Bridging the Genotype-Phenotype Gap in Complex Diseases: From Genomic Architecture to AI-Driven Discovery
This article provides a comprehensive exploration of the strategies and technologies revolutionizing our ability to link complex genotypes to phenotypes, a central challenge in modern biomedical research.
Bridging the Genotype-Phenotype Gap in Complex Diseases: From Genomic Architecture to AI-Driven Discovery
Abstract
This article provides a comprehensive exploration of the strategies and technologies revolutionizing our ability to link complex genotypes to phenotypes, a central challenge in modern biomedical research. We examine the fundamental architecture of complex disease genetics, including the interplay between rare and common variants and the role of polygenic liability. The review covers cutting-edge methodological advances from massively parallel genetics to generative AI and machine learning frameworks that integrate multi-omics data for phenotype prediction and drug discovery. We address critical troubleshooting considerations for overcoming species translatability issues, data scarcity in rare diseases, and analytical optimization. Finally, we evaluate validation frameworks and comparative performance of emerging approaches, providing researchers and drug development professionals with actionable insights for advancing personalized medicine and therapeutic development.
The Genomic Architecture of Complex Diseases: Unraveling Variant Spectrums and Polygenic Foundations
Abstract The journey from genotype to phenotype represents a central challenge in human genetics. While Mendelian diseases follow clear inheritance patterns driven by mutations in single genes, complex diseases arise from intricate interactions between numerous genetic variants and environmental factors. This whitepaper delineates the spectrum of genetic architecture, from monogenic to highly polygenic traits, and explores the evolutionary forces and advanced methodologies shaping our understanding of these architectures. We provide a technical guide for researchers and drug development professionals, complete with standardized data tables, experimental protocols, and visualization tools to navigate this challenging landscape.
1. Introduction: From Mendelian Simplicity to Complex Trait Complexity The past decades have witnessed remarkable success in identifying approximately 1,200 genes associated with Mendelian diseases through positional cloning, fundamentally clarifying the molecular basis of these disorders [1] [2]. However, the genetic architecture of complex diseases—including diabetes, schizophrenia, and autoimmune disorders—presents a far more formidable challenge. The term "genetic architecture" refers to the comprehensive description of how genes and environment interact to produce phenotypes, encompassing the number of contributing loci, their effect sizes, allele frequencies, and patterns of epistasis and pleiotropy [3] [4]. This whitepaper examines this architectural spectrum within the broader context of mapping genotype to phenotype, providing technical guidance for researchers tackling the complexities of polygenic diseases.
2. The Architectural Spectrum of Human Disease Genetic diseases span a continuum from simple Mendelian disorders to highly complex polygenic traits, with considerable architectural diversity even among related phenotypes.
Table 1: Spectrum of Genetic Architecture in Human Diseases
| Architectural Feature | Mendelian Diseases | Complex Diseases |
|---|---|---|
| Number of Loci | Typically single gene | Dozens to thousands of loci [3] [5] |
| Variant Effect Size | Large, often necessary and sufficient for disease | Small to moderate (typically odds ratio <1.5) [3] |
| Allele Frequency | Rare to common | Common to rare, with most heritability from common variants [3] [5] |
| Environmental Influence | Often minimal | Substantial |
| Examples | Cystic Fibrosis, Huntington's disease | Height, Crohn's disease, schizophrenia [3] |
Even within "simple" Mendelian traits, striking heterogeneity exists. For instance, nearly 2,000 different mutations in the CFTR gene can cause Cystic Fibrosis, while variation at additional modifier loci influences symptom severity [3] [4]. This demonstrates that even monogenic diseases can exhibit complex phenotypic expression.
3. Evolutionary Forces Shaping Genetic Architecture The mutation-selection-drift balance (MSDB) model provides a framework for understanding how evolutionary forces shape the genetic architecture of complex diseases [6]. According to this model, genetic variation influencing disease susceptibility is introduced by mutation and removed through natural selection and genetic drift. For complex diseases with substantial fitness costs, common variation appears minimally affected by directional selection, instead being shaped primarily by pleiotropic stabilizing selection on other traits [6]. In contrast, directional selection may exert stronger effects on rare, large-effect variants. This evolutionary perspective helps explain why highly polygenic architectures persist for many common diseases.
4. Methodological Framework for Dissecting Complex Architecture 4.1 Genome-Wide Association Studies (GWAS) and the Missing Heritability Challenge GWAS has been the workhorse for identifying common variants associated with complex traits. As of 2013, a catalog of published GWAS included 1,659 publications and 10,986 associated SNPs [3]. However, a persistent challenge has been the "missing heritability" problem—the discrepancy between heritability estimates from family studies and the variance explained by significant GWAS hits [3] [4]. For example:
- For human height (heritability ~80%), 54 validated variants accounted for only ~5% of phenotypic variation [3] [4].
- For Crohn's disease, 32 identified loci explained approximately 20% of the disease heritability [3].
This missing heritability arises partly because GWAS, focused on common variants, lacks power to detect the numerous loci with very small effect sizes predicted by the infinitesimal model [3]. Yang et al. demonstrated that 294,000 SNPs collectively explained 45% of height variance, with most failing significance thresholds due to small effects [3].
Table 2: Approaches for Elucidating Genetic Architecture
| Method | Application | Insights Gained |
|---|---|---|
| GWAS with SNP arrays | Identifying common variant associations | Limited by missing heritability; small effect sizes [3] [5] |
| Whole Genome Sequencing (WGS) | Accessing rare and structural variants | Identifies rare variants with larger effects; better for understudied populations [5] |
| Genomic SEM | Modeling shared genetic factors across traits | Reveals pleiotropy; increases power for gene discovery [7] |
| Expression QTL (eQTL) mapping | Treating transcript abundance as quantitative traits | Reveals genetic architecture of gene expression [3] |
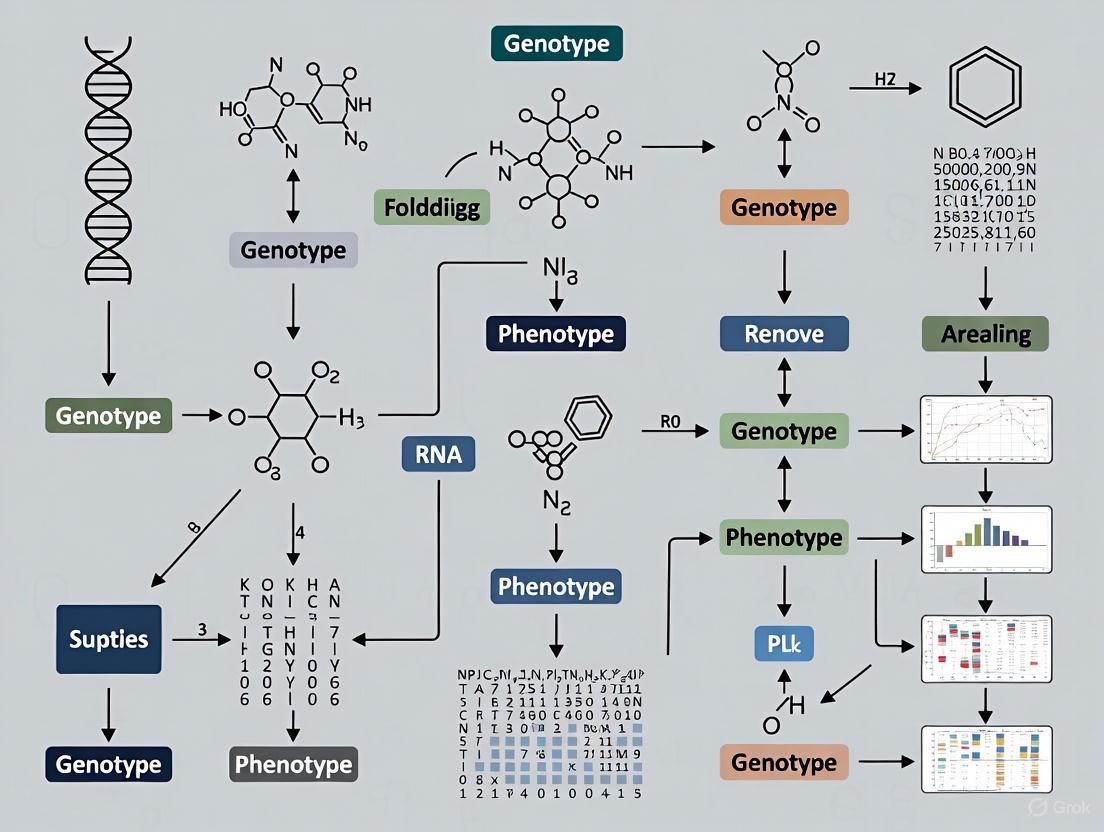
Figure 1: Integrated workflow for analyzing genetic architecture, combining multiple genomic approaches.
4.2 Whole Genome Sequencing for Rare Variant Discovery WGS provides direct access to genetic variation across the entire frequency spectrum without relying on pre-defined variant panels [5]. This technology has enabled:
- Identification of rare variants with large effect sizes, such as a cardioprotective rare variant burden in the APOC3 gene [5].
- Enhanced studies in underrepresented populations where rare or population-enriched variation is poorly characterized [5].
Despite these advances, the proportion of heritability explained by rare variants remains low for most traits. For 22 common traits, rare coding variants explain only 1.3% of phenotypic variance on average [5].
4.3 Integrative Modeling with Genomic SEM Genomic Structural Equation Modeling (Genomic SEM) enables multivariate analysis of shared genetic factors across related traits [7]. This approach integrates GWAS summary statistics from multiple cognitive traits (intelligence, educational attainment, processing speed, etc.) to model latent genetic factors, increasing power for gene discovery and illuminating pleiotropic architecture [7].
5. The Scientist's Toolkit: Research Reagents and Platforms Table 3: Essential Research Reagents and Platforms for Genetic Architecture Studies
| Resource/Platform | Type | Function | Example/Provider |
|---|---|---|---|
| BiologicalNetworks | Visualization & analysis platform | Constructs, visualizes, and analyzes biological networks; integrates heterogeneous data [8] | http://brak.sdsc.edu/pub/BiologicalNetworks [8] |
| PathSys | Data warehouse | Backend for BiologicalNetworks; integrates molecular interactions, ontologies, and expression data from 20+ databases [8] | NLM/NCBI [8] |
| GenomicSEM | R package | Multivariate method for modeling shared genetic factors across traits using GWAS summary statistics [7] | R CRAN [7] |
| Whole Genome Sequencing | Technology | Comprehensive variant detection across all frequency spectra; identifies structural variants [5] | Illumina, PacBio |
| LD Score Regression | Statistical tool | Estimates heritability and genetic correlation while correcting for confounding [7] | Bulik-Sullivan et al. |
6. Experimental Protocol: Multivariate GWAS for Cognitive Traits 6.1 Protocol: Genomic SEM Analysis for Cognitive Abilities This protocol outlines the multivariate analysis of cognitive traits using Genomic SEM [7].
Objective: To identify shared genetic architecture across cognitive ability-related traits using genomic structural equation modeling.
Input Data Preparation:
- GWAS Summary Statistics Collection: Obtain summary statistics from published GWAS on cognitive traits:
Quality Control:
- Filter to autosomal SNPs with MAF > 0.01
- Exclude SNPs with zero effect estimates
- Resolve allele strand alignment across studies
- Apply standard MHC region exclusion (chr6:25-35Mb) due to complex LD [7]
LD Reference Panel: Use 1000 Genomes Project European population data as the LD reference panel [7].
Genomic SEM Execution:
- Genetic Covariance Matrix Estimation: Calculate the genetic covariance matrix using LD Score regression [7].
- Model Fitting:
- Specify a common factor model with cognitive ability as the latent variable
- Evaluate model fit using CFI (>0.90), SRMR (<0.05), and RMSEA (<0.05) [7]
- GWAS of the Common Factor: Conduct GWAS on the latent cognitive ability factor using the weighted least squares approach in Genomic SEM [7].
Downstream Analysis:
- Gene Mapping: Apply transcriptome-wide association methods to identify candidate causal genes.
- Genetic Correlation: Assess shared genetics with brain imaging phenotypes and neuropsychiatric disorders.
- Pathway Analysis: Conduct functional enrichment analysis of identified loci.
Figure 2: Multi-omics data integration framework for elucidating biological mechanisms from genetic associations.
7. Future Directions and Clinical Translation The future of genetic architecture research lies in integrating WGS with multi-omics data (transcriptomics, proteomics, metabolomics) to functionally characterize associated variants, particularly in the non-coding genome [5]. Combining association results with functional information will be essential for translating genetic findings into biological mechanisms and therapeutic targets [5]. Additional priorities include:
- Expanding diverse population representation in genetic studies to improve equity and discovery [5]
- Developing improved statistical methods for rare variant association testing [5]
- Leveraging long-read sequencing to comprehensively assess structural variation [5]
For drug development, understanding genetic architecture enables target prioritization through variant effect size, pleiotropy assessment, and functional validation. Genes with supportive functional evidence and favorable pleiotropic profiles make promising therapeutic targets [3].
8. Conclusion The spectrum from Mendelian to complex disease architectures reflects fundamental differences in how genetic variation maps to phenotypic outcomes. While Mendelian diseases follow relatively straightforward genotype-phenotype relationships, complex diseases emerge from intricate networks of small-effect variants, rare larger-effect mutations, and environmental interactions. Advanced methodologies including WGS, multivariate approaches like Genomic SEM, and integrated network analyses are progressively illuminating this complexity. As these tools mature and datasets expand, researchers and drug developers will be increasingly equipped to decode the genetic architecture of complex diseases, ultimately enabling more targeted interventions and personalized therapeutic strategies.
The central challenge in complex disease research lies in deciphering the relationship between genotype and phenotype, a connection characterized by substantial polygenicity. Rather than being governed by single genes, most common disorders—including schizophrenia, coronary artery disease, and type 2 diabetes—arise from the cumulative effect of numerous genetic variants, each contributing modestly to overall risk [9]. This polygenic architecture has necessitated the development of quantitative methods capable of capturing this distributed genetic liability across the genome.
Polygenic risk scores (PRS) have emerged as a primary tool for quantifying this cumulative risk, providing a single metric that reflects an individual's genetic predisposition to a specific disease or trait [10]. Calculated as a weighted sum of an individual's risk alleles based on effect sizes from genome-wide association studies (GWAS), PRS effectively stratifies individuals according to their genetic susceptibility [9]. These scores represent a operationalization of the common variant burden, enabling researchers to move beyond single-variant analyses to a more comprehensive assessment of genetic risk.
The clinical and research applications of PRS are multifaceted. Beyond risk prediction, PRS provide insights into disease prognosis, mechanisms, and subtypes; illuminate shared genetic architecture between distinct disorders; and offer potential for enriching clinical trials by identifying individuals with desired risk profiles [10]. As GWAS sample sizes have expanded, revealing thousands of trait-associated variants, the predictive power of PRS has correspondingly increased, making them increasingly valuable tools for both basic research and translational applications [9].
Technical Foundations of Polygenic Scoring
Core Methodological Approaches
The computational foundation of polygenic scoring rests on integrating genome-wide association data into individualized risk metrics. Several methodological approaches have been developed, each with distinct advantages for handling the statistical challenges inherent in PRS construction.
Clumping and Thresholding methods represent one of the earliest approaches, employing linkage disequilibrium (LD)-based pruning (clumping) to select a subset of relatively independent single-nucleotide polymorphisms (SNPs). Variants are further filtered based on their association p-values from GWAS (thresholding), with scores calculated by summing allele counts weighted by their effect sizes across all SNPs meeting these criteria [9]. This approach is implemented in tools such as PRSice and PLINK and benefits from computational efficiency and straightforward interpretation.
Bayesian Methods represent a more sophisticated approach that explicitly models the underlying genetic architecture and correlation structure between variants without requiring preliminary SNP selection. LDpred, one of the most widely used Bayesian methods, employs a prior on effect sizes that accounts for LD and assumes a continuous distribution with many small effects across the genome [9]. More recent developments like SBayesR further refine this approach by using more flexible mixture priors, typically improving predictive accuracy, particularly for traits with more complex genetic architectures [9].
Ensemble Methods represent the cutting edge of PRS methodology, recognizing that no single method consistently outperforms all others across diverse traits and populations. These approaches combine PGS derived via multiple methods through meta-algorithms like elastic net models, which perform well because different methods may capture complementary aspects of the genetic architecture [11]. Evaluation across five biobanks and 16 traits demonstrated that ensemble PGS tuned in the UK Biobank provided consistent, high, and cross-biobank transferable performance, increasing PGS effect sizes by a median of 5.0% relative to the best-performing single methods [11].
Advanced Methodological Extensions
Recent methodological innovations have expanded the scope of polygenic scoring beyond common variants. Pharmagenic Enrichment Scores (PES) represent a biologically supervised framework that quantifies an individual's common variant enrichment in clinically actionable systems responsive to existing drugs [12]. Unlike standard PRS that aggregate risk across the genome, PES leverages the joint effect of common variants in pathways that can be putatively modulated by known pharmacological compounds, thus providing a pharmacologically directed annotation of genomic burden [12].
For rare variant integration, novel frameworks have been developed to construct complex trait PGS from rare variants, addressing methodological challenges distinct from common variant scoring. These approaches typically include genes based on their aggregate P-values and functional annotations, with variant weights assigned based on aggregate effect sizes for bioinformatically defined variant masks [13]. This methodology has demonstrated that rare variants can meaningfully contribute to PGS for complex traits, with one study identifying a PGS comprising 21,293 rare variants across 154 genes that significantly improved the identification of undiagnosed type 2 diabetes cases [13].
Table 1: Comparison of Primary Polygenic Scoring Methods
| Method | Core Approach | Advantages | Limitations | Implementation Examples |
|---|---|---|---|---|
| Clumping & Thresholding | Selects LD-independent SNPs below p-value threshold | Computationally efficient; straightforward interpretation | Sensitive to p-value threshold choice; may discard informative SNPs | PRSice, PLINK |
| Bayesian Methods | Models SNP effect sizes with priors accounting for LD | Captures more genetic architecture; typically higher prediction accuracy | Computationally intensive; requires LD reference panel | LDpred, SBayesR |
| Ensemble Methods | Combines scores from multiple methods | Robust performance across traits; transferable across biobanks | Increased complexity in implementation and tuning | Elastic net combinations of multiple methods |
| PES Framework | Biologically supervised pathway enrichment | Clinically actionable; targets specific drug-responsive systems | Requires specialized pathway annotation | Custom implementations based on TCRD, DGidb |
Quantitative Performance and Validation Metrics
Measures of Predictive Accuracy
The predictive utility of polygenic scores is quantified through several standardized metrics, each capturing different aspects of performance. For binary traits such as disease status, the most commonly reported metrics include the area under the receiver operating characteristic curve (AUC-ROC), which measures discriminative accuracy across all possible classification thresholds; odds ratios (OR) or hazard ratios (HR) per standard deviation increase in PGS, which quantify effect size; and variance explained on the liability scale (R²), which estimates the proportion of phenotypic variance attributable to the score [9].
For continuous traits, such as biomarker levels or cognitive performance, incremental R² (the increase in variance explained after accounting for covariates) and correlation coefficients between observed and predicted values are standard metrics [14]. The coefficient of determination (R²) is particularly useful for comparing model performance across studies, though it must be interpreted in the context of trait heritability and study design.
Recent large-scale evaluations have quantified PGS performance across diverse diseases. For example, in a multi-biobank analysis of 18 high-burden diseases, PGS hazard ratios per standard deviation ranged from 1.06 (95% CI: 1.05–1.07) for appendicitis to 2.18 (95% CI: 2.13–2.23) for type 1 diabetes [15]. The fraction of phenotypic variance explained by PGS for rare neurodevelopmental conditions was estimated at 11.2% (8.5–13.8%) on the liability scale, assuming a population prevalence of 1% [16].
Stratified Performance and Effect Modification
PGS performance is not uniform across demographic groups or clinical contexts, highlighting the importance of stratified analyses. Age significantly modifies PGS effects for many conditions, with a larger effect typically observed in younger individuals. In a study of 18 diseases, significant heterogeneity across age quartiles was detected in 13 phenotypes, with effects decreasing approximately linearly with age [15]. For type 1 diabetes, the PGS effect per standard deviation was 2.57 (95% CI: 2.47–2.68) in the youngest quartile (age < 12.6) compared to 1.66 (95% CI: 1.58–1.74) in the oldest quartile (age > 33.3) [15].
Sex-specific effects have also been identified for several conditions. Significant interactions between disease-specific PGS and sex were observed for five diseases: coronary heart disease, gout, hip osteoarthritis, and asthma showed larger effects in men, while type 2 diabetes showed a larger effect in women [15]. These stratified effects have important implications for the equitable application of PGS in clinical settings and highlight the potential for genetically informed, demographically tailored risk assessment.
Table 2: Performance of Polygenic Scores Across Selected Diseases
| Disease/Trait | Key Metric | Performance Estimate | Modifiers | Clinical Applications |
|---|---|---|---|---|
| Type 1 Diabetes | HR per SD | 2.18 (95% CI: 2.13–2.23) | Strong age effect (younger > older) | Risk stratification from early life |
| Schizophrenia | Variance explained | Pseudo-R²: 1.3–7.7% across psychosis spectrum | Cross-predictive for bipolar disorder | Differential diagnosis in psychosis spectrum |
| Coronary Heart Disease | HR per SD | Range: 1.13–1.41 across biobanks | Larger effect in men; decreases with age | Complementary to clinical risk factors |
| Rare Neurodevelopmental Conditions | SNP heritability | 11.2% (8.5–13.8%) on liability scale | Less polygenic risk in monogenic diagnoses | Elucidation of missing heritability |
| HbA1C (combined rare+common) | Reclassification OR | 2.71 (P = 1.51×10⁻⁶) | Erythrocytic variants affect diagnostic accuracy | Genetically-informed diagnostic thresholds |
Integration of Common and Rare Variant Contributions
Interplay Between Variant Classes
The traditional dichotomy between common and rare variants in complex disease etiology is increasingly being replaced by a more nuanced understanding of their interplay. Evidence suggests that complex phenotypes are influenced by both low-effect common variants and high-effect rare deleterious variants, with both contributions potentially acting additively or interactively to determine disease risk [14].
The liability threshold model provides a useful framework for understanding this relationship, proposing that individuals develop disease when their total burden of genetic and environmental risk factors exceeds a critical threshold [16]. Under this model, patients with highly penetrant rare variants (constituting a monogenic diagnosis) would require, on average, less polygenic load to cross the diagnostic threshold than those without such variants. Supporting this model, patients with rare neurodevelopmental conditions who had a monogenic diagnosis demonstrated significantly less polygenic risk than those without, consistent with the threshold model wherein those carrying highly penetrant variants require fewer common risk variants to reach the diagnostic threshold [16].
This interplay has practical implications for diagnostic yields. Analyses of neurodevelopmental disorders, hypercholesterolemia, type 2 diabetes, and certain cancers have shown that individuals carrying rare pathogenic variants tend to cluster in the low PRS range, while those with high PRS are more likely to have symptoms consistent with a complex polygenic architecture rather than a single-gene cause [17]. In one genetic obesity clinic, rare pathogenic variants in obesity genes were more than twice as common among individuals in the low-risk PRS segment [17].
Analytical Frameworks for Combined Risk Modeling
Methodological innovations now enable more integrated analysis of common and rare variant contributions. Gene-based burden scores represent one approach, collapsing information about rare functional variants within a gene into a single genetic burden score that can be used for association analysis [14]. These scores can then be integrated with PRS based on common variants for more comprehensive genetic risk modeling.
For blood biomarkers, this combined approach has revealed important patterns. Association analyses using gene-based scores for rare variants identified significant genes with heterogeneous effect sizes and directionality, highlighting the complexity of biomarker regulation [14]. For example, the ALPL gene showed a strong negative effect on alkaline phosphatase levels (effect size = -49.6), while LDLR showed a positive effect on LDL direct measurement (effect size = 23.4) [14]. However, for prediction, combined models for many biomarkers showed little or no improvement compared to PRS models alone, suggesting that while rare variants play strong roles at an individual level, common variant-based PRS might be more informative for genetic susceptibility prediction at the population level [14].
Diagram 1: Integrated Framework for Combining Common and Rare Variant Information in Polygenic Risk Modeling. This workflow illustrates the parallel processing of common variants from GWAS and rare variants from sequencing data, culminating in integrated risk models with enhanced predictive utility.
Experimental Protocols and Implementation
Standard PRS Derivation Workflow
The construction of polygenic scores follows a systematic workflow with defined quality control steps. The foundational requirement is access to genome-wide association study summary statistics from a large discovery sample, preferably from a consortium-level meta-analysis to ensure adequate power. For the target dataset, genotype data must undergo rigorous quality control, including filters for call rate, Hardy-Weinberg equilibrium, heterozygosity rates, and relatedness [9].
The core analytical steps include:
LD Reference Preparation: Obtain an appropriate reference panel matched to the ancestry of the target sample, such as the 1000 Genomes Project, to account for linkage disequilibrium patterns.
Clumping and Thresholding: For clumping-based methods, perform LD-based pruning (typically using r² < 0.1 within a 250kb window) to select independent SNPs, then apply p-value thresholds to determine which SNPs to include. Multiple thresholds (e.g., PT < 0.001, 0.05, 0.1, 0.5, 1) are often tested, with the optimal threshold selected via validation in an independent sample [12].
Score Calculation: For each individual, calculate the polygenic score as S = Σ(βᵢ × Gᵢ), where βᵢ is the effect size of SNP i from the discovery GWAS and Gᵢ is the genotype dosage (0, 1, or 2) of the effect allele [9].
Normalization: Standardize the resulting scores to have mean = 0 and standard deviation = 1 for easier interpretation and comparison.
For Bayesian methods like LDpred, the process involves:
GWAS Summary Statistics: Ensure summary statistics are properly formatted and aligned to a reference panel.
LD Estimation: Calculate the LD matrix from the reference panel.
Gibbs Sampling: Run the LDpred algorithm with recommended parameters (e.g., fraction of causal variants grid = 1, 0.3, 0.1, 0.03, 0.01, 0.003, 0.001, 0.0003) [9].
Validation: Evaluate the performance of each parameter setting in a validation sample, selecting the optimal model for application in the target dataset.
Pharmagenic Enrichment Score Protocol
The Pharmagenic Enrichment Score (PES) framework represents a specialized extension of polygenic scoring that focuses on clinically actionable pathways. The protocol involves:
Pathway Definition: Identify gene sets representing biological pathways with known drug targets using databases like TCRD (Target Central Resource Database) and DGidb (Drug Gene Interaction Database) [12].
Gene-wise Variant Enrichment: Calculate common variant enrichment for each gene at varying p-value thresholds (PT) to capture different components of the polygenic signal. Typical thresholds include all SNPs, PT < 0.5, PT < 0.05, and PT < 0.005 [12].
Pathway Scoring: Construct PES for each pathway by aggregating the cumulative effect sizes of variants within that pathway for each individual.
Clinical Annotation: Match pathway genes to known drug interactions using the DGidb database, selecting candidate pharmacological agents based on interaction confidence scores [12].
Expression Validation: Where available, validate the biological saliency of PES profiles through their impact on gene expression using matched transcriptomic data [12].
In schizophrenia research, this approach identified eight clinically actionable gene-sets with putative drug interactions, including the HIF-2 pathway (P = 3.12×10⁻⁵), one carbon pool by folate (P = 1.4×10⁻⁴), and pathways related to GABA and acetylcholine neurotransmission [12].
Rare Variant PGS Construction
The integration of rare variants into PGS requires specialized methodologies distinct from common variant approaches:
Variant Annotation: Annotate rare variants (typically MAF < 0.01) for predicted functional impact using tools like ANNOVAR, VEP, or similar pipelines, focusing on predicted high or moderate impact variants [13].
Gene-based Aggregation: Collapse rare variants by gene, considering different variant masks based on functional annotations and frequency thresholds.
Gene Selection: Include genes in the rare variant PGS based on their aggregate association p-values and supporting evidence from functional annotations or prior knowledge (e.g., from knockout mouse models) [13].
Weight Assignment: Assign weights to variants based on aggregate effect sizes for the bioinformatically defined masks that contain the variant, using a "nested" method where each variant receives a weight equal to the aggregate effect size of variants with annotations at least as severe [13].
Score Calculation: Construct the rare variant PGS by summing the weighted burden across all selected genes.
This approach has been successfully applied to hemoglobin A1C, where a rare variant PGS comprising 21,293 variants across 154 genes identified significantly more undiagnosed type 2 diabetes cases than expected by chance (OR = 2.71, P = 1.51×10⁻⁶) [13].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Resources for Polygenic Score Research
| Resource Category | Specific Tools/Databases | Primary Function | Application Notes |
|---|---|---|---|
| GWAS Summary Statistics | PGC, GWAS Catalog, IEU GWAS Database | Effect size estimates for PRS construction | Ensure ancestry matching; check for overlapping samples |
| Genotyping Platforms | Illumina Global Screening Array, UK Biobank Axiom Array | Generate genotype data for target samples | Consider imputation to reference panels for enhanced coverage |
| PRS Software | PRSice, PLINK, LDpred, LDPred2, SBayesR | Implement polygenic scoring methods | Method choice depends on trait architecture and sample size |
| LD Reference Panels | 1000 Genomes, HRC, TOPMed | Account for linkage disequilibrium | Critical for Bayesian methods; must match target ancestry |
| Functional Annotation | ANNOVAR, VEP, CADD, REVEL | Annotate variant functional impact | Essential for rare variant PGS and pathway enrichment |
| Drug-Gene Interaction | DGidb, TCRD, DrugBank | Identify clinically actionable targets | Core for pharmagenic enrichment score approaches |
| Pathway Databases | GO, KEGG, Reactome | Define biological pathways for enrichment | Enables systems-level interpretation of polygenic risk |
| Biobanks | UK Biobank, FinnGen, All of Us | Validation cohorts for PGS performance | Facilitate cross-population evaluation and method benchmarking |
Current Challenges and Future Directions
Ancestry-Related Limitations and Equity Concerns
A significant limitation in current polygenic scoring approaches is their reduced performance in non-European populations, creating potential for health disparities. The transferability of PRS across populations is limited, with scores generated from GWAS in one population typically providing attenuated predictive accuracy in other populations [9]. This limitation stems from multiple factors, including differences in linkage disequilibrium patterns, allele frequency differences, potential differences in causal variants or effect sizes, and the Eurocentric bias in most large GWAS [9].
Currently, only a small proportion of GWAS participants are of non-European ancestry, with less than 3% of study participants in the GWAS Catalog being of African ancestry as of 2020 [9]. This representation imbalance creates a critical methodological challenge: the use of tagging SNPs optimized for European populations, differences in LD patterns between populations, and SNP arrays biased to variants of European descent all contribute to reduced portability [9].
Potential solutions include large-scale GWAS in diverse populations, development of transancestral methods, and creation of ancestry-matched reference panels. Novel methods for 'polyethnic' scores, like XP-BLUP and Multi-ethnic PRS, which improve predictive accuracy by combining transethnic with ethnic-specific information, are under development [9]. Substantial investment will be needed to achieve equivalence of genetic information required for equity of access when polygenic risk scores are applied in the clinic [9].
Integration into Clinical Diagnostics
The potential integration of PRS into clinical diagnostics presents both opportunities and challenges. Several implementation scenarios have been proposed, each with distinct trade-offs:
PRS as First-Tier Screen: Using PRS to stratify patients for subsequent rare variant testing, leveraging the lower cost and faster turnaround time of SNP arrays compared to sequencing. This approach may be cost-effective for increasing the diagnostic yield of whole-exome sequencing, particularly for disorders where both monogenic and polygenic forms exist [17].
Parallel Testing: Performing rare variant detection and common variant analysis simultaneously from whole-genome sequencing data. This comprehensive approach provides both monogenic and polygenic risk information in a single assay but raises challenges related to data storage, interpretation complexity, and potential secondary findings [17].
Selective Testing Based on Clinical Features: Prioritizing either PRS or rare variant testing based on specific clinical characteristics, such as the presence of syndromic features or early disease onset. This patient-centered approach aligns with current clinical practice but requires maintaining multiple diagnostic workflows [17].
PRS in Unexplained Cases: Applying PRS only after negative results from rare variant testing, helping to identify patients in whom a polygenic contribution to disease risk is more likely. This approach reserves costly sequencing for cases with higher pre-test probability of monogenic causes [17].
Key challenges for clinical implementation include defining clinically meaningful risk thresholds, translating relative risks to absolute risks through accurate calibration, developing standards for reporting and interpretation, and ensuring equitable performance across diverse patient populations [17].
Diagram 2: Clinical Decision Framework for Integrating PRS and Rare Variant Testing. This diagnostic workflow illustrates how clinical features can guide test selection, with PRS particularly valuable for cases lacking classic monogenic presentations.
Polygenic scores represent a powerful approach for quantifying the cumulative impact of common genetic variants on complex disease risk, providing a crucial bridge between genotype and phenotype in complex diseases research. As methodological refinements continue and GWAS sample sizes expand, the accuracy and utility of these scores will further improve. The integration of PRS with rare variant information, clinical biomarkers, and environmental factors will enable more comprehensive risk prediction models. However, realizing the full potential of polygenic scoring will require addressing critical challenges related to ancestry-based performance disparities, clinical implementation pathways, and ethical considerations. As these challenges are met, polygenic scores are poised to become increasingly integral to both basic research and clinical application in complex disease genetics.
The central challenge in modern genetics lies in elucidating the pathway from genetic blueprint to observable trait or disease manifestation—the genotype to phenotype problem. Complex human diseases such as diabetes, cancer, and asthma are rarely governed by single-gene mutations but rather emerge from intricate networks of multiple genes working in concert [18]. The sheer number of possible gene combinations creates a formidable analytical challenge for researchers attempting to pinpoint specific causal factors. Systems biology approaches that map gene regulatory networks and protein-protein interactions provide the foundational framework for understanding how genetic information flows through biological systems to produce phenotypic outcomes. These networks represent the functional architecture through which cellular states are established, maintained, and disrupted in disease pathology. Recent advances in artificial intelligence, single-cell technologies, and network reconstruction algorithms are now enabling unprecedented resolution in modeling these complex relationships, offering new pathways for therapeutic intervention in complex diseases [18] [19].
Computational Methodologies for Network Reconstruction
AI-Driven Identification of Causal Gene Sets
The Transcriptome-Wide conditional Variational auto-Encoder represents a breakthrough in generative artificial intelligence for identifying gene combinations underlying complex traits. Unlike traditional methods that examine individual gene effects in isolation, TWAVE employs a sophisticated approach combining machine learning with optimization to identify groups of genes that collectively cause complex traits to emerge. The model amplifies limited gene expression data, enabling researchers to resolve patterns of gene activity that cause complex traits by emulating diseased and healthy states so that changes in gene expression can be matched with changes in phenotype [18].
A key innovation of this approach is its focus on gene expression rather than gene sequence, providing dynamic snapshots of cellular activity that implicitly account for environmental factors which can turn genes "up" or "down" to perform various functions. The method uses an optimization framework to pinpoint specific gene changes most likely to shift a cell's state from healthy to diseased or vice versa. When tested across several complex diseases, TWAVE successfully identified disease-causing genes—some missed by existing methods—and revealed that different sets of genes can cause the same complex disease in different people, suggesting personalized treatments could be tailored to a patient's specific genetic drivers of disease [18].
Population-Level Gene Regulatory Network Inference
SCORPION represents another significant advancement for reconstructing comparable gene regulatory networks from single-cell/nuclei RNA-sequencing data suitable for population-level studies. The algorithm addresses critical challenges in single-cell data analysis, including high sparsity and cellular heterogeneity, which have previously limited robust network comparisons across samples [19] [20].
The SCORPION algorithm implements a five-step iterative process:
- Coarse-graining: Highly sparse single-cell data are processed by collapsing a k number of the most similar cells identified at the low-dimensional representation of the multidimensional RNA-seq data, reducing sample size while decreasing data sparsity.
- Initial network construction: Three distinct initial unrefined networks are built as described in the PANDA algorithm: the co-regulatory network (representing co-expression patterns between genes), the cooperativity network (accounting for known protein-protein interactions between transcription factors from STRING database), and the regulatory network (describing relationships between transcription factors and their target genes through transcription factor footprint motifs).
- Availability and responsibility calculation: A modified version of Tanimoto similarity designed for continuous values generates the availability network (representing information flow from a gene to a transcription factor) and the responsibility network (representing information flow from a transcription factor to a gene).
- Network updating: The average of the availability and responsibility networks is computed, and the regulatory network is updated to include a user-defined proportion (α = 0.1 by default) of information from the other two original unrefined networks.
- Iterative refinement: Steps three to five are repeated until the Hamming distance between networks reaches a user-defined threshold (0.001 by default) [19].
Table 1: Performance Comparison of Network Reconstruction Methods
| Method | Precision | Recall | Transcriptome-Wide Capability | Prior Information Integration |
|---|---|---|---|---|
| SCORPION | 18.75% higher than other methods | 18.75% higher than other methods | Excellent | Yes (multiple sources) |
| PPCOR | Similar to SCORPION | Similar to SCORPION | Limited | Limited |
| PIDC | Similar to SCORPION | Similar to SCORPION | Limited | Limited |
| WGCNA | Lower than SCORPION | Lower than SCORPION | Moderate | No |
When systematically evaluated against 12 other network construction techniques using BEELINE, SCORPION generated 18.75% more precise and sensitive gene regulatory networks than other methods and consistently ranked first across seven evaluation metrics [19]. The method has demonstrated particular utility in identifying differences in regulatory networks between wild-type and transcription factor-perturbed cells, and has shown scalability to population-level analyses using a single-cell RNA-sequencing atlas containing 200,436 cells from colorectal cancer and adjacent healthy tissues [20].
Deep Learning Architectures for Protein-Protein Interaction Prediction
Deep learning has revolutionized protein-protein interaction prediction through several core architectural paradigms. Graph Neural Networks (GNNs) based on graph structures and message passing adeptly capture local patterns and global relationships in protein structures by aggregating information from neighboring nodes to generate representations that reveal complex interactions and spatial dependencies [21].
Key GNN variants include:
- Graph Convolutional Networks (GCNs) employ convolutional operations to aggregate information from neighboring nodes, making them highly effective for node classification and graph embedding tasks.
- Graph Attention Networks (GATs) introduce an attention mechanism that adaptively weights neighboring nodes based on their relevance, enhancing flexibility for graphs with diverse interaction patterns.
- GraphSAGE is designed for large-scale graph processing, utilizing neighbor sampling and feature aggregation to reduce computational complexity.
- Graph Autoencoders (GAEs) utilize an autoencoder-based approach with GCN layers to generate compact low-dimensional node embeddings for graph reconstruction or predictive tasks [21].
Innovative frameworks like AG-GATCN integrate GAT and temporal convolutional networks to provide robust solutions against noise interference in PPI analysis, while RGCNPPIS integrates GCN and GraphSAGE to simultaneously extract macro-scale topological patterns and micro-scale structural motifs. The Deep Graph Auto-Encoder innovatively combines canonical auto-encoders with graph auto-encoding mechanisms for hierarchical representation learning [21].
Experimental Protocols and Methodologies
TWAVE Implementation Protocol
The TWAVE framework requires specific computational and data processing steps for proper implementation:
Data Requirements and Preparation:
- Collect gene expression data from clinical samples with known disease status (healthy vs. diseased)
- Ensure data privacy by using expression data rather than genetic sequence data
- Normalize expression data to account for technical variability across samples
- Partition data into training and validation sets
Model Training Procedure:
- Initialize the conditional variational autoencoder with appropriate architecture dimensions
- Train the model to learn latent representations that capture the joint distribution of gene expression profiles and phenotypic states
- Implement optimization to identify minimal gene changes that shift cellular states
- Validate model predictions against experimental perturbation data where available
- Perform cross-validation to ensure robustness of identified gene sets
Validation and Interpretation:
- Compare identified gene sets with known disease-associated pathways
- Test robustness across different patient subgroups
- Validate predictions in independent cohorts where possible
- Interpret results in context of potential multi-target therapeutic strategies [18]
SCORPION Experimental Workflow
Input Data Preparation:
- Obtain single-cell or single-nuclei RNA-sequencing count data
- Perform quality control to remove low-quality cells and genes
- Normalize data using standard single-cell processing pipelines
- Identify and remove technical artifacts using appropriate batch correction methods
Network Reconstruction:
- Construct SuperCells or MetaCells by grouping similar cells to reduce sparsity
- Download protein-protein interaction data from STRING database
- Obtain transcription factor binding motif data from relevant databases (JASPAR, TRANSFAC)
- Set algorithm parameters (convergence threshold = 0.001, α = 0.1)
- Execute iterative message-passing algorithm until convergence
- Extract final regulatory network as matrix with transcription factors in rows and target genes in columns [19]
Differential Network Analysis:
- Reconstruct networks for different experimental conditions (e.g., healthy vs. diseased)
- Compare edge weights between conditions to identify significant changes
- Perform enrichment analysis on differentially regulated targets
- Validate findings using orthogonal methods or perturbation data [20]
SCORPION Algorithm Workflow: From single-cell data to gene regulatory networks.
Enhanced Genetic Discovery Using Predicted Phenotypes
Recent methodological advances demonstrate how machine learning-derived continuous disease representations can enhance genetic discovery beyond traditional case-control genome-wide association studies. This approach involves:
Continuous Phenotype Generation:
- Train machine learning models using comprehensive electronic health record data to generate continuous predicted representations of eight complex diseases
- Ensure model calibration using Brier scores and validate discriminant ability using AUROC and AUPRC metrics
- Generate right-skewed probability distributions representing disease probabilities
Genetic Association Analysis:
- Test common variant associations with both case-control and predicted phenotypes
- Assess genetic correlations between predicted and case-control phenotypes
- Perform multi-trait analysis of GWAS to integrate information from both phenotype types
- Calculate LD-independent variants and heritability estimates for each approach [22]
Validation and Interpretation:
- Replicate findings in independent cohorts
- Assess enrichment in known biological pathways
- Evaluate potential spurious associations
- Compare drug target identification capabilities between methods [22]
Table 2: Performance of Predicted vs. Case-Control Phenotypes in Genetic Discovery
| Metric | Case-Control Phenotypes | Predicted Phenotypes | Improvement |
|---|---|---|---|
| Median LD-independent variants | 125 | 306 | 160% increase |
| Median genes identified | 91 | 252 | 180% increase |
| Median genetic correlation | 0.66 (with case-control) | 0.66 (with case-control) | - |
| Replication rate at nominal significance | - | 79-90% (AFib, CAD, T2D) | - |
| Drug targets identified | Baseline | +14 additional genes | Enhanced target prioritization |
Table 3: Key Research Reagents and Computational Resources
| Resource Category | Specific Tools/Databases | Function/Application |
|---|---|---|
| Network Reconstruction Algorithms | TWAVE, SCORPION, PANDA | Identify multi-gene determinants of disease and reconstruct regulatory networks from single-cell data |
| PPI Databases | STRING, BioGRID, IntAct, MINT, HPRD | Source of known and predicted protein-protein interaction data |
| Gene Expression Data | Single-cell RNA-seq, Bulk RNA-seq | Input data for network inference and expression quantification |
| Deep Learning Frameworks | GCN, GAT, GraphSAGE, Graph Autoencoders | Predict PPIs and model complex network relationships |
| Evaluation Tools | BEELINE | Systematic benchmarking of network reconstruction algorithms |
| Motif Databases | JASPAR, TRANSFAC | Source of transcription factor binding site information |
| Pathway Databases | Reactome, KEGG | Contextualize findings within known biological pathways |
Analytical Frameworks for Network Interpretation
Comparative Analysis of Network Modeling Approaches
Research comparing gene-gene co-expression network approaches for analyzing cell differentiation and specification on single-cell RNA sequencing data reveals that network modeling choice has less impact on downstream results than the network analysis strategy selected. The largest differences in biological interpretation were observed between node-based and community-based network analysis methods, with additional distinctions between single time point and combined time point modeling [23].
Differential gene expression-based methods have demonstrated superior performance in modeling cell differentiation processes, while combined time point modeling approaches generally yield more stable results than single time point modeling. These findings highlight the importance of selecting analytical strategies matched to specific biological questions rather than relying on a one-size-fits-all approach to network analysis [23].
Visualization and Interpretation of Network Relationships
Information Flow from Genotype to Phenotype: How genetic variation propagates through molecular networks.
Applications in Complex Disease Research and Therapeutic Development
The application of systems biology approaches to gene networks and protein interactions has yielded significant insights into complex disease mechanisms. In colorectal cancer, SCORPION analysis of single-cell RNA-sequencing data from 200,436 cells derived from 47 patients revealed differences between intra- and intertumoral regions consistent with established understanding of disease progression through the chromosomal instability pathway. These findings were confirmed in an independent cohort of patient-derived xenografts from left- and right-sided tumors and provided insight into phenotypic regulators that may impact patient survival [20].
Similarly, the TWAVE framework has demonstrated that different sets of genes can cause the same complex disease in different people, suggesting personalized treatments could be tailored to a patient's specific genetic drivers of disease. This finding has profound implications for precision medicine approaches to complex diseases, moving beyond one-size-fits-all therapeutic strategies toward targeted interventions based on individual network pathology [18].
The integration of predicted continuous phenotypes with traditional genetic association approaches has identified 14 genes targeted by phase I–IV drugs that were not identified by case-control phenotypes alone. Combined polygenic risk scores using both phenotype types demonstrated improved prediction performance with a median 37% increase in Nagelkerke's R2, highlighting the utility of these approaches for enhancing drug target prioritization and risk prediction across diverse populations [22].
These advances collectively represent a paradigm shift in our approach to complex disease, transforming the conceptual framework from one focused on individual molecular components to one embracing the complex network interactions that ultimately determine phenotypic outcomes.
The relationship between genetic variation and phenotypic manifestation represents a central challenge in modern biomedical research. This whitepaper synthesizes current understanding of how mutations—from nearly neutral to strongly deleterious—distribute across populations and influence complex disease etiology. We examine the population genetic principles governing mutation-selection-balance, explore advanced computational and experimental methodologies for quantifying mutational effects, and demonstrate how integrating diverse data modalities enhances gene discovery and therapeutic target identification. Framed within the context of linking genotype to phenotype, this review provides researchers and drug development professionals with a technical framework for interpreting mutational impact across the effect-size spectrum.
The comprehensive mapping of genetic variation to phenotypic outcomes requires understanding the full distribution of fitness effects (DFE). The DFE describes the spectrum of selection coefficients for new mutations, ranging from strongly deleterious variants removed by purifying selection to nearly neutral variants whose dynamics are shaped by genetic drift, and rare beneficial mutations that drive adaptation [24] [25]. The shape of the DFE is not static; it is influenced by genetic background, environment, effective population size, and mutation bias—the non-random occurrence of certain mutation types over others [24].
In complex disease research, this framework is paramount. While strongly deleterious, rare variants often underlie Mendelian disorders, nearly neutral variants with subtle effects contribute significantly to complex disease architecture through polygenic mechanisms. Recent technological advances, including large-scale biobanks, machine learning, and high-throughput experimental assays, are now enabling unprecedented resolution in characterizing this mutational spectrum and its consequences for human health.
Theoretical Framework and Population Genetic Principles
Mutation-Selection-Drift Balance
The population frequency of deleterious alleles reflects a balance between the rate at which new mutations arise, their selective cost, and random fluctuations due to genetic drift. For semidominant mutations with heterozygous fitness cost hs, the expected equilibrium frequency is approximately u/(hs), where u is the mutation rate [26]. This model predicts that highly deleterious alleles will be maintained at similarly low frequencies across all ancestry groups due to recurrent mutation, a prediction supported by empirical data from gnomAD showing that protein-coding disruptions (e.g., loss-of-function alleles in constrained genes) occur at comparably low frequencies across diverse populations [26].
Table 1: Key Population Genetic Parameters Governing Mutation Distributions
| Parameter | Symbol | Biological Meaning | Impact on DFE |
|---|---|---|---|
| Effective Population Size | Ne | Number of individuals contributing genes to next generation | Determines efficacy of selection vs. drift on nearly neutral mutations |
| Selection Coefficient | s | Relative fitness reduction of genotype | Directly determines strength of selection against a variant |
| Mutation Rate | u | Probability of a mutation per generation per site | Governs input of new genetic variation |
| Dominance Coefficient | h | Proportion of selection effect expressed in heterozygotes | Affects visibility of recessive alleles to selection |
Demographic History and Ancestry
Demographic processes profoundly influence the distribution of deleterious variation. Population bottlenecks, such as those experienced by non-African populations, reduce the efficacy of purifying selection against nearly neutral variants, allowing mildly deleterious alleles to drift to higher frequencies [25]. Consequently, non-African populations often harbor a higher proportion of rare, deleterious variants and a greater number of homozygous derived deleterious genotypes per individual compared to African populations [25]. However, despite these distributional differences, the overall genetic load—the cumulative fitness reduction from deleterious alleles—is remarkably similar across human populations [26] [25]. This apparent paradox is resolved by considering that while non-African populations may carry more deleterious alleles at intermediate frequencies, African populations harbor a greater number of very rare deleterious variants due to their larger effective population size and greater genetic diversity [25].
Quantitative Analysis of Mutation Effects
Empirical Characterization of the DFE
Experimental studies in model organisms provide direct measurements of how mutation bias influences the DFE. Research in Escherichia coli demonstrates that reversing the ancestral transition mutation bias (97% transitions) to a transversion bias (98% transversions) shifts the DFE, increasing the proportion of beneficial mutations by providing access to previously under-sampped mutational space [24]. Conversely, reinforcing the ancestral bias depletes beneficial mutations. This demonstrates that the DFE is not a fixed property but is dynamically shaped by the interplay between a population's mutational history and its current mutation spectrum.
Table 2: Experimentally Determined Distribution of Fitness Effects in E. coli Mutator Strains
| E. coli Strain | Mutation Bias | Key Finding on DFE | Experimental Environment |
|---|---|---|---|
| Wild Type | ~54% Transitions (Ts) | Baseline DFE | Lysogeny Broth (LB) and M9 Glucose |
| Strong Ts Bias (e.g., ΔmutT) | Up to 97% Ts | Up to 10-fold fewer beneficial mutations | Lysogeny Broth (LB) and M9 Glucose |
| Strong Tv Bias (e.g., ΔmutY) | Up to 98% Transversions (Tv) | Highest proportion of beneficial mutations (~6% increase) | Lysogeny Broth (LB) and M9 Glucose |
Mutation Rate and Adaptive Evolution
The relationship between mutation rate and adaptation speed is complex and non-linear. Evolution experiments using E. coli mutator strains with varying mutation rates exposed to five different antibiotics revealed that adaptation speed generally increases with mutation rate [27]. However, an optimum exists; the strain with the very highest mutation rate showed a significant decline in evolutionary speed, likely due to the accumulation of deleterious mutations that overwhelm any beneficial effects [27]. This relationship further depends on the selective environment, varying between bacteriostatic and bactericidal antibiotics.
Methodological Approaches for Assessing Mutational Impact
Computational Protein Mutation Effect Predictors
Accurately predicting the functional consequences of missense mutations is crucial for interpreting genetic variation. Computational predictors are broadly categorized into sequence-based, structure-informed, and evolutionary approaches. The VenusMutHub benchmark, which evaluated 23 models on 905 small-scale experimental datasets spanning 527 proteins, provides practical guidance for method selection based on the target property (e.g., stability, activity, binding affinity) [28].
Physics-based methods like Free Energy Perturbation (FEP) simulations offer a rigorous, first-principles approach. The QresFEP-2 protocol, a hybrid-topology FEP method, demonstrates excellent accuracy in predicting mutation-induced changes in protein stability, protein-ligand binding, and protein-protein interactions, serving as a powerful tool for protein engineering and drug design [29].
Diagram 1: QresFEP-2 Workflow for Predicting Mutation Effects on Protein Stability.
AI and Knowledge-Guided Deep Learning for Complex Disease
For complex, polygenic diseases, new computational approaches move beyond single-variant analysis. The TWAVE model uses a generative AI framework to identify groups of genes that collectively cause complex traits by analyzing gene expression data, thereby bridging the gap between genotype and phenotype while implicitly accounting for environmental factors [18].
In the challenging domain of rare genetic diseases, where labeled data is scarce, the SHEPHERD framework employs few-shot learning. It trains a graph neural network on a knowledge graph enriched with rare disease information and simulated patient data to perform causal gene discovery and patient similarity matching, demonstrating effectiveness in diagnosing patients with novel disease presentations [30].
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents and Computational Tools
| Tool/Reagent | Type | Primary Function | Application Context |
|---|---|---|---|
| gnomAD Database | Data Resource | Catalog of genetic variation from diverse populations | Population-level frequency analysis of variants [26] |
| E. coli Keio Collection | Biological Strain | Library of single-gene knockouts in E. coli | Study of gene function and mutational effects [24] |
| QresFEP-2 Software | Computational Tool | Hybrid-topology Free Energy Perturbation | Predict ΔΔG of point mutations on stability/binding [29] |
| SHEPHERD Framework | AI Model | Knowledge-grounded graph neural network | Few-shot learning for rare disease diagnosis [30] |
| Exomiser | Bioinformatics Pipeline | Variant prioritization tool | Filters candidate genes from WES/WGS data [30] |
| VenusMutHub | Benchmark Platform | Systematic evaluation of predictors | Compare performance of 23 mutation effect models [28] |
Applications in Complex Disease Gene Discovery and Drug Target Prioritization
Linking the DFE to complex disease requires sophisticated phenotyping strategies. Traditional case-control definitions in GWAS often inadequately capture disease heterogeneity. Using machine learning to generate continuous predicted phenotypes from electronic health records (EHRs) significantly enhances genetic discovery. For eight complex diseases, this approach increased the number of identified independent associations by a median of 160% and uncovered 14 genes targeted by phase I–IV drugs that were missed by case-control analyses [22].
Furthermore, integrating these continuous phenotypes into polygenic risk scores (PRS) improved prediction performance, with a median 37% increase in Nagelkerke's R², and enhanced portability across diverse ancestry populations [22]. This demonstrates that refining phenotypic definitions to better reflect the continuous spectrum of disease can powerfully accelerate the mapping from genetic variation to clinical outcome.
Diagram 2: Enhancing Gene Discovery with Continuous Phenotypes and MTAG.
The journey from genetic variant to organismal phenotype is governed by the complex interplay of evolutionary forces encapsulated in the distribution of mutation effects. Key insights emerge: first, strongly deleterious variants are universally rare, but the spectrum of nearly neutral variation is shaped by demographic history and mutation bias. Second, accurately mapping these effects requires a multi-faceted methodological arsenal, from physics-based simulations and AI-driven knowledge graphs to advanced phenotyping from EHRs. Finally, embracing the full complexity of the DFE—and moving beyond simplistic binary models of mutation effect—is essential for unraveling the genetic architecture of complex diseases and translating these insights into novel therapeutic strategies. The continued integration of population genetic theory, large-scale biobank data, and sophisticated computational tools promises to further refine our understanding and accelerate personalized medicine.
The Mutation-Selection Balance and Evolutionary Forces Shaping Disease Genes
Understanding the genetic architecture of complex diseases requires a framework that links static genetic blueprints (genotype) to dynamic, observable outcomes (phenotype). This relationship is not linear but is shaped and filtered by evolutionary forces over generations. The core thesis of modern complex disease research posits that the prevalence and genetic architecture of common, polygenic diseases are a direct consequence of an evolutionary equilibrium between the introduction of new genetic variation by mutation and its removal by natural selection and genetic drift—the mutation-selection-drift balance (MSDB) [31]. This guide explores the technical foundations of this balance, its quantitative modeling, and the experimental paradigms used to decipher how evolutionary forces shape the disease-associated genes we study today.
The Mutation-Selection-Drift Balance (MSDB) Model: A Quantitative Framework
The MSDB model provides a population genetics framework to predict the distribution of genetic effects and allele frequencies for variants influencing disease risk. For complex, polygenic diseases with substantial fitness costs, the model moves beyond classic Mendelian assumptions [31].
Core Assumptions of the Complex Disease MSDB Model:
- Genetic Architecture: Disease risk is influenced by many loci of small effect, consistent with the liability threshold model.
- Selection Source: Selection against disease-risk variants stems primarily from the fitness cost of the disease itself.
- Evolutionary Forces: The population frequency of a risk variant is determined by the equilibrium between its mutation rate (introduction), the selection coefficient against it (removal), and random genetic drift.
A key prediction from recent modeling is that for common diseases, common genetic variation (e.g., GWAS hits) appears to be largely unaffected by strong directional selection related to the disease. Instead, its frequency is likely shaped by pleiotropic stabilizing selection on other traits. Stronger directional selection is predicted to act more efficiently on rare, large-effect variants [31]. This has profound implications for interpreting GWAS results and estimating true disease heritability, which current methods may systematically bias [31].
Evolutionary Driving Forces and Their Impact on Disease Gene Architecture
The MSDB operates through the interplay of four fundamental evolutionary forces, each leaving a distinct signature on the genetic landscape of disease [32].
- Mutation: The ultimate source of new genetic variation, including deleterious alleles that increase disease risk. The rate and effect size spectrum of mutations are critical parameters in MSDB models [33].
- Natural Selection:
- Negative/Purifying Selection: Removes deleterious, high-penetrance disease alleles from the population. This is a primary force in the MSDB for diseases with high fitness costs [32].
- Positive Selection: Can increase the frequency of an allele that is advantageous in a specific environment, potentially carrying linked disease-risk alleles to higher frequency via genetic hitchhiking (e.g., the IBD5 risk haplotype and Crohn's disease) [32].
- Balancing Selection: Maintains multiple alleles at a locus, often when heterozygotes have a fitness advantage. This can preserve ancient disease-risk alleles in populations, as hypothesized for some autoimmune disorders under the "hygiene hypothesis" [32].
- Genetic Drift: Random fluctuations in allele frequencies, particularly powerful in small or founder populations. Drift can allow deleterious alleles to rise in frequency, contributing to population-specific disease risk [33].
- Gene Flow: The transfer of genetic variation between populations through migration. It can introduce new disease alleles or dilute existing ones, altering local MSDB dynamics [32].
Data Synthesis: Quantitative Parameters from Evolutionary Genetics Studies
The following tables summarize key quantitative data and genetic parameters relevant to modeling the evolution of complex diseases.
Table 1: Estimated Parameters for Mutation-Selection-Drift Balance Models in Complex Diseases
| Parameter | Symbol | Typical Estimated Range/Value | Biological Interpretation | Source Context |
|---|---|---|---|---|
| Selection Coefficient (against risk allele) | s | ~0.001 - 0.05 for moderately deleterious variants | Strength of natural selection acting to remove the allele from the population. | Inferred from MSDB models [31] |
| Mutation Rate (per locus per generation) | μ | ~1.2 x 10⁻⁸ per base pair (human genome average) | Rate at which new risk alleles are introduced. | Standard population genetic parameter |
| Heritability (in the wild) | h² | Often lower than GWAS estimates | Proportion of phenotypic variance due to genetic factors under real-world selection. MSDB suggests GWAS estimates are biased upward [31]. | Prediction from MSDB theory [31] |
| Population-Scaled Selection Coefficient | γ = 2Nₑs | Determines whether selection (γ >> 1) or drift (γ << 1) dominates an allele's fate. | Core parameter in population genetics |
Table 2: Evolutionary Signatures in Human Complex Disease Genetics
| Evolutionary Force | Genetic Signature | Example Disease Association | Method of Detection |
|---|---|---|---|
| Positive Selection | Long-range haplotype homozygosity, extreme allele frequency differentiation (FST) | Lactase persistence (LCT), Malaria resistance (HbS, G6PD) | iHS, XP-EHH, FST scans [32] |
| Balancing Selection | High genetic diversity, intermediate allele frequency, trans-species polymorphism | Major Histocompatibility Complex (MHC) loci, Inflammatory Bowel Disease (IL23R pathway) | Tajima's D, Hudson-Kreitman-Aguadé test [32] |
| Purifying Selection | Depletion of common variants, enrichment of rare, functional variants in coding regions | Severe developmental disorders, highly penetrant cancer genes (BRCA1) | Comparison of rare vs. common variant burden [32] |
| Genetic Drift / Founder Effect | High frequency of specific rare variant in an isolated population | Finnish disease heritage (e.g., Northern Epilepsy), Ashkenazi Jewish disorders (e.g., Gaucher) | Population-specific allele frequency analysis |
Experimental Protocols for Investigating Evolutionary Forces on Disease Genes
Protocol 1: Genome-Wide Scans for Natural Selection
- Objective: Identify genomic regions that have undergone recent positive or balancing selection by analyzing patterns of genetic variation.
- Workflow:
- Data Generation: Obtain high-coverage whole-genome sequencing or dense genotype data from multiple individuals across populations (e.g., 1000 Genomes Project).
- Variant Calling & Phasing: Use tools like GATK and SHAPEIT to identify variants and reconstruct haplotype phases.
- Selection Statistic Calculation: Compute statistics per SNP or region:
- iHS (Integrated Haplotype Score): Detects recent positive selection by measuring the length of shared haplotypes around a core allele.
- Tajima's D: Identifies deviations from neutral evolution (negative D suggests positive/balancing selection; positive D suggests balancing selection/population contraction).
- FST: Measures genetic differentiation between populations; high FST can indicate local adaptation.
- Significance Testing: Compare observed statistics to a null distribution generated from coalescent simulations under a neutral model.
- Functional Annotation: Overlap significant regions with GWAS loci, coding exons, and regulatory elements to link selection signals to disease phenotypes [32].
Protocol 2: Estimating Selection Coefficients (s) from Population Genetic Data
- Objective: Quantify the strength of natural selection acting on a specific disease-associated variant.
- Workflow:
- Allele Frequency Spectrum (AFS) Modeling: Fit the observed distribution of allele frequencies for putatively deleterious variants (e.g., loss-of-function mutations) to a population genetic model that includes parameters for mutation rate (μ), effective population size (Nₑ), and selection coefficient (s).
- Use the Site Frequency Spectrum (SFS): Tools like
dadiorfastsimcoal2can infer demographic history and selection parameters by comparing the observed SFS to simulated ones. - Leverage Allele Age and Trajectory: For a known pathogenic allele, estimate its age using linkage disequilibrium decay or phylogenetic methods. Its current frequency and estimated age can be used to infer the selective pressure it has experienced, often using forward simulations.
- Constraint Metrics: Use metrics like pLI (probability of being loss-of-function intolerant) from gnomAD, which indirectly reflect the strength of purifying selection on a gene over evolutionary time.
Visualizing Concepts and Workflows
Title: Evolutionary Forces Influencing Disease Allele Frequencies
Title: MSDB Model Simulation and Inference Workflow
Table 3: Essential Resources for Evolutionary Analysis of Disease Genes
| Item / Resource | Function / Description | Example / Source |
|---|---|---|
| Population Genomic Datasets | Provide the raw allele frequency and haplotype data needed to compute selection statistics and fit models. | 1000 Genomes Project, gnomAD, UK Biobank, TOPMed. |
| GWAS Catalog & Summary Statistics | Source of published disease-variant associations for cross-referencing with signals of selection. | NHGRI-EBI GWAS Catalog, GWAS ATLAS. |
| Selection Scan Software | Tools to compute statistics (Tajima's D, iHS, XP-EHH) and identify genomic regions under selection. | PLINK, SELSCAN, PopGenome (R). |
| Population Genetic Simulators | Generate expected genetic data under complex models of demography and selection for hypothesis testing. | SLiM (forward-time), msms/COAL (coalescent), dadi. |
| Functional Annotation Databases | Annotate significant variants/regions with gene context, regulatory element maps, and disease ontology terms. | ENSEMBL, ANNOVAR, GeneHancer, DISEASES [34]. |
| Curated Gene-Disease Evidence | Provides manually curated scores for gene-disease associations, crucial for prioritizing candidates from selection scans. | DISEASES Curated Gene-Disease Association Evidence Scores [34]. |
| High-Performance Computing (HPC) Cluster | Essential for running large-scale genomic analyses, simulations, and data processing. | Local university cluster, cloud computing (AWS, GCP). |
Next-Generation Mapping Technologies: From Deep Mutational Scanning to Generative AI
Understanding the relationship between genetic variation (genotype) and observable traits or disease states (phenotype) remains a fundamental challenge in biomedical research. This is particularly true for complex diseases, such as type 2 diabetes, amyotrophic lateral sclerosis (ALS), and many cancers, where phenotypic outcomes are shaped by the interplay of numerous genetic variants, environmental factors, and complex biological networks rather than single-gene defects [35] [36]. For decades, genetic mapping studies were limited by throughput, cost, and resolution. The advent of massively parallel genetics—high-throughput methodologies that enable the simultaneous functional assessment of thousands to millions of genetic variants—has revolutionized our ability to decipher these complex relationships.
Two cornerstone methodologies in this field are Deep Mutational Scanning (DMS) and related EMPIRIC approaches. DMS combines comprehensive mutagenesis with high-throughput functional selection and deep sequencing to quantify the effects of thousands of mutations in a single, highly multiplexed experiment [37] [38]. These technologies provide an unprecedented, high-resolution view of how sequence changes affect protein function, protein-protein interactions, and cellular fitness. By systematically probing the genotype-phenotype map, DMS and EMPIRIC empower researchers to interpret human genetic variation, identify pathogenic mutations, understand drug resistance, and reveal fundamental principles of protein structure and function, thereby directly informing drug discovery and development efforts [39] [40].
Core Principles and Methodologies of Deep Mutational Scanning
A typical DMS experiment follows a structured, three-stage pipeline designed to link genotype to phenotype on a massive scale [37] [38]. The core concept is to measure the change in frequency of each variant in a mutant library before and after a functional selection, thereby inferring its effect on fitness or activity.
The Deep Mutational Scanning Workflow
The workflow can be broken down into three main stages, as illustrated in the diagram below.
Key Methodological Components
Generating a Comprehensive Mutant Library
The first and crucial step is constructing a library that encompasses a wide spectrum of genetic diversity for the gene of interest. Several methods are employed, each with distinct advantages and limitations [37] [38].
- Error-Prone PCR: This method uses low-fidelity DNA polymerases to introduce random mutations during PCR amplification. It is relatively cheap and easy but introduces sequence biases (e.g., Taq polymerase mutates A/T bases more frequently than C/G) and rarely achieves full coverage of all possible amino acid substitutions [37].
- Oligonucleotide Library Synthesis: This is a more precise and widely used method. Synthetic oligonucleotides containing degenerate codons (e.g., NNK or NNS, where N is any base, K is G/T, and S is G/C) are used to systematically saturate each codon position with all 19 possible amino acid substitutions. This approach reduces bias and provides more uniform coverage, especially when combined with advanced techniques like trinucleotide cassette (T7 Trinuc) mutagenesis, which ensures an equitable distribution of amino acids and avoids stop codons [37] [38].
- CRISPR/Cas9-Mediated Mutagenesis: This method enables the introduction of mutations directly into the genome of the host cell (in situ). Using CRISPR/Cas9 to create double-strand breaks and supplying oligonucleotide donors guides homology-directed repair (HDR) to incorporate specific mutations. This is particularly valuable for studying variants in their native genomic context, accounting for effects of gene dosage, regulation, and splicing that might be absent in plasmid-based systems [38].
High-Throughput Phenotyping (Functional Selection)
The mutant library is subjected to a selective pressure that enriches for functional variants and depletes non-functional ones. The choice of assay depends entirely on the biological question and the protein's function [38] [41].
- Display Technologies: Phage, yeast, or mammalian cell surface display are powerful platforms for selecting variants based on binding affinity to a target antigen or receptor [39].
- Growth-Based Selections: For enzymes or proteins essential for cell survival, competitive growth in a selective medium can directly link protein function to cellular fitness. The DHFR Protein-fragment Complementation Assay (PCA), used in deepPCA, is a prime example where the reconstitution of a essential enzyme upon protein-protein interaction enables cell growth in selective medium, thereby quantifying interaction strength [41].
- Transcriptional Reporters: Variants can be linked to the activation or repression of a reporter gene (e.g., GFP), allowing for fluorescence-activated cell sorting (FACS) to separate populations based on activity.
- In Vitro Selections: For biochemical characterization, non-cell-based systems like in vitro transcription/translation (e.g., the PURE system) can be used to screen for functional variants [38].
Deep Sequencing and Data Analysis
Before and after selection, the mutant library is subjected to high-throughput DNA sequencing. The frequency of each variant in the pre-selection (input) and post-selection (output) pools is quantified. A functional score is then calculated for each variant, typically as the log₂ ratio of its output-to-input frequency. Positive scores indicate enrichment (gain-of-function), while negative scores indicate depletion (loss-of-function) [39] [37]. These raw scores often require normalization and correction for technical artifacts and non-linearities inherent to the assay system [41].
Quantitative Profiling of Protein Function and Stability
DMS generates vast quantitative datasets that reveal how mutations impact specific protein functions. The following table summarizes key quantitative findings from a landmark DMS study on Plasminogen Activator Inhibitor-1 (PAI-1), a protein involved in fibrinolysis and a model system for studying serpin latency [39].
Table 1: Quantitative Effects of Missense Mutations on PAI-1 Function and Stability from a Deep Mutational Scan [39]
| Category of Mutational Effect | Number of Single Amino Acid Substitutions | Functional Half-Life Relative to Wild-Type (t₁/₂ ≈ 2.1h) | Key Functional Interpretation |
|---|---|---|---|
| Stability-Enhancing Mutations | 439 | Increased | Mutations that prolong the active, inhibitory conformation of PAI-1, potentially useful for therapeutic development. |
| Active but Less Stable Mutations | 1,549 | Less than or equal to wild-type | Variants that retain the ability to inhibit the target protease (uPA) but transition to the latent state more rapidly. |
| Non-Functional Mutations | Not specified (depleted at 0h) | Not applicable | Mutations that abrogate inhibitory activity from the outset, likely due to protein misfolding or direct disruption of the active site. |
This data illustrates the power of DMS to systematically classify mutations, revealing that a significant number of mutations (439 out of ~2,000 characterized) can actually enhance functional stability, a finding with potential therapeutic implications. The study further used a massively parallel kinetics method to quantify the functional half-lives for 697 missense variants, providing an exhaustive biophysical resource for this clinically relevant protein [39].
The Scientist's Toolkit: Essential Reagents and Methods
Success in massively parallel genetics relies on a suite of specialized reagents and methodologies. The following table outlines key solutions and their applications in DMS experiments.
Table 2: Research Reagent Solutions for Deep Mutational Scanning
| Research Reagent / Method | Function in DMS/EMPIRIC | Key Considerations and Examples |
|---|---|---|
| Mutagenesis Oligo Pools | To synthesize variant libraries with defined mutations (e.g., NNK codons). | Enables systematic amino acid substitutions. Methods like T7 Trinuc reduce amino acid bias and stop codon frequency [37] [38]. |
| CRISPR/Cas9 System | For in-situ, genome-wide saturation mutagenesis. | Allows for functional screening in a native genomic and transcriptional context, revealing variant effects under physiological conditions [38]. |
| Display Systems (Phage, Yeast) | To link genotype to phenotype for binding or stability screens. | Phage display was used to screen ~7201 PAI-1 variants for functional stability [39]. Yeast surface display is common for antibody engineering. |
| Protein Complementation Assays (e.g., DHFR-PCA) | To quantitatively measure protein-protein interaction (PPI) strength for thousands of variants. | Used in deepPCA to study determinants of specificity in human bZIP transcription factors by coupling PPI to cell growth [41]. |
| High-Fidelity Polymerase | For accurate amplification of mutant libraries without introducing additional errors. | Critical for maintaining library integrity during preparation and amplification steps. |
| Next-Generation Sequencing (NGS) | To quantify variant abundance before and after selection. | The enabling technology for all DMS studies, providing the deep, quantitative readout of variant frequencies. |
Optimizing Experimental Protocols for Robust Quantification
Technical optimization is critical for generating high-quality, reproducible DMS data. Non-linear effects can distort functional scores and lead to misinterpretation. Key parameters to control include [41]:
- Library Transformation Efficiency: A high multiplicity of infection or transformation can lead to multiple plasmids per cell, causing the cell's phenotype to be dominated by the strongest variant and skewing enrichment calculations for weaker ones. The transformation protocol must be optimized to minimize double transformants.
- Selection Pressure and Harvest Timepoint: The stringency of the selection (e.g., drug concentration in a growth assay) and the duration of the selection must be calibrated to the dynamic range of the assay. Harvesting too early or too late can compress the range of observed functional scores.
- Library Composition and Coverage: The mutant library must have high complexity and be deeply sequenced to ensure that even mildly deleterious variants are statistically robustly represented in the input pool. Inadequate coverage leads to noisy estimates for low-frequency variants.
For a protein-protein interaction study using deepPCA, a recommended optimized protocol is as follows [41]:
- Library Construction: Generate DH- and FR-tagged fusion libraries with random DNA barcodes. Determine the barcode-variant association by sequencing.
- Yeast Transformation: Combine the libraries into a single plasmid and transform into yeast cells using a high-efficiency protocol. Use a low amount of DNA (e.g., 250 ng to 1 µg) to keep the fraction of cells with multiple different plasmids below 5%.
- Competitive Growth Assay: Inoculate transformed cells into selective medium containing methotrexate (MTX). The growth rate is proportional to the concentration of the reconstituted DHFR complex, which depends on the affinity of the PPI.
- Harvesting and Sequencing: Harvest input (pre-selection) and output (post-selection) cultures. Extract plasmids and deep sequence the molecular barcodes.
- Data Analysis: Calculate the growth rate (generations/hour) for each variant pair from the change in barcode frequency. Model the data using appropriate thermodynamic models to account for non-linearities and derive additive effects on binding energy.
Integrating Massively Parallel Data into Complex Disease Research
The data generated by DMS and EMPIRIC are invaluable for tackling the problem of "missing heritability" in complex diseases. This heritability is thought to reside in a vast number of variants, each with small effects, rare variants, and, crucially, in non-additive (epistatic) interactions that are invisible to standard genome-wide association studies (GWAS) [35] [36].
- Informing Disease Models: DMS data provides a functional annotation for variants of unknown significance (VUS) found in patient sequencing studies. For example, a DMS of PAI-1 creates a database for interpreting human genetic variants associated with bleeding diathesis or thrombotic risk [39].
- Guiding Predictive Models: New machine learning approaches, such as the DiseaseCapsule framework, leverage whole-genome sequence data and are designed to capture non-additive, omnigenic interactions. In one study, DiseaseCapsule achieved 86.9% accuracy in predicting ALS, outperforming linear models by leveraging non-linear interactions across the genome [36]. This demonstrates how functional insights can be scaled to complex, polygenic diseases.
- Multi-Omics Integration: For small sample sizes, methods that integrate genotype with intermediate molecular phenotypes like gene expression (eQTLs) are being developed. These approaches use biological networks (e.g., protein-protein interaction networks) to cluster genes and SNPs, improving the power to link genetic loci to disease phenotypes even with limited patient data [42].
The logical flow from variant discovery to disease mechanism is summarized below.
The fundamental challenge in modern genetics lies in bridging the knowledge gap between genetic makeup (genotype) and observable traits (phenotype) for complex diseases. Unlike single-gene disorders, conditions such as diabetes, cancer, and asthma are influenced by intricate networks of multiple genes working in concert [18]. The relationship between genotype and phenotype remains an outstanding question for organism-level traits specifically because these traits are complex, determined by combinations of multiple genes leading to an explosion of possible genotype-phenotype mappings [43]. The primary techniques to resolve these mappings, such as genome-wide association studies (GWAS), attempt to find individual genes linked to a trait but lack the statistical power to detect the collective effects of gene groups [18]. This limitation is particularly problematic given that the Human Genome Project revealed humans have only about six times as many genes as a single-cell bacterium, yet exhibit vastly greater sophistication - a discrepancy that highlights the prevalence and importance of multigenic relationships in giving rise to complex life [18].
TWAVE: A Generative AI Framework for Multigenic Analysis
Core Architecture and Methodology
The Transcriptome-Wide conditional Variational auto-Encoder (TWAVE) represents a sophisticated computational approach that combines machine learning with optimization frameworks to identify gene combinations underlying complex illnesses [18] [43]. TWAVE employs a generative artificial intelligence model that amplifies limited gene expression data, enabling researchers to resolve patterns of gene activity that cause complex traits [18]. Unlike methods that examine DNA sequences, TWAVE focuses on gene expression data, which provides dynamic snapshots of cellular activity and indirectly accounts for environmental factors that can turn genes "up" or "down" to perform various functions [18].
The methodology involves several innovative components:
- A variational autoencoder trained on human transcriptional data endowed with causal information [43]
- An optimization framework that pinpoints specific gene changes most likely to shift a cell's state from healthy to diseased or vice versa [18]
- Dimensional reduction through identification of independently varying generalized pathways (eigengenes) [43]
- Constrained optimization to find causal gene sets whose measured transcriptomic responses best explain trait phenotype differences [43]
Key Technical Differentiators
TWAVE fundamentally differs from traditional approaches in several critical aspects. Whereas genome-wide association studies lack causal inference and statistical power for multigenic effects, TWAVE leverages generative AI to emulate both diseased and healthy states, enabling matching of gene expression changes with phenotype alterations [18] [43]. The model identifies groups of genes that collectively cause complex traits to emerge rather than examining effects of individual genes in isolation [18]. Furthermore, TWAVE utilizes gene expression data rather than genetic sequences, which bypasses patient privacy issues associated with DNA sequences while capturing the dynamic interplay between genetic predispositions and environmental influences [18].
Experimental Framework and Validation Protocols
Data Acquisition and Preprocessing
The experimental implementation of TWAVE requires specific data inputs and preprocessing steps to ensure robust identification of causal gene sets:
Data Sources: TWAVE is trained on gene expression data from clinical trials, which provides confirmed expression profiles for both healthy and diseased states [18]. For a smaller subset of genes, experimental data indicating network responses when genes are turned on or off is essential for matching with expression data to find disease-implicated genes [18].
Expression Profiling: The model requires transcriptome-wide expression data that captures the dynamic activity patterns across the genome. This data implicitly accounts for environmental factors that influence gene expression without altering underlying DNA sequences [18].
Validation Framework: TWAVE's effectiveness has been demonstrated across several complex diseases, where it successfully identified causal genes - including some missed by existing methods [18]. The validation involves comparing TWAVE's predictions against known genetic associations and experimental results to verify both accuracy and novel insights.
Workflow Implementation
The following diagram illustrates the core TWAVE analytical workflow:
Table 1: Essential Research Reagents and Computational Tools for TWAVE Implementation
| Resource Category | Specific Examples | Function/Purpose |
|---|---|---|
| Gene Expression Data | Clinical trial datasets, Transcriptomic repositories | Training and validation data for the AI model |
| Computational Framework | Variational Autoencoder architecture, Optimization algorithms | Core AI infrastructure for pattern recognition and causal inference |
| Validation Resources | Experimental gene perturbation data, Known genetic associations | Benchmarking and verification of TWAVE predictions |
| Bioinformatics Tools | BOLT-LMM (for GWAS comparisons), LDSC regression analysis | Complementary analysis for genetic correlation studies [44] |
Key Findings and Quantitative Results
Enhanced Detection of Causal Genes
TWAVE has demonstrated significant advantages in identifying causal genes for complex traits compared to traditional methods. The approach identifies causal genes that cannot be detected by primary existing techniques such as genome-wide association studies [43]. This enhanced detection capability stems from TWAVE's ability to recognize the collective influence of gene groups rather than focusing on individual gene effects, thereby addressing a fundamental limitation of conventional approaches.
A critical finding from TWAVE implementation is the revelation that different sets of genes can cause the same complex disease in different people [18]. This discovery suggests that many complex diseases are not only polygenic but also exhibit distinct subtypes driven by different genotype-phenotype mappings [43]. This heterogeneity has profound implications for personalized medicine, as it indicates that effective treatments may need to be tailored to a patient's specific genetic drivers of disease rather than applying uniform therapeutic strategies across all cases.
Quantitative Performance Metrics
Table 2: Comparative Performance of TWAVE Versus Traditional Genetic Analysis Methods
| Analysis Metric | Traditional GWAS | TWAVE Framework | Implications |
|---|---|---|---|
| Multigenic Detection | Limited statistical power for gene combinations | Enhanced identification of collective gene effects | Reveals polygenic architecture of complex traits |
| Causal Inference | Identifies associations without established causality | Provides causal inference through optimization framework | Enables targeted therapeutic development |
| Disease Subtyping | Limited resolution for phenotypic subtypes | Identifies distinct genetic subtypes of same disease | Supports personalized treatment approaches |
| Environmental Integration | Minimal accounting for environmental factors | Indirectly accounts for environmental influences via expression data | More comprehensive disease modeling |
Implications for Drug Development and Therapeutic Strategies
The identification of causal gene sets through TWAVE opens new avenues for therapeutic intervention in complex diseases. Rather than targeting single genes or gene products, the approach enables the design of multi-target therapies that address the collective genetic drivers of disease [18]. This multi-target strategy may prove particularly effective for complex conditions that emerge from network disturbances rather than isolated genetic defects.
Furthermore, TWAVE's ability to identify different genetic subtypes for the same disease phenotype suggests that pharmaceutical development could benefit from more precise patient stratification in clinical trials [18]. By grouping patients according to their underlying genetic drivers rather than phenotypic presentation alone, drug developers may achieve better clinical outcomes and identify more responsive patient populations.
The generative nature of the TWAVE model also facilitates tailored experimental design by identifying the most promising multigenic targets for further laboratory investigation [43]. This capability helps prioritize research efforts and resources toward gene combinations with the highest likelihood of therapeutic relevance, potentially accelerating the drug discovery process for complex diseases that have proven resistant to conventional single-target approaches.
Future Directions and Methodological Advancements
The TWAVE framework represents a significant advancement in resolving the genotype-phenotype relationship for complex traits, but several promising directions for further development remain. Future iterations could integrate additional data types beyond gene expression, such as epigenetic modifications and protein interaction networks, to create more comprehensive models of biological complexity. Additionally, as single-cell technologies advance, applying TWAVE to single-cell expression data could reveal cell-type-specific multigenic effects that are obscured in bulk tissue analyses.
Another promising direction involves the incorporation of longitudinal data to model how multigenic effects evolve over time and in response to therapeutic interventions. This temporal dimension could prove particularly valuable for understanding progressive complex diseases and designing staged treatment approaches that address different genetic drivers at different disease stages.
As TWAVE and similar approaches mature, they may eventually enable not just identification of causal gene sets but also predictive modeling of intervention outcomes - allowing researchers to simulate how targeted therapies would affect the broader gene network and ultimately modify disease phenotypes. This capability would represent a significant step toward truly predictive and personalized medicine for complex diseases.
Rare diseases collectively affect an estimated 300-400 million people worldwide, yet each individual condition may impact as few as 1 in 2,000 individuals or fewer [30] [45]. This low prevalence creates a fundamental challenge for traditional diagnostic approaches: most frontline clinicians lack direct experience with these conditions, and the heterogeneity of clinical presentations means that approximately 70% of individuals seeking a diagnosis remain undiagnosed [30] [46] [47]. The diagnostic odyssey for these patients often involves years of specialty referrals, expensive clinical workups, and unnecessary medical procedures, potentially leading to irreversible disease progression if critical intervention windows are missed [30].
Linking genotype to phenotype represents one of the most significant challenges in modern genetics research [48] [49]. While deep learning has revolutionized diagnostic accuracy for common diseases, its success has been contingent on accessing large, labeled datasets with thousands of diagnosed patients per condition—a requirement that is mathematically impossible to meet for rare diseases [30] [50]. This data scarcity problem has necessitated innovative computational approaches that can extrapolate beyond the training distribution to novel genetic conditions and atypical disease presentations.
SHEPHERD (ScHEma for PHEnotype-driven Rare Disease Diagnosis) represents a breakthrough in this domain, demonstrating how knowledge-grounded deep learning can overcome the data limitations inherent to rare disease research [30] [50] [47]. By leveraging structured biomedical knowledge and simulated patient data, SHEPHERD performs multi-faceted diagnosis even for conditions with only a handful of known cases, providing researchers and clinicians with powerful tools for causal gene discovery, patient similarity matching, and novel disease characterization.
Knowledge Graph Foundations for Rare Disease Diagnosis
The Role of Biomedical Knowledge Graphs
Biomedical knowledge graphs serve as the foundational framework for encoding relationships between phenotypes, genes, and diseases in computational rare disease diagnosis. These graphs structure biological entities as nodes (e.g., phenotypes, genes, diseases) and their relationships as edges (e.g., "gene-causes-disease," "phenotype-manifests-in-disease") [30] [45]. The semantic structure provided by ontologies like the Human Phenotype Ontology (HPO), which contains over 15,000 terms describing phenotypic abnormalities, enables computational methods to reason across the complex hierarchy of clinical features and their genetic underpinnings [30] [51].
RDBridge represents one of the most comprehensive rare disease knowledge graphs to date, incorporating 11,704 rare diseases (4,145 matched to OMIM), 3,153 disease-gene relationships, 15,349 gene-compound relationships, and 3,791 disease-pathway relationships mined from biomedical literature using advanced natural language processing techniques [45]. This structured knowledge enables researchers to explore complex genotype-phenotype relationships that would otherwise remain trapped within unstructured text.
Knowledge Graph Sparsification Techniques
Recent advances in knowledge graph sparsification have addressed computational challenges associated with large-scale biomedical graphs. Techniques implemented in models like RareNet leverage subgraph extraction to focus computational resources on the most relevant portions of the knowledge graph for a given patient's phenotypic profile [52]. This approach not only improves computational efficiency but also enhances model interpretability by producing focused patient subgraphs for targeted clinical investigation [52].
Table 1: Key Components of Rare Disease Knowledge Graphs
| Component | Description | Data Sources | Scale in RDBridge |
|---|---|---|---|
| Diseases | Rare genetic conditions with standardized identifiers | OMIM, Orphanet | 11,704 diseases (4,145 OMIM-matched) |
| Phenotypes | Standardized clinical observations | HPO | 15,000+ terms in HPO |
| Genes | Protein-coding genes associated with diseases | Ensembl, NCBI Gene | 3,153 disease-gene relationships |
| Compounds | Potential therapeutic agents | DrugBank, ChEMBL | 15,349 gene-compound relationships |
| Pathways | Biological pathways implicated in disease mechanisms | WikiPathways, ConsensusPathDB | 3,791 disease-pathway relationships |
| Literature | Scientific publications supporting relationships | PubMed, PMC | 235,631 publications |
| Medical Images | Visual evidence of disease manifestations | ROCO dataset | 90,249 medical images |
The SHEPHERD Architecture and Methodology
SHEPHERD employs a few-shot learning approach that combines knowledge-guided metric learning with adaptive patient simulation to overcome the data scarcity problem in rare disease diagnosis [30] [50] [47]. The system is designed to operate at multiple points throughout the diagnostic process: (1) after clinical workup to find similar patients, (2) after sequencing analysis to identify strong candidate genes, and (3) after case review to prioritize candidate genes and characterize novel disease presentations [53].
The core innovation of SHEPHERD lies in its ability to project patient phenotypic profiles into an embedding space whose geometry is optimized by broader knowledge of phenotype-gene-disease relationships [47]. When a new patient is presented, SHEPHERD positions them in this latent space such that they are proximate to their most promising causal genes and diseases, as well as other patients with the same genetic conditions, while being distant from irrelevant genes and diseases [30] [47].
Diagram 1: SHEPHERD Architecture Overview (Max Width: 760px)
Knowledge-Guided Metric Learning
SHEPHERD's embedding space is constructed through knowledge-guided metric learning, a deep learning paradigm specifically designed for diagnostic scenarios with extremely scarce labeled data [47]. The model is trained to minimize the distance between patients and their causal genes/diseases in the embedding space while maximizing the distance to unrelated entities [30]. This approach allows SHEPHERD to nominate candidate genes and diseases for patients even when no other patients are known to be diagnosed with the same condition—a common scenario in rare disease diagnosis where 79% of genes and 83% of diseases may be represented in only a single patient [30].
The training process incorporates multi-faceted objective functions that simultaneously optimize for causal gene discovery, patient similarity matching, and disease characterization. This multi-task approach ensures that the learned representations capture clinically meaningful relationships that generalize across different diagnostic scenarios [30] [53].
Adaptive Patient Simulation
To address the critical data scarcity problem, SHEPHERD employs an adaptive simulation approach that generates realistic rare disease patients with varying numbers of phenotype terms and candidate genes [30]. These simulated patients are created using the rich associations in the rare disease knowledge graph, ensuring that the generated profiles reflect biologically plausible genotype-phenotype relationships.
The simulation process accounts for the heterogeneity of clinical presentations by introducing variability in the number and specificity of HPO terms, mirroring the real-world challenge that patients with the same disease may share only 67% of phenotype terms on average [30]. This training on simulated data enables SHEPHERD to learn robust phenotypic patterns that transfer effectively to real-world patients, as demonstrated in evaluations across multiple independent cohorts [30] [50].
Experimental Framework and Evaluation Protocols
Datasets and Patient Cohorts
SHEPHERD was rigorously evaluated on three real-world patient cohorts representing diverse diagnostic scenarios and clinical settings:
Undiagnosed Diseases Network (UDN): 465 patients with molecular diagnoses representing 299 unique diseases, 378 unique genes, with 79% of genes and 83% of diseases represented in only a single patient [30]. Each patient was characterized by an average of 23.9 HPO terms (SD = 16.1) and candidate gene lists at two different stages of the diagnostic pipeline: VARIANT-FILTERED (244.3 genes on average) and EXPERT-CURATED (13.3 genes on average) [30].
MyGene2: 146 patients from a nationwide patient-centered platform for sharing genetic and phenotypic data [30] [50].
Deciphering Developmental Disorders (DDD) study: 1,431 patients from a large-scale investigation of developmental disorders [30] [50].
The UDN cohort underwent particularly extensive validation, with patients receiving thorough clinical workups, whole genome or exome sequencing, and iterative analysis by clinicians and genetic counselors to identify causal genes [30]. This comprehensive diagnostic process established high-quality ground truth for evaluating SHEPHERD's performance.
Evaluation Metrics and Experimental Protocol
SHEPHERD's performance was assessed using multiple quantitative metrics tailored to different diagnostic facets:
- Causal Gene Discovery: Measured by the rank position of the true causal gene in candidate lists, with success rates calculated for top-1, top-5, and top-10 predictions [30].
- Patient Similarity Matching: Evaluated using adjusted mutual information (AMI) to quantify how well patient embeddings capture clinically meaningful similarity [30].
- Novel Disease Characterization: Assessed through qualitative analysis of how well the model could provide interpretable characterizations for previously undescribed disease presentations [30].
The experimental protocol involved training SHEPHERD exclusively on simulated patients and then evaluating its performance on the held-out real-world cohorts, ensuring that the model's ability to generalize to novel conditions could be properly assessed [30] [53].
Table 2: SHEPHERD Performance Across Diagnostic Tasks
| Diagnostic Task | Evaluation Cohort | Performance Metric | Result | Comparative Advantage |
|---|---|---|---|---|
| Causal Gene Discovery | UDN (VARIANT-FILTERED) | Top-1 Accuracy | 40% | 2x improvement over non-guided baseline |
| Causal Gene Discovery | UDN (EXPERT-CURATED) | Mean Rank | 3.56 | Sustained performance on challenging candidates |
| Patients-Like-Me Retrieval | UDN + MyGene2 | Adjusted Mutual Information | 0.304 | Meaningful patient similarity capture |
| Novel Disease Diagnosis | UDN Atypical Presentations | Top-5 Accuracy | 77.8% | Effective for hard-to-diagnose cases |
| Cross-Site Generalization | UDN (12 clinical sites) | Performance Variation | Minimal | Consistent across healthcare settings |
Implementation and Training Details
SHEPHERD was implemented in PyTorch and PyTorch Geometric, with complete code available in a GitHub repository to ensure reproducibility [53]. The model leverages a graph neural network architecture that operates directly on the rare disease knowledge graph, learning to propagate information across related entities to generate informative patient representations [53].
Training followed a two-stage process: (1) pretraining on the rare disease knowledge graph to learn generalizable representations of phenotypes, genes, and diseases, and (2) fine-tuning on simulated patient data for specific diagnostic tasks [53]. This approach ensured that the model could leverage both the structured knowledge in the graph and the phenotypic patterns in the simulated patients.
Key hyperparameters included embedding dimensions of 256 for entities in the knowledge graph, a learning rate of 0.001 with Adam optimizer, and batch sizes tailored to the specific diagnostic task (causal gene discovery, patient similarity matching, or disease characterization) [53].
Comparative Analysis with Alternative Approaches
Performance Relative to Traditional Methods
When compared to traditional rare disease diagnostic tools, SHEPHERD demonstrates significant advantages, particularly in scenarios with limited patient data. In the UDN cohort, SHEPHERD achieved a top-1 accuracy of 40% for causal gene discovery, representing at least a twofold improvement over non-guided baselines [30]. The model maintained strong performance even for the more challenging EXPERT-CURATED gene lists, where it ranked the causal gene at position 3.56 on average [30] [50].
Notably, SHEPHERD excelled at diagnosing patients with novel genetic conditions, ranking up to 86% of these patients as well as or better than domain-specific approaches [30]. This capability is particularly valuable for the estimated 50% of Mendelian conditions whose genetic basis remains unknown [30].
Comparison with Contemporary Deep Learning Approaches
SHEPHERD represents a significant departure from both traditional phenotype-driven tools and contemporary deep learning approaches. Unlike methods that rely solely on the hierarchical structure of the HPO for semantic similarity, SHEPHERD learns phenotypic relationships directly from the knowledge graph, capturing more nuanced clinical patterns [30] [51].
Compared to other deep learning frameworks like PhenoDP, which focuses on disease ranking and symptom recommendation, SHEPHERD provides a more comprehensive diagnostic suite that includes causal gene discovery, patient similarity matching, and novel disease characterization [51]. While PhenoDP demonstrates strengths in generating clinical summaries and recommending additional HPO terms for differential diagnosis, SHEPHERD offers broader functionality across the diagnostic pipeline [51].
Diagram 2: SHEPHERD Diagnostic Workflow Integration (Max Width: 760px)
Table 3: Key Research Reagents and Computational Resources for Rare Disease Diagnosis
| Resource | Type | Function in Research | Access Information |
|---|---|---|---|
| Human Phenotype Ontology (HPO) | Biomedical Ontology | Standardized vocabulary for phenotypic abnormalities; enables computational reasoning across clinical features | https://hpo.jax.org/ |
| SHEPHERD Implementation | Software Tool | Multi-faceted rare disease diagnosis using knowledge-graph neural networks | https://github.com/mims-harvard/SHEPHERD |
| RDBridge Knowledge Graph | Data Resource | Comprehensive rare disease knowledge graph with diseases, genes, compounds, and pathways | http://rdb.lifesynther.com/ |
| Undiagnosed Diseases Network Data | Patient Cohort | Clinically curated dataset of rare disease patients with molecular diagnoses | dbGaP accession phs001232 |
| PhenoDP Toolkit | Software Tool | Deep learning-based phenotype summarization, disease ranking, and symptom recommendation | https://github.com/TianLab-Bioinfo/PhenoDP |
| MyGene2 Platform | Data Resource | Patient-centered portal for sharing phenotypic and genetic data | https://www.mygene2.org/ |
| DECIPHER Database | Data Resource | Platform for sharing genotypic and phenotypic data on developmental disorders | https://deciphergenomics.org/ |
Implications for Genotype-Phenotype Mapping in Complex Disease Research
The approaches pioneered by SHEPHERD have significant implications for the broader challenge of mapping genotypes to phenotypes, particularly for complex diseases with multifactorial etiology. By demonstrating that knowledge-grounded deep learning can effectively bridge the genotype-phenotype gap even in extremely low-data environments, SHEPHERD provides a template for future research in complex disease genetics [30] [47].
The methodology of leveraging structured biomedical knowledge to guide neural network training addresses a fundamental limitation of purely data-driven approaches: their requirement for large, labeled datasets [30]. This hybrid paradigm, combining the reasoning capabilities of symbolic AI with the pattern recognition strengths of neural networks, offers a promising path forward for understanding the complex interplay between genetic variation and clinical presentation across the disease spectrum [30] [48].
Furthermore, SHEPHERD's ability to characterize novel disease presentations by relating them to known conditions through the embedding space provides clinicians with valuable starting points for investigating previously undescribed genetic disorders [30] [47]. This functionality not only accelerates diagnosis for individual patients but also contributes to the collective understanding of rare disease mechanisms by identifying potentially related conditions that may share underlying biological pathways.
As rare disease research continues to evolve, knowledge-graph neural networks like SHEPHERD will play an increasingly important role in unraveling the complex relationships between genetic variation and clinical presentation, ultimately shortening the diagnostic odyssey for millions of patients worldwide and paving the way for targeted therapeutic interventions.
The fundamental challenge in treating complex human diseases often lies in the intricate and often obscured pathway from a patient's genetic makeup (genotype) to their observable clinical characteristics (phenotype). Untangling this complex interplay is crucial for the effective characterization and subtyping of diseases [54]. For decades, drug development has been hampered by tumor heterogeneity and a limited availability of well-defined drug targets, particularly in complex diseases like cancer [55]. Current approaches, whether target-based or phenotype-based, face significant limitations; the former struggles when the best molecular targets are unknown, while the latter often relies on gene expression data that is rarely available in real-world clinical settings and is susceptible to technical biases [55].
Generative artificial intelligence (AI) presents a paradigm shift, offering the potential to design novel therapeutic candidates conditioned directly on complex genomic features. This paper examines a groundbreaking approach at the forefront of this shift: the Genotype-to-Drug Diffusion (G2D-Diff) model. G2D-Diff represents a significant advance in AI-guided, personalized drug discovery by leveraging drug response data to generate hit-like small molecule structures tailored to specific cancer genotypes and a desired efficacy condition [55]. This methodology moves beyond simply searching existing compound libraries, instead creating entirely new therapeutic candidates designed from the ground up to match a genetic profile, thereby streamlining the hit identification process and accelerating drug development for challenging cancers.
Background: From Network Medicine to AI-Generated Therapeutics
The Multiplex Network of Human Diseases
Modern systems biology views human diseases not as isolated entities but as interconnected nodes in a vast biological network. Research has shown that diseases can be systematically mapped into a multiplex network consisting of a genotype-based layer and a phenotype-based layer [54]. In this network model, two diseases are linked in the genotype layer if they share a common disease gene, and in the phenotype layer if they share a common symptom. Studies have revealed a highly significant enrichment of coinciding disease-disease interactions across these layers, demonstrating that diseases with common genetic constituents also tend to share symptoms [54]. This network-based understanding provides the foundational rationale for approaches that simultaneously consider genetic and phenotypic information in therapeutic development.
The Drug Repositioning Paradigm
Traditional drug development is a lengthy and costly process, with an average cost of $1.2 billion to bring each new drug to market and only a 10% probability of success [56]. Drug repositioning—identifying new applications for existing drugs—has emerged as a complementary strategy that can save valuable time and money spent on preclinical studies and phase I clinical trials [56]. Computational approaches that integrate genetic, bioinformatic, and drug data have demonstrated that currently available drugs may be repositioned as novel therapeutics for complex diseases. For instance, one study identified 428 candidate genes as novel therapeutic targets for seven complex diseases and 2,130 drugs feasible for repositioning against these predicted targets [56].
Knowledge Graphs in Biomedical Data Integration
The integration of heterogeneous biological data sets is a critical enabling technology for modern drug discovery. Knowledge graphs (KGs) have emerged as a powerful database model based on graph architecture, incorporating information from different entities, their relationships, and associated metadata [57]. Unlike traditional relational databases, KGs facilitate network analysis by enabling the identification of operational modules, measuring element relevance, and deriving insights from previously unknown connections between biological entities. Their flexible structure, fast query retrieval, and intuitive nature make them particularly suited for identifying new protein and/or gene targets and for drug discovery [57].
The G2D-Diff Framework: Architecture and Methodology
The Genotype-to-Drug Diffusion (G2D-Diff) model represents a novel synthesis of multiple AI technologies designed specifically to address the limitations of previous therapeutic discovery approaches.
Model Architecture
G2D-Diff employs a two-component architecture that combines a chemical variational autoencoder (VAE) with a conditional latent diffusion model [55].
Chemical VAE: This component is pre-trained on a large chemical structure dataset of approximately 1.5 million known compounds to learn an efficient latent representation of chemical space. The VAE encodes molecules into latent vectors and decodes them back into Simplified Molecular-Input Line-Entry System (SMILES) format, creating a well-structured molecular latent space that captures essential features of drug-like compounds [55].
Conditional Latent Diffusion Model: This component generates compound latent vectors conditioned on input genotypes and desired drug responses. The model processes genotype and response information through a condition-encoder module, which generates a numerical condition encoding that guides the diffusion process in generating appropriate compound structures [55].
Table 1: Core Components of the G2D-Diff Architecture
| Component | Function | Training Data | Output |
|---|---|---|---|
| Chemical VAE | Learns latent representation of chemical structures | ~1.5 million known compounds | Molecular latent vectors |
| Condition Encoder | Generates numerical encoding from genotype and desired response | Drug response data from cell lines | Condition embedding |
| Latent Diffusion Model | Generates novel compound structures | Conditioned on genotype-response pairs | Novel molecular latent vectors |
Condition Encoder and Contrastive Learning
A key innovation in G2D-Diff is its use of a pre-trained condition encoder based on contrastive learning. Inspired by the CLIP framework, this approach enhances the model's generalizability to unseen genotypes by ensuring the condition encoding captures not only basic information about the genotype and response but also the structural information of condition-matching drugs [55]. This pre-training enables the model to generate distinguishable encodings for different genotype-response conditions, with principal component analysis revealing that the primary axis distinguishes conditions based on response class (sensitive, moderate, resistant), while secondary axes differentiate conditions according to genotype variations [55].
Workflow Visualization
The following diagram illustrates the complete G2D-Diff workflow from genetic input to compound generation:
Diagram 1: G2D-Diff workflow (76 characters)
Experimental Protocol for Model Evaluation
The evaluation of G2D-Diff involves a comprehensive assessment of both its component parts and the integrated system:
Chemical VAE Evaluation Protocol:
- Reconstruction Task: Randomly select 1000 molecules from validation set, encode into latent vectors, then decode to test reconstruction capability.
- Random Generation Task: Generate molecules by decoding 1000 randomly sampled latent vectors from normal distribution.
- Assessment Metrics: Calculate validity, uniqueness, novelty, diversity, and reconstruction success rate.
- Drug-like Properties Evaluation: Compute Quantitative Estimates of Drug-likeness (QED), Synthetic Accessibility Scores (SAS), and calculated logarithm of the partition coefficient (LogP) for generated molecules.
Condition Encoder Evaluation Protocol:
- Principal Component Analysis: Project condition encodings to visualize separation of different genotype-response conditions.
- Similarity-based Retrieval: Identify top 5 and top 10 potential drug candidates by cosine similarity in shared space.
- Odds Ratio Calculation: Compute the odds ratio between the odds of a drug being in the top most similar drugs for a given condition and the odds of a drug having the matching condition in the entire dataset.
Performance and Results
Chemical VAE Performance
The chemical VAE component of G2D-Diff demonstrates proficient capability in generating feasible, drug-like compounds. Comprehensive evaluation shows exceptional performance across standard metrics [55]:
Table 2: Chemical VAE Performance Metrics
| Evaluation Task | Validity | Uniqueness | Novelty | Diversity | Reconstruction Success |
|---|---|---|---|---|---|
| Reconstruction | 1.00 | 1.00 | N/A | N/A | 0.99 |
| Random Generation | 0.86 | 1.00 | 1.00 | 0.89 | N/A |
The evaluation of drug-like properties revealed that a similar percentage of randomly generated molecules fell within acceptable ranges for QED, SAS, and LogP when compared to molecules in the validation set [55].
The condition encoder successfully learns to generate distinguishable condition representations that capture the relationship between genotypes and drug responses. Principal component analysis demonstrates that the encodings separate effectively by both response class and genotype differences [55]. The model shows exceptional performance in identifying condition-matching drugs, with odds ratios consistently above zero across all conditions and particularly high for sensitive conditions [55].
G2D-Diff significantly outperforms existing methods across multiple evaluation metrics, demonstrating exceptional performance in generating diverse, feasible, and condition-matching compounds. The model's attention mechanism provides valuable interpretability by offering insights into potential cancer targets and pathways relevant to the generated compounds [55].
Research Reagent Solutions and Implementation Toolkit
Implementing genotype-to-drug diffusion models requires specialized computational resources and biological data assets. The following table details essential components for establishing this research capability:
Table 3: Research Reagent Solutions for Genotype-to-Drug Modeling
| Resource Category | Specific Examples | Function/Purpose |
|---|---|---|
| Chemical Structure Data | ~1.5 million compound dataset [55] | Training chemical VAEs to learn molecular representations |
| Drug Response Data | GDSC, CTRP, NCI60 [55] | Providing growth response data for conditioning compound generation |
| Gene-Disease Associations | Gentrepid, PharmGKB, DrugBank [56] | Linking genetic markers to disease mechanisms and known drug targets |
| Knowledge Graph Platforms | Custom biomedical KGs [57] | Integrating heterogeneous biological data for target identification |
| Validation Databases | Therapeutic Target Database, PharmGKB [56] | Benchmarking generated compounds against known therapeutic targets |
| Specialized Software | GeneDive application [58] | Visualizing and exploring gene-drug-disease interactions from literature |
Pathway to Therapeutic Application
The application of G2D-Diff in triple-negative breast cancer case studies demonstrates its practical utility, where the model generated plausible hit-like candidates by focusing on relevant pathways [55]. The workflow from genetic analysis to candidate therapeutic can be visualized as follows:
Diagram 2: Therapeutic development pathway (67 characters)
Discussion and Future Directions
The development of G2D-Diff represents a significant milestone in AI-driven therapeutic discovery, but several challenges and opportunities remain. Future work should focus on improving the bioavailability and cell selectivity of generated compounds, as well as addressing the challenge of controlling the number of gene copies transferred in gene therapy applications [59]. Furthermore, disorders involving multiple genes in their underlying pathophysiology present particular challenges for targeted therapy development [59].
The integration of knowledge graphs with generative AI models presents a promising direction for future research. As noted by researchers, "KGs are favored for their flexible structure, fast query retrieval, intuitive nature, and ease of use" [57], which could enhance the biological relevance of generated compounds. Additionally, the application of these approaches beyond oncology to other complex diseases with strong genetic components represents an important expansion area.
In conclusion, genotype-to-drug diffusion models like G2D-Diff offer a powerful framework for addressing the fundamental challenge of connecting genotype to phenotype in therapeutic development. By directly generating targeted chemical entities based on genetic profiles and desired efficacy conditions, these approaches have the potential to significantly accelerate the discovery of personalized therapeutics for complex diseases.
Unraveling the genetic architecture of complex human diseases remains a central challenge in modern biomedical research. These conditions, influenced by hundreds of genetic variants and environmental factors, require the synthesis of vast amounts of data from genome-wide association studies (GWAS), expression quantitative trait loci (eQTL) analyses, and phenotypic databases [60] [61]. The sheer volume and heterogeneity of this data necessitate sophisticated integrative tools that can bridge disparate genomic resources. This technical guide focuses on two pivotal platforms—the Phenotype-Genotype Integrator (PheGenI) and PhenoScanner—designed to empower researchers and drug development professionals in mining associations, prioritizing variants, and generating testable biological hypotheses [62] [63]. Framed within a broader thesis on linking genotype to phenotype, this whitepaper details their functionalities, provides experimental protocols, and illustrates their application in translational research.
Phenotype-Genotype Integrator (PheGenI)
PheGenI is a web-based resource developed by the National Center for Biotechnology Information (NCBI) that merges NHGRI GWAS Catalog data with several NCBI databases [62] [60]. It is a phenotype-oriented resource intended for clinicians and epidemiologists to follow up on GWAS results.
Key Integrated Data Sources:
- GWAS Data: Association records from the NHGRI GWAS Catalog and significant hits from dbGaP study analyses [62] [64].
- Genomic Databases: Direct integration with NCBI Gene, dbSNP, and OMIM.
- Functional Genomics: eQTL data from the GTEx project and planned molecular QTL data (molQTL) [62].
- Study-Level Data: Links to dbGaP studies for authorized access to individual-level data.
Search Capabilities: Users can search by chromosomal location (e.g., 1M-10M), gene symbol/ID, dbSNP rs number, or Medical Subject Headings (MeSH) phenotype terms [62] [65]. Results are presented in annotated, downloadable tables alongside a dynamic genomic viewer.
PhenoScanner
PhenoScanner is a curated database of publicly available results from large-scale genetic association studies, facilitating "phenome scans" [63] [66]. Its primary aim is to cross-reference genetic variants with a vast array of phenotypes to elucidate disease pathways.
Key Features:
- Extensive Curation: Contains over 350 million association results and more than 10 million unique genetic variants, predominantly SNPs [63].
- Proxy Search: Allows querying for trait associations with proxy variants (in linkage disequilibrium) using data from the 1000 Genomes and HapMap projects (European samples) [63].
- Allele Alignment: Presents results with consistent effect and non-effect alleles for user-specified input variants.
The following table summarizes the core quantitative and functional aspects of PheGenI and PhenoScanner, highlighting their complementary strengths for association mining.
Table 1: Comparative Overview of PheGenI and PhenoScanner
| Feature | PheGenI | PhenoScanner |
|---|---|---|
| Primary Purpose | Integrate GWAS findings with deep genomic annotations for hypothesis generation and variant prioritization [62] [60]. | Perform rapid phenome-wide scans of genetic variants to uncover pleiotropy and shared biology [63]. |
| Core Data Sources | NHGRI GWAS Catalog, dbGaP, NCBI Gene, dbSNP, OMIM, GTEx (eQTL) [62] [60]. | Curated results from published large-scale genetic association studies (e.g., GWAS, meta-analyses) [63] [66]. |
| Association Records | Integrates over 66,000 association records from the GWAS Catalog (as of 2014) [60]. | Houses over 350 million association results (as of 2016) [63]. |
| Variant Scope | SNPs from GWAS and dbGaP, linked to genes and functional classes. | Over 10 million unique genetic variants, mostly SNPs [63]. |
| Key Search Modalities | Phenotype (MeSH), Gene, Genomic Location, SNP [62]. | Genetic variant (rsID), with optional proxy search based on LD [63]. |
| Phenotype Ontology | Relies on exact MeSH terms; parent/child terms not currently indexed [62]. | Utilizes trait descriptions from original source studies. |
| Output & Visualization | Annotated tables, dynamic genomic sequence viewer, ideogram, gene expression data [62]. | Tabular association results, linked to source publications. |
| Data Accessibility | Direct links to underlying NCBI resources and dbGaP for controlled-access data application [62]. | Publicly available web tool; provides summary statistics. |
Experimental Protocols for Association Mining
Protocol 1: Deep-Dive Variant Annotation with PheGenI
This protocol is designed to explore all genomic context and functional evidence for a GWAS-identified locus.
Materials: PheGenI web interface (https://www.ncbi.nlm.nih.gov/gap/phegeni), target variant or locus information.
Method:
- Define Search Input.
- Apply Phenotypic Filters (Optional). To narrow results to a specific disease context, enter a MeSH term (e.g., "Celiac Disease") in the phenotype field. Use the "Browse..." button to explore categories [62].
- Set Statistical Thresholds. Optionally limit the P-value for Association Results and eQTL data to a stringent cutoff (e.g.,
< 5e-8) to filter the most significant hits. - Execute Search and Retrieve Data.
- Review the "Association Results" tab for a comprehensive list of phenotype-variant associations from the GWAS Catalog and dbGaP.
- Navigate to the "Genes" tab to see annotated genes within the locus, including official symbols, descriptions, aliases, and OMIM links [65].
- Examine the "SNPs" tab for detailed variant information from dbSNP.
- Analyze the "eQTL Data" tab to identify variants that may regulate gene expression in tissues relevant to your disease of interest [62].
- Visualize and Synthesize. Use the "Genome View" ideogram to visually inspect the genomic region, including the positions of significant SNPs and genes. Download all result tables for offline analysis.
Protocol 2: Phenome-Wide Cross-Referencing with PhenoScanner
This protocol assesses the pleiotropic effects of a candidate variant by examining its associations across thousands of traits.
Materials: PhenoScanner web tool (http://www.phenoscanner.medschl.cam.ac.uk), target variant rsID.
Method:
- Input Target Variant. Enter the dbSNP rs identifier (e.g.,
rs7412) into the query box. Thersprefix is optional. Multiple variants can be entered on separate lines. - Configure Proxy Search (Critical for Fine-Mapping). Enable the option to "Include results for proxy SNPs." This will query the database for associations with variants in high linkage disequilibrium (LD) with your input, using LD structure from the 1000 Genomes EUR population. Set an appropriate r² threshold (e.g.,
0.8). - Set P-value and Ancestry Filters. Apply a significance threshold (e.g.,
P < 1e-5) to manage output volume. Optionally restrict results to specific ancestral populations if required. - Execute Query and Interpret Results. The tool returns a table listing all significant trait associations for the input and/or proxy variants. Key columns include:
- Variant: The associated SNP.
- Trait: The phenotype description from the source study.
- P-value & Beta/OR: The association strength and effect estimate.
- Effect/Non-effect Alleles: Ensures consistent interpretation of the effect direction.
- Downstream Analysis. Results can identify shared genetic influences (pleiotropy) between your target disease and other traits, suggest potential confounding factors, or reveal novel therapeutic hypotheses based on cross-phenotype associations.
Visualization of Integrative Analysis Workflows
The following diagrams, generated using Graphviz DOT language, illustrate the logical workflows for using each tool and their role in an integrated analysis pipeline.
The effective use of PheGenI and PhenoScanner relies on an ecosystem of underlying databases and resources. The table below details key "research reagents" in this digital toolkit.
Table 2: Key Research Reagent Solutions for Genotype-Phenotype Integration
| Resource Name | Type | Primary Function in Analysis | Relevant Tool |
|---|---|---|---|
| NHGRI-EBI GWAS Catalog | Curated Database | Provides a comprehensive, publicly available collection of published GWAS summary statistics, serving as a primary source of variant-trait associations [60]. | PheGenI |
| dbGaP (Database of Genotypes and Phenotypes) | Archival Repository | Archives and distributes individual-level genotype and phenotype data from studies, allowing for deeper replication and meta-analysis. PheGenI links to dbGaP study pages [62] [64]. | PheGenI |
| NCBI Gene & dbSNP | Reference Databases | Provide authoritative gene annotations (locations, functions, aliases) and records for genetic variation, forming the foundational genomic context for associations [62]. | PheGenI |
| GTEx (Genotype-Tissue Expression) Project | Resource | Supplies eQTL data linking genetic variants to gene expression levels across diverse human tissues, crucial for inferring variant function [62]. | PheGenI |
| MeSH (Medical Subject Headings) | Controlled Vocabulary | Provides standardized terminology for diseases and phenotypes, enabling consistent phenotype-based searching in PheGenI [62]. | PheGenI |
| 1000 Genomes Project & HapMap | Reference Panels | Provide genotype data used to calculate linkage disequilibrium (LD) and identify proxy variants for a query SNP, expanding the searchable variant space [63]. | PhenoScanner |
| Phecode Map | Phenotype Classification | Used in large-scale biobank studies (e.g., UK Biobank, FinnGen) to map ICD codes into biologically meaningful phenotype clusters, facilitating disease endpoint harmonization across cohorts [67]. | Supporting Analysis |
Overcoming Translational Challenges: Data Scarcity, Species Differences, and Model Optimization
The mission to link genotype to phenotype represents a central challenge in modern genetics, particularly for complex diseases [42]. This challenge is most acute in the realm of rare genetic diseases, which collectively affect 300-400 million people worldwide yet individually may impact fewer than 50 per 100,000 individuals [30]. The fundamental obstacle is data scarcity: with approximately 7,000 known rare diseases, clinicians have limited experience with any single condition, and the heterogeneity of clinical presentations means that approximately 70% of individuals seeking a diagnosis remain undiagnosed [30]. This diagnostic deficit results in substantial cumulative loss of quality-adjusted life years and disproportionate healthcare system burdens [68].
While deep learning has revolutionized many clinical areas by automatically learning valuable features from patient data, its application to rare diseases has been severely limited by data availability [30]. Traditional deep learning approaches require thousands of diagnosed patients per disease, but rare disease datasets are typically three orders of magnitude smaller [30]. This scarcity creates a critical bottleneck in genotype-to-phenotype mapping, where identifying the genetic underpinnings of a patient's phenotypic presentation becomes exponentially more difficult with fewer data points. Overcoming this limitation requires innovative computational approaches that can extrapolate beyond the training distribution to novel genetic conditions and atypical disease presentations.
The Data Scarcity Landscape in Rare Disease Research
Quantifying the Data Deficit
The data scarcity problem in rare disease research manifests across multiple dimensions, from limited case numbers to phenotypic heterogeneity. Table 1 summarizes key quantitative challenges.
Table 1: Data Scarcity Challenges in Rare Disease Diagnosis
| Challenge Dimension | Statistical Measure | Impact on Diagnosis |
|---|---|---|
| Disease Prevalence | ≤50 per 100,000 individuals [30] | Limited clinical experience per disease |
| Diagnostic Rate | ~70% undiagnosed after initial evaluation [30] | Prolonged diagnostic odyssey for patients |
| Phenotypic Heterogeneity | 67% average phenotype commonality among same-disease patients [30] | Difficulty recognizing disease patterns |
| Molecular Diagnostic Yield | Up to 50% of Mendelian conditions have unknown genes [68] | Incomplete genetic understanding of diseases |
| Data Availability | 79% of genes and 83% of diseases represented in only single patients in cohorts [30] | Insufficient data for traditional deep learning |
The Genotype-Phenotype Mapping Complexity
The genotype-to-phenotype problem is further complicated by biological complexity. Research in model organisms indicates that phenotypic expression often results from complex genetic interactions involving multiple modifiers rather than simple monogenic relationships [69]. This complexity means that identical mutations can produce different phenotypes in different genetic backgrounds, a phenomenon observed even in organisms with highly similar genomes [69]. In humans, this translates to significant phenotypic variability among patients with the same genetic disorder, making pattern recognition and diagnosis particularly challenging.
Innovative Computational Solutions
Few-Shot Learning with Knowledge Graphs
The SHEPHERD approach represents a breakthrough in few-shot learning for rare disease diagnosis [30]. This method performs deep learning over a knowledge graph enriched with rare disease information and is trained primarily on simulated rare disease patients rather than exclusively on real patient data [30]. The framework addresses data scarcity through several innovative mechanisms:
- Knowledge-Guided Deep Learning: By incorporating medical knowledge of known phenotype, gene, and disease associations, SHEPHERD can learn patient representations informed by existing medical knowledge rather than relying solely on labeled examples [30].
- Multi-Faceted Diagnosis: The system operates at multiple points in the diagnostic process to perform causal gene discovery, retrieve "patients-like-me" with similar genetic and phenotypic features, and provide interpretable names for novel disease presentations [30].
- Embedding Space Optimization: When a new patient arrives, SHEPHERD produces a mathematical representation (embedding) of the patient in a latent space such that the patient is embedded near their causal gene(s), disease, and other patients with the same causal gene(s) or disease, while being positioned far from irrelevant genes and diseases [30].
Table 2: SHEPHERD Performance on Real-World Rare Disease Cohorts
| Patient Cohort | Cohort Size | Diagnostic Task | Performance Metric | Result |
|---|---|---|---|---|
| Undiagnosed Diseases Network (UDN) | 465 patients | Causal gene discovery (variant-filtered candidates) | Top-1 accuracy | 40% [30] |
| UDN | 465 patients | Challenging diagnoses (atypical presentations/novel diseases) | Top-5 accuracy | 77.8% [30] |
| UDN | 465 patients | Novel condition diagnosis | Comparison to domain-specific approaches | Up to 86% same or better [30] |
| MyGene2 | 146 patients | Cross-cohort validation | Sustained performance | Comparable to UDN [30] |
Patient Simulation Frameworks
Simulation of undiagnosed patients with novel genetic conditions provides a complementary approach to address data scarcity [68]. These frameworks jointly simulate complex phenotypes and challenging candidate genes to produce realistic patients with novel genetic conditions, creating scalable, publicly shareable datasets for method development and evaluation [68]. Key aspects include:
- Joint Phenotype-Genotype Modeling: Unlike earlier approaches that unrealistically modeled patient genotype and phenotype disjointly, modern simulation frameworks jointly sample genes and phenotypes according to biologically plausible categories to simulate nontrivial and realistic patients [68].
- Modeling Diagnostic Challenges: The simulation incorporates "distractor" genes that do not cause the patient's presenting syndrome yet would be considered plausible candidates during clinical evaluation, reflecting real-world diagnostic dilemmas [68].
- Novel Condition Simulation: By curating a knowledge graph time-stamped to a specific year (e.g., 2015), simulations can define post-date medical genetics discoveries as novel, enabling evaluation of methods on previously unpublished conditions [68].
Validation shows that simulated patients closely resemble real-world patients from the Undiagnosed Diseases Network in terms of candidate gene numbers (13.13 vs. 13.94 on average) and positive phenotype terms (24.08 vs. 21.57 on average), with real-world patients clustering with simulated patients in dimensionality reduction visualization [68].
Experimental Protocols and Methodologies
SHEPHERD Implementation Protocol
Knowledge Graph Construction:
- Data Integration: Assemble a comprehensive knowledge graph incorporating gene-disease associations from OMIM, phenotype-gene associations from HPO, and protein-protein interactions from dedicated databases [30].
- Temporal Segmentation: For novel disease simulation, time-stamp the knowledge graph to a specific year to define novelty relative to subsequent discoveries [68].
- Graph Enrichment: Incorporate additional relationships including pathway information, functional annotations, and tissue-specific expression patterns [30].
Patient Representation Learning:
- Input Processing: Process patient phenotype terms (HPO codes) and optional candidate gene lists through embedding layers [30].
- Graph Neural Network Processing: Propagate information through multiple layers of a graph neural network to capture complex relationships between phenotypes, genes, and diseases [30].
- Contrastive Learning Optimization: Train the model using a contrastive loss function that minimizes distance between patients and their causal genes/diseases while maximizing distance to irrelevant entities [30].
Evaluation Framework:
- Dataset Partitioning: Evaluate on real-world cohorts from Undiagnosed Diseases Network (N=465), MyGene2 (N=146), and Deciphering Developmental Disorders study (N=1431) [30].
- Task-Specific Metrics: Assess performance on causal gene discovery (top-k accuracy), patient similarity (adjusted mutual information), and novel disease characterization [30].
- Comparative Analysis: Compare against traditional variant prioritization tools and phenotype-based methods across different disease areas and clinical sites [30].
Patient Simulation Methodology
Simulation Pipeline:
- Disease Initialization: Initialize each simulated patient with a genetic disorder profiled in the Orphanet database, ensuring biological plausibility [68].
- Phenotype Modeling:
- Apply phenotype dropout to mimic partially observed symptoms
- Implement phenotype obfuscation by replacing specific symptoms with more general terms
- Add unrelated symptoms and comorbidities proportionally to their prevalence in age-matched patients from medical insurance claims databases [68]
- Candidate Gene Generation:
- Include the true causal gene(s) for the condition
- Generate challenging distractor genes from six distinct modules representing different biological and clinical scenarios [68]
- Validation: Compare simulated patients to real patients from the Undiagnosed Diseases Network using similarity metrics and classifier analysis [68].
Visualization of Computational Frameworks
SHEPHERD Architecture and Workflow
SHEPHERD Few-Shot Learning Framework
Patient Simulation Pipeline
Patient Simulation Pipeline
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Rare Disease Computational Research
| Resource Category | Specific Tool/Database | Function in Research | Application Context |
|---|---|---|---|
| Phenotype Ontologies | Human Phenotype Ontology (HPO) [30] | Standardized vocabulary for phenotypic abnormalities | Patient characterization, similarity calculation |
| Disease Databases | Orphanet [68] | Comprehensive rare disease information | Disease modeling, knowledge graph construction |
| Genotype-Phenotype Resources | OMIM [30] | Catalog of human genes and genetic disorders | Establishing gene-disease relationships |
| Biological Networks | Protein-protein interaction networks [42] [70] | Map of molecular interactions | Pathway analysis, network propagation |
| Expression Quantitative Trait Loci | GTEx [42] | Tissue-specific gene regulation data | Understanding genotype-expression relationships |
| Simulation Frameworks | Adaptive patient simulation [30] [68] | Generation of synthetic rare disease patients | Data augmentation, method validation |
| Analysis Platforms | Exomiser [30] | Variant prioritization tool | Candidate gene generation, benchmarking |
| Pathway Simulation | PHENSIM [71] | In silico phenotype simulation | Predicting molecular phenotype effects |
Discussion and Future Directions
The integration of few-shot learning and patient simulation represents a paradigm shift in tackling the genotype-to-phenotype challenge in rare diseases. By leveraging knowledge graphs and simulated patients, these approaches address the fundamental data scarcity problem that has long hindered progress in this field. The demonstrated success of SHEPHERD in real-world clinical cohorts—ranking the correct gene first in 40% of patients and among the top five for 77.8% of challenging cases—provides compelling evidence for the utility of these methods in actual diagnostic settings [30].
Future research directions should focus on several key areas. First, expanding the knowledge graphs to include more diverse data types, such as single-cell expression profiles and spatial transcriptomics, could enhance the biological resolution of these models. Second, developing more sophisticated simulation frameworks that capture longitudinal disease progression and treatment responses would create additional value for both diagnostic and therapeutic applications. Third, improving model interpretability through attention mechanisms and explainable AI techniques will be crucial for clinical adoption, as healthcare providers require understandable rationale for diagnostic decisions.
These computational advances in linking genotype to phenotype in data-scarce environments have implications beyond rare diseases. The same fundamental challenges appear in cancer subtypes, complex disease endotypes, and other areas of precision medicine where patient populations are small and heterogeneous. The methodologies developed for rare diseases may therefore provide a template for addressing data scarcity across multiple clinical domains, accelerating the era of personalized medicine for all patients regardless of disease prevalence.
The pursuit of understanding how genetic information manifests as observable traits—the genotype to phenotype relationship—represents a fundamental challenge in biomedical science. This challenge is particularly acute in complex disease research and drug development, where biological differences between model organisms and humans create a significant translational gap. This gap manifests starkly in drug development statistics, where approximately 90% of drug candidates fail during clinical development, often due to unexpected toxicity or lack of efficacy in humans despite promising preclinical results [72]. Such failures frequently originate from an underappreciation of the fundamental Genotype-Phenotype Differences (GPD) between the model systems used in discovery research and human patients [73] [74].
Bridging this translational gap requires a sophisticated understanding that genotype-phenotype relationships are not simple one-to-one mappings. As research in model organisms like yeast has demonstrated, identical mutations can produce different phenotypic outcomes in different genetic backgrounds due to complex interactions with multiple modifier genes [69]. This complexity is magnified when translating findings from preclinical models to humans. This whitepaper examines the sources of GPD, outlines novel methodologies for its quantification, and presents practical strategies for integrating this understanding into complex disease research and therapeutic development.
Defining Genotype-Phenotype Differences (GPD) in Translational Research
Genotype-Phenotype Differences (GPD) refer to the disparities in phenotypic expression of similar genotypes across different species, strains, or populations. In the context of translational research, GPD specifically captures the biological differences that cause a drug target or pathway to function differently in humans compared to preclinical models [73] [74].
The core concepts are defined as follows:
- Genotype: The complete set of genes carried by an organism, representing its unique DNA sequence [75].
- Phenotype: All observable characteristics of an organism, resulting from the expression of its genotype combined with environmental influences [75].
- GPD: The systematic variation in how similar genotypes produce different phenotypes across biological contexts, particularly between preclinical models and humans.
The Complexity of Genotype-Phenotype Mapping in Complex Diseases
Most diseases of contemporary interest, including Alzheimer's, Parkinson's, autoimmune disorders, and many cancers, are complex diseases [76]. Unlike single-gene disorders, these conditions arise from intricate combinations of multiple genetic factors, environmental exposures, and lifestyle influences that do not follow simple Mendelian inheritance patterns [76]. This complexity means that identifying causal genetic factors requires sophisticated approaches that can disentangle these interacting influences.
Research in model systems has revealed that conditional essentiality—where genes are essential in one genetic background but not another—is typically governed by complex genetic interactions involving multiple modifiers rather than simple one-to-one gene interactions [69]. This has direct implications for translational research, as it suggests that therapeutic targets identified in model systems may have different functional consequences in humans due to differences in genetic background.
Quantifying GPD: Key Biological Dimensions and Methodologies
A robust framework for assessing GPD across three fundamental biological contexts enables researchers to systematically evaluate potential translatability challenges early in the drug discovery process.
Table 1: Key Dimensions for Assessing Genotype-Phenotype Differences
| Biological Context | Measurement Approach | Translational Implication |
|---|---|---|
| Gene Essentiality | CRISPR-based knockout screens to determine perturbation impact on cellular survival [73] | Genes essential in model systems but not in humans (or vice versa) may produce misleading therapeutic validation |
| Tissue Expression Profiles | RNA sequencing and spatial transcriptomics to quantify expression patterns across tissues [77] [73] | Differential expression patterns can lead to unexpected on-target toxicity in human tissues not observed in models |
| Network Connectivity | Protein-protein interaction mapping and pathway analysis to define molecular context [73] | Differences in network position and interaction partners can alter pharmacological manipulation effects |
Experimental Protocols for GPD Assessment
Protocol for Assessing Gene Essentiality Differences
Objective: Quantify differences in gene essentiality between human cell lines and preclinical models for target validation.
Methodology:
- Perform parallel CRISPR-Cas9 screens in human cell lines (e.g., iPSCs) and corresponding model organism cells (e.g., mouse embryonic fibroblasts)
- Design single-guide RNA (sgRNA) libraries targeting orthologous genes across species
- Transduce cells with lentiviral sgRNA libraries at low MOI to ensure single integration
- Harvest cells at multiple time points to monitor fitness effects
- Sequence genomic DNA and quantify sgRNA abundance changes using MAGeCK algorithm
- Calculate essentiality scores based on sgRNA depletion rates
- Identify divergent essentiality using statistical methods that account for basal fitness differences
Key Reagents: Cas9-expressing cell lines, lentiviral sgRNA libraries, next-generation sequencing reagents, cell culture media optimized for each model system.
Protocol for Tissue Expression Profile Comparison
Objective: Systematically identify differences in gene expression patterns across tissues and cell types.
Methodology:
- Obtain single-cell RNA sequencing data from relevant tissues across species from resources like the Human Cell Atlas [77]
- Process data using standardized pipelines (Cell Ranger) for uniform alignment and quantification
- Perform cross-species integration using tools like SCENIC to identify conserved and divergent cell types
- Calculate cell-type-specific expression scores for target genes
- Validate findings using spatial transcriptomics on tissue sections
- Perform differential expression analysis to quantify species-specific expression patterns
Key Reagents: Single-cell suspension reagents, single-cell sequencing kits, spatial transcriptomics slides, cross-species antibody panels for validation.
Computational Approaches: Bridging the GPD Gap with Artificial Intelligence
Machine learning frameworks that explicitly incorporate GPD features offer a promising approach to improve the predictability of translational research.
GPD-Enhanced Toxicity Prediction Framework
A novel AI framework incorporating GPD features has demonstrated significantly improved prediction of human drug toxicity compared to conventional chemical structure-based models [73] [74]. The framework development process follows this workflow:
This computational approach extracts GPD features from three biological contexts outlined in Table 1 and integrates them with chemical descriptor data using a Random Forest algorithm. When validated using 434 risky drugs and 790 approved drugs, the GPD-enhanced model demonstrated substantially improved predictive accuracy compared to chemical-only approaches [73]:
Table 2: Performance Comparison of Toxicity Prediction Models
| Model Type | AUPRC | AUROC | Key Strengths |
|---|---|---|---|
| Chemical Structure-Based (Baseline) | 0.35 | 0.50 | Standard approach, requires only compound structure |
| GPD-Enhanced Model | 0.63 | 0.75 | Captures biological context differences, significantly better prediction of neurotoxicity and cardiovascular toxicity |
The model demonstrated practical utility in chronological validation, correctly predicting 95% of drugs that would be withdrawn from the market post-1991 when trained only on pre-1991 data [74]. This demonstrates its potential for anticipating future clinical failures based on GPD assessment.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing GPD-aware research requires specialized reagents and tools designed specifically for cross-species comparative analysis.
Table 3: Essential Research Reagents for GPD Studies
| Reagent/Tool | Function | Application in GPD Research |
|---|---|---|
| Cross-reactive Antibodies | Immunodetection of orthologous proteins | Quantifying protein expression and localization differences across species |
| CRISPR-Cas9 Systems | Gene editing in multiple model systems | Performing parallel functional genomic screens to assess gene essentiality differences |
| Species-Specific Primers/Probes | Quantitative PCR and molecular detection | Accurate measurement of gene expression across species with high sequence specificity |
| Lipid Nanoparticles (LNPs) | Nucleic acid delivery | Testing therapeutic modalities across biological systems with different cellular uptake mechanisms [77] |
| Organoid Culture Systems | 3D tissue modeling | Creating human and model organism-derived tissue models for parallel drug testing [77] |
| Single-Cell RNA-seq Kits | Gene expression profiling at single-cell resolution | Identifying conserved and divergent cell types and states across species [77] |
Advanced Statistical Methods for Causal Inference in Complex Diseases
Overcoming environmental confounding in genotype-phenotype studies requires specialized statistical approaches. The Phenotype Differences Model offers a novel solution for detecting causal genetic effects while addressing dynastic genetic effects and population stratification [78].
The model regresses the phenotypic difference between siblings ((y{1j} - y{2j})) on the genotype of one sibling, adjusted for the expected genetic difference:
[ y{1j} - y{2j} = \alpha + \beta{PD}(g{1j}(1-\rho)) + \varepsilon_{1j} ]
Where ( \rho ) represents the genetic correlation between siblings. This approach provides consistent estimates of genetic effects using just a single individual's genotype, dramatically increasing analytical power and sample representativeness compared to traditional sibling pair methods [78].
Application of this model to lifespan data has identified that polygenic indices for body mass index, self-rated health, and chronic obstructive pulmonary disease have statistically significant causal effects on mortality risk [78]. This illustrates how advanced statistical methods can extract causal insights from complex genotype-phenotype relationships in human populations.
Implementing GPD-Aware Research Strategies: A Practical Framework
Organizational Strategies for Effective Translational Research
Bridging the translational gap requires not only technical solutions but also organizational approaches that facilitate collaboration between basic and clinical researchers:
- Maintain Strong, Open Communication: Establish clear protocols for decision-making, authorship, and data sharing between clinical and basic science team members [79].
- Structured Team Building: Implement separate but overlapping weekly meetings for clinical and laboratory teams, with joint leadership attending both to ensure information flow [79].
- Pilot Project Initiation: Begin collaborations with manageable pilot studies to establish working relationships and demonstrate feasibility before undertaking complex projects [79].
- Cross-Disciplinary Training: Encourage team members to develop understanding of both clinical and basic research challenges to foster mutual respect and innovative problem-solving [79].
Strategic Implementation of GPD Assessment in the Drug Development Pipeline
Integrating GPD assessment early in the therapeutic development process can significantly de-risk pipeline candidates:
This framework enables early identification of candidates with high GPD risk profiles, allowing for resource reallocation or additional validation studies before significant investment in clinical development.
The systematic integration of Genotype-Phenotype Differences into biomedical research represents a paradigm shift in how we approach the challenges of translational science. By explicitly acknowledging and quantifying the biological differences between model systems and humans, researchers can develop more predictive models of human disease and therapeutic response. The computational and methodological frameworks outlined in this whitepaper provide a roadmap for implementing GPD-aware research strategies that have demonstrated potential to significantly improve the efficiency and success rate of therapeutic development.
As single-cell technologies, artificial intelligence, and functional genomics continue to advance, the precision of GPD assessment will continue to improve. Future directions will likely include the development of comprehensive GPD databases, standardized metrics for translatability assessment, and the integration of GPD considerations into regulatory decision-making. For researchers focused on complex diseases, embracing these approaches will be essential for unraveling the intricate relationships between genotype and phenotype that underlie human health and disease.
The integration of chemical features with rich biological context represents a paradigm shift in predictive modeling for complex disease research. This technical guide examines sophisticated computational approaches that fuse chemical structure data with multimodal biological information to enhance the prediction of compound activity, drug-target interactions, and phenotypic outcomes. By synthesizing methodologies across cheminformatics, deep phenotyping, and multi-scale biological profiling, we provide a comprehensive framework for researchers seeking to bridge the critical gap between genotype and phenotype in complex diseases. The strategies outlined herein demonstrate how integrated models achieve superior predictive performance compared to single-modality approaches, ultimately accelerating therapeutic discovery and precision medicine initiatives.
Complex diseases present a formidable challenge in biomedical research due to their heterogeneous nature and multifactorial etiology, where genetic predisposition interacts with environmental factors across a disease continuum [80]. Traditional reductionist approaches that focus on isolated biological components have proven inadequate for capturing the systems-level complexity inherent in conditions like cancer, neurodegenerative disorders, and autoimmune diseases. The integration of chemical features with comprehensive biological context addresses this gap by creating predictive models that more accurately reflect the multidimensional nature of disease mechanisms.
The fundamental premise of this approach recognizes that chemical compounds induce complex biological responses that cannot be fully captured by structural information alone. As Merino notes, complex diseases "are heterogeneous and evolve along a continuum, limiting individual-level prediction with current approaches" [80]. This limitation has prompted the development of novel frameworks such as the Human Phenotype Project (HPP), which integrates "deep phenotyping with generative artificial intelligence (AI) to identify early deviations in health parameters" [80]. Such initiatives highlight the critical need for models that incorporate diverse data modalities to advance precision healthcare across diverse populations.
The Scientific Rationale for Multi-Modal Integration
Complementary Strengths of Data Modalities
Research demonstrates that chemical structures, morphological profiles, and gene expression data capture distinct yet complementary aspects of compound activity. A comprehensive study evaluating these three data sources found that each modality could independently predict compound activity for different subsets of assays, with minimal overlap in their prediction capabilities [81]. This complementarity arises because each data type interrogates different levels of biological organization:
- Chemical structures encode intrinsic physicochemical properties that determine fundamental interaction potentials
- Morphological profiles (e.g., from Cell Painting assays) capture phenotypic changes at the cellular level
- Gene expression profiles (e.g., from L1000 assays) reveal transcriptomic responses to compound exposure
The study revealed that "all three profile types (chemical structures, gene expression, and morphological profiles) can predict different subsets of assays with high accuracy, revealing a lack of major overlap among the prediction ability by each profiling modality alone" [81]. This fundamental insight underscores why integrated approaches substantially outperform single-modality models.
Quantitative Evidence for Integration Benefits
Table 1: Predictive Performance Across Single and Integrated Modalities
| Data Modality | Assays Predicted (AUROC > 0.9) | Assays Predicted (AUROC > 0.7) | Unique Assays Not Predicted by Other Modalities |
|---|---|---|---|
| Chemical Structures (CS) | 16 | ~100 | 3 |
| Gene Expression (GE) | 19 | ~70 | 2 |
| Morphological Profiles (MO) | 28 | ~100 | 19 |
| CS + MO (Late Fusion) | 31 | 137 | 6 |
| CS + GE (Late Fusion) | 18 | 112 | 2 |
| All Three Combined | 44 | 173 | - |
Data adapted from [81]
The quantitative evidence demonstrates that "adding morphological profiles to chemical structures yields 31 well-predicted assays (CS + MO) as compared to 16 assays for CS alone" [81]. This represents nearly a 100% improvement in predictive capability for high-accuracy applications. When considering practical applications where slightly lower accuracy is acceptable (AUROC > 0.7), the combination of chemical structures with phenotypic data "increases the assays that can be predicted from 37% with chemical structures alone up to 64%" [81].
Methodological Framework for Data Integration
Data Preparation and Curation
The foundation of any robust predictive model lies in rigorous data preparation. Each step in model development significantly affects its accuracy, including "the quality and quantity of the input dataset, the selection of significant descriptors, the appropriate splitting of the data, [and] the statistical tools used" [82]. Several critical considerations must be addressed:
Data Quality and Diversity: The compound dataset should contain structurally diverse molecules covering a wide range of values for the target property. Structurally diverse datasets "capture a broad range of structural features that ultimately will provide a larger applicability domain" [82]. This enables models to better generalize underlying structure-property relationships while reducing bias toward specific chemical classes.
Addressing Data Imbalance: Biological datasets frequently suffer from imbalance, with a survey of ChEMBL showing "only 11% of the registered biological targets have a balanced dataset (same proportion of active and inactive compounds)" [82]. This bias toward reporting active compounds necessitates specific strategies such as data augmentation algorithms for rare diseases and intentional inclusion of negative data, which "is valuable and should not be perceived as useless" [82].
Entity Disambiguation: Successful integration requires meticulous reconciliation of biological and chemical entities across datasets. As experts note, "if it's a specific kind of entity—such as a small molecule, a protein, or a pathway—we reconcile those to our authority constructs. This involves resolving the many different expressions of an entity into a singular identifier or component" [83]. This process often requires human curation, as "in published literature, it's common to see hundreds of different representations of a protein or a chemical structure" [83].
Integration Architectures and Fusion Strategies
Table 2: Data Fusion Strategies for Multi-Modal Predictive Modeling
| Fusion Approach | Implementation | Advantages | Limitations |
|---|---|---|---|
| Early Fusion | Concatenation of raw features from all modalities before model training | Preserves potential cross-modal interactions; Single model architecture | Susceptible to overfitting; Requires aligned feature spaces |
| Late Fusion | Separate models for each modality with integration at prediction level | Leverages modality-specific architectures; More robust to missing data | May miss subtle cross-modal interactions |
| Intermediate/Hybrid Fusion | Integration at intermediate model layers | Balances interaction capture with training efficiency | Increased architectural complexity |
| Ensemble Methods | Multiple models with consensus prediction | Higher confidence levels; Robustness to modality-specific noise | Computational intensity; Interpretation challenges |
Research indicates that "for both phenotypic profiling modalities, early fusion performed worse than late fusion (integration of probabilities after separate predictions), yielding fewer predictors with AUROC > 0.9 for all combinations of data types" [81]. This suggests that initially modeling modality-specific relationships independently before integration may be advantageous for many biological applications.
Advanced implementations like CAS BioFinder employ "a cluster of five different predictive models, each with its own methodology. Some models are very structure-based and leverage our chemical data exceptionally well, while others might focus on different data characteristics" [83]. This ensemble approach combines predictions from multiple perspectives to achieve higher confidence levels than any single model could achieve independently.
Experimental Protocols and Workflows
Protocol: Multi-Modal Assay Prediction
Objective: To predict compound bioactivity using integrated chemical structures and phenotypic profiles.
Materials:
- Compound libraries (typically 10,000-50,000 compounds)
- Cell Painting assay reagents for morphological profiling [81]
- L1000 assay kits for gene expression profiling [81]
- High-content screening instrumentation
- Computational infrastructure for deep learning
Methodology:
- Profile Generation:
- Generate morphological profiles using Cell Painting assay with 5-6 fluorescent channels capturing 1,500-2,000 features per compound [81]
- Generate gene expression profiles using L1000 assay measuring 978 landmark transcripts [81]
- Compute chemical structure profiles using graph convolutional networks or extended connectivity fingerprints [81]
Data Partitioning:
- Implement scaffold-based splits to ensure compounds in test sets are structurally dissimilar from training sets [81]
- Apply 5-fold cross-validation to assess model robustness
Model Training:
- Train separate predictors for each modality using multi-task learning architectures
- Apply late fusion via max-pooling of output probabilities from modality-specific predictors [81]
- Regularize using dropout and weight decay to prevent overfitting
Validation:
- Evaluate using Area Under Receiver Operating Characteristic curve (AUROC)
- Assess using additional metrics including mean absolute error (MAE) and root mean squared error (RMSE) [82]
Figure 1: Experimental workflow for multi-modal predictive modeling
Protocol: Next-Generation Phenotyping for Genetic Diagnostics
Objective: To integrate deep phenotyping with genetic data for diagnosing ultrarare disorders.
Materials:
- Exome sequencing platforms
- Standardized phenotyping tools (HPO terms)
- 3D facial imaging systems for dysmorphology assessment
- Electronic health record systems with structured data capture
Methodology:
- Deep Phenotyping:
Genetic Analysis:
- Perform exome sequencing with coverage >100x
- Annotate variants using population frequency and in silico prediction tools
Data Integration:
- Apply genotype-phenotype correlation algorithms
- Utilize machine learning approaches to prioritize variants based on phenotypic match [84]
- Implement case similarity matching across the network
Validation:
- Confirm candidate variants by Sanger sequencing
- Perform functional studies where feasible
This approach has demonstrated significant success, with one study reporting "molecular genetic diagnoses were established in 32% of the patients totaling 370 distinct [disease associations]" [84], highlighting the power of integrated phenotypic and genetic data.
Computational Architectures and Implementation
Advanced Model Architectures
Modern integrated models employ sophisticated deep learning architectures tailored to different data types. For drug-target binding affinity prediction, models like InceptionDTA "leverage CharVec, an enhanced variant of Prot2Vec, to incorporate both biological context and categorical features into protein sequence encoding" [85]. These architectures utilize "a multi-scale convolutional architecture based on the Inception network to capture features at various spatial resolutions, enabling the extraction of both local and global features from protein sequences and drug SMILES" [85].
For chemical structure representation, graph convolutional networks (GCNs) have emerged as powerful tools that "excels at extracting features from raw sequences" [85], overcoming limitations of traditional manually engineered features. These approaches capture both structural patterns and physicochemical properties directly from molecular graphs.
Figure 2: Multi-scale architecture for integrated predictive modeling
Validation Strategies and Performance Metrics
Robust validation is essential for reliable predictive models. Beyond standard cross-validation, specialized approaches include:
- Scaffold-based splits: Ensure compounds in test sets are structurally dissimilar from training data to assess generalization capability [81]
- Cold-start validation: Evaluate performance on new targets or compound classes absent from training data [85]
- Temporal validation: Assess performance on data collected after model training to simulate real-world deployment
Comprehensive evaluation should extend beyond basic metrics to include "mean absolute error (MAE) and the root mean squared error (RMSE)" [82], which provide complementary insights to classification metrics like AUROC. For binding affinity prediction, ranking metrics such as Pearson correlation coefficient are also valuable for assessing model utility in virtual screening.
Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Integrated Predictive Modeling
| Category | Specific Tools/Platforms | Function | Key Features |
|---|---|---|---|
| Phenotypic Profiling | Cell Painting Assay | Captures morphological features | 5-6 fluorescent channels, 1,500+ features/cell [81] |
| Transcriptomic Profiling | L1000 Assay | Gene expression profiling | 978 landmark genes, low cost per sample [81] |
| Chemical Informatics | CDD Vault | Chemical data management | SAR analysis, visualization, collaboration [86] |
| Molecular Visualization | PyMOL, ChimeraX | 3D structure analysis | Protein-ligand interaction mapping [87] |
| Pathway Analysis | KEGG, Reactome | Biological context mapping | Metabolic and signaling pathways [87] |
| Genomic Visualization | UCSC Genome Browser | Genomic data exploration | Reference genomes, annotation tracks [87] |
| Data Integration | CAS BioFinder Platform | Multi-modal predictive modeling | Ensemble models, curated data [83] |
| Machine Learning | Scikit-learn, PyTorch | Model development | Flexible architectures, preprocessing [88] |
The integration of chemical features with biological context represents a fundamental advancement in predictive modeling for complex disease research. By leveraging complementary data modalities through sophisticated computational architectures, researchers can achieve substantially improved prediction of compound activity, drug-target interactions, and phenotypic outcomes. The methodologies outlined in this technical guide provide a roadmap for developing models that more accurately capture the complexity of biological systems, ultimately accelerating the translation of genetic insights into therapeutic strategies.
Future developments in this field will likely focus on several key areas: the incorporation of additional data modalities such as proteomic and metabolomic profiles; the development of more efficient fusion strategies that better capture cross-modal interactions; and the creation of interpretable models that provide biological insights alongside predictions. As these technologies mature, integrated predictive models will play an increasingly central role in bridging the genotype-phenotype gap and advancing precision medicine for complex diseases.
The central challenge in modern genomic medicine lies in accurately linking genotype to phenotype, a process complicated by the pervasive issue of variants of uncertain significance (VUS). These genetic variants represent alterations for which the clinical impact on disease risk cannot be definitively classified as either pathogenic or benign. Current data indicate that VUS substantially outnumber pathogenic findings in clinical testing, with one meta-analysis of breast cancer predisposition testing revealing a VUS to pathogenic variant ratio of 2.5:1 [89]. The interpretation of these variants represents a critical bottleneck in realizing the full potential of genomic medicine for both rare disease diagnosis and complex disease risk assessment.
The fundamental problem stems from the observed variable penetrance—the phenomenon where individuals carrying the same genetic variant exhibit considerable differences in disease expression, ranging from complete absence of symptoms to full manifestation. This variability has traditionally complicated attempts to assign clinical significance to rare genetic variants. Emerging evidence now implicates an individual's background polygenic liability—the cumulative effect of common genetic variants distributed across the genome—as a key modifier of monogenic disease risk and expression [90] [91] [92]. This whitepaper examines the mechanistic role of polygenic liability in resolving variable penetrance and provides a technical framework for incorporating this evidence into VUS interpretation protocols for researchers and drug development professionals.
Quantitative Evidence: Establishing Polygenic Liability as a Modifier
Systematic Mapping of Polygenic Associations in Rare Disease
Recent large-scale studies have provided compelling quantitative evidence supporting the role of polygenic background in modifying rare disease presentation. A comprehensive 2024 analysis of the Genomic Answers for Kids (GA4K) cohort systematically mapped individual polygenic liability for 1,102 open-source polygenic scores (PGS) across 3,059 rare disease probands [90] [91]. This phenome-wide association study approach revealed extensive associations between rare disease phenotypes and PGS for common complex diseases, blood protein levels, and organ morphological measurements.
Table 1: Key Findings from GA4K Cohort Analysis of Polygenic Liability [91]
| Analysis Metric | Finding | Implication for VUS Interpretation |
|---|---|---|
| Significant HPO-PGS Pairs | 897 pairs (FDR 20%) comprising 525 PGS and 154 HPO cohorts | Demonstrates widespread pleiotropic effects between common variant burden and rare disease phenotypes |
| Probands with PGS Associations | 67% (1,775 of 2,641 probands) | Indicates polygenic liability affects a majority of rare disease cases |
| Model Fit (Pseudo-R²) | Median 0.62% (range 0.21-3.30%) | Quantifies the proportion of phenotypic variance explained by polygenic scores |
| Diagnostic Status Impact | Each additional PGS-associated HPO decreased diagnostic likelihood (OR=0.97, p=0.01) | Suggests polygenic effects complicate molecular diagnosis |
| VUS Status Impact | Each additional PGS-associated HPO increased VUS likelihood (OR=1.03, p=0.009) | Supports polygenic burden as mechanism underlying unresolved cases |
Direct Evidence from Trio and Family-Based Studies
Perhaps the most compelling evidence for polygenic liability as a penetrance modifier comes from direct comparisons within families carrying inherited VUS. In the GA4K cohort, probands with inherited autosomal dominant VUS exhibited significantly increased polygenic liability for their associated phenotypes compared to their unaffected carrier parents (proband median PGS = 0.23 vs. carrier parent median PGS = -0.50; Wilcoxon Rank Sum test, P = 5×10⁻⁴) [91]. This effect was more pronounced at more stringent statistical thresholds, demonstrating a dose-response relationship between polygenic burden and disease expression. No significant difference was observed between probands and non-carrier parents, indicating specificity of the effect to the relevant phenotypic domains.
Similar findings have emerged from studies of specific disease domains. Research on telomere biology disorders demonstrated that polygenic modifiers significantly impact both penetrance and expressivity, helping explain the substantial clinical variability observed among carriers of pathogenic variants in telomere-related genes [92]. These findings across diverse disease contexts establish polygenic liability as a generalizable mechanism underlying variable penetrance.
Methodological Framework: Assessing Polygenic Liability in VUS Interpretation
Core Analytical Workflow
The integration of polygenic liability assessment into VUS interpretation requires a systematic methodological approach. The following diagram illustrates the core analytical workflow:
Experimental Protocols for Polygenic Liability Assessment
Polygenic Score Calculation and Quality Control
Objective: To generate standardized polygenic scores for relevant traits and diseases.
Protocol:
- PGS Source Selection: Obtain PGS weights from the PGS Catalog or recent large-scale genome-wide association studies. Prioritize scores with optimal predictive performance in independent validation cohorts [91].
- Genotype Data Processing: Perform standard quality control on patient genotype data, including filtering for call rate (>99%), Hardy-Weinberg equilibrium (p>10⁻⁶), and relatedness estimation. Impute to a reference panel (e.g., 1000 Genomes Phase 3) using standard protocols.
- PGS Calculation: Compute individual PGS using the pruning and thresholding method or continuous shrinkage approaches (e.g., LDpred2). The PGS for an individual i is calculated as:
- Normalization: Standardize PGS within the analysis cohort to Z-scores to facilitate interpretation and comparison.
Phenotype-Driven HPO-PGS Association Testing
Objective: To identify significant associations between patient phenotypes and polygenic scores.
Protocol:
- Phenotype Encoding: Annotate patients using Human Phenotype Ontology (HPO) terms to create standardized phenotypic profiles. For the GA4K study, probands had a median of 6 HPO terms each [91].
- Cohort Definition: For each HPO term, define case/control cohorts based on term presence/absence.
- Association Testing: Implement logistic regression models for each HPO-PGS pair:
- Significance Assessment: Apply false discovery rate (FDR) correction for multiple testing (recommended threshold: FDR < 20% for discovery analyses) [91]. Generate empirical P-values through permutation testing (e.g., 10,000 permutations) to account for distributional assumptions.
Family-Based Polygenic Liability Comparison
Objective: To assess whether probands with VUS have increased polygenic liability compared to unaffected family members.
Protocol:
- Trio Selection: Identify probands with inherited VUS where both parents are available for genotyping.
- PGS Calculation: Compute identical PGS for all family members using the same scoring weights and normalization approach.
- Within-Family Analysis: For PGS significantly associated with the proband's phenotype, calculate the difference in PGS liability between:
- Proband and unaffected carrier parent
- Proband and unaffected non-carrier parent
- Statistical Testing: Apply Wilcoxon Rank Sum tests to compare PGS distributions between probands and carrier parents versus non-carrier parents. For the GA4K cohort, this approach revealed significantly increased PGS liability in probands compared to carrier parents (P = 5×10⁻⁴) but not non-carrier parents [91].
Advanced Network-Based Integration Methods
For complex diseases where multiple biological pathways may be involved, network-based approaches provide enhanced resolution for VUS interpretation. The VariantClassifier (VarClass) methodology utilizes biological network information to identify synergistically acting variants [93].
Protocol:
- Backbone Network Construction: Build evidence-based gene association networks using protein-protein interactions, co-expression, genetic interactions, and pathway data from resources like GeneMANIA.
- VUS Mapping: Iteratively place VUS on these networks through gene association.
- Informative Subnetwork Selection: Identify network neighborhoods containing both known disease-associated genes and VUS-containing genes.
- Risk Model Evaluation: Develop polygenic risk models incorporating both known variants and VUS from the subnetwork, assessing classification improvement using AUC and Integrated Discrimination Improvement metrics [93].
Table 2: Research Reagent Solutions for Polygenic Liability Assessment
| Research Reagent | Function in Analysis | Implementation Considerations |
|---|---|---|
| PGS Catalog | Repository of pre-calculated polygenic scores | Source scores with highest predictive performance and largest training sample sizes [91] |
| Human Phenotype Ontology (HPO) | Standardized phenotype annotation | Encode clinical features using HPO terms for computational analysis [91] |
| GTEx eQTL Catalog | Expression quantitative trait loci data | Identify tissue-specific regulatory consequences of variants [42] |
| GeneMANIA | Biological network construction | Build evidence-based gene association networks [93] |
| ClinVar | Variant pathogenicity database | Obtain known pathogenic and benign variants for comparison [93] |
Conceptual Framework: Integrating Polygenic Liability into Variant Interpretation
The following conceptual model illustrates how polygenic liability modifies the penetrance of candidate disease variants and informs VUS interpretation:
This framework demonstrates how polygenic liability acts as a biological rheostat, modulating the phenotypic expression of genetic variants. When a VUS is inherited against a background of low polygenic liability for relevant traits, the result is typically non-penetrance (unaffected carrier status). Conversely, when the same VUS is coupled with high polygenic liability in the same phenotypic domain, disease manifestation occurs, explaining the observed variable penetrance within families [91].
Implementation Considerations and Future Directions
Technical Validation and Clinical Translation
Implementing polygenic liability assessment in VUS interpretation requires careful attention to technical and analytical considerations:
- Ancestry and Population Diversity: Current PGS predominantly derived from European ancestry populations can lead to biased estimates in diverse populations. Future efforts must prioritize inclusion of diverse ancestry groups in PGS development [89].
- Statistical Power: HPO-PGS association testing requires careful cohort definition and multiple testing correction. Collaborative consortia are essential for adequate sample sizes.
- Integration with Functional Evidence: Polygenic evidence should be integrated with other lines of evidence including segregation data, functional assays, and computational predictions [89] [93].
- Standardization and Reporting: Develop standardized frameworks for reporting polygenic liability in clinical variant interpretation, including quantitative estimates of its contribution to penetrance.
Implications for Drug Development and Therapeutic Targeting
For pharmaceutical researchers, understanding polygenic modifiers of penetrance has significant implications:
- Clinical Trial Enrichment: Patient stratification based on polygenic liability could enrich clinical trials for individuals more likely to show treatment response.
- Target Validation: Genes harboring VUS that show strong polygenic modifier effects represent high-confidence targets for therapeutic development.
- Pleiotropy Assessment: Comprehensive PGS mapping reveals shared genetic architecture between rare diseases and common traits, informing safety and efficacy profiles.
The integration of polygenic liability assessment represents a paradigm shift in VUS interpretation, moving beyond the binary classification of variants to a more nuanced model that accounts for the complex genetic architecture underlying human disease. The methodological framework presented here provides researchers and drug development professionals with evidence-based protocols for quantifying this relationship and applying it to resolve the long-standing challenge of variable penetrance. As genomic medicine continues to evolve, the simultaneous consideration of both rare large-effect variants and common polygenic background will be essential for accurate genotype-phenotype mapping across diverse disease contexts.
Navigating Batch Effects and Technical Noise in Multi-Omics Data Integration
The integration of multi-omics data represents a transformative approach for unraveling the complex relationships between genotype and phenotype in complex diseases. However, this promising field faces substantial technical challenges, primarily stemming from batch effects and technical noise that can obscure biological signals and lead to spurious findings. This technical guide comprehensively examines the sources and impacts of these artifacts across diverse omics technologies, evaluates current computational strategies for mitigation, and provides detailed experimental protocols for robust data integration. By synthesizing the latest methodological advancements in the field, we offer researchers a structured framework to enhance data quality and biological interpretability, ultimately accelerating discovery in complex disease research and therapeutic development.
The fundamental goal of multi-omics research in complex diseases is to establish causal pathways from genetic makeup to observable clinical traits through intermediate molecular phenotypes. This endeavor requires the integrated analysis of genomic, transcriptomic, epigenomic, and proteomic data to reconstruct complete biological networks. However, technical variability introduced during sample processing, sequencing, and measurement threatens the validity of these analyses [94] [95].
Batch effects arise from systematic technical differences when data are collected in separate batches, while technical noise refers to stochastic measurement errors inherent to high-throughput technologies. In single-cell sequencing, for instance, technical noise manifests as "dropout" events where expressed genes fail to be detected, creating sparsity rates of 50-90% in some datasets [96]. These artifacts disproportionately affect the study of complex diseases because the subtle molecular signatures distinguishing disease states are often comparable in magnitude to technical artifacts.
The integration of multiple omics layers amplifies these challenges because each data type possesses distinct statistical distributions, noise profiles, and batch effect characteristics. Effective integration requires specialized approaches that can distinguish true biological signal from technical artifacts across these diverse data modalities [97] [95].
Classification of Technical Artifacts
Multi-omics data integration faces two primary classes of technical challenges that must be understood and addressed to ensure biological validity.
Table 1: Classification of Technical Artifacts in Multi-Omics Data
| Artifact Type | Primary Sources | Characteristic Manifestations | Impact on Downstream Analysis |
|---|---|---|---|
| Batch Effects | Different sequencing runs, laboratory conditions, reagent lots, personnel, or protocols | Systematic shifts in expression profiles between batches; batch-confounded clustering | Spurious associations, reduced statistical power, compromised reproducibility |
| Technical Noise | Stochastic molecular sampling, amplification biases, low input materials, sequencing depth limitations | Dropout events (zero inflation), over-dispersion, false negatives, increased sparsity | Obscured rare cell populations, distorted differential expression, hampered trajectory inference |
| Modality-Specific Heterogeneity | Distinct measurement principles, feature spaces, and statistical distributions across omics types | Incommensurate scales, missing values, non-overlapping feature sets | Challenges in direct data integration, requires specialized normalization and alignment |
Technology-Specific Noise Profiles
Different omics technologies exhibit characteristic noise patterns that necessitate tailored correction approaches:
- Single-cell RNA sequencing: Exhibits significant dropout events and over-dispersion due to low starting mRNA quantities. Technical noise follows a mean-dependent variance structure and affects high- and low-expression genes differently [96].
- Single-cell ATAC-seq: Suffers from sparsity in chromatin accessibility data, with most regions in most cells showing no signal due to technical rather than biological causes.
- Spatial transcriptomics: Contains both technical noise from molecular detection and spatial artifacts from tissue preparation and imaging [96].
- Proteomics: Experiences dynamic range limitations and missing values for low-abundance proteins, with batch effects introduced during sample preparation and mass spectrometry runs.
Computational Methodologies for Noise Reduction
Computational methods for addressing technical artifacts in multi-omics data have evolved from simple normalization procedures to sophisticated machine learning frameworks. These approaches can be broadly categorized by their underlying mathematical principles and integration strategies.
Table 2: Computational Methods for Multi-Omics Data Integration and Noise Mitigation
| Method Category | Representative Tools | Key Strengths | Primary Limitations | Ideal Use Cases |
|---|---|---|---|---|
| Matrix Factorization | MOFA+, intNMF, JIVE, scMFG | Clear interpretability of factors, identifies shared and specific variation, scalable | Assumes linear relationships, sensitive to initialization, may not capture complex interactions | Unsupervised discovery of latent factors, cohort-level multi-omics patterns |
| Deep Learning/Generative Models | Flexynesis, TWAVE, RECODE/iRECODE, VAEs | Captures non-linear relationships, flexible architectures, handles missing data | High computational demands, limited interpretability, requires large sample sizes | Complex non-linear integration, prediction tasks, data imputation |
| Network-Based Approaches | SNF, GLUE | Robust to missing data, captures complex relationships, preserves global structure | Sensitive to similarity metrics, may require extensive parameter tuning | Patient similarity networks, cross-modality relationship mapping |
| Supervised Integration | DIABLO, SDGCCA | Directly links omics to phenotypes, enhanced biological relevance, feature selection | Risk of overfitting, requires high-quality phenotype data | Biomarker discovery, classification tasks, diagnostic model development |
| Feature Grouping | scMFG | Reduces dimensionality, enhances interpretability, identifies feature modules | Depends on grouping quality, may miss global patterns | Single-cell multi-omics, fine-grained cellular heterogeneity |
Advanced Noise Reduction Protocols
The iRECODE Framework for Dual Noise Reduction
iRECODE represents a significant advancement for simultaneously addressing technical noise and batch effects in single-cell data. The method synergizes high-dimensional statistics with established batch correction approaches through a multi-stage computational pipeline [96]:
Noise Variance Stabilizing Normalization (NVSN): Maps gene expression data to an essential space where technical noise characteristics are standardized across cells and genes.
Singular Value Decomposition (SVD): Decomposes the normalized matrix to separate biological signal from technical noise based on differential variance patterns across eigenvalues.
Principal Component Variance Modification: Applies eigenvalue modification theory to suppress components representing technical noise while preserving biological signal.
Integrated Batch Correction: Incorporates established batch correction methods (e.g., Harmony) within the essential space to minimize computational costs while effectively removing batch effects.
The key innovation of iRECODE is performing batch correction in the essential space after initial noise reduction, which prevents the accumulation of errors that occurs when applying these methods sequentially. Benchmarking experiments demonstrate that iRECODE reduces relative errors in mean expression values from 11.1-14.3% to just 2.4-2.5% while maintaining computational efficiency approximately ten times greater than sequential approaches [96].
Feature Grouping Integration with scMFG
The scMFG (single-cell Multi-omics integration based on Feature Grouping) approach addresses noise challenges by organizing features with similar characteristics before integration. The methodology employs a four-stage process [98]:
Feature Group Identification: Applies Latent Dirichlet Allocation (LDA) to group features within each omics layer based on similar expression patterns, effectively creating biologically meaningful feature modules.
Shared Pattern Analysis: Within each feature group, the method identifies shared expression patterns that represent coherent biological signals rather than technical noise.
Cross-Omics Pattern Matching: Identifies similar molecular expression patterns across different omics modalities by comparing feature groups across data types.
Group-Wise Integration: Integrates corresponding feature groups across omics layers using a matrix factorization-based approach (MOFA+), enabling fine-grained integration while maintaining interpretability.
This approach demonstrates particular strength in identifying rare cell types and deciphering cellular heterogeneity at finer resolutions, as validated on complex datasets including mouse kidney, neonatal mouse cortex, and human PBMCs [98].
Experimental Protocols for Robust Multi-Omics Integration
Standardized Preprocessing Workflow
Establishing consistent preprocessing protocols across omics layers is fundamental to mitigating technical artifacts. The following workflow outlines critical steps for matched multi-omics data:
Step 1: Quality Control and Filtering
- scRNA-seq: Filter cells with <200 detected genes; filter genes detected in <10 cells
- scATAC-seq: Filter cells with <200 accessible peaks; remove peaks in <10 cells
- Cross-modality: Remove cells failing QC in any modality to maintain matched samples
Step 2: Normalization and Transformation
- scRNA-seq: Normalize by sequencing depth (counts per million), log-transform with pseudocount
- scATAC-seq: Apply term frequency-inverse document frequency (TF-IDF) transformation
- Proteomics: Perform median centering and variance stabilization
Step 3: Feature Selection
- Identify highly variable genes (2,000-5,000) using mean-variance relationships
- Select informative peaks based on accessibility variance
- Employ cross-modality feature selection when possible to enhance integration
Step 4: Batch Effect Diagnostics
- Perform Principal Component Analysis (PCA) coloring by batch
- Calculate integration metrics (iLISI, cLISI) to quantify batch mixing and biological separation
- Assess correlation structures between negative control features across batches
Benchmarking Framework for Method Selection
Selecting appropriate integration methods requires systematic benchmarking against study-specific data characteristics. We recommend the following evaluation protocol:
Create Gold Standards: Use datasets with known biological ground truth (e.g., cell labels, known disease subtypes) where possible.
Quantify Integration Quality:
- Batch mixing: Local Inverse Simpson's Index (iLISI) scores >0.7 indicate sufficient batch mixing
- Biological preservation: Cell-type Label Inverse Simpson's Index (cLISI) should maintain biological separation
- Feature conservation: Assess correlation of known biomarker expression before/after integration
Evaluate Downstream Performance:
- Cluster purity and adjusted Rand index for cell type identification
- Differential expression consistency across batches
- Trajectory inference robustness to technical variations
Assess Computational Efficiency:
- Scaling with cell numbers and features
- Memory requirements for large-scale datasets
- Compatibility with high-performance computing environments
Table 3: Essential Research Reagents and Computational Tools for Multi-Omics Integration
| Category | Item/Resource | Specific Function | Application Context |
|---|---|---|---|
| Wet-Lab Reagents | 10x Genomics Multiome Kit | Simultaneous profiling of gene expression and chromatin accessibility from single nuclei | Single-cell multi-omics experimental design |
| SCI-seq/SHARE-seq Reagents | High-throughput single-cell combinatorial indexing for coupled measurements | Large-scale single-cell multi-omics studies | |
| CITE-seq Antibodies | Linked detection of protein abundance with transcriptome profiling | Immunophenotyping with transcriptomics | |
| Computational Tools | RECODE/iRECODE Platform | Comprehensive noise reduction for single-cell transcriptomic, epigenomic, and spatial data | Technical noise and batch effect mitigation across modalities |
| Flexynesis Deep Learning Toolkit | Modular deep learning framework for bulk multi-omics integration | Predictive modeling in precision oncology | |
| MOFA+ (Multi-Omics Factor Analysis) | Unsupervised integration using statistical factor models | Discovery of latent factors across omics data types | |
| DIABLO (Data Integration Analysis for Biomarker discovery) | Supervised multi-omics integration for classification and biomarker discovery | Development of diagnostic and prognostic signatures | |
| Data Resources | TCGA/ICGC Pan-Cancer Atlas | Curated multi-omics data across cancer types | Benchmarking, method development, cross-validation |
| Human Cell Atlas | Single-cell multi-omics reference across human tissues | Biological reference construction, normalization | |
| GTEx (Genotype-Tissue Expression) | Tissue-specific molecular QTL mapping | Contextualizing genotype-phenotype relationships |
Implementation Workflow for Robust Genotype-Phenotype Mapping
The following diagram illustrates a comprehensive workflow for managing technical artifacts in multi-omics studies focused on genotype-phenotype mapping in complex diseases:
As multi-omics technologies continue to evolve, several emerging trends promise to further address the challenges of technical artifacts in genotype-phenotype mapping. Foundation models pre-trained on large-scale multi-omics datasets offer potential for transfer learning approaches that require less data for specific applications [97]. The integration of spatial context through spatial transcriptomics and proteomics introduces new dimensions for understanding tissue microenvironment effects while presenting unique normalization challenges [96]. Additionally, the development of explainable AI approaches will be crucial for maintaining biological interpretability in complex deep learning models [99].
The successful navigation of batch effects and technical noise requires a holistic approach spanning experimental design, computational method selection, and rigorous validation. By implementing the protocols and frameworks outlined in this technical guide, researchers can enhance the reliability of their multi-omics integrations and accelerate the discovery of meaningful genotype-phenotype relationships in complex diseases. As the field progresses, continued development of standardized benchmarks, reporting standards, and open-source tools will be essential for advancing reproducible multi-omics science.
Benchmarking Predictive Frameworks: Validation Strategies and Performance Metrics
Linking genotype to phenotype is a fundamental challenge in complex disease research. Unlike single-gene disorders, complex diseases such as diabetes, cancer, and neurodegenerative conditions are influenced by intricate networks of multiple genes working in concert with environmental factors [18] [100]. This complexity presents substantial challenges for identifying robust and reproducible genetic associations, as individual genetic variants typically explain only a tiny fraction of disease susceptibility [100]. In this context, validation through independent cohorts has emerged as an indispensable methodological standard for distinguishing true biological signals from false positives arising from sampling variability, cohort-specific characteristics, or analytical approaches.
The concepts of replicability and generalizability, while related, represent distinct milestones in scientific validation. Replicability refers to the ability to obtain consistent results on repeated observations within similar populations, while generalizability refers to the ability to apply findings from one sample population to different target populations that may vary in age, sex, location, socioeconomic status, or other parameters [101]. The crisis in replication across scientific domains, notably highlighted in psychology where only 36% of replication studies achieved statistically significant results, has underscored the critical importance of robust validation frameworks [102]. For genotype-phenotype mapping in complex diseases, where effect sizes are typically small and multiple testing burdens are substantial, rigorous cross-study validation is not merely beneficial but essential for credible scientific progress and eventual clinical translation.
Methodological Foundations for Cross-Study Validation
Statistical Power and Sample Size Considerations
The foundation of replicable genotype-phenotype research rests upon adequate statistical power. Sample size determination is particularly crucial in complex disease research because biological variables often exhibit relatively small effect sizes [101]. Empirical evidence from population neuroimaging demonstrates that brain-behavior correlations typically fall in the range of r = 0.10 or smaller, with measures of mental health showing even weaker associations with brain measures than cognitive traits [101]. At these effect sizes, samples in the tens to hundreds of individuals exhibit tremendous sampling variability, potentially yielding observed correlations anywhere between r = -0.25 and r = 0.45 for a true correlation of r = 0.10 [101].
Table 1: Sample Size Requirements for Detecting Brain-Behavior Associations
| Effect Size (r) | Minimum Sample for 80% Power | Example from Literature |
|---|---|---|
| 0.20 | ~200 | Largest effect in HCP (N=900) for RSFC-fluid intelligence [101] |
| 0.12 | ~540 | Largest effect in ABCD (N=3,928) for RSFC-fluid intelligence [101] |
| 0.07 | ~1,600 | Largest effect in UK Biobank (N=32,725) for RSFC-fluid intelligence [101] |
| ≤0.10 | Several thousand | Typical brain-mental health associations [101] |
The relationship between sample size and replicability is further illustrated by the progressive refinement of effect size estimates as samples grow larger. For instance, the maximum observed association between resting-state functional connectivity (RSFC) and fluid intelligence decreased from r = 0.21 in the Human Connectome Project (N = 900) to r = 0.12 in the Adolescent Brain Cognitive Development (ABCD) Study (N = 3,928), and further to r = 0.07 in the UK Biobank (N = 32,725) [101]. This pattern demonstrates how small samples tend to inflate effect size estimates due to sampling variability, highlighting the necessity of large-scale cohorts for accurate effect estimation.
Cross-Validation and Internal Replication Techniques
When collecting new independent cohorts is impractical due to cost or feasibility constraints, cross-validation techniques provide a methodological approach for simulating replicability within a single dataset [102]. Cross-validation involves partitioning the dataset and repeatedly generating models to test their future predictive power, thereby protecting against overfitting and increasing confidence that obtained effects will replicate [102].
Table 2: Cross-Validation Schemes for Simulated Replication
| Method | Procedure | Advantages | Limitations |
|---|---|---|---|
| Holdout Cross-Validation | Single split into training and testing sets (typically 2/3 - 1/3) | Low computational load | High variance depending on specific split |
| K-Fold Cross-Validation | Data divided into k folds; each fold serves as test set once | Reduced variance compared to holdout | Requires k times more computation |
| Leave-One-Subject-Out | Each subject serves as test set once | Mirrors clinical diagnostic scenarios | Computationally intensive for large N |
| Leave-One-Trial-Out | Each observation serves as test set once | Maximizes training data | Extremely computationally demanding |
These internal validation approaches are particularly valuable for rare diseases or specialized populations where large sample sizes are difficult to achieve [102]. However, it is crucial to recognize that internal validation primarily addresses replicability within similar populations, while generalizability to different populations requires external validation in truly independent cohorts.
Advanced Analytical Frameworks for Enhanced Generalizability
Multivariate and Systems Genetics Approaches
Traditional univariate approaches to genotype-phenotype mapping have limitations for capturing the complex, interconnected nature of biological systems. Multivariate methods that consider patterns of covariance across multiple biological variables simultaneously offer both conceptual and methodological advantages [103]. For example, a multiblock multivariate approach mapping associations between hippocampal subregion volume, whole-brain grey matter volume, and behavioral variables successfully identified a left anterior hippocampal network related to self-regulation abilities that generalized across both young adult and aging cohorts [103].
Systems genetics represents a powerful framework that integrates intermediate molecular phenotypes (e.g., transcriptomics, proteomics, metabolomics) to understand the pathways linking DNA sequence variation to complex clinical traits [100]. This approach follows the flow of information from genetic variation through molecular intermediates to physiological traits, enabling researchers to identify causal pathways and mediators through techniques like Mendelian randomization and mediation analysis [100]. The value of systems genetics lies in its ability to move beyond mere association to understand how genetic variation perturbs biological systems to affect disease outcomes.
Machine Learning and AI-Driven Phenotyping
Conventional genome-wide association studies (GWAS) often rely on binary case-control phenotypes that inadequately represent the continuous and heterogeneous nature of complex disease manifestation [22]. Machine learning approaches using electronic health record-derived clinical data can generate continuous predicted representations of complex diseases that serve as composite biomarkers capturing both disease probability and severity [22]. These continuous phenotypes increase statistical power for genetic discovery, enable identification of additional therapeutically relevant targets, and improve polygenic risk score performance across diverse ancestry populations [22].
For diseases with particularly complex genetic architectures, such as amyotrophic lateral sclerosis (ALS), deep learning approaches like capsule networks (CapsNets) have demonstrated remarkable efficacy. The DiseaseCapsule framework, which employs a novel gene-scale dimensionality reduction protocol followed by capsule network analysis, achieved 86.9% accuracy in predicting ALS occurrence from whole-genome genotype data, significantly outperforming traditional methods [36]. This approach identified 644 "non-additive" genes that play crucial roles in disease prediction but remain masked within linear analytical schemes, highlighting the potential of AI methods to capture the omnigenic nature of complex traits [36].
Practical Implementation: Protocols for Cross-Study Validation
Coordinated Analysis Across Research Networks
The IALSA (Integrative Analysis of Longitudinal Studies of Aging) research network provides a model for implementing coordinated analysis across independent studies to achieve replicable and generalizable results [104]. This approach involves harmonization at multiple levels: research questions, statistical models, and measurements, while carefully considering sources of cross-study variability such as age, birth cohort, health, education, assessment timing, and attrition rates [104]. Successful implementation requires acknowledging that careful interpretation of multistudy results must include consideration of the broader historical context, including representativeness of population sampling and historical period [104].
The following workflow illustrates a robust cross-cohort validation framework as implemented in hippocampal-brain-behavior research [103]:
Addressing Spurious Associations in Predictive Phenotypes
While machine learning-derived continuous phenotypes enhance genetic discovery, they can introduce spurious associations if not properly handled [22]. For example, a GWAS on type 2 diabetes predicted using hemoglobin A1c might yield variants that actually affect erythrocyte traits rather than glycemic traits [22]. To mitigate this risk, multi-trait analysis of GWAS (MTAG) with predicted phenotypes can be employed to reduce false discoveries while increasing power [22]. This approach has demonstrated high replication rates (73% in FinnGen) for additional variants identified through predicted phenotypes while maintaining low false discovery rates [22].
Table 3: Research Reagent Solutions for Cross-Study Validation
| Resource | Type | Primary Application | Key Features |
|---|---|---|---|
| UK Biobank | Human Cohort | Multi-disease genetic discovery | ~500,000 participants; extensive phenotyping [22] |
| Human Connectome Project | Human Cohort | Brain-behavior mapping | Young adult and aging cohorts; multimodal imaging [103] |
| ABCD Study | Human Cohort | Developmental neurogenetics | ~11,000 children; longitudinal design [101] |
| FinnGen | Human Cohort | Genetic replication | Finnish population; unique genetic structure [22] |
| Project MinE | Disease-Specific Cohort | ALS genetics | 10,405 whole-genome samples [36] |
| TWAVE | Computational Tool | Gene network identification | Generative AI for gene expression analysis [18] |
| DiseaseCapsule | Computational Tool | Disease prediction | Capsule network for whole-genome data [36] |
| PredPsych | Software Platform | Multivariate analysis | Toolbox for psychological science [102] |
The path from genotype to phenotype in complex diseases requires rigorous validation frameworks that prioritize both replicability and generalizability. As research increasingly recognizes the omnigenic nature of most complex traits, where disease-associated variants spread across most of the genome rather than concentrating in a few core pathways [36], the importance of comprehensive validation strategies only grows. Future advances will likely involve even larger, more diverse samples with comprehensive phenotyping, improved methods for distinguishing causal from spurious associations in machine learning-derived phenotypes, and sophisticated multivariate approaches that can capture the hierarchical structure of biological data.
For drug development professionals and translational researchers, the implications are clear: genetic discoveries without robust cross-study validation carry substantial risk for failed clinical translation. The resources and methodologies outlined in this technical guide provide a roadmap for building a more cumulative and reliable science of complex disease genetics, ultimately accelerating the development of effective, personalized therapies for some of medicine's most challenging conditions.
A major hurdle in pharmaceutical development is the poor translatability of preclinical toxicity findings to human outcomes, largely due to fundamental biological differences between humans and model organisms [105]. This translational gap leads to high clinical trial attrition rates and post-marketing drug withdrawals, resulting in significant wasted development costs and patient safety risks [105]. Existing toxicity prediction methods have primarily relied on chemical properties of compounds, typically overlooking these critical inter-species differences in genotype-phenotype relationships [105] [106].
Chronological validation has emerged as a critical methodology for assessing the real-world predictive power of safety assessment frameworks. This approach tests a model's ability to anticipate future drug withdrawals by training on historical data and evaluating performance on subsequent compounds, thereby simulating real-world diagnostic challenges [105]. Within the broader context of genotype-phenotype research in complex diseases, chronological validation provides a rigorous testing ground for assessing how well computational frameworks can bridge the translational gap between preclinical models and human outcomes.
The Genotype-Phenotype Disconnect in Drug Safety
Biological Basis of Species-Specific Toxicity
Drug failures due to toxicity often arise from perturbation of target genes, but the relationship between genetic perturbation and phenotypic effect is not conserved across species [105]. Evolutionary divergence influences phenotypic consequences of gene perturbation by altering protein-protein interaction networks and noncoding regulatory elements [105]. These evolutionary modifications lead to species-specific phenotypic responses to drug-induced gene perturbations, creating fundamental challenges for predicting human drug toxicity based on preclinical models.
For instance, the appetite suppressant sibutramine exhibited no severe cytotoxic effects in preclinical studies but was later withdrawn due to life-threatening cardiovascular risks in humans [105]. Such discrepancies highlight the limitations of conventional approaches that fail to account for fundamental differences in genotype-phenotype relationships between preclinical models and humans.
Current Limitations in Phenotype Prediction
Traditional genome-wide association studies rely on binary case-control phenotypes, which inadequately represent the continuous and heterogeneous nature of complex disease manifestation [22]. This simplification extends to drug safety assessment, where complex toxicity phenotypes are often reduced to binary classifications. Furthermore, existing methods for drug toxicity prediction primarily focus on chemical structure-based features, neglecting the biological context of drug targets [105].
The expansion of biobanks containing extensive electronic health records linked to genetic data has created opportunities for more nuanced phenotype definitions [22] [107]. However, EHR data typically encodes diseases as binary diagnoses using administrative codes designed for billing rather than research, failing to capture the continuous spectrum of disease presentations and severities [22]. This represents a significant limitation in developing accurate models for predicting complex adverse drug reactions.
Methodological Framework for Chronological Validation
Core Principles of Chronological Validation
Chronological validation assesses a model's practical utility in real-world drug development settings by evaluating its ability to anticipate future outcomes based on historical data. Unlike random cross-validation, which shuffles temporal relationships, chronological validation maintains the natural sequence of events, providing a more realistic assessment of predictive performance for future drug withdrawals [105].
This approach involves:
- Training models exclusively on drugs with known outcomes up to a specific cutoff date
- Evaluating performance on drugs approved or entering clinical trials after this date
- Measuring the model's ability to correctly identify drugs that ultimately become withdrawn due to safety concerns
- Comparing performance against state-of-the-art benchmarks using appropriate metrics
Experimental Design and Dataset Curation
The foundation of robust chronological validation is careful dataset construction. One established approach utilizes clinical risk information on drugs obtained from published reports, data sources, and databases without bias [105]. The dataset should include:
Risky Drugs (434 drugs in published framework) [105]:
- Drugs that failed in clinical trials due to safety issues (sourced from specialized databases like ClinTox) [105]
- Drugs withdrawn from markets due to severe adverse events identified through post-marketing surveillance [105]
- Drugs carrying boxed warnings for life-threatening adverse events [105]
Approved Drugs (790 drugs in published framework) [105]:
- Drugs approved for any indication while excluding anticancer drugs due to their distinct toxicity tolerance profiles [105]
- Duplicate drugs with analogous chemical structures should be removed to minimize bias [105]
To ensure reliable estimation of drug perturbation effects, only drugs with target gene information covering more than 50% of relevant data should be included [105].
Quantitative Performance Metrics
Chronological validation requires robust metrics that reflect real-world utility. The following table summarizes key performance indicators from an established genotype-phenotype differences (GPD) framework:
Table 1: Performance Metrics for Chronological Validation of Toxicity Prediction Models
| Metric | GPD-Based Model Performance | Baseline Chemical Model Performance | Interpretation |
|---|---|---|---|
| Area Under Precision-Recall Curve (AUPRC) | 0.63 | 0.35 | Superior ability to identify high-risk drugs among candidates |
| Area Under ROC Curve (AUROC) | 0.75 | 0.50 | Excellent overall classification performance |
| Neurotoxicity Prediction | Significant improvement | Previously overlooked | Addresses major cause of clinical failure |
| Cardiovascular Toxicity Prediction | Significant improvement | Previously overlooked | Addresses major cause of clinical failure |
Data sourced from PMC10597050 [105]
These metrics demonstrate that incorporating genotype-phenotype differences substantially enhances prediction of human drug toxicity, particularly for toxicity classes that frequently lead to clinical trial failures.
Integrating Genotype-Phenotype Differences for Enhanced Prediction
Conceptual Framework for GPD Features
The Genotype-Phenotype Differences (GPD) framework incorporates inter-species and inter-organism differences in genotype-phenotype relationships to improve toxicity assessment [105]. This approach systematically compares biological contexts between preclinical models (cell lines and mice) and humans across three key domains:
Gene Essentiality: Differences in whether perturbation of a gene is lethal or detrimental to the organism [105]
Tissue Expression Profiles: Discrepancies in where and when drug target genes are expressed across tissues [105]
Network Connectivity: Variations in how drug targets are positioned within biological networks and protein-protein interactions [105]
These GPD features are significantly associated with drug failures due to severe adverse events, providing biologically grounded predictors of human-specific toxicities [105].
Machine Learning Implementation
The GPD framework employs a Random Forest model that integrates both GPD features and traditional chemical descriptors [105]. This ensemble method demonstrates enhanced predictive accuracy compared to state-of-the-art chemical structure-based models. The model's robustness is evaluated through independent datasets of drug-adverse event associations and chronological validation confirms its utility for anticipating future drug withdrawals in real-world settings [105].
Table 2: Research Reagent Solutions for Genotype-Phenotype Toxicity Assessment
| Research Reagent | Function in Chronological Validation | Application Context |
|---|---|---|
| STITCH Database | Provides drug-target interactions and chemical similarity data | Mapping drugs to targets; removing chemically analogous duplicates |
| ChEMBL Database | Source of approved drugs and safety warnings (e.g., boxed warnings) | Constructing reference datasets of approved vs. risky drugs |
| ClinTox Database | Contains drugs that failed clinical trials due to safety issues | Curating dataset of risky drugs for model training |
| Human Phenotype Ontology (HPO) | Standardized vocabulary for phenotypic abnormalities | Representing adverse drug reactions consistently |
| UK Biobank EHR Data | Large-scale linked genetic and clinical data | Developing continuous phenotype representations |
Data compiled from multiple sources [105] [22] [30]
Experimental Protocols for Model Development and Validation
Protocol 1: GPD Feature Extraction
This protocol details the process for extracting genotype-phenotype differences features for drug toxicity prediction [105]:
Drug Target Identification: Annotate each drug with its primary protein targets using the STITCH database (version 5) and ChEMBL (version 32)
Gene Essentiality Data Collection:
- Obtain gene essentiality scores for human cell lines from dependency maps (e.g., DepMap)
- Collect lethal phenotype data for mouse orthologs from model organism databases
- Calculate essentiality difference metrics for each drug target
Tissue Expression Profiling:
- Acquire tissue-specific gene expression data for human tissues from resources like GTEx
- Obtain corresponding expression data for mouse tissues from comparable databases
- Compute expression correlation distances between human and mouse for each drug target
Network Analysis:
- Map drug targets onto human protein-protein interaction networks
- Map orthologs onto mouse protein-protein interaction networks
- Calculate network topological differences (degree centrality, betweenness centrality)
Feature Integration: Combine essentiality, expression, and network features into a unified GPD feature vector for each drug
Protocol 2: Chronological Validation Implementation
This protocol establishes the procedure for performing chronological validation of predictive models [105]:
Temporal Dataset Partitioning:
- Sort all drugs by initial approval date or entry into clinical trials
- Establish a cutoff date that represents a realistic point for model deployment
- Assign drugs approved before the cutoff to training set
- Assign drugs approved after the cutoff to test set
Model Training:
- Train Random Forest classifier using GPD and chemical features on training set
- Optimize hyperparameters through temporal cross-validation
- Establish classification threshold based on precision-recall tradeoffs
Temporal Performance Assessment:
- Apply trained model to test set drugs in chronological order
- Record prediction scores for each drug
- Compare predicted risk against actual withdrawal status
- Calculate AUPRC, AUROC, and time-to-detection metrics
Benchmarking:
- Compare performance against state-of-the-art chemical structure-based models
- Assess performance specifically for neurotoxicity and cardiovascular toxicity endpoints
- Evaluate using drugs withdrawn after the cutoff date
Protocol 3: EHR-Based Phenotype Algorithm Development
This protocol outlines the creation of accurate phenotype algorithms from electronic health records for genetic studies [107], which can be adapted for adverse drug reaction detection:
Multi-Domain Data Extraction:
- Extract condition occurrences (ICD codes) from billing data
- Collect medication exposure records from prescription data
- Obtain procedure occurrences from procedural databases
- Retrieve laboratory measurements and vital signs
- Gather observation data including medical history and family history
Algorithm Definition:
- Define inclusion criteria using combinations of domains
- Establish exclusion criteria to improve specificity
- Implement temporal constraints between criteria
- Require multiple occurrences of key criteria where appropriate
Validation Framework:
- Develop gold standard dataset through chart review
- Calculate positive predictive value and negative predictive value
- Compare against simplified algorithms (2+ conditions, Phecode)
- Assess impact on genetic discovery power
Visualization of Methodological Frameworks
Chronological Validation Workflow
Diagram 1: Chronological validation simulates real-world deployment by testing on future compounds.
GPD-Based Toxicity Prediction Framework
Diagram 2: The GPD framework integrates biological differences with chemical features.
Discussion and Future Directions
The integration of genotype-phenotype differences with chronological validation represents a paradigm shift in drug safety assessment. By explicitly accounting for biological differences between preclinical models and humans, this approach addresses a fundamental limitation of traditional chemical-based prediction methods [105]. The significant improvement in predicting neurotoxicity and cardiovascular toxicity is particularly noteworthy, as these toxicity classes represent major causes of clinical failure that were previously overlooked [105].
Future research should focus on expanding the biological contexts incorporated into GPD features, including differences in epigenetic regulation, metabolic pathways, and immune system function. As drug-target annotations and functional genomics datasets continue to expand, GPD-based frameworks are expected to play an increasingly pivotal role in the development of safer and more effective therapeutics [105]. Additionally, the integration of continuous phenotype representations from EHR data [22] and few-shot learning approaches for rare adverse events [30] will further enhance the detection of complex toxicity patterns.
Chronological validation provides the rigorous testing framework necessary to translate these advanced computational approaches into practical tools for drug development. By demonstrating real-world predictive power for future drug withdrawals, this methodology bridges the critical gap between model performance metrics and clinical impact, ultimately contributing to reduced attrition rates, improved patient safety, and more efficient therapeutic development pipelines.
For two decades, genome-wide association studies (GWAS) have served as the cornerstone for mapping genetic variants to complex human diseases and traits [108] [109]. While successful in cataloguing thousands of statistically robust associations, traditional GWAS have faced persistent obstacles in translating these discoveries into actionable biological mechanisms and clinical applications [109] [110]. The inherent polygenicity of most traits, coupled with challenges like linkage disequilibrium (LD) and the "missing heritability" gap, has limited their direct utility for personalized medicine [108] [111]. Concurrently, the field of genomics is experiencing a data deluge, with genomic datasets projected to reach 40 exabytes by 2025 [112]. This convergence of biological complexity and big data has catalyzed the integration of artificial intelligence (AI) and machine learning (ML) models as transformative tools. This whitepaper provides a comparative analysis of these emerging AI paradigms against traditional GWAS and statistical frameworks, contextualized within the critical mission of linking genotype to phenotype for therapeutic discovery.
Part I: Traditional GWAS and Statistical Approaches – Foundations and Limitations
Core Methodology and Historical Success Traditional GWAS operate on a straightforward statistical principle: testing for associations between hundreds of thousands to millions of single-nucleotide polymorphisms (SNPs) and a phenotype across a large population [108] [111]. The strength of this approach lies in its hypothesis-free, genome-wide scan, which has robustly identified thousands of loci associated with hundreds of traits since its inception around 2005-2007 [108] [109]. These studies have provided invaluable biological insights, such as highlighting unexpected genes and revealing the highly polygenic nature of common diseases [108].
Key Limitations and Persistent Obstacles Despite their success in discovery, traditional GWAS face several well-documented constraints that hinder translation:
- Small Effect Sizes and Limited Clinical Utility: The vast majority of identified common variants confer very small individual risk (odds ratios typically <1.4), offering minimal predictive power for individual patients [108]. The bankruptcy of direct-to-consumer genetics companies like 23andMe in 2025 underscores the limited public appetite for tests based on these findings alone [109].
- The LD Bottleneck and Causal Inference: Linkage disequilibrium makes it difficult to pinpoint the causal variant(s) and the target gene(s) from a cluster of associated SNPs, especially when associations fall in non-coding regions [108] [109].
- Focus on Heritability over Actionability: A historical obsession with "closing the heritability gap" has sometimes diverted focus from improving the clinical actionability of discoveries [109].
- Phenotype Definition Challenges: GWAS outcomes are highly sensitive to how cases and controls are defined. Simple definitions based on billing codes can be inaccurate, while more complex, multi-domain phenotyping algorithms (e.g., integrating lab values, medications, procedures) can improve cohort accuracy and GWAS power [107].
- Sample Diversity Gap: Over 80% of GWAS participants are of European ancestry, leading to poor generalizability and potential health disparities [109].
Table 1: Quantitative Outcomes of Traditional GWAS for Complex Traits
| Metric | Typical Finding from Traditional GWAS | Source |
|---|---|---|
| Number of Independent Loci (e.g., T2D) | ~70 variants identified (as of 2014) | [108] |
| Per-Allele Effect Size (Odds Ratio) | Often <1.4 (e.g., TCF7L2 for T2D) | [108] |
| Predictive Power (AUC for 40 T2D variants) | ~0.63 (where 0.5=random, 0.8=useful) | [108] |
| Heritability Explained | Vast majority often remains unexplained | [108] |
| Impact of High-Complexity Phenotyping | Increases GWAS power & functional hits | [107] |
Part II: AI and Machine Learning Models – A New Paradigm
Core Technologies and Learning Paradigms AI for genomics encompasses a hierarchy of techniques, with machine learning (ML) and deep learning (DL) as key subsets [112]. These models learn patterns from data without explicit programming.
- Supervised Learning: Trains on labeled data (e.g., variants annotated as pathogenic/benign) to classify new instances [112].
- Unsupervised Learning: Discovers hidden structures in unlabeled data, useful for clustering patient subgroups [112].
- Reinforcement Learning: An agent learns decision sequences to maximize reward, applicable to designing treatment strategies [112].
Key AI Model Architectures in Genomics
- Convolutional Neural Networks (CNNs): Excel at recognizing spatial patterns, adapted to treat DNA sequences as 1D images for tasks like variant calling (e.g., DeepVariant) and motif discovery [112].
- Recurrent Neural Networks (RNNs)/Long Short-Term Memory (LSTMs): Designed for sequential data, ideal for modeling genomic and protein sequences to predict structure or function [112].
- Transformer Models: Use attention mechanisms to weigh the importance of different sequence parts, forming the basis of powerful foundation models pre-trained on vast genomic data [112].
- Generative Models (GANs, VAEs): Can generate novel protein sequences or synthetic genomic data for research and drug design [112].
Primary Applications in Genetic Analysis
- Enhanced Phenotyping and GWAS Augmentation: ML can derive predicted continuous disease representations from electronic health records, which can complement traditional case-control definitions. A 2025 study showed such predicted phenotypes identified more independent genetic associations (median 306 vs. 125) and improved polygenic risk score (PRS) prediction (37% median increase in R²) for eight complex diseases [113].
- Post-GWAS Functional Interpretation: AI models integrate multi-omic data (genomics, transcriptomics, proteomics) to prioritize causal genes, interpret non-coding variants, and predict variant effects, directly addressing the biological insight gap left by GWAS [112] [110].
- Drug Discovery and Target Prioritization: AI sifts through genetic and molecular data to identify novel drug targets, repurpose existing drugs, and predict patient-specific drug responses. For example, predicted phenotypes have identified genes targeted by phase I-IV drugs that were missed by case-control GWAS [112] [113].
Part III: Direct Comparison of Performance and Outcomes
Table 2: Comparative Performance: Traditional GWAS vs. AI-Augmented Approaches
| Aspect | Traditional GWAS/Statistics | AI/ML-Augmented Approaches | Key Evidence |
|---|---|---|---|
| Discovery Power (# of Loci) | Identifies foundational loci. | Identifies significantly more independent associations. | Predicted phenotypes found median 306 vs. 125 loci [113]. |
| Phenotype Definition | Relies on often simplistic (e.g., ICD codes) or labor-intensive clinical definitions. | Can infer sophisticated, continuous phenotypes from multimodal EHR data. | Predicted phenotypes are composite biomarkers with high genetic correlation to clinical diagnoses (median rg=0.66) [113]. |
| Risk Prediction (PRS) | Limited predictive accuracy for many diseases. | Can significantly improve PRS performance. | Combined PRS using both case-control and predicted phenotypes increased Nagelkerke's R² by median 37% [113]. |
| Causal & Biological Insight | Limited; identifies association, not mechanism. | Directly enables functional interpretation and causal gene prioritization. | AI models predict variant effects, protein structures (AlphaFold), and gene function [112] [110]. |
| Susceptibility to Bias | Prone to confounding from population structure; requires careful correction. | Risk of New Biases: ML-assisted GWAS can introduce severe false positives if not properly designed. | GWAS on an ML-imputed T2D phenotype had an 81% replication failure rate due to learning non-glycemic HbA1c pathways [114]. |
| Handling of Rare Variants | Underpowered for rare variant association studies. | Enables integrated analysis of rare and common variant contributions. | Methods like "Causal Pivot" use PRS to subgroup patients driven by rare pathogenic variants [115]. |
The Critical Caveat: Risk of False Positives in ML-Assisted GWAS A paramount distinction is the risk profile. Traditional GWAS, with rigorous quality control and population structure correction, yield extremely robust associations [108]. In contrast, a 2024 study sounded a major alarm: performing GWAS on an ML-imputed phenotype without accounting for imputation uncertainty leads to pervasive false positives [114]. For example, a GWAS on an imputed type 2 diabetes phenotype, which relied heavily on hemoglobin A1c (HbA1c) levels, falsely identified variants affecting red blood cell lifespan (non-glycemic HbA1c pathways) as being associated with T2D risk, resulting in an 81% replication failure rate [114]. This highlights that high imputation accuracy does not guarantee valid genetic associations.
Part IV: Methodological Deep Dive: Experimental Protocols
1. Protocol for Valid ML-Assisted GWAS (POP-GWAS) To address the false-positive crisis, the Post-Prediction GWAS (POP-GWAS) framework was developed [114].
- Objective: To obtain valid SNP effect estimates from a GWAS performed on an ML-imputed phenotype.
- Input Requirements: GWAS summary statistics only.
- Procedure:
- Partition the full dataset into a labeled set (with observed phenotype) and an unlabeled set.
- Train an ML model (e.g., SoftImpute, XGBoost) to impute the phenotype using the labeled set.
- Perform three separate GWAS:
- GWAS A: On the imputed phenotype in the unlabeled samples (β̂Ŷ,unlab).
- GWAS B: On the observed phenotype in the labeled samples (β̂Y,lab).
- GWAS C: On the imputed phenotype in the labeled samples (β̂_Ŷ,lab).
- Compute the POP-GWAS estimate for each SNP j using the formula:
β̂_POP,j = r * (N_unlab/(N_unlab+N_lab)) * β̂_Ŷ,j_unlab + β̂_Y,j_lab - r * (N_unlab/(N_unlab+N_lab)) * β̂_Ŷ,j_labwhereris the correlation between observed and imputed phenotypes in the labeled set.
- Outcome: Unbiased effect size estimates, controlling for imputation error. Applied to bone mineral density, POP-GWAS identified 89 novel loci [114].
2. Protocol for Disentangling Genetic Drivers (Causal Pivot)
- Objective: To identify subgroups of patients where disease is driven by rare variants versus polygenic risk.
- Principle: If a rare pathogenic variant is a strong driver, affected carriers will have a lower polygenic risk score (PRS) than affected non-carriers, as the rare variant itself provides sufficient disease risk [115].
- Procedure:
- Calculate a PRS for the disease of interest for all cases.
- For a putatively causal rare variant or gene set, test for a significant difference in PRS distribution between carrier and non-carrier cases.
- Implement rigorous statistical safeguards to control for confounding factors like ancestry.
- Validation: Successfully detected known subgroups (e.g., LDLR carriers in hypercholesterolemia, BRCA1 in breast cancer) in UK Biobank data [115].
3. Protocol for Multi-Domain Phenotyping for GWAS
- Objective: Construct more accurate case/control cohorts from electronic health records to improve GWAS power [107].
- Procedure:
- Access Data: Obtain EHR data in a structured format like OMOP CDM.
- Apply Algorithms: Define cases using rules of varying complexity:
- Low Complexity: Require ≥2 condition codes (ICD) for the disease.
- Medium Complexity: Use curated code sets (Phecodes) or integrate 2-3 domains (e.g., conditions + drugs).
- High Complexity: Integrate multiple domains (conditions, drugs, procedures, lab measurements, observations) as in OHDSI or UK Biobank ADO algorithms.
- Perform GWAS: Conduct standard GWAS on cohorts defined by each algorithm, adjusting for covariates.
- Evaluate: Compare power, number of hits, heritability estimates, and functional enrichment of results.
Part V: Integrated Pathways and Future Directions
The future lies not in replacement but in synthesis. The most powerful framework leverages the robust association mapping of GWAS with the interpretive and predictive power of AI.
Integrated Workflow for Genotype-to-Phenotype Translation:
Diagram 1: Integrated Genotype-to-Phenotype Pipeline (96 chars)
Emerging Solutions and Research Vectors
- Bridging the LD Bottleneck with AI: Future models may learn LD patterns directly to generate necessary matrices, moving beyond computationally burdensome reference panels [109].
- From Heritability to Actionability: The focus must shift towards explaining risk at the individual level and identifying actionable pathways, not just maximizing variance explained [109].
- Global, Diverse Research Ecosystems: Expanding biobanks to include diverse ancestries is a scientific and moral imperative to ensure equitable genetic discoveries and applications [109].
- Explainable AI (XAI) for Biological Insight: Developing interpretable AI models is crucial for generating testable biological hypotheses from black-box predictions [110].
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Key Resources for Modern Genetic Analysis
| Category | Item/Solution | Function/Description |
|---|---|---|
| Reference Data | GRCh37/GRCh38 Reference Genome | Standardized genomic coordinate system for alignment and variant calling. Adoption of newer pangenome references is emerging [109]. |
| Cohort Data | UK Biobank, All of Us, FinnGen | Large-scale biobanks providing integrated genetic, clinical, and lifestyle data for discovery and validation [113] [114] [115]. |
| Genotyping Data | High-Density SNP Microarray Data | The foundational data for most GWAS, often imputed to higher density [108] [111]. |
| Software (Traditional) | PLINK, SAIGE, METAL, LDSC | Industry-standard tools for GWAS QC, association testing, meta-analysis, and heritability estimation [109] [116]. |
| Software (AI/ML) | TensorFlow/PyTorch, POP-GWAS, AlphaFold | Frameworks for building custom models, specialized tools for valid ML-GWAS, and revolutionary protein structure prediction [112] [114]. |
| Phenotyping Tools | OHDSI Phenotype Library, Phecode Maps, PheValuator | Libraries of curated algorithms for defining diseases from EHRs and tools to evaluate algorithm accuracy [107]. |
| Hardware | GPU Accelerators (e.g., NVIDIA H100) | Essential for training and running large-scale deep learning models on genomic data [112]. |
| Analytical Framework | Causal Pivot Methodology | A statistical framework to identify patient subgroups driven by rare variants using polygenic risk scores as a pivot [115]. |
Conclusion The journey from genotype to phenotype in complex diseases is being fundamentally reshaped. Traditional GWAS provided the essential, robust map of associations. AI and ML models now offer the tools to navigate this map, interpreting its features, predicting outcomes, and identifying actionable destinations. However, this powerful synergy comes with new responsibilities—rigorous methodologies like POP-GWAS are required to avoid false discoveries, and a renewed commitment to diversity and clinical relevance is paramount. The integrated use of both paradigms represents the most promising path toward unraveling disease etiology and delivering on the promise of precision medicine.
The central challenge in post-genomics biology is bridging the gap between genetic data and clinical phenotypes, particularly for complex diseases influenced by multiple genetic and environmental factors. The surge of high-throughput sequencing technologies has revealed extensive genetic variations within human populations, with the vast majority classified as variants of uncertain significance (VUS) because their phenotypic consequences remain unknown [117]. In the post-sequencing era, the primary task has shifted from data generation to data interpretation—converting rich genetic data into biologically and clinically meaningful information.
This challenge is particularly acute for missense single-nucleotide variants (SNVs), which account for the majority of VUS. According to one analysis, in commonly sequenced genes, the proportions of variants with uncertain significance or conflicting information can be remarkably high (e.g., BRCA1: 52% uncertain, 3% conflicting) [117]. For complex diseases like diabetes, cancer, and asthma, the situation is further complicated by their multigenic nature. As Motter explains, "You can compare a disease like cancer to an airplane crash. In most cases, multiple failures need to occur for a plane to crash, and different combinations of failures can lead to similar outcomes" [18]. This complexity underscores the critical need for robust functional validation frameworks to move from statistical associations to biological understanding.
Computational Prediction: The First Line of Assessment
Artificial Intelligence in Variant Effect Prediction
Artificial intelligence (AI) has become an invaluable tool for initial VUS assessment, providing high-efficiency predictions that help prioritize variants for experimental validation. Two main computational approaches have emerged: supervised training, which relies on clinical labels of pathogenic versus benign variants, and unsupervised models of evolutionary sequences that predict variant effects directly from multiple sequence alignments without relying on labels [117].
Breakthroughs in protein structure prediction, particularly AlphaFold2 and RoseTTAFold, have significantly enhanced AI variant predictors by incorporating information about protein tertiary structures [117]. These structure-based algorithms can be divided into energy-based methods (utilizing differences in free energy (ΔΔG) between wild-type and variant structures) and non-energy-based methods that leverage structural features without energy calculations [117].
Table 1: State-of-the-Art Computational Tools for Missense Variant Prediction
| Predictor | Structure Accepted | Predicted Structure Accepted | ΔΔG Accepted | Approach |
|---|---|---|---|---|
| DEOGEN2 | N | N | N | Supervised |
| REVEL | N | N | N | Supervised |
| CADD | N | N | N | Supervised |
| EVE | N | N | N | Unsupervised |
| EVmutation | N | N | N | Unsupervised |
| SIFT | N | N | N | Unsupervised |
| Dynamut2.0 | Y | Y | Y | Energy-based |
| MutPred2 | Y | N | N | Structure-based |
| AlphaMissense | Y | Y | N | Structure-based |
Beyond Single Variants: Network and Continuous Phenotypes
Traditional genome-wide association studies (GWAS) rely on binary case-control phenotypes, which inadequately represent the continuous and heterogeneous nature of complex disease manifestation [22]. Novel approaches using machine learning with electronic health record-derived clinical data can generate continuous predicted representations of complex diseases, serving as composite biomarkers that represent both the probability and severity of disease [22].
Tools like TWAVE (Transcriptome-Wide conditional Variational auto-Encoder) leverage generative AI to identify patterns from limited gene expression data, enabling researchers to resolve patterns of gene activity that cause complex traits [18]. Instead of examining the effects of individual genes in isolation, such models identify groups of genes that collectively cause a complex trait to emerge [18]. This approach has demonstrated practical utility, identifying 160% more linkage disequilibrium-independent variants compared to traditional case-control phenotypes [22].
Experimental Validation: From Omics to Physiological Assays
Functional Genomics and Omics Strategies
Holistic screening approaches provide powerful tools for obtaining additional evidence for variant pathogenicity. mRNA expression analysis by RNA-seq can provide crucial data for variants causing alternative splice events or loss of expression [118]. In one study, combining mRNA expression profile analysis in mitochondrial disease patient fibroblasts with whole exome sequencing increased the diagnostic yield by 10% compared to WES alone [118].
According to established guidelines, there are five criteria regarded as strong indicators of pathogenicity for unknown genetic variants, with established functional studies showing a deleterious effect representing one of the most compelling categories of evidence [118]. Other indicators include prevalence in affected populations, specific mutation types, de novo occurrence, and amino acid changes at established pathogenic positions.
Table 2: Functional Validation Methodologies for Variant Assessment
| Method Category | Specific Techniques | Information Provided | Throughput |
|---|---|---|---|
| Transcriptomics | RNA-seq, qPCR | Effects on mRNA expression, splicing defects | Medium-High |
| Proteomics | Western blot, mass spectrometry | Effects on protein expression, stability, post-translational modifications | Medium |
| Metabolomics | Mass spectrometry, NMR | Changes in metabolite levels, pathway disruptions | Medium |
| Biomarker Studies | Biochemical assays, enzymatic activity | Functional consequences in relevant pathways | Low-Medium |
| Cell-based Assays | Immunofluorescence, subcellular localization | Effects on protein trafficking and cellular distribution | Low |
Detailed Experimental Protocols
RNA Sequencing for Splice Variant Assessment
Purpose: To identify aberrant splicing events caused by genetic variants. Methodology:
- Isolate total RNA from patient-derived fibroblasts or other relevant cell types using a column-based extraction method.
- Assess RNA quality using Bioanalyzer or TapeStation (RIN > 8.0 required).
- Prepare sequencing libraries using poly-A selection or rRNA depletion kits.
- Sequence on an Illumina platform to obtain a minimum of 30 million paired-end reads per sample.
- Align reads to the reference genome using STAR aligner.
- Detect aberrant splicing events using tools like rMATS or LeafCutter.
- Validate significant findings by RT-PCR using primers flanking the putative aberrant exon.
Interpretation: Significantly altered inclusion rates of exons (ΔPSI > 0.1, FDR < 0.05) in proximity to the genetic variant provide strong evidence for pathogenicity through effects on splicing.
Enzyme Activity Assay for Metabolic Disorders
Purpose: To quantitatively assess the functional impact of variants in enzymes implicated in inborn errors of metabolism. Methodology:
- Obtain patient-derived fibroblasts or create recombinant expression system with wild-type and variant constructs.
- Prepare cell lysates using non-ionic detergents in appropriate buffer systems.
- Measure protein concentration using Bradford or BCA assay.
- Incubate lysates with enzyme-specific substrates under optimal pH and temperature conditions.
- Monitor product formation spectrophotometrically or fluorometrically over time.
- Calculate enzymatic activity as nmol product formed/min/mg protein.
- Normalize activities to wild-type controls (set at 100%).
Interpretation: Significant reduction in enzymatic activity (<20% of wild-type) provides strong evidence for pathogenicity, while intermediate activities (20-60%) may suggest partial function requiring additional evidence.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Functional Validation Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Cell Culture Systems | Patient-derived fibroblasts, iPSCs, HEK293T | Provide cellular context for functional studies |
| Antibodies | Anti-target protein, loading control | Protein detection and quantification |
| Sequencing Kits | RNA-seq library prep, poly-A selection | Transcriptome analysis |
| Cloning Vectors | pcDNA3.1, pEGFP, lentiviral constructs | Recombinant protein expression |
| Enzymatic Assay Kits | Spectrophotometric substrates, coupled assays | Quantitative enzyme activity measurement |
| CRISPR Components | Cas9 nucleases, guide RNAs, repair templates | Genome editing for variant introduction |
| Protein Markers | Size standards, molecular weight ladders | Gel electrophoresis reference |
Integrating Functional Data into Drug Discovery
Functional validation provides crucial evidence for drug target prioritization, particularly for complex diseases where multiple gene networks may be involved. A recent study demonstrated that predicted phenotypes identified 14 genes targeted by phase I–IV drugs that were not identified by case-control phenotypes [22]. This highlights how functional understanding of variant mechanisms can reveal new therapeutic opportunities.
The finding that different sets of genes can cause the same complex disease in different individuals suggests that personalized treatments could be tailored to a patient's specific genetic drivers of disease [18]. Furthermore, combined polygenic risk scores using both traditional and predicted phenotypes have shown improved prediction performance, with a median 37% increase in Nagelkerke's R², enhancing our ability to stratify patient populations for clinical trials [22].
Visualizing Workflows and Biological Relationships
Functional Validation Workflow
Multigenic Disease Mechanism
From Genotype to Phenotype
The functional validation pipeline represents an indispensable framework for translating genetic findings into biological understanding and therapeutic opportunities. By integrating computational predictions with experimental validation across multiple biological layers, researchers can bridge the critical gap between genotype and phenotype in complex diseases. As functional genomics technologies continue to advance and computational models become increasingly sophisticated, our ability to decrypt variants of uncertain significance will dramatically accelerate, ultimately enabling more precise diagnostics and targeted therapeutics for complex multigenic disorders.
In the pursuit of linking genotype to phenotype for complex diseases, researchers face a fundamental challenge: traditional binary disease classifications (case-control) often inadequately represent the continuous and heterogeneous nature of disease manifestation [22]. This limitation constrains the statistical power of genetic association studies and hampers the discovery of novel therapeutic targets. Clinical utility provides a critical framework for evaluating how diagnostic genomic information, such as that from whole-genome sequencing (WGS), improves patient management and outcomes, thereby bridging the gap between genetic discovery and clinical application [119]. Within a broader thesis on complex diseases, this guide details the metrics and methodologies for quantifying diagnostic yield improvement and therapeutic relevance, which are essential for demonstrating the value of genomic testing in a research and clinical context.
Defining and Measuring Clinical Utility: A Hierarchical Framework
A robust approach to measuring clinical utility extends beyond simple laboratory accuracy. The Fryback and Thornbury hierarchical model of efficacy, adapted for genomic applications, offers a structured framework for evidence collection [119]. This model progresses through several levels of efficacy, from technical performance to broader societal impact.
For the diagnostic application of WGS in rare diseases, clinical utility is most practically operationalized across four key domains [119]:
- Diagnostic Thinking Efficacy: The impact of a test on a clinician's diagnostic thinking and decision-making.
- Therapeutic Efficacy: The influence of a test on treatment selection and management.
- Patient Outcome Efficacy: The effect on health outcomes, including morbidity, mortality, and quality of life.
- Societal Efficacy: The broader impact on families and healthcare systems, including cost-effectiveness.
Core Metrics for Diagnostic Test Performance
The intrinsic performance of any diagnostic test is characterized by its sensitivity and specificity, which are foundational to its clinical utility [120].
- Sensitivity and Specificity: These are intrinsic properties of a test. Sensitivity (true positive rate) is the ability to correctly identify those with the disease. Specificity (true negative rate) is the ability to correctly identify those without the disease [120].
- Predictive Values: Unlike sensitivity and specificity, Positive Predictive Value (PPV) and Negative Predictive Value (NPV) are performance characteristics that describe a test's real-world diagnostic capability. They are strongly influenced by the prevalence of the disease in the population being tested [120]. The formulas for calculating PPV and NPV are:
PPV = (Sensitivity × Prevalence) / (Sensitivity × Prevalence + (1 – Specificity) × (1 – Prevalence))
NPV = (Specificity × (1 – Prevalence)) / ((1 – Sensitivity) × Prevalence + Specificity × (1 – Prevalence)) [120]
The relationship between these metrics is summarized in the table below.
Table 1: Core Performance Metrics for Diagnostic Tests
| Metric | Definition | Interpretation | Key Influence |
|---|---|---|---|
| Sensitivity | Proportion of truly diseased individuals correctly identified as abnormal by the test [120]. | A test with high sensitivity is good at ruling out a disease if the result is negative (SnNout) [120]. | Intrinsic test property |
| Specificity | Proportion of healthy individuals correctly identified as normal by the test [120]. | A test with high specificity is good at ruling in a disease if the result is positive (SpPin) [120]. | Intrinsic test property |
| Positive Predictive Value (PPV) | Proportion of patients with a positive test result who are correctly diagnosed [120]. | Probability that a person with a positive test actually has the disease. | Disease Prevalence |
| Negative Predictive Value (NPV) | Proportion of patients with a negative test result who are correctly identified as disease-free [120]. | Probability that a person with a negative test truly does not have the disease. | Disease Prevalence |
Strategies for Improving Diagnostic Yield
Diagnostic yield refers to the ability of a test to successfully identify a causative diagnosis. In complex diseases, which are influenced by networks of multiple genes working together, improving yield requires moving beyond single-gene approaches [18].
Moving Beyond Binary Phenotypes with Machine Learning
A primary strategy for improving yield is to replace simplistic binary (case-control) disease definitions with continuous, machine learning (ML)-derived phenotypes. This approach better reflects the biological spectrum of disease.
- Methodology: Researchers can use comprehensive phenotypic data from electronic health records (EHRs)—including clinical measurements, laboratory results, and survey data—to train ML models that predict disease status. These models generate a continuous predicted phenotype, which is a composite biomarker representing both the probability and severity of disease [22].
- Experimental Workflow: The following diagram illustrates the workflow for creating and using these continuous phenotypes for genetic discovery.
Quantitative Impact on Genetic Discovery
The use of ML-derived continuous phenotypes has a quantifiable impact on the outcomes of genome-wide association studies (GWAS). Research across eight complex diseases showed that predicted phenotypes significantly enhance genetic discovery compared to traditional case-control definitions [22].
Table 2: Impact of Predicted Phenotypes on Genetic Discovery [22]
| Disease | LD-Independent Variants (Case-Control) | LD-Independent Variants (Predicted Phenotype) | Percentage Increase | Genetic Correlation (rg) |
|---|---|---|---|---|
| Coronary Artery Disease | 125 (Median) | 306 (Median) | 160% (Median) | 0.84 (Max) |
| Type 2 Diabetes | Information not available in source | Information not available in source | Information not available in source | 0.91 (Max) |
| Atrial Fibrillation | Information not available in source | Information not available in source | Information not available in source | Information not available in source |
Mitigating Spurious Associations with Multi-Trait Analysis
A known caveat of using predicted phenotypes is the potential for spurious genetic associations, even with high prediction accuracy. For instance, a GWAS for a diabetes phenotype predicted using hemoglobin A1c might identify variants that actually influence erythrocyte traits rather than glycemic control [22].
- Methodology: To reduce false discoveries while retaining true associations, researchers can employ Multi-trait analysis of GWAS (MTAG). This statistical method integrates the GWAS summary statistics from both the binary case-control phenotype and the continuous predicted phenotype [22].
- Protocol: The analysis is performed in a dataset where all participants have both phenotype labels. The MTAG framework boosts the power of the case-control GWAS by leveraging genetic correlations with the predicted phenotype, which itself distills hundreds of disease-correlated traits into a single score. This approach does not require manual trait selection and has been shown to have a low false discovery rate, with a high proportion of identified variants replicating in independent cohorts [22].
Establishing Therapeutic Relevance and Drug Target Prioritization
A primary goal of linking genotype to phenotype is to identify new therapeutic targets and stratify patients for existing treatments. Clinical utility in this domain is measured by therapeutic efficacy [119].
From Genetic Loci to Actionable Drug Targets
Genetic associations identified through enhanced GWAS can directly inform drug discovery and development.
- Methodology: Researchers can map identified genetic variants to genes and then cross-reference these genes with drugs in various stages of development (Phase I-IV) using drug target databases. A key validation step is to assess whether the gene is a known target of an existing drug or is being investigated in clinical trials [22].
- Experimental Evidence: Studies have demonstrated that predicted phenotypes can identify genes targeted by phase I–IV drugs that were not identified by case-control phenotypes alone. For example, in a study of eight complex diseases, this approach revealed 14 such additional drug targets [22].
Enhancing Risk Prediction for Clinical Application
Improving the accuracy of polygenic risk scores (PRS) is another critical pathway to therapeutic relevance, as it enables better patient stratification and prevention strategies.
- Protocol: Construct separate PRS using the GWAS summary statistics from both the case-control and the predicted phenotype GWAS. These scores can then be combined. The performance of the PRS is typically evaluated by measuring the increase in Nagelkerke's R² (a pseudo R-squared measure for logistic regression models) when the scores are applied to diverse ancestry populations [22].
- Quantitative Outcome: Research shows that combined PRS using both phenotypes can achieve a median 37% increase in Nagelkerke's R² compared to using a PRS derived from a case-control GWAS alone [22].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key resources and their functions for conducting research in clinical utility and genetic discovery for complex diseases.
Table 3: Research Reagent Solutions for Genotype-Phenotype Studies
| Item | Function / Application |
|---|---|
| Biobank with EHR Linkage (e.g., UK Biobank) | Provides a large-scale cohort with linked genetic and deep phenotypic data for model training and genetic association studies [22]. |
| Machine Learning Frameworks (e.g., Python, R libraries) | Used to construct models that generate continuous predicted phenotypes from raw EHR and clinical data [22]. |
| GWAS Software (e.g., PLINK, BOLT-LMM, REGENIE) | Performs genome-wide association testing to identify genetic variants correlated with binary or continuous traits [22]. |
| Multi-Trait Analysis Tool (e.g., MTAG) | A statistical tool that integrates summary statistics from multiple GWAS to increase power and reduce spurious associations [22]. |
| LD Score Regression (LDSC) | Used to estimate heritability, genetic correlation between traits, and to assess genomic inflation in GWAS [22]. |
| Polygenic Risk Score (PRS) Software (e.g., PRSice, LDpred2) | Calculates individual-level genetic risk scores based on GWAS summary statistics [22]. |
| Drug Target Database (e.g., ChEMBL, Open Targets) | Platforms to cross-reference genes identified in GWAS with known or investigational drug molecules [22]. |
Quantifying diagnostic yield improvement and therapeutic relevance is paramount for advancing complex disease research. By adopting a hierarchical framework for clinical utility and leveraging modern computational strategies—such as continuous phenotype derivation and multi-trait genetic analysis—researchers can significantly enhance genetic discovery, prioritize viable drug targets, and develop more accurate risk prediction tools. This rigorous, metrics-driven approach is essential for solidifying the critical link between genotype and phenotype and for translating genomic discoveries into tangible clinical benefits.
Conclusion
The integration of advanced computational methods with large-scale genomic data is fundamentally transforming our capacity to link genotypes to phenotypes in complex diseases. Key takeaways include the necessity of moving beyond single-gene models to embrace polygenic and network-based frameworks, the power of AI to resolve collective genetic effects, and the critical importance of addressing translational challenges between model systems and humans. Future progress will depend on enhanced functional genomics annotations, improved cross-species models, and the development of even more sophisticated integrative AI frameworks. These advances promise to accelerate therapeutic discovery, enable truly personalized treatment strategies based on individual genetic architecture, and ultimately bridge the long-standing gap between genetic information and clinical manifestation in complex diseases.
References
- 1. Discovering genotypes underlying human phenotypes : past... [https://pubmed.ncbi.nlm.nih.gov/12610532/]
- 2. Discovering genotypes underlying human phenotypes : past... [https://www.nature.com/articles/ng1090z?error=cookies_not_supported]
- 3. Genetic architecture of quantitative traits and complex ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6764439/]
- 4. Genetic architecture of quantitative traits and complex ... [https://www.sciencedirect.com/science/article/abs/pii/S0959437X13001433]
- 5. Unravelling the genetic architecture of human complex ... [https://www.nature.com/articles/s41467-023-39259-x]
- 6. Mutation-selection-drift balance models of complex diseases [https://pubmed.ncbi.nlm.nih.gov/41073879/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=0280qBldWH9RInRF9mB9jlMdlDMx03tFUVcKauoE7Oa&fc=None&ff=20251122001348&v=2.18.0.post22+67771e2]
- 7. Multivariate genome-wide analysis reveals shared genetic ... [https://www.nature.com/articles/s41598-025-25509-z]
- 8. BiologicalNetworks: visualization and analysis tool for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1538788/]
- 9. Polygenic risk scores: from research tools to clinical instruments [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-020-00742-5]
- 10. Polygenic scores in biomedical research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9391275/]
- 11. Evaluation of polygenic scoring methods in five biobanks ... [https://www.sciencedirect.com/science/article/pii/S000292972400209X]
- 12. Pharmacological enrichment of polygenic for precision medicine... risk [https://pmc.ncbi.nlm.nih.gov/articles/PMC6972917/]
- 13. A combined polygenic score of 21293 rare and 22 common ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9995082/]
- 14. Gene-based burden scores identify rare variant associations ... [https://bmcgenomdata.biomedcentral.com/articles/10.1186/s12863-023-01155-0]
- 15. A unified framework for estimating country-specific ... [https://www.nature.com/articles/s41467-024-48938-2]
- 16. Examining the role of common variants in rare ... [https://www.nature.com/articles/s41586-024-08217-y]
- 17. in routine genetic diagnostics: what lies ahead? Polygenic risk scores [https://link.springer.com/article/10.1007/s12687-025-00835-x]
- 18. AI identifies key gene sets that cause complex disease [https://news.northwestern.edu/stories/2025/06/ai-identifies-key-gene-sets-that-cause-complex-disease]
- 19. Population-level comparisons of gene regulatory networks ... [https://www.nature.com/articles/s43588-024-00597-5]
- 20. Population-level comparisons of gene regulatory networks ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10965443/]
- 21. Recent advances in deep learning for protein-protein interaction [https://pmc.ncbi.nlm.nih.gov/articles/PMC12168265/]
- 22. Genetic analyses of eight complex diseases using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12461582/]
- 23. Comparing gene-gene co-expression network approaches ... [https://www.sciencedirect.com/science/article/pii/S2001037025001990]
- 24. Mutation bias alters the distribution of fitness effects of mutations [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3003282]
- 25. The distribution of deleterious genetic variation in human ... [https://www.sciencedirect.com/science/article/abs/pii/S0959437X14001002]
- 26. The distribution of highly deleterious variants across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12130832/]
- 27. Quantitative analysis of relationship between mutation rate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11975134/]
- 28. A systematic evaluation of protein mutation effect predictors ... [https://www.sciencedirect.com/science/article/pii/S2211383525001650]
- 29. Accurate predictions of protein mutational effects ... [https://www.nature.com/articles/s42004-025-01771-0]
- 30. Few shot learning for phenotype-driven diagnosis of ... [https://www.nature.com/articles/s41746-025-01749-1]
- 31. Mutation-selection-drift balance models of complex diseases [https://pubmed.ncbi.nlm.nih.gov/41073879/]
- 32. The Impact of Evolutionary Driving Forces on Human Complex ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4904122/]
- 33. Insights from Evolutionary Genetics Quantitative [https://www.numberanalytics.com/blog/evolutionary-insights-quantitative-genetics]
- 34. DISEASES Curated Gene-Disease Association Evidence ... [https://maayanlab.cloud/Harmonizome/dataset/DISEASES+Curated+Gene-Disease+Association+Evidence+Scores+2025]
- 35. Evaluating empirical bounds on complex disease genetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4158716/]
- 36. Predicting the prevalence of complex genetic diseases ... [https://www.nature.com/articles/s42256-022-00604-2]
- 37. Deep mutational scanning: A versatile tool in systematically ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9878224/]
- 38. Deep Mutational Scanning in Immunology: Techniques ... [https://www.mdpi.com/2076-0817/14/10/1027]
- 39. Deep mutational scanning and massively parallel kinetics of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9667310/]
- 40. GPCards: An integrated database of genotype–phenotype ... [https://www.sciencedirect.com/science/article/pii/S2001037021000830]
- 41. Optimization of a deep mutational scanning workflow to ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10524-7]
- 42. Linking genotype to phenotype in multi-omics data of small ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-021-07867-w]
- 43. Generative prediction of causal gene sets responsible for ... [https://pubmed.ncbi.nlm.nih.gov/40504147/]
- 44. Genetic evidence for T-wave area from 12-lead ... [https://www.medrxiv.org/content/10.1101/2023.08.30.23294832v1.full-text]
- 45. RDBridge: a knowledge graph of rare diseases based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10368801/]
- 46. Few shot learning for phenotype-driven diagnosis of patients ... [https://pubmed.ncbi.nlm.nih.gov/40542121/]
- 47. Few Shot Learning for Phenotype-Driven Diagnosis of ... [https://zitniklab.hms.harvard.edu/projects/SHEPHERD/]
- 48. and Phenotypic data genotypic and exploration through... integration [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/1471-2105-10-S12-S5]
- 49. Identifying genotype-phenotype relationships in biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5719522/]
- 50. Few shot learning for phenotype-driven diagnosis of ... [https://www.medrxiv.org/content/10.1101/2022.12.07.22283238v2]
- 51. PhenoDP: leveraging deep learning for phenotype-based ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01496-8]
- 52. Knowledge Graph Sparsification for GNN-based Rare ... [https://arxiv.org/abs/2510.08655]
- 53. Few shot learning for phenotype-driven diagnosis of ... [https://github.com/mims-harvard/SHEPHERD]
- 54. The multiplex network of human diseases [https://www.nature.com/articles/s41540-019-0092-5]
- 55. A genotype-to-drug diffusion model for generation of ... [https://www.nature.com/articles/s41467-025-60763-9]
- 56. Identification of novel therapeutics for complex diseases from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4101352/]
- 57. Knowledge Graphs for Drug Discovery and Target ID [https://www.zeclinics.com/blog/knowledge-graphs-for-drug-discovery-transforming-target-identification-and-biomedical-data-integration]
- 58. Search and visualization of gene-drug-disease interactions for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9042200/]
- 59. Gene Therapy: Next Generation Treatment Options for ... [https://www.delveinsight.com/blog/gene-therapy-to-treat-complex-diseases]
- 60. Phenotype–Genotype Integrator (PheGenI) [https://www.nature.com/articles/ejhg201396]
- 61. Database tools in genetic diseases research [https://www.sciencedirect.com/science/article/pii/S0888754312002091]
- 62. PheGenI: Phenotype-Genotype Integrator - NCBI - NIH [https://www.ncbi.nlm.nih.gov/gap/phegeni]
- 63. PhenoScanner | Datasets2Tools [https://maayanlab.cloud/datasets2tools/landing/tool/PhenoScanner]
- 64. The Database of Genotypes and Phenotypes (dbGaP ... [https://www.semanticscholar.org/paper/The-Database-of-Genotypes-and-Phenotypes-(dbGaP)-Tryka-Hao/8a51639b7df68337727d1b6deb59b0addd09129b]
- 65. PheGenI: Phenotype-Genotype Integrator - NCBI - NIH [https://www.ncbi.nlm.nih.gov/gap/PheGenI?tab=1&gene=253559]
- 66. PhenoScanner - Database Commons [https://ngdc.cncb.ac.cn/databasecommons/database/id/2015]
- 67. Genetic associations of protein-coding variants in human ... [https://www.nature.com/articles/s41586-022-04394-w]
- 68. Simulation of undiagnosed patients with novel genetic ... [https://www.nature.com/articles/s41467-023-41980-6]
- 69. Genotype to Phenotype: A Complex Problem - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4412269/]
- 70. Bridging the Gap between Genotype and Phenotype via ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2012.00227/full]
- 71. PHENSIM: Phenotype Simulator - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8224893/]
- 72. What Is the Translational Gap and How Do You Close It? [https://www.verisimlife.com/publications-blog/what-is-the-translational-gap]
- 73. Drug toxicity prediction based on genotype-phenotype ... [https://pubmed.ncbi.nlm.nih.gov/?term=Woomin%20Song%5BAuthor%5D]
- 74. Drug toxicity predicted by differences between preclinical ... [https://www.eurekalert.org/news-releases/1105039]
- 75. Genotype vs. phenotype differences | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/genotype-and-phenotype-definitions-similarities-and-differences/]
- 76. Complex Diseases: Research and Applications [http://www.nature.com/scitable/topicpage/complex-diseases-research-and-applications-748]
- 77. The translational gap: bridging basic research, clinical ... [https://www.nature.com/articles/d42473-023-00253-y]
- 78. Using the phenotype differences model to identify genetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11626128/]
- 79. Bridging the Translational Research Gap: A Successful ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3519100/]
- 80. Complex diseases meet deep phenotyping and generative AI [https://pubmed.ncbi.nlm.nih.gov/40930930/]
- 81. Predicting compound activity from phenotypic profiles and ... [https://www.nature.com/articles/s41467-023-37570-1]
- 82. The pursuit of accurate predictive models of the bioactivity of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10848664/]
- 83. How Predictive Models Empower Drug Discovery [https://www.cas.org/industries/drug-discovery/challenges/how-predictive-models-empower-drug-discovery]
- 84. Next-generation phenotyping integrated in a national ... [https://www.nature.com/articles/s41588-024-01836-1]
- 85. InceptionDTA: Predicting drug-target binding affinity with ... [https://www.sciencedirect.com/science/article/pii/S2405844025008564]
- 86. Scientific Data Visualization Software | CDD Vault [https://www.collaborativedrug.com/scientific-data-visualization-software]
- 87. How To Visualize Biological Data ? [https://medium.com/@hannahzae/how-to-visualize-biological-data-85722096f8e6]
- 88. Drug Discovery in the Age of Artificial Intelligence [https://pmc.ncbi.nlm.nih.gov/articles/PMC11594879/]
- 89. The challenge of genetic variants of uncertain clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10555957/]
- 90. Complex trait associations in rare diseases and impacts on ... [https://pubmed.ncbi.nlm.nih.gov/39294130/]
- 91. Complex trait associations in rare diseases and impacts on ... [https://www.nature.com/articles/s41467-024-52407-1]
- 92. Polygenic modifiers impact penetrance and expressivity in ... [https://www.jci.org/articles/view/191107]
- 93. Selecting variants of unknown significance through ... [https://www.nature.com/articles/s41598-019-39796-w]
- 94. 2025 Trends: Multiomics [https://www.genengnews.com/topics/omics/2025-trends-multiomics/]
- 95. Multi-Omics: Challenges and Solutions [https://bigomics.ch/blog/key-challenges-in-multi-omics-data-integration/]
- 96. Comprehensive noise reduction in single-cell data with the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570323/]
- 97. A technical review of multi-omics data integration methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC12315550/]
- 98. scMFG: a single-cell multi-omics integration method based on ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11319-0]
- 99. Flexynesis: A deep learning toolkit for bulk multi-omics data ... [https://www.nature.com/articles/s41467-025-63688-5]
- 100. Systems genetics approaches for understanding complex ... [https://elifesciences.org/articles/91004]
- 101. Replicability and generalizability in population psychiatric ... [https://www.nature.com/articles/s41386-024-01960-w]
- 102. Cross-Validation Approaches for Replicability in Psychology [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2018.01117/full]
- 103. Discovery, Replicability, and Generalizability of a Left ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11661003/]
- 104. Establishing the Replicability and Generalizability of Multi- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7740176/]
- 105. Drug toxicity prediction based on genotype-phenotype ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597050/]
- 106. Research Highlight | POSTECH Life Science [https://life.postech.ac.kr/eng/html/information/research.php?mode=view&no=240&page_num=32]
- 107. Multi-domain rule-based phenotyping algorithms enable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318046/]
- 108. Genome-wide association studies: the good, the bad and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4952840/]
- 109. Twenty years of genome-wide association studies: Health ... [https://www.nature.com/articles/s41431-025-01951-5]
- 110. Decoding genetic susceptibility to human diseases via ... [https://www.sciencedirect.com/science/article/pii/S2666979X23000885]
- 111. The advantages and limitations of trait analysis with GWAS [https://plantmethods.biomedcentral.com/articles/10.1186/1746-4811-9-29]
- 112. AI for Genomics: The 2025 Revolution [https://lifebit.ai/blog/ai-for-genomics/]
- 113. Genetic analyses of eight complex diseases using ... [https://pubmed.ncbi.nlm.nih.gov/40714005/]
- 114. Valid inference for machine learning-assisted genome-wide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11972620/]
- 115. Statistical tool reveals genetic drivers of complex human ... [https://blogs.bcm.edu/2025/08/21/from-the-labs-statistical-tool-reveals-genetic-drivers-of-complex-human-diseases-paving-the-way-for-personalized-genetic-medicine/]
- 116. The 2025 International Statistical Genetics Workshop [https://www.open-bio.org/2025/04/30/2025-04-30-Kyra-Feuer-2025-International-Statistical-Genetics-Workshop/]
- 117. Structural and functional prediction, evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10787220/]
- 118. functional validation of genetic variants - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5959958/]
- 119. Clinical utility of genomic sequencing: a measurement toolkit [https://www.nature.com/articles/s41525-020-00164-7]
- 120. Diagnostic Tests: Understanding Results, Assessing Utility, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6359896/]