Brain Size Dichotomy in Autism: A Comparative Analysis of Overgrowth and Undergrowth in Preclinical ASD Models
This review provides a comprehensive analysis of the divergent brain growth phenotypes—overgrowth and undergrowth—observed in Autism Spectrum Disorder (ASD).
Brain Size Dichotomy in Autism: A Comparative Analysis of Overgrowth and Undergrowth in Preclinical ASD Models
Abstract
This review provides a comprehensive analysis of the divergent brain growth phenotypes—overgrowth and undergrowth—observed in Autism Spectrum Disorder (ASD). Tailored for researchers and drug development professionals, it synthesizes foundational neuropathological evidence, explores the methodological landscape of animal and cellular models, addresses key challenges in model optimization, and offers a comparative validation of findings across different model systems. The article highlights how specific genetic mutations dysregulate fundamental neurodevelopmental processes, leading to distinct anatomical and behavioral outcomes. By integrating the latest research, including studies on PTEN, DYRK1A, and FXS, this analysis aims to inform the development of targeted, phenotype-specific therapeutic strategies and refine preclinical research paradigms.
The Prenatal Origins of ASD: Defining the Spectrum of Brain Growth Pathologies
Autism spectrum disorder (ASD) is a complex neurodevelopmental condition characterized by persistent deficits in social communication and interaction, as well as restricted, repetitive patterns of behavior, interests, or activities [1] [2]. Despite extensive research, the underlying neuropathological mechanisms remain incompletely understood. Postmortem brain studies and advanced neuroimaging have revealed consistent patterns of early brain overgrowth and cortical disorganization that appear fundamental to ASD pathogenesis [1] [3]. This comprehensive analysis synthesizes current evidence regarding the core neuropathological hallmarks of ASD, focusing on neuron overabundance and laminar disorganization, and provides detailed methodological frameworks for their investigation.
The neurobiological basis of ASD involves atypical early brain development and connectivity, with pathological processes beginning during prenatal development [4]. Evidence indicates that the peak period for detecting the early biological basis of autism spans from prenatal life to the first three years postnatally [4]. The disorder exhibits enormous phenotypic heterogeneity, which is reflected in diverse neuroanatomical variations across individuals [4]. This review systematically compares key neuropathological findings across different methodological approaches and brain regions to establish a coherent framework for understanding ASD pathogenesis.
Core Neuropathological Hallmarks in ASD
Neuron Overabundance and Brain Overgrowth
Table 1: Regional Neuron Overabundance and Brain Overgrowth Patterns in ASD
| Brain Region | Specific Findings | Developmental Timing | Functional Correlates |
|---|---|---|---|
| Prefrontal Cortex | 67% increase in neuron number [5]; Increased cortical surface area [3] | Prenatal origin; evident by age 2 years [3] [5] | Executive dysfunction; impaired social cognition |
| Amygdala | Rapid early increases in size; greater spine density in youth [4] | Early postnatal enlargement; persists through childhood [4] | Deficits in social interaction and communication [4] |
| Temporal Lobe | Disproportionate white matter enlargement [3]; Patches of disorganization [5] | Present by age 2 years [3] | Language processing; social cognition |
| Whole Brain | Generalized cerebral cortical enlargement [3]; Increased head circumference [6] | Accelerated growth prior to age 2 [3] | Overall ASD symptom severity |
One of the most consistent neuropathological findings in ASD is early brain overgrowth (EBO), characterized by an abnormal acceleration of brain growth within the first two years of life [6]. Children with ASD show early increases in brain volume and cortical thickness during infancy and toddler years (2-4 years), followed by an accelerated rate of decline in size from adolescence to late middle age [4]. This aberrant growth pattern does not typically occur at birth but develops throughout the first 2 years of life [4].
The sites of regional overgrowth in ASD include frontal and temporal cortices and the amygdala [4]. A seminal study found that young autistic males present a very significant excess of neuron number in the dorsolateral prefrontal cortex (PFC)—approximately 67% more neurons compared to typically developing controls [5]. Since no known neurobiological mechanism in humans can generate large excesses of frontal cortical neurons during postnatal life, this magnitude of excess most probably results from dysregulation of layer formation and layer-specific neuronal differentiation at prenatal developmental stages [4].
The brain overgrowth in ASD follows a distinct gradient in the cerebrum: greatest in frontal and temporal cortices (which are most abnormally enlarged) and least in the occipital cortex [4]. Longitudinal MRI studies have demonstrated generalized cerebral cortical enlargement in individuals with ASD at both 2 and 4-5 years of age, with no increased rate of cerebral cortical growth during this interval, indicating that brain enlargement in ASD results from an increased rate of brain growth prior to age 2 [3].
Cortical Laminar Disorganization
Table 2: Characteristics of Cortical Laminar Disorganization in ASD
| Feature | Findings | Detection Method | Prevalence |
|---|---|---|---|
| Focal Patches | Abnormal laminar cytoarchitecture and cortical disorganization [5] | RNA in situ hybridization with layer-specific markers [5] | 10 of 11 children with ASD [5] |
| Affected Layers | Most evident in layers 4 and 5; no layer uniformly spared [5] | Molecular markers (CALB1, RORB, PCP4, etc.) [5] | Heterogeneous across cases |
| Affected Cell Types | Abnormalities primarily in neurons, not glia [5] | Cell-type specific markers [5] | Varies by case |
| Regional Distribution | Prefrontal and temporal cortices; spared occipital cortex [5] | Multi-region comparison [5] | Consistent across studies |
A groundbreaking discovery in ASD neuropathology is the finding of focal patches of abnormal laminar cytoarchitecture and cortical disorganization in young children with autism [5]. These patches represent localized disruptions in the precise layered organization of the cerebral cortex and are most frequently observed in prefrontal and temporal cortical regions [5].
In a detailed analysis of postmortem samples from children with ASD ages 2-15 years, researchers observed these patches in 10 of 11 children with autism compared to only 1 of 11 unaffected children [5]. The patches exhibit heterogeneity between cases with respect to the cell types that are most abnormal and the layers that are most affected, though the clearest signs of abnormal expression typically occur in layers 4 and 5 [5]. No cortical layer is uniformly spared from these disruptions [5].
Three-dimensional reconstruction of layer markers confirmed the focal geometry and size of these patches, which reflect a probable dysregulation of layer formation and layer-specific neuronal differentiation at prenatal developmental stages [5]. This disruption in the normal cytoarchitecture of the cortex likely underlies the functional impairments in information processing observed in ASD.
Figure 1: Developmental Pathway of ASD Neuropathology. This diagram illustrates the proposed sequence of events leading from initial prenatal disruptions to the manifestation of ASD behavioral symptoms, highlighting the critical developmental window and core pathological hallmarks.
Regional Specificity of Neuropathological Alterations
Prefrontal Cortex Abnormalities
The prefrontal cortex (PFC) emerges as a consistently affected region in ASD neuropathology. Beyond the marked neuron overabundance, the PFC exhibits disorganized gray and white matter with thickening in the subependymal layer and various forms of cortical dyslamination [1]. Minicolumns, representing functional structures where afferent, efferent and local connections of pyramidal projection neurons converge in the neocortex, show significant alterations in ASD [1].
Patients with ASD have been found to have smaller and more numerous minicolumns with more dispersed neurons in Brodmann's areas 9, 21, and 22 [1]. These minicolumnar abnormalities may be related to macroencephaly, abnormal connectivity, and early age of onset of ASD [1]. Differences in frontal minicolumnar growth trajectory show narrower minicolumns in the dorsal and orbital frontal cortex in ASD, changes that appear to be regionally specific as they are not present in the primary visual cortex [1].
Amygdala and Limbic System Pathology
The amygdala displays distinctive pathological changes in ASD. In typical fetal brain development, the amygdala displays structural connectivity across the cortex, particularly toward frontal and temporal lobes, by gestational week GW13 and achieves a mature structure by 8 months [4]. In ASD, the most consistent findings include:
- Rapid and early increases in the size of the right and left amygdala, which correlate positively with the extent of deficits in social interaction and communication at age 5 [4]
- Greater amygdala spine density in youths with ASD than in age-matched typically developing controls (<18 years), which decreases as they grow older—a pattern not found in typical development [4]
- Initial overabundance of amygdala neurons in young ASD subjects, followed by a reduction in all nuclei during adult years [4]
The paralaminar nucleus (PL), a unique subregion of the amygdala densely innervated by serotonergic fibers, appears particularly relevant to ASD pathology due to its role in neuronal plasticity [4].
Cerebellar and Brainstem Involvement
While less emphasized than cortical abnormalities, consistent neuropathological alterations have been reported in the cerebellum and brainstem in ASD [1]. Global brain developmental abnormalities manifest in the archicortex, cerebellum, brainstem, and other subcortical structures, with region-specific severity of neuropathology in young children with ASD [1].
The consistent presence of changes in the cerebellum revealed by neuropathologic investigations in ASD has been identified as one of the successful examples of this research approach [1]. These findings highlight that ASD neuropathology extends beyond cerebral cortex to include subcortical structures that contribute to the diverse behavioral manifestations of the condition.
Methodological Approaches for Neuropathological Investigation
Experimental Protocol: Marker-Based Phenotyping of Cortical Organization
Objective: To systematically examine neocortical architecture and identify patches of disorganization in postmortem brain tissue from individuals with ASD.
Materials and Methods:
Tissue Acquisition: Obtain fresh-frozen postmortem cortical tissue blocks (1-2 cm³) from dorsolateral prefrontal cortex, posterior superior temporal cortex, and occipital cortex (Brodmann's area 17) [5].
Marker Selection: Select cortical layer-specific molecular markers through initial screening of genes with robust, consistent, and specific expression patterns. Final markers should include:
- Layer-specific excitatory neuron markers
- Inhibitory neuron markers (GABAergic)
- Glial cell markers
- Autism candidate risk genes [5]
Tissue Processing:
- Serially cryosection tissue at 20μm thickness in a plane containing all cortical layers
- Group sections into series of 30 sections per series
- Allocate sections for in situ hybridization, Nissl staining, and future use [5]
RNA In Situ Hybridization:
- Implement automated high-throughput in situ hybridization protocols
- Process postmortem samples of young human postnatal fresh-frozen brain tissue
- Acquire whole-slide digital imaging for analysis [5]
Three-Dimensional Reconstruction:
- Use sequential section analysis to reconstruct patch geometry
- Confirm focal nature and size of disrupted areas
- Correlate with layer-specific marker expression [5]
Figure 2: Experimental Workflow for Cortical Patch Analysis. This diagram outlines the key methodological steps for identifying and characterizing patches of cortical disorganization in postmortem brain tissue, from initial tissue preparation to final statistical analysis.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for ASD Neuropathology Investigation
| Reagent Category | Specific Examples | Application/Function | Experimental Context |
|---|---|---|---|
| Layer-Specific Markers | CALB1, RORB, PCP4, PDE1A, NEFL [5] | Identify cortical layers and laminar organization | RNA in situ hybridization |
| Cell-Type Markers | GAD1 (GABAergic neurons), GFAP (astrocytes), IBA1 (microglia) [5] | Distinguish neuronal and glial populations | Cell-type specific analysis |
| Autism Risk Gene Probes | Genes from genetic studies (e.g., SHANK3, NLGN3) [1] [5] | Assess expression of ASD-associated genes | Candidate gene analysis |
| Nissl Stain | Cresyl violet, Thionin [5] | Visualize overall cytoarchitecture | General histology |
| RNA Quality Assessment | RIN (RNA Integrity Number) measurement [5] | Ensure sample quality | Quality control |
Comparative Analysis of ASD Models
Animal Models Recapitulating Neuropathological Hallmarks
Table 4: Animal Models of ASD Neuropathology
| Model Category | Specific Models | Neuropathological Features | Correlation with Human Findings |
|---|---|---|---|
| Monogenic ASD Models | NLGN3, NLGN4, NRXN1, SHANK3, MECP2, FMR1 mutants [1] | Altered dendritic spine density; synaptic defects | High for specific genetic syndromes |
| CNV Models | 15q11-13 deletion/duplication, 16p11.2 deletion/duplication [1] | Brain overgrowth/undergrowth; connectivity changes | Variable based on genetic alteration |
| Idiopathic ASD Models | BTBR inbred strain; prenatal valproate exposure [1] | Cortical disorganization; social behavior deficits | Recapitulates broader ASD phenotype |
| Environmental Models | Maternal immune activation; maternal autoantibodies [1] | Neuron overabundance; inflammatory changes | Relevant for idiopathic ASD cases |
Animal models have been instrumental in exploring the impact of genetic and non-genetic factors clinically relevant for the ASD phenotype [1]. Genetically modified models include those based on well-studied monogenic ASD genes (NLGN3, NLGN4, NRXN1, CNTNAP2, SHANK3, MECP2, FMR1, TSC1/2), emerging risk genes (CHD8, SCN2A, SYNGAP1, ARID1B, GRIN2B, DSCAM, TBR1), and copy number variants (15q11-q13 deletion, 15q13.3 microdeletion, 15q11-13 duplication, 16p11.2 deletion and duplication, 22q11.2 deletion) [1].
A common finding in several animal models of ASD is altered density of dendritic spines, with the direction of the change depending on the specific genetic modification, age and brain region [1]. This aligns with findings in human postmortem studies showing abnormalities in dendritic spine density and morphology [1].
Models of idiopathic ASD include inbred rodent strains that mimic ASD behaviors as well as models developed by environmental interventions such as prenatal exposure to sodium valproate, maternal autoantibodies, and maternal immune activation [1]. In addition to replicating some of the neuropathologic features seen in postmortem studies, these models have been particularly valuable for exploring developmental trajectories and testing potential therapeutic interventions.
Limitations and Translational Challenges
While animal models provide invaluable insights into ASD pathophysiology, important limitations must be considered:
Species differences in cortical development and organization may limit direct translation to human neuropathology [1]
Genetic heterogeneity of human ASD is difficult to fully recapitulate in animal models [1]
Behavioral manifestations in animals may not fully capture the complexity of human ASD phenotypes [1]
Developmental timelines differ significantly between humans and model organisms [1]
Postmortem neuropathologic studies with larger sample sizes representative of the various ASD risk genes and diverse clinical phenotypes are warranted to clarify putative etiopathogenic pathways further and to promote the emergence of clinically relevant diagnostic and therapeutic tools [1].
The neuropathological hallmarks of ASD—from neuron overabundance to laminar disorganization—paint a complex picture of altered brain development that begins prenatally and evolves throughout the lifespan. The consistent findings of early brain overgrowth followed by abnormal developmental trajectories, focal patches of cortical disorganization, and region-specific alterations in neuronal populations provide critical insights into the biological underpinnings of ASD.
Future research should prioritize:
Larger-scale postmortem studies with better representation of the genetic and phenotypic diversity within ASD [1]
Advanced computational approaches for integrating multi-dimensional data from molecular, cellular, and systems levels [2]
Longitudinal designs that can track neuropathological changes across development [3]
Standardized methodological frameworks to enable direct comparison across studies [5]
Understanding the neuropathological hallmarks of ASD not only advances fundamental knowledge of the condition but also creates opportunities for developing targeted interventions that address the underlying biological processes rather than merely managing symptoms. As research progresses, the integration of neuropathological findings with genetic, epigenetic, and clinical data will be essential for unraveling the complexity of autism spectrum disorder.
Autism spectrum disorder (ASD) is a highly heterogeneous neurodevelopmental condition characterized by atypical social communication and restricted, repetitive patterns of behavior, interests, or activities [7] [8]. Its complex genetic architecture involves contributions from rare monogenic variants with large effect sizes and polygenic factors comprising numerous common variants with small individual effects [9] [10]. Despite this heterogeneity, high-confidence ASD risk genes frequently converge onto shared biological pathways and cellular processes, notably chromatin remodeling, transcriptional regulation, and synaptic signaling [11] [12] [13]. Among the hundreds of genes implicated in ASD, PTEN, DYRK1A, and SHANK3 represent paradigmatic examples of pleiotropic risk genes whose haploinsufficiency impacts multiple neurodevelopmental processes. These genes illustrate the principle that distinct genetic lesions can disrupt common functional modules, thereby contributing to overlapping behavioral phenotypes associated with ASD [13] [14]. This comparative analysis examines the molecular functions, pathogenic mechanisms, and experimental approaches for studying these three high-confidence ASD risk genes, providing a framework for understanding convergent pathways in neurodevelopmental disorders.
Gene-Specific Profiles and Functional Roles
Table 1: Comparative Profile of High-Confidence ASD Risk Genes
| Feature | PTEN | DYRK1A | SHANK3 |
|---|---|---|---|
| Genomic Location | 10q23.31 | 21q22.13 | 22q13.33 |
| Protein Function | Phosphatase; PI3K/AKT/mTOR pathway regulator | Dual-specificity tyrosine-phosphorylation-regulated kinase | Postsynaptic scaffolding protein |
| Primary Domain | Tensin-like phosphatase domain | Kinase domain | Multiple domains including SH3, PDZ, and SAM |
| Biological Process | Growth suppression, synaptic plasticity, neuronal size | Transcriptional regulation, cell cycle control, neuronal differentiation | Synaptic organization, glutamate receptor anchoring, signal transduction |
| ASD Association Evidence | High confidence (SFARI Score 1) | High confidence (SFARI Score 1) | High confidence (SFARI Score 1) |
| Associated Syndromes | PTEN Hamartoma Tumor Syndrome, macrocephaly | Mental retardation, autosomal dominant 7, microcephaly | Phelan-McDermid syndrome, 22q13.3 deletion syndrome |
| Neuronal Expression Pattern | Developing and mature neurons | High in fetal brain, regulates neurogenesis | Predominantly postsynaptic density of excitatory synapses |
| Common Variant Types | Loss-of-function, missense mutations | De novo truncating mutations | De novo and inherited truncating mutations, CNV deletions |
PTEN (Phosphatase and TENsin homolog) encodes a lipid phosphatase that primarily antagonizes the PI3K/AKT/mTOR signaling pathway, serving as a critical regulator of cell growth, proliferation, and metabolic homeostasis [14] [8]. In neurons, PTEN controls soma size, dendritic arborization, and synaptic plasticity, with its haploinsufficiency leading to macrocephaly and altered neural connectivity frequently observed in ASD [8].
DYRK1A (Dual-specificity tyrosine-phosphorylation-regulated kinase 1A) belongs to the DYRK kinase family and plays multifunctional roles in neuronal development, including cell cycle control, neuronal differentiation, and synaptic function [9]. DYRK1A haploinsufficiency is strongly associated with microcephaly and intellectual disability, with the kinase functioning as a regulatory hub that phosphorylates transcription factors, splicing factors, and synaptic proteins [9].
SHANK3 (SH3 and multiple ankyrin repeat domains 3) encodes a master scaffolding protein located in the postsynaptic density of excitatory synapses, where it organizes glutamate receptors, cytoskeletal elements, and signaling molecules into functional complexes [11] [14]. As a central organizer of synaptic architecture, SHANK3 deficiency disrupts the balance between excitatory and inhibitory neurotransmission and impairs synaptic plasticity, leading to the core behavioral deficits observed in ASD and Phelan-McDermid syndrome [11] [13].
Pleiotropic Pathways and Convergent Mechanisms
Despite their distinct molecular functions, PTEN, DYRK1A, and SHANK3 converge on shared neurodevelopmental pathways. Research reveals that ASD risk genes primarily cluster into two functional categories: gene expression regulation (GER) and neuronal communication (NC) [11]. DYRK1A falls squarely within the GER group, influencing transcriptional networks and chromatin remodeling, while SHANK3 functions predominantly in the NC group, directly mediating synaptic signaling. PTEN exhibits pleiotropic influences across both categories through its regulation of the mTOR pathway, which coordinates protein synthesis with synaptic growth and function [11] [8].
A molecular network analysis examining multiple high-confidence ASD risk genes, including ADNP, KDM6B, CHD2, and MED13, revealed extensive cross-regulatory relationships and convergent targets [13]. This study demonstrated that deficiency in any of these genes impacts the expression of others, creating an interconnected regulatory network. Furthermore, these ASD risk genes commonly regulate synaptic genes such as SNAP25 and NRXN1, either through direct promoter binding or indirect mechanisms via intermediate regulators like CTNNB1 and SMARCA4 [13]. This convergence on shared downstream targets helps explain why genetically heterogeneous forms of ASD manifest similar behavioral phenotypes.
Table 2: Convergent Pathways and Cross-Regulatory Mechanisms
| Convergent Pathway | PTEN Role | DYRK1A Role | SHANK3 Role | Functional Convergence |
|---|---|---|---|---|
| Synaptic Signaling | Regulates mTOR-dependent protein synthesis at synapses | Phosphorylates synaptic proteins; modulates NMDA receptor function | Scaffolds glutamate receptors and signaling complexes | All three genes ultimately regulate synaptic plasticity and excitation/inhibition balance |
| Chromatin Remodeling | Indirect regulation via mTOR-EP300 axis | Direct phosphorylation of chromatin modifiers | Limited direct role; downstream effects on activity-dependent transcription | Convergence on transcriptional networks controlling neuronal differentiation |
| Neuronal Morphogenesis | Controls soma size, dendritic arborization via mTOR | Regulates neuronal differentiation and migration | Shapes dendritic spine structure and stability | Coordinated regulation of neuronal cytoarchitecture and connectivity |
| Cross-Regulatory Interactions | Expression modulated by DYRK1A activity | Phosphorylates transcription factors regulating PTEN expression | Transcriptional regulation by PTEN and DYRK1A targets | Forms an interconnected regulatory network with feedback loops |
The pleiotropic nature of these ASD risk genes extends to their influences on brain development trajectories. Recent evidence indicates that the polygenic architecture of ASD can be decomposed into genetically correlated factors associated with different developmental profiles [10]. One genetic factor is linked to early childhood diagnosis and lower social-communication abilities, while another factor associates with later diagnosis and increased mental health challenges in adolescence [10]. This developmental stratification of genetic risk may reflect the differential impacts of genes within neurodevelopmental networks, with some influencing early circuit formation (like SHANK3) and others affecting later maturation processes (like DYRK1A-mediated transcriptional regulation).
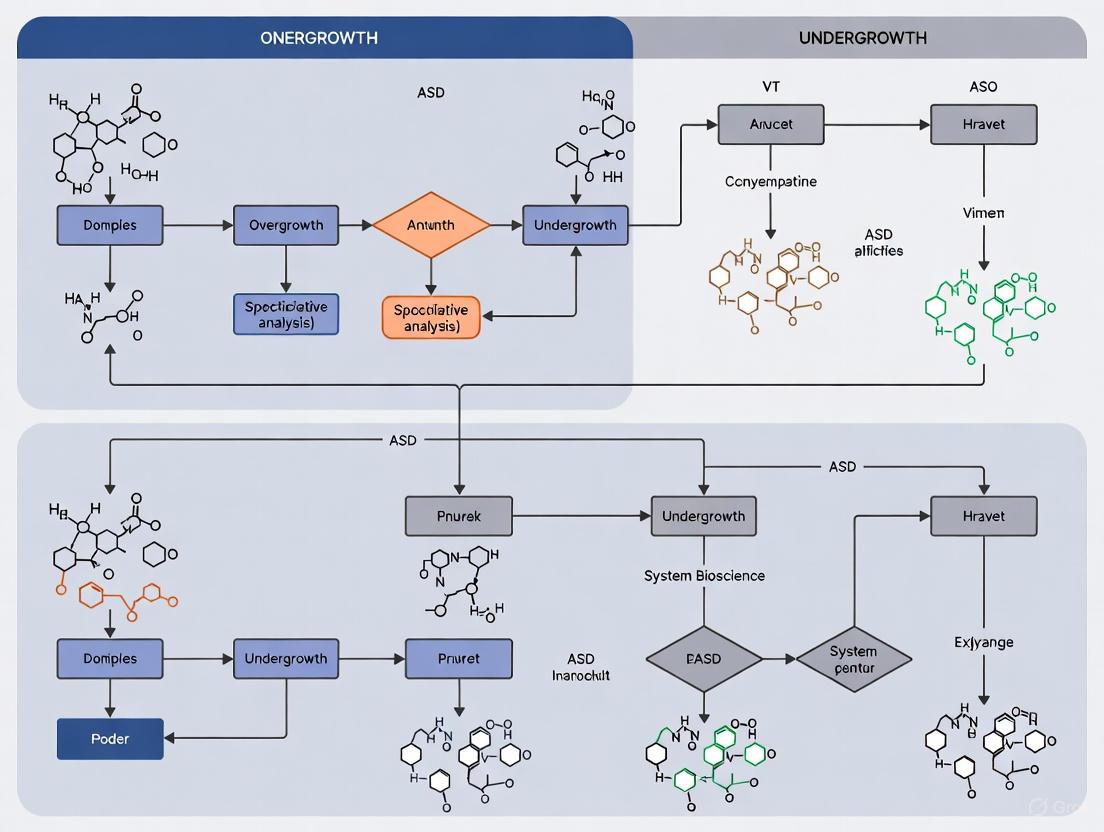
Figure 1: Pleiotropic Pathways Converging on Core ASD Phenotypes. PTEN (yellow), DYRK1A (red), and SHANK3 (green) influence overlapping neurodevelopmental processes through distinct molecular mechanisms. PTEN regulates processes via mTOR signaling; DYRK1A acts through transcription factor (TF) phosphorylation and NMDA receptor modulation; SHANK3 serves as a synaptic organizer. These convergent pathways ultimately contribute to ASD-related phenotypes (blue).
Experimental Models and Methodological Approaches
Model Systems for Functional Validation
The functional characterization of PTEN, DYRK1A, and SHANK3 has employed diverse model systems, each offering distinct advantages for probing ASD pathogenesis. Traditional animal models, particularly rodents, have been indispensable for elucidating the roles of these genes in brain development and behavior. PTEN knockout mice exhibit macrocephaly, neuronal hypertrophy, and social deficits, replicating key features of human PTEN-associated ASD [12]. Similarly, DYRK1A haploinsufficient mice show impaired cognitive function and reduced brain size, while SHANK3-deficient models display repetitive behaviors and social interaction deficits, alongside specific synaptic impairments [12].
While invaluable, animal models cannot fully recapitulate human-specific aspects of neurodevelopment, such as protracted neuronal maturation and human-specific transcriptional programs [12]. To address these limitations, human stem cell-based models have emerged as powerful complementary systems. Induced pluripotent stem cells (iPSCs) derived from patients with PTEN, DYRK1A, or SHANK3 mutations can be differentiated into 2D neuronal cultures or 3D brain organoids, providing human-specific platforms for investigating disease mechanisms and therapeutic interventions [12]. These systems allow researchers to study the impact of genetic variants during critical developmental windows and test patient-specific pharmacological responses.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating ASD Risk Genes
| Reagent Category | Specific Examples | Research Applications | Key Insights Generated |
|---|---|---|---|
| Animal Models | Pten conditional knockout mice; Dyrk1a haploinsufficient mice; Shank3 mutant mice | Behavioral phenotyping, circuit analysis, electrophysiology | Social deficits, repetitive behaviors, synaptic physiology, brain connectivity alterations |
| iPSC-Derived Models | Patient-derived iPSCs; CRISPR-corrected isogenic controls; cortical organoids | Human neuronal development, transcriptomic profiling, drug screening | Altered neuronal differentiation, transcriptional dysregulation, patient-specific therapeutic responses |
| Antibodies | Anti-PTEN phosphospecific antibodies; Anti-DYRK1A monoclonal antibodies; Anti-SHANK3 postsynaptic density markers | Protein localization, expression quantification, post-translational modifications | Subcellular distribution, expression changes in mutant models, protein-protein interactions |
| Molecular Reporters | mTOR activity biosensors; Calcium indicators (GCaMP); Synaptic markers (GFP-tagged PSD95) | Live imaging of signaling dynamics, synaptic activity, neuronal morphology | Pathway hyperactivity, altered calcium signaling, dendritic spine abnormalities |
| Gene Manipulation Tools | CRISPR-Cas9 kits; shRNA knockdown vectors; Conditional Cre-lox systems | Gene editing, functional validation, cell-type specific deletion | Causality establishment, rescue experiments, cell-autonomous versus non-autonomous effects |
Experimental Workflow for Mechanistic Studies
A standardized experimental approach for validating ASD gene function typically begins with comprehensive genetic characterization using whole-exome or whole-genome sequencing to identify pathogenic variants [11] [8]. Following variant identification, functional validation employs a multi-tiered strategy including in vitro assays in neuronal cell lines, electrophysiological assessments in primary neurons or brain slices, and behavioral characterization in animal models. For synaptic proteins like SHANK3, critical experiments include immunocytochemistry to visualize dendritic spine morphology, electrophysiology to measure miniature excitatory postsynaptic currents (mEPSCs), and analysis of protein complexes through co-immunoprecipitation [11] [13]. For regulatory proteins like DYRK1A and PTEN, transcriptomic profiling (RNA-seq) and chromatin immunoprecipitation (ChIP-seq) help identify downstream target genes and affected pathways [13].
Figure 2: Experimental Workflow for ASD Gene Validation. A multi-stage approach for characterizing ASD risk genes begins with Gene Discovery through sequencing, progresses through In Vitro and Cellular models for mechanistic studies, utilizes In Vivo systems for functional assessment, and culminates in Therapeutic development. WES: whole-exome sequencing; WGS: whole-genome sequencing.
Comparative Pathogenic Mechanisms and Therapeutic Implications
The pathogenic mechanisms of PTEN, DYRK1A, and SHANK3 highlight both shared and distinct approaches to therapeutic intervention. PTEN loss-of-function leads to constitutive activation of the mTOR pathway, suggesting potential utility for mTOR inhibitors like rapamycin in normalizing synaptic function and neuronal growth [8]. DYRK1A haploinsufficiency may be amenable to pharmacological approaches that enhance its kinase activity or modulate downstream pathways, although this strategy remains exploratory. SHANK3 deficiency represents a particular challenge, as it involves structural synaptic defects that may require early developmental intervention or gene therapy approaches [12].
Notably, these genes illustrate the complex relationship between genetic lesions and brain size in ASD. PTEN mutations typically cause macrocephaly through mTOR-mediated cellular hypertrophy, while DYRK1A mutations lead to microcephaly via impaired neurogenesis and neuronal differentiation [9] [8]. SHANK3 mutations generally do not cause dramatic changes in brain volume but specifically disrupt synaptic connectivity and function [11]. These divergent effects on neuroanatomy underscore the precision required in therapeutic targeting, as interventions must address pathway-specific perturbations.
Recent evidence also indicates that the effects of these risk genes extend beyond the formal ASD diagnosis. Carriers of pathogenic variants in high-confidence ASD genes show modest but significant decreases in fluid intelligence, educational attainment, and socioeconomic outcomes, even in the absence of diagnosis [9]. These findings emphasize the importance of studying variant effects across the entire phenotypic spectrum rather than focusing solely on categorical diagnoses, and highlight the need for supportive interventions that address broader functional impacts.
The comparative analysis of PTEN, DYRK1A, and SHANK3 reveals both the complexity and convergence of pathogenic mechanisms in ASD. While each gene has distinct molecular functions, they ultimately disrupt overlapping neurodevelopmental processes involving synaptic regulation, neuronal growth, and network formation. Understanding these convergent pathways provides a strategic framework for developing targeted interventions that may benefit multiple genetic forms of ASD. Future research directions should include comprehensive analysis of gene-gene interactions within regulatory networks, developmental stage-specific investigations of pathogenic mechanisms, and personalized therapeutic approaches based on genetic profiling and human cellular models. As our knowledge of the genetic landscape of ASD expands, comparative analyses of high-confidence risk genes will continue to illuminate shared pathogenic hubs that represent promising targets for therapeutic development.
The trajectory of brain growth in autism spectrum disorder (ASD) represents a central focus in neurodevelopmental research, with profound implications for understanding underlying mechanisms and developing targeted interventions. The scientific community is divided between two principal models: one proposing a transient phase of early brain overgrowth followed by normalization, and another suggesting persistent overgrowth that continues into later life stages. This debate is complicated by ASD's exceptional heterogeneity, with research increasingly indicating that distinct subgroups may follow unique neurodevelopmental paths. Resolving this dichotomy is critical, as each trajectory suggests different biological mechanisms, windows for intervention, and relationships with clinical outcomes.
A key stratifying factor is the presence of macrocephaly (head circumference above the 97th percentile), which affects approximately 20% of individuals with ASD and often coincides with more severe clinical symptoms [15]. This review systematically compares the evidence for transient versus persistent brain overgrowth models, synthesizing quantitative data from longitudinal neuroimaging studies, detailing the experimental methodologies that underpin this research, and exploring the molecular pathways potentially driving atypical brain growth in ASD.
Comparative Analysis of Brain Growth Trajectories
Evidence for Transient Brain Overgrowth
The transient overgrowth hypothesis posits that brain volume in ASD is near-typical at birth, undergoes a period of accelerated growth during early childhood, and then normalizes or shows reduced volume relative to typically developing peers by adolescence or adulthood. This model draws substantial support from cross-sectional and some longitudinal MRI studies.
A seminal 2025 study analyzing the Autism Brain Imaging Data Exchange (ABIDE) dataset provided compelling evidence for a dynamic developmental shift. The research, which included 301 individuals with ASD and 375 typically developing controls (TDCs) aged 8-18 years, revealed that during early adolescence, ASD participants showed positive gray matter volume (GMV) deviations relative to TDCs. This pattern reversed in late adolescence, shifting to negative GMV deviations, suggesting a trajectory from overgrowth to delayed maturation [16]. The brain regions most affected by this shift included the superior temporal sulcus, cingulate gyrus, insula, and superior parietal lobule—areas critically involved in social cognition and attention [16].
This trajectory is thought to reflect an underlying disruption in typical neurodevelopmental programming, potentially involving early overproduction of neurons and synapses followed by atypical pruning processes. Network diffusion modeling from the same study demonstrated that functional brain networks constrain how these atypical morphological patterns develop and spread across the brain over time [16].
Evidence for Persistent Brain Overgrowth
In contrast, the persistent overgrowth model contends that brain enlargement remains evident beyond early childhood into adolescence and adulthood, particularly in a subset of individuals with ASD. The Autism Phenome Project, a major longitudinal study, found that boys with ASD and disproportionate macrocephaly continued to have enlarged brains until at least 13 years of age [15]. This pattern of persistent enlargement has been documented in other studies as well, with some research showing increased brain volume in adolescents and adults with ASD [15].
A meta-analysis of 44 MRI and 27 head circumference studies concluded that while brain overgrowth and macrocephaly in ASD are most pronounced at early ages, they remain detectable across all age groups [15]. This suggests that for a significant subgroup of individuals with ASD, brain overgrowth is not a transient phenomenon but an enduring neuroanatomical feature. Neuroanatomical studies further indicate that this persistent overgrowth may affect the brain globally or may show regional specificity, with some reports highlighting disproportionate enlargement in the frontal, temporal, and parietal lobes, or specific structures like the amygdala and hippocampus [15].
Table 1: Key Evidence Supporting Transient versus Persistent Overgrowth Models
| Aspect of Evidence | Transient Overgrowth Model | Persistent Overgrowth Model |
|---|---|---|
| Developmental Trajectory | Early overgrowth followed by normalization or volume reduction | Sustained overgrowth continuing into adolescence/adulthood |
| Primary Supporting Studies | ABIDE dataset analysis (2025) [16]; Courchesne et al. studies [15] | Autism Phenome Project [15]; Hazlett et al. studies [15] |
| Age of Peak Deviation | Early childhood (before age 5) | Variable: childhood, adolescence, or persistent across lifespan |
| Macrocephaly Association | Often present in early childhood only | Typically persistent, affecting ~20% of ASD cases [15] |
| Regional Specificity | Superior temporal sulcus, cingulate gyrus, insula, superior parietal lobule [16] | Frontal, temporal, and parietal lobes; amygdala; hippocampus [15] |
Confounding Factors and Methodological Considerations
The interpretation of brain growth trajectories in ASD is complicated by several methodological factors. Cross-sectional studies, which compare different individuals at different ages, are vulnerable to sampling biases and may yield different patterns than longitudinal studies that track the same individuals over time [15]. Additionally, variations in image acquisition protocols, segmentation algorithms, and statistical controls for intracranial volume can significantly influence results [17].
Normal brain development follows complex, nonlinear trajectories characterized by early increases in cortical gray matter volume followed by post-childhood decreases, while cerebral white matter volume increases more monotonically into mid-to-late adolescence [17]. These typical patterns must be accounted for when identifying atypical trajectories in ASD.
Table 2: Longitudinal Studies of Brain Development in ASD and Typical Development
| Study / Cohort | Sample Characteristics | Key Findings on Brain Volume Trajectory |
|---|---|---|
| ABIDE Dataset Analysis [16] | 301 ASD vs. 375 TDC, aged 8-18 years | Shift from positive GMV deviations in early adolescence to negative deviations in late adolescence |
| Autism Phenome Project [15] | Longitudinal study of boys with ASD | 15% of boys with ASD had megalencephaly that persisted until at least age 13 |
| dHCP and CHILD Cohorts [18] | Infant brain MRI with follow-up at 18 months | Reduced TBV in first months associated with higher autistic traits at 18 months |
| Four Longitudinal Samples [17] | 391 participants (8-30 years), 852 scans | Typical development: CGMV peaks in childhood, decreases thereafter; CWMV increases until adolescence |
Experimental Protocols and Methodologies
Neuroimaging Acquisition and Processing Protocols
Research on brain growth trajectories in ASD relies heavily on advanced neuroimaging techniques, particularly magnetic resonance imaging (MRI). The standard experimental workflow involves meticulous image acquisition, processing, and statistical analysis tailored to account for the challenges of neurodevelopmental data.
For studies including infant participants, T1-weighted and T2-weighted MR images are typically acquired on 3.0-T scanners while infants sleep without sedation [19]. In the dHCP and CHILD cohort studies, scans were performed during the perinatal period (late fetal and early infancy) to associate brain structure with later autistic traits measured by the Quantitative Checklist for Autism in Toddlers (Q-CHAT) at 18 months [18]. Participant exclusion criteria often address potential confounds, excluding infants from multiplex pregnancies, those born very preterm, or cases with radiological scores indicating atypical patterns like white matter injury or ventricular dilatation [18].
Image processing employs specialized tools such as the Melbourne Children's Regional Infant Brain (M-CRIB) atlas, which enables accurate segmentation of infant brains in an age-appropriate way that matches parcellations used for older children and adults [20]. Processing pipelines typically involve tissue segmentation into gray matter, white matter, and cerebrospinal fluid, followed by parcellation into regions of interest. For volumetric analyses, total brain volume (TBV), cortical gray matter volume (CGMV), and cerebral white matter volume (CWMV) are common primary outcomes [17].
Analytical Approaches for Developmental Trajectories
Analyzing brain development requires specialized statistical approaches that can model nonlinear changes over time. Sliding-window approaches stratify participants by age to identify stage-specific patterns [16]. To quantify morphological differences between ASD and control groups, researchers have employed Kullback-Leibler (KL) divergence to measure distribution deviations (DEV) in gray matter volume, providing a robust metric of morphological connectivity [16].
More advanced analytical frameworks include network diffusion modeling (NDM), which simulates how morphological deviations might spread through functional networks over time. This approach has demonstrated that DEV values of atypical brain regions at preceding age stages can significantly predict subsequent ones, suggesting that intrinsic functional networks constrain anatomical development in ASD [16].
Longitudinal analyses must also carefully account for typical developmental patterns. Studies of typical development have established that intracranial volume (ICV) and whole brain volume (WBV) continue developing through adolescence, following distinct trajectories, with CGMV peaking in childhood then decreasing, while CWMV increases until mid-to-late adolescence before decelerating [17]. These normative trajectories provide essential reference points for identifying atypical development in ASD.
Molecular Mechanisms and Signaling Pathways
The macrocephalic subgroup of ASD provides a valuable model for investigating the molecular drivers of brain overgrowth. Several overlapping biological processes and signaling pathways have been implicated, affecting fundamental developmental mechanisms.
Biological Processes in Brain Overgrowth
Multiple cellular mechanisms may contribute to brain overgrowth in ASD, including:
- Excess neurogenesis: Increased production of neurons, potentially due to prolonged proliferation or symmetric division of neural progenitor cells [15]
- Decreased apoptosis: Reduced programmed cell death during development, leading to more neurons surviving than typical [15]
- Neuronal hypertrophy: Enlargement of individual neurons rather than increased cell numbers [15]
- Elevated gliogenesis: Increased production or proliferation of glial cells [15]
- Enhanced myelination: Excessive formation of myelin sheaths around neuronal axons [15]
These processes are not mutually exclusive and may occur in combination in different ASD subgroups. For example, studies of prenatal valproate (VPA) exposure models have shown reduced natural apoptosis of neural progenitor cells alongside increased neurogenesis [21].
Key Signaling Pathways
Genetic and epigenetic studies have identified several signaling pathways frequently dysregulated in macrocephalic ASD:
- PI3K-AKT-mTOR pathway: A critical regulator of cell growth, proliferation, and survival frequently hyperactivated in ASD with macrocephaly [15]
- PTEN signaling: Tumor suppressor pathway whose loss leads to mTOR activation and increased cell proliferation [15]
- WNT/β-catenin pathway: Essential for neural patterning and progenitor cell proliferation; often dysregulated in ASD [15]
- SHH signaling: Controls cerebellar development and neural tube patterning; implicated in some ASD forms [15]
These pathways form a complex regulatory network that coordinates brain growth during development, with mutations in any node potentially disrupting typical scaling mechanisms.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for ASD Brain Growth Studies
| Reagent/Material | Primary Application | Function/Utility | Example Use Cases |
|---|---|---|---|
| 3.0-T MRI Scanner | Neuroimaging acquisition | High-resolution structural imaging of brain volume | Volumetric analysis across development [19] [18] |
| M-CRIB Atlas [20] | Infant brain segmentation | Age-appropriate parcellation of infant brain regions | Longitudinal studies from infancy to adolescence |
| Doublecortin (DCX) Antibodies | Histological analysis | Marker of newly generated and immature neurons | Assessing neurogenesis in postmortem tissue [22] |
| ABIDE Dataset [16] | Large-scale analysis | Pre-existing multi-site neuroimaging data | Testing developmental trajectory models |
| Network Diffusion Modeling [16] | Computational framework | Predicts spread of morphological changes | Modeling how functional networks constrain development |
The debate between transient and persistent brain overgrowth in ASD reflects the condition's inherent heterogeneity rather than contradictory findings. Current evidence suggests that both trajectories exist in different ASD subgroups, with the macrocephalic subgroup more likely to show persistent overgrowth while other subgroups may exhibit transient enlargement or even typical brain volume throughout development.
Future research should prioritize longitudinal designs that track the same individuals from infancy through adulthood, combined with advanced genetic stratification to identify distinct biological subtypes. This approach will ultimately enable more precise mapping of brain growth trajectories to underlying molecular mechanisms and clinical outcomes, moving the field beyond one-size-fits-all models toward personalized understanding of neurodevelopment in ASD.
Autism Spectrum Disorder (ASD) represents a complex neurodevelopmental condition characterized by significant heterogeneity in both its biological underpinnings and clinical presentation. Within this heterogeneity, patterns of early physical and brain growth have emerged as potentially crucial biomarkers for identifying distinct ASD subtypes. The concept of Early Generalized Overgrowth (EGO) has gained substantial empirical support, describing a phenomenon of accelerated growth in head circumference, height, and weight within the first years of life [23] [24]. Concurrently, emerging evidence reveals a contrasting pattern of early undergrowth in a different ASD subgroup [18] [25]. This comparative analysis examines the evidence for both overgrowth and undergrowth models, their relationship to clinical severity, and the underlying molecular mechanisms. Understanding these divergent growth trajectories is fundamental for advancing precision medicine in autism research and therapeutic development.
Defining Early Generalized Overgrowth: Core Concepts and Trajectory
Early Generalized Overgrowth (EGO) in ASD is characterized by a synchronized acceleration in the development of multiple somatic measures rather than an isolated enlargement of head circumference. The trajectory follows a specific sequence: increased length/height typically emerges around 4 months of age, followed by accelerated head circumference growth between 8-10 months, and increased weight by approximately 11 months [23] [24]. This pattern suggests a generalized dysregulation of growth mechanisms affecting both neural and non-neural tissues during critical early developmental windows.
The prevalence of extreme EGO is significantly higher in boys with ASD (18.0%) compared to typically developing community controls (3.4%) [23]. This growth pattern appears specific to ASD, as other clinical comparison groups (e.g., global developmental delay) do not exhibit the same consistent overgrowth profile [26]. The phenomenon highlights the importance of investigating factors responsible for coordinated development of neural and skeletal systems in ASD, moving beyond isolated focus on brain development.
Comparative Analysis: EGO versus Early Undergrowth Models
Recent large-scale neuroimaging studies utilizing normative modeling approaches have identified at least two distinct ASD subgroups with opposing brain morphology profiles, herein referred to as the "H" (high-growth) and "L" (low-growth) subtypes [25]. The table below summarizes the key characteristics of these contrasting biological subtypes.
Table 1: Comparative Characteristics of ASD Growth Subtypes
| Feature | EGO/"H" Subtype (Overgrowth) | "L" Subtype (Undergrowth) |
|---|---|---|
| Brain Volume | Larger regional brain volumes [25] | Smaller regional brain volumes [25] |
| Postnatal Total Brain Volume | Increased [27] | Reduced [18] |
| Head Circumference | Enlarged after 9.5 months [23] [26] | Not enlarged [18] |
| Body Growth | Generalized overgrowth (height/weight) [23] | Less pronounced physical differences |
| Prevalence of Extreme Phenotype | ~18% in boys with ASD [23] | Higher abnormality rates across brain regions [25] |
| Associated Autistic Traits | More severe social deficits [23] [26] | Higher Q-CHAT scores [18] |
| Functional Outcomes | Lower adaptive functioning [23] [26] | Correlated with family history of ASD [18] |
This dichotomous presentation suggests different underlying biological mechanisms and developmental trajectories. The "L" subtype demonstrates that reduced brain volume in the first months of life associates with higher autistic trait scores on the Q-CHAT at 18 months, particularly in cohorts enriched for familial autism history [18]. This undergrowth pattern appears independent of the overgrowth trajectory, supporting the existence of multiple biological pathways to ASD.
Linking Growth Patterns to Clinical Severity and Functional Outcomes
The relationship between growth patterns and clinical outcomes represents a critical dimension for understanding the prognostic significance of these biomarkers. Children exhibiting the EGO phenotype show distinct clinical profiles, with larger body size at birth and postnatal overgrowth independently associating with poorer social, verbal, and nonverbal skills at age 4 years [23]. Those in the top 10% for physical size during infancy exhibit greater severity of social deficits and lower adaptive functioning [26].
Brain overgrowth shows particularly strong correlations with symptom severity. Children with the most severe ASD social symptoms demonstrate brains up to 41% larger than controls, with the degree of embryonic brain cortical organoid enlargement directly correlating with later social symptom severity (r = 0.719-0.873) [27]. This relationship follows a dose-response pattern where "the larger the embryonic BCO size in ASD, the more severe the toddler's social symptoms" and the more reduced the language ability and IQ [27].
Regional brain analyses further refine these associations. In the "H" subtype, the volume of the isthmus cingulate cortex directly correlates with autistic mannerisms, potentially reflecting its slower post-peak volumetric decline during typical development [25]. These findings position growth biomarkers as potentially valuable tools for predicting clinical trajectories and identifying individuals at risk for more significant support needs.
Experimental Models and Methodological Approaches
Longitudinal Growth Studies
Retrospective cohort designs using medical record data have been instrumental in establishing EGO trajectories. The typical protocol involves:
- Data Collection: Head circumference, height, and weight measurements extracted from medical records spanning birth to 24 months [23] [24]
- Participant Groups: Children with ASD compared with typically developing community controls and other developmental delay groups [26]
- Assessment Points: Longitudinal measurements at birth, 4-6 months, 8-10 months, 12 months, and 24 months [23]
- Outcome Measures: Standardized assessments of social functioning (ADOS), cognitive skills (Mullen Scales), and adaptive behavior (Vineland) at age 2-4 years [23] [26]
This approach demonstrates that boys with autism become significantly longer by age 4.8 months, develop larger head circumference by 9.5 months, and weigh more by 11.4 months compared to typically developing controls [26].
Brain Organoid Models
Human brain cortical organoids (BCOs) derived from induced pluripotent stem cells provide unprecedented insight into embryonic origins of growth abnormalities:
- Organoid Generation: BCOs created from iPSCs derived from blood samples of children with ASD and controls [27]
- Size Measurement: Analysis of 4,910 individual BCOs with approximately 196 organoids measured per subject [27]
- Growth Tracking: Size changes monitored between 1- and 2-months of organoid development [27]
- Molecular Analysis: Assessment of neurogenesis markers and Ndel1 enzyme activity [27]
This experimental system revealed that ASD organoids were 39-41% larger than controls and grew at nearly 3 times faster rates, with accelerated neurogenesis and altered Ndel1 activity [27].
Normative Modeling of Neuroimaging Data
Large-scale cross-cultural neuroimaging approaches address heterogeneity through normative modeling:
- Datasets: Combining ABIDE and China Autism Brain Imaging Consortium (CABIC) datasets [25]
- Normative References: Using Lifespan Brain Chart Consortium data for percentile-based comparisons [25]
- Statistical Clustering: Spectral clustering of Out-of-Sample centile scores to identify biological subtypes [25]
- Feature Selection: Support Vector Machines with Recursive Feature Elimination to identify key differentiating regions [25]
This method identified the two distinct neurostructural subtypes ("H" and "L") with specific regional vulnerability patterns [25].
Molecular Mechanisms: Signaling Pathways and Biomarkers
The molecular underpinnings of aberrant growth patterns in ASD involve dysregulated cellular processes during critical developmental windows. The following diagram illustrates the key signaling pathway implicated in brain overgrowth:
Diagram 1: Ndel1 Signaling Pathway in Brain Overgrowth
The enzyme Ndel1 emerges as a crucial regulator, with its activity highly correlated with brain organoid growth rate and size (r > 0.7) [27]. Altered Ndel1 function disrupts typical cell cycle regulation, leading to increased neural progenitor proliferation and accelerated neurogenesis during embryogenesis. This results in excessive neuron production and disrupted migration patterns, ultimately manifesting as macroscopic brain overgrowth and more severe clinical symptoms [27].
Table 2: Key Research Reagents and Methodologies for ASD Growth Studies
| Resource | Application | Research Utility |
|---|---|---|
| Brain Cortical Organoids | Modeling embryonic brain development [27] | Reveals prenatal origins of overgrowth; enables drug screening |
| Ndel1 Activity Assays | Quantifying enzyme function [27] | Biomarker for overgrowth risk; mechanistic studies |
| Lifespan Brain Charts | Normative neuroimaging reference [25] | Identifies deviations from typical growth trajectories |
| ddPCR/NGS Platforms | CSF ctDNA analysis [28] | Detects brain tumor-derived mutations; monitors treatment response |
| Quiet Ego Scale (QES) | Assessing psychological traits [29] | Measures coping strategies in parents of children with ASD |
| SAETBQ Questionnaire | Evaluating bias awareness [30] | Studies metacognitive aspects in ASD caregivers |
These resources enable multidimensional investigation of growth mechanisms from molecular to systems levels. The integration of biological and psychological measures is particularly valuable for understanding gene-environment interactions and family dynamics in ASD.
The compelling evidence for both EGO and undergrowth models in ASD underscores the biological heterogeneity of the condition and necessitates a precision medicine approach. Growth patterns represent quantifiable, early biomarkers that can stratify individuals into more biologically homogeneous subgroups with distinct clinical trajectories and treatment needs. Future research should prioritize:
- Prospective longitudinal studies integrating molecular, neuroimaging, and behavioral measures from infancy
- Drug development targeting specific growth pathways, particularly the Ndel1 signaling cascade
- Refined normative models incorporating genetic, environmental, and developmental factors
- Clinical translation of growth biomarkers for early identification and intervention planning
The recognition of multiple growth subtypes in ASD moves the field beyond one-size-fits-all approaches and provides a roadmap for developing targeted interventions based on individual biological profiles.
From Bench to Biomarker: Animal, Cellular, and Imaging Models in ASD Research
Autism Spectrum Disorder (ASD) represents a group of complex neurodevelopmental conditions characterized by challenges in social communication, restricted interests, and repetitive behaviors. With a global prevalence of approximately 1-3% and a pronounced male-to-female ratio of 4.2:1, ASD has emerged as a significant public health concern [15] [31] [32]. The disorder exhibits extensive clinical and genetic heterogeneity, with hundreds of identified risk genes and diverse pathological mechanisms [15] [33]. Genetically engineered mouse models have become indispensable tools for dissecting the causal relationships between genetic risk factors and the development of ASD-related behaviors and neuropathology [33] [34].
These models are particularly valuable for studying both monogenic forms of ASD, where mutations in a single gene (such as SHANK3, MECP2, or FMR1) are sufficient to cause the disorder, and syndromic forms of ASD, which occur as part of broader genetic syndromes like Fragile X syndrome or tuberous sclerosis complex [33] [34] [32]. The complex interplay between genetic susceptibility and environmental influences during critical developmental windows underscores the importance of animal models in elucidating ASD pathophysiology [35]. By providing opportunities for direct manipulation of brain regions and circuits, these models enable researchers to test precise functional hypotheses that cannot be addressed in human studies [33].
Model Validation Criteria and Genetic Landscape
Validation Frameworks for ASD Mouse Models
Animal models of psychiatric disorders are traditionally evaluated using three core validity criteria, which have been adapted for ASD research [33] [35]:
Construct Validity: Refers to how well the model recapitulates the known etiology of the disorder. For ASD models, this typically involves mimicking genetic mutations observed in human patients (e.g., mutations in SHANK3, MECP2, or TSC1/2) and their molecular consequences [33].
Face Validity: Describes the model's resemblance to clinical features of ASD, particularly core behavioral symptoms such as social interaction deficits, communication impairments, and repetitive behaviors. This may also include physiological biomarkers when available [33] [35].
Predictive Validity: Indicates the model's ability to accurately predict responses to therapeutic interventions that are effective in humans. This aspect remains challenging due to the limited number of evidence-based pharmacological treatments for core ASD symptoms [33].
Additional considerations include ethological validity (behavioral resemblance), biomarker validity (physiological resemblance), and pathogenic validity (shared disease mechanisms) [33].
Genetic Complexity of ASD
The genetic architecture of ASD encompasses several types of variations, each contributing differently to disease risk:
Table 1: Types of Genetic Variations in ASD
| Variant Type | Prevalence in ASD | Examples | Key Characteristics |
|---|---|---|---|
| Monogenic | ~50-60% of cases have genetic etiology [34] | SHANK3, MECP2, FMR1, TSC1/2 [34] [32] | Single gene mutations with large effect sizes; often associated with syndromic forms |
| Copy Number Variants (CNVs) | ~10% of non-syndromic ASD [33] | 15q13.3 deletion, 16p11.2 duplication [36] | Deletions or duplications of genomic regions containing multiple genes |
| De Novo Variants | Account for substantial fraction of sporadic cases [32] | CHD8, DYRK1A [32] | New mutations absent in parents; more common in paternal age effect |
| Common Variants | Contribute to 17-52% of ASD risk [15] [32] | Polygenic risk scores [32] | Individual small effects that cumulatively increase susceptibility |
According to the Simons Foundation Autism Research Initiative (SFARI) database, over 1,400 genes have been implicated in ASD to varying degrees of confidence, categorized as "syndromic," "high confidence," "strong candidate," or "suggestive evidence" [15] [35]. This genetic diversity is mirrored by the heterogeneity of clinical presentations, ranging from individuals with low support needs to those requiring constant care [32].
Monogenic ASD Mouse Models: Key Examples and Characteristics
Mouse models targeting specific high-confidence ASD genes have provided crucial insights into molecular and circuit mechanisms underlying autistic behaviors.
Table 2: Key Monogenic Mouse Models of ASD
| Gene Model | Molecular Function | Core Behavioral Phenotypes | Neurobiological Findings | Model Validity |
|---|---|---|---|---|
| Fmr1 KO [33] [35] | RNA-binding protein regulating synaptic protein translation | Social deficits, repetitive behaviors, anxiety [35] | Enhanced mGluR-dependent LTD, dendritic spine abnormalities | High construct and face validity [35] |
| Mecp2 KO [33] [35] | Epigenetic regulator of gene expression | Social deficits, repetitive behaviors, motor abnormalities [35] | Altered synaptic transmission, impaired cortical plasticity | High construct and face validity [35] |
| Shank3 KO [33] [35] [34] | Postsynaptic scaffolding protein | Social deficits, repetitive behaviors, anxiety [35] | Deficits in glutamate receptor function, altered spine morphology | High construct and face validity; responsive to oxytocin [35] |
| Ube3a [33] [34] | Ubiquitin ligase involved in synaptic protein degradation | ASD-like behaviors, seizures | Defects in experience-dependent synaptic plasticity | Strong construct validity |
| Pten KO [33] [34] | Phosphatase regulating PI3K/AKT/mTOR pathway | Macrocephaly, social deficits, anxiety | Neuronal hypertrophy, disrupted connectivity | High construct validity |
| Tsc1/2 KO [35] | GTPase-activating proteins regulating mTOR pathway | Social deficits, abnormal sensory responses [35] | Neuronal overgrowth, synaptic dysfunction | High predictive validity - responsive to mTOR inhibitors [35] |
| Cntnap2 KO [35] | Neuronal adhesion molecule | Hyperactivity, epileptic seizures, social deficits [35] | Cortical migration defects, reduced interneurons | High construct validity [35] |
| Nlgn3 R451C [35] | Postsynaptic cell adhesion protein | Repetitive behavior, impaired social interactions [35] | Altered inhibitory transmission, increased excitatory transmission | High construct validity [35] |
Emerging Insights from Monogenic Models
Recent studies comparing multiple monogenic models have revealed both shared and distinct circuit abnormalities. A 2025 study examining three different ASD mouse models (Tbr1+/–, Nf1+/–, and Vcp+/R95G) found that while each mutation caused unique connectivity alterations, sensory regions—particularly the piriform cortex—were consistently impaired across all models [37]. All three mutants exhibited common olfactory discrimination impairments, and manipulation of piriform cortex activity altered social behavior patterns, highlighting this region's potential role in ASD-linked circuit dysfunction [37].
Another significant advancement is the development of a comprehensive library of 63 genetically engineered mouse embryonic stem cell lines, each carrying a specific ASD-linked copy number variation (CNV) [36]. This resource enables systematic comparison of how different mutations affect neuronal development and function, revealing that diverse CNVs disrupt protein production and quality control mechanisms in neurons, particularly through mTOR and EIF4E pathways [36].
Syndromic ASD Models: Recapitulating Complex Genetic Disorders
Syndromic forms of ASD occur in the context of broader genetic syndromes where autism is one component of the clinical presentation.
Fragile X Syndrome (FMR1)
Fragile X syndrome represents the most common monogenic cause of ASD, resulting from a trinucleotide repeat expansion in the FMR1 gene that silences expression of its protein product, FMRP [33] [34]. Fmr1 knockout mice recapitulate several core features of the human syndrome, including social deficits, repetitive behaviors, and cognitive impairments [35]. At the neurobiological level, these mice exhibit enhanced metabotropic glutamate receptor (mGluR)-dependent long-term depression (LTD), dendritic spine abnormalities, and synaptic plasticity deficits [33] [35]. The strong construct and face validity of this model has facilitated preclinical testing of therapeutic strategies targeting mGluR signaling pathways [33].
Rett Syndrome (MECP2)
Rett syndrome, primarily affecting females, is caused by mutations in the X-linked MECP2 gene encoding methyl-CpG-binding protein 2, an epigenetic regulator of gene expression [33] [34]. Mecp2 knockout mice develop normally for the first few weeks of life before exhibiting progressive neurological symptoms including social withdrawal, repetitive movements, motor impairments, and breathing abnormalities reminiscent of the human disorder [33] [35]. Neuropathological findings include reduced dendritic complexity, altered synaptic transmission, and impaired cortical plasticity [33]. This model has been instrumental in establishing the critical role of MeCP2 in maintaining neuronal function after the initial period of normal development.
Tuberous Sclerosis Complex (TSC1/TSC2)
Tuberous sclerosis complex results from mutations in either TSC1 or TSC2 genes, which encode proteins that form a complex inhibiting the mTOR signaling pathway [35]. Mouse models with mutations in these genes exhibit several ASD-relevant behaviors including social deficits and abnormal responses to sensory stimuli [35]. At the cellular level, these models demonstrate neuronal overgrowth and synaptic dysfunction attributable to dysregulated mTOR signaling [35]. Importantly, these models show strong predictive validity, as treatment with mTOR inhibitors like rapamycin or everolimus ameliorates social deficits in these animals [35].
Brain Phenotypes: Overgrowth and Undergrowth in ASD Models
A notable feature of ASD is the heterogeneity in brain growth patterns, with some individuals exhibiting macrocephaly (enlarged head circumference) and others microcephaly (reduced head circumference).
Macrocephaly Models
Approximately 20% of children with ASD have macrocephaly, often corresponding with megalencephaly (brain enlargement) [15]. This subgroup typically presents with more severe symptoms, including lower IQ, delayed language onset, and increased social deficits [15]. The PTEN knockout mouse model exemplifies this phenotype, exhibiting pronounced macrocephaly due to neuronal hypertrophy and disrupted connectivity resulting from dysregulated PI3K/AKT/mTOR signaling [33] [34]. These models demonstrate that brain overgrowth can originate from various cellular mechanisms, including excess neurogenesis, decreased cell death, neuronal hypertrophy, and elevated myelination [15].
The developmental trajectory of brain overgrowth in ASD remains controversial. While some studies suggest precocious growth during early childhood followed by normalization during adolescence, longitudinal research indicates that boys with ASD and disproportionate macrocephaly may maintain enlarged brains until at least 13 years of age [15]. Neuroanatomical studies reveal both generalized overgrowth of frontal, temporal, and parietal lobes and regional specificity affecting structures like the amygdala and hippocampus [15].
Microcephaly Models
In contrast to macrocephaly models, some ASD mouse models exhibit reduced brain size. For example, certain models involving impaired synaptic function or neuronal migration demonstrate microcephaly alongside ASD-like behaviors [15]. Interestingly, a 2025 study examining perinatal brain growth and autistic traits found that reduced total brain volume in the first two months of life was associated with higher numbers of autistic traits at 18 months [38]. This suggests that early brain undergrowth, rather than overgrowth, may predict later emergence of ASD symptoms in some cases, highlighting the complex relationship between brain size and ASD phenotypes.
Experimental Approaches and Methodologies
Gene Editing Technologies
The creation of genetically engineered mouse models has been revolutionized by advances in gene editing technologies:
Gene Editing Technologies Evolution
Table 3: Gene Editing Technologies for ASD Mouse Models
| Technology | Mechanism | Advantages | Limitations |
|---|---|---|---|
| Zinc Finger Nucleases (ZFNs) [34] | Fusion of zinc finger DNA-binding domains with DNA cleavage domain | First targeted nuclease approach | High cost, complex design, off-target effects |
| Transcription Activator-Like Effector Nucleases (TALENs) [34] | Fusion of TALE DNA-binding domains with DNA cleavage domain | Improved specificity over ZFNs | Still complex and costly to design |
| CRISPR/Cas9 [34] | RNA-guided DNA endonuclease system using Cas9 protein and guide RNA | Easy design, high efficiency, cost-effective | Potential off-target effects requiring careful validation |
| Cre-loxP System [34] | Cre recombinase mediates site-specific recombination between loxP sites | Precise spatiotemporal control of gene expression | Requires generation of complex mouse lines |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for ASD Model Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Genetically Engineered Cell Lines | Library of 63 mouse embryonic stem cell lines with ASD-linked CNVs [36] | Standardized models for comparing effects of different mutations |
| Reporter Lines | Thy1-YFP transgenic mice (B6.Cg-Tg(Thy1-YFP)HJrs/J) [37] | Visualization of neuronal morphology and connectivity |
| Behavioral Assessment Tools | Three-chamber social test, ultrasonic vocalization recording, repetitive behavior assays | Quantification of ASD-relevant behaviors |
| Connectivity Mapping Platforms | BM-auto (Brain Mapping with Auto-ROI correction) [37] | AI-powered analysis of whole-brain connectivity using deep learning |
| Single-Cell Transcriptomics | Single-cell RNA sequencing (37,000+ cells in CNV study) [36] | Identification of cell-type-specific molecular alterations |
| Neural Circuit Manipulation | Chemogenetics (DREADDs), optogenetics | Testing causal relationship between circuit activity and behavior |
Signaling Pathways in Monogenic ASD Models
Multiple signaling pathways have been implicated across different monogenic ASD models, revealing potential convergent mechanisms:
Signaling Pathways in Monogenic ASD
Comparative Analysis: Strengths and Limitations Across Model Systems
While genetically engineered mouse models have significantly advanced our understanding of ASD pathophysiology, each model system presents unique advantages and limitations.
Model Organism Considerations
Mouse models offer several key advantages for ASD research, including well-established genetic manipulation techniques, relatively low maintenance costs, and rapid reproduction cycles that facilitate studies across developmental stages [33] [32]. Their mammalian brain organization shares fundamental similarities with humans, particularly in basic circuit organization and neurotransmitter systems [32]. However, significant limitations include species-specific differences in brain complexity, particularly in cortical expansion and organization, and the challenge of fully recapitulating human-specific social and cognitive behaviors [32].
Emerging Complementary Approaches
Human stem cell-based models, including 2D cultures and 3D organoids, have emerged as valuable complements to animal models by addressing some of these limitations [32]. These systems enable study of human-specific features of neuronal development and function, including protracted maturation timelines and species-specific transcriptional programs [32]. The ability to generate patient-specific cells also supports personalized therapeutic approaches [32]. However, these in vitro systems currently lack the complex circuit-level organization and sensory-motor integration present in intact organisms [32].
Genetically engineered mouse models have proven indispensable for elucidating the neurobiological mechanisms underlying monogenic and syndromic forms of ASD. The continuing refinement of these models, coupled with advanced genetic tools and analytical approaches, promises to further enhance their utility in both basic research and therapeutic development.
Future directions in the field include developing more sophisticated models that incorporate multiple genetic risk factors to better reflect the polygenic nature of most ASD cases, creating humanized models that better recapitulate human-specific aspects of brain development and function, and implementing high-throughput screening approaches to identify novel therapeutic targets across different genetic subtypes [32]. The integration of data from multiple model systems—including mouse models, stem cell-based platforms, and human clinical studies—will be essential for advancing our understanding of ASD and developing effective interventions for affected individuals.
As research progresses, the comparative analysis of overgrowth and undergrowth phenotypes across different ASD models will continue to provide valuable insights into the diverse biological pathways that can lead to similar behavioral manifestations, ultimately supporting the development of more targeted, personalized treatment approaches for this complex spectrum of disorders.
The pursuit of accurate human models for autism spectrum disorder (ASD) has led to the pivotal adoption of induced pluripotent stem cell (iPSC)-derived brain organoids. These three-dimensional structures recapitulate early human brain development, providing an unprecedented window into the embryonic pathogenesis of complex neurodevelopmental disorders [39] [40]. This comparison guide objectively evaluates the performance of brain organoid models, particularly in the context of a broader thesis on comparative analysis of overgrowth and undergrowth in ASD research. We synthesize experimental data, protocols, and reagent toolkits to inform researchers and drug development professionals.
Comparative Analysis of ASD Brain Organoid Models: Overgrowth vs. Undergrowth Phenotypes
Modeling ASD requires capturing its profound heterogeneity, including extremes in early brain development such as macrocephaly (overgrowth) and microcephaly (undergrowth). Brain organoids derived from patient iPSCs have successfully replicated key aspects of these phenotypes, offering a platform for comparative mechanistic studies [39] [41].
Modeling Early Brain Overgrowth (Macrocephaly): A seminal study using iPSCs from ASD individuals with early brain overgrowth revealed a consistent cellular phenotype: neural progenitor cells (NPCs) displayed increased proliferation [42]. This was linked to the dysregulation of a β-catenin/BRN2 transcriptional cascade. Consequently, neurons derived from these iPSCs showed abnormal neurogenesis and reduced synaptogenesis, leading to functional defects in neuronal networks. This model directly connects a prenatal cellular mechanism (excessive proliferation) to a known in vivo pathological trait (early brain overgrowth) [42] [41].
Modeling Brain Undergrowth (Microcephaly): Cerebral organoids have been effectively used to study disorders of small brain size. The protocol detailed by Lancaster et al. was applied to study microcephaly, revealing premature neuronal differentiation at the expense of the progenitor pool, effectively modeling the disease phenotype in a dish [39]. This contrasts with the overgrowth model, highlighting how organoids can capture opposing pathogenic trajectories stemming from distinct genetic disruptions.
Functional Convergence: Despite differing initial morphological phenotypes, both types of models can converge on similar functional deficits at the neuronal network level. Studies on idiopathic ASD models (not selected for brain size) consistently show impaired neuronal activity, such as reduced calcium transients, decreased synaptic connectivity, and aberrant network bursting [43]. This suggests that diverse prenatal pathogenic cascades can ultimately disrupt the functional maturation of neural circuits, a core hypothesized mechanism in ASD [41].
Table 1: Quantitative Comparison of Key Phenotypes in ASD iPSC-Derived Models
| Phenotype / Measure | Control Models | ASD Overgrowth Models | ASD Idiopathic/Functional Models | Source |
|---|---|---|---|---|
| NPC Proliferation Rate | Baseline | Significantly Increased | Varied (Not always primary readout) | [42] |
| Calcium Transient Frequency | 100% (baseline) | Data not specified | 29.8% ± 0.7% of control | [43] |
| Synaptic Network Bursting | Robust, synchronized | Reduced bursting & synaptogenesis | Impaired synchronization | [42] [43] [40] |
| Key Dysregulated Pathway | N/A | β-catenin/BRN2 cascade | miRNAs (let-7e-5p, miR-135b-5p, etc.); Synaptic signaling | [42] [43] |
| Responsiveness to IGF-1 | N/A | Improved network activity | Data not specified | [42] |
Table 2: Comparison of Organoid Protocol Methodologies
| Protocol Step | Cerebral Organoid Method [39] | Neural Rosette/NPC-Based Method [42] [44] | Primary Advantage |
|---|---|---|---|
| Starting Point | Human PSCs (ESCs/iPSCs) | Human iPSCs | Patient-specificity |
| Initial Aggregate | Embryoid Bodies (EBs) in low bFGF | Embryoid Bodies (EBs) in N2/B27 | Uniform neural induction |
| Neural Induction | Minimal media, suspension culture | Dorsomorphin (BMP inhibition), EB suspension | Dual-SMAD inhibition efficiency |
| 3D Structure Formation | Embedding in Matrigel & agitation | Often 2D rosette selection; can be reaggregated | High-throughput, easier analysis |
| Patterning | Spontaneous, minimal factors | Can be guided with specific morphogens | Region-specific control |
| Key Outcome | Heterogeneous, multiple brain regions; continuous neuroepithelium | Homogeneous populations or region-specific neurons | Protocol flexibility for question |
Detailed Experimental Protocols
This protocol emphasizes self-organization to generate organoids containing multiple brain regions.
A. Embryoid Body (EB) Formation:
- Method: Dissociate human PSCs to single cells and plate in ultra-low attachment plates in ESC medium supplemented with a low dose of bFGF (e.g., 4 ng/mL) and a ROCK inhibitor (Y-27632, 10 µM) to enhance survival.
- Duration: Culture for 5-6 days, allowing aggregate formation.
B. Neural Induction:
- Method: Transfer EBs to neural induction medium. A successful formulation is based on a minimal medium, such as DMEM/F12 supplemented with N2, non-essential amino acids, heparin, and insulin.
- Duration: Culture for 5-11 days in suspension. The neural ectoderm forms as a uniform outer layer.
C. Matrigel Embedding and Expansion:
- Method: Individually embed each neural-induced EB in a droplet of Matrigel. Plate the Matrigel-embedded constructs in a dish and allow it to solidify. Overlay with differentiation medium (e.g., Neurobasal medium with B27 supplement, vitamin A, BDNF, GDNF).
- Duration: Initial embedding takes minutes; culture statically for 3-5 days to allow neuroepithelial buds to form.
D. Agitated Culture for Long-Term Maturation:
- Method: Transfer organoids to an agitated culture system, such as a spinning bioreactor or an orbital shaker, in the same differentiation medium.
- Duration: Culture for over a month, with medium changes every 3-4 days. Organoids can be maintained for over a year for studies of late maturation.
This protocol is optimized for generating neurons for electrophysiological and calcium imaging studies.
A. iPSC Reprogramming and Maintenance:
- Method: Reprogram patient fibroblasts using non-integrating methods (e.g., Sendai virus) expressing OCT4, SOX2, KLF4, and MYC. Maintain established iPSC clones on Matrigel-coated plates in mTeSR or equivalent defined medium [42] [45].
B. Neural Induction via EB Formation and Rosette Selection:
- Method: Detach iPSC colonies and culture in suspension in N2/B27 medium supplemented with dorsomorphin (a BMP inhibitor) to promote neural fate. Form EBs for 1-2 weeks.
- Rosette Selection: Plate EBs on coated dishes. Neural rosettes will appear. Manually isolate or enzymatically dissociate and replate rosette structures to expand as NPCs in N2/B27 medium with FGF2 [42] [44].
C. Terminal Neuronal Differentiation:
- Method: Plate NPCs at high density. Withdraw FGF2 and switch to neuronal differentiation medium (e.g., Neurobasal/B27 with BDNF, ascorbic acid, cAMP). Culture for 6-8 weeks to obtain mature, functionally active neurons [43].
D. Functional Assay - Calcium Imaging:
- Method: Transduce neurons with a genetically encoded calcium indicator (e.g., GCaMP6s). Record spontaneous calcium transients using live-cell fluorescence microscopy. Analyze frequency, amplitude, and synchronicity of transients as a proxy for network activity [43].
Visualizing Signaling Pathways and Workflows
Diagram 1: iPSC Organoid Workflow and a Key ASD Pathway
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details critical reagents and their functions for establishing and analyzing iPSC-derived brain organoid models for ASD research.
Table 3: Key Research Reagent Solutions for iPSC Brain Organoid Models
| Reagent / Material | Primary Function | Key Protocol Step | Rationale & Note |
|---|---|---|---|
| Matrigel / Geltrex | Extracellular matrix (ECM) hydrogel providing structural support and signaling cues. | Organoid embedding [39]; Coating plates for iPSC/NPC culture [42] [44]. | Critical for 3D neuroepithelial bud expansion and apical-basal polarity. Batch variability is a known challenge. |
| B27 Supplement (with Vitamin A) | Serum-free supplement containing antioxidants, hormones, and vitamins. | Neuronal differentiation and long-term organoid/neuron culture medium [39] [42]. | Supports survival and maturation of post-mitotic neurons. Vitamin A (source of retinoic acid) influences later differentiation. |
| N2 Supplement | Defined supplement for serum-free culture of neural cells. | Neural induction and NPC expansion medium [42] [44]. | Provides essential components for neural progenitor survival and maintenance. |
| Dorsomorphin (DMH1) | Small molecule inhibitor of BMP type I receptors. | Neural induction (Dual-SMAD inhibition) [42] [44]. | Blocks BMP signaling, synergizing with TGF-β inhibition to robustly direct cells toward neural ectoderm fate. |
| ROCK Inhibitor (Y-27632) | Inhibitor of Rho-associated protein kinase. | Used during single-cell passaging of iPSCs and initial EB formation. | Enhances survival of dissociated pluripotent and neural cells by inhibiting apoptosis. |
| Recombinant FGF2 (bFGF) | Basic Fibroblast Growth Factor. | Maintenance of iPSCs and expansion of neural progenitor cells (NPCs). | Promotes proliferation and maintains the undifferentiated state of iPSCs and NPCs. |
| Neurobasal Medium | Optimized medium for long-term survival of mature neurons. | Base medium for neuronal differentiation and organoid maturation [39] [43]. | Contains nutrients and antioxidants that promote neuronal health and reduce glial overgrowth. |
| GCaMP6s Calcium Indicator | Genetically encoded fluorescent calcium sensor. | Functional neuronal activity assay via live-cell imaging [43]. | Allows real-time, non-invasive measurement of neuronal spiking and network synchronicity in live cultures. |
| AAV Vectors (e.g., serotype IVB-2) | Adeno-associated virus for gene delivery. | Transduction of organoids for gene expression modulation or reporter assays [40]. | Enables efficient gene delivery into 3D organoid tissues for mechanistic studies or therapy testing. |
The quest to elucidate the neuroanatomical underpinnings of autism spectrum disorder (ASD) has positioned structural magnetic resonance imaging (sMRI) and voxel-based morphometry (VBM) as pivotal technologies in neuropsychiatric research. These automated, hypothesis-free techniques enable comprehensive analysis of brain structure throughout the entire brain, offering millimeter-range resolution for detecting subtle morphological changes associated with neurodevelopmental conditions [46]. The application of these methods to ASD has been particularly challenging due to the condition's significant heterogeneity, developmental trajectory complexities, and methodological variations across studies [47] [48]. This guide provides a comparative analysis of structural MRI and VBM methodologies, their experimental implementations, and findings in ASD research, contextualized within the broader thesis of comparative analysis of overgrowth and undergrowth models in ASD.
Fundamental Principles of Voxel-Based Morphometry
Voxel-based morphometry is a fully automated computational technique that identifies regional differences in brain tissue composition through voxel-wise statistical comparison of structural MRI scans [46]. The method involves several sequential processing steps: spatial normalization of all images to a standard template, segmentation into distinct tissue classes (gray matter, white matter, cerebrospinal fluid), modulation to preserve tissue volume information, and spatial smoothing to reduce inter-subject variability and conform to Gaussian field assumptions [46] [49].
A critical methodological consideration in VBM implementation is the selection of appropriate templates and prior probability images. Evidence suggests that using study-specific custom templates and tissue priors, rather than standardized templates like the Montreal Neurological Institute (MNI) template, yields more biologically plausible results, particularly when studying populations with substantial brain morphological differences such as children or individuals with neurodevelopmental disorders [49]. The statistical analysis phase employs parametric tests across all brain voxels, with rigorous correction for multiple comparisons using family-wise error (FWE) or false discovery rate (FDR) methods to minimize Type I errors [46].
Comparative Analysis of Brain Morphometry in Autism Spectrum Disorder
Total Brain and Tissue Volume Findings
Table 1: Summary of Brain Volume Findings in Autism Spectrum Disorder
| Brain Measure | Direction of Change | Effect Size | Developmental Pattern | Key Supporting Studies |
|---|---|---|---|---|
| Total Brain Volume | Increase | ~1-2% in children >6 years; ~5-10% in children 2-4 years | Early overgrowth followed by normalization | [50] [47] |
| Gray Matter Volume | Increase | ~1-2% | Regional specificity varies with age | [50] [47] |
| White Matter Volume | Inconsistent | Variable | Possible early overgrowth | [50] [51] |
| Cerebellar Volume | Decrease | Not quantified | Consistent across age groups | [52] [48] |
| Ventricular Volume | Increase | Not quantified | May progress with age | [53] |
Research consistently demonstrates increased total brain volume (TBV) in ASD, particularly during early childhood. Between ages 2-4 years, children with ASD exhibit approximately 10% enlargement in TBV compared to typically developing peers, with this effect attenuating to approximately 1-2% in individuals aged 6 years and older [50] [47]. This pattern supports the early overgrowth model of ASD, which proposes accelerated brain growth in the first years of life followed by normalization or even reduced growth trajectories later in development [50].
Gray matter (GM) abnormalities constitute the most consistent structural finding in ASD, with volumetric increases reported across multiple studies. In a large-scale analysis of the Autism Brain Imaging Data Exchange (ABIDE) database comprising over 1100 participants, GM volume was enlarged by approximately 1-2% in ASD participants compared to typically developing controls [50]. The regional distribution of GM abnormalities appears to vary across development, with studies reporting increased volume in frontal, temporal, and parietal regions at different ages [47].
Regional Gray Matter Alterations
Table 2: Regional Gray Matter Abnormalities in Autism Spectrum Disorder
| Brain Region | Direction of Change | Functional Correlates | Developmental Specificity | Consistency Across Studies |
|---|---|---|---|---|
| Superior Temporal Gyrus | Increase/Decrease | Social cognition, auditory processing | Childhood: decrease; Adulthood: mixed | Moderate |
| Inferior Frontal Gyrus | Increase | Language processing, social interaction | Across age groups | High |
| Cerebellum | Decrease | Motor control, cognition | Across age groups | High |
| Anterior Cingulate Cortex | Increase | Social behavior, emotion regulation | Across age groups | Moderate |
| Fusiform Gyrus | Decrease | Face processing | Across age groups | Moderate |
| Amygdala | Increase/Decrease | Emotion processing, anxiety | Varies by age | Low |
| Caudate Nucleus | Increase | Repetitive behaviors, executive function | Across age groups | Moderate |
Regional GM alterations in ASD demonstrate considerable heterogeneity, though several patterns emerge from the literature. The superior temporal gyrus (STG), critical for social cognition and auditory processing, shows particular vulnerability, with studies reporting both increases and decreases in volume potentially related to developmental stage [50] [47]. Frontal regions, including the inferior frontal gyrus and medial prefrontal areas, frequently exhibit volumetric increases that correlate with social and communication impairments [51] [54].
Subcortical structures also demonstrate consistent abnormalities in ASD. The cerebellum shows volume reduction across multiple studies, particularly in vermal regions [52] [48]. The caudate nucleus is frequently enlarged, with some evidence linking this enlargement to repetitive behaviors characteristic of ASD [52]. Limbic structures such as the amygdala and hippocampus show inconsistent directional changes, possibly reflecting methodological differences or subpopulation variability within the autism spectrum [48].
Methodological Approaches and Experimental Protocols
VBM Experimental Workflow
VBM Experimental Workflow Diagram
Detailed Methodological Protocols
Image Acquisition Parameters
The foundational step in VBM analysis involves acquiring high-resolution T1-weighted volumetric MRI scans. Standard parameters include: repetition time (TR) = 4.78-20 ms, echo time (TE) = 2.02-4.6 ms, flip angle = 8°-15°, field of view (FOV) = 24-26 cm, matrix size = 240-256 × 240-256, slice thickness = 1.0-1.5 mm, yielding isotropic voxel sizes of 1.0 mm³ [47] [49]. Consistent acquisition parameters across participants within a study are critical for minimizing technical variability.
Spatial Normalization and Segmentation
Spatial normalization transforms individual brains into a standardized coordinate space to enable voxel-wise comparisons. This typically involves a 12-parameter affine transformation followed by nonlinear warping using basis functions such as discrete cosine transform [46] [49]. The creation and use of study-specific custom templates, rather than standardized templates, has been shown to produce more biologically plausible results, particularly for specialized populations like children with ASD [49].
Segmentation partitions the normalized images into distinct tissue classes (gray matter, white matter, CSF) using a modified Gaussian mixture model that incorporates prior probability maps and accounts for intensity non-uniformity [49]. The modulation step multiplies voxel values by the Jacobian determinant derived from the spatial normalization, preserving the absolute amount of tissue while accounting for volumetric changes introduced during warping [46].
Statistical Analysis and Multiple Comparison Correction
Voxel-wise statistical comparisons employ the general linear model with random field theory to control for multiple comparisons across thousands of voxels [46]. Family-wise error (FWE) correction maintains the probability of any false positives across the entire brain below 5%, while false discovery rate (FDR) correction controls the expected proportion of false positives among significant voxels [46]. Small volume correction (SVC) may be applied to restrict analyses to a priori regions of interest, increasing sensitivity in hypothesis-driven investigations [46].
Table 3: Essential Research Resources for Structural MRI and VBM Studies
| Resource Category | Specific Tools/Resources | Primary Function | Application Notes |
|---|---|---|---|
| Analysis Software | SPM, FSL, CAT12 | Image processing and statistical analysis | SPM most commonly cited; multiple version dependencies |
| Template Atlases | MNI, IXI, Custom Templates | Spatial normalization reference | Custom templates recommended for developmental populations |
| Data Repositories | ABIDE, UK Biobank, ADNI | Source of participant data | Multi-site datasets increase sample size and generalizability |
| Quality Control Tools | MRIQC, CNG | Automated quality assessment | Critical for large datasets and multi-site studies |
| Segmentation Tools | New Segment, FAST | Tissue classification | Algorithm choice affects segmentation accuracy |
| Statistical Packages | SPM Statistics, R, SPSS | Hypothesis testing | Multiple comparison correction essential |
Advanced Analytical Frameworks and Machine Learning Approaches
Subject-Level Predictive Modeling
Recent advances in machine learning have enabled a shift from group-level comparisons to subject-level prediction in ASD neuroimaging. These approaches incorporate regularized linear regression with elastic net penalty to achieve sparse solutions from high-dimensional imaging data [54]. By implementing strict case-control matching and distance-based prediction of symptom severity, these models can identify cortical features associated with individual differences in ASD manifestation [54].
Key regions identified through machine learning approaches include the cingulate (anterior and posterior) cortex, inferior parietal cortex, lateral frontal cortex, orbitofrontal cortex, temporal regions, and fusiform gyri [51] [54]. These distributed cortical regions facilitate social, language, and sensory functioning, deficits of which align with core ASD symptomatology.
Multi-Site Data Harmonization
The emergence of large-scale, multi-site neuroimaging databases such as the Autism Brain Imaging Data Exchange (ABIDE) has addressed sample size limitations that plagued earlier VBM studies [50] [51]. However, multi-site data introduces methodological challenges related to scanner variability, acquisition parameters, and participant characteristics. Computational harmonization techniques such as ComBat have been developed to remove site effects while preserving biological variability [51]. Leave-one-site-out cross-validation approaches further enhance generalizability by testing classification accuracy across independent samples [51].
Computational Analysis Framework Diagram
Genetic and Developmental Considerations
Neuroimaging genetics represents a growing frontier in ASD research, with evidence linking specific genetic variants to structural brain phenotypes. Copy number variants (CNVs) at loci including 1q21.1, 15q11.2, 16p11.2, and 22q11.2 demonstrate associations with structural brain abnormalities in ASD [53]. These CNVs typically involve dosage-sensitive genes that influence brain development through pathways regulating neuronal maturation, synaptic function, and cortical organization [53].
The developmental trajectory of brain structure in ASD follows a complex timecourse characterized by early overgrowth followed by attenuated growth or even volume reduction in later childhood and adolescence [47]. This dynamic pattern underscores the importance of considering age as a critical moderator in structural neuroimaging studies of ASD. Cross-sectional comparisons across different age cohorts (childhood: 6-12 years; adolescence: 13-18 years; adulthood: 19-30 years) reveal distinct patterns of regional gray matter abnormalities at different developmental stages [47].
Structural MRI and VBM provide powerful methodological approaches for investigating neuroanatomical correlates of ASD. The consistent observation of early brain overgrowth followed by normalized trajectories supports developmental models of ASD that emphasize aberrant growth regulation. Methodological considerations—including template selection, multiple comparison correction, and accounting for developmental effects—critically influence result interpretation. Future directions include integrating multi-modal imaging genetics, adopting subject-level predictive frameworks, and leveraging large-scale data repositories to parse the heterogeneity inherent to autism spectrum disorder.
The Auditory Brainstem Response (ABR) is an objective, non-invasive electrophysiological measure that provides a window into the integrity and timing of neural conduction along the central auditory pathways. By recording far-field potentials generated by the auditory nerve and brainstem structures in response to acoustic stimuli, ABR yields quantifiable metrics of neural synchrony and transmission speed. Its value as a functional biomarker is increasingly recognized, particularly for quantifying altered neural conduction in complex neurodevelopmental conditions such as Autism Spectrum Disorder (ASD). The application of ABR in this context is framed by a compelling theoretical model, the overgrowth-undergrowth hypothesis of ASD, which posits an atypical trajectory of brain development involving early hyperplasia followed by abnormally slowed growth [55]. This model provides a biological basis for interpreting ABR latency patterns across the lifespan, positioning ABR not merely as a hearing test but as a sensitive indicator of broader neural network efficiency.
ABR in the Context of ASD Neurodevelopmental Models
The Overgrowth-Undergrowth Hypothesis and Its Relationship to ABR
The overgrowth-undergrowth hypothesis suggests that ASD is characterized by a specific developmental trajectory: early brain overgrowth in infancy and toddlerhood is followed by a period of abnormally slow growth, leading to undergrowth relative to typical development by adulthood [55]. This pattern of aberrant growth is theorized to directly impact the neural structures responsible for generating the ABR. Prolonged ABR latencies in infancy and childhood may reflect aberrant myelination or inefficient synaptic pruning during the early overgrowth phase, which slows neural transmission [56] [55]. Conversely, the meta-analysis by Miron and colleagues found that the prolonged wave V latency observed in children with ASD shows a significant negative correlation with age and, in adulthood, can even reverse to become shorter than in neurotypical controls [55]. This shift in latency patterns across the lifespan aligns with the overgrowth-undergrowth model and underscores the critical importance of age when interpreting ABR findings in ASD research.
Etiological Heterogeneity and Functional Connectivity
ASD is characterized by immense etiological heterogeneity, with hundreds of associated genetic risk factors [12]. Research using animal models indicates that different ASD-related genetic mutations lead to diverse, often diverging, patterns of functional brain connectivity [57]. Despite this heterogeneity, a cross-etiological study of 16 different ASD mouse models revealed that the resulting connectivity alterations could be classified into a discrete set of four predominant subtypes [57]. This suggests that while the underlying causes vary, the functional consequences on neural circuitry may converge into a finite number of abnormal states. Within this framework, ABR serves as a robust, low-level metric of brainstem neural conduction that may be affected by, and therefore serve as a biomarker for, a range of these underlying network dysfunctions.
The following tables synthesize key quantitative findings from clinical and research studies, highlighting how ABR parameters, particularly wave V latency, vary across developmental stages and populations.
Table 1: Summary of ABR Wave V Latency Findings in ASD Across Age Groups
| Age Group | Wave V Latency Pattern in ASD | Standardized Mean Difference (SMD) or Key Statistic | Theoretical Interpretation | Key References |
|---|---|---|---|---|
| Infants & Children (0-18 years) | Consistent and significant prolongation | SMD = 0.6 (95% CI: 0.5–0.8); p < 0.001 [55] | Early brain overgrowth, impaired myelination, or reduced synaptic efficiency [56] [55] | Miron et al., 2015; Cohen et al., 2013 [55] |
| Adults (18+ years) | Significant shortening | SMD = -0.6 (95% CI: -1.0 to -0.2); p = 0.004 [55] | Later-life undergrowth relative to typical development [55] | Courchesne et al., 1985; Grillon et al., 1989 [55] |
| Aging & Cognition (Non-ASD) | Longer latency associated with poorer cognitive performance | Wave V Latency B = -0.101, p = 0.021 (age-adjusted) [58] | General marker of age-related decline in subcortical neural transmission speed [58] | PMC Article (2024) [58] |
Table 2: Comparison of Key ABR Parameters and Stimuli in Experimental Protocols
| Parameter | Typical Clinical/Research Application | Impact on ABR Measurement | Example from Literature |
|---|---|---|---|
| Stimulus Type | Clicks vs. LS CE-Chirps | LS CE-Chirps compensate for cochlear travel time, enhance neural synchrony, and produce longer absolute latencies (e.g., Wave V) than clicks [59] | LS CE-Chirp Wave V latency significantly longer under binaural conditions vs. monaural; no such difference with clicks [59] |
| Presentation Mode | Monaural vs. Binaural | Binaural interaction components (BIC) reflect processing in superior olivary complex; longer latencies indicate more complex binaural integration [59] | BIC latencies for waves III and V were significantly longer for LS CE-Chirp stimuli [59] |
| Stimulus Intensity | e.g., 65 dB nHL [59] | Higher intensities generally produce shorter latencies and larger amplitudes; essential for standardization in longitudinal studies. | Intensity levels in ASD infant studies range from 80-90 dB nHL [55] |
Detailed Experimental Protocols for ABR Assessment
To ensure the reproducibility and comparability of ABR data in research, particularly for longitudinal studies tracking neurodevelopmental trajectories, standardized experimental protocols are essential.
Participant Preparation and Recording Setup
- Participant State: For infant and child populations, recordings are ideally performed during natural sleep to minimize myogenic artifacts. For adults, participants are instructed to relax and recline in a comfortable position with their eyes closed [59].
- Acoustic Environment: All recordings must be conducted in a quiet, electrically shielded, or sound-attenuated booth to minimize background noise and interference.
- Electrode Montage: A standard vertical montage is used. Surface electrodes (e.g., Ag-AgCl) are placed with impedances maintained below 3-5 kΩ [59].
- Non-inverting electrode: High forehead (Fz) or vertex (Cz).
- Inverting electrodes: On the ipsilateral and contralateral mastoids (A1, A2) or earlobes.
- Ground electrode: Low forehead (Fpz) or mid-forehead.
Stimulus Presentation and Data Acquisition
- Stimulus Parameters:
- Type: Click stimuli are the historical gold standard. LS CE-Chirp stimuli are increasingly used for enhanced wave detectability, particularly for earlier waves [59].
- Polarity: Rarefaction or alternating polarity is common. Alternating polarity can help reduce stimulus artifact.
- Intensity: Presented at 65 dB nHL for neurodiagnostic purposes, though infant studies may use higher intensities (e.g., 80-90 dB nHL) [59] [55].
- Rate: A presentation rate of 21.1-32.1 clicks per second is typical. Higher rates (e.g., 51-90 Hz) can stress the auditory system and reveal more subtle neural deficits [58] [59].
- Transduction: Insert earphones (e.g., Etymotic Research ER-2) are used to deliver stimuli and minimize acoustic crossover.
- EEG Acquisition:
- Amplification and Filtering: The EEG signal is amplified and bandpass filtered, typically between 100-3000 Hz [59].
- Analysis Time: A 10-15 ms post-stimulus time window is standard for analyzing the brainstem response.
- Sweeps/Artifact Rejection: A minimum of 1,500-3,000 sweeps are averaged to resolve a clear waveform. An artifact rejection threshold (e.g., ±40 μV) is applied to exclude sweeps contaminated by high-amplitude muscle activity or movement [59].
Data Analysis and Interpretation
- Waveform Identification: Trained analysts identify the peak latencies of waves I, III, and V, and the interpeak latencies (IPLs) I-III, III-V, and I-V. Wave I is generated by the auditory nerve, wave III by the cochlear nucleus/superior olivary complex, and wave V by the lateral lemniscus/inferior colliculus.
- Binaural Interaction Component (BIC): For studies of binaural processing, the BIC is derived by subtracting the binaural ABR waveform from the sum of the right and left monaural ABR waveforms. The BIC latency is calculated by subtracting the binaural latency from the average of the monaural latencies for each wave [59].
- Statistical Comparison: Latency and amplitude measures are compared to age-matched normative data or a control group using appropriate statistical tests (e.g., t-tests, ANOVA, non-parametric equivalents for non-normal data).
Visualizing the Theoretical Model and Experimental Workflow
ABR in the Context of the ASD Overgrowth-Undergrowth Model
This diagram illustrates the theoretical relationship between the atypical neurodevelopmental trajectory in ASD and the corresponding changes in ABR wave V latency.
Standard ABR Recording and Experimental Workflow
This diagram outlines the key steps in a standard ABR recording protocol, from participant preparation to data analysis.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for ABR Studies
| Item | Function/Application in ABR Research |
|---|---|
| ABR Recording System | Integrated hardware and software platform (e.g., Eclipse by Interacoustics, Bio-Logic) for stimulus generation, EEG amplification, signal averaging, and waveform display. The core of the experimental setup. |
| Insert Earphones | Transducers (e.g., Etymotic ER-2) that deliver acoustic stimuli directly into the ear canal. Provide high fidelity, reduce stimulus artifact, and allow for masking in the contralateral ear. |
| Surface Electrodes | Disposable or reusable electrodes (e.g., Ag-AgCl) for recording scalp electrical activity. Low impedance is critical for obtaining a high signal-to-noise ratio. |
| Electrode Gel/Prep Solution | Abrasive gels and conductive pastes used to prepare the skin and lower electrode impedance at the recording sites, ensuring optimal signal quality. |
| Acoustic Booths/Sound Chambers | Shielded rooms that provide a controlled, sound-attenuated, and electromagnetically quiet environment to prevent contamination of the low-amplitude ABR signal by external noise. |
| Calibrated Sound Level Meter | Essential for verifying the precise intensity (in dB SPL or nHL) of the acoustic stimuli presented by the transducers, ensuring experimental consistency and replicability. |
Navigating Model Complexity: Challenges and Refinements in ASD Preclinical Research
Addressing Etiological and Phenotypic Heterogeneity in Model Selection and Design
Table of Contents
- The Challenge of Heterogeneity in ASD Research
- A New Framework: Data-Driven ASD Subtypes
- A Comparative Guide to Preclinical ASD Models
- Experimental Protocols for Targeted Research
- Research Reagent Solutions
- Conclusion and Future Directions
The Challenge of Heterogeneity in ASD Research
Autism Spectrum Disorder (ASD) is a quintessential example of a highly heterogeneous condition, characterized by immense diversity in both its underlying causes (etiology) and its observable characteristics (phenotype). This heterogeneity presents a significant challenge in developing accurate preclinical models, which are essential for understanding neurobiology and advancing therapeutic development. Etiologically, ASD arises from a complex interplay of genetic and environmental factors. Genetically, it is associated with rare inherited variants, de novo mutations, and polygenic risk, with each individual risk gene accounting for less than 1% of cases [32]. Phenotypically, ASD manifests across a wide spectrum, ranging from individuals with low support needs to those with profound challenges, often accompanied by co-occurring conditions such as intellectual disability, ADHD, anxiety, and epilepsy [32] [60].
This vast heterogeneity has historically led to a "one-size-fits-all" approach in modeling, where animal or cell-based models are evaluated against an overarching ASD diagnosis rather than specific biological subtypes. This approach often fails to recapitulate the full clinical picture and has been a major barrier to translation. The limitations of traditional models include their inability to fully capture human-specific features of brain development, such as protracted neuronal maturation [32]. The key to advancing the field, therefore, lies in aligning model selection and design with the newly emerging, data-driven understanding of ASD subtypes and their distinct biological pathways.
A New Framework: Data-Driven ASD Subtypes
A transformative 2025 study published in Nature Genetics has provided a robust new framework for deconstructing ASD heterogeneity. Using a person-centered computational approach on a large cohort, researchers identified four clinically and biologically distinct subtypes of autism [61] [62] [63]. This subtyping offers a critical roadmap for selecting and designing models that are fit for purpose.
The following table outlines the core characteristics of these four subtypes, which should guide hypothesis-driven model selection.
Table 1: Clinically and Biologically Distinct Subtypes of Autism
| Subtype Name | Approx. Prevalence | Core Clinical Presentation | Genetic & Biological Hallmarks |
|---|---|---|---|
| Social/Behavioral Challenges | 37% | Core social communication deficits and repetitive behaviors; co-occurring ADHD, anxiety, depression; developmental milestones typically met [61] [62]. | Highest burden of high-impact variants in neuronal genes expressed postnatally; elevated ADHD and depression polygenic scores; enrichment of mutations affecting microtubule, chromatin organization, and DNA repair pathways [61] [63]. |
| Mixed ASD with Developmental Delay | 19% | Significant developmental delays (e.g., walking, talking); features of repetitive behavior and social challenges; lower levels of co-occurring ADHD/anxiety [61] [62]. | Strong inherited genetic component; enrichment of rare inherited variations and de novo mutations; LoF mutations affect genes expressed primarily during fetal and early newborn stages; enrichment of FMRP target genes [61] [62] [63]. |
| Moderate Challenges | 34% | Core ASD behaviors present but less severe than other groups; developmental milestones typically met; minimal co-occurring psychiatric conditions [61] [62]. | Enrichment for variants in genes with lower evolutionary constraint, suggesting milder developmental impact; less enrichment for high-effect de novo mutations [61] [63]. |
| Broadly Affected | 10% | Profound and wide-ranging challenges: developmental delays, social-communication difficulties, repetitive behaviors, and co-occurring psychiatric conditions [61] [62]. | Highest proportion of damaging de novo mutations (LoF/missense); enrichment in highly constrained genes and FMRP targets; gene dysregulation spans all developmental stages and cell types; lowest IQ polygenic score [61] [62] [63]. |
This refined classification makes it clear that a single model cannot interrogate all aspects of ASD. The schematic below illustrates a strategic workflow for aligning research questions with the appropriate model systems based on this new subtyping.
A Comparative Guide to Preclinical ASD Models
Different model systems offer unique advantages and limitations. The selection must be guided by the specific biological question, the ASD subtype of interest, and the experimental requirements for throughput and translatability.
Table 2: Comparative Analysis of Preclinical ASD Models
| Model System | Key Characteristics | Ideal for Subtype(s) | Applications & Strengths | Limitations & Considerations |
|---|---|---|---|---|
| Rodent Models (e.g., Cntnap2 KO, Shank3 KO) | - Genetic manipulation to mimic specific risk genes.- Well-established behavioral assays (e.g., social interaction, repetitive behaviors) [32] [64]. | - Social/Behavioral: For studying circuit-level deficits underlying behavior and co-occurring conditions [65].- Moderate Challenges: For investigating milder genetic effects. | - In vivo analysis of neural circuits and complex behaviors.- Testing therapeutic efficacy in a whole-body system.- Ability to control genetic and environmental factors precisely. | - Cannot recapitulate human-specific brain development [32].- Limited genetic scalability; typically models monogenic contributions.- Behavioral readouts may not fully translate to human symptoms. |
| iPSC-Derived 2D Neuronal Cultures | - Patient-derived cells (e.g., fibroblasts reprogrammed to neurons).- Captures patient-specific genetic background [32] [66]. | - Mixed ASD with DD: For studying early neurodevelopmental defects.- Broadly Affected: For modeling complex genetic burden and its impact on fundamental cellular processes. | - Study patient-specific in vitro phenotypes (e.g., neuronal maturation, synaptogenesis, electrophysiology).- Platform for personalized drug screening.- Infinite source of genetically matched cells [32]. | - Lack complex brain circuitry and architecture.- Immature neuronal state may not reflect later developmental stages.- Variable differentiation efficiency can introduce noise. |
| Brain Organoids & Assembloids | - 3D self-organizing structures that mimic aspects of early human brain development and regional connectivity [32]. | - Mixed ASD with DD: For modeling fetal-stage disruptions in brain organization.- Broadly Affected: For studying pan-developmental dysregulation. | - Model human-specific cytoarchitecture and cell-cell interactions.- Study the role of glial cells and network-level activity.- Can be generated from multiple patients for cohort studies. | - High degree of variability between organoid batches.- Lack of vascularization and sensory input.- Still simplistic compared to the mature human brain. |
Experimental Protocols for Targeted Research
To ensure reproducibility and translational relevance, experimental design must be meticulous. Below are detailed protocols for two key experiments cited in the search results, reflecting the targeted approach enabled by ASD subtyping.
Protocol 1: Targeting a Neural Circuit in a Rodent Model of Autism
This protocol is based on the 2025 Stanford study that identified hyperactivity in the reticular thalamic nucleus (RTN) as a driver of autism-like behaviors and successfully reversed symptoms, providing a template for testing therapeutics for subtypes with prominent behavioral and seizure comorbidities [60] [65].
- Objective: To assess the causal role of RTN hyperactivity in autism-like behaviors and evaluate the efficacy of an repurposed anti-epileptic drug.
- Model:
Cntnap2knockout (KO) mice, a validated model exhibiting core autism-like behaviors and comorbidity with epilepsy [65]. - Methodology:
- Behavioral Phenotyping: Subject
Cntnap2KO and wild-type (WT) control mice to a standardized battery of tests: social interaction (e.g., three-chamber test), repetitive behaviors (e.g., self-grooming, marble burying), anxiety (e.g., open field test), and seizure susceptibility. - In vivo Electrophysiology: Implant microelectrodes into the RTN of freely moving mice. Record neural activity during rest and in response to sensory stimuli (e.g., light flashes, air puffs) to confirm RTN hyperactivity in the KO model.
- Pharmacological Intervention: Administer the experimental T-type calcium channel blocker Z944 (or vehicle) to
Cntnap2KO mice. This drug was selected based on its mechanism to suppress neuronal hyperactivity [65]. - DREADD Validation: Inject
Cntnap2KO mice with a viral vector expressing inhibitory DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) specifically in RTN neurons. Administer the designer drug CNO to selectively suppress RTN activity. In a separate cohort of WT mice, use excitatory DREADDs to artificially induce RTN hyperactivity. - Post-Intervention Assessment: Repeat the behavioral phenotyping and electrophysiological recordings following pharmacological and DREADD manipulations to evaluate rescue or induction of phenotypes.
- Behavioral Phenotyping: Subject
- Outcome Measures: Quantifiable changes in social approach, repetitive behavior scores, locomotor activity, and seizure thresholds, correlated with changes in RTN firing rates.
Protocol 2: Functional Validation of Genetic Hits in a Human iPSC Model
This protocol is inspired by the genetic findings of the 2025 subtyping study, which implicated de novo and inherited mutations in specific subtypes. It is ideal for modeling the "Broadly Affected" and "Mixed ASD with DD" subtypes [61] [32].
- Objective: To investigate the functional consequences of a high-confidence, loss-of-function de novo mutation in a proband from the "Broadly Affected" subtype.
- Model: iPSC lines derived from the proband and a genetically matched control (e.g., an unaffected sibling, if available).
- Methodology:
- iPSC Generation & Validation: Reprogram patient fibroblasts into iPSCs. Fully characterize the lines for pluripotency markers and karyotypic normality.
- Neuronal Differentiation: Differentiate iPSCs into cortical neurons using a standardized, dual-SMAD inhibition protocol, which directs cells toward a forebrain fate. Maintain cultures for up to 120 days to allow for neuronal maturation and synaptogenesis.
- Isogenic Control Generation: Use CRISPR-Cas9 gene editing to correct the pathogenic mutation in the patient-derived iPSC line, creating a perfect genetic control.
- Phenotypic Screening:
- Multi-electrode Array (MEA): Plate neurons on MEA chips to record network-level activity (e.g., mean firing rate, burst patterns, synchrony) over time.
- Immunocytochemistry & Imaging: Fix neurons and stain for synaptic markers (e.g., PSD-95, Synapsin), dendritic arborization (MAP2), and neuronal subtypes. Use high-content imaging for quantitative morphological analysis.
- RNA-Sequencing: Perform transcriptomic profiling on patient and isogenic control neurons to identify differentially expressed pathways (e.g., FMRP targets, synaptic pathways).
- Pharmacological Rescue: If a phenotype is identified, test candidate compounds (e.g., growth factors, small molecules) for their ability to normalize the cellular or molecular deficits.
- Outcome Measures: Significant differences in neuronal network activity, synapse density, dendritic complexity, or gene expression between patient and isogenic control lines, which can be potentially rescued by a therapeutic compound.
Research Reagent Solutions
A successful research program in this field relies on a toolkit of validated reagents and technologies. The following table details essential solutions for designing experiments that address ASD heterogeneity.
Table 3: Essential Research Reagents and Tools
| Reagent / Technology | Function & Application | Specific Examples / Notes |
|---|---|---|
| CRISPR-Cas9 Gene Editing | - Function: To introduce or correct specific pathogenic mutations in iPSCs or animal models. - Application: Generating isogenic controls for iPSC studies or creating novel genetic rodent models that reflect subtype-specific genetic findings [61]. | - Can be used to model de novo LoF variants from the "Broadly Affected" subtype or inherited variants from the "Mixed ASD with DD" subtype. |
| DREADD Technology | - Function: Chemogenetic tool for precise, reversible activation or inhibition of specific neuronal populations in vivo. - Application: Establishing causal links between circuit dysfunction (e.g., in the RTN) and behavioral phenotypes, as demonstrated in recent studies [65]. | - hM4Di (inhibitory) and hM3Dq (excitatory) DREADDs are commonly used. The ligand CNO is used for remote control of neural activity. |
| Multi-Electrode Arrays (MEA) | - Function: To record extracellular electrical activity from networks of neurons in 2D or 3D cultures. - Application: Quantifying functional phenotypes in iPSC-derived neurons, such as hyperexcitability or altered network synchronization, relevant to several ASD subtypes [32]. | - Provides a non-invasive, long-term readout of network maturation and function, ideal for longitudinal studies and drug screening. |
| Polygenic Risk Score (PRS) Algorithms | - Function: Computational tools to calculate an individual's cumulative genetic risk from common variants. - Application: Stratifying patient-derived iPSC cohorts or clinical populations based on polygenic burden, moving beyond single-gene effects [32] [63]. | - Tools like PRSice-2 are used to calculate scores. In research, this can help explain phenotypic variability within and across subtypes. |
| T-type Calcium Channel Blocker | - Function: Small molecule inhibitor that suppresses neuronal hyperactivity. - Application: A repurposed experimental drug (e.g., Z944) used to test hypotheses about neural hyperexcitability and to reverse behavioral deficits in rodent models, highlighting a potential therapeutic pathway [65]. | - Represents a promising strategy for ASD subtypes with co-occurring epilepsy or sensory hypersensitivity. |
The relationships between these core reagents, the models they are used in, and the biological insights they generate can be visualized as an iterative research cycle.
The paradigm for ASD research is shifting from seeking a unified theory to acknowledging and investigating its distinct biological narratives. The recent identification of data-driven subtypes provides an essential framework for this new era. By aligning model selection with these subtypes—choosing rodent models for postnatal circuit-level analysis of behavioral subtypes, and stem cell models for fetal-stage developmental disruptions—researchers can design more focused and clinically relevant experiments.
The integration of sophisticated tools, from CRISPR for precise genetic modeling to DREADDs and MEAs for functional analysis, empowers this targeted approach. The promising results from studies repurposing drugs like Z944 underscore the therapeutic potential of understanding specific biological mechanisms underlying different presentations of ASD [65]. Future work will involve further refining these subtypes, developing more complex multi-assembly organoid models to study connectivity, and running high-throughput drug screens on patient-derived cells stratified by their genetic and phenotypic profiles. Ultimately, embracing etiological and phenotypic heterogeneity is not a barrier but the key to unlocking precision medicine for autism.
Autism Spectrum Disorder (ASD) represents a complex set of neurodevelopmental conditions characterized by significant heterogeneity in both behavioral presentation and underlying biology. Historically understood through a behavioral lens, research has increasingly focused on identifying the neurobiological underpinnings of ASD, particularly atypical brain growth trajectories. The conventional narrative of universal "brain overgrowth" in ASD has been challenged by recent studies revealing a more complex picture encompassing both overgrowth and undergrowth patterns across different developmental windows and ASD subgroups [18] [25]. This paradigm shift acknowledges that critical periods for intervention must be calibrated to specific neurobiological profiles rather than applying a one-size-fits-all approach.
The concept of critical periods—defined as time windows where specific neural circuits are highly plastic and receptive to environmental influences—provides a crucial framework for understanding ASD development and targeting interventions [67]. During these sensitive phases, experience actively refines genetically established neural circuits, with proper synaptic pruning and network specialization depending on a precise excitatory/inhibitory (E/I) balance [67]. Disruption of this delicate balance may alter the expression or timing of critical periods across brain regions, potentially contributing to ASD phenotypes. This review synthesizes contemporary evidence on distinct brain growth trajectories in ASD, identifies associated critical periods for intervention, and delineates targeted experimental approaches for rescuing aberrant neurodevelopment.
Comparative Analysis of Brain Growth Trajectories in ASD
Evidence for Brain Undergrowth in Early Development
Contrary to the dominant overgrowth hypothesis, emerging evidence from longitudinal neuroimaging studies has identified an early brain undergrowth phenotype in specific ASD subgroups. A comprehensive analysis of two independent cohorts—the developing Human Connectome Project (dHCP) and Cambridge Human Imaging and Longitudinal Development (CHILD) study—revealed that reduced total brain volume in the first two months of life was associated with higher numbers of autistic traits at 18 months of age [18]. This negative association was observed for total brain volume, cortical grey matter volume, and white matter volume after controlling for covariates including sex, maternal age, birth weight, and post-conception age at scanning [18]. Notably, this undergrowth pattern was not apparent in prenatal assessments, suggesting a postnatal critical period where developmental trajectories diverge.
The clinical significance of these findings is substantial, as early undergrowth may represent a viable biomarker for intervention targeting. In the CHILD cohort, the association between reduced brain volume and autistic traits was particularly pronounced in infants with a first-degree relative diagnosed with ASD, indicating potential familial patterns of neurodevelopmental vulnerability [18]. Regional analyses further implicated the temporal lobe in these early alterations, highlighting a potential locus for circuit-specific interventions during critical windows of opportunity.
Established Patterns of Brain Overgrowth
In contrast to early undergrowth phenotypes, substantial evidence supports a pattern of aberrant brain overgrowth in many children with ASD, typically emerging after the first six months of life [18]. This accelerated growth trajectory is particularly evident in grey matter volume (GMV), with children diagnosed with idiopathic ASD demonstrating significantly accelerated GMV growth across nearly all brain regions of interest compared to both typically developing controls and children with Fragile X Syndrome [68]. This positioning of aberrantly accelerated growth as a key feature of idiopathic ASD in early childhood highlights the temporal specificity of critical intervention windows—what may be therapeutic for one growth phenotype could be ineffective or even detrimental for another.
The neurobiological mechanisms driving overgrowth appear distinct from those underlying undergrowth, potentially involving disrupted synaptic pruning during critical developmental periods. Research indicates that synaptic plasticity depends on adequate sleep, particularly during critical periods of brain development, and that sleep deficits frequently co-occur with plasticity impairments in ASD models [69]. This suggests that sleep-focused interventions during specific developmental windows might normalize overgrowth trajectories by restoring typical synaptic refinement processes.
Heterogeneity of Brain Morphology in ASD: Distinct Subtypes
Advanced analytical approaches have substantially advanced understanding of neuroanatomical heterogeneity in ASD. Normative modeling of brain morphology across cross-cultural cohorts has identified two distinct ASD subgroups with divergent neuroanatomical profiles [25]:
- Subgroup L: Characterized by generally smaller brain region volumes and higher rates of abnormality across multiple cortical areas.
- Subgroup H: Exhibits larger brain volumes with less pronounced deviations in specific regions.
These subgroups display clinically meaningful differences in brain-behavior relationships. For instance, in subgroup H, the regional volume of the isthmus cingulate cortex showed a direct correlation with autistic mannerisms, potentially reflecting its slower post-peak volumetric declines during development [25]. This regional specificity suggests that critical period interventions may need to target circuit-specific molecular mechanisms rather than applying global approaches.
Table 1: Distinct ASD Subgroups Based on Brain Morphology
| Subgroup | Brain Volume Pattern | Key Regional Abnormalities | Clinical Correlations |
|---|---|---|---|
| Subgroup L | Generally smaller brain region volumes | Higher rates of abnormality across multiple cortical areas | More pronounced clinical impairments |
| Subgroup H | Larger brain volumes | Less pronounced deviations in specific regions | Isthmus cingulate volume correlates with autistic mannerisms |
Critical Period Mechanisms and Intervention Timing
Excitatory/Inhibitory Balance and Critical Period Plasticity
Critical period plasticity is tightly regulated by the balance of excitatory and inhibitory (E/I) neurotransmission, with GABAergic inhibition playing a particularly crucial role in initiating and terminating windows of heightened plasticity [67]. Disruption of this E/I balance during development may significantly contribute to ASD pathophysiology by altering the expression or timing of critical periods across brain systems. Evidence from animal models indicates that specifically manipulating inhibitory circuit maturation can either prematurely open or delay critical period windows, with lasting consequences for circuit function and behavior [67].
In the visual system critical period—one of the best-characterized models—the maturation of specific inhibitory circuits triggers the opening of the plasticity window, which subsequently closes after structural consolidation of neuronal connectivity [67]. Similar mechanisms likely govern critical periods for higher-order cognitive and social functions affected in ASD. When E/I balance is disrupted through genetic or environmental mechanisms, the timing and trajectory of these critical periods may be altered, potentially leading to asynchronous development across different functional domains and brain regions.
Molecular Mechanisms and Nutritional Interventions
Specific molecular pathways during critical prenatal and early postnatal periods establish conditions for either neurotypical development or ASD emergence. Two particularly promising intervention targets include:
Folate Metabolism: Folate (vitamin B-9) serves as a crucial methyl donor needed for DNA regulation during neurodevelopment [70]. Notably, approximately 70% of children with ASD show positivity for folate receptor autoantibodies (FRAA), which inhibit folate transport across the blood-brain barrier, resulting in cerebral folate deficiency (CFD) [70]. Clinical trials demonstrate that when FRAA-positive children with ASD receive daily supplementation with reduced folate (e.g., folinic acid) over a three-month period, approximately two-thirds show improvement in communication abilities [70]. This intervention appears most effective when implemented during early developmental windows, highlighting the time-sensitive nature of folate-dependent processes.
Taurine Pathways: Taurine, a non-protein amino acid, functions as a neuroprotectant, antioxidant, and anti-inflammatory agent during development [70]. It enhances cell proliferation and neuronal development in fetal neuroprogenitor cells and reduces microglial activation—a potentially crucial mechanism given that excessive microglial activation in ASD can impair synaptic pruning, leading to abnormal dendritic spine persistence [70]. Taurine supplementation during critical periods may support typical neurogenesis and synaptic pruning processes, potentially mitigating ASD symptom severity.
Table 2: Critical Period Interventions for ASD Growth Phenotypes
| Intervention Type | Biological Target | Developmental Window | Evidence Base |
|---|---|---|---|
| Reduced Folate Supplementation | Cerebral folate deficiency (CFD) | Early postnatal (potentially extending into fetal period) | Multiple clinical trials showing communication improvement in FRAA-positive children [70] |
| Taurine Supplementation | Neurogenesis and synaptic pruning | Fetal and early postnatal critical periods | Preclinical models show increased neuronal count and synaptogenesis [70] |
| Sleep Enhancement | Synaptic pruning and plasticity | Critical periods throughout development | ASD mouse models show co-occurrence of sleep and plasticity deficits [69] |
| Circuit-Based Neuromodulation | Reticular thalamic nucleus hyperactivity | Postnatal period (potentially extending into adulthood) | Preclinical models show symptom reversal when targeting this node [60] |
Regional Critical Periods and Circuit-Specific Interventions
Different neural systems exhibit distinct critical period timelines, creating a hierarchical succession of plasticity windows across development. Primary sensory areas typically mature earlier than higher-order association cortices, suggesting that interventions targeting fundamental sensory processing might need to precede those addressing complex social-cognitive functions [67]. Research indicates that abnormal primary sensory processing is common in ASD, with potential cascading effects on higher-order integration [67].
Promisingly, recent research has identified specific neural nodes whose targeted manipulation may rescue ASD-related behaviors. Stanford researchers discovered that hyperactivity in the reticular thalamic nucleus underlies behaviors associated with ASD in mouse models [60]. By dampening activity in this region using experimental drugs and neuromodulation techniques, they reversed autism-like symptoms—from seizures to social deficits—suggesting this nucleus represents a promising intervention target [60]. The experimental seizure drug Z944 demonstrated particular efficacy in reversing behavioral deficits in the autism mouse model, highlighting the potential of repurposing existing therapeutics for critical period interventions [60].
Experimental Approaches and Methodologies
Neuroimaging and Normative Modeling
Advanced neuroimaging approaches have been instrumental in parsing heterogeneity in ASD brain development. Normative modeling of brain morphology—which compares individual brain structures to population-based references—has emerged as a powerful framework for identifying meaningful subgroups with distinct neurobiological signatures [25]. The Lifespan Brain Chart Consortium (LBCC) provides particularly robust reference models for identifying deviations from typical neurodevelopment trajectories [25].
In practice, researchers calculate Out-of-Sample (OoS) centile scores across multiple cortical regions to quantify how much an individual's brain morphology deviates from normative growth patterns [25]. Spectral clustering of these scores then identifies naturally occurring subgroups within ASD populations. This approach has successfully distinguished the previously described subgroups L and H based on their distinct morphological profiles [25]. Support Vector Machines (SVM) with Recursive Feature Elimination and Cross-Validation (RFECV) can further identify key brain regions driving subgroup classification, highlighting potential targets for circuit-specific interventions.
Diagram 1: Neuroimaging Analysis Workflow for ASD Subgroup Identification
Genetic Model Systems
Genetic animal models provide indispensable tools for investigating molecular mechanisms underlying critical period disruptions in ASD. Several well-characterized genetic lines recapitulate core aspects of ASD pathophysiology, with particular value for studying cerebellar contributions to the disorder [71]. Key models include:
- Fmr1 (Fragile X): Models fragile X syndrome, the most common monogenic cause of ASD, characterized by cerebellar Purkinje cell dysfunction and connectivity abnormalities [71].
- Mecp2 (Rett Syndrome): Captures features of Rett syndrome, demonstrating cerebellar morphological deficits and motor coordination impairments [71].
- Tsc1/2 (Tuberous Sclerosis): Models tuberous sclerosis complex, showing cerebellar pathology including Purkinje cell disruption and altered synaptic function [71].
- Nlgn3/4 (Neuroligin): Investigates synaptic abnormalities relevant to ASD, revealing cerebellar circuit dysfunction and social behavior deficits [71].
These models enable precise investigation of critical periods by allowing researchers to manipulate gene expression at specific developmental timepoints, thereby identifying when interventions might be most effective. For instance, restoring gene function during early postnatal periods often rescues phenotypic abnormalities more effectively than later interventions, highlighting the time-sensitive nature of these molecular pathways.
Behavioral Intervention Protocols
Structured behavioral interventions represent another key approach for capitalizing on critical period plasticity. Two particularly well-validated methodologies include:
Applied Behavior Analysis (ABA): Employs a "stimulus-response-reinforcement" model, breaking down skills into small steps for repetitive practice with timely rewards [72]. Typical protocols involve multiple sessions daily (e.g., 4 sessions/day, 5 days/week), with each session lasting approximately 40 minutes [72]. Skills targeted include speech, imitation, language, daily living skills, social skills, motor skills, and cognitive abilities.
Early Start Denver Model (ESDM): A developmental relationship-based approach that emphasizes naturalistic teaching within play-based interactions [72]. Standard protocols typically include 2 hours of one-on-one sessions plus 0.5 hours of group sessions daily, 5 days per week [72]. Intervention is centered on child interests and emphasizes positive affect sharing within parent-child interactions.
Both interventions have demonstrated efficacy in improving PEP-3 scores across multiple domains, including cognitive verbal/pre-verbal, expressive language, receptive language, and social reciprocity after six months of intervention [72]. The Psycho-educational Profile-Third Edition (PEP-3) provides comprehensive assessment of skills and behaviors pre- and post-intervention.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Critical Period Investigations
| Reagent/Material | Primary Research Application | Key Function in ASD Research |
|---|---|---|
| Folinic Acid | Nutritional intervention studies | Bypasses FRAA blockade to restore cerebral folate levels [70] |
| Taurine Supplements | Neuroprotection studies | Reduces oxidative stress and microglial activation; supports neurogenesis [70] |
| Z944 Experimental Drug | Circuit-based intervention studies | Calcium channel blocker targeting reticular thalamic nucleus hyperactivity [60] |
| PEP-3 Assessment | Behavioral intervention trials | Comprehensive evaluation of skills and behaviors in ASD children [72] |
| ADOS-2 Protocol | Subject characterization | Gold-standard diagnostic assessment for ASD phenotype [72] |
| Structural MRI Protocols | Neuroimaging studies | Quantifies brain volume, cortical thickness, and structural connectivity [18] [25] |
| FRAA Assay Kits | Biomarker identification | Detects folate receptor autoantibodies for patient stratification [70] |
Integrated Discussion and Future Directions
The emerging paradigm in ASD research acknowledges multiple neurodevelopmental trajectories with distinct critical periods for intervention. Rather than a unified pathophysiology, evidence supports at least two broad biological subtypes characterized by divergent growth patterns—early undergrowth versus accelerated overgrowth—each with potentially different optimal intervention windows [18] [25]. This heterogeneity demands precision medicine approaches that match interventions to individual neurobiological profiles and developmental stages.
Future research directions should prioritize:
- Longitudinal studies tracking brain growth trajectories from prenatal periods through early childhood to precisely map critical periods for different ASD subtypes.
- Circuit-specific interventions targeting nodes such as the reticular thalamic nucleus [60] or isthmus cingulate [25] with temporal precision.
- Combination approaches integrating nutritional support (e.g., reduced folate, taurine) [70] with behavioral interventions [72] during defined developmental windows.
- Cross-species validation using genetic models [71] to identify conserved molecular pathways governing critical period plasticity.
The clinical implications of this research are profound: identifying a child's specific neurodevelopmental subtype and implementing targeted interventions during the appropriate critical period could substantially improve outcomes. As research advances, the goal remains to translate these findings into personalized, time-sensitive interventions that effectively rescue aberrant growth trajectories and support optimal neurodevelopment across the autism spectrum.
Autism Spectrum Disorder (ASD) presents a profound sex bias, with males diagnosed approximately four times more frequently than females according to historical epidemiological studies [73] [74]. This consistent observation has prompted extensive investigation into its biological underpinnings, positioning ASD as a crucial model for understanding sex-differential risk in neurodevelopmental conditions. The prevailing female protective effect model hypothesizes that females possess a higher threshold for genetic liability, requiring a greater burden of risk factors to manifest the ASD phenotype [75] [74]. Concurrently, research reveals that the biological architecture of ASD encompasses opposing growth pathways—neural overgrowth and undergrowth—that may interact differently with sex-specific biological factors [76]. This review systematically compares these sex-biased manifestations through integrated analysis of molecular pathways, brain development trajectories, and clinical presentation patterns, providing a framework for researchers and drug development professionals to advance targeted diagnostic and therapeutic strategies.
Comparative Analysis of Clinical Presentation and Diagnostic Challenges
The manifestation of ASD core symptoms demonstrates significant sex differences that directly impact identification and diagnosis. While core impairments in social communication and restricted/repetitive behaviors are present across sexes, their expression often varies considerably.
Table 1: Comparative Clinical Presentation of ASD Across Sexes
| Clinical Feature | Typical Male Presentation | Typical Female Presentation |
|---|---|---|
| Social Challenges | More overt, easily observable | Often subtler; compensated via camouflaging [77] |
| Repetitive Behaviors | More pronounced and stereotyped | May be less obvious; interests can appear more "socially acceptable" [77] |
| Diagnostic Timing | Often diagnosed in early childhood | Frequently diagnosed later, sometimes not until adolescence/adulthood [77] [74] |
| Comorbidities | Often with ADHD and conduct issues | More often with internalizing conditions (anxiety, depression, eating disorders) [77] [74] |
| Cognitive Profile | Wider distribution including intellectual disability | Often without intellectual disability [74] |
Recent research utilizing the Autism Diagnostic Observation Schedule (ADOS) has revealed measurement bias in standard diagnostic instruments. Females demonstrate less impairment in specific social communication behaviors, including eye contact, response to joint attention, and quality of social overtures, even at similar levels of underlying social difficulty [78]. This measurement difference contributes to the under-identification of females, particularly those without co-occurring intellectual disabilities. The diagnostic gap narrows significantly when accounting for autistic individuals without intellectual disabilities, with sex ratios approaching 3:1 rather than the historically cited 4:1 [74]. These findings underscore the critical limitations of diagnostic frameworks developed primarily on male-presenting cases and highlight the necessity for sex-informed assessment protocols.
Neural Systems: Growth Pathways and Sexual Dimorphism
Neurobiological research reveals that ASD encompasses heterogeneous trajectories of brain development, with evidence of both neural overgrowth and undergrowth across different individuals or subgroups [76]. These divergent pathways interact with sexually dimorphic brain development, potentially explaining differential vulnerability and manifestation across sexes.
Table 2: Neural Growth Patterns in ASD and Sex Interactions
| Growth Pattern | Biological Correlates | Genetic Associations | Sex-Specific Considerations |
|---|---|---|---|
| Overgrowth | Macrocephaly, increased cortical neurons, hyperconnectivity in certain networks [76] | PTEN mutations, PI3K-AKT-mTOR pathway dysregulation [76] [79] | Male brain development may be more vulnerable to pro-growth pathway disruptions [73] |
| Undergrowth | Microcephaly, hypoconnectivity in long-range networks, reduced synaptic density [76] | DYRK1A mutations, Wnt-β-catenin pathway disruptions [76] | Female brain development may be more resilient to growth pathway perturbations [75] |
| Cortical Organization | Laminar disorganization, aberrant migration [41] | Somatic mutations in PI3K/AKT pathway [41] | Early amygdala enlargement more pronounced in males with ASD [73] |
The PTEN-PI3K-AKT-mTOR pathway represents a critically studied mechanism in ASD-related overgrowth. Research demonstrates that heterozygous mutations in PTEN (PTEN+/−) lead to brain overgrowth from birth through adulthood, driven by cellular hyperplasia and coinciding with excess neurons at birth and excess glia in adulthood [79]. This pathway interacts with β-catenin signaling, with evidence that a heterozygous mutation in Ctnnb1 (encoding β-catenin) can suppress Pten+/− cortical overgrowth [79]. The identification of these growth regulatory pathways provides a biological framework for understanding how sex-differential factors might modulate ASD vulnerability.
ASD Growth Signaling Pathways: PTEN-β-catenin interactions regulate neural development.
Gene expression analyses of human cerebral cortex tissue reveal that ASD risk genes themselves do not show systematic sex-differential expression [75]. Instead, naturally occurring sexually dimorphic processes—particularly those involving microglial and astrocyte function—appear to modulate the impact of risk variants. Genes expressed at higher levels in males are significantly enriched for those upregulated in post-mortem autistic brain, including astrocyte and microglia markers [75]. This suggests that the male brain's intrinsic molecular environment may potentiate the effects of ASD-risk genetic variants, particularly through neuron-glial interactions that differ between sexes.
Molecular Mechanisms: Genetic and Hormonal Modulators
Genetic Liability and Polygenic Architecture
Recent large-scale genetic studies provide compelling evidence for the female protective effect model. Whole-genome studies demonstrate that females with ASD carry a greater burden of common and rare genetic variants associated with the condition [75] [10]. This supports the multiple threshold liability model, which posits that a higher minimum liability is required for females to manifest the ASD phenotype [75].
Advanced polygenic profiling has revealed that the genetic architecture of ASD can be decomposed into two modestly correlated factors (rg = 0.38) with different developmental trajectories and sex interactions [10]. The first factor associates with earlier autism diagnosis and lower social/communication abilities in early childhood, showing only moderate genetic correlation with ADHD and mental health conditions. Conversely, the second factor links to later autism diagnosis and increased socioemotional/behavioral difficulties in adolescence, demonstrating moderate to high positive genetic correlations with ADHD and mental health conditions [10]. These distinct genetic profiles correspond with different developmental courses observed clinically, with implications for sex-specific vulnerability.
Hormonal Influences
The extreme male brain theory proposes that elevated prenatal testosterone exposure increases ASD risk by amplifying typically male-typical cognitive patterns characterized by stronger systemizing versus empathizing tendencies [73]. Longitudinal amniocentesis studies measuring fetal testosterone (fT) levels have found correlations with autistic traits in childhood, providing support for this theory [73]. The hormonal environment during critical prenatal periods may thus organize brain development in ways that either protect females or potentiate male vulnerability to ASD.
Beyond testosterone, research indicates that sex steroid hormones more broadly influence ASD characteristics through their modulation of gene expression networks in the developing brain [80]. These hormonal factors interact with genetic vulnerability in complex ways that remain incompletely characterized but represent promising targets for pharmacological intervention.
Experimental Models and Methodological Approaches
Key Experimental Protocols
Investigation of sex-biased mechanisms in ASD employs diverse methodological approaches across clinical, genetic, and basic research domains:
Prospective Birth Cohort Studies: Longitudinal follow-up of high-familial-likelihood infant siblings of children with ASD enables examination of developmental trajectories before diagnosis. Studies incorporate repeated behavioral assessments (e.g., Autism Diagnostic Observation Schedule), neuroimaging, and genetic analysis to identify sex-differential early markers [78] [10].
Growth Mixture Modeling of Developmental Trajectories: Statistical approach applied to longitudinal data from birth cohorts to identify latent subgroups based on socioemotional and behavioral development patterns. This method has revealed distinct trajectories associated with early versus late diagnosis [10].
Postmortem Brain Tissue Analysis: Histological examination of cortical architecture, neuron number, and laminar organization in ASD versus control brains. This approach provided foundational evidence for prenatal origins of ASD through discovery of cortical neuron excess and laminar disorganization [41].
Induced Pluripotent Stem Cell (iPSC) Models: Reprogramming of patient fibroblasts to pluripotent stem cells followed by differentiation into neural lineages enables in vitro modeling of early neurodevelopmental processes. This approach has demonstrated increased cell proliferation in iP-derived neural progenitor cells from ASD individuals with macrocephaly [41].
Moderated Nonlinear Factor Analysis (MNLFA): Advanced psychometric method to evaluate measurement invariance across sex in diagnostic instruments like the ADOS. This approach has identified specific items showing differential functioning between males and females [78].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Sex-Biased Mechanisms in ASD
| Reagent/Resource | Function/Application | Key Characteristics |
|---|---|---|
| PTEN haploinsufficient mice | Modeling ASD with macrocephaly | Exhibits brain overgrowth, social deficits; used to study PI3K-AKT-mTOR pathway [79] |
| iPSC-derived neural progenitors | In vitro modeling of early neurodevelopment | Enables study of proliferation, differentiation; preserves patient-specific genetics [41] |
| TCF/Lef:H2B-GFP reporter mice | Monitoring Wnt/β-catenin signaling | GFP expression indicates pathway activity; used to study growth regulation [79] |
| Autism Diagnostic Observation Schedule (ADOS) | Standardized diagnostic assessment | Identifies social communication deficits and RRBs; requires sex-adjusted interpretation [78] |
| Strengths and Difficulties Questionnaire (SDQ) | Behavioral screening in population cohorts | Tracks socioemotional development; identifies divergent trajectories [10] |
| RNA-seq from human cortex | Sex-differential gene expression analysis | Identifies dimorphically expressed genes and pathways in neurotypical and ASD brain [75] |
Integrated Research Approach for Studying Sex-Biased Mechanisms in ASD.
Implications for Diagnostic and Therapeutic Development
The recognition of sex-biased manifestations in ASD carries significant implications for diagnostic refinement and therapeutic innovation. Current diagnostic instruments demonstrate measurement bias that disadvantages females, necessitating development of sex-informed assessment tools that better capture the female ASD phenotype [78] [77]. The camouflaging and compensatory behaviors more frequently employed by females—including social mimicry, scripting, and masking—represent both a diagnostic challenge and a potential intervention target [77] [74].
From a therapeutic perspective, the identification of sex-differential molecular pathways suggests potential for sex-stratified treatment approaches. The prominent role of the PTEN-PI3K-AKT-mTOR pathway in growth dysregulation, particularly in cases with macrocephaly, highlights this pathway as a promising target for pharmacological intervention [79] [41]. Similarly, the involvement of β-catenin signaling in regulating brain growth trajectory suggests additional targets for modulating neural development [79]. Emerging evidence that microglial and astrocyte function differs by sex and interacts with ASD genetic risk further suggests the potential for sex-specific immunomodulatory approaches [75].
The ASD Living Biology framework—which advocates integrating in vitro prenatal models with in vivo postnatal clinical data—offers a promising approach for advancing personalized medicine in ASD [41]. This paradigm emphasizes the need to understand individual developmental trajectories from abnormal prenatal beginnings to early clinical presentation, enabling more targeted interventions based on an individual's specific growth pathway and genetic profile.
The male predominance in ASD emerges from complex interactions between sex-differential genetic liability, hormonal influences during critical developmental periods, and sexually dimorphic brain development processes. The comparative analysis of overgrowth and undergrowth models reveals distinct biological subtypes that cut across current diagnostic categories and interact differently with sex-specific factors. Future research must prioritize sex-balanced participant recruitment, development of sex-sensitive diagnostic tools, and stratified clinical trials to ensure advances benefit all individuals with ASD. The integration of dimensional approaches with categorical diagnosis, informed by greater understanding of growth pathways and their sex interactions, promises to advance both biological understanding and clinical practice for this heterogeneous condition.
The pursuit of biologically relevant in vitro models for complex neurodevelopmental disorders like Autism Spectrum Disorder (ASD) has led to the emergence of brain organoid technology. These three-dimensional, self-organizing structures derived from human pluripotent stem cells recapitulate key aspects of early human brain development, enabling researchers to study disease processes previously inaccessible in traditional models [81] [82]. A particularly promising avenue lies in correlating quantifiable organoid morphological features—especially size and growth patterns—with clinical phenotypes observed in patients, thereby creating a bridge between laboratory observations and human disease manifestations.
ASD affects approximately 1% of the global population and is characterized by significant heterogeneity in both behavioral symptoms and underlying biology [83] [84]. This heterogeneity poses substantial challenges for developing effective therapeutics. Brain organoids model ASD across molecular, cellular, and tissue levels, providing unprecedented opportunities to identify convergent biological processes despite clinical variability [81]. Notably, organoids generated from ASD patients frequently exhibit altered cell cycles and neural progenitor proliferation, leading to measurable differences in organoid size and cellular composition that may reflect in vivo neurodevelopmental trajectories [81] [85].
Quantitative Phenotypes in ASD Organoid Models
Organoid Size as a Biomarker
Multiple independent studies have consistently reported significant alterations in the physical dimensions of organoids derived from individuals with ASD compared to those from neurotypical controls. These findings suggest that organoid size may serve as a valuable quantitative biomarker reflecting underlying neurodevelopmental processes.
Table 1: Documented Size Abnormalities in ASD Organoid Models
| Study Model | Size Phenotype | Associated Clinical Feature | Biological Correlates |
|---|---|---|---|
| Idiopathic ASD Forebrain Organoids [84] | Significantly larger diameter | Not specified | Increased progenitor pool, reduced neurogenesis |
| Macrocephalic ASD Organoids [85] | Increased growth | Macrocephaly in patients | Altered balance between excitatory neurons and other lineages |
| Idiopathic ASD Cortical Organoids [85] | Size variations | Macrocephaly vs. normocephaly | Opposite disruption of cortical plate development |
Research involving forebrain organoids derived from idiopathic ASD patients revealed they were significantly larger in diameter compared to healthy control organoids [84]. This increased size was associated with pathological correlates including an expanded progenitor pool and reduced neuronal differentiation, mirroring observations from postmortem studies of ASD brains [84]. The consistency between in vitro organoid phenotypes and documented postmortem neuropathology strengthens the validity of size as a meaningful metric.
Further refining this approach, investigators have stratified ASD organoid models based on patient head size, recognizing that macrocephaly presents in a substantial subset of ASD individuals and may represent a distinct biological subtype [85]. In these studies, organoids from macrocephalic ASD probands exhibited distinct growth patterns and cellular imbalances compared to those from normocephalic individuals, suggesting that organoid size phenotypes may help resolve the heterogeneity of ASD into biologically meaningful subgroups [85].
Methodologies for Organoid Size Quantification
Accurate and consistent measurement of organoid morphological properties is fundamental to establishing robust correlations with clinical phenotypes. Several methodologies have been employed, each with distinct advantages and limitations for specific research applications.
Table 2: Organoid Size Quantification Methodologies
| Method | Throughput | Key Advantages | Principal Limitations | Best Applications |
|---|---|---|---|---|
| Manual Brightfield Microscopy [86] | Low | Accessibility, minimal equipment needs | Susceptibility to investigator fatigue and bias, ±10% size error can cause 45-90% counting error | Small-scale pilot studies |
| Confocal Microscopy [86] | Very Low | High-resolution 3D reconstruction, precise volumetric data | Time-consuming imaging and analysis, limited throughput, shared equipment access | Detailed structural studies with limited sample numbers |
| Automated Platforms (e.g., GelCount) [86] | High (12 minutes for four 6-well plates) | Elimination of observer bias, consistent thresholds, volumetric data, high reproducibility | Equipment cost, method optimization required | Large-scale screening, standardized drug testing |
Manual counting using brightfield microscopy remains common but introduces significant variability due to investigator fatigue and subjective size thresholds [86]. Notably, even a modest ±10% error in visual size estimation can propagate into dramatic counting errors ranging from +90% to -45% [86]. Confocal microscopy provides superior resolution and accurate three-dimensional reconstruction but suffers from extremely low throughput, making it impractical for large-scale studies [86].
To address these limitations, automated platforms like the GelCount system have been developed specifically for high-throughput organoid quantification [86]. These systems apply consistent thresholds across entire experiments, simultaneously capturing count, diameter, and volume data while eliminating inter-observer variability [86]. This standardization is particularly valuable for drug screening applications and longitudinal growth studies where precise size trajectories are informative.
Experimental Workflows: From Organoid Data to Clinical Insights
Standardized Protocols for Organoid Generation and Analysis
Establishing robust correlations between organoid phenotypes and clinical outcomes requires standardized experimental workflows that ensure reproducibility across batches and laboratories. The typical pipeline begins with careful patient selection and iPSC generation, followed by organoid differentiation using region-specific protocols designed to answer particular research questions [82] [85].
For ASD modeling, forebrain organoid protocols have proven particularly valuable, as they recapitulate development of brain regions most frequently implicated in ASD pathophysiology [85]. These protocols typically guide pluripotent stem cell differentiation toward anterior neuroectoderm fates using specific morphogen combinations, with organoids harvested at timepoints corresponding to key developmental milestones (e.g., 30-60 days of differentiation) [85]. At these stages, organoids exhibit diverse neural cell types including radial glia, intermediate progenitor cells, and both excitatory and inhibitory neurons, mirroring the cellular diversity of the developing fetal brain [85].
Following differentiation, systematic quantification of organoid morphological features provides the foundation for correlation with clinical data. Advanced analysis methods include single-cell RNA sequencing to identify transcriptomic signatures associated with size phenotypes [85], proteomic profiling of organoid-derived extracellular vesicles [84], and electrophysiological characterization of functional properties [87]. Integration of these diverse data types through multi-omics approaches enables researchers to construct comprehensive models linking organoid phenotypes to clinical presentations.
Molecular Signatures Underlying Size Phenotypes
The molecular mechanisms underlying organoid size variations in ASD models involve dysregulated developmental pathways controlling cell fate decisions and proliferation-differentiation balance. Single-cell transcriptomic analyses of ASD organoids have revealed opposite disruptions in the balance between excitatory neurons of the dorsal cortical plate and other neuronal lineages in macrocephalic versus normocephalic ASD cases [85].
In macrocephalic ASD organoids, researchers observed altered expression of transcription factors driving cell fate during early cortical development, leading to expansion of specific progenitor populations [85]. These findings align with human neuroimaging studies suggesting that brain overgrowth in ASD stems from disruptions in the normal sequence of cortical development during early childhood.
Beyond intrinsic cellular composition, extracellular vesicle (EV) profiling of ASD organoids has revealed distinct molecular signatures associated with disease status [84]. EVs secreted by ASD-derived forebrain organoids carry significantly different RNA and protein cargo compared to healthy controls, providing insights into disease mechanisms and potential diagnostic biomarkers [84]. These EV signatures may reflect intercellular communication defects that contribute to the observed size phenotypes and offer promising targets for therapeutic intervention.
The Scientist's Toolkit: Essential Reagents and Platforms
Table 3: Essential Research Tools for Organoid-Based ASD Modeling
| Tool Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Stem Cell Sources | Patient-derived iPSCs [85], CRISPR-edited lines [83] | Disease modeling, genetic rescue studies | Maintain genetic background, isogenic controls |
| Differentiation Matrices | Matrigel [82], Defined synthetic matrices [88] | 3D structural support, morphogen presentation | Batch variability, defined composition needs |
| Molecular Analysis | scRNA-seq platforms [85], Proteomic workflows [84], EV isolation kits [84] | Molecular signature identification | Integration with morphological data |
| Quantification Platforms | GelCount [86], Confocal microscopy [86] | High-throughput size measurement | Balance between throughput and resolution |
| Specialized Culture | Bioreactors [89], Organ-on-chip systems [90] [88] | Long-term culture, enhanced maturation | Improved nutrient exchange, physiological relevance |
Successful implementation of organoid-based disease modeling requires specialized research tools and platforms carefully selected for specific applications. The foundation of any organoid study lies in the stem cell sources, with patient-derived iPSCs offering the distinct advantage of preserving the complete genetic background of donors, including both rare variants and common risk alleles that may contribute to ASD susceptibility [85]. For mechanistic studies, CRISPR-edited isogenic lines enable researchers to introduce or correct specific mutations in otherwise identical genetic backgrounds, allowing precise dissection of gene function [83].
During organoid differentiation, extracellular matrices provide the essential three-dimensional environment that supports self-organization and morphogenesis. While Matrigel remains widely used, its batch-to-batch variability has prompted development of defined synthetic matrices that offer greater reproducibility and experimental control [88]. Similarly, specialized culture systems like bioreactors and organ-on-chip platforms enhance organoid viability and maturation by improving nutrient exchange and incorporating physiological cues such as fluid flow and mechanical stimulation [90] [89] [88].
For phenotypic characterization, automated quantification systems like the GelCount platform enable high-throughput, reproducible size measurements across large experimental batches [86]. These are complemented by molecular profiling tools including single-cell RNA sequencing for transcriptomic analysis, proteomic workflows for protein expression assessment, and specialized kits for extracellular vesicle isolation and characterization [84] [85]. Integration across these methodological domains provides the comprehensive dataset needed to correlate organoid phenotypes with clinical outcomes.
Challenges and Future Directions
Despite considerable progress, several technical challenges remain in optimizing the correlation between organoid features and clinical phenotypes. Organoid systems currently exhibit limitations in standardization and reproducibility, with variability in size, shape, and cellular composition between batches potentially confounding experimental results [90] [88]. This variability stems partly from incomplete control over organoid self-organization processes and differences in starting cell populations.
The absence of vascularization in most current organoid models limits their size and maturity, as diffusion alone cannot support adequate nutrient and oxygen exchange in larger structures [90] [88]. This can lead to necrotic core formation and altered cellular behavior that may not accurately reflect in vivo development. Emerging approaches to address this limitation include co-culture with endothelial cells, incorporation of vascular organoids to create assembloids, and use of microfluidic devices to enhance perfusion [90] [82].
Another significant challenge lies in the fetal phenotype of most current brain organoid models, which may not fully capture the pathophysiology of disorders like ASD that manifest throughout childhood and adulthood [90] [88]. While patient-derived organoids can provide some insight into later stages of disease, their lower throughput presents practical limitations for large-scale screening applications.
Future directions in the field include developing more complex multi-region assembloids that better recapitulate neural circuit formation, integrating immune cells to model neuroinflammation, and implementing advanced engineering approaches such as bioprinting for greater control over organoid structure [82]. Additionally, computational methods incorporating artificial intelligence and machine learning are being deployed to improve organoid characterization, reduce variability, and identify subtle patterns that might escape conventional analysis [90] [88]. As these technologies mature, organoid size and related morphological features will likely play an increasingly important role in bridging the gap between in vitro observations and clinical phenotypes in ASD and other neurodevelopmental disorders.
Cross-Model Validation: Contrasting Neuroanatomical and Developmental Trajectories in ASD and FXS
Autism Spectrum Disorder (ASD) and Fragile X Syndrome (FXS) represent two distinct yet overlapping neurodevelopmental disorders. FXS, stemming from a well-defined genetic mutation on the FMR1 gene, is the most common monogenic cause of ASD [91]. Idiopathic ASD (iASD), in contrast, has a complex and heterogeneous genetic etiology [92]. Despite shared behavioral symptoms, a key question in neuroscience is whether these disorders share a common neurobiological basis. Advanced neuroimaging reveals that iASD and FXS are characterized by divergent patterns of gray matter volume (GMV) and distinct development trajectories, challenging the notion of a single "autism brain" and pointing to unique underlying pathophysiologies [93] [94] [95]. This guide provides a comparative analysis of GMV abnormalities and growth patterns in iASD and FXS for researchers and drug development professionals.
Comparative Neuroanatomy: Gray Matter Volume Profiles
Structural MRI studies consistently demonstrate that while both groups may exhibit generalized brain overgrowth compared to typically developing (TD) controls, the specific regional patterns of GMV alteration are distinct.
Key Regional Differences in Gray Matter Volume
The table below summarizes the most consistently reported GMV differences from cross-sectional and longitudinal studies.
Table 1: Regional Gray Matter Volume Alterations in iASD vs. FXS
| Brain Region | Idiopathic ASD | Fragile X Syndrome (FXS) | Comparative Direction |
|---|---|---|---|
| Caudate Nucleus | Modest enlargement or mixed findings [93] [91] | Pronounced and consistent enlargement [93] [94] [95] | FXS > iASD |
| Amygdala | Larger volume, particularly in young children [93] [91] | Significantly smaller volume [93] [91] | iASD > FXS |
| Cerebellar Gray Matter | Mixed findings; less consistent signature [93] | Increased volume in Crus I [94] [95]; decreased volume in vermis lobules VIII/IX [94] [95] and cerebellar vermis [96] | FXS shows a distinct, mixed pattern |
| Frontal/Insular Cortex | Faster GMV growth rates; potential initial overgrowth [94] [95] | Decreased GMV [94] [95] | iASD > FXS |
| Temporal Lobe | Generalized cortical lobe enlargement [93] [97] | Specific enlargement in temporal lobe white matter rather than gray matter [93] [97] | Patterns differ (GM vs. WM focus) |
Global Brain Volume and Growth Trajectories
Beyond regional differences, the global growth patterns of the brain also diverge between the two conditions.
Table 2: Comparative Brain Growth Trajectories in Early Childhood
| Characteristic | Idiopathic ASD | Fragile X Syndrome (FXS) | References |
|---|---|---|---|
| Global Brain Volume | Increased total brain volume (TBV) compared to TD, evident at age 2-3 [93] [92] | Increased TBV compared to TD, evident at age 2-3 and not different from iASD [93] [97] | [93] [97] [92] |
| Growth Rate (Ages 2-5) | Significant, faster growth rates of morphological volumes [94] [95] | Rate of brain growth parallels that of TD controls; no accelerated growth in this period [93] [97] | [93] [94] [95] |
| Developmental Trajectory | Potential early overgrowth followed by a slowdown or normalization later in childhood/adolescence [92] | Brain overgrowth is evident at age 2 and maintained (not accelerated) across ages 4-5 [93] [97] | [93] [97] [92] |
Experimental Protocols and Methodologies
A direct comparison of findings requires an understanding of the core experimental protocols used in this field. The following workflows and methodologies are standard in studies comparing neuroanatomy in iASD and FXS.
Participant Ascertainment and Characterization
Figure 1: Participant Characterization Workflow. (DSM-5: Diagnostic and Statistical Manual of Mental Disorders, 5th Edition; ADOS-2: Autism Diagnostic Observation Schedule-2; SRS: Social Responsiveness Scale; ADI-R: Autism Diagnostic Interview-Revised).
Neuroimaging Data Acquisition and Analysis Pipeline
The cornerstone of this research is structural Magnetic Resonance Imaging (MRI) and its computational analysis.
Table 3: Key MRI Acquisition Parameters for Structural T1-Weighted Imaging
| Parameter | Typical Specification | Function |
|---|---|---|
| Sequence | 3D Fast Spoiled Gradient Echo (FSPGR) or MPRAGE | Provides high-resolution T1-weighted contrast for optimal segmentation of brain tissues. |
| Field Strength | 3.0 Tesla | Ensures a high signal-to-noise ratio for detailed anatomical images. |
| Voxel Size | 1×1×1 mm³ | Provides isotropic resolution, allowing for accurate volumetric measurements and re-slicing in any plane. |
| Repetition Time (TR) | ~8.2 ms | A fundamental sequence parameter controlling image contrast and acquisition time. |
| Echo Time (TE) | ~3.2 ms | A fundamental sequence parameter controlling image contrast and acquisition time. |
| Scan Duration | ~8-9 minutes | Balances data quality with practicality for scanning young children, often during natural sleep. |
Figure 2: Neuroimaging Analysis Pipeline. (GM: Gray Matter; WM: White Matter; CSF: Cerebrospinal Fluid).
Protocol Details:
- Voxel-Based Morphometry (VBM): This fully automated technique allows an unbiased whole-brain analysis to identify voxel-wise differences in gray matter density or volume between groups [94] [95] [98]. Key steps include spatial normalization to a standard template, tissue segmentation, smoothing, and modulation to preserve absolute volume information. Statistical models then compare groups at each voxel, controlling for covariates like age, sex, and total intracranial volume [99] [100].
- Manual Volumetrics: This method involves manually or semi-automatically tracing regions of interest (ROIs) on consecutive MRI slices. It is considered the gold standard for quantifying specific structures like the caudate nucleus or amygdala, as it is less susceptible than VBM to misregistration errors [93] [97]. This approach requires high inter-rater reliability.
- Longitudinal Analysis: To model growth, researchers acquire MRI scans at multiple time points (e.g., ages 2-3 and 4-5) [93] [97]. Advanced statistical models, such as linear mixed-effects models, are used to analyze the rate of change in brain volumes over time, comparing trajectory slopes between iASD, FXS, and TD groups [94] [95].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagents and Solutions for Neurodevelopmental Disorder Research
| Item | Function/Application | Examples/Details |
|---|---|---|
| DNA Analysis Kits | Confirmatory diagnosis of FXS and exclusion in iASD cohorts. Detects CGG trinucleotide repeat expansions in the FMR1 gene. | Southern Blot analysis [93], Capillary Electrophoresis [98]. |
| Immunostaining Assays | Quantify FMRP (Fragile X Mental Retardation Protein) expression levels in peripheral blood lymphocytes, correlating with molecular and phenotypic severity [93]. | FMRP Antibodies, fluorescence microscopy. |
| Behavioral Assessment Kits | Standardized phenotypic characterization. Critical for diagnosing autism and quantifying symptom severity across groups. | Autism Diagnostic Observation Schedule (ADOS-2) [93] [98], Autism Diagnostic Interview-Revised (ADI-R) [93], Social Responsiveness Scale (SRS) [99]. |
| Cognitive & Developmental Scales | Measure intellectual and developmental functioning, a key covariate in neuroimaging analyses. | Griffiths Development Scales (GDS) [98], various IQ tests (e.g., WISC). |
| Statistical Analysis Software | Perform complex statistical modeling on imaging and behavioral data, including voxel-wise comparisons and longitudinal growth models. | SPM12, CAT12 toolbox [98], FSL, R, SAS. |
Integrated Discussion and Pathophysiological Implications
The distinct neuroanatomical profiles of iASD and FXS suggest divergent underlying pathophysiological mechanisms, a crucial consideration for targeted drug development.
The most striking difference is the consistent and pronounced enlargement of the caudate nucleus in FXS, which is less robust in iASD [93] [94] [95]. The caudate is rich in FMRP, and its enlargement may reflect a direct consequence of its absence, leading to dysregulated synaptic pruning and connectivity in corticostriatal pathways [96]. This makes the caudate a strong candidate biomarker and target for FXS-specific therapeutics.
Conversely, the amygdala shows a divergent pattern, being larger in iASD and smaller in FXS [93] [91]. This highlights that clinically overlapping symptoms (e.g., anxiety, social fear) may arise from distinct neural substrates. The amygdala's role in emotional processing and social fear is well-established, and its differential development in these disorders points to unique etiologies requiring different intervention strategies.
Furthermore, cerebellar and frontal-insular differences underscore distinct developmental trajectories. The FXS brain exhibits a specific pattern of cerebellar dysgenesis (vermis hypoplasia and Crus I hyperplasia) and reduced frontal-insular GMV, while iASD is associated with faster GMV growth rates in frontal regions [94] [95]. The frontal-insular network is critical for social cognition and salience detection, and its differential development aligns with the nuanced variations in social challenges observed between the two conditions.
These findings robustly demonstrate that despite behavioral overlap, iASD and FXS are neurobiologically distinct. The "overgrowth/undergrowth" model must be applied region-specifically, not globally. Future research and clinical trials must move beyond behavioral diagnoses and incorporate these neuroanatomical biomarkers to stratify populations and validate the efficacy of mechanism-based treatments.
Thesis Context: Comparative Analysis of Overgrowth and Undergrowth in ASD Models
The heterogeneity of Autism Spectrum Disorder (ASD) presents a significant challenge in elucidating its pathophysiology. A powerful approach to dissect this complexity is the comparative analysis of biological subgroups, particularly those defined by opposing anatomical phenotypes: brain overgrowth (megalencephaly) and undergrowth (microcephaly). This guide frames the convergent roles of PI3K/AKT and RAS/ERK signaling within this comparative thesis, examining how dysregulation of these evolutionarily conserved pathways drives divergent neurodevelopmental trajectories—from excessive cell proliferation and survival to synaptic dysfunction—that culminate in ASD [15] [101]. By comparing molecular signatures, model systems, and therapeutic interventions across these phenotypes, researchers can identify core, targetable mechanisms.
Table 1: Comparative Overview of ASD Subgroups with Overgrowth vs. Undevelopment Phenotypes
| Feature | Macrocephalic ASD (Overgrowth Model) | Reference (Typical Development) | Microcephalic ASD/Undergrowth Models |
|---|---|---|---|
| Prevalence in ASD | ~20% of cases [15] | N/A | Less common; rate may not differ from general population [15] |
| Primary Anatomical Feature | Head circumference >97th percentile (macrocephaly); Brain enlargement (megalencephaly) [15] | Head circumference within normal distribution | Head circumference <3rd percentile; reduced brain volume |
| Proposed Growth Trajectory | Possible precocious early growth with later regression OR sustained overgrowth from embryogenesis [15] | Standard neurodevelopmental curve | Impaired prenatal and postnatal brain growth |
| Associated Symptom Severity | Lower IQ, delayed language onset, more severe social deficits [15] | N/A | Often associated with greater intellectual disability |
| Key Signaling Pathways Implicated | PI3K/AKT, RAS/ERK, WNT/β-catenin [102] [101] | Homeostatic regulation of same pathways | Mutations leading to impaired PI3K/AKT/mTOR or RAS/ERK signaling (e.g., PTEN overactivity) |
| Core Cellular Processes | Excess neurogenesis/gliogenesis, decreased apoptosis, neuronal hypertrophy [15] | Balanced proliferation, differentiation, and pruning | Reduced neural progenitor proliferation, increased apoptosis, impaired neuronal differentiation |
Table 2: Molecular Signature of Convergent Pathways in ASD from Leukocyte Transcriptomics
| Parameter | Finding in Toddlers with ASD (vs. TD) | Experimental Support & Correlation |
|---|---|---|
| Transcriptional Activity | Increased co-expression magnitude in a perturbed gene network [102] | Higher co-expression in ASD vs. TD (p<0.01) [102] |
| Network Enrichment | Genes highly expressed in prenatal neocortex (p<4.3×10⁻³⁰) [102] | Peak activity coincides with 10-19 post-conception weeks (peak neurogenesis) [102] |
| Upstream Regulators | High-confidence ASD risk genes [101] | SFARI genes implicated as upstream regulators of the network [101] |
| Pathway Convergence | Modulation of RAS/ERK, PI3K/AKT, and WNT/β-catenin pathways [101] [103] | Many ASD risk genes predicted to impact these signaling cascades [101] |
| Clinical Correlation | Degree of network dysregulation correlates with socialization symptom severity [101] [103] | Provides a molecular link between prenatal pathway dysregulation and postnatal behavior |
Table 3: Outcomes of Targeted Pathway Inhibition in Overgrowth Disorders
| Therapeutic Agent | Target Pathway | Disorder (Mutation) | Key Efficacy & Safety Findings (Trial/Case) |
|---|---|---|---|
| Miransertib (ARQ 092) | Pan-AKT inhibitor | PROS (PIK3CA), Proteus (AKT1) [104] | Safe/tolerable in phase 1/2 (n=49). Common AEs: decreased neutrophils, increased blood insulin, stomatitis [104]. |
| Alpelisib | PIK3CA inhibitor | PROS (PIK3CA) [104] | Compassionate use: 37.5% had ≥20% target lesion volume reduction. Tolerable safety profile [104]. |
| Sirolimus | mTOR inhibitor | PROS, vascular anomalies [104] | Reduced tissue volume in affected areas, but with clinically important adverse events [104]. |
Experimental Protocols for Key Cited Studies
- Sample Cohort: 226 male toddlers (1-4 years old): 119 with ASD, 107 with typical development (TD). Diagnosis confirmed using ADOS and clinical judgment.
- RNA Profiling: Leukocyte RNA collected via PAXgene tubes. Gene expression profiling performed using microarray or RNA-Seq (GEO: GSE42133, GSE111175).
- Differential Expression & Network Analysis:
- Identify Differentially Expressed (DE) genes using robust linear regression (FDR <0.05).
- Construct a static interaction network from known physical/regulatory interactions among DE genes.
- Prune to create diagnosis-specific context networks (DE-ASD, DE-TD) by retaining only interactions with significant co-expression (FDR <0.05) within each group.
- Calculate co-expression magnitude for interactions in the merged network and compare between ASD and TD groups using paired Wilcoxon-Mann-Whitney test.
- Pathway & Enrichment Analysis:
- Overlay network genes on BrainSpan developmental transcriptome data to assess prenatal brain expression enrichment.
- Use upstream regulator analysis to link high-confidence ASD (SFARI) risk genes to the dysregulated network.
- Perform pathway enrichment to identify implicated signaling cascades (PI3K/AKT, RAS/ERK, WNT/β-catenin).
- Clinical Correlation: Correlate individual-level network dysregulation scores with standardized ASD symptom severity scores (e.g., ADOS social affect score).
- Cell Model: Cultured rodent or human neurons.
- Genetic Perturbation: RNAi-mediated knockdown of 16 ASD/SCZ-associated risk genes (e.g., SHANK3, NRXN1).
- Multiplexed Imaging:
- Immunofluorescence staining for 10 excitatory synaptic proteins (e.g., PSD-95, GluA1, SHANK).
- Sequential Fluorescence Imaging using antibody stripping and re-probing cycles to achieve multiplexing on the same sample.
- High-resolution microscopy to capture single-synapse data.
- Image & Data Analysis:
- Single-Synapse Measurement: Use CellProfiler to segment individual synapses and extract intensity values for all 10 proteins per synapse.
- Phenotype Identification: Compare synaptic protein composition and distribution profiles between knockdown and control conditions.
- Bayesian Network Inference: Apply Bayesian structure learning algorithms on the single-synapse, multi-protein data to infer hierarchical dependency networks among the 8 most variable synaptic proteins.
- Convergence Analysis: Identify shared alterations in the inferred synaptic dependency network architecture across different gene knockdowns.
- Study Design: Open-label, multicenter trial (MOSAIC, NCT03094832).
- Participants: ≥2 years old with PROS (PIK3CA mutation) or Proteus syndrome (AKT1 mutation), measurable disease, and progressive symptoms.
- Dosing Regimen:
- Lead-in: Miransertib 15 mg/m² orally once daily for 3 cycles (28 days each).
- Dose Escalation: If tolerated, increase to 25 mg/m² daily for subsequent cycles.
- Treatment Duration: Continue for up to 48 cycles or until progression/unacceptable toxicity.
- Safety Assessment: Primary outcome (amended). Monitor adverse events (CTCAE), hematology, and blood chemistry regularly.
- Efficacy Assessment (Exploratory): Serial MRI or photography to measure lesion volume/characteristics. Challenges in standardization limited formal efficacy analysis.
Pathway and Workflow Visualization
Diagram 1: Convergence of Heterogeneous ASD Genetics on PI3K/AKT and RAS/ERK Signaling.
Diagram 2: Experimental Workflow for Leukocyte-Based Transcriptomic Network Discovery.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents and Materials for Research in Convergent ASD Pathways
| Item/Category | Example Product/Specification | Primary Function in Research Context |
|---|---|---|
| Pathway-Targeted Inhibitors (for functional validation) | Miransertib (AKTi), Alpelisib (PI3Kαi), Trametinib (MEKi), Rapamycin (mTORi) | Pharmacologically modulate target pathways in cellular or animal models of overgrowth/synaptic dysfunction to establish causal roles and therapeutic potential [105] [104]. |
| Multiplexed Imaging Antibody Panels | Validated antibodies for synaptic proteins (PSD-95, Synapsin, GluN1, SHANK3, VGLUT1) with distinct fluorophores (e.g., Alexa Fluor 488, 555, 647). | Enable simultaneous quantification of multiple synaptic proteins at single-synapse resolution, crucial for network inference studies as in [106]. |
| RNAi/shRNA Libraries | Lentiviral shRNA pools targeting high-confidence ASD risk genes (e.g., from SFARI gene list). | Perform systematic loss-of-function screens in neuronal cultures to model genetic perturbations and observe convergent phenotypic effects on signaling and synapses [106]. |
| hiPSC-Derived Neural Progenitors & Neurons | Commercially available control and ASD-patient-derived hiPSC lines (e.g., with PTEN, CHD8 mutations). | Provide a human, physiologically relevant model system to study cell-autonomous effects of ASD mutations on neurodevelopment, proliferation, and pathway activity [102] [101]. |
| Leukocyte RNA Stabilization Tubes | PAXgene Blood RNA Tubes. | Ensure high-quality, reproducible RNA preservation from peripheral blood samples for transcriptomic studies linking leukocyte signatures to brain-relevant pathways [102] [101]. |
| Pathway Activity Reporters | Phospho-specific antibodies (p-AKT S473, p-ERK T202/Y204), FRET-based biosensors (AKAR, EKAR). | Quantify real-time activity and localization of PI3K/AKT and RAS/ERK signaling in live or fixed cells under various genetic/pharmacological manipulations. |
The comparative analysis of cortical architecture and cerebellar anatomy provides a powerful lens for understanding both typical brain development and neurodevelopmental conditions such as autism spectrum disorder (ASD). This approach examines neuropathological features across species, experimental models, and human subtypes to identify fundamental organizational principles and pathological deviations. Research indicates that the cerebello-cerebral system has evolved in tandem to support diverse mental functions, with modular adaptations in primates potentially supporting cognitive functions [107]. The consistent observation of cerebellar alterations across ASD studies makes it a focal point for comparative analysis [108] [71]. Similarly, investigation of cortical architecture reveals patterns of disruption that may underlie the heterogeneous symptoms observed in ASD. By systematically comparing these neuroanatomical features across different contexts, researchers can distinguish conserved pathological mechanisms from model- or species-specific variations, ultimately advancing our understanding of complex neurodevelopmental conditions.
Cortical Architecture: A Comparative Perspective
Cytoarchitectural Abnormalities in ASD
Postmortem studies of human brains with ASD have revealed consistent abnormalities in cortical organization, despite the etiological and phenotypic heterogeneity of the condition. The average number of cases in these neuropathology studies is approximately 7.43, indicating the preliminary nature of these findings and the need for larger sample sizes [1]. A key observation is the presence of gray and white matter disorganization, often manifested as cortical dysplasia and heterotopia, which reflect alterations in neuronal maturation and migration processes [1]. Subjects with ASD exhibit decreased expression of Reelin, a protein crucial for neuronal migration during cortical lamination [1].
Minicolumnar pathology represents another consistent finding, with patients with ASD showing smaller and more numerous minicolumns with more dispersed neurons in Brodmann's areas 9, 21, and 22 [1]. These changes appear to be regionally specific, as they are not present in the primary visual cortex [1]. It is important to note, however, that these minicolumnar findings originate primarily from one research group using indirect quantification methods from 2-dimensional images rather than 3-dimensional stereological techniques, indicating the need for independent replication [1].
Perikaryal abnormalities are also evident in ASD, with young children showing significantly reduced neuronal and cytoplasmic volumes in most examined brain areas compared to age-matched controls [1]. Interestingly, the developmental trajectories of these measures differ between ASD and control groups, with nuclear volumes increasing with age in ASD in half of examined brain areas, while decreasing in most brain areas of controls as they age [1].
Table 1: Cortical Architecture Abnormalities in Autism Spectrum Disorder
| Feature | Observation in ASD | Brain Regions Affected | Functional Implications |
|---|---|---|---|
| Gray/White Matter Organization | Disorganization, dysplasia, heterotopia | Multiple cortical and subcortical regions | Altered neuronal migration and maturation |
| Minicolumnar Structure | Smaller, more numerous minicolumns | Prefrontal, temporal cortex (Brodmann's 9, 21, 22) | Potential information processing deficits |
| Neuronal Soma Size | Reduced volume in childhood; altered developmental trajectory | Multiple brain areas | Possible disruption of neuronal connectivity |
| Cortical Layer Organization | Disrupted lamination by "pencil fibers" | Prefrontal cortex | Altered local circuit function |
Brain Overgrowth Phenomena in ASD
A prominent theory in ASD research posits that a subset of individuals exhibits precocious brain growth during early childhood, followed by normalization of brain volume by adolescence [15]. This theory originated from findings of enlarged brains in young children with ASD and the absence of such enlargement in adolescents and adults [15]. However, longitudinal studies have challenged this trajectory, with the Autism Phenome Project finding that boys with ASD and disproportionate macrocephaly continue to have enlarged brains until at least 13 years of age [15].
Approximately 20% of children with ASD have macrocephaly (head circumference above the 97th percentile), with ASD patients with macrocephaly exhibiting more severe disability than those with normal head size [15]. Recent evidence suggests that the biological basis for ASD subtypes develops much earlier than previously thought. Research using induced pluripotent stem cells (iPSCs) derived from toddlers with autism to create brain cortical organoids (BCOs) - models of the brain's cortex during embryonic development - found that BCOs from toddlers with autism grew roughly 40% larger than those from neurotypical controls [109]. The severity of this overgrowth correlated with clinical outcomes: "We found the larger the embryonic BCO size, the more severe the child's later autism social symptoms," researchers reported [109].
The growth patterns in macrocephalic ASD appear to be heterogeneous. Some patients display macrocephaly only prenatally, others only during childhood, and some throughout life [15]. The neuroanatomy of this overgrowth is similarly multifaceted, with some studies pointing to general overgrowth of the frontal, temporal, and parietal lobes, while others identify specific structures like the amygdala or hippocampus as particularly affected [15].
Table 2: Brain Growth Patterns in Autism Spectrum Disorder
| Growth Pattern | Developmental Timing | Prevalence in ASD | Clinical Correlations |
|---|---|---|---|
| Transient Overgrowth | Early childhood with subsequent normalization | Subset of cases | Original theory based on cross-sectional studies |
| Persistent Overgrowth | Prenatal through adolescence | ~20% (macrocephaly) | More severe symptoms, lower IQ |
| Region-Specific Overgrowth | Varies by region | Unknown | May correlate with specific symptom profiles |
| Embryonic Overgrowth | First trimester | Associated with profound autism | Predicts social symptom severity |
Contrary to the overgrowth hypothesis, some recent evidence points to a different trajectory. A 2025 study examining perinatal brain growth found that reduced total brain volume in the first two months of life was associated with a higher number of autistic traits at 18 months [18]. This association was found in two independent cohorts (dHCP and CHILD) and was particularly pronounced in individuals with a family history of autism [18]. This suggests potential subtypes of ASD with distinct neurodevelopmental trajectories.
Cerebellar Anatomy in Evolution and Disease
Comparative Cerebellar Neuroanatomy
The cerebellum contains the largest number of neurons and synapses of any structure in the central nervous system, and its expansion throughout primate evolution, particularly in apes and humans, has been substantial [108]. Notably, the human cerebellum comprises approximately 10% of total brain volume yet contains about 80% of all brain neurons [107] [108]. This expansion has been especially prominent in the posterior lobe of the cerebellum, a substructure crucial for rapid processing of cognitive and language skills [108].
A comparative study of cerebellar neuronal morphology across eight large-brained mammalian species revealed both conserved features and significant quantitative variation [110]. The cerebellar cortex in all species exhibited the trilaminate pattern common to all mammals, consisting of the molecular layer, Purkinje cell layer, and granular layer [110]. Despite this conserved architecture, dendritic measures of various cerebellar neurons (stellate, basket, Lugaro, Golgi, and granule cells) tended to increase with cerebellar volume across species [110]. Notably, Lugaro neurons in the African elephant appeared disproportionately larger than those in other species, suggesting potential species-specific adaptations [110].
The exceptional volumetric increase of the lateral cerebellum in primates, particularly in conjunction with its connectivity to cerebral cortical association areas, may be linked to non-motor functions and mental operations [107]. Lateral cerebellar lobules crura I-II and their reciprocal connections to cerebral cortical association areas have substantially expanded in great apes and humans [107]. This expansion, along with a notable increase in the ventral portions of the dentate nucleus and a shift to increased relative prefrontal-cerebellar connectivity, suggests that modular cerebellar adaptations support cognitive functions in humans [107].
Cerebellar Pathology in ASD
Cerebellar impairments are among the most widely recognized neural correlates of ASD [71]. As a critical computational hub, the cerebellum controls and coordinates motor, affective, and cognitive processes, with specific alterations potentially contributing to ASD symptomatology [71]. Postmortem studies have consistently revealed abnormalities in cerebellar cellular architecture, with Purkinje cell loss being a particularly common finding [108].
Genetic forms of ASD provide compelling evidence for cerebellar involvement. Studies of experimental models with mutations in genes such as FMR1 (fragile X syndrome), MECP2 (Rett syndrome), TSC1/2 (tuberous sclerosis), and NLGN3/4 have been critical in uncovering molecular pathology and neurobehavioral correlates [71]. These genetic models demonstrate that cerebellar dysfunction can contribute to ASD phenotypes, even when the genetic alterations are not restricted to the cerebellum.
The link between cerebellar pathology and ASD symptoms is further supported by studies of humans with brain damage restricted to the cerebellum, who can exhibit features of the cerebellar cognitive affective syndrome, including impairments in executive function, spatial cognition, and emotional regulation [108]. This connection underscores the cerebellum's role in domains beyond motor control, particularly those affected in ASD.
Diagram 1: Neuropathological Pathways in Autism Spectrum Disorder. This diagram illustrates the convergent pathways through which genetic and environmental factors contribute to cerebellar and cortical pathology in ASD, ultimately manifesting as core symptoms.
Experimental Models and Methodologies
Key Experimental Protocols in Comparative Neuropathology
Brain Organoid Modeling of Embryonic Development
The development of brain cortical organoids (BCOs) from induced pluripotent stem cells (iPSCs) represents a significant advance in modeling early neurodevelopmental processes. The protocol involves obtaining blood samples from toddlers with ASD and neurotypical controls, then reprogramming these cells into iPSCs [109]. These iPSCs are subsequently differentiated into BCOs that model the brain's cortex during the first weeks of embryonic development [109]. Researchers found that BCOs from toddlers with autism grew roughly 40% larger than those from neurotypical controls, demonstrating embryonic growth patterns that predicted later symptom severity [109]. This methodology enables researchers to identify molecular causes of atypical brain development, such as reduced expression of NDEL1, a protein/enzyme that regulates growth of the embryonic brain [109].
Comparative Neuronal Morphometry
The quantitative analysis of neuronal morphology across species provides insights into both conserved and specialized features of brain organization. In one comprehensive approach, researchers applied a modified rapid Golgi technique to cerebellar tissue from eight mammalian species, staining various neuron types including stellate, basket, Lugaro, Golgi, and granule neurons [110] [111]. The impregnated neurons were quantified using a computer-assisted microscopy system, measuring dendritic parameters such as length, branching complexity, and spatial extent [110]. This methodology revealed that while the basic morphological characteristics of cerebellar neurons were consistent across species, there was substantial quantitative variation, with most dendritic measures increasing with cerebellar volume [110].
Longitudinal Neuroimaging Analysis
Longitudinal magnetic resonance imaging (MRI) studies have been essential for characterizing developmental brain trajectories in ASD. The developing Human Connectome Project (dHCP) and Cambridge Human Imaging and Longitudinal Development (CHILD) study represent exemplary approaches in this domain [18]. These prospective cohorts include both prenatal and postnatal MRI brain scans, with subsequent assessment of autistic traits at 18 months using the Quantitative Checklist for Autism in Toddlers (Q-CHAT) [18]. Analytical protocols involve controlling for covariates such as maternal age, birth weight, sex, and age post-conception at the time of scan, enabling researchers to distinguish specific associations between early brain development and later autistic traits [18].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Neuropathological Investigation
| Reagent/Material | Application | Function in Research | Examples from Literature |
|---|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | Brain organoid development | Modeling early embryonic brain development | Derived from blood samples of toddlers with ASD [109] |
| Golgi Staining Solutions | Neuronal morphology analysis | Visualizing complete neuronal structure | Modified rapid Golgi technique for cerebellar neurons [110] |
| MRI Contrast Agents | In vivo brain imaging | Enhancing tissue contrast for volumetric analysis | Used in dHCP and CHILD studies [18] |
| Antibodies for Reelin | Histopathological analysis | Identifying neuronal migration deficits | Decreased expression in ASD cortical areas [1] |
| Genetic Engineering Tools | Animal model development | Creating specific genetic alterations | Mutations in FMR1, MECP2, TSC1/2, NLGN3/4 [71] |
Integration and Future Directions
The comparative analysis of cortical architecture and cerebellar anatomy across species, experimental models, and clinical populations reveals both shared and unique features of neurodevelopmental conditions like ASD. The consistent observation of cerebellar pathology across genetic models and human postmortem studies suggests a central role for this structure in ASD pathogenesis [108] [71]. Similarly, abnormalities in cortical organization, including minicolumnar pathology and disrupted lamination, point to developmental disturbances in neuronal migration and circuit formation [1].
The apparent contradiction between studies reporting brain overgrowth and those identifying reduced brain volume in ASD may reflect the substantial heterogeneity of the condition [15] [109] [18]. It is likely that distinct neurobiological subtypes of ASD exist, with different developmental trajectories and underlying mechanisms. Future research that integrates multiple levels of analysis - from molecular and cellular to systems and behavioral - will be essential for parsing this heterogeneity.
The comparative approach also highlights the importance of evolutionary perspectives in understanding human-specific vulnerabilities. The exceptional expansion of the lateral cerebellum and its connections with cerebral cortical association areas in humans and other apes may represent a specialization that, when disrupted, contributes to neurodevelopmental conditions [107] [108]. Similarly, the species-specific variations in neuronal morphology observed in comparative studies suggest that some pathological features may be unique to humans or particularly pronounced in our lineage [110].
As research advances, the integration of patient-derived cellular models, genetically engineered animal systems, and detailed clinical phenotyping promises to reveal the complex interplay between genetic vulnerability, environmental factors, and developmental timing in shaping neurodevelopmental outcomes. This integrated perspective will ultimately support the development of more targeted interventions for individuals with ASD and related conditions.
Autism Spectrum Disorder (ASD) represents a profound challenge in neurodevelopmental research and drug development due to its extensive clinical and genetic heterogeneity. As a spectrum condition, ASD encompasses a wide range of presentations characterized by challenges in social interaction, communication, and restricted or repetitive behaviors [15]. This heterogeneity is mirrored at the biological level, where hundreds of associated genes and diverse neurological manifestations create a complex landscape for therapeutic development [15] [112]. The emerging recognition that ASD comprises multiple biologically distinct subtypes necessitates a sophisticated approach to model system selection and validation [112]. Understanding this variability is crucial for developing targeted interventions, as the biological mechanisms underlying one subgroup may differ significantly from another.
The critical importance of model system selection stems from the high failure rates in drug development, particularly for complex neurodevelopmental disorders. The traditional approach of treating ASD as a single entity has yielded limited therapeutic success, prompting a shift toward stratification and precision medicine [112]. By identifying and validating model systems that accurately recapitulate specific ASD subtypes, researchers can improve the predictive validity of preclinical studies and increase the likelihood of clinical translation. This comparative analysis focuses on evaluating model systems across key ASD subgroups, particularly those characterized by divergent brain growth patterns—overgrowth and undergrowth phenotypes—which may represent distinct neurobiological mechanisms with implications for therapeutic development.
Classifying ASD Subgroups: Implications for Model Selection
Behavioral and Genetic Stratification
Recent large-scale analyses have begun to unravel the heterogeneity of ASD through systematic stratification approaches. A landmark study analyzing data from 5,392 autistic individuals identified four distinct subtypes based on behavioral manifestations and their genetic correlates [112]. The "Social and/or behavioral" subtype exhibits core autism features with co-occurring mood and attention disorders but without developmental delays. The "Moderate challenges" subtype includes individuals with milder expression across all core autism features. The "Broadly affected" subtype encompasses those significantly impacted across all core criteria with high levels of co-occurring conditions. Finally, the "Mixed ASD with DD" subtype presents with social communication challenges, developmental delays, and repetitive behaviors but typically without mood disorders or attention challenges [112].
Crucially, these behavioral subtypes align with distinct genetic patterns. The "Broadly affected" subtype shows strong association with de novo variants linked to fragile X syndrome and intellectual disabilities, while the "Social/behavioral" subtype demonstrates genetic signals associated with ADHD and depression [112]. This stratification provides a framework for developing model systems that mirror specific ASD subgroups rather than attempting to model the entire spectrum with a single approach.
Neuroanatomical Stratification: Overgrowth vs. Undergrowth Phenotypes
Beyond behavioral and genetic classification, neuroanatomical differences provide another critical axis for stratification. Approximately 20% of individuals with ASD present with macrocephaly (head circumference above the 97th percentile), often accompanied by megalencephaly (brain enlargement) [15]. This macrocephalic ASD subgroup typically experiences more severe symptoms, including lower IQ, delayed language onset, and more significant social deficits [15]. In contrast, other ASD presentations may involve typical or reduced brain volume.
Brain overgrowth phenotypes in ASD demonstrate complex developmental trajectories. Some individuals exhibit precocious growth during early childhood followed by normalization during later childhood/adolescence, while others show persistent overgrowth throughout life [15]. Regional specificity varies, with some cases showing general overgrowth across frontal, temporal, and parietal lobes, while others demonstrate specific structural enlargement in areas like the amygdala or hippocampus [15].
Recent evidence challenging traditional overgrowth narratives comes from a 2025 study examining perinatal brain development in relation to later autistic traits. This research found that reduced total brain volume in the first two months of life was associated with higher numbers of autistic traits at 18 months, suggesting that early undergrowth rather than overgrowth may characterize some ASD presentations [38]. This finding highlights the importance of developmental timing and subtype specificity in model selection.
Table 1: Comparative Analysis of ASD Subgroups Based on Brain Growth Patterns
| Feature | Macrocephalic ASD Subgroup | Non-Macrocephalic ASD Subgroup |
|---|---|---|
| Prevalence | ~20% of ASD cases [15] | ~80% of ASD cases [15] |
| Head/Brain Size | Head circumference >97th percentile; Often megalencephaly [15] | Head circumference within normal range [15] |
| Symptom Severity | More severe: lower IQ, language delays, social deficits [15] | Variable severity [15] |
| Developmental Trajectory | Possible precocious growth with regression OR persistent overgrowth [15] | Recent evidence suggests early undergrowth may be associated with autistic traits [38] |
| Regional Specificity | General overgrowth or specific structures (amygdala, hippocampus) [15] | Regional variations; potential reduced volume [38] |
| Implications for Modeling | Requires models with increased neuronal production, decreased apoptosis, or neuronal hypertrophy [15] | May require models with different circuit organization or connectivity patterns |
Comparative Analysis of Model Systems
Genetic Model Systems
Genetic models represent a cornerstone of ASD research, with varying capabilities to recapitulate specific subtypes.
Fragile X Syndrome (FXS) models provide a genetically homogeneous system for understanding ASD associated with this specific monogenic cause. A 2025 study directly comparing young children with idiopathic ASD and FXS revealed distinct neuroanatomical signatures [68]. FXS was characterized by a complex pattern of regional volume alterations including significant gray matter volume increases in subcortical structures (particularly the caudate nucleus) and cerebellar Crus I, alongside substantial volume reductions in the frontal insular cortex and cerebellar vermis [68]. These findings provide a clear structural fingerprint for validating FXS models.
Idiopathic ASD models face greater challenges due to genetic heterogeneity. However, the identification of specific genetic programs associated with behavioral subtypes enables more targeted model development [112]. Models based on high-confidence ASD risk genes such as CHD8, SHANK3, or NRXN1 deletions must be evaluated against subtype-specific criteria rather than general ASD phenotypes.
Table 2: Experimental Data Comparing ASD and FXS Model Systems
| Parameter | Idiopathic ASD | Fragile X Syndrome (FXS) | Research Implications |
|---|---|---|---|
| Gray Matter Volume (GMV) Patterns | Accelerated GMV growth across brain regions [68] | Increased GMV in subcortical areas; Decreased GMV in cortical regions [68] | Distinct structural fingerprints suggest different underlying mechanisms |
| Growth Trajectories | Significantly accelerated GMV growth across most regions [68] | Growth similar to typical development or slower than ASD in cerebellar regions [68] | Aberrant growth acceleration may be specific to idiopathic ASD |
| Developmental Timing | Differences detectable in early childhood (ages 2-8) [68] | Pattern consistent across early childhood (ages 2-8) [68] | Early developmental windows critical for both disorders |
| Regional Specificity | Widespread differences across multiple brain regions [68] | Specific patterns: caudate nucleus increase, frontal insular cortex decrease [68] | FXS models must recapitulate specific regional alterations |
| Genetic Basis | Highly heterogeneous, polygenic [15] [112] | Monogenic (FMR1 mutation) [68] | FXS offers genetically defined modeling advantage |
In Silico and Computational Model Systems
Machine Learning (ML) approaches have emerged as powerful tools for ASD subtyping and prediction. Supervised ML methods using questionnaire data have demonstrated impressive accuracy in classifying ASD subtypes, with one study achieving an area under the curve (AUC) of 0.82 using combined assessment tools [113]. These computational approaches enable stratification of heterogeneous ASD populations into more homogeneous subgroups for targeted intervention.
Multimodal AI frameworks represent the cutting edge of computational approaches. A 2025 study developed a two-stage multimodal AI system that integrated voice data from parent-child interactions with semantically processed screening questionnaire data [114]. The framework achieved exceptional performance, with Stage 1 (differentiating typically developing from high-risk/ASD children) reaching an AUROC of 0.942, and Stage 2 (distinguishing high-risk from ASD children) achieving an AUROC of 0.914 [114]. This approach demonstrates how computational models can integrate diverse data modalities to achieve clinically relevant stratification.
Automated machine learning (AutoML) systems further streamline the development of predictive models. A study applying the Tree-based Pipeline Optimization Tool (TPOT) to ASD detection achieved 78% accuracy, with precision of 83%, recall of 90%, and F1-score of 86% for the autistic class [115]. These automated approaches increase accessibility and reproducibility of computational models for ASD research.
Diagram 1: Multimodal AI Framework for ASD Risk Stratification
Experimental Protocols for Model Validation
Neuroanatomical Phenotyping Protocol
Objective: To quantitatively assess brain structure differences between ASD subgroups and validate model system recapitulation of human neuroanatomy.
Sample Preparation:
- Utilize T1-weighted structural MRI data from human participants and model systems
- Ensure consistent age-matching between human cohorts and model systems at equivalent developmental stages
- For human data: include typically developing controls, idiopathic ASD, and syndromic ASD (e.g., FXS) [68]
Image Acquisition Parameters:
- Implement voxel-based morphometry (VBM) for gray matter volume quantification
- Acquire high-resolution anatomical images with standardized protocols
- For longitudinal studies: establish regular imaging timepoints across development [68]
Data Analysis Pipeline:
- Preprocessing: spatial normalization, segmentation, smoothing
- Whole-brain analysis: identify regions of significant volume difference
- Region-of-interest (ROI) analysis: focus on structures implicated in ASD (amygdala, hippocampus, cerebellum, frontal cortex)
- Cross-species alignment: map human findings to equivalent regions in model systems
- Growth trajectory modeling: quantify developmental changes across age [68]
Validation Metrics:
- Statistical significance of volume differences between groups
- Effect sizes for regional volume alterations
- Developmental trajectory correlations between model systems and human subgroups
Multi-modal Behavioral Assessment Protocol
Objective: To comprehensively characterize behavioral phenotypes across ASD models and human subtypes.
Social Communication Assessment:
- Implement standardized social approach tasks
- Quantify vocalization patterns in model systems
- Assess social reciprocity through structured interactions [114]
Repetitive Behavior Analysis:
- Score stereotyped motor movements
- Quantify insistence on sameness behaviors
- Assess restricted interests through choice paradigms [112]
Cognitive Function Evaluation:
- Administer learning and memory tasks
- Assess executive function through cognitive flexibility paradigms
- Evaluate attention through sustained attention tasks [112]
Data Integration:
- Apply machine learning approaches to identify behavioral clusters
- Correlate behavioral dimensions with neural circuit function
- Validate cross-species behavioral homology
Signaling Pathways and Molecular Mechanisms
The biological processes underlying brain overgrowth in macrocephalic ASD involve several interconnected signaling pathways that represent potential targets for therapeutic intervention.
PI3K-AKT-mTOR Pathway: This signaling cascade emerges as a central regulator of cell growth, proliferation, and survival in macrocephalic ASD. Gain-of-function mutations in upstream regulators lead to pathway overactivation, driving increased neuronal size and number through enhanced protein synthesis and suppressed apoptosis [15].
RAS-ERK Pathway: Activated by growth factors and synaptic activity, this pathway coordinates cell cycle progression and differentiation. Mutations in RASopathies demonstrate the consequence of pathway dysregulation, often resulting in macrocephaly and ASD features through altered neural progenitor proliferation [15].
WNT-β-catenin Signaling: Crucial for patterning and proliferation during brain development, excessive WNT signaling can expand progenitor pools and delay cell cycle exit. This pathway interacts with PI3K-AKT signaling, creating synergistic effects on brain growth [15].
Synaptic Signaling Pathways: Deficits in GABAergic and glutamatergic signaling contribute to excitation-inhibition imbalance in ASD. While not directly growth-promoting, these circuit-level abnormalities may indirectly influence neuronal survival and connectivity through activity-dependent mechanisms [15].
Diagram 2: Signaling Pathways in Macrocephalic ASD
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents for ASD Model System Characterization
| Reagent Category | Specific Examples | Research Application | Considerations for ASD Subgroups |
|---|---|---|---|
| Genetic Modifiers | CRISPR/Cas9 systems, Cre-lox lines, shRNA vectors | Specific genetic perturbation in model systems | Match genetic alterations to ASD subgroups (e.g., FMR1 KO for FXS) [68] |
| Cell Type Markers | NeuN (neurons), GFAP (astrocytes), Iba1 (microglia), Olig2 (oligodendrocytes) | Cell population quantification and analysis | Assess cell-type specific contributions to overgrowth/undergrowth [15] |
| Synaptic Markers | PSD-95, Synapsin, VGAT, VGLUT1, GAD65/67 | Synaptic density and excitation-inhibition balance evaluation | Critical for models with connectivity deficits vs. growth abnormalities [15] |
| Proliferation Assays | BrdU/EdU, Ki67, PH3 | Quantification of cell division and neurogenesis | Essential for validating models of brain overgrowth phenotypes [15] |
| Apoptosis Assays | TUNEL, cleaved caspase-3, Annexin V | Cell death quantification | Decreased apoptosis may contribute to macrocephaly in some subtypes [15] |
| Pathway Inhibitors/Activators | Rapamycin (mTOR), LY294002 (PI3K), CHIR99021 (WNT) | Functional validation of signaling pathways | Target specific pathways dysregulated in different ASD subgroups [15] |
| Behavioral Assessment Tools | Automated tracking systems, ultrasonic vocalization detection, social preference apparatus | Standardized behavioral phenotyping | Must align with specific ASD subtype behavioral profiles [112] |
| MRI Contrast Agents | Gadolinium-based agents, manganese-enhanced MRI | Structural and functional connectivity mapping | Enable cross-species comparison of neuroanatomical phenotypes [68] |
The comparative analysis of model systems for ASD research reveals that no single model adequately captures the spectrum's heterogeneity. Instead, a precision approach matching specific models to validated ASD subgroups offers the most promising path forward for therapeutic development. The critical distinction between overgrowth and undergrowth phenotypes, along with genetically defined subtypes, provides a framework for model selection and validation.
Future directions should prioritize the development of integrated models that combine genetic engineering with environmental factors, the creation of human cellular models (iPSCs) from genetically stratified populations, and the implementation of cross-species validation pipelines. Furthermore, as machine learning approaches advance, in silico models will play an increasingly important role in predicting therapeutic responses across subtypes.
For drug development professionals, this stratified approach suggests a shift from seeking universal ASD treatments to developing targeted interventions for specific biological subtypes. The benchmarking criteria established here—including neuroanatomical fidelity, behavioral relevance, and molecular pathway recapitulation—provide a framework for evaluating model systems throughout the drug discovery process. By aligning model systems with ASD subgroups based on their predictive validity for specific biological mechanisms, researchers can increase the translational potential of preclinical findings and ultimately deliver more effective, personalized interventions for autism spectrum disorder.
Conclusion
The comparative analysis of overgrowth and undergrowth models in ASD reveals a complex, multistage prenatal neuropathology. Key takeaways indicate that embryonic brain overgrowth, driven by genes like PTEN, is a strong predictor of later social symptom severity, while undergrowth models, such as those involving DYRK1A, present distinct therapeutic challenges and opportunities. The emergence of human iPSC-derived models provides an unprecedented window into these earliest developmental stages. Future research must prioritize the 'ASD Living Biology' approach, integrating longitudinal data from in vitro models to in vivo clinical presentation in each individual. This will be crucial for developing precision medicine strategies, where interventions are timed to specific critical windows and tailored to an individual's underlying growth phenotype, ultimately moving beyond a one-size-fits-all approach to ASD treatment.
References
- 1. Autism spectrum disorder: Neuropathology and animal models [https://pmc.ncbi.nlm.nih.gov/articles/PMC5693718/]
- 2. Neurocognitive mechanisms underlying autism spectrum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532009/]
- 3. Early Brain Overgrowth in Autism Associated with an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3315057/]
- 4. Autism spectrum disorders pathogenesis: Toward a ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2022.988735/full]
- 5. Patches of Disorganization in the Neocortex of Children ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4499461/]
- 6. COMPARED TO WHAT? EARLY BRAIN OVERGROWTH ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4837958/]
- 7. A holistic review of autism spectrum disorder mechanisms ... [https://www.sciencedirect.com/science/article/pii/S0969996125004048]
- 8. Biological implications of genetic variations in autism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8298259/]
- 9. Phenotypic effects of genetic variants associated with autism [https://www.nature.com/articles/s41591-023-02408-2]
- 10. Polygenic and developmental profiles of autism differ by ... [https://www.nature.com/articles/s41586-025-09542-6]
- 11. Advancing precision diagnosis in autism: Insights from large ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12275934/]
- 12. The Evolving Landscape of Functional Models of Autism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190894/]
- 13. Identification of a molecular network regulated by ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/38588587/]
- 14. Symptomatic, Genetic, and Mechanistic Overlaps between ... [https://www.mdpi.com/2218-273X/11/11/1635]
- 15. Mechanisms of brain overgrowth in autism spectrum ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1586550/full]
- 16. Diffusion trajectory of atypical morphological development in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12533118/]
- 17. Structural brain development between childhood and ... [https://www.sciencedirect.com/science/article/pii/S1053811916303512]
- 18. Perinatal brain growth and autistic traits in toddlers [https://www.nature.com/articles/s41398-025-03665-0]
- 19. Structural Growth Trajectories and Rates of Change in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4940157/]
- 20. Tracking regional brain growth up to age 13 in children ... [https://www.nature.com/articles/s41467-020-14334-9]
- 21. Clinical and Neurobiological Relevance of Current Animal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4859786/]
- 22. Brain Structural Plasticity: From Adult Neurogenesis to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7010851/]
- 23. Early Generalized Overgrowth in Autism Spectrum Disorder [https://pmc.ncbi.nlm.nih.gov/articles/PMC4173120/]
- 24. Early Generalized Overgrowth in Autism Spectrum Disorder [https://www.sciencedirect.com/science/article/abs/pii/S0890856714005309]
- 25. Profiling brain morphology for autism spectrum disorder with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325702/]
- 26. Early Generalized Overgrowth in Boys With Autism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4878118/]
- 27. Brain Overgrowth Linked to Autism Symptom Severity [https://neurosciencenews.com/brain-overgrowth-autism-genetics-27563/]
- 28. Cerebrospinal fluid biomarkers for brain tumor detection [https://pmc.ncbi.nlm.nih.gov/articles/PMC7191171/]
- 29. The Quiet Ego: A Meta-Analytical Review [https://link.springer.com/article/10.1007/s10902-025-00923-2]
- 30. Development and validation of the Self-Awareness of Ego ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12266406/]
- 31. Age of machine learning: new trends in autism spectrum ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1492484/full]
- 32. The Evolving Landscape of Functional Models of Autism ... [https://www.mdpi.com/2073-4409/14/12/908]
- 33. Monogenic Mouse Models of Autism Spectrum Disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC4803542/]
- 34. Gene editing in monogenic autism spectrum disorder [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2022.1043018/full]
- 35. Developmental Disturbances in Animal Models of Autism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12152516/]
- 36. Cell Bank Reveals Autism's Genetic Roots [https://www.technologynetworks.com/genomics/news/cell-bank-reveals-autisms-genetic-roots-400835]
- 37. Shared and divergent alteration of whole-brain connectivity ... [https://www.nature.com/articles/s41380-025-03340-2]
- 38. Perinatal brain growth and autistic traits in toddlers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623961/]
- 39. Generation of Cerebral Organoids from Human Pluripotent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4160653/]
- 40. to reach new neurological disease frontiers Brain organoids [https://www.news-medical.net/whitepaper/20250523/Brain-organoids-to-reach-new-neurological-disease-frontiers.aspx]
- 41. The ASD Living Biology: from cell proliferation to clinical ... [https://www.nature.com/articles/s41380-018-0056-y]
- 42. Altered proliferation and networks in neural cells derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5215991/]
- 43. Analysis of neuronal activity impairment in iPSC-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12546973/]
- 44. Human Pluripotent Stem Cell-Derived Models and Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8193821/]
- 45. Induced pluripotent stem cells (iPSCs) [https://www.nature.com/articles/s41392-024-01809-0]
- 46. Voxel-Based Morphometry: An Automated Technique for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6666603/]
- 47. Developmental brain structural atypicalities in autism: a voxel ... [https://capmh.biomedcentral.com/articles/10.1186/s13034-022-00443-4]
- 48. Studying Autism Spectrum Disorder with Structural and ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2016.00211/full]
- 49. Comparison of Different Methodological Implementations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2739382/]
- 50. Brain structure in autism: A voxel-based morphometry analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5010794/]
- 51. Identifying and Predicting Autism Spectrum Disorder Based ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2021.765517/full]
- 52. A voxel-based morphometry comparison of regional gray ... [https://www.sciencedirect.com/science/article/abs/pii/S0925492709001139]
- 53. Assessment of Brain Morphological Abnormalities and ... [https://www.mdpi.com/1422-0067/26/15/7062]
- 54. Quantifying individual differences in brain morphometry ... [https://www.nature.com/articles/s41598-019-45774-z]
- 55. Auditory brainstem response in infants and children with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5836986/]
- 56. Early neurophysiological markers of aberrant auditory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12175640/]
- 57. Brain mapping across 16 autism mouse models reveals a ... [https://www.nature.com/articles/s41380-021-01245-4]
- 58. Auditory brainstem responses as a biomarker for cognition [https://pmc.ncbi.nlm.nih.gov/articles/PMC11659319/]
- 59. Latency Characteristics of Auditory Brainstem Responses to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580943/]
- 60. Promising Autism Research Breakthroughs in 2025 [https://linksaba.com/promising-autism-research-breakthroughs/]
- 61. Decomposition of phenotypic heterogeneity in autism ... [https://www.nature.com/articles/s41588-025-02224-z]
- 62. Major autism study uncovers biologically distinct subtypes, ... [https://www.princeton.edu/news/2025/07/09/major-autism-study-uncovers-biologically-distinct-subtypes-paving-way-precision]
- 63. Person-focused approach explains distinct autism genetic ... [https://www.news-medical.net/news/20250715/Person-focused-approach-explains-distinct-autism-genetic-subtypes.aspx]
- 64. Preclinical models for autism spectrum disorder [https://pubmed.ncbi.nlm.nih.gov/41203106/]
- 65. Repurposed epilepsy drugs show potential for new autism ... [https://www.drugtargetreview.com/news/184268/repurposed-epilepsy-drugs-show-potential-for-new-autism-therapies/]
- 66. The Evolving Landscape of Functional Models of Autism ... [https://pubmed.ncbi.nlm.nih.gov/40558535/]
- 67. Autism: A “Critical Period” Disorder? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3150222/]
- 68. Prof. Rihui Li's team Uncovers Distinct and Developing ... [https://ccbs.ici.um.edu.mo/prof-rihui-lis-team-uncovers-distinct-and-developing-brain-anatomy-in-young-children-with-autism-and-fragile-x-syndrome/]
- 69. Critical periods and Autism Spectrum Disorders, a role for ... [https://www.sciencedirect.com/science/article/pii/S2451994422000141]
- 70. Neurodevelopment of Autism: Critical Periods, Stress and ... [https://www.mdpi.com/2073-4409/13/23/1968]
- 71. Cerebellar impairments in genetic models of autism ... [https://www.sciencedirect.com/science/article/pii/S0301008224001217]
- 72. Longitudinal changes in children with autism spectrum ... [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1546001/full]
- 73. Why Are Autism Spectrum Conditions More Prevalent in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3114757/]
- 74. Women in Autism [https://autism.org/women-in-autism/]
- 75. Gene expression in human brain implicates sexually ... [https://www.nature.com/articles/ncomms10717]
- 76. Frontiers | Characterizing autism spectrum disorders by key biochemical pathways [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2015.00313/full]
- 77. Unmasking autism: gender differences in diagnostic ... [https://www.frontiersin.org/journals/education/articles/10.3389/feduc.2025.1552943/full]
- 78. Sex-Related Measurement Bias in Autism Spectrum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12334962/]
- 79. Pten Mutations Alter Brain Growth Trajectory and Allocation of Cell Types through Elevated β-Catenin Signaling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6605343/]
- 80. Towards understanding sex differences in autism spectrum ... [https://www.sciencedirect.com/science/article/pii/S0006899324001318]
- 81. Advancing autism research: Insights from brain organoid ... [https://www.sciencedirect.com/science/article/pii/S0959438825000613]
- 82. Brain organoids: a new paradigm for studying human ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1699814/full]
- 83. Review Preclinical models for autism spectrum disorder [https://www.sciencedirect.com/science/article/abs/pii/S0306452225010619]
- 84. Extracellular vesicle profiling reveals novel autism ... [https://www.nature.com/articles/s41398-025-03607-w]
- 85. Modelling idiopathic autism in forebrain organoids reveals an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10573709/]
- 86. Quantifying Organoid Size and Counts: Solving a Common ... [https://www.oxford-optronix.com/resources/quantifying-organoid-size-and-counts]
- 87. Autism spectrum disorder related phenotypes in a mouse ... [https://pubmed.ncbi.nlm.nih.gov/40078324/]
- 88. Iteration of Tumor Organoids in Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566727/]
- 89. An Efficient Organoid Cutting Method for Long-Term ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12209159/]
- 90. 2025 Trends: Organoids [https://www.genengnews.com/topics/genome-editing/2025-trends-organoids/]
- 91. Autism Spectrum Disorder (ASD) and Fragile X Syndrome (FXS) [https://pmc.ncbi.nlm.nih.gov/articles/PMC4493458/]
- 92. Neurobiological basis of autism spectrum disorder [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2025.1558081/full]
- 93. Trajectories of Early Brain Volume Development in Fragile X and Autism RH: Trajectory of Brain Volume in Fragile X - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3428739/]
- 94. Age-Varying Distinct Neuroanatomy in Young Children with ... [https://sciety-labs.elifesciences.org/articles/by?article_doi=10.21203/rs.3.rs-7070338/v1]
- 95. Age-varying distinct neuroanatomy in young children with autism spectrum disorder and fragile X syndrome | Molecular Psychiatry [https://www.nature.com/articles/s41380-025-03350-0]
- 96. Imaging study discovers brain development differences in kids ... [https://med.stanford.edu/news/all-news/2010/05/imaging-study-discovers-brain-development-differences-in-kids-with-fragile-x-syndrome.html]
- 97. Trajectories of Early Brain Volume Development in Fragile ... [https://www.sciencedirect.com/science/article/abs/pii/S0890856712004996]
- 98. Age-Varying Distinct Neuroanatomy in Young Children ... [https://www.researchsquare.com/article/rs-7070338/latest]
- 99. Neural systems for social cognition: gray matter volume ... [https://pubmed.ncbi.nlm.nih.gov/26233431/]
- 100. No significant brain volume decreases or increases in ... [https://www.sciencedirect.com/science/article/abs/pii/S0925492714001292]
- 101. A perturbed gene network containing PI3K–AKT, RAS ... [https://www.nature.com/articles/s41593-019-0489-x]
- 102. A perturbed gene network containing PI3K/AKT, RAS/ERK ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6764590/]
- 103. A perturbed gene network containing PI3K-AKT, RAS-ERK ... [https://pubmed.ncbi.nlm.nih.gov/31551593/]
- 104. Safety findings from the phase 1/2 MOSAIC study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12296598/]
- 105. Targeting PI3K/Akt signal transduction for cancer therapy [https://www.nature.com/articles/s41392-021-00828-5]
- 106. A synaptic molecular dependency network in knockdown of ... [https://www.sciencedirect.com/science/article/pii/S2211124723004412]
- 107. A Comparative Perspective on the Cerebello-Cerebral System ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10657313/]
- 108. Autism spectrum disorders and neuropathology of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4635214/]
- 109. Embryonic Brain Overgrowth Dictates Autism Severity, New ... [https://today.ucsd.edu/story/embryonic-brain-overgrowth-dictates-autism-severity-new-research-suggests]
- 110. Comparative neuronal morphology of the cerebellar cortex ... [https://www.frontiersin.org/journals/neuroanatomy/articles/10.3389/fnana.2014.00024/full]
- 111. Comparative neuronal morphology of the cerebellar cortex in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4005950/]
- 112. New Autism Subtypes Identified Based on Genes, ... [https://www.brainfacts.org/diseases-and-disorders/childhood-disorders/2025/new-autism-subtypes-identified-based-on-genes-individual-traits-111125]
- 113. Development and Validation of Prediction Models for the ... [https://www.sciencedirect.com/science/article/pii/S2949732924000425]
- 114. Multimodal AI for risk stratification in autism spectrum ... [https://www.nature.com/articles/s41746-025-01914-6]
- 115. Early Detection of Autism Spectrum Disorder Through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346167/]