Decoding Autism: Biochemical Pathways, Genetic Subtypes, and Precision Medicine Approaches
This article synthesizes the latest breakthroughs in understanding the biochemical and genetic architecture of Autism Spectrum Disorder (ASD).
Decoding Autism: Biochemical Pathways, Genetic Subtypes, and Precision Medicine Approaches
Abstract
This article synthesizes the latest breakthroughs in understanding the biochemical and genetic architecture of Autism Spectrum Disorder (ASD). We explore the paradigm shift from a unitary condition to one of distinct biologically defined subtypes, each with unique genetic programs, developmental trajectories, and pathophysiological mechanisms. For a research and drug development audience, the review details advanced computational methodologies for subtype stratification, analyzes challenges in therapeutic development—including drug metabolism considerations and target identification—and evaluates emerging preclinical and clinical validation strategies. The integration of multi-omics data, exposomics, and a precision medicine framework is highlighted as the future of ASD research and treatment.
The New Biology of Autism: From a Single Spectrum to Distinct Biochemical Subtypes
Autism spectrum disorder (ASD) represents one of the most complex challenges in modern neuropsychiatry, characterized by astounding phenotypic and genetic heterogeneity that has long confounded research efforts to establish coherent biological models. The prevailing clinical adage, "If you've met one person with autism, you've met one person with autism," underscores the extraordinary diversity of experiences falling under the ASD diagnosis [1]. While the spectrum concept usefully captures this variability, it simultaneously obscures crucial differences that may hold the key to understanding etiology and developing targeted interventions. As noted by Fred Volkmar, a psychiatrist and professor emeritus at Yale University, "The beauty of the autism spectrum is: it speaks to this heterogeneity. And the downside [is that] it covers up the differences" [1].
The current diagnostic framework categorizes individuals based on severity levels of two core criteria: social communication difficulties and restricted, repetitive behaviors. However, these coarse groupings fail to capture the nuanced clinical presentations and varied developmental trajectories observed across the spectrum [1]. For decades, researchers have attempted to delineate meaningful subtypes that connect observable traits to underlying biological mechanisms, with limited success until recently. The critical barrier has been bridging the gap between the hundreds of genes associated with autism and their translation into specific autistic traits and developmental outcomes [1].
A transformative study published in Nature Genetics in July 2025 has successfully addressed this challenge through an innovative computational approach that integrates broad phenotypic data with genetic information from a large cohort of autistic individuals [2]. This research has identified four biologically distinct subtypes of autism, each defined by unique patterns of clinical presentation, developmental trajectory, and genetic architecture. These findings mark a paradigm shift from viewing autism as a single diagnostic entity toward understanding it as a collection of distinct disorders with shared core features but different underlying biological narratives [3].
Experimental Framework and Methodological Innovation
Cohort Characteristics and Data Collection
The research leveraged data from the SPARK (Simons Foundation Powering Autism Research) cohort, the largest autism research study in the United States, which has enrolled over 150,000 autistic individuals and 200,000 family members since its inception [4]. The analysis focused on 5,392 autistic children aged 4-18 years, for whom both comprehensive phenotypic data and genetic information were available [2]. This sample size provided sufficient statistical power to detect robust patterns amid the inherent heterogeneity of autism.
The phenotypic data encompassed 239 meticulously defined item-level and composite features drawn from standardized diagnostic instruments and developmental assessments [2]. These included:
- Social Communication Questionnaire-Lifetime (SCQ): Assessing core social communication deficits characteristic of autism
- Repetitive Behavior Scale-Revised (RBS-R): Measuring restricted and repetitive behaviors
- Child Behavior Checklist 6-18 (CBCL): Evaluating emotional, behavioral, and social problems
- Developmental history forms: Documenting milestone achievement and medical history
Genetic data comprised whole-exome or genome sequencing, enabling analysis of both common and rare variants across the coding regions of the genome [2].
Computational Approach: Person-Centered Mixture Modeling
The research team employed a generative finite mixture model (GFMM), a sophisticated computational approach that fundamentally differed from previous trait-centric analyses [2]. This methodology represented a critical innovation in several respects:
Table 1: Key Features of the Generative Finite Mixture Model
| Feature | Description | Advantage over Traditional Methods |
|---|---|---|
| Data Type Handling | Simultaneously accommodated continuous, binary, and categorical data types | Eliminated need for data simplification that loses information |
| Person-Centered Approach | Maintained individual phenotypic profiles intact during analysis | Preserved natural co-occurrence patterns of traits within individuals |
| Probabilistic Classification | Assigned individuals to classes based on probability distributions | Acknowledged potential membership across multiple classes |
| Model Selection | Evaluated 2-10 latent classes using Bayesian information criterion and clinical interpretability | Balanced statistical rigor with clinical relevance |
The person-centered approach proved particularly significant, as it modeled the complex interplay of traits within individuals rather than analyzing isolated traits across populations [4]. As explained by Natalie Sauerwald, a co-lead author of the study, "Our goal with the person-centered approach is to maintain representation of the whole individual so that we can more fully model their complex spectrum of traits together" [4]. This methodology effectively captured the developmental reality that traits influence each other in complex ways, compensating for or exacerbating individual phenotypic measures throughout development [2].
The model's robustness was rigorously tested through multiple validation approaches, including stability analysis under perturbation and replication in an independent cohort (the Simons Simplex Collection), demonstrating consistent class structure across different populations [2].
The Four Autism Subtypes: Clinical and Genetic Profiles
The analysis revealed four distinct subtypes of autism, each demonstrating unique constellations of clinical features, developmental trajectories, and genetic architectures. These subtypes were not merely differentiated by severity but represented qualitatively different presentations with specific biological underpinnings.
Social and Behavioral Challenges Subtype
This group represented the largest subtype, comprising 37% of the study population [1] [3]. Clinically, these individuals exhibited significant difficulties with social communication and restrictive, repetitive behaviors, alongside elevated rates of co-occurring conditions including ADHD, anxiety disorders, depression, and obsessive-compulsive disorder [1] [5]. Despite these challenges, children in this subgroup did not experience significant developmental delays, reaching milestones at ages comparable to non-autistic peers [1].
Genetically, this subtype showed a distinct profile characterized by:
- Enrichment of common genetic variants associated with psychiatric conditions such as ADHD and depression [5]
- Predominance of mutations in genes that become active after birth, particularly during childhood [3]
- Impact on genes expressed in brain cells involved in social and emotional processing [5]
- Lower burden of rare, damaging de novo mutations compared to other subtypes [3]
The postnatally active genetic signature aligns with the clinical presentation of typical early development followed by emerging behavioral and social challenges, and corresponds with later ages at diagnosis [3].
Mixed ASD with Developmental Delay Subtype
This heterogeneous subgroup accounted for 19% of the study population [1] [3]. Their clinical presentation was characterized by developmental delays in motor, language, and cognitive domains, alongside core autism symptoms [6]. Notably, these children showed significantly lower rates of anxiety, depression, and disruptive behaviors compared to other subtypes [3]. The "mixed" designation reflects the variable expression of repetitive behaviors and social challenges within this group [3].
Genetic features distinctive to this subtype included:
- Combination of both de novo and rare inherited variants [3] [5]
- Mutations predominantly affecting genes active during prenatal brain development [3]
- Strong association with language delays, intellectual disability, and motor disorders [3]
- Earlier age at diagnosis consistent with observable developmental concerns [3]
The genetic profile suggests a more complex inheritance pattern compared to other subtypes, with contributions from both spontaneously arising and familial genetic variants [5].
Moderate Challenges Subtype
Representing 34% of the cohort, this group exhibited milder manifestations across all core autism domains [1] [3]. While these individuals demonstrated more difficulties than non-autistic peers, their challenges were less pronounced than other autistic children [1]. They typically achieved developmental milestones on schedule and showed low rates of co-occurring psychiatric conditions [3] [6].
Genetic characteristics included:
- Lower burden of damaging genetic variants overall [3]
- Rare variants in genes less critical for fundamental neurological functioning [7]
- Gene expression patterns primarily active during fetal and neonatal development [7]
- Minimal association with known psychiatric genetic risk factors [5]
This subtype appears to represent a form of autism with less biological disruption, manifesting in milder clinical presentation.
Broadly Affected Subtype
The most severely impacted subgroup comprised 10% of the study population [1] [3]. These individuals presented with widespread challenges including significant developmental delays, severe social communication deficits, pronounced repetitive behaviors, and high rates of co-occurring psychiatric conditions [3] [6]. Medical and cognitive comorbidities included intellectual disability, language impairment, and mood dysregulation [3] [5].
The genetic signature of this subtype was marked by:
- Highest burden of damaging de novo mutations not inherited from parents [3] [5]
- Enrichment for mutations in genes crucial for early brain development [5]
- Association with genes linked to fragile X syndrome and other intellectual disability disorders [8]
- Genetic disruptions affecting both prenatal and postnatal developmental periods [7]
This profile aligns with the profound and multifaceted clinical challenges observed in this subgroup.
Table 2: Comprehensive Profile of the Four Autism Subtypes
| Characteristic | Social/Behavioral (37%) | Mixed ASD with DD (19%) | Moderate (34%) | Broadly Affected (10%) |
|---|---|---|---|---|
| Core Social Challenges | Severe | Variable | Mild | Severe |
| Repetitive Behaviors | Severe | Variable | Mild | Severe |
| Developmental Milestones | Typical | Delayed | Typical | Delayed |
| Co-occurring ADHD/Anxiety | High | Low | Low | High |
| Intellectual Disability | Rare | Common | Rare | Common |
| Age at Diagnosis | Later | Earlier | Variable | Earliest |
| Genetic Signature | Common psychiatric variants | Rare inherited + de novo | Milder variants | High-impact de novo mutations |
| Key Biological Pathways | Postnatal synaptic signaling | Prenatal neurodevelopment | Diverse, mild impact | Proliferation, differentiation |
| Developmental Timing | Postnatal | Prenatal | Prenatal | Prenatal + Postnatal |
Distinct Genetic Architectures and Biological Pathways
The four autism subtypes demonstrated remarkable biological divergence, with minimal overlap in the specific molecular pathways affected in each subgroup [4]. As senior author Olga Troyanskaya noted, "To me, the biggest surprise was how different the four subtypes turned out to be... The underlying genetics and biology are very different" [1].
Subtype-Specific Genetic Risk Profiles
Comprehensive genetic analysis revealed distinct patterns of common and rare genetic variation across the subtypes:
Common Variant Contributions: The Social/Behavioral Challenges subtype showed the strongest influence of common genetic variants associated with psychiatric conditions like ADHD and depression, suggesting a shared genetic architecture with these disorders [5]. Notably, none of the subtypes demonstrated strong associations with common variants specifically linked to autism core features, highlighting the complexity of autism's genetic architecture [5].
Rare Variant Patterns: The Broadly Affected subtype carried the highest burden of rare, high-impact de novo mutations, particularly in genes critical for early brain development [5]. These mutations often occurred in genes previously associated with intellectual disability and severe developmental disorders [5]. The Mixed ASD with Developmental Delay subtype showed a combination of both de novo and rare inherited variants, indicating more complex inheritance patterns [3].
Temporal Expression Patterns: Critical differences emerged in the developmental timing of gene expression affected by subtype-specific mutations. In the Social/Behavioral subtype, mutated genes were predominantly active after birth, aligning with their clinical presentation of typical early development followed by emerging challenges [3]. Conversely, in subtypes with developmental delays (Mixed ASD with DD and Broadly Affected), mutations affected genes predominantly active during prenatal brain development [3].
Divergent Biological Pathways and Mechanisms
Pathway analysis revealed distinct biological narratives for each subtype, with minimal overlap between the molecular pathways affected:
Social/Behavioral Challenges Subtype: Showed enrichment for pathways involved in neuronal signaling, synaptic plasticity, and neurotransmitter regulation, particularly in systems mature during childhood and adolescence [4] [5].
Mixed ASD with Developmental Delay Subtype: Demonstrated disruption in fundamental neurodevelopmental processes including neuronal migration, axon guidance, and cortical organization [4].
Broadly Affected Subtype: Exhibited the most widespread pathway disruptions, affecting basic cellular processes including proliferation, differentiation, chromatin organization, and DNA repair mechanisms [3] [9].
The biological distinctions were so pronounced that Sauerwald analogized the challenge to "trying to put together a puzzle, but actually, you have four different puzzles mixed together, and you can't find any common pieces" [8]. This fundamental insight explains why previous studies seeking unified biological explanations for autism consistently encountered limited success.
Research Implications and Experimental Toolkit
This groundbreaking research was enabled by sophisticated methodological approaches and specialized resources that provide a toolkit for future investigations into autism heterogeneity:
Table 3: Essential Research Resources for Autism Subtype Investigations
| Resource/Technology | Specifications | Research Application |
|---|---|---|
| SPARK Cohort Database | >150,000 autistic participants; genomic + deep phenotypic data [4] | Large-scale discovery cohort for subtype identification and validation |
| Generative Finite Mixture Models | Multimodal integration of continuous, categorical, and binary data [2] | Person-centered classification accommodating real-world data complexity |
| Simons Simplex Collection | Deeply phenotyped independent cohort with genomic data [2] | Replication cohort for validating subtype generalizability |
| Whole Exome/Genome Sequencing | Comprehensive variant detection across coding regions [2] | Identification of rare inherited and de novo mutations |
| Polygenic Risk Scoring | Aggregate common variant contributions to psychiatric traits [5] | Quantifying shared genetic architecture with related conditions |
| Developmental Gene Expression Atlas | Brain transcriptome data across developmental timeline [3] | Mapping mutational impact to specific developmental periods |
| Pathway Enrichment Analysis | MSigDB Hallmark pathways and custom gene sets [9] | Identifying biological processes disrupted in each subtype |
Methodological Framework for Subtype Validation
The study established a rigorous methodological framework for identifying and validating biologically meaningful subtypes in heterogeneous neurodevelopmental conditions:
Data Integration Protocol: Standardized collection of 239 phenotypic features across diagnostic, behavioral, developmental, and medical domains, matched with genomic data [2].
Model Selection Criteria: Simultaneous optimization of statistical fit indices (Bayesian information criterion, validation log likelihood) and clinical interpretability when determining the optimal number of subtypes [2].
Biological Validation: Integration of genetic data only after phenotypic class establishment, ensuring unbiased confirmation of biological distinctness [2].
Cross-Cohort Replication: Application of classification models to independent cohorts (Simons Simplex Collection) to demonstrate generalizability beyond the discovery sample [2].
This framework provides a template for deconstructing heterogeneity in other complex neuropsychiatric conditions.
Discussion and Future Research Directions
The identification of four biologically distinct autism subtypes represents a paradigm shift in autism research with far-reaching implications for both basic science and clinical practice. Rather than searching for a unified biological explanation for autism, researchers can now investigate the distinct genetic and biological processes driving each subtype [3]. As noted by Chandra Theesfeld, co-author of the study, "This opens the door to countless new scientific and clinical discoveries" [3].
Research Implications
This refined understanding of autism heterogeneity enables more precisely targeted research approaches:
Gene Discovery: Focused analysis within subtypes increases power to identify subtle genetic effects that may be obscured in heterogeneous samples [4].
Pathway Validation: Subtype-specific biological pathways generate testable hypotheses regarding disease mechanisms and potential therapeutic targets [4].
Developmental Modeling: The temporal alignment between gene expression patterns and clinical features enables more accurate modeling of developmental trajectories [3].
Preclinical Models: Development of animal and cellular models can now be guided by subtype-specific genetic and biological profiles, increasing translational relevance [9].
Clinical Applications and Precision Medicine
The subtyping framework holds significant promise for advancing precision medicine approaches in autism:
Diagnostic Refinement: Incorporating biological subtyping could complement behavioral diagnosis, providing more prognostically meaningful categorizations [1] [5].
Early Identification: Understanding subtype-specific developmental timelines could guide age-appropriate screening and monitoring protocols [3].
Treatment Targeting: Subtype-specific biological pathways offer targets for developing tailored interventions rather than one-size-fits-all approaches [10].
Prognostic Forecasting: Different subtypes demonstrate distinct developmental trajectories and outcomes, enabling more accurate long-term planning [3].
Limitations and Future Directions
While transformative, these findings represent a starting point rather than a complete nosology of autism. Important limitations and future directions include:
Ancestral Diversity: The current findings are based primarily on individuals of European ancestry, necessitating validation in more diverse populations [8]. Research suggests that certain genetic variations may occur at different frequencies across ancestries [8].
Subtype Expansion: As noted by the researchers, "This doesn't mean that there are only four classes" [4]. Larger samples and additional data modalities will likely reveal further subdivisions.
Longitudinal Dynamics: The current study provides a cross-sectional view; longitudinal tracking is needed to understand how subtypes evolve across the lifespan.
Non-Coding Variation: Future work incorporating the 98% of the genome that does not code for proteins may reveal additional regulatory mechanisms [4].
Neurobiological Validation: Integration of neuroimaging, electrophysiological, and postmortem data will strengthen the biological grounding of these subtypes.
This research fundamentally reorients our approach to autism heterogeneity, providing a robust framework for understanding its biological diversity and advancing toward personalized approaches to care and treatment. As concluded by the researchers, "The ability to define biologically meaningful autism subtypes is foundational to realizing the vision of precision medicine for neurodevelopmental conditions" [3].
Autism spectrum disorder (ASD) represents a complex neurodevelopmental condition characterized by significant heterogeneity in its clinical presentation and underlying genetic architecture. Historically, the search for a unified biological explanation has been challenging due to the diverse phenotypic manifestations and multifactorial etiology. The condition's core features encompass persistent deficits in social communication and interaction alongside restricted, repetitive patterns of behavior, interests, or activities [11]. For decades, researchers have sought to parse this heterogeneity by linking the varying observable traits, or phenotypes, to specific genetic underpinnings [4].
The emerging paradigm in autism research recognizes that what is clinically diagnosed as autism likely comprises multiple biologically distinct conditions, each with unique developmental trajectories and genetic profiles. The integration of large-scale genomic data with deep phenotypic information has enabled a more nuanced understanding of these subtypes. This whitepaper synthesizes recent advances in deconstructing the genetic architecture of autism subtypes, focusing specifically on the distinct roles of de novo versus inherited variants and their interplay with polygenic risk profiles. Furthermore, it frames these findings within the context of biochemical pathways implicated in autism pathogenesis, providing a mechanistic foundation for targeted therapeutic development.
Subtype Classification: Phenotypic and Genetic Heterogeneity
Data-Driven Subtype Identification
Recent large-scale studies have employed person-centered computational approaches to identify robust autism subtypes based on comprehensive phenotypic data. One seminal analysis of the SPARK cohort (n=5,392) utilized a general finite mixture model (GFMM) to analyze 239 phenotypic features, identifying four clinically and biologically distinct subtypes [3] [2]. This person-centered approach maintains the representation of the whole individual, modeling the complex spectrum of traits together rather than fragmenting individuals into separate phenotypic categories [2].
Table 1: Clinically Distinct Subtypes of Autism
| Subtype | Prevalence | Core Phenotypic Features | Developmental Milestones | Common Co-occurring Conditions |
|---|---|---|---|---|
| Social and Behavioral Challenges | ~37% | Prominent social challenges, repetitive behaviors, communication difficulties | Typically reached at pace similar to children without autism | ADHD, anxiety disorders, depression, OCD, mood dysregulation |
| Mixed ASD with Developmental Delay | ~19% | Mixed social/repetitive behavior profiles, strong enrichment of developmental delays | Reached later than peers without autism | Language delay, intellectual disability, motor disorders |
| Moderate Challenges | ~34% | Core autism behaviors present but less pronounced | Typically reached at pace similar to children without autism | Generally absence of co-occurring psychiatric conditions |
| Broadly Affected | ~10% | Widespread challenges across all measured domains | Significant developmental delays | Anxiety, depression, mood dysregulation, multiple co-occurring conditions |
The four-class model demonstrated optimal balance across multiple statistical fit measures, including Bayesian information criterion (BIC) and validation log likelihood, while offering strong clinical interpretability [2]. This classification system has been successfully replicated in the independent Simons Simplex Collection (SSC) cohort, confirming the robustness of these subtypes across different populations [2].
Developmental Trajectories and Age at Diagnosis
Longitudinal analyses across multiple birth cohorts have revealed distinct developmental trajectories associated with age at autism diagnosis. Growth mixture modeling of socioemotional and behavioral development using the Strengths and Difficulties Questionnaire (SDQ) has identified two primary latent trajectories [12]:
- Early Childhood Emergent Trajectory: Characterized by difficulties in early childhood that remain stable or modestly attenuate in adolescence.
- Late Childhood Emergent Trajectory: Characterized by fewer difficulties in early childhood that increase in late childhood and adolescence.
Autistic individuals in the early childhood emergent trajectory are more likely to receive diagnosis in childhood, while those in the late childhood emergent trajectory tend toward later diagnosis [12]. These trajectory differences explain a substantial portion (11.7%-30.3%) of the variance in age of autism diagnosis, surpassing the explanatory power of sociodemographic variables (4.8%-5.5%) [12].
Genetic Architecture of Autism Subtypes
Distinct Variant Profiles Across Subtypes
The identified autism subtypes demonstrate divergent genetic architectures, with varying contributions of de novo and inherited variation across subgroups.
Table 2: Genetic Profiles Across Autism Subtypes
| Subtype | De Novo Mutations | Inherited Variants | Polygenic Architecture | Key Biological Pathways |
|---|---|---|---|---|
| Social and Behavioral Challenges | Lower proportion | Moderate burden | Later-onset genetic factor (rg=0.38) correlated with ADHD/mental health conditions | Genes active after birth; neuronal function |
| Mixed ASD with Developmental Delay | Moderate proportion | Highest burden of rare inherited protein-truncating variants | Earlier-onset genetic factor | Prenatally active genes; chromatin organization |
| Moderate Challenges | Not specifically reported | Not specifically reported | Not specifically reported | Not specifically reported |
| Broadly Affected | Highest proportion | Moderate burden | Not specifically reported | Multiple pathways; widespread disruption |
The Social and Behavioral Challenges subtype shows a distinct genetic signature characterized by mutations in genes that become active after birth, aligning with their typical developmental milestones and later average age of diagnosis [3]. Conversely, the Mixed ASD with Developmental Delay subtype demonstrates enrichment for rare inherited variants affecting genes predominantly active prenatally [3].
In multiplex families (families with multiple autistic individuals), autistic children show an increased burden of rare inherited protein-truncating variants in known ASD risk genes [13]. Furthermore, ASD polygenic score (PGS) is overtransmitted from nonautistic parents to autistic children who also harbor rare inherited variants, suggesting combinatorial effects that may explain the reduced penetrance of these rare variants in parents [13].
Polygenic Risk Stratification
Common genetic variants account for approximately 11% of the variance in age at autism diagnosis, similar to the contribution of individual sociodemographic and clinical factors [12]. The polygenic architecture of autism can be decomposed into two modestly genetically correlated (rg = 0.38, s.e. = 0.07) polygenic factors [12]:
- Factor 1: Associated with earlier autism diagnosis, lower social and communication abilities in early childhood, and moderate genetic correlations with ADHD and mental health conditions.
- Factor 2: Associated with later autism diagnosis, increased socioemotional and behavioral difficulties in adolescence, and moderate to high positive genetic correlations with ADHD and mental-health conditions.
These findings support a developmental model wherein earlier- and later-diagnosed autism have different underlying developmental trajectories and polygenic architectures, rather than a unitary model where the same genetic factors operate across the spectrum [12].
Experimental Methodologies
Cohort Recruitment and Phenotyping
SPARK Cohort Protocol: The SPARK study represents the largest autism cohort to date, engaging over 150,000 autistic individuals and 200,000 family members [4]. Recruitment employs nationwide outreach with online registration and consent procedures. Phenotypic assessment includes:
- Diagnostic Questionnaires: Social Communication Questionnaire-Lifetime (SCQ), Repetitive Behavior Scale-Revised (RBS-R), Child Behavior Checklist 6-18 (CBCL) [2].
- Developmental History: Comprehensive background history form focusing on developmental milestones [2].
- Medical and Psychiatric Comorbidity Assessment: Structured reporting of diagnosed co-occurring conditions including ADHD, anxiety, depression, and language delays [2].
Simons Simplex Collection (SSC) Protocol: The SSC comprises approximately 2,600 simplex families (families with one autistic child and unaffected parents and siblings) [2]. Phenotypic characterization includes:
- Autism Diagnostic Observation Schedule (ADOS): Administered by research-reliable clinicians.
- Cognitive and Adaptive Behavior Assessments: Full-scale IQ, verbal and non-verbal IQ, Vineland Adaptive Behavior Scales.
- Medical and Genetic History: Detailed medical history and physical examination [2].
Genomic Sequencing and Analysis
Whole-Genome Sequencing (WGS) Protocol:
- DNA Extraction: High-molecular-weight DNA extracted from saliva or blood samples using standardized kits [13] [11].
- Library Preparation: Illumina TruSeq DNA PCR-Free Library Prep Kit for 350 bp insert sizes [13].
- Sequencing: Illumina HiSeq X platform at 30x mean coverage [13].
- Variant Calling: GATK Best Practices pipeline for SNP and indel calling; rare variant filtering (<0.1% frequency in gnomAD) [13].
De Novo Mutation Detection:
- Trio-Based Analysis: Sequencing of autistic child and both biological parents [13] [2].
- Denovo Filtering: DenovoGear and custom scripts requiring variants to be absent in both parents, present in child, and satisfying depth and quality thresholds [13].
- Validation: Sanger sequencing or deep resequencing of putative de novo variants [13].
Inherited Variant Analysis:
- Rare Inherited Variant Identification: Segregation analysis in multiplex families; protein-truncating variants (PTVs) prioritized [13].
- Burden Testing: Comparison of variant burden in cases versus controls using optimized sequence kernel association test (SKAT-O) [13].
- Gene-Based Association: Combined analysis with external datasets using meta-analysis approaches [13].
Statistical Modeling and Classification
General Finite Mixture Model (GFMM):
- Model Framework: Generative mixture model accommodating heterogeneous data types (continuous, binary, categorical) without assuming normal distributions [2].
- Feature Selection: 239 item-level and composite phenotype features representing responses on standard diagnostic questionnaires [2].
- Class Determination: Model selection based on Bayesian information criterion (BIC), validation log likelihood, and clinical interpretability for 2-10 latent classes [2].
- Validation: Internal stability testing via bootstrap resampling and external replication in independent cohort [2].
Growth Mixture Modeling for Developmental Trajectories:
- Data Source: Longitudinal Strengths and Difficulties Questionnaire (SDQ) scores from birth cohorts (Millennium Cohort Study, Longitudinal Study of Australian Children) [12].
- Model Fitting: Maximum likelihood estimation with full-information maximum likelihood to handle missing data [12].
- Class Assignment: Posterior probabilities for trajectory class membership; association with age at diagnosis via chi-square tests [12].
Pathway Visualization and Biochemical Mechanisms
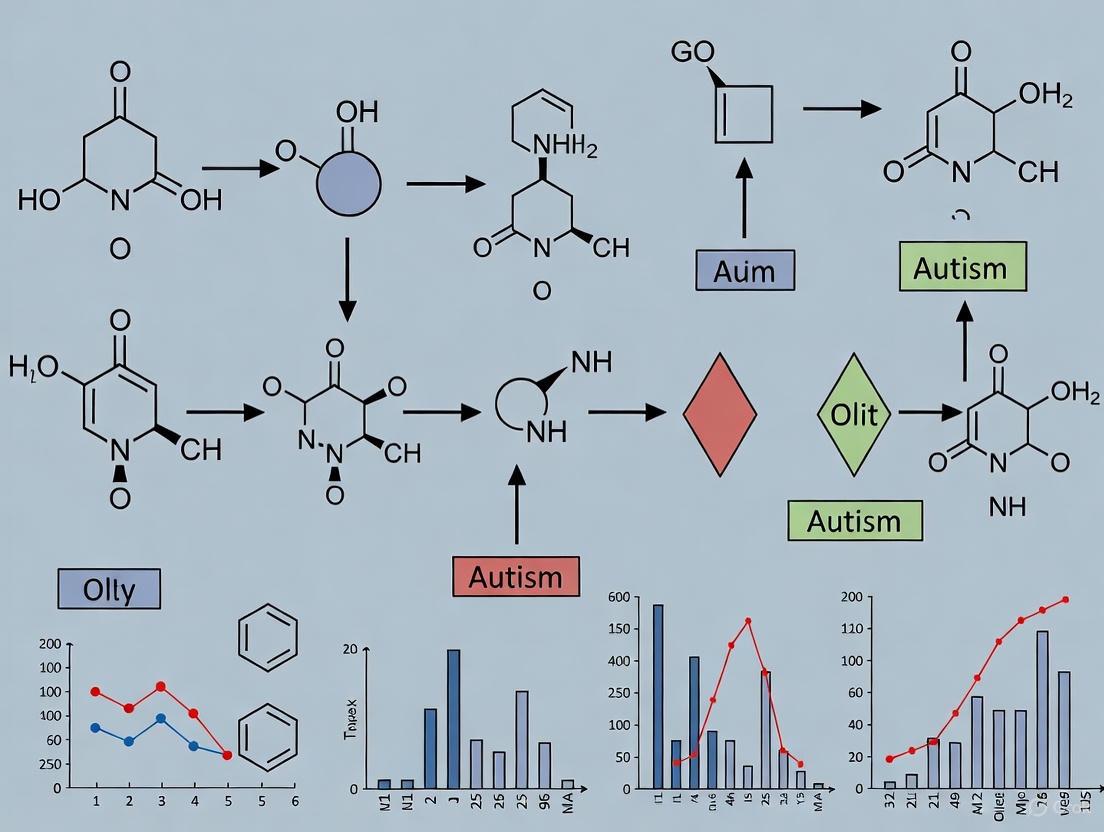
Genetic Subtype Pathway Diagram
Experimental Workflow for Genetic Subtyping
Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms
| Reagent/Platform | Specific Product/Assay | Application in Autism Genetics Research |
|---|---|---|
| DNA Collection | Oragene DNA Self-Collection Kit | Non-invasive saliva collection for large-scale cohort genomic DNA extraction |
| Sequencing Library Prep | Illumina TruSeq DNA PCR-Free Library Prep Kit | Preparation of WGS libraries with minimal bias for variant detection |
| Whole Genome Sequencing | Illumina HiSeq X Ten System | High-throughput sequencing at 30x coverage for comprehensive variant discovery |
| Variant Calling | GATK Best Practices Pipeline | Identification of SNVs, indels, and structural variants from WGS data |
| De Novo Detection | DenovoGear Software Package | Statistical framework for identifying de novo mutations from trio sequencing data |
| Phenotypic Assessment | Social Communication Questionnaire (SCQ) | Standardized measure of autism symptoms and social communication deficits |
| Behavioral Phenotyping | Repetitive Behavior Scale-Revised (RBS-R) | Quantification of restricted, repetitive patterns of behavior, interests, or activities |
| Psychiatric Comorbidity | Child Behavior Checklist (CBCL) | Assessment of emotional, behavioral, and social problems across developmental periods |
| Statistical Modeling | R mclust Package | Implementation of general finite mixture models for subtype identification |
| Pathway Analysis | Enrichr Web Tool | Functional enrichment analysis of gene sets against multiple biological databases |
The decomposition of autism heterogeneity into biologically meaningful subtypes represents a transformative advance in neurodevelopmental disorder research. The distinct genetic architectures underlying these subtypes—varying in their balance of de novo versus inherited variants and their polygenic risk profiles—provide a new framework for understanding autism pathogenesis. Critically, the identification of subtype-specific biochemical pathways and developmental timelines enables a precision medicine approach to autism research and therapeutic development.
Future directions should focus on expanding diverse cohort representation, integrating non-coding genomic variation, and developing subtype-specific cellular models for functional validation. The continued convergence of deep phenotyping, advanced genomics, and computational biology promises to accelerate the translation of these genetic findings into targeted interventions that address the specific biological mechanisms underlying each autism subtype.
Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition characterized by persistent deficits in social communication and interaction, along with restricted, repetitive patterns of behavior, interests, or activities [14]. The pathological framework of ASD is increasingly understood through the lens of specific biochemical pathway disruptions that converge during critical neurodevelopmental windows. Current research reveals that heterogeneous genetic risk factors funnel into convergent biological pathways, primarily affecting neuronal signaling, chromatin remodeling, and cellular metabolism [15] [16]. This whitepaper synthesizes recent advances in understanding these core pathway disruptions, providing a technical resource for researchers and therapeutic developers. We examine the specific mechanisms within each pathway category, present quantitative multi-omics findings, detail experimental methodologies for pathway analysis, and discuss the implications for targeted therapeutic interventions.
Neuronal Signaling Pathway Disruptions
Core Signaling Systems Implicated in ASD
The intricate balance of neuronal communication is frequently disrupted in ASD, with particular impact on synaptic organization, excitatory-inhibitory balance, and neuromodulatory systems. Large-scale genomic studies have identified enrichment of risk genes in two primary functional categories: neuronal communication (NC) and gene expression regulation (GER) [15].
Synaptic Gene Networks: Early genomic investigations identified recurrent de novo copy number variants (CNVs) affecting pivotal synaptic scaffolding and adhesion molecules, including NRXN1, NLGN3, NLGN4X, SHANK2, SHANK3, and SYNGAP1 [15]. These genes encode proteins critical for organizing the postsynaptic density and maintaining proper synaptic adhesion. SHANK3 in particular functions as a master scaffolding protein at excitatory synapses, anchoring glutamate receptors and associated signaling complexes. Haploinsufficiency of SHANK3 disrupts this molecular architecture, leading to aberrant synaptic transmission and plasticity, which manifests as core ASD phenotypes in model systems [15].
Excitatory/Inhibitory Imbalance: A fundamental pathophysiological hypothesis in ASD suggests altered balance between excitatory (glutamatergic) and inhibitory (GABAergic) signaling. This imbalance stems from disruptions in genes controlling the development, maintenance, and function of these systems [17]. The proper maturation of GABAergic circuits is especially vulnerable, potentially leading to network hyperexcitability.
Purinergic Signaling: Emerging evidence positions purinergic signaling as a central regulator of ASD-associated network dysfunction. Extracellular adenosine triphosphate (eATP) functions as a potent signaling molecule that binds purinergic receptors on virtually every cell type, initiating a cascade known as the Cell Danger Response (CDR) [18]. Chronic disruption of this system has far-reaching consequences:
- Metabolic Dysregulation: eATP release triggers mitochondrial reprogramming, increasing oxidative stress and altering energy metabolism [18].
- Immune Activation: eATP is a powerful activator of microglia and innate immune responses, contributing to neuroinflammation [18].
- Synaptic Plasticity: Purinergic receptors directly modulate synaptic strength and plasticity mechanisms [18].
Developmental studies reveal that the purine metabolic network shows profoundly altered regulation in ASD. Hub analysis of the purine network shows a characteristic 17-fold reversal during typical development that fails to occur in ASD, indicating a fundamental disruption in purinergic signaling maturation [18].
Table 1: Key Neuronal Signaling Genes and Their Functional Roles in ASD
| Gene | Protein Function | Biological Process | Impact of Mutation |
|---|---|---|---|
| SHANK3 | Postsynaptic scaffold protein | Synaptic organization & glutamate receptor anchoring | Haploinsufficiency disrupts excitatory synaptic transmission and plasticity [15] |
| NRXN1 | Presynaptic cell adhesion | Synapse formation & maintenance | Disrupted trans-synaptic signaling, impairing circuit assembly [15] |
| SYNGAP1 | RAS/RAP GTPase activator | Synaptic plasticity & dendritic spine maturation | Haploinsufficiency alters spine dynamics, causing E/I imbalance [15] |
| SCN2A | Voltage-gated sodium channel | Neuronal action potential generation | Altered neuronal excitability and network synchronization [3] |
Experimental Analysis of Neuronal Signaling Defects
Electrophysiological Protocols:
- Brain Slice Patch-Clamp Recording: Acute hippocampal or cortical slices (300-400 µm) prepared from ASD model mice (e.g.,
Chd8+/- orShank3+/-) at relevant developmental stages (e.g., P14-P21, P56-P70). Recordings target principal neurons in specific layers (e.g., L5 PFC pyramidal neurons) or cerebellar Purkinje cells. Measure miniature excitatory/inhibitory postsynaptic currents (mEPSCs/mIPSCs) in voltage-clamp mode (Vhold = -70 mV for mEPSCs, +10 mV for mIPSCs) with tetrodotoxin (1 µM) in artificial cerebrospinal fluid (aCSF) to isolate action-potential-independent release. Analyze amplitude, frequency, and kinetics of events to assess synaptic strength, presynaptic release probability, and receptor composition [16]. - Field Potential Recording: Assess long-term potentiation (LTP) and long-term depression (LTD) at the Schaffer collateral-CA1 synapse. Deliver test stimuli to establish baseline fEPSP slope, then apply conditioning protocols (e.g., 100 Hz tetanus for LTP, 1 Hz for LTD). Compare the magnitude and persistence of plasticity between genotypes.
Figure 1: Neuronal Signaling Disruptions in ASD. This diagram illustrates key presynaptic (NRXN1) and postsynaptic (NLGN3/4X, SHANK3, SYNGAP1) protein interactions crucial for synaptic adhesion, scaffolding, and glutamate receptor anchoring. Disruption leads to altered excitatory synaptic potential. Extracellular ATP (eATP) signaling via P2R purinergic receptors triggers the Cell Danger Response (CDR) and microglial activation, contributing to neuroinflammation [18] [15].
Chromatin Remodeling and Transcriptional Dysregulation
Epigenetic Mechanisms in ASD Pathogenesis
Chromatin remodeling complexes, which dynamically regulate DNA accessibility and gene expression, are central players in ASD etiology. Mutations in genes encoding components of these complexes, particularly the SWI/SNF (BAF) complex, are among the most significant genetic risk factors for ASD [14] [15].
Master Regulator: CHD8 The gene encoding CHD8 is one of the most prominent ASD-associated genes, functioning as an ATP-dependent chromatin remodeler [16]. CHD8 haploinsufficiency produces a recognizable ASD subtype often accompanied by macrocephaly, establishing it as a high-penetrance risk factor.
- Network-Level Influence: CHD8 acts as a master transcriptional regulator during early cortical development, controlling the proliferation of neural progenitors, cell fate specification, and synaptic maturation [16]. Its broad regulatory scope means that disruption cascades across multiple developmental stages and cell types.
- Cerebellar Impact: Single-nucleus transcriptomic and chromatin accessibility profiling in
Chd8+/- models reveal significant vulnerabilities in specific cerebellar cell populations, including Purkinje neurons, oligodendrocytes, and interneurons. These changes are accompanied by transcriptional signatures linked to synaptic regulation, RNA processing, and mitochondrial function, extending the pathology beyond the cerebral cortex [16].
Convergent Transcriptional Networks: Multiple high-confidence ASD genes converge on co-expression networks active during mid-fetal development in deep-layer cortical projection neurons [15]. These include:
ARID1B: A component of the SWI/SNF chromatin remodeling complex that modulates accessibility in excitatory neurons and interneurons.FOXP1: A transcription factor that regulates neuronal gene expression and converges withARID1Bat shared genomic targets.TBR1: A key transcription factor participating in the same midgestational transcriptional network.
These factors collectively regulate a critical period of transcriptional programming that, when disrupted, alters cortical lamination, neuronal migration, and circuit formation [15]. Post-mortem studies have identified patches of cortical disorganization in the dorsolateral prefrontal cortex of children with ASD, supporting the notion of early developmental disruption [14].
Table 2: Chromatin Remodeling Genes and Their Functional Consequences in ASD
| Gene/Complex | Molecular Function | Neurodevelopmental Role | Consequence of Disruption |
|---|---|---|---|
| CHD8 | ATP-dependent chromatin remodeler | Master regulator of neurodevelopmental gene expression; controls progenitor proliferation | Haploinsufficiency alters cerebellar development & cortical circuits; linked to macrocephaly [16] |
| SWI/SNF (BAF) Complex (e.g., ARID1B) | Nucleosome positioning & chromatin accessibility | Neural fate specification, neuronal migration | Altered chromatin accessibility in cortical neurons, disrupted cortical lamination & E/I balance [15] |
| FOXP1 | Transcription factor | Neuronal gene expression regulation | Disrupts shared genomic targets with ARID1B and TBR1 in fetal cortex [15] |
Methodologies for Profiling Chromatin Landscapes
Single-Cell Multi-Omics Protocols:
- snRNA-seq + snATAC-seq Co-assay: Isolate nuclei from fresh-frozen post-mortem brain tissue (e.g., dorsolateral PFC or cerebellum) from ASD and control donors. Using a commercial platform (e.g., 10x Multiome), perform simultaneous snATAC-seq and snRNA-seq on the same nuclei. For snATAC-seq: tagment nuclei with Tn5 transposase, amplify libraries, and sequence. For snRNA-seq: capture and reverse-transcribe polyA+ RNA, then amplify and sequence. Bioinformatically map accessible chromatin regions (peaks) and gene expression to specific cell types (excitatory neurons, inhibitory neurons, oligodendrocytes, microglia) [16].
- Data Integration & Analysis: Cluster cells based on gene expression and chromatin accessibility. Identify differentially accessible regions (DARs) and differentially expressed genes (DEGs) in ASD versus control within each cell type. Link putative regulatory elements (enhancers) to target genes based on correlation between accessibility and expression. Overlap DARs with known ASD-associated genetic variants from GWAS and WGS studies to prioritize functional non-coding disruptions [15] [16].
Figure 2: Chromatin Remodeling Disruption Cascade. This workflow depicts the sequence by which mutations in high-penetrance ASD risk genes (e.g., CHD8, ARID1B) dysregulate chromatin remodeling complexes, leading to altered chromatin accessibility and aberrant transcriptional programs during critical neurodevelopmental windows. This disruption impacts both cortical and cerebellar development, ultimately contributing to ASD phenotypes [15] [16].
Metabolic Pathway Dysregulation
Systemic Metabolic Impairments in ASD
Metabolic dysfunction in ASD extends beyond the brain, exhibiting characteristic signatures in peripheral biofluids that reflect systemic alterations in energy metabolism, antioxidant defense, and lipid handling.
Purine Metabolism and Mitochondrial Dysfunction: A core metabolic disruption in ASD involves the purine metabolic network, which is intrinsically linked to mitochondrial function [18].
- Developmental Dysregulation: In typically developing children, the purine network undergoes a characteristic 17-fold reversal during early childhood. This developmental switch fails to occur in children with ASD, indicating a arrested maturational program in one of the most fundamental metabolic pathways [18].
- Mitochondrial Involvement: Mitochondria produce over 90% of cellular ATP and contain approximately half of all metabolic enzymes, many regulated by ATP and related nucleotides. Chronic mitochondrial dysfunction is a well-established feature of ASD that can remodel the entire metabolic network, influence gene expression, and shift neurodevelopmental trajectories [18].
Altered Lipid Metabolism and Antioxidant Defenses: Cross-sectional studies of newborns who later develop ASD (pre-ASD) and 5-year-old children with ASD reveal consistent alterations in lipid metabolism and redox homeostasis.
- Shared Pathway Impact: Fourteen core biochemical pathways account for approximately 80% of the metabolic impact in both pre-ASD newborns and 5-year-olds with ASD [18].
- Lipid Metabolism Dominance: Altered lipid metabolism accounts for 63-71% of the total metabolic impact, with sphingolipids (ceramides, sphingomyelins) and phospholipids being particularly affected [18].
- Redox Imbalance: There is a consistent decrease in anti-inflammatory and antioxidant defenses, coupled with increased levels of physiological stress molecules including lactate, glycerol, glycerol-3-phosphate, cholesterol, and ceramides [18].
Table 3: Key Metabolic Pathway Disruptions in ASD Development
| Metabolic Pathway | Change in Pre-ASD Newborns | Change in 5-Year-Olds with ASD | Functional Interpretation |
|---|---|---|---|
| Purine Metabolism | Altered network regulation | Failed developmental reversal (17-fold) | Dysregulated purinergic signaling & CDR; arrested maturation [18] |
| Sphingolipid Metabolism | ↑ Ceramides, ↑ Sphingomyelins (25% of impact) | ↑ Ceramides, ↑ Sphingomyelins (25% of impact) | Increased cellular stress, altered membrane integrity, & signaling [18] |
| Phospholipid Metabolism | ↑ Key phospholipids (20% of impact) | ↑ Key phospholipids (26% of impact) | Membrane remodeling, inflammation, and signaling defects [18] |
| Antioxidant Defenses | ↓ Glutathione-related metabolites | ↓ Glutathione-related metabolites | Increased oxidative stress & vulnerability to inflammation [18] |
| Lactate & Alanine | ↑ Levels | ↑ Levels (54% greater than newborns) | Increased glycolytic flux & physiologic stress [18] |
Metabolomic Profiling and Network Analysis
Protocol: LC-MS/MS Based Metabolomics:
- Sample Preparation: Collect EDTA plasma from cohort participants (e.g., pre-ASD newborns, 5-year-old children with ASD, and matched typically developing controls). Deproteinize samples using cold methanol (1:3 sample:methanol ratio), vortex, and centrifuge (14,000 × g, 15 min, 4°C). Transfer supernatant and dry under nitrogen. Derivatize if analyzing certain lipid classes [18].
- Liquid Chromatography Separation: Use a reversed-phase C18 column (e.g., 2.1 × 100 mm, 1.8 µm) with a binary gradient. Mobile phase A: 10 mM ammonium acetate in water with 0.1% formic acid. Mobile phase B: 10 mM ammonium acetate in 90% acetonitrile with 0.1% formic acid. Use a gradient from 5% B to 100% B over 15-20 minutes. Maintain column temperature at 40°C [18].
- Mass Spectrometry Analysis: Operate a high-resolution tandem mass spectrometer (e.g., Q-TOF) in both positive and negative electrospray ionization modes. Set source temperature to 150°C, desolvation temperature to 500°C, and capillary voltage to 3.0 kV. Use data-independent acquisition (MSE) to fragment all ions for MS/MS spectral matching [18].
- Data Processing & Network Analysis: Process raw data using vendor software for peak picking, alignment, and compound identification against commercial databases (e.g., HMDB, LipidMaps). Perform multivariate statistical analysis (PLS-DA) to identify discriminating metabolites (VIP ≥ 1.5). Calculate z-scores for significantly altered metabolites. Construct metabolic networks and calculate novel parameters like ( \dot{V}_{\text{net}} ) to quantify differences in network connectivity and hub structure between ASD and control groups [18].
Figure 3: Integrated Metabolic Dysregulation in ASD. Genetic and environmental stressors trigger mitochondrial dysfunction, which disrupts purine metabolism and increases extracellular ATP (eATP) release. This initiates a chronic Cell Danger Response (CDR), driving lipid metabolism dysregulation (increased ceramides, phospholipids) and oxidative stress (reduced antioxidant defenses). These interconnected metabolic disturbances collectively contribute to altered neurodevelopment and neural function [18].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Tools for Investigating ASD Pathways
| Reagent / Resource | Specific Example (Catalog # if possible) | Research Application | Key Function in ASD Research |
|---|---|---|---|
| SPARK Cohort Data | SPARK (Simons Foundation) [3] [2] | Genotype-Phenotype Correlation | Largest U.S. ASD cohort; provides integrated WGS & deep phenotypic data for >5, 000 individuals for subtype discovery [3] [2] [4] |
| General Finite Mixture Model (GFMM) | Custom R/Python implementation [2] | Phenotypic Decomposition | Person-centered computational approach to identify clinically relevant ASD subtypes based on >230 trait combinations [2] |
| snRNA-seq + snATAC-seq Kits | 10x Genomics Multiome ATAC + Gene Expression | Single-Cell Multi-Omics | Simultaneously profiles chromatin accessibility & gene expression in same nucleus; identifies cell-type-specific regulatory disruptions in post-mortem brain [16] |
| LC-MS/MS Metabolomics Platform | Agilent 6495C QQQ or Thermo Q Exactive HF-X | Metabolic Phenotyping | Quantifies ~450 polar & lipid metabolites; identifies dysregulated pathways (e.g., purine, lipid metabolism) in plasma/serum [18] |
| CHD8 Haploinsufficiency Mouse Model | Chd8+/- (JAX Stock #) |
In Vivo Functional Validation | Models a high-penetrance monogenic ASD form; used for electrophysiology, behavior, and multi-omics studies, especially cerebellar [16] |
| Transmission and De Novo Association (TADA) | TADA R package | Statistical Genetics | Bayesian framework for identifying ASD-risk genes by integrating de novo and rare inherited variant burden from WES/WGS data [15] |
The pathogenesis of Autism Spectrum Disorder is increasingly understood through discrete yet interconnected biochemical pathway disruptions. Research now demonstrates that heterogeneous genetic risks funnel into convergent biological narratives affecting chromatin remodeling, neuronal signaling, and metabolic regulation [14] [15] [16]. The recent decomposition of ASD into biologically distinct subtypes represents a paradigm shift, moving the field beyond a "one-size-fits-all" model toward a precision medicine framework [3] [2] [4].
Future research must prioritize several key areas:
- Non-Coding Genome Integration: Expanding analyses to include the 98% of the genome that does not code for proteins will likely reveal additional regulatory disruptions contributing to ASD heterogeneity [15] [4].
- Developmental Timeline Mapping: Precise temporal mapping of when and where specific pathway disruptions exert their effects will be crucial for identifying critical intervention windows [3] [2].
- Therapeutic Translation: The identification of subtype-specific biological narratives, such as distinct pathway disruptions in the "Social and Behavioral Challenges" versus "Broadly Affected" subgroups, provides a rational foundation for developing targeted, mechanism-based therapies [3] [2] [4].
By leveraging large-scale multi-omics datasets, advanced computational models, and precise experimental systems, researchers are now equipped to dissect the complex architecture of ASD pathogenesis and develop interventions that target its root biological causes.
Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition characterized by persistent deficits in social communication and interaction, alongside restricted, repetitive patterns of behavior, interests, or activities [19]. Research from the past decade has revolutionized our understanding of ASD's origins, revealing it to be a multistage prenatal disorder that impacts a child's ability to perceive and react to social information [20]. Rather than beginning in early childhood, ASD is now understood as a highly heritable, brain-wide disorder of prenatal and early postnatal development, with most ASD risk genes expressing prenatally and falling into two functional categories: broadly expressed regulatory genes and brain-specific genes [20]. The developmental timeline of these genetic risk programs is not uniform; instead, it follows specific epochs of vulnerability that profoundly influence brain development and clinical outcomes.
The prenatal origin of ASD is supported by multiple lines of evidence. Postmortem studies of young ASD cases reveal an overabundance of cortical neurons—on average, 67% more prefrontal neurons than controls—which must originate during prenatal neurogenesis since cortical neuron proliferation occurs primarily between 10 and 20 weeks of gestation [20]. Furthermore, in utero brain overgrowth is a recognized phenomenon in ASD, and focal disorganization of cortical layers provides evidence of disrupted second and third-trimester development [20]. This review examines the precise developmental timing of genetic risk program activation within the context of biochemical pathway dysregulation, providing a technical framework for researchers investigating ASD pathogenesis and therapeutic development.
Genetic Risk Programs: Prenatal vs. Postnatal Expression Patterns
Temporal Expression of ASD Risk Genes
The majority of high-confidence ASD (hcASD) risk genes exhibit predominant prenatal expression, with their peak influence aligning with specific developmental processes [20]. Analysis of gene expression patterns reveals two primary epochs of vulnerability during neurodevelopment:
- Epoch-1 (68% of ASD genes): Spanning trimesters 1-3, involving broadly expressed regulatory genes (the majority) and brain-specific genes that disrupt cell proliferation, neurogenesis, migration, and cell fate [20].
- Epoch-2 (32% of ASD genes): Spanning trimester 3 and early postnatal periods, involving primarily brain-specific genes that disrupt neurite outgrowth, synaptogenesis, and cortical "wiring" [20].
Recent genetic studies of 102 putative ASD risk genes found that 98 had their highest expression in prenatal cortex compared with postnatal development [20]. This prenatal predominance is consistently observed across multiple brain regions implicated in ASD, including cortex, cerebellum, amygdala, hippocampus, and striatum [20].
Table 1: Developmental Timeline of ASD Risk Gene Expression and Primary Functions
| Developmental Period | % of hcASD Genes | Primary Gene Categories | Key Disrupted Processes | Associated Brain Regions |
|---|---|---|---|---|
| Epoch-1 (Trimesters 1-3) | 68% | Broadly-expressed regulatory (majority), Brain-specific | Cell proliferation, Neurogenesis, Migration, Cell fate | Cortex, Cerebellum, Amygdala, Hippocampus, Striatum |
| Epoch-2 (Trimester 3-Early Postnatal) | 32% | Brain-specific (majority) | Neurite outgrowth, Synaptogenesis, "Wiring" of cortex | Cortex, Hippocampus |
Functional Classification of ASD Risk Genes
ASD risk genes demonstrate significant functional pleiotropy, with approximately two-thirds influencing two or more neurodevelopmental processes [20]. A recent literature survey of 58 functionally characterized hcASD genes revealed their involvement across multiple prenatal stages:
- 57% are involved in proliferation
- 26% in migration and cell fate specification
- 52% in neurite outgrowth
- 59% in synaptogenesis and synapse functioning [20]
This pleiotropy adds a genetic explanation to the developmental pathobiology revealed by postmortem, neuroimaging, and induced pluripotent stem cell (iPSC) studies, showing that ASD risk genes collectively impact excess cell proliferation, disrupted neurogenesis and maturation, mis-migration, disrupted synaptic development and function, and deviant neurofunctional activity and connectivity [20].
Table 2: Functional Roles of Characterized ASD Risk Genes in Neurodevelopmental Processes
| Neurodevelopmental Process | % of Characterized hcASD Genes Involved | Specific Functions Disrupted | Consequence of Dysregulation |
|---|---|---|---|
| Proliferation | 57% | Cell cycle regulation, G1/S transition, Apoptosis | Excess neurons, Brain overgrowth, Early overgrowth |
| Migration & Cell Fate | 26% | Neuronal positioning, Cortical layer formation | Focal cortical dyslamination, Mis-migrated neurons |
| Neurite Outgrowth | 52% | Axon guidance, Dendritic arborization | Reduced neuron size, Altered connectivity |
| Synaptogenesis & Function | 59% | Spine formation, Synapse maturation, Neural activity | Excitation/inhibition imbalance, Network dysfunction |
Biochemical Pathways in ASD Pathogenesis
Key Signaling Pathways Disrupted in ASD
The mechanistic basis of ASD involves dysregulation of core signaling pathways that coordinate neurodevelopment. Upstream highly interconnected regulatory ASD gene mutations disrupt transcriptional programs or signaling pathways, resulting in dysregulation of downstream processes such as proliferation, neurogenesis, synaptogenesis, and neural activity [20]. Pathway analysis has identified several key pathways consistently implicated in ASD pathogenesis:
- Chromatin remodeling pathways: Involving changes in DNA and histone structure that regulate gene expression without altering the DNA sequence itself, significantly impacting neuronal differentiation and synapse formation [14].
- Wnt and Notch signaling pathways: Critical for brain development and neuroplasticity, with dysregulation leading to altered cell fate determination and circuit formation [14].
- Redox system dysfunction: A progressive maladaptation where reactive oxidant species, molecular targets, and reducing/antioxidant counterparts function as dynamic circuitry whose disruption undermines cellular homeostasis [21].
- ARP2/3 mediated actin dynamics: Regulated by genes such as CYFIP1, which interacts with WAVE1 to modulate actin branching, affecting cell survival and migration of newborn neurons [22].
These pathways do not operate in isolation but form an interconnected network that guides proper brain development. Dysregulation at specific developmental timepoints can create cascading effects that manifest as ASD symptomatology.
Diagram: Signaling Pathways in ASD Neurodevelopment
Experimental Models and Methodologies
iPSC Models of Idiopathic ASD
Induced pluripotent stem cell (iPSC) studies have provided direct insights into prenatal origins in idiopathic ASD, revealing disruptions across multiple developmental stages [20].
Experimental Protocol: iPSC to Neuron Differentiation
Primary Research Objective: To model early neurodevelopmental processes disrupted in ASD using patient-derived iPSCs.
Methodology Details:
- iPSC Generation: Dermal fibroblasts or peripheral blood mononuclear cells from ASD individuals and healthy controls are reprogrammed using non-integrating Sendai virus vectors containing OCT4, SOX2, KLF4, and c-MYC.
- Neural Induction: iPSCs are differentiated into neural progenitor cells (NPCs) using dual SMAD inhibition (LDN-193189 and SB431542) in neural induction medium for 10-14 days.
- Neuronal Differentiation: NPCs are dissociated and plated on poly-ornithine/laminin-coated surfaces in neuronal differentiation medium containing BDNF, GDNF, cAMP, and ascorbic acid for 4-8 weeks.
- Functional Analysis: Neurons are analyzed at multiple timepoints for morphological, molecular, and functional properties.
Key Parameters Assessed:
- Cell proliferation: Measured via EdU incorporation assays and Ki67 immunostaining at NPC stage
- Cell cycle analysis: Flow cytometry for G1/S phase duration
- Neuronal differentiation: Quantified by Tuj1/TBR1/CTIP2 immunostaining
- Synaptic maturation: Analyzed via synapsin/PSD95 staining and electrophysiology
- Neural activity: Measured using calcium imaging or multi-electrode arrays
Representative Findings: In the largest iPSC study to date (n=8 ASD, n=5 controls), every ASD child showed disruptions in multiple prenatal stages including proliferation, maturation, synaptogenesis, and neural activity [20]. Specifically, ASD cells displayed high rates of cell proliferation, G1/S shortening, reduced differentiation and neuronal maturation, abnormal inhibitory and excitatory synaptic maturation, and reduced neural activity [20].
Animal Models of Genetic Risk Factors
Animal models, particularly rodents, provide critical platforms for investigating the temporal requirements of ASD gene function and testing therapeutic interventions.
Experimental Protocol: Cyfip1 Haploinsufficiency Model
Primary Research Objective: To investigate how haploinsufficiency of Cyfip1, a candidate risk gene in the 15q11.2(BP1-BP2) deletion, impacts postnatal hippocampal neurogenesis.
Methodology Details:
- Animal Model: Cyfip1tm2a(EUCOMM)Wtsi animals maintained heterozygously on C57/BL6J background, with wild-type littermates as controls.
- Tissue Preparation: Paraformaldehyde fixed brains from 8-12-week-old animals sectioned at 40μm using cryostat.
- Immunohistochemistry: Free-floating sections incubated with primary antibodies (BrdU, Ki67, DCX, NeuN, cleaved-caspase 3) followed by appropriate secondary antibodies.
- Cell Culture: Primary hippocampal progenitors isolated from P7-P8 animals, cultured on poly-L-lysine/laminin with EGF and FGF2.
- Microglial Culture: Primary microglia isolated from P7-P8 whole brain mixed glia via shake-off method.
- Time-lapse Imaging: Primary hippocampal progenitors imaged at 5 DIV for 2 hours with image acquisition every 5 minutes.
- Actin Analysis: Cells stained with Alexafluor 488-conjugated DNAseI and Alexafluor 647-conjugated phalloidin.
- Arp2/3 Inhibition: Cells treated with 50μM CK-548 or 250μM CK-666 in DMSO prior to imaging.
Key Findings: Cyfip1 haploinsufficiency led to increased numbers of adult-born hippocampal neurons due to reduced apoptosis, without altering proliferation [22]. This resulted from a cell autonomous failure of microglia to induce apoptosis through secretion of appropriate factors [22]. Additionally, abnormal migration of adult-born neurons was observed due to altered Arp2/3 mediated actin dynamics [22].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating ASD Developmental Timeline
| Reagent/Category | Specific Examples | Research Application | Technical Function |
|---|---|---|---|
| iPSC Differentiation | LDN-193189, SB431542 | Neural induction from iPSCs | Dual SMAD inhibition to direct neural fate |
| Neuronal Markers | Tuj1 (β-III-tubulin), MAP2, NeuN | Identifying neuronal identity | Cytoskeletal and nuclear markers for neurons |
| Synaptic Markers | Synapsin, PSD95, VGLUT1, GAD67 | Assessing synaptic development | Pre- and post-synaptic protein localization |
| Proliferation Assays | EdU, BrdU, Ki67 antibody | Measuring cell division | Nucleotide analogs for DNA labeling, cell cycle marker |
| Apoptosis Assays | Cleaved-caspase 3, TUNEL | Quantifying programmed cell death | Marker of apoptotic activation, DNA fragmentation |
| Cytoskeletal Probes | Phalloidin (F-actin), DNAseI (G-actin) | Visualizing actin dynamics | Selective binding to filamentous/globular actin |
| Arp2/3 Inhibitors | CK-548, CK-666 | Disrupting actin branching | Specific inhibition of Arp2/3 complex formation |
Environmental Influences on Genetic Risk Programs
Maternal Immune Activation and Fetal Brain Development
Environmental challenges during the prenatal period can significantly modulate genetic risk programs, with maternal immune activation (MIA) representing a well-characterized pathway [23]. MIA triggered by infection or inflammation during pregnancy has been associated with developmental difficulties in children, including increased risk of speech, language, and motor delays, behavioral and emotional problems, and altered connectivity in brain regions supporting working memory [23].
The mechanistic pathway involves:
- Cytokine elevation: MIA elevates circulating and central proinflammatory cytokines in animal models, potentially impacting fetal immunity and neurodevelopment [23].
- Placental signaling: The placenta expresses toll-like receptors that can directly recognize microbial products, leading to increased placental inflammation and inflammatory cytokine release that affects fetal brain development [23].
- Specific cytokine effects: IL-6 plays a critical role in promoting MIA-induced ASD-like deficits in inhibition control and social interaction in mice [23]. Blocking placental IL-6 signaling prevents MIA-induced immune activation in the fetal brain and subsequent behavioral abnormalities [23].
Diagram: Maternal Immune Activation Experimental Workflow
Teratogenic Exposures and Gene Expression Modulation
Prenatal exposure to specific teratogens has been associated with increased incidence of ASD, providing insights into critical developmental windows [24]. Valproic acid, ethanol, thalidomide, and misoprostol have all been documented to increase ASD risk, with exposure timing particularly critical during early pregnancy (estimated between the 18th and 42nd day) [24].
These teratogens share common mechanisms of action:
- Gene expression modulation: Each drug can modulate the expression of numerous genes involved in proliferation, apoptosis, neuronal differentiation, migration, synaptogenesis, and synaptic activity [24].
- Early neurodevelopment disruption: These compounds affect development at very early stages, potentially inducing not only autism but also malformations of ears, eyes, and limbs, along with language delay and mental retardation [24].
- Biological process deregulation: Common processes affected include proliferation/apoptosis balance, neuronal differentiation, connectivity, and circulatory system development [24].
Implications for Therapeutic Development
Targeting Developmental Windows
The precise temporal mapping of ASD risk gene activation provides critical insights for therapeutic intervention strategies. The recognition that most ASD risk genes express prenatally suggests that optimal intervention timeframes may be earlier than previously recognized [20]. Two key strategic approaches emerge:
- Epoch-specific interventions: Targeting mechanisms specific to each developmental epoch, such as proliferation modulation during Epoch-1 versus synaptic stabilization during Epoch-2.
- Pathway-based approaches: Focusing on downstream convergent pathways rather than individual genetic mutations, given the pleiotropic nature of ASD genes and their convergence on common biological processes.
The recognition that the majority of ASD risk genes are broadly expressed, not limited to the brain, suggests that many ASD individuals may benefit from being treated as having a broader medical disorder rather than exclusively a brain disorder [20]. This has significant implications for both therapeutic development and clinical management approaches.
Biomarker Discovery and Early Identification
Understanding the developmental timeline of genetic risk programs enables a more targeted approach to biomarker discovery. Several promising biomarker candidates have emerged:
- Maternal autoantibodies: Specific maternal autoantibody patterns reactive against fetal brain proteins (MAR ASD) are observed in approximately 20% of ASD cases, with mothers exhibiting these antibodies being 31 times more likely to have a child with ASD [25].
- Immune markers: Altered cytokine and chemokine profiles in mothers during pregnancy and in newborns at birth show associations with subsequent ASD diagnosis [25].
- Redox system markers: Evidence of redox system dysfunction provides potential biomarkers of altered metabolic and signaling pathways in ASD [21].
These biomarkers not only offer potential for early identification but also begin to define biologically distinct subtypes of ASD, which may respond differentially to targeted interventions.
The developmental timeline of genetic risk program activation in ASD reveals a predominantly prenatal disorder with two main epochs of vulnerability: Epoch-1 (trimesters 1-3) involving broadly expressed regulatory genes disrupting proliferation, neurogenesis, migration and cell fate; and Epoch-2 (trimester 3 and early postnatal) involving primarily brain-specific genes disrupting neurite outgrowth, synaptogenesis and cortical wiring [20]. This temporal mapping, framed within the context of biochemical pathway dysregulation, provides a critical framework for understanding ASD pathogenesis and developing targeted interventions.
Future research directions should prioritize the non-invasive study of ASD cell biology, further refinement of developmental timelines for specific genetic risk programs, and the development of epoch-specific therapeutic approaches that account for the temporal dynamics of ASD pathogenesis. The integration of genetic, epigenetic, and environmental factors across developmental time will be essential for advancing our understanding of ASD and developing effective, biologically-based interventions.
The Gut-Brain Axis and Neuroimmune Dysregulation in ASD Pathophysiology
Autism Spectrum Disorder (ASD) represents a group of complex neurodevelopmental conditions characterized by two primary symptom domains: persistent deficits in social communication and social interaction, and restricted, repetitive patterns of behavior, interests, or activities [26]. These core symptoms typically emerge in early childhood and often lead to clinically significant impairment in social, occupational, or other important areas of functioning. The diagnostic criteria according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) require that symptoms be present in the early developmental period, though they may not become fully manifest until social demands exceed limited capacities [26].
The epidemiological landscape of ASD has undergone significant changes over recent decades, with steadily increasing prevalence rates observed worldwide. According to the Centers for Disease Control and Prevention (CDC) Autism and Developmental Disabilities Monitoring (ADDM) Network, the identified prevalence has risen from 1 in 150 children in 2000 to approximately 1 in 31 children (3.2%) as of 2022 surveillance data [27]. This increasing trend reflects both improved awareness and diagnostic practices as well as potential changes in risk factors. ASD is reported to occur across all racial, ethnic, and socioeconomic groups, though a striking gender disparity persists with males being diagnosed approximately 3 times more frequently than females [27] [26].
Beyond the core behavioral symptoms, ASD is frequently accompanied by numerous comorbidities and associated features. These include neurological conditions such as epilepsy, sleep disorders, and motor abnormalities; psychiatric comorbidities including anxiety, depression, and attention-deficit/hyperactivity disorder; and various medical conditions including gastrointestinal disorders, immune dysregulation, and metabolic abnormalities [26] [28]. The substantial clinical heterogeneity of ASD is reflected not only in the variability of core symptom severity but also in the pattern and prevalence of these associated conditions, presenting significant challenges for diagnosis, treatment, and research.
Table 1: Epidemiological Trends in ASD Prevalence Based on CDC ADDM Network Data
| Surveillance Year | Birth Year | Combined Prevalence per 1,000 Children | Approximate Ratio |
|---|---|---|---|
| 2000 | 1992 | 6.7 | 1 in 150 |
| 2006 | 1998 | 9.0 | 1 in 110 |
| 2008 | 2000 | 11.3 | 1 in 88 |
| 2012 | 2004 | 14.5 | 1 in 69 |
| 2016 | 2008 | 18.5 | 1 in 54 |
| 2020 | 2012 | 27.6 | 1 in 36 |
| 2022 | 2014 | 32.2 | 1 in 31 |
The Gut-Brain Axis: Fundamental Mechanisms and Pathways
The microbiota-gut-brain axis (MGBA) represents a complex, bidirectional communication network linking the gastrointestinal tract with the central nervous system. This system integrates neural, endocrine, and immune signaling pathways to facilitate continuous cross-talk between the brain and the gut microbiota, which comprises the trillions of microorganisms residing in the intestinal tract [29] [30]. In ASD pathophysiology, this axis has emerged as a crucial area of investigation, with mounting evidence suggesting its significant contribution to the disorder's development and manifestation.
The MGBA consists of several integrated components: the gut microbiota with its diverse microbial communities; the intestinal mucosal barrier and epithelium; the enteric nervous system (often described as the "second brain"); the autonomic nervous system, particularly the vagus nerve; and various neuroendocrine and neuroimmune pathways [30]. These elements work in concert to monitor and regulate gastrointestinal function while simultaneously influencing brain development, neural activity, and behavior. In individuals with ASD, multiple aspects of this complex system appear to be dysregulated, potentially contributing to both the core behavioral symptoms and frequent gastrointestinal comorbidities.
The primary communication pathways of the MGBA include:
- Neural pathways: The vagus nerve serves as a direct neural connection between the gut and brain, transmitting sensory information from the periphery to central nervous system nuclei and relaying efferent signals back to the gastrointestinal tract. Studies have demonstrated that children with ASD frequently exhibit parasympathetic dysregulation and reduced vagal tone, which correlates with the severity of core symptoms including social interaction deficits and language impairments [30].
- Endocrine pathways: The hypothalamic-pituitary-adrenal (HPA) axis mediates stress responses and is significantly influenced by gut microbiota composition and activity. In ASD, alterations in microbial communities can lead to HPA axis dysregulation, resulting in elevated cortisol levels that may contribute to anxiety and repetitive behaviors [30].
- Immune pathways: The intestinal mucosa houses approximately 70% of the body's immune tissue, and gut microbiota play a crucial role in immune system development and regulation. Dysbiosis in ASD can trigger localized and systemic immune activation, leading to increased production of pro-inflammatory cytokines that can cross the blood-brain barrier and influence neurodevelopment and function [29] [31].
- Metabolic pathways: Gut microbiota produce numerous neuroactive metabolites during food digestion, including short-chain fatty acids (SCFAs), neurotransmitters, and tryptophan derivatives. These microbial metabolites can enter systemic circulation and directly or indirectly influence brain function, neurotransmission, and behavior [29] [32].
Table 2: Key Microbial Metabolites Implicated in ASD Pathophysiology
| Metabolite Category | Specific Molecules | Proposed Mechanisms in ASD | Observed Alterations in ASD |
|---|---|---|---|
| Short-chain fatty acids | Butyrate, Propionate, Acetate | Epigenetic modulation, Blood-brain barrier permeability, Microglial activation | Reduced butyrate-producing bacteria; Variable SCFA levels |
| Tryptophan metabolites | Kynurenine, Kynurenate, Serotonin | Neuroimmune activation, Neurotransmitter synthesis, Oxidative stress | Reduced kynurenate; Disrupted kynurenine pathway [32] |
| Neurotransmitters | GABA, Serotonin, Dopamine | Direct receptor activation, Neural circuit modulation | Altered microbial GABA production; Peripheral serotonin dysregulation |
| Bacterial neuroactives | p-Cresol, 4-Ethylphenylsulfate | Mitochondrial function, Dopamine metabolism, Blood-brain barrier transport | Increased p-cresol sulfate in some studies |
Figure 1: Bidirectional Communication Pathways of the Microbiota-Gut-Brain Axis. The diagram illustrates the integrated neural, endocrine, immune, and metabolic pathways facilitating continuous communication between the gut environment and the central nervous system, with relevance to ASD pathophysiology.
Gut Microbiota Alterations in ASD: Characterization and Functional Consequences
Individuals with ASD demonstrate distinct alterations in gut microbiota composition compared to neurotypical individuals, a phenomenon characterized as gut dysbiosis. While findings across studies show some variability, likely due to population heterogeneity, methodological differences, and confounding factors such as dietary patterns and gastrointestinal symptoms, several consistent patterns have emerged from microbiome research in ASD [29] [30].
At the phylum level, children with ASD often exhibit a markedly reduced proportion of Firmicutes, a decreased Bacteroidetes-to-Firmicutes ratio, and an increased abundance of Acidobacteria [30]. These shifts in major bacterial phyla represent a fundamental alteration in the gut microbial ecosystem that may have cascading effects on host physiology, immune function, and metabolism. Additionally, specific butyrate-producing bacterial groups—including Ruminococcaceae, the Eubacterium rectale group, Lachnospiraceae, and Erysipelotrichaceae—are frequently reduced in children with ASD, while the abundance of Clostridium is typically significantly increased [30].
At the genus and species levels, more consistent alterations have been observed, providing potential microbial biomarkers for ASD. The abundance of Bifidobacterium and Prevotella is often reduced, while Veillonella parvula, Lactobacillus rhamnosus, and Desulfovibrio are enriched in the gut of individuals with ASD [30]. Particularly noteworthy is the increased presence of Sutterella and Desulfovibrio in children with ASD; the latter genus may produce hydrogen sulfide through sulfate reduction, potentially exacerbating intestinal inflammation and contributing to stereotyped behaviors [30].
The functional consequences of these microbial alterations are multifaceted and potentially highly relevant to ASD pathophysiology:
- Increased intestinal permeability: Often described as "leaky gut," this condition allows microbial metabolites and neuroactive compounds to enter systemic circulation, potentially disrupting the HPA axis and contributing to behavioral abnormalities including anxiety and repetitive behaviors [30].
- Altered microbial metabolite production: The reduction in beneficial bacteria like Bifidobacterium impairs the synthesis of short-chain fatty acids and is associated with decreased serum levels of folate and vitamin B12, both crucial for neurological function [30].
- Vitamin and nutrient deficiencies: Children with ASD frequently exhibit significantly lower serum levels of folate and vitamin B12 compared to healthy controls, and the metabolism of these vitamins depends substantially on the biosynthetic activity of the gut microbiota [30].
- Exacerbation through dietary patterns: The monotonous dietary habits commonly observed in individuals with ASD—such as preferences for high-sugar foods and inadequate intake of fruits and vegetables—further exacerbate vitamin deficiencies and microbial dysbiosis, creating a self-perpetuating cycle that reinforces both gastrointestinal and behavioral symptoms [30].
The relationship between gut microbiota composition and ASD symptoms is further complicated by the inconsistent findings regarding alpha and beta diversity measures across studies, with some investigations failing to detect significant differences between ASD and neurotypical groups [30]. This variability highlights the substantial heterogeneity within the ASD population and suggests that microbiome-based subgroups may exist within the broader autism spectrum.
Neuroimmune Dysregulation: Mechanisms and Pathways
Immune system dysregulation represents a core component of ASD pathophysiology, with substantial evidence implicating both peripheral and central nervous system immune mechanisms. The immune hypothesis of autism has gained increasing support from multiple lines of investigation, including genetic studies, biomarker analyses, neuropathological examinations, and animal models [31] [28]. This immune dysregulation manifests across both innate and adaptive immune systems and involves complex interactions between genetic susceptibility and environmental factors.
Cytokine Dysregulation and Neuroinflammation
Cytokines, as key signaling molecules in immune responses, show consistent alterations in individuals with ASD. Pro-inflammatory cytokines including IL-1β, IL-6, and TNF-α are frequently elevated in the plasma, cerebrospinal fluid, and postmortem brain samples of individuals with ASD [28]. These cytokines play crucial roles in establishing a neuroinflammatory milieu that can significantly impact brain development and function:
- IL-1β modulates neural plasticity and is necessary for long-term potentiation maintenance in the hippocampal CA1 region. Abnormally elevated levels or depleted IL-1 lead to memory impairments, suggesting that precise regulation of this cytokine is essential for normal cognitive function [28].
- IL-6 is particularly important during brain development, where it influences neuronal cellular adhesion, migration, and synapse formation. Dysregulated IL-6 signaling during critical developmental windows may disrupt the normal establishment of neural circuits relevant to social behavior and communication [28].
- TNF-α serves as a master regulator of inflammation and cytokine production. In addition to its pro-inflammatory effects, TNF-α influences synaptic scaling and may contribute to the imbalance between excitatory and inhibitory neurotransmission observed in ASD [28].
Beyond these primary pro-inflammatory cytokines, other immune signaling molecules show alteration in ASD. Macrophage inhibitory factor (MIF) demonstrates increased serum concentrations that correlate with worsening behavioral assessments in individuals with ASD compared to their unaffected siblings [31]. Additionally, the IL-23/Th17 pathway has been implicated in ASD pathogenesis, with IL-17 identified as a critical mediator of neurodevelopmental abnormalities associated with maternal immune activation models [31].
Adaptive Immune System Alterations
The adaptive immune system also demonstrates significant dysregulation in ASD, with alterations observed in multiple lymphocyte populations:
- T cell imbalances: Earlier observations described decreased lymphocyte responses to mitogens in children with ASD, with subsequent studies revealing a decreased helper/suppressor ratio with decreased percentage of helper-inducer T cells and decreased percentage of cells positive to IL-2R under mitogenic stimulation [31]. A significant increase in CD4+ memory and decrease in CD4+ naïve T cells has been observed in autism, along with an imbalance of cytokines produced by CD4+ and CD8+ T cells with reported skewing toward a Th2 response [31].
- Regulatory T cell deficiency: Studies have revealed a lower number of CD4+ CD25 high Tregs in the blood of autistic children, supporting the reporting of allergic problems and family history of autoimmunity as risk factors for ASD [31]. This deficit in regulatory populations may contribute to the breakdown of immune tolerance and increased inflammation observed in ASD.
- B cell abnormalities: Recent studies reveal high levels of pro-inflammatory cytokines (IL-6 and TNF-α) and low levels of the anti-inflammatory cytokine IL-10 in peripheral blood lymphocytes of ASD children, suggesting B cell contribution to the overall inflammatory state [28].
Genetic and Molecular Basis of Immune Dysregulation
The genetic architecture of ASD provides important insights into the molecular basis of immune dysregulation in this disorder. Multiple immune-related genes have been associated with ASD risk, highlighting the biological plausibility of immune mechanisms in disease pathogenesis:
- Major Histocompatibility Complex (MHC) genes: Specific human leukocyte antigen (HLA) alleles including HLA-A2, DR4, and DR11 are associated with diminished lymphocyte response and increased susceptibility for ASD [31]. Within the HLA class III region, a complement C4B null allele resulting from duplications of C4A confers a relative risk of 4.3 for the development of ASD [31].
- MHC-I neuronal functions: Beyond their traditional immune functions, MHC-I proteins are expressed on neuronal surfaces where they localize to synapses and control axonal and dendritic outgrowth. MHC-I negatively regulates the initial establishment of connections in the CNS and bidirectionally regulates both the initial establishment and strength of synapses, with potential implications for the altered connectivity observed in ASD [31].
- Non-MHC immune genes: The serine and threonine kinase C gene PRKCB1, involved in both B-cell activation and neuronal function, has been linked to ASD in some studies [31]. Similarly, functional polymorphisms of macrophage inhibitory factor (MIF), which has diverse effects on innate and adaptive immune responses, have been associated with ASD individuals [31].
Table 3: Key Immune System Alterations in ASD Pathophysiology
| Immune Component | Specific Alterations in ASD | Functional Consequences |
|---|---|---|
| Innate Immunity | Microglial activation; Increased monocytes; Elevated pro-inflammatory cytokines | Neuroinflammation; Synaptic pruning defects; Oxidative stress |
| Adaptive Immunity | T cell imbalances (↑memory, ↓naïve); Th2 skewing; Treg deficiency; Altered B cell function | Reduced immune regulation; Autoimmunity risk; Chronic inflammation |
| Cytokine Profile | ↑IL-1β, IL-6, TNF-α, IL-17; ↑MIF; Altered chemokines | Blood-brain barrier disruption; Altered neurodevelopment; Behavioral changes |
| Genetic Factors | HLA associations; Complement C4B null allele; MHC-I dysregulation | Synaptic development alterations; Immune response dysregulation |
Figure 2: Neuroimmune Dysregulation Pathways in ASD. The diagram illustrates how genetic and environmental factors converge to drive immune system dysregulation, which in turn impacts brain development and function through multiple mechanisms, ultimately contributing to the behavioral phenotype of ASD.
Key Signaling Pathways in ASD Pathophysiology
Research into the molecular basis of ASD has revealed convergence onto several key biochemical pathways that integrate signals from both the gut-brain axis and immune system. These pathways represent crucial points of intersection where genetic susceptibility, environmental factors, and physiological systems interact to influence neurodevelopment and neural function. Pathway network analyses of ASD-associated genes have identified calcium signaling pathway and neuroactive ligand-receptor interaction as the most enriched, statistically significant pathways, with calcium signaling pathways and MAPK signaling pathway serving as interactive hubs connecting multiple biological processes [33] [26].
The calcium-PKC-Ras-Raf-MAPK/ERK cascade has emerged as a major contributor to ASD pathophysiology, integrating signals from multiple ASD-associated genes and environmental factors [33]. This pathway connects extracellular signals to intracellular responses through a series of phosphorylation events, ultimately influencing gene expression, protein synthesis, and synaptic plasticity. Dysregulation at multiple points along this cascade can lead to either excessive or deficient neural growth and connectivity, potentially explaining the divergent neuroanatomical and connectivity findings in different ASD subtypes [34].
The mTOR signaling pathway represents another crucial hub in ASD pathophysiology, integrating signals from growth factors, nutrients, and cellular energy status to regulate numerous cellular processes including protein synthesis, autophagy, and metabolism. Both hyperactive and hypoactive mTOR signaling have been implicated in different forms of ASD, consistent with the observation of both overgrowth and undergrowth phenotypes across the autism spectrum [26] [34]. In syndromic forms of ASD such as tuberous sclerosis and PTEN hamartoma tumor syndrome, mTOR pathway dysregulation represents a primary disease mechanism, while in idiopathic ASD, more subtle alterations in mTOR signaling may contribute to synaptic dysfunction and neural circuit abnormalities.
Growth factor signaling pathways including those mediated by BDNF, IGF-1, and FGF also demonstrate alterations in ASD and interact closely with both immune signaling and gut-brain axis communication. These pathways influence neuronal survival, differentiation, and synaptic maturation during critical developmental windows, with dysregulation potentially leading to the altered trajectory of brain development observed in ASD [26] [34]. Interestingly, these same pathways can be modulated by microbial metabolites and immune molecules, providing potential mechanisms through which gut dysbiosis and neuroinflammation might influence brain development.
The concept of opposing growth phenotypes in ASD provides a useful framework for understanding how diverse genetic and environmental factors can converge onto common pathophysiological processes. Evidence from both syndromic and non-syndromic ASD suggests that conditions currently classified under the autism spectrum may fundamentally differ by underlying pro- or anti-growth abnormalities in key biochemical pathways, giving rise to either excessive or reduced synaptic connectivity in affected brain regions [34]. This classification approach has the potential not only to aid research efforts but also to ultimately facilitate early diagnosis and direct appropriate therapeutic interventions.
Experimental Methodologies and Research Approaches
The investigation of gut-brain axis and neuroimmune mechanisms in ASD employs diverse methodological approaches spanning molecular biology, systems neuroscience, and clinical research. Below, we detail key experimental protocols that have advanced understanding of this complex interplay.
Functional Brain Connectivity Analysis in ASD
Objective: To identify differential patterns of functional connectedness between typically developed (TD) individuals and ASD subjects across different developmental stages using contrast subgraph analysis [35].
Protocol Details:
- Participant Selection: Include 57 males with ASD (15 children, 42 adolescents) and 80 typically developed males (17 children, 63 adolescents) matched for age and intelligence where possible [35].
- fMRI Data Acquisition: Acquire resting-state fMRI data using standardized protocols (e.g., ABIDE dataset parameters: TR=2.0-2.5s, TE=30ms, voxel size=3×3×3mm³) [35].
- Functional Connectivity Matrices: Compute standard functional connectivity matrices from preprocessed timeseries using Pearson's correlation coefficient between regional time courses [35].
- Network Sparsification: Sparsify correlation matrices using SCOLA algorithm to obtain individual sparse weighted networks with densities consistent with standard sparsification methods [35].
- Summary Graph Construction: Combine functional networks within each group (ASD vs. TD) into a single summary graph representing common connectivity patterns [35].
- Difference Graph Calculation: Create a difference graph where edge weights equal the difference between summary graph weights of the two groups [35].
- Contrast Subgraph Extraction: Solve optimization problem on the difference graph to identify the set of ROIs that maximizes density difference between groups using bootstrapping for robustness [35].
- Statistical Validation: Apply Frequent Itemset Mining to select statistically significant overrepresented node sets from candidate contrast subgraphs [35].
- Classification Validation: Validate discriminative power using linear SVM classification based on contrast subgraph connectivity features [35].
Key Applications: This approach has revealed significantly larger connectivity among occipital cortex regions and between the left precuneus and superior parietal gyrus in ASD subjects, alongside reduced connectivity in superior frontal gyrus and temporal lobe regions, reconciling previous conflicting reports of both hyper- and hypo-connectivity in ASD [35].
Gut Microbiome-Metabolome Profiling in ASD
Objective: To comprehensively characterize alterations in the gut microbiome and associated neuroactive metabolites in children with ASD and examine their relationship to brain activity and behavior [32].
Protocol Details:
- Participant Recruitment: Include 84 children and teenagers ages 8-17, with half meeting diagnostic criteria for ASD and half being neurotypical controls [32].
- Stool Sample Collection: Collect fresh stool samples using standardized collection kits, immediately freeze at -80°C, and maintain cold chain during transport [32].
- Microbiome Analysis: Extract microbial DNA using commercial kits (e.g., QIAamp PowerFecal Pro DNA Kit), amplify 16S rRNA gene regions (V3-V4), sequence on Illumina platform, and process using QIIME2 or similar pipeline [32].
- Metabolomic Profiling: Perform liquid chromatography-mass spectrometry (LC-MS) on stool samples to quantify neuroactive metabolites including short-chain fatty acids, tryptophan-kynurenine pathway metabolites, and bacterial neuroactives [32].
- Neuroimaging Acquisition: Conduct functional and structural brain scans (resting-state fMRI, T1-weighted structural) using standardized protocols across all participants [32].
- Behavioral Assessment: Administer comprehensive behavioral batteries including ADOS-2, SRS-2, and related instruments to quantify ASD symptom severity [32].
- Integrative Statistical Analysis: Employ multivariate methods (canonical correlation analysis, partial least squares regression) to identify associations between microbial taxa, metabolite levels, brain activity patterns, and behavioral measures [32].
Key Findings: This approach has demonstrated that children with ASD have significantly decreased levels of gut-derived neuroactive metabolites, particularly in the kynurenine pathway, and that these metabolite alterations correlate with changes in task-based brain activity and increased severity of ASD symptoms [32].
Pathway Network Analysis of ASD-Associated Genes
Objective: To systematically characterize gene ontologies, pathways, and functional linkages in the large set of genes associated with autism spectrum disorders [33].
Protocol Details:
- Gene List Curation: Download ASD-associated genes from SFARI Gene Human Gene Module (667 genes as of 2014, currently >1,000 genes) [33] [28].
- Gene Set Enrichment Analysis: Perform enrichment analysis using Molecular Signatures Database (MSigDB) with Kyoto Encyclopedia of Genes and Genomes (KEGG) Pathway Database and Gene Ontology (GO) collections [33].
- Overlap Computation: Apply hypergeometric distribution to examine overlaps between SFARI genes and KEGG gene sets using "Compute Overlaps" tool from MSigDB [33].
- Redundancy Control: Use ReCiPa algorithm to minimize impact of redundancy among enriched gene sets by merging highly overlapped pathways (Max=0.85, Min=0.10) [33].
- Pathway-Pathway Interaction Mapping: Determine functional interactions between pathways by tabulating instances where one pathway appears in the map of another pathway based on KEGG documentation [33].
- Network Visualization and Analysis: Generate pathway network diagrams and calculate interaction metrics to identify highly connected hub pathways with central importance in ASD pathophysiology [33].
Key Applications: This methodology has identified calcium signaling pathway and neuroactive ligand-receptor interaction as the most enriched pathways in ASD, revealed calcium signaling and MAPK signaling as interactive hubs, and identified the process "calcium-PKC-Ras-Raf-MAPK/ERK" as a major contributor to ASD pathophysiology [33].
Table 4: The Scientist's Toolkit: Essential Research Reagents and Platforms
| Research Tool Category | Specific Examples | Primary Applications | Key Considerations |
|---|---|---|---|
| Genomic Resources | SFARI Gene Database, MSSNG WGS Database, AUT10K | Gene discovery, Pathway analysis, Genetic stratification | Sample size, Ethnic diversity, Phenotypic depth |
| Microbiome Tools | 16S rRNA sequencing (Illumina), Shotgun metagenomics, QIIME2 pipeline | Microbial community profiling, Functional potential assessment | Contamination control, Batch effects, Computational resources |
| Metabolomic Platforms | LC-MS/MS, GC-MS, NMR spectroscopy | Targeted/untargeted metabolite profiling, Metabolic pathway analysis | Standardization, Sensitivity, Database completeness |
| Neuroimaging Resources | ABIDE database, resting-state fMRI protocols, DTI sequences | Brain connectivity mapping, Structural analysis, Network neuroscience | Motion artifacts, Site effects, Analytical pipeline variability |
| Immune Assays | Multiplex cytokine arrays, Flow cytometry panels, ELISA kits | Cytokine profiling, Immune cell characterization, Autoantibody detection | Sample stability, Dynamic range, Cross-reactivity |
| Animal Models | Maternal immune activation, Genetic models (e.g., Shank3, BTBR), Germ-free mice | Mechanistic studies, Therapeutic testing, Microbiome manipulations | Species differences, Environmental controls, Behavioral relevance |
The investigation of gut-brain axis and neuroimmune mechanisms in ASD has evolved from isolated observations to an integrated framework recognizing the complex, multidirectional interactions between genetic susceptibility, microbial communities, immune function, and neural development. The evidence reviewed demonstrates that gut dysbiosis, characterized by altered microbial composition and function, interacts with host immune dysregulation to create a systemic and central nervous system environment that disrupts typical neurodevelopmental trajectories. These disruptions manifest at multiple levels, from molecular signaling pathways to neural circuit organization, ultimately contributing to the behavioral phenotype recognized as ASD.
Several key principles emerge from this synthesis of current research. First, the considerable heterogeneity of ASD likely reflects not only diverse genetic causes but also variations in the specific patterns of gut-immune-brain dysfunction. Second, the developmental timing of these disruptions appears crucial, with prenatal and early postnatal periods representing particularly vulnerable windows for interventions. Third, the bidirectional nature of gut-brain communication means that interventions targeting any single component of this system may have cascading effects throughout the entire network.
Future research directions should prioritize:
- Longitudinal studies examining the developmental trajectory of gut-immune-brain interactions from infancy through childhood, ideally beginning in prenatal periods.
- Mechanistic investigations using animal models and in vitro systems to elucidate precise molecular pathways linking specific microbial products to immune activation and neural changes.
- Intervention trials targeting the gut microbiome (e.g., probiotics, prebiotics, fecal microbiota transplantation) and immune system (e.g., anti-inflammatory approaches) with careful monitoring of neural and behavioral outcomes.
- Personalized medicine approaches recognizing that different ASD subgroups may require distinct therapeutic strategies based on their specific pattern of gut and immune dysfunction.
- Integration of multi-omics data combining genomic, microbiomic, metabolomic, immunologic, and neuroimaging data to develop comprehensive biomarkers and treatment response predictors.
The reconceptualization of ASD as a disorder involving integrated gut-immune-brain systems opens promising new avenues for understanding disease mechanisms, developing objective biomarkers, and creating novel therapeutic strategies that extend beyond traditional neurological approaches. As research in this area continues to advance, it holds the potential to transform how we diagnose, classify, and treat autism spectrum disorders.
Advanced Methodologies: Computational Biology, Omics, and Model Systems in Autism Research
The pursuit of understanding autism spectrum disorder (ASD) pathogenesis presents a formidable challenge due to its immense phenotypic heterogeneity and complex genetic architecture. Traditional "trait-centric" approaches, which analyze individual symptoms in isolation, have failed to capture the integrated clinical reality of autistic individuals. Person-centered computational modeling represents a paradigm shift that addresses this limitation by maintaining the holistic phenotypic profile of each individual throughout analysis. This approach has revealed biologically distinct ASD subtypes with unique genetic correlates, developmental trajectories, and clinical manifestations, fundamentally advancing our understanding of the biochemical pathways underlying autism pathogenesis.
The integration of broad phenotypic data with genotypic information through advanced computational frameworks has enabled researchers to move beyond symptom-level associations to identify coherent biological narratives. By leveraging generative mixture modeling and other machine learning techniques on large-scale datasets such as the SPARK cohort (comprising over 5,000 autistic individuals with matched phenotypic and genetic data), researchers can now decompose phenotypic heterogeneity into clinically meaningful classes with distinct pathway disruptions [4] [2]. This technical guide provides methodologies and frameworks for implementing person-centered computational approaches to elucidate the biochemical basis of complex neurodevelopmental conditions.
Core Methodological Framework
Data Acquisition and Preprocessing
The foundation of robust person-centered modeling lies in comprehensive data acquisition. Researchers should collect extensive phenotypic and genotypic data from large, well-characterized cohorts. The SPARK cohort exemplifies this approach with detailed phenotypic information from 5,392 autistic individuals [2].
Phenotypic Data Collection:
- Utilize standardized diagnostic questionnaires including Social Communication Questionnaire-Lifetime (SCQ), Repetitive Behavior Scale-Revised (RBS-R), and Child Behavior Checklist (CBCL)
- Incorporate developmental history forms focusing on milestone achievement
- Collect medical history of co-occurring conditions (ADHD, anxiety disorders, etc.)
- Document intervention histories (medications, therapies, counseling)
Genotypic Data Processing:
- Perform whole exome or genome sequencing to identify rare and common variants
- Annotate variants using population databases and prediction algorithms
- Calculate polygenic risk scores for relevant neuropsychiatric traits
- Identify de novo and rare inherited variants through family-based sequencing
Data Integration Framework: The integration of heterogeneous data types requires specialized preprocessing. Continuous variables should be Z-score normalized, while categorical and binary variables require one-hot encoding. Missing data imputation should be performed using multivariate imputation by chained equations (MICE) to preserve data structure and relationships.
Generative Finite Mixture Modeling (GFMM)
The core analytical approach for person-centered modeling employs generative finite mixture models to identify latent classes within heterogeneous populations. This method accommodates mixed data types (continuous, binary, categorical) without requiring unrealistic distributional assumptions [2].
Model Specification: Let ( X = {X1, X2, ..., X_n} ) represent the mixed-type data for n individuals. The GFMM assumes that the data are generated from a mixture of K multivariate distributions:
[ P(Xi|\Theta) = \sum{k=1}^K \pik fk(Xi|\thetak) ]
where ( \pik ) represents the mixing proportion for class k (( \sum{k=1}^K \pik = 1 )), and ( fk(\cdot|\thetak) ) is the class-specific density function with parameters ( \thetak ).
Implementation Protocol:
- Feature Selection: Identify 239 item-level and composite phenotype features across seven categories: limited social communication, restricted/repetitive behavior, attention deficit, disruptive behavior, anxiety/mood symptoms, developmental delay, and self-injury [2]
- Model Training: Train GFMM with 2-10 latent classes using the Expectation-Maximization (EM) algorithm
- Class Selection: Determine optimal class number (K=4) using Bayesian Information Criterion (BIC), validation log likelihood, and clinical interpretability
- Validation: Assess model stability through bootstrap resampling and perturbation testing
- Replication: Apply trained model to independent cohort (Simons Simplex Collection, n=861) to validate class structure
Computational Requirements:
- High-performance computing cluster with minimum 64GB RAM
- R Statistical Environment with mixtools, clustMD, and PseudoP packages
- Parallel processing capabilities for EM algorithm implementation
Experimental Results and Biological Validation
Phenotypically Derived Autism Classes
Application of the GFMM framework to the SPARK cohort revealed four distinct phenotypic classes with characteristic profiles [4] [36] [2]:
Table 1: Characteristic Profiles of Autism Subtypes Identified Through Person-Centered Modeling
| Class Name | Prevalence | Core Phenotypic Features | Co-occurring Conditions | Developmental Trajectory |
|---|---|---|---|---|
| Social & Behavioral Challenges | 37% | Prominent social difficulties, repetitive behaviors, emotional dysregulation | High rates of ADHD (FE=2.36), anxiety (FE=1.65), depression | Typical milestone achievement; later diagnosis (6.2±3.1 years) |
| Mixed ASD with Developmental Delay | 19% | Variable social/behavioral scores with significant developmental delays | Language delay (FE=8.8), intellectual disability (FE=20.0) | Early developmental delays; diagnosis by 3.4±1.8 years |
| Moderate Challenges | 34% | Milder expression across all phenotypic domains | Lower rates of co-occurring psychiatric conditions | Typical milestone achievement; intermediate diagnosis age |
| Broadly Affected | 10% | Severe impairments across all phenotypic categories | Multiple co-occurring conditions including motor disorders | Significant developmental delays; earliest diagnosis (2.8±1.2 years) |
These classes demonstrated significant differences in external validation measures including medical diagnoses, intervention requirements, and developmental histories, confirming their clinical relevance [2].
Genetic Correlates of Phenotypic Classes
Following phenotypic classification, genotypic analysis revealed distinct genetic architectures underlying each class, supporting their biological validity [36] [2]:
Table 2: Genetic Profiles Associated with Autism Subtypes
| Class Name | De Novo Mutation Burden | Rare Inherited Variants | Key Biological Pathways | Developmental Timing |
|---|---|---|---|---|
| Social & Behavioral Challenges | Moderate | Lower burden | Synaptic transmission, neuronal communication | Postnatal gene expression peak |
| Mixed ASD with Developmental Delay | Lower | Significant enrichment | Chromatin remodeling, Wnt signaling | Prenatal gene expression peak |
| Moderate Challenges | Lower | Moderate burden | Mixed pathway involvement | Variable developmental timing |
| Broadly Affected | Highest burden | Moderate burden | Chromatin remodeling, transcriptional regulation | Prenatal and early postnatal |
Remarkably, the analysis revealed minimal overlap in disrupted biological pathways between classes, with each subtype exhibiting distinct pathway enrichment patterns [4] [2]. Furthermore, the developmental timing of gene expression differed significantly between classes, with the Social/Behavioral class showing enrichment for genes active postnatally, while the Mixed ASD with Developmental Delay class was associated with prenatal gene expression peaks [36].
Visualization of Computational Workflow
The following diagram illustrates the complete experimental workflow for person-centered computational modeling, from data integration through biological validation:
Pathway-Specific Biochemical Implications
Person-centered modeling has revealed distinct biochemical pathway disruptions across autism subtypes, with profound implications for understanding pathogenesis and developing targeted interventions.
Redox System Dysfunction
Emerging evidence situates redox system dysfunction as a central hub in autism pathophysiology, progressing through three temporal stages [21]:
- Primary redox dysfunction manifesting as alterations in metabolic, signaling, and defense pathways
- Functional derailment of cellular compartments including mitochondrial and peroxisomal deficits
- Neurodevelopmental alterations including impaired neurotransmission, synaptic dysfunction, and abnormal plasticity
This framework connects dispersed biochemical evidence into a coherent model that spans from molecular disruptions to clinical manifestations, resonating with the ecological principles of the holobiont and One Health framework [21].
Neurotransmitter System Alterations
Computational modeling of four key neurotransmitter systems has revealed class-specific alterations [37]:
Serotonergic System:
- Altered development of serotonergic circuitry affecting mood, cognition, and gastrointestinal function
- Differential expression of serotonin transporters and receptors across classes
Dopaminergic System:
- Reward processing abnormalities linked to social motivation deficits
- Class-specific alterations in dopamine signaling pathways
Glutamatergic/GABAergic Systems:
- Excitation/inhibition imbalance contributing to sensory processing differences
- Differential expression of glutamate decarboxylase and GABA receptors
These neurotransmitter alterations represent promising targets for class-specific pharmacological interventions.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Person-Centered Computational Modeling
| Reagent/Resource | Function | Specifications | Application in Person-Centered Modeling |
|---|---|---|---|
| SPARK Cohort Data | Primary dataset | 5,392 individuals with phenotypic & genetic data | Training and validation of classification models |
| Simons Simplex Collection | Independent replication cohort | 861 deeply phenotyped individuals | Model generalizability testing |
| GFMM Software Package | Implementation of mixture modeling | R mixtools package with custom extensions | Identification of latent phenotypic classes |
| Exomiser | Variant prioritization | v13.0.0 with phenotype integration | Genotype-phenotype correlation analysis |
| NEURON Simulation Environment | Biophysically detailed modeling | v8.0 with Python interface | Simulation of neuronal network alterations |
| Human Phenotype Ontology | Phenotypic standardization | HPO v2024 with disease annotations | Semantic similarity calculations |
| ACMG Guidelines | Variant interpretation | 2015 standards with 2020 updates | Pathogenicity assessment of identified variants |
| SynGO Knowledgebase | Synaptic gene annotation | v2.0 with cellular component enrichment | Pathway analysis of class-specific gene sets |
Discussion and Future Directions
Person-centered computational modeling represents a transformative approach to understanding complex neurodevelopmental conditions like autism. By maintaining the integrity of individual phenotypic profiles throughout analysis, this methodology has revealed biologically distinct autism subtypes with unique genetic correlates, developmental trajectories, and clinical manifestations.
The identification of these subtypes enables researchers to formulate specific mechanistic hypotheses about autism pathogenesis. For instance, the discovery that genes associated with the Social/Behavioral Challenges subtype peak in expression during postnatal development, while those linked to the Mixed ASD with Developmental Delay subtype show prenatal expression peaks, suggests fundamentally different developmental origins for these conditions [36]. This temporal mapping of genetic influences onto clinical presentations represents a major advance in neurodevelopmental disorder research.
Future applications of this approach should expand to include additional data modalities such as neuroimaging, transcriptomics, and metabolomics. Incorporating the non-coding genome, which constitutes over 98% of the genome but remains understudied in autism, represents another critical frontier [4]. Additionally, longitudinal modeling of class trajectories across the lifespan will provide crucial insights into developmental progressions and inform timing of interventions.
The person-centered computational framework described herein extends beyond autism to offer a powerful approach for deconstructing heterogeneity in other complex neuropsychiatric conditions. By integrating deep phenotypic characterization with genomic data through advanced computational methods, researchers can advance toward precision medicine approaches that respect biological reality and clinical complexity.
An In-Depth Technical Guide
Thesis Context: This whitepaper frames the utilization of large-scale cohorts within the broader thesis that autism spectrum disorder (ASD) pathogenesis arises from the disruption of distinct, yet interconnected, biochemical and developmental pathways. The integration of deep phenotyping with multi-omics data is critical for deconvolving this heterogeneity, mapping phenotypic clusters to specific genetic programs and environmental interactions, and ultimately informing targeted therapeutic strategies [4] [2] [38].
The complexity of ASD necessitates research at an unprecedented scale. Two synergistic initiatives exemplify this approach: the Simons Foundation Powering Autism Research (SPARK) study and the National Institutes of Health (NIH) Autism Data Science Initiative (ADSI).
SPARK is the world's largest autism research study, with over 157,000 autistic individuals and 380,000 total participants as of 2025 [39]. Its core design integrates remote recruitment, broad phenotypic data collection via online questionnaires, and centralized genomic analysis (whole-exome sequencing and genotyping) from saliva samples [40]. A foundational principle is the return of individual genetic results to participants, creating a re-contactable cohort for longitudinal and subtype-specific research [40] [39].
The NIH ADSI, launched in 2025, is a $50 million effort that harnesses existing large datasets—including SPARK—to investigate gene-environment interactions (GxE) and drivers of rising ASD prevalence [41] [38]. Its exposomics approach comprehensively studies environmental, medical, and lifestyle factors in combination with genetics [38]. The initiative funds 13 projects, including two dedicated to replication and validation, ensuring robust and reproducible findings [41].
Key Insights from Cohort-Based Research
Data-Driven Phenotypic and Genetic Subtyping
A landmark analysis of SPARK data (n=5,392) used a general finite mixture model (GFMM) to adopt a "person-centered" approach, analyzing over 230 phenotypic features per individual [4] [2]. This identified four clinically and biologically distinct subtypes, summarized in Table 1.
Table 1: Phenotypic and Genetic Subtypes of Autism Identified in SPARK
| Subtype | Approx. Prevalence | Core Phenotypic Profile | Distinct Genetic & Biological Features |
|---|---|---|---|
| Social/Behavioral Challenges | 37% | Core ASD traits, multiple co-occurring conditions (ADHD, anxiety, depression), no developmental delays [4] [2]. | Impacted genes active postnatally; strong polygenic overlap with ADHD/mental health conditions [4] [3] [2]. |
| Mixed ASD with Developmental Delay (DD) | 19% | Developmental delays, core ASD traits, but low co-occurring psychiatric conditions [4] [3]. | Highest burden of rare inherited variants; impacted genes active prenatally [3] [2]. |
| Moderate Challenges | 34% | Milder expression of core ASD traits, typically no co-occurring psychiatric conditions or developmental delays [4] [3]. | – |
| Broadly Affected | 10% | Severe, widespread challenges including core ASD traits, DD, and multiple co-occurring conditions [4] [2]. | Highest proportion of damaging de novo mutations [3]. |
Critically, each subtype was linked to non-overlapping biological pathways (e.g., neuronal action potentials, chromatin organization) [4], providing a direct link between cohort-scale data and testable hypotheses about distinct biochemical pathways in pathogenesis.
Developmental Trajectories and Polygenic Architecture
Independent research using longitudinal birth cohorts complements SPARK's findings by linking developmental trajectories to genetics. Studies identify two socio-behavioral trajectories: "early childhood emergent" and "late childhood emergent," which are strongly associated with earlier vs. later age of ASD diagnosis, respectively [12].
Furthermore, the polygenic architecture of ASD can be decomposed into two genetically correlated factors (r_g = 0.38) [12]:
- Factor 1: Associated with earlier diagnosis, lower early childhood social-communication ability, and moderate genetic correlation with ADHD/mental health conditions.
- Factor 2: Associated with later diagnosis, increased adolescent difficulties, and high genetic correlation with ADHD/mental health conditions.
This evidence supports a "developmental model" of ASD with distinct polygenic etiologies, challenging a unitary model [12].
The Gene-Environment Interaction Framework
The ADSI explicitly tackles the interplay between biochemical pathways and environmental exposures. Funded projects employ diverse methodologies, as summarized in Table 2, to dissect GxE contributions.
Table 2: Selected ADSI Project Methodologies and Targets
| Project Focus | Primary Datasets | Core Methodology | Target Pathways/Exposures |
|---|---|---|---|
| Causal Inference for Prevalence | SEED, EHRs [41] | Causal inference models | Parental age, other demographic factors |
| Adult Outcomes & Quality of Life | SPARK, ACE cohorts [41] | Longitudinal survey analysis | Services, community participation, mental health |
| Prenatal Diet & Metabolism | ECHO Program [41] | Epidemiology & metabolomics | Maternal diet, pesticides, metabolic health |
| Geocoded Environmental Exposure | CHOP EHR (n~104,000) [41] | Risk prediction modeling | Air/water quality, poverty, policy changes |
| Gene-Environment in Organoids | IBIS stem cell lines [41] | scRNA-seq on exposed organoids | Hydrocortisone, PFAS, pesticides, heavy metals |
| Exposome-Wide Analysis | EARLI, SEED [41] | High-resolution metabolomics | Thousands of environmental chemicals |
Detailed Experimental Protocols
Protocol: Phenotypic Decomposition via General Finite Mixture Modeling (GFMM)
Objective: To identify latent classes of individuals with shared phenotypic profiles from heterogeneous data types.
Input Data:
- Cohort: 5,392 autistic individuals from SPARK.
- Features: 239 item-level and composite variables from validated instruments (SCQ, RBS-R, CBCL, developmental history) representing continuous, binary, and categorical data types [2].
Procedure:
- Data Integration: No pre-aggregation of traits. The model treats each phenotypic feature according to its statistical distribution.
- Model Training: Fit multiple GFMMs with 2 to 10 latent classes. The GFMM calculates a probability distribution for each feature within each putative class and a likelihood for each individual belonging to each class.
- Model Selection: The optimal number of classes (four) was determined by balancing:
- Statistical fit indices (Bayesian Information Criterion, validation log-likelihood).
- Clinical interpretability and phenotypic separation assessed by expert clinicians.
- Validation & Replication:
Protocol: Identifying Developmental Trajectories via Growth Mixture Modeling
Source: [12]
Objective: To model longitudinal socioemotional/behavioral trajectories and test their association with age of diagnosis.
Input Data:
- Cohorts: Longitudinal birth cohorts (e.g., Millennium Cohort Study).
- Measures: Repeated measures of the Strengths and Difficulties Questionnaire (SDQ) total difficulties and subscale scores across childhood and adolescence in autistic individuals.
- Outcome: Age at first parent-reported ASD diagnosis.
Procedure:
- Trajectory Modeling: Apply growth mixture models to SDQ scores to identify latent trajectory classes without a priori grouping.
- Class Definition: Across cohorts, a two-trajectory model was optimal:
- Class A (Early Childhood Emergent): High difficulties in early childhood that remain stable.
- Class B (Late Childhood Emergent): Low early difficulties that increase in late childhood/adolescence.
- Association Testing: Use chi-square tests to assess if trajectory class membership is associated with earlier vs. later age of diagnosis.
- Variance Analysis: Employ multiple regression to quantify the variance in diagnosis age explained by trajectory class versus sociodemographic factors.
Protocol:In VitroGene-Environment Interaction Modeling
Source: [41]
Objective: To model GxE effects on neurodevelopmental pathways using a controlled stem cell model.
Input Biological Material:
- 115 induced pluripotent stem cell (iPSC) lines derived from the Infant Brain Imaging Study (IBIS) cohort, providing diverse genetic backgrounds.
Procedure:
- Organoid Generation: Differentiate iPSCs into 3D cerebral organoids.
- Environmental Exposure: Expose organoids to selected compounds at physiologically relevant doses (e.g., hydrocortisone, PFAS, pesticides).
- Molecular Phenotyping: Perform single-cell RNA sequencing on exposed vs. control organoids.
- Data Integration & Analysis:
- Identify differentially expressed genes and perturbed pathways.
- Test for interaction effects between specific genetic variants (from donor genotypes) and exposure responses.
- Cross-reference findings with epidemiological data from human cohorts.
Visualization of Core Concepts and Workflows
Diagram 1: SPARK Phenotypic & Genetic Decomposition Workflow
Diagram 2: ADSI Gene-Environment Interaction Framework
Table 3: Key Reagent Solutions for Autism Cohort & Pathway Research
| Resource | Description & Function in Research |
|---|---|
| SPARK Cohort Dataset | The foundational resource providing linked deep phenotyping and genomic data for >150k autistic individuals, enabling discovery and validation of subtypes [40] [39]. |
| ADSI Project Data Repositories | Consolidated access to diverse datasets (e.g., ECHO, SEED, ABCD, geocoded EHR) for exposomics and GxE analysis [41] [38]. |
| Validated Phenotypic Batteries (SCQ, RBS-R, CBCL) | Standardized questionnaires essential for capturing the heterogeneous trait profiles required for person-centered modeling [2]. |
| Global Screening Array-24 v.1.0 | Genotyping array optimized for diverse cohorts, used in SPARK for common variant analysis and CNV detection [40]. |
| Whole-Exome Sequencing (WES) Data | Critical for identifying rare coding variants (de novo and inherited) associated with specific ASD subtypes and pathways [40] [2]. |
| iPSC Lines from Characterized Cohorts (e.g., IBIS) | Enable functional validation of GxE findings in a controlled, human cellular model, bridging epidemiology and molecular biology [41]. |
| Cerebral Organoid Differentiation Protocols | 3D in vitro models for studying the impact of genetic variants and environmental exposures on early neurodevelopmental pathways [41]. |
| General Finite Mixture Modeling (GFMM) Software | Computational tools (e.g., in R/Python) for implementing the person-centered, integrative statistical models key to subtyping [4] [2]. |
| High-Resolution Metabolomics Platforms | Technologies for mapping the internal exposome and linking chemical exposures to metabolic pathway perturbations [41]. |
The synergy between large-scale observational cohorts like SPARK and focused, mechanism-driving initiatives like the ADSI represents a paradigm shift in autism research. By moving from a trait-centric to a person-centered, pathway-focused approach, researchers can now stratify ASD into biologically coherent subtypes. This stratification is the critical first step towards:
- Precision Medicine: Tailoring pharmacological and behavioral interventions based on an individual's underlying pathway disruption.
- Prevention Strategies: Identifying modifiable environmental risk factors that interact with specific genetic backgrounds.
- Target Discovery: Prioritizing biochemical pathways—such as chromatin remodeling, synaptic function, or specific prenatal/postnatal signaling cascades—for novel therapeutic development.
Future work must expand diversity in cohorts, integrate proteomic and epigenomic data layers, and leverage the defined subtypes and GxE models for functional screening in cellular and animal systems. The ultimate goal is to translate insights from vast datasets into precise biochemical hypotheses that can be tested and remediated, transforming the landscape of autism therapeutics.
The process of drug discovery begins with the identification of a disease-modifying target, a critical step that has been transformed by the advent of high-throughput omics technologies. These approaches allow for quantitative measurements of numerous putative targets—including DNA, RNA, proteins, and metabolites—generating unprecedented volumes of data for systematic target evaluation [42]. Omics-driven strategies provide a powerful framework for elucidating complex disease mechanisms and identifying therapeutic intervention points, particularly for complex polygenic disorders like autism spectrum disorder (ASD) where traditional "one gene–one disease" paradigms have proven insufficient [42].
In the context of ASD pathogenesis, omics technologies have revealed profound insights into the interconnected biological systems involved. ASD is no longer viewed solely as a neurological condition but rather as a multi-system disorder involving intricate interactions between genetics, immunity, gut microbiota, and metabolism [43] [18]. Recent multi-omics studies have demonstrated that genetic variants associated with ASD exert cross-tissue regulatory effects that coordinate dynamic balance between brain neural development, blood-immune responses, and gut microbiota interactions through molecular networks [43]. This systemic perspective is essential for understanding ASD pathogenesis and identifying effective therapeutic targets.
The integration of diverse omics datasets creates a more comprehensive understanding of disease pathophysiology than any single approach could provide. As discussed in this technical guide, omics-based elucidation of drug targets involves sophisticated computational and experimental methodologies that leverage genomics, transcriptomics, metabolomics, and network analysis to map the complex biochemical networks underlying ASD and identify key nodal points for therapeutic intervention.
Technology Platforms and Their Applications
Omics technologies encompass multiple molecular profiling domains, each contributing unique insights to the drug target discovery pipeline. Genomics, including genome-wide association studies (GWAS) and whole genome sequencing, identifies genetic variants associated with disease risk and progression. Transcriptomics measures gene expression patterns, revealing how genetic variants influence RNA expression across tissues and developmental stages. Proteomics characterizes protein expression, post-translational modifications, and interactions, while metabolomics profiles small-molecule metabolites that represent functional outputs of cellular processes [42].
For ASD research, large-scale bio-collections have been instrumental in facilitating omics discoveries. These repositories contain biologically characterized samples from individuals with ASD and controls, enabling generation of clinical and scientific data on a scale necessary to address the condition's heterogeneity [44]. The Autism Genetic Resource Exchange (AGRE), for instance, has contributed to identifying numerous ASD candidate genes including CNTNAP2, MET, GABRB3, and UBE3A through genomic studies [44].
Table 1: Key Omics Technologies for ASD Drug Target Discovery
| Omics Domain | Primary Technologies | Data Outputs | ASD Applications |
|---|---|---|---|
| Genomics | GWAS, WGS, WES | SNPs, CNVs, structural variants | Identification of ~134 risk genes and numerous regulatory variants [18] [45] |
| Transcriptomics | RNA-seq, microarrays | Gene expression levels, alternative splicing | Revealed immune gene upregulation and synaptic gene downregulation [46] |
| Epigenomics | ChIP-seq, bisulfite sequencing | DNA methylation, histone modifications | mQTL analysis revealing epigenetic regulation of gene expression [43] |
| Metabolomics | LC/MS, GC/MS, NMR | Metabolite concentrations, metabolic pathways | Identified purine metabolism alterations and lipid dysregulation [18] |
| Microbiomics | 16S rRNA sequencing, metagenomics | Microbial composition, functional potential | Revealed gut microbiota-immune-brain axis interactions [43] |
Data Integration and Computational Platforms
The volume and complexity of omics data necessitate advanced computational platforms for integration and analysis. More than 30 drug target discovery (DTD) platforms have been developed to help researchers identify putative targets and pre-evaluate their therapeutic efficacy and potential side effects [42]. These platforms provide information-rich databases and graphical interfaces that integrate multiple data sources, including omics databases and scientific literature, to identify and rank disease-relevant targets.
Successful omics integration requires addressing several computational challenges: the high-dimensional nature of omics data, tissue and context specificity of molecular interactions, and the need to distinguish causal drivers from correlative associations. Methods such as Summary-data-based Mendelian Randomization (SMR) can help identify putative causal genes by testing for associations between genetic variants influencing exposure traits (e.g., gene expression) and outcome traits (e.g., disease status) [43] [45].
Omics Insights into Autism Pathogenesis
Genetic Architecture and Regulatory Networks
ASD exhibits a complex genetic architecture characterized by high heritability (estimated at 64-91%) and significant heterogeneity [43]. While numerous reliable risk loci have been identified through large-scale sequencing studies, no single mutation accounts for more than 1% of ASD cases [43]. This suggests that ASD risk emerges from the combined effects of many common and rare variants acting within biological networks.
Multi-omics studies have revealed that ASD-associated genetic variants are significantly enriched in regulatory regions, particularly those influencing gene expression in brain tissues. A 2023 network analysis identified four genes at the 17q21.31 locus (LINC02210, LRRC37A4P, RP11-259G18.1, and RP11-798G7.6) as putatively causal for ASD in fetal cortical tissue, with LINC02210 also significant in adult cortical tissue [45]. These findings highlight the importance of non-coding RNAs and developmental stage-specific gene regulation in ASD pathogenesis.
Network analysis integrating protein-protein interactions with autism-specific gene regulatory networks has revealed clusters of co-occurring traits associated with ASD. The 17q21.31 locus contributes to neurological traits, while the 3p21.1 locus is linked to cognition and worry-related traits [45]. These pleiotropic networks demonstrate how genetic risk for ASD intersects with other neurodevelopmental and psychiatric conditions.
Metabolic Dysregulation in ASD
Metabolomic studies have revealed consistent alterations in biochemical pathways in individuals with ASD, with implications for both biomarker development and pathophysiological understanding. A 2024 study comparing pre-ASD newborns and 5-year-old children with ASD found that 80% of the metabolic impact in ASD was caused by 14 shared biochemical pathways that led to decreased anti-inflammatory and antioxidant defenses and increased physiologic stress molecules [18].
Notably, the developmental regulation of the purine network emerged as the most significantly altered metabolic system. Hub analysis of the purine network revealed a 17-fold reversal in typically developing children that did not occur in ASD, suggesting a failure of normal metabolic maturation [18]. This finding is particularly significant given the fundamental role of purinergic signaling in the Cell Danger Response (CDR), a universal response to genetic or environmental stress that coordinates metabolic, inflammatory, and neuroendocrine responses [18].
Table 2: Key Metabolic Findings in ASD from Omics Studies
| Metabolic Pathway | Alterations in ASD | Proposed Functional Significance |
|---|---|---|
| Purine Metabolism | Disrupted developmental trajectory; altered eATP signaling | Impacts Cell Danger Response; regulates neuroimmune function and synaptic plasticity [18] |
| Lipid Metabolism | Increased ceramides, cholesterol; altered phospholipids and sphingolipids (63-71% of metabolic impact) | Affects membrane structure, cell signaling, and inflammation [18] |
| Amino Acid Metabolism | Increased phenylalanine, citrulline, threonine, alanine | Potential biomarker profile; indicates oxidative stress and immune activation [46] |
| Antioxidant Defenses | Glutathione pathway alterations | Reduced protection against oxidative stress; linked to gene-gene interactions in ASD [44] [18] |
| Mitochondrial Function | Chronic changes in mitochondrial metabolism | Remodels metabolic network; regulates gene expression and neurodevelopment [18] |
Immune-Metabolic Crosstalk in ASD
Integrated transcriptomic and metabolomic analyses have revealed significant immune system dysregulation in ASD, characterized by upregulation of pro-inflammatory cytokines including IL-1β, IL-6, IFN-γ, and TNF-α [46]. This immune activation correlates with metabolic changes, particularly in amino acid and lipid metabolism, suggesting interconnected immunometabolic mechanisms in ASD pathogenesis.
Weighted Gene Co-expression Network Analysis (WGCNA) of blood transcriptomes from ASD patients has identified key transcription factors driving this immune dysregulation, including RARA, NFKB2, and ETV6 [46]. These factors regulate genes involved in immune responses and pro-inflammatory cytokine production, creating a feed-forward loop of neuroinflammation that may impact brain development and function.
The gut-immune-brain axis represents another critical interface in ASD pathophysiology. Multi-omics studies have revealed that genetic variants in ASD participate in gut microbiota regulation, involving immune pathways such as T cell receptor signaling and neutrophil extracellular trap formation [43]. These findings suggest that genetic risk factors may exert their effects through peripheral systems that subsequently influence brain development and function.
Methodological Framework for Omics-Based Target Discovery
Integrative Analysis of Multi-Omics Data
Diagram 1: Multi-omics data integration workflow for identifying and prioritizing drug targets in complex disorders like ASD.
The workflow for omics-based target discovery begins with the identification of genetic variants through GWAS meta-analysis. This involves integrating data from multiple independent cohorts to enhance statistical power. For example, a recent ASD study combined data from four independent GWAS datasets totaling over 60,000 individuals [43]. Quality control steps include genomic coordinate conversion, allele alignment, and exclusion of single nucleotide polymorphisms (SNPs) with significant frequency differences across studies.
Functional annotation follows variant identification, using approaches such as:
- Polygenic Priority Score (PoPS) analysis to identify genes enriched for associations with ASD
- Expression Quantitative Trait Loci (eQTL) enrichment analysis in brain regions and cell types
- Methylation Quantitative Trait Loci (mQTL) analysis to identify variants influencing epigenetic regulation
Network construction integrates these annotations with additional omics data to map molecular interactions. Protein-protein interaction networks extended from autism-specific gene regulatory networks can identify traits pleiotropic with ASD [45]. For metabolic networks, parameters such as $\dot{V}!$net can reveal differences in network connectivity and identify hub metabolites with central regulatory roles [18].
Causal inference methods, particularly Mendelian Randomization (MR) and Summary-data-based MR (SMR), help distinguish causal relationships from correlative associations by leveraging genetic variants as instrumental variables [43] [45]. These approaches can identify putatively causal genes and pathways by testing whether genetic variants influencing gene expression are also associated with disease risk.
Experimental Protocols for Key Analyses
GWAS Meta-Analysis Protocol
Data Collection and Harmonization: Obtain GWAS summary statistics from multiple independent cohorts. Convert all genomic coordinates to the same build (e.g., hg38) using tools like CrossMap (v0.6.5). Align alleles to a reference panel (e.g., 1000 Genomes Phase 3) using PLINK (v1.9) [43].
Quality Control: Exclude SNPs with significant allele frequency differences across studies (e.g., eAF differences >0.2) and those with poor imputation quality (info score <0.6).
Meta-Analysis: Perform fixed-effects meta-analysis using METAL software with SCHEME STDERR and STDERR SE strategies to weight studies by standard error. Calculate heterogeneity metrics (Cochran's Q and I²); if substantial heterogeneity is detected (Q test P < 0.1 and I² > 50%), apply random-effects models using the DerSimonian-Laird method [43].
Novel Locus Identification: Define novel loci as SNPs located ≥500 kb from previously reported loci on the same chromosome. Perform linkage disequilibrium pruning (r² < 0.001 within 10,000 kb window) to identify independent signals.
Metabolic Network Analysis Protocol
Sample Collection and Preparation: Collect plasma or serum samples following standardized protocols. For neonatal studies, use dried blood spots; for older children, employ fasting blood draws when possible [18].
Metabolomic Profiling: Utilize combined liquid chromatography-mass spectrometry (LC-MS) and gas chromatography-mass spectrometry (GC-MS) platforms to cover a broad range of polar and lipid metabolites. Include quality control samples (pooled reference samples, process blanks) throughout the run sequence.
Data Preprocessing: Apply peak detection, alignment, and integration using platform-specific software. Perform normalization using probabilistic quotient normalization or internal standards. Address missing values using appropriate imputation methods.
Multivariate Statistical Analysis: Conduct Partial Least Squares Discriminant Analysis (PLS-DA) to identify metabolite patterns distinguishing ASD from controls. Calculate Variable Importance in Projection (VIP) scores to identify the most discriminative metabolites.
Pathway and Network Analysis: Aggregate significant metabolites (VIP ≥1.5) into biochemical pathways using KEGG or HMDB annotations. Construct metabolic correlation networks and calculate network parameters (e.g., $\dot{V}!$net) to identify differences in connectivity patterns [18].
Cross-Omics Integration Protocol
Differential Analysis: Identify differentially expressed genes (DEGs) from transcriptomic data using DESeq2 or similar tools, and differentially abundant metabolites (DMs) from metabolomic data using MetaboAnalyst [46].
Functional Annotation: Perform pathway enrichment analysis (KEGG, GO) separately for DEGs and DMs. Identify overlapping pathways across omics layers.
Network Integration: Use Cytoscape to construct integrated networks connecting genetic variants, gene expression changes, and metabolic alterations. Incorporate protein-protein interaction data from STRING database to extend networks [45] [46].
Regulatory Inference: Identify key transcription factors (e.g., RARA, NFKB2) driving observed expression patterns using regulatory network analysis. Validate findings through literature mining and independent datasets.
Biochemical Networks in Autism Pathogenesis
The Gut Microbiota-Immune-Brain Axis
Diagram 2: The gut microbiota-immune-brain axis in ASD, showing key interactions between genetic risk factors and peripheral systems that influence neurodevelopment.
Multi-omics studies have revealed a critical role for the gut microbiota-immune-brain axis in ASD pathogenesis. Genetic variants associated with ASD participate in gut microbiota regulation and influence immune pathways such as T cell receptor signaling and neutrophil extracellular trap formation [43]. These variants can cis-regulate neurodevelopmental genes like HMGN1 and H3C9P or synergistically influence epigenetic methylation modifications to regulate the expression of BRWD1 and ABT1 [43].
The bidirectional nature of this axis is evident from experimental models. For example, defects in the ASD high-risk gene Chd8 can induce abnormal activation of brain microglia while simultaneously causing intestinal immune homeostasis imbalance, manifested as disrupted T and B lymphocyte differentiation and reduced immunoglobulin IgA levels [43]. These findings demonstrate how genetic risk factors can simultaneously impact central nervous and peripheral systems.
Metabolomic studies provide further evidence for this interconnected axis. ASD-associated metabolic changes affect multiple systems, with alterations in purine metabolism, mitochondrial function, and lipid metabolism potentially serving as both biomarkers and functional mediators of pathophysiology [18]. The central role of extracellular ATP (eATP) in purinergic signaling represents a key node connecting these systems, as eATP is a powerful signaling molecule that regulates mitochondria, immune responses, and neural function [18].
Metabolic Network Alterations
Metabolic network analysis has revealed previously unknown phenotypes in ASD, including developmental alterations in network connectivity and organization. In typically developing children, the purine network undergoes a 17-fold reversal during early development, a pattern that is disrupted in ASD [18]. This finding underscores the importance of developmental timing in metabolic processes and suggests that ASD may involve a failure of normal metabolic maturation.
Beyond purine metabolism, multiple biochemical pathways show consistent alterations in ASD. A cross-sectional study of newborns who later developed ASD and 5-year-old children with ASD found that 80% of the metabolic impact was caused by 14 shared biochemical pathways [18]. These shared pathways led to decreased anti-inflammatory and antioxidant defenses and increased physiologic stress molecules like lactate, glycerol, cholesterol, and ceramides.
The lipid metabolism network is particularly affected in ASD, accounting for 63-71% of the total metabolic impact [18]. Within this network, sphingolipids (including sphingomyelins, ceramides, and glycosphingolipids) contribute approximately 25% of the impact, while phospholipids contribute 20-26%. These lipid classes play critical roles in membrane structure, cell signaling, and inflammation, suggesting their alteration may have broad functional consequences.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Omics Studies in ASD
| Category | Specific Tools/Reagents | Application in ASD Research |
|---|---|---|
| Genomic Analysis | PLINK (v1.9), METAL, CrossMap (v0.6.5), biomaRt | GWAS meta-analysis, genomic coordinate conversion, gene annotation [43] |
| Transcriptomics | DESeq2, WGCNA, Cytoscape, STRING database | Differential expression analysis, gene co-expression networks, protein-protein interactions [45] [46] |
| Metabolomics | LC-MS/GC-MS platforms, MetaboAnalyst, CIRCOS | Metabolic profiling, pathway analysis, visualization of metabolic networks [18] |
| Multi-Omics Integration | TwoSampleMR, SMR, CoDeS3D pipeline | Mendelian randomization, causal inference, spatial eQTL analysis [43] [45] |
| Bio-collections | Autism Genetic Resource Exchange (AGRE), GEO datasets | Access to well-characterized ASD samples and associated multi-omics data [44] [46] |
| Network Visualization | Graphviz, Cytoscape, custom R/Python scripts | Diagramming signaling pathways, experimental workflows, logical relationships [45] |
Omics-based approaches have fundamentally transformed our understanding of ASD pathogenesis, revealing it as a multi-system disorder involving complex interactions between genetics, metabolism, immunity, and the gut microbiome. Through integrated analysis of diverse molecular datasets, researchers have identified key biochemical networks and nodal points that represent promising targets for therapeutic intervention.
The future of omics research in ASD will likely focus on several key areas: First, longitudinal studies tracking molecular changes across developmental stages will be essential for understanding the dynamic nature of ASD pathophysiology. Second, increased attention to tissue- and cell-type-specific mechanisms will help resolve the functional consequences of identified molecular alterations. Third, integration of environmental exposure data with multi-omics measurements will provide a more complete understanding of gene-environment interactions in ASD.
From a therapeutic perspective, omics findings are already suggesting novel intervention strategies. The central role of purinergic signaling and the Cell Danger Response indicates potential for targeting eATP signaling pathways [18]. Similarly, the identified immune-metabolic crosstalk suggests opportunities for immunomodulatory approaches. As these strategies move toward clinical application, omics-based patient stratification will be crucial for matching the right therapies to the right patients.
The omics revolution in ASD research demonstrates the power of integrated molecular profiling for elucidating complex disease mechanisms. By continuing to refine these approaches and address remaining challenges—including functional validation of candidate targets and translation of findings into clinical applications—researchers can advance toward the ultimate goal of effective, personalized interventions for autism spectrum disorder.
The quest to elucidate the biochemical pathways underlying Autism Spectrum Disorder (ASD) pathogenesis relies fundamentally on the availability and sophistication of preclinical models. ASD is a complex neurodevelopmental condition characterized by persistent deficits in social communication and interaction, along with restricted, repetitive patterns of behavior, interests, or activities [19]. With a prevalence of 1 in 31 children according to recent CDC data [27] and affecting approximately 1% of the global population [47], ASD presents a significant challenge to neuroscience research and therapeutic development. The disorder's etiology involves intricate interactions between genetic predispositions and environmental factors, leading to alterations in key neurobiological processes including synaptic function, neuronal connectivity, and circuit formation [19] [14].
The field of preclinical modeling has evolved substantially from traditional rodent models to encompass a diverse toolkit including non-rodent organisms, human stem cell-derived systems, and most recently, sophisticated three-dimensional brain organoids and assembloids. This evolution reflects the growing recognition that no single model system can fully capture the complexity of human neurodevelopment or the multifaceted nature of ASD pathophysiology. A reliable preclinical model must demonstrate three key forms of validity: face validity (resemblance to human symptoms), construct validity (similarity to underlying disease mechanisms), and predictive validity (accurate treatment response prediction) [47]. Each model system offers unique advantages and limitations for studying specific aspects of ASD-associated biochemical pathways, from synaptic dysfunction and excitatory/inhibitory imbalance to mitochondrial impairment and neuroimmune interactions.
Traditional Animal Models: From Rodents to Small Organisms
Rodent Models of ASD
Rodent models have been invaluable workhorses in ASD research, providing critical insights into disease mechanisms and potential therapeutic avenues. Their value stems from conserved biological pathways, well-characterized neurotransmitter systems, and behavioral parallels with humans [47]. Genetically engineered rodent models have been particularly instrumental in elucidating the roles of specific ASD-risk genes in circuit formation and function.
Table 1: Key Rodent Models for Studying ASD-Associated Biochemical Pathways
| Model Type | Specific Model/Genes | Key Biochemical & Circuit Alterations | Research Applications |
|---|---|---|---|
| Genetic Models | Syngap1 haploinsufficiency | Disrupted pyramidal cell structural maturation; impaired cortical circuit assembly [47] | Synaptic development, cortical connectivity |
| En2 knockout | Neurobehavioral and neurochemical alterations relevant to ASD [47] | Cerebellar-forebrain circuitry, motor learning | |
| Gabrb3 deficient | Impaired social and exploratory behaviors; cerebellar vermal hypoplasia; attention deficits [47] | GABAergic signaling, inhibitory circuitry | |
| Oxytocin knockout | Altered social approach behaviors; context-dependent phenotypes [47] | Social circuitry, neuropeptide signaling | |
| Mecp2 models (Rett syndrome) | Postnatal forebrain loss mediates behavioral aspects; synaptic dysfunction [47] | Epigenetic regulation, synaptic maturation | |
| Environmental/Chemical Models | Valproic acid (VPA) exposure | Rearranged dendritic morphology in limbic regions; altered exploratory behavior [47] | Neural connectivity, dendritic arborization |
| Maternal immune activation | Altered immune signaling; synaptic dysfunction; circuit miswiring [47] | Neuroimmune interactions, cortical development | |
| Lead exposure | Oxidative damage; sensory processing defects [47] | Redox system dysfunction, sensory circuitry |
Rodent models have enabled detailed investigation of well-defined microcircuits, allowing researchers to dissect the role of specific genes at morphological, physiological, and behavioral levels [47]. However, substantial differences between human and rodent physiology limit the extent to which these models can fully represent human disease pathophysiology. For instance, recent studies have revealed that human astrocytes are not only three times larger but also exhibit more complex morphology and potentially different functional capabilities compared to their rodent counterparts [47].
Non-Rodent Organism Models
Small organism models offer significant advantages for high-throughput screening and rapid genetic manipulation, providing complementary approaches to rodent studies.
Zebrafish models have emerged as particularly valuable tools, offering advantages including high fecundity, transparent embryos, and rapid development that enables real-time monitoring of neurodevelopmental processes [47]. In social neurobiology, zebrafish effectively bridge in vitro studies and mammalian in vivo models [47]. Larval zebrafish exhibit distinct sensorimotor behaviors with well-defined circuitry, making them suitable for high-throughput drug screening. Valproic acid-induced zebrafish models have been used to study ASD-related behavioral and neurodevelopmental alterations [47], with these models demonstrating social behavior deficits and biochemical changes relevant to ASD pathogenesis.
Drosophila melanogaster (fruit fly) models provide a simplified nervous system with limited neurons that facilitates mapping of neural circuits, combined with ease of genetic manipulation [47]. Their short lifespan makes them suitable for studying neurodevelopmental processes across the entire life course. Drosophila models have been particularly valuable for elucidating the role of conserved ASD-risk genes in fundamental processes including neural signaling, synapse formation, and neural circuit assembly.
C. elegans models offer an even simpler system with a completely mapped connectome, transparency for neural imaging, and a short life span ideal for developmental studies [47]. Models such as the neuroligin-deficient mutant exhibit ASD-relevant phenotypes including sensory processing defects and oxidative stress responses, providing insights into conserved molecular pathways disrupted in ASD [47].
Human Cell-Based Models: The Rise of Brain Organoids
Fundamentals of Brain Organoid Technology
The development of brain organoid technology represents a paradigm shift in preclinical modeling of neurodevelopmental disorders. Brain organoids are three-dimensional, self-organizing in vitro culture models derived from human pluripotent stem cells that recapitulate key aspects of early human brain development [48]. By generating diverse cell types, including neurons and glia relevant to specific brain regions, these 3D architectures mimic the complex cellular composition, spatial organization, and cell-cell interactions found in the developing human brain to a degree unattainable in traditional 2D cell cultures [48].
The foundational protocol for brain organoid generation was established in 2013 by Jürgen Knoblich and Madeline Lancaster, who employed Matrigel to simulate the developing brain microenvironment while using a rotating cell culture system to promote uniform distribution of metabolic substances and gas exchange [48]. This approach resulted in the formation of brain organoids containing interconnected functional units resembling the forebrain, choroid plexus, hippocampus, and prefrontal cortex, with cellular composition and tissue architecture similar to the developing fetal brain [48].
Table 2: Brain Organoid Protocols and Their Applications in ASD Research
| Protocol/Lab | Key Features | Advantages for ASD Research | Limitations |
|---|---|---|---|
| Whole-Brain/Unpatterned Organoids (Knoblich/Lancaster) | Relies on cellular self-organization; Embedded in Matrigel; Uses rotating bioreactors [48] | Models interactions between multiple brain regions; No exogenous patterning factors required; Suitable for studying global developmental events [48] | High batch-to-batch variability; Uncontrolled regional composition; Frequent necrotic core formation [48] |
| Region-Specific/Patterned Organoids (Pasca et al.) | Uses small molecule morphogens; Directed differentiation into specific brain regions; Precise control of developmental pathways [48] | High regional consistency and reproducibility; Good cellular purity; Ideal for studying region-specific disorders and circuits [48] | Sacrifices whole-brain complexity; Requires pre-definition of target brain region; Demands precise timing and concentration of morphogens [48] |
| Assembloids (Pasca et al.) | Assembly of organoids from different regions; Models inter-regional connectivity; Studies cell migration and projections [48] | Enables study of long-range neuronal connections; Reveals mechanisms of brain region interactions; Models complex neural circuits relevant to ASD [48] | Higher technical complexity; Assembly efficiency requires optimization; Fusion consistency needs improvement [48] |
| Hi-Q Brain Organoids (Ramani et al.) | Bypasses embryoid body stage; Uses custom uncoated microplates; Precise control of neurosphere size [48] | High reproducibility and consistency; Minimal activation of cellular stress pathways; Supports cryopreservation and large-scale screening [48] | Relatively new protocol; Long-term developmental potential requires further validation [48] |
Experimental Protocol: Generation and Analysis of Forebrain Organoids for ASD Modeling
Phase 1: iPSC Culture and Quality Control
- Maintain human induced pluripotent stem cells (iPSCs) in vitronectin-coated plates using defined culture conditions [49].
- Perform regular karyotype analysis and pluripotency marker validation (OCT4, SOX2, NANOG) to ensure genomic integrity and stem cell quality.
- For ASD modeling, utilize iPSCs from multiple genetically characterized donors, including both healthy controls and individuals with ASD diagnoses [49].
Phase 2: Embryoid Body Formation and Neural Induction
- Dissociate iPSCs to single cells using Accutase enzyme treatment [49].
- Transfer cell suspensions to low-attachment plates to promote 3D embryoid body (EB) formation.
- Culture EBs in neural induction medium supplemented with SMAD inhibitors (dorsomorphin and SB431542) to promote neural ectoderm specification.
- Alternative Hi-Q protocol bypasses EB formation by directly differentiating iPSCs into neurospheres using custom uncoated microplates for improved reproducibility [48].
Phase 3: Brain Organoid Maturation and Patternization
- At approximately day 6, embed developing organoids in Matrigel droplets to provide structural support and microenvironmental cues [48] [49].
- Transfer to rotating bioreactors or orbital shakers to enhance nutrient exchange and reduce necrotic core formation.
- For dorsal forebrain patterning (cortical organoids), maintain in Cortical Differentiation Medium with appropriate morphogens [49].
- Culture for extended periods (60+ days) to allow for the generation of mature neuronal and glial cell types [49].
Phase 4: Organoid Characterization and Analysis
- Perform immunohistochemistry for regional markers (PAX6, SOX1 for progenitors; TBR1, CTIP2 for cortical layers) to validate organoid identity.
- Conduct electrophysiological recordings using multi-electrode arrays to assess neuronal network activity and synchronization [50].
- Utilize single-cell RNA sequencing to characterize cellular diversity and identify aberrant developmental trajectories in ASD-derived organoids.
- Employ morphological analysis to quantify organoid size and structural features, as ASD-derived forebrain organoids often exhibit significantly larger diameters compared to controls [49].
Advanced Organoid Systems: Assembloids and Integrated Circuits
To overcome the limitation of studying isolated brain regions, researchers have developed "assembloids" - complex multi-region organoid assemblies that model interactions between different brain areas [48]. By assembling organoids from different brain regions, this approach simulates more complex neurodevelopmental processes and reveals subtle pathological changes in neurological disorders. Several specialized assembloid systems have been established:
Cortical-striatal assembloids model the connections between cortex and striatum, circuits known to be involved in repetitive behaviors and reward processing that are frequently disrupted in ASD [48]. Cortical-thalamic assembloids enable study of thalamocortical circuits that govern sensory processing and integration, processes often altered in ASD [48]. Midline assembloids model the development of midline brain structures and their connectivity [48].
These assembloid systems have demonstrated that human neurons can extend long-range projections and form functional connections between distinct regions, recapitulating aspects of human brain connectivity that were previously impossible to model in vitro. This capability is particularly valuable for studying ASD, which is increasingly recognized as a disorder of brain connectivity and neural circuit function.
Biochemical Pathways in ASD: Insights from Preclinical Models
Redox System Dysfunction and Mitochondrial Impairment
Recent research has reframed our understanding of oxidative stress in ASD from a simple imbalance between oxidants and antioxidants to a broader concept of redox system dysfunction [21]. This progressive dysfunction unfolds in three stages: primary redox dysfunction manifesting as alterations in metabolic, signaling, and defense pathways; functional derailment of cellular compartments including mitochondrial and peroxisomal deficits; and finally, neurodevelopmental alterations including impaired neurotransmission, synaptic dysfunction, abnormal plasticity, and morphogenetic defects [21].
Preclinical models have been instrumental in characterizing these redox abnormalities. In mercury-induced oxidative damage models in C. elegans, researchers observed sensory processing defects analogous to those seen in ASD [47]. Zebrafish models exposed to environmental toxins have demonstrated similar redox imbalances accompanied by behavioral alterations [47]. Patient-derived organoids have provided human-specific insights into how these redox disruptions affect early brain development, with identified alterations in polyol pathways, protein synthesis, ubiquitination, and chromatin remodeling - all processes linked to synaptic plasticity, cellular signaling, and protein homeostasis [49].
Proton Magnetic Resonance Spectroscopy (¹H-MRS) studies integrated with genetic analysis have revealed significant neurometabolic alterations in ASD patients with specific genetic variants in neurotransmission and synaptic genes [51]. These studies have identified predicted damaging variants in 12 neurotransmission and synaptic genes in ASD individuals, most mapping to genes involved in Gamma-aminobutyric acid (GABA) and glutamate pathways [51].
Key findings from these integrated analyses include significantly lower levels of total creatine (a marker of bioenergetics) and total N-acetyl aspartate (a marker of neuronal metabolism) in ASD patients with genetic alterations in neurotransmission and synaptic genes compared to controls [51]. These metabolic alterations provide a direct link between genetic risk factors and functional brain abnormalities in ASD, particularly affecting the excitatory/inhibitory balance that is crucial for proper information processing in neural circuits.
Extracellular Vesicle-Mediated Pathophysiology
A novel area of research emerging from organoid studies involves the role of extracellular vesicles (EVs) in ASD pathophysiology. EVs, particularly exosomes (40-200 nm nanoparticles), play critical roles in intercellular communication within the brain by transferring proteins, RNAs, and other bioactive molecules between cells [49]. Recent studies utilizing patient-derived cortical organoid models have characterized EVs secreted by human 3D tissue and defined their cargo, revealing substantial differences in both RNA and protein content of ASD-derived EVs compared to healthy controls [49].
These EV alterations point toward disruptions in polyol pathways, protein synthesis, ubiquitination, and chromatin remodeling - all processes linked to synaptic plasticity, cellular signaling, and protein homeostasis [49]. Intriguingly, researchers have identified several known ASD risk genes among the differentially regulated RNAs and proteins in EVs derived from ASD forebrain organoids [49]. This emerging field highlights the potential of exosome-based diagnostics and therapies for ASD, with previous studies demonstrating that treatment of MECP2-knockdown cultures with control exosomes rescued defects in neuronal growth and differentiation [49].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Research Reagent Solutions for Preclinical ASD Modeling
| Category | Specific Reagents/Platforms | Function/Application | Key Features |
|---|---|---|---|
| Stem Cell Culture | Human iPSCs from ASD patients and controls | Foundation for patient-specific modeling | Genetically characterized; multiple lines available [49] |
| Vitronectin-coated plates | iPSC attachment and maintenance | Defined, xeno-free substrate [49] | |
| Accutase enzyme | Gentle cell dissociation | Single-cell suspension for 3D culture [49] | |
| 3D Culture & Patterning | Matrigel | Extracellular matrix simulation | Provides structural support and microenvironmental cues [48] |
| SMAD inhibitors (dorsomorphin, SB431542) | Neural induction | Promotes neural ectoderm specification [48] | |
| Cortical Differentiation Medium | Dorsal forebrain patterning | Specific regional identity [49] | |
| Small molecule morphogens (e.g., WNT agonists/antagonists) | Regional patterning | Precise control of brain region specification [48] | |
| Culture Systems | Rotating bioreactors/orbital shakers | Enhanced nutrient exchange | Reduces necrotic core formation [48] |
| Low-attachment plates | Embryoid body formation | Promotes 3D aggregation [49] | |
| Custom uncoated microplates (Hi-Q protocol) | Controlled neurosphere formation | Improved reproducibility and consistency [48] | |
| Characterization Tools | Multi-electrode arrays (MEAs) | Electrophysiological recording | Network activity and synchronization assessment [50] |
| Nanoparticle tracking analysis (NTA) | EV characterization | Size and concentration measurements [49] | |
| Transmission electron microscopy | EV morphology visualization | Cup/rose-like morphology confirmation [49] | |
| CD9, CD63 antibodies | EV marker validation | Western blot confirmation [49] |
The landscape of preclinical modeling for ASD research has expanded dramatically, evolving from reliance primarily on rodent models to a diversified toolkit encompassing traditional animal models, human stem cell-based systems, and sophisticated 3D organoid and assembloid platforms. Each model system offers unique advantages and addresses specific aspects of ASD pathophysiology, from circuit-level dysfunction in rodent models to human-specific developmental processes in brain organoids.
The integration of findings across these complementary model systems is providing unprecedented insights into the biochemical pathways underlying ASD pathogenesis. Redox system dysfunction, neurometabolic alterations affecting excitation/inhibition balance, and extracellular vesicle-mediated intercellular communication emerge as key mechanisms intersecting with genetic vulnerability and environmental influences. These advances are gradually unraveling the complex interplay between molecular pathways, neural circuit development, and ultimately, the behavioral manifestations of ASD.
As the field continues to progress, the strategic combination of these preclinical approaches - leveraging the physiological relevance of animal models, the human specificity of organoids, and the circuit modeling capabilities of assembloids - promises to accelerate our understanding of ASD mechanisms and the development of targeted therapeutic interventions. The future of ASD research lies not in identifying a single superior model, but in wisely integrating multiple complementary approaches to address the multifaceted complexity of this spectrum of neurodevelopmental conditions.
The profound heterogeneity of Autism Spectrum Disorder (ASD) presents a significant challenge for diagnosis, prognosis, and therapeutic development. Traditional behavioral diagnostics often fail to capture the underlying biological diversity, limiting personalized intervention strategies. This whitepaper examines how machine learning (ML) is revolutionizing ASD research by disentangling this heterogeneity through data-driven subtype identification and prognostic stratification, with a specific focus on the correlations with distinct biochemical pathways. For researchers and drug development professionals, these approaches provide a framework for developing precision medicine strategies that align interventions with an individual's specific neurobiological profile, thereby increasing the likelihood of successful outcomes.
Machine Learning Frameworks for ASD Subtype Identification
Advanced computational approaches are moving beyond symptom-based classification to uncover biologically distinct subgroups of ASD. These methods integrate multimodal data to define subtypes with unique genetic underpinnings and developmental trajectories.
Person-Centered Subtyping Reveals Biologically Distinct Groups
A landmark study by Princeton University and the Simons Foundation analyzed over 230 clinical traits from more than 5,000 children in the SPARK cohort, using a person-centered computational model to identify four clinically and biologically distinct subtypes of autism [3]. This approach considered a broad range of traits—from social interactions to developmental milestones—rather than searching for genetic links to single traits.
The table below summarizes the key characteristics and prevalence of these four data-driven subtypes:
Table 1: Four Biologically Distinct Autism Subtypes Identified via Machine Learning
| Subtype Name | Prevalence | Clinical Characteristics | Genetic Profiles |
|---|---|---|---|
| Social and Behavioral Challenges | ~37% | Core autism traits without developmental delays; high rates of co-occurring conditions (ADHD, anxiety, depression) [3]. | Mutations in genes active later in childhood, suggesting biological mechanisms emerge postnatally [3]. |
| Mixed ASD with Developmental Delay | ~19% | Developmental milestones reached later; minimal co-occurring psychiatric conditions; mixed social and repetitive behaviors [3]. | Higher likelihood of carrying rare inherited genetic variants [3]. |
| Moderate Challenges | ~34% | Milder core autism traits; no co-occurring psychiatric conditions; typical developmental milestones [3]. | Not specified in the study. |
| Broadly Affected | ~10% | Severe, wide-ranging challenges including developmental delays, social difficulties, and co-occurring psychiatric conditions [3]. | Highest burden of damaging de novo mutations (not inherited from parents) [3]. |
Critically, this research linked each subtype to distinct genetic patterns and developmental trajectories. The discovery that the Social and Behavioral Challenges subtype involves mutations in genes that become active later in childhood suggests its biological mechanisms may unfold after birth, aligning with the often-later diagnosis of these individuals [3]. Furthermore, the study demonstrated that superficially similar clinical presentations, such as developmental delays shared by the "Broadly Affected" and "Mixed ASD with Developmental Delay" groups, have fundamentally different genetic origins—a finding only possible through a subtyping approach [3].
Neuroimaging-Based Subtyping Using Gray Matter Networks
Complementing the clinical trait-based approach, other researchers have utilized neuroimaging data to identify subtypes. One study applied a semi-supervised machine learning algorithm called Heterogeneity through Discriminative Analysis (HYDRA) to T1-weighted MRI data from 225 male participants with ASD [52]. The analysis of gray matter networks revealed three distinct subtypes:
- Subtype 1: Exhibited high connectivity in sensorimotor regions (left anterior and right posterior central gyri), suggesting altered sensorimotor processing.
- Subtype 2: Showed decreased connectivity in motor control regions but increased connectivity in visual and language processing areas (left fusiform and lingual gyri).
- Subtype 3: Displayed alterations in higher-order cognitive regions (left medial superior frontal gyrus and left middle frontal gyrus), implicating challenges with executive function and social cognition [52].
These brain-based subtypes also correlated with significant differences in clinical measures, such as verbal and performance intelligence scores, underscoring the clinical relevance of the neural stratification [52].
Experimental Protocols for Data-Driven Diagnostics
The implementation of ML models for subtype identification and risk stratification requires rigorous methodological pipelines. The following section details two key experimental frameworks.
Protocol 1: Multimodal AI for Early Risk Stratification
A novel two-stage multimodal AI framework demonstrates a protocol for scalable ASD screening and risk stratification using data from 1,242 children aged 18-48 months [53].
- Objective: To accurately differentiate typically developing children from those at high risk or with ASD, and subsequently to distinguish high-risk children from those with an ASD diagnosis.
- Data Modalities:
- Audio Data: Naturalistic parent-child interaction videos were analyzed to extract vocal features using the Whisper speech recognition model, capturing objective linguistic and prosodic biomarkers [53] [54].
- Text Data: The textual content of standardized screening questionnaires (MCHAT, SCQ-L, SRS) was processed using Natural Language Processing (NLP) with the RoBERTa-large model to extract nuanced behavioral semantic information beyond simple scores [53].
- Workflow:
- Stage 1: A multimodal neural network integrated audio features and questionnaire text to differentiate Typically Developing (TD) children from a combined High-Risk/ASD group.
- Stage 2: A fine-tuned RoBERTa model integrated behavioral task success/failure data with SRS questionnaire text to differentiate the High-Risk group from the ASD group [53].
- Performance: The framework achieved an Area Under the Receiver Operating Characteristic curve (AUROC) of 0.942 in Stage 1 and an AUROC of 0.914 in Stage 2. The model's predicted risk categories showed 79.59% accuracy and a strong correlation (Pearson r = 0.830) with gold-standard ADOS-2 assessments [53].
The following diagram visualizes this two-stage experimental workflow:
Protocol 2: Deep Learning for High-Accuracy Screening
Another study utilized a large dataset from the Autism Genetic Resource Exchange (AGRE) repository, containing Autism Diagnostic Interview-Revised (ADI-R) scores from 2,794 individuals, to develop a high-accuracy screening model [55].
- Objective: To optimize the accuracy of ASD screening using a large-scale ADI-R dataset and to identify a minimal set of items for efficient diagnosis.
- Data: ADI-R version 2003 data from 2,480 ASD individuals and 314 non-ASD individuals [55].
- Workflow:
- Model Training and Comparison: Seven supervised ML algorithms were trained and optimized. A Deep Learning (DL) model achieved the highest accuracy at 95.23% (CI 94.32–95.99%) [55].
- Feature Reduction: Sparse Partial Least Squares Discriminant Analysis (sPLS-DA) was applied to reduce the number of items from the full 93-question ADI-R. This identified a streamlined set of just 27 critical sub-items [55].
- Validation: Models trained on the 27-item set demonstrated comparable performance to the full-item model, with accuracy and sensitivity differing by only 1-2% [55].
Table 2: Performance Comparison of Machine Learning Models for ASD Screening (n=2514)
| Machine Learning Algorithm | Accuracy (%) | Sensitivity (%) | Specificity (%) |
|---|---|---|---|
| Deep Learning (DL) | 95.23 | 97.94 | 73.76 |
| Support Vector Machine (SVM) | 92.52 | 98.50 | 56.00 |
| Random Forest (RF) | 92.48 | 99.70 | 50.00 |
| Logistic Regression (LR) | 92.36 | 97.94 | 63.82 |
| k-Nearest Neighbor (k-NN) | 92.16 | 97.81 | 61.15 |
| Decision Tree (DTree) | 90.89 | 99.10 | 50.00 |
| Naïve Bayes (NB) | 89.62 | 91.27 | 81.60 |
Source: Adapted from Scientific Reports [55]
Linking Data-Driven Subtypes to Biochemical Pathways in Pathogenesis
The true power of ML-derived subtypes lies in their ability to bridge clinical presentation with underlying molecular mechanisms, providing a functional context for autism pathogenesis centered on dysregulated biochemical pathways.
A Framework of Convergent Biochemical Pathways
A compelling model proposes that genetically diverse forms of ASD can be parsed into entities resulting from converse patterns of growth regulation at the molecular level. This leads to correlates of either general synaptic and neural overgrowth or undergrowth [56]. Abnormal brain growth is a well-documented feature in children with autism and corresponding mouse models [56] [14].
This model suggests that disparate genetic mutations can converge onto a limited set of key biochemical pathways that control cell growth, proliferation, and synaptic maturation. Two central pathways implicated in this dysregulation are:
- The mTOR Pathway: A central regulator of cell growth and protein synthesis. Hyperactivation of mTOR signaling is associated with synaptic overgrowth and has been linked to syndromic forms of ASD like tuberous sclerosis [56].
- The MAPK/ERK Signaling Pathway: Involved in a wide array of cellular processes, including differentiation and proliferation. Dysregulation of this pathway can similarly lead to abnormal neural growth patterns [56].
The direction of dysregulation in these pathways (over- vs. under-activation) may correspond to the distinct neural and clinical phenotypes observed in different subtypes. For instance, the "Broadly Affected" subtype with its high burden of damaging mutations [3] might be enriched for individuals with specific pathway dysregulations.
Subtype-Specific Molecular Narratives
The Princeton/Simons study powerfully confirmed that "What we’re seeing is not just one biological story of autism, but multiple distinct narratives" [3]. By first separating individuals into clinically meaningful subtypes, researchers were able to detect distinct genetic signals and divergent biological processes that were obscured in aggregate analyses [3]. This paradigm shift allows for the formation of specific hypotheses linking various biochemical pathways to different ASD presentations.
For example, the finding that the "Social and Behavioral Challenges" subtype involves mutations in genes active later in childhood opens up a novel line of inquiry into the specific postnatal biochemical pathways that govern the development of social circuits and how they might be perturbed [3]. This moves the field beyond a purely prenatal focus on pathogenesis.
The Scientist's Toolkit: Research Reagent Solutions
The advancement of data-driven diagnostics relies on a suite of specialized reagents, tools, and datasets. The following table details key resources for conducting similar research.
Table 3: Essential Research Reagents and Resources for ML-Driven Autism Subtyping
| Resource Category | Specific Example | Function/Application in Research |
|---|---|---|
| Cohort Datasets | SPARK Cohort [3] | Large-scale resource with genetic and phenotypic data from over 5,000 children with ASD; essential for person-centered subtyping. |
| Autism Brain Imaging Data Exchange (ABIDE) [52] | Repository of brain imaging data from individuals with ASD and controls; used for neuroimaging-based subtype discovery. | |
| Autism Genetic Resource Exchange (AGRE) [55] | Database providing genetic and phenotypic data from families affected by ASD; used for training screening models. | |
| Computational Tools | RoBERTa-large Model [53] | A pre-trained Natural Language Processing (NLP) model used to extract semantic meaning from screening questionnaire text. |
| Whisper Model [53] | A state-of-the-art speech recognition model used to process and extract features from audio of parent-child interactions. | |
| HYDRA [52] | A semi-supervised machine learning algorithm used for identifying neuroanatomical subtypes from MRI data. | |
| Biomarker Assays | Gene Expression Panels (e.g., CALB1, RORB) [14] | Used to analyze post-mortem brain tissue for markers of cortical disorganization in specific subtypes. |
| Plasma Proteome Profiling [57] | Multiplex assays to identify protein biomarkers in blood that correlate with ASD risk or specific subtypes. | |
| Validation Instruments | ADOS-2 [53] | Gold-standard diagnostic observation tool used to validate the output of ML risk stratification models. |
| ADI-R [55] | Gold-standard diagnostic interview used as a rich data source for training and validating screening models. |
Machine learning is fundamentally reshaping the diagnostic and stratification landscape for autism spectrum disorder. By integrating multimodal data—from clinical traits and neuroimaging to genetics—these methods are deconstructing ASD heterogeneity into biologically meaningful subtypes. This refined taxonomy provides a critical lens through which to view the dysregulated biochemical pathways, such as mTOR and MAPK/ERK signaling, that underlie pathogenesis. For researchers and drug developers, this new paradigm is foundational for precision medicine. It enables the alignment of therapeutic targets with specific neurobiological narratives, transforming the approach from one-size-fits-all to tailored interventions based on an individual's data-driven profile, ultimately promising more effective outcomes for the diverse autism community.
Challenges and Solutions in Autism Therapeutic Development and Translation
Autism Spectrum Disorder (ASD) represents a complex neurodevelopmental condition characterized by persistent deficits in social communication and interaction, as well as restricted, repetitive patterns of behavior, interests, or activities. The profound heterogeneity in ASD presentation has long presented a formidable challenge for developing effective, targeted pharmacotherapies. Current medication management for individuals with ASD is complicated by the fact that only aripiprazole and risperidone are approved to treat irritability associated with ASD in children and adolescents, with no pharmacologic treatments available that target the underlying etiology of ASD [58]. Without medications approved to target ASD-specific etiology, multiple psychotropic medications are frequently prescribed to manage both ASD-related symptoms and those associated with co-occurring psychiatric conditions, resulting in significant psychotropic polypharmacy [58]. This practice is further complicated by the fact that children with ASD often experience more adverse effects and show limited response to psychotropic medications compared to children not diagnosed with ASD [58].
The emerging field of pharmacogenomics (PGx) offers promising approaches to address these challenges by optimizing medication selection and dosing based on genetic factors. PGx testing analyzes genetics to predict pharmacokinetic (PK) and pharmacodynamic (PD) responses to medications, addressing the limited response rates to first-line medications, which are reported to range from 42% to 53% in depression alone [58]. This review examines the current state of pharmacogenomics in ASD treatment within the broader context of biochemical pathways in autism pathogenesis, providing researchers and drug development professionals with a comprehensive framework for addressing patient variability in therapeutic development.
Biological Subtyping: A Framework for Precision Medicine in ASD
Four Distinct Autism Subtypes
Groundbreaking research published in 2025 has identified four clinically and biologically distinct subtypes of autism, marking a transformative step in understanding the condition's genetic underpinnings and enabling personalized care [3]. This study, analyzing data from over 5,000 children in the SPARK autism cohort, used a computational model to group individuals based on their combinations of over 230 traits, from social interactions to repetitive behaviors to developmental milestones [3]. The identification of these subtypes provides a crucial framework for understanding patient variability in drug response and metabolism.
Table 1: Four Biologically Distinct Autism Subtypes and Their Characteristics
| Subtype Name | Prevalence | Clinical Presentation | Genetic Features | Developmental Trajectory |
|---|---|---|---|---|
| Social and Behavioral Challenges | 37% | Core autism traits with co-occurring ADHD, anxiety, depression, or OCD; minimal developmental delays | Common psychiatric-related variants; genes active after birth | Typical milestone attainment; later diagnosis |
| Mixed ASD with Developmental Delay | 19% | Developmental delays, language impairments, intellectual disability; fewer behavioral issues | Rare inherited variants; genes active prenatally | Later milestone attainment; earlier diagnosis |
| Moderate Challenges | 34% | Milder symptoms across domains; limited co-occurring conditions | Not specified | Typical milestone attainment |
| Broadly Affected | 10% | Widespread challenges including cognitive impairment, developmental delays, and psychiatric conditions | Highest burden of de novo mutations; brain development genes | Significant delays; earlier diagnosis |
Subtype-Specific Biological Pathways
Each autism subtype demonstrates distinct genetic signatures and affected biological pathways, with remarkably little overlap between subtypes [4]. The Broadly Affected subtype shows the highest proportion of damaging de novo mutations impacting genes crucial for early brain development, while the Social and Behavioral Challenges subtype involves mutations in genes that become active later in childhood, suggesting biological mechanisms that emerge after birth [3]. The Mixed ASD with Developmental Delay subtype was more likely to carry rare inherited genetic variants [3]. These distinct biological narratives explain why past genetic studies often fell short—they were essentially trying to solve multiple different puzzles mixed together without recognizing the distinct subtypes [3].
Diagram 1: Autism Subtypes and Their Distinct Genetic Pathways. This diagram illustrates the four biologically distinct autism subtypes and their associated genetic features and biological pathways, highlighting the heterogeneous nature of ASD pathophysiology.
Pharmacogenomic Mechanisms in ASD Drug Metabolism
Pharmacokinetic Considerations
Significant advances in psychotropic dosing have emerged from a deeper understanding of pharmacokinetics, allowing clinicians to optimize dosing strategies [59]. Pharmacogenetics complements this progress by examining how genetic variations influence drug metabolism and interactions, enabling personalized treatment plans that adjust dosages to enhance efficacy and minimize adverse effects [59]. Genetic variants of multiple PK-related enzymes may confer ultra-rapid, intermediate, or poor metabolism of select psychotropic medications, potentially resulting in poor therapeutic response due to altered plasma concentrations and delayed drug clearance [58].
For ASD treatment, risperidone metabolism presents a particularly well-studied example. Risperidone is mainly metabolized in the liver by the CYP450 isoenzyme CYP2D6, with CYP3A4 and CYP3A5 partially involved in its 9-hydroxylation [60]. The resulting metabolite, 9-OH-risperidone, is a pharmacologically active metabolite approximately equipotent to the parent drug, with both concentrations collectively referred to as the total active moiety [60]. However, a large-scale study involving psychiatric patients of various ages revealed that the positive predictive value of an RIS/9-OH-RIS ratio >1 to predict CYP2D6 poor metabolizers was only 35%, indicating that CYP2D6 variation alone cannot fully explain the interindividual variability in risperidone exposure [60].
Beyond CYP450: Expanded Pharmacogenomic Targets
Recent exploratory pharmacogenetic testing has revealed novel markers beyond classical metabolic pathways that influence drug response in ASD. A 2024 prospective cohort study enrolled 89 Saudi children with ASD treated with risperidone-based antipsychotic therapy and identified 27 PGx variants with prominent impact on various risperidone PK parameters, most located outside genes involved in the classical risperidone PK pathway [60]. Notably, certain human leukocyte antigen (HLA) markers were found to enhance various risperidone exposure parameters, reinforcing the gut-brain axis theory of ASD etiology and its suggested inflammatory impacts on drug bioavailability through modulation of the brain, gastrointestinal tract, and/or hepatic expression of metabolizing enzymes and transporters [60].
Table 2: Key Pharmacogenetic Variants Influencing Drug Response in ASD
| Gene | Metabolizer Phenotypes | Affected Medications | Clinical Impact | Evidence Level |
|---|---|---|---|---|
| CYP2D6 | Poor, Intermediate, Extensive, Ultrarapid | Risperidone, Aripiprazole, Antidepressants | Altered drug levels, efficacy, and side effect profile | Established [58] [60] |
| CYP2C19 | Poor, Intermediate, Extensive, Ultrarapid | SSRIs, Clomipramine, Citalopram | Modified therapeutic response and tolerability | Established [59] |
| UGT2B17 | Variable activity | Risperidone (indirect) | Influences metabolic ratio | Exploratory [60] |
| HLA genes | Not applicable | Various psychotropics | Possible immune-mediated drug metabolism alterations | Hypothetical [60] |
| ABCB1 | Transporter variants | Risperidone, Multiple drugs | Potential impact on drug distribution and clearance | Preliminary [60] |
The Gut-Brain Axis and Drug Metabolism in ASD
Gut Microbiota Metabolite Interactions
The microbiota-gut-brain axis plays a crucial role in the pathophysiology of ASD, with gut microbial metabolites significantly influencing neurodevelopment, neurotransmission, and behavioral regulation [61]. A 2025 study integrating network pharmacology, molecular docking, and multi-database analysis identified 51 core targets that intersect with ASD-related genes and gut metabolite targets, validating AKT1 and IL6 as pivotal genes through protein-protein interaction (PPI) network analysis [61]. Functional enrichment highlighted important associations with the PI3K/Akt and IL-17 signaling pathways, with the Microbiome-Metabolite-Target-Signaling (MMTS) network linking eight key metabolites (including short-chain fatty acids and indole derivatives) to AKT1/IL6 regulation [61].
Molecular docking revealed strong binding affinity between glycerylcholic acid (AKT1: -10.2 kcal/mol) and 3-indolepropionic acid (IL6: -4.9 kcal/mol), suggesting they are closely related to ASD pathophysiology [61]. This research provides a new direction for understanding the relationship between microbial metabolites and ASD, offering potential avenues for leveraging gut microbiome modulation to enhance therapeutic efficacy.
Gut Microbiome Influence on Drug Metabolism
The gut microbiome significantly influences drug metabolism through multiple mechanisms, including direct enzymatic transformation of drugs, alteration of host metabolic enzyme expression, and modulation of immune system function that indirectly affects drug disposition [61]. For individuals with ASD, who frequently experience gastrointestinal comorbidities and gut dysbiosis, this microbiome-mediated drug metabolism may represent a critical source of interindividual variability in treatment response.
Diagram 2: Gut-Brain Axis Signaling in ASD Drug Response. This diagram illustrates how gut microbiome dysbiosis in ASD leads to altered microbial metabolite production, which subsequently impacts core signaling pathways involved in drug metabolism and response.
Experimental Approaches and Methodologies
Pharmacogenomic Testing Platforms
Advanced genomic technologies enable comprehensive profiling of genetic variants affecting drug metabolism and response. The GeneSight Psychotropic test represents one commercially available approach that analyzes multiple genes relevant to psychotropic medication metabolism [58]. These platforms typically utilize DNA microarray or sequencing technologies to identify single nucleotide polymorphisms (SNPs), copy number variations (CNVs), and other genetic alterations in a targeted panel of pharmacogenes.
For research applications, the Axiom PharmacoFocus Array provides a focused exploratory testing platform, including probe sets targeting PK/PD genes, enabling identification of novel PGx markers beyond classical pathways [60]. In the risperidone pharmacokinetics study previously mentioned, this approach allowed researchers to identify 720 PGx markers for association analysis, ultimately finding 27 variants with prominent impact on risperidone PK parameters [60].
Analytical Frameworks for Pharmacogenomic Data
Sophisticated computational approaches are essential for interpreting the complex relationships between genetic variants and drug response. Machine learning algorithms, particularly general finite mixture modeling, have proven valuable for integrating different data types and classifying individuals into clinically meaningful subgroups [4]. This "person-centered" approach maintains representation of the whole individual rather than focusing on single traits, enabling more complete modeling of the complex spectrum of traits that characterize ASD [4].
Network pharmacology represents another powerful analytical framework that integrates systems biology and pharmacology, enabling comprehensive analysis through target identification, protein-protein interaction (PPI) network construction, and molecular docking validation [61]. This approach has successfully identified potential therapeutic metabolites derived from gut microbiota and their molecular targets in ASD.
Table 3: Experimental Resources for ASD Pharmacogenomics Research
| Research Tool/Resource | Application in ASD PGx | Key Features | Research Utility |
|---|---|---|---|
| SPARK Cohort Database | Autism subtype identification | >5,000 participants with extensive phenotypic and genotypic data | Person-centered analysis of trait combinations [3] [4] |
| Axiom PharmacoFocus Array | Exploratory PGx testing | 720 PGx markers targeting PK/PD genes | Identification of novel biomarkers beyond classical pathways [60] |
| Network Pharmacology Approach | Gut microbiota metabolite analysis | Integration of multiple databases and molecular docking | Identifies core targets and signaling pathways [61] |
| General Finite Mixture Modeling | Data integration and classification | Handles different data types (categorical, continuous) | Enables person-centered approach to subgrouping [4] |
| gutMGene Database | Gut metabolite-target identification | Curated database of human gut microbiota and metabolites | Facilitates gut-brain axis research in ASD [61] |
Clinical Implementation and Therapeutic Implications
Current Evidence for PGx-Guided Treatment in ASD
The clinical utility of pharmacogenomic testing in ASD continues to be evaluated, with current evidence presenting a complex picture. A 2025 retrospective study of 99 individuals with ASD compared PGx testing to treatment as usual (TAU) in a high-acuity behavioral health care setting [58]. At admission, 93% of individuals were prescribed at least one psychotropic medication, with over half prescribed medications with potential gene-drug interactions [58]. Following PGx testing, there was an overall reduction in prescribed medications with potential gene-drug interactions; however, no differences were observed between the PGx and TAU groups in polypharmacy, quality of life, or symptom assessments of depression, anxiety, obsessive-compulsive disorder, and body-focused repetitive behaviors [58].
These findings contrast with the broader field of psychotropic pharmacogenetics, where landmark studies such as the EU-PGx trial demonstrated significant clinical benefits. This trial, assessing adverse drug reactions across both psychiatric and nonpsychiatric medications in nearly 7000 adults, utilized a 12-gene panel focused primarily on pharmacokinetic polymorphisms based on the Dutch Pharmacogenetic Working Group guidelines [59]. Among patients with actionable PGx results, adverse drug reactions occurred in only 21.0% of the PGx group compared to 27.7% in the control group, resulting in a significant 30% reduction [59]. Since nearly 45% of the medications used in the trial were psychotropic drugs, these findings highlight PGx's relevance in psychiatric care, though not specifically in ASD [59].
Subtype-Guided Therapeutic Approaches
The identification of biologically distinct autism subtypes enables more targeted therapeutic development tailored to specific underlying mechanisms. Each subtype's distinct genetic profile and developmental trajectory suggest they may respond differently to various pharmacologic interventions [3] [5]. For instance, the Social and Behavioral Challenges subtype, with its strong genetic links to common psychiatric disorders and postnatal gene expression patterns, might respond better to medications targeting anxiety, depression, or ADHD symptoms compared to other subtypes [5].
Conversely, the Broadly Affected subtype, characterized by severe disruptions in core neurodevelopmental pathways and the highest burden of de novo mutations, may require more comprehensive intervention strategies addressing multiple systems [5]. Understanding these subtype-specific biological narratives provides a foundation for developing precision medicine approaches that move beyond the current one-size-fits-all model of ASD treatment.
Future Directions and Research Opportunities
Emerging Research Initiatives
The field of ASD pharmacogenomics is rapidly evolving, with several major initiatives poised to advance our understanding. The National Institutes of Health launched the Autism Data Science Initiative (ADSI) in 2025, a landmark research effort that will harness large-scale data resources to explore contributors to the causes and rising prevalence of ASD [10]. This initiative will apply advanced analytic methods, including machine learning, exposome-wide analyses, and organoid models, to study how gene-environment interactions contribute to autism and how current treatments and services may be improved [10].
Additional promising research directions include investigating the non-coding genome, which constitutes more than 98% of the genome but remains less studied because these regions do not code for proteins [4]. These areas play important roles in regulating gene expression and other cellular processes implicated in autism, offering substantial potential for new discoveries [4].
Therapeutic Development Strategies
Future drug development for ASD must account for the substantial biological heterogeneity now known to exist within the spectrum. Rather than seeking universal treatments for all individuals with ASD, more productive approaches will likely target specific biological subtypes or pathway disruptions shared across subsets of individuals [3] [5]. The Princeton Precision Health initiative exemplifies this approach, using artificial intelligence and computational modeling to integrate across biological and clinical data to enable more precise diagnostic and therapeutic strategies [3].
Additionally, the growing understanding of the gut-brain axis in ASD suggests promising avenues for microbiota-targeted interventions that might optimize drug response [61]. Clinical trials utilizing microbiota transfer therapy have reported symptomatic improvement in children with ASD, highlighting the therapeutic potential of gut microbiota modulation [61]. Future research exploring how these microbiome-focused interventions influence drug metabolism and efficacy represents a promising frontier in ASD pharmacogenomics.
The integration of pharmacogenomics into autism research and treatment represents a paradigm shift from symptom-focused approaches to biologically-informed precision medicine. The recent identification of four distinct autism subtypes, each with unique genetic profiles, developmental trajectories, and biological pathways, provides a crucial framework for understanding and addressing patient variability in drug response. While current evidence for PGx-guided treatment in ASD remains mixed, the compelling results from broader psychotropic pharmacogenetics and the emerging understanding of subtype-specific mechanisms suggest significant potential for future applications.
For researchers and drug development professionals, these advances highlight the importance of considering ASD not as a single entity but as a collection of biologically distinct conditions requiring personalized therapeutic approaches. Future progress will depend on continued efforts to map the complex relationships between genetic variants, gut microbiome composition, metabolic pathways, and treatment response across autism subtypes. By embracing this multifaceted perspective, the field can move closer to realizing the promise of precision medicine for individuals with ASD, ultimately improving therapeutic outcomes and quality of life across the autism spectrum.
Target pleiotropy, wherein a single gene regulates multiple, often disparate, biological functions, presents a significant challenge in developing targeted therapies for complex disorders like autism spectrum disorder (ASD). This whitepaper elucidates the phenomenon of pleiotropy among high-confidence ASD risk genes, focusing on chromatin regulators with dual roles in nuclear and cytoskeletal processes. We provide a structured analysis of the convergent molecular pathways, detailed experimental methodologies for delineating primary mechanisms of action, and a strategic framework for leveraging these insights into novel therapeutic design. Within the broader thesis of biochemical pathways in ASD pathogenesis, this guide underscores the necessity of moving beyond annotated gene function to identify precise, therapeutically actionable targets.
Autism spectrum disorder is characterized by a complex aetiology involving hundreds of risk genes that converge on a smaller set of key biological pathways [26]. A prominent feature of many high-confidence ASD risk genes, particularly those encoding chromatin regulators, is their profound pleiotropy—the execution of multiple biochemical functions in different cellular contexts. This multifunctionality complicates the identification of the primary pathological mechanisms whose correction would yield therapeutic benefit.
Gene ontology analyses have historically emphasized the enrichment of ASD risk genes in synaptic function and chromatin regulation [62]. However, hypothesis-naive functional investigations have repeatedly implicated additional processes, including tubulin biology and cellular proliferation [62]. The discovery that chromatin regulators such as ADNP and CHD3 directly regulate both histones and tubulins exemplifies this challenge [62]. Consequently, a mutation in a pleiotropic gene may disrupt chromatin remodeling, microtubule dynamics, or both, creating a confounding pathobiological landscape. Overcoming target pleiotropy requires systematic experiments to define which of these disrupted functions is the primary driver of disease phenotypes, thereby enabling the design of precise molecular interventions.
Pleiotropy in Action: ASD Chromatin Regulators at the Microtubule
Key Evidence of Microtubule Localization
Recent empirical evidence demonstrates that the pleiotropic functions of ASD-associated chromatin regulators extend to direct involvement with microtubule-based structures. Investigation of the five chromatin regulators with the strongest statistical evidence for ASD association—ADNP, CHD8, CHD2, POGZ, and KMT5B—revealed their consistent localization to the microtubule-rich mitotic spindle during cell division, in addition to their expected nuclear localization during interphase [62].
These findings were consistent across multiple model systems:
- In vivo models: Strep-tagged human cDNAs expressed in Xenopus embryos showed clear mitotic spindle localization during metaphase [62].
- In vitro models: Human HEK293T cells and human induced pluripotent stem cell (iPSC)-derived neural progenitor cells (NPCs) confirmed spindle and, in neurons, axonal microtubule localization [62].
This direct physical association with tubulin structures provides a mechanistic link through which mutations in these genes could disrupt cell proliferation, neuronal migration, and axonal outgrowth—processes critical to neurodevelopment.
Functional Consequences of Disrupted Microtubule Function
The functional significance of this localization is underscored by phenotypic consequences observed upon loss of function. Focusing on CHD2, CRISPR interference (CRISPRi)-mediated knockdown in human iPSC-derived cortical NPCs led to a cascade of microtubule-related defects [62]:
- Spindle Organization: A significant increase in abnormal mitotic spindles.
- Cell Cycle Stalling: Increased cyclin B (a G2/M marker) and decreased cyclin E (a G1/S marker), indicating M-phase stalling.
- Genomic Instability: A significant increase in phosphorylated H2AX (pH2AX) puncta, a marker of DNA damage.
- Cell Death: Increased apoptosis, as measured by cleaved caspase 3 staining.
Furthermore, a specific ASD-associated missense mutation in CHD2 (p.R1772T) was shown to disrupt the protein's localization to the mitotic spindle without affecting its nuclear localization, providing direct evidence that patient-derived mutations can selectively impair one function of a pleiotropic gene [62].
Quantitative Data Synthesis
Table 1: Phenotypic Consequences of CHD2 Haploinsufficiency in Human iPSC-Derived Neural Progenitor Cells
| Phenotype Category | Specific Assay | Measurement Outcome | Statistical Significance |
|---|---|---|---|
| Mitotic Spindle Defects | β-tubulin & phospho-histone H3 staining | Increased frequency of abnormal spindles | χ² test, P = 0.047 [62] |
| Cell Cycle Stalling | Cyclin B immunostaining | Increased proportion of cells in G2/M | Rank sum test, P < 0.0001 [62] |
| DNA Damage | pH2AX puncta count | Increased number of pH2AX foci per nucleus | Rank sum test, P < 0.0001 [62] |
| Cell Death | Cleaved caspase 3 staining | Increased apoptotic activity | Rank sum test, P < 0.0001 [62] |
Table 2: Core ASD-Associated Pleiotropic Chromatin Regulators and Their Functions
| Gene | Primary Annotated Function | Pleiotropic Function | Associated Cellular Phenotypes from Loss of Function |
|---|---|---|---|
| ADNP | Chromatin remodeling | Microtubule binding & mitotic spindle regulation | Transcriptional dysregulation, cell cycle defects, impaired neurite outgrowth [62] |
| CHD8 | Chromatin remodeling | Microtubule binding & mitotic spindle regulation | Transcriptional dysregulation, cell cycle defects, macrocephaly models [62] |
| CHD2 | Chromatin remodeling | Microtubule binding & mitotic spindle organization | Spindle defects, DNA damage, cell death, seizures [62] |
| POGZ | Chromatin remodeling | Microtubule binding & mitotic spindle regulation | Transcriptional dysregulation, mitotic errors, microcephaly models [62] |
| KMT5B | Histone methylation (H4K20) | Microtubule binding & mitotic spindle regulation | Transcriptional dysregulation, genomic instability [62] |
Defining Primary Mechanisms: Essential Experimental Workflows
A systematic, multi-stage workflow is required to dissect primary mechanisms from secondary effects in pleiotropic targets.
Workflow for Dissecting Pleiotropic Mechanisms
Detailed Experimental Protocols
Protocol: Subcellular Localization of Pleiotropic Proteins
Objective: To determine the localization of a pleiotropic protein (e.g., a chromatin regulator) to various cellular compartments, including the nucleus and microtubule structures.
Materials:
- Cell Lines: Human iPSC-derived neural progenitor cells (NPCs) or cortical neurons.
- Expression Constructs: Plasmids for wild-type and mutant (e.g., p.R1772T CHD2) cDNA with Strep or GFP tags.
- Antibodies: Primary antibodies against the target protein (validated via knockout/knockdown as in [62]), β-tubulin (microtubules), γ-tubulin (centrosomes), and histone H3 (phospho S10 for mitotic cells).
- Imaging System: High-resolution confocal microscope.
Method:
- Cell Culture and Transfection: Culture NPCs on poly-D-lysine-coated coverslips. Transfect with expression constructs using a nucleofection system optimized for primary neural cells.
- Cell Fixation and Permeabilization: At 24-48 hours post-transfection, fix cells with 4% paraformaldehyde for 15 minutes at room temperature. Permeabilize with 0.1% Triton X-100 in PBS for 10 minutes.
- Immunostaining: Block cells with 5% normal goat serum for 1 hour. Incubate with primary antibodies diluted in blocking buffer overnight at 4°C. Use appropriate species-specific secondary antibodies conjugated to Alexa Fluor dyes (e.g., 488, 568, 647) for 1 hour at room temperature. Include DAPI for nuclear counterstaining.
- Image Acquisition and Analysis: Acquire z-stack images on a confocal microscope using identical settings across experimental conditions. Quantify co-localization using Pearson's correlation coefficient or Mander's overlap coefficient between the target protein signal and microtubule markers in defined regions of interest (e.g., mitotic spindle).
Protocol: Functional Phenotyping via CRISPRi and Rescue
Objective: To assess the contribution of specific protein domains to pleiotropic phenotypes via targeted knockdown and domain-specific functional rescue.
Materials:
- CRISPRi System: dCas9-KRAB expressing NPC line, sgRNAs targeting the gene promoter.
- Rescue Constructs: sgRNA-resistant cDNA constructs for:
- Wild-type full-length protein.
- Chromatin-domain mutant (e.g., lacking ATPase activity).
- Microtubule-binding-domain mutant (e.g., p.R1772T for CHD2).
- Assay Reagents: Antibodies for Cyclin B, pH2AX, cleaved caspase 3, and β-tubulin.
Method:
- Stable Cell Line Generation: Transduce NPCs with lentivirus expressing dCas9-KRAB and select with puromycin. Subsequently, transduce with lentivirus expressing gene-specific sgRNAs and select again.
- Rescue Experiments: Transfect knockdown cells with the various rescue constructs.
- Phenotypic Analysis:
- Cell Cycle: Analyze by flow cytometry for DNA content (Propidium Iodide) and Cyclin B intensity.
- DNA Damage: Immunostain for pH2AX and count foci per nucleus.
- Spindle Morphology: Fix and stain cells for β-tubulin and phospho-Histone H3. Classify spindles as normal or abnormal (monopolar, multipolar, disorganized).
- Viability: Measure apoptosis via flow cytometry for Annexin V and/or immunostaining for cleaved caspase 3.
- Data Interpretation: The construct that most effectively reverses the pathological phenotypes identifies the function (chromatin vs. microtubule) that is the primary disease driver.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Investigating Pleiotropic Mechanisms in ASD
| Reagent / Tool | Category | Specific Example | Function in Experimental Design |
|---|---|---|---|
| iPSC-Derived Neural Cells | Cellular Model | Cortical Neural Progenitor Cells (NPCs), Glutamatergic Neurons | Provides a physiologically relevant human background for studying neurodevelopmental processes like proliferation, migration, and synaptogenesis [62]. |
| CRISPR Interference (CRISPRi) | Gene Knockdown | dCas9-KRAB with gene-specific sgRNAs | Enables targeted, reversible gene suppression without double-strand breaks, allowing for clean phenotypic analysis and rescue experiments [62]. |
| Live-Cell Imaging Markers | Visualization | GFP-/Strep-tagged cDNA constructs, SiR-Tubulin dye | Allows for dynamic tracking of protein localization and microtubule dynamics in real-time, capturing transient events like mitosis [62]. |
| Validated Antibodies | Detection & Staining | Anti-CHD2 (validated by knockdown), β-Tubulin, pH2AX, Cleaved Caspase-3 | Critical for quantifying subcellular localization, mitotic defects, DNA damage, and cell death endpoints via immunofluorescence [62]. |
| Domain-Specific Rescue Constructs | Functional Analysis | sgRNA-resistant cDNAs for WT, chromatin-mutant, and microtubule-mutant proteins | The core tool for dissecting pleiotropy; determines which specific protein function is necessary and sufficient to reverse pathological phenotypes [62]. |
Pathway Convergence and Therapeutic Implications
Convergent Molecular Pathways in ASD
The investigation of pleiotropic genes reveals a broader principle in ASD pathogenesis: disparate genetic lesions converge onto a limited set of core biochemical pathways. While synaptic pathways are well-established, the evidence now strongly implicates tubulin biology and cellular proliferation as a major node of convergence [62]. Protein-protein interaction data demonstrate that ASD risk genes are significantly enriched among tubulin-associated proteins [62]. This convergence provides a strategic opportunity for therapeutic development, as targeting a downstream convergent pathway may benefit multiple ASD genetic subtypes.
From Mechanisms to Targeted Therapeutics
Understanding primary mechanisms enables the design of precise interventions:
- For haploinsufficiency due to null mutations: Gene replacement therapy is a promising strategy, as explored in Rett syndrome (MECP2) and Phelan-McDermid syndrome (SHANK3) [63]. Critical challenges include regulating gene dosage and achieving correct spatiotemporal delivery [63].
- For dysfunctional protein networks: Targeting convergent downstream pathways with small molecules is viable. For example, trofinetide, a synthetic analog of IGF-1, was approved for Rett syndrome and is being investigated for other ASDs like Phelan-McDermid syndrome, aiming to correct shared synaptic deficits [63].
- For epigenetic silencing: Allele reactivation strategies can be employed. In Angelman syndrome, antisense oligonucleotides or CRISPR/Cas9 are used to unsilence the paternal UBE3A allele [63]. For Fragile X syndrome, strategies focus on reactivating the silenced FMR1 gene [63].
Overcoming target pleiotropy is not merely an academic exercise but a fundamental prerequisite for precision medicine in ASD. The systematic deconstruction of pleiotropic genes, as illustrated for ASD-associated chromatin regulators, reveals that the primary pathological mechanism is not always the most obvious one. By employing a rigorous functional workflow—combining precise localization, detailed phenotypic profiling, and domain-specific rescue—researchers can distinguish primary disease drivers from secondary phenomena. This clarity directs therapeutic development towards the most actionable targets, whether they be the pleiotropic genes themselves or the convergent pathways they regulate, ultimately paving the way for effective, biologically grounded treatments for autism spectrum disorder.
1. Introduction: Biomarkers in the Context of Autism Spectrum Disorder Pathogenesis
The pursuit of predictive biomarkers represents a cornerstone of precision medicine, aiming to translate the heterogeneous presentation of complex conditions into actionable, individualized clinical strategies. Within the field of autism spectrum disorder (ASD) research, this pursuit is framed by a critical understanding of the disorder's multifactorial origins, which involve intricate and dysregulated biochemical pathways [64] [65] [66]. ASD is no longer viewed solely as a behavioral diagnosis but as a whole-body condition with significant metabolic, immunological, and neurological underpinnings [64] [66]. Emerging evidence strongly links ASD pathology to mechanisms such as oxidative stress, mitochondrial dysfunction, neuroinflammation, and imbalances in neurotransmitter and lipid metabolism [64] [65]. These aberrant pathways not only contribute to core and co-occurring symptoms but also present a rich source of quantifiable biological signals—potential biomarkers.
The development of biomarkers, defined as objectively measured indicators of normal or pathogenic processes or responses to an intervention [67] [68], is particularly urgent for ASD. Current diagnosis relies on behavioral observation, often leading to delays, while no FDA-approved drugs target the core symptoms [69] [66]. Predictive biomarkers, a subtype intended to forecast an individual's response to a specific therapeutic intervention, hold the promise of revolutionizing ASD care [67] [66]. They could enable early risk detection, stratify patients into biologically defined subgroups, and guide the selection of mechanism-based treatments, thereby moving from a one-size-fits-all approach to personalized intervention [69] [66]. This technical guide outlines the systematic process of identifying and validating predictive biomarker signatures, with a specific focus on the biochemical pathway dysregulations characteristic of ASD pathogenesis.
2. The Biomarker Development Pipeline: From Discovery to Clinical Application
The translation of a candidate biomarker into a validated clinical tool requires a rigorous, phased pipeline. This process mirrors drug development and ensures that the biomarker is fit-for-purpose [67].
Table 1: Phases of Biomarker Development and Their Objectives in ASD Research
| Phase | Primary Objective | Key Activities & Methodological Considerations |
|---|---|---|
| Discovery | Identify candidate biomarkers associated with ASD pathology or subtypes. | Multi-omics profiling (genomics, proteomics, metabolomics); AI-driven analysis of complex datasets; Case-control studies comparing ASD vs. neurotypical cohorts [64] [69] [65]. |
| Qualification | Establish a link between the biomarker and a biological process or clinical endpoint. | Demonstrate association with core pathways (e.g., oxidative stress, immune dysregulation); Link to clinical features (severity, GI symptoms) [64] [67] [68]. |
| Analytical Validation | Demonstrate that the biomarker can be measured accurately, precisely, and reliably. | Assess accuracy, precision, sensitivity, specificity, and reproducibility of the assay; Define standard operating procedures (SOPs) [67] [68]. |
| Clinical Validation | Confirm the biomarker's predictive performance in independent, prospective patient cohorts. | Conduct clinical studies to evaluate sensitivity/specificity for diagnosis or prediction of treatment response; Use independent validation cohorts to prevent overfitting [69] [67] [68]. |
| Utilization | Integrate the validated biomarker into clinical practice or therapeutic development. | Develop IVD assays; secure regulatory approval; use for patient stratification in clinical trials [69] [67]. |
3. Experimental Protocols for Key Phases
3.1 Discovery Phase Protocol: Multi-Omics Profiling for Candidate Identification
- Objective: To identify differentially expressed molecules in blood, CSF, or other biospecimens from individuals with ASD versus controls.
- Sample Collection: Collect plasma/serum, PBMCs, or urine from well-phenotyped cohorts (ASD and age-/sex-matched controls). Immediate processing and storage at -80°C is critical.
- Profiling Techniques:
- Metabolomics/Lipidomics: Using LC-MS/MS or NMR to quantify small molecules. Target pathways: oxidative stress markers (glutathione, methionine), lipid profiles, and mitochondrial metabolites [64].
- Proteomics/Immunoassays: Using multiplex immunoassays (e.g., Luminex) or mass spectrometry to measure cytokines (e.g., IL-6, IL-10, TNF-α), neuropeptides (oxytocin), and acute-phase proteins [64] [70] [65].
- Transcriptomics: Isolate RNA from blood and perform RNA-seq or microarray analysis to identify differentially expressed mRNA signatures [69].
- Data Analysis: Employ bioinformatics tools (Reactome, Panther, STRING) for pathway analysis [64]. Use AI/ML platforms (e.g., unsupervised learning, Gaussian mixture models) to identify complex, non-linear biomarker signatures from multimodal data without prior outcome bias [69] [70] [66].
3.2 Analytical Validation Protocol: Assay Performance Characterization
- Objective: To validate the assay used to measure the candidate biomarker panel.
- Parameters Assessed:
- Precision: Calculate intra-assay (repeatability) and inter-assay (reproducibility) coefficients of variation (CV) using replicate measurements of quality control samples [67] [68].
- Accuracy: Perform spike-and-recovery experiments by adding known quantities of analytic to a matrix.
- Linearity & Range: Test serial dilutions of a high-concentration sample to establish the assay's dynamic range.
- Lower Limit of Detection (LLOD)/Quantification (LLOQ): Determine the lowest concentration distinguishable from blank and measurable with acceptable precision [67].
- Reference Standards: Use certified reference materials where available.
4. Predictive Biomarker Signatures in ASD: Current Evidence and Quantitative Data
Research has identified several promising, interconnected biochemical domains harboring predictive biomarker candidates for ASD.
Table 2: Candidate Predictive Biomarker Domains and Quantitative Findings in ASD
| Biomarker Domain | Specific Candidate Biomarkers | Reported Alterations in ASD (vs. Controls) | Potential Predictive Utility |
|---|---|---|---|
| Oxidative Stress & Mitochondrial Function | Glutathione (GSH/GSSG ratio), Lipid peroxidation markers (MDA), Organic acids | Significantly elevated oxidative stress; mitochondrial dysfunction [64]. | Predicting severity, co-occurring GI issues, and response to antioxidant therapies [64]. |
| Neurotransmitters & Neuropeptides | Serotonin (5-HT), Oxytocin, Dopamine metabolites | Elevated whole-blood serotonin; decreased plasma oxytocin levels [65]. | Stratifying subgroups; predicting response to SSRIs or oxytocin-augmenting therapies. |
| Immune & Inflammatory Markers | Cytokines (IL-6, IL-10, TNF-α), CRP, Autoantibodies | Altered cytokine profiles; evidence of chronic neuroinflammation [64] [65]. | Identifying an inflammatory endophenotype for immune-modulating interventions. |
| Metabolic & Lipid Profiles | Amino acids (e.g., branched-chain), Ceramides, Cholesterol | Imbalances in amino acid metabolism; abnormal lipid profiles linked to cardiovascular risk [64]. | Linking metabolic subtypes to dietary or metabolic treatments. |
| Epigenetic Marks | DNA methylation patterns, Histone modifications | Differential methylation at specific loci [65]. | Early risk detection and understanding gene-environment interactions. |
Recent industry-led research using AI-driven platforms has reported the discovery of mRNA biomarker panels demonstrating >90% sensitivity and specificity in detecting ASD and its subtypes, highlighting the power of integrated, multi-analyte signatures [69].
5. Validation and Integration: The Path to Clinical Utility
The transition from a research finding to a clinically useful predictive tool requires robust validation. This involves testing the biomarker signature in independent, prospective cohorts to confirm its ability to stratify patients or predict treatment response [67] [68]. For a predictive biomarker in ASD, a clinical validation study might involve measuring the signature in patients before they begin a novel therapeutic (e.g., an antioxidant, immune modulator, or neuropeptide analog) and then correlating the baseline signature with clinical outcome measures after treatment. The statistical challenge is significant, requiring careful study design to avoid overfitting and to demonstrate that the biomarker adds predictive value beyond standard clinical assessments [67] [68].
Furthermore, the heterogeneity of ASD necessitates that biomarker development moves beyond a single diagnostic marker towards signatures that define biological subtypes. This aligns with the precision medicine goal of matching specific pathway dysregulations (e.g., oxidative stress-dominant vs. immune-dominant) with targeted therapies [66].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Platforms for ASD Biomarker Research
| Item/Category | Function in Biomarker Research | Example/Notes |
|---|---|---|
| Multiplex Immunoassay Kits | Simultaneous quantification of dozens of cytokines, chemokines, and growth factors from small sample volumes. | Luminex xMAP, Meso Scale Discovery (MSD) electrochemiluminescence assays. Critical for immune profiling [70]. |
| Mass Spectrometry Systems | Untargeted and targeted identification/quantification of metabolites, lipids, and proteins. | LC-MS/MS systems for metabolomics/lipidomics. Essential for oxidative stress and metabolic pathway analysis [64]. |
| Next-Generation Sequencing (NGS) Platforms | Transcriptomic profiling (RNA-seq) and analysis of epigenetic modifications. | Illumina sequencers for discovering mRNA biomarkers and differential expression signatures [69]. |
| AI/ML Data Analysis Platforms | Agnostic discovery of non-linear biomarker patterns and signatures from complex, high-dimensional data. | Platforms like Liquid Biosciences' Emerge AI for integrative multi-omics analysis [69]. |
| Certified Reference Materials & Quality Controls | Ensuring accuracy, precision, and reproducibility of biomarker measurements during assay validation. | Commercially available purified analytes and pooled human serum/plasma for assay calibration and QC [67]. |
| DNA/RNA/Protein Extraction Kits | High-quality, reproducible isolation of analytes from various biospecimens (blood, saliva, tissue). | Kits optimized for stability of labile biomarkers (e.g., phosphorylated proteins, RNA). |
6. Visualizing the Workflow and Pathway Complexity
Diagram 1: Biomarker Development Pipeline for ASD
Diagram 2: Interconnected Pathways & Biomarker Convergence in ASD
The intricate relationship between co-occurring conditions (multimorbidity) and the use of multiple medications (polypharmacy) presents a substantial challenge in autism spectrum disorder (ASD) research and treatment. The genetic and phenotypic heterogeneity of ASD often leads to varied biochemical manifestations, complicating clinical trial design and therapeutic development. This whitepaper examines the convergence of disparate ASD genetic lesions onto a limited number of key biochemical pathways, proposing a framework for classifying patients by pathogenic profiles rather than etiological categories. We explore the implications of multimorbidity and polypharmacy within this context, providing quantitative analyses, experimental protocols, and visualization tools to guide future research and clinical trials toward more targeted, effective interventions.
Autism spectrum disorder is characterized by significant genetic and phenotypic heterogeneity, with over 500 identified risk genes contributing to its etiology [71]. Despite this diversity, emerging evidence suggests that these genetic variations converge on a limited number of key biochemical pathways and neural circuits [72] [71]. This pathogenic convergence provides a crucial framework for understanding how co-occurring conditions and polypharmacy manifest in ASD populations.
The high heritability of autism suggests the disease process begins at conception, though diagnosis typically occurs around age 3 [71]. This developmental trajectory allows for the accumulation of secondary conditions and complex medication regimens that must be considered in research and clinical practice. Investigations into the underlying molecular etiology of ASD have often yielded mixed and sometimes opposing findings, necessitating more nuanced approaches to trial design and therapeutic development [72].
Key Biochemical Pathways in ASD Pathogenesis
Pathway Dysregulation Patterns
Research indicates that genetically diverse forms of ASD may be parsed into entities resulting from converse patterns of growth regulation at the molecular level, leading to correlates of general synaptic and neural overgrowth or undergrowth [72]. Abnormal brain growth during development is a characteristic feature observed in both children with autism and mouse models of the disorder.
Table 1: Key Biochemical Pathways in ASD Pathogenesis
| Pathway | Functional Role | Growth Dysregulation | Therapeutic Implications |
|---|---|---|---|
| mTOR Signaling | Regulates cell growth, proliferation, and protein synthesis | Overgrowth phenotype | mTOR inhibitors may normalize synaptic connectivity |
| ERK/MAPK Signaling | Mediates cellular responses to stimuli | Both overgrowth and undergrowth patterns | Pathway-specific modulators under investigation |
| Neurotrophic Factors | Support neuronal survival and differentiation | Altered synaptic pruning | Growth factor modulation strategies |
| Group I mGluR Signaling | Regulates synaptic plasticity and protein synthesis | Downstream cascade disruptions | Targeted receptor modulators |
| mRNA Networks (FMRP/UBE3A) | Controls translational regulation | Protein synthesis dysregulation | Precision RNA-targeted approaches |
Neural Circuit Implications
These biochemical disruptions manifest in specific neural circuits, including dorsal and ventral striatal pathways, amygdalar circuits, cerebellar networks, hypothalamic projections, and prefrontal and anterior cingulate cortical circuits [71]. The identification of these circuit-level manifestations provides opportunities for targeted interventions that address the core pathophysiology of ASD alongside co-occurring conditions.
Quantitative Analysis of Multimorbidity and Polypharmacy in ASD
Population-Level Data
Understanding the prevalence of multimorbidity and polypharmacy is crucial for designing clinically relevant trials. Recent studies of middle-aged and older adults provide insight into these co-occurring health states, though data specific to ASD populations remains limited.
Table 2: Prevalence of Multimorbidity and Polypharmacy in General Population Studies
| Health State | Definition | CLSA Cohort Prevalence | CPCSSN Cohort Prevalence | Age-Stratified Prevalence (65-85 years) |
|---|---|---|---|---|
| Multimorbidity | ≥2 conditions | 66.7% | 52.0% | 21.4% (CLSA), 18.3% (CPCSSN) |
| Polypharmacy | ≥5 medications | 14.9% | 22.6% | Similar increase observed in older adults |
| Co-occurrence | Both multimorbidity & polypharmacy | 14.3% | 13.5% | Approximately 20% in older adults |
These epidemiological data highlight several critical patterns. Females consistently show higher estimates of multimorbidity, polypharmacy, and their co-occurrence across both cohorts and age groups [73]. Additionally, the prevalence of co-occurring multimorbidity and polypharmacy approximately doubles from middle-aged (45-64 years) to older adults (65-85 years), with nearly 20% of older adults experiencing both conditions [73]. These findings have significant implications for ASD trial design, particularly given the lifespan perspective necessary for understanding autism trajectory and treatment.
Metabolic Profiling in ASD
Quantitative analysis of metabolism has emerged as a powerful approach for identifying driver reactions occurring during pathological development [74]. In ASD research, metabolic flux analysis based on material balance provides critical insights into the dynamic behaviors underlying complex metabolic processes [74].
The STELLA algorithm represents an advanced computational method to investigate microbiome dysregulation beyond mere evaluation of microbial composition, instead quantifying metabolites associated with given microbiomic profiles [75]. When applied to ASD datasets, this approach has identified significant alterations in key metabolites that differentiate children with ASD from neurotypical patients.
Methodological Framework for Investigating Co-occurring Conditions
Metabolic Flux Analysis Protocols
Objective: To quantify metabolic activity in central carbon metabolism and identify driver reactions in ASD pathophysiology.
Experimental Workflow:
- Cell Culture Preparation: Establish lymphoblastoid cell lines from ASD patients and matched controls.
- Isotope Labeling: Incubate cells with (^{13})C-labeled glucose tracers (e.g., [1,2-(^{13})C]glucose) for specified duration.
- Metabolite Extraction: Implement rapid quenching of metabolism followed by methanol:water extraction.
- Mass Spectrometry Analysis: Utilize LC-MS/MS for determination of (^{13})C-labeling patterns in intracellular metabolites.
- Flux Calculation: Apply computational modeling to estimate metabolic flux distribution from isotopic labeling data.
- Pathway Analysis: Identify significantly altered pathways through integration with biochemical database.
Key Considerations: Metabolic flux is defined as the number of converted molecules per unit time per cell (mol h(^{-1}) cell(^{-1})) and serves as the definitive parameter for investigating cell metabolism because the activation and inactivation of metabolic pathways can be directly evaluated by determining flux levels [74].
Microbiome-Metabolite Integration Protocol
Objective: To derive ASD-specific metabolic spectra from individual microbiome profiles and identify altered metabolic pathways.
STELLA Algorithm Workflow:
- Data Input: 16S rRNA sequencing data from fecal samples of ASD and neurotypical participants.
- Pathway Retrieval: Query MACADAM and METACYC databases to retrieve metabolic pathways present in microbiota operational taxonomic units (OTUs).
- Stoichiometric Analysis: Calculate production/consumption scores for each metabolite considering reaction stoichiometry and directionality.
- Abundance Weighting: Merge score matrix with OTU abundance data, weighting pathway contributions accordingly.
- Metabolite Estimation: Output quantitative estimates of metabolite concentrations associated with the microbiome profile.
- Batch Effect Correction: Apply singular value decomposition to remove technical artifacts when merging datasets.
- Feature Selection: Perform stepwise feature selection through linear discriminant analysis to identify discriminatory metabolites.
Validation Metrics: The STELLA algorithm demonstrates (F1 = 0.67), (F2 = 0.73), and (F_{1/2} = 0.61) scores, comparable to other metabolite prediction algorithms [75].
Implications for Clinical Trial Design
Stratification Strategies
The conventional approach to ASD trial design often fails to account for the biochemical heterogeneity and co-occurring conditions that significantly impact treatment outcomes. We propose a stratification framework based on pathogenic pathways rather than symptomatic presentations:
- Growth Dysregulation Stratification: Categorize participants by evidence of synaptic overgrowth versus undergrowth patterns.
- Metabolic Profile Grouping: Utilize metabolic flux data to identify subtypes with shared pathway disruptions.
- Comorbidity Burden Tiers: Stratify by number and severity of co-occurring conditions to control for polypharmacy effects.
- Microbiome-Metabolite Alignment: Group participants by shared microbiome-derived metabolic alterations.
Polypharmacy Management in Trial Protocols
The high prevalence of polypharmacy in ASD populations, particularly among older individuals, necessitates specific methodological considerations:
- Medication Interaction Mapping: Pre-trial assessment of potential interactions between investigational products and common concomitant medications.
- Pharmacokinetic Profiling: Enhanced PK sampling for participants on multiple medications to identify clearance alterations.
- Staged Recruitment: Prioritize recruitment of medication-naïve participants in early-phase trials, gradually including those with complex medication regimens in later phases.
- Deprescribing Protocols: Structured approaches for managing necessary medication adjustments during trial participation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for ASD Co-occurrence Studies
| Reagent/Category | Specific Examples | Experimental Function | Application Context |
|---|---|---|---|
| Isotopic Tracers | [1,2-(^{13})C]glucose, [U-(^{13})C]glutamine | Enables metabolic flux analysis by tracing atom transitions | 13C-MFA in patient-derived cell lines |
| Metabolic Sensors | FRET-based NADPH sensors, TFA-based metabolite biosensors | Real-time monitoring of metabolic states in single cells | Live-cell imaging of metabolic fluctuations |
| Pathway Inhibitors | mTOR inhibitors (rapamycin), ERK pathway modulators | Experimental manipulation of key ASD-related pathways | Target validation in animal models |
| Sequencing Reagents | 16S rRNA sequencing kits, metagenomic libraries | Characterization of gut microbiome composition | Microbiome-metabolite integration studies |
| Mass Spectrometry Standards | Stable isotope-labeled internal standards | Absolute quantification of metabolite concentrations | Targeted metabolomics profiling |
Visualizing Pathway Relationships and Experimental Workflows
Pathway Convergence in ASD Pathogenesis: This diagram illustrates how diverse genetic risk factors in ASD converge on a limited number of key biochemical pathways, which subsequently affect specific neural circuits and ultimately manifest as co-occurring conditions (multimorbidity) and complex medication regimens (polypharmacy).
Integrated Experimental Workflow for ASD Co-occurrence Studies: This diagram outlines a comprehensive methodological approach for investigating co-occurring conditions in ASD, incorporating multi-omics data collection, computational integration, and clinical application for improved trial design and polypharmacy management.
The complex interplay between ASD pathophysiology, multimorbidity, and polypharmacy necessitates a fundamental shift in clinical trial design and therapeutic development. By recognizing the convergence of diverse genetic lesions onto limited biochemical pathways, researchers can develop more targeted stratification approaches that account for both core ASD features and co-occurring conditions. The integration of metabolic profiling, microbiome analysis, and systematic assessment of medication interactions provides a pathway toward personalized interventions that address the multifaceted nature of autism across the lifespan. As our understanding of these relationships deepens, trial methodologies must evolve to incorporate these complexities, ultimately leading to more effective, tailored approaches for individuals with ASD and co-occurring conditions.
The translation of preclinical research into clinically effective treatments represents one of the most significant challenges in modern biomedical science, particularly in complex neurodevelopmental disorders such as autism spectrum disorder (ASD). With attrition rates exceeding 90% for novel therapeutic candidates and the average cost of developing a single successful drug exceeding $2.6 billion, the imperative to bridge this translational gap has never been more pressing [76]. This comprehensive review examines the multifaceted challenges inherent in the translational pipeline and presents evidence-based strategies to enhance the predictive validity and clinical relevance of preclinical research, with a specific focus on ASD pathophysiology. By integrating advances in biochemical pathway analysis, refined animal models, computational approaches, and structured frameworks for evidence assessment, we outline a systematic approach to navigating the "valley of death" between bench discoveries and bedside applications.
Autism spectrum disorder is characterized by persistent deficits in social communication and interaction, alongside restricted, repetitive patterns of behavior, interests, or activities [77]. The etiological complexity of ASD presents particular challenges for therapeutic development, with approximately 85% of cases classified as idiopathic (without a known specific cause) and only 15% classified as secondary to identifiable genetic or environmental factors [77]. The molecular pathogenesis of ASD involves diverse pathways including transcriptional regulation, proteostasis, cytoskeletal organization, synaptic development and plasticity, neuroinflammation, and metabolic disturbances [77] [19].
The traditional linear model of therapeutic development—proceeding sequentially from basic target identification through animal testing to human clinical trials—has proven inadequate for addressing this complexity. This is evidenced by the high failure rates of clinical trials; approximately 50% of experimental drugs fail in Phase III trials, and only 0.1% of drug candidates ultimately receive regulatory approval [76]. In the context of ASD, where heterogeneity is the rule rather than the exception, this translational gap is particularly pronounced, necessitating novel approaches to preclinical research and validation.
Current Challenges in Translational Research for ASD
Limitations in Preclinical Models
Animal models of ASD, while invaluable for understanding basic mechanisms, frequently fail to recapitulate the full complexity of the human condition. Key limitations include:
- Narrow experimental conditions that do not account for the varied age, genetic makeup, and environmental factors present in human populations [78]
- Species-specific differences in physiology and neural circuitry that limit extrapolation to humans
- Inadequate representation of clinical heterogeneity, with most models focusing on single genetic alterations while most ASD cases involve complex polygenic interactions [77]
- Behavioral tests with limited translational validity for core ASD symptoms such as social communication deficits
Methodological and Conceptual Hurdles
Beyond model limitations, several methodological issues plague the translational pipeline:
- Poor hypothesis formulation and insufficient attention to clinical relevance during early-stage discovery [76]
- Irreproducible data stemming from underpowered studies, publication bias, and insufficient methodological rigor
- Inadequate statistical approaches that overestimate effect sizes and fail to account for multiple comparisons
- Organizational and funding structures that prioritize novel discoveries over translational validation [76]
Table 1: Major Challenges in Translating ASD Preclinical Research
| Challenge Category | Specific Limitations | Impact on Translation |
|---|---|---|
| Model Systems | Single-species focus, limited genetic diversity, narrow age representation | Reduced predictive validity for heterogeneous human populations |
| Experimental Design | Small sample sizes, narrow experimental conditions, inadequate controls | Overestimation of therapeutic efficacy, failure to identify adverse effects |
| Methodological | Poorly characterized biomarkers, subjective behavioral assessments | Difficulty correlating preclinical findings with clinical endpoints |
| Analytical | Inappropriate statistical methods, publication bias toward positive results | Inflated effect sizes, irreproducible findings |
Biochemical Pathways in ASD Pathogenesis: Therapeutic Targets and Translation Challenges
The molecular pathophysiology of ASD involves dysregulation across multiple interconnected biological systems. Understanding these pathways is essential for developing targeted interventions with improved translational potential.
Key Signaling Pathways in ASD
GABAergic/Glutamatergic Imbalance: Reduced expression of GABAA and GABAB receptor subunits and decreased differentiation of GABAergic neurons contribute to neural network dysfunction in ASD [77]. The excitation-inhibition ratio appears to play a role in synaptic homeostasis rather than directly causing hyperexcitability [77].
Calcium Signaling Dysregulation: Mutations in CACNA1C (encoding L-type voltage gated calcium channels), impaired inositol triphosphate receptors, and presynaptic Ca2+-activated K+ channel mutations have all been linked to ASD pathogenesis [77].
ERK Signaling Pathway: Dysregulation of the ERK pathway has been implicated in numerous syndromic forms of autism, including Fragile X syndrome, 16p11.2 deletion syndrome, tuberous sclerosis, and Phelan-McDermid syndrome [79]. Transcriptomic analyses of post-mortem brain tissue from individuals with ASD have revealed significant alterations in ERK signaling pathways [79].
Wnt-ERK Signaling Axis: Recent research has identified the Wnt5a-Erk axis as a critical regulator of oligodendrocyte dysfunction in Shank3-related ASD. Shank3 deficiency induces hyperactivation of the Erk signaling pathway, compromising oligodendrocyte maturation and contributing to hypomyelination [79].
Additional Pathophysiological Mechanisms
Neuroinflammation: Elevated levels of inflammatory cytokines, anti-brain autoantibodies, and maternal immune dysregulation during pregnancy have been reported in ASD [77]. Cerebellar pathology with immune dysregulation and abnormal cytokine alterations has been identified in post-mortem ASD brains [77].
Metabolic and Gut-Brain Axis Disruption: Reduced production of indole-3-propionic acid, a tryptophan metabolite of gut microbiota, due to a dysregulated microbiota-IPA-brain axis increases ASD susceptibility [77]. Abnormal lipid metabolism pathways, including decreased lipid metabolism and increased sphingolipid and fatty acid byproducts, have been observed in ASD subgroups [77].
Vitamin D Deficiency: As a neurosteroid with neuroprotective roles, vitamin D deficiency has been associated with ASD, with children with ASD showing significantly lower serum levels (13.79 ± 1.03 ng/ml) compared to healthy controls (16.58 ± 1.06 ng/ml) [77].
Table 2: Key Biochemical Pathways in ASD Pathogenesis and Translation Challenges
| Pathway | Molecular Components | ASD Associations | Translation Challenges |
|---|---|---|---|
| ERK Signaling | Shank3, Erk1/2, Wnt5a | Hyperactivation in Shank3 deficiency, oligodendrocyte dysfunction, myelination deficits | Pathway cross-talk, compensatory mechanisms in humans |
| GABA/Glutamate | GABAA/B receptors, glutamate receptors | Excitation/inhibition imbalance, sensory processing abnormalities | Species differences in receptor distribution and function |
| Calcium Signaling | CACNA1C, IP3R, BKCa channels | Altered neurotransmitter release, synaptic dysfunction | Pleiotropic effects throughout nervous system |
| Neuroimmune | Cytokines, microglia, autoantibodies | Cerebellar inflammation, altered brain development | Temporal specificity of interventions, blood-brain barrier penetration |
Visualization of Key ASD-Relevant Signaling Pathways
Shank3-ERK-Oligodendrocyte Pathway in ASD
Integrated ASD Pathophysiology and Therapeutic Targeting
Strategic Framework for Enhancing Translational Success
PATH Framework: Preclinical Assessment for Translation to Humans
The PATH framework provides a structured approach for assessing evidence supporting early-phase trials [80]. This methodology requires connecting nine mechanistic steps supporting a clinical claim through:
- Parsing supporting evidence across multiple lines of investigation
- Assessing evidence strength at each step in the mechanistic pathway
- Evaluating the complete chain of evidence linking drug administration to clinical effect
This approach reduces opacity, arbitrariness, and biases in current ways of presenting and assessing scientific support for early-phase trials [80].
Robustness-Based Preclinical Validation
Enhancing robustness—defined as stability/reproducibility in the face of challenges—represents a key strategy for improving translational success [78]. This involves:
- Testing therapeutic approaches across multiple animal models with different genetic backgrounds
- Incorporating age and sex as biological variables in experimental designs
- Utilizing environmental challenges to assess resilience of therapeutic effects
- Employing multi-center preclinical trials to identify site-specific effects
Advanced Model Systems and Computational Approaches
Human-Centric AI Platforms: Tools like Causaly enable identification and exploration of biochemical pathways by extracting and analyzing relationships from millions of scientific papers, helping prioritize targets and understand pathway interactions [81].
Biochemical Pathway Modeling: Computational tools based on mathematical modeling of biomedically relevant networks and pathways allow for description and analysis of signaling, genetic and metabolic networks involved in complex diseases [82].
Organoid and CTiD Approaches: Three-dimensional organoids and "clinical trials in a dish" (CTiD) techniques enable testing of promising therapies for safety and efficacy on human cells, allowing drug development for specific populations [83].
Drug Repurposing Strategies: Identifying new uses for existing drugs can shorten development timelines to 4-5 years with reduced risk and cost, as these compounds have already passed early safety hurdles [83].
Table 3: Strategies for Enhancing Translational Success in ASD Therapeutic Development
| Strategy | Key Components | Application in ASD |
|---|---|---|
| PATH Framework | Mechanistic step validation, evidence chain assessment, bias reduction | Systematic evaluation of targets like mGluR5, OXTR, or ERK pathway modulators |
| Robustness Testing | Multi-model validation, environmental challenges, diverse genetic backgrounds | Testing interventions across multiple ASD models (e.g., Shank3, Fmr1, BTBR) |
| Computational Modeling | Pathway analysis, target prioritization, network pharmacology | Identification of key nodes in ASD-relevant signaling networks |
| Human Biomimetic Systems | Organoids, CTiD, human tissue models | Testing cell-type specific effects in human-derived neural systems |
Experimental Protocols for Enhanced Translational Research
Oligodendrocyte Differentiation Protocol for Myelination Studies
Based on recent research investigating Shank3-related oligodendrocyte alterations [79]:
- Cortical Dissection: Isolate cortical tissue from postnatal day 0-2 (P0-P2) wild-type Shank3(+/+) mouse pups
- Mixed Glial Culture: Seed dissociated cortical tissue in poly-L-lysine-coated (0.1 mg/ml) 75 cm² flasks
- Culture Medium: Maintain cells in OPC medium consisting of DMEM supplemented with L-glutamine, 4.5 g/l glucose, 1% sodium pyruvate, 2% B27, 1% FBS, 1% Pen-Strep, 10 ng/mL human FGF-basic, and 30 ng/mL rhPDGF-AA
- Medium Refreshment: Replenish medium every 2-3 days until confluence
- Insulin Supplementation: At 7 days in vitro (DIV), supplement OPC medium with insulin (5 μg/ml final concentration)
- OPC Isolation: At 9 DIV, isolate oligodendrocyte precursor cells using 0.25% trypsin, centrifuge, and seed at density of 2.5 × 10⁴ cells/cm² onto laminin-coated dishes
- Differentiation Induction: One day post-purification, replace medium completely with differentiation medium containing DMEM with 2% B27, 1% FBS, 1% Pen-Strep, and differentiation additives including apo-transferrin (100 μg/ml), BSA (100 μg/ml), sodium selenite (40 μg/ml), progesterone (60 ng/ml), putrescine (16 μg/ml), insulin (5 μg/ml), bFGF (10 ng/ml), T3 (30 ng/ml), and thyroxine (40 ng/ml)
- Analysis Timing: Cultures are ready for immunocytochemical analysis and pharmacological treatments after 4 or 10 days in differentiation medium
In Vivo Pharmacological Rescue Protocol
- Animal Model: Shank3Δ11(−/−) mice and wild-type controls
- Compound Administration: Mirdametinib (30 mg/kg body weight in saline with 1% DMSO) or vehicle (saline with 1% DMSO)
- Dosing Schedule: Intraperitoneal injection once daily for six days per week over 4-5 weeks
- Treatment Window: Begin treatment on postnatal day (P) 27-P29, sacrifice animals on P60-P62
- Outcome Measures: Biochemical analysis of myelination proteins, behavioral assessment of autism-related phenotypes, motor function tests
Research Reagent Solutions for ASD Translational Research
Table 4: Essential Research Reagents for ASD Pathway Investigation
| Reagent/Category | Specific Examples | Research Application | Function in ASD Studies |
|---|---|---|---|
| Animal Models | Shank3Δ11(−/−) mice, BTBR T+ tf/J, Fmr1 KO mice | In vivo pathophysiological and therapeutic studies | Recapitulate specific genetic alterations associated with ASD |
| Cell Culture Systems | Primary oligodendrocyte cultures, cortical neurons | Mechanistic studies in controlled environments | Investigate cell-type specific effects of ASD-related mutations |
| Signaling Modulators | Mirdametinib (ERK inhibitor), Wnt3a/Wnt5a, Ozuriftamib (Anti-ROR2) | Pathway manipulation and validation | Target specific dysregulated pathways in ASD |
| Differentiation Media | OPC medium, oligodendrocyte differentiation medium | Cell fate and maturation studies | Investigate developmental processes relevant to ASD |
| Antibodies | Anti-MBP, anti-Shank3, anti-phospho-ERK | Protein detection and quantification | Assess molecular and structural changes in ASD models |
| Cytokines/Growth Factors | rhPDGF-AA, human FGF-basic, BDNF, NT-3 | Cell signaling and survival studies | Modulate pathways involved in neural development |
Bridging the gap between preclinical findings and clinically effective treatments for ASD requires a multifaceted approach that addresses the complexity of the disorder and the limitations of current models. By implementing structured frameworks like PATH for evidence assessment, enhancing robustness through multi-model validation, leveraging computational approaches for pathway analysis and target prioritization, and employing human-relevant systems such as organoids and CTiD, the translational success rate for ASD therapeutics can be significantly improved.
The integration of these strategies—combined with a deepened understanding of ASD-relevant biochemical pathways such as the Wnt5a-Erk axis in oligodendrocyte dysfunction—provides a roadmap for navigating the "valley of death" in therapeutic development. As these approaches continue to evolve and be refined, they offer the promise of accelerating the delivery of effective, mechanism-based treatments for individuals with ASD, ultimately bridging the persistent gap between preclinical promise and clinical reality.
Validation and Comparative Analysis of Emerging ASD Mechanisms and Interventions
Cerebral Folate Deficiency (CFD) is a neurological syndrome characterized by severely low folate levels in the central nervous system despite normal peripheral folate status. This whitepaper examines the validation of leucovorin (folinic acid) as a targeted therapy for CFD, with a specific focus on its implications for understanding biochemical pathways in autism spectrum disorder (ASD) pathogenesis. Emerging research indicates that a significant subset of individuals with ASD presents with CFD, often associated with folate receptor alpha (FRα) autoantibodies that disrupt folate transport across the blood-brain barrier. The targeted mechanism of leucovorin, which bypasses this impaired transport, offers a compelling model for developing biomarker-driven treatments for neurodevelopmental disorders.
Cerebral Folate Deficiency (CFD) is defined as any neuropsychiatric or developmental disorder characterized by decreased cerebrospinal fluid (CSF) levels of 5-methyltetrahydrofolate (5-MTHF)—the active folate metabolite in the CNS—in the presence of normal folate status outside the nervous system [84]. The primary cause of CFD is identified as impaired folate transport into the brain, frequently mediated by the presence of serum folate receptor-alpha (FRα) autoantibodies [85] [84]. These autoantibodies are reported in 58% to 76% of children with ASD, compared to approximately 10-15% of the general population [85] [86], establishing a significant pathophysiological link between folate metabolism and a subtype of autism.
The recognition of CFD as a treatable contributor to ASD symptomatology represents a paradigm shift in autism research, moving from purely behavioral management to targeted biological intervention. FRα autoantibodies impair folate transport by binding to and blocking the FRα protein, which is responsible for active folate transport across the choroid plexus into the CSF [85] [84]. This transport disruption creates a cerebral folate deficiency that affects critical neurodevelopmental processes, including purine and thymidine synthesis, neurotransmitter production, DNA methylation, and glutathione-mediated antioxidant activity [85].
Biochemical Pathways: Folate Transport Mechanisms and the Site of Leucovorin Action
Folate transport into the central nervous system is a specialized process primarily mediated by the folate receptor alpha (FRα) at the choroid plexus. Understanding this mechanism is crucial for appreciating leucovorin's therapeutic action.
Normal Folate Transport Across the Blood-Brain Barrier
The primary circulating folate form, 5-methyltetrahydrofolate (5-MTHF), is transported across the blood-brain barrier through a coordinated mechanism involving FRα and the proton-coupled folate transporter (PCFT) [84]. Through energy-dependent endocytosis, folate bound to FRα is transported from the apical to the basolateral side of choroid plexus epithelial cells against a concentration gradient, maintaining CNS folate levels several times higher than in serum [85]. This active transport is essential for normal neurodevelopment and neurological function.
Pathophysiology of CFD and FRα Autoantibodies
In CFD, particularly cases associated with FRα autoantibodies, this transport system becomes compromised. Two types of autoantibodies have been identified:
- Blocking autoantibodies: Directly interfere with folate binding to FRα
- Binding autoantibodies: Bind to FRα without complete receptor blockade but may still impair function [85] [84]
Both types correlate with reduced CSF folate concentrations, creating a functional deficiency within the CNS despite normal systemic folate levels [85].
Leucovorin's Bypass Mechanism
Leucovorin (5-formyltetrahydrofolate) represents a reduced folate form that can utilize the reduced folate carrier (RFC), an alternate transport pathway with lower folate affinity but sufficient capacity when administered at therapeutic doses [85]. This bypass mechanism allows leucovorin to circumvent the FRα blockade, delivering folate to the CNS through an alternative route and addressing the core transport defect in CFD.
The following diagram illustrates the normal folate transport pathway, the disruption caused by FRα autoantibodies in CFD, and leucovorin's bypass mechanism via the RFC transporter:
Quantitative Clinical Evidence: Efficacy of Leucovorin in CFD and ASD
The therapeutic efficacy of leucovorin for CFD, particularly in ASD populations with FRα autoantibodies, is supported by clinical studies ranging from case reports to controlled trials. The table below summarizes key quantitative findings from the literature:
Table 1: Clinical Evidence for Leucovorin in CFD and ASD
| Study Type | Patient Population | Dosing Regimen | Key Efficacy Outcomes | FRAA Status Correlation |
|---|---|---|---|---|
| Case Series (Frye et al.) | Children with CFD & ASD symptoms [85] | 0.5-2 mg/kg/day | Marked improvement in neurological, behavioral, and cognitive symptoms; substantial improvements in language and communication [85] | FRAA positive |
| Open-Label Study (Frye & Rossignol) | 44 children with ASD [85] | 2 mg/kg/day (max 50 mg) for 4 months | ~67% showed improvement in receptive and expressive language; significant improvement in verbal communication and stereotypical behavior vs. controls [85] | 100% FRAA positive |
| Randomized Controlled Trial (Panda et al., 2024) | Children with ASD [86] | Not specified | Positive outcomes in communication and social interaction [86] | Benefit regardless of FRAA status |
| Clinical Response Rates (Various) | ASD with FRAA [86] | 0.5-2 mg/kg/day | Improvements in core ASD symptoms, especially verbal communication [86] | 58-76% FRAA positive in ASD |
The most robust improvements have been observed in verbal communication, with one open-label study reporting approximately 67% of children showing enhancement in both receptive and expressive language skills after a mean treatment duration of four months [85]. These benefits appear particularly pronounced in children positive for FRα autoantibodies, though recent evidence suggests potential efficacy regardless of autoantibody status [86].
Experimental Protocols: Methodologies for Clinical Validation
Diagnostic Workflow for CFD in ASD Populations
The accurate identification of CFD requires a structured diagnostic approach:
- Clinical Assessment: Document neurological symptoms (developmental regression, seizures, movement disorders) and ASD behavioral profiles [87] [84]
- CSF Analysis: Measure 5-MTHF levels (definitive diagnosis requires CSF 5-MTHF ≤10 nmol/L with normal peripheral folate) [87] [84]
- FRα Autoantibody Testing: Assess serum for blocking and binding antibodies (though test standardization remains limited) [86] [88]
- Genetic Analysis: Sequence FOLR1 gene for loss-of-function mutations in suspected hereditary cases [87]
- Exclusion of Confounders: Rule out vitamin B12 deficiency, MTHFR polymorphisms, and other metabolic disorders [88]
Dosing and Treatment Protocol
Based on clinical studies, the following treatment protocol has emerged:
- Initial Dose: 0.5 mg/kg/day divided twice daily (morning and evening) [86]
- Titration: Gradually increase to 2 mg/kg/day (maximum 50 mg/day) as tolerated [86] [88]
- Formulation: Tablets (5 mg, 10 mg, 15 mg, 25 mg) that may be split or crushed [86]
- Duration: Evaluate progress at 12-24 weeks; maximal gains often appear after 4-6 months of continuous use [86]
Outcome Measurement Strategies
- Primary Endpoints: Standardized measures of verbal communication, social interaction, and adaptive behavior [85] [86]
- Secondary Endpoints: Reduction in repetitive behaviors, improvement in attention, and neurological symptoms [85]
- Safety Monitoring: Assessment of agitation, insomnia, GI symptoms, and potential masking of B12 deficiency [86] [88]
The following workflow diagram outlines the comprehensive diagnostic and treatment protocol for managing CFD in ASD:
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Research into leucovorin as a targeted therapy for CFD requires specific reagents, assays, and methodological approaches. The following table details essential components of the CFD research toolkit:
Table 2: Essential Research Reagents and Methodologies for CFD Investigations
| Reagent/Method | Function/Application | Research Context |
|---|---|---|
| d,l-Leucovorin (Racemic Mixture) | Active intervention; composed of 1:1 mixture of dextrorotary and levorotary isomers [89] | Clinical trials; in vivo studies |
| l-Leucovorin (Active Isomer) | Pharmacologically active levo-isomer; rapidly converted to biologically available methyl-tetrahydrofolate [90] [89] | Mechanistic studies; targeted interventions |
| FRα Autoantibody Assay | Detection of serum blocking and binding antibodies to folate receptor alpha [85] [86] | Patient stratification; biomarker correlation |
| CSF 5-MTHF Measurement | Quantification of 5-methyltetrahydrofolate in cerebrospinal fluid (gold standard CFD diagnosis) [87] [84] | Diagnostic confirmation; treatment monitoring |
| FOLR1 Gene Sequencing | Identification of loss-of-function mutations in folate receptor alpha gene [87] | Genetic CFD diagnosis; mechanistic studies |
| Reduced Folate Carrier (RFC) Expression Systems | In vitro models to study leucovorin transport via alternate pathway [85] [90] | Mechanistic transport studies |
| PCFT Transport Assays | Evaluation of proton-coupled folate transporter activity [90] [84] | Intestinal absorption and CNS transport studies |
Regulatory Landscape and Future Research Directions
The regulatory environment for leucovorin in CFD is evolving. In 2025, the FDA initiated a fast-tracked approval process for leucovorin specifically for CFD indication, though this pending approval does not extend to autism in general [91] [88]. This regulatory recognition underscores the validity of CFD as a distinct neurological entity and leucovorin as its targeted treatment.
Critical research gaps remain, particularly regarding optimal patient selection, long-term outcomes, and the fundamental mechanisms linking cerebral folate status to neurodevelopment. Future research priorities should include:
- Biomarker Validation: Standardization and FDA-approval of FRα autoantibody testing [88]
- Predictive Modeling: Identification of clinical and biochemical factors predicting treatment response [86] [88]
- Longitudinal Studies: Assessment of long-term efficacy and safety in pediatric populations [88]
- Mechanistic Elucidation: Further exploration of folate's role in neurodevelopmental pathways [85] [84]
The validation of leucovorin as a targeted therapy for Cerebral Folate Deficiency represents a significant advancement in precision medicine for neurodevelopmental disorders. By addressing a specific metabolic impairment in a defined ASD subgroup, this approach exemplifies the potential of biomarker-driven interventions in heterogeneous conditions like autism. The mechanistic basis—bypassing autoantibody-blocked folate transport—provides a robust biochemical rationale for treatment efficacy, particularly for the 58-76% of children with ASD who test positive for FRα autoantibodies. As research continues to refine diagnostic criteria and predictive biomarkers, leucovorin therapy offers a compelling model for developing targeted treatments that address the underlying pathophysiology of specific autism subtypes.
The therapeutic landscape for autism spectrum disorder (ASD) is undergoing a paradigm shift, moving from a one-size-fits-all symptom-management approach towards precision medicine strategies that target specific biological pathways. This whitepaper provides a comparative analysis of mechanism-based versus symptom-based treatment strategies, evaluating their efficacy, methodological frameworks, and application in ASD. We synthesize recent breakthroughs in autism subclassification that enable meaningful targeting of biological mechanisms and review the clinical trial outcomes for therapies developed against specific signaling pathways. For researchers and drug development professionals, this review offers a technical guide to the experimental models, reagent solutions, and methodological considerations essential for advancing mechanism-based therapeutics in complex neurodevelopmental disorders.
Autism spectrum disorder (ASD) is a clinically and etiologically heterogeneous neurodevelopmental condition characterized by core deficits in social communication and the presence of restricted, repetitive behaviors [26]. The historical understanding of autism has evolved substantially from its initial description in the 1940s to the current conceptualization as a spectrum disorder with strong biological underpinnings [92] [26]. This evolution has directly informed therapeutic approaches, which have traditionally focused on managing observable symptoms through behavioral, educational, and pharmacological interventions that target co-occurring conditions rather than core pathophysiology [93].
The highly heritable nature of ASD and advances in genomic technologies have revealed hundreds of genes associated with autism risk, converging on several key signaling pathways and biological processes [92] [26]. This genetic complexity presents both challenges and opportunities for therapeutic development. Mechanism-based therapeutics represent a novel approach that targets specific pathological processes identified through genetic findings, rather than focusing solely on symptomatic manifestations [94]. This approach differs fundamentally from symptom-based treatments, which aim to reduce behavioral challenges without addressing their underlying biological causes.
Recent research has enabled significant progress in deconstructing autism heterogeneity. A landmark 2025 study identified four biologically distinct subtypes of autism through person-centered analysis of over 5,000 individuals in the SPARK cohort [3] [4] [2]. These subtypes—Social and Behavioral Challenges, Mixed ASD with Developmental Delay, Moderate Challenges, and Broadly Affected—exhibit distinct developmental trajectories, co-occurring conditions, and critically, different patterns of genetic variation affecting discrete biological pathways [3] [2]. This refined subclassification provides a crucial framework for evaluating mechanism-based treatment strategies in biologically coherent patient populations.
Autism Pathogenesis: Key Signaling Pathways and Biological Mechanisms
Genetic Landscape of ASD
ASD exhibits substantial heritability, with current evidence indicating complex genetic architecture involving both rare mutations with large effects and common variants with small effects [92] [26]. Monogenic forms of ASD, though individually rare, provide critical insights into disease mechanisms. Several well-characterized genetic syndromes including Fragile X Syndrome (FMR1), Tuberous Sclerosis Complex (TSC1/TSC2), Rett Syndrome (MECP2), and Phelan-McDermid Syndrome (SHANK3) have high rates of ASD comorbidity and have become testbeds for mechanism-based therapeutic development [94] [92] [26].
Table 1: Key Monogenic Syndromes Associated with ASD and Their Signaling Pathways
| Gene/Syndrome | Primary Function | Affected Signaling Pathways | ASD Comorbidity Rate |
|---|---|---|---|
| FMR1 (Fragile X) | RNA metabolism, translational regulation | mGluR5, MAPK, PI3K | 30-60% |
| TSC1/TSC2 (Tuberous Sclerosis) | Cell growth, proliferation regulation | mTOR, PI3K/AKT | 40-50% |
| MECP2 (Rett Syndrome) | Transcriptional regulation, chromatin remodeling | BDNF, IGF-1, mTOR | 50-80% |
| SHANK3 (Phelan-McDermid) | Synaptic scaffolding protein | mTOR, synaptic plasticity | 75-80% |
| PTEN | Phosphatase, cell cycle regulation | PI3K/AKT/mTOR | 20-30% |
Convergent Signaling Pathways in ASD Pathogenesis
Despite genetic heterogeneity, research has revealed remarkable convergence of ASD-risk genes on several key signaling pathways and biological processes. The identification of these shared mechanisms across genetically distinct forms of ASD provides validated targets for therapeutic development [94] [26].
The mTOR signaling pathway has emerged as a central node in ASD pathogenesis, integrating signals from various ASD-associated genes to regulate protein synthesis, cell growth, and synaptic plasticity [94] [26]. Dysregulation of mTOR signaling is particularly prominent in TSC, PTEN-associated ASD, and Fragile X syndrome. The mGluR5 pathway represents another key mechanism, with evidence suggesting that Group 1 metabotropic glutamate receptor signaling is hyperactive in Fragile X syndrome due to loss of FMRP-mediated translational repression [94].
Additionally, impairments in synaptic development and function are common across multiple forms of ASD, with genes such as SHANK3, NRXN1, and NLGN3 affecting the formation, maturation, and maintenance of neuronal connections [92]. Chromatin remodeling and transcriptional regulation pathways are disrupted in syndromes such as Rett (MECP2) and CHARGE (CHD8), leading to altered gene expression profiles during critical periods of brain development [92]. Finally, growth factor signaling pathways, particularly those involving BDNF and IGF-1, are dysregulated in several ASD models and contribute to impaired neuronal development and circuit formation [94].
Diagram 1: Signaling Pathway Integration in ASD Pathogenesis. This diagram illustrates how genetically distinct forms of ASD converge on common signaling pathways that ultimately lead to shared phenotypic manifestations. Key nodes represent potential targets for mechanism-based therapeutics.
Mechanism-Based Treatment Strategies: Targeted Biological Interventions
Preclinical Foundations and Molecular Targets
Mechanism-based therapies for ASD are predicated on detailed understanding of pathological processes arising from specific genetic mutations. These approaches target the cascading molecular consequences of genetic risk factors, with the goal of normalizing disrupted biological processes rather than merely alleviating symptoms [94].
In Fragile X syndrome, loss of FMRP leads to exaggerated mGluR5-dependent protein synthesis and subsequent synaptic dysfunction. Preclinical studies demonstrated that genetic reduction or pharmacological inhibition of mGluR5 could rescue cellular and behavioral phenotypes in Fmr1 knockout mice [94]. This provided the foundation for clinical trials of mGluR5 antagonists such as mavoglurant and basimglurant.
For Tuberous Sclerosis Complex, mutations in TSC1 or TSC2 cause dysregulated mTOR signaling due to loss of inhibition of the mTOR complex 1. Rapamycin (sirolimus) and its analog everolimus inhibit mTOR activation and have shown efficacy in rescuing cognitive deficits and autistic-like features in TSC mouse models [94] [26].
In Rett syndrome, mutations in MECP2 reduce expression of growth factors including BDNF and IGF-1. IGF-1 treatment in Mecp2 mutant mice rescues a broad range of RTT-like phenotypes including social, motor, and respiratory abnormalities, providing rationale for clinical testing [94].
Clinical Trial Outcomes for Mechanism-Based Therapies
Despite promising preclinical results, the translation of mechanism-based therapies for neurodevelopmental aspects of ASD has faced significant challenges. Clinical trials have yielded mixed results, highlighting the complexities of targeting biological mechanisms in human populations.
Table 2: Clinical Trial Outcomes for Selected Mechanism-Based Therapies in Genetic Forms of ASD
| Therapeutic Agent | Target | Genetic Syndrome | Trial Phase | Primary Outcome | Key Findings |
|---|---|---|---|---|---|
| Mavoglurant | mGluR5 antagonist | Fragile X | Phase IIb/III | ABC-C, ADAMS | No significant effect on primary endpoints [94] |
| Basimglurant | mGluR5 antagonist | Fragile X | Phase IIb/III | ABC-C, ADAMS | No significant effect on primary endpoints [94] |
| Everolimus | mTOR inhibitor | TSC | Phase II/III | Neurocognitive measures | No significant effect on primary endpoints [94] |
| Sirolimus | mTOR inhibitor | TSC | Early-phase | Cognitive endpoints (secondary) | Pro-cognitive effects in open-label trial [94] |
| IGF-1 (Mecasermin) | IGF-1 receptor agonist | Rett Syndrome | Phase I/II | CGI, autonomic measures | Mixed results; improved autonomic function but not CGI [94] |
| Trofinetide | IGF-1 tripeptide analog | Rett Syndrome | Phase II | VABS, CGI | Improvement in clinical impressions and adaptive behavior [94] |
The variable outcomes in these trials underscore several methodological challenges. For mGluR5 antagonists in Fragile X syndrome, early-phase trials suggested potential efficacy on the Aberrant Behavior Checklist (ABC) in post-hoc analyses of patients with complete FMR1 silencing, but larger subsequent trials failed to demonstrate significant effects on primary outcome measures [94]. Similarly, while mTOR inhibitors show clear benefit for somatic manifestations in TSC and seizure control, their effects on neurocognitive endpoints have been limited [94].
Experimental Protocols for Mechanism-Based Therapeutic Development
Preclinical Validation Pipeline
The development of mechanism-based therapies requires rigorous preclinical validation across multiple model systems. Standard protocols include:
In vitro mechanistic studies: Utilize patient-derived induced pluripotent stem cells (iPSCs) differentiated into neurons to assess molecular pathway dysregulation and perform high-content screening of candidate compounds. Protocol includes RNA sequencing to confirm pathway engagement and multielectrode arrays for functional neuronal assessment.
Animal model therapeutic testing: Employ genetically modified mouse models (e.g., Fmr1 KO, Mecp2 mutant, Tsc1/2 heterozygous) for in vivo efficacy studies. Standardized behavioral batteries include social approach tests, repetitive behavior assessments, and cognitive assays such as Morris water maze or fear conditioning. Treatment typically initiated during critical developmental windows (e.g., 4-8 weeks of age) with longitudinal assessment.
Biomarker development: Incorporate electrophysiological (EEG), neuroimaging (DTI, fMRI), and molecular biomarkers to demonstrate target engagement and biological effect prior to clinical translation.
Clinical Trial Methodological Considerations
Optimized clinical trial designs for mechanism-based therapies in ASD include:
Patient stratification: Enrollment based on specific genetic mutations and consideration of additional stratification factors such as methylation status in Fragile X or ASD co-diagnosis in TSC [94].
Critical window timing: Intervention during developmental periods of maximum plasticity, as evidenced by ongoing trials of basimglurant in younger children with Fragile X (NCT02920892) based on hypothesis that previous trials failed due to intervention outside optimal neurodevelopmental window [94].
Endpoint selection: Combination of primary behavioral outcomes with secondary biomarker assessments to demonstrate proof of mechanism. Examples include white matter fractional anisotropy in TSC trials as a marker of target engagement [94].
Symptom-Based Treatment Strategies: Current Standard of Care
Behavioral and Educational Interventions
Symptom-based approaches represent the current standard of care for ASD and focus on reducing core behavioral symptoms and improving adaptive functioning without targeting underlying biological mechanisms [93]. These interventions are categorized into several modalities:
Behavioral approaches such as Applied Behavior Analysis (ABA) use principles of reinforcement to shape behaviors and teach new skills. Discrete Trial Training (DTT) breaks skills into discrete components, while Pivotal Response Training (PRT) targets core pivotal areas such as motivation and self-management [93]. These interventions have the strongest evidence base for treating symptoms of ASD.
Developmental approaches focus on building specific developmental skills through structured interactions. The Early Start Denver Model (ESDM) integrates developmental and behavioral principles for children 12-48 months, using play-based activities to improve social, communication, and cognitive skills [95] [93]. Speech and language therapy and occupational therapy address specific functional impairments.
Educational approaches such as the Treatment and Education of Autistic and Related Communication-Handicapped Children (TEACCH) method utilize structured teaching environments with visual supports and predictable routines to accommodate learning styles associated with ASD [93].
Pharmacological Management of Co-occurring Symptoms
Pharmacological treatments for ASD primarily target co-occurring symptoms rather than core social-communication deficits. No medications are currently approved specifically for the core symptoms of ASD [93].
Common medication classes include:
- Atypical antipsychotics (risperidone, aripiprazole) for irritability, aggression, and self-injurious behavior
- Stimulants and non-stimulants for attention deficits and hyperactivity
- Selective serotonin reuptake inhibitors for anxiety and repetitive behaviors
- Anticonvulsants for seizure disorders common in ASD
These symptomatic treatments require careful monitoring of side effects and are typically implemented as part of a comprehensive intervention plan [93].
Comparative Analysis: Efficacy, Limitations, and Future Directions
Efficacy Comparison Across Treatment Modalities
Direct comparison of mechanism-based and symptom-based approaches is challenging due to fundamental differences in therapeutic targets, outcome measures, and populations studied. However, emerging evidence enables preliminary assessment of their relative strengths and limitations.
Table 3: Comparative Analysis of Treatment Strategies for ASD
| Parameter | Mechanism-Based Therapies | Symptom-Based Behavioral Therapies | Symptom-Based Pharmacotherapies |
|---|---|---|---|
| Primary Target | Specific biological pathways (mTOR, mGluR5) | Core ASD symptoms and adaptive skills | Co-occurring symptoms (irritability, ADHD) |
| Theoretical Basis | Molecular pathology identified through genetic studies | Learning theory, developmental psychology | Neurotransmitter systems modulation |
| Evidence Strength | Preclinical: StrongClinical: Limited efficacy to date | Multiple RCTs, extensive clinical validation | FDA-approved for specific co-occurring symptoms |
| Personalization Potential | High (genetically-defined subgroups) | Moderate (individualized based on behavioral profile) | Low to moderate (symptom-based selection) |
| Limitations | Limited efficacy in clinical trials, narrow applicability | Resource-intensive, variable response | Does not address core symptoms, side effects |
| Development Timeline | Long (10+ years for novel compounds) | Rapid implementation possible | Moderate (drug repurposing possible) |
Critical Challenges in Mechanism-Based Therapeutic Development
Several factors have contributed to the limited success of mechanism-based therapies in clinical trials for ASD:
Placebo effects: Substantial placebo responses (effect size ~0.5) in neurodevelopmental disorders reduce signal-to-noise ratio in clinical trials [94].
Endpoint selection limitations: Existing behavioral measures may lack sensitivity to capture specific effects of targeted biological interventions, particularly over short trial durations [94].
Developmental timing: Interventions may need to be delivered during critical developmental windows for maximum effect, as suggested by differential gene expression patterns across subtypes [3] [2].
Biological heterogeneity: Even within genetically defined syndromes, modifier genes and environmental factors create additional variability in treatment response [94].
Target engagement verification: Difficulty demonstrating adequate central nervous system penetration and pathway modulation at safe dosage levels.
Integrated Approaches and Future Directions
The future of ASD treatment lies in integrating mechanism-based and symptom-based approaches within a precision medicine framework. Key strategic priorities include:
Biologically-informed subtyping: Utilization of recently identified autism subtypes with distinct genetic profiles to enrich clinical trials for responsive populations [3] [4] [2].
Biomarker development: Identification and validation of objective measures reflecting both symptomatic features and underlying biological mechanisms to serve as early indicators of efficacy [94].
Combination therapies: Simultaneous targeting of multiple pathways or integration of mechanism-based medications with behavioral interventions to address complexity of ASD pathogenesis.
Developmental timing optimization: Alignment of interventions with critical windows of neurodevelopment informed by subtype-specific patterns of gene expression timing [3] [2].
Diagram 2: Precision Medicine Framework for ASD Treatment. This workflow illustrates an integrated approach to treatment selection that incorporates multiple patient characteristics to optimize therapeutic outcomes through personalized intervention strategies.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Advancing the development of both mechanism-based and symptom-based interventions requires specialized research tools and methodologies. The following table outlines key resources for investigating ASD treatment strategies.
Table 4: Essential Research Reagents and Platforms for ASD Therapeutic Development
| Research Tool Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Genetic Models | Fmr1 KO mice, Mecp2 mutant mice, Tsc1/2 heterozygous mice, Shank3 mutant mice | Preclinical therapeutic testing | Recapitulate specific genetic alterations to study pathological mechanisms and treatment responses |
| Cellular Models | Patient-derived iPSCs, iPSC-derived neurons, cerebral organoids | In vitro screening and mechanistic studies | Model human-specific aspects of neurodevelopment and enable high-throughput compound screening |
| Behavioral Assays | Three-chamber social test, self-grooming analysis, ultrasonic vocalizations, fear conditioning | Preclinical efficacy assessment | Quantify core ASD-relevant behaviors in animal models and assess functional outcomes |
| Genomic Tools | Whole exome/genome sequencing, RNA sequencing, single-cell sequencing, CRISPR screening | Patient stratification, biomarker discovery | Identify genetic subtypes, molecular signatures, and therapeutic targets |
| Neuroimaging Biomarkers | Diffusion tensor imaging (DTI), functional MRI, MR spectroscopy | Target engagement, treatment response monitoring | Assess neural circuitry, structural connectivity, and metabolic changes in response to intervention |
| Clinical Assessment Tools | ADOS-2, ABC, SRS, SCQ, VABS, CBCL | Clinical trial endpoints | Standardized measurement of core symptoms, adaptive function, and co-occurring conditions |
The comparative evaluation of mechanism-based and symptom-based treatment strategies reveals complementary strengths that argue for an integrated approach to ASD intervention. While mechanism-based therapies offer the potential for fundamentally altering disease progression by targeting core biological pathways, their clinical translation has been challenged by biological complexity, developmental factors, and methodological limitations in trial design. Symptom-based approaches, particularly behavioral interventions, currently have stronger empirical support for efficacy but may be limited in their ability to address underlying pathophysiology.
Recent advances in parsing the heterogeneity of ASD into biologically meaningful subtypes create new opportunities for precision medicine approaches [3] [4] [2]. The identification of four distinct autism classes with different genetic profiles, developmental trajectories, and clinical presentations provides a framework for matching specific therapeutic mechanisms to patient subgroups most likely to benefit.
Future progress will depend on resolving key methodological challenges including optimization of clinical trial design, development of sensitive biomarkers, identification of critical intervention windows, and creation of innovative assessment tools that capture meaningful change in targeted domains. The integration of mechanism-based and symptom-based approaches within personalized treatment algorithms represents the most promising path forward for improving outcomes across the autism spectrum.
Autism spectrum disorder (ASD) is characterized by profound phenotypic and biological heterogeneity, presenting a formidable challenge for mechanistic research and therapeutic development. Cross-model validation—the systematic correlation of findings from animal models with human post-mortem studies—has emerged as a critical paradigm for addressing this complexity. This approach bridges the complementary strengths of experimental model systems and human biological data, enabling researchers to distinguish core pathological mechanisms from species-specific or model-specific epiphenomena. The fundamental challenge in autism research lies in reconciling the high heritability of the condition with its striking heterogeneity in clinical presentation, trajectory, and underlying biology [3] [2]. Historically, the field has been hampered by a lack of robust biological stratification, with the Diagnostic and Statistical Manual of Mental Disorders (DSM) moving from multiple ASD categories to a single broad spectrum due to the failure of previous subtyping approaches [96].
Recent technological advances in genomics, neuroimaging, and molecular profiling have created unprecedented opportunities for cross-model validation. Large-scale genomic studies have identified hundreds of ASD-associated genes, while detailed phenotypic characterization has revealed clinically distinct subtypes with different biological underpinnings [3] [2] [97]. Simultaneously, innovations in animal model systems, particularly genetically engineered mice that recapitulate specific ASD-related genetic mutations, provide experimentally tractable platforms for investigating pathological mechanisms and testing therapeutic interventions [98]. This whitepaper provides a comprehensive technical framework for designing, executing, and interpreting cross-model validation studies in autism research, with particular emphasis on bridging the gap between animal models and human post-mortem findings within the context of dysregulated biochemical pathways.
Experimental Frameworks for Cross-Model Validation
Establishing Face and Construct Validity in Animal Models
The foundation of robust cross-model validation rests on the development of animal models with strong face validity (phenotypic resemblance) and construct validity (etiological similarity) to human autism. Current approaches utilize genetically engineered mouse models harboring mutations in high-confidence ASD-risk genes, with careful attention to mimicking human genetic alterations (e.g., knockout, knock-in, or conditional alleles). The cross-species fMRI study analyzed 20 distinct mouse models representing mutations spanning different biological pathways, including synaptic mechanisms (e.g., Shank3, Nlgn), transcriptional regulation (e.g., Chd8), chromatin remodeling, and immune-related mechanisms [98]. Each model included wild-type control littermates to control for genetic and environmental confounds, enabling precise attribution of fMRI connectivity alterations to specific etiological mechanisms.
Phenotypic characterization follows a multi-tiered approach assessing behaviors across domains relevant to autism core features: (1) Social interaction and communication (e.g., ultrasonic vocalizations, three-chamber social approach); (2) Repetitive and restrictive behaviors (e.g., self-grooming, marble burying, perseverative behaviors in T-maze); (3) Cognitive flexibility (e.g., reversal learning, set-shifting); and (4) Associated features (e.g., anxiety, seizure susceptibility, sensory processing). This comprehensive behavioral profiling ensures that models recapitulate not only core autism phenotypes but also the spectrum of co-occurring features observed in human populations [98].
Human Post-Mortem Study Design and Tissue Processing
Human post-mortem studies provide essential validation of findings from animal models but require meticulous attention to tissue quality, demographic matching, and clinical characterization. Best practices include: (1) Detailed retrospective phenotyping using standardized instruments (e.g., ADI-R, ADOS) when available; (2) Careful matching of cases and controls for age, sex, post-mortem interval (PMI), tissue pH, and cause of death; (3) Standardized dissection protocols focusing on brain regions implicated in autism (prefrontal cortex, anterior cingulate cortex, cerebellum, striatum); and (4) Preservation of tissue for multiple analytical modalities (e.g., frozen for molecular studies, fixed for histology).
Recent research has demonstrated the critical importance of molecular subtyping in human post-mortem cohorts. The identification of four biologically distinct autism subtypes—Social and Behavioral Challenges, Mixed ASD with Developmental Delay, Moderate Challenges, and Broadly Affected—suggests that post-mortem studies must account for this heterogeneity in their experimental design [3] [2]. For example, the Broadly Affected subtype shows the highest proportion of damaging de novo mutations and widespread challenges, while the Social and Behavioral Challenges subtype exhibits distinct genetic profiles with postnatal gene activation patterns [3]. These subtype differences necessitate stratification in post-mortem analyses to ensure appropriate cross-model correlations.
Table 1: Key Methodological Considerations for Cross-Model Validation Studies
| Experimental Component | Key Parameters | Technical Standards |
|---|---|---|
| Animal Model Selection | Genetic construct validity; Behavioral face validity; Physiological relevance | Isogenic controls; Multiple model comparison; Cross-species translatability metrics |
| Human Tissue Collection | Post-mortem interval; Tissue pH; Agonal state; Clinical phenotyping | PMI < 24 hours; pH > 6.0; Standardized dissection protocols; RNA integrity number (RIN) > 7 |
| Molecular Profiling | RNA sequencing; Proteomic analysis; Epigenetic mapping | Batch effect correction; Reference gene normalization; Multiple testing correction |
| Imaging Validation | Resolution; Contrast mechanism; Anatomical correspondence | Cross-species registration; Multiple comparison correction; Quantitative metrics |
Key Biochemical Pathways in Autism Pathogenesis
Synaptic Signaling and Homeostasis
Convergent evidence from animal models and human studies implicates disrupted synaptic development and function as a core mechanism in autism pathogenesis. Post-mortem studies using PET imaging with the novel radiotracer 11C‑UCB‑J have directly demonstrated reduced synaptic density (approximately 17% reduction) in the brains of autistic adults compared to neurotypical controls [96]. Importantly, the degree of synaptic deficit correlated with the severity of autistic features, providing a direct structure-function relationship. This human finding validates earlier observations from multiple mouse models of autism, including Shank3, Nlgn, and Syn2 mutants, which showed structural and functional synaptic deficits [98].
The Shh/Wnt signaling crosstalk represents another critical pathway implicated in both neurodevelopment and synaptic function. These evolutionarily conserved pathways control angiogenesis, barriergenesis, neurodevelopment, CNS morphogenesis, and neuronal guidance [99]. The balance between Wnt-β-catenin and Shh pathways is critical for maintaining blood-brain barrier (BBB) function, and disruption of this crosstalk may compromise BBB development and integrity in autism [99]. Genetic mutations of key components of these pathways have been identified in ASD patients and animal models, correlating with symptom severity [99].
Transcriptional Regulation and Chromatin Remodeling
Chromatin remodeling complexes play a fundamental role in coordinating gene expression programs during brain development, and their disruption represents a major mechanism in autism pathogenesis. Mutations in genes such as CHD8, ARID1B, and ADNP are among the most common causes of autism with large effect sizes [98]. Animal models harboring mutations in these genes show widespread alterations in gene expression during critical developmental windows, providing a link between genetic risk and circuit-level dysfunction. The cross-species fMRI study identified a hyperconnectivity subtype associated with transcriptional and immune-related alterations, suggesting that dysregulation of gene expression programs may drive distinct neural phenotypes in autism [98].
Human post-mortem studies have begun to validate these findings, showing altered expression of chromatin modifiers in autistic individuals. Notably, the functional consequences of these transcriptional disruptions appear to vary across autism subtypes. For example, in the Social and Behavioral Challenges subtype—which typically has substantial social and psychiatric challenges but no developmental delays—mutations were found in genes that become active later in childhood [3]. This contrasts with subtypes featuring developmental delays, where affected genes are predominantly active during prenatal development [3]. This temporal dimension of gene expression highlights the importance of considering developmental trajectories in cross-model validation.
Neuroimmune Dysregulation and Blood-Brain Barrier Integrity
Neuroimmune dysregulation has emerged as a significant pathway in autism pathogenesis, with evidence from both animal models and human studies. The cross-species fMRI study identified a hyperconnectivity subtype linked to immune-related alterations, demonstrating the translational relevance of this mechanism [98]. Animal models of maternal immune activation (MIA) reproduce core behavioral features of autism and show persistent neuroimmune alterations, including microglial activation and increased cytokine expression [98].
The blood-brain barrier (BBB) represents a critical interface between peripheral and central immune function. Disruption of Shh/Wnt signaling crosstalk may compromise BBB integrity in autism, potentially allowing the influx of pathogens and inflammatory cells [99]. Post-mortem human studies and some animal ASD models have shown brain neuroinflammation, oxidative stress, and changes in BBB integrity, although the signaling pathways leading to these inflammatory findings and vascular alterations remain unclear [99]. This pathway exemplifies the complex interplay between different biological systems in autism and highlights the importance of integrated cross-model approaches.
Table 2: Key Biochemical Pathways in Autism Pathogenesis
| Pathway | Key Components | Evidence from Animal Models | Human Post-Mortem Validation |
|---|---|---|---|
| Synaptic Signaling | SHANK3, NLGN, NRXN, SYNGAP1 | Altered synaptic density and function in Shank3, Nlgn mutants [98] | 17% reduced synaptic density via PET imaging [96] |
| Shh/Wnt Signaling | SHH, WNT, β-catenin, GLI | BBB disruption in genetic models [99] | Genetic mutations in pathway components [99] |
| Chromatin Remodeling | CHD8, ARID1B, ADNP | Altered cortical development in Chd8 mutants [98] | Dysregulated gene expression networks [3] |
| Neuroimmune Function | Cytokines, Microglia, TREM2 | Hyperconnectivity in immune models [98] | Microglial activation and neuroinflammation [99] |
Methodological Approaches and Technical Protocols
Cross-Species Neuroimaging
Resting-state functional MRI (fMRI) provides a powerful translational tool for bridging animal model and human studies. The cross-species fMRI study established a rigorous protocol for comparative imaging [98]: For mouse imaging, animals are anesthetized with isoflurane and scanned using a 7T MRI scanner with a phased-array coil. Acquisition parameters included: gradient-echo EPI sequence, TR=1500ms, TE=15ms, matrix=96×96, 19 slices, 0.2×0.2×0.5 mm resolution. For human subjects, scanning is performed on 3T scanners using standardized protocols: T1-weighted structural images and resting-state fMRI (TR=720ms, TE=33ms, multiband acceleration factor=8). To enable cross-species comparison, researchers used weighted-degree centrality—a metric that quantifies the mean fMRI connectivity of each voxel—which has previously revealed comparable brain dysconnectivity signatures in rodents and humans harboring syntenic autism-risk variants [98].
The analytical workflow involves: (1) Preprocessing (motion correction, spatial normalization, smoothing); (2) Connectivity matrix generation; (3) Graph theory metric extraction; and (4) Multivariate pattern analysis. This approach successfully identified two prominent hypo- and hyperconnectivity subtypes that were replicable across species and linked to distinct biological pathways [98]. Hypoconnectivity was associated with synaptic dysfunction, while hyperconnectivity reflected transcriptional and immune-related alterations, demonstrating how cross-species neuroimaging can decode biological heterogeneity in autism.
Molecular Profiling and Validation
Integrated molecular profiling across species requires standardized protocols for tissue processing, nucleic acid extraction, and sequencing library preparation. For transcriptomic studies, the recommended approach includes: (1) RNA extraction with column-based purification; (2) RNA integrity assessment (RIN > 8.0); (3) Library preparation with ribosomal RNA depletion; (4) Paired-end sequencing (minimum 30M reads per sample); and (5) Cross-species alignment and normalization. For human post-mortem tissue, careful matching of pH, PMI, and age is critical for minimizing technical variability.
The Princeton/Simons Foundation study demonstrated the power of integrating genetic and phenotypic data at scale [3] [2]. Their approach involved: (1) Whole exome or genome sequencing; (2) Identification of rare inherited and de novo variants; (3) Gene set enrichment analysis; (4) Pathway mapping; and (5) Developmental expression analysis using reference transcriptome datasets. This comprehensive molecular profiling revealed that different autism subtypes have distinct genetic profiles and are associated with mutations in biologically coherent pathways with specific developmental timing [3].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Cross-Model Validation Studies
| Reagent/Category | Specific Examples | Application & Function |
|---|---|---|
| Genetically Engineered Mouse Models | Shank3^ΔC/ΔC, Cntnap2^-/^-, Chd8^+/-, Fmr1^-/y [98] | Model specific genetic alterations; Study gene-phenotype relationships; Test therapeutic interventions |
| Radiotracers for Synaptic Imaging | ^11^C-UCB-J [96] | Quantify synaptic density in living brain using PET; Correlate synaptic deficits with behavior |
| Antibodies for Post-Mortem Validation | Anti-PSD95, Anti-Synaptophysin, Anti-GFAP, Anti-IBA1 | Validate protein expression changes; Identify cell-type specific alterations; Confirm pathological features |
| Bulk & Single-Cell RNA Sequencing Kits | 10x Genomics Chromium, SMART-Seq v4 | Profile transcriptomic changes; Identify cell-type specific signatures; Discover novel pathways |
| Behavioral Assessment Tools | Three-chamber social test, Marble burying, Self-grooming analysis, Ultrasonic vocalization recording | Quantify autism-relevant behaviors; Establish face validity of models; Measure treatment efficacy |
Discussion and Future Directions
The systematic implementation of cross-model validation approaches has fundamentally advanced our understanding of autism pathogenesis. The identification of biologically distinct subtypes—each with characteristic genetic profiles, developmental trajectories, and clinical presentations—provides a roadmap for precision medicine approaches in autism [3] [2]. The demonstration that different subtypes show mutations in different biological pathways with distinct developmental timing patterns represents a paradigm shift in how we conceptualize autism heterogeneity [3].
Future research directions should focus on: (1) Expanding the non-coding genome analysis in subtype-specific contexts, as current studies have primarily focused on protein-coding regions despite evidence that non-coding variants contribute significantly to autism risk [4] [97]; (2) Developing more sophisticated cross-species computational frameworks that can integrate multi-omic data across biological scales from genes to circuits to behavior; (3) Linking specific biochemical pathways to targeted therapeutic strategies, as exemplified by the Stanford research that identified hyperactivity in the reticular thalamic nucleus as a potential therapeutic target and demonstrated that the experimental seizure drug Z944 could reverse behavioral deficits in an autism mouse model [10].
The continued refinement of cross-model validation approaches promises to accelerate the translation of basic research findings into clinically meaningful interventions. By rigorously correlating findings from animal models and human post-mortem studies within the context of biologically defined subtypes, researchers can develop targeted strategies that address the specific pathological mechanisms underlying an individual's autism, ultimately enabling personalized approaches to treatment and support.
The quest to delineate the biological underpinnings of Autism Spectrum Disorder (ASD) is fundamentally challenged by its profound heterogeneity and frequent comorbidity with other neurodevelopmental conditions, most notably Attention-Deficit/Hyperactivity Disorder (ADHD) [100]. A cornerstone finding in modern psychiatric genetics is the substantial shared genetic liability between ASD and ADHD, evidenced by moderate genetic correlations (rg) from family and molecular studies [100]. This overlap presents a critical confound: observed genetic associations with ASD may in fact reflect a broader neurodevelopmental risk rather than pathways specific to the core social-communication and repetitive behavior phenotypes of ASD [100].
This technical guide posits that resolving this shared liability is not merely a statistical exercise but a prerequisite for advancing the central thesis of biochemical pathway research in autism. If diverse genetic risks converge on final common pathways governing synaptic growth, connectivity, and plasticity [34], then accurately isolating the unique genetic components of ASD is essential for mapping the precise biochemical etiology. This document provides an in-depth methodology for applying genetic correlation analyses, specifically Genomic Structural Equation Modeling (SEM), to dissect ASD-specific pathways from those shared with ADHD and other traits, thereby generating refined targets for mechanistic exploration and therapeutic development.
Core Analytical Framework: Genomic Structural Equation Modeling (SEM)
The primary method for disentangling shared genetic variance is Genomic SEM, a multivariate technique applied to Genome-Wide Association Study (GWAS) summary statistics [100].
2.1. Experimental Protocol: The Cholesky Decomposition Model
- Objective: To derive a latent genetic factor representing variance unique to ASD (uASD), orthogonal to genetic variance shared with ADHD.
- Input Data Preparation:
- GWAS Summary Statistics: Obtain QC-filtered summary statistics for ASD and childhood-diagnosed ADHD. The ASD meta-analysis should include ~18,381 cases and 27,969 controls [100]. Childhood ADHD data (~14,878 cases) show higher genetic overlap with ASD [100].
- Quality Control (QC): Using the
mungefunction in the GenomicSEM R package, restrict SNPs to the HapMap3 panel, apply minor allele frequency (MAF < 1%) and imputation quality (INFO < 0.9) filters [100]. - Covariance Estimation: Process QC-ed data through multivariable Linkage Disequilibrium Score Regression (LDSC) via the
ldscfunction. This generates a genetic covariance matrix and a sampling covariance matrix, the latter accounting for sample overlap [100]. - Scale Conversion: For binary traits (ASD, ADHD), convert heritability estimates to the liability scale using population prevalence and effective sample size [100].
- Model Fitting:
- A Cholesky decomposition model is fitted using the genetic covariance matrix as input.
- The model specifies two latent factors:
cADHD(genetic variance of ADHD and the ASD variance shared with ADHD) anduASD(residual genetic variance unique to ASD). - Both ASD and ADHD are regressed onto
cADHD. ASD is additionally regressed ontouASD. The latent factorsuASDandcADHDare modeled as orthogonal (rg = 0) [100].
- Output: The model yields an estimate of the
uASDfactor, which can be used in downstream genetic analyses as a "purified" ASD genetic signal.
2.2. Data Table: Key Genetic Correlation Findings with External Traits
Applying this model, the genetic correlations (rg) between the derived uASD factor and a range of external phenotypes can be calculated. Significant correlations highlight domains of unique ASD genetic liability [100].
Table 1: Genetic Correlations (rg) of Unique ASD (uASD) with Selected External Traits [100].
| Trait Domain | Specific Trait | Genetic Correlation (rg) with uASD | Interpretation |
|---|---|---|---|
| Cognitive/Educational | Educational Attainment | Positive Correlation [101] | uASD genetics are positively linked to higher educational attainment, independent of ADHD. |
| Intelligence (INT) | Positive Correlation (rg ~ 0.22) [101] | uASD genetics share a positive polygenic overlap with cognitive ability. | |
| Psychiatric | Internalizing Traits (e.g., Anxiety, Depression) | Positive Correlation [100] | Unique ASD risk is genetically correlated with internalizing symptomatology. |
| Cardiometabolic | Body Mass Index (BMI), Type 2 Diabetes | Small Positive Correlation in shared variants [102] | Shared genetic loci between ASD and metabolic traits often have concordant effect directions. |
| Systolic/Diastolic Blood Pressure, CAD | Negative Correlation in shared variants [102] | Shared genetic loci between ASD and cardiovascular traits often have discordant effect directions. |
Downstream Functional and Gene-Expression Analyses
With the uASD factor defined, its biological basis can be interrogated at functional and transcriptional levels.
3.1. Experimental Protocol: Stratified Genomic SEM & Transcriptome-Wide SEM (T-SEM)
- Stratified Genomic SEM (Heritability Enrichment):
- Objective: Identify categories of genes or functional annotations enriched for uASD heritability.
- Method: Apply Stratified LDSC (S-LDSC) using a set of functional annotations (e.g., conserved genomic regions, histone marks, tissue-specific chromatin states). The
enrichfunction in GenomicSEM calculates an enrichment ratio (observed vs. expected proportion of heritability explained by an annotation) [100]. - Key Finding: uASD heritability is significantly enriched in genes involved in evolutionarily conserved processes and specific histone marks in the germinal matrix [100].
- Transcriptome-Wide SEM (T-SEM):
- Objective: Identify genes whose expression levels are associated with uASD genetic risk.
- Method: Integrate uASD GWAS summary statistics with gene expression reference data (e.g., from GTEx) using T-SEM. This tests for association between the uASD genetic signal and genetically predicted expression of each gene [100].
- Key Finding: T-SEM can reveal dozens of unique genes with expression associated with uASD, many of which are novel candidates not identified in standard ASD GWAS [100].
3.2. Data Table: Summary of Polygenic Overlap with Cognitive Traits
The bivariate causal mixture model (MiXeR) offers a complementary view, estimating the total number of shared genetic variants irrespective of the net genetic correlation.
Table 2: MiXeR Analysis of Polygenic Overlap Between ASD and Cognitive Traits [101].
| Trait Pair | Estimated 'Causal' SNPs for ASD | SNPs Shared with Cognitive Trait | Dice Coefficient (Similarity) | Interpretation |
|---|---|---|---|---|
| ASD & Educational Attainment (EDU) | ~12.7k | ~12.0k | High | Extensive polygenic overlap; majority (~59-68%) of shared variants have concordant effects. |
| ASD & Intelligence (INT) | ~12.7k | ~11.1k | High | Extensive polygenic overlap; similar proportion of concordant effects. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Resources for Genetic Correlation Analyses in ASD.
| Item / Resource | Function / Purpose | Example / Notes |
|---|---|---|
| GWAS Summary Statistics | Primary input data for LDSC and Genomic SEM. | PGC ASD GWAS (N=46,350) [100]; iPSYCH childhood ADHD GWAS [100]; SSGAC EDU GWAS [101]. |
| LD Reference Panel | Provides population-specific LD structure for variance estimation. | 1000 Genomes Project Phase 3 (European ancestry) [100]. |
| Functional Annotation Sets | Used in S-LDSC to test for heritability enrichment. | 1000 Genomes Baseline LD v2.2, Roadmap Epigenomics, GTEx tissue-specific annotations [100]. |
| Gene Expression Reference | Essential for Transcriptome-Wide SEM (T-SEM). | GTEx v8 brain tissue expression quantitative trait loci (eQTL) data [100]. |
| GenomicSEM R Package | Integrated software suite for all core analyses (LDSC, SEM, S-LDSC, T-SEM). | Available on GitHub; includes munge, ldsc, enrich, and tsem functions [100]. |
| MiXeR Software Tool | Estimates polygenic overlap and number of causal variants between two traits. | Useful for quantifying shared genetic architecture beyond global rg [101]. |
| FUMA / GARFIELD | Platform for functional mapping and annotation of GWAS results. | Used for post-analysis annotation of identified loci and genes [101]. |
Visualizing the Analytical Workflow and Convergent Pathways
The following diagrams, generated with Graphviz using the specified color palette and contrast rules, illustrate the core analytical pipeline and the resultant convergence onto biochemical pathways.
Workflow for Disentangling ASD-Specific Genetic Signals.
Genetic Risks Converge on Growth Pathways Driving ASD Heterogeneity.
The application of genetic correlation analyses, specifically the Genomic SEM framework, moves the field beyond cataloging genetic associations toward a functional dissection of ASD etiology. By isolating the uASD signal, researchers can more confidently map genetic risks to specific biochemical pathways—such as mTOR and ERK1/2 signaling—that directly influence synaptic protein synthesis and neural growth trajectories [34]. This refined mapping is critical for the thesis that ASD heterogeneity can be parsed into states of neural overgrowth versus undergrowth [34]. For drug development professionals, this approach clarifies target identification: therapies modulating a pathway like mTOR may be most effective for the subset of ASD patients whose genetic and biochemical profile indicates pathological overgrowth, while being ineffective or detrimental for those with undergrowth pathologies. Thus, distinguishing shared from unique genetic risks is not the end goal, but the essential starting point for developing precise, pathophysiology-based interventions for ASD.
Autism spectrum disorder (ASD) research is undergoing a paradigm shift, moving from broad behavioral categorization to precise biological subtyping and circuit-level understanding. This transformation is critical for developing targeted interventions for a condition characterized by extensive heterogeneity. Groundbreaking research has identified four biologically distinct subtypes of autism, each with unique genetic profiles and clinical trajectories [3] [2]. Concurrently, neuroscientists have pinpointed specific neural circuits, particularly those involving the reticular thalamic nucleus (RTN), as key drivers of ASD pathophysiology [103] [104] [105]. This whitepaper integrates these advances to provide researchers and drug development professionals with a comprehensive framework for evaluating novel circuit-based intervention targets, with particular emphasis on the RTN as a promising therapeutic node.
The RTN serves as the central gatekeeper of thalamocortical information flow, regulating sensory processing, attention, and sleep rhythms—functions frequently disrupted in ASD [103] [106]. Its unique position as the primary source of inhibition within thalamocortical circuits makes it particularly relevant to ASD pathophysiology, especially given the high comorbidity between autism and conditions like epilepsy (30% in ASD versus 1% in general population) and sensory abnormalities [104] [105]. Recent studies directly demonstrate that RTN hyperexcitability drives core ASD behaviors in multiple mouse models, and that targeted suppression of this hyperactivity can reverse behavioral deficits [103] [107] [104].
Deconstructing Heterogeneity: The Four Subtypes Framework
A Data-Driven Subclassification of Autism
The landmark study by Princeton University and the Simons Foundation analyzed phenotypic and genotypic data from over 5,000 individuals in the SPARK cohort, employing a person-centered computational approach to identify four clinically and biologically distinct ASD subtypes [3] [4] [2]. This subtyping framework provides essential context for understanding how circuit-based interventions might benefit specific patient populations.
Table 1: The Four Autism Subtypes: Clinical and Biological Profiles
| Subtype Name | Prevalence | Core Clinical Features | Developmental Trajectory | Co-occurring Conditions |
|---|---|---|---|---|
| Social & Behavioral Challenges | 37% | Prominent social challenges, repetitive behaviors, psychiatric comorbidities | Typical developmental milestones, later diagnosis (after age 6) | High rates of ADHD, anxiety, depression, OCD |
| Mixed ASD with Developmental Delay | 19% | Developmental delays, variable social and repetitive behaviors | Delayed milestones (walking, talking), early diagnosis | Language delay, intellectual disability, motor disorders |
| Moderate Challenges | 34% | Milder core ASD symptoms across domains | Typical developmental milestones | Low rates of psychiatric comorbidities |
| Broadly Affected | 10% | Severe challenges across all domains | Significant developmental delays, early diagnosis | Multiple co-occurring conditions: anxiety, depression, mood dysregulation, cognitive impairment |
Genetic Architecture Underlying the Subtypes
Critically, each subtype demonstrates distinct genetic signatures with minimal overlap in affected biological pathways [3] [2]. The Social and Behavioral Challenges subtype involves genes predominantly active postnatally, aligning with their typical early development and later diagnosis. Conversely, the Mixed ASD with Developmental Delay subtype involves genes active prenatally, consistent with their early developmental delays [3] [4]. The Broadly Affected group shows the highest burden of damaging de novo mutations, while the Mixed ASD with Developmental Delay group is more likely to carry rare inherited variants [3]. This genetic dissection reveals that what was previously considered a single disorder actually represents multiple distinct biological narratives with implications for therapeutic targeting [3] [2].
The Reticular Thalamic Nucleus: A Central Node in ASD Circuitry
Anatomy and Physiology of the RTN
The reticular thalamic nucleus is a slender, shell-like GABAergic structure that envelops the dorsal thalamus. It serves as the primary source of inhibition within thalamocortical circuits, functioning as a critical gatekeeper for sensory information and cognitive processing [103] [106]. RTN neurons exhibit two distinct firing modes: tonic firing during awake states and burst firing during sleep or pathological conditions, with burst firing driven primarily by T-type calcium channels (particularly Cav3.2 and Cav3.3 isoforms) [103].
The RTN contains functionally distinct subpopulations: first-order (FO) neurons in the core region primarily innervate primary sensory thalamic nuclei and exhibit high burst firing capacity, while higher-order (HO) neurons in the anterior and peripheral regions project to associative thalamic nuclei with lower burst firing propensity [106]. This functional specialization enables the RTN to coordinate diverse functions from sensory gating to cognitive flexibility—many of which are impaired in ASD.
RTN Dysfunction in ASD Pathophysiology
Multiple lines of evidence from mouse models demonstrate RTN dysfunction in ASD:
In Cntnap2 knockout mice (modeling ASD with epilepsy), RTN neurons display:
- Hyperexcitability with enhanced burst firing and intrathalamic oscillations [103] [107]
- Elevated T-type calcium currents driving pathological burst firing [103]
- Increased spontaneous and evoked oscillations in thalamocortical circuits [103]
- Behavior-correlated hyperactivity confirmed through in vivo fiber photometry [103] [104]
In Shank3 knockout mice (modeling Phelan-McDermid syndrome), RTN alterations include:
- Reduced rebound burst firing specifically in FO-projecting neurons [106]
- Blurred core/shell segregation of FO/HO projecting neurons [106]
- Decreased inhibitory postsynaptic currents in both ventroposteromedial (VPM) and posteromedial (POm) thalamic nuclei [106]
These findings position RTN dysfunction as a convergent mechanism across multiple ASD genetic models, with hyperexcitability particularly prominent in models with seizure comorbidity.
Diagram Title: RTN Hyperexcitability as Convergent ASD Mechanism
Experimental Models and Methodologies for RTN Investigation
Electrophysiological Characterization Protocols
Table 2: Key Electrophysiological Assays for RTN Function Assessment
| Method | Technical Specifications | Key Measurements | Relevance to ASD Models |
|---|---|---|---|
| Ex vivo brain slice recordings | Horizontal thalamic slices (300-350μm), 32-34°C, artificial CSF | Spontaneous oscillations, evoked oscillations (internal capsule stimulation), burst/tonic firing modes | Quantifies intrinsic thalamic hyperexcitability in Cntnap2−/− mice [103] |
| In vivo fiber photometry | GCaMP6f expression in RTN, 470nm excitation, implanted optical fiber | RTN population calcium dynamics during behavior (social interaction, sensory stimuli) | Correlates RTN hyperactivity with specific ASD-like behaviors [103] |
| Whole-cell patch clamp | Voltage-clamp and current-clamp configurations in identified RTN neurons | T-type calcium currents, input resistance, firing properties, synaptic currents | Identifies ion channel mechanisms (elevated T-currents in Cntnap2−/−) [103] |
| EEG telemetry | Cortical electrode implantation, continuous recording | Spike-wave discharges, seizure monitoring, sleep architecture | Documents epilepsy comorbidity and network hyperexcitability [103] |
Behavioral Paradigms for Assessing Circuit-Based Interventions
Comprehensive behavioral testing is essential for evaluating potential ASD treatments. The following standardized protocols have demonstrated sensitivity to RTN-targeted interventions:
Social Interaction Test: Measures time spent interacting with a novel conspecific versus object in a three-chamber apparatus. Cntnap2−/− mice show significantly reduced social preference that improves after RTN suppression [103] [104].
Open Field Locomotor Activity: Assesses total distance traveled in a novel arena over 10 minutes. Cntnap2−/− mice display hyperactivity reversed by Z944 treatment and chemogenetic RTN inhibition [103].
Repetitive Behavior Assessment: Quantifies self-grooming duration during a 10-minute session. Cntnap2−/− mice exhibit elevated grooming that normalizes after RTN suppression [103].
Seizure Susceptibility Testing: Evaluates response to subconvulsive pentylenetetrazole (PTZ, 20mg/kg i.p.) using Racine scale scoring. Cntnap2−/− mice show significantly enhanced seizure susceptibility with shorter latency to spike-wave discharges and myoclonic jerks [103].
Sensory Processing Tests: Measures responses to mild sensory stimuli (light air puffs, auditory tones). Cntnap2−/− mice demonstrate heightened sensitivity correlated with RTN hyperexcitability [104] [105].
Therapeutic Targeting of the RTN: Experimental Evidence
Pharmacological Interventions
The T-type calcium channel blocker Z944 has demonstrated significant efficacy in correcting ASD-related behaviors in the Cntnap2−/− model:
- Administration: Acute systemic injection (dosage optimized for T-type channel blockade)
- Mechanism: Selective inhibition of T-type calcium channels (particularly Cav3.2/Cav3.3) in RTN neurons
- Effects: Normalizes RTN burst firing, reduces intrathalamic oscillations, and reverses social deficits, hyperactivity, and repetitive behaviors [103] [104] [105]
- Significance: Highlights T-type channels as molecular targets for ASD with epilepsy comorbidity
Chemogenetic Approaches
Designer Receptors Exclusively Activated by Designer Drugs (DREADD) provide precise neuromodulatory control:
- Viral Vector Delivery: AAV-hSyn-DIO-hM4Di-mCherry injected into RTN of Cntnap2−/− mice
- Activation: Clozapine-N-oxide (CNO, 1-3mg/kg i.p.) or more selective compound C21 activates inhibitory Gi-coupled hM4Di receptors
- Effects: Significant improvement in social preference, reduced repetitive behaviors, and normalized locomotor activity [103]
- Causality Establishment: Artificial RTN activation in wild-type mice induces ASD-like behaviors, confirming sufficiency of RTN hyperexcitability to drive pathology [104] [105]
Diagram Title: RTN-Targeted Intervention Strategies
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating RTN in ASD Models
| Reagent / Tool | Specifications | Application | Experimental Notes |
|---|---|---|---|
| Cntnap2−/− mice | Complete knockout of contactin-associated protein-like 2 | Model of ASD with epilepsy, cortical dysplasia, and RTN hyperexcitability | Display robust thalamocortical oscillation deficits and comorbid epilepsy [103] [107] |
| Shank3 KO mice | Mutations in SH3 and multiple ankyrin repeat domains 3 | Model of Phelan-McDermid syndrome with specific RTN FO/HO alterations | Shows subtype-specific RTN changes unlike hyperexcitability pattern [106] |
| Z944 | Experimental T-type calcium channel blocker | Pharmacological suppression of RTN burst firing | Reverses behavioral deficits in Cntnap2−/− mice; potential epilepsy-ASD overlap therapy [103] [104] |
| DREADD vectors | AAV-hSyn-DIO-hM4Di-mCherry for inhibitory chemogenetics | Precise RTN neuron suppression using CNO or C21 | Establishes causal relationship between RTN activity and ASD behaviors [103] [105] |
| GCaMP6f | Genetically encoded calcium indicator | In vivo fiber photometry of RTN population activity | Correlates neural dynamics with specific behaviors in real-time [103] |
| Ntsr1-Cre mice | Cre recombinase expression in layer 6 corticothalamic neurons | Optogenetic control of corticothalamic inputs to RTN | Enables circuit-specific interrogation of RTN modulation [103] |
Integrating Circuit and Subtype Frameworks for Precision Medicine
The convergence of autism subclassification and circuit-level targeting represents a transformative opportunity for precision medicine in ASD. The four biologically distinct subtypes provide a stratification framework for targeting circuit-specific interventions like RTN modulation [3] [2]. Notably, the Broadly Affected and Mixed ASD with Developmental Delay subtypes, which show higher rates of neurological comorbidities including epilepsy, may be particularly responsive to RTN-targeted therapies [3] [10].
Future research directions should include:
- Mapping RTN dysfunction across ASD genetic subtypes to identify which human subtypes correspond to the hyperexcitability observed in Cntnap2 models
- Developing subtype-specific biomarkers for RTN dysfunction, potentially using EEG signatures of thalamocortical dysrhythmia
- Optimizing T-type calcium channel blockers for ASD with better blood-brain barrier penetration and Cav3.2/3.3 subtype selectivity
- Exploring combination therapies that target both RTN hyperactivity and subtype-specific genetic vulnerabilities
The reticular thalamic nucleus represents a promising circuit-level target for ASD intervention, particularly for subtypes with comorbid epilepsy, sensory hypersensitivity, and sleep disturbances. Robust experimental evidence from multiple ASD models demonstrates that RTN hyperexcitability drives core behavioral deficits, and that pharmacological or chemogenetic suppression of this hyperactivity can reverse these abnormalities [103] [107] [104]. The integration of this circuit-level understanding with the newly established framework of four biologically distinct autism subtypes creates an unprecedented opportunity for developing precision therapies tailored to an individual's specific biological profile of ASD.
Future therapeutic development should prioritize targets within the thalamocortical circuit, particularly T-type calcium channels in the RTN, while considering which ASD subtypes are most likely to benefit from such circuit-based interventions. This approach marks a fundamental shift from symptom management to targeted correction of underlying circuit pathophysiology in autism spectrum disorder.
Conclusion
The field of autism research is undergoing a transformative shift, moving from a symptom-based definition to a biology-driven understanding grounded in distinct biochemical pathways and genetic subtypes. The identification of these subtypes provides a foundational framework for precision medicine, enabling the development of targeted therapies aligned with an individual's specific biological narrative. Future progress hinges on the continued integration of large-scale multi-omics data, exposomics, and advanced computational models. For researchers and drug developers, this new paradigm demands a focus on stratified clinical trials, the development of validated biomarkers, and a deep understanding of the pharmacokinetic and pharmacodynamic properties of interventions within specific subtypes. The ultimate goal is to translate this intricate knowledge of biochemical pathogenesis into personalized, effective, and timely interventions that improve the lives of individuals with ASD.
References
- 1. Four New Autism Subtypes Link Genes to Children's Traits [https://www.scientificamerican.com/article/four-new-autism-subtypes-link-genes-to-childrens-traits/]
- 2. Decomposition of phenotypic heterogeneity in autism ... [https://www.nature.com/articles/s41588-025-02224-z]
- 3. Major autism study uncovers biologically distinct subtypes, ... [https://www.princeton.edu/news/2025/07/09/major-autism-study-uncovers-biologically-distinct-subtypes-paving-way-precision]
- 4. New Study Reveals Subclasses of Autism by Linking Traits ... [https://www.simonsfoundation.org/2025/07/09/new-study-reveals-subclasses-of-autism-by-linking-traits-to-genetics/]
- 5. New Autism Study Uncovers Four Biological Subtypes [https://www.psychiatrist.com/news/new-autism-study-uncovers-four-biological-subtypes/]
- 6. Proposed Subtypes of Autism [https://www.necc.org/proposed-subtypes-of-autism/]
- 7. ASD Subtypes Study: Autism Brain Connectivity Patterns ... [https://www.additudemag.com/autism-spectrum-disorder-subtypes-adhd-asd-brain-connectivity/?srsltid=AfmBOorBB9xNo6WcycVispZnjsNLX8uUb017PU5DUmHp066Wc9E70QF6]
- 8. New Autism Subtypes Identified Based on Genes, ... [https://www.brainfacts.org/diseases-and-disorders/childhood-disorders/2025/new-autism-subtypes-identified-based-on-genes-individual-traits-111125]
- 9. Subtype-Specific Molecular Insights into Autism Spectrum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11469458/]
- 10. Promising Autism Research Breakthroughs in 2025 [https://linksaba.com/promising-autism-research-breakthroughs/]
- 11. Decoding the genetic landscape of autism - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11438927/]
- 12. Polygenic and developmental profiles of autism differ by ... [https://www.nature.com/articles/s41586-025-09542-6]
- 13. The contributions of rare inherited and polygenic risk to ASD ... [https://pubmed.ncbi.nlm.nih.gov/37506195/]
- 14. Neurobiological basis of autism spectrum disorder [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2025.1558081/full]
- 15. Advancing precision diagnosis in autism: Insights from large ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12275934/]
- 16. CHD8 in Cerebellar Function and Autism [https://www.technologynetworks.com/neuroscience/articles/how-chd8-shapes-neurodevelopment-in-autism-spectrum-disorder-405503]
- 17. The developing brain: pathway disruptions contributing to ... [https://www.frontiersin.org/research-topics/71784/the-developing-brain-pathway-disruptions-contributing-to-autism-and-intellectual-disabilitiesundefined]
- 18. Metabolic network analysis of pre-ASD newborns and 5 ... [https://www.nature.com/articles/s42003-024-06102-y]
- 19. A holistic review of autism spectrum disorder mechanisms ... [https://www.sciencedirect.com/science/article/pii/S0969996125004048]
- 20. PRENATAL ORIGINS OF ASD: THE WHEN, WHAT AND ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7373219/]
- 21. Redox System Dysfunction as a Key Mechanism in Autism ... [https://pubmed.ncbi.nlm.nih.gov/41155144/]
- 22. Haploinsufficiency of the schizophrenia and autism ... risk gene [https://www.nature.com/articles/s41398-021-01415-6?error=cookies_not_supported&code=396f51a5-5e99-468c-84f2-b490d029fbe3]
- 23. Prenatal environmental risk factors for autism spectrum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11404034/]
- 24. Fetal exposure to teratogens: Evidence of genes involved ... [https://www.sciencedirect.com/science/article/abs/pii/S0149763410002149]
- 25. Gestational Influences and Autism [https://autism.org/gestational-influences-2023/]
- 26. Signalling pathways in autism spectrum disorder - Nature [https://www.nature.com/articles/s41392-022-01081-0]
- 27. Data and Statistics on Autism Spectrum Disorder [https://www.cdc.gov/autism/data-research/index.html]
- 28. Re-emerging concepts of immune dysregulation in autism ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2022.1006612/full]
- 29. The Microbiota-Gut-Brain Axis in Autism [https://pubmed.ncbi.nlm.nih.gov/41305382/]
- 30. Gut microbiota and autism spectrum disorder: advances in ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1587818/full]
- 31. Immune Dysregulation in Autism Spectrum Disorder [https://pmc.ncbi.nlm.nih.gov/articles/PMC8955336/]
- 32. Kids with autism show altered gut microbiome-brain ... [https://www.uclahealth.org/news/article/kids-with-autism-gut-microbiome-brain]
- 33. Pathway Network Analyses for Autism Reveal Multisystem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4824422/]
- 34. Characterizing autism spectrum disorders by key ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2015.00313/full]
- 35. Contrast subgraphs catch patterns of altered functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12234876/]
- 36. Major autism study uncovers biologically distinct subtypes ... [https://engineering.princeton.edu/news/2025/07/09/major-autism-study-uncovers-biologically-distinct-subtypes-paving-way-precision-diagnosis-and-care]
- 37. Computational Neuroscience's Influence on Autism Neuro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189925/]
- 38. NIH launches $50M Autism Data Science Initiative to ... [https://www.nih.gov/news-events/news-releases/nih-launches-fifty-million-autism-data-science-initiative-unlock-causes-improve-outcomes]
- 39. About SPARK for Autism - Autism Research [https://sparkforautism.org/portal/page/about-spark/]
- 40. SPARK: A US Cohort of 50,000 Families to Accelerate Autism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7444276/]
- 41. Meet the Autism Data Science Initiative grantees [https://www.thetransmitter.org/spectrum/meet-the-autism-data-science-initiative-grantees/]
- 42. An omics perspective on drug target discovery platforms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7711264/]
- 43. Multi-omics reveals cross-tissue regulatory mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572420/]
- 44. Bio-collections in autism research - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5504648/]
- 45. De novo network analysis reveals autism causal genes ... [https://www.life-science-alliance.org/content/6/10/e202302142]
- 46. Characterizing immune and metabolic profiles in autism ... [https://www.sciencedirect.com/science/article/abs/pii/S002239562500456X]
- 47. Review Preclinical models for autism spectrum disorder [https://www.sciencedirect.com/science/article/abs/pii/S0306452225010619]
- 48. Brain organoids: a new paradigm for studying human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620469/]
- 49. Extracellular vesicle profiling reveals novel autism ... [https://www.nature.com/articles/s41398-025-03607-w]
- 50. Humans may be born with preconfigured brains that help ... [https://www.earth.com/news/humans-born-with-preconfigured-brains-neural-circuits-that-help-us-understand/]
- 51. Neurometabolic profiles of autism spectrum disorder ... [https://www.nature.com/articles/s41598-025-20090-x]
- 52. Machine learning algorithm identifies three unique autism ... [https://www.psypost.org/machine-learning-algorithm-identifies-three-unique-autism-subtypes-in-males/]
- 53. Multimodal AI for risk stratification in autism spectrum ... [https://www.nature.com/articles/s41746-025-01914-6]
- 54. How Technology Advances Research and Practice in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384708/]
- 55. Machine learning of clinical phenotypes facilitates autism ... [https://www.nature.com/articles/s41598-025-95291-5]
- 56. Characterizing autism spectrum disorders by key ... [https://pure.johnshopkins.edu/en/publications/characterizing-autism-spectrum-disorders-by-key-biochemical-pathw-3/]
- 57. Age of machine learning: new trends in autism spectrum ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1492484/full]
- 58. Polypharmacy and pharmacogenomics in high-acuity ... [https://capmh.biomedcentral.com/articles/10.1186/s13034-025-00915-3]
- 59. Psychotropic pharmacogenetics in adult populations [https://pmc.ncbi.nlm.nih.gov/articles/PMC12569124/]
- 60. Exploratory focused pharmacogenetic testing reveals novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10875102/]
- 61. The identification of metabolites from gut microbiota in ... [https://www.nature.com/articles/s41598-025-15921-w]
- 62. Pleiotropy of autism-associated chromatin regulators - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10399978/]
- 63. Genetic and environmental influences in autism [https://pmc.ncbi.nlm.nih.gov/articles/PMC12618061/]
- 64. Biochemical Markers as Predictors of Health Outcomes in ... [https://pubmed.ncbi.nlm.nih.gov/39913064/]
- 65. Review Early detection of autism with the help of biomarkers [https://www.sciencedirect.com/science/article/pii/S2950588725000746]
- 66. Does the current state of biomarker discovery in autism reflect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9992810/]
- 67. Validation of Analytical Methods for Biomarkers Employed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2744124/]
- 68. Methods and Challenges in Quantitative Imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4258641/]
- 69. Ignite Biomedical and Liquid Biosciences Announce the ... [https://www.biospace.com/press-releases/ignite-biomedical-and-liquid-biosciences-announce-the-discovery-of-biomarkers-for-the-diagnosis-and-treatment-of-autism-spectrum-disorder]
- 70. An inflammatory biomarker signature of response to CAR-T ... [https://www.nature.com/articles/s41591-025-03532-x]
- 71. Essential pathways and circuits of autism pathogenesis [https://www.frontiersin.org/research-topics/3508/essential-pathways-and-circuits-of-autism-pathogenesis/articles]
- 72. Characterizing autism spectrum disorders by key biochemical ... [https://pubmed.ncbi.nlm.nih.gov/26483618/]
- 73. The co-occurrence of multimorbidity and polypharmacy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11734935/]
- 74. Learning from quantitative data to understand central ... [https://www.sciencedirect.com/science/article/abs/pii/S0734975017301179]
- 75. Quantitative analysis of disease-related metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9823209/]
- 76. Lost in translation: the valley of death across preclinical and ... [https://transmedcomms.biomedcentral.com/articles/10.1186/s41231-019-0050-7]
- 77. Molecular basis of autism spectrum disorders - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12119779/]
- 78. Uncertainty in the Translation of Preclinical Experiments to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2864134/]
- 79. Shank3 related oligodendrocyte alterations in autism are ... [https://www.nature.com/articles/s41380-025-03333-1]
- 80. Preclinical assessment for translation to humans [https://www.sciencedirect.com/science/article/pii/S2666634024002964]
- 81. Exploring Biochemical Pathways with Human-Centric AI [https://www.causaly.com/blog/exploring-biochemical-pathways-with-human-centric-ai]
- 82. Biochemical pathway modeling tools for drug target detection ... [https://pubmed.ncbi.nlm.nih.gov/21187230/]
- 83. Bridging the gap between preclinical and clinical research [https://pmc.ncbi.nlm.nih.gov/articles/PMC10043823/]
- 84. Cerebral Folate Deficiency Syndrome: Early Diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9370123/]
- 85. Treatment of Folate Metabolism Abnormalities in Autism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7477301/]
- 86. Leucovorin and Autism: What Pediatricians Should Know [https://www.childrensmercy.org/health-care-providers/refer-or-manage-a-patient/connect-with-childrens-mercy/newsletter-the-link/the-link-2025/the-link---october-2025/mental-health-leucovorin-and-autism-what-pediatricians-should-know/]
- 87. FOLR1-Related Cerebral Folate Transport Deficiency - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK599286/]
- 88. Leucovorin Use in Autism and Cerebral Folate Deficiency [https://www.aap.org/en/patient-care/autism/use-of-leucovorin-in-autistic-pediatric-patients/frequently-asked-questions-faqs-for-pediatricians-and-other-prescribing-pediatric-clinicians/?srsltid=AfmBOoopXRITeRAKt_2heNJofw-DOBL2-QhRosCQtTG17ufgK1ELfjb4]
- 89. Leucovorin: Uses, Interactions, Mechanism of Action [https://go.drugbank.com/drugs/DB00650]
- 90. The role of l-leucovorin uptake and metabolism in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11371747/]
- 91. FDA Takes Action to Make a Treatment Available for ... [https://www.fda.gov/news-events/press-announcements/fda-takes-action-make-treatment-available-autism-symptoms]
- 92. New advances in the diagnosis and treatment of autism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11163702/]
- 93. Treatment and Intervention for Autism Spectrum Disorder [https://www.cdc.gov/autism/treatment/index.html]
- 94. The Way Forward for Mechanism-Based Therapeutics in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6175613/]
- 95. Potential neural mechanisms underlying the effectiveness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4163495/]
- 96. A Key Brain Difference Linked to Autism Is Found for the First Time in... [https://medicine.yale.edu/news-article/a-key-brain-difference-linked-to-autism-is-found-for-the-first-time-in-living-people/]
- 97. Advancing precision diagnosis in autism: Insights from ... [https://www.sciencedirect.com/science/article/pii/S101684782500072X]
- 98. Biological subtyping of autism via cross-species fMRI - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11908180/]
- 99. Potential crosstalk between sonic hedgehog-WNT signaling and... [https://pubmed.ncbi.nlm.nih.gov/34169527/]
- 100. Characterizing Genetic Pathways Unique to Autism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11178016/]
- 101. Bidirectional genetic overlap between autism spectrum ... [https://www.nature.com/articles/s41398-023-02563-7]
- 102. W63. GENETIC OVERLAP AND SHARED RISK LOCI ... [https://www.sciencedirect.com/science/article/pii/S0924977X25005735]
- 103. Reticular thalamic hyperexcitability drives autism spectrum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366697/]
- 104. Autism symptoms vanish in mice after Stanford brain ... [https://www.sciencedaily.com/releases/2025/09/250907172644.htm]
- 105. Hyperactivity in reticular thalamic nucleus drives autism- ... [https://www.news-medical.net/news/20250820/Hyperactivity-in-reticular-thalamic-nucleus-drives-autism-like-behaviors-in-mice.aspx]
- 106. and higher-order thalamic reticular neurons in the Shank3 ... [https://www.sciencedirect.com/science/article/pii/S0969996125003250]
- 107. Reticular thalamic hyperexcitability drives autism spectrum ... [https://pubmed.ncbi.nlm.nih.gov/40834072/]