Decoding Disease Endotypes: A Systems Biology Approach to Precision Medicine
The paradigm of 'one-size-fits-all' medicine is rapidly giving way to precision medicine, necessitating a deeper understanding of disease heterogeneity.
Decoding Disease Endotypes: A Systems Biology Approach to Precision Medicine
Abstract
The paradigm of 'one-size-fits-all' medicine is rapidly giving way to precision medicine, necessitating a deeper understanding of disease heterogeneity. This article explores how systems biology, through the integration of multi-omics data, computational modeling, and machine learning, enables the identification of disease endotypes—subtypes defined by distinct biological mechanisms. Aimed at researchers and drug development professionals, we cover the foundational concepts distinguishing phenotypes from endotypes, detail methodological workflows from data generation to analytical pipelines, address key challenges in data integration and biomarker validation, and evaluate the clinical impact of this approach through comparative studies. The synthesis of these elements provides a comprehensive framework for developing targeted, effective therapies and advancing personalized patient care.
From Phenotypes to Precision: Unraveling the Core Concepts of Disease Endotypes
In the era of precision medicine, the historical approach of classifying complex diseases based solely on collective symptoms is proving insufficient. Diseases such as asthma, COPD, and atopic dermatitis are now recognized as heterogeneous disorders encompassing multiple distinct biological entities beneath a common clinical facade [1] [2]. This paradigm shift necessitates a new taxonomic framework that moves beyond descriptive symptomatology to embrace mechanistic underpinnings. The evolving landscape of disease classification now integrates phenotypes (observable characteristics) with endotypes (distinct biological mechanisms), facilitated by advances in systems biology and multi-omics technologies [1]. This whitepaper delineates the critical distinctions between phenotypes and endotypes, establishes methodologies for endotype discovery, and frames this classification within a systems biology research context essential for researchers, scientists, and drug development professionals aiming to develop targeted therapeutic strategies.
Conceptual Foundations: Phenotype, Endotype, and the Bridging Biomarker
Phenotype: The Observable Clinical Presentation
A phenotype refers to the collection of observable clinical characteristics, including symptoms, exacerbation frequency, physiological parameters, and imaging patterns that can be identified through routine clinical assessment [1]. Phenotypes are defined by their direct correlation with clinically relevant outcomes such as treatment responses, disease progression rates, and mortality. For example, in Chronic Obstructive Pulmonary Disease (COPD), well-established clinical phenotypes include the "frequent-exacerbator" and "emphysema-dominant" subtypes [1]. These classifications are valuable for prognostic stratification and initial therapeutic guidance but do not inherently reveal the underlying biological pathways responsible for the clinical presentation.
Endotype: The Underlying Biological Mechanism
An endotype represents a distinct disease subcategory defined by a unique functional or pathobiological mechanism [1]. Unlike phenotypes, endotypes are characterized by specific biochemical pathways, molecular mechanisms, or genetic underpinnings that are conceptually independent of the observable clinical features. The identification of an endotype typically requires specialized molecular profiling and is validated by its ability to predict response to a targeted therapy. Key examples include:
- Eosinophilic inflammation in asthma and COPD [1]
- α1-antitrypsin deficiency in COPD [1]
- Neutrophilic airway inflammation in severe respiratory disease
Critically, a single phenotype can arise from multiple distinct endotypes [1]. For instance, the "frequent-exacerbator" phenotype in COPD may result from an eosinophilic inflammation-driven endotype, which would respond well to corticosteroids, or from an infection-dominated endotype, which might require different therapeutic management [1]. This distinction explains why patients with similar clinical presentations may demonstrate markedly different responses to the same treatment.
Biomarkers: The Operational Bridge
Biomarkers serve as the crucial operational link between phenotypes and endotypes, providing measurable indicators of biological processes [1] [2]. They enable the translation of mechanistic understanding into clinically applicable tools for patient stratification and treatment selection. Promising biomarkers in respiratory disease and dermatology include:
- Blood eosinophil counts for identifying Th2-high inflammation [1]
- Sputum transcriptomics for airway inflammation profiling [1]
- Serum C-reactive protein (CRP) for systemic inflammation assessment [1]
- Specific IgE and other molecular signatures in atopic dermatitis [2]
Table 1: Comparative Analysis of Phenotypes and Endotypes
| Feature | Phenotype | Endotype |
|---|---|---|
| Definition | Observable clinical characteristics and disease manifestations | Subtype defined by distinct biological mechanisms |
| Basis | Clinical features, imaging, physiological tests | Molecular pathways, genetic factors, specific biomarkers |
| Identification Method | Clinical observation, standard diagnostics | Molecular profiling, multi-omics technologies |
| Primary Utility | Prognostication, initial treatment grouping | Predicting response to targeted therapies |
| Example in COPD | "Frequent-exacerbator," "Emphysema-dominant" | Eosinophilic inflammation, α1-antitrypsin deficiency |
| Relationship | One phenotype can map to multiple endotypes | One endotype may manifest as different phenotypes |
The Systems Biology Framework for Endotype Discovery
From Reductionism to Integration: The Systems Approach
Systems biology represents a fundamental paradigm shift from reductionist approaches to an integrative framework that examines complex interactions within biological systems [3]. This approach is particularly suited for endotype discovery because it acknowledges that complex diseases emerge from dynamic networks of molecular and environmental interactions rather than single pathway disruptions. The emerging field of "systems quantitative genetics" exemplifies this transition, extending beyond DNA sequence variations to integrate contributions from multiple biological layers including epigenetics, transcriptomics, proteomics, and metabolomics [3].
This integrative framework enables researchers to address the fundamental challenge in complex disease taxonomy: the lack of complete congruence between genetic polymorphisms and phenotypic manifestations [3]. By capturing the interplay between various molecular layers, systems biology provides the methodological foundation for delineating mechanistically distinct endotypes that transcend superficial phenotypic classification.
Methodological Framework: A Decision Tree Approach for Endotype Identification
A robust data-driven methodology for endotype discovery has been demonstrated through a multi-step decision tree-based approach that integrates gene expression data with clinical and demographic covariates [4] [5]. This method was developed specifically to identify novel, mechanistically distinct disease subtypes from large, multi-dimensional datasets and has been successfully applied to childhood asthma as a case study [5].
The decision tree method outperformed alternative approaches including Student's t-test, single-data domain clustering, and the Modk-prototypes algorithm in its ability to segregate asthmatics from non-asthmatics while providing accessible biological interpretation of the distinguishing features [5]. The strength of this approach lies in its ability to handle the complexity of multi-factorial diseases without relying exclusively on pre-established clinical criteria, thereby enabling discovery of previously unrecognized disease mechanisms [5].
Table 2: Key Research Reagent Solutions for Endotype Discovery
| Research Reagent | Function in Endotyping | Application Examples |
|---|---|---|
| Gene Expression Microarrays | Genome-wide transcriptional profiling | Identifying expression signatures in blood or target tissues [5] |
| Peripheral Blood Samples | Surrogate for target tissue analysis | Evaluating gene expression relevant to disease mechanisms [5] |
| Protein Assays (CRP, IgE) | Quantifying inflammatory biomarkers | Stratifying patients by inflammatory endotypes [1] [5] |
| Flow Cytometry Reagents | Immune cell population analysis | Differentiating inflammatory cell patterns (e.g., eosinophil vs. neutrophil) [1] |
| Multi-omics Platforms | Integrated molecular profiling | Revealing interactions across genomic, transcriptomic, and proteomic layers [3] |
Experimental Workflow for Endotype Discovery
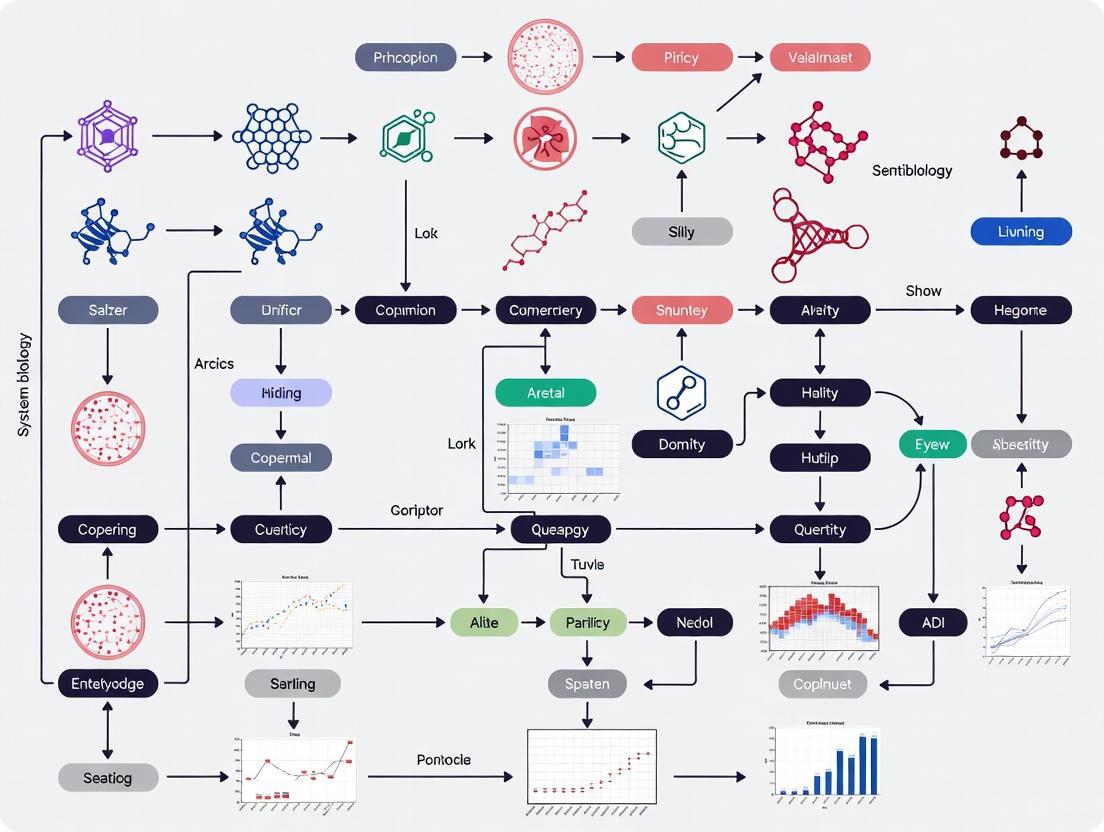
The following Graphviz diagram illustrates the systematic workflow for identifying disease endotypes through integrated data analysis:
Systematic Workflow for Endotype Discovery
Integrating Qualitative and Quantitative Data in Parameter Identification
Systems biology models for endotype characterization benefit from incorporating both qualitative and quantitative data in parameter identification [6]. This approach formalizes qualitative biological observations as inequality constraints on model outputs, which are combined with quantitative measurements through constrained optimization techniques [6]. The objective function in such analyses typically takes the form:
f_tot(x) = f_quant(x) + f_qual(x)
where f_quant(x) represents the sum of squares distance from quantitative data points, and f_qual(x) represents penalty terms for violation of qualitative constraints derived from biological observations [6]. This methodology has been successfully applied to models of Raf inhibition and yeast cell cycle regulation, demonstrating that combining both data types leads to higher confidence in parameter estimates than either dataset could provide individually [6].
Case Studies in Disease Endotyping
Chronic Obstructive Pulmonary Disease (COPD)
COPD exemplifies disease heterogeneity with distinct phenotypic classifications including "emphysema-dominant" (Type A, "pink puffer") and "chronic bronchitis" (Type B, "blue bloater") presentations [1]. The 2023 GOLD guidelines further recognize etiologic heterogeneity by introducing "etiotypes" - causal subtypes including genetically determined COPD (COPD-G), biomass exposure COPD (COPD-P), and COPD with asthma (COPD-A) [1].
Emerging endotypic classifications focus on biological mechanisms rather than clinical presentations:
- Eosinophilic endotype: Characterized by elevated blood or sputum eosinophils, associated with better response to corticosteroids [1]
- Neutrophilic endotype: Dominated by neutrophil-mediated inflammation, often less responsive to standard therapies [1]
- α1-antitrypsin deficiency endotype: Defined by specific genetic abnormality with distinct pathogenesis [1]
These endotypes demonstrate superior predictive value for therapeutic responses compared to phenotypic classification alone, underscoring their clinical utility [1].
Asthma and Atopic Dermatitis
In childhood asthma, the decision tree approach to endotype discovery successfully segregated asthmatics from non-asthmatics by integrating gene expression data from peripheral blood with clinical covariates including allergen sensitivity tests, total serum IgE, and white blood cell differential counts [5]. This methodology provided not only effective classification but also biological interpretation of the distinguishing mechanisms.
Similarly, in atopic dermatitis, research focuses on identifying biomarkers that define endophenotypes to move beyond the historical approach of grouping diverse clinical variants without considering their heterogeneity [2]. These efforts aim to develop phenotype- and endotype-adapted therapeutic strategies tailored to the specific biological mechanisms driving disease in individual patients [2].
Methodological Protocols for Endotype Research
Protocol 1: Decision Tree Analysis for Endotype Identification
This protocol outlines the multi-step decision tree method for identifying endotypes from integrated genomic and clinical data [5]:
Data Collection and Preprocessing
- Collect gene expression data from appropriate tissue (e.g., peripheral blood, target tissue)
- Assemble clinical covariates including demographic, physiological, and biochemical measurements
- Include disease status indicators for supervised analysis
- Normalize and standardize all data domains
Integrated Analysis
- Apply decision tree classification using all available data domains
- Identify key splitting variables that best segregate disease subgroups
- Validate tree structure through cross-validation techniques
- Compare performance against alternative methods (e.g., clustering, t-tests)
Biological Interpretation
- Extract genes and clinical covariates that distinguish the groups
- Perform pathway analysis on distinguishing genes
- Relate findings to known biological mechanisms
- Generate hypotheses for novel disease mechanisms
Protocol 2: Quantitative Morphological Cell Phenotyping
Quantitative morphological phenotyping (QMP) provides a method for capturing morphological features at cellular and population levels [7]. The systematic workflow includes:
Image Acquisition and Processing
- High-content imaging of cellular populations
- Image preprocessing and quality control
- Cell segmentation and feature extraction
Data Analysis and Interpretation
- Multivariate analysis of morphological features
- Identification of morphological signatures associated with disease states
- Integration with molecular data for multi-scale profiling
This approach enables leveraging subtle cellular morphological changes for precise disease subclassification and has been applied to yeast mutant collections among other model systems [7].
The distinction between phenotypes and endotypes represents a fundamental advancement in disease taxonomy that aligns with the core principles of precision medicine. This approach acknowledges that complex diseases are often umbrella terms encompassing multiple mechanistically distinct disorders [1]. The integration of systems biology methodologies, multi-omics technologies, and data-driven classification approaches enables researchers to move beyond descriptive symptomatology to mechanistic disease understanding.
For drug development professionals, this paradigm offers the potential to design more targeted therapies with higher likelihood of success in specific patient subpopulations. The "treatable traits" framework operationalizes this approach by addressing modifiable factors beyond conventional disease classifications [1]. Future directions in the field include early detection of pre-disease states, integration of dynamic phenotyping through machine learning, and pragmatic clinical trials evaluating precision-guided interventions [1].
As systems biology continues to evolve, the integration of multi-scale data from genomics to clinical manifestations will further refine our ability to identify clinically meaningful endotypes. This progression from reactive, symptom-based medicine to proactive, mechanism-targeted therapeutic paradigms holds promise for transforming the management of complex diseases across medical specialties.
In the pursuit of precision medicine, the clinical classification of diseases based solely on observable symptoms—the phenotype—has proven insufficient for predicting treatment outcomes and understanding underlying disease mechanisms. Systems biology research has introduced the crucial concept of the endotype, defined as a distinct biological subtype of a disease characterized by a specific functional or pathophysiological mechanism [8]. Unlike phenotypes, which describe what a disease looks like, endotypes explain why the disease manifests and progresses in a particular way, driven by distinct molecular pathways that can be targeted therapeutically [9] [8]. This paradigm shift is transforming drug development by enabling patient stratification based on molecular mechanisms rather than clinical presentation alone, thereby addressing the critical challenge of heterogeneity in treatment response across patient populations.
Defining the Endotype Concept: Molecular Drivers of Disease Heterogeneity
The endotype concept represents a fundamental advancement in disease classification. Endotypes are characterized by specific immunological, inflammatory, metabolic, and remodeling pathways that explain the mechanisms underlying a disease's clinical presentation [8]. This mechanistic understanding enables researchers to move beyond descriptive categorizations toward biologically meaningful disease subdivisions.
Several key features distinguish endotypes from traditional disease classifications:
- Mechanistic Basis: Endotypes are defined by specific molecular pathways and pathological processes [8] [10]
- Stability: Unlike fluctuating clinical symptoms, endotypes typically represent stable biological traits
- Predictive Value: Endotype classification can forecast disease progression, complication risks, and treatment responses [11]
- Therapeutic Relevance: Endotypes often align with specific therapeutic targets, enabling personalized treatment approaches [10]
The relationship between phenotypes and endotypes is complex and multidimensional. A single clinical phenotype may encompass multiple distinct endotypes, while a single endotype might manifest through varied phenotypic expressions across different patients [12]. This complexity underscores the necessity of molecular profiling for accurate endotype identification.
Disease Case Studies: Endotype Identification and Clinical Impact
Sepsis: Molecular Endotypes Predict Mortality
A comprehensive multi-cohort study analyzing host gene expression profiles from 494 sepsis patients across global populations identified four distinct molecular endotypes with significant mortality implications [13].
Table 1: Sepsis Endotypes Identified by Host Gene Expression Profiling
| Endotype | 28-Day Mortality | Defining Molecular Features | Clinical Characteristics |
|---|---|---|---|
| Immunocompetent | Low | Adaptive immune system activation; robust T-cell and B-cell signaling | Favorable prognosis; minimal organ dysfunction |
| Immunosuppressed | High | Dysfunctional immune response; impaired host defense pathways | High susceptibility to secondary infections |
| Acute-Inflammation | High | Innate immune system hyperactivation; pronounced inflammatory signaling | Severe multiple organ dysfunction; systemic inflammation |
| Immunometabolic | High | Metabolic pathway dysregulation (e.g., heme biosynthesis) | Significant metabolic disturbances alongside organ failure |
This endotypic classification provides a framework for developing tailored immunotherapeutic interventions and biomarkers for predicting outcomes in specific sepsis subgroups [13].
Atopic Dermatitis: Proteomic Profiling Reveals Inflammatory Subtypes
Research on moderate-to-severe atopic dermatitis (AD) has identified distinct molecular endotypes through comprehensive serum proteomic analysis. Using k-means clustering of 1,248 serum protein analytes, researchers consistently identified two stable patient clusters characterized by high (ADHI) and low (ADLO) inflammatory profiles [11].
The AD_HI endotype demonstrated upregulation of both canonical AD inflammatory mediators (including IL-13, IL-19, TARC, and CCL27) and proteins not typically associated with AD, suggesting novel axes of dysregulation. These proteomic signatures were correlated with skin-based disease severity scores, confirming their clinical relevance [11]. The stability of these clusters was validated through rigorous reproducibility testing, including analyses with and without healthy control data.
Neutrophilic Asthma: Distinct Mechanism and Therapeutic Target
Neutrophilic asthma constitutes a distinct endotype characterized by neutrophil-dominated airway inflammation and resistance to corticosteroids [10]. Research has identified Milk fat globule-EGF factor 8 (MFGE8) as a key regulator in this endotype. MFGE8 protein levels are significantly reduced in the sputum supernatant of patients with neutrophilic asthma, and mechanistic studies reveal that MFGE8 inhibits the formation of neutrophil extracellular traps (NETosis) through interaction with integrin β3 [10].
This endotype-specific mechanism presents a promising therapeutic target. Experimental models demonstrate that recombinant MFGE8 protein effectively mitigates neutrophilic airway inflammation, suggesting potential for targeted therapy in this treatment-resistant asthma population [10].
Sjögren's Disease: Heterogeneity in Autoimmunity
Sjögren's disease exemplifies the challenges posed by patient heterogeneity in autoimmune conditions. Molecular stratification studies have identified three to four distinct patient subgroups, potentially representing different disease endotypes or stages [12]. The most consistently identified molecular signature across Sjögren's patients is interferon pathway activation, observed in more than half of patients [12].
Table 2: Stratification Approaches in Sjögren's Disease
| Stratification Method | Basis of Classification | Identified Subgroups | Therapeutic Implications |
|---|---|---|---|
| Clinical Symptom-Based | Patient-reported symptoms followed by biomarker analysis | 3-4 clinical clusters (e.g., low symptom burden, high systemic activity) | Tailored symptomatic management |
| Molecular Pattern-Driven | Multi-omics profiling of whole blood samples | Inflammatory, lymphoid, interferon, and undefined molecular subgroups | Targeted immunomodulatory approaches |
| Serological Profile-Based | Autoantibody patterns and inflammatory markers | Subgroups with distinct autoantibody specificities | Predictors of extraglandular manifestations and lymphoma risk |
The ongoing debate about whether these subgroups represent true endotypes or disease stages highlights the dynamic nature of endotype discovery and validation [12].
Experimental Methodologies for Endotype Identification
Proteomic Profiling Workflow
The identification of atopic dermatitis endotypes exemplifies a rigorous proteomic approach [11]:
This workflow yielded 1,248 protein analytes for cluster analysis, with stability assessed through multiple validation approaches including bootstrapping methods and comparison of clustering outcomes with and without healthy control data [11].
Transcriptomic Analysis in Sepsis
The sepsis endotype study employed sophisticated transcriptomic methodologies [13]:
- RNA Sequencing: Peripheral blood RNA was collected in PAXgene RNA tubes, with ribosomal and globin RNA depletion to enhance sensitivity.
- Bioinformatic Processing: Sequencing reads were aligned to the human genome (GRCh38) using Hisat2, and transcripts were assembled using Stringtie.
- Data Normalization: Raw read counts were normalized using Median Ratio Normalization with Variance Stabilizing Transformation, yielding 3,061 genes for analysis.
- Dimensionality Reduction: Multiple approaches including Principal Component Analysis (PCA), Uniform Manifold Approximation and Projection (UMAP), and Topological Data Analysis (TDA) identified patient subgroups with similar gene expression profiles.
- Differential Expression Analysis: Welch two-sample t-test with Benjamini-Hochberg correction identified significantly differentially expressed genes between endotypes.
- Pathway Analysis: Gene set enrichment analysis against Hallmark pathways revealed the biological processes distinguishing each endotype.
Systems Immunology Approaches
For recessive dystrophic epidermolysis bullosa (RDEB), systems immunology approaches using single-cell high-dimensional techniques captured the signature of peripheral immune cells and metabolic profile diversity [8]. Artificial intelligence prediction models and principal component analysis characterized the complex systemic endotypes marked by immune dysregulation and hyperinflammation, laying the groundwork for translational interventions.
Research Reagent Solutions for Endotype Discovery
Table 3: Essential Research Tools for Endotype Identification
| Research Tool | Specific Application | Function in Endotype Discovery |
|---|---|---|
| Olink Explore 1536 Assay [11] | High-throughput proteomics | Simultaneously measures 1,248 protein biomarkers in serum samples |
| PAXgene Blood RNA System [13] | RNA stabilization from blood | Preserves transcriptomic profiles for gene expression analysis |
| Single-cell RNA Sequencing [8] | High-dimensional immune profiling | Captures diversity of immune cell populations and states |
| Globin-Zero Gold rRNA Removal Kit [13] | RNA library preparation | Depletes ribosomal and globin RNA to enhance sensitivity |
| Weighted Gene Co-expression Network Analysis [11] | Bioinformatics analysis | Identifies modules of highly correlated genes and their associations |
| Topological Data Analysis [13] | Dimensionality reduction | Groups participants with similar gene expression profiles unbiasedly |
Discussion: Implications for Drug Development and Clinical Trial Design
The integration of endotype-based classification into drug development represents a paradigm shift with far-reaching implications. By enabling patient stratification according to underlying molecular mechanisms rather than symptomatic manifestations, endotype discovery directly addresses the challenge of treatment response heterogeneity that has plagued many clinical trials [12] [11].
The practical applications of endotyping in pharmaceutical development include:
- Enrichment Strategies: Selecting patient populations most likely to respond to targeted therapies
- Biomarker Development: Identifying companion diagnostics for treatment selection
- Clinical Trial Design: Structuring trials based on molecular subgroups rather than broad diagnostic categories
- Combination Therapies: Rational pairing of treatments targeting different mechanisms in complex diseases
- Clinical Practice: Ultimately enabling treatment decisions based on molecular profiling rather than trial-and-error approaches
As integrative omics technologies continue to advance, together with computational methods for analyzing high-dimensional data, the framework for identifying and validating disease endotypes will become increasingly sophisticated [14]. This progress promises to accelerate the development of personalized therapeutic strategies tailored to the specific molecular drivers of disease in individual patients, ultimately fulfilling the promise of precision medicine.
Systems biology represents a fundamental shift in biological research, moving from a reductionist study of individual components to a holistic, integrative analysis of complex systems. This approach is paramount for deciphering the intricate mechanisms of human disease, particularly through the lens of endotypes—subclassifications of disease defined by distinct functional or pathobiological mechanisms [15]. Unlike phenotypes, which are observable characteristics tied to clinical outcomes, endotypes delineate the underlying biological drivers that explain why a particular phenotype manifests [15]. The identification of endotypes is crucial for advancing precision medicine, as it enables the move from symptomatic treatments to therapies targeted at specific pathological mechanisms. Systems biology serves as the primary engine for endotype discovery by integrating multi-omics data, computational modeling, and high-throughput experiments to unravel the complex, dynamic interactions within biological systems [16] [17].
The Core Methodologies of Systems Biology
Systems biology employs a diverse toolkit of computational and experimental methods to generate and validate hypotheses about biological function. These methodologies are interdependent, forming an iterative cycle of prediction and experimentation.
Mathematical Modeling and Simulation
Mathematical modeling is a key tool in systems biology used to determine the mechanisms by which elements of biological systems interact to produce complex dynamic behavior [18]. By conducting computational experiments that simulate these systems, researchers can gain valuable insights into the mechanisms governing dynamic behavior that are difficult to understand by intuitive reasoning alone [18] [19].
- Model Types and Applications: The field utilizes various model frameworks, including:
- Ordinary Differential Equations (ODEs): Used to model the dynamics of biological systems over time, such as signaling pathways and metabolic networks. For instance, ODEs can model the cGAS-STING signaling pathway to understand its dual role in non-small cell lung cancer (NSCLC) promotion and inhibition [19].
- Stochastic Models: Account for random fluctuations in biological processes, such as radiation-induced DNA damage kinetics, where outcomes can deviate from deterministic predictions due to clustering of damage events [18].
- Constraint-Based Models: Leverage genomic information to predict metabolic fluxes in genome-scale metabolic networks.
- Parameter Estimation and Identifiability: A critical step in model development is parameter estimation, ensuring models are calibrated to real-world data. Practical identifiability analysis assesses whether model parameters can be uniquely determined from noisy, experimental data [20]. Advanced computational frameworks, such as the VeVaPy Python library, aid in model verification and validation by running parameter optimization algorithms and ranking models based on their fit to experimental data [18].
Data Integration and Multi-Omic Analysis
The rise of high-throughput technologies has enabled the comprehensive profiling of biological systems across multiple layers, from genomics and transcriptomics to proteomics and metabolomics. Systems biology provides the analytical framework to integrate these disparate data types.
- Tools for Discovery: Computational tools are essential for extracting meaningful biological signals from complex omics datasets. For example, ProstaMine is a systems biology tool designed to systematically identify co-alterations of genes associated with aggressiveness in prostate cancer. It integrates multi-omics and clinical data to prioritize co-alterations enriched in metastatic disease, uncovering subtype-specific mechanisms of progression [16].
- Single-Cell Technologies: Advanced techniques like mass cytometry (CyTOF) and imaging mass cytometry (IMC) allow for deep, high-dimensional immunophenotyping at the single-cell level. These methods can capture the diversity of immune cell populations and their functional states in patient samples, revealing endotype-specific immune signatures [17].
Table 1: Key Analytical Techniques in Systems Biology
| Technique | Function | Application Example |
|---|---|---|
| Principal Component Analysis (PCA) | Reduces data dimensionality to reveal underlying patterns. | Used in cGAS-STING model analysis and to stress systemic immune dysregulation in RDEB [17] [19]. |
| Sensitivity Analysis | Quantifies how model output is affected by variations in parameters. | Identifies key regulatory parameters in mathematical models of signaling pathways [20] [19]. |
| Uniform Manifold Approximation and Projection (UMAP) | Non-linear dimensionality reduction for visualization of high-dimensional data. | Mapping single-cell CyTOF data to identify distinct immune cell clusters in RDEB patients [17]. |
| PhenoGraph | Algorithm for clustering high-dimensional single-cell data. | Automated annotation of immune cell populations from CyTOF and IMC data [17]. |
Case Study: Uncovering Endotypes in Recessive Dystrophic Epidermolysis Bullosa (RDEB)
Recessive Dystrophic Epidermolysis Bullosa (RDEB), a severe blistering disease caused by mutations in the COL7A1 gene, serves as a powerful example of how systems immunology can reveal complex systemic endotypes.
Experimental Workflow and Findings
A systems immunology approach was applied to RDEB adults, using single-cell high-dimensional techniques to capture the signature of peripheral immune cells and the diversity of metabolic profiles [17]. The workflow involved:
- Comprehensive Immune Profiling: Peripheral blood leukocytes were analyzed using CyTOF with a large panel of lineage-specific metal-tagged antibodies. Dimensionality reduction with UMAP and clustering with PhenoGraph revealed substantial differences in major innate and adaptive immune cell populations in RDEB adults compared to healthy controls [17].
- Tissue Validation: Imaging mass cytometry (IMC) was performed on formalin-fixed paraffin-embedded skin biopsies from RDEB patients, confirming elevated infiltrates of various CD45+ immune cell populations in skin lesions [17].
- In-Depth PBMC Analysis: Further profiling of peripheral blood mononuclear cells (PBMC) identified increased frequencies of effector and central memory CD4+ and CD8+ T cell subsets, as well as CD14+CD16+ intermediate monocytes in RDEB adults [17].
- Metabolic Profiling: Large-scale profiling of energy and lipid metabolism was conducted, revealing a pro-inflammatory lipid signature concomitant with the immune findings [17].
Identified Endotype and Implications
The study demonstrated that RDEB is not solely a skin disorder but has complex systemic endotypes marked by immune dysregulation and hyperinflammation. The specific endotype was characterized by activated/effector T cell signatures, dysfunctional natural killer (NK) cell signatures, and an overall pro-inflammatory lipid signature [17]. Artificial intelligence prediction models and principal component analysis confirmed these findings, laying the groundwork for translational interventions aimed at lessening inflammation to alleviate patient suffering [17].
Systems Immunology Workflow for RDEB Endotype Discovery
Experimental Protocols for Model-Informed Discovery
Protocol: Minimally Sufficient Experimental Design Using Identifiability Analysis
A critical challenge in model-informed discovery is designing experiments that yield the most informative data for model parametrization without being prohibitively costly or time-consuming. The following protocol uses practical identifiability analysis to determine a minimally sufficient experimental design [20].
- Variable and Model Selection: Identify the experiment that measures the variable of interest (e.g., percent target occupancy in a tumor). Develop, parameterize, and validate a mathematical model describing the system [20].
- Parameter Selection: Select parameters of interest for analysis by first removing those that are easily measurable experimentally. Then, perform a local sensitivity analysis to identify the most sensitive parameters for fitting the data of interest [20].
- Profile Likelihood Analysis: Use the profile likelihood method to assess the practical identifiability of parameters given different hypothetical experimental datasets. This involves determining if parameters can be uniquely estimated from noisy data [20].
- Design Optimization: Iteratively test different experimental sampling schedules (e.g., time points for measurement) to find the minimal set that ensures all parameters of interest are practically identifiable. The goal is to find the protocol that robustly ensures identifiability while minimizing experimental burden [20].
Protocol: Reconstructing a Signaling Pathway Model with MATLAB
To understand complex pathways like cGAS-STING in NSCLC, a mathematical model can be reconstructed and analyzed using computational tools [19].
- Model Reconstruction:
- Launch MATLAB and open the SimBiology toolbox.
- In the diagram editor, create compartments representing cellular structures (e.g., plasma membrane, cytoplasm, nucleus).
- Drag and drop "Species" into the compartments to represent signaling intermediates, receptors, and transcription factors.
- Connect species via "Reactions" to form the network. Define reaction kinetics:
- For association, dissociation, and translocation, use the law of mass action (define rate constant
kf). - For enzyme kinetics (e.g., phosphorylation), use Michaelis-Menten kinetics (define
VmaxandKm). - For gene expression, use Hill's kinetics (define
Vmax,Km, and Hill coefficientn).
- For association, dissociation, and translocation, use the law of mass action (define rate constant
- Set initial concentrations of species in the range of 10³–10⁶ molecules [19].
- Model Simulation and Analysis:
- Simulate the model to observe system dynamics over time.
- Perform a local sensitivity analysis to determine which parameters most influence model outputs.
- Conduct principal component analysis to understand parameter interdependence.
- Apply model reduction techniques to simplify the model while retaining critical dynamics [19].
Iterative Cycle of Model Development and Validation
Table 2: Key Research Reagent Solutions for Systems Biology Studies
| Item / Resource | Function | Application Example |
|---|---|---|
| Metal-tagged Antibody Panels | Enable high-dimensional, single-cell protein analysis via mass cytometry (CyTOF). | Comprehensive immunophenotyping of peripheral blood leukocytes in RDEB studies [17]. |
| Illumina Global Screening Array (GSA) | A cost-effective, array-based platform for large-scale genotyping. | Used in pharmacogenomics testing workflows to identify clinically actionable genetic variants [16]. |
| MATLAB with SimBiology Toolbox | Provides a platform for modeling, simulating, and analyzing dynamic systems; supports SBML format. | Reconstruction and simulation of ODE-based models, such as the cGAS-STING signaling pathway in NSCLC [19]. |
| VeVaPy Python Library | A computational framework for the verification and validation of systems biology models. | Used to optimize parameters and rank competing models of the hypothalamic-pituitary-adrenal (HPA) axis against novel datasets [18]. |
| COPASI | Software application for simulation and analysis of biochemical networks and their dynamics. | An alternative platform for model simulation and analysis [19]. |
Systems biology, through its integrative and hypothesis-driven approach, is the indispensable engine for discovery in modern biomedical research. By leveraging mathematical modeling, multi-omics data integration, and advanced computational tools, it provides the methodological foundation to move beyond superficial phenotypes and uncover the mechanistic endotypes that drive disease. This high-level overview has detailed the core methodologies, showcased a practical application in disease endotyping, and provided actionable experimental protocols. As these approaches continue to mature, they will profoundly accelerate the development of targeted, effective therapeutics, ultimately realizing the promise of precision medicine.
The field of clinical medicine is undergoing a fundamental transformation, moving from a syndrome-based classification of disease toward a mechanism-driven framework centered on the concept of endotypes. An endotype represents a distinct biological subtype of a disease, defined by specific molecular mechanisms, genetic underpinnings, and pathophysiological pathways that differ from other subtypes within the same clinical syndrome [21]. This precision medicine approach is particularly crucial for complex, heterogeneous conditions such as asthma, chronic obstructive pulmonary disease (COPD), and allergic diseases, where significant variability in clinical presentation, disease progression, and treatment response has long complicated management and drug development [1].
The identification of disease endotypes represents a cornerstone of modern systems biology research, which seeks to integrate multi-dimensional data from genomics, transcriptomics, proteomics, and metabolomics to define coherent biological networks underlying disease manifestations [21]. This approach recognizes that different pathological mechanisms can converge on similar clinical presentations, while the same treatment may yield dramatically different outcomes across patient subgroups. For researchers and drug development professionals, understanding and targeting specific endotypes offers the promise of more effective therapies with improved safety profiles, moving beyond the traditional one-size-fits-all approach that has dominated respiratory and allergy therapeutics [1].
Asthma Endotypes: From T2 Inflammation to Epithelial Dysfunction
Molecular Classification of Asthma Heterogeneity
Asthma has been traditionally classified using observable characteristics or phenotypes, such as allergic asthma, nonallergic asthma, adult-onset asthma, and obesity-associated asthma [21]. However, these clinical categories often mask substantial underlying biological diversity. The application of omics technologies to sputum, bronchial epithelium, and blood has revealed that asthma consists of multiple molecular endotypes, broadly categorized as T2-high and non-T2 asthma, each with distinct mechanistic pathways [21].
Research has progressively refined this classification. Early work focused on T-helper (Th) cell pathways, but the discovery that innate immune cells like innate lymphoid cells (ILC2) can produce Th2-associated cytokines prompted a shift in terminology from "Th2" to "T2" inflammation [21]. Transcriptomic analyses of sputum cells have further delineated these endotypes. One pivotal study measuring cytokine expressions identified that 67% of asthmatics exhibited a T2-high pattern, characterized by significantly elevated levels of IL-4, IL-5, and IL-13, which was associated with increased eosinophils and more severe, treatment-resistant disease requiring biologics [21].
Beyond the T2/non-T2 dichotomy, more sophisticated clustering approaches have revealed additional complexity. One analysis of sputum cytokine patterns identified five distinct clusters: (1) high IL-5, IL-10, IL-25, IL-17A, IL-17F; (2) high IL-5/IL-10 with normal IL-17F; (3) high IL-6; (4) high IL-22; and (5) normal cytokine levels [21]. These clusters demonstrated different inflammatory cell profiles, with clusters 1 and 5 showing higher sputum eosinophil percentages, while clusters 1 and 4 had more neutrophils.
The Emerging Role of Airway Epithelium in Asthma Pathogenesis
A paradigm shift in asthma research is the growing recognition that airway epithelial dysfunction may represent the primary driver of inflammatory cascades, marking the beginning of what researchers term the "epithelium era" in asthma investigation [21]. The airway epithelium consists of multiple cell types—including basal cells, club cells, ciliated cells, goblet cells, pulmonary neuroendocrine cells, tuft cells, and pulmonary ionocytes—connected by junctional complexes [21]. In health, this epithelium maintains homeostasis, defends against threats, and regulates immunity, but chronic barrier dysfunction can instigate and propagate excessive immune responses in asthma.
This epithelial paradigm suggests a potentially more straightforward therapeutic approach: targeting the initial epithelial defect rather than the multitude of downstream inflammatory genes affected by the disturbed airway epithelium [21]. Understanding the cellular composition and differentiation of the airway epithelium is now considered vital for developing treatments to restore airway integrity in established asthma.
Early-Life Determinants of Asthma Endotypes
Recent research has illuminated how early-life respiratory patterns influence the development of specific asthma endotypes later in life. A multi-cohort study analyzing data from 961 participants identified four distinct wheeze trajectories: Infrequent, Transient, Late-onset, and Persistent [22]. Each trajectory was associated with unique molecular signatures in upper airway transcriptomes during adolescence and early adulthood:
- Persistent wheezers exhibited elevated gene expression related to mast cell activation and T2 inflammation, but those who developed asthma showed upregulation of neuronal signaling and ciliary function genes rather than traditional T2 inflammation [22].
- Late-onset wheezers demonstrated decreased expression in pathways associated with insulin signaling and carbohydrate metabolism, suggesting a link between airway metabolic dysfunction and later-onset wheeze risk [22].
- Both late-onset and persistent wheeze displayed reduced expression of modules related to innate immune defense and interferon signaling, indicating potentially impaired antiviral and immune responses [22].
These findings suggest that asthma endotypes are shaped by early wheezing patterns, and that neuronal dysregulation and epithelial dysfunction—rather than allergic inflammation alone—may be central to sustained disease pathogenesis in high-risk children [22].
Table 1: Key Asthma Endotypes and Their Characteristics
| Endotype Category | Key Defining Features | Biomarkers | Therapeutic Implications |
|---|---|---|---|
| T2-high | Elevated type 2 inflammation | High IL-4, IL-5, IL-13; sputum/bood eosinophilia; elevated FeNO | Responsive to corticosteroids; anti-IL-4/IL-13, anti-IL-5 biologics |
| Non-T2 | Absence of T2 inflammation | Normal eosinophils; may show neutrophilic or paucigranulocytic inflammation | Poor response to corticosteroids; requires alternative approaches |
| Early-life persistent wheeze | Mast cell activation, neuronal signaling, epithelial dysfunction | T2 inflammation initially; later neuronal and ciliary genes | May benefit from non-T2 targeted interventions |
| Late-onset wheeze | Metabolic dysfunction, impaired innate immunity | Decreased insulin signaling and interferon pathways | Metabolic modulators? |
COPD Endotypes: Beyond the Smoker's Lung
Etiological Diversity in COPD
COPD has traditionally been conceptualized as a single disease entity primarily caused by smoking, but this perspective fails to capture the condition's substantial heterogeneity. The 2023 Global Initiative for Chronic Obstructive Lung Disease (GOLD) report formally acknowledges this diversity by introducing a novel "etiotype" classification system that categorizes COPD based on predominant risk factors [1]. The seven identified etiotypes include:
- Genetically determined COPD (COPD-G) - including alpha-1 antitrypsin deficiency
- COPD due to abnormal lung development (COPD-D) - resulting from early-life events
- Cigarette smoking COPD (COPD-C) - the traditional phenotype
- Biomass and pollution exposure COPD (COPD-P) - common in non-smokers, particularly women in developing countries
- COPD due to infections (COPD-I) - such as post-tuberculosis
- COPD with asthma (COPD-A) - the overlap syndrome
- COPD of unknown cause (COPD-U) [1]
This classification underscores that multiple pathogenic pathways can lead to the final common pathway of irreversible airflow limitation. For instance, biomass-associated COPD frequently manifests greater airway fibrosis with less emphysematous destruction compared to tobacco-related disease [1]. This etiological diversity has profound implications for both prevention strategies and targeted therapeutics.
Inflammatory Endotypes and Treatable Traits
Beyond etiology, COPD heterogeneity is evident at the biological level, particularly in the inflammatory patterns observed across patients. Emerging research emphasizes endotypes defined by distinct biological mechanisms, including neutrophilic inflammation, eosinophilic airway involvement, or specific genetic deficiencies like α1-antitrypsin deficiency [1]. These endotypes demonstrate superior predictive value for therapeutic responses compared to clinical phenotypes alone.
The eosinophilic endotype in COPD, characterized by elevated blood or sputum eosinophil counts, has gained particular attention due to its implications for inhaled corticosteroid (ICS) responsiveness. Similarly, biomarkers encompassing blood eosinophil counts, serum C-reactive protein, and sputum transcriptomics are progressively being implemented for patient stratification and guidance of targeted therapies, including inhaled corticosteroids or biologics [1].
The "treatable traits" framework represents a practical approach to implementing precision medicine in COPD by addressing modifiable factors beyond airflow limitation, such as comorbidities, psychosocial determinants, and exacerbation triggers [1]. This strategy moves beyond the traditional one-dimensional focus on FEV1 improvement to embrace a multidimensional approach to patient management.
Table 2: Major COPD Endotypes and Their Biomarkers
| COPD Endotype | Defining Biological Mechanism | Key Biomarkers | Therapeutic Implications |
|---|---|---|---|
| Eosinophilic | Type 2 inflammation | Blood/sputum eosinophilia | ICS responsiveness |
| Neutrophilic | Neutrophil-dominated inflammation, often with infection | Sputum neutrophils, IL-8, NLRP3 inflammasome activation | Macrolides, potentially phosphodiesterase-4 inhibitors |
| Paucigranulocytic | Minimal inflammatory cell infiltration | Normal inflammatory cell counts | Limited anti-inflammatory benefit |
| α1-antitrypsin deficiency | Protease-antiprotease imbalance | Low AAT levels, specific genetic variants | AAT augmentation therapy |
Allergic Disease Endotypes: From Skin to Systemic Inflammation
Atopic Dermatitis Endotypes
Atopic dermatitis (AD) exemplifies the heterogeneity within allergic conditions, with emerging research revealing distinct molecular endotypes beneath the common clinical presentation. A comprehensive proteomic profiling study of Japanese adults with moderate-to-severe AD analyzed 1,248 serum proteins and identified two stable and reproducible patient clusters characterized by high (ADHI) and low (ADLO) inflammatory profiles [11].
Both clusters showed upregulation of canonical AD inflammatory mediators—including IL-13, IL-19, pulmonary and activation-regulated chemokine (PARC), thymus and activation-regulated chemokine (TARC), CCL22, CCL26, and CCL27—but with significantly greater upregulation in the ADHI cluster [11]. Additionally, the ADHI cluster exhibited upregulation of proteins not typically associated with AD-related inflammation and was associated with protein networks representing a range of immune and non-immune pathways. These dysregulated protein signatures correlated with skin-based disease severity scores, providing a molecular basis for the clinical variability observed in AD [11].
Genetic and Epigenetic Foundations of Allergic Endotypes
Research into the genetic contributions to allergic endotypes has revealed that epigenetic mechanisms mediate the interaction between genetic susceptibility and environmental exposures in shaping disease expression. A study of 284 children from the Urban Environment and Childhood Asthma (URECA) birth cohort identified three DNA methylation (DNAm) signatures associated with allergic phenotypes [23]. These signatures reflected three cardinal endotypes of asthma:
- Inhibited immune response to microbes
- Impaired epithelial barrier integrity
- Activated type 2 immune pathways [23]
The joint SNP heritability of each signature was significant (0.21, 0.26, and 0.17 respectively), indicating that genetic variation contributes substantially to these epigenetic signatures of allergic phenotypes [23]. This suggests that susceptibility to developing specific asthma endotypes is present at birth and poised to mediate individual epigenetic responses to early-life environments.
Methodologies for Endotype Discovery: A Technical Guide
Omics Technologies and Bioinformatics Approaches
The discovery and validation of disease endotypes rely heavily on advanced omics technologies and sophisticated bioinformatics pipelines. Transcriptomic analyses typically utilize RT-qPCR, DNA microarrays, and increasingly, RNA-Seq to profile gene expression patterns in relevant tissues [21]. Proteomic platforms like the Olink Explore 1536 assay enable comprehensive profiling of circulating proteins, providing insights into the systemic inflammatory state associated with different endotypes [11].
The analytical workflow for endotype discovery generally involves multiple steps:
- Unsupervised clustering (k-means, hierarchical clustering) to identify patient subgroups based on molecular data
- Differential expression analysis to define molecular signatures distinguishing clusters
- Network analysis (weighted gene co-expression network analysis) to identify coordinated protein or gene modules
- Validation in independent cohorts to ensure reproducibility [11]
For clustering analysis, determining the optimal number of clusters is critical. Researchers typically use methods like the within-cluster sum of squares (WCSS) elbow plot and cluster stability assessment across different parameters to establish the most biologically plausible and reproducible clustering scheme [11].
Integration of Real-World Data and Knowledge Graphs
A emerging methodology in endotype research involves linking electronic health records (EHRs) to biomedical knowledge graphs (BKGs) to create comprehensive patient representations that integrate clinical and molecular data [24]. This approach was applied to atopic dermatitis, mapping EHR data from over 107 million U.S. patients to the integrative Biomedical Knowledge Hub (iBKH), which contains 2,384,501 entities from 18 publicly available biomedical databases [24].
This integration enabled the identification of seven distinct AD subgroups each characterized by clinical and genomic features, demonstrating how computational approaches can uncover disease heterogeneity from real-world data [24]. Graph machine learning applied to these connected data sources facilitates the interpretation and extension of findings, particularly in disease subtype identification with molecular data contained in the BKG.
Experimental Protocols for Key Studies
Protocol 1: Sputum Transcriptomic Endotyping in Asthma
Objective: To identify asthma endotypes based on gene expression profiles in induced sputum.
Sample Collection:
- Collect induced sputum using hypertonic saline (3-5%) inhalation
- Process samples within 2 hours of collection using dithiothreitol (DTT) to dissolve mucus
- Separate supernatant and cell pellet by centrifugation
- Count differential cell counts to determine inflammatory cell profile
RNA Extraction and Quality Control:
- Extract total RNA from cell pellet using commercial kits with DNase treatment
- Assess RNA quality using Bioanalyzer or TapeStation (RIN >7.0 required)
- Quantify RNA concentration by fluorometry
Transcriptomic Profiling:
- Perform whole-genome gene expression profiling using RNA-Seq or microarrays
- For RNA-Seq: Library preparation using poly-A selection, sequence on Illumina platform (minimum 30 million reads per sample)
- Alternatively, use RT-qPCR for targeted gene expression analysis of key cytokines (IL-4, IL-5, IL-13, etc.)
Bioinformatic Analysis:
- Preprocess raw data: quality trimming, adapter removal, alignment to reference genome
- Perform normalization (TPM for RNA-Seq, RMA for microarrays)
- Conduct differential expression analysis (DESeq2, limma)
- Apply unsupervised clustering (k-means, hierarchical) to identify transcriptional phenotypes
- Perform pathway enrichment analysis (Gene Set Enrichment Analysis, Gene Set Variation Analysis) [21]
Protocol 2: Serum Proteomic Endotyping in Atopic Dermatitis
Objective: To identify molecular endotypes in moderate-to-severe atopic dermatitis based on circulating protein profiles.
Sample Collection and Preparation:
- Collect blood serum samples after appropriate washout periods for systemic and topical therapies (4-week systemic, 2-week topical)
- Use serum separator tubes, allow to clot for 30 minutes, centrifuge at 1,500 × g for 15 minutes
- Aliquot supernatant and store at -70°C until analysis
- Include healthy control samples matched for age and sex
Proteomic Profiling:
- Use Olink Explore 1536 panel following manufacturer's specifications
- Platform combines antibody-based immunoassay with proximity extension assay technology
- Signal detection via next-generation sequencing (Illumina NovaSeq6000)
- Include appropriate controls and calibrators across runs
Data Processing and Normalization:
- Normalize protein expression values relative to plate controls to generate Normalized Protein Expression (NPX) values
- Perform quality control filtering: exclude proteins with coefficient of variation <20%
- Typically, ~1,200 protein analytes remain for downstream analysis after QC
Cluster Analysis and Validation:
- Apply k-means clustering to proteomic data
- Determine optimal cluster number using within-cluster sum of squares (WCSS) elbow method
- Assess cluster stability by including/excluding healthy controls and comparing assignments
- Validate clusters through differential expression analysis and correlation with clinical parameters [11]
Research Reagent Solutions
Table 3: Essential Research Reagents for Endotyping Studies
| Reagent/Category | Specific Examples | Application in Endotyping |
|---|---|---|
| Transcriptomics Platforms | RNA-Seq (Illumina), RT-qPCR, Microarrays | Gene expression profiling for molecular classification |
| Proteomic Assays | Olink Explore 1536, SOMAscan, Mass Spectrometry | Comprehensive protein profiling for endotype identification |
| Single-Cell Technologies | 10X Genomics, Parse Biosciences | Cell-type specific expression analysis at single-cell resolution |
| Epigenetic Tools | Illumina MethylationEPIC array, ATAC-Seq | DNA methylation profiling and chromatin accessibility mapping |
| Bioinformatics Tools | DESeq2, Seurat, Weighted Gene Co-expression Network Analysis | Differential expression, clustering, and network analysis |
| Cell Sorting Technologies | FACS, MACS | Immune cell isolation and characterization |
| Biomarker Assays | ELISA, Luminex, Meso Scale Discovery | Validation of key protein biomarkers in patient samples |
Signaling Pathways and Molecular Networks
The following diagrams illustrate key signaling pathways and molecular networks implicated in respiratory and allergic disease endotypes.
Diagram 1: T2-High Inflammation Pathway in Asthma
Diagram 2: Endotype Discovery Workflow
The study of endotypes in asthma, COPD, and allergic diseases represents a fundamental shift in how we conceptualize, classify, and treat these complex conditions. Moving beyond superficial clinical phenotypes to underlying biological mechanisms holds the promise of truly personalized medicine in respiratory and allergic diseases. The integration of multi-omics data, together with advanced computational approaches, is progressively revealing the intricate molecular architecture of disease heterogeneity.
For drug development professionals, the endotype framework offers opportunities to design more targeted clinical trials with enriched patient populations likely to respond to specific mechanism-based therapies. The ongoing development of accessible biomarkers for endotype identification will be crucial for translating these research insights into clinical practice.
Future directions in the field include the application of machine learning and artificial intelligence to dynamic phenotyping, the integration of real-world evidence with molecular data through biomedical knowledge graphs, and a focus on early disease pathogenesis to enable preventive strategies [1] [24]. As these efforts mature, the vision of delivering the right treatment to the right patient at the right time moves closer to reality, potentially transforming outcomes for millions of patients with respiratory and allergic diseases worldwide.
The Systems Biology Toolkit: Methodologies for Endotype Discovery and Characterization
The pursuit of disease endotypes—distinct subtypes of conditions defined by unique functional or pathobiological mechanisms—represents a core challenge in modern precision medicine. Traditional single-omics approaches have provided valuable but fragmented insights into disease mechanisms. Multi-omics integration combines data from genomic, transcriptomic, proteomic, and metabolomic layers to create a holistic model of biological systems, enabling the identification of these clinically meaningful endotypes [25] [26]. Systems biology provides the foundational framework for this integration, treating diseases not as isolated defects in single components but as emergent properties of perturbed molecular networks [27] [28].
The clinical imperative is clear: complex diseases such as cancer, autoimmune disorders, and metabolic conditions exhibit profound heterogeneity in their clinical presentation and therapeutic response. Multi-omics profiling moves beyond superficial symptom-based classifications to reveal the molecular architecture underlying this heterogeneity [26] [29]. For example, integrating clinical parameters with multi-omic profiles has successfully identified molecularly distinct asthma endotypes with divergent therapeutic responses [30]. This approach facilitates a transition from reactive medicine to predictive, personalized healthcare by uncovering the fundamental biological processes that drive disease progression in specific patient subsets.
Multi-Omics Technologies and Data Characteristics
Core Omics Technologies and Their Measurements
Each omics layer captures a distinct aspect of biological organization, together forming a comprehensive picture of the flow of genetic information to functional phenotype.
Genomics identifies alterations at the DNA level, including single nucleotide polymorphisms (SNPs), copy number variations (CNVs), and mutations through whole exome sequencing (WES) and whole genome sequencing (WGS). Landmark projects like The Cancer Genome Atlas (TCGA) have mapped the genomic landscape of numerous cancers, revealing actionable alterations in approximately 37% of tumors [26].
Transcriptomics examines RNA expression patterns using microarray or RNA sequencing (RNA-seq) technologies, capturing mRNA, long non-coding RNAs (lncRNAs), and miRNAs. Clinically validated gene-expression signatures such as Oncotype DX (21-gene) and MammaPrint (70-gene) demonstrate the utility of transcriptomic biomarkers in guiding adjuvant chemotherapy decisions in breast cancer [26].
Proteomics investigates protein abundance, post-translational modifications (e.g., phosphorylation, acetylation), and interactions using mass spectrometry (MS) and liquid chromatography–mass spectrometry (LC-MS). Proteomic data can reveal functional subtypes and druggable vulnerabilities missed by genomics alone [26].
Metabolomics focuses on the dynamic complement of small molecule metabolites, including carbohydrates, lipids, peptides, and nucleosides, typically analyzed via MS, LC-MS, or gas chromatography–mass spectrometry (GC-MS). Metabolites represent the most downstream products of cellular processes, providing a direct readout of physiological state and metabolic pathway activity [25] [26].
Experimental Design for Multi-Omics Studies
Robust multi-omics integration begins with careful experimental design to minimize technical artifacts and enable valid biological inference. Key considerations include:
- Sample Selection and Handling: The ideal biological matrices (e.g., blood, plasma, tissues) allow for concurrent generation of multiple omics data types from the same sample set. Sample collection, processing, and storage protocols must be optimized to preserve the integrity of labile molecules like RNA and metabolites [25].
- Replication Strategy: The experimental design must account for biological, technical, analytical, and environmental replication to ensure statistical rigor and reproducibility.
- Meta-data Collection: Comprehensive meta-information about samples, experimental conditions, and processing protocols is essential for contextualizing multi-omics findings and ensuring their reinterpretation [25].
Computational Methods and Integration Strategies
Data Processing and Horizontal Integration
Before cross-omics integration, each individual omics dataset requires extensive preprocessing and quality control. This "horizontal integration" ensures data quality within each molecular layer [26]. Key steps include:
- Quality Control and Normalization: Removal of technical artifacts, batch effect correction, and normalization to account for varying library sizes or signal intensities.
- Feature Selection: Identification of biologically relevant features (e.g., differentially expressed genes, abundant proteins) to reduce dimensionality and computational complexity while retaining meaningful biological signal.
- Intra-Omics Analysis: Initial analysis within each omics layer to identify patterns, clusters, or associations with phenotypes of interest.
Vertical Integration Approaches
"Vertical integration" combines processed data from different omics layers to uncover interactions and relationships across molecular levels [26]. Several computational approaches exist:
- Network-Based Integration: This approach maps multiple omics datasets onto shared biochemical networks (e.g., metabolic pathways, protein-protein interaction networks) to improve mechanistic understanding. Analytes are connected based on known interactions, such as transcription factors mapped to their target transcripts or enzymes mapped to their metabolic substrates and products [29] [28].
- Concatenation-Based Methods: These methods merge diverse omics datasets into a single combined matrix for subsequent multivariate analysis. While straightforward, this approach requires careful handling of scale and distribution differences between data types.
- Model-Based Approaches: Methods like Multi-Omics Factor Analysis (MOFA+) use statistical models to decompose multi-omics data into a set of latent factors that represent shared sources of variation across data modalities [31].
- Machine Learning and AI: Advanced computational methods, including supervised and unsupervised machine learning, are increasingly used to detect intricate patterns and dependencies within multi-omics datasets [26] [32].
Table 1: Comparison of Multi-Omics Integration Methods
| Method Type | Representative Tools | Key Principles | Advantages | Limitations |
|---|---|---|---|---|
| Network-Based | Pathway Tools [33], Cytoscape | Maps omics data onto known biological networks | Provides mechanistic context, intuitive visualization | Limited to known interactions, less discovery potential |
| Concatenation-Based | MANAclust [30] | Merges datasets into a combined matrix | Simple implementation, preserves all information | Sensitive to data scaling, high dimensionality |
| Factorization-Based | MOFA+ [31], intNMF | Decomposes data into latent factors | Identifies co-varying features, handles missing data | Linear assumptions may not capture complex interactions |
| Non-Linear Dimensionality Reduction | GAUDI [31] | Uses UMAP embeddings to capture non-linear relationships | Handles complex data structures, powerful clustering | Parameter sensitivity, computational intensity |
Advanced Integration Tools and Visualization
Effective visualization is critical for interpreting complex multi-omics data. Tools like the Pathway Tools Cellular Overview enable simultaneous visualization of up to four omics data types on organism-scale metabolic network diagrams, using different visual channels (e.g., reaction arrow color and thickness, metabolite node color and thickness) to represent different data types [33]. Emerging methods like GAUDI (Group Aggregation via UMAP Data Integration) leverage independent UMAP embeddings for concurrent analysis of multiple data types, effectively uncovering non-linear relationships among different omics layers and facilitating intuitive cluster identification [31].
Experimental Protocols for Multi-Omics Biomarker Discovery
A Protocol for Predictive Biomarker Identification
The following protocol outlines a machine learning pipeline for identifying predictive protein biomarkers for complex diseases, based on methodology successfully applied to UK Biobank data [34]:
- Cohort Selection and Matching: Identify patient cohorts with the disease of interest and select age/sex-matched controls. Divide patients into incident (diagnosed after assessment) and prevalent (already diagnosed at assessment) cases.
- Multi-Omics Data Collection: Acquire genomic (e.g., 90 million genetic variants), proteomic (e.g., 1,453 proteins), and metabolomic (e.g., 325 metabolites) data for all subjects.
- Data Preprocessing: Clean data by removing outliers and technical artifacts. Impute missing values using appropriate methods (e.g., k-nearest neighbors). Normalize data to account for technical variance.
- Feature Selection: Apply feature selection algorithms to identify the most discriminative molecules for separating cases from controls. For genomics, use established polygenic risk scores where available.
- Model Training and Validation: Train classification models (e.g., logistic regression, random forests) using tenfold cross-validation on training datasets. Compare results on holdout test sets to evaluate performance.
- Performance Evaluation: Generate receiver operating characteristic (ROC) curves and calculate areas under the curve (AUCs) to assess predictive performance. Determine the minimal number of biomarkers needed for clinically significant prediction (AUC ≥0.8).
- Biological Interpretation: Perform functional enrichment analysis (e.g., Gene Ontology analysis) on the top protein biomarkers to identify significantly enriched pathways and biological processes.
Protocol for Clinical Endotype Discovery Using MANAclust
MANAclust (Merged Affinity Network Association Clustering) provides an automated pipeline for integrating clinical and multi-omics profiles to identify disease endotypes [30]:
- Data Collection: Assemble comprehensive datasets including clinical parameters (e.g., age, symptom scores, treatment response) and multi-omics data (genomics, transcriptomics, proteomics, metabolomics).
- Feature Selection: Apply MANAclust's inter-variable relative information algorithm to select meaningful categorical and numerical features from both clinical and molecular data.
- Affinity Network Construction: Build affinity networks for each data type based on similarity metrics between samples.
- Network Merging: Merge affinity networks into a single combined network that incorporates information from all data modalities.
- Unsupervised Clustering: Perform clustering on the merged network to identify patient subgroups with distinct clinical and molecular profiles.
- Cluster Validation: Validate clusters by assessing their association with clinical outcomes, survival differences, or treatment responses.
- Molecular Characterization: Identify the key molecular features (e.g., specific genetic variants, protein abundances, metabolite levels) that distinguish each cluster, defining the endotype.
Table 2: Essential Research Reagents and Computational Tools for Multi-Omics Studies
| Category | Item | Specification/Function |
|---|---|---|
| Sample Collection | PAXgene Blood RNA Tubes | Stabilizes intracellular RNA for transcriptomics |
| EDTA or Citrate Plasma Tubes | Preserves proteins and metabolites for proteomics/metabolomics | |
| Formalin-Fixed Paraffin-Embedded (FFPE) Tissue | Preserves tissue architecture for spatial omics (with limitations for some assays) [25] | |
| Sequencing & Analysis | Next-Generation Sequencer (Illumina, PacBio) | Whole genome, exome, and transcriptome sequencing [26] |
| SWATH-MS Kit | Data-independent acquisition proteomics for comprehensive protein quantification [25] | |
| UPLC-MS/MS System | Ultra-performance liquid chromatography tandem mass spectrometry for metabolomics [25] | |
| Computational Tools | Pathway Tools | Metabolic network visualization and multi-omics painting [33] |
| MANAclust | Joint clustering of clinical and multi-omics data [30] | |
| GAUDI | Non-linear integration using UMAP embeddings [31] | |
| DriverDBv4, HCCDBv2 | Multi-omics databases for specific cancer types [26] |
Applications in Disease Endotype Identification and Clinical Translation
Biomarker Performance Across Omics Layers
Comparative analyses of different omics layers have yielded insights into their relative strengths for predictive applications. A comprehensive assessment of genomic, proteomic, and metabolomic data from the UK Biobank revealed that proteins demonstrated superior predictive performance for both incident and prevalent cases of nine complex diseases, including rheumatoid arthritis, type 2 diabetes, and atherosclerotic vascular disease [34]. The median AUC for incidence prediction using just five proteins was 0.79, compared to 0.70 for metabolites and 0.57 for genetic variants. This suggests that a limited panel of proteins may suffice for both predicting incident disease and diagnosing prevalent conditions, though the optimal biomarker combination is context-dependent.
Table 3: Predictive Performance of Different Omics Layers for Complex Diseases
| Omics Layer | Median AUC (Incidence) | Median AUC (Prevalence) | Number of Features for AUC ≥0.8 | Representative Biomarkers |
|---|---|---|---|---|
| Proteomics | 0.79 (0.65-0.86) | 0.84 (0.70-0.91) | 5 or fewer for most diseases | MMP12, TNFRSF10B, HAVCR1 for ASVD [34] |
| Metabolomics | 0.70 (0.62-0.80) | 0.86 (0.65-0.90) | Variable by disease | 2-hydroxyglutarate for IDH1/2-mutant gliomas [26] |
| Genomics | 0.57 (0.53-0.67) | 0.60 (0.49-0.70) | Often cannot reach 0.8 with PRS alone | Tumor Mutational Burden for immunotherapy response [26] |
Case Studies in Endotype Discovery
Asthma Endotyping: Application of MANAclust to a clinically and multi-omically phenotyped asthma cohort revealed clinically and molecularly distinct clusters, including heterogeneous groups of "healthy controls" and viral and allergy-driven subsets of asthmatic subjects. Importantly, subjects with similar clinical presentations showed disparate molecular profiles, highlighting the need for additional molecular testing to uncover true asthma endotypes [30].
Cancer Subtyping and Survival Prediction: GAUDI has demonstrated exceptional performance in identifying clinically relevant cancer subtypes from TCGA multi-omics data. In acute myeloid leukemia (AML), GAUDI identified a small high-risk group with a median survival of only 89 days—a threshold not reached by other integration methods. This precision in identifying extreme survival groups enables more targeted therapeutic approaches for high-risk patients [31].
The Cancer Biomarker Atlas: The creation of an interactive atlas of genomic, proteomic, and metabolomic biomarkers enables systematic prioritization of biomarker types and numbers for different complex diseases. This resource facilitates the selection of optimal biomarker panels based on the specific clinical context and required sensitivity/specificity trade-offs [34].
Future Perspectives and Challenges
As multi-omics integration continues to evolve, several key trends and challenges are shaping its trajectory:
- Single-Cell and Spatial Multi-Omics: The field is rapidly advancing toward single-cell resolution, enabling the characterization of cellular heterogeneity within tissues. Spatial multi-omics technologies further add geographical context, preserving the architectural relationships between cells that are critical for understanding tissue function and disease pathology [26] [32].
- Data Harmonization and Standardization: The integration of multiple discrepant data sources remains a significant challenge. Advances in computational methods, particularly data harmonization techniques, are essential for unifying disparate datasets with varying formats, scales, and biological contexts [32].
- AI and Machine Learning: Artificial intelligence and machine learning are becoming increasingly sophisticated at detecting intricate patterns and dependencies within multi-omics datasets. The development of purpose-built analysis tools specifically designed for multi-omics data will be crucial for extracting meaningful biological insights [26] [32].
- Clinical Implementation: The translation of multi-omics discoveries to clinical practice requires addressing issues of reproducibility, validation in diverse patient populations, and the development of clinically feasible assay platforms. Liquid biopsies exemplify the clinical impact of multi-omics, analyzing biomarkers like cell-free DNA, RNA, proteins, and metabolites non-invasively for early disease detection and treatment monitoring [32].
The ongoing integration of multi-omics data with clinical measurements promises to revolutionize patient stratification, disease prognosis, and treatment optimization. By embracing collaborative efforts across academia, industry, and regulatory bodies, the field will continue to advance personalized medicine, offering deeper insights into human health and disease [29] [32].
Leveraging Single-Cell Technologies to Map Cellular Heterogeneity and Immune Profiles
The emergence of single-cell technologies represents a paradigm shift in systems biology, enabling unprecedented resolution in the study of cellular heterogeneity and immune responses. These approaches have become indispensable for identifying disease endotypes—distinct functional or pathobiological mechanisms underlying clinical presentations—by moving beyond tissue-level averaging to reveal cell-to-cell variation at genomic, transcriptomic, and epigenomic levels. Single-cell RNA sequencing (scRNA-seq) specifically allows researchers to analyze complex cell mixtures correct to a single cell and single molecule, making it uniquely qualified to deconstruct immune reactions in various diseases [35]. This technical capability is fundamentally advancing how researchers investigate the immunological, inflammatory, metabolic, and remodeling pathways that explain disease mechanisms, facilitating a more precise understanding of pathophysiology that aligns with the goals of precision medicine [8].
The central premise of single-cell approaches in systems immunology is that comprehensive profiling of individual cells within tissues reveals previously obscured cellular states and interactions that contribute to disease heterogeneity. For instance, in autoimmune conditions like systemic sclerosis (SSc), patients present with diverse organ manifestations that complicate clinical management. Single-cell technologies enable researchers to link specific immune cell abnormalities to particular clinical presentations, moving beyond generic disease classifications to identify mechanistically distinct endotypes [36]. Similarly, in cancer biology, scRNA-seq has detailed the cellular composition of the tumor microenvironment (TME), revealing how distinct endothelial cell subpopulations contribute differently to disease progression across breast cancer subtypes [37]. This granular understanding of cellular diversity provides the foundation for identifying therapeutic targets tailored to specific disease mechanisms.
Core Single-Cell Methodologies and Experimental Workflows
Fundamental Technical Approaches
A standard scRNA-seq protocol encompasses multiple critical steps: single-cell isolation, lysis, reverse transcription, cDNA amplification, library preparation, sequencing, and computational analysis [35]. Among these, cell isolation, library construction, and data analysis represent particularly crucial phases that significantly impact experimental outcomes. Current cell isolation methods include limiting dilution, micromanipulation, flow-activated cell sorting (FACS), laser capture microdissection (LCM), microdroplets, and microfluidics [35]. Each approach offers distinct advantages and limitations regarding throughput, viability, and preservation of cellular states.
Library construction methods substantially influence data quality and applicability. Full-length transcript sequencing approaches like SMART-seq2 enable detection of more genes within the same sample and allow for the identification of rare transcripts, selective transcription isomers, and single nucleotide polymorphisms [35]. However, these methods typically have lower cell throughput. In contrast, non-full-length sequencing methods (e.g., 5' or 3' sequencing such as Drop-Seq and STRT-seq) offer higher throughput and lower cost, making them advantageous for comparing different groups of cells where larger cell numbers are required [35]. The introduction of unique molecular identifiers (UMIs) has been particularly valuable for accurate quantification of different transcripts from the same gene, addressing amplification biases that can distort expression measurements [35].
Recent methodological innovations have expanded the analytical possibilities of single-cell technologies. Spatial transcriptomics integrates positional information with gene expression data, preserving crucial contextual information about cellular neighborhoods and tissue organization [38]. Multi-omics approaches simultaneously capture different molecular layers from the same cells, such as combining transcriptomic with epigenomic profiling through technologies like single-cell ATAC-seq [35]. CITE-seq (Cellular Indexing of Transcriptomes and Epitopes by Sequencing) enables simultaneous measurement of transcriptome and surface protein expression, providing complementary information that enhances cell type identification and characterization [36]. These advanced methodologies offer increasingly comprehensive views of cellular states and functions within complex tissues.
Experimental Workflow Specification
The following diagram illustrates a generalized single-cell RNA sequencing workflow, from tissue preparation through data analysis:
Figure 1: Single-Cell RNA Sequencing Workflow
Specialized Considerations for Tissue-Specific Applications
Different tissue types present unique challenges for single-cell analysis that require methodological adaptations. Tendon tissues, for example, possess a dense collagenous structure where Type I collagen comprises approximately 86% of the content, creating a rigid extracellular matrix that prevents conventional enzymatic digestion protocols from efficiently releasing functional cells [38]. The dissociation process often generates filamentous collagen residues that compromise droplet capture efficiency, while mechanical shear forces may induce aberrant expression of stress-response genes, introducing transcriptomic bias [38]. Furthermore, transitional zones like the enthesis (tendon-bone interface) contain heterogeneous cell populations (tenocytes, chondrocytes, osteoblasts) with different physicochemical properties, making dissociation homogeneity challenging and potentially leading to loss or enrichment bias of specific subpopulations [38].
Similar tissue-specific considerations apply across biological systems. In cancer research, the complex cellular ecosystem of the tumor microenvironment requires careful processing to preserve vulnerable cell types like endothelial cells and immune populations [37]. For blood-based immunology studies, preservation of cell viability and surface epitopes is crucial for accurate immune cell profiling [36]. These tissue-specific requirements necessitate optimized protocols for dissociation, cell capture, and library preparation to ensure representative sampling of all cell populations present in the original tissue.
Analytical Frameworks for Immune Cell Mapping
Computational Pipelines and Cell Type Annotation
Bioinformatic analysis of single-cell data requires specialized computational tools and approaches. After sequencing, raw data undergoes quality control to remove technical artifacts, including inviable cells, doublets (two cells in one droplet), and environmental RNA that frequently contaminate the raw data [35]. Normalization methods address biases introduced during reverse transcription and amplification that can result from factors like gene length and sequencing depth [35]. Subsequent analytical steps typically include dimensional reduction (using techniques like PCA or UMAP), unsupervised clustering, and differential expression analysis to identify distinct cell populations and their marker genes.
Immune cell annotation presents particular challenges due to the high heterogeneity and sparsity of scRNA-Seq data, as well as the similarity in gene expression among immune cell types [39]. To address this, specialized computational tools like sc-ImmuCC have been developed for hierarchical annotation of immune cell types from scRNA-Seq data based on optimized gene sets and the ssGSEA (single-sample Gene Set Enrichment Analysis) algorithm [39]. This approach simulates the natural differentiation of immune cells through a three-layer annotation system that can identify nine major immune cell types and 29 cell subtypes, achieving an average accuracy of 71-90% across different tissue datasets [39]. The hierarchical strategy first annotates major immune cell types (T cells, B cells, monocytes, macrophages, dendritic cells, natural killer cells, innate lymphoid cells, mast cells, and neutrophils), then subtypes within each major type, reducing interference between similar cell types and improving annotation accuracy.
Advanced Analytical Techniques
Beyond basic cell type identification, single-cell data enables more sophisticated analytical approaches that provide insights into dynamic biological processes. Trajectory inference (or pseudotemporal ordering) algorithms reconstruct cellular transitions along differentiation pathways, allowing researchers to map the progression from progenitor to mature cell states [38]. In tendon research, for example, this approach has revealed hierarchical maturation of T cells from CD4-CD8- precursors to effector subsets, while neutrophils bifurcate into phagocytosis-specialized and oxidative phosphorylation-driven functional branches [40]. These analyses provide critical insights into the cellular dynamics underlying tissue homeostasis and disease processes.
Cell-cell communication analysis represents another powerful application of single-cell data. By examining ligand-receptor interactions across different cell types, researchers can infer signaling networks within tissues. In breast cancer research, interactome analysis has revealed novel and subtype-specific communications between endothelial cell subsets and immune cells, particularly CD8+ T cells and macrophages [37]. Experimental validation demonstrated that endothelial cells overexpressing APP can mediate the M2 polarization of macrophages, underscoring diverse immunomodulatory roles for endothelial cell subsets across different cancer contexts [37]. Such analyses provide mechanistic insights into how different cell types coordinate their functions within complex tissue environments.
Applications in Disease Endotyping and Immune Profiling
Cancer Heterogeneity and Microenvironment Mapping
Single-cell technologies have revolutionized our understanding of cancer heterogeneity and tumor microenvironment composition. In breast cancer, scRNA-seq analysis of 98,000 cells from healthy, primary tumor, and lymph node metastatic tissues revealed pronounced molecular and cellular heterogeneity that fundamentally dictates prognosis [37]. This approach identified two previously uncharacterized, tumor-enriched endothelial cell subtypes (designated EC4 and EC5) that demonstrate subtype-specific functional adaptations and prognostic significance [37]. EC4 cells, highly prevalent across breast cancer subtypes, are principally characterized by antigen presentation, immune cell recruitment, and pro-inflammatory signaling, while EC5 cells exhibit robust extracellular matrix remodeling and potent tumor angiogenesis [37]. These findings establish endothelial cells as active and heterogeneous modulators of the tumor microenvironment, identifying specific therapeutic vulnerabilities within the tumor vasculature.
The power of single-cell approaches in cancer research extends to understanding metastatic processes and immune evasion mechanisms. Comparison of primary tumors with lymph node metastases in breast cancer revealed conserved endothelial programming mechanisms across breast cancer subtypes coexisting with distinct tumor microenvironment-driven transcriptional adaptations [37]. Such findings provide critical insights into the complex interplay between novel endothelial cell subtypes and the immune microenvironment in cancer progression and metastasis, offering a foundational blueprint for developing future precision immunotherapeutic strategies [37].
Autoimmune and Inflammatory Disease Endotyping
In autoimmune diseases, single-cell technologies have enabled the identification of distinct cellular endotypes underlying clinical heterogeneity. In systemic sclerosis (SSc), single-cell profiling of peripheral blood mononuclear cells from 21 treatment-naïve patients revealed specific immune cell abnormalities associated with different organ complications [36]. Researchers identified a subset of EGR1+ CD14+ monocytes in patients with scleroderma renal crisis (SRC), the most severe acute organ complication [36]. These monocytes activate NF-kB signaling and differentiate into tissue-damaging macrophages that accumulate at sites of tissue injury [36]. Additionally, a CD8+ T cell subset with type II interferon signature was identified in the peripheral blood and lung tissue of patients with progressive interstitial lung disease (ILD), suggesting that chemokine-driven migration of these cells contributes to ILD progression [36].
The analytical process for identifying these disease-relevant cell subsets typically involves multiple steps, as illustrated in the following diagram:
Figure 2: Disease Endotype Identification Workflow
Infectious Disease and Comparative Immunology
Single-cell technologies have also provided novel insights into host-pathogen interactions and evolutionary immunology. Research on the large yellow croaker (Larimichthys crocea), a marine teleost fish, generated the first single-cell transcriptomic atlas of spleen tissue, profiling 10 major immune-cell types and 57 transcriptionally distinct subpopulations [40]. This study revealed that Pseudomonas infection provoked dynamic cellular reorganization, evidenced by a 2.7-fold increase of neutrophils, a 20.85% reduction in mature B cells through cell-death pathways, and an expansion of progenitor B cells suggestive of hematopoietic compensation [40]. The research also identified evolutionary insights through transitional cell types, including a TCR/BCR co-expressing T-B chimera and BCR-expressing macrophages, suggesting potential cross-lineage functional plasticity and possible links to hypotheses on the evolutionary origin of B cells from phagocytic ancestors [40].
These findings in comparative immunology highlight how single-cell approaches can reveal fundamental principles of immune system organization and response patterns that are conserved across species, while also identifying lineage-specific adaptations. The identification of core genes that were universally upregulated across immune compartments in response to infection indicates conserved antibacterial strategies that may represent promising targets for therapeutic intervention [40].
Essential Research Reagent Solutions
The successful implementation of single-cell technologies requires specialized reagents and platforms optimized for various aspects of the experimental workflow. The following table summarizes key solutions and their applications in single-cell research:
Table 1: Essential Research Reagent Solutions for Single-Cell Technologies
| Reagent Category | Specific Examples | Function & Application | Technical Considerations |
|---|---|---|---|
| Cell Isolation Systems | 10x Genomics Chromium, Fluidigm C1, BD Rhapsody | Single-cell partitioning, barcoding, and library preparation | Droplet-based vs. plate-based; throughput vs. sequencing depth |
| Enzymatic Dissociation Kits | Tissue-specific dissociation cocktails (e.g., collagenase blends for tendon) | Release viable single cells from tissue matrices | Optimization required to minimize stress responses and preserve cell viability |
| Viability Stains | Propidium iodide, DAPI, SYTOX dyes | Distinguish live/dead cells during quality control | Membrane integrity assessment; exclusion from viable cells |
| Multimodal Profiling Reagents | CITE-seq antibodies, cell hashing reagents | Simultaneous protein and transcriptome measurement | Antibody validation crucial; requires unique oligonucleotide barcodes |
| Amplification & Library Prep Kits | SMART-seq2, Smart-seq3, MATQ-seq | cDNA amplification from single cells | Full-length vs. 3'/5' enriched; impacts on gene detection sensitivity |
| Spatial Transcriptomics | 10x Visium, Slide-seq, MERFISH | Preservation of spatial context in gene expression | Resolution limits (single-cell vs. multi-cell spots); tissue compatibility |
| Cell Annotation Databases | sc-ImmuCC, SingleR, Garnett | Reference datasets for cell type identification | Species-, tissue-, and disease-specific references improve accuracy |
Quantitative Insights from Single-Cell Studies
Single-cell technologies have generated substantial quantitative data regarding cellular heterogeneity across various biological systems. The following table summarizes key numerical findings from recent studies:
Table 2: Quantitative Cellular Heterogeneity Revealed by Single-Cell Studies
| Biological System | Cell Numbers Profiled | Major Cell Types Identified | Subpopulations/Subtypes | Key Quantitative Findings |
|---|---|---|---|---|
| Breast Cancer Microenvironment [37] | 98,000 cells | 6 major types (T cells, myeloid cells, B cells, EC, fibroblasts, epithelial) | 7 endothelial cell subtypes (EC1-EC7) | Two tumor-enriched EC subtypes (EC4, EC5) with prognostic significance |
| Systemic Sclerosis PBMC [36] | 238,924 cells | 8 major immune populations | 5 CD14+ monocyte subsets, multiple T cell subsets | CD14_EGR1 monocytes enriched in SRC (log2FC: +1.9); CD8+ TEM enriched in ILD |
| Tendon/Enthesis Healing [38] | Variable by study | Tendon stem/progenitor cells, tenocytes, immune cells | Functionally distinct TSPC subpopulations | Rotator cuff repairs show recurrence rates up to 94% within 2 years |
| Large Yellow Croaker Spleen [40] | Not specified | 10 major immune cell types | 57 transcriptionally distinct subpopulations | 2.7-fold neutrophil increase, 20.85% mature B cell reduction post-infection |
| Healthy vs. Primary BC [37] | 97,990 cells total (23,971 ER, 27,143 HER2, 19,848 ER_LN, 27,038 normal) | 6 major cell types across conditions | Endothelial heterogeneity across subtypes | B cells, T cells, myeloid cells significantly enriched in TME vs. normal |
Single-cell technologies have fundamentally transformed our ability to map cellular heterogeneity and immune profiles, providing the resolution necessary to identify distinct disease endotypes within clinically heterogeneous conditions. By moving beyond tissue-level averages to examine individual cells, these approaches have revealed previously unappreciated cellular diversity in cancer, autoimmune diseases, infectious conditions, and developing tissues. The continued refinement of single-cell methodologies—including multimodal integration, spatial context preservation, and computational analytics—promises to further enhance our understanding of the cellular ecosystems underlying health and disease. As these technologies become more accessible and comprehensive, they will increasingly enable the identification of precise therapeutic targets tailored to specific disease mechanisms, advancing the goals of precision medicine across diverse pathological conditions.
Computational and Machine Learning Pipelines for Unsupervised Endotype Identification
Within the framework of systems biology research, the concept of an endotype represents a critical advancement beyond traditional clinical phenotyping. An endotype is defined as a subtype of a health condition characterized by a distinct functional or pathobiological mechanism [41]. This distinction is fundamental; while a phenotype describes a collection of observable clinical characteristics (e.g., symptoms, exacerbation frequency), the endotype explains the underlying biological drivers that give rise to those observable traits [1]. The identification of endotypes is therefore essential for precision medicine, as it enables the move from a "one-size-fits-all" treatment approach to targeted therapies for specific mechanistic pathways [42].
The high degree of heterogeneity in complex diseases—evident in sepsis, asthma, chronic obstructive pulmonary disease (COPD), and immune-mediated inflammatory diseases (IMIDs)—means that patients who appear clinically similar may have vastly different underlying disease processes and, consequently, treatment responses [43] [42]. Unsupervised computational methods are uniquely powerful for endotype discovery because they can identify these distinct molecular subgroups from high-dimensional data without prior assumptions or labels, thus revealing naturally existing biological groupings that might otherwise be obscured [43] [44].
Core Machine Learning Methodologies
The discovery of endotypes relies heavily on a suite of unsupervised machine learning techniques designed to find hidden structure within complex, high-dimensional molecular data.
Unsupervised Learning Algorithms
The following table summarizes the key algorithms and their applications in endotype identification.
Table 1: Core Unsupervised Machine Learning Algorithms for Endotype Discovery
| Algorithm Category | Specific Methods | Primary Function in Endotyping | Key Advantages |
|---|---|---|---|
| Clustering | k-means, Consensus Clustering [43] | Identifies discrete, mutually exclusive patient subgroups based on gene expression or other molecular patterns. | Provides clear patient stratification; consensus methods enhance robustness. |
| Dimensionality Reduction | PCA, t-SNE, UMAP [44] | Reduces data complexity for visualization and reveals global (PCA) or local (t-SNE, UMAP) group structures. | Aids in data quality control and exploratory analysis; simplifies complex datasets. |
| Matrix Factorization | Non-negative Matrix Factorization (NMF) [44] | Decomposes high-dimensional data into metagenes and sample weights, often yielding biologically interpretable components. | Results in non-negative, more interpretable factors that can represent biological pathways. |
| Anomaly Detection | Denoising Autoencoders (DAE) [45] | Isolates rare, biologically relevant events (e.g., circulating tumor cells) in data without prior knowledge of their signature. | Does not require pre-defined event signatures; useful for discovering novel cell types or rare biomarkers. |
End-to-End Computational Pipeline
A typical endotype discovery pipeline involves sequential steps from data acquisition to biological validation [43] [46]. The workflow below illustrates the process of identifying sepsis endotypes from RNA-seq data.
Detailed Experimental Protocols
To ensure reproducibility and provide a clear technical roadmap, this section outlines specific methodologies from seminal endotyping studies.
RNA-seq Meta-Analysis for Sepsis Endotyping
A 2025 meta-analysis established a robust protocol for identifying sepsis endotypes from integrated RNA-seq datasets [43].
Table 2: Key Research Reagents and Computational Tools for Sepsis Endotyping
| Item Name | Type | Function/Application | Implementation Details |
|---|---|---|---|
| SRA Toolkit | Software | Converts sequence read archive (SRA) data to FASTQ format. | Used for initial data retrieval and format conversion. |
| Fastp | Software | Performs quality control on raw sequencing data; trims adapters and removes low-quality reads. | Applied for read processing and filtering. |
| Salmon | Software | Quantifies transcript abundance from processed reads with high accuracy. | Run with GC bias correction and mapping validation options; reference: GRCh38. |
| R package: edgeR | Software | Filters low-expression genes and normalizes count data. | Uses the filterByExpr function for filtering; TMM method for normalization. |
| R package: sva | Software | Corrects for technical batch effects across different studies. | Applies the ComBat-seq function to integrated data from multiple cohorts. |
| R package: ConsensusClusterPlus | Software | Performs unsupervised clustering to identify distinct molecular endotypes. | Run with 100 iterations, 80% subsampling, k-means, Euclidean distance. |
| CIBERSORTx | Software | Deconvolutes immune cell fractions from bulk transcriptome data. | Uses LM22 signature matrix to quantify 22 immune cell types. |
| LASSO Regression | Algorithm | Selects minimal gene features for endotype classification. | Implemented via R caret package with fivefold cross-validation. |
Protocol Steps:
- Data Acquisition and Inclusion Criteria: Systematically search public databases (e.g., MEDLINE, Scopus) for RNA-seq studies of adult sepsis patients. Include only patients meeting Sepsis-3 criteria, analyzing only the initial time point (within 24 hours of admission) [43].
- RNA-seq Data Preprocessing:
- Convert SRA files to FASTQ using SRA Toolkit.
- Perform quality control and adapter trimming with
Fastp. - Quantify gene-level expression using
Salmonwith the GRCh38 human transcriptome as a reference. - Import transcript-level estimates to gene-level counts using
tximportin R. - Exclude samples with mapping rates below 60%.
- Filter low-expression genes using
edgeR::filterByExpr. - Normalize data using the TMM method and correct for batch effects using
sva::ComBat-seq.
- Consensus Clustering for Endotyping:
- Execute unsupervised clustering via
ConsensusClusterPlusin R. - Use 100 resampling iterations, each with 80% subsampling of samples and 100% of features.
- Employ k-means clustering with Euclidean distance.
- Determine the optimal number of clusters (k) by evaluating consensus matrices, cluster consensus values, and the relative change in area under the cumulative distribution function (CDF) curve.
- Execute unsupervised clustering via
- Biological and Clinical Characterization:
- Perform differential expression analysis between endotypes using
limma, defining significant genes as those with an absolute Log2 fold change ≥ 1 and FDR < 0.05. - Conduct Gene Set Enrichment Analysis (GSEA) with the
fgseapackage against Hallmark and Gene Ontology gene sets. - Estimate immune cell abundances using
CIBERSORTxand the LM22 signature matrix. - Assess association with mortality using unadjusted logistic regression models.
- Perform differential expression analysis between endotypes using
- Development and Validation of a Gene Classifier:
- Train a multiclass LASSO regression model using the top 200 differentially expressed genes from each cluster comparison.
- Apply fivefold cross-validation to prevent overfitting and identify a minimal gene classifier.
- Validate the classifier by applying it to an independent external cohort (e.g., a microarray dataset) and reassessing the reproducibility of endotype characteristics and mortality patterns.
Unsupervised Rare Event Detection in Liquid Biopsies
For diseases like cancer, relevant endotypic information can be carried by rare circulating cells. The following protocol uses a Denoising Autoencoder (DAE) for unsupervised rare event detection [45].
Protocol Steps:
- Image Preparation and Tiling:
- Obtain four-channel immunofluorescence (IF) images of peripheral blood samples (channels: DAPI for DNA, cytokeratins for epithelial cells, vimentin for mesenchymal cells, and CD45/CD31 for immune/endothelial cells).
- Divide each image into approximately 2.5 million smaller tiles of 32x32 pixels, a size designed to contain, on average, up to 4 cellular events.
- Denoising Autoencoder (DAE) Training:
- Add uncorrelated Gaussian noise to each tile to create noisy inputs.
- Train a DAE using pairs of clean (target) and noisy (input) tiles. The DAE learns to denoise the input, effectively learning the distribution of common events.
- The reconstruction error (the magnitude of the difference between the DAE's output and the original clean tile) is calculated for each tile and channel. This error is weighted by user-defined channel importance and summed to produce a single "rarity metric" for each tile.
- Rare Event Isolation:
- Rank all tiles based on their rarity metric, from highest (most rare) to lowest.
- Select a top cohort of tiles (e.g., ~2500) for downstream analysis. This cohort is enriched for biologically interesting and rare events, such as circulating tumor cells (CTCs).
Case Studies in Disease Endotyping
The application of these pipelines has successfully revealed endotypic structures across multiple diseases, validating the utility of this approach.
Sepsis: Three Molecular Endotypes with Clinical Implications
The meta-analysis of 280 sepsis patients from four RNA-seq cohorts identified three consensus endotypes [43]:
- Coagulopathic Endotype (30%): Characterized by upregulated coagulation signaling and increased proportions of monocytes and neutrophils. This endotype carried a significantly higher risk of mortality (30%) compared to the adaptive endotype (OR 2.19, 95% CI 1.04–4.78, p = 0.04).
- Inflammatory Endotype (42%): Defined by activation of TNF-α/NF-κB signaling and IL-6/JAK/STAT3 pathways, alongside an increased neutrophil composition.
- Adaptive Endotype (28%): Exhibited enhanced adaptive immune responses, marked by elevated T and B cell compositions, and was associated with the lowest mortality risk (16%).
A 14-gene classifier was developed from this analysis, and its application to an external validation cohort of 123 patients successfully reproduced the mortality risk pattern, confirming the robustness of these findings [43].
Asthma: From T2-Hi/LO to Finer Stratification
Asthma research has been a pioneer in endotype discovery. Unsupervised approaches have moved beyond the broad classification of Type 2 (T2-high) and non-Type 2 (T2-low) endotypes [41] [42]. The T2-high endotype is driven by Th2 cytokines (IL-4, IL-5, IL-13) and eosinophilic inflammation, while the T2-low endotype is associated with Th1/Th17 activation and neutrophilic, often steroid-resistant, asthma [42]. Current research aims to harness multi-omics data and machine learning to identify finer-grained endotypes within these broad categories, which would explain the significant variability in treatment response to T2-targeted biologics [41].
Atopic Dermatitis: Integrating EHRs with Knowledge Graphs
A 2025 study on atopic dermatitis (AD) demonstrated a novel pipeline integrating Electronic Health Records (EHRs) with a Biomedical Knowledge Graph (BKG) [46]. This methodology:
- Mapped clinical features from EHRs (diagnoses, treatments) to nodes in a large BKG (iBKH) containing 2.3 million entities from 18 biomedical databases.
- Used graph machine learning to create novel patient representations within this connected knowledge space.
- Identified seven distinct patient subgroups, each characterized by unique clinical and genomic features, thereby uncovering potential new endotypes of AD by linking real-world clinical phenotypes to molecular mechanisms [46].
Unsupervised computational pipelines are indispensable for deconvoluting the heterogeneity of complex diseases into discrete molecular endotypes. The integration of high-throughput transcriptomic data, as in sepsis, innovative algorithms for rare event detection, as in liquid biopsies, and the fusion of real-world data with structured biological knowledge, as in atopic dermatitis, provides a powerful, multi-pronged arsenal for endotype discovery [43] [45] [46]. The consistent output of these studies—biologically distinct subgroups with direct clinical implications for prognosis and therapy—strongly validates the systems biology thesis that mechanistic disease subtypes exist and are discoverable. The ongoing development of robust, validated gene classifiers is the critical next step in translating these discoveries from a research context into clinical tools for precision medicine, ultimately ensuring the right patient receives the right treatment at the right time [43] [42].
Contemporary disease classification is undergoing a fundamental shift from phenotype-based categorization toward mechanism-driven stratification. The concept of endotypes—disease subtypes defined by distinct pathophysiological mechanisms rather than symptomatic presentation—has emerged as a transformative framework in systems biology research. Unlike phenotypes, which represent observable characteristics, endotypes reflect underlying biological pathways that can inform targeted therapeutic development and personalized treatment strategies. The identification of disease endotypes represents a core challenge in modern biomedical research, particularly for complex conditions like asthma, atopic dermatitis, and eosinophilic esophagitis that exhibit highly heterogeneous clinical presentations and treatment responses.
Artificial intelligence (AI) has dramatically accelerated endotype discovery by enabling integration and analysis of multi-omic datasets that capture system-wide biological information. These approaches span multiple levels of biological organization, from the genome to the exposome, providing unprecedented resolution for delineating disease mechanisms. This technical guide outlines comprehensive methodologies for developing AI-powered prediction models and diagnostic classifiers within the context of endotype discovery, providing researchers and drug development professionals with validated frameworks for translating complex biological data into clinically actionable insights.
Multi-Omic Data Integration for Endotype Discovery
Endotype discovery requires integration of diverse data types that collectively capture the multi-factorial complexity of disease. The Table 1 summarizes primary data modalities used in contemporary endotype research.
Table 1: Multi-Omic Data Types for Endotype Discovery
| Data Domain | Specific Data Types | Biological Insight | Example Technologies |
|---|---|---|---|
| Genomics | SNP arrays, Whole genome sequencing | Genetic predisposition, Inherited risk variants | DNA microarrays, Next-generation sequencing |
| Transcriptomics | RNA-seq, Microarray data | Gene expression patterns, Pathway activation | RNA sequencing, Single-cell RNA-seq |
| Epigenomics | DNA methylation, Histone modification | Regulatory mechanisms, Gene-environment interactions | Bisulfite sequencing, ChIP-seq |
| Microbiomics | 16S rRNA, Metagenomics | Microbial communities, Host-microbe interactions | 16S sequencing, Shotgun metagenomics |
| Proteomics | Mass spectrometry, Affinity arrays | Protein expression, Post-translational modifications | LC-MS/MS, SomaSCAN, Olink |
| Metabolomics | Mass spectrometry, NMR | Metabolic pathways, Small molecule signatures | GC-MS, LC-MS, NMR spectroscopy |
| Clinical Data | EHRs, Laboratory values, Symptom scores | Phenotypic manifestation, Disease severity | Electronic health records, Clinical assessments |
Multi-omic data integration enables researchers to move beyond single-dimensional classifications toward comprehensive molecular taxonomies. For example, investigations of asthma have revealed endotypes comprising different combinations of transcriptional and methylation activity related to T-cell differentiation alongside varying relative abundances of airway Moraxella, Corynebacterium, Staphylococcus, and Streptococcus [47]. Similarly, studies of atopic dermatitis have identified distinct endotypes based on skin barrier integrity, microbiome composition, and immune activation patterns that correlate with clinical outcomes and therapeutic responses [47].
Data Preprocessing and Quality Control
Effective data integration requires rigorous preprocessing and quality control across all omic domains. The following experimental protocols outline critical steps for ensuring data quality and compatibility:
Protocol 1: Multi-Omic Data Harmonization
- Batch Effect Correction: Apply ComBat, remove unwanted variation (RUV), or similar algorithms to address technical variability across sequencing runs, processing dates, or experimental batches.
- Normalization: Implement domain-specific normalization methods (e.g., TPM for RNA-seq, CSS for microbiome data, quantile normalization for proteomics) to enable cross-assay comparisons.
- Missing Data Imputation: Use appropriate imputation methods (e.g., k-nearest neighbors for metabolomics, missForest for mixed data types) while documenting imputation rates and potential biases.
- Feature Filtering: Remove uninformative features (e.g., low variance, low abundance) while preserving biologically relevant signals.
Protocol 2: Quality Assessment for Molecular Data
- RNA-seq: Assess sequencing depth, alignment rates, GC content, and 3'/5' bias using tools such as FastQC and MultiQC.
- Microbiome Data: Evaluate sequencing depth, rarefaction curves, and contamination signals using QIIME2 or similar platforms.
- DNA Methylation Arrays: Examine detection p-values, bisulfite conversion efficiency, and sex chromosome consistency.
- Proteomics: Assess peptide spectrum match quality, missing value patterns, and intensity distributions.
The integrity of downstream analyses and resulting endotype classifications depends critically on these preprocessing steps, which should be thoroughly documented using frameworks such as TRIPOD+AI for prediction models [48].
AI Model Development for Diagnostic Classification
Algorithm Selection for Endotype Discovery
AI model selection should be guided by data characteristics, sample size, and the specific objectives of endotype classification. The Table 2 summarizes algorithmic approaches with proven utility in endotype discovery.
Table 2: AI Algorithms for Endotype Discovery and Diagnostic Classification
| Algorithm Category | Specific Methods | Best Use Cases | Considerations |
|---|---|---|---|
| Clustering Methods | k-means, Hierarchical clustering, MANAclust [47] | Unsupervised endotype discovery from multi-omic data | Requires determination of cluster number, sensitive to data scaling |
| Dimensionality Reduction | PCA, UMAP, t-SNE, MOFA | Visualization of high-dimensional data, feature extraction | Interpretability challenges, parameter sensitivity |
| Decision Tree-Based | Random Forest, Gradient Boosting, Multi-step decision trees [4] | Feature selection, non-linear relationships, model interpretability | Risk of overfitting, requires careful parameter tuning |
| Deep Learning | Autoencoders, Neural networks | Complex pattern recognition, integration of heterogeneous data | Large sample size requirements, "black box" limitations |
| Multi-Omic Integration | Similarity Network Fusion, mixOmics, Integration workflows | Joint analysis of diverse data types | Computational complexity, method selection critical |
The MANAclust algorithm represents a particularly advanced approach for joint clustering of multi-omic and clinical data, having successfully identified 14 endotypes of asthma and health by leveraging clinical data alongside airway microbiome, transcriptome, and methylome profiles [47]. Similarly, decision tree-based methods have demonstrated particular utility for integrating gene expression, demographic, and clinical data to determine disease endotypes in a completely data-driven manner [4].
Model Training and Validation Framework
Protocol 3: Model Development Workflow
- Data Partitioning: Split data into training (70%), validation (15%), and test (15%) sets using stratified sampling to preserve outcome distribution. For multi-site studies, ensure each partition contains data from all sites.
- Feature Selection: Apply appropriate feature selection methods (e.g., LASSO, MRMR, domain knowledge-based selection) to reduce dimensionality and enhance model interpretability.
- Hyperparameter Tuning: Implement systematic hyperparameter optimization using grid search, random search, or Bayesian optimization with cross-validation on the training set only.
- Model Training: Train multiple candidate algorithms using the training set, employing appropriate regularization techniques to prevent overfitting.
- Model Validation: Evaluate model performance on the held-out test set using domain-appropriate metrics (e.g., AUC-ROC, precision-recall, calibration metrics).
Protocol 4: Validation Strategies for Robust Endotype Classification
- Internal Validation: Employ k-fold cross-validation or bootstrapping to assess model stability and performance variability.
- External Validation: Validate models in completely independent cohorts to evaluate generalizability across populations and settings.
- Temporal Validation: Test models on data collected from the same population but at later time points to assess temporal stability.
- Clinical Validation: Evaluate whether endotype classifications predict treatment response, disease progression, or other clinically relevant outcomes.
Recent systematic reviews highlight that inadequate validation represents a critical limitation in current AI-based diagnostic models, with most models demonstrating high risk of bias due to insufficient sample sizes, inappropriate handling of missing data, and suboptimal evaluation methods [49]. Adherence to rigorous validation standards is therefore essential for generating clinically useful endotype classifiers.
Data Visualization for Interpretable AI
Principles of Effective Visualization in Scientific Communication
Effective data visualization is essential for interpreting complex AI models and communicating endotype classifications to diverse audiences. The following principles, drawn from comprehensive analyses of scientific visualization [50] [51] [52], ensure clarity and interpretability:
Maximize Data-Ink Ratio: Prioritize ink (or pixels) that directly represent data, eliminating non-data ink and redundant elements [51]. This principle emphasizes simplicity and clarity in visual design.
Diagram Before Coding: Envision the core message and visual design before implementing software, focusing on the information rather than specific geometries [50].
Select Appropriate Geometries: Match visual representations to data types and communication goals:
- Amounts/Comparisons: Bar plots, dot plots
- Distributions: Box plots, violin plots, histograms
- Relationships: Scatter plots, heatmaps
- Compositions: Stacked bar charts, treemaps (avoid pie charts) [50]
Direct Labeling: Label elements directly rather than relying on legends to minimize cognitive load and facilitate interpretation [51].
Color Optimization: Select color palettes based on data characteristics (qualitative for categorical data, sequential for ordered numeric data, diverging for data with critical midpoint) while ensuring accessibility for colorblind readers [52].
These principles address common deficiencies in scientific visualization, including inappropriate geometry selection, excessive chartjunk, and ineffective color schemes that can obscure meaningful patterns in complex datasets [50] [51].
Visualization Strategies for Multi-Omic Endotype Data
Effective visualization of multi-omic endotype data requires specialized approaches that enable intuitive interpretation of high-dimensional relationships. The following workflows represent proven strategies for endotype visualization:
Diagram 1: Multi-Omic Endotype Discovery Workflow
Diagram 2: Diagnostic Classifier Development Pipeline
Visualization techniques should be matched to specific analytical goals in endotype research. Heatmaps effectively display patterns across molecular features and samples, enabling identification of endotype-specific signatures. Network visualizations illustrate relationships between molecular features across omic domains. Sankey diagrams can effectively map the flow of samples from clinical phenotypes to molecular endotypes and subsequent treatment responses.
Implementation and Reporting Standards
Clinical Translation and Validation
The transition from research findings to clinically applicable diagnostic classifiers requires rigorous evaluation frameworks. Recent systematic reviews indicate that most AI-based diagnostic models are not yet ready for clinical implementation, with high risk of bias identified in 60% of published models [49]. Common limitations include unjustified small sample sizes, failure to exclude predictors from outcome definitions, and inappropriate evaluation of performance measures.
Protocol 5: Clinical Validation Framework for Diagnostic Classifiers
- Prospective Validation: Evaluate classifier performance in prospective cohorts that reflect the intended use population and clinical setting.
- Comparator Assessment: Compare classifier performance against standard diagnostic approaches and clinical expert judgment.
- Utility Evaluation: Assess impact on clinical decision-making, workflow integration, and patient outcomes through randomized trials or well-designed observational studies.
- Implementation Monitoring: Continuously monitor performance following implementation to detect degradation and ensure ongoing safety and effectiveness.
For primary care settings, particular attention should be paid to integration with electronic health record systems, workflow compatibility, and interpretability for general practitioners [49].
Reporting Guidelines and Ethical Considerations
Comprehensive reporting is essential for evaluating, validating, and implementing AI-based diagnostic classifiers. The STARD-AI guideline provides a specialized framework for reporting diagnostic accuracy studies using AI, with 40 essential items that address AI-specific considerations [48]. Key reporting elements include:
- Dataset Practices: Detailed description of data sources, eligibility criteria, annotation processes, and preprocessing methods
- AI Index Test: Comprehensive specification of the AI model, version, and implementation details
- Algorithmic Bias and Fairness: Evaluation of potential performance disparities across demographic subgroups
- Reproducibility: Documentation of code availability and external audit processes
Similar reporting standards should be applied to endotype discovery research, with clear documentation of methodological choices, analytical parameters, and validation approaches. The TRAPODS-CM initiative represents a domain-specific adaptation of these principles for Chinese medicine diagnostic prediction models, highlighting the importance of domain-appropriate reporting frameworks [53].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools for Endotype Discovery
| Category | Specific Tools/Reagents | Function | Implementation Considerations |
|---|---|---|---|
| Data Integration Platforms | MOFA+, mixOmics, Similarity Network Fusion | Integration of heterogeneous multi-omic datasets | Compatibility with data types, scalability to large datasets |
| Clustering Algorithms | MANAclust [47], k-means, hierarchical clustering | Identification of patient subgroups based on molecular profiles | Determination of optimal cluster number, stability assessment |
| Machine Learning Libraries | Scikit-learn, TensorFlow, PyTorch, XGBoost | Development of predictive models for endotype classification | Hardware requirements, computational efficiency, interpretability |
| Visualization Tools | ggplot2, Matplotlib, Seaborn, ComplexHeatmap | Creation of publication-quality visualizations | Customization options, compatibility with analysis pipelines |
| Bioinformatics Suites | QIIME2 (microbiome), DESeq2 (RNA-seq), Limma (microarrays) | Domain-specific data processing and analysis | Data format requirements, computational resources |
| Statistical Analysis Tools | R, Python Pandas, NumPy, SciPy | Data manipulation, statistical testing, results generation | Learning curve, community support, reproducibility features |
These tools collectively enable the end-to-end analytical workflow from raw data processing through endotype identification and validation. Selection should be guided by specific research questions, data characteristics, and computational resources, with particular attention to reproducibility and documentation standards.
The development of AI prediction models and diagnostic classifiers for disease endotyping represents a powerful approach for advancing precision medicine. By integrating multi-omic data within rigorous analytical frameworks, researchers can move beyond symptomatic classifications toward mechanism-based disease stratification. Successful implementation requires attention to data quality, methodological rigor, comprehensive validation, and transparent reporting. As these approaches mature, they hold significant promise for identifying patient subgroups most likely to benefit from targeted therapies, ultimately enabling more precise and effective interventions across diverse disease contexts.
The field continues to evolve rapidly, with emerging opportunities in areas such as large language models for clinical text analysis, multi-modal AI for integrated data interpretation, and federated learning for privacy-preserving model development across institutions. By adhering to established best practices while remaining adaptable to technological innovations, researchers can contribute meaningfully to the growing toolkit for endotype discovery and personalized medicine.
Navigating the Complexities: Overcoming Challenges in Endotype Research
Addressing Dynamic Variability and Overlap in Complex Endotypes
The paradigm of disease treatment is shifting from a symptom-based to a mechanism-driven approach, necessitating the precise identification of disease endotypes—subtypes of disease defined by distinct functional or pathobiological mechanisms [1]. Unlike phenotypes, which are observable clinical characteristics, endotypes represent the underlying biological pathways that give rise to these observable traits [1]. However, the inherent dynamic variability and significant overlap between endotypes present substantial challenges for their clear delineation and therapeutic targeting. A single phenotype, such as the "frequent-exacerbator" phenotype in Chronic Obstructive Pulmonary Disease (COPD), may arise from multiple distinct endotypes (e.g., eosinophilic inflammation-driven vs. infection-dominant), each requiring different therapeutic strategies [1]. Systems biology, through the integration of multi-omics data and computational modeling, provides the foundational framework necessary to dissect this complexity, moving beyond static classification to capture the dynamic and interconnected nature of disease mechanisms [54] [28].
Systems Biology Framework for Endotype Resolution
Multi-Scale Data Integration
The resolution of complex endotypes requires the integration of biological data across multiple scales and organizational layers. Traditional, single-layer omics analyses provide limited insights into the coordinated interactions that define functional endotypes [28]. A systems approach vertically integrates data from genomics, transcriptomics, proteomics, and metabolomics to construct a comprehensive map of molecular regulation and metabolic processes [54] [28]. This integration allows researchers to connect molecular-level interactions (e.g., protein-DNA binding) to cellular-level responses (e.g., cytokine secretion) and ultimately to organ-level or organism-level phenotypes [55]. The resulting multi-scale models are essential for identifying the critical control points within cellular communication networks that govern the emergence and dynamics of specific endotypes [55].
Static and Dynamic Modeling Approaches
Computational systems biology employs two primary, complementary approaches to model the interactions that define endotypes.
Static Network Modeling: This approach visualizes functional interactions between components (e.g., genes, proteins, drugs) as nodes and edges in a network [28]. Protein-Protein Interaction (PPI) networks and gene co-expression networks are used to identify densely connected modules associated with specific disease phenotypes or therapeutic responses [28]. The underlying assumption is that diseases with overlapping network modules show significant co-expression patterns and symptom similarity [28]. For example, hub genes with high connectivity in a co-expression network, identified through methods like Weighted Gene Co-expression Network Analysis (WGCNA), can point to potential endotype regulators [28].
Dynamic Modeling: Unlike static snapshots, dynamic models use differential equations or agent-based simulations to formalize the elementary interactions between system components, enabling the study of how system behavior emerges over time [55]. This is crucial for understanding endotype dynamics, as feedback mechanisms can transform small initial differences in the timing and amount of signals into all-or-nothing cellular differentiations [55]. Computational tools with graphical interfaces now allow biologists to define these quantitative models without advanced computational skills, facilitating the simulation of complex signaling pathways and their perturbation [55].
Table 1: Core Analytical Methods in Computational Systems Biology
| Method Category | Specific Methods | Primary Function | Key Considerations |
|---|---|---|---|
| Differential Expression | Limma (R package) [28] | Identifies disease-related genes from RNA-sequencing data via moderated t-statistics and empirical Bayes. | Performance is sensitive to sample size. Requires normal samples for comparison. |
| Gene Co-expression Network | WGCNA [28], Context Likelihood of Relatedness [28] | Detects functional gene clusters based on correlation of gene expressions. | WGCNA is sensitive to gene quantity and parameter settings. CLR can capture non-linear relationships. |
| Protein Interaction | Protein-Protein Interaction (PPI) Network [28] | Maps interactions between proteins to identify disease-related modules and hub proteins. | Based on the "guilt-by-association" principle; shared components may cause similar phenotypes. |
Machine Learning for Pattern Recognition and Prediction
Machine learning techniques are increasingly applied to predict potential molecular interactions from known interaction data, overcoming the high cost and limitations of clinical experiments [28]. These methods can mine structural motifs within biological networks to predict novel interactions and identify disease subcategories with superior predictive value for therapeutic responses [54] [1]. Furthermore, machine learning-driven dynamic phenotyping is emerging as a future direction for identifying pre-disease states and treatable traits, enhancing the ability to perform early, proactive interventions [1].
Experimental Protocols for Endotype Identification
This section details a standardized workflow for constructing and validating network models to identify distinct endotypes from multi-omics data.
Protocol 1: Network Construction from Omics Data
Objective: To build a static network model from transcriptomic data for the identification of candidate endotype-related genes and protein modules.
- Data Acquisition and Pre-processing: Obtain RNA-sequencing or microarray data from patient cohorts representing the disease phenotype of interest. Normalize raw data to account for technical variability.
- Identify Differentially Expressed Genes (DEGs): Using the Limma package in R, perform differential expression analysis to select genes with large variations in expression based on fold-change and p-value thresholds [28].
- Construct Co-expression Network: For the DEGs, calculate pairwise correlation coefficients. Use Pearson Correlation Coefficient (PCC) for linearly correlated data or Mutual Information for non-linear relationships [28]. Apply a correlation cutoff or use an algorithm like WGCNA to construct an approximately scale-free network [28].
- Map to Protein-Protein Interaction (PPI) Network: Map the identified DEGs to a public PPI database (e.g., STRING, BioGRID) to build a PPI network. This step integrates prior knowledge of known physical interactions.
- Detect Functional Modules: Use network clustering algorithms (e.g., Markov Clustering, greedy algorithms) to identify tightly connected subnetwork modules within the larger co-expression or PPI network [28].
- Select Hub Genes/Proteins: Analyze network connectivity to select hub nodes (genes/proteins) with high connectivity within the functional clusters. These hub elements are candidate regulators for further investigation [28].
Protocol 2: Dynamic Simulation and In-Silico Perturbation
Objective: To create a dynamic computational model of a key signaling pathway and simulate interventions to predict endotype-specific responses.
- Model Definition: Select a signaling pathway implicated in endotype divergence (e.g., T-cell receptor signaling driving Th1/Th2 differentiation [55]). Using a computational tool with a graphical interface (e.g., BioNetGen, COPASI), define the molecular species and their interactions.
- Formalize Interactions: Instead of manually defining every possible molecular complex, use a binding site-centred approach. Define interactions between molecular binding sites and allow the software to automatically generate the resulting signaling complexes, reducing effort and potential for error [55].
- Parameterization: Assign initial concentrations to molecular species and reaction rates to interactions. These parameters should be derived from quantitative experimental data, such as intracellular protein concentrations and interaction rates [55].
- Model Simulation: Run simulations to establish a baseline time-course of component concentrations and pathway activity.
- In-Silico Knock-Down Experiments: Perturb the model by simulating the knock-down or inhibition of hub genes/proteins identified in Protocol 1. Observe the resulting changes in pathway dynamics and output.
- Validation and Refinement: Compare the model's predictions (e.g., the effect of a specific inhibition on cytokine production) with new experimental data. Iteratively refine the model to improve its biological fidelity and predictive power [55].
Visualization of Endotype Networks and Dynamics
Effective visualization is critical for interpreting the complex relationships within and between endotypes. The following diagrams, generated with Graphviz, illustrate key concepts and workflows.
Endotype Overlap and Phenotype Convergence
This diagram illustrates how multiple distinct biological endotypes can give rise to overlapping clinical phenotypes, and how they can be resolved through multi-omics data integration.
Multi-Scale Endotype Analysis Workflow
This diagram outlines the core computational workflow for resolving endotypes, from data acquisition to model simulation and therapeutic stratification.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Resources for Endotype Research and Analysis
| Tool / Resource | Type | Primary Function | Application in Endotype Research |
|---|---|---|---|
| Limma (R Package) [28] | Software | Differential expression analysis from microarray or RNA-seq data. | Statistically identifies disease-related genes for network construction. |
| WGCNA [28] | Software Algorithm | Construction of weighted gene co-expression networks. | Detects functional gene clusters (modules) associated with disease traits from transcriptomic data. |
| PPI Databases (e.g., STRING) [28] | Database | Repository of known and predicted protein-protein interactions. | Provides a scaffold for building interaction networks and inferring protein function. |
| BioNetGen [55] | Software Tool | Rule-based modeling of biochemical networks. | Enables precise, large-scale dynamic simulations of signaling pathways, including automated complex formation. |
| Context Likelihood of Relatedness [28] | Software Algorithm | Inference of gene regulatory networks using mutual information. | Discovers non-linear regulatory relationships between genes that may define endotypic mechanisms. |
| Blood Eosinophil Count [1] | Biomarker | Measure of type 2 inflammation. | Clinically accessible biomarker for stratifying patients into eosinophilic vs. non-eosinophilic COPD endotypes for targeted therapy. |
Addressing the dynamic variability and overlap in complex endotypes is a formidable challenge that lies at the forefront of precision medicine. The path forward requires a concerted effort to expand the current network medicine framework by incorporating more realistic assumptions about biological units and their interactions across multiple relevant scales [54]. Future progress will depend on the early detection of pre-disease states, the robust integration of multi-omics data, and the validation of precision-guided interventions through pragmatic clinical trials [1]. By systematically applying the principles of systems biology and computational modeling, researchers can transition disease management from a reactive, phenotype-based approach to a proactive, endotype-driven paradigm, ultimately delivering the right interventions to the right patient at the right time.
Biomarker Validation and Standardization for Clinical Translation
The identification of disease endotypes through systems biology research represents a paradigm shift in our understanding of disease heterogeneity. This approach moves beyond traditional phenotypic classification to define distinct subpopulations based on underlying molecular mechanisms. Biomarker validation and standardization serves as the critical bridge connecting these mechanistic insights to clinically actionable tools, enabling precision medicine approaches that target specific disease drivers rather than superficial symptoms [56]. The validation pathway transforms exploratory findings from multi-omics analyses into reliable, clinically implemented biomarkers that can accurately identify patient endotypes and predict their response to targeted therapies.
Despite remarkable advances in biomarker discovery, a troubling chasm persists between preclinical promise and clinical utility. Less than 1% of published biomarkers successfully transition to routine clinical practice, creating significant roadblocks in drug development and precision medicine implementation [57]. This translational gap stems from multiple factors: over-reliance on traditional animal models with poor human correlation, lack of robust validation frameworks, inadequate reproducibility across cohorts, and failure to account for disease heterogeneity in human populations [57]. Overcoming these challenges requires systematic approaches to biomarker validation that prioritize clinical relevance, analytical robustness, and standardization across the entire development pipeline.
Regulatory and Conceptual Framework for Biomarker Validation
Biomarker Categories and Context of Use
The U.S. Food and Drug Administration (FDA) emphasizes that biomarker validation must be fit-for-purpose, with the level of evidence required depending on the specific Context of Use (COU) and application in drug development or clinical decision-making [58]. The Biomarkers, EndpointS, and other Tools (BEST) resource provides a standardized glossary categorizing biomarkers by their specific application, with each category demanding distinct validation approaches and evidence requirements [58].
Table 1: Biomarker Categories and Context of Use Framework
| Biomarker Category | Primary Function | Validation Emphasis | Example |
|---|---|---|---|
| Susceptibility/Risk | Identifies increased disease likelihood | Epidemiological evidence, biological plausibility | BRCA1/2 mutations for cancer risk [58] |
| Diagnostic | Identifies or confirms disease presence | Sensitivity, specificity across diverse populations | Hemoglobin A1c for diabetes [58] |
| Prognostic | Predicts disease outcome regardless of treatment | Correlation with clinical outcomes across cohorts | Total kidney volume for polycystic kidney disease [58] |
| Monitoring | Tracks disease status over time | Ability to reflect status changes longitudinally | HCV RNA viral load for Hepatitis C [58] |
| Predictive | Forecasts response to specific treatments | Sensitivity, specificity, mechanistic link to response | EGFR mutation status for NSCLC therapy [58] |
| Pharmacodynamic/Response | Measures biological response to intervention | Direct relationship between drug action and biomarker change | HIV RNA viral load in HIV treatment trials [58] |
| Safety | Detects potential adverse effects | Consistent indication of adverse effects across populations | Serum creatinine for kidney injury [58] |
Regulatory Pathways and Evolution
Regulatory frameworks for biomarker validation continue to evolve, with the FDA's 2025 Biomarker Guidance building upon previous versions while maintaining consistency in fundamental principles. The guidance recognizes that while biomarker assays should address the same validation parameters as drug assays (accuracy, precision, sensitivity, selectivity, parallelism, range, reproducibility, and stability), the technical approaches must be adapted to demonstrate suitability for measuring endogenous analytes [59]. This continuity in regulatory thinking reinforces that biomarker validation must focus on the measurement of endogenous analytes rather than relying solely on spike-recovery approaches used in drug concentration analysis [59].
The FDA provides several pathways for regulatory acceptance of biomarkers, including early engagement via Critical Path Innovation Meetings (CPIM), the Investigational New Drug (IND) application process, and the Biomarker Qualification Program (BQP) [58]. The BQP offers a structured framework for broader acceptance of biomarkers across multiple drug development programs, involving three stages: Letter of Intent, Qualification Plan, and Full Qualification Package. While this pathway may require more extensive supporting evidence, once qualified, a biomarker can be used by any drug developer without requiring FDA re-review, provided it is used within the specified COU [58].
Methodological Approaches to Biomarker Validation
Analytical Validation Protocols
Analytical validation establishes that a biomarker measurement method is reliable, reproducible, and fit-for-purpose. This process assesses critical performance characteristics including accuracy, precision, analytical sensitivity, analytical specificity, reportable range, and reference range [58]. The specific requirements vary based on the detection method and analyte of interest, but must consistently demonstrate robust performance under conditions mimicking intended use.
For liquid biopsy technologies, expected advancements by 2025 include significantly enhanced sensitivity and specificity through improved circulating tumor DNA (ctDNA) analysis and exosome profiling. These developments will make liquid biopsies more reliable for early disease detection and monitoring, facilitating real-time tracking of disease progression and treatment responses [60]. The validation of these technologies requires particular attention to pre-analytical variables, matrix effects, and the establishment of appropriate reference materials for endogenous analytes.
Clinical Validation Strategies
Clinical validation demonstrates that a biomarker accurately identifies or predicts the clinical outcome of interest. This process involves assessing sensitivity and specificity, determining positive and negative predictive values, and evaluating biomarker performance in the intended population [58]. For endotype-defining biomarkers, clinical validation must establish a clear connection between the molecular signature and distinct disease trajectories or treatment responses.
Longitudinal sampling strategies provide particularly powerful approaches for clinical validation, capturing temporal biomarker dynamics that single measurements miss. Repeated biomarker measurements over time reveal subtle changes that may indicate disease development or recurrence before clinical symptoms appear, offering a more robust picture than static measurements [57]. For complex chronic conditions, these dynamic profiles often provide more comprehensive predictive information than single time-point assessments [61].
Standardization and Pre-analytical Variables
Standardized sample handling protocols are fundamental to reliable biomarker measurement, particularly for neurological biomarkers where pre-analytical variations can significantly impact results. The Global Biomarker Standardization Consortium has established evidence-based handling protocols for blood-based Alzheimer's disease biomarkers after systematic assessment of pre-analytical effects [62].
Table 2: Impact of Pre-analytical Variables on Neurological Blood-Based Biomarkers
| Pre-analytical Variable | Effect on Aβ42/Aβ40 | Effect on pTau | Effect on NfL/GFAP | Recommended Protocol |
|---|---|---|---|---|
| Collection Tube Type | >10% variation | >10% variation | >10% variation | Standardize tube type across study |
| Centrifugation Delay (RT) | >10% decline | Stable | >10% increase | Process within 1 hour at RT |
| Centrifugation Delay (2-8°C) | <10% decline | Stable | Stable | Process within 8 hours at 2-8°C |
| Storage Delay (RT) | Significant decline | Stable | >10% increase | Freeze plasma immediately |
| Freeze-Thaw Cycles | Variable decline | Highly stable | Moderate increase | Limit freeze-thaw cycles |
According to their findings, plasma Aβ42 and Aβ40 are particularly sensitive to pre-analytical variations, showing significant declines under storage and centrifugation delays, especially at room temperature. In contrast, pTau isoforms demonstrate remarkable stability across most pre-analytical variations, while neurofilament light (NfL) and glial fibrillary acidic protein (GFAP) levels tend to increase with room temperature storage [62]. These findings underscore the necessity of standardized, evidence-based protocols tailored to specific biomarker characteristics.
Advanced Models and Technologies for Translational Biomarker Development
Human-Relevant Disease Models
Conventional animal models frequently fail to predict human clinical outcomes due to fundamental biological differences between species. Advanced human-relevant models now offer more physiologically accurate platforms for biomarker validation [57]:
Patient-derived organoids: These 3D structures retain characteristic biomarker expression better than two-dimensional cultures and have demonstrated effectiveness in predicting therapeutic responses and guiding personalized treatment selection [57].
Patient-derived xenografts (PDX): These models more accurately recapitulate human cancer characteristics, tumor progression, and evolution, producing convincing preclinical results for biomarker validation [57].
3D co-culture systems: Incorporating multiple cell types (immune, stromal, endothelial), these systems provide comprehensive models of the human tissue microenvironment for identifying context-specific biomarkers [57].
These advanced models become particularly powerful when integrated with multi-omics strategies, enabling the identification of clinically actionable biomarkers that might be missed with single-approach methodologies [57].
Multi-omics Integration and AI Approaches
The integration of multiple omics technologies (genomics, transcriptomics, proteomics, metabolomics) represents a fundamental shift in biomarker development, enabling comprehensive molecular profiling that captures disease complexity. By 2025, multi-omics approaches are expected to be standard practice, providing holistic understanding of disease mechanisms and facilitating identification of complex biomarker signatures [60].
Artificial intelligence and machine learning are revolutionizing biomarker discovery by identifying patterns in large datasets that traditional methods overlook. By 2025, AI-driven algorithms will enable more sophisticated predictive models that forecast disease progression and treatment responses based on biomarker profiles [60]. These technologies facilitate automated analysis of complex datasets, significantly reducing time required for biomarker discovery and validation [60]. The convergence of multi-omics data and AI creates powerful frameworks for identifying endotype-specific biomarker signatures that accurately predict disease behavior and treatment response.
Figure 1: Multi-Omics and AI Integration Workflow for Biomarker Discovery
Implementation Challenges and Emerging Solutions
Addressing the Translational Gap
The transition from preclinical biomarker discovery to clinical application faces multiple significant hurdles. The translational gap remains a major roadblock, often due to preclinical models that fail to accurately reflect human biology [57]. Additional challenges include lack of robust validation frameworks, inadequate reproducibility across cohorts, and disease heterogeneity in human populations versus uniformity in preclinical testing [57].
Strategies to bridge this gap include integrating human-relevant models, implementing longitudinal and functional validation approaches, and leveraging advanced analytics such as AI-driven correlations [57]. Functional validation is particularly important, moving beyond correlative evidence to demonstrate biological relevance and therapeutic impact. Functional assays that confirm a biomarker's active role in disease processes strengthen the case for real-world utility and many are already displaying significant predictive capacities [57].
Data Heterogeneity and Standardization
Data heterogeneity presents a critical challenge in biomarker development, requiring sophisticated integration approaches. Proposed frameworks to address this challenge prioritize three pillars: multi-modal data fusion, standardized governance protocols, and interpretability enhancement [61]. These approaches systematically address implementation barriers from data acquisition to clinical adoption, enhancing early disease screening accuracy while supporting risk stratification and precision diagnosis.
Standardization initiatives are increasingly important, with collaborative efforts among industry stakeholders, academia, and regulatory bodies promoting established protocols for biomarker validation [60]. By 2025, regulatory frameworks are expected to place greater emphasis on real-world evidence in evaluating biomarker performance, allowing for more comprehensive understanding of clinical utility in diverse populations [60].
Clinical Workflow Integration and Infrastructure
For biomarkers to influence clinical decision-making, they must be embedded into clinical-grade infrastructure ensuring reliability, traceability, and compliance. This requires purpose-built laboratories combined with quality frameworks that enable genomic and multi-omic assays to achieve regulatory and clinical standards [63]. The digital backbone supporting these services is equally critical, with providers implementing Laboratory Information Management Systems (LIMS), electronic Quality Management Systems (eQMS), and clinician portals to streamline complex data flows from sample to report [63].
Digital pathology platforms serve as natural bridges between imaging and molecular biomarker workflows, with AI-driven image interpretation and fully digital reporting environments delivering greater consistency, scalability, and interoperability across sites [63]. These infrastructure considerations are essential for translating biomarker discoveries into routine clinical practice.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Biomarker Validation
| Tool Category | Specific Technologies | Research Application | Function in Biomarker Workflow |
|---|---|---|---|
| Human-Relevant Models | Patient-derived organoids, PDX models, 3D co-culture systems | Physiological disease modeling | Biomarker validation in human-relevant contexts [57] |
| Single-Cell Analysis | 10x Genomics, Element Biosciences AVITI24 | Cellular heterogeneity resolution | Identification of rare cell populations and tumor microenvironment biomarkers [60] [63] |
| Multi-omics Platforms | Sapient Biosciences, Element Biosciences | Comprehensive molecular profiling | Simultaneous measurement of DNA, RNA, protein, and metabolites [63] |
| Digital Pathology | PathQA, AIRA Matrix, Pathomation | AI-driven image analysis | Bridge between imaging and molecular biomarkers [63] |
| Liquid Biopsy Technologies | ctDNA analysis, exosome profiling | Non-invasive biomarker monitoring | Real-time disease progression and treatment response tracking [60] |
Figure 2: Biomarker Validation Pipeline from Endotype Discovery to Clinical Implementation
The field of biomarker validation is evolving rapidly, with several key trends shaping its future trajectory. By 2025, patient-centric approaches will become more pronounced, incorporating patient-reported outcomes into biomarker studies and engaging diverse populations to ensure relevance across demographics [60]. Single-cell analysis technologies will mature, providing deeper insights into tumor microenvironments and enabling identification of rare cell populations that drive disease progression or therapy resistance [60].
The regulatory landscape will continue to adapt, with agencies implementing more streamlined approval processes for biomarkers validated through large-scale studies and real-world evidence [60]. Europe's In Vitro Diagnostic Regulation (IVDR), while creating initial implementation challenges, is expected to evolve toward stronger frameworks and closer collaboration between pharma and diagnostics companies [63].
For biomarker validation to successfully support the translation of systems biology endotypes to clinical practice, a comprehensive, integrated approach is essential. This requires leveraging human-relevant models, implementing rigorous analytical and clinical validation strategies, standardizing pre-analytical and analytical processes, and building robust infrastructure for clinical implementation. As precision medicine advances, validated biomarkers will increasingly serve as the critical link connecting disease endotypes to targeted therapeutic strategies, ultimately realizing the promise of personalized patient care.
Strategies for Integrating High-Dimensional, Multi-Source Data
In the field of modern systems biology, a paradigm shift is occurring from traditional disease classification based on symptoms towards a precision medicine approach focused on disease endotypes—subtypes of conditions defined by distinct functional or pathobiological mechanisms [64]. Identifying these endotypes is crucial for developing targeted therapies and improving patient outcomes. This endeavor, however, generates immense volumes of high-dimensional data from diverse sources such as genomics, transcriptomics, proteomics, and metabolomics. The central challenge for researchers and drug development professionals lies in the integrative analysis of these complex, multi-source datasets to uncover coherent biological signatures that define specific endotypes [65] [66]. Successfully addressing this challenge requires a sophisticated arsenal of computational strategies for data fusion, dimensionality reduction, and pattern recognition. This guide details these essential strategies, framing them within the practical context of identifying clinically actionable disease endotypes.
Foundational Concepts: From Phenotypes to Precision Endotypes
Defining the Precision Medicine Taxonomy
A clear understanding of the terminology is essential for research in this domain.
- Phenotype: The clinically observable characteristics of a disease, such as age of onset, triggers, and treatment response. These are often heterogeneous and overlapping, providing limited insight into underlying mechanisms [64].
- Endotype: A molecularly defined disease subtype characterized by a distinct functional or pathological pathway. Endotypes provide the mechanistic understanding needed for targeted interventions [64] [66]. For example, "type 2-high" asthma is an endotype driven by a specific immune pathway involving Th2 cells, ILC2s, and their cytokines (IL-4, IL-5, IL-13) [64].
- Biomarker: A measurable indicator that links an endotype to a phenotype. Biomarkers are critical for diagnosing, monitoring, and stratifying patients in clinical practice and trials [64].
The Multi-Source Data Landscape in Systems Biology
Research aimed at endotype discovery typically relies on several layers of high-dimensional biological data, which constitute the multiple sources for integration:
- Genomics: Provides data on DNA sequence variations and mutations.
- Transcriptomics: Reveals gene expression patterns through RNA sequencing.
- Proteomics: Identifies and quantifies protein expression and post-translational modifications.
- Metabolomics: Measures the abundances of small-molecule metabolites.
The core objective of integrative analysis is to fuse these disparate data modalities to build a comprehensive model of disease pathophysiology, moving beyond the limitations of single-source analysis [66].
Core Technical Strategies for Data Integration
Matrix Factorization and Multimodal Fusion
Joint factorization methods are powerful for discovering latent (hidden) structures that are consistent across different data types.
- Joint Non-Negative Matrix Factorization (jNMF): This technique simultaneously factorizes multiple non-negative data matrices (e.g., mRNA expression, miRNA expression, DNA methylation) into a set of common latent factors. Each data source contributes to the discovery of shared molecular patterns, which can represent candidate endotypes [65]. The jNMF problem is formulated as an optimization problem that is inherently non-convex and iterative, making the choice of initialization critical for convergence and solution quality.
- Meta-Heuristic Enhanced jNMF: To overcome the limitations of standard jNMF, advanced approaches use meta-heuristic algorithms for initialization. For instance, the Chaotic Driven Gorilla Troops Optimizer (CD-GTO) has been used to initialize the factor matrices in sparse-jNMF. This hybrid method has demonstrated an 11% average improvement in silhouette score and a 4% improvement in cluster purity on multi-omics cancer data compared to traditional initialization methods [65].
Table 1: Evaluation of jNMF Initialization Methods on Multi-Omics Cancer Data
| Initialization Method | Average Silhouette Score | Average Purity Measure | Key Characteristic |
|---|---|---|---|
| CD-GTO sparse-jNMF | 0.XX | 0.XX | Incorporates chaos theory for superior global search |
| Standard GTO sparse-jNMF | 0.YY | 0.YY | Uses nature-inspired population-based algorithm |
| Traditional (e.g., NNDSVD) | 0.ZZ | 0.ZZ | Standard deterministic initialization |
Dimensionality Reduction and Pattern Discovery
Before or during integration, reducing the number of variables is essential to visualize patterns and avoid the "curse of dimensionality."
- Principal Component Analysis (PCA): A linear technique that transforms the data to a new coordinate system, highlighting the directions (principal components) that capture the greatest variance. PCA is invaluable for visualizing high-dimensional data in 2D or 3D plots and for identifying major sources of variation that may correspond to different endotypes [67].
- Clustering for Unsupervised Endotype Discovery: Clustering algorithms group patients or samples based on the similarity of their multi-omics profiles.
- K-Means Clustering: Partitions samples into a pre-defined number (K) of clusters by minimizing the within-cluster sum of squares. It assumes clusters are spherical and of similar size [67].
- Hierarchical Clustering: Builds a tree-like structure (dendrogram) of nested clusters, allowing exploration at multiple levels of granularity. The choice of linkage rule (e.g., complete, average) impacts the shape of the resulting clusters [67].
Data Preprocessing and Harmonization
The feasibility of integration depends on rigorous data preprocessing.
- Centering and Scaling: Bringing variables (e.g., gene expression counts) to a common scale is critical. Z-score normalization (centering then dividing by the standard deviation) ensures that analysis is independent of the original units and prevents variables with large variances from dominating the results [67].
- Batch Effect Correction: Technical variation introduced by different experimental batches must be identified and removed to prevent spurious findings.
- Schema Harmonization: In the context of multi-source data, this involves agreeing on common entity definitions (e.g., "patient," "sample") and standardized column names, types, and identifiers across all datasets [68].
Diagram 1: Multi-Source Data Integration Workflow
Visualization of High-Dimensional Integrated Data
Effective visualization is key to interpreting the results of integrative analysis and communicating findings.
- Heatmaps with Clustering: Heatmaps display data matrices as images by color-coding their entries. When combined with hierarchical clustering on both rows (samples/patients) and columns (molecular features), heatmaps can reveal clear patterns and subgroups, visually suggesting potential endotypes [67]. Libraries like
pheatmapin R facilitate the creation of such visualizations. - Multi-Source Dashboards: Interactive dashboards can serve as a central command center, enabling researchers to visualize and correlate data from multiple integrated sources. They allow for dynamic filtering across datasets, maintaining data relationships and ensuring coherent visualizations [69] [70].
- Geomaps for Regiotypes: The concept of "regiotypes" acknowledges that disease triggers and appearances vary by region (e.g., predominant allergens, microbiome differences). Integrating and visualizing this geographical information with molecular data can provide critical context for endotype discovery [64].
Practical Experimental Protocol: jNMF for Cluster Analysis
The following provides a detailed methodology for applying jNMF to multi-omics data for integrative cluster analysis, as validated in recent research [65].
Research Reagent Solutions
Table 2: Essential Reagents and Tools for Multi-Omics Integration Analysis
| Item / Tool Name | Function / Description | Application in Protocol |
|---|---|---|
| Multi-Omics Datasets | Matrices of genomic, transcriptomic, proteomic, and/or metabolomic measurements. | The core input data for integration (e.g., TCGA, in-house cohorts). |
| Chaotic Gorilla Troops Optimizer (CD-GTO) | A meta-heuristic optimization algorithm enhanced with chaos theory. | Used to initialize the factor matrices in jNMF to improve solution quality. |
| Silhouette Score Metric | A measure of how similar an object is to its own cluster compared to other clusters. | The primary metric for evaluating the quality of the identified clusters/endotypes. |
| Purity Measure Metric | A measure of the extent to which each cluster contains data points from a single class. | A validation metric for assessing clustering accuracy against known labels. |
| Computational Framework (e.g., Python/R) | Software environment with libraries for matrix algebra and machine learning. | The platform for implementing the jNMF algorithm and analysis. |
Step-by-Step Workflow
Data Collection and Preprocessing:
- Assemble your (n \times p) data matrices (\mathbf{X}^{(1)}, \mathbf{X}^{(2)}, ..., \mathbf{X}^{(V)}) for each of the (V) data views (e.g., mRNA, methylation).
- Apply necessary normalization, log-transformation, and Z-score scaling to each matrix individually to ensure they are on a comparable scale and are non-negative [67].
Meta-Heuristic Initialization:
- Utilize the CD-GTO algorithm to initialize the shared basis matrix (\mathbf{W}) and the view-specific coefficient matrices (\mathbf{H}^{(v)}). The chaos dynamics enhance the algorithm's global search ability, helping to avoid local minima [65].
jNMF Algorithm Execution:
- Solve the jNMF optimization problem, which aims to minimize the following objective function for all integrated views: [ \min{\mathbf{W}, \mathbf{H}^{(v)} \geq 0} \sum{v=1}^{V} ||\mathbf{X}^{(v)} - \mathbf{W} \mathbf{H}^{(v)}||_F^2 ]
- Perform iterative updates to (\mathbf{W}) and (\mathbf{H}^{(v)}) until convergence criteria are met (e.g., minimal change in reconstruction error).
Cluster Assignment:
- Use the resulting shared matrix (\mathbf{W}) for downstream analysis. Each column of (\mathbf{W}) represents a metagene or latent factor.
- Apply K-means or hierarchical clustering to the columns of (\mathbf{W}) (or the consolidated coefficient matrices) to assign each sample to a cluster. These clusters represent putative disease endotypes [65].
Validation and Interpretation:
- Evaluate the clustering performance using internal validation metrics like the silhouette score [65].
- If ground truth labels are available, compute external validation metrics like cluster purity [65].
- Biologically interpret the discovered endotypes by analyzing the features (genes, proteins, etc.) that contribute most to each latent factor in (\mathbf{W}) and (\mathbf{H}^{(v)}).
Diagram 2: jNMF Experimental Protocol
The integration of high-dimensional, multi-source data is no longer a theoretical challenge but an operational necessity for advancing systems biology and precision medicine. By leveraging computational strategies such as joint matrix factorization, dimensionality reduction, and robust clustering, researchers can deconvolute the heterogeneity of complex diseases into mechanistically defined endotypes. This process, supported by rigorous preprocessing and insightful visualization, provides a clear path from disparate, large-scale molecular data to discover novel biomarkers and therapeutic targets. As these methodologies continue to mature, they will undoubtedly accelerate the development of more effective, personalized treatments for patients.
Optimizing Computational Workflows and Ensuring Model Robustness
In systems biology, the pursuit of understanding complex human diseases requires moving beyond superficial phenotypes to decipher underlying disease endotypes—subgroups of conditions defined by distinct functional or pathobiological mechanisms [8]. The identification of these endotypes is critical for advancing precision medicine, as it enables the matching of therapeutic interventions to specific disease mechanisms. This process is inherently dependent on computational models of immense scale and complexity, making the optimization of workflows and the robustness of these models foundational to successful research outcomes.
Biological robustness describes a system's ability to maintain specific functions or traits when exposed to perturbations, a property pervasive across all organizational levels in biology [71]. In the context of computational research, model robustness provides a crucial measure of plausibility, as only a minute fraction of possible model instantiations will display the robust expression patterns observed in actual biological networks [71]. For researchers identifying disease endotypes through systems biology approaches, ensuring computational robustness is not merely a technical concern but a fundamental requirement for generating biologically meaningful insights that can translate to clinical applications.
Foundational Principles of Model Robustness in Systems Biology
Defining and Quantifying Robustness
Robustness in computational systems biology can be systematically defined as the property of a model to maintain invariant outputs with respect to a defined set of perturbations [71]. This definition requires precise specification of four elements: the system being studied, the property of interest, the perturbations considered, and the degree of invariance expected [72]. In practical terms for disease endotype research, this means explicitly stating which network behaviors or classification outcomes must remain stable despite variations in parameters, input data, or model structure.
Several methodologies have been established for quantifying robustness in biological models:
- Robustness of cell types: Measured as the percentage of gain- or loss-of-function mutations the system can resist without losing specific stationary or cyclic patterns of molecular activation [72].
- Robustness to update rule changes: Evaluated by generating numerous model instances, each affected by minimal changes to the update rules, then calculating the mean number of attractors and their variance across the population [72].
- Sensitivity analysis: Measures how each component of the update rule responds to molecular activation noise by testing the system's response to bit-flip perturbations in random initial states [72].
- Targeted perturbation robustness: Assesses the fraction of perturbations to key molecular nodes (e.g., transcription factors, microenvironment signals) that the system can absorb while maintaining original classification behavior [72].
Mechanisms Underlying Biological and Computational Robustness
Biological systems achieve robustness through several well-characterized architectural principles that can be mirrored in computational approaches:
- Functional redundancy: Multiple components capable of performing the same function [71]
- Response diversity: Varied response characteristics among functionally similar components [71]
- Modularity: Decomposition into functionally separable subsystems [71]
- Bow-tie architectures: Organizational structures where diverse inputs converge to a common core, which then fans out to diverse outputs [71]
- Degeneracy: The ability of structurally different elements to perform similar functions under certain conditions [71]
These biological principles inform the design of robust computational workflows for endotype identification. For instance, incorporating degeneracy through multiple algorithmic approaches for the same classification task can enhance overall system resilience to variations in input data quality or type.
Table 1: Strategies for Achieving Robustness in Biological Systems and Their Computational Analogues
| Biological Strategy | Description | Computational Analogue |
|---|---|---|
| Homeostasis | Maintenance of internal stability through feedback mechanisms | Automated parameter optimization with constraint enforcement |
| Adaptive Plasticity | Ability to adjust to environmental changes | Transfer learning and model fine-tuning for new data types |
| Environment Shaping | Modifying external conditions to maintain function | Data preprocessing and normalization pipelines |
| Environment Tracking | Following changing conditions | Online learning and model versioning systems |
Computational Workflow Optimization for Endotype Discovery
Integrated Systems Biology Platform Architecture
An optimized computational workflow for disease endotype discovery requires a systematic, multi-stage architecture that integrates diverse data types and analytical approaches. The platform should facilitate the characterization of key pathways contributing to the Mechanism of Disease (MOD) followed by identification of therapies that can reverse pathological mechanisms through targeted Mechanisms of Action (MOA) [73]. This process bridges molecular-level discoveries with clinical applications through several interconnected phases.
The foundational phase involves data acquisition and integration from multi-omics technologies, including genomics, transcriptomics, proteomics, and metabolomics [73]. The increasing ability to probe biology at cellular and organ levels with these technologies provides unprecedented potential to decode complex biological systems implicated in disease, though challenges remain in data fidelity, experimental costs, and translatability of preclinical models [73]. Subsequent phases include network construction and analysis, predictive modeling, and clinical translation, each requiring specialized computational tools and optimization strategies.
Workflow Optimization Strategies
Optimizing computational workflows for endotype discovery requires addressing several performance bottlenecks while maintaining scientific rigor:
- Parallelization of data processing: Distributing computationally intensive omics data preprocessing across high-performance computing clusters can reduce processing time from days to hours.
- Modular pipeline architecture: Implementing workflow management systems (e.g., Nextflow, Snakemake) enables reproducible, scalable, and portable analyses across computing environments.
- Incremental model training: For machine learning components, implementing checkpointing and transfer learning approaches minimizes computational costs when expanding models with new data.
- Multi-resolution modeling: Combining coarse-grained and fine-grained modeling approaches allows researchers to focus computational resources on the most critical pathway components.
Table 2: Quantitative Performance Metrics for Optimized Computational Workflows in Endotype Discovery
| Workflow Component | Baseline Performance | Optimized Performance | Key Optimization Strategy |
|---|---|---|---|
| Genomic Data Processing | 48-72 hours for 1000 samples | 4-8 hours for 1000 samples | Distributed computing with Spark |
| Network Inference | Limited to 500 nodes | Scalable to 10,000+ nodes | Approximate algorithms with theoretical guarantees |
| Single-Cell Analysis | Memory-intensive, limited by RAM | Streamlined processing | Dimensionality reduction and sparse matrix operations |
| Cross-Validation | Sequential processing | Parallelized execution | Distributed hyperparameter optimization |
| Model Interpretation | Manual feature importance | Automated significance testing | Integrated SHAP values with statistical validation |
Experimental Protocols for Robustness Assessment
Comprehensive Robustness Testing Framework
Ensuring model robustness requires systematic experimental protocols that evaluate performance under diverse perturbation conditions. The framework should assess robustness across multiple dimensions: structural robustness (sensitivity to model architecture changes), parametric robustness (sensitivity to parameter variations), and data robustness (sensitivity to input data quality and completeness) [72]. This multi-faceted approach provides a comprehensive assessment of model reliability for endotype classification.
A robust testing protocol begins with defining the specific traits or outputs being evaluated—in endotype discovery, this typically includes cluster stability, classification accuracy, and biological interpretability. The system is then exposed to controlled perturbations while measuring the preservation of these key properties [72]. Documenting both the magnitude of perturbations the system can withstand and the conditions under which it fails provides crucial information for interpreting model outputs in research contexts.
Protocol for Assessing Endotype Classification Robustness
The following step-by-step protocol provides a standardized approach for evaluating the robustness of computational methods for disease endotype identification:
Define Evaluation Metrics: Establish quantitative measures for endotype classification performance, including cluster stability indices, biological coherence scores, and clinical relevance metrics.
Generate Perturbation Set: Create systematic perturbations of input data, including:
- Additive noise at varying signal-to-noise ratios
- Subsampling to simulate missing data scenarios
- Batch effect simulations to mimic technical variability
- Biological noise estimation through bootstrap resampling
Execute Robustness Tests:
- For each perturbation level, run the complete endotype discovery pipeline
- Compute concordance between original and perturbed results using adjusted Rand index or similar measures
- Track performance metrics across perturbation intensities
Analyze Failure Modes:
- Identify specific perturbation thresholds where classification performance degrades significantly
- Document which endotype categories show greatest sensitivity to perturbations
- Map fragile components to specific biological pathways or algorithmic steps
Implement Robustness Improvements:
- Integrate stabilization techniques where fragility is identified
- Apply ensemble methods to reduce variance in sensitive components
- Introduce regularization to prevent overfitting to noise
Validate with Experimental Data:
- Test robustness predictions using independent validation datasets
- Correlate computational robustness measures with experimental reproducibility
- Establish acceptable robustness thresholds for clinical translation
Successful implementation of robust computational workflows for endotype discovery requires both wet-lab and computational resources. The following toolkit outlines essential components for an integrated research pipeline:
Table 3: Research Reagent Solutions for Endotype Discovery and Model Validation
| Resource Category | Specific Examples | Function in Workflow |
|---|---|---|
| Multi-omics Data Platforms | RNA sequencing kits, Mass spectrometry systems, Epigenetic profiling assays | Generate molecular profiling data for endotype classification |
| Public Data Repositories | GEO, TCGA, GTEx, Human Cell Atlas | Provide reference datasets for model training and validation |
| Computational Libraries | Scikit-learn, TensorFlow, PyTorch, Scanpy, Seurat | Implement machine learning and statistical analysis methods |
| Network Analysis Tools | Cytoscape, NetworkX, igraph, Gephi | Construct and analyze biological networks for mechanism identification |
| Visualization Platforms | ggplot2, Plotly, Matplotlib, Tableau | Create interpretable visualizations of endotype classifications |
| Workflow Management Systems | Nextflow, Snakemake, Galaxy, Cromwell | Ensure reproducibility and scalability of analytical pipelines |
| High-Performance Computing | Cloud computing platforms, SLURM clusters, Docker containers | Provide computational resources for large-scale analyses |
Visualization Strategies for Quantitative Data in Endotype Research
Effective Visualization Selection
Communicating complex quantitative relationships in endotype research requires careful selection of visualization approaches based on the specific analytical task. Different visualization types serve distinct purposes in the analytical workflow:
- Heatmaps: Ideal for displaying gene expression patterns across endotype subgroups, allowing rapid identification of differentially expressed pathways [74].
- Network diagrams: Essential for visualizing interaction networks and signaling pathways that define specific endotypes, highlighting key regulatory nodes and connections.
- Dimensionality reduction plots: Techniques like t-SNE and UMAP provide intuitive representations of high-dimensional omics data, revealing natural clustering of samples into endotypes.
- Bar and line charts: Effective for comparing quantitative metrics (e.g., pathway activation scores, clinical measurements) across identified endotype groups [75].
Color and Contrast Considerations for Scientific Visualization
Adhering to accessibility guidelines in data visualization ensures that research findings are interpretable by all audience members, including those with color vision deficiencies. The Web Content Accessibility Guidelines (WCAG) specify a minimum color contrast ratio of 4.5:1 for regular text and 3:1 for large text and essential icons [76]. Using the specified color palette while maintaining these contrast requirements involves:
- Applying sufficient luminance difference between foreground and background elements
- Avoiding color alone to convey critical information
- Utilizing patterns, textures, or direct labels as supplemental discriminators
- Testing visualizations in grayscale to detect potential interpretation issues
The identification of disease endotypes through systems biology represents a paradigm shift in biomedical research, moving beyond symptomatic classifications toward mechanism-based stratification. The reliability of this approach depends fundamentally on the robustness of the computational workflows and models employed. By implementing systematic robustness assessment protocols, optimizing computational pipelines for performance and reproducibility, and adhering to visualization best practices, researchers can accelerate the discovery of meaningful disease endotypes with potential for transformative clinical applications.
As systems biology continues to evolve with advancements in single-cell technologies, spatial omics, and artificial intelligence, the principles of model robustness will become increasingly critical for distinguishing biologically significant patterns from analytical artifacts. Building these considerations into the foundational architecture of computational workflows—rather than as afterthoughts—will enhance both the scientific validity and clinical translation of endotype research, ultimately supporting the development of targeted therapeutics for patients with distinct disease mechanisms.
Bench to Bedside: Validating Endotypes and Assessing Clinical Impact
Complex diseases have long been diagnosed and treated based on observable clinical characteristics, or phenotypes. However, individuals with similar symptom profiles often exhibit markedly different responses to treatment, underscoring the limitations of this approach. The emerging paradigm of precision medicine seeks to address this by classifying diseases based on endotypes—distinct biological mechanisms or pathways that underlie the observable disease characteristics [64]. Clinical validation of these endotypes represents a critical bridge between the discovery of novel disease mechanisms and the delivery of improved patient outcomes. This process systematically evaluates whether endotypic classifications reliably predict disease course, treatment response, and health impacts, thereby enabling a more targeted and effective approach to patient care [77] [78]. This guide details the framework, methodologies, and tools required for this rigorous validation process within the broader context of identifying disease endotypes through systems biology research.
Defining the Framework: From Phenotypes to Validated Endotypes
Conceptual Foundations
A clear understanding of the terminology is essential for clinical validation:
- Phenotype: The observable characteristics of a disease (e.g., symptoms, exacerbation frequency, imaging patterns) without implication of the underlying mechanism [1] [78]. Phenotypes are clinically valuable but often represent heterogeneous groups.
- Endotype: A disease subtype defined by a distinct functional or pathobiological mechanism [64] [78]. Endotypes are characterized by specific biomarker profiles and are ideally suited for targeted therapies.
- Treatable Trait: A detectable and clinically relevant disease characteristic that can be targeted by therapy [1].
A single clinical phenotype, such as "severe asthma" or "frequent exacerbator COPD," can encompass multiple underlying endotypes. For instance, the "frequent exacerbator" phenotype in Chronic Obstructive Pulmonary Disease (COPD) may be driven by an eosinophilic inflammation endotype or an infection-dominant endotype, each requiring different therapeutic strategies [1]. The primary goal of clinical validation is to confirm that this mechanistic distinction translates to meaningful differences in patient outcomes.
The Clinical Validation Pathway
The translation of a putative endotype from a research concept to a clinically useful tool follows a structured pathway. The working group on Obstructive Sleep Apnea (OSA) endophenotyping has outlined a development framework from derivation to implementation, which can be generalized to other complex diseases [77]. The key phases and associated research priorities are summarized in the table below.
Table 1: Key Areas and Research Priorities for Clinical Validation of Endotypes
| Key Area | Description | Specific Research Priorities |
|---|---|---|
| Technical Standards & Validation | Establishing reliability and generalizability of endotypic metrics. | - Set standards for signal quality and data scoring [77].- Establish thresholds based on clinically important outcomes [77].- Examine generalizability across diverse populations and stability over time [77]. |
| Prospective Study Conduct | Demonstrating utility in real-world clinical decision-making. | - Investigate joint effects and interplay among endotypes and clinical characteristics [77].- Use precision medicine principles to design studies of endotype-informed therapy [77].- Pre-specify hypotheses, analysis plans, and outcomes [77]. |
| Impact Analysis & Implementation | Assessing the real-world value and feasibility of endotype-driven care. | - Assess potential clinical and financial benefits via comparative effectiveness research [77].- Establish clinical registries for collaborative knowledge exchange [77]. |
A critical challenge in this pathway is establishing minimally clinically important differences (MCIDs) for endotypic metrics. Validation requires linking these metrics to patient-centric outcomes, such as symptom improvement, reduced exacerbations, enhanced quality of life, or survival benefit [77].
Experimental and Methodological Approaches
Integrating Multi-Modal Data for Endotype Discovery
The initial discovery of endotypes often relies on integrative analysis of high-dimensional data. A multi-step decision tree-based method has been developed for this purpose, effectively combining gene expression, demographic, and clinical data to define disease endotypes in a purely data-driven manner [79] [4]. This method was successfully applied in the Mechanistic Indicators of Childhood Asthma (MICA) study, where it outperformed traditional approaches like t-tests or single-domain clustering in segregating asthmatics from non-asthmatics and providing biological insights [79]. The core workflow of this methodology is outlined below.
Diagram 1: Endotype discovery workflow. This data-driven process integrates clinical and molecular data to define distinct patient subgroups.
Protocol for Prospective Validation Studies
Robust clinical validation requires prospective studies designed to test specific hypotheses about an endotype's predictive value. The core components of such a study protocol, based on Good Clinical Practice (GCP) guidelines, must be meticulously planned [80].
Table 2: Key Elements of a Prospective Endotype Validation Study Protocol
| Protocol Component | Description & Application to Endotype Validation |
|---|---|
| Objectives & Endpoints | Clearly state the primary objective (e.g., to test if Endotype X predicts superior response to Therapy Y). Define corresponding endpoints (e.g., exacerbation rate, symptom score, lung function). |
| Study Design | Use a randomized controlled trial (RCT) design, ideally double-blind. Framework: endotype-informed therapy vs. standard care. Include measures to minimize bias (randomization, blinding) [80]. |
| Eligibility Criteria | Define inclusion/exclusion criteria that ensure an appropriate study population. Criteria should be specific enough for scientific validity but not so restrictive as to hinder recruitment [80]. |
| Interventions | Detail the dosing, frequency, and duration of the investigational and control treatments. Describe procedures for allocating participants to treatment arms based on endotypic status. |
| Assessments & Schedule | Provide a detailed plan for all efficacy and safety assessments. A Schedule of Events table is crucial for mapping all visits and measurements over the study course [80]. |
| Statistical Plan | Specify the statistical tests for the primary endpoint and justify the sample size with a power calculation. Pre-specify how missing data and interim analyses will be handled [77] [80]. |
A common pitfall is "unfocused or overambitious objectives." The protocol should prioritize a clear primary objective and a few secondary ones to maintain feasibility and scientific integrity [80].
The Scientist's Toolkit: Essential Reagents and Assays
Validating endotypes requires a suite of reliable tools to measure key biomarkers and biological processes. The following table catalogs essential research reagents and their applications, drawing from examples in allergy, COPD, and chronic rhinosinusitis.
Table 3: Key Research Reagent Solutions for Endotype Validation
| Reagent / Assay | Function / Target | Application in Endotyping |
|---|---|---|
| Cytokine-Specific ELISA/Kits | Quantify protein levels of key cytokines (e.g., IL-4, IL-5, IL-13, IL-17A, IFN-γ, IL-8) [81]. | Discriminate between T2-high (IL-4, IL-5, IL-13) and T2-low (IL-17, IFN-γ) inflammatory endotypes in asthma, CRS, and COPD [78] [81]. |
| Flow Cytometry Panels | Immunophenotyping of immune cells (e.g., eosinophils, neutrophils, Th1/Th2/Th17 cells, ILCs) using fluorescently-labeled antibodies. | Profile cellular inflammation in blood or tissue. Essential for identifying eosinophilic vs. neutrophilic endotypes [78] [81]. |
| Gene Expression Microarrays/RNA-Seq | Genome-wide profiling of transcriptomic signatures from blood or tissue [79]. | Identify gene expression endotypes (e.g., T2-high "Th2-signature") and discover novel molecular subtypes [64] [79]. |
| qPCR Assays | Targeted quantification of specific mRNA transcripts (e.g., periostin, CXCL9, CXCL10, MPO) [81]. | Measure validated gene biomarkers in a high-throughput, cost-effective manner for patient stratification. |
| Immunofluorescence Staining Kits | Visualize and quantify protein localization and cell types in tissue sections (e.g., human neutrophil elastase (HNE)+ cells) [81]. | Confirm tissue-level pathology and immune cell infiltration characteristic of specific endotypes (e.g., T3 CRS). |
Case Studies: Signaling Pathways in Defined Endotypes
The clinical significance of endotypes is best illustrated by examining well-characterized immune pathways. Chronic Rhinosinusitis (CRS) offers a clear example, with distinct type 1 (T1), type 2 (T2), and type 3 (T3) endotypes driven by different cytokine networks [81]. The following diagrams delineate the key signaling pathways for the T2 and T3 endotypes, which are clinically relevant for biologic therapy.
Type 2 (T2) High Endotype Pathway
The T2 endotype, common in Western CRS cohorts and allergic asthma, is driven by epithelial-derived alarmins that activate a characteristic inflammatory cascade.
Diagram 2: T2 high endotype pathway. This pathway underlies eosinophilic inflammation and is targeted by modern biologics.
Type 3 (T3) Endotype Pathway
The T3 endotype, more prevalent in Asian CRS cohorts, is characterized by neutrophil-dominant inflammation and is often associated with corticosteroid resistance.
Diagram 3: T3 endotype neutrophilic pathway. This pathway drives steroid-resistant disease and requires different therapeutic strategies.
The clinical validation of endotypes is a multi-stage, iterative process that moves from mechanistic discovery to demonstrated clinical utility. By employing robust systems biology approaches for discovery, followed by rigorous prospective studies and standardized biomarker assays, researchers can successfully link endotypic mechanisms to meaningful patient outcomes. This foundational work is pushing medicine toward a future where treatment is no longer based solely on symptomatic phenotypes but is precisely targeted to the underlying pathological drivers of an individual's disease. The ongoing development of new biologic therapies makes this paradigm shift not just a scientific opportunity, but a clinical and economic imperative for improving patient care [77] [78] [81].
Comparative Analysis of Endotype-Driven vs. Phenotype-Driven Therapies
The paradigm of disease management is transitioning from a one-size-fits-all approach to precision strategies that account for individual patient variability. This shift is underpinned by two distinct frameworks: phenotype-driven therapies, which target observable clinical characteristics, and endotype-driven therapies, which target underlying biological mechanisms. Within the context of systems biology research, this review provides a comparative analysis of these approaches, examining their conceptual foundations, therapeutic implications, and experimental methodologies. Using chronic obstructive pulmonary disease (COPD) and allergic diseases as key examples, we demonstrate how the identification of disease endotypes through multi-omics integration enables more precise therapeutic targeting. The analysis further details standardized protocols for endotype discovery and presents a structured framework for evaluating both approaches, offering researchers and drug development professionals a technical roadmap for implementing precision medicine paradigms.
Precision medicine represents a transformative approach to patient care that moves beyond universal treatment strategies to account for individual variability in disease susceptibility, presentation, and therapeutic response. This paradigm shift is catalyzed by advancements in systems biology, which enables the integration of multi-omics data to delineate disease heterogeneity. Within this framework, two complementary yet distinct concepts have emerged: phenotypes, defined as collections of observable clinical characteristics such as symptoms, exacerbation frequency, and imaging patterns; and endotypes, defined as disease subtypes characterized by distinct biological or pathophysiological mechanisms [1] [64].
The fundamental distinction between these approaches lies in their level of biological explanation. Phenotypic classification facilitates the identification of clinically relevant subgroups based on manifestations that can be readily observed in practice, such as the "frequent-exacerbator" or "emphysema-dominant" subtypes in COPD [1]. While clinically valuable, phenotypes do not necessarily reveal underlying disease mechanisms and may encompass multiple distinct biological pathways. In contrast, endotype-driven strategies aim to align therapeutics with the specific molecular pathways driving disease, such as neutrophilic inflammation, eosinophilic airway involvement, or α1-antitrypsin deficiency in COPD [1]. This mechanistic alignment promises more targeted interventions with potentially greater efficacy and fewer off-target effects.
Systems biology serves as the foundational discipline bridging these concepts by providing the methodological toolkit for endotype discovery. Through integrated analysis of genomic, proteomic, transcriptomic, and metabolomic data, systems biology maps the complex network of molecular interactions that give rise to observable clinical presentations [28]. This multi-layered approach enables the transition from descriptive phenotyping to mechanistic endotyping, facilitating the development of therapies that target causal pathways rather than symptomatic manifestations.
Conceptual Foundations and Definitions
Phenotype-Driven Approach: Clinical Manifestations
The phenotype-driven approach to disease classification and treatment focuses on clustering patients based on observable properties, including clinical symptoms, physiological traits, trigger factors, comorbidities, and treatment responses [64]. In clinical practice, phenotypic classification has proven valuable for identifying patient subgroups with distinct prognostic outcomes and therapeutic needs.
In COPD, prominent phenotypes include the chronic bronchitis phenotype characterized by productive cough and airway inflammation, and the emphysematous phenotype (historically labeled "pink puffer") characterized by extensive alveolar destruction, diminished diffusion capacity, and pulmonary hyperinflation [1]. Another clinically significant classification is the "frequent-exacerbator" phenotype, which identifies patients prone to recurrent acute worsening of symptoms regardless of disease severity [1]. Similarly, in allergic diseases, phenotypic classification often categorizes patients based on inflammatory cell patterns observed in sputum (eosinophilic, neutrophilic, mixed granulocytic, and paucigranulocytic) or blood [64].
A significant limitation of phenotypic classification is its potential instability over time and tendency for overlap between categories [64]. Furthermore, while phenotypes effectively describe clinical presentations, they do not inherently provide insight into the underlying pathogenetic mechanisms, potentially limiting their utility for developing targeted therapeutics.
Endotype-Driven Approach: Biological Mechanisms
The endotype-driven approach represents a more granular framework that classifies disease based on distinct biological mechanisms, pathological pathways, or molecular signatures. Unlike phenotypes, which are descriptive, endotypes are explanatory, delineating the causal pathways that give rise to observable clinical features [1] [64].
In COPD, endotypic characterization has identified several mechanistically distinct subgroups, including those driven by neutrophilic inflammation, eosinophilic airway involvement, or specific genetic determinants such as α1-antitrypsin deficiency [1]. These endotypes may demonstrate superior predictive value for therapeutic responses compared to phenotypic classifications alone. In allergic diseases, endotyping has primarily distinguished between type 2-high and type 2-low immune responses [64]. The type 2-high endotype involves multiple immune components including Th2 cells, type 2 innate lymphoid cells (ILC2s), eosinophils, mast cells, and their associated cytokines (IL-4, IL-5, IL-13) and IgE antibodies [64].
Modern systems biology recognizes that endotypes are frequently dynamic and complex, with nonlinear interactions between multiple pathogenic pathways that may not be present in all patients or at all time points [64]. The concept of "complex endotypes" acknowledges this multidimensionality, as seen in the complex type 2 endotype which encompasses several molecular subendotypes that may vary longitudinally.
The "Treatable Traits" Framework: Bridging Concepts
A strategic framework that integrates both phenotypic and endotypic approaches is the "treatable traits" model. This paradigm emphasizes identifying and targeting modifiable clinical, physiological, inflammatory, microbiological, psychosocial, and comorbidity factors that extend beyond traditional disease classification systems [1]. In COPD, the treatable traits framework enables personalized management by addressing factors such as exacerbation triggers, comorbid conditions, and psychosocial determinants that influence disease expression and progression [1]. Similarly, in infectious diseases, this approach aims to identify host traits amenable to therapeutic intervention, potentially altering disease trajectories in susceptible individuals [82].
Table 1: Comparative Characteristics of Phenotype-Driven and Endotype-Driven Approaches
| Characteristic | Phenotype-Driven Approach | Endotype-Driven Approach |
|---|---|---|
| Definition | Based on observable clinical characteristics and manifestations | Based on underlying biological mechanisms and pathways |
| Primary Focus | Symptoms, imaging patterns, exacerbation frequency, treatment response | Molecular pathways, inflammatory patterns, genetic determinants |
| Stability | May change over time and overlap with other phenotypes | Relatively stable, though dynamic complex endotypes exist |
| Measurement | Clinical assessment, imaging, physiological tests | Biomarkers, multi-omics profiling, molecular assays |
| Therapeutic Implication | Empiric therapy based on clinical presentation | Targeted therapy aligned with pathological mechanism |
| Examples | "Frequent-exacerbator" COPD, emphysema-dominant COPD | Eosinophilic inflammation-driven COPD, α1-antitrypsin deficiency |
Therapeutic Implications and Clinical Applications
Phenotype-Driven Therapeutic Strategies
Phenotype-driven therapies have established value in guiding empirical treatment approaches for complex diseases. In COPD management, phenotypic classification directly informs therapeutic selection:
- Emphysema-dominant phenotype: These patients typically demonstrate limited response to inhaled corticosteroids but may derive significant benefit from bronchodilators and lung volume reduction procedures [1].
- Chronic bronchitis phenotype: This subgroup may respond more favorably to mucolytic agents and phosphodiesterase-4 inhibitors targeting airway inflammation and mucus hypersecretion [1].
- Frequent-exacerbator phenotype: Regardless of baseline severity, these patients are often prescribed inhaled corticosteroids to reduce exacerbation frequency, though with variable response rates [1].
The strength of phenotype-driven therapy lies in its immediate clinical applicability, as phenotypic classification typically relies on readily available clinical parameters rather than specialized molecular assays. However, the variable treatment responses observed within phenotypic groups highlight the limitations of this approach, which necessarily groups together patients with diverse underlying disease mechanisms.
Endotype-Driven Targeted Therapies
Endotype-driven therapies represent a more mechanistic approach that aligns treatments with specific pathological pathways, often yielding more predictable responses:
- Eosinophilic inflammation endotype: In both COPD and severe asthma, patients with this endotype, characterized by elevated blood or sputum eosinophils, demonstrate consistent response to corticosteroid therapy and targeted biologics such as anti-IL-5 agents (mepolizumab, reslizumab) and anti-IL-5Rα (benralizumab) [1] [64].
- Type 2-high endotype: This complex inflammatory pattern, identifiable through biomarkers including blood eosinophils, fractional exhaled nitric oxide (FeNO), and serum periostin, predicts favorable response to multiple targeted therapies including anti-IgE (omalizumab), anti-IL-4/IL-13 (dupilumab), and CRTH2 antagonists [64].
- Neutrophilic inflammation endotype: Preclinical and clinical investigations are exploring targeted approaches for this COPD endotype, including CXCR2 antagonists to dampen neutrophil recruitment and activation [1].
The predictive value of endotypic classification is particularly evident in the context of biologic therapies, where targeting specific molecular pathways (IL-5, IL-4/IL-13, IgE, TSLP) yields dramatically different responses across patient subgroups defined by their underlying biological mechanisms [64].
Comparative Therapeutic Outcomes
Table 2: Therapeutic Responses in Phenotype-Driven vs. Endotype-Driven Approaches
| Disease Context | Approach | Classification Method | Therapeutic Intervention | Response Rate |
|---|---|---|---|---|
| Severe Asthma | Phenotype-Driven | Sputum inflammatory cells (eosinophilic vs. neutrophilic) | Inhaled corticosteroids | Variable; higher in eosinophilic phenotype |
| Severe Asthma | Endotype-Driven | Type 2-high biomarkers (FeNO, blood eosinophils, periostin) | Anti-IL-5/IL-13 biologics | Consistently high in type 2-high endotype |
| COPD | Phenotype-Driven | Frequent-exacerbator phenotype | Inhaled corticosteroids | Moderate (~20-30% reduction in exacerbations) |
| COPD | Endotype-Driven | Blood eosinophil count ≥300/μL | Inhaled corticosteroids | Stronger reduction (~40-50%) in exacerbations |
| Allergic Diseases | Phenotype-Driven | Clinical presentation and triggers | Allergen avoidance, antihistamines | Symptomatic relief only |
| Allergic Diseases | Endotype-Driven | Specific IgE, component-resolved diagnostics | Allergen immunotherapy | Potential disease-modifying effects |
Experimental Methodologies for Endotype Identification
Multi-Omics Integration and Systems Biology Approaches
The identification of disease endotypes requires experimental methodologies capable of capturing the complex molecular networks underlying disease manifestations. Systems biology provides an integrative framework for combining data from multiple omics layers:
- Genomic analyses: Identify hereditary susceptibility patterns and rare variants contributing to disease pathogenesis. Whole genome or exome sequencing facilitates the discovery of genetic endotypes, as demonstrated in rare genetic diseases where specific gene mutations define distinct endotypes [83].
- Transcriptomic profiling: RNA sequencing and microarray analyses of relevant tissues (e.g., bronchial epithelium in COPD, nasal polyps in chronic rhinosinusitis) reveal gene expression signatures characteristic of specific endotypes [64] [28]. For instance, IL-13-responsive gene signatures including periostin identify type 2-high inflammation endotypes [64].
- Proteomic and metabolomic analyses: Mass spectrometry-based profiling of proteins and metabolites in biofluids or tissues provides functional readouts of pathway activities, offering insights into inflammatory endotypes and metabolic dysregulation [28].
Network-based modeling approaches visualize and analyze the complex interactions between molecular components, identifying functional modules associated with specific endotypes [28]. Protein-protein interaction networks, gene co-expression networks, and multiplex-heterogeneous networks that integrate different data types enable the prediction of novel molecular interactions and pathway associations [28].
Protocol for Endotype Discovery Using Multi-Omics Data
Objective: To identify molecular endotypes in a heterogeneous disease population through integrated multi-omics analysis.
Materials:
- Patient biospecimens (blood, tissue, bronchoalveolar lavage)
- RNA/DNA extraction kits
- Microarray or RNA-sequencing platform
- Mass spectrometry system for proteomic/metabolomic analysis
- Computational infrastructure for bioinformatic analyses
Procedure:
Cohort Selection and Phenotypic Characterization:
- Recruit well-characterized patient cohort representing disease heterogeneity
- Document comprehensive clinical parameters, including symptoms, exacerbation history, treatment response, and comorbidities
- Obtain informed consent and ethical approval
Sample Processing and Data Generation:
- Process biospecimens for multi-omics analyses using standardized protocols
- Perform RNA/DNA extraction with quality control (RNA integrity number >7.0)
- Conduct transcriptomic profiling using RNA-sequencing (minimum 30 million reads per sample)
- Perform proteomic analysis using liquid chromatography-mass spectrometry
- Generate metabolomic profiles using nuclear magnetic resonance or mass spectrometry
Data Integration and Network Analysis:
- Preprocess raw data: normalize expression data, impute missing values, and batch correct
- Identify differentially expressed genes, proteins, and metabolites between clinical subgroups
- Construct correlation networks using weighted gene co-expression network analysis (WGCNA)
- Perform pathway enrichment analysis using databases such as KEGG and Reactome
- Apply multivariate statistical methods (principal component analysis, partial least squares-discriminant analysis) to identify multi-omics signatures
Endotype Validation:
- Validate identified endotypes in independent patient cohorts
- Correlate molecular endotypes with clinical outcomes and treatment responses
- Develop simplified biomarker panels for clinical translation
Visualization of Endotype Discovery Framework
Diagram 1: Systems Biology Framework for Endotype Discovery. This workflow illustrates the integration of clinical phenotyping with multi-omics data to identify molecular endotypes and develop targeted therapies.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Endotype Research
| Category | Specific Tools/Reagents | Research Application |
|---|---|---|
| Omics Technologies | RNA-sequencing platforms | Transcriptomic profiling of disease tissues |
| LC-MS/MS systems | Proteomic and metabolomic analyses | |
| DNA microarrays | Genotypic variation screening | |
| Bioinformatics Tools | WGCNA (Weighted Gene Co-expression Network Analysis) | Construction of gene co-expression networks |
| Limma R package | Differential expression analysis | |
| STRING database | Protein-protein interaction network mapping | |
| Cell Assay Systems | ELISA kits | Cytokine quantification |
| Flow cytometry panels | Immune cell phenotyping | |
| Multiplex immunoassays | Simultaneous measurement of multiple analytes | |
| Computational Resources | Graph databases | Network representation and analysis |
| Machine learning frameworks | Pattern recognition in high-dimensional data | |
| Cloud computing platforms | Large-scale data processing and storage |
The comparative analysis of endotype-driven versus phenotype-driven therapeutic approaches reveals a progressive evolution in precision medicine, from symptom-based classification to mechanism-targeted intervention. While phenotypic characterization remains clinically valuable for initial patient stratification, its limitations in predicting treatment response highlight the necessity of incorporating endotypic understanding into therapeutic development. The integration of systems biology methodologies, particularly multi-omics data integration and network-based analysis, provides the foundational toolkit for identifying molecular endotypes across diverse disease contexts. As these approaches mature, the paradigm of "treatable traits" offers a pragmatic framework for implementing precision medicine in clinical practice, simultaneously addressing phenotypic manifestations while targeting their underlying biological mechanisms. For researchers and drug development professionals, the strategic integration of both approaches will be essential for advancing the next generation of targeted therapeutics with optimized efficacy and minimal off-target effects.
The Role of Endotypes in Clinical Trial Design and Patient Stratification
The paradigm of drug development is shifting from a one-size-fits-all model towards precision medicine. This transition is fundamentally driven by the identification of disease endotypes—distinct biological subtypes defined by unique functional or pathophysiological mechanisms. Grounded in systems biology research, endotyping provides a powerful framework for deconstructing clinical heterogeneity into mechanistically discrete populations. This whitepaper delineates the critical role of endotypes in refining clinical trial design and patient stratification. It details how molecular profiling and advanced analytics are enabling a more targeted approach, which promises to enhance clinical trial success rates, identify responsive patient subpopulations, and ultimately, deliver more effective, personalized therapies.
In traditional medicine, disease classification and treatment have largely been based on clinical phenotypes, the observable characteristics and symptoms presented by a patient. However, significant variability in treatment response among patients with similar clinical presentations has underscored the limitations of this approach. This heterogeneity often masks distinct underlying disease drivers.
The concept of the endotype has emerged to address this gap. An endotype is a subtype of a condition defined by a distinct functional or pathobiological mechanism [8]. While a phenotype is what a clinician observes, an endotype explains why the disease manifests in a particular way. The identification of endotypes, facilitated by systems biology approaches that integrate multi-omics data, is revolutionizing clinical practice and therapeutic development by enabling mechanistic stratification of patient populations.
Methodologies for Endotype Discovery
The discovery of endotypes relies on high-dimensional data and sophisticated analytical tools to uncover the fundamental pathways that define a disease.
Systems Biology and Multi-Omics Integration
Systems immunology and other holistic approaches are critical for integrating the complex endotypes of diseases. These methods involve:
- Single-cell high-dimensional techniques to capture the signature of peripheral immune cells and the diversity of metabolic profiles [8].
- Transcriptomic and Proteomic Profiling: Uncovering gene expression patterns and protein abundance that point to activated pathways, such as interferon signatures or specific inflammatory cascades.
- Metabolomic and Lipidomic Analyses: Identifying unique metabolic dysregulations, such as a pro-inflammatory lipid signature, which can characterize a specific endotype [8].
Data Analysis and Artificial Intelligence
Once generated, this complex data requires advanced computational methods for interpretation:
- Cluster Analysis: Statistical techniques like k-means clustering or hierarchical clustering are applied to patient data to identify subgroups with shared molecular features.
- Artificial Intelligence Prediction Models: AI and machine learning models can process multi-omics data to predict endotype membership and uncover novel, non-intuitive subgroups [8].
- Principal Component Analysis (PCA): This technique helps to reduce the dimensionality of the data, visualizing and confirming the separation of distinct endotypes based on the most significant sources of variation [8].
Application in Clinical Trials and Patient Stratification
Integrating endotypes into clinical trial design transforms all phases of therapeutic development, making them more efficient and predictive of real-world success.
Enriching Trial Populations and Target Identification
A primary application of endotyping is in the strategic enrichment of clinical trial populations. By screening potential participants for specific molecular markers, trials can enroll a cohort that is more likely to respond to a mechanism-based intervention. This was exemplified in a randomized trial for chest pain with no obstructive coronary artery disease, where stress cardiovascular magnetic resonance imaging (MRI) was used to measure myocardial blood flow and endotype individual patients. This approach successfully reclassified the diagnosis in 53.0% of participants (131 patients), moving them from a generic "non-cardiac" diagnosis to a specific mechanistic endotype like microvascular angina [84]. This precise stratification is a prerequisite for successful targeted therapy.
Table 1: Impact of Endotyping on Diagnosis in a Chest Pain Trial [84]
| Diagnostic Group | Initial Angiography-Based Diagnosis | Post-CMR Endotyping Diagnosis |
|---|---|---|
| Microvascular Angina | 1 patient (0.4%) | 127 patients (51.0%) |
| Non-Cardiac Chest Pain | 244 patients (97.6%) | 117 patients (47.0%) |
| Reclassification Rate | 131 patients (53.0%) |
"Precision Treat-to-Target" and Biomarker Development
The endotype framework naturally supports a "precision treat-to-target" (T2T) strategy. In this model, treatment decisions are dynamically guided by the patient's underlying endotype and its associated biomarkers, rather than a static clinical protocol [56]. For instance, in primary Sjögren's disease, distinct endotypes are associated with differential responses to B cell-targeted therapies, interferon (IFN) pathway inhibitors, and immune regulatory interventions [56]. The development of this approach requires:
- Composite Clinical Endpoints: Endpoints that capture the multifaceted nature of complex diseases.
- Dynamic Monitoring Tools: The use of multi-omics biomarkers and AI-assisted stratification to track disease activity and treatment response over time, allowing for therapy adjustment [56].
Demonstrating Clinical Utility
Randomized controlled trials provide the highest level of evidence for the clinical utility of endotype-guided therapy. In the chest pain trial, the intervention group, which received endotyping-informed therapy, showed dramatically improved outcomes compared to the control group. The primary outcome was the Seattle Angina Questionnaire (SAQ) summary score at 12 months [84].
Table 2: Clinical Outcomes from an Endotyping-Informed Randomized Trial [84]
| Study Group | Baseline SAQ Summary Score | 12-Month SAQ Summary Score | Change from Baseline |
|---|---|---|---|
| Intervention (Endotype-Guided) | 49.2 | 70.9 | +21.7 |
| Control (Standard Care) | 52.9 | 52.1 | -0.8 |
| Adjusted Mean Difference | 20.9 (95% CI: 15.8–26.0) |
The intervention group also showed significant improvement in the health-related quality of life metric (EQ-5D-5L), with an adjusted mean difference of 0.09, confirming that endotype-guided care translates into tangible patient benefits [84].
Experimental Protocols for Endotype Investigation
Protocol: Non-Invasive Endotyping for Coronary Microvascular Dysfunction
This protocol is adapted from a published randomized trial [84].
Objective: To identify the vasomotor endotype (e.g., microvascular angina) in patients with chest pain and no obstructive coronary artery disease using quantitative perfusion imaging.
Materials:
- Patients with chest pain and a recent report of no obstructive coronary artery disease on invasive coronary angiography.
- Pharmacological stress agent (e.g., adenosine).
- 3T MRI scanner with quantitative perfusion mapping software.
- Electrocardiogram (ECG) monitoring equipment.
Procedure:
- Patient Preparation: Obtain informed consent. Withhold caffeine for 24 hours prior to the scan.
- Adenosine Stress CMR: Administer adenosine intravenously at a standard dose (e.g., 140 μg/kg/min) for 4-6 minutes under continuous ECG and blood pressure monitoring.
- Image Acquisition: Acquire myocardial perfusion images during the first pass of a gadolinium-based contrast agent bolus, both at rest and during peak adenosine stress.
- Quantitative Analysis: Calculate global myocardial blood flow (MBF) in mL min⁻¹ g⁻¹ for both rest and stress states. Derive the myocardial perfusion reserve (MPR) as the ratio of stress MBF to rest MBF.
- Endotyping: Classify patients based on quantitative MBF and MPR thresholds. For example, a globally reduced stress MBF (< ~2.3 mL min⁻¹ g⁻¹) in the absence of obstructive coronary artery disease indicates a microvascular angina endotype.
Protocol: Systems Immunology Endotyping
This protocol outlines a general approach for immune-endotype discovery, as applied in conditions like recessive dystrophic epidermolysis bullosa (RDEB) [8].
Objective: To characterize systemic immune and inflammatory endotypes through high-dimensional profiling of peripheral blood mononuclear cells (PBMCs).
Materials:
- Whole blood samples collected in sodium heparin tubes.
- Ficoll-Paque density gradient medium.
- Fluorescently conjugated antibodies for surface and intracellular markers (e.g., CD3, CD4, CD8, CD56, CD19, IFN-γ, TNF-α).
- Viability dye.
- Mass cytometer (CyTOF) or high-parameter flow cytometer.
- Cell culture medium (e.g., RPMI-1640 with fetal bovine serum).
Procedure:
- PBMC Isolation: Isolate PBMCs from whole blood using density gradient centrifugation. Cryopreserve cells or proceed with immediate staining.
- Cell Staining: Stimulate cells with PMA/ionomycin or specific antigens in the presence of a protein transport inhibitor for intracellular cytokine analysis. Stain cells with a panel of metal-conjugated or fluorescently conjugated antibodies against surface and intracellular targets.
- Data Acquisition: Acquire data on a high-dimensional cytometer.
- Computational Analysis: Use dimensionality reduction algorithms (e.g., t-SNE, UMAP) and clustering approaches (e.g., PhenoGraph) to identify distinct immune cell populations and activation states. Compare cluster abundances and functional states between patient groups and healthy controls to define endotypic signatures, such as activated/effector T cells and dysfunctional natural killer cells [8].
Visualization of Endotype-Informed Clinical Pathways
The following diagram illustrates the logical workflow for integrating endotyping into clinical research and patient management.
The Scientist's Toolkit: Key Research Reagents and Materials
The following table details essential materials used in the featured experimental protocols for endotype discovery.
Table 3: Key Research Reagent Solutions for Endotyping Studies
| Item | Function/Application in Endotyping |
|---|---|
| Adenosine | Pharmacologic stress agent used in cardiac MRI to assess coronary microvascular function and identify microvascular angina endotypes [84]. |
| Gadolinium-Based Contrast Agent | MRI contrast agent essential for first-pass perfusion imaging to quantitatively measure myocardial blood flow [84]. |
| Fluorescently/Metal-Labeled Antibodies | Panel of antibodies for high-dimensional cytometry (flow or mass) to profile immune cell populations and functional states for immune endotyping [8]. |
| PBMC Isolation Tubes (e.g., CPT) | Tubes containing sodium heparin and a density gradient medium for simplified and standardized isolation of peripheral blood mononuclear cells from whole blood [8]. |
| PMA/Ionomycin/Brefeldin A | Cell stimulation cocktail used in intracellular cytokine staining protocols to evaluate the functional capacity of T cells and other immune cells. |
| RNA Stabilization Reagent (e.g., PAXgene) | Reagent for immediate stabilization of RNA in whole blood samples, preserving the transcriptomic profile for subsequent RNA-seq analysis. |
The integration of endotypes into clinical trial design and patient stratification represents the forefront of precision medicine. Future research must focus on validating dynamic monitoring tools and optimizing biomarker-guided treatment pathways to advance personalized care [56]. Key challenges include the standardization of multi-omic assays, the development of accessible computational tools for clinical deployment, and the design of agile clinical trials that can adapt to evolving endotypic definitions.
In conclusion, moving from a phenotype-based to an endotype-driven framework deconvolutes disease heterogeneity, provides clear mechanistic targets for drug development, and enables the design of more efficient and successful clinical trials. By aligning therapeutic interventions with the specific pathobiological pathways active in a given patient, endotyping fulfills the promise of systems biology to deliver truly personalized and effective healthcare.
Evaluating the Efficacy of Targeted Biologics in Defined Endotypic Populations
The management of severe inflammatory diseases, particularly severe asthma, has been revolutionized by the advent of biologic therapies. However, significant clinical heterogeneity and complex, overlapping molecular pathways mean that single biologic agents often provide only partial disease control. This whitepaper examines the efficacy of targeted biologics within defined endotypic populations, framed through the lens of systems biology. By integrating multi-omics data to delineate disease endotypes—the specific biological mechanisms underpinning clinical phenotypes—we explore the rationale for, and outcomes of, precision-based biologic interventions. Furthermore, we present emerging evidence on dual biologic therapy as a strategic approach for managing multi-mechanistic severe disease, supported by real-world clinical data, quantitative efficacy metrics, and experimental protocols for endotype characterization.
In the era of precision medicine, the traditional classification of disease by clinical presentation (phenotype) is being superseded by a focus on the distinct functional or pathobiological mechanisms (endotypes) that drive these observable traits [85]. This endotypic approach is particularly relevant for complex, heterogeneous syndromes like severe asthma, where different underlying molecular pathways can result in similar symptoms but demand different therapeutic strategies [85].
Systems biology provides the foundational framework for identifying these endotypes. It integrates multi-layer omics data—genomic, proteomic, transcriptomic, and metabolomic—to model the complex intracellular networks and interactions that lead to disease manifestation [28]. Rather than examining single biomarkers in isolation, systems biology employs computational models to uncover the dynamic interplay between genes, proteins, and signaling pathways, thereby predicting disease mechanisms and drug responses [28]. As one study notes, "Endotypes are characterized by the immunological, inflammatory, metabolic, and remodelling pathways that explain the mechanisms underlying the clinical presentation (phenotype) of a disease" [8]. The goal of this whitepaper is to detail how this endotypic understanding, derived from systems biology, directly informs the evaluation and application of targeted biologics, leading to improved clinical outcomes.
Mapping Severe Asthma Endotypes to Biologic Therapies
Severe asthma is a paradigm for the application of endotype-driven treatment. The majority of severe asthma cases are driven by type 2 (T2) inflammation, an endotype characterized by the activation of innate and adaptive immune pathways leading to eosinophilia and elevated biomarkers like IgE and FeNO [85]. This T2-high endotype can be further subdivided, but it is collectively defined by cytokines including IL-4, IL-5, and IL-13, which are produced by T-helper 2 (Th2) cells and group 2 innate lymphoid cells (ILC2s) [85]. These pathways provide the targets for monoclonal antibody therapies.
Table 1: Mapping Severe Asthma Endotypes to Targeted Biologics
| Targeted Pathway | Biologic Agent(s) | Molecular Mechanism | Primary Endotypic Biomarkers |
|---|---|---|---|
| Immunoglobulin E (IgE) | Omalizumab | Binds to IgE, preventing activation of FcεRI receptors on mast cells and basophils [85]. | High serum IgE levels, allergic sensitization [85]. |
| Interleukin-5 (IL-5) | Mepolizumab, Reslizumab | Binds to IL-5, inhibiting eosinophil maturation, survival, and activation [85]. | Elevated blood/sputum eosinophils [86] [85]. |
| IL-5 Receptor α | Benralizumab | Binds to IL-5Rα, inducing antibody-dependent cell-mediated cytotoxicity of eosinophils [86]. | Elevated blood/sputum eosinophils [86]. |
| IL-4/IL-13 Receptor | Dupilumab | Binds to IL-4Rα, blocking signaling of both IL-4 and IL-13 [86] [85]. | Elevated FeNO, high periostin, eosinophilia [86] [85]. |
| TSLP (Alarmin) | Tezepelumab | Binds to TSLP, blocking its interaction with the TSLP receptor complex, thus inhibiting upstream initiation of type 2 inflammation [85]. | Broad T2-inflammatory biomarkers (e.g., FeNO, eosinophils) [85]. |
The rationale for biologic therapy is to specifically inhibit these key drivers of the inflammatory endotype. For example, in a patient with a severe eosinophilic asthma endotype, characterized by high blood or sputum eosinophil counts, targeting IL-5 with mepolizumab is a logical and evidence-based choice [85]. This precision approach moves beyond a one-size-fits-all strategy to a mechanism-driven selection of therapy.
Quantitative Efficacy of Biologics in Defined Populations
The efficacy of a biologic is most accurately evaluated when prescribed to a patient population sharing the specific endotype it targets. The following table summarizes key efficacy outcomes from clinical studies and real-world evidence, demonstrating the impact of this targeted approach.
Table 2: Efficacy Outcomes of Biologics in Targeted Severe Asthma Endotypes
| Biologic Agent | Clinical Context | Exacerbation Reduction | OCS Reduction | Lung Function (FEV1) Improvement | Biomarker Improvement |
|---|---|---|---|---|---|
| Mepolizumab (anti-IL-5) | Severe Eosinophilic Asthma [86] | Significant reduction (e.g., Case 1: 0 exacerbations post-therapy from 3/year) [86] | OCS discontinuation or significant dose reduction achieved [86] | Case 1: FEV1 increased from 1.39L to 1.58L [86] | BEC: 490 → 120 cells/µL; SEC: 67% → 4.5% [86] |
| Dupilumab (anti-IL-4Rα) | T2-high Asthma with Comorbidities [86] | Effective reduction of exacerbations [86] | Facilitated OCS tapering [86] | Improvements observed [86] | FeNO: 60 → 38 ppb; tIgE: 272.8 → 36.53 IU/mL [86] |
| Benralizumab (anti-IL-5Rα) | Severe Eosinophilic Asthma [86] | Stopped exacerbations in a case with EGPA [86] | OCS reduced from 30mg to 20mg/day [86] | Minimal improvement in a specific case [86] | Effectively depletes eosinophils [86] |
| Dual Therapy (e.g., Mepo + Dupi) | Multi-mechanistic or Refractory Disease [86] | Cessation of exacerbations in previously uncontrolled patients [86] | Enabled further OCS reduction (e.g., to 5-10mg/day) [86] | Varied response, from significant to minimal improvement [86] | Controlled dupilumab-induced hypereosinophilia (BEC: 1000 → 150 cells/µL) [86] |
The data in Table 2, drawn from a recent case series, highlights several key concepts. First, targeted biologics can achieve dramatic improvements in clinical outcomes and biomarker profiles. Second, for some patients with complex or overlapping endotypes, a single biologic may only achieve partial control, creating a rationale for dual therapy [86]. The series reported that all ten patients on dual biologics "exhibited good tolerance to the combined biologic therapies, leading to improvements in asthma and comorbidity management, and a reduction in OCS usage. No serious adverse events were reported" [86].
The Rationale and Evidence for Dual Biologic Therapy
For a subset of patients, disease persistence despite single biologic therapy has led to the exploration of dual biologic therapy. This advanced approach is considered when different pathological mechanisms continue to drive disease activity. The clinical decision-making for combination therapy generally follows three scenarios [86]:
- Inadequately Controlled Asthma Symptoms: When a patient's asthma remains uncontrolled despite an appropriate single biologic agent, suggesting involvement of additional inflammatory pathways not being suppressed [86].
- Poor Control of Type 2 Comorbidities: When a patient has severe asthma alongside uncontrolled T2-comorbidities such as Chronic Rhinosinusitis with Nasal Polyps (CRSwNP) or Atopic Dermatitis (AD). A combination can target the specific pathways dominant for each condition (e.g., mepolizumab for eosinophilic asthma and dupilumab for CRSwNP/AD) [86].
- Therapy-Induced Hypereosinophilia: In some patients, dupilumab (anti-IL-4/13R) can induce a marked increase in blood eosinophil counts. Adding an anti-IL-5 agent like mepolizumab can maintain clinical control of asthma and comorbidities while normalizing the eosinophil count [86].
The same case series provides examples of successful combinations, primarily mepolizumab + dupilumab, for these specific indications, demonstrating both efficacy and an acceptable safety profile over a mean duration of 13.5 months [86].
Experimental Protocols for Endotype Identification and Validation
The reliable identification of disease endotypes is a prerequisite for targeted therapy. The following workflow outlines a core experimental protocol based on systems biology principles.
Diagram 1: Endotype Identification Workflow (82 characters)
Detailed Methodology
Step 1: Sample Collection and Clinical Phenotyping: Recruit a well-characterized patient cohort. Collect relevant biospecimens (e.g., blood, tissue, BAL fluid) and compile extensive clinical data, including symptom scores (e.g., ACT), exacerbation history, lung function, and comorbidity status [86]. This establishes the clinical phenotype that will be linked to molecular data.
Step 2: Multi-Omics Data Acquisition: Process samples to generate high-dimensional data from multiple layers:
- Genomics: DNA sequencing to identify pathogenic variants or SNPs associated with disease [28].
- Transcriptomics: RNA-sequencing (RNA-seq) to profile gene expression patterns. Differentially Expressed Genes (DEGs) are identified using statistical packages like Limma in R [28].
- Proteomics/Metabolomics: Mass spectrometry to quantify protein or metabolite abundance, revealing functional effectors of disease [28].
Step 3: Network and Cluster Analysis: Use computational biology to integrate the omics data and infer functional interactions.
- Gene Co-expression Network Analysis: Tools like WGCNA (Weighted Gene Co-expression Network Analysis) are used to construct a scale-free network and detect functional gene clusters (modules) based on Pearson Correlation Coefficient (PCC) of gene co-expression [28]. Highly interconnected "hub genes" within disease-associated modules are considered key players.
- Protein-Protein Interaction (PPI) Networks: Map identified genes/proteins onto known PPI databases (e.g., STRING) to visualize densely connected modules that may correspond to functional pathways [28].
Step 4: Endotype Identification: The cohesive molecular modules (e.g., a "type 2 inflammation module" defined by co-expressed genes for IL-4, IL-5, IL-13, and their receptors) are defined as distinct endotypes. These are then correlated back to the specific clinical features from Step 1.
Step 5: Mechanistic Validation: The functional role of key drivers (hub genes) identified in the network analysis is validated in vitro (e.g., using cell lines) or in vivo (e.g., using animal models) through techniques like CRISPR/Cas9 gene editing or antibody-based inhibition.
Step 6: Therapeutic Target Selection: Validated key drivers within an endotype become candidates for therapeutic intervention with targeted biologics. For example, identification of IL-5 as a hub gene in an eosinophil-dominant module validates the use of anti-IL-5 biologics for that patient subgroup.
Table 3: Essential Research Reagents for Endotype and Biologic Research
| Reagent / Resource | Function and Application in Research |
|---|---|
| RNA-sequencing Kits | Profile the entire transcriptome from patient samples (e.g., blood, tissue) to identify differentially expressed genes and signaling pathways defining an endotype [28]. |
| Flow Cytometry Panels | Characterize and quantify specific immune cell populations (e.g., eosinophils, T-cells, ILC2s) in peripheral blood or bronchoalveolar lavage fluid to link cellular profiles to endotypes [85]. |
| ELISA/Multiplex Assays | Measure concentrations of specific cytokines (e.g., IL-5, IL-13, TSLP), immunoglobulins (IgE), or other soluble biomarkers (e.g., periostin) in serum or supernatant to validate molecular pathways [86]. |
| Monoclonal Antibodies (Therapeutic) | Used both as the clinical intervention and as critical tools in in vitro validation experiments to block specific cytokine pathways and confirm their functional role in an endotype [86] [85]. |
| Network Analysis Software (e.g., WGCNA, Cytoscape) | Computational tools to construct, visualize, and analyze gene co-expression networks and protein-protein interaction networks from omics data, identifying key hub genes and modules [28]. |
The evaluation of biologic efficacy is intrinsically linked to the precise definition of patient endotypes. Systems biology, through the integration of multi-omics data into network models, provides the powerful analytical framework needed to move beyond superficial phenotyping and uncover the root causes of disease. For most patients, this allows for the rational selection of a single, highly effective biologic. However, as the evidence for dual biologic therapy demonstrates, the endotypic approach also provides a logical and structured methodology for managing the most complex, multi-mechanistic cases. Future research must focus on refining these endotypic definitions, validating combination strategies in larger trials, and expanding this precision paradigm to non-type 2 and other complex inflammatory diseases.
Conclusion
The integration of systems biology into disease research marks a pivotal shift towards a mechanistic understanding of human pathology. By moving beyond superficial phenotypes to define actionable endotypes, this approach provides the foundational knowledge required for true precision medicine. The key takeaways underscore that endotypes, characterized by distinct pathobiological mechanisms, enable superior patient stratification, predict therapeutic responses, and guide the development of targeted biologics. Future progress hinges on overcoming challenges related to biomarker validation, dynamic disease modeling, and the integration of multi-omics data into routine clinical practice. The continued application of these strategies promises to transform patient care from a reactive to a proactive, personalized paradigm, ultimately improving outcomes across a spectrum of complex diseases.
References
- 1. Toward precision medicine in COPD: phenotypes, endotypes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12482825/]
- 2. Biomarkers for phenotype-endotype relationship in atopic ... [https://www.sciencedirect.com/science/article/pii/S2352396424001567]
- 3. Understanding Quantitative Genetics in the Systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2631226/]
- 4. Decision tree-based method for integrating gene ... [https://www.rti.org/publication/decision-tree-based-method-integrating-gene-expression-demographic-clinical-data-determine-disease-e]
- 5. Decision tree-based method for integrating gene expression ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4228284/]
- 6. Using both qualitative and quantitative data in parameter ... [https://www.nature.com/articles/s41467-018-06439-z]
- 7. Systematic data analysis pipeline for quantitative ... [https://www.sciencedirect.com/science/article/pii/S2001037024002460]
- 8. Systems immunology integrates the complex endotypes of ... [https://pubmed.ncbi.nlm.nih.gov/39809737/]
- 9. Deconstructing the “types” of osteoarthritis [https://www.sciencedirect.com/science/article/pii/S2772654124000916]
- 10. The MFGE8/integrin β3 axis mitigates experimental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12224391/]
- 11. Comprehensive proteome profiling of molecular endotypes ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1649918/full]
- 12. Insights into Patient Heterogeneity in Sjögren's Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249559/]
- 13. Sepsis endotypes identified by host gene expression ... [https://www.nature.com/articles/s43856-024-00542-7]
- 14. Integrative omics redefining allergy mechanisms and ... [https://www.sciencedirect.com/science/article/pii/S1323893025000917]
- 15. Phenotypes and endotypes in bronchiectasis: a narrative ... [https://jtd.amegroups.org/article/view/99544/html]
- 16. State‐of‐the‐art hypothesis-driven systems pharmacology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11979609/]
- 17. Systems immunology integrates the complex endotypes of ... [https://www.nature.com/articles/s41467-025-55934-7]
- 18. Mathematical Modeling in Systems Biology [https://www.mdpi.com/1099-4300/25/10/1380]
- 19. Computational Cellular Mathematical Model Aids ... [https://bio-protocol.org/en/bpdetail?id=5223&type=0]
- 20. Minimally sufficient experimental design using identifiability ... [https://www.nature.com/articles/s41540-023-00325-1]
- 21. Next Decade Research in Asthma - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12653571/]
- 22. Early-life wheezing trajectories shape asthma endotype [https://www.aaaai.org/tools-for-the-public/latest-research-summaries/the-journal-of-allergy-and-clinical-immunology/2025/wheez]
- 23. Genetic contributions to epigenetic-defined endotypes of ... [https://pubmed.ncbi.nlm.nih.gov/40614707/]
- 24. Connecting electronic health records to a biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11760951/]
- 25. Systems Biology and Multi-Omics Integration - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6523452/]
- 26. Multi-omics strategies for biomarker discovery and application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638490/]
- 27. A conceptual review on systems biology in health and diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC3933630/]
- 28. Computational systems biology in disease modeling and ... [https://www.nature.com/articles/s41540-022-00247-4]
- 29. Integrating Multi-Omics Data: Methods and Applications in ... [https://www.sciencedirect.com/science/article/pii/S2215017X25000657]
- 30. Joint multi-omic/clinical clustering to identify disease ... [https://www.sciencedirect.com/science/article/pii/S2211124721002898]
- 31. GAUDI: interpretable multi-omics integration with UMAP ... [https://www.nature.com/articles/s41467-025-60822-1]
- 32. 2025 Trends: Multiomics [https://www.genengnews.com/topics/omics/2025-trends-multiomics/]
- 33. Visual analysis of multi-omics data [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2024.1395981/full]
- 34. An interactive atlas of genomic, proteomic, and ... [https://www.nature.com/articles/s41598-024-63399-9]
- 35. Single-cell RNA Sequencing in Immunology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7770633/]
- 36. Single-cell analysis reveals immune cell abnormalities ... [https://www.nature.com/articles/s41467-025-60034-7]
- 37. Single-cell profiling identifies heterogeneity of the immune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1690992/full]
- 38. Single-cell sequencing reveals cellular heterogeneity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605242/]
- 39. sc-ImmuCC: hierarchical annotation for immune cell types ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1223471/full]
- 40. Single-cell profiling reveals immune cell diversity and ... [https://www.sciencedirect.com/science/article/pii/S2667325825005096]
- 41. Determining asthma endotypes and outcomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC9798025/]
- 42. Endotyping: The Path to Precision Medicine for Immune- ... [https://www.genedata.com/resources/learn/details/blog/precision-medicine-imid-endotyping]
- 43. Molecular endotypes in sepsis: integration of multicohort ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12123803/]
- 44. The benefits and pitfalls of machine learning for biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10558383/]
- 45. Unsupervised detection of rare events in liquid biopsy assays [https://www.nature.com/articles/s41698-025-01015-3]
- 46. Connecting electronic health records to a biomedical ... [https://www.nature.com/articles/s41598-024-78794-5]
- 47. Multi-omic Approaches for Endotype Discovery in Allergy/ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12513499/]
- 48. The STARD-AI reporting guideline for diagnostic accuracy ... [https://www.nature.com/articles/s41591-025-03953-8]
- 49. Diagnostic Prediction Models for Primary Care, Based on AI ... [https://medinform.jmir.org/2025/1/e62862]
- 50. Principles of Effective Data Visualization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7733875/]
- 51. 16 Guidelines for Effective Data Visualizations in ... - Luís Cruz [https://luiscruz.github.io/2021/03/01/effective-visualizations.html]
- 52. Designing Effective Data Visualizations [https://guides.library.jhu.edu/datavisualization/design]
- 53. Developing a transparent reporting tool for AI-based ... [https://pubmed.ncbi.nlm.nih.gov/40453809/]
- 54. Challenges and opportunities in the network medicine of ... [https://www.sciencedirect.com/science/article/pii/S2666634025003472]
- 55. Understanding diseases by mouse click: the promise and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2219318/]
- 56. From endotypes to therapeutic targets [https://pubmed.ncbi.nlm.nih.gov/41108351/]
- 57. Bridging the Gap: Translating Preclinical Biomarkers to ... [https://blog.crownbio.com/bridging-the-gap-translating-preclinical-biomarkers-to-clinical-success]
- 58. Use of Biomarkers in Drug Development for Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12489174/]
- 59. The 2025 FDA Biomarker Guidance: Understanding ... [https://www.linkedin.com/pulse/2025-fda-biomarker-guidance-understanding-lxoke]
- 60. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 61. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 62. Evidence-based standardized sample handling protocol for ... [https://pubmed.ncbi.nlm.nih.gov/41025225/]
- 63. Insights from Biomarkers & Precision Medicine 2025 [https://www.signifyresearch.net/insights/biomarkers-billions-and-breakthroughs-insights-from-biomarkers-precision-medicine-2025/]
- 64. Precision medicine and phenotypes, endotypes, genotypes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6436902/]
- 65. Chaotic driven gorilla troops optimizer based NMF approach for... [https://link.springer.com/article/10.1007/s41870-022-00928-7]
- 66. A systems biology approach to better understand human ... [https://www.sciencedirect.com/science/article/abs/pii/S1471492222002598]
- 67. Chapter 5 High dimensional visualizations | Data Analysis and ... [https://gagneurlab.github.io/dataviz/high-dimensional-visualizations.html]
- 68. from Data : Methods, Best Practices... Integration Multiple Sources [https://www.domo.com/learn/article/integrate-data-from-multiple-sources]
- 69. How to work with multiple data sources in ... [https://grafana.com/blog/2024/11/07/how-to-work-with-multiple-data-sources-in-grafana-dashboards-best-practices-to-get-started/]
- 70. 7 Multi-Source Data Visualization Strategies That Reveal ... [https://www.maplibrary.org/11092/7-multi-source-data-visualization-strategies/]
- 71. Biological Robustness: Paradigms, Mechanisms, and Systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3350086/]
- 72. Robustness of the Model [https://bio-protocol.org/exchange/minidetail?id=5843704&type=30]
- 73. Systems biology platform for efficient development and ... [https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2023.1229532/full]
- 74. 332. Examples of scientific data visualization with ... [https://medium.com/@ilakk2023/examples-of-scientific-data-visualization-with-quantitative-components-77ec53b7ce43]
- 75. 7 Types of Comparison Charts for Effective Data Visualization [https://ninjatables.com/types-of-comparison-charts/?srsltid=AfmBOorPRvzGf94yHjx-Rtd3l6p8_2VnPl6wN7EPTSrsCG54uPFipxAR]
- 76. Color and contrast [https://web.dev/learn/accessibility/color-contrast]
- 77. Research Priorities for Translating Endophenotyping of Adult ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12432412/]
- 78. Resolving Clinical Phenotypes into Endotypes in Allergy [https://pmc.ncbi.nlm.nih.gov/articles/PMC8209667/]
- 79. Decision tree-based method for integrating gene expression ... [https://bmcsystbiol.biomedcentral.com/articles/10.1186/1752-0509-7-119]
- 80. Protocol design for clinical trials - the complete checklist [https://clinicaltrialrisk.org/clinical-trial-design/protocol-design-for-clinical-trials-the-complete-checklist/]
- 81. Clinical Significance of Endotypes of Asian Chronic ... [https://www.mdpi.com/2673-351X/9/2/19]
- 82. Goals for systems biology in infectious disease [https://www.sciencedirect.com/science/article/pii/S2452310017300781]
- 83. Few shot learning for phenotype-driven diagnosis of ... [https://www.nature.com/articles/s41746-025-01749-1]
- 84. Endotyping-informed therapy for patients with chest pain ... [https://www.nature.com/articles/s41591-025-04044-4]
- 85. Novel Biological Therapies for Severe Asthma Endotypes [https://www.mdpi.com/2227-9059/10/5/1064]
- 86. Combining dual biologics therapy for severe asthma: a series of ten ca | JAA [https://www.dovepress.com/combining-dual-biologics-therapy-for-severe-asthma-a-series-of-ten-cas-peer-reviewed-fulltext-article-JAA]