Autism as a Complex Systems Disorder: Decoding Biological Heterogeneity for Precision Therapeutics
This article synthesizes the latest research reconceptualizing Autism Spectrum Disorder (ASD) as a complex systems disorder, moving beyond a monolithic condition to a convergence of distinct biological subtypes.
Autism as a Complex Systems Disorder: Decoding Biological Heterogeneity for Precision Therapeutics
Abstract
This article synthesizes the latest research reconceptualizing Autism Spectrum Disorder (ASD) as a complex systems disorder, moving beyond a monolithic condition to a convergence of distinct biological subtypes. For researchers and drug development professionals, we explore the foundational shift towards data-driven subtyping, methodological advances in computational genomics and neuroscience, the challenges in translating these findings into targeted therapies, and the comparative validation of this new framework against traditional models. The analysis integrates recent breakthroughs, including the identification of four biologically distinct ASD subtypes, novel genetic mechanisms like tandem repeat expansions, and emerging therapeutic targets, providing a roadmap for a new era of precision medicine in autism.
Deconstructing the Monolith: The Biological Subtypes and Genetic Architecture of Autism
The nosology of autism is undergoing a fundamental transformation, moving from a behaviorally-defined unitary spectrum towards a data-driven framework of biologically distinct subtypes. This paradigm shift is propelled by accumulating evidence that autism spectrum disorder (ASD) represents a heterogeneous collection of conditions with diverse genetic underpinnings, developmental trajectories, and neurobiological mechanisms. This whitepaper examines the evolution of autism diagnostic criteria, synthesizes recent breakthroughs in subtype identification, and details the methodological innovations enabling this transition. For researchers and drug development professionals, these advances provide a critical foundation for precision medicine approaches in autism research and therapeutic development.
The diagnostic conceptualization of autism has evolved substantially since Leo Kanner's initial description in 1943 [1]. Originally characterized as a form of childhood schizophrenia resulting from psychological factors, autism was first officially recognized as a distinct diagnostic category in the DSM-III (1980) [1] [2]. This edition established autism as a "pervasive developmental disorder" with specific diagnostic criteria, marking a significant departure from previous psychoanalytic interpretations.
The subsequent revision in DSM-IV (1994) further complexified the diagnostic landscape by introducing categorical diagnoses including Asperger's disorder, childhood disintegrative disorder, Rett's disorder, and PDD-NOS (Pervasive Developmental Disorder Not Otherwise Specified) [3]. This proliferation of categories reflected the growing recognition of autism's heterogeneity while maintaining a primarily behavior-based classification system.
A substantial reorganization occurred with DSM-5 (2013), which collapsed previous categorical distinctions into a single umbrella diagnosis of autism spectrum disorder (ASD) [2] [3]. This shift to a spectrum model acknowledged the continuous nature of autistic traits while aiming to improve diagnostic consistency. However, this framework has faced increasing scrutiny due to the extreme heterogeneity within the spectrum and the failure to identify unified biological mechanisms that transcend behavioral observations [4].
The Case for a Paradigm Shift: Limitations of Current Nosology
Scientific and Clinical Limitations
The current spectrum model of autism faces significant challenges that necessitate a paradigm shift in nosology:
Biological Incoherence: Neurobiological research has failed to identify consistent patterns unique to ASD as defined by DSM-5. Genetic studies reveal polygenic, pleiotropic risk factors on a continuum with typical behavior rather than discrete categories [4]. Neuroimaging findings present mixed results with few unique patterns definitively attributable to the diagnosis [4].
Diagnostic Heterogeneity: The DSM-5 ASD diagnosis allows extreme within-category heterogeneity without validated sub-groupings [4]. Attempts to define meaningful subgroups within the spectrum have historically failed, complicating both research and clinical practice.
Lack of Predictive Power: Current diagnostic criteria show limited predictive power regarding developmental trajectories and intervention outcomes [4]. This limitation significantly impacts clinical management and therapeutic development.
Theoretical Frameworks in Psychiatric Nosology
The debate surrounding autism nosology reflects broader philosophical tensions in psychiatric classification:
- Realism posits that psychiatric disorders represent natural kinds with objective existence independent of human observation [4].
- Pragmatism views diagnostic categories as practical tools for organizing interventions and support systems regardless of their correspondence to natural divisions [4].
- Constructivism acknowledges the role of social and cultural factors in shaping diagnostic concepts while not entirely abandoning biological realism [4].
Kendler's "limited realism" suggests that a diagnosis is "real to the degree that it coheres well with what we know empirically and feel comfortable about" [4]. By this standard, ASD as currently defined falls short, as genetic, neurobiological, and behavioral findings fail to present a coherent picture of a unified entity [4].
Breakthrough Research: Data-Driven Subtype Identification
The Princeton-Simons Foundation Study
A landmark 2025 study from Princeton University and the Simons Foundation has marked a transformative step in autism nosology by identifying four clinically and biologically distinct subtypes of autism through analysis of data from over 5,000 children in the SPARK autism cohort [5]. The research employed a person-centered computational approach that analyzed over 230 traits per individual across social interactions, repetitive behaviors, and developmental milestones [5].
Table 1: Clinically Distinct Subtypes of Autism Identified in Recent Research
| Subtype Name | Prevalence | Clinical Presentation | Developmental Trajectory |
|---|---|---|---|
| Social and Behavioral Challenges | 37% | Core autism traits with co-occurring conditions (ADHD, anxiety, depression) | Typical developmental milestone attainment |
| Mixed ASD with Developmental Delay | 19% | Developmental delays in walking/talking, variable repetitive behaviors and social challenges | Later achievement of developmental milestones |
| Moderate Challenges | 34% | Milder expression of core autism behaviors, fewer co-occurring conditions | Typical developmental milestone attainment |
| Broadly Affected | 10% | Severe, wide-ranging challenges including developmental delays, social-communication difficulties, and co-occurring psychiatric conditions | Significant developmental delays across multiple domains |
Genetic Architecture of Autism Subtypes
Critically, each identified subtype demonstrates distinct genetic profiles:
- The Broadly Affected subgroup shows the highest proportion of damaging de novo mutations (those not inherited from parents) [5].
- The Mixed ASD with Developmental Delay group is more likely to carry rare inherited genetic variants [5].
- The Social and Behavioral Challenges subtype exhibits mutations in genes that become active later in childhood, suggesting post-natal biological mechanisms [5].
These findings indicate that superficially similar clinical presentations (e.g., developmental delays across subtypes) may have distinct genetic underpinnings, explaining why previous genetic studies searching for unified "autism genes" have largely fallen short [5].
Methodological Innovations: Enabling the Subtype Revolution
Person-Centered Computational Approach
The identification of biologically meaningful subtypes required moving beyond traditional analysis methods that examined single traits in isolation. Key methodological advances include:
- High-Dimensional Phenotyping: Comprehensive assessment of 230+ clinical and behavioral traits across multiple domains [5].
- Computational Modeling: Advanced machine learning algorithms to identify natural groupings across multidimensional data [5].
- Data Integration: Simultaneous analysis of genetic and clinical data to establish biologically-grounded classifications [5].
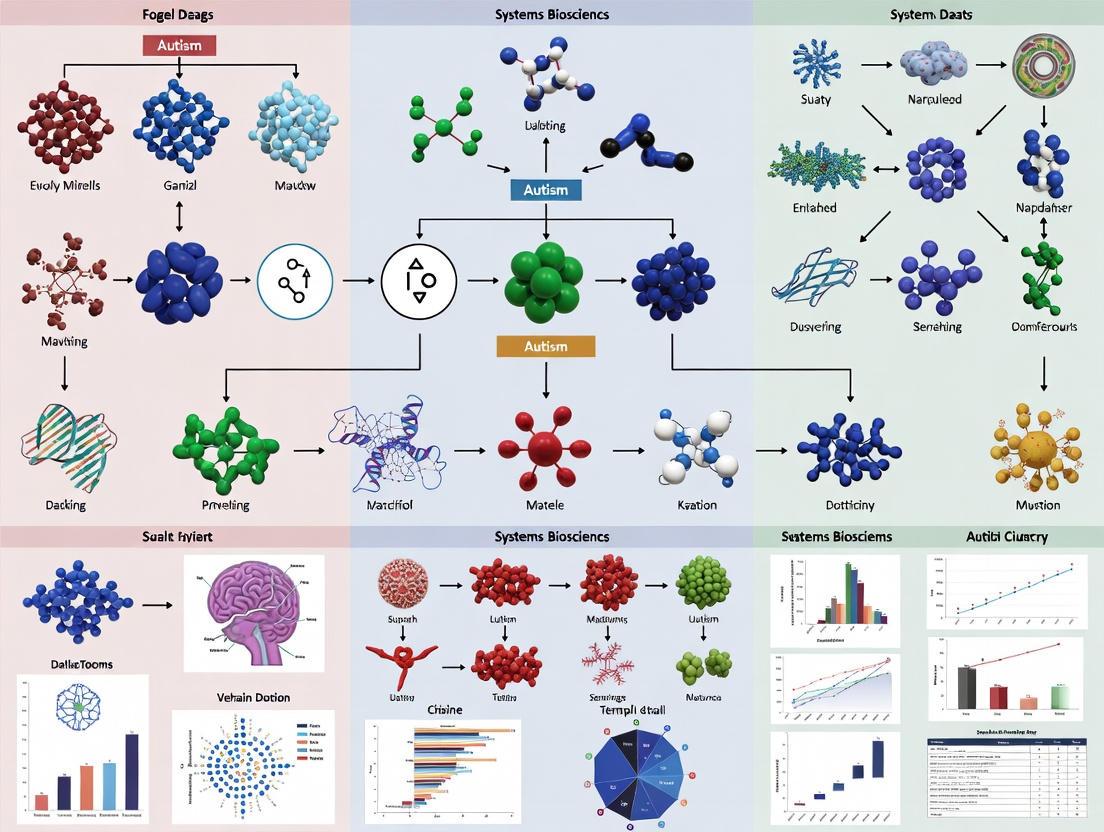
The following workflow diagram illustrates the comprehensive analytical process:
Table 2: Key Research Reagents and Resources for Autism Subtype Investigation
| Resource Type | Specific Examples | Research Application |
|---|---|---|
| Cohort Resources | SPARK cohort, Simons Simplex Collection | Large-scale participant data with deep phenotyping and genetic information |
| Genomic Tools | Whole exome sequencing, polygenic risk score analysis, gene expression profiling | Identification of genetic variants, inheritance patterns, and functional pathways |
| Computational Methods | Machine learning clustering algorithms, multidimensional scaling, factor analysis | Data-driven subtype identification from high-dimensional datasets |
| Clinical Assessment | ADOS-2, ADI-R, developmental history, psychiatric comorbidity measures | Standardized phenotyping across behavioral and clinical domains |
| Neurobiological Tools | fMRI (including sleeping-state fMRI), EEG, brain complexity measures (Sample Entropy, Transfer Entropy) | Investigation of neural structure, function, and connectivity differences |
Experimental Protocol: Subtype Identification Workflow
For researchers seeking to replicate or extend subtype identification, the following detailed methodology provides a framework:
Step 1: Participant Recruitment and Data Collection
- Recruit a minimum of 2,000 participants to ensure sufficient power for subtype detection
- Collect comprehensive phenotypic data across 200+ traits including social communication, repetitive behaviors, developmental milestones, medical history, and psychiatric comorbidities
- Obtain genetic material for whole genome or exome sequencing
- Secure informed consent following institutional review board protocols
Step 2: Data Integration and Cleaning
- Harmonize data across collection sites using standardized scoring procedures
- Implement quality control measures for genetic data including variant calling standardization
- Address missing data using appropriate imputation methods
- Create unified database linking phenotypic and genetic information
Step 3: Computational Modeling and Subtype Identification
- Apply multiple clustering algorithms (k-means, hierarchical clustering, Gaussian mixture models) to identify robust subgroups
- Validate cluster stability through bootstrapping and cross-validation techniques
- Determine optimal number of clusters using statistical indices (e.g., silhouette score, Bayesian information criterion)
- Characterize resulting subtypes based on distinctive feature profiles
Step 4: Genetic Validation
- Compare genetic variant burden across identified subtypes
- Conduct pathway enrichment analysis to identify distinct biological processes
- Examine differences in inherited versus de novo variation patterns
- Assess polygenic risk scores for psychiatric conditions across subtypes
Step 5: Clinical Validation
- Examine developmental trajectories across subtypes using longitudinal data
- Compare treatment responses and outcomes across subgroups
- Assess comorbidity patterns and medical correlates
- Validate subtypes in independent cohorts to ensure generalizability
Neurobiological Underpinnings of Autism Subtypes
Brain Complexity and Connectivity
Emerging research reveals distinct neurobiological differences associated with autism presentations. A 2025 sleeping-state functional MRI study investigated brain complexity in children with ASD compared to typically developing children, employing sample entropy (SampEn) and transfer entropy (TE) analyses [6]. Findings indicated that children with ASD showed significantly increased SampEn in the right inferior frontal gyrus, suggesting aberrant randomness in local brain activity [6].
Furthermore, investigation of information flow between brain regions revealed that the typically developing group exhibited 13 pairs of brain regions with higher TE compared to the ASD group, while the ASD group showed 5 pairs of brain regions with higher TE than controls [6]. These findings demonstrate anomalous information transmission between brain regions in ASD, providing potential biomarkers for distinguishing neurobiological subtypes.
Differential Genetic Pathways and Timing Effects
The identification of autism subtypes has revealed distinct biological narratives rather than a single unified story [5]. Crucially, genetic impacts appear to operate on different developmental timelines across subtypes:
- For the Social and Behavioral Challenges subtype, mutations occur in genes that become active later in childhood, suggesting post-natal biological mechanisms [5].
- The Broadly Affected subgroup shows strongest genetic signals in genes active during early neurodevelopment [5].
- Distinct biological pathways are affected in each subtype, explaining differential clinical presentations and outcomes [5].
The following diagram illustrates the distinct genetic and biological pathways underlying autism subtypes:
Implications for Research and Therapeutic Development
Impact on Clinical Trials and Drug Development
The recognition of biologically distinct autism subtypes has profound implications for therapeutic development:
- Stratified Clinical Trials: Future clinical trials must recruit based on biological subtypes rather than behavioral diagnoses alone to detect meaningful treatment effects.
- Targeted Interventions: Therapies can be developed to address specific pathway disruptions in each subtype rather than employing one-size-fits-all approaches.
- Biomarker Development: Subtype-specific biomarkers will enable earlier identification and intervention matching.
- Outcome Measurement: Clinical trials must incorporate subtype-appropriate outcome measures that reflect the distinct challenges of each subgroup.
Future Research Directions
This paradigm shift opens several critical research avenues:
- Expanding Subtype Classification: Current findings of four subtypes represent a starting point rather than a final taxonomy [5]. Further refinement is expected as sample sizes increase and analytical methods improve.
- Longitudinal Validation: Tracking subtype trajectories across the lifespan will provide crucial insights into developmental courses and intervention timing.
- Mechanistic Studies: Detailed investigation of subtype-specific biological pathways will identify novel therapeutic targets.
- Global Representation: Ensuring diverse population representation in subtype research to avoid biases inherent in current predominantly Western cohorts [4].
The identification of biologically distinct autism subtypes represents a fundamental paradigm shift from behaviorally-defined spectra to data-driven nosology. This transformation, enabled by advanced computational approaches integrating multidimensional data, provides a framework for realizing precision medicine in autism research and clinical care. For researchers and drug development professionals, these advances offer the potential to develop targeted interventions based on underlying biological mechanisms rather than surface-level behavioral similarities. As this field rapidly evolves, embracing this new nosological framework will be essential for advancing both scientific understanding and clinical outcomes for autistic individuals.
Recent large-scale, person-centered computational analyses have revolutionized the understanding of Autism Spectrum Disorder (ASD) by decomposing its profound phenotypic heterogeneity into biologically meaningful subtypes [5] [7]. This whitepaper synthesizes a landmark study that integrated deep phenotypic and genotypic data from over 5,000 individuals within the SPARK cohort to define four clinically and biologically distinct ASD subtypes [5]. Framed within the context of autism as a complex systems disorder, this work demonstrates that the spectrum is composed of multiple discrete "puzzles," each with unique genetic architectures, developmental trajectories, and altered neurobiological pathways [5] [8]. The identification of these subtypes—Social and Behavioral Challenges, Mixed ASD with Developmental Delay, Moderate Challenges, and Broadly Affected—provides a foundational data-driven framework for precision medicine, offering new avenues for targeted diagnostics, mechanistic research, and therapeutic development [5] [7].
Autism Spectrum Disorder is a quintessential complex systems disorder, characterized by emergent properties arising from dynamic interactions across genetic, neural circuit, and behavioral levels [8]. Traditional diagnostic approaches, focusing on a unitary set of core social and repetitive behaviors, have failed to capture this systemic complexity, leading to inconsistent genetic associations and limited progress in targeted interventions [5]. The inherent heterogeneity suggests not a single continuum but a multiplicity of distinct neurodevelopmental pathways converging on a similar phenotypic landscape [7]. This perspective necessitates a shift from a trait-centered to a person-centered analytical paradigm, which considers the full spectrum of over 230 clinical traits per individual to model the system as a whole [5]. The following sections detail a transformative study that applied this complex systems lens, leveraging large-scale data integration and machine learning to identify robust subtypes, thereby mapping distinct biological narratives onto the clinical heterogeneity of ASD [5] [7].
Experimental Protocols & Computational Methodology
Cohort and Data Acquisition
The research utilized data from the SPARK (Simons Foundation Powering Autism Research) cohort, the largest study of autism to date, which includes genetic and deep phenotypic data from over 150,000 individuals with autism and family members [7]. For this analysis, phenotypic and genotypic data from more than 5,000 participants with autism, aged 4–18, were analyzed [7]. The phenotypic data encompassed a broad range of over 230 traits, including social interaction challenges, repetitive behaviors, developmental milestones (e.g., age of walking, talking), co-occurring psychiatric conditions (ADHD, anxiety, depression), and medical histories [5]. Genetic data included whole-exome or genome sequencing to identify inherited and de novo variants [5].
Computational Subtyping Algorithm
The core methodology employed a person-centered, data-driven approach using general finite mixture modeling [7].
- Model Selection: Instead of examining single traits in isolation (trait-centered), the model considered the complete phenotypic profile of each individual. Finite mixture modeling was chosen for its unique ability to handle heterogeneous data types (binary yes/no, categorical, continuous) within a single probabilistic framework [7].
- Integration and Clustering: The model integrated the diverse phenotypic measures to calculate a probability for each individual belonging to a latent class or subtype. This allowed individuals to be grouped based on shared multidimensional phenotypic profiles [5] [7].
- Validation and Genetic Correlation: The subtypes derived purely from phenotypic data were subsequently analyzed for enrichment of specific genetic variants (e.g., damaging de novo mutations, rare inherited variants) and distinct biological pathways using gene set enrichment and functional genomics analyses [5].
Supplementary Neuroimaging Protocol (Example of Complexity Analysis)
Complementary to genetic discovery, investigating the systems-level neurobiology of ASD involves protocols like sleep-state functional magnetic resonance imaging (ss-fMRI) to assess brain complexity, as exemplified in related research [9].
- Participant Preparation: Children (e.g., aged 12-36 months) undergo adaptive training to acclimate to the MRI environment. Scanning is performed during natural sleep without sedation, a sensitive state for detecting neurodevelopmental anomalies [9].
- Data Acquisition: MRI datasets are acquired using a 3.0T scanner with a multi-channel head coil. High-resolution T1-weighted anatomical images and resting-state (sleep-state) fMRI sequences (e.g., TR/TE=2000/30 ms, voxel size=3x3x3 mm³) are collected [9].
- Complexity Analysis: Brain complexity is quantified using metrics like Sample Entropy (SampEn) to assess local signal randomness and Transfer Entropy (TE) to measure directed information flow between brain regions, capturing both aberrant local activity and anomalous network communication [9].
Diagram Title: Data-Driven ASD Subtyping Workflow
Results: The Four Subtypes and Their Quantitative Profiles
The finite mixture model robustly identified four subtypes, each with a distinct clinical profile and genetic signature. The quantitative characteristics are summarized below.
Table 1: Clinical and Demographic Profiles of ASD Subtypes
| Subtype | Approximate Prevalence | Core Clinical Presentation | Developmental Milestones | Common Co-occurring Conditions |
|---|---|---|---|---|
| Social & Behavioral Challenges | 37% | Pronounced social challenges and repetitive behaviors. | Typically on pace with children without autism. | High rates of ADHD, anxiety, depression, OCD, mood dysregulation [5] [7]. |
| Mixed ASD with Developmental Delay | 19% | Mixed presentation of social/repetitive behaviors with developmental delay. | Delays in milestones (e.g., walking, talking). | Generally absent of anxiety, depression, or disruptive behaviors [5] [7]. |
| Moderate Challenges | 34% | Core autism behaviors present but less severe. | Typically on pace. | Generally absent of co-occurring psychiatric conditions [5] [7]. |
| Broadly Affected | 10% | Severe and wide-ranging challenges across all domains. | Significant developmental delays. | High rates of anxiety, depression, mood dysregulation, intellectual disability [5] [7]. |
Table 2: Distinct Genetic and Biological Characteristics
| Subtype | Key Genetic Findings | Implicated Biological Pathways (Examples) | Timing of Genetic Effect |
|---|---|---|---|
| Social & Behavioral Challenges | Not specified as having highest burden of de novo mutations. | Neuronal action potential, synaptic signaling. | Genes active postnatally, aligning with later diagnosis [5] [7]. |
| Mixed ASD with Developmental Delay | Enriched for rare inherited genetic variants [5]. | Chromatin organization, transcriptional regulation. | Genes active prenatally [5] [7]. |
| Moderate Challenges | Genetic profile less extreme than other groups. | Pathways distinct from other classes (specifics not detailed). | Not specified. |
| Broadly Affected | Highest proportion of damaging de novo mutations [5]. | Multiple pathways involved in severe neurodevelopmental disruption. | Likely prenatal and early postnatal. |
Biological Mechanisms: Signaling Pathways and Systems Dysregulation
The subtypes are driven by divergent biological narratives. Pathway analysis revealed minimal overlap between subtypes, with each linked to specific, previously implicated but now subclass-distinct mechanisms [7].
- Neuronal Signaling & Synaptic Function: Particularly relevant to the Social and Behavioral Challenges subtype, pathways involving neuronal excitability, action potentials, and synaptic transmission are disrupted [7] [8]. This aligns with postnatally active genes and may relate to findings of altered brain complexity, such as increased local entropy in frontal regions [9].
- Chromatin Remodeling & Transcriptional Regulation: This mechanism is prominently associated with the Mixed ASD with Developmental Delay subtype, enriched for inherited variants affecting genes active during prenatal development [5] [7]. Dysregulation here impacts broad neurodevelopmental programs.
- Integrated Systems View: ASD pathophysiology can be visualized as the convergence of multiple risk pathways onto final common circuits, such as the mTOR signaling pathway (integrating genetic, synaptic, and metabolic inputs) or immune-inflammatory responses, which may modulate severity across subtypes [8].
Diagram Title: Biological Pathways Converge on ASD Subtypes
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Solutions for ASD Subtype & Mechanisms Research
| Item | Function / Application | Relevance to Featured Research |
|---|---|---|
| SPARK Cohort Data | Large-scale, integrated repository of genotypic and deep phenotypic data from individuals with ASD. | Foundational resource for person-centered computational subtyping and genetic correlation studies [5] [7]. |
| General Finite Mixture Modeling Software | Computational framework for clustering heterogeneous data types (R packages, Python libraries). | Core algorithm for identifying latent subtypes from multidimensional phenotypic vectors [7]. |
| Whole Genome Sequencing Kits | Reagents for high-throughput sequencing of coding and non-coding genomic regions. | Essential for identifying de novo and rare inherited variants associated with specific subtypes [5]. |
| Sleep-state fMRI Protocol | Tailored MRI sequences and participant acclimation procedures for scanning sleeping infants/children. | Enables study of early brain development and complexity (SampEn, TE) in naturalistic states, critical for understanding neural systems pathology [9]. |
| Pathway Enrichment Analysis Tools | Software (e.g., GSEA, Ingenuity) and curated gene-set databases. | For translating genetic hit lists from each subtype into distinct biological pathways and processes [5] [7]. |
| Induced Pluripotent Stem Cell (iPSC) Differentiation Kits | Reagents to derive neuron/glia from patient fibroblasts, specific to a subtype's genetic background. | Enables in vitro modeling of subtype-specific cellular and molecular pathophysiology [8]. |
| Animal Models with Subtype-Relevant Mutations | Genetically engineered mice or organoids carrying human variant homologs. | For testing causal mechanisms and potential therapeutics within a defined biological narrative [8]. |
Autism spectrum disorder (ASD) presents a profound genetic paradox. Despite high heritability estimates, no single genetic locus accounts for more than a fraction of cases, pointing to a complex architecture involving multiple genetic factors operating across different biological scales. The emerging "multi-hit" model resolves this paradox by proposing that ASD risk emerges from combinatorial effects of rare and common genetic variants that collectively disrupt neurodevelopmental processes. This framework represents a fundamental shift from single-gene determinism to a systems-level understanding where autism manifests through interactions between various genetic "hits" that converge on critical biological pathways and networks.
Groundbreaking research published in 2023 analyzing the largest whole-genome sequencing cohort of multiplex families to date provides compelling evidence for this model, demonstrating that autistic children from these families "demonstrate an increased burden of rare inherited protein-truncating variants in known ASD risk genes" and that "ASD polygenic score (PGS) is overtransmitted from nonautistic parents to autistic children who also harbor rare inherited variants, consistent with combinatorial effects in the offspring" [10]. These findings establish a concrete genetic foundation for understanding autism as a complex systems disorder wherein the total mutational burden and its interaction with polygenic background determine phenotypic outcomes.
Genetic Architecture of Autism: Deconstructing the Multi-Hit Framework
Variant Classes in Autism Risk
The multi-hit model integrates three principal classes of genetic variation that contribute to ASD susceptibility through distinct mechanisms and effect sizes [11]:
Table 1: Genetic Variant Classes in Autism Spectrum Disorder
| Variant Class | Population Frequency | Effect Size | Heritability Contribution | Transmission Pattern |
|---|---|---|---|---|
| Rare De Novo | <1% | Large (OR > 10) | 15-20% | Not inherited; spontaneous |
| Rare Inherited | 1-5% | Moderate (OR 2-5) | ~10-15% | Familial transmission |
| Common Variants | >5% | Small (OR <1.2) | ~50% | Polygenic inheritance |
This integrated model explains key aspects of autism inheritance that were previously puzzling, particularly why "autism tends to run in families" despite the strong association with de novo mutations [11]. The multi-hit framework posits that in multiplex families, inherited rare variants combine with a favorable polygenic background to reach the threshold for autism manifestation, whereas in simplex families, large-effect de novo mutations may be sufficient to cross this threshold independently.
Evidence for Combinatorial Effects
The 2023 whole-genome sequencing study of 4,551 individuals from 1,004 multiplex families provides robust evidence for interactive effects between different variant classes. The research identified "seven previously unrecognized ASD risk genes supported by a majority of rare inherited variants," finding support for a total of 74 genes in their cohort and 152 genes after combined analysis with other studies [10]. Crucially, the study demonstrated that common ASD genetic risk is "overtransmitted from nonautistic parents to autistic children with rare inherited variants," explaining the "reduced penetrance of these rare variants in parents" [10]. This combinatorial risk architecture follows an additive threshold model where the total genetic burden determines phenotypic expression.
Further supporting this model, researchers have found that "people who have both a large spontaneous mutation linked to autism as well as a rare, inherited harmful mutation are more affected than those who carry only the former" [11]. This gene-gene interaction (epistasis) exemplifies the multi-hit principle where the combined effect of multiple variants exceeds the sum of their individual effects, creating emergent properties through nonlinear dynamics characteristic of complex systems.
Diagram 1: Multi-Hit Threshold Model of Autism Genetic Risk. This diagram illustrates how different classes of genetic variants combine additively and interactively to exceed the threshold for ASD diagnosis. Rare de novo variants (red), rare inherited variants (yellow), and common polygenic risk (blue) collectively contribute to total genetic liability, with combinatorial effects (dashed lines) potentially creating non-additive impacts that push total risk above the diagnostic threshold.
Methodological Framework: Experimental Approaches for Elucidating Multi-Hit Architecture
Whole-Genome Sequencing in Multiplex Families
The 2023 PNAS study established a comprehensive methodological pipeline for investigating multi-hit genetics in ASD [10]. The research utilized the largest whole-genome sequencing cohort of multiplex families to date, consisting of 1,004 families with two or more autistic children, amplifying the signal of inherited risk factors often obscured in simplex families. The experimental workflow encompassed:
Sample Collection and Processing: The study sequenced 4,551 individuals from the Autism Genetic Resource Exchange (AGRE) at mean coverage >30× with 80.6% of bases covered at ≥30×, ensuring high-quality variant detection. Participants included 1,836 autistic children and 418 nonautistic children with both biological parents sequenced (fully-phaseable trios) to enable transmission pattern analysis [10].
Variant Calling and Annotation: The pipeline employed an Artifact Removal by Classifier (ARC) to distinguish true rare de novo variants from sequencing errors or artifacts from lymphoblastoid culture. This quality control step was crucial for reducing false positives in variant detection. Variants were categorized as:
- Rare de novo variants (RDNVs)
- Rare inherited protein-truncating variants (PTVs)
- Rare inherited missense variants
- Common variants for polygenic risk scoring
Burden Analysis: The researchers compared variant rates between autistic and nonautistic children using logistic regression, examining different functional classes (PTVs, missense variants) and genomic contexts (highly constrained genes with pLI ≥ 0.9 or LOEUF < 0.35) [10].
Diagram 2: Experimental Workflow for Multi-Hit Genetic Analysis. This diagram outlines the comprehensive pipeline used in recent large-scale studies to identify and integrate different classes of genetic risk variants for ASD, from sample collection through multi-hit integration analysis.
Polygenic Risk Scoring Methodologies
The calculation of polygenic risk scores (PGS) represents a critical methodological component for quantifying common variant contribution. The 2023 study computed ASD PGS for participants of European ancestry, representing "the weighted sum of their common variants tied to autism" [12]. The technical approach involved:
Reference GWAS Data: Utilizing the largest available genome-wide association study summary statistics for ASD to define effect sizes (beta coefficients) for common variants across the genome.
PGS Calculation: Implementing standardized PGS software such as PRSice-2 or PRS-CS to calculate individual risk scores based on genotype data [13]. These tools apply clumping and thresholding or Bayesian shrinkage methods to optimize predictive accuracy.
Overtransmission Analysis: Testing whether PGS was significantly overtransmitted from parents to autistic children using linear mixed models that account for familial relatedness, with specific focus on children carrying rare inherited variants [10].
Recent methodological advances enable more sophisticated rare variant polygenic risk scores (rvPRS). A 2025 study in Communications Biology established that "single-SNP-based rvPRS outperform gene-burden models, and imputed genotype-derived rvPRS generally surpass WES-derived models," providing an optimized protocol for rare variant risk quantification [13]. For six of twelve validated traits, "combined tPRS (cvPRS + rvPRS) improves prediction over cvPRS alone," demonstrating the value of integrated risk models [13].
Research Reagents and Computational Tools
Table 2: Essential Research Reagents and Computational Tools for Multi-Hit Studies
| Resource Type | Specific Tool/Resource | Function | Application in ASD Studies |
|---|---|---|---|
| Sequencing Platforms | Illumina Whole-Genome Sequencing | High-coverage variant discovery | Identifies rare de novo and inherited variants [10] |
| Variant Callers | GATK, Platypus | SNP/indel detection | Standardized variant calling across cohorts |
| Quality Control | Artifact Removal by Classifier (ARC) | Filters technical artifacts | Distinguishes true RDNVs from sequencing errors [10] |
| Gene Constraint Metrics | pLI, LOEUF | Quantifies gene tolerance to variation | Prioritizes variants in constrained genes [10] |
| PGS Software | PRSice-2, PRS-CS | Polygenic risk score calculation | Quantifies common variant burden [13] |
| Statistical Packages | R, PLINK, GCTA | Genetic association testing | Burden analysis, heritability estimation [10] [13] |
| Functional Annotation | ANNOVAR, VEP | Variant functional prediction | Prioritizes deleterious missense/PTV variants |
Key Findings: Empirical Support for the Multi-Hit Model
Genetic Evidence from Multiplex Families
The analysis of multiplex families has yielded particularly compelling evidence for the multi-hit model. The 2023 study revealed that:
Table 3: Key Genetic Findings from Multiplex Family Studies
| Finding Category | Specific Result | Statistical Evidence | Interpretation |
|---|---|---|---|
| Novel Gene Discovery | 7 previously unrecognized ASD risk genes | FDR < 0.1 | Genes primarily supported by rare inherited variants [10] |
| Rare Inherited Burden | Increased PTV burden in ASD risk genes | P < 0.05 (specific values not reported) | Confirms contribution of inherited rare variation [10] |
| PGS Overtransmission | Higher PGS in autistic children with rare inherited variants | Significant overtransmission (P < 0.05) | Common variants compound rare variant effects [10] [12] |
| Language Association | PGS associated with social dysfunction and language delay | Significant association (P < 0.05) | Suggests language as core biological feature [10] |
| De Novo Depletion | Reduced RDNV burden in multiplex vs simplex families | Significant depletion (P < 0.05) | Different genetic architecture in multiplex families [10] |
These findings collectively demonstrate that "autism's heritability in families stems from a combination of both common and rare inherited variants that team up to hit a threshold in some people" [12]. The evidence supports an "additive complex genetic risk architecture of ASD involving rare and common variation" [10] that operates differently across family types.
Phenotypic Correlations and Clinical Implications
Beyond genetic risk quantification, the multi-hit model provides explanatory power for understanding phenotypic heterogeneity in ASD. The 2023 study made the crucial observation that "in addition to social dysfunction, language delay is associated with ASD PGS overtransmission" [10]. This finding has significant clinical implications as it suggests that "language is a core biological feature of ASD," despite not being a core clinical criterion in current diagnostic frameworks [10].
The multi-hit model also explains variability in expressivity among carriers of the same rare variant. For example, "only about 20 percent of people with a mutation in 16p11.2 — among the strongest risk factors for autism — have the condition; all have some combination of other traits, such as developmental delay, obesity and language problems" [11]. This variability likely depends on "the rest of a person's genetic background," [11] consistent with modifier effects from common polygenic risk.
Research Gaps and Future Directions
Despite significant advances, key challenges remain in fully elucidating autism's multi-hit architecture. Current studies are limited by:
Ancestral Diversity: Most large-scale genetic studies have focused primarily on European ancestry populations, limiting generalizability of polygenic risk scores across ancestries.
Non-Coding Variation: The role of regulatory variants in multi-hit models remains underexplored, though the 2023 study began investigating "noncoding regions of the genome" [10].
Functional Validation: While statistical genetic evidence is accumulating, functional validation of multi-hit interactions in model systems represents a critical next step.
Future research directions should include:
- Expanded whole-genome sequencing in diverse ancestral populations
- Development of multi-ancestry polygenic risk scores
- Functional studies of gene-gene interactions in neurodevelopment
- Integration of epigenetic and transcriptomic data to understand mechanistic pathways
- Prospective studies of genetic risk accumulation across development
The multi-hit model continues to evolve as empirical evidence accumulates, offering an increasingly sophisticated framework for understanding autism's complex etiology and guiding therapeutic development toward pathway-based interventions rather than gene-specific approaches.
Autism spectrum disorder (ASD) represents a paradigm of neurodevelopmental complexity, where clinical heterogeneity reflects multifaceted biological underpinnings. Framing autism as a complex systems disorder necessitates understanding how distinct genetic perturbations converge onto shared molecular pathways. Emerging evidence positions tandem repeat expansions (TREs) and their disruption of RNA splicing as a critical mechanism contributing to this complexity [14] [15]. These repetitive DNA sequences, comprising 2-20 base pair motifs repeated in tandem, demonstrate extensive polymorphism in the human genome, with over 37,000 motifs identified across nearly 32,000 distinct genomic regions [14]. Their expansion beyond normal thresholds introduces system-wide perturbations, particularly through disrupting the precise regulation of alternative splicing essential for neurodevelopment. This whitepaper examines how TREs constitute a previously underappreciated source of genetic variation in ASD, operating through mechanisms that align with complex systems principles—where small, recurrent genetic variations at multiple loci produce emergent effects on neural circuitry and clinical presentation.
Quantitative Evidence: Tandem Repeat Expansions in Autism
Genome-Wide Burden and Prevalence
Large-scale genomic studies have quantified the significant contribution of tandem repeat expansions to autism etiology. A landmark study analyzing 17,231 genomes revealed that rare tandem repeat expansions in gene-associated regions demonstrate a statistically significant increased prevalence in individuals with autism (23.3%) compared to unaffected siblings (20.7%), suggesting a collective contribution to autism risk of approximately 2.6% [14]. The research identified 2,588 loci where rare TREs were significantly more prevalent in autism-affected individuals than population controls, with these expansions particularly enriched in exonic regions, near splice junctions, and in genes related to nervous system development [14].
Table 1: Prevalence of Tandem Repeat Expansions in Autism Studies
| Study Population | Sample Size | TRE Prevalence in ASD | TRE Prevalence in Controls | Contribution to ASD Risk |
|---|---|---|---|---|
| MSSNG/SSC Cohorts | 17,231 genomes | 23.3% (affected children) | 20.7% (unaffected siblings) | ~2.6% [14] |
| Myotonic Dystrophy Type 1 (DM1) | N/A | ~14% (in DM1 population) | ~1% (general population) | 14-fold increased risk [15] |
Genomic Distribution and Characteristics
Tandem repeats demonstrate non-random distribution throughout the genome, with distinctive patterns relevant to their functional impact:
- Motif Size Distribution: The majority (72.2%) of repeat tracts have motifs <7 bp, with 2 bp motifs being most common (27.7%) [14]. Even-numbered motif sizes (2, 4, 6 bp) significantly outnumber odd-numbered sizes (3, 5 bp) in smaller size ranges [14].
- Sequence Composition: Motifs are predominantly (>40%) AC- or AG-rich, with only 0.4% composed exclusively of C or G nucleotides [14].
- Genomic Location: TREs are enriched in GC-rich regions and fragile sites but depleted within conserved DNA sequences and 3' untranslated regions [14]. They correlate strongly with cytogenetic fragile sites, co-localizing with 9 of 11 (81.8%) molecularly mapped rare folate-sensitive fragile sites [14].
Table 2: Characteristics of Tandem Repeats in the Human Genome
| Characteristic | Pattern/Observation | Functional Significance |
|---|---|---|
| Motif Size | 72.2% <7 bp; 2 bp most common (27.7%) | Influences detectability and expansion potential |
| Sequence Bias | >40% AC- or AG-rich; only 0.4% C- or G-only | Affects DNA structure and protein binding properties |
| Genomic Distribution | Enriched in fragile sites (OR=1.12; p=1.2×10⁻⁴) | Links to genome instability regions |
| Gene Region Enrichment | Upstream (OR=1.33) and 5' UTR (OR=1.2) regions | Potential impact on gene regulation |
| Exonic Depletion | Reduced in exons (OR=0.61) and 3' UTR (OR=0.43) | Suggests selective pressure against coding expansions |
Molecular Mechanisms: From Genetic Expansion to Splicing Disruption
RNA Toxicity and Protein Sequestration
The molecular pathway linking TREs to autism pathogenesis involves a toxic RNA mechanism that disrupts normal splicing regulation. Research connecting myotonic dystrophy type 1 (DM1) and autism has revealed that expanded repeats in the DMPK gene produce "toxic RNA" that binds to and sequesters RNA-binding proteins (RBPs), particularly muscleblind-like (MBNL) proteins [15]. This sequestration creates a functional protein deficiency, preventing these splicing regulators from performing their normal functions in processing other RNA transcripts. The resulting imbalance affects multiple genes involved in brain development and function, ultimately contributing to autistic symptoms [15]. This mechanism represents a systems-level disruption where a single genetic variation produces cascading effects across the transcriptome.
Splicing Regulation in Neurodevelopment
Alternative splicing is particularly critical in the nervous system, where it generates exceptional proteomic diversity necessary for proper neural development and function. RNA-binding proteins including PTBP, RBFOX, and FMRP (fragile X mental retardation protein) are essential for neurogenesis, axon guidance, synapse formation, and synaptic plasticity [16]. The regulation of splicing involves a complex network of RBP interactions, where proteins such as serine-/arginine-rich (SR) proteins generally promote exon inclusion, while heterogeneous nuclear ribonucleoproteins (hnRNPs) typically inhibit exon inclusion [16]. When TREs disrupt this finely balanced system, the consequences are particularly severe in neural tissue, where splicing diversity is highest.
Figure 1: Molecular Pathway from Tandem Repeat Expansions to ASD Symptoms
Autism Subtypes and Genetic Heterogeneity
Biologically Distinct Subtypes
Recent research has identified four clinically and biologically distinct subtypes of autism, each with different genetic profiles and developmental trajectories [5] [17]. This stratification helps explain the heterogeneous relationship between TREs and clinical presentation:
- Social and Behavioral Challenges Subtype (37% of participants): Characterized by core autism traits without developmental delays, and frequent co-occurring conditions like ADHD, anxiety, and depression [5].
- Mixed ASD with Developmental Delay (19%): Features developmental delays but generally absence of anxiety, depression, or disruptive behaviors [5].
- Moderate Challenges (34%): Milder core autism behaviors with typical developmental milestone achievement [5].
- Broadly Affected (10%): Severe, wide-ranging challenges including developmental delays, social-communication difficulties, and co-occurring psychiatric conditions [5].
Genetic Correlates of Subtypes
These subtypes demonstrate distinct genetic patterns relevant to TRE mechanisms. The Broadly Affected subtype shows the highest burden of damaging de novo mutations, while the Mixed ASD with Developmental Delay group is more likely to carry rare inherited variants [5]. Importantly, the Social and Behavioral Challenges subtype—which typically has substantial social and psychiatric challenges but no developmental delays—involves mutations in genes that become active later in childhood, suggesting the biological mechanisms may emerge postnatally [5]. This temporal dimension aligns with how TRE effects might manifest at different developmental timepoints.
Experimental and Diagnostic Approaches
Detection Methodologies
Advancements in detecting tandem repeat expansions have been crucial to understanding their role in autism. The following table summarizes key methodological approaches:
Table 3: Diagnostic and Research Methods for Tandem Repeat Expansion Detection
| Method | Principle | Advantages | Limitations |
|---|---|---|---|
| ExpansionHunter Denovo (EHdn) [14] | Computational algorithm detecting repeats from short-read sequencing | Works irrespective of prior knowledge; detects 2-20 bp motifs | Limited by read length for very large expansions |
| Repeat-Primed PCR (RP-PCR) [18] | PCR with primers binding repetitive sequences | Highly sensitive for detecting expansions | Does not provide precise sizing |
| Southern Blotting [18] | DNA fragment hybridization | Gold standard for large expansions; provides sizing | Time-consuming; requires large DNA samples |
| Long-Read Sequencing [18] | Sequencing long DNA fragments | Accurate for large, complex repeats; can detect methylation | Higher cost; limited accessibility |
| Nanopore Cas9-Targeted Sequencing [18] | Cas9-assisted targeted sequencing | Precise, targeted analysis; cost-effective for specific regions | Complex setup; specialized equipment |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Tandem Repeat and Splicing Studies
| Reagent/Resource | Function/Application | Key Features |
|---|---|---|
| ExpansionHunter Denovo [14] | Genome-wide TRE detection from short-read data | Detects motifs of 2-20 bp without prior knowledge |
| SPARK Cohort Data [5] [17] | Large-scale genetic and phenotypic data | 50,000+ families; genetic data with detailed trait information |
| RNA-Binding Protein Databases [16] | Cataloguing RBP-binding sites | Identifies potential protein targets of toxic RNA |
| Repeat-Primed PCR Assays [18] | Screening for specific repeat expansions | Sensitive detection of expanded alleles |
| Antisense Oligonucleotides (ASOs) [18] [19] | Experimental therapeutic approach | Target specific RNA sequences to modulate splicing |
Figure 2: Experimental Workflow for TRE Detection and Validation
Therapeutic Implications and Future Directions
RNA-Targeted Therapeutic Strategies
The mechanistic understanding of TRE-mediated splicing disruption has enabled development of targeted therapeutic approaches:
- Antisense Oligonucleotides (ASOs): These synthetic nucleic acid strands can bind to expanded repeat RNAs, blocking their toxic interactions with RBPs or triggering degradation pathways [18] [19]. ASOs have demonstrated success through mechanisms like allele-specific knockdown and splice modulation [18].
- Small Molecule Interventions: Research has identified small molecules that selectively bind structured RNA repeats, potentially stimulating their decay via endogenous pathways like the exosome complex [20]. In Fuchs endothelial corneal dystrophy, one such molecule facilitates intron excision and degradation of the toxic repeat-containing RNA [20].
- Gene Editing Technologies: Emerging CRISPR-Cas systems offer potential for directly correcting repeat expansions at the DNA level, though this approach remains primarily investigational [18].
Precision Medicine Approaches
The identification of autism subtypes with distinct genetic profiles enables more targeted therapeutic development [5] [17]. For instance, individuals in the Broadly Affected subtype, with their high burden of de novo mutations, might benefit from different intervention strategies than those in the Social and Behavioral Challenges subtype, where mutations affect genes active later in childhood [5]. This stratification moves the field toward personalized approaches based on an individual's specific genetic and biological subtype.
Tandem repeat expansions and their disruption of RNA splicing represent a significant genetic mechanism in autism spectrum disorder, accounting for approximately 2.6% of autism risk and providing a mechanistic link between genetic variation and neurodevelopmental pathology. The complex systems perspective reveals how these expansions introduce cascading perturbations throughout the RNA processing network, particularly through toxic RNA sequestration of splicing regulators. The recent identification of biologically distinct autism subtypes further refines our understanding of how different genetic profiles, including TREs, manifest in particular clinical presentations. Ongoing advances in detection methodologies, particularly long-read sequencing and specialized computational tools, continue to uncover the full scope of TRE contributions to autism. Most promisingly, the elucidation of these mechanisms has enabled development of targeted therapeutic strategies, including antisense oligonucleotides and small molecule approaches, that may eventually allow precision interventions for specific genetic subtypes of autism.
Autism spectrum disorder (ASD) is a complex neurodevelopmental condition characterized by persistent deficits in social communication and interaction, as well as restricted, repetitive patterns of behavior, interests, or activities. These features are associated with atypical early brain development and connectivity [21]. While ASD has been traditionally associated with molecular genetic alterations, recent research highlights that the timing of genetic disruptions during neurodevelopment plays a crucial role in determining clinical heterogeneity and phenotypic expression [5] [22]. The emerging paradigm recognizes autism not as a single disorder but as a collection of neurodevelopmental conditions with varying underlying biological narratives that unfold across different developmental timelines [5].
The human brain develops through a series of carefully orchestrated, sequential processes beginning in fetal life and continuing into adolescence. These include neural induction and patterning, neurogenesis, neuronal migration, neuronal morphogenesis (axonal and dendritic outgrowth), synaptogenesis, and synaptic pruning [22]. While earlier developmental processes such as neurogenesis are largely experience-independent, later processes including synaptic refinement are highly experience-dependent and influenced by environmental factors [22]. Genetic disruptions occurring at distinct points along this developmental continuum appear to produce different subtypes of autism with characteristic clinical presentations, trajectories, and comorbidities.
Genetic Architecture of ASD and Temporal Dynamics
The genetic architecture of autism is highly heterogeneous, involving hundreds of genetic loci that contribute to disease risk through varied mechanisms. These include single gene mutations, monogenic disorders, copy number variants (CNVs), and chromosomal abnormalities [23]. ASD is highly familial, with studies reporting a heritability of 70-90%, confirmed by twin studies showing concordance rates of 70-90% in monozygotic twins compared to 30-40% in dizygotic twins [23]. However, the specific clinical manifestations and developmental trajectories associated with these genetic risks are increasingly recognized as being determined by when during neurodevelopment these genetic programs are disrupted.
Polygenic Factors and Developmental Timing
Recent evidence reveals that the polygenic architecture of autism can be decomposed into genetically distinct factors associated with different developmental trajectories and ages at diagnosis [24]. Research demonstrates the existence of two modestly genetically correlated (rg = 0.38) autism polygenic factors:
- Factor 1: Associated with earlier autism diagnosis and lower social and communication abilities in early childhood, with only moderate genetic correlations with attention deficit-hyperactivity disorder (ADHD) and mental-health conditions
- Factor 2: Associated with later autism diagnosis and increased socioemotional and behavioural difficulties in adolescence, with moderate to high positive genetic correlations with ADHD and mental-health conditions [24]
These findings indicate that earlier- and later-diagnosed autism have different developmental trajectories and genetic profiles, supporting a developmental model of autism heterogeneity rather than a unitary model [24].
Table 1: Characteristics of Autism Polygenic Factors and Their Relationship to Developmental Timing
| Polygenic Factor | Age at Diagnosis | Developmental Trajectory | Genetic Correlations with Comorbidities | Early Childhood Social-Communication Abilities |
|---|---|---|---|---|
| Factor 1 | Earlier diagnosis | Difficulties emerge in early childhood and remain stable | Moderate correlations with ADHD and mental health conditions | Lower abilities |
| Factor 2 | Later diagnosis | Difficulties increase in late childhood/adolescence | High positive correlations with ADHD and mental health conditions | Increased difficulties emerge in adolescence |
Data-Driven Autism Subtypes and Genetic Programs
A groundbreaking 2025 study analyzing data from over 5,000 children in the SPARK autism cohort identified four clinically and biologically distinct subtypes of autism, each with distinct developmental trajectories and genetic programs [5] [17]. This person-centered approach considered over 230 traits in each individual rather than searching for genetic links to single traits, enabling the discovery of subtypes with distinct genetic profiles [5].
Table 2: Characteristics of Autism Subtypes and Their Associated Genetic Programs
| Autism Subtype | Prevalence | Developmental Milestones | Co-occurring Conditions | Genetic Features |
|---|---|---|---|---|
| Social and Behavioral Challenges | 37% | Typically reached on time | ADHD, anxiety, depression, OCD | Mutations in genes active later in childhood; highest genetic signals for ADHD and depression |
| Mixed ASD with Developmental Delay | 19% | Delayed walking and talking | Generally absent anxiety, depression, or disruptive behaviors | Highest proportion of rare inherited genetic variants |
| Moderate Challenges | 34% | Typically reached on time | Generally absent co-occurring psychiatric conditions | Milder genetic risk profile |
| Broadly Affected | 10% | Developmental delays present | Anxiety, depression, mood dysregulation | Highest proportion of damaging de novo mutations |
Critically, these subtypes differ in when genetic disruptions affect brain development. While much genetic impact was thought to occur prenatally, the Social and Behavioral Challenges subtype (typically with later diagnosis) shows mutations in genes that become active later in childhood, suggesting biological mechanisms may emerge postnatally [5]. This temporal dimension of genetic action provides a model for understanding autism diversity.
Experimental Approaches for Mapping Temporal Dynamics
Single-Cell Genomics and Brain Mapping
A groundbreaking UCLA Health study as part of the PsychENCODE consortium has provided unprecedented resolution in connecting genetic risk for autism to changes observed in the brain across development [25]. The researchers employed advanced single-cell assays to isolate and analyze genetic information from over 800,000 nuclei from post-mortem brain tissue of 66 individuals (ages 2 to 60, including 33 with ASD) [25]. This approach enabled identification of:
- Major cortical cell types affected in ASD (both neurons and glial cells)
- Specific vulnerability in neurons connecting brain hemispheres and somatostatin interneurons
- Transcription factor networks that drive observed changes
- Direct links between changes in ASD brains and underlying genetic causes [25]
Figure 1: Single-Cell Genomics Workflow for Mapping Temporal Dynamics in ASD
Longitudinal Phenotyping and Developmental Trajectories
Research using longitudinal data from birth cohorts has identified distinct socioemotional and behavioural trajectories associated with age at autism diagnosis [24]. Growth mixture modeling of Strengths and Difficulties Questionnaire (SDQ) data across multiple cohorts revealed:
- Early childhood emergent latent trajectory: Difficulties in early childhood that remain stable or modestly attenuate in adolescence
- Late childhood emergent latent trajectory: Fewer difficulties in early childhood that increase in late childhood and adolescence [24]
These trajectories are strongly associated with age at diagnosis, with the early childhood trajectory linked to earlier diagnosis and the late childhood trajectory associated with later diagnosis [24]. These associations remain robust after controlling for sociodemographic variables and in sensitivity analyses including individuals with co-occurring ADHD.
Artificial Intelligence and Gene Discovery
Researchers have developed artificial intelligence approaches that accelerate the identification of genes contributing to neurodevelopmental conditions [26]. This powerful computational tool analyzes patterns among genes already linked to neurodevelopmental diseases to predict additional genes that might also be involved. The approach incorporates:
- Gene expression data from developing human brain at single-cell resolution
- More than 300 biological features including mutation intolerance measures
- Protein interaction networks with known disease-associated genes
- Functional roles in biological pathways [26]
These models show exceptionally high predictive value, with top-ranked genes up to six-fold more enriched for high-confidence neurodevelopmental disorder risk genes compared to traditional genic intolerance metrics alone [26]. This approach helps validate genes emerging from sequencing studies that lack sufficient statistical proof of involvement in neurodevelopmental conditions.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents and Methodologies for Investigating Temporal Dynamics in ASD
| Research Tool Category | Specific Examples | Function/Application | Key Insights Enabled |
|---|---|---|---|
| Genomic Technologies | Single-cell RNA sequencing, Array comparative genomic hybridization (a-CGH), Next-generation sequencing (NGS) | Identification of genetic variants, gene expression patterns, and cellular heterogeneity | Cell-type specific expression changes in ASD; identification of de novo and inherited variants |
| Computational Tools | AI-based prediction models, Growth mixture models, Statistical genetic packages | Pattern recognition in large genomic and phenotypic datasets, trajectory analysis | Identification of autism subtypes; gene discovery; developmental trajectory mapping |
| Biological Samples | Post-mortem brain tissue banks, Saliva samples for DNA analysis, Longitudinal birth cohorts | Genetic and molecular profiling, developmental tracking | Brain region-specific changes; large-scale genetic studies; developmental course documentation |
| Model Systems | Mouse models (e.g., Pten-mutant, Mecp2-null), Human cell cultures, Cerebral organoids | Functional validation of genetic findings, mechanistic studies | Neuronal arborization abnormalities; synaptic function defects; circuit-level consequences |
Signaling Pathways and Molecular Mechanisms Across Development
Genetic studies have pinpointed several critical molecular processes in autism that operate across different developmental timelines [22]. These include: (1) regulation of gene expression; (2) pre-mRNA splicing; (3) protein localization, translation, and turnover; (4) synaptic transmission; (5) cell signaling; (6) cytoskeletal and scaffolding proteins; and (7) neuronal cell adhesion molecules [22]. While these molecular mechanisms appear broad, they may converge on specific steps during neurodevelopment that perturb neuronal circuitry structure, function, and plasticity.
Figure 2: Neurodevelopmental Processes and Associated ASD Subtypes Across Time
The timing of these molecular disruptions maps onto specific neurodevelopmental processes. For example, genes associated with the Broadly Affected autism subtype often impact early developmental processes, while those associated with the Social and Behavioral Challenges subtype typically affect later developmental processes such as synaptic refinement and circuit maturation [5] [22]. This temporal mapping provides a framework for understanding how genetic programs disrupt neurodevelopment at specific timepoints to produce distinct autism phenotypes.
Implications for Therapeutic Development and Precision Medicine
The recognition of temporally distinct genetic programs in autism has profound implications for therapeutic development. Rather than seeking a unified treatment for autism, this perspective suggests interventions should be timed and targeted to specific biological pathways active during different developmental windows [5] [22]. For individuals with genetic disruptions affecting early brain development, interventions might focus on promoting neuronal connectivity and circuit formation during critical periods. For those with later-onset genetic mechanisms, treatments might target synaptic function, refinement, and maintenance during childhood and adolescence.
The identification of biologically distinct subtypes enables a precision medicine approach to autism treatment [5] [17]. Understanding which genetic program and developmental trajectory an individual has could help clinicians anticipate challenges, select appropriate interventions, and predict long-term outcomes. Furthermore, this framework emphasizes that therapeutic windows may be specific to biological subtypes rather than applying uniformly across the autism spectrum.
The complex systems perspective on autism recognizes that genetic risks interact with environmental factors and developmental timing to produce diverse outcomes. This conceptualization moves beyond linear cause-effect models toward dynamic, developmental models that account for the emergence of autism phenotypes across time. Future research mapping the precise temporal sequences of genetic expression, brain development, and behavioral manifestation will be essential for developing targeted, effective interventions for different forms of autism.
The New Toolbox: Computational Biology, Multi-Omics, and Novel Therapeutic Targets
Harnessing AI and Machine Learning for Subtype Identification and Trajectory Prediction
Autism Spectrum Disorder (ASD) represents a quintessential example of a complex systems disorder, characterized by emergent phenotypes arising from dynamic, multi-scale interactions between genetic, molecular, neural circuit, and environmental factors [5] [27] [28]. The profound heterogeneity in clinical presentation, developmental trajectory, and treatment response has long hindered the development of targeted therapies and precise prognostic tools [29] [30]. Traditional categorical diagnostics fail to capture this multidimensional complexity, necessitating a paradigm shift towards data-driven, quantitative frameworks [28].
This whitepaper outlines how artificial intelligence (AI) and machine learning (ML) are revolutionizing ASD research by deconvoluting this heterogeneity. We detail computational methodologies for identifying biologically distinct subtypes and predicting individual developmental trajectories, thereby providing a roadmap for precision medicine in neurodevelopmental disorders [5] [31] [32].
AI/ML Methodological Framework for Deconstructing Heterogeneity
The core challenge is integrating high-dimensional, multimodal data—spanning genomics, phenomics, neuroimaging, and longitudinal behavioral assessments—to extract clinically and biologically meaningful patterns. The following AI/ML approaches are foundational.
2.1 Person-Centered Subtyping via Finite Mixture Modeling A transformative alternative to trait-centered analyses, this approach models the complete phenotypic profile of an individual to identify latent subgroups [5] [7].
- Experimental Protocol: As employed in the landmark SPARK cohort study (n>5,000), researchers utilized general finite mixture modeling to cluster individuals based on over 230 phenotypic traits [5] [7].
- Data Integration: Diverse data types (binary, categorical, continuous) are handled separately within the model and integrated into a single probability of class membership for each participant.
- Model Training: The algorithm estimates parameters that define latent classes, maximizing the likelihood that individuals within a class share a similar multivariate trait profile.
- Validation & Biological Correlation: Derived subtypes are validated for clinical coherence and then correlated with distinct genetic profiles (e.g., damaging de novo mutations, rare inherited variants) and divergent biological pathways [5].
2.2 Trajectory Prediction via Supervised Machine Learning Predicting longitudinal outcomes requires modeling the relationship between baseline features and future state.
- Experimental Protocol: A clinical cohort study (n=1,225) used latent class growth mixture modeling (LCGMM) to first identify distinct adaptive behavior trajectories, then applied supervised ML to predict trajectory membership from intake data [29].
- Outcome Definition (LCGMM): Repeated measures of Vineland Adaptive Behavior Scales (VABS-3) scores are modeled to identify clusters of individuals following similar growth curves (e.g., "Improving" vs. "Stable" trajectories) [29].
- Feature Engineering: Comprehensive intake data (socioeconomic status, developmental history, baseline symptom severity, co-occurring conditions, paternal age) is compiled [29].
- Model Training & Comparison: Algorithms like Random Forest, Support Vector Machine (SVM), and Elastic Net GLM are trained on a subset (n=729) to predict trajectory class. Performance is compared using accuracy, with Random Forest achieving ~77% accuracy in the cited study [29].
- Predictor Importance: The model is interrogated to identify the strongest baseline predictors of outcome (e.g., socioeconomic status, history of regression, baseline severity) [29].
AI/ML Workflow for Autism Research
Data Integration & Quantitative Trait Paradigm
A systems-level understanding requires moving beyond binary diagnosis to a spectrum of quantitative traits (QTs) that more closely reflect underlying biology [28].
- Key Data Sources: Large-scale cohorts like SPARK provide matched phenotypic and genetic data at an unprecedented scale [5] [7]. Longitudinal networks like the ADDM provide community-level prevalence and trend data [33] [34].
- Quantitative Traits: Measures like the Social Responsiveness Scale (SRS) and Broader Autism Phenotype Questionnaire (BAP-Q) capture continuous distributions of social communication and other core traits across clinical and general populations, offering greater statistical power and biological relevance [28].
Table 1: Key Quantitative Data from Featured Studies
| Study Focus | Cohort / Sample Size | Key Quantitative Finding | Source |
|---|---|---|---|
| Subtype Prevalence | SPARK (N > 5,000) | Social & Behavioral Challenges: ~37%; Mixed ASD with Developmental Delay: ~19%; Moderate Challenges: ~34%; Broadly Affected: ~10% | [5] |
| Trajectory Prediction Accuracy | Clinical Cohort (N = 729) | Random Forest model predicted adaptive behavior trajectory membership with ~77% accuracy. | [29] |
| Current ASD Prevalence (US) | ADDM Network (2022) | Approximately 1 in 31 (3.2%) 8-year-old children identified with ASD. | [34] [32] |
| Genetic Diagnostic Yield | Standard Care | Genetic testing explains etiology for ~20% of ASD patients. | [5] |
Core Findings: Subtypes, Trajectories & Biology
4.1 Four Biologically Distinct Subtypes The 2025 Nature Genetics study identified four subtypes with distinct clinical and genetic profiles [5] [7] [32]:
- Social & Behavioral Challenges (37%): Core ASD traits, typical developmental milestones, high co-occurring psychiatric conditions (ADHD, anxiety). Genetics involve genes active postnatally.
- Mixed ASD with Developmental Delay (19%): Significant developmental delays, fewer psychiatric conditions. Linked to rare inherited variants and genes active prenatally.
- Moderate Challenges (34%): Milder core traits, typical milestones, low psychiatric co-occurrence.
- Broadly Affected (10%): Severe, wide-ranging challenges including delay, core traits, and psychiatric conditions. Highest burden of damaging de novo mutations.
4.2 Predictors of Developmental Trajectory The trajectory prediction study highlighted that socioeconomic status, history of developmental regression, baseline symptom severity, and paternal age were stronger predictors of adaptive behavior outcome than cumulative hours of standard therapies like ABA [29].
Subtype-Linked Genetic & Pathway Differences
The Scientist's Toolkit: Essential Research Reagents & Platforms
Table 2: Key Research Reagent Solutions for AI-Driven ASD Research
| Item / Solution | Function in Research | Example / Note |
|---|---|---|
| SPARK Cohort Data | Provides large-scale, matched genotypic and deep phenotypic data essential for training robust AI models for subtyping. | Simons Foundation initiative; >150,000 individuals [5] [7]. |
| High-Throughput Sequencing Platforms | Enable whole exome/genome sequencing to identify genetic variants (de novo, inherited) for correlation with subtypes. | Critical for linking subtypes to distinct genetic architectures [5] [32]. |
| Quantitative Trait Assessment Batteries | Measure continuous distributions of core ASD traits (social communication, RRB) and co-occurring conditions. | SRS, BAP-Q, VABS-3 [29] [28]. |
| Cloud-Based Computational Infrastructure | Provides scalable resources (CPU/GPU) for running intensive mixture models, deep learning, and large-scale simulations. | Essential for analyzing multimodal "big data" [5] [31]. |
| FDA-Cleared Digital Phenotyping Tools | Provide objective, scalable measures of behavior (e.g., eye gaze, motor patterns) for model input. | EarliPoint (eye-tracking), tablet-based motor analysis apps [31]. |
| Biobank & Integrated 'Omics Data | Tissue/DNA samples linked to clinical data for exploring transcriptomic, proteomic, and metabolomic correlates of subtypes. | Enables mapping of biological pathways downstream of genetics [5] [27]. |
The integration of AI and ML represents a paradigm shift in autism research, transforming it from a search for a unified explanation to the dissection of a complex system into tractable, biologically coherent components [5] [32]. The identification of data-driven subtypes linked to distinct genetic mechanisms and developmental timelines provides a foundational framework for precision medicine. Future directions include:
- Incorporating non-coding genomic data and additional 'omics layers (transcriptomics, proteomics) [7].
- Validating subtypes and predictive models in prospective, independent cohorts.
- Using these frameworks to stratify patients for targeted clinical trials, moving beyond symptom-based to mechanism-based interventions [32]. This approach finally offers a path to align the complexity of autism's clinical presentation with the precision required for effective scientific discovery and therapeutic development.
Autism Spectrum Disorder (ASD) exemplifies a complex systems disorder where perturbations across multiple biological scales—from molecular splicing to neural circuitry—interact to produce behavioral outcomes. The integration of multi-omics data (genomics, transcriptomics, proteomics, metabolomics) is indispensable for mapping these cascading effects. This technical review delineates how initial genetic risks, mediated through mechanisms like alternative splicing and gut-brain axis communication, propagate through proteomic and metabolic networks to disrupt synaptic homeostasis, autophagy, and ultimately, neural circuit function. We synthesize findings from recent large-scale omics studies, provide detailed experimental workflows for key methodologies, and visualize critical signaling pathways. The synthesis underscores that therapeutic innovation in ASD necessitates a systems-level approach capable of interrogating these dynamic, cross-scale interactions.
The etiology of Autism Spectrum Disorder (ASD) is characterized by profound heterogeneity and polygenicity, with heritability estimates ranging from 64% to 91% [35] [36]. Traditional single-omics approaches have identified hundreds of risk loci but have struggled to explain the mechanistic pathways from genetic variation to circuit-level dysfunction and behavioral symptoms. The conceptualization of ASD as a complex systems disorder posits that its pathogenesis arises from the dynamic interplay of genetic susceptibility, environmental factors, and dysregulated biological networks across multiple organ systems, including the brain, immune system, and gastrointestinal tract [37] [8] [35].
Multi-omics integration provides the analytical framework to dissect this complexity. By concurrently analyzing data from genomes, transcriptomes, proteomes, and metabolomes, researchers can construct predictive models of how a mutation in a non-coding region influences RNA splicing, how the resulting aberrant protein disrupts synaptic phospho-signaling, and how gut microbiome-derived metabolites may modulate this process through peripheral immune activation [38] [39] [35]. This whitepaper details the core technical pathways and methodologies for mapping this cascade, providing a guide for researchers and drug development professionals aiming to identify coherent therapeutic targets within this entangled network.
Core Pathway: From Splicing to Circuit Dysfunction
Genetic Variation and Aberrant Splicing
The pathway to neural circuit dysfunction often originates with genetic variation that disrupts the precise regulation of alternative splicing (AS). AS is a critical RNA regulatory mechanism that allows a single gene to generate multiple mRNA and protein isoforms, and its dysregulation is a key contributor to ASD pathogenesis [19]. Splicing defects are particularly consequential for genes encoding synaptic cellular adhesion molecules (CAMs) and scaffold proteins, such as neurexins (NRXN), neuroligins (NLGN), and SHANK proteins [19] [40].
- Mechanism: Splicing of pre-mRNA is directed by the spliceosome, a complex of over 100 core proteins and modulators that recognize cis-regulatory motifs within introns and exons. Genetic variants (SNPs, rare mutations) can disrupt these cis-motifs or affect trans-acting splice factors, leading to aberrant splicing [40].
- Functional Impact: The specific spliceoform of a CAM determines its trans-synaptic binding partners. For example, alternative splicing of neuroligin mRNA, particularly at the AChE-like domain, regulates its affinity for α-neurexins and subsequently influences whether a synapse adopts an excitatory (glutamatergic) or inhibitory (GABAergic) phenotype [40]. Dysregulation of this process disrupts the excitatory/inhibitory (E/I) balance, a well-documented feature of ASD models.
- Evidence: Studies have identified atypical splicing patterns in ASD patients for genes including NLGN3, NLGN4X, NRXN1, SHANK3, and CADPS2 [19] [40]. A notable finding is that gut microbiota-derived neuroactive metabolites (e.g., 5-aminovaleric acid, taurine) can also regulate the alternative splicing of neuronal genes in the brain, creating a pathway for environmental modulation of genetic risk [35] [36].
The following diagram illustrates the central pathway from genetic and environmental perturbations to neural circuit dysfunction, integrating key findings from multi-omics studies.
Pathway from Multi-Omics Perturbations to ASD Phenotypes
The Gut Microbiota-Immunity-Brain Axis
A pivotal finding from multi-omics studies is that genetic risk does not operate solely within the brain. Cross-tissue regulatory mechanisms, particularly those involving the gut microbiota-immunity-brain axis, play a fundamental role [37] [38] [35]. Multi-omics meta-analyses have identified specific SNPs (e.g., rs2735307, rs989134) that exert cross-tissue effects by participating in gut microbiota regulation and immune pathways [37] [35] [36].
- Mechanism: Host genetics influences the composition of the gut microbiota. In turn, dysbiosis (characterized by reduced microbial diversity and shifts in taxa like Tyzzerella in ASD) leads to the production of bacterial metaproteins and metabolites (e.g., glutamate, DOPAC, SCFAs) that can cross the blood-brain barrier [38]. These molecules directly impact neurodevelopment and immune regulation.
- Immune Crosstalk: This axis also involves significant immune activation. Gut dysbiosis can trigger peripheral immune pathways, such as T cell receptor signaling and neutrophil extracellular trap formation. These signals are relayed to the brain, leading to neuroinflammation, characterized by microglial activation and altered cytokine profiles, which subsequently disrupts neuronal function and synaptic pruning [37] [35].
- Evidence: A multi-omics study of children with ASD revealed an altered host proteome response involving proteins like kallikrein (KLK1) and transthyretin (TTR), which are implicated in neuroinflammation and immune regulation [38]. Furthermore, gut microbiota from ASD patients have been shown to be sufficient to induce alternative splicing abnormalities in risk genes like FMR1 and Nrxn2 in animal models, directly linking the gut microbiome to the central splicing mechanism [35] [36].
Proteomic and Phosphoproteomic Convergence
The disruptions at the genetic, transcriptomic, and microbial levels converge at the proteome, with particular clarity revealed through global proteomics and phosphoproteomics. Studies on ASD mouse models (e.g., Shank3Δ4–22 and Cntnap2−/−) have identified that shared molecular changes frequently impact autophagy and mTOR signaling [39].
- Mechanism: Autophagy is a crucial cellular recycling process that maintains neuronal homeostasis. Phosphoproteomic analyses have identified unique phosphorylation sites in autophagy-related proteins (e.g., ULK2, RB1CC1, ATG16L1, ATG9) in ASD models, suggesting that altered phosphorylation impairs autophagic flux [39].
- Nitric Oxide Connection: A key finding links elevated nitric oxide (NO) from neuronal NO synthase (nNOS) to autophagy disruption. Inhibition of nNOS by 7-NI normalized autophagy markers in cell cultures and improved synaptic and behavioral phenotypes in mouse models, revealing a modifiable pathway [39].
- Evidence: In Shank3-deficient cells, elevated levels of LC3-II and p62 alongside reduced LAMP1 indicate autophagosome accumulation but impaired autophagosome-lysosome fusion, pointing to a blockage in the later stages of autophagy [39]. This dysfunction can lead to the accumulation of damaged proteins and organelles, contributing to synaptic deficits.
The table below summarizes key quantitative findings from recent multi-omics studies.
Table 1: Key Quantitative Findings from Multi-Omics Studies in ASD
| Omics Layer | Finding | Measurement/Model | Biological Implication |
|---|---|---|---|
| Genomics [35] | Identification of novel ASD-risk SNPs (rs2735307, rs989134) | Meta-analysis of 4 GWAS cohorts (>18k cases) | SNPs exert cross-tissue regulation via gut microbiota and immunity |
| Microbiomics [38] | Significantly lower microbial diversity & richness in ASD | 16S rRNA sequencing of 30 ASD vs. 30 control children | Characteristic community shuffling and reduced stability in gut ecosystem |
| Metabolomics [38] | Altered neurotransmitters (e.g., Glutamate, DOPAC) | Untargeted LC-MS/MS on fecal samples | Metabolites can cross BBB, contributing to neurodevelopmental dysregulation |
| Phosphoproteomics [39] | Altered phosphorylation of ULK2, RB1CC1, ATG16L1 | Cortex of Shank3Δ4–22 and Cntnap2−/− mice | Disrupted autophagic flux, a convergent pathway in ASD models |
| Transcriptomics [41] | SOX7 gene significantly associated and upregulated in ASD | Gene-based GWAS & RNA-seq (20 cases/19 controls) | Transcription factor involved in cell fate, a novel candidate gene |
Experimental Protocols for Multi-Omics Integration
To generate the data required for the analyses above, standardized yet advanced protocols are essential. Below are detailed methodologies for key omics workflows cited in the literature.
This protocol aims to characterize the functional output of the gut microbiome and its interaction with the host.
Sample Preparation:
- Homogenization: Rinse 1g of frozen fecal sample with cold PBS, homogenize for 15 minutes, and centrifuge at 300 × g at 4°C for 5 minutes to remove food debris.
- Protein Precipitation: Pool the supernatant and subject it to acetone precipitation overnight at -20°C. Recover proteins by centrifugation at 12,000 × g at 4°C for 30 minutes.
- Protein Digestion: Dissolve the protein pellet in lysis buffer (4% SDS, 100 mM Tris-HCl, pH 8.5). Reduce disulfide bonds with Tris(2-carboxyethyl)phosphine (TCEP). After another acetone precipitation, dissolve the lysate in 8M Urea. Perform protein quantification via bicinchoninic acid (BCA) assay. Digest proteins using trypsin following SDS-PAGE or filter-aided sample preparation (FASP).
Mass Spectrometry Analysis:
- LC-MS/MS for Metaproteomics: Analyze digested peptides using nano liquid chromatography-tandem mass spectrometry (LC-MS/MS) on a platform like TripleTOF 5600+. Use Information Dependent Acquisition (IDA) to fragment the most intense ions.
- LC-MS/MS for Metabolomics: For metabolite extraction, use 100 mg of fecal sample with 400 μl of pre-chilled extraction solvent (ACN:MeOH, 3:1). Analyze extracts using SWATH (Sequential Window Acquisition of all Theoretical Mass Spectra)-based LC-MS/MS for untargeted metabolome profiling.
Data Integration: Identify bacterial metaproteins and host proteins by searching MS/MS spectra against combined human and microbial databases. Correlate protein abundance with metabolite levels to identify potential functional relationships.
This protocol is designed to capture post-translational modifications that are central to signaling networks in the brain.
Tissue Processing and Protein Extraction:
- Dissection and Lysis: Dissect the cortical region from fresh or flash-frozen mouse brain (e.g., Shank3Δ4–22, Cntnap2−/−). Homogenize the tissue in a lysis buffer containing 8M Urea, protease inhibitors, and phosphatase inhibitors.
- Protein Digestion: Reduce and alkylate proteins. Digest the protein extract with trypsin overnight. Desalt the resulting peptides using C18 solid-phase extraction.
Phosphopeptide Enrichment and Analysis:
- Enrichment: Enrich phosphorylated peptides from the total peptide mixture using immobilized metal affinity chromatography (IMAC) or titanium dioxide (TiO2) tips.
- LC-MS/MS Analysis: Separate the enriched phosphopeptides using nano-flow LC and analyze them with a high-resolution mass spectrometer (e.g., Orbitrap). Use data-dependent acquisition or parallel accumulation–serial fragmentation (PASEF) for MS/MS.
- Data Processing: Identify and quantify phosphorylation sites by searching the MS/MS data against a mouse protein database. Use software like MaxQuant for peak picking, database search, and site localization. Perform pathway analysis on proteins with differentially expressed phosphorylation sites.
The workflow for this integrated analysis, from sample to insight, is visualized below.
Multi-Omics Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents and Solutions
The following table details key reagents, tools, and technologies that are foundational for conducting the multi-omics research described in this whitepaper.
Table 2: Essential Research Reagents and Solutions for ASD Multi-Omics
| Reagent / Technology | Specific Example | Function in Research |
|---|---|---|
| Animal Models | Shank3Δ4–22 mice [39]; Cntnap2−/− mice [39] | Model monogenic forms of ASD to study convergent molecular pathways (e.g., autophagy, synaptic proteomics). |
| nNOS Inhibitor | 7-Nitroindazole (7-NI) [39] | Pharmacological tool to investigate the role of nitric oxide signaling in autophagy disruption and behavioral phenotypes. |
| LC-MS/MS Systems | TripleTOF 5600+ [38]; Orbitrap series [39] | High-resolution mass spectrometry for untargeted metabolomics, metaproteomics, and phosphoproteomics. |
| Splicing Analysis Tools | Long-read sequencing (PacBio, Nanopore) [19]; Single-cell RNA-seq [19] | To fully characterize transcript isoforms and assess splicing heterogeneity across different cell types in the brain. |
| Bioinformatic Pipelines | BERTopic for literature mining [42]; HunFlair for NER [42]; SMR for Mendelian Randomization [35] | Tools for automating literature reviews, extracting biological entities, and integrating GWAS with QTL data. |
| Autophagy Markers | Antibodies for LC3-II, p62, LAMP1 [39] | Immunoblotting and immunofluorescence to assess autophagosome formation and lysosomal function in cellular and tissue models. |
The integration of multi-omics data is transforming our understanding of ASD from a collection of disparate symptoms into a coherent, albeit complex, systems disorder. The pathway from gene splicing to neural circuit dysfunction is not linear but a web of interacting networks spanning the genome, microbiome, immunome, and proteome. Key convergent pathways, such as dysregulated autophagy and gut-immune-brain signaling, are emerging as promising focal points for therapeutic intervention.
Future efforts must focus on the temporal dimension of these interactions through longitudinal multi-omics studies, and on increasing cellular resolution through widespread application of single-cell multi-omics technologies. Furthermore, the development of computational tools and AI-driven pipelines, like the literature mining model that analyzed 28,304 PubMed abstracts to identify trends in ASD research [42], will be crucial for synthesizing this ever-growing data into actionable biological insight. For drug development professionals, this systems-level map underscores that effective therapeutics may need to target peripheral systems like the gut or immune system, or critical convergence nodes like nNOS or mTOR, to successfully modulate the central neural circuits that underlie ASD behaviors.
Abstract This whitepaper elucidates the principles and methodologies of brain network neuroscience, with a specific focus on linking functional connectivity (FC) to behavioral phenotypes. Framed within the context of autism spectrum disorder (ASD) as a quintessential complex systems disorder [5] [21], we detail the experimental and computational pipelines that transform neuroimaging data into quantifiable network phenotypes. We provide standardized protocols, synthesize key quantitative findings into comparative tables, and illustrate core concepts with computational workflows and pathway diagrams. This guide serves as a technical roadmap for researchers and drug development professionals aiming to deconstruct the neurobiological architecture of behavior and its alterations in neurodevelopmental conditions.
1. Introduction: Autism as a Complex Systems Disorder Autism Spectrum Disorder (ASD) is characterized by heterogeneous clinical presentations arising from multifactorial etiologies, including genetic, environmental, and immunological factors [43] [21]. Traditional reductionist approaches have struggled to explain its diversity. A complex systems framework, operationalized through network neuroscience, posits that ASD symptoms emerge from atypical patterns of interaction within and between large-scale brain networks [44]. The core thesis is that clinically distinct autism subtypes reflect disruptions in distinct biological pathways and network trajectories [5]. Therefore, linking the topology of functional brain networks to detailed behavioral phenotyping is foundational for precision psychiatry.
2. Fundamental Principles: From Regions to Networks The evolution of neuroimaging has shifted the focus from localized regional activations to the analysis of distributed connectivity and network modules [44].
- Functional Connectivity (FC): FC represents statistical dependencies (e.g., correlation, coherence) between time-series of neural activity from distinct brain regions, typically measured using functional MRI (fMRI) or magneto/electroencephalography (MEG) [44] [45].
- The Connectome: The comprehensive map of neural connections, structural or functional, is termed the connectome [44] [46].
- Network Phenotypes: Graph theory provides metrics to quantify connectome topology. Key heritable global metrics include Global Efficiency (integration), Characteristic Path Length (segregation/integration), and Transitivity (clustering) [45].
3. Experimental Protocols & Methodological Pipeline
3.1. Data Acquisition and Preprocessing
- fMRI Protocol: Resting-state fMRI data is acquired (e.g., TR=720ms, multiband acceleration). Preprocessing includes motion correction, slice-timing correction, spatial normalization to standard space (e.g., MNI152), band-pass filtering (0.01-0.1 Hz), and regression of nuisance signals (white matter, cerebrospinal fluid, motion parameters) [45].
- MEG Protocol: Resting-state MEG data is recorded. Preprocessing involves noise reduction (SSS, tSSS), filtering, and artifact rejection (ICA for eye/heart). Sensor-level data is then projected to source space using beamforming and parcellated according to a brain atlas (e.g., Brainnetome Atlas with 246 regions) [45].
- Phenotypic Deep Phenotyping: Concurrently, a broad range of behavioral, cognitive, and clinical traits (>230 variables) are collected, encompassing social communication, repetitive behaviors, developmental milestones, and co-occurring psychiatric conditions [5].
3.2. Connectivity and Network Analysis
- FC Matrix Construction: For fMRI, pairwise Pearson correlation between regional time-series generates a symmetric connectivity matrix. For MEG, metrics like amplitude envelope correlation (AEC) and debiased weighted phase lag index (dwPLI) are computed across frequency bands (delta to gamma) [45].
- Graph Theoretical Computation: The connectivity matrix is thresholded to create a graph. Key metrics are calculated:
- Global Efficiency: The average inverse shortest path length; higher values indicate efficient integration.
- Characteristic Path Length: The average shortest path length; lower values indicate efficient integration.
- Transitivity: A measure of clustering coefficient; reflects local segregation.
- Nodal Strength/Centrality: The sum of weights of connections linked to a node [44] [45].
3.3. Linking Networks to Behavior: Multivariate Analytics Univariate correlations between single network metrics and single traits are often insufficient due to degeneracy [44]. Advanced multivariate techniques are employed:
- Canonical Correlation Analysis (CCA): Identifies linear combinations of FC features (e.g., edge weights) and behavioral variables that are maximally correlated with each other, revealing latent brain-behavior modes [44].
- Person-Centered Subtyping: Computational models (e.g., clustering) group individuals based on their multidimensional phenotypic profiles. These data-driven subgroups are then interrogated for distinct FC patterns and genetic correlates [5].
4. Key Quantitative Findings in Autism Research Table 1: Heritability of Global Graph Metrics in Resting-State Networks [45]
| Modality | FC Metric / Band | Global Efficiency (h²) | Char. Path Length (h²) | Transitivity (h²) | Notes |
|---|---|---|---|---|---|
| MEG | AEC (Theta Band) | 0.75-0.90 (High) | 0.75-0.90 (High) | 0.75-0.90 (High) | Amplitude synchrony shows high heritability. |
| MEG | dwPLI (Alpha Band) | 0.59-0.90 (High) | 0.59-0.90 (High) | 0.59-0.90 (High) | Phase synchrony also highly heritable in alpha. |
| MEG | AEC (Low Gamma) | 0.46-0.59 (Moderate) | 0.46-0.59 (Moderate) | 0.46-0.59 (Moderate) | Heritability lower in higher frequencies. |
| fMRI | Positive Correlation | 0.63-0.66 (High) | 0.63-0.66 (High) | 0.53 (Moderate) | Positive FC more heritable than negative. |
| fMRI | Negative Correlation | 0.46-0.47 (Moderate) | 0.46-0.47 (Moderate) | 0.29-0.33 (Low) |
Table 2: Data-Driven Autism Subtypes and Associated Features [5]
| Subtype | Approx. Prevalence | Core Clinical Presentation | Genetic Profile | Developmental Trajectory |
|---|---|---|---|---|
| Social & Behavioral Challenges | 37% | Core ASD traits, typical milestones, high psychiatric comorbidity (ADHD, anxiety). | Mutations in genes active later in childhood. | Later diagnosis; biological mechanisms may emerge postnatally. |
| Mixed ASD with Developmental Delay | 19% | Developmental delays, variable social/repetitive behaviors, low psychiatric comorbidity. | Enriched for rare inherited genetic variants. | Early developmental delays. |
| Moderate Challenges | 34% | Milder core ASD traits, typical milestones, low psychiatric comorbidity. | Not specified in study. | Similar to neurotypical development. |
| Broadly Affected | 10% | Severe delays, core ASD traits, high psychiatric comorbidity. | Highest burden of damaging de novo mutations. | Significant global developmental impacts. |
5. Application: Pathway Dysregulation in ASD Dysregulation in key neurotransmitter systems, integral to network communication, is implicated in ASD pathophysiology [43].
- GABA/Glutamate Imbalance: Disrupted excitation/inhibition (E/I) balance in cortical circuits.
- Serotonergic Dysregulation: Altered modulation of mood, sensory processing, and synaptic plasticity.
- Dopaminergic Signaling: Impacts reward processing, motivation, and motor control. Computational models integrate these molecular data to simulate network-level dysfunction [43].
6. The Scientist's Toolkit: Essential Research Reagents & Materials Table 3: Key Reagents and Solutions for Connectomics Research
| Item | Function/Description | Example/Note |
|---|---|---|
| Brain Atlas Parcellation | Digital template defining network nodes (ROIs). | Brainnetome Atlas (246 regions) [45]; Schaefer/Yeo networks. |
| Connectivity Estimation Software | Computes FC matrices from time-series data. | Nilearn (Python), CONN (MATLAB), FieldTrip (MEG). |
| Graph Analysis Toolkit | Calculates graph theoretical metrics. | Brain Connectivity Toolbox (BCT), igraph. |
| Multivariate Statistics Package | Implements CCA, partial least squares, etc. | scikit-learn (Python), PLS Toolbox. |
| Genetic Analysis Suite | For heritability estimation & genetic correlation. | SOLAR, GCTA, PLINK. |
| High-Performance Computing (HPC) Cluster | Essential for processing large datasets (e.g., >5000 subjects) and running complex simulations [5]. | Cloud or institutional HPC resources. |
| Biophysical Simulation Platform | Models neuronal dynamics and circuit function. | NEURON, NEST, Brian. |
| Viral Tracers (for animal models) | For anterograde/retrograde connectomic mapping. | AAVs, rabies virus variants [46]. |
| Tissue Clearing Reagents | Renders brain tissue transparent for mesoscale imaging. | CLARITY, CUBIC, or iDISCO protocols [46]. |
7. Visualizations: Workflows and Pathways
Brain-Behavior Linkage Analytic Workflow
Neurotransmitter Pathways to Network Dysfunction in ASD
Autism Spectrum Disorder (ASD) is increasingly recognized not as a single disorder but as a complex systems disorder arising from multifactorial etiologies that disrupt integrated brain networks [21]. This paradigm shift acknowledges that ASD pathophysiology emerges from dynamic interactions across genetic, circuit, and systemic levels, creating heterogeneous clinical presentations. The estimated prevalence has risen dramatically to approximately 1 in 31 children in the United States, reflecting improved diagnosis and possibly changing risk factors [32]. Rather than searching for a unified biological explanation, contemporary research focuses on identifying distinct subtypes and their specific underlying mechanisms. Groundbreaking 2025 research has identified four biologically distinct subtypes of autism using advanced computational methods applied to data from over 5,000 children [32]. This complex systems framework necessitates therapeutic interventions at multiple biological levels, from molecular targets to brain-wide network modulation, which this review comprehensively explores.
Molecular Therapeutics: Targeting the Central Dogma
Therapeutic strategies designed to rescue haploinsufficiency in ASD risk genes target all three levels of the central dogma of molecular biology, offering multiple intervention points for monogenic forms of autism.
DNA-Level Interventions
At the genetic level, CRISPR-Cas9 genome editing and transgene delivery represent promising approaches for monogenic ASD syndromes.
Gene Delivery Approaches: Transgene delivery using adeno-associated virus (AAV) vectors has shown success in preclinical models. In Fragile X Syndrome models, delivery of the unexpanded FMR1 gene via AAV vectors directly injected into mouse brains rescued repetitive behaviors, social deficits, and seizures [47]. Similarly, for Rett Syndrome, delivery of an instability-prone Mecp2 (iMecp2) transgene using an AAV vector in symptomatic mutant mice improved locomotor activity, lifespan, and normalized gene expression [47]. The primary challenge remains achieving proper dosing and brain-wide delivery while overcoming the blood-brain barrier.
CRISPR-Mediated Genome Editing: CRISPR-Cas9 systems can be directed toward natural antisense transcripts (NATs) that regulate imprinted genes. This approach has shown remarkable success for Angelman Syndrome, where CRISPR-Cas9-mediated transcriptional inhibition of the UBE3A antisense transcript reactivated the paternal copy of UBE3A in mice [47]. For Fragile X Syndrome, an alternative approach using CRISPR-Cas9 to delete pathological CGG repeat expansions in induced pluripotent stem cells restored FMR1 expression [47].
Table 1: DNA-Level Therapeutic Approaches for Monogenic ASD Syndromes
| Syndrome | Gene | Therapeutic Approach | Model System | Key Outcomes |
|---|---|---|---|---|
| Angelman | UBE3A | CRISPR inhibition of UBE3A-ATS | Mouse | Reactivated paternal UBE3A expression [47] |
| Fragile X | FMR1 | CRISPR deletion of CGG repeats | iPSCs | Restored FMR1 expression [47] |
| Rett | MECP2 | AAV-Mecp2 transgene delivery | Mouse | Improved locomotion, lifespan [47] |
| Fragile X | FMR1 | AAV-FMR1 transgene delivery | Mouse | Rescued social deficits, seizures [47] |
RNA-Level Interventions
RNA-targeting therapies represent a rapidly advancing frontier with multiple technological approaches for modulating gene expression.
Antisense Oligonucleotides (ASOs): ASOs are single-stranded DNA, RNA, or hybrid molecules (<50 bp) that can modulate gene expression through various mechanisms. For Angelman Syndrome, ASOs targeting the UBE3A antisense transcript (UBE3A-ATS) successfully unsilenced the paternal allele, restoring UBE3A expression in vitro and in vivo [48]. These ASOs are now in phase 1 or 2 clinical trials [48]. For SYNGAP1-related ASD, ASOs designed to bind the 3' splice site between exon 10 and 11 increased productive splicing, elevating both mRNA and protein levels in vitro [48].
SINEUP RNA Technology: A novel RNA-based approach utilizes synthetically constructed antisense long non-coding RNAs called SINEUPs. These molecules bind to 5' untranslated regions of mRNA, stabilizing the molecule and preventing degradation, leading to protein upregulation without affecting mRNA levels [48]. Proof-of-concept research targeting CHD8 mutations demonstrated that SINEUP application raised CHD8 protein levels 1.5-fold in human-derived neural progenitor cells from ASD patients, sufficient to support normal function [49]. In zebrafish embryos with reduced CHD8, this approach prevented enlarged head size, a characteristic feature of CHD8 mutations in humans [49].
RNA Editing Approaches: Emerging technologies enable direct RNA editing to correct pathogenic mutations. While still in early development, this approach offers potential for addressing specific point mutations without permanent genomic changes.
The following diagram illustrates the molecular mechanisms of RNA-targeting therapies:
Protein-Level Interventions
Small molecule drugs targeting downstream molecular pathways offer advantages in blood-brain barrier penetration and administration.
Experimental Compounds: Stanford researchers discovered that hyperactivity in the reticular thalamic nucleus underlies behaviors associated with ASD. They tested an experimental seizure drug, Z944, which reversed behavioral deficits in autism mouse models [32]. This highlights the potential of repurposing existing neurological medications for ASD.
Novel Therapeutics in Development: Multiple pharmaceutical companies currently have over 20 potential medicines in various development stages for ASD [50]. These include Hoffmann-La Roche's RO6953958, Jazz Pharmaceuticals' JZP541, Yamo Pharmaceuticals' L1-79 (which showed improved social skills in trials), and Axial Therapeutics' AB-2004 [50]. These compounds target diverse mechanisms from neurotransmission to gut-brain axis modulation.
Circuit-Based Neuromodulation: Targeting Distributed Brain Networks
The complex systems perspective of ASD emphasizes dysfunction in distributed brain networks rather than isolated regions, making circuit-based neuromodulation a promising therapeutic avenue.
Neural Circuit Mechanisms of Social Behavior
Social behavior is mediated by a distributed brain-wide network involving cortical and subcortical structures. Key nodes include the medial prefrontal cortex (mPFC), anterior cingulate cortex, insular cortex (IC), nucleus accumbens, basolateral amygdala (BLA), and ventral tegmental area [51]. These regions are influenced by multiple neuromodulatory systems including oxytocin, dopamine, and serotonin. Research particularly highlights the insular cortex as a unique area mediating multisensory integration, encoding of ongoing social interaction, social decision-making, emotion, and empathy [51]. Studies of ASD mouse models consistently demonstrate dysfunctions in mPFC-BLA circuitry, highlighting this pathway as a promising therapeutic target [51].
Transcranial Magnetic Stimulation Approaches
Repetitive Transcranial Magnetic Stimulation (rTMS) represents a non-invasive neuromodulation technique that can target specific neural circuits.
Protocol Specifications: In a study of 27 children with ASD, researchers administered weekly 0.5 Hz rTMS bilaterally over the dorsolateral prefrontal cortex (DLPFC) [52]. This low-frequency approach aims to reduce cortical hyperexcitability and normalize network dynamics. Stimulation parameters typically involve 15-20 minute sessions delivered weekly over 12-16 weeks, though optimal protocols remain under investigation.
Physiological and Behavioral Outcomes: rTMS treatment significantly improved autonomic nervous system (ANS) regulation, with heart rate variability (HRV) indices indicating increased parasympathetic activity and reduced sympathetic arousal [52]. Several parental behavioral rating scores improved post-TMS, with parasympathetic HRV indices negatively correlating with repetitive behaviors, while sympathetic arousal indices showed positive correlation with the same behaviors [52]. This suggests rTMS can improve core ASD symptoms by enhancing psychophysiological flexibility.
Personalized Targeting Approaches: Recent advances in neuroimaging enable personalized TMS target selection based on individual brain network architecture [53]. Higher-order regions like the prefrontal cortex show high interindividual variability, providing rationale for person-specific targeting. Methodology for determining reproducible personalized targets with millimeter precision is now feasible in clinically tractable acquisition times [53].
Table 2: Circuit-Based Neuromodulation Approaches and Outcomes
| Approach | Target | Parameters | Key Physiological Effects | Behavioral Outcomes |
|---|---|---|---|---|
| rTMS [52] | DLPFC | 0.5 Hz, weekly | Increased HRV, reduced SCL | Improved social function, reduced repetitive behaviors |
| Personalized TMS [53] | Individual-specific | Individualized | Normalized network dynamics | Under investigation |
| Experimental Drugs [32] | Reticular thalamic nucleus | Z944 compound | Reduced thalamic hyperactivity | Reversed social deficits, seizures |
The following diagram illustrates the neural circuits and neuromodulation targets in ASD:
Experimental Protocols and Methodologies
Preclinical Gene Therapy Protocols
CRISPR-Cas9 for Angelman Syndrome:
- Guide RNA Design: Design gRNAs complementary to the UBE3A antisense transcript promoter region
- Vector Packaging: Package CRISPR construct into AAV vectors (serotype 9 preferred for CNS penetration)
- Administration: Intracerebroventricular injection in postnatal day 21-28 mouse models
- Validation: Measure UBE3A protein levels via Western blot at 4-8 weeks post-injection
- Behavioral Assessment: Conduct social interaction, seizure threshold, and motor coordination tests
SINEUP RNA for CHD8 Haploinsufficiency:
- Molecule Design: Synthesize antisense lncRNA complementary to CHD8 mRNA 5'UTR
- In Vitro Testing: Transfert human neural progenitor cells derived from ASD patient iPSCs
- Protein Quantification: Measure CHD8 protein levels via ELISA 48-72 hours post-transfection
- Functional Rescue: Assess normalization of transcriptional dysregulation via RNA-seq
- In Vivo Validation: Microinject into zebrafish embryos; measure head size at 72 hours post-fertilization
rTMS Protocol for ASD
Patient Selection: Children aged 8-17 with ASD diagnosis, excluding those with seizure history or metallic implants Target Localization:
- Structural MRI acquisition (T1-weighted)
- DLPFC identification using Beam F3 method or neuronavigation
- Motor threshold determination for intensity calibration Stimulation Parameters:
- Frequency: 0.5 Hz
- Intensity: 90% of resting motor threshold
- Duration: 15-20 minutes per session
- Course: 12 weekly sessions Outcome Measures:
- Autonomic: HRV time/frequency domain analysis, skin conductance level
- Behavioral: Aberrant Behavior Checklist, Repetitive Behavior Scale
- Parent-reported: Social Responsiveness Scale
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for ASD Therapeutic Development
| Reagent/Model | Application | Key Features | Example Use |
|---|---|---|---|
| SHANK3 mouse models [48] | Monogenic ASD research | Reproduces synaptic deficits | Testing gene therapies for Phelan-McDermid syndrome |
| Non-human primate MECP2 models [47] | Translational research | Recapitulates human developmental timelines | Evaluating gene therapy safety and efficacy |
| Human iPSC-derived neurons [47] | In vitro screening | Patient-specific genetic background | Testing ASOs and SINEUP molecules |
| AAV9 vectors [48] [47] | CNS gene delivery | Efficient blood-brain barrier crossing | Delivering transgenes in preclinical models |
| Zebrafish CHD8 models [49] | Rapid genetic screening | Transparent embryos, rapid development | Proof-of-concept therapeutic testing |
| CRISPR-Cas9 systems [47] | Genome editing | Precise genetic modification | Reactivating imprinted genes |
The emerging therapeutic landscape for ASD reflects its identity as a complex systems disorder, requiring interventions at multiple biological levels. Molecular approaches targeting DNA, RNA, and protein dysfunction offer precision for monogenic forms, while circuit-based neuromodulation addresses network-level dysfunction common across ASD subtypes. The most promising future direction involves combining these approaches—using genetic therapies to correct molecular deficits while employing neuromodulation to normalize resulting circuit dysfunction. Furthermore, the identification of distinct ASD subtypes enables personalized treatment matching based on underlying biology. As research continues to accelerate, these emerging avenues offer genuine promise for transforming outcomes across the autism spectrum through mechanisms that respect and address the complexity of neurodevelopment.
Autism Spectrum Disorder (ASD) represents a group of neurodevelopmental disorders characterized by substantial heterogeneity in clinical presentation, underlying genetics, and neurobiological mechanisms. With a prevalence of 1:36 according to latest estimates, ASD imposes a significant socioeconomic burden on global mental health systems [54]. The conceptualization of autism as a complex systems disorder arises from its multifaceted etiology, involving dynamic interactions between numerous genetic susceptibilities, environmental factors, and developmentally accumulated dysregulations across neural circuits [55]. This framework necessitates preclinical research strategies that can address the interconnected pathophysiological pathways underlying core ASD symptoms—social communication deficits and restricted/repetitive behaviors.
The neurobiological basis of ASD remains incompletely understood, though several prominent hypotheses are under investigation, including roles for neuroinflammation, imbalances in excitatory/inhibitory neurotransmission, and structural/functional alterations in brain regions such as the striatum and hippocampus [54]. The extreme variability in ASD presentation aligns with research demonstrating that traits associated with autism extend continuously into the general population, suggesting that quantitative approaches may provide greater insight into underlying biology than categorical diagnoses alone [28]. This review examines recent pre-clinical successes in reversing behavioral deficits through specific biological targets, highlighting innovative approaches that reflect the systems-level complexity of ASD.
Key Animal Models in ASD Research
Animal models remain indispensable tools for elucidating the pathophysiology of ASD and evaluating potential therapeutic interventions. The optimal modeling approach must demonstrate strong face validity (recapitulating core behavioral symptoms), construct validity (sharing underlying neurobiological mechanisms with human ASD), and predictive validity (responding to interventions with known clinical efficacy) [56]. Researchers have developed diverse models to address the heterogeneous nature of ASD, each with distinct advantages and limitations for studying this complex disorder.
Genetic Models
Genetic models targeting specific ASD-risk genes allow researchers to investigate well-defined biological pathways and their contribution to behavioral phenotypes:
- Drd2-KO mice: These dopamine receptor D2 knockout mice exhibit social behavior deficits and excessive grooming, representing core ASD symptoms. The model demonstrates disrupted expression of multiple ASD-associated genes including Disc1, Cnr1, Ppp1r1b, Oxt, and Oxtr in striatal and hippocampal regions [55].
- Shank3-KO mice: Lacking a postsynaptic scaffold protein preferentially expressed in the striatum, these mice display defective striatal neuron excitability and autistic-like behaviors, making them valuable for studying synaptic abnormalities in ASD [55].
- Adcy5-KO mice: Adenylyl cyclase-5 knockout mice exhibit autistic-like behaviors, with Adcy5 serving as a crucial integrator of signals from various G-protein-coupled receptors including D2 dopamine receptors and mGluR5 [55].
- Oxtr-KO mice: Heterozygous oxytocin receptor knockout mice demonstrate social deficits, implicating the oxytocin system in ASD-related social impairments [55].
Pharmacological Models
Pharmacologically induced models offer complementary approaches for studying ASD-like behaviors and screening potential therapeutics:
- Amphetamine (AMPH) models: Administration of AMPH can induce hyperactivity, reward-seeking behaviors, and stereotypies resembling manic symptoms often associated with ASD. These effects are mediated through disruption of monoaminergic transmission, particularly dopamine, aligning with the dopamine hyperactivity hypotheses in neurodevelopmental disorders [56].
- Modeling parameters: Acute regimens typically employ 2.5-4.0 mg/kg i.p. injections, while chronic models use extended 10-day regimens. Lower doses preferentially elicit core manic symptomatology including psychomotor hyperactivity and enhanced novelty-seeking behavior [56].
Table 1: Key Genetic Mouse Models of ASD
| Model | Target Gene | Core Behavioral Phenotypes | Key Neurobiological Alterations |
|---|---|---|---|
| Drd2-KO | Dopamine receptor D2 | Social interaction deficits; Excessive grooming | Dysregulated ASD-associated gene expression in striatum; Disrupted dopamine signaling |
| Shank3-KO | Postsynaptic scaffold protein | Social deficits; Repetitive behaviors | Defective striatal neuron excitability; Synaptic dysfunction |
| Adcy5-KO | Adenylyl cyclase-5 | Autistic-like behaviors | Disrupted GPCR signaling integration |
| Oxtr-KO | Oxytocin receptor | Social behavior deficits | Impaired oxytocin signaling pathways |
Reversing Behavioral Deficits: Specific Targets and Mechanisms
Recent preclinical research has identified several promising targets for reversing behavioral deficits in ASD models, with interventions ranging from probiotic-derived vesicles to neuromodulatory approaches.
Lactobacillus paracasei-Derived Extracellular Vesicles (LpEV)
Emerging evidence suggests that extracellular vesicles (EVs) derived from the probiotic Lactobacillus paracasei (LpEV) possess significant neuroprotective properties with potential application for ASD core symptoms [55].
- Behavioral improvements: LpEV treatment significantly improved social behavior deficits and reduced excessive grooming in Drd2-KO mice. The three-chamber sociability test demonstrated restoration of social preference and social novelty recognition following LpEV administration [55].
- Molecular mechanisms: RNA sequencing and Gene Ontology enrichment analysis revealed that LpEV treatment reversed dysregulated expression of ASD-associated genes in Drd2-KO mice. A substantial proportion of these genes overlapped with known ASD genes in the SFARI database, indicating targeted effects on relevant pathways [55].
- Multi-model efficacy: LpEV treatment demonstrated therapeutic potential across multiple genetic models, improving autistic-like behaviors in Oxtr-KO heterozygous mice, Adcy5-KO mice, and Shank3-KO mice. This suggests broader mechanisms beyond single-gene pathway correction [55].
- Oxytocin system involvement: Further investigation identified oxytocin and oxytocin receptor (Oxtr) as potential therapeutic targets of LpEV, connecting the intervention to a well-established neurobiological system implicated in social behavior [55].
Striatal Circuitry Targets
The striatum has emerged as a critical brain region contributing to core ASD symptoms, with several studies demonstrating that dysfunction in this area and its associated neural circuits underlies social deficits and repetitive behaviors [55].
- Dopaminergic signaling: siRNA-mediated knockdown of Drd2, GluN2B, GluA1, or mGluR3 within the dorsal striatum produced substantial deficits in social behaviors and excessive grooming, establishing the causal role of striatal dysfunction in these behaviors [55].
- Therapeutic restoration: Interventions that normalize striatal dysfunction, whether through probiotic-derived vesicles or other approaches, demonstrate capacity to reverse these behavioral deficits, supporting the striatum as a promising target for ASD therapeutics [55].
Enriched Environmental Interventions
Non-pharmacological approaches also show promise for mitigating ASD-like behaviors in animal models, potentially through modulation of neuroplasticity mechanisms.
- Multi-system effects: Enriched environmental interventions can improve autistic symptoms by increasing activity in specific brain regions and positively modulating synaptic plasticity [54].
- Neuroinflammatory modulation: These interventions may also impact inflammatory activity mediated by glial cells, suggesting effects on the neuroinflammatory components hypothesized to contribute to ASD pathophysiology [54].
Table 2: Quantitative Behavioral Improvements in ASD Models Following Intervention
| Intervention | Model | Behavior Test | Improvement | Molecular Correlates |
|---|---|---|---|---|
| LpEV | Drd2-KO | Three-chamber sociability | Restored social preference and novelty recognition | Reversal of dysregulated ASD gene expression |
| LpEV | Drd2-KO | Repetitive behavior assessment | Reduced excessive grooming | Normalization of oxytocin pathway genes |
| LpEV | Oxtr-KO, Adcy5-KO, Shank3-KO | Social behavior tests | Improved autistic-like behaviors across models | Effects beyond single-gene pathways |
| Enriched environment | Multiple ASD models | Social interaction, repetitive behavior | Improved autistic symptoms | Enhanced synaptic plasticity; Reduced neuroinflammation |
Experimental Protocols and Methodologies
Behavioral Assessment of ASD-like Phenotypes
Comprehensive behavioral characterization is essential for validating animal models of ASD and evaluating potential therapeutic interventions. The following tests represent gold-standard approaches for assessing core ASD-related behaviors:
- Three-chamber sociability test: This paradigm evaluates social approach and social novelty preference. The test apparatus consists of a rectangular, three-chambered box with removable doors dividing each chamber. In the sociability phase, the test mouse can choose between an unfamiliar conspecific (social target) contained within a wire cup and an empty cup. In the social novelty phase, the mouse chooses between the now-familiar conspecific and a novel unfamiliar conspecific. Typical mice spend significantly more time with the social target versus the empty cup and with the novel versus familiar mouse, whereas ASD models show impaired social preference [55].
- Repetitive behavior assessments: Self-grooming measurements involve placing mice in a novel, empty cage and recording behavior for 10 minutes. Excessive grooming is defined as prolonged bouts of patterned sequences of face-washing, body-grooming, and head-licking. Marble burying tests can also assess repetitive/digging behaviors, with ASD models typically displaying increased marble burying [55].
- Elevated Plus Maze (EPM): This test assesses anxiety-like behavior and risk-taking behavior, which are frequently altered in ASD models. The apparatus consists of a plus-shaped platform elevated above the floor with two open and two enclosed arms. Mice are placed in the center and allowed to explore for 5 minutes, with time spent in open versus closed arms quantified [56].
Molecular and Cellular Analyses
Integration of behavioral assessments with molecular analyses provides mechanistic insights into intervention effects:
- RNA sequencing and Gene Ontology analysis: Following behavioral testing, brain regions of interest (e.g., dorsal striatum, hippocampus) are dissected for RNA extraction. Sequencing data are analyzed for differential gene expression, followed by Gene Ontology enrichment analysis to identify biological processes and pathways affected by the intervention [55].
- Real-time PCR validation: Candidate genes identified through sequencing are validated using RT-PCR with specific primers, allowing quantification of expression changes in multiple brain regions [55].
- Biodistribution studies: Orally administered interventions (e.g., LpEV) can be labeled with radioactive isotopes such as indium-111 to track distribution throughout the body and brain, establishing bioavailability to relevant target tissues [55].
Signaling Pathways in ASD Pathophysiology and Treatment
The complexity of ASD as a systems disorder is reflected in the multiple interconnected signaling pathways implicated in its pathophysiology. The following diagram illustrates key pathways involved in ASD and targeted by successful interventions:
Diagram 1: Key Signaling Pathways in ASD Pathophysiology and Intervention Targets. This systems-level view illustrates how multiple interconnected pathways contribute to ASD-related behaviors and how successful interventions target these pathways.
The Scientist's Toolkit: Research Reagent Solutions
Advancing ASD research requires specialized reagents and tools designed to probe specific biological mechanisms. The following table details essential research materials for studying ASD pathophysiology and evaluating potential therapeutics:
Table 3: Essential Research Reagents for ASD Preclinical Studies
| Reagent/Tool | Function/Application | Example Use in ASD Research |
|---|---|---|
| Lactobacillus paracasei-derived extracellular vesicles (LpEV) | Probiotic-derived therapeutic nanovesicles | Reversal of social deficits and repetitive behaviors in genetic ASD models; Modulation of oxytocin signaling pathways |
| Dopamine receptor D2 knockout mice | Genetic model of ASD with striatal dysfunction | Study of social behavior deficits and excessive grooming; Testing interventions targeting dopamine signaling |
| Shank3 knockout mice | Genetic model of syndromic ASD | Investigation of synaptic abnormalities and repetitive behaviors; Evaluation of synaptic-targeted therapies |
| Oxytocin receptor knockout mice | Genetic model of social impairment | Study of oxytocin system in social behavior; Testing social behavior interventions |
| Three-chamber sociability apparatus | Behavioral assessment of social approach and preference | Quantification of social deficits in ASD models; Measurement of intervention effects on social behavior |
| Self-grooming assessment protocol | Behavioral measurement of repetitive behaviors | Evaluation of repetitive behavior phenotypes; Assessment of intervention effects on stereotypies |
| SFARI Gene Database | Curated database of ASD-associated genes | Identification of candidate genes; Pathway analysis of transcriptomic data |
| RNA sequencing with GO analysis | Transcriptomic profiling and pathway identification | Uncovering molecular mechanisms underlying ASD behaviors; Identifying pathways modulated by interventions |
The investigation of specific biological targets for reversing behavioral deficits in ASD models represents a promising frontier in neurodevelopmental disorder research. The demonstrated success of interventions such as LpEV across multiple genetic models highlights the potential for approaches that address the systems-level complexity of ASD rather than targeting single genes or pathways in isolation. The striatum has emerged as a critical node in the circuitry underlying core ASD symptoms, with dysfunction in this region sufficient to produce social deficits and repetitive behaviors that can be reversed through targeted interventions.
Future research directions should include more comprehensive investigation of circuit-level mechanisms linking specific molecular interventions to behavioral improvements, potentially through innovative techniques such as in vivo calcium imaging during social behavior tasks. Additionally, the exploration of combination therapies targeting multiple systems simultaneously may yield enhanced efficacy given the heterogeneous and multifactorial nature of ASD. The continued refinement of quantitative trait measures for assessing ASD-related behaviors across species will further strengthen the translational value of preclinical findings [28].
As our understanding of ASD as a complex systems disorder deepens, therapeutic development will likely shift from symptom suppression toward targeted modulation of core pathophysiological processes. The promising pre-clinical successes reviewed herein provide a foundation for this evolving approach, offering hope for more effective and personalized interventions for ASD.
Bridging the Translation Gap: Challenges in Diagnostics, Clinical Trials, and Biomarker Development
Autism Spectrum Disorder (ASD) is defined and diagnosed behaviorally, relying on clinician observation of social communication deficits and restricted, repetitive behaviors [57]. This subjective process, utilizing tools like the Autism Diagnostic Observation Schedule (ADOS), is time-consuming, resource-intensive, and prone to inter-rater variability, creating a significant diagnostic bottleneck that delays early intervention [58]. The core challenge stems from treating ASD as a monolithic behavioral syndrome rather than a complex systems disorder—a condition arising from dynamic, multi-level interactions between genetic vulnerability, molecular pathways, neural circuitry, and environmental factors [57] [59]. This systems perspective necessitates a shift from purely descriptive behavioral phenotyping to the discovery of objective, quantifiable biomarkers. Biomarkers—measurable indicators of biological processes—offer the potential for earlier, more precise diagnosis, patient stratification into biologically coherent subgroups, and objective measurement of treatment response [60] [61]. This whitepaper details the current landscape of ASD biomarker research, provides experimental protocols for key findings, and outlines a framework for integrating multi-modal data to overcome the diagnostic bottleneck.
A Complex Systems View: Biomarkers Across Biological Scales
Viewing ASD through a complex systems lens requires biomarkers that capture interactions across different biological tiers. The table below summarizes major biomarker categories, their evidence grade, and key findings from the literature.
Table 1: Multi-Scale Biomarker Categories in ASD Research
| Biomarker Category | Example Biomarkers | Reported Performance/Association | Level of Evidence (Oxford CEBM) | Key References |
|---|---|---|---|---|
| Genetic | FMR1 mutations, CHD8, SHANK3, 16p11.2 CNV | High penetrance for specific syndromes; >400 genes associated with ASD phenotypes. Subgroup prevalence: Cytogenetic (3%), CMA (8-26%), WES (9-26%) [60] [59] [61]. | B (for specific syndromes like FXS) | [60] [59] [61] |
| Metabolic | Methylation-redox imbalance (GSH/GSSG), acyl-carnitines, branched-chain amino acids (BCAA), lactate | Methylation-redox accuracy: 97% (Sen:98%, Spec:96%). Acyl-carnitines/amino acids accuracy: 69%. Subgroup prevalence for metabolic dysfunction: 17-98% [60] [62] [61]. | B (for methylation-redox) | [60] [62] [61] |
| Immunologic | Maternal fetal brain-directed autoantibodies, elevated cytokines (IL-6, IL-1β, TNF-α), FRAA autoantibodies | Maternal autoantibodies associated with 12-23% ASD risk. FRAA prevalence in ASD subgroups: 65-77% [60] [61]. | B (for maternal autoantibodies) | [60] [61] |
| Neuroimaging (Structural) | Cortical surface area expansion (6-12 months), brain volume, amygdala volume | Cortical surface area predictive accuracy: 94% (Sen:88%, Spec:95%) in presymptomatic infants. Brain volume diagnostic accuracy: 78% [60] [63]. | C | [60] [63] |
| Neuroimaging (Functional) | Functional connectivity (FC) patterns, EEG spectral power/coherence | Resting-state FC predictive accuracy up to 97% in infants. AI-EEG classifiers report 85-99% accuracy [60] [63] [64]. | C | [60] [63] [64] |
| Neurophysiological & Behavioral | Eye-tracking (reduced attention to eyes), EEG event-related potentials (N170, P300) | Quantifiable differences in visual attention and neural response to social stimuli; used in infant sibling studies [57] [59] [63]. | C (emerging) | [57] [59] [63] |
| Epigenetic | Differential DNA methylation patterns, histone acetylation signatures | Associated with ≥68% of ASD cases in prefrontal/temporal cortex post-mortem studies [62] [61]. | C | [62] [61] |
| Gut Microbiome | Dysbiosis (e.g., Bacteroidetes/Firmicutes ratio), levels of Coprococcus, Bifidobacterium | Correlated with social impairment severity; produces metabolites (SCFAs) influencing brain function [61]. | C (emerging) | [61] |
Detailed Experimental Protocols for Key Biomarker Domains
Protocol: Multimodal Neuroimaging and AI Analysis for Diagnostic Classification
Objective: To classify ASD vs. typically developing (TD) individuals using fused structural MRI (sMRI) and behavioral data within an explainable AI framework [65]. Materials: ABIDE-I dataset (1112 subjects: 539 ASD, 573 TD), T1-weighted sMRI scans, phenotypic/behavioral data (e.g., ADOS scores). Workflow: 1. Data Preprocessing: sMRI data processed using standard pipelines (e.g., FSL, FreeSurfer) for brain extraction, tissue segmentation, and cortical parcellation based on the Harvard-Oxford atlas to extract regional volumetric features. 2. Behavioral Embedding: Process behavioral phenotypes using a Generalized Additive Model with Interactions (GAMI-Net). This model generates an interpretable "ASD_Probability" score by modeling non-linear, additive contributions of each behavioral feature [65]. 3. Neuroimaging Embedding: Implement a hybrid CNN-Graph Neural Network (GNN). * A Convolutional Neural Network (CNN) extracts voxel-level spatial features from sMRI data. * A Graph Neural Network (GNN) models the brain as a graph, where nodes are atlas-defined regions (features from CNN), and edges represent anatomical or functional connectivity. This captures inter-regional relationships [65]. 4. Multimodal Fusion: The behavioral (GAMI-Net) and neuroimaging (CNN-GNN) embeddings are compressed into a common, low-dimensional latent space using an Autoencoder to learn shared representations and avoid simple concatenation [65]. 5. Personalized Classification: A Hypernetwork generates unique weights for a final Multi-Layer Perceptron (MLP) classifier based on each subject's fused latent embedding, enabling subject-specific decision boundaries [65]. Validation: Perform stratified 5-fold cross-validation and hold-out testing. Reported performance: Accuracy up to 99.4%, F1-score 99.42% on held-out test sets [65].
Protocol: Metabolomic Profiling for Subgroup Identification
Objective: To identify plasma/serum metabolic signatures distinguishing ASD and to stratify ASD into metabolic subgroups [60] [61]. Materials: Fasting plasma/serum samples from ASD and TD cohorts, matched for age, sex, and diet. Liquid Chromatography-Mass Spectrometry (LC-MS) platform. Workflow: 1. Sample Preparation: Deproteinize plasma using cold methanol or acetonitrile. Centrifuge and collect supernatant for LC-MS analysis. 2. Untargeted Metabolomics: Run samples on a high-resolution LC-MS system. Use hydrophilic interaction liquid chromatography (HILIC) for polar metabolites and reversed-phase chromatography for lipids. 3. Data Processing: Use software (e.g., XCMS, MS-DIAL) for peak picking, alignment, and annotation against public databases (HMDB, METLIN). 4. Statistical Analysis: * Perform multivariate analysis (Partial Least Squares-Discriminant Analysis, PLS-DA) to find metabolites differentiating ASD from TD. * Conduct univariate analysis (t-tests with FDR correction) to identify specific dysregulated metabolites (e.g., glutathione, acyl-carnitines, BCAA, lactate). * Cluster ASD participants based on their metabolic profiles using k-means or hierarchical clustering. 5. Pathway Analysis: Input significant metabolites into pathway analysis tools (MetaboAnalyst) to identify disturbed pathways (e.g., glutathione metabolism, mitochondrial energy production, aminoacyl-tRNA biosynthesis) [61]. Validation: Internal cross-validation of PLS-DA model. Validate discriminative metabolites in an independent cohort. Reported accuracy for methylation-redox biomarkers: 97% [60].
Protocol: Eye-Tracking as a Digital Phenotyping Tool in Infants
Objective: To identify early deviations in visual attention as a risk biomarker for ASD in infant siblings [57] [59]. Materials: High-speed eye-tracker, calibrated display, age-appropriate visual stimuli (e.g., dynamic social scenes with faces vs. non-social objects). Workflow: 1. Participant Cohort: Recruit infants (e.g., 6-12 months) with an older sibling diagnosed with ASD (high-risk group) and infants with no family history (low-risk group). 2. Stimulus Presentation: Present standardized videos or images while the infant sits on a caregiver's lap. Ensure good tracking calibration. 3. Data Acquisition: Record gaze coordinates, fixations, and saccades at a high sampling rate (e.g., 500 Hz). 4. Feature Extraction: Calculate key metrics: * Time to First Fixation: Latency to look at social vs. non-social regions. * Total Fixation Duration: Proportion of time spent looking at eyes, mouth, or objects. * Scan Path Patterns: Complexity and distribution of saccades. 5. Analysis: Compare high-risk and low-risk infant groups on these metrics. Use longitudinal design to correlate early eye-tracking measures with later ASD diagnosis at 24-36 months. Outcome: High-risk infants who later receive an ASD diagnosis often show reduced attention to eyes and social scenes, and atypical scan paths, as early as 9-12 months [63].
Visualizing Systems Interactions and Workflows
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Research Tools for ASD Biomarker Discovery
| Tool Category | Specific Solution/Technology | Primary Function in ASD Research |
|---|---|---|
| Neuroimaging Acquisition | 3T/7T MRI Scanner with fMRI, DTI, and sMRI sequences | Captures high-resolution brain structure, white matter integrity, and functional connectivity patterns for identifying neuroanatomical and functional biomarkers [63] [64]. |
| Electrophysiology | High-density EEG system (128-256 channels) with event-related potential (ERP) capabilities | Measures millisecond-level neural dynamics, oscillatory power, and connectivity for investigating sensory processing and social brain function [63]. |
| Digital Phenotyping | Remote or lab-based eye-tracking system (e.g., Tobii Pro) | Quantifies visual attention patterns (e.g., eye gaze, pupillometry) as objective, early behavioral biomarkers, especially in infant studies [57] [59]. |
| Genomic Analysis | Next-Generation Sequencing (NGS) platforms for Whole Exome/Genome Sequencing (WES/WGS) and Microarray for CNV detection | Identifies rare and common genetic variants, copy number variations (CNVs), and facilitates genotype-first approaches to delineate biological subgroups [60] [59]. |
| Metabolomics/Lipidomics | High-Resolution Liquid Chromatography-Mass Spectrometry (LC-MS) systems | Enables untargeted and targeted profiling of small molecules in biofluids (plasma, urine) to discover metabolic dysregulation signatures and subgroup classifiers [60] [61]. |
| Multimodal Data Fusion & AI | Deep Learning Frameworks (PyTorch, TensorFlow) with libraries for GNNs (PyTorch Geometric) and Explainable AI (SHAP, Captum) | Develops and trains hybrid models (e.g., CNN-GNN) to integrate multimodal data, perform classification, and extract interpretable biomarker features [66] [65]. |
| Biomarker Validation | Multiplex Immunoassay platforms (e.g., Luminex, MSD) | Validates candidate protein/cytokine biomarkers across large cohorts with high sensitivity and throughput for immune and metabolic panels [61]. |
| Standardized Behavioral Assessment | Autism Diagnostic Observation Schedule, 2nd Edition (ADOS-2) | Provides the current clinical gold-standard behavioral phenotype against which objective biomarkers are validated and correlated [58]. |
The path beyond the behavioral diagnostic bottleneck lies in embracing ASD as a complex systems disorder. No single biomarker will suffice; rather, a panel of biomarkers spanning genetic, molecular, circuit-level, and digital phenotypic domains is required [60] [61]. The integration of these multi-scale data through advanced AI and network analysis methods, as demonstrated in recent multimodal studies [65] [64], offers a powerful strategy to identify reproducible signatures for early risk detection, precise diagnosis, and biologically informed stratification. Future research must prioritize large-scale, longitudinal studies from infancy to validate these integrated models, establish standardized protocols for biomarker measurement, and rigorously test their utility in guiding targeted interventions. The convergence of systems biology, neurotechnology, and computational analytics holds the key to transforming ASD from a behaviorally defined syndrome into a mechanistically understood disorder with objective pathways for diagnosis and care.
The inherent heterogeneity within complex neurodevelopmental disorders like autism spectrum disorder (ASD) presents a fundamental challenge for clinical trial design. Traditional "one-size-fits-all" approaches have consistently failed to demonstrate efficacy in broad ASD populations, not due to a lack of biologically active compounds, but because of the failure to account for the diverse etiologies and phenotypic presentations that characterize the condition. This whitepaper delineates the critical need for stratification methodologies in clinical trials for heterogeneous populations. We provide a technical framework for incorporating stratification based on genetic, phenotypic, and biomarker profiles, contextualized within the paradigm of autism as a complex systems disorder. By synthesizing recent advances in subtype identification with established clinical trial methodology, this guide offers researchers and drug development professionals a pathway to more precise, powerful, and informative clinical investigations.
Autism spectrum disorder is a quintessential example of a complex systems disorder, with estimates of potentially 1,000 genes that may be associated with risk, in addition to environmental and other non-genetic contributors [67]. This etiological heterogeneity is mirrored at the phenotypic level, where individuals present with disparate symptoms across social communication, repetitive behaviors, sensory processing, and a spectrum of co-occurring conditions [67] [68]. This multi-dimensional heterogeneity has dire consequences for clinical development: trials of biologically targeted interventions have repeatedly failed to show significant benefit on primary outcomes, despite subsets of participants appearing to respond well [67]. The fundamental problem is that treatments designed for one biological etiology may not benefit individuals with ASD resulting from perturbations in other biological pathways.
The high failure rate in late-phase ASD trials underscores the inadequacy of current diagnostic criteria as a framework for clinical trial enrollment. The "intent-to-treat" paradigm, when applied to a biologically heterogeneous population, dilutes treatment effects to the point of statistical non-significance. This necessitates a paradigm shift toward precision medicine approaches that explicitly account for this heterogeneity through sophisticated stratification strategies early in the drug development pathway [67].
The Biological Basis for Stratification in Autism
Data-Driven Identification of Autism Subtypes
Recent large-scale studies have successfully deconstructed ASD's heterogeneity into biologically meaningful subtypes. A seminal 2025 study analyzed 239 phenotypic features across 5,392 individuals from the SPARK cohort using a generative mixture model, identifying four clinically and biologically distinct subtypes [5] [68].
Table 1: Clinically Distinct Autism Subtypes and Their Characteristics
| Subtype Name | Prevalence | Core Clinical Features | Co-occurring Conditions | Developmental Trajectory |
|---|---|---|---|---|
| Social/Behavioral Challenges | ~37% | Core autism traits including social challenges and repetitive behaviors | High rates of ADHD, anxiety, depression, OCD | Typical developmental milestone attainment |
| Mixed ASD with Developmental Delay | ~19% | Social communication challenges, developmental delays, restricted/repetitive behaviors | Language delays, intellectual disability, motor disorders | Significant developmental delays in walking/talking |
| Moderate Challenges | ~34% | Core autism behaviors present but less pronounced | Generally absence of co-occurring psychiatric conditions | Typical developmental milestone attainment |
| Broadly Affected | ~10% | Severe challenges across all core domains | Multiple co-occurring conditions including anxiety, depression, mood dysregulation | Significant developmental delays |
Genetic Architecture Underlying Subtypes
These phenotypic subtypes demonstrate distinct genetic architectures, validating their biological validity. The Broadly Affected subgroup shows the highest proportion of damaging de novo mutations (those not inherited from parents), while only the Mixed ASD with Developmental Delay group was more likely to carry rare inherited genetic variants [5]. Crucially, subtypes also differ in the temporal dynamics of genetic disruptions, with the Social/Behavioral Challenges subtype showing mutations in genes that become active later in childhood, aligning with their later clinical presentation [5]. Another 2025 study further established that common polygenic architecture can be broken down into two genetically correlated factors (rg = 0.38) associated with early versus late diagnosis [24].
Stratification Methodologies for Clinical Trials
Foundations of Stratified Randomization
Stratified randomization is the partitioning of subjects and results by a factor other than the treatment given to ensure equal allocation of subgroups of participants to each experimental condition [69]. This methodology serves to control for confounding variables—factors that might influence the outcome independent of treatment effects—thereby increasing the likelihood of detecting a true treatment effect if one exists [69].
For small trials (<400 patients), stratification prevents type I error and improves power when the stratification factors have a large effect on prognosis [70]. The maximum desirable number of strata should be kept small to maintain practicality in trial execution [70].
Proposed Stratification Framework for Autism Trials
We propose a multi-dimensional stratification framework that integrates recent biological insights with clinical trial methodology:
Table 2: Stratification Dimensions for Autism Clinical Trials
| Stratification Dimension | Specific Measures | Application in Trial Design |
|---|---|---|
| Genetic Stratification | De novo mutation burden, rare inherited variants, polygenic risk scores for specific ASD factors | Enrichment for specific biological pathways; exclusion of populations unlikely to respond |
| Phenotypic Subtype | Alignment with identified subtypes (Social/Behavioral, Mixed ASD with DD, etc.) | Ensuring balanced allocation of subtypes across treatment arms; targeted recruitment of responsive subtypes |
| Developmental Stage | Chronological age, developmental age, age at diagnosis | Accounting for critical periods of intervention; analysis of age-dependent treatment effects |
| Biomarker Profile | EEG patterns, MRS measures of GABA/glutamate, eye-tracking metrics, plasma oxytocin levels | Predictive enrichment for patients most likely to respond to specific mechanism of action |
| Co-occurring Conditions | ADHD, anxiety, intellectual disability, seizure disorders | Control for confounding medications and symptoms; subgroup analysis |
The Phase 2m Biomarker Exploration Phase
The conventional clinical trial pathway (Phase 1-3) is insufficient for heterogeneous conditions. We advocate for the explicit incorporation of a "Phase 2m" (marker exploration phase) specifically dedicated to developing biomarker profiles for stratification [67]. This phase should:
- Utilize a moderately large population (n=several hundred) to capture heterogeneity
- Incorporate a rich set of biomarkers including genomic, neuroimaging, electrophysiological, and behavioral measures
- Employ blinded crossover designs or staggered start designs to distinguish true biomarker-response relationships from placebo effects
- Focus on identifying mechanistic biomarkers (e.g., GABAergic activity markers for GABAergic agents) and broader biomarker profiling for unpredicted relationships [67]
Experimental Protocols for Stratification
Protocol for Subtype Identification in Trial Screening
Objective: To classify trial participants into validated autism subtypes for stratified randomization.
Materials:
- Social Communication Questionnaire-Lifetime (SCQ)
- Repetitive Behavior Scale-Revised (RBS-R)
- Child Behavior Checklist 6-18 (CBCL)
- Developmental history form (milestones, medical history)
- Genetic sequencing data (whole exome or genome)
Procedure:
- Administer standardized questionnaires and collect developmental history during screening
- Extract 239 item-level and composite phenotype features [68]
- Apply pre-trained generative finite mixture model (GFMM) to assign probabilistic class membership
- Confirm genetic characterization where feasible (e.g., de novo mutation analysis)
- Utilize subtype classification for stratification in randomization procedure
Analysis: Participants are stratified across treatment arms based on subtype classification, with additional stratification by age and verbal IQ if sample size permits.
Protocol for Biomarker-Driven Enrichment
Objective: To identify patients most likely to respond to a GABA-B agonist based on neurophysiological biomarkers.
Materials:
- Magnetic resonance spectroscopy (MRS) for GABA quantification
- EEG equipment for gamma band activity measurement
- Plasma serotonin level assessment
- Eye-tracking system for pupillometry
Procedure:
- Conduct baseline biomarker assessments prior to randomization
- Analyze MRS data for GABA levels in target regions (e.g., prefrontal cortex)
- Calculate EEG gamma power as indicator of GABAergic interneuron function
- Correlate biomarker status with primary outcome measure in Phase 2m
- Establish biomarker threshold for predictive enrichment in Phase 3
Analysis: Use receiver operating characteristic (ROC) analysis to determine optimal biomarker cutpoints for predicting clinical response.
Visualization of Stratification Frameworks
Stratified Trial Workflow for Heterogeneous Populations
Phase 2m Biomarker Development Pathway
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for Stratified Autism Trials
| Reagent/Material | Function | Application in Stratification |
|---|---|---|
| Whole Exome/Genome Sequencing Kits | Comprehensive identification of genetic variants | Genetic stratification by de novo mutations, rare inherited variants, and polygenic risk profiles |
| Standardized Phenotypic Assessments (SCQ, RBS-R, CBCL) | Quantification of core and associated features | Phenotypic subtyping using validated instrument batteries |
| Magnetic Resonance Spectroscopy | In vivo measurement of neurotransmitter levels | Biomarker identification for target engagement (e.g., GABA/glutamate levels) |
| High-Density EEG Systems | Recording of neural oscillatory activity | Identification of electrophysiological biomarkers (e.g., gamma band activity) |
| Eye-Tracking Systems | Quantification of visual attention and pupillometry | Objective behavioral biomarkers of social attention and arousal |
| Multiplex Immunoassays | Measurement of protein biomarkers in plasma/serum | Assessment of inflammatory markers, growth factors, oxytocin levels |
| Biomarker Data Integration Platform | Computational analysis of multi-modal data | Implementation of classification algorithms for subtype assignment |
The stratification of clinical trials in heterogeneous populations like autism is no longer a theoretical ideal but an operational necessity. The continued failure of monolithic trials threatens the entire neurodevelopmental drug development enterprise. The methodologies outlined herein—grounded in recent advances in autism biology and subtype identification—provide a actionable framework for implementing stratification across the clinical development pathway.
Future directions must include:
- Development of standardized, scalable biomarker panels for routine clinical trial implementation
- Refinement of autism subtypes through integration of multi-omic data (transcriptomic, epigenomic, proteomic)
- Adaptive trial designs that allow for stratification refinement during the trial
- Increased inclusion of diverse ancestral backgrounds to ensure stratification generalizability [17]
The vision of precision medicine for autism will remain elusive without systematic approaches to clinical trial stratification. By embracing the complexity of autism as a complex systems disorder and designing trials that account for its heterogeneity, we can finally translate biological insights into meaningful treatments for specific subgroups of individuals.
The pharmacological treatment landscape for Autism Spectrum Disorder (ASD) presents a fundamental paradox: despite the condition's defining core symptoms of social communication deficits and restricted/repetitive behaviors, currently approved medications exclusively target interfering comorbidities rather than these central features. This whitepaper examines the complex etiological and neurobiological underpinnings of ASD that have hindered development of core symptom treatments, analyzes the current comorbidity-focused treatment paradigm, and explores emerging research directions that leverage our growing understanding of ASD as a complex systems disorder. By synthesizing findings from genetic studies, molecular pathways, and clinical trials, this analysis provides researchers and drug development professionals with a comprehensive framework for understanding the existing treatment landscape and future opportunities for targeted interventions.
Autism Spectrum Disorder (ASD) is a group of neurodevelopmental disorders characterized by core deficits in social interaction and communication, alongside restricted interests and repetitive behaviors [71]. With current prevalence estimates reaching 1 in 36 children according to the Centers for Disease Control and Prevention, ASD represents one of the most common neurodevelopmental disorders worldwide [72]. The diagnostic criteria for ASD center on these two core symptom domains, yet the clinical presentation is remarkably heterogeneous, often accompanied by numerous co-occurring medical and psychiatric conditions [73].
The pharmacological treatment landscape for ASD reveals a significant disconnect between diagnostic criteria and therapeutic options. Presently, only two medications - risperidone and aripiprazole - have received FDA approval for use in ASD, and both are indicated specifically for treating irritability associated with autism rather than core symptoms [72] [74]. This discrepancy underscores a fundamental challenge in ASD therapeutics: the core symptoms have proven remarkably resistant to pharmacological intervention, while associated comorbidities often respond to targeted treatments.
This whitepaper examines the multifactorial origins of this treatment paradox through the lens of ASD as a complex systems disorder. We analyze the genetic heterogeneity, diverse molecular mechanisms, and complex neurobiology that underlie the core symptoms and complicate targeted drug development. Additionally, we explore how this understanding is informing new approaches that may eventually yield effective treatments for the core symptoms of ASD.
The Current Treatment Landscape: A Comorbidity-Focused Paradigm
Extent and Impact of Comorbidities
The high prevalence of comorbidities in ASD populations is well-documented across multiple large-scale studies. Research utilizing the SPARK study database, which includes over 42,000 individuals with ASD, found that 74% had at least one comorbidity, with affected individuals exhibiting a greater average number of comorbidities than their non-ASD siblings [73]. A separate retrospective chart review of 1,858 children diagnosed with ASD found that 29.0% had at least one significant medical comorbidity, with neurological conditions being most prevalent (37.1%) [75].
Table 1: Prevalence of Common Comorbidities in ASD Populations
| Comorbidity Category | Specific Conditions | Reported Prevalence | Study Details |
|---|---|---|---|
| Psychiatric & Behavioral | Attention/Behavior Problems, Anxiety, Depression | Among most common comorbidities | SPARK Study (N=42,564 ASD individuals) [73] |
| Neurological | Epilepsy, Sleep Disorders, GDD | 23.0% had Global Developmental Delay | Manitoba Study (N=1,858) [75] |
| Neurological | Cerebral Palsy, Seizures, Hypotonia | 37.1% of those with comorbidities | Manitoba Study [75] |
| Genetic Syndromes | Fragile X Syndrome, Rett Syndrome | Varies by specific syndrome | Common genetic disorders with autistic features [71] |
| Gastrointestinal | Feeding Difficulties, GERD | Documented but not quantified | Frequently occurring physical comorbidity [76] |
These comorbidities have significant clinical implications. Left untreated, they can severely impact quality of life, hinder educational and employment opportunities, increase family stress, and in some cases, elevate suicide risk [72]. The high comorbidity burden has naturally directed pharmacological interventions toward these more treatable aspects of ASD, often leaving core symptoms unaddressed by medication management.
Currently Approved Pharmacological Approaches
The current FDA-approved medications for ASD exclusively target irritability and agitation symptoms rather than core diagnostic features:
Risperidone and aripiprazole are both atypical antipsychotics approved for treating irritability in children with ASD [72] [74]. These medications function primarily as dopamine D2 receptor antagonists with additional serotonergic activity, helping to modulate emotional regulation and aggressive behaviors.
Beyond these approved treatments, clinicians frequently prescribe medications off-label to address other common comorbidities:
Table 2: Common Pharmacological Treatments for ASD Comorbidities
| Target Symptom | Medication Classes | Examples | Notes/Differences from Standard Care |
|---|---|---|---|
| Irritability | Atypical Antipsychotics | Risperidone, Aripiprazole | Only FDA-approved medications for ASD symptoms [72] [74] |
| ADHD | α2-adrenergic Agonists | Guanfacine, Clonidine | Often preferred over stimulants for ASD patients [72] |
| Anxiety | Anxiolytics | Buspirone, Mirtazapine | SSRIs often less effective/tolerable in ASD [72] |
| Depression | Antidepressants | Duloxetine, Bupropion, Vortioxetine | Often preferred over SSRIs for ASD patients [72] |
| Sleep Disturbances | Melatonin agonists | Melatonin | First-line with sleep hygiene practices [72] |
Clinical guidance emphasizes that medication approaches for co-occurring conditions in ASD patients often differ from standard of care for neurotypical individuals, with differences in medication efficacy, tolerability, and side effect profiles [72].
The Biological Complexity of Core ASD Symptoms
Genetic Heterogeneity
The remarkable genetic heterogeneity of ASD represents a fundamental challenge for targeted drug development. Research indicates that no single genetic mutation accounts for more than 1-2% of ASD cases [71]. Studies of monozygotic twins have shown concordance rates up to 90%, supporting strong genetic components, but the disorder's etiology involves numerous genes and biological pathways [71].
Advanced genomic techniques have identified hundreds of genes associated with ASD risk, including:
- Synaptic genes: SHANK/ProSAP, NLGN (neuroligins), NRXN (neurexins) [71] [77]
- Chromatin remodeling genes: CHD8 [71]
- Neuronal signaling genes: GRIK2, GRM8, GRIN2A/B [71]
- Cell adhesion molecules: CDH9, CDH10, PCDH (protocadherin) [71] [77]
This extensive genetic diversity suggests that ASD represents a common clinical endpoint for numerous distinct biological disturbances, making single-target therapeutic approaches unlikely to benefit broad ASD populations.
Diverse Molecular and Cellular Mechanisms
Beyond genetic heterogeneity, research has revealed multiple disrupted biological pathways contributing to ASD pathogenesis:
Synaptic Dysfunction: Mutations in genes encoding synaptic proteins like neurexins, neuroligins, and SHANK family proteins suggest that impaired synaptogenesis and synaptic plasticity represent core pathophysiological mechanisms in ASD [71] [77]. These proteins organize pre- and post-synaptic complexes crucial for neuronal communication, and their disruption can alter neural circuit formation and function.
Excitation/Inhibition Imbalance: Alterations in GABAergic signaling and glutamatergic transmission may create an imbalance between excitatory and inhibitory activity in key brain circuits [77]. This imbalance particularly affects networks involved in social behavior, communication, and information processing.
Neuroimmune Interactions: Immune system disturbances and neuroinflammation have been increasingly recognized as contributors to ASD pathophysiology [77]. Aberrant cytokine profiles, microglial activation, and maternal immune activation during pregnancy may influence fetal brain development.
Calcium Signaling Alterations: Abnormalities in calcium channel function and intracellular calcium signaling can affect numerous neuronal processes including neurotransmitter release, synaptic plasticity, and gene expression [77].
The diagram below illustrates how these diverse mechanisms interconnect to contribute to ASD core symptoms:
ASD Core Symptom Pathophysiology
This complex web of interacting biological systems creates substantial challenges for developing unitary pharmacological treatments for core ASD symptoms, as interventions targeting single pathways may only benefit specific ASD subgroups.
Methodological Approaches in ASD Research
Experimental Models and Research Tools
Research into ASD mechanisms employs diverse methodological approaches across multiple biological levels:
Genetic Analysis Methods:
- Genome-wide Association Studies (GWAS): Identify common genetic variants associated with ASD risk across populations [71]
- Exome and Whole-Genome Sequencing: Detect rare inherited and de novo mutations contributing to ASD susceptibility, particularly in simplex families [71]
- Copy Number Variation (CNV) Analysis: Identify chromosomal rearrangements and deletions/duplications associated with ASD
Animal Models:
- Genetic Manipulation: Creating transgenic mice with mutations in ASD-associated genes (e.g., SHANK, NLGN, MECP2) to study resulting behavioral and neurobiological phenotypes [71]
- Environmental Exposure Models: Investigating effects of prenatal insults (e.g., maternal immune activation, certain medications) on neurodevelopment
Clinical Assessment Tools:
- Behavioral Phenotyping: Standardized assessments including ADOS-2 (Autism Diagnostic Observation Schedule) for core symptom evaluation [75]
- Neuroimaging: MRI, fMRI, and DTI to examine brain structure, function, and connectivity
- Electrophysiology: EEG and ERP measures to study neural processing differences
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Materials for ASD Investigation
| Research Tool Category | Specific Examples | Research Applications |
|---|---|---|
| Genetic Models | SHANK3 KO mice, NLGN mutants, FMR1 KO (Fragile X model) | Study synaptic, behavioral phenotypes of ASD-risk gene mutations [71] |
| Cell Culture Systems | Patient-derived iPSCs, Cerebral organoids | Model human neurodevelopment and screen therapeutic compounds [77] |
| Molecular Biology Reagents | SNPs arrays, RNA-seq libraries, CRISPR-Cas9 systems | Identify risk variants, profile transcriptome, manipulate genes [71] |
| Neurobiological Assays | Calcium imaging dyes, Electrophysiology setups, Synaptic markers | Study neuronal signaling, connectivity, and synaptic function [77] |
| Behavioral Assessment | Social approach tasks, Repetitive behavior measures, Learning assays | Quantify core ASD-related behaviors in model systems [71] |
Emerging Directions and Future Perspectives
Despite the historical focus on comorbid symptoms, research into treatments targeting core ASD features is advancing across several fronts:
Targeted Biological Interventions:
- Arbaclofen: GABA-B receptor agonist that may restore excitatory/inhibitory balance, particularly in Fragile X Syndrome [74]
- Oxytocin: Neuropeptide involved in social cognition being investigated for enhancing social function in ASD [74]
- Bumetanide: NKCC1 chloride transporter inhibitor that may restore GABAergic inhibition [74]
- Trofinetide: Synthetic analog of glycine-proline currently in clinical trials [74]
Mechanism-Based Approaches: Research is increasingly focusing on identified molecular pathways rather than generic symptom reduction:
- mGluR5 antagonists in Fragile X Syndrome represent a paradigm for targeting specific genetic subtypes [74]
- Metformin is being investigated for its potential effects on metabolic pathways relevant to ASD [74]
- Cannabidiol is being studied for its modulatory effects on neural signaling and behavior [74]
The following diagram illustrates a strategic framework for future ASD therapeutic development:
Future ASD Therapeutic Framework
This approach recognizes ASD as a complex systems disorder requiring targeted interventions matched to specific biological subtypes, moving beyond the current one-size-fits-all comorbidity management paradigm.
The current focus of approved ASD medications on comorbidities rather than core symptoms reflects the fundamental biological complexity of autism spectrum disorder. The extensive genetic heterogeneity, diverse molecular mechanisms, and varied neural circuit alterations underlying ASD have presented significant challenges for developing effective pharmacological treatments targeting social-communication deficits and restricted/repetitive behaviors. The comorbidity-focused treatment paradigm addresses the most pressing and tractable symptoms while research continues to unravel ASD's complex pathophysiology. Future progress will likely depend on identifying biologically defined ASD subtypes, developing biomarkers for patient stratification, and creating interventions that target specific molecular pathways rather than generic behavioral symptoms. This precision medicine approach offers the promise of eventually addressing the core symptom conundrum that has long defined autism pharmacotherapy.
Overcoming Hurdles in Drug Repurposing and Novel Therapeutic Development
Autism spectrum disorder (ASD) represents one of the most complex challenges in neuropsychiatric therapeutics, characterized by vast genotypic and phenotypic heterogeneity. As the most strongly genetic of all complex neuropsychiatric disorders, ASD involves hundreds of genetic and genomic disorders, with no single gene accounting for more than 1% of cases [57]. This heterogeneity manifests in variable profiles of strengths and deficits, change over time, and comorbidities with common psychiatric conditions, defining ASD as a true complex systems disorder rather than a single disease entity. The traditional drug development pipeline remains extraordinarily complex, resource-intensive, and time-consuming, typically requiring $1-3 billion in investment and spanning 9-15 years from target identification to market approval [78]. In this context, drug repurposing has emerged as a promising strategy to accelerate therapeutic development for ASD by identifying new therapeutic indications for existing, marketed drugs, thereby substantially reducing the risks, costs, and time typically required [79].
Key Challenges in Autism Therapeutic Development
Biological Complexity and Heterogeneity
The development of effective therapeutics for autism spectrum disorder faces fundamental challenges rooted in its biological complexity:
- Genotypic Heterogeneity: Genome-wide association studies have identified de novo variations strongly implicated in ASD, but the condition involves hundreds of genetic and genomic disorders, the majority of which remain unknown [57]
- Phenotypic Variability: Individuals with ASD span the entire range of IQ and language function, with variable profiles of strengths and deficits, symptom characteristics, and developmental trajectories [57]
- Diagnostic Limitations: ASD is still defined and diagnosed behaviorally rather than through biological markers, creating challenges for patient stratification and treatment targeting [57]
Biomarker Limitations in Clinical Applications
The search for reliable biomarkers for ASD has encountered significant hurdles across multiple domains:
Table 1: Challenges in ASD Biomarker Development
| Challenge Category | Specific Limitations | Impact on Therapeutic Development |
|---|---|---|
| Sensitivity | Low universal applicability of proposed biomarkers spanning gene expression, proteomics, metabolomics, and neuroimaging [57] | Inability to positively identify majority of study participants; limits patient stratification |
| Specificity | Proposed biomarkers often associated with multiple neuropsychiatric conditions beyond ASD [57] | Compromised diagnostic accuracy and treatment targeting |
| Clinical Relevance | High measurement variability, cost-prohibitive technologies, requirement for specialized expertise [57] | Limited translation from research to clinical practice |
| Developmental Dynamics | Phenotypic manifestations unfold over time through dynamic developmental interactions [57] | Challenge in identifying developmentally invariant biomarkers |
Promising Repurposing Strategies and Case Studies
Mechanism-Driven Repurposing Approaches
Recent advances have identified several promising mechanism-driven repurposing strategies for ASD therapeutics:
Cerebral Folate Deficiency (CFD) Targeting The FDA recently initiated the approval of leucovorin calcium tablets for patients with cerebral folate deficiency (CFD), a neurological condition that affects folate transport into the brain. Individuals with CFD have been observed to have developmental delays with autistic features, seizures, and problems with movement and coordination [80]. The FDA conducted a systematic analysis of literature published between 2009-2024, including published case reports with patient-level information, and determined that the information supports a finding that leucovorin calcium can help individuals suffering from CFD. This repurposing effort reflects the FDA's commitment to identify opportunities to repurpose drugs to treat chronic diseases and to finding and treating the root causes of autism [80].
Epilepsy Drug Repurposing for Shared Neural Circuitry Stanford Medicine scientists investigating the brain mechanisms of autism have identified hyperactivity in the reticular thalamic nucleus as a driver of autism-like behaviors in mice. This brain region serves as a gatekeeper of sensory information between the thalamus and cortex. Researchers successfully reversed autism-like symptoms by administering drugs that suppressed this area of the brain, including the experimental seizure drug Z944 [81]. The connection between autism and epilepsy is well-established, with epilepsy being much more prevalent in people with autism than in the general population (30% versus 1%). This approach highlights where processes underlying autism and epilepsy may overlap in the brain and why they often occur in the same patients [81].
Data-Driven Repurposing Methodologies
Computational approaches have emerged as powerful tools for systematic drug repurposing:
Literature-Based Repurposing Pipeline A novel literature-based approach analyzes biomedical literature data through the Jaccard coefficient to identify potential drug pairs for repurposing. This method established connections between drugs and literature through genes associated with the literature, effectively creating a citation network based on literature related to drugs [79]. The methodology demonstrated that literature-based Jaccard similarity outperformed other similarity measures based on AUC and F1 score, enabling identification of de novo drug repurposing candidates using a threshold defined as the γth upper quantile of Jaccard similarities [79].
Table 2: Computational Drug Repurposing Platforms and Applications
| Platform/Method | Data Sources | Key Applications | ASD Relevance |
|---|---|---|---|
| Literature-Based Jaccard Similarity | PubMed, OpenAlex, citation networks [79] | Drug-drug similarity measurement, candidate prioritization | Identification of shared biological pathways relevant to ASD |
| Pathway-Based Computational Pipeline | ChEMBL, BindingDB, GtoPdb [78] | Repositioning predictions across disease types | Application to neurodevelopmental disorders |
| Network-Based Proximity Quantification | Human interactome, disease genes, drug targets [79] | Quantifying proximity between disease genes and drug targets | Mapping ASD genetic risk factors to known drug targets |
| Multi-Modal Deep Learning (MMAtt-DTA, TransDTI) | Drug-target interaction databases [78] | Predicting binding affinities across chemical and proteomic spaces | Screening existing drugs against ASD-relevant protein targets |
Experimental Design and Methodological Frameworks
In Silico Repurposing Workflow
The computational pipeline for drug repurposing involves multiple integrated steps from data acquisition to experimental validation:
Preclinical Validation Protocol
For candidates identified through computational methods, rigorous preclinical validation is essential:
Neuromodulation Studies for Causal Validation Using DREADD-based neuromodulation, researchers can suppress overactivity in specific brain regions like the reticular thalamic nucleus and reverse behavioral abnormalities in autism mouse models. This approach enables researchers to induce behavioral deficits in normal mice by ramping up activity in targeted brain regions, establishing causal relationships rather than mere correlations [81].
Comprehensive Behavioral Assessment The study flow for preclinical validation should follow established templates for complex experimental designs, incorporating detailed inclusion/exclusion criteria and accounting for attrition at each stage [82]. This includes:
- Sensory Processing Assessments: Measuring responses to stimuli like light or puff of air in model systems
- Motor Activity Monitoring: Quantifying increased motor activity as autism-like behavior
- Seizure Susceptibility Testing: Evaluating spontaneous activity bursts causing seizures
- Social Behavior Analysis: Assessing core social interaction deficits
Table 3: Key Research Reagents and Platforms for ASD Drug Repurposing
| Resource Category | Specific Tools | Function and Application | Access Considerations |
|---|---|---|---|
| Drug-Target Databases | ChEMBL, BindingDB, GtoPdb [78] | Provide curated drug-target interaction data, binding affinities, and pharmacological profiles | Publicly available with version-controlled releases |
| Literature Mining Platforms | OpenAlex, PubMed [79] | Enable literature-based similarity calculations and citation network analysis | Comprehensive coverage of biomedical literature |
| Computational Prediction Tools | MMAtt-DTA, TransDTI [78] | Predict binding affinities for compounds and protein targets using deep learning | Require high-quality training data from curated databases |
| Experimental Validation Systems | DREADD-based neuromodulation, Cntnap2 KO mice [81] | Establish causal relationships between target engagement and behavioral outcomes | Specialized expertise required for implementation |
| Clinical Data Resources | repoDB [79] | Provide standardized datasets for validation of repurposing predictions | Benchmark against known drug-disease associations |
The complex systems nature of autism spectrum disorder demands innovative approaches to therapeutic development. Drug repurposing represents a promising strategy to overcome traditional hurdles in this field, leveraging existing compounds with known safety profiles to address the multifaceted biology of ASD. The integration of computational approaches with mechanistic insights into shared neural circuitry, as demonstrated by the repurposing of epilepsy medications and folate pathway treatments, provides a roadmap for future efforts. Success in this endeavor will require continued advancement in biomarker development, patient stratification strategies, and computational methods that can navigate the biological complexity of ASD. As these approaches mature, they offer the potential to deliver meaningful therapeutics to address the diverse needs of individuals with autism spectrum disorder.
The Autism Data Science Initiative (ADSI), launched in 2025 by the National Institutes of Health (NIH), represents a landmark $50 million research effort designed to unlock the complex causes of autism spectrum disorder (ASD) and improve long-term outcomes [83]. This initiative marks a strategic pivot toward leveraging large-scale, multi-dimensional data resources to explore the multifaceted contributors to autism's rising prevalence. ADSI funds 13 pioneering projects that harness a wide array of data types, including genomic, epigenomic, metabolomic, proteomic, clinical, behavioral, and autism services data [83]. A defining characteristic of ADSI is its commitment to a comprehensive exposomics approach, studying environmental, medical, and lifestyle factors in combination with genetics and biology. This includes investigating environmental contaminants like pesticides and air pollutants, maternal nutrition and diet, perinatal complications, psychosocial stress, and immune responses during critical windows of early development [83]. The initiative aims to integrate, aggregate, and analyze existing data resources, generate targeted new data, and, crucially, validate findings through independent replication hubs to ensure transparency, reproducibility, and real-world applicability [83].
Autism as a Complex Systems Disorder: The Imperative for a Data Science Framework
Autism Spectrum Disorder (ASD) epitomizes a complex systems disorder, characterized by vast heterogeneity in its behavioral presentation, underlying biology, and developmental trajectories. The reported prevalence of ASD in the United States has risen dramatically from fewer than 1 in 2,000 children in the 1970s to approximately 1 in 31 among 8-year-old children in a 2022 sample, underscoring the urgency of this research [34] [83]. This increase, coupled with the absence of universal biomarkers or singular causative factors, highlights the limitations of traditional, reductionist research models. The disorder's etiology is now understood to be multifactorial, involving a strong genetic component alongside a range of less-understood nongenetic factors [83] [84].
A complex systems view necessitates a shift from seeking single causes to understanding the dynamic, multilevel interactions within neurodevelopmental pathways. As illustrated by the "developmental cascades" framework, development emerges from dynamic interactions among networks of neural activity, behavior systems, and experience-dependent processes [85]. In this model, a change in one domain (e.g., motor skills like sitting) can have far-reaching, cross-domain effects on other, seemingly unrelated areas (e.g., language and social communication) [85]. For instance, delayed independent sitting in infants with ASD can constrain opportunities for sophisticated object manipulation and joint attention with caregivers, thereby altering the language input the infant receives and potentially cascading into social-communication differences [85]. This framework captures the cumulative, transactional nature of development, where unique pathways driven by individual-context interactions lead to the diverse phenotypes observed in ASD.
Theoretical models like the Pathogenetic Triad and the Rigid-Autonomous Phase Sequence (RAPS) further conceptualize autism as a systems-level disorder. The Pathogenetic Triad deconstructs autism into three interacting features: a common Autistic Personality dimension (a non-pathological core), Cognitive Capacity (compensation), and Neuropathological Burden (risk factors) [84]. It posits that risk factors disrupt neurodevelopment, which secondarily inhibits cognitive capacity, thereby "disinhibiting" a maladaptive behavioral phenotype from the core autistic dimension [84]. Similarly, the RAPS theory suggests that individuals with ASD exhibit altered, inflexible neural connections (phase sequences) that lead to cognitive, sensory-motor, and memory-related challenges, providing a unifying neural explanation for diverse symptoms [86]. These models, combined with the cascades framework, provide a compelling theoretical foundation for why a data science approach that can model complexity and interaction is essential for progress.
Core Methodological Paradigms and Technical Approaches in ADSI
The ADSI employs a suite of advanced analytical methods to tackle the complexity of ASD. These methodologies are designed to handle the "big data" characterized by high volume, velocity, and variety [87], moving from raw data to usable scientific insight.
Big Data Analytics and Integrative Omics
A core technical challenge in autism data science is the management and analysis of large-scale datasets. ADSI projects involve the integration of diverse data types—from genetics and epigenetics to clinical and environmental exposures. This requires sophisticated computational hardware and software solutions to handle storage and processing demands that can range from hundreds of gigabytes for a single genome to terabytes for brain imaging data [87]. A critical methodological step is ensuring data veracity, the "4th V" of big data. In autism research, a primary data quality issue is the validation of ASD diagnoses in large datasets, where reliance on billing or diagnostic codes can be error-prone [87]. ADSI emphasizes rigorous quality control, such as using validated algorithms (e.g., from the Chronic Conditions Warehouse for claims data) or conducting chart reviews on subsets to confirm clinical diagnoses [87].
Causal Inference and Machine Learning
A significant methodological challenge in large observational studies is confounding, where an observed association may be due to unmeasured variables [87]. ADSI promotes advanced causal inference methods to address this. For example, sibling control studies—a workaround enabled by large sample sizes—can help control for unobserved genetic and familial confounding by comparing discordantly exposed siblings [87]. Furthermore, ADSI leverages machine learning and deep learning to enhance diagnostic accuracy, personalize interventions, and identify subtypes from multimodal data [88]. These data-driven methods can uncover complex, non-linear patterns within the data that traditional statistics might miss. However, challenges such as algorithmic bias, model interpretability ("black box" problems), and the need for diverse, representative datasets remain significant hurdles for widespread implementation [88].
Exposome-Wide Association Studies (ExWAS) and Gene-Environment Interaction Modeling
Mirroring the genome-wide association study (GWAS) approach, ADSI's focus on exposomics necessitates methods like exposome-wide association studies (ExWAS). These analyses systematically test a vast array of environmental exposures for association with ASD risk, without prior hypotheses. This is complemented by sophisticated models of gene-environment interaction (GxE), which investigate how genetic susceptibility and environmental exposures interact to influence neurodevelopment and ASD probability. Projects within ADSI are using these methods to examine how prenatal exposures interact with genetic risk in large autism cohorts [83]. The integration of exposome data with genomic and other omics data is a key innovation, requiring specialized statistical models and computational frameworks to manage the high dimensionality and complexity of the data.
Table 1: Core Data Types and Analytical Methods in the ADSI Framework
| Data Category | Specific Data Types | Core Analytical Methods | Primary Objective |
|---|---|---|---|
| Genomic & Molecular | Genomics, Epigenomics, Metabolomics, Proteomics | Integrative Omics, Machine Learning, Organoid Models | Identify biological pathways and biomarkers for ASD. |
| Clinical & Behavioral | Electronic Health Records, Diagnostic Codes, Behavioral Assessments | Natural Language Processing, Predictive Modeling, Validation Algorithms | Validate ASD phenotypes, model disease progression and outcomes. |
| Environmental & Exposomic | Air Pollutants, Pesticides, Maternal Health Data, Diet | Exposome-Wide Analysis (ExWAS), Causal Inference (e.g., Sibling Designs) | Uncover environmental risk factors and GxE interactions. |
| Services & Outcomes | Medicaid/Medicare Claims, Service Utilization Data | Big Data Analytics, Longitudinal Modeling | Improve service delivery and understand adult outcomes. |
Experimental Protocols and Workflows for Key Analytical Approaches
Protocol 1: Validating ASD Phenotypes in Large Administrative Datasets
Objective: To ensure the accurate identification of ASD cases in large-scale electronic health record (EHR) or insurance claims databases for downstream analysis. Materials: Source database (e.g., Medicaid T-MSIS Analytic Files), validated algorithm for ASD detection. Methodology:
- Population Definition: Restrict the study sample to children within the target age range (e.g., 3-17 years) who were continuously enrolled in the health plan for a defined period (e.g., at least 89 days in a calendar year) [34].
- Case Identification: Apply a validated algorithm to identify children with ASD. A common approach is to require at least two outpatient billing codes for ASD (ICD-9: 299.XX; ICD-10: F84.X) or one inpatient billing code for ASD within the specified year [34] [87].
- Validation Sub-study (if possible): For a random subset of identified cases, conduct a manual chart review to confirm the diagnosis based on standardized criteria (e.g., DSM-5). This step assesses the Positive Predictive Value (PPV) of the algorithm [87].
- Data Quality Control: Check for implausible data patterns (e.g., terminal digit preference in physiological measurements) that may indicate systematic recording errors [87].
Protocol 2: Sibling-Control Study for Causal Inference
Objective: To control for unmeasured genetic and familial confounding when assessing the relationship between a putative risk factor (e.g., prenatal exposure) and ASD. Materials: Population-based registries with linked family data, data on exposure and ASD diagnosis. Methodology:
- Cohort Identification: Identify families in the registry with at least two children (sibling pairs).
- Exposure Assessment: Determine the exposure status (e.g., in utero antidepressant exposure) for each sibling.
- Case Ascertainment: Identify ASD diagnosis within each sibling using validated methods from Protocol 1.
- Discordant Pair Analysis: Select sibling pairs who are discordant for both the exposure and the outcome. This creates matched sets where one sibling was exposed and has ASD, and the other was unexposed and does not have ASD.
- Statistical Analysis: Use conditional logistic regression models stratified by family to compare the odds of ASD between exposed and unexposed siblings. This design inherently controls for all factors that are shared between siblings (e.g., maternal genetics, shared home environment) [87].
Table 2: Key Research Reagents and Resources for Autism Data Science
| Resource Category | Specific Item | Function & Application |
|---|---|---|
| Data Repositories & Cohorts | NIH ADSI Funded Projects [83] | Provides integrated, multi-omics and exposomic data for hypothesis testing and model validation. |
| Autism and Developmental Disabilities Monitoring (ADDM) Network [34] | Supplies community-level, record-review-based prevalence estimates and demographic data for epidemiological studies. | |
| Medicaid Analytic eXtract (MAX) / T-MSIS Analytic Files (TAF) [34] | Large-scale administrative claims data for studying healthcare utilization, treatment patterns, and comorbidities in ASD. | |
| Analytical Software & Tools | Machine Learning Frameworks (e.g., TensorFlow, PyTorch) [88] | Enable development of predictive models for diagnosis, prognosis, and subgroup identification from complex data. |
| Causal Inference Software (e.g., for sibling designs, propensity scoring) [87] | Facilitate robust analysis of potential risk factors by accounting for observed and unobserved confounding. | |
| Color Contrast Analyzers (e.g., WebAIM's Checker) [89] | Ensure data visualizations and scientific tools meet accessibility standards (WCAG) for all users, including those with low vision. | |
| Computational Models | Organoid Models [83] | Used within ADSI to study how gene-environment interactions affect neurodevelopment in a controlled, human-derived model system. |
| The Pathogenetic Triad Framework [84] | A theoretical model for deconstructing ASD into core, compensatory, and risk components to guide experimental design and data interpretation. |
The NIH Autism Data Science Initiative represents a paradigm shift in autism research, moving the field toward a more integrative, data-driven, and systems-oriented understanding of the disorder. By harnessing big data, advanced analytics, and a commitment to causal inference and validation, ADSI is poised to make significant strides in elucidating the complex etiology of ASD and improving the lives of individuals on the spectrum and their families. The future of autism research lies in continued innovation in these methodologies, a steadfast commitment to ethical data use and algorithmic fairness, and the fostering of collaborative, interdisciplinary science that can translate data-driven insights into meaningful clinical applications.
Validating the Framework: Comparative Analysis of Subtypes, Models, and Therapeutic Outcomes
Recent advancements in autism spectrum disorder (ASD) research have successfully deconstructed the condition's profound heterogeneity by identifying biologically distinct subtypes. A landmark 2025 study published in Nature Genetics analyzed phenotypic and genotypic data from over 5,000 individuals in the SPARK cohort, revealing four clinically and genetically distinct ASD subtypes. This whitepaper provides a technical breakdown of the divergent genetic architectures, implicated biological pathways, and developmental timelines characterizing these subtypes. We present structured comparative data, detailed experimental methodologies from the cited research, and visualizations of disrupted genetic programs. The findings underscore autism's nature as a complex systems disorder, comprising multiple etiologically distinct conditions that require tailored research and therapeutic strategies.
Autism spectrum disorder (ASD) represents a classic example of a complex systems disorder, characterized by extensive phenotypic and genetic heterogeneity that has long challenged coherent biological explanation [68]. The condition is highly heritable, yet traditional genetic analyses explain only approximately 20% of cases, suggesting the existence of multiple distinct biological narratives rather than a single unified etiology [5] [90]. The prevailing "spectrum" model, while clinically useful, often obscures the underlying discrete pathophysiological mechanisms. Research has identified hundreds of ASD-associated genes, but mapping these genetic variations to specific clinical presentations has remained elusive until recently [68] [90]. A paradigm-shifting study employing a person-centered computational approach has now identified four robust ASD subtypes, each with distinct genetic signatures and developmental trajectories [5] [68] [7]. This decomposition of phenotypic heterogeneity reveals that what was previously considered a single complex system actually comprises multiple biologically distinct disorders with shared behavioral manifestations, offering a new framework for precision medicine in autism research and therapeutic development.
Subtype Characterization and Clinical Profiles
The identification of ASD subtypes was achieved through a person-centered analysis of 239 phenotypic features across 5,392 individuals from the SPARK cohort [5] [68]. Unlike trait-centered approaches that examine single variables in isolation, this methodology preserved the complex combinations of traits observed in each individual, much like a clinician would assess a whole person [7]. The general finite mixture model (GFMM) employed could handle heterogeneous data types (continuous, binary, and categorical) simultaneously, identifying four latent classes with distinct clinical profiles [68].
Table 1: Clinical Profiles of ASD Subtypes
| Subtype Name | Prevalence | Core Clinical Features | Developmental Milestones | Common Co-occurring Conditions |
|---|---|---|---|---|
| Social/Behavioral Challenges | 37% | Prominent social difficulties, repetitive behaviors, disruptive behaviors | Typically on time, similar to neurotypical children | High rates of ADHD, anxiety, depression, OCD [5] [91] [92] |
| Moderate Challenges | 34% | Milder core ASD symptoms across all domains | Typically on time | Generally absence of psychiatric comorbidities [5] [91] |
| Mixed ASD with Developmental Delay | 19% | Variable social/behavioral scores, significant developmental delays | Delayed in early milestones (walking, talking) | Language delays, intellectual disability; lower rates of anxiety/depression [5] [91] [92] |
| Broadly Affected | 10% | Severe challenges across all core ASD domains | Significant delays | Multiple psychiatric conditions (anxiety, depression, mood dysregulation), cognitive impairment [5] [91] [92] |
These subtypes demonstrated external validation through distinct patterns of medically diagnosed co-occurring conditions not included in the original model [68]. Notably, the Broadly Affected and Mixed ASD with Developmental Delay subtypes received earlier diagnoses, likely due to more apparent developmental concerns, while the Social/Behavioral Challenges group was diagnosed later despite significant behavioral and psychiatric manifestations [5] [68].
Methodological Framework: Experimental Design and Protocols
Cohort Characteristics and Data Acquisition
The research utilized data from the SPARK (Simons Foundation Powering Autism Research for Knowledge) cohort, the largest autism research study in the United States [17]. The analysis included 5,392 autistic individuals aged 4-18 years with matched genetic data [5] [68]. Participants provided data through:
- Standardized diagnostic questionnaires: Social Communication Questionnaire-Lifetime (SCQ), Repetitive Behavior Scale-Revised (RBS-R), and Child Behavior Checklist 6-18 (CBCL) [68]
- Developmental history forms: Capturing milestone achievement ages and medical history [5]
- Genetic material: Saliva samples for DNA analysis through whole-exome or whole-genome sequencing [17]
The cohort was predominantly of European ancestry (77%), representing a limitation for generalizability to diverse populations [17] [90].
Phenotypic Feature Selection and Processing
Researchers identified 239 item-level and composite phenotype features spanning seven clinically defined categories [68]:
- Limited social communication
- Restricted and/or repetitive behavior
- Attention deficit
- Disruptive behavior
- Anxiety and/or mood symptoms
- Developmental delay
- Self-injury
Features were processed to accommodate different data types (continuous, binary, categorical) within the GFMM framework without assuming normal distributions [68].
Statistical Modeling and Class Validation
The core analytical approach utilized General Finite Mixture Modeling (GFMM) to identify latent classes [68]:
- Model selection: Models with 2-10 latent classes were evaluated using Bayesian Information Criterion (BIC), validation log likelihood, and clinical interpretability
- Four-class solution: Provided optimal balance of statistical fit and clinical relevance
- Stability assessment: The model demonstrated robustness to various perturbations through bootstrapping methods
- Replication: Findings were validated in an independent cohort (Simons Simplex Collection) using 108 matched phenotypic features [68]
Genetic Analysis Protocols
Following phenotypic classification, genetic analyses examined multiple variation types:
- Polygenic risk scores: Calculated for psychiatric traits using summary statistics from genome-wide association studies
- De novo mutations: Identified through trio-based sequencing (comparing affected child to unaffected parents)
- Rare inherited variants: Analyzed through family-based segregation patterns
- Pathway enrichment analysis: Conducted using gene set enrichment methods on genes harboring class-specific mutations [68]
- Developmental gene expression timing: Analyzed using BrainSpan atlas data to determine prenatal vs. postnatal expression peaks [5]
Diagram 1: Experimental workflow for ASD subtyping.
Comparative Genetic Architecture Across Subtypes
Genetic analyses revealed distinct patterns of variation across the four subtypes, providing biological validation of the phenotypic classifications [5] [68] [92].
Table 2: Genetic Profiles Across ASD Subtypes
| Subtype | De Novo Mutation Burden | Inherited Variation Patterns | Polygenic Risk Profiles | Developmental Timing of Genetic Effects |
|---|---|---|---|---|
| Social/Behavioral Challenges | Lower burden | Common variant influence | High genetic predisposition for ADHD, depression, anxiety [92] [93] | Predominantly postnatal gene expression [5] [90] |
| Moderate Challenges | Intermediate burden | Less critical rare variants | Lower polygenic risk scores across domains [5] | Prenatal and neonatal expression peaks [93] |
| Mixed ASD with Developmental Delay | Intermediate burden | High rare inherited variants [5] [92] | Not strongly associated with common psychiatric variants [68] | Predominantly prenatal gene expression [5] [7] |
| Broadly Affected | Highest burden of damaging de novo mutations [5] [92] | Mixed inheritance patterns | Broad dysregulation across multiple domains [92] | Both prenatal and postnatal disruptions [93] |
The Broadly Affected subtype showed the highest burden of damaging de novo mutations, particularly in genes crucial for brain development, many previously associated with intellectual disability and severe developmental disorders [5] [92]. Conversely, the Social/Behavioral group showed stronger influences from common genetic variants associated with psychiatric traits like ADHD and depression, with mutations affecting genes active after birth, particularly in brain regions involved in social and emotional processing [5] [92] [93].
Distinct Biological Pathways and Systems
Pathway analysis revealed strikingly divergent biological processes affected in each subtype, with minimal overlap between classes [7]. Each subtype was associated with distinct molecular pathways, despite all being previously implicated in autism broadly.
Diagram 2: Biological pathways and developmental timing by subtype.
The Social/Behavioral Challenges subtype showed enrichment for mutations affecting biological pathways involved in neuronal action potentials and synaptic signaling, aligning with their presentation of significant behavioral and psychiatric challenges without developmental delays [7]. The Moderate Challenges group demonstrated disruptions in chromatin organization and transcriptional regulation pathways, suggesting more fundamental cellular processes are affected but with milder consequences [7].
The Mixed ASD with Developmental Delay subtype was characterized by mutations in genes critical for early brain development and neuronal migration, consistent with their early developmental presentations [7]. Most remarkably, the Broadly Affected subtype showed evidence of "broad dysregulation" across multiple biological systems without a single predominant pathway, reflecting their widespread clinical challenges [92] [93].
Developmental Trajectories: A Temporal Perspective
A crucial finding was the discovery that subtype-specific genetic disruptions operate on different developmental timelines [5] [90]. Analysis using BrainSpan atlas data revealed that genes harboring damaging mutations in each subtype had distinct temporal expression patterns throughout brain development.
In the Social/Behavioral Challenges group, mutated genes were predominantly active after birth, peaking in expression during childhood and adolescence [5]. This pattern aligns clinically with the absence of developmental delays, later age at diagnosis, and emergence of symptoms coinciding with social and behavioral demands increasing with age.
Conversely, both the Mixed ASD with Developmental Delay and Broadly Affected subtypes showed strong enrichment for mutations in genes with prenatal expression peaks, particularly during early to mid-fetal development [5] [7]. This corresponds with their early apparent developmental delays and earlier diagnoses. The Moderate Challenges group showed an intermediate pattern with some prenatal and neonatal expression peaks [93].
This temporal dimension provides compelling evidence that genetic disruptions occurring at different critical periods of brain development produce distinct autism subtypes with characteristic clinical trajectories.
Table 3: Key Research Reagents and Resources for ASD Subtyping Studies
| Resource Category | Specific Examples | Function/Application |
|---|---|---|
| Cohort Resources | SPARK cohort (n>150,000) [7] [17]; Simons Simplex Collection (SSC) [68] | Large-scale datasets with matched phenotypic and genetic data for discovery and validation |
| Phenotypic Assessments | Social Communication Questionnaire (SCQ) [68]; Repetitive Behavior Scale-Revised (RBS-R) [68]; Child Behavior Checklist (CBCL) [68] | Standardized measures of core ASD features and co-occurring conditions |
| Genetic Sequencing | Whole exome sequencing; Whole genome sequencing; Genotyping arrays [17] | Identification of de novo mutations, rare inherited variants, and common variant contributions |
| Computational Tools | General Finite Mixture Models (GFMM) [68]; Pathway enrichment analysis; Polygenic risk scoring [68] | Statistical modeling of heterogeneous data types and biological interpretation |
| Developmental Expression Data | BrainSpan Atlas of the Developing Human Brain [5] | Mapping genetic findings to specific developmental periods and brain regions |
Discussion and Research Implications
The identification of these four biologically distinct ASD subtypes represents a transformative advancement for autism research and drug development. The findings fundamentally reframe autism as a collection of distinct neurobiological disorders rather than a single spectrum, with direct implications for therapeutic development.
From a clinical trial perspective, these subtypes explain the historical challenge of variable treatment responses and could inform future patient stratification strategies. The distinct genetic pathways identified offer novel targets for precision therapeutics, potentially allowing interventions tailored to an individual's subtype-specific biological profile.
For diagnostic applications, this work moves beyond the current behavior-based classification system toward a more biologically grounded taxonomy. The different developmental timelines observed across subtypes suggest critical windows for intervention may vary substantially between subgroups.
Several limitations and future directions merit emphasis. First, the predominantly European ancestry of the study cohort limits generalizability, as genetic variations can differ across ancestral backgrounds [17] [90]. Second, these four subtypes likely do not represent the complete taxonomy of autism, and additional subtypes may emerge with larger, more diverse samples and inclusion of additional data types [7] [90]. Future research should incorporate non-coding genomic regions, longitudinal data tracking developmental trajectories, and integration with neuroimaging and other biomarker data [7] [93].
This systematic comparison of genetic profiles across ASD subtypes demonstrates that autism's heterogeneity can be decomposed into biologically meaningful subgroups with distinct genetic architectures, pathway disruptions, and developmental trajectories. The Social/Behavioral, Moderate, Mixed ASD with Developmental Delay, and Broadly Affected subtypes each tell different biological stories with direct implications for both basic research and clinical practice.
For researchers and drug development professionals, these findings provide a new framework for understanding autism's pathophysiology, designing targeted interventions, and stratifying clinical trials. The person-centered computational approach demonstrated here also offers a template for deconstructing heterogeneity in other complex neuropsychiatric conditions. As these subtypes are refined and validated, they pave the way for truly personalized approaches to autism treatment and support, moving beyond one-size-fits-all interventions toward precision medicine tailored to an individual's specific biological subtype.
The study of autism spectrum disorder (ASD) has been historically constrained by the limitations of animal models, which often fail to recapitulate the complex genetics and pathophysiology of the human condition. The advent of human pluripotent stem cell (hPSC)-derived brain organoids presents a transformative opportunity to model early human neurodevelopment in a three-dimensional, human-specific context. This whitepaper details the application of these organoid models to validate findings in ASD research, framing ASD as a complex systems disorder. We provide a technical guide on advanced organoid methodologies, quantitative genetic data, standardized experimental protocols, and essential research reagents, aiming to equip scientists with the tools to elucidate the distinct biological narratives underlying autism's heterogeneity.
Autism spectrum disorder is a highly heritable, complex neurodevelopmental condition characterized by remarkable genetic and clinical heterogeneity. While rodent models have provided foundational insights into neurobiology, they present significant limitations for ASD research. These include substantial interspecies variation in brain structure and function, an inability to fully capture human-specific social and cognitive behaviors, and the challenge of modeling a disorder where an estimated 1,000+ risk genes contribute to a spectrum of phenotypes [94] [95]. The "single end-term picture" provided by post-mortem human studies further limits our understanding of dynamic developmental processes [95].
Human brain organoids, derived from induced pluripotent stem cells (iPSCs), offer a powerful alternative. These 3D structures self-organize to mimic the cellular diversity and spatial architecture of the early developing human brain, providing a scalable, patient-specific system to probe the molecular and cellular underpinnings of ASD as it unfolds [96] [95]. A recent landmark study has further underscored the necessity for such human-specific models by identifying four clinically and biologically distinct subtypes of autism, each with unique genetic profiles and developmental trajectories [5] [17]. This finding confirms that ASD is not a single disorder but a collection of multiple "puzzles" with distinct biological narratives, necessitating research models capable of capturing this diversity [5] [17].
The Heterogeneous Landscape of Autism: A Framework for Organoid Research
The genetic architecture of ASD involves a combination of rare de novo mutations, inherited variants, and common genetic variations that converge on a limited number of key biological pathways [95]. The recent identification of four data-driven ASD subtypes provides a crucial new framework for organoid-based research, moving beyond a one-size-fits-all approach [5].
Table 1: Clinically Distinct Subtypes of Autism Spectrum Disorder
| Subtype Name | Prevalence | Core Clinical Features | Co-occurring Conditions | Developmental Milestones |
|---|---|---|---|---|
| Social & Behavioral Challenges | ~37% | High core autism traits (social challenges, repetitive behaviors) | ADHD, anxiety, depression, OCD | Typically on time, similar to neurotypical children |
| Mixed ASD with Developmental Delay | ~19% | Core social challenges, restricted/repetitive behaviors, developmental delay | Generally absent | Delayed (e.g., walking, talking) |
| Moderate Challenges | ~34% | Milder core autism traits | Generally absent | Typically on time |
| Broadly Affected | ~10% | Severe social/communication difficulties, repetitive behaviors | Anxiety, depression, mood dysregulation, intellectual disability | Delayed |
These subtypes are underpinned by distinct genetic architectures. For instance, the "Broadly Affected" subtype shows the highest burden of damaging de novo mutations, often affecting genes associated with chromatin remodeling and synaptic function. In contrast, the "Mixed ASD with Developmental Delay" subtype is more strongly linked to rare inherited variants [5]. Furthermore, the biological impact of these genetic risks unfolds on different developmental timelines; mutations in the "Social and Behavioral Challenges" subtype, for instance, are enriched in genes that become active later in childhood, aligning with its later diagnosis and prominent psychiatric co-morbidities [5]. This refined subtyping allows researchers to generate organoids from patient cohorts with specific genetic and phenotypic profiles, enabling the investigation of subtype-specific pathophysiological mechanisms.
Human Organoid Modeling: Methodologies and Validation
Core Experimental Protocol: Generating ASD Brain Organoids
The following workflow outlines a standard methodology for generating cerebral organoids from patient-derived iPSCs to model ASD [94] [96] [95].
- iPSC Generation and Culture: Generate iPSCs from patient somatic cells (e.g., fibroblasts, blood cells) via reprogramming using defined factors (e.g., Yamanaka factors). Maintain iPSCs in feeder-free conditions using essential media like mTeSR1.
- Embryoid Body Formation: Dissociate iPSCs into single cells and aggregate them in low-attachment plates to form embryoid bodies, in neural induction media.
- Neural Induction and Expansion: After 5-7 days, embed embryoid bodies in Matrigel droplets to provide a 3D scaffold that mimics the extracellular matrix. Transfer to a spinning bioreactor or orbital shaker to enhance nutrient and oxygen exchange.
- Regional Patterning (Optional): To generate region-specific organoids (e.g., cortical, forebrain), add specific morphogens like SMAD inhibitors (e.g., LDN-193189, Noggin) to dorsalize the tissue, or Sonic Hedgehog (SHH) to ventralize it.
- Long-term Maturation: Culture organoids for extended periods (several months), allowing for the emergence of complex neural structures, including layered cortex-like zones, progenitor regions, and diverse cell types (neurons, astrocytes, oligodendrocytes).
- Validation and Characterization:
- Immunohistochemistry: Confirm the presence of neural progenitors (SOX2, Nestin), neurons (TUJ1, MAP2), and cortical layers (CTIP2, TBR1).
- Transcriptomics: Perform RNA sequencing to validate that the organoid's gene expression profile mirrors that of the developing human brain.
- Electrophysiology: Use multi-electrode arrays (MEAs) or patch clamping to confirm functional neuronal network activity.
Diagram 1: Workflow for generating and analyzing patient-derived brain organoids.
Key Signaling Pathways in ASD and Organoid Validation
ASD risk genes converge on a limited set of biological pathways critical for neurodevelopment. The following diagram and table summarize how these pathways can be studied and validated in organoid models.
Diagram 2: Key ASD pathways and validation assays in organoids.
Table 2: Convergent Biological Pathways in ASD and Organoid Interrogation Methods
| Dysregulated Pathway | Key ASD Risk Genes | Functional Consequence | Organoid Validation Assays |
|---|---|---|---|
| Chromatin Remodeling & Transcriptional Regulation | CHD8, MECP2, ADNP | Altered gene expression networks, disrupted neuronal differentiation and connectivity. | Bulk/Single-cell RNA-seq, ATAC-seq, Immunostaining for neuronal markers. |
| mTOR Signaling & Local Protein Synthesis | PTEN, TSC1/2, FMRP | Disrupted synaptic protein homeostasis, neuronal hypertrophy, altered cell proliferation. | Western Blot for phospho-proteins (p-S6, p-AKT), assessment of neuronal soma size. |
| Synaptic Scaffolding & Function | SHANK3, NRXN1/2/3, NLGN3/4 | Imbalanced excitatory/inhibitory (E/I) signaling, defective synaptogenesis. | Multi-electrode Array (MEA) for network activity, Patch-clamp, Immunostaining (vGLUT1, GAD67). |
| Ion Channel Permeability & Neuronal Conduction | SCN2A, CACNA1C, GRIN2B | Altered neuronal excitability and signal transduction, contributing to E/I imbalance. | Calcium Imaging, MEA, Patch-clamp to measure action potentials and currents. |
Success in organoid modeling relies on a standardized set of high-quality reagents and resources. The following table details essential components for generating and analyzing brain organoids for ASD research.
Table 3: Essential Research Reagent Solutions for Brain Organoid Modeling
| Reagent / Resource | Function / Purpose | Example Products / Specifications |
|---|---|---|
| Reprogramming Factors | Generates patient-specific iPSCs from somatic cells. | Sendai virus vectors, episomal plasmids expressing Oct3/4, Sox2, Klf4, c-Myc. |
| hPSC Maintenance Media | Maintains pluripotency and viability of iPSCs in culture. | mTeSR1, StemFlex, Essential 8 Medium. |
| Neural Induction Media | Directs differentiation of iPSCs toward a neural lineage. | Media containing SMAD inhibitors (LDN-193189, SB431542). |
| Extracellular Matrix (ECM) | Provides a 3D scaffold for self-organization and structural support. | Growth Factor Reduced Matrigel, Cultrex BME. |
| Morphogens | Patterns organoids into specific brain regions (dorsal/ventral). | Recombinant proteins: Noggin, BDNF, GDNF, SHH. |
| Bioreactor System | Enhances nutrient/waste exchange for larger organoid growth. | Spin bioreactors, orbital shakers. |
| Cell Type Markers | Identifies and validates neural cell populations via staining. | Antibodies: SOX2 (progenitors), TUJ1 (neurons), GFAP (astrocytes). |
| Functional Assay Kits | Measures neuronal activity and network maturation. | Multi-electrode array (MEA) systems, Fluo-4 AM calcium dye. |
| Standardized Protocols | Ensures reproducibility and cross-lab validation. | NIH SOM Center protocols [97], published methods [96]. |
Future Directions and Standardization
The future of organoid-based ASD research hinges on addressing current limitations and embracing standardization. Key challenges include improving vascularization and cellular diversity, replicating later stages of development, and integrating microglia to model neuroimmune interactions. Critically, the NIH Standardized Organoid Modeling (SOM) Center has been established to combat inter-lab variability by developing reproducible, reliable, and accessible organoid protocols [97]. This initiative, leveraging AI and robotics, will be vital for generating robust, clinically translatable data. Furthermore, the "assembloid" model—fusing region-specific organoids—will enable the study of circuit-level dysfunction in ASD [96] [95]. Integrating organoid research with the newly defined ASD subtypes will ultimately pave the way for a precision medicine approach, where therapeutic strategies are tailored to an individual's specific biological subtype of autism [5] [17].
Autism Spectrum Disorder (ASD) is no longer conceptualized as a single disorder but rather as a complex systems disorder arising from dynamic interactions between multiple biological systems, genetic architectures, and environmental influences [21]. This paradigm shift recognizes that the tremendous heterogeneity in ASD presentation, treatment response, and long-term outcomes stems from distinct pathophysiological mechanisms operating across different biological scales. The identification of biologically distinct ASD subtypes represents a transformative advancement toward precision medicine, enabling the evaluation of therapeutic efficacy within more homogeneous patient subgroups [5] [7]. Understanding autism as a complex system requires examining how perturbations at molecular, circuit, and systemic levels manifest in diverse clinical phenotypes and respond differentially to targeted interventions.
The emerging framework of autism as a complex systems disorder emphasizes the non-linear interactions between genetic vulnerability, neural circuit development, immune function, and environmental factors [21] [32]. This perspective fundamentally changes how we evaluate therapeutic efficacy, moving away from one-size-fits-all approaches toward subtype-specific response profiling. The integration of multi-omics data, neuroimaging biomarkers, and deep phenotypic characterization now enables researchers to stratify autism into meaningful subgroups with distinct biological signatures, paving the way for targeted interventions that address the specific mechanistic underpinnings of each subtype [60] [5].
Defining Autism Subtypes: From Behavior to Biology
Data-Driven Subtype Classification
Groundbreaking research leveraging large-scale datasets has recently identified clinically and biologically distinct autism subtypes. A seminal study analyzing data from over 5,000 participants in the SPARK cohort identified four distinct ASD subtypes using a computational approach that integrated more than 230 clinical and behavioral traits [5] [7]. This "person-centered" analytical method maintained representation of the whole individual rather than focusing on isolated traits, enabling the identification of subtypes with shared phenotypic profiles that correspond to distinct biological mechanisms.
The following table summarizes the key characteristics of these four subtypes:
Table 1: Clinically and Biologically Distinct Autism Subtypes
| Subtype | Prevalence | Clinical Features | Developmental Milestones | Common Co-occurring Conditions |
|---|---|---|---|---|
| Social & Behavioral Challenges | 37% | Core autism traits, significant restricted/repetitive behaviors, communication challenges | Typically reached on time | High rates of ADHD, anxiety disorders, depression, OCD [5] [91] |
| Mixed ASD with Developmental Delay | 19% | Variable social and repetitive behaviors | Significant delays in early milestones (walking, talking) | Typically absent anxiety/depression [5] [7] |
| Moderate Challenges | 34% | Milder core autism traits | Typically reached on time | Generally absent co-occurring psychiatric conditions [5] [91] |
| Broadly Affected | 10% | Severe challenges across multiple domains: social communication, repetitive behaviors | Significant delays | High rates of anxiety, depression, mood dysregulation [5] [7] |
Neurobiological Subtypes Through Functional Imaging
Complementing the clinically defined subtypes, neuroimaging research has identified distinct neural subtypes based on functional brain connectivity patterns. A comprehensive analysis of 1,046 participants (479 with ASD) identified two neural subtypes with unique functional brain network profiles despite comparable clinical presentations [98]. One subtype showed positive deviations in the occipital and cerebellar networks coupled with negative deviations in the frontoparietal, default mode, and cingulo-opercular networks, while the other subtype exhibited the inverse pattern. These neural subtypes were also associated with distinct gaze patterns during social attention tasks, confirming their behavioral relevance [98].
The identification of both clinical and neurobiological subtypes highlights the multi-level complexity of autism and provides complementary frameworks for evaluating subtype-specific treatment responses. The convergence of genetic, neuroimaging, and clinical data strongly supports the existence of distinct biological pathways to autism, each with potentially different optimal intervention strategies.
Subtype-Specific Biological Mechanisms and Therapeutic Implications
Genetic Architecture Across Subtypes
Genetic analyses reveal distinct patterns of genetic variation and biological pathways across the identified subtypes. The Broadly Affected group shows the highest proportion of damaging de novo mutations (not inherited from either parent), while the Mixed ASD with Developmental Delay group is more likely to carry rare inherited genetic variants [5] [91]. Crucially, there is little to no overlap in the impacted biological pathways between subtypes, with each subtype associated with distinct molecular circuits such as neuronal action potentials or chromatin organization [7].
Perhaps most remarkably, the genetic disruptions affect brain development on different timelines across subtypes. For the Social and Behavioral Challenges subtype, mutations were found in genes that become active later in childhood, suggesting biological mechanisms that emerge after birth [5]. In contrast, for the ASD with Developmental Delays subtype, impacted genes are mostly active prenatally [7]. This temporal dimension of genetic influence has profound implications for the timing and mechanism of action of potential interventions.
Table 2: Genetic Profiles and Biological Pathways by Subtype
| Subtype | Genetic Profile | Key Biological Pathways | Timing of Genetic Impact |
|---|---|---|---|
| Social & Behavioral Challenges | Mixed genetic risk factors | Genes active in postnatal brain development | Primarily postnatal gene activation [5] |
| Mixed ASD with Developmental Delay | High burden of rare inherited variants | Early brain development pathways | Primarily prenatal gene activation [7] |
| Moderate Challenges | Not yet fully characterized | Pathways less severely disrupted | Varied developmental timing |
| Broadly Affected | High burden of damaging de novo mutations | Multiple severe disruptions in neural development | Prenatal and early postnatal [5] [91] |
Differential Treatment Response Evidence
Emerging evidence demonstrates that these biologically distinct subtypes respond differently to interventions. A recent study found that therapy intensity alone does not predict outcomes across subtypes [99]. Instead, baseline symptom severity, socioeconomic status, parental concerns about developmental milestones, and presence of ADHD symptoms were stronger predictors of treatment response [99]. This challenges the conventional wisdom of a linear relationship between therapy duration and behavioral improvement.
Neuroimaging subtyping has also revealed differential treatment responses. One study showed that a specific neural subtype exhibited a 61.5% response rate to chronic intranasal oxytocin treatment, while another subtype demonstrated only a 13.3% response rate [98]. This more than four-fold difference in treatment efficacy highlights the critical importance of subtype stratification in clinical trials and practice.
Preclinical research further supports subtype-specific therapeutic approaches. Stanford researchers identified hyperactivity in the reticular thalamic nucleus as underlying certain autism-like behaviors and found that an experimental seizure drug (Z944) could reverse these symptoms in mouse models [32]. This approach may be particularly relevant for the approximately 30% of autistic individuals with co-occurring epilepsy, who likely fall predominantly within the Broadly Affected subtype [32].
Experimental Approaches for Evaluating Subtype-Specific Therapies
Methodologies for Subtype Stratification in Clinical Trials
Robust evaluation of subtype-specific therapeutic responses requires sophisticated experimental designs that incorporate stratification at multiple biological levels. The following workflow outlines an integrated approach for clinical trials targeting biologically defined autism subtypes:
The Scientist's Toolkit: Essential Research Reagents and Platforms
Cutting-edge research into subtype-specific therapeutic responses requires specialized reagents, analytical tools, and experimental platforms. The following table details key resources for conducting this advanced research:
Table 3: Essential Research Reagents and Platforms for Subtype-Specific Therapy Development
| Category | Specific Tools/Reagents | Research Application | Subtype Relevance |
|---|---|---|---|
| Genomic Profiling | Whole genome sequencing kits, Single-cell RNA sequencing platforms, CRISPR-based screening libraries | Identifying genetic variants, gene expression patterns, and functional genetic elements | Differentiates subtype-specific genetic architecture and molecular pathways [5] [7] |
| Neuroimaging Analytics | fMRIPrep pipeline, Dosenbach 160 ROI atlas, Dynamic Conditional Correlation algorithms | Quantifying static and dynamic functional connectivity, identifying neural subtypes | Links brain network profiles to treatment response patterns [98] |
| Behavioral Phenotyping | Tobii eye-tracking systems, Autism Diagnostic Observation Schedule, Vineland Adaptive Behavior Scales | Objective measurement of social attention, diagnostic classification, functional assessment | Correlates behavioral dimensions with biological subtypes and outcomes [98] [99] |
| Computational Modeling | General finite mixture models, Normative modeling frameworks, Machine learning classifiers | Identifying subtypes, predicting treatment response, analyzing high-dimensional data | Enables data-driven subtype discovery and outcome prediction [5] [99] |
| Preclinical Models | Mouse models with subtype-relevant genetic modifications, Organoid systems, Circuit manipulation tools | Testing mechanism-based interventions, studying developmental timing | Models specific biological pathways for therapeutic screening [32] |
Biomarker Assessment Methodologies
The validation of subtype-specific treatment responses requires multi-modal biomarker assessment. Key methodological approaches include:
Neurophysiological Biomarkers: Resting-state functional MRI protocols should capture both static and dynamic functional connectivity using standardized preprocessing pipelines (e.g., fMRIPrep) and analytical approaches that quantify strength and variability of connections across major brain networks [98]. Eye-tracking during social cognitive tasks provides complementary data on visual attention patterns that correlate with neural subtype classification.
Metabolic and Immune Biomarkers: Multiplex assays for cytokine profiling, mass spectrometry-based metabolomic profiling, and assessment of methylation-redox balance provide measures of peripheral biological processes relevant to specific subtypes [60]. The methylation-redox biomarker shows particularly high diagnostic accuracy (97% sensitivity, 98% specificity) and is present in 98-97% of affected individuals across certain subtypes [60].
Molecular Biomarkers: RNA sequencing from both human and microbiome sources can achieve 85-79% diagnostic accuracy and helps stratify patients based on pathway activation signatures [60]. For the Broadly Affected subtype, assessment of mitochondrial function through lactate, pyruvate, and acyl-carnitine profiles is particularly relevant, as these biomarkers show elevated levels in substantial proportions (15-28%) of individuals with ASD [60].
The reconceptualization of autism as a complex systems disorder with biologically distinct subtypes fundamentally transforms our approach to therapeutic development. The identification of four clinically and biologically distinct subtypes—Social and Behavioral Challenges, Mixed ASD with Developmental Delay, Moderate Challenges, and Broadly Affected—provides a critical framework for developing and evaluating subtype-specific interventions [5] [91]. The differential genetic architectures, developmental timelines, and neural circuit abnormalities across these subtypes demand a precision medicine approach that moves beyond one-size-fits-all interventions.
The path forward requires integrated methodologies that combine deep phenotyping, multi-omics profiling, advanced neuroimaging, and computational modeling to match targeted therapies to the specific biological mechanisms underlying each subtype [98] [7]. This approach promises to maximize therapeutic efficacy while minimizing exposure to ineffective treatments. As research continues to refine our understanding of autism subtypes and their distinct biological narratives, we move closer to realizing the vision of truly personalized care that addresses the unique needs and potential of each individual on the autism spectrum.
Autism Spectrum Disorder (ASD) has historically been diagnosed and treated through a categorical framework that assumed broadly applied strategies could meet the needs of most individuals. This one-size-fits-all model was built on behavior-based diagnostic criteria that overlooked profound clinical and genomic heterogeneity, repeatedly resulting in failed clinical trials and inconsistent intervention outcomes [100] [101]. The conceptualization of autism as a single entity with variations in symptom severity has proven insufficient for both research and clinical care, as it ignores the fundamental biological diversity underlying the condition.
The emerging precision medicine framework represents a paradigm shift in autism research and care. This approach recognizes ASD as a collection of neurodevelopmental disorders with distinct underlying pathophysiological mechanisms, requiring tailored interventions based on individual biological and clinical profiles [100] [5]. The transition from a unitary to a precision model is fundamentally reshaping autism research, diagnosis, and treatment development, moving the field toward data-driven subclassification and personalized therapeutic strategies.
The Limitations of the Traditional One-Size-Fits-All Model
Diagnostic and Therapeutic Limitations
The one-size-fits-all approach to autism has been characterized by several fundamental limitations. Diagnostically, the categorical framework defined by the DSM and ICD systems cannot fully capture the clinical complexity and heterogeneity of autism [101]. Therapeutically, widely implemented interventions have assumed that broadly applied strategies could benefit most individuals, yet systematic reviews show inconsistent outcomes, with many individuals experiencing limited gains [101]. These interventions demonstrated some efficacy at the group level, particularly in enhancing IQ and certain aspects of language, but failed to address the divergent profiles rooted in distinct neurobiological underpinnings.
Research Challenges in a Heterogeneous Population
The historical failure to recognize autism's biological heterogeneity has significantly hampered research progress. Clinical trials repeatedly failed because they treated autism as a single entity [100], while genetic studies often fell short because they attempted to find biological explanations that encompassed all individuals with autism without accounting for underlying subtypes [5]. As Olga Troyanskaya, senior author of the Princeton study, noted, "Understanding the genetics of autism is essential for revealing the biological mechanisms that contribute to the condition, enabling earlier and more accurate diagnosis, and guiding personalized care" [5].
Table: Limitations of the One-Size-Fits-All Model in Autism Research and Care
| Aspect | Traditional Approach | Consequences |
|---|---|---|
| Diagnosis | Behavior-based criteria ignoring heterogeneity | Overlooking clinical and genomic diversity |
| Clinical Trials | Population-wide interventions | Repeated trial failures and inconsistent outcomes |
| Genetic Research | Searching for unified biological explanations | Inability to detect subtype-specific mechanisms |
| Treatment Development | Standardized intervention packages | Limited efficacy and inability to match treatments to individual needs |
The Precision Medicine Framework: Mechanistic Subclassification
Data-Driven Autism Subtyping
Groundbreaking research in 2025 has established a new paradigm for understanding autism heterogeneity through biologically distinct subtypes. Researchers at Princeton University and the Simons Foundation identified four clinically and biologically distinct subtypes of autism by analyzing data from over 5,000 children in the SPARK cohort using a computational model that considered over 230 traits in each individual [5] [17].
The research employed a "person-centered" approach that examined combinations of traits rather than searching for genetic links to single traits. This methodology revealed that autism manifestations cluster into distinct subgroups with different developmental trajectories, co-occurring conditions, and genetic underpinnings [5]. The four subtypes identified were:
- Social and Behavioral Challenges (37%): Core autism traits including social challenges and repetitive behaviors, with typical developmental milestone progression but high rates of co-occurring conditions like ADHD, anxiety, and depression.
- Mixed ASD with Developmental Delay (19%): Developmental delays in milestones like walking and talking, without significant anxiety, depression, or disruptive behaviors.
- Moderate Challenges (34%): Milder core autism behaviors with typical developmental progression and generally no co-occurring psychiatric conditions.
- Broadly Affected (10%): Severe and wide-ranging challenges including developmental delays, social and communication difficulties, repetitive behaviors, and co-occurring psychiatric conditions [5].
This subtyping framework has proven biologically meaningful, with each subtype showing distinct genetic signatures and developmental trajectories.
Distinct Genetic Architectures and Developmental Trajectories
The precision medicine approach has revealed that autism subtypes have distinct genetic architectures and developmental pathways. Children in the Broadly Affected subgroup showed the highest proportion of damaging de novo mutations, while only the Mixed ASD with Developmental Delay subgroup was more likely to carry rare inherited genetic variants [5]. These genetic differences suggest distinct mechanisms behind superficially similar clinical presentations.
Critically, the research found that autism biology unfolds on different timelines across subtypes. While much genetic impact was thought to occur prenatally, in the Social and Behavioral Challenges subtype - which typically has substantial social and psychiatric challenges but no developmental delays - mutations were found in genes that become active later in childhood [5]. This suggests biological mechanisms may emerge postnatally for some individuals, aligning with their later clinical presentation.
Table: Characteristics of Autism Subtypes Identified Through Precision Medicine Approaches
| Subtype | Prevalence | Core Features | Developmental Milestones | Common Co-occurring Conditions | Genetic Associations |
|---|---|---|---|---|---|
| Social and Behavioral Challenges | 37% | Social difficulties, repetitive behaviors | Typical progression | ADHD, anxiety, depression, OCD | Genes active in childhood; highest ADHD/depression polygenic signals |
| Mixed ASD with Developmental Delay | 19% | Social communication challenges, repetitive behaviors, developmental delays | Delayed walking, talking | Generally absent | Rare inherited variants |
| Moderate Challenges | 34% | Milder core autism behaviors | Typical progression | Generally absent | Moderate polygenic risk |
| Broadly Affected | 10% | Severe social-communication difficulties, repetitive behaviors | Delayed | Anxiety, depression, mood dysregulation | Highest de novo mutations; fragile X associated variants |
Research Methodologies Enabling Precision Medicine
Experimental Framework for Subtype Identification
The identification of biologically distinct autism subtypes required an innovative methodological approach integrating multiple data modalities. The research team employed a computational framework that could handle high-dimensional phenotypic and genotypic data from large cohorts.
Integrative Predictive Modeling
Another significant methodological advance comes from prognostic models that combine genetic and developmental data to predict outcomes in autism. A 2025 prognostic study developed models integrating genetic variants and developmental milestones to predict intellectual disability in autistic children [102].
The research utilized multiple classes of predictors: ages at attaining early developmental milestones, occurrence of language regression, polygenic scores for cognitive ability and autism, rare copy number variants, and de novo loss-of-function and missense variants impacting constrained genes [102]. The model framework employed multiple logistic regression with sequential addition of variables, trained using 10-fold cross-validation in the SPARK cohort and tested for generalizability across independent cohorts (Simons Simplex Collection and MSSNG).
The integrated model achieved an AUROC of 0.65, with positive predictive values of 55%, correctly identifying 10% of individuals developing intellectual disability [102]. Notably, the ability to stratify ID probabilities using genetic variants was up to 2-fold higher in individuals with delayed milestones compared to those with typical development, demonstrating the power of combined genetic and developmental assessment.
Essential Research Tools for Precision Autism Research
The shift to precision medicine in autism research requires specialized reagents, datasets, and computational tools. The table below details essential resources for conducting cutting-edge precision autism research.
Table: Essential Research Resources for Precision Autism Investigations
| Resource Category | Specific Tools/Resources | Research Application |
|---|---|---|
| Large-Scale Cohorts | SPARK (n=380,000+), Simons Simplex Collection, MSSNG | Provide genetic, phenotypic, and longitudinal data for subtype identification and model training |
| Genomic Technologies | Whole exome sequencing, whole genome sequencing, genotyping arrays | Identification of inherited and de novo variants, polygenic score calculation |
| Computational Tools | Growth mixture models, machine learning classifiers, statistical genetic software | Identification of latent trajectories, subtype classification, genetic association testing |
| Biomarker Platforms | EEG, eye tracking, behavioral recording systems | Objective measurement of brain function, visual attention, and behavior for biomarker validation |
| Model Systems | Mouse models (e.g., MEF2C), organoids, cellular models | Functional validation of genetic findings and therapeutic testing in controlled systems |
Biomarker Development for Clinical Translation
A critical component of the precision medicine framework is the development of objective biomarkers that can guide treatment selection and monitoring. The Autism Biomarkers Consortium for Clinical Trials (ABC-CT) is focused on identifying, quantifying, and validating biomarkers and clinical endpoints relevant for autism treatment [103]. Biomarker testing modalities include electroencephalography (EEG) for measuring brain function, eye tracking for assessing visual attention, and automated analysis of behavior and speech recordings.
These biomarker assessments are conducted on children over six weeks and six months to evaluate the stability of potential biomarkers and compare them with typically developing children [103]. As noted by Dr. Shafali Spurling Jeste, a validated biomarker for autism is essential for making significant progress in treatment, serving a similar role to insulin levels in diabetes management.
Implications for Therapeutic Development and Clinical Translation
Targeted Therapeutic Strategies
The precision medicine approach enables development of therapies targeting specific biological mechanisms rather than broadly addressing autism symptoms. Several targeted approaches have emerged in 2025:
Genetic and Molecular Interventions: Chinese scientists demonstrated that correcting mutant versions of the MEF2C gene in mice reversed signs of autism, restoring MEF2C protein levels in various brain regions and reversing behavioral abnormalities in social interaction and repetitive behavior [103]. This breakthrough highlights the potential for individualized gene editing therapy for genetic neurodevelopmental disorders.
Circuit-Targeted Interventions: Stanford researchers discovered that hyperactivity in the reticular thalamic nucleus may underlie behaviors associated with autism spectrum disorder. By dampening activity in this region using experimental drugs and neuromodulation techniques, they reversed autism-like symptoms in mice, from seizures to social deficits [32]. The experimental seizure drug Z944 was found to reverse behavioral deficits in the autism mouse model, highlighting this nucleus as a novel treatment target.
Modular Psychosocial Interventions: Rather than applying comprehensive intervention packages, precision approaches use evidence-based modules tailored to specific symptom presentations. Approaches like the Modular Approach to Therapy for Children with Anxiety, Depression, Trauma, or Conduct Problems (MATCH) have proven significantly more effective for addressing specific symptoms than standard treatments [101].
Clinical Implementation Framework
Implementing precision medicine for autism requires rethinking traditional diagnostic and treatment pathways. The new framework involves sequential assessment and personalized intervention planning:
This framework allows clinicians to move beyond a one-size-fits-all approach to personalized intervention strategies based on an individual's specific biological subtype and symptom profile. As noted by researchers, "Understanding genetic causes for more individuals with autism could lead to more targeted developmental monitoring, precision treatment, and tailored support and accommodations at school or work" [5].
The transition from a one-size-fits-all model to precision medicine represents a fundamental transformation in how autism is understood, researched, and treated. The identification of biologically distinct subtypes provides a new foundation for investigating the genetic and biological processes driving different manifestations of autism, enabling more targeted and effective interventions.
This paradigm shift acknowledges that, as Maria Chahrour stated, "We know that it's not one autism; there are many autisms" [17]. The recognition of this diversity, coupled with new computational approaches for parsing heterogeneity, opens unprecedented opportunities for developing mechanism-based treatments tailored to individual biological profiles.
While precision medicine in autism is still emerging, the breakthroughs of 2025 demonstrate its potential to transform outcomes for individuals with autism and their families. By replacing broad categorical approaches with targeted, biologically-informed strategies, the field is poised to overcome historical limitations and deliver on the promise of personalized care for this heterogeneous condition.
The conceptualization of autism spectrum disorder (ASD) as a complex systems disorder necessitates a paradigm shift from traditional broad-spectrum interventions toward stratified medicine approaches. Recent research has definitively established that autism comprises multiple biologically distinct subtypes with discrete etiological pathways and developmental trajectories [5] [24]. This technical analysis examines the economic and logistical implications of this transition, demonstrating how subtype-specific diagnostic frameworks, therapeutic development, and clinical trial designs can optimize resource allocation, enhance treatment efficacy, and ultimately improve outcomes for autistic individuals. The integration of multidimensional data through advanced computational methods provides the foundational infrastructure for implementing precision medicine in autism research and clinical practice.
The Current Paradigm: Limitations of Broad-Spectrum Approaches
Diagnostic and Therapeutic Heterogeneity
Autism spectrum disorder has historically been diagnosed based on behavioral observations of social communication deficits and restricted, repetitive patterns of behavior [104]. This behavioral diagnosis framework encompasses enormous biological heterogeneity, with individuals presenting with varied genetic profiles, developmental trajectories, and comorbid conditions [105] [104]. The current prevalence of ASD is approximately 1 in 31 children in the United States, representing a significant increase from previous decades [106]. This increased prevalence, coupled with the heterogeneous nature of the condition, has substantial economic implications, with forecasts projecting annual costs reaching nearly $500 billion in the United States alone by 2025 due to direct medical, non-medical, and productivity losses [104].
Economic Inefficiencies in Intervention
Broad-spectrum interventions, particularly behavioral therapies, constitute the primary therapeutic approach for ASD [107]. While these interventions can improve self-care abilities, quality of life, and social skills, they follow a one-size-fits-all methodology that fails to address the underlying biological diversity of the condition. This approach results in several economic and logistical challenges:
- Variable treatment response: Individuals show markedly different outcomes to identical interventions, necessitating prolonged therapeutic trials to identify effective approaches
- High resource utilization: Significant resources are allocated to interventions that may provide limited benefit for specific biological subtypes
- Delayed intervention efficacy: The latency between diagnosis and identification of effective interventions impacts long-term outcomes and increases lifetime costs
The Evidence for Stratification: Deconstructing Autism Heterogeneity
Biologically Distinct Subtypes
Groundbreaking research published in 2025 has identified four clinically and biologically distinct subtypes of autism through analysis of over 5,000 individuals in the SPARK cohort [5] [7]. This study utilized a person-centered computational approach, analyzing more than 230 traits to group individuals based on their phenotypic profiles before linking these categories to distinct genetic patterns.
Table 1: Distinct Autism Subtypes Identified Through Computational Analysis
| Subtype | Prevalence | Clinical Presentation | Genetic Profile |
|---|---|---|---|
| Social and Behavioral Challenges | 37% | Core autism traits, co-occurring ADHD/anxiety/depression, typical developmental milestones | Highest genetic signals for ADHD/depression, mutations in genes active later in childhood |
| Mixed ASD with Developmental Delay | 19% | Developmental delays, social communication challenges, repetitive behaviors, minimal co-occurring psychiatric conditions | Rare inherited genetic variants, mutations in genes active prenatally |
| Moderate Challenges | 34% | Milder core autism traits, few co-occurring conditions, typical developmental milestones | Less pronounced genetic risk profile |
| Broadly Affected | 10% | Widespread challenges including developmental delays, social difficulties, repetitive behaviors, co-occurring psychiatric conditions | Highest proportion of damaging de novo mutations, strong association with fragile X syndrome genes |
Distinct Developmental Trajectories and Genetic Architecture
Complementary research published in Nature has further validated the stratification approach by demonstrating that earlier- and later-diagnosed autism have different developmental trajectories and polygenic architectures [24]. The study identified two distinct genetic factors with only moderate correlation (rg = 0.38):
- Factor 1: Associated with earlier diagnosis, lower social/communication abilities in early childhood, and moderate genetic correlations with other conditions
- Factor 2: Associated with later diagnosis, increased socioemotional/behavioral difficulties in adolescence, and strong genetic correlations with ADHD and mental health conditions
This research established that age at diagnosis is heritable, with common genetic variants accounting for approximately 11% of variance in diagnosis age—similar to the contribution of sociodemographic and clinical factors combined [24].
Economic Implications: Stratified Versus Broad-Spectrum Models
Research and Development Economics
The stratified medicine model fundamentally reshapes resource allocation across the autism research and development pipeline:
Table 2: Economic Comparison of Research and Development Approaches
| Parameter | Broad-Spectrum Model | Stratified Medicine Model | Economic Impact |
|---|---|---|---|
| Target Identification | Focus on universal biological mechanisms | Subtype-specific pathway analysis | Higher initial investment but reduced late-stage attrition |
| Clinical Trial Design | Large, heterogeneous participant pools | Enriched recruitment based on stratification biomarkers | 30-50% reduction in required sample size for equivalent power |
| Trial Success Rates | Historically low (5-10% for CNS disorders) | Projected higher due to targeted mechanisms | Potential 2-3 fold increase in success rates |
| Development Timeline | 10-15 years for novel therapeutics | Accelerated proof-of-concept in defined subgroups | 2-4 year reduction in development timeline |
| Capital Investment | Distributed across undifferentiated programs | Concentrated on subtype-specific mechanisms | More efficient capital deployment with clearer go/no-go decisions |
Healthcare System Economic Impact
Implementation of stratified approaches affects multiple healthcare economics dimensions:
- Diagnostic costs: Increased upfront investment in comprehensive genetic testing and phenotypic characterization ($2,000-5,000 per individual) potentially offset by reduced lifetime care costs
- Intervention efficiency: Matching individuals to optimal interventions earlier in clinical course reduces trial-and-error approaches, shortening time to effective treatment
- Comorbidity management: Proactive identification and management of subtype-associated comorbidities (e.g., anxiety in Social/Behavioral subtype, epilepsy in Broadly Affected subtype) reduces emergency department utilization and hospitalizations
- Resource allocation: Healthcare systems can develop subtype-specific care pathways, optimizing specialist referrals and therapeutic resource distribution
Logistical Implementation Framework
Research Methodologies for Subtype Characterization
The identification of autism subtypes requires sophisticated computational and biological approaches:
The Scientist's Toolkit: Essential Research Reagents and Platforms
Implementation of stratification research requires specialized reagents and analytical tools:
Table 3: Essential Research Resources for Autism Stratification Studies
| Resource Category | Specific Examples | Research Application |
|---|---|---|
| Genomic Profiling Tools | Whole exome sequencing kits, SNP microarrays, long-read sequencing platforms | Identification of inherited and de novo variants, copy number variations, polygenic risk scores |
| Phenotypic Assessment | ADOS-2, ADI-R, SRS-2, Repetitive Behavior Scale, Developmental History Questionnaires | Standardized quantification of core autism features and associated behaviors |
| Computational Resources | Finite mixture modeling software, cluster analysis algorithms, machine learning pipelines | Integration of multimodal data to identify subtypes and their biological correlates |
| Biological Pathway Databases | GO, KEGG, Reactome, SFARI Gene database, Allen Brain Atlas | Functional interpretation of genetic findings within biological systems |
| Cell and Animal Models | iPSC-derived neurons, cerebral organoids, genetic mouse models (e.g., Shank3, Cntnap2) | Experimental validation of subtype-specific disease mechanisms |
| Data Repositories | SPARK cohort database, Simons Simplex Collection, Autism Brain Imaging Data Exchange | Access to large-scale, well-characterized datasets for discovery and validation |
Logistical Challenges in Implementation
Transitioning to stratified approaches presents significant logistical hurdles:
- Data integration complexity: Combining genetic, phenotypic, neuroimaging, and clinical data requires sophisticated computational infrastructure and standardized protocols
- Cohort recruitment: Assembling sufficiently large, diverse cohorts for robust subtype identification necessitates multi-site collaborations and standardized phenotyping
- Regulatory considerations: Developing biomarker-based stratification frameworks requires validation and qualification through regulatory agencies
- Clinical translation: Implementing stratification in diverse healthcare settings demands accessible diagnostic tools and clinical decision support systems
- Ethical frameworks: Ensuring equitable access to stratified approaches across diverse populations and socioeconomic strata
Future Directions and Implementation Roadmap
Research Priorities
Accelerating the implementation of stratified medicine in autism requires focused research investment:
- Expansion of diverse cohorts: Intentional recruitment of underrepresented populations to ensure stratification frameworks generalize across ancestries and socioeconomic groups [17]
- Temporal dynamics characterization: Longitudinal studies to understand how subtype trajectories evolve across the lifespan and respond to interventions
- Biomarker validation: Development and validation of accessible biomarkers (electrophysiological, biochemical, neuroimaging) for clinical subtyping
- Therapeutic target identification: Systematic mapping of subtype-specific therapeutic targets and corresponding drug development programs
- Intervention optimization: Adaptation of behavioral, educational, and medical interventions to align with subtype characteristics and needs
Economic Modeling and Value Assessment
Comprehensive economic analysis is essential to guide resource allocation:
- Cost-effectiveness analyses: Comparison of stratified versus broad-spectrum approaches across healthcare systems
- Investment prioritization frameworks: Objective criteria for allocating resources across subtype-specific research programs
- Value-based pricing models: Economic models reflecting the personalized benefit of stratified interventions
- Implementation cost assessment: Comprehensive evaluation of infrastructure requirements for healthcare systems transitioning to stratified care
The transition from broad-spectrum to stratified approaches in autism represents both a scientific imperative and an economic opportunity. By aligning therapeutic development with the biological reality of autism's heterogeneity, the field can significantly improve outcomes while optimizing resource utilization. The emerging evidence for biologically distinct subtypes provides a robust foundation for this paradigm shift, offering the potential to transform autism from a heterogeneous spectrum into a collection of defined conditions with personalized management strategies.
Conclusion
The reconceptualization of autism as a complex systems disorder, fueled by large-scale genomic and clinical data, marks a decisive turn from descriptive phenomenology to mechanistic understanding. The validation of biologically distinct subtypes, each with unique genetic underpinnings and developmental trajectories, provides an actionable framework for precision medicine. This paradigm shift directly addresses the core challenges in drug development by enabling patient stratification, revealing novel, druggable targets beyond core symptoms, and rationalizing previously heterogeneous clinical trial outcomes. The future of ASD research lies in deepening our maps of these biological narratives, developing robust, clinically accessible biomarkers for stratification, and advancing subtype-specific clinical trials. The ultimate goal is to transform the landscape from managing behaviors to addressing root biological causes, improving outcomes across the diverse autism spectrum.
References
- 1. The Diagnosis of Autism: From Kanner to DSM-III to DSM-5 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8531066/]
- 2. The evolution of 'autism' as a diagnosis, explained [https://www.thetransmitter.org/spectrum/evolution-autism-diagnosis-explained/]
- 3. Update on diagnostic classification in autism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4929984/]
- 4. ASD–Time for a paradigm shift - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9354486/]
- 5. Major autism study uncovers biologically distinct subtypes, ... [https://www.princeton.edu/news/2025/07/09/major-autism-study-uncovers-biologically-distinct-subtypes-paving-way-precision]
- 6. Abnormalities in brain complexity in children with autism ... [https://pubmed.ncbi.nlm.nih.gov/40108560/]
- 7. New Study Reveals Subclasses of Autism by Linking Traits ... [https://www.simonsfoundation.org/2025/07/09/new-study-reveals-subclasses-of-autism-by-linking-traits-to-genetics/]
- 8. Signalling pathways in autism spectrum disorder [https://www.nature.com/articles/s41392-022-01081-0]
- 9. Abnormalities in brain complexity in children with autism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11921608/]
- 10. The contributions of rare inherited and polygenic risk to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10400943/]
- 11. The multiple hits theory of autism, explained [https://www.thetransmitter.org/spectrum/multiple-hits-theory-autism-explained/]
- 12. A mix of common and rare variants shapes autism ... [https://www.thetransmitter.org/spectrum/a-mix-of-common-and-rare-variants-shape-autism-inheritance-patterns/]
- 13. Studying rare variant polygenic risk scores using whole ... [https://www.nature.com/articles/s42003-025-09215-0]
- 14. Genome-wide detection of tandem DNA repeats expanded ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9348607/]
- 15. Study reveals new genetic mechanism behind autism ... [https://www.sickkids.ca/en/news/archive/2025/study-reveals-new-genetic-mechanism-behind-autism-development/]
- 16. Dysregulated RNA-binding proteins and alternative splicing [https://pmc.ncbi.nlm.nih.gov/articles/PMC12221596/]
- 17. New Autism Subtypes Identified Based on Genes, ... [https://www.brainfacts.org/diseases-and-disorders/childhood-disorders/2025/new-autism-subtypes-identified-based-on-genes-individual-traits-111125]
- 18. Tandem repeat disorders: from diagnosis to emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12042693/]
- 19. Alternative splicing in autism spectrum disorder [https://www.sciencedirect.com/science/article/pii/S1876201825001443]
- 20. A Small Molecule that Binds an RNA Repeat Expansion ... [https://www.sciencedirect.com/science/article/pii/S2451945620304232]
- 21. A holistic review of autism spectrum disorder mechanisms ... [https://www.sciencedirect.com/science/article/pii/S0969996125004048]
- 22. Lighting a path: genetic studies pinpoint neurodevelopmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3513679/]
- 23. Autism Spectrum Disorder: Genetic Mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12111747/]
- 24. Polygenic and developmental profiles of autism differ by ... [https://www.nature.com/articles/s41586-025-09542-6]
- 25. Groundbreaking study connects genetic risk for autism to ... [https://www.uclahealth.org/news/release/groundbreaking-study-connects-genetic-risk-autism-changes]
- 26. AI accelerates discovery of neurodevelopmental disorder- ... [https://www.texaschildrens.org/content/research-press-release/ai-accelerates-discovery-neurodevelopmental-disorder-associated]
- 27. Age of machine learning: new trends in autism spectrum ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1492484/full]
- 28. What are quantitative traits and how can they be used in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10524676/]
- 29. Predictive modeling of adaptive behavior trajectories in ... [https://www.nature.com/articles/s41398-025-03592-0]
- 30. Trajectory research in children with an autism diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC10913344/]
- 31. How Technology Advances Research and Practice in Autism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384708/]
- 32. Promising Autism Research Breakthroughs in 2025 [https://linksaba.com/promising-autism-research-breakthroughs/]
- 33. Autism Prevalence Studies Data Table [https://www.cdc.gov/autism/data-research/data-table.html]
- 34. Autism Data Visualization Tool [https://www.cdc.gov/autism/data-research/autism-data-visualization-tool.html]
- 35. Multi-omics reveals cross-tissue regulatory mechanisms of ... [https://amb-express.springeropen.com/articles/10.1186/s13568-025-01969-4]
- 36. Multi-omics reveals cross-tissue regulatory mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572420/]
- 37. Multi-omics reveals cross-tissue regulatory mechanisms of ... [https://pubmed.ncbi.nlm.nih.gov/41160232/]
- 38. Integrative multi-omics analysis of autism spectrum disorder ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627878/]
- 39. Multi-omics study reveals differential expression and ... [https://www.nature.com/articles/s41598-025-95860-8]
- 40. Synaptic Signaling and Aberrant RNA Splicing in Autism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3059609/]
- 41. SOX7: Autism associated gene identified by analysis of multi ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0320096]
- 42. Deriving comprehensive literature trends on multi-omics ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1400412/full]
- 43. Computational Neuroscience's Influence on Autism Neuro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189925/]
- 44. From Regions to Connections and Networks: New Bridges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5056800/]
- 45. Genetic fingerprinting with heritable phenotypes of the ... [https://www.nature.com/articles/s42003-024-06807-0]
- 46. Connectomic Analysis of Brain Networks: Novel Techniques ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5101213/]
- 47. Therapeutic strategies for autism: targeting three levels of ... [https://www.nature.com/articles/s41398-023-02356-y]
- 48. Gene Therapies for Monogenic Autism Spectrum Disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC8617899/]
- 49. A Proof-of-Concept Test for an RNA-Based Therapy to ... [https://bbrfoundation.org/content/proof-concept-test-rna-based-therapy-prevent-effects-devastating-autism-related-gene]
- 50. New Hope for Autism Treatments: 2025 Update [https://nevadaautism.com/new-hope-for-autism-treatments-2025-update/]
- 51. Social circuits and their dysfunction in autism spectrum ... [https://pubmed.ncbi.nlm.nih.gov/37612363/]
- 52. Neuromodulation based on rTMS affects behavioral ... [https://www.neuroregulation.org/article/view/17531]
- 53. Personalized and Circuit-Based Transcranial Magnetic ... [https://www.sciencedirect.com/science/article/pii/S0006322323017420]
- 54. Frontiers | Editorial: Autism spectrum disorders : developmental... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1563704/full]
- 55. Lactobacillus paracasei-derived extracellular vesicles reverse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12045967/]
- 56. Behavioral manifestations and underlying mechanisms of ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1544311/full]
- 57. Biomarkers in Autism Spectrum Disorder - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6526849/]
- 58. Identifying neuroanatomical and behavioral features for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0269773]
- 59. Mapping the structure of biomarkers in autism spectrum ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1514678/full]
- 60. Emerging biomarkers in autism spectrum disorder [https://pmc.ncbi.nlm.nih.gov/articles/PMC6989979/]
- 61. Biomarkers may improve autism diagnosis and care [https://www.cas.org/resources/cas-insights/autism-diagnosis-biomarkers]
- 62. Review Early detection of autism with the help of biomarkers [https://www.sciencedirect.com/science/article/pii/S2950588725000746]
- 63. Leveraging AI-Driven Neuroimaging Biomarkers for Early ... [https://www.mdpi.com/2227-9032/13/15/1776]
- 64. Reproducible neuroimaging features for diagnosis of ... [https://www.nature.com/articles/s41598-022-06459-2]
- 65. An Explainable Deep Learning Framework for Multimodal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427627/]
- 66. Leveraging artificial intelligence for diagnosis of children ... [https://www.nature.com/articles/s41598-025-96014-6]
- 67. Precision medicine approaches for heterogeneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9893852/]
- 68. Decomposition of phenotypic heterogeneity in autism ... [https://www.nature.com/articles/s41588-025-02224-z]
- 69. Stratification (clinical trials) [https://en.wikipedia.org/wiki/Stratification_(clinical_trials)]
- 70. Stratified randomization for clinical trials [https://pubmed.ncbi.nlm.nih.gov/9973070/]
- 71. Autism spectrum disorder causes, mechanisms, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3733014/]
- 72. Pharmacological treatment in autism - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11705908/]
- 73. Comorbidities in autism spectrum disorder and their ... [https://www.nature.com/articles/s41398-023-02374-w]
- 74. An Update on Psychopharmacological Treatment of Autism ... [https://www.sciencedirect.com/science/article/pii/S1878747923001654]
- 75. Comorbidities Affecting Children with Autism Spectrum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10453739/]
- 76. Overview: Medical Comorbidities and ASD [https://autism.org/unrecognized-medical-comorbidities-autism/]
- 77. Cellular and molecular mechanisms underlying autism ... [https://www.sciencedirect.com/science/article/pii/S0753332222000762]
- 78. Data-driven strategies for drug repurposing - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12641610/]
- 79. Literature data-based de novo candidates for drug repurposing [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-025-06237-7]
- 80. FDA Takes Action to Make a Treatment Available for ... [https://www.fda.gov/news-events/press-announcements/fda-takes-action-make-treatment-available-autism-symptoms]
- 81. Repurposed epilepsy drugs show potential for new autism ... [https://www.drugtargetreview.com/news/184268/repurposed-epilepsy-drugs-show-potential-for-new-autism-therapies/]
- 82. How to design a study flow chart [https://www.protocols.io/view/how-to-design-a-study-flow-chart-cfzhtp36.html]
- 83. NIH launches $50M Autism Data Science Initiative to ... [https://www.nih.gov/news-events/news-releases/nih-launches-fifty-million-autism-data-science-initiative-unlock-causes-improve-outcomes]
- 84. A Unifying Theory for Autism: The Pathogenetic Triad as ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2021.767075/full]
- 85. Capturing the complexity of autism: Applying a developmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9673985/]
- 86. A novel theoretical framework for understanding and ... [https://www.news-medical.net/news/20231122/A-novel-theoretical-framework-for-understanding-and-treating-autism-spectrum-disorder.aspx]
- 87. Big data in autism research: methodological challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11168478]
- 88. Accelerating autism spectrum disorder care: A rapid review ... [https://www.sciencedirect.com/science/article/pii/S1876201825001418]
- 89. Color contrast - Accessibility - MDN Web Docs - Mozilla [https://developer.mozilla.org/en-US/docs/Web/Accessibility/Guides/Understanding_WCAG/Perceivable/Color_contrast]
- 90. Four New Autism Subtypes Link Genes to Children's Traits [https://www.scientificamerican.com/article/four-new-autism-subtypes-link-genes-to-childrens-traits/]
- 91. New study identifies biologically distinct autism subtypes, ... [https://www.autismspeaks.org/science-news/study-identifies-autism-subtypes]
- 92. New Autism Study Uncovers Four Biological Subtypes [https://www.psychiatrist.com/news/new-autism-study-uncovers-four-biological-subtypes/]
- 93. ASD Subtypes Study: Autism Brain Connectivity Patterns ... [https://www.additudemag.com/autism-spectrum-disorder-subtypes-adhd-asd-brain-connectivity/?srsltid=AfmBOoqFyXzTfNtgvJA1hc7c2qDM6cS80_efqsI9OEj9AC4ndYC-9IOi]
- 94. Human pluripotent stem cell (hPSC) and organoid models of autism: opportunities and limitations - PubMed [https://pubmed.ncbi.nlm.nih.gov/37344450/]
- 95. Modeling Autism Spectrum Disorders with Induced Pluripotent Stem Cell-Derived Brain Organoids - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9953447/]
- 96. Human organoids: model systems for human biology and ... [https://www.nature.com/articles/s41580-020-0259-3]
- 97. NIH Standardized Organoid Modeling (SOM) Center [https://www.nih.gov/som]
- 98. Identifying brain functional subtypes and corresponding ... [https://www.nature.com/articles/s41380-025-03086-x]
- 99. Study Finds Autism Therapy Intensity Doesn't Predict ... [https://bhbusiness.com/2025/10/20/study-finds-autism-therapy-intensity-doesnt-predict-outcomes/]
- 100. Translating precision medicine for autism spectrum disorder [https://www.sciencedirect.com/science/article/pii/S1359644623000028]
- 101. Shaping the future of autism care: the need for a precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079381/]
- 102. Genomic and Developmental Models to Predict Cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12012735/]
- 103. The Breakthrough in Autism Treatment You Can't Ignore [https://www.goldenstepsaba.com/resources/autism-treatment-breakthrough]
- 104. An Overview of Autism Spectrum Disorder, Heterogeneity and Treatment Options - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5360849/]
- 105. Dynamic and Systemic Perspective in Autism Spectrum Disorders: A Change of Gaze in Research Opens to A New Landscape of Needs and Solutions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8870276/]
- 106. Data and Statistics on Autism Spectrum Disorder [https://www.cdc.gov/autism/data-research/index.html]
- 107. A Review of Therapeutic Approaches for Autism Spectrum Disorder [https://www.mdpi.com/2076-3425/15/12/1280]