of Maternal Immune Activation ... [https://www.mdpi.com/1467-3045/47/9/721]
- 25. Characterizing immune and metabolic profiles in autism ... [https://www.sciencedirect.com/science/article/abs/pii/S002239562500456X]
- 26. Early-life exposure to widespread environmental toxicants ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969721017824]
- 27. Immunological Biomarkers in Autism Spectrum Disorder [https://pmc.ncbi.nlm.nih.gov/articles/PMC11432970/]
- 28. Does the current state of biomarker discovery in autism ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2023.1085445/full]
- 29. Environmental toxicants and the developing immune system [https://pmc.ncbi.nlm.nih.gov/articles/PMC3033466/]
- 30. Epigenetic age is associated with regional brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12313265/]
- 31. Unveiling How Childhood Trauma Affects Our Genes [https://www.u-fukui.ac.jp/en-research/109626/]
- 32. Epigenetic regulation of brain development, plasticity, and ... [https://www.nature.com/articles/s41386-025-02179-z]
- 33. Neuroscience Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-analysis-support-center/neuroscience-support/neuroscience-support-troubleshooting.html]
- 34. Big data approaches to decomposing heterogeneity across ... [https://www.nature.com/articles/s41380-018-0321-0]
- 35. Heterogeneity in Autism and How Science is Addressing It [https://autismsciencefoundation.org/the-big-h-word-heterogeneity-in-autism-and-how-science-is-addressing-it/]
- 36. Genomic insights and advanced machine learning [https://pmc.ncbi.nlm.nih.gov/articles/PMC10799794/]
- 37. Blood biomarker discovery for autism spectrum disorder [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0302951]
- 38. Unlocking autism's complexity: the Move Initiative's path to ... [https://www.frontiersin.org/journals/integrative-neuroscience/articles/10.3389/fnint.2024.1496165/full]
- 39. Rationale of an Advanced Integrative Approach Applied to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8230111/]
- 40. A study of genetic heterogeneity in autism spectrum disorders ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10518435/]
- 41. Integrative multi-omics analysis of autism spectrum ... [https://www.sciencedirect.com/science/article/pii/S2090123225000554]
- 42. Multi-Omics: Challenges and Solutions [https://bigomics.ch/blog/key-challenges-in-multi-omics-data-integration/]
- 43. Integrating Multi-Omics for Precision Medicine: 2025 Guide [https://lifebit.ai/blog/integrating-multi-modal-genomic-and-multi-omics-data-for-precision-medicine/]
- 44. Integrating Multi-Omics Data: Methods and Applications in ... [https://www.sciencedirect.com/science/article/pii/S2215017X25000657]
- 45. Proteomics and Metabolomics Approaches towards a ... [https://www.mdpi.com/1422-0067/21/17/6274]
- 46. 2025 Trends: Multiomics [https://www.genengnews.com/topics/omics/2025-trends-multiomics/]
- 47. Predictive modeling of adaptive behavior trajectories in ... [https://www.nature.com/articles/s41398-025-03592-0]
- 48. Genomic and Developmental Models to Predict Cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12012735/]
- 49. The Lazy Data Scientist's Guide to AI/ML Troubleshooting [https://imerit.net/resources/blog/model-or-data-all-pbm/]
- 50. Autism Spectrum Disorder: What Do We Know and Where Do ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468522/]
- 51. Decomposition of phenotypic heterogeneity in autism ... [https://www.nature.com/articles/s41588-025-02224-z]
- 52. Autism symptoms vanish in mice after Stanford brain ... [https://www.sciencedaily.com/releases/2025/09/250907172644.htm]
- 53. Promising Autism Research Breakthroughs in 2025 [https://linksaba.com/promising-autism-research-breakthroughs/]
- 54. Autism Treatment Breakthrough [https://www.gratefulcareaba.com/blog/autism-treatment-breakthrough]
- 55. Precision diagnostic and therapeutic interventions in rare ... [https://www.nature.com/articles/s41390-025-04611-y]
- 56. The Potential of Autism Gene Therapy [https://www.mastermindbehavior.com/post/autism-gene-therapy]
- 57. Can stratification biomarkers address the heterogeneity of ... [https://pubmed.ncbi.nlm.nih.gov/34823622/]
- 58. Can stratification biomarkers address the heterogeneity of ... [https://www.cambridge.org/core/journals/irish-journal-of-psychological-medicine/article/can-stratification-biomarkers-address-the-heterogeneity-of-autism-spectrum-disorder/673518A0ACC4FB64B8B5248E2051673A]
- 59. Electroencephalography-Based Machine Learning for ... [https://pubmed.ncbi.nlm.nih.gov/41008759/]
- 60. Age of machine learning: new trends in autism spectrum ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1492484/full]
- 61. Towards the Development of a Diagnostic Test for ... [https://autism.org/using-machine-learning-for-biomarker-discovery/]
- 62. Sample size determination: A practical guide for health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000262/]
- 63. Size matters: how sample size affects the reproducibility and ... [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-019-0226-2]
- 64. Standardization and Methodology for Multimodal Biomarkers [https://www.ncbi.nlm.nih.gov/books/NBK596791/]
- 65. Identification of statistical tools to aid in biomarker analysis [https://www.projectguru.in/identification-statistical-tools-aid-biomarker-analysis/]
- 66. Guidelines for the standardization of preanalytic variables ... [https://www.sciencedirect.com/science/article/pii/S1552526014027654]
- 67. Challenges in Biomarker Discovery: Combining Expert ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3548234/]
- 68. Autism Biomarkers [https://medschool.ucla.edu/research/themed-areas/neuroscience-research/brain-development/autism-biomarkers]
- 69. Methods for Assessing Improvement in Specificity when a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2802069/]
- 70. Common Lab Issues That Impact Biomarker Data [https://blog.omni-inc.com/blog/common-lab-issues-that-impact-biomarker-data]
- 71. Pivotal Evaluation of the Accuracy of a Biomarker Used for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2567415/]
- 72. Neurobiological basis of autism spectrum disorder [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2025.1558081/full]
- 73. Does the current state of biomarker discovery in autism reflect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9992810/]
- 74. The Future of Disentangling the Heterogeneity of Autism ... [https://www.sciencedirect.com/science/article/abs/pii/S0006322324015361]
- 75. Quantitative Biomarkers Derived from a Novel, Contrast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10814019/]
- 76. Optimizing intensive longitudinal designs for clinical ... [https://pubmed.ncbi.nlm.nih.gov/41129391/]
- 77. Longitudinal Design - an overview [https://www.sciencedirect.com/topics/mathematics/longitudinal-design]
- 78. Decomposition of phenotypic heterogeneity in autism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12283356/]
- 79. Decomposition of phenotypic heterogeneity in autism ... [https://www.medrxiv.org/content/10.1101/2024.08.15.24312078v1.full-text]
- 80. Study reveals genetic and developmental differences in ... [https://www.cam.ac.uk/research/news/study-reveals-genetic-and-developmental-differences-in-people-with-earlier-versus-later-autism]
- 81. An integrated approach to biomarker discovery reveals ... [https://www.nature.com/articles/s41598-020-78126-3]
- 82. Multiple autism genes influence GABA neuron remodeling via ... [https://pubmed.ncbi.nlm.nih.gov/40666880/]
- 83. Biomarker Discovery for Heterogeneous Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3842033/]
- 84. Developmental Trajectories of Autism - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/37615073/]
- 85. Emerging biomarkers in autism spectrum disorder [https://pmc.ncbi.nlm.nih.gov/articles/PMC6989979/]
- 86. Autism Biomarkers Consortium for Clinical Trials (ABC-CT) [https://medicine.yale.edu/ycci/clinicaltrials/categories/children/autism-biomarkers-consortium/]
- 87. The Autism Biomarkers Consortium for Clinical Trials (ABC ... [https://www.frontiersin.org/journals/integrative-neuroscience/articles/10.3389/fnint.2020.00016/full]
- 88. Large scale validation of an early-age eye-tracking ... [https://www.nature.com/articles/s41598-022-08102-6]
- 89. Clinical trial designs for evaluating the medical utility of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2851173/]
- 90. ELISA Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/elisa-troubleshooting-guide.html]
- 91. MarkerPredict: predicting clinically relevant ... [https://www.nature.com/articles/s41540-025-00603-0]
- 92. Navigating Biomarker Testing: Frequently Asked Questions [https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/symptoms-diagnosis/biomarker-testing/biomarker-faqs]
- 93. Ethical dimensions of translational developmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7611913/]
- 94. Not your “typical” research: Inclusion ethics in ... [https://www.cambridge.org/core/journals/industrial-and-organizational-psychology/article/not-your-typical-research-inclusion-ethics-in-neurodiversity-scholarship/5BC6558D60DE8A05AB8EB259D81A691A]
- 95. AI and the future of biomarker analysis in early R&D [https://www.drugtargetreview.com/article/190428/ai-and-the-future-of-biomarker-analysis-in-early-rd/]
- 96. Emerging Technologies in Biomarker Discovery You ... [https://blog.crownbio.com/emerging-technologies-in-biomarker-discovery-you-should-know-about]
- 97. Insights from an autism imaging biomarker challenge [https://www.sciencedirect.com/science/article/pii/S1053811922002981]