Assessing Predictive Models of Patient Outcomes: From Machine Learning to Clinical Impact
This article provides a comprehensive framework for researchers and drug development professionals to develop, evaluate, and implement predictive models for patient outcomes.
Assessing Predictive Models of Patient Outcomes: From Machine Learning to Clinical Impact
Abstract
This article provides a comprehensive framework for researchers and drug development professionals to develop, evaluate, and implement predictive models for patient outcomes. It explores the foundational principles of predictive modeling, examines cutting-edge methodologies from machine learning to large language models, and addresses critical challenges in data quality, generalizability, and ethical implementation. A strong emphasis is placed on rigorous validation, comparative performance analysis, and the pathway to demonstrating tangible clinical impact, synthesizing recent advancements to guide evidence-based model integration into biomedical research and clinical practice.
The Foundation of Predictive Healthcare: Principles, Promise, and Core Metrics
The healthcare landscape is undergoing a fundamental transformation, moving from a traditional reactive model—treating symptoms of established disease—to a proactive paradigm focused on prevention, early intervention, and personalization [1] [2]. This shift is propelled by molecular insights into disease pathophysiology and enabled by technological advancements in data science and artificial intelligence (AI) [1]. Within this broader transition, the development and assessment of predictive models for patient outcomes have become a cornerstone of modern clinical research and drug development. This guide objectively compares the performance and methodologies of key modeling approaches that underpin proactive and personalized care, providing researchers and scientists with a framework for evaluation.
Comparative Analysis of Predictive Modeling Paradigms
The efficacy of a predictive model is contingent on its design, the data it utilizes, and its intended clinical application. The table below summarizes the experimental performance and key characteristics of three dominant modeling paradigms discussed in recent literature.
Table 1: Performance and Characteristics of Patient Outcome Predictive Models
| Model Paradigm | Primary Study / Application | Key Performance Metric (AUC) | Dataset & Sample Size | Core Advantage | Primary Limitation |
|---|---|---|---|---|---|
| Global (Population) Model | Diabetes Onset Prediction [3] | 0.745 (Baseline Reference) | 15,038 patients from medical claims data | Captures broad population-level risk factors; simpler to implement. | "One size fits all" may miss individual-specific risk factors [3]. |
| Personalized (KNN-based) Model | Diabetes Onset Prediction [3] | Up to ~0.76 (with LSML metric) | 15,038 patients; models built per patient from similar cohort | Dynamically customized for individual patients; can identify patient-specific risk profiles [3]. | Performance depends on quality of similarity metric and cohort size [3]. |
| Deep Learning (Sequential Data) Model | Systematic Review of Outcome Prediction [4] | Positive correlation with sample size (P=.02) | 84 studies; sample sizes varied widely | Captures temporal dynamics and hierarchical relationships in EHR data; end-to-end learning [4]. | High risk of bias (70% of studies); often lacks generalizability and explainability [4]. |
| Unified Time-Series Framework | Pneumonia Outcome Forecasting [5] | Effective & Robust (Specific metrics N/A) | CAP-AI dataset from University Hospitals of Leicester | Leverages sequential clinical data of varying lengths; models imbalanced and skewed outcome distributions. | Requires sophisticated handling of irregular time-series and admission data integration. |
| Equity-Aware AI Model (BE-FAIR) | Population Health Management [6] | Calibrated to reduce underprediction for minority groups | UC Davis Health patient population | Framework embeds equity assessment to mitigate health disparities in prediction [6]. | Requires custom development and systematic evaluation specific to a health system's population. |
Detailed Experimental Protocols
Protocol 1: Personalized Predictive Modeling for Diabetes Onset
This protocol is derived from the study employing Locally Supervised Metric Learning (LSML) to build personalized logistic regression models [3].
- Cohort Construction: Assemble a longitudinal dataset from Electronic Health Records (EHR) or medical claims. Identify incident cases (e.g., patients with a new diabetes diagnosis in the latter half of the observation window) and match them with controls based on demographics (age, gender) [3].
- Feature Engineering: Define an observation window (e.g., first 24 months). Aggregate patient events (diagnoses, medications, procedures) within the window into feature vectors (e.g., counts for categorical variables). Perform global feature selection (e.g., using information gain) to reduce dimensionality [3].
- Similarity Metric Training: Train the LSML distance metric ((D{LSML}(xi, xj) = (xi - xj)^T W W^T (xi - x_j))) on the training set to maximize local class discriminability for the specific target condition (e.g., diabetes onset) [3].
- Personalized Model Training (per test patient):
- Identify the K most clinically similar patients from the training set for a given test patient using the trained LSML metric.
- Apply feature filtering to the similar cohort, retaining features present in the test patient or in ≥2 similar patients.
- Train a logistic regression model on this filtered, similar-patient cohort.
- Use the model to compute a diabetes onset risk score for the test patient [3].
- Validation: Employ 10-fold cross-validation. Evaluate performance using the Area Under the ROC Curve (AUC) and compare against a global logistic regression model trained on all data [3].
Protocol 2: Development of an Equity-Aware AI Predictive Model (BE-FAIR Framework)
This protocol outlines the nine-step framework used by UC Davis Health to create a bias-reduced model for predicting hospitalizations and ED visits [6].
- Multidisciplinary Team Assembly: Form a team encompassing population health, information technology, and health equity expertise [6].
- Problem & Outcome Definition: Define the target prediction (e.g., 12-month risk of hospitalization or emergency department visit).
- Data Source Identification: Consolidate relevant patient data from EHR and other health system sources.
- Predictor Variable Selection: Choose candidate variables based on clinical relevance and data availability.
- Model Training & Algorithm Selection: Train initial predictive models (e.g., ensemble ML methods) on historical data.
- Equity-Focused Evaluation: Rigorously evaluate model calibration and performance across different racial, ethnic, and demographic subgroups to identify underprediction or bias [6].
- Threshold Adjustment & Mitigation: Adjust prediction thresholds or implement post-processing techniques to improve equity in risk scoring and patient identification [6].
- Implementation & Workflow Integration: Integrate the model into clinical workflows, providing care managers with risk scores. Establish protocols for proactive patient outreach [6].
- Continuous Monitoring & Re-evaluation: Establish ongoing monitoring of model performance and equity metrics, with plans for periodic retraining [6].
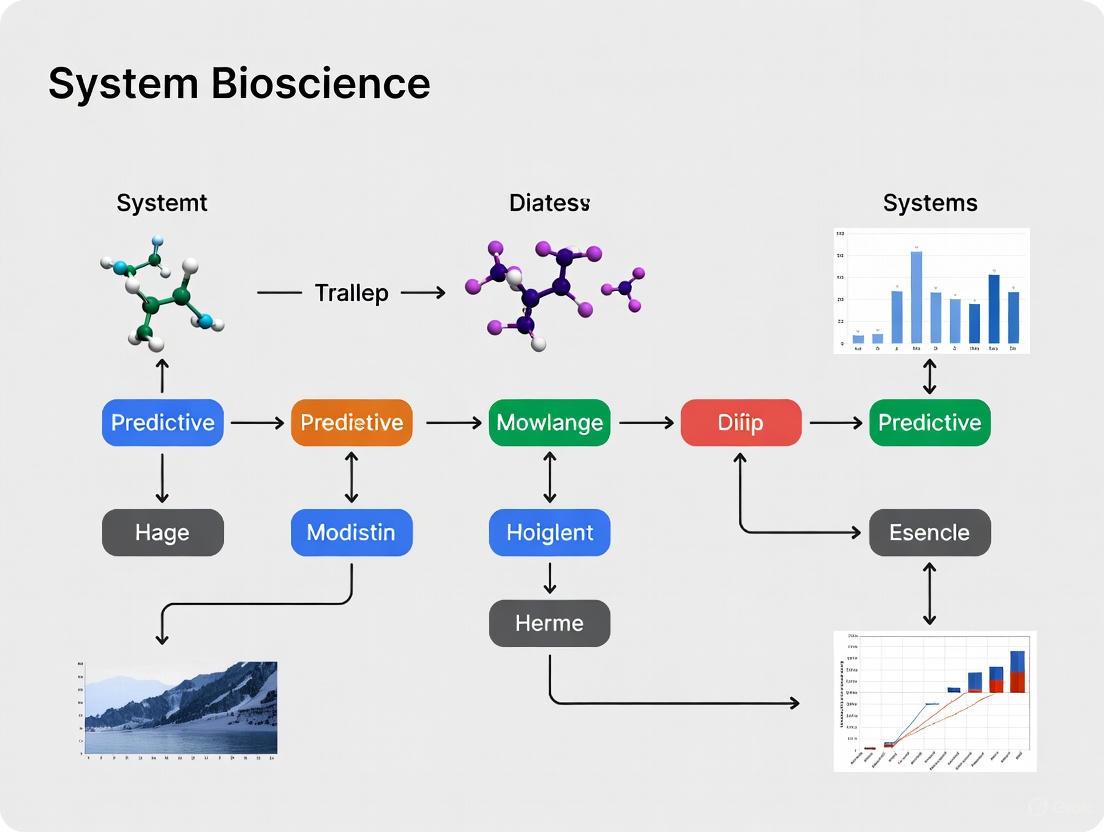
Visualizing the Predictive Modeling Workflow and AI Pipeline
Diagram 1: Workflows for Personalized Prediction and AI-Driven Discovery
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Materials and Solutions for Predictive Outcomes Research
| Item | Function & Application in Research | Example from Context |
|---|---|---|
| Longitudinal EHR/Claims Datasets | Provides the raw, time-stamped patient event data (diagnoses, medications, labs) necessary for feature engineering and model training. | 15,038 patient cohort for diabetes prediction [3]; CAP-AI dataset for pneumonia outcomes [5]. |
| Structured Medical Code Vocabularies (ICD-10, SNOMED-CT) | Standardizes diagnosis, procedure, and medication data, enabling consistent feature extraction and model generalizability across systems. | Sequential diagnosis codes used as primary input for deep learning models [4]. |
| Trainable Similarity Metric (e.g., LSML) | A crucial algorithmic component for personalized models that learns a disease-specific distance measure to find clinically similar patients [3]. | LSML used to customize cohort selection for diabetes onset prediction [3]. |
| Deep Learning Architectures (RNN/LSTM, Transformers) | Software frameworks (e.g., TensorFlow, PyTorch) implementing these architectures are essential for modeling sequential, temporal relationships in patient journeys. | RNNs/Transformers used in 82% of studies analyzing sequential diagnosis codes [4]. |
| Equity Assessment Toolkit | A set of statistical and visualization tools (e.g., calibration plots by subgroup, fairness metrics) required to evaluate and mitigate bias in predictive models. | Core component of the BE-FAIR framework to identify and correct underprediction for racial/ethnic groups [6]. |
| Model Explainability (XAI) Libraries | Software tools (e.g., SHAP, LIME) that help interpret complex model predictions, building trust and facilitating clinical translation. | Needed to address the explainability gap noted in 45% of DL-based studies [4]. |
| Validation Frameworks (PROBAST, TRIPOD) | Methodological guidelines and checklists that provide a standardized protocol for assessing the risk of bias and reporting quality in predictive model studies. | PROBAST used to assess high risk of bias in 70% of reviewed DL studies [4]. |
The paradigm shift toward proactive and personalized care is intrinsically linked to advances in predictive analytics. As evidenced by the comparative data, no single modeling approach is universally superior. Global models offer baseline efficiency, while personalized models promise tailored accuracy at the cost of complexity [3]. Deep learning methods unlock temporal insights but raise concerns regarding bias, generalizability, and explainability that must be actively managed [6] [4]. For researchers and drug developers, the critical task is to align the choice of modeling paradigm—be it for patient risk stratification, clinical trial enrichment, or drug safety prediction [8]—with the specific clinical question, available data quality, and an unwavering commitment to equitable and interpretable outcomes. The future of patient outcomes research lies in the rigorous, context-aware application and continuous refinement of these powerful tools.
In patient outcomes research, the assessment of predictive models extends beyond simple accuracy. For researchers and drug development professionals, a model's value is determined by its discriminative ability, the reliability of its probability estimates, and its overall predictive accuracy. These aspects are quantified by three cornerstone classes of metrics: Discrimination (AUC-ROC, C-statistic), Calibration, and Overall Performance (Brier Score). The machine learning community often focuses on discrimination, but in clinical settings, a model with high discrimination that is poorly calibrated can lead to overconfident or underconfident predictions that misguide clinical decisions and compromise patient safety [9] [10]. For instance, a model predicting a 90% risk of heart disease should mean that 9 out of 10 such patients actually have the disease; calibration measures this agreement. Therefore, a comprehensive evaluation integrating all three metric classes is not just best practice—it is a fundamental requirement for deploying trustworthy models in healthcare [11] [12].
Metric Definitions and Theoretical Frameworks
Discrimination: The AUC-ROC and C-Statistic
Discrimination is a model's ability to distinguish between different outcome classes, such as patients who will versus will not experience an adverse event. The Area Under the Receiver Operating Characteristic Curve (AUC-ROC), often equivalent to the C-statistic in binary outcomes, is the primary metric for this purpose [13].
The ROC curve is a plot of a model's True Positive Rate (Sensitivity) against its False Positive Rate (1 - Specificity) across all possible classification thresholds. The AUC-ROC summarizes this curve into a single value. Mathematically, the AUC can be interpreted as the probability that a randomly chosen positive instance (e.g., a patient with the disease) will have a higher predicted risk than a randomly chosen negative instance (a patient without the disease) [10]. Its value ranges from 0 to 1, where 0.5 indicates performance no better than random chance, and 1.0 represents perfect discrimination.
Calibration: The Reliability of Probabilities
Calibration refers to the agreement between predicted probabilities and observed event frequencies. A perfectly calibrated model ensures that among all instances assigned a predicted probability of p, the proportion of actual positive outcomes is p [10]. Formally, this is expressed as:
ℙ(Y=1|f(X)=p)=p ∀p ∈[0,1]
where f(X) is the model's predicted probability [10].
Unlike discrimination, calibration is not summarized by a single metric. Instead, it is assessed using a suite of tools:
- Calibration Plots (Reliability Diagrams): A visual tool plotting predicted probabilities (x-axis) against observed event frequencies (y-axis). A well-calibrated model will have points close to the 45-degree diagonal line [10].
- Expected Calibration Error (ECE): A weighted average of the absolute difference between confidence and accuracy within bins of predicted probability [9] [10].
- Spiegelhalter's Z-Test: A statistical test for calibration where a non-significant p-value (e.g., p > 0.05) suggests no major miscalibration [14] [9].
- Hosmer-Lemeshow (HL) Test: Another goodness-of-fit test for calibration, where a non-significant p-value indicates good calibration [14].
The Brier Score is an overall measure of predictive accuracy. It is defined as the mean squared difference between the predicted probability and the actual outcome [12] [10].
BS = 1/n * ∑(f(x_i) - y_i)²
where f(x_i) is the predicted probability and y_i is the actual outcome (0 or 1).
The Brier score ranges from 0 to 1, with 0 representing perfect accuracy. Its key strength is that it incorporates both discrimination and calibration into a single value. A model with good discrimination but poor calibration will be penalized with a higher Brier score [12]. Recent research has proposed a weighted Brier score to align this metric more closely with clinical utility by incorporating cost-benefit trade-offs inherent in clinical decision-making [12].
Comparative Analysis of Performance Metrics
The table below provides a structured comparison of these core metrics, highlighting what they measure, their interpretation, and inherent strengths and weaknesses.
Table 1: Comparative Analysis of Key Performance Metrics for Predictive Models
| Metric | What It Measures | Interpretation & Range | Key Strengths | Key Limitations |
|---|---|---|---|---|
| AUC-ROC / C-statistic | Model's ability to rank order patients (e.g., high-risk vs. low-risk). | 0.5 (No Disc.) - 1.0 (Perfect). A value of 0.7-0.8 is considered acceptable, 0.8-0.9 excellent, and >0.9 outstanding. | Threshold-invariant: Provides an overall performance measure across all decision thresholds. Intuitive interpretation as probability. | Does not assess calibration: A model can have high AUC but be severely miscalibrated. Insensitive to class imbalance in some cases. |
| Calibration Metrics | Agreement between predicted probabilities and observed outcomes. | Perfect calibration is achieved when the calibration curve aligns with the diagonal. ECE/Spiegelhalter's test should be low/non-significant. | Crucial for risk estimation: Essential for models whose outputs inform treatment decisions based on risk thresholds. | No single summary statistic: Requires multiple metrics and visualizations for a complete picture. Can be dependent on the binning strategy (for ECE). |
| Brier Score | Overall accuracy of probability estimates, combining discrimination and calibration. | 0 (Perfect) - 1 (Worst). A lower score indicates better overall performance. | Composite Measure: Naturally balances discrimination and calibration. A strictly proper scoring rule, meaning it is optimized by predicting the true probability. | Less intuitive: The absolute value can be difficult to interpret without a baseline. Amalgamates different types of errors into one number. |
Experimental Protocols for Metric Evaluation
Case Study: Calibration Assessment in Heart Disease Prediction
A 2025 study on heart disease prediction provides a robust experimental protocol for a comprehensive model evaluation, benchmarking six classifiers and two post-hoc calibration methods [9].
1. Study Objective: To evaluate and improve the calibration and uncertainty quantification of machine learning models for heart disease classification.
2. Dataset and Preprocessing:
- Dataset: A structured clinical dataset with 1,025 records related to heart disease.
- Train-Test Split: An 85/15 split was used, a common hold-out validation method.
- Models Benchmark: Six classifiers were trained: Logistic Regression, Support Vector Machine (SVM), k-Nearest Neighbors (KNN), Naive Bayes, Random Forest, and XGBoost.
3. Performance Evaluation Workflow: The experiment followed a structured workflow to assess baseline performance and the impact of post-hoc calibration, as visualized below.
Model Evaluation and Calibration Workflow
4. Key Findings and Quantitative Results: The study demonstrated that models with perfect discrimination could still be poorly calibrated. Post-hoc calibration, particularly Isotonic Regression, consistently improved probability quality without harming discrimination.
Table 2: Experimental Results from Heart Disease Prediction Study [9]
| Model | Baseline Accuracy | Baseline ROC-AUC | Baseline Brier Score | Baseline ECE | Post-Calibration (Isotonic) Brier Score | Post-Calibration (Isotonic) ECE |
|---|---|---|---|---|---|---|
| Random Forest | ~100% | ~100% | 0.007 | 0.051 | 0.002 | 0.011 |
| SVM | 92.9% | 99.4% | N/R | 0.086 | N/R | 0.044 |
| Naive Bayes | N/R | N/R | 0.162 | 0.145 | 0.132 | 0.118 |
| k-NN (KNN) | N/R | N/R | N/R | 0.035 | N/R | 0.081* |
Note: N/R = Not Explicitly Reported in Source; *Platt scaling worsened ECE for KNN, highlighting the need to evaluate both methods.
Building and evaluating predictive models requires a suite of statistical tools and software resources. The table below details key "research reagents" for a robust evaluation protocol.
Table 3: Essential Reagents for Predictive Model Evaluation
| Tool / Resource | Category | Function in Evaluation | Application Example |
|---|---|---|---|
| PROBAST Tool [13] | Methodological Guideline | A structured tool to assess Risk Of Bias and applicability in prediction model studies. | Used in systematic reviews to ensure included models are methodologically sound. |
| Platt Scaling [9] [10] | Post-hoc Calibration Algorithm | A parametric method that fits a sigmoid function to map classifier outputs to better-calibrated probabilities. | Improving the probability outputs of an SVM model for clinical use. |
| Isotonic Regression [9] [10] | Post-hoc Calibration Algorithm | A non-parametric method that learns a monotonic mapping to calibrate probabilities, more flexible than Platt scaling. | Calibrating a Random Forest model that showed significant overconfidence. |
| Reliability Diagram [11] [10] | Visual Diagnostic Tool | Plots predicted probabilities against observed frequencies to provide an intuitive visual assessment of calibration. | The primary visual tool used in the heart disease study to show calibration before and after intervention [9]. |
| Brier Score Decomposition [12] | Analytical Framework | Breaks down the Brier score into reliability (calibration), resolution, and uncertainty components for nuanced analysis. | Diagnosing whether a poor Brier score is due to miscalibration or poor discrimination. |
| Decision Curve Analysis (DCA) [13] [12] | Clinical Usefulness Tool | Evaluates the net benefit of using a model for clinical decision-making across a range of risk thresholds. | Justifying the clinical implementation of a model by showing its added value over default strategies. |
For professionals in drug development and patient outcomes research, a singular focus on any one class of performance metrics is a critical oversight. Discrimination (AUC-ROC), Calibration, and Overall Performance (Brier Score) are three pillars of a robust model assessment. The evidence shows that a model with stellar discrimination can produce dangerously miscalibrated probabilities, undermining its clinical utility [9]. Therefore, the routine application of a comprehensive evaluation protocol—incorporating the metrics, experimental frameworks, and tools detailed in this guide—is indispensable. This rigorous approach ensures that predictive models are not only statistically sound but also clinically trustworthy and actionable, ultimately enabling better-informed decisions in healthcare and therapeutic development.
The Role of Predictive Modeling in Modern Drug Development and Clinical Trials
The development of new pharmaceuticals is undergoing a transformative shift from traditional trial-and-error approaches to a precision-driven paradigm powered by predictive modeling. Model-Informed Drug Development (MIDD) has emerged as an essential framework that provides quantitative, data-driven insights throughout the drug development lifecycle, from early discovery to post-market surveillance [15]. This approach leverages mathematical models and simulations to predict drug behavior, therapeutic effects, and potential risks, thereby accelerating hypothesis testing and reducing costly late-stage failures [15]. The fundamental strength of predictive modeling lies in its ability to synthesize complex biological, chemical, and clinical data into actionable insights that support more informed decision-making.
The adoption of predictive modeling represents nothing less than a paradigm shift, replacing labor-intensive, human-driven workflows with AI-powered discovery engines capable of compressing timelines and expanding chemical and biological search spaces [16]. Evidence from drug development and regulatory approval has demonstrated that well-implemented MIDD approaches can significantly shorten development cycle timelines, reduce discovery and trial costs, and improve quantitative risk estimates, particularly when facing development uncertainties [15]. As the field continues to evolve, the integration of artificial intelligence and machine learning is further expanding the capabilities and applications of predictive modeling in pharmaceutical research.
Comparative Analysis of Predictive Modeling Techniques
Traditional Statistical Approaches
Traditional statistical methods have formed the backbone of clinical research and drug development for decades. These approaches include Cox Proportional Hazards (CPH) models for time-to-event data such as survival analysis, and logistic regression for binary outcomes [17] [18]. The CPH model, in particular, has been widely used for predicting survival outcomes in oncology studies, while logistic regression has been valued for its interpretability and simplicity in clinical settings [17] [19].
These conventional methods operate on well-established statistical principles and offer high interpretability, making them attractive for regulatory submissions. However, they face significant limitations when dealing with complex, high-dimensional datasets characterized by non-linear relationships and multiple interacting variables [17] [4]. Traditional models typically require manual feature selection, which is both time-consuming and dependent on extensive domain expertise, and they often struggle to effectively capture the temporal chronological sequence of patients' medical history [4].
Modern Machine Learning and AI-Driven Approaches
Modern machine learning techniques have dramatically expanded the toolkit available for predictive modeling in drug development. These include tree-based ensemble methods like Random Forest and Gradient Boosting Trees (GBT), deep learning architectures such as Recurrent Neural Networks (RNNs) and Transformers, and hybrid approaches that combine multiple methodologies [16] [19] [4].
These advanced techniques offer significant advantages in handling complex, high-dimensional data with minimal need for feature engineering. They can automatically uncover associations between inputs and outputs, generate effective embedding spaces to manage high-dimensional problems, and effectively capture temporal patterns in sequential data [4]. However, they often require substantial computational resources, extensive datasets for training, and present challenges in interpretability – a significant concern in clinical and regulatory contexts [19] [4].
Table 1: Comparison of Predictive Modeling Techniques in Drug Development
| Technique | Primary Applications | Strengths | Limitations |
|---|---|---|---|
| Cox Regression [17] [18] | Survival analysis, time-to-event outcomes | Statistical robustness, high interpretability, regulatory familiarity | Limited handling of non-linear relationships, proportional hazards assumption |
| Logistic Regression [19] [20] | Binary classification tasks, diagnostic models | Simplicity, interpretability, clinical transparency | Limited capacity for complex relationships, requires feature engineering |
| Random Survival Forest [17] | Censored data, survival analysis with multiple predictors | Handles non-linearity, robust to outliers, requires less preprocessing | Less interpretable, computationally intensive with large datasets |
| Gradient Boosting Machines [19] [20] | Various prediction tasks including CVD risk and COVID-19 case identification | High predictive accuracy, handles mixed data types | Prone to overfitting without careful tuning, complex interpretation |
| Deep Learning (RNNs/Transformers) [4] | Sequential health data, medical history patterns | Automatic feature learning, captures complex temporal relationships | High computational demands, "black box" nature, requires large datasets |
| Quantitative Systems Pharmacology [15] | Mechanistic modeling of drug effects | Incorporates physiological knowledge, explores system-level behaviors | Complex model development, requires specialized expertise |
Performance Comparison: Traditional vs. Machine Learning Approaches
Comparative studies have yielded nuanced insights into the performance of traditional versus machine learning approaches. A 2025 systematic review and meta-analysis of machine learning models for cancer survival outcomes found that ML models showed no superior performance over CPH regression, with a standardized mean difference in AUC or C-index of just 0.01 (95% CI: -0.01 to 0.03) [17]. This suggests that while machine learning approaches offer advantages in handling complex data structures, they do not necessarily outperform well-specified traditional models for all applications.
However, in other domains, machine learning has demonstrated superior performance. A 2024 study comparing AI/ML approaches with classical regression for COVID-19 case prediction found that the Gradient Boosting Trees (GBT) method significantly outperformed multivariate logistic regression (AUC = 0.796 ± 0.017) [20]. Similarly, in predicting cardiovascular disease risk among type 2 diabetes patients, the XGBoost model demonstrated consistent performance (AUC = 0.75 training, 0.72 testing) with better generalization ability compared to other algorithms [19].
These comparative results highlight that the optimal modeling approach depends heavily on the specific application, data characteristics, and clinical context, rather than there being a universally superior technique.
Key Applications in the Drug Development Pipeline
Drug Discovery and Preclinical Development
Predictive modeling has revolutionized early-stage drug discovery through approaches like quantitative structure-activity relationship (QSAR) modeling and physiologically based pharmacokinetic (PBPK) modeling [15]. AI-driven platforms have demonstrated remarkable efficiency gains, with companies like Exscientia reporting in silico design cycles approximately 70% faster and requiring 10× fewer synthesized compounds than industry norms [16]. Insilico Medicine's generative-AI-designed idiopathic pulmonary fibrosis drug progressed from target discovery to Phase I trials in just 18 months, dramatically compressing the typical 5-year timeline for discovery and preclinical work [16].
Leading AI-driven drug discovery platforms have employed diverse approaches, including generative chemistry (Exscientia), phenomics-first systems (Recursion), integrated target-to-design pipelines (Insilico Medicine), knowledge-graph repurposing (BenevolentAI), and physics-plus-ML design (Schrödinger) [16]. These platforms leverage machine learning and generative models to accelerate tasks that were long reliant on cumbersome trial-and-error approaches, representing a fundamental shift in early-stage research and development.
Clinical Trial Optimization
In clinical development, predictive modeling enhances trial design and execution through several critical applications. First-in-Human (FIH) dose algorithms incorporate toxicokinetic PK, allometric scaling, and semi-mechanistic PK/PD approaches to determine starting doses and escalation schemes [15]. Adaptive trial designs enable dynamic modification of clinical trial parameters based on accumulated data, while clinical trial simulations use mathematical and computational models to virtually predict trial outcomes and optimize study designs before conducting actual trials [15].
Population pharmacokinetics and exposure-response (PPK/ER) modeling characterize clinical population pharmacokinetics and exposure-response relationships, supporting dosage optimization and regimen selection [15]. These approaches help explain variability in drug exposure among individuals and establish relationships between drug exposure and effectiveness or adverse effects, ultimately supporting more efficient and informative clinical trials.
Clinical Implementation and Patient Outcome Prediction
In clinical settings, predictive models are increasingly deployed to guide diagnostic and therapeutic decisions. A systematic review of deep learning models using sequential diagnosis codes from electronic health records found these approaches particularly valuable for predicting patient outcomes, with the most frequent applications being next-visit diagnosis (23%), heart failure (14%), and mortality (13%) prediction [4]. The analysis revealed that using multiple types of features, integrating time intervals, and including larger sample sizes were generally related to improved predictive performance [4].
However, challenges remain in clinical implementation. A systematic review of implemented clinical prediction models found that only 13% of models have been updated following implementation, and external validation was performed for just 27% of models [21]. Additionally, 70% of deep learning-based prediction models were found to have a high risk of bias, highlighting the importance of rigorous methodology and validation [4].
Table 2: Applications of Predictive Modeling Across Drug Development Stages
| Development Stage | Modeling Approaches | Key Questions Addressed | Impact Metrics |
|---|---|---|---|
| Drug Discovery [15] [16] | QSAR, Generative AI, Knowledge Graphs | Target identification, lead compound optimization | 70% faster design cycles (Exscientia), 10× fewer compounds synthesized |
| Preclinical Development [15] | PBPK, Semi-mechanistic PK/PD | Preclinical prediction accuracy, FIH dose selection | 18 months from target to Phase I (Insilico Medicine) vs. typical 5 years |
| Clinical Trials [15] | PPK/ER, Clinical Trial Simulation, Adaptive Designs | Dose optimization, trial efficiency, subgroup identification | Reduced trial costs, improved probability of success |
| Regulatory Review [15] [22] | Model-Integrated Evidence, Bayesian Inference | Safety and effectiveness evaluation, label claims | >500 submissions with AI components to CDER (2016-2023) |
| Post-Market Surveillance [15] | Model-Based Meta-Analysis, Virtual Population Simulation | Real-world safety monitoring, label updates | Ongoing benefit-risk assessment |
Experimental Protocols and Methodological Considerations
Protocol Development for Predictive Model Studies
Robust development of predictive models requires rigorous methodological planning. Protocol registration on platforms such as ClinicalTrials.gov is essential for reducing transparency risks and methodological inconsistencies [18]. A comprehensive study protocol should detail all aspects of model development and evaluation, including data sources, preprocessing methods, feature selection approaches, model training procedures, and validation strategies [18].
Engaging end-users including clinicians, patients, and public representatives early in the development process is critical for ensuring model relevance and usability in real-world settings [18]. This collaborative approach helps clarify clinical questions, informs selection of meaningful predictors, and guides how predictions will integrate into clinical workflows – all essential factors for successful implementation and impact.
Data Preprocessing and Feature Selection
High-quality data preprocessing is fundamental to developing reliable predictive models. The Boruta algorithm, a random forest-based wrapper method, has demonstrated effectiveness for feature selection in clinical datasets by iteratively comparing feature importance with randomly permuted "shadow" features [19]. This approach identifies all relevant predictors rather than just a minimal subset, which is particularly advantageous in clinical research where disease risk is typically influenced by multiple interacting factors [19].
For handling missing data, Multiple Imputation by Chained Equations (MICE) provides a flexible approach that models each variable with missing data conditionally on other variables in an iterative fashion [19]. This method is particularly well-suited for clinical datasets containing different types of variables (continuous, categorical, binary) and complex missing patterns, as it accounts for multivariate relationships among variables and produces multiple imputed datasets that fully incorporate uncertainty caused by missingness.
Model Training and Validation Frameworks
Comprehensive validation is essential for assessing model performance and generalizability. Internal validation using bootstrapping or cross-validation provides initial performance estimates, while external validation in completely independent datasets is crucial for assessing real-world applicability [18]. When possible, internal-external validation approaches, where a prediction model is iteratively developed on data from multiple subsets and validated on remaining excluded subsets, can explore heterogeneity in model performance across different settings [18].
Model evaluation should extend beyond discrimination metrics (e.g., AUC, C-index) to include calibration assessment and clinical utility evaluation [18]. Calibration plots examine how well predicted probabilities align with observed outcomes, while decision curve analysis can assess the net benefit of using the model for clinical decision-making across different threshold probabilities.
Research Reagent Solutions: Computational Tools and Platforms
Table 3: Essential Research Reagents and Computational Platforms for Predictive Modeling
| Tool/Category | Representative Examples | Primary Function | Application Context |
|---|---|---|---|
| AI-Driven Discovery Platforms [16] | Exscientia, Insilico Medicine, Recursion, BenevolentAI, Schrödinger | End-to-end drug candidate identification and optimization | Small-molecule design, target discovery, clinical candidate selection |
| Feature Selection Algorithms [19] | Boruta Algorithm | Identify all relevant predictors in high-dimensional clinical datasets | Preprocessing for clinical prediction models, biomarker identification |
| Machine Learning Frameworks [19] [20] | XGBoost, LightGBM, Random Forest, Deep Neural Networks | Model development for classification and prediction tasks | CVD risk prediction, COVID-19 case identification, survival analysis |
| Model Interpretation Tools [19] | SHAP (SHapley Additive exPlanations) | Visual interpretation of complex model predictions | Explainability for clinical adoption, feature importance analysis |
| Data Imputation Methods [19] | MICE (Multiple Imputation by Chained Equations) | Handle missing data in clinical datasets with mixed variable types | Data preprocessing for real-world clinical datasets |
| Deployment Platforms [19] | Shinyapps.io | Web-based deployment of predictive models for clinical use | Clinical decision support tools, risk assessment platforms |
Visualization of Predictive Modeling Workflows
The MIDD Framework Across Drug Development Stages
The following diagram illustrates how predictive modeling integrates throughout the drug development lifecycle, based on the Model-Informed Drug Development (MIDD) framework:
MIDD Framework in Drug Development - This diagram illustrates how predictive modeling integrates throughout the drug development lifecycle using the Model-Informed Drug Development (MIDD) framework, emphasizing the "fit-for-purpose" approach where tools are aligned with specific development stage questions.
AI-Driven Drug Discovery Platform Architecture
The following diagram outlines the core architecture and workflow of modern AI-driven drug discovery platforms:
AI-Driven Drug Discovery Platform - This architecture diagram shows the core components and workflow of modern AI-driven drug discovery platforms, highlighting how diverse data sources feed into specialized AI approaches that accelerate the candidate identification and optimization process.
Regulatory Landscape and Implementation Challenges
Regulatory Evolution and Current Framework
The regulatory landscape for predictive modeling in drug development is rapidly evolving to keep pace with technological advancements. The U.S. Food and Drug Administration (FDA) has recognized the increased use of AI throughout the drug product lifecycle and has established the CDER AI Council to provide oversight, coordination, and consolidation of AI-related activities [22]. This council serves as a decisional body that coordinates, develops, and supports both internal and external AI-related activities in the Center for Drug Evaluation and Research.
International harmonization efforts are also underway, with the International Council for Harmonization (ICH) expanding its guidance to include MIDD through the M15 general guidance [15]. This global harmonization promises to improve consistency among global sponsors in applying MIDD in drug development and regulatory interactions, potentially promoting more efficient processes worldwide. The FDA has also published a draft guidance in 2025 titled "Considerations for the Use of Artificial Intelligence to Support Regulatory Decision Making for Drug and Biological Products," which provides recommendations on using AI to produce information supporting regulatory decisions regarding drug safety, effectiveness, or quality [22].
Implementation Barriers and Mitigation Strategies
Despite significant advances, substantial barriers impede the widespread implementation of predictive models in clinical practice and drug development. A systematic review of implemented clinical prediction models found that 86% of publications had high risk of bias, and only 32% of models were assessed for calibration during development and internal validation [21]. This highlights critical methodological shortcomings that undermine model reliability and trust.
Additional implementation challenges include limited stakeholder engagement during development, insufficient evidence of clinical utility, and lack of consideration for workflow integration [18]. Furthermore, fewer than half of deep learning-based prediction models address explainability challenges, and only 8% evaluate generalizability across different populations or settings [4]. These limitations significantly hamper clinical adoption and real-world impact.
To address these challenges, researchers should prioritize early and meaningful stakeholder engagement, comprehensive external validation, rigorous fairness assessment across demographic groups, and development of post-deployment monitoring plans [18]. Following established reporting guidelines such as TRIPOD+AI (Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis Or Diagnosis + Artificial Intelligence) enhances transparency, reproducibility, and critical appraisal of predictive models [18].
Predictive modeling has fundamentally transformed drug development, enabling more efficient, targeted, and evidence-based approaches across the entire pharmaceutical lifecycle. The integration of artificial intelligence and machine learning has further accelerated this transformation, with AI-designed therapeutics now advancing through human trials across diverse therapeutic areas [16]. However, the field must address critical challenges related to model robustness, fairness, explainability, and generalizability to fully realize the potential of these advanced approaches.
Future progress will depend on developing more transparent and interpretable models, establishing standardized validation frameworks, and fostering collaboration between computational scientists, clinical researchers, and regulatory experts. As predictive modeling continues to evolve, its role in supporting personalized treatment approaches, optimizing clinical trial designs, and improving drug safety monitoring will expand, ultimately enhancing the efficiency of pharmaceutical development and the quality of patient care. The organizations that successfully navigate this complex landscape – balancing innovation with methodological rigor – will lead the next wave of advances in drug development and clinical research.
Understanding Results-Based Management (RBM) for Healthcare Performance
Results-Based Management (RBM) is a strategic framework that shifts the focus of healthcare programs and interventions from activities to measurable outcomes. Within the context of assessing predictive models for patient outcomes research, RBM provides a structured approach to define expected results, monitor progress using performance indicators, and utilize evidence for evaluation and decision-making [23] [24]. This guide compares the application and performance of different predictive models used within the RBM framework to enhance healthcare delivery and patient care.
The RBM Framework in Healthcare
RBM operates on three core principles: goal-orientedness, which involves setting clear targets; causality, which requires mapping the logical links between inputs, activities, and results; and continuous improvement, which uses performance data for learning and adaptation [23]. In healthcare, this translates to a management cycle of planning, monitoring, and evaluation to improve efficiency and effectiveness [25] [24].
The "Results Chain" is a central tool in RBM, providing a visual model of the causal pathway from a program's inputs to its long-term impact [26] [24]. The following diagram illustrates this logic as applied to a healthcare intervention.
Figure 1: RBM Results Chain for Healthcare. This logic model shows the cause-and-effect pathway from program inputs to long-term health impact [23] [26] [24].
Comparative Analysis of Predictive Models for RBM
Predictive models are crucial for analyzing performance indicator results, forecasting trends, and enabling evidence-based decision-making within the RBM framework [25]. The table below compares three established statistical models.
Table 1: Performance Comparison of Predictive Models in Healthcare RBM
| Predictive Model | Best-Performing Context (from studies) | Key Performance Metric | Reported Result | Primary Strength | Key Limitation |
|---|---|---|---|---|---|
| Linear Regression (LR) | Analyzing 9 out of 10 medical performance indicators (e.g., hospital efficiency, bed turnover) [25] | Mean Absolute Error (MAE) | Lowest MAE for 9 indicators; 7 with p < 0.05 [25] | Powerful, widely applicable statistical tool [25] | Sensitive to outliers; requires checking of assumptions (normality, homoskedasticity) [25] |
| Autoregressive Integrated Moving Average (ARIMA) | Forecasting patient attendance at hospital services [25] | Forecast Error | ~3% error in predicting expected annual patients [25] | Effectively captures linear patterns and trends in time series data [25] | Less effective with non-linear data patterns [25] |
| Exponential Smoothing (ES) | Short-term forecasting with limited historical data (e.g., electricity demand) [25] | Error Rate | Highly accurate predictions with minimal errors [25] | Robust, simple formulation, requires few calculations [25] | Best for short-term forecasts; may not capture complex long-term trends [25] |
Advanced and Hybrid Predictive Models
Beyond traditional statistical models, machine learning (ML) and hybrid deep learning approaches offer advanced capabilities for handling complex healthcare data, such as high-dimensional electronic health records (EHRs) and medical images [27].
Table 2: Performance of Hybrid Deep Learning Models in Healthcare Prediction
| Hybrid Model | Reported Accuracy | Reported Precision | Reported Recall | Notable Strength |
|---|---|---|---|---|
| Random Forest + Neural Network (RF + NN) | 96.81% [27] | 70.08% [27] | 90.48% [27] | Highest overall accuracy [27] |
| XGBoost + Neural Network (XGBoost + NN) | 96.75% [27] | 73.54% [27] | 96.75% [27] | Better at identifying true positives [27] |
| Autoencoder + Random Forest (Autoencoder + RF) | Not Specified | 91.36% [27] | 66.22% [27] | Highest precision, reduces data dimensionality [27] |
These models combine the strengths of different algorithms. For instance, autoencoders perform unsupervised feature extraction from high-dimensional data, which is then used for classification by robust tree-based models like Random Forest or XGBoost [27]. The workflow for such a hybrid approach is illustrated below.
Figure 2: Hybrid Predictive Model Workflow. This workflow shows the process from raw data to prediction, highlighting the feature extraction and optimization stage used in advanced models [28] [27].
Experimental Protocols and Methodologies
Protocol 1: Validating Predictive Models for Performance Indicators
This protocol is based on a retrospective study comparing three models to forecast medical performance indicators in a National Institute of Health [25].
- Objective: To identify the most accurate predictive model (Exponential Smoothing, ARIMA, or Linear Regression) for forecasting results of key performance indicators within an RBM system.
- Data Collection: Performance indicator data arranged in time series. The study analyzed 10 medical performance indicators [25].
- Model Execution:
- Exponential Smoothing (ES): Applied for its robustness with limited historical data.
- ARIMA: Formulated to capture autoregressive (AR) and moving average (MA) components in the time series data. The level of differentiation (I) was determined to ensure data stationarity [25].
- Linear Regression (LR): Used to model the relationship between the dependent variable (the performance indicator) and time or other independent variables.
- Validation & Analysis:
- The Mean Absolute Error (MAE) was the primary metric for comparing model performance and identifying the best one [25].
- For the top-performing Linear Regression model, three key assumptions were checked:
Protocol 2: Implementing a Hybrid Deep Learning Model
This protocol outlines the methodology for developing a hybrid model, such as Autoencoder + Random Forest, for complex healthcare predictions [27].
- Objective: To leverage automated feature extraction and robust classification for predicting healthcare outcomes like disease onset.
- Data Collection: Using large-scale, often high-dimensional datasets from open-source platforms (e.g., Kaggle) or institutional EHRs. Data includes clinical variables, lab results, and demographic information [27].
- Model Execution:
- Feature Extraction: An Autoencoder (an unsupervised neural network) is trained to compress the input data and learn a reduced, meaningful representation (encoded features), effectively performing dimensionality reduction [27].
- Classification: The optimized feature set from the autoencoder is used as input to a Random Forest classifier, which makes the final prediction (e.g., disease presence or absence) [27].
- Validation & Analysis:
- Models are evaluated using standard performance metrics: Accuracy, Precision, Recall, and F1-score [27].
- The model's performance is compared against other hybrid models and traditional machine learning algorithms to demonstrate its relative strength in handling imbalanced datasets and improving predictive accuracy [27].
The Scientist's Toolkit: Essential Reagents for RBM Predictive Analysis
This toolkit details key methodological components and their functions for conducting predictive analytics within a healthcare RBM framework.
Table 3: Essential Analytical Toolkit for RBM Predictive Research
| Tool / Method | Function in RBM Predictive Analysis |
|---|---|
| Performance Indicators | Quantitative or qualitative variables (e.g., rates, proportions, averages) used to measure results in dimensions like effectiveness, quality, economy, and efficiency [25]. |
| Mean Absolute Error (MAE) | A key metric to identify the best predictive model by measuring the average magnitude of errors between predicted and actual values of a performance indicator [25]. |
| Time Series Analysis | The foundation for arranging and analyzing performance indicator data to generate accurate predictions for resource planning and optimization [25]. |
| Statistical Assumption Tests (e.g., Shapiro-Wilk, Breusch-Pagan) | Used to validate the core assumptions of statistical models like Linear Regression, ensuring the reliability and interpretability of the results [25]. |
| Autoencoders | A type of neural network used for unsupervised feature extraction and dimensionality reduction from high-dimensional healthcare data (e.g., EHRs), improving subsequent modeling [27]. |
| Tree-Based Models (e.g., Random Forest, XGBoost) | Powerful classifiers that work well on structured data and can detect complex interactions, often used in ensembles or hybrids to improve predictive accuracy and robustness [27]. |
Methodologies in Action: Machine Learning, AI, and Real-World Clinical Applications
Predictive modeling has become a cornerstone of modern patient outcomes research, enabling advancements in personalized medicine and proactive healthcare management. The evolution from traditional statistical methods to sophisticated machine learning (ML) algorithms has expanded the toolkit available to researchers and clinicians. This guide provides a systematic comparison of three prominent modeling techniques—Linear Regression, Random Forest (RF), and eXtreme Gradient Boosting (XGBoost)—within the context of healthcare research. By examining their theoretical foundations, practical applications, and performance metrics across various clinical scenarios, this analysis aims to equip researchers with the knowledge needed to select appropriate methodologies for their specific predictive modeling tasks.
The growing complexity of healthcare data, characterized by high dimensionality, non-linear relationships, and intricate interaction effects, necessitates modeling approaches that can capture these patterns effectively. Whereas linear regression offers simplicity and interpretability, ensemble methods like Random Forest and XGBoost provide powerful alternatives for handling complex data structures. This comparison synthesizes evidence from recent studies to objectively evaluate these techniques' relative strengths and limitations in predicting patient outcomes.
Theoretical Foundations and Algorithmic Mechanisms
Linear Regression
Linear regression establishes a linear relationship between a continuous dependent variable (outcome) and one or more independent variables (predictors). The model is represented by the equation Y = a + b × X, where Y is the dependent variable, a is the intercept, b is the regression coefficient, and X represents the independent variable[s]. For multivariable analysis, the equation extends to incorporate multiple predictors. The coefficients indicate the direction and strength of the relationship between each predictor and the outcome, providing straightforward interpretation of each variable's effect. The model's goodness-of-fit is typically assessed using R-squared, which represents the proportion of variance in the dependent variable explained by the independent variables. Linear regression requires certain assumptions including linearity, normality of residuals, and homoscedasticity, which, if violated, can compromise the validity of its results.
Random Forest
Random Forest is an ensemble, tree-based machine learning algorithm that operates by constructing a multitude of decision trees at training time. As a bagging (bootstrap aggregating) method, it creates multiple subsets of the original data through bootstrapping and builds decision trees for each subset. A critical feature is that when building these trees, instead of considering all available predictors, the algorithm randomly selects a subset of predictors at each split, thereby decorrelating the trees and reducing overfitting. The final prediction is determined by aggregating the predictions of all individual trees, either through majority voting for classification tasks or averaging for regression problems. This ensemble approach typically results in improved accuracy and stability compared to single decision trees. Random Forest can automatically handle non-linear relationships and complex interactions between variables without requiring prior specification, making it particularly suitable for exploring complex healthcare datasets where these patterns are common but not always hypothesized in advance.
XGBoost (eXtreme Gradient Boosting)
XGBoost is another ensemble tree-based algorithm that employs a gradient boosting framework. Unlike Random Forest's bagging approach, XGBoost builds trees sequentially, with each new tree designed to correct the errors made by the previous ones in the sequence. The algorithm optimizes a differentiable loss function plus a regularization term that penalizes model complexity, which helps control overfitting. XGBoost incorporates several advanced features including handling missing values, supporting parallel processing, and implementing tree pruning. The sequential error-correction approach, combined with regularization, often yields highly accurate predictions. However, this complexity can make XGBoost more computationally intensive and potentially less interpretable than simpler methods. Its performance advantages have made it particularly popular in winning data science competitions and complex prediction tasks where accuracy is paramount.
Table 1: Core Algorithmic Characteristics Comparison
| Feature | Linear Regression | Random Forest | XGBoost |
|---|---|---|---|
| Algorithm Type | Parametric | Ensemble (Bagging) | Ensemble (Boosting) |
| Model Structure | Linear equation | Multiple independent decision trees | Sequential dependent decision trees |
| Handling Non-linearity | Poor (requires transformation) | Excellent | Excellent |
| Interpretability | High | Moderate (via feature importance) | Moderate (via feature importance/SHAP) |
| Native Handling of Missing Data | No | No | Yes |
| Primary Hyperparameters | None | nestimators, maxdepth, minsamplesleaf | nestimators, learningrate, max_depth, subsample |
Comparative Performance Analysis in Healthcare Applications
Predictive Accuracy Across Clinical Domains
Multiple studies have directly compared the performance of these modeling techniques in predicting patient outcomes, with performance typically measured using area under the receiver operating characteristic curve (AUC), accuracy, F-1 scores, and other domain-specific metrics.
In predicting attrition from diabetes self-management programs, researchers found that XGBoost with downsampling achieved the highest performance among tested models with an AUC of 0.64, followed by Random Forest, while both outperformed logistic regression. However, the generally low AUC values (ranging 0.53-0.64 across models) highlighted the challenge of predicting behavioral outcomes like program adherence, with the authors noting that "machine learning models showed poor overall performance" in this specific context despite identifying meaningful predictors of attrition.
Conversely, in predicting neurological improvement after cervical spinal cord injury, all models performed well, with XGBoost and logistic regression demonstrating comparable performance. XGBoost achieved 81.1% accuracy with an AUC of 0.867, slightly outperforming logistic regression (80.6% accuracy, AUC 0.877) and substantially surpassing a single decision tree (78.8% accuracy, AUC 0.753). This suggests that for certain clinical prediction tasks, ensemble methods can provide meaningful improvements in accuracy.
For predicting unplanned readmissions in elderly patients with coronary heart disease, XGBoost demonstrated strong performance with an AUC of 0.704, successfully identifying key clinical predictors including length of stay, age-adjusted Charlson comorbidity index, monocyte count, blood glucose level, and red blood cell count. Similarly, in forecasting hospital outpatient volume, XGBoost outperformed both Random Forest and SARIMAX (a time-series approach) across multiple metrics including Mean Absolute Error (MAE), Root Mean Squared Error (RMSE), and R-squared, effectively capturing relationships between environmental factors, resource availability, and patient volume.
Table 2: Performance Metrics Across Healthcare Applications
| Clinical Application | Linear Regression/Logistic | Random Forest | XGBoost | Key Predictors Identified |
|---|---|---|---|---|
| Diabetes Program Attrition | Lower performance (AUC ~0.53-0.61) | Intermediate performance | Highest performance (AUC 0.64, F-1 0.36) | Quality of life scores, DCI score, race, age, drive time to grocery store |
| Neurological Improvement (SCI) | Accuracy 80.6%, AUC 0.877 | Not reported | Accuracy 81.1%, AUC 0.867 | Demographics, neurological status, MRI findings, treatment strategies |
| Unplanned Readmission (CHD) | Not reported | Not reported | AUC 0.704 | Length of stay, comorbidity index, monocyte count, blood glucose |
| Self-Perceived Health | Not reported | AUC 0.707 | Not reported | Nine exposome factors from different domains |
| Hospital Outpatient Volume | Lower performance (benchmark) | Intermediate performance | Highest performance (lowest MAE/RMSE, highest R²) | Specialist availability, temporal variables, temperature, PM2.5 |
Interpretability and Factor Identification
Beyond pure predictive accuracy, identifying key factors driving outcomes is crucial for clinical research and intervention development. Linear regression provides direct interpretation through coefficients indicating the direction and magnitude of each variable's effect. For ensemble methods, techniques like feature importance and SHAP (SHapley Additive exPlanations) values enable interpretation despite the models' complexity.
In diabetes self-management attrition prediction, SHAP analysis applied to the XGBoost model identified "health-related measures – specifically the SF-12 quality of life scores, Distressed Communities Index (DCI) score, along with demographic factors (race, age, height, and educational attainment), and spatial variables (drive time to the nearest grocery store)" as influential predictors, providing actionable insights for designing targeted retention strategies despite the model's overall modest predictive power.
Similarly, in a study of patient satisfaction drivers, Random Forest identified 'age' as the most important patient-related determinant across both registration and consultation stages, with 'total time taken for registration' and 'attentiveness and knowledge of the doctor' as the leading provider-related determinants in each respective stage. The radar charts further revealed that 'demographics' questions were most influential in the registration stage, while 'behavior' questions dominated in the consultation stage, demonstrating how ML models can identify varying factor importance across different healthcare process stages.
Methodological Protocols for Healthcare Outcome Prediction
Data Preprocessing and Feature Engineering
Robust predictive modeling requires meticulous data preprocessing. For healthcare data, this typically involves handling missing values through imputation methods (e.g., Multiple Imputation by Chained Equations - MICE), addressing class imbalance in outcomes through techniques like downsampling or upweighting, and normalizing or standardizing continuous variables. Categorical variables require appropriate encoding (e.g., one-hot encoding), and domain-specific feature engineering may incorporate temporal trends (e.g., Area-Under-the-Exposure - AUE - and Trend-of-the-Exposure - TOE for longitudinal data) or clinical composite scores.
Model Development and Hyperparameter Tuning
Optimal model performance requires appropriate hyperparameter tuning. For Random Forest, key hyperparameters include nestimators (number of trees), maxdepth (maximum tree depth), minsamplesleaf (minimum samples required at a leaf node), and minsamplessplit (minimum samples required to split an internal node). For XGBoost, essential parameters include nestimators, learningrate (step size shrinkage), maxdepth, subsample (proportion of observations used for each tree), and colsamplebytree (proportion of features used for each tree).
Systematic approaches like grid search with cross-validation (typically 5-fold or 10-fold) are recommended to identify optimal parameter combinations while mitigating overfitting. The dataset should be divided into training (typically 80%), validation (for hyperparameter tuning), and test sets (for final performance evaluation), with temporal validation for time-series healthcare data.
Model Evaluation and Interpretation
Comprehensive evaluation extends beyond single metrics to include discrimination measures (AUC, accuracy), calibration (calibration curves), and clinical utility (decision curve analysis). For healthcare applications, model interpretability is crucial, with Linear Regression providing natural interpretation, while ensemble methods require techniques like feature importance rankings, partial dependence plots, accumulated local effects plots, or SHAP values to understand variable effects and facilitate clinical adoption.
Diagram 1: Predictive Modeling Workflow in Healthcare Research
Research Reagent Solutions: Essential Tools for Predictive Modeling
Table 3: Essential Computational Tools for Healthcare Predictive Modeling
| Tool Category | Specific Solutions | Function | Representative Applications |
|---|---|---|---|
| Programming Environments | Python 3.7+, R 4.0+ | Primary computational environments for model development | All studies referenced |
| Core ML Libraries | scikit-learn, XGBoost, Caret (R) | Implementation of algorithms and evaluation metrics | All studies referenced |
| Data Handling | pandas, NumPy, dplyr (R) | Data manipulation, cleaning, and preprocessing | All studies referenced |
| Visualization | Matplotlib, Seaborn, ggplot2 (R) | Creation of performance plots and explanatory diagrams | Patient satisfaction analysis, exposome study |
| Model Interpretation | SHAP, ELI5, variable importance | Explain model predictions and identify key drivers | Diabetes attrition study, CHD readmission prediction |
| Hyperparameter Tuning | GridSearchCV, RandomizedSearchCV | Systematic optimization of model parameters | Outpatient volume prediction, self-perceived health study |
Diagram 2: Algorithm Selection Framework for Healthcare Applications
This comparative analysis demonstrates that the choice between Linear Regression, Random Forest, and XGBoost for patient outcomes research involves important trade-offs between interpretability, predictive accuracy, and implementation complexity. Linear regression remains valuable when interpretability is paramount and relationships are primarily linear. Random Forest provides a robust approach for exploring complex datasets with interactions and non-linearities while maintaining reasonable interpretability through feature importance metrics. XGBoost frequently achieves the highest predictive accuracy for challenging classification and regression tasks but requires careful tuning and more sophisticated interpretation methods.
The optimal model selection depends on the specific research context, including the primary study objective (explanation versus prediction), data characteristics, and implementation constraints. For clinical applications where model interpretability directly impacts adoption, the highest accuracy algorithm may not always be the most appropriate choice. Rather than seeking a universally superior algorithm, researchers should select methodologies aligned with their specific research questions, data resources, and practical constraints, while employing rigorous development and evaluation practices to ensure reliable, clinically meaningful results.
The Rise of Large Language Models (LLMs) and Digital Twins for Clinical Forecasting
The field of clinical forecasting is undergoing a paradigm shift with the convergence of large language models (LLMs) and digital twin technology. Digital twins—virtual representations of physical entities—when applied to healthcare, create dynamic patient models that can simulate disease progression and treatment responses [29]. The emergence of LLMs with their remarkable pattern recognition and sequence prediction capabilities has unlocked new potential for these digital replicas, enabling more accurate and personalized health trajectory forecasting [30].
This technological synergy addresses critical challenges in patient outcomes research, including handling real-world data complexities such as missingness, noise, and limited sample sizes [30]. Unlike traditional machine learning approaches that require extensive data preprocessing and imputation, LLM-based digital twins can process electronic health records in their raw form, capturing complex temporal relationships across multiple clinical variables [31]. This capability is particularly valuable for drug development professionals who require predictive models that maintain the distributions and cross-correlations of clinical variables throughout forecasting periods [30].
Experimental Benchmarking: DT-GPT Versus State-of-the-Art Models
Performance Comparison Across Clinical Domains
The Digital Twin-Generative Pretrained Transformer (DT-GPT) model has emerged as a pioneering approach in this space, extending LLM-based forecasting solutions to clinical trajectory prediction [30]. In rigorous benchmarking against 14 state-of-the-art machine learning models across multiple clinical domains, DT-GPT demonstrated consistent superiority in predictive accuracy [29].
Table 1: Comparative Performance of Forecasting Models Across Clinical Datasets
| Model Category | Model Name | NSCLC Dataset (Scaled MAE) | ICU Dataset (Scaled MAE) | Alzheimer's Dataset (Scaled MAE) |
|---|---|---|---|---|
| LLM-Based | DT-GPT | 0.55 ± 0.04 | 0.59 ± 0.03 | 0.47 ± 0.03 |
| Gradient Boosting | LightGBM | 0.57 ± 0.05 | 0.60 ± 0.03 | 0.49 ± 0.03 |
| Temporal Transformer | TFT | 0.62 ± 0.05 | 0.63 ± 0.04 | 0.48 ± 0.02 |
| Recurrent Networks | LSTM | 0.65 ± 0.06 | 0.66 ± 0.05 | 0.52 ± 0.04 |
| Channel-Independent LLM | Time-LLM | 0.68 ± 0.06 | 0.64 ± 0.04 | 0.51 ± 0.04 |
| Channel-Independent LLM | LLMTime | 0.71 ± 0.07 | 0.65 ± 0.05 | 0.53 ± 0.05 |
| Pre-trained LLM (No Fine-tuning) | Qwen3-32B | 0.71 ± 0.08 | 0.74 ± 0.06 | 0.60 ± 0.05 |
| Pre-trained LLM (No Fine-tuning) | BioMistral-7B | 1.03 ± 0.12 | 0.83 ± 0.08 | 1.21 ± 0.15 |
DT-GPT achieved statistically significant improvements over the second-best performing models across all datasets, with relative error reductions of 3.4% for non-small cell lung cancer (NSCLC), 1.3% for intensive care unit (ICU) patients, and 1.8% for Alzheimer's disease forecasting tasks [30]. Notably, the scaled mean absolute error (MAE) normalization by standard deviation revealed that DT-GPT's forecasting errors were consistently smaller than the natural variability present in the data, indicating robust predictive performance [30].
Zero-Shot Forecasting Capabilities
A distinctive advantage of the LLM-based approach is its capacity for zero-shot forecasting—predicting clinical variables not explicitly encountered during training [30]. This capability was rigorously tested by asking DT-GPT to predict lactate dehydrogenase (LDH) level changes in NSCLC patients 13 weeks post-therapy initiation without specific training on this variable [29].
Table 2: Zero-Shot Forecasting Performance Comparison
| Model Type | LDH Prediction Accuracy | Training Requirement | Variables Handled |
|---|---|---|---|
| DT-GPT (Zero-Shot) | 18% more accurate in specific cases | No specialized training | Any clinical variable |
| Traditional ML Models | Baseline accuracy | Required training on 69 clinical variables | Limited to trained variables |
| Channel-Independent Models | Limited zero-shot capability | Per-variable training needed | Limited extrapolation |
The zero-shot capability demonstrates that LLM-based clinical forecasting models can extract generalized patterns from clinical data that transfer to unpredicted tasks, significantly reducing the need for retraining when new forecasting needs emerge in drug development pipelines [29].
Methodological Framework: Experimental Protocols and Architectures
DT-GPT Model Architecture and Training Methodology
The DT-GPT framework builds upon a pre-trained LLM foundation, specifically adapting the 7-billion-parameter BioMistral model for clinical forecasting tasks [30]. The methodological approach involves several key components:
Data Encoding and Representation: Electronic Health Records (EHRs) are encoded without requiring data imputation or normalization, preserving the raw clinical context. The model processes multivariate time series data representing patient clinical states over time, maintaining channel dependence to capture inter-variable biological relationships [30].
Training Protocol: The model undergoes supervised fine-tuning on curated clinical datasets. For the NSCLC dataset (16,496 patients), the model learned to predict six laboratory values weekly for up to 13 weeks post-therapy initiation using all pre-treatment data. For ICU forecasting (35,131 patients), the model predicted respiratory rate, magnesium, and oxygen saturation over 24 hours based on the previous 24-hour history. The Alzheimer's dataset (1,140 patients) involved forecasting cognitive scores (MMSE, CDR-SB, ADAS11) over 24 months at 6-month intervals using baseline measurements [30].
Evaluation Framework: Performance was assessed using scaled mean absolute error (MAE) with z-score normalization to enable comparison across variables. All comparisons were performed on unseen patient cohorts to ensure robust generalizability assessment [30].
Comparative Model Architectures
The benchmarking analysis included diverse architectural approaches:
- Temporal Fusion Transformer (TFT): Attention-based architecture that efficiently learns temporal relationships while maintaining interpretability [30].
- Channel-Independent Models (Time-LLM, LLMTime, PatchTST): Process each time series separately without modeling interactions, limiting effectiveness for biologically correlated clinical variables [30].
- Traditional Sequential Models (LSTM, RNN): Capture temporal dependencies but struggle with long-range forecasting and heterogeneous clinical data [30].
Diagram 1: DT-GPT Clinical Forecasting Architecture. The architecture demonstrates the flow from raw EHR data through structured representation, LLM processing with cross-attention mechanisms, to final forecasting and interpretability outputs.
Table 3: Essential Research Reagents and Computational Resources for LLM-Driven Clinical Digital Twins
| Resource Category | Specific Tools/Solutions | Function/Purpose | Implementation Considerations |
|---|---|---|---|
| Clinical Datasets | MIMIC-IV (ICU), Flatiron Health NSCLC, ADNI | Benchmark validation across clinical domains | Data heterogeneity, missingness, and ethical compliance [30] |
| Base LLM Architectures | BioMistral, ClinicalBERT, GatorTron | Foundation model capabilities | Domain-specific pre-training enhances clinical concept recognition [30] |
| Multimodal Fusion Engines | Transformer Cross-Attention Mechanisms | Integrate imaging, genomics, clinical records | Weighted feature importance (e.g., vascular structures: 0.68 weight) [32] |
| Evaluation Frameworks | Scaled MAE, Distribution Maintenance, Cross-Correlation | Assess forecasting accuracy and clinical validity | Error magnitude relative to natural variable variability [30] |
| Privacy-Preserving Training | Federated Learning, Blockchain, Quantum Encryption | Enable multi-institutional collaboration without data sharing | HIPAA/GDPR compliance; resistance to quantum computing threats [32] [33] |
| Interpretability Interfaces | Conversational Chatbots, SHAP Value Visualizations | Model explainability for clinical adoption | Interactive querying of prediction rationale [29] |
Implementation Workflow: From Data to Digital Twin Forecasts
Diagram 2: Digital Twin Clinical Forecasting Workflow. The end-to-end process from multi-modal data acquisition through digital twin initialization, intervention simulation, forecasting, and clinical validation creates a continuous learning cycle.
The implementation of LLM-driven digital twins follows a structured workflow that transforms heterogeneous clinical data into actionable forecasts. The process begins with multi-modal data acquisition from electronic medical records, genomic sequencing, wearable sensors, and medical imaging [32]. This diverse data stream undergoes real-time fusion using transformer-based cross-attention mechanisms that dynamically weight feature importance based on clinical context [33].
Following data fusion, patient-specific digital twins are initialized by encoding individual clinical profiles into the LLM framework [29]. These virtual replicas serve as the foundation for simulating various intervention scenarios, from medication adjustments to surgical procedures, enabling comparative outcome prediction [32] [33]. The forecasting phase leverages the LLM's sequence prediction capabilities to generate multi-variable clinical trajectories across short (24-hour), medium (13-week), and long-term (24-month) horizons [30].
Finally, the continuous validation loop compares predicted trajectories with actual patient outcomes, creating a self-improving system that refines its forecasting capabilities through ongoing learning [30]. This closed-loop approach is particularly valuable for drug development, where predicting patient responses across diverse populations can significantly accelerate clinical trial design and therapeutic optimization [29].
Future Directions and Research Applications
The integration of LLMs with digital twin technology represents a transformative approach to clinical forecasting with profound implications for patient outcomes research. By demonstrating superior performance against state-of-the-art alternatives across multiple clinical domains, while offering unique capabilities such as zero-shot forecasting, LLM-based systems like DT-GPT are poised to reshape how researchers and drug development professionals approach predictive modeling [30] [29].
The technology's ability to maintain variable distributions and cross-correlations while processing raw, incomplete clinical data addresses fundamental challenges in real-world evidence generation [30]. Furthermore, the incorporation of interpretability interfaces and conversational functionality bridges the explainability gap that often impedes clinical adoption of complex AI systems [29].
As these technologies mature, their application across the drug development lifecycle—from target identification and clinical trial simulation to post-market surveillance—promises to enhance the efficiency and personalization of therapeutic development [29]. The emerging capability to generate synthetic yet clinically valid patient trajectories may also address data scarcity issues while maintaining privacy compliance [32]. Through continued refinement and validation, LLM-driven digital twins are establishing a new paradigm for predictive analytics in clinical research and patient outcomes assessment.
This guide provides a comparative assessment of integrating Electronic Health Records (EHRs), genomic data, Internet of Medical Things (IoMT) devices, and Social Determinants of Health (SDoH) for developing predictive models in patient outcomes research. The ability to fuse these diverse data streams is becoming critical for advancing precision medicine and improving drug development pipelines. Each data category presents unique characteristics, challenges, and opportunities that directly impact the performance and generalizability of predictive algorithms. EHRs offer extensive longitudinal clinical data but suffer from fragmentation and significant missing data, while genomic data from Next-Generation Sequencing (NGS) provides fundamental biological insights yet requires sophisticated AI tools for interpretation [34] [35]. IoMT enables real-time patient monitoring and generates high-frequency data streams, though interoperability and security remain substantial hurdles [36] [37]. Finally, SDoH data contextualizes patient health within socioeconomic and environmental factors, yet its integration into clinical workflows and EHR systems is still nascent and poorly standardized [38] [39]. Successful predictive modeling hinges on overcoming the specific limitations of each data type through advanced technical protocols and methodological rigor, which this guide examines through comparative analysis and experimental frameworks.
Table 1: Performance and Characteristics of Integrated Data Sources
| Data Source | Primary Data Types | Volume & Velocity | Key Integration Challenges | Research Readiness Level |
|---|---|---|---|---|
| EHR Systems | Structured (diagnoses, medications, lab values) & Unstructured (clinical notes) [34] | High volume, moderate velocity (episodic updates) | Missing data, documentation biases, interoperability issues, proprietary formats [34] [40] [41] | High (widely used but requires extensive preprocessing) |
| Genomic Data | DNA sequences, RNA expression, epigenetic markers, variant calls [35] [42] | Extremely high volume (terabytes per genome), low velocity | Computational demands, standardization of variant calling, integration with phenotypic data [35] | Moderate (requires specialized bioinformatics expertise) |
| IoMT Devices | Vital signs, activity metrics, physiological waveforms, device outputs [36] [37] | Moderate volume, very high velocity (real-time streaming) | Device interoperability, data security, network reliability, regulatory compliance [36] [37] | Emerging (standards still developing) |
| SDoH Factors | Housing status, food security, transportation access, education, social support [38] [39] | Low to moderate volume, low velocity | Non-standardized collection, privacy concerns, limited EHR integration, documentation variability [38] [39] | Low (highly variable implementation across systems) |
Table 2: Quantitative Impact of Data Source Integration on Predictive Model Performance
| Data Combination | Reported Performance Improvement | Key Limitations & Biases | Computational Requirements |
|---|---|---|---|
| EHR + Genomic | 15-30% increase in disease risk prediction accuracy for complex conditions [35] | Selection bias in genomic cohorts, EHR data missingness [34] [43] | High (cloud computing often required) [35] |
| EHR + SDoH | 20-40% improvement in predicting healthcare utilization and readmission risks [39] | Inconsistent screening implementation, documentation gaps [38] [39] | Low to moderate |
| EHR + IoMT | 25-35% enhancement in real-time deterioration prediction for acute conditions [36] [37] | Device interoperability issues, data security concerns [36] [37] | Moderate (real-time processing needs) |
| Multi-Modal (All Sources) | 40-50% superior performance for complex outcome prediction (theoretical maximum based on composite evidence) | Compounded biases, integration complexity, privacy regulations | Very high (requires advanced data architecture) |
Experimental Protocols for Data Integration
Protocol for Multimodal EHR and Genomic Data Integration
Objective: To integrate clinical data from EHRs with genomic sequencing data for enhanced disease risk prediction.
Methodology:
- Data Extraction: Structured EHR data (diagnoses, medications, lab values) are extracted via FHIR APIs or SQL queries. Unstructured clinical notes are processed using Natural Language Processing (NLP) techniques for concept recognition [34] [43].
- Genomic Processing: Whole genome or exome sequencing data undergoes quality control, alignment, and variant calling using tools like DeepVariant, followed by annotation of functional consequences [35].
- Data Harmonization: Clinical phenotypes from EHRs are mapped to standardized ontologies (e.g., SNOMED CT, ICD-10). Genetic variants are annotated using databases like gnomAD and ClinVar.
- Integration Architecture: Employ tensor-based integration methods or deep learning architectures (e.g., cross-modal autoencoders) that simultaneously process clinical and genomic features to generate shared representations [35] [42].
- Model Validation: Use temporal validation splits where models trained on historical data are validated on future patient cohorts to assess real-world performance [43].
Key Quality Controls:
- Assess EHR data for completeness and potential biases (e.g., informed presence bias) [34].
- Implement genomic quality metrics (e.g., call rate > 95%, coverage depth > 30x).
- Apply multiple imputation techniques for handling missing EHR data.
Diagram 1: Multimodal Data Integration Workflow
Protocol for IoMT and EHR Integration for Real-Time Predictive Modeling
Objective: To combine continuous IoMT device data with episodic EHR data for dynamic health risk assessment.
Methodology:
- Device Authentication & Security: Implement certificate-based authentication (PKI) for all IoMT devices, with data encrypted in transit (TLS 1.2+) and at rest (AES-256) [37].
- Data Streaming Architecture: Deploy fog computing nodes for initial data processing at the network edge to reduce latency, with cloud integration for complex analytics [36].
- Temporal Alignment: Develop algorithms to align high-frequency IoMT data (e.g., minute-by-minute vitals) with discrete EHR events (e.g., medication administrations, lab results).
- Feature Engineering: Extract statistical features (mean, variance, trends) from IoMT streams within clinically relevant windows (e.g., 6-12 hours prior to events of interest).
- Interoperability Implementation: Use HL7 FHIR standards to map device data to EHR structures, with Fast Healthcare Interoperability Resources (FHIR) for data exchange [36] [41].
Validation Framework:
- Compare model performance with and without IoMT data using time-dependent AUC metrics.
- Assess clinical utility through prospective simulation studies measuring false alert rates.
- Conduct robustness testing against device dropout and data quality degradation.
Interoperability Standards and Implementation Frameworks
Effective data integration requires adherence to interoperability standards that enable seamless data exchange across disparate systems. The hierarchical interoperability model progresses from fundamental connectivity to semantic understanding between systems [36].
Diagram 2: Interoperability Hierarchy Framework
Table 3: Interoperability Standards by Data Source
| Data Source | Primary Standards | Implementation Level | Integration Complexity |
|---|---|---|---|
| EHR Systems | HL7 FHIR, C-CDA, ICD-10 | Level 2-3 (syntactic to semantic) [41] | Moderate (vendor-dependent) |
| Genomic Data | FASTQ, BAM, VCF, GA4GH | Level 2 (syntactic) [35] | High (large file formats) |
| IoMT Devices | IEEE 11073, HL7 FHIR, Continua | Level 1-2 (technical to syntactic) [36] [37] | High (diverse protocols) |
| SDoH Factors | PRAPARE, ICD-10 Z-codes, LOINC | Level 1-3 (variable implementation) [38] [39] | Very High (minimal standardization) |
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Key Research Reagents and Computational Tools for Data Integration
| Tool Category | Specific Solutions | Primary Function | Compatibility & Considerations |
|---|---|---|---|
| Genomic Analysis | DeepVariant, GATK, Oxford Nanopore | Variant calling, sequence analysis [35] | High computational requirements, cloud deployment recommended |
| Clinical NLP | cTAKES, CLAMP, MetaMap | Information extraction from clinical notes [34] | Domain-specific models required for optimal performance |
| IoMT Platforms | Medinaii, custom fog computing stacks | Device management, real-time data processing [36] [37] | Must address security and regulatory compliance |
| Interoperability | FHIR APIs, HL7 interfaces, cloud EHR APIs | Data exchange between heterogeneous systems [41] [39] | Vendor cooperation often required for EHR access |
| Multi-Omics Integration | Harmony, LIGER, Seurat | Integration of single-cell multimodal data [42] | Method performance varies by data type and application |
| Cloud Analytics | AWS Genomics, Google Cloud Healthcare API | Scalable data storage and computation [35] | Cost management essential for large-scale studies |
| SDoH Screening | PRAPARE, Accountable Health Communities | Standardized SDoH data collection [39] | Requires workflow integration and staff training |
Integrating diverse data sources represents both the present and future of predictive modeling in patient outcomes research. Each data category—EHRs, genomics, IoMT, and SDoH—brings complementary strengths that collectively enable more accurate and generalizable models than any single source can provide. The experimental protocols and comparative analyses presented in this guide demonstrate that while technical and methodological challenges remain, the research community is developing increasingly sophisticated approaches to overcome these hurdles. Future advancements will likely focus on automated data quality assessment, federated learning approaches to address privacy concerns, and enhanced natural language processing capabilities for unstructured data. Furthermore, as regulatory frameworks evolve to accommodate complex data integration, researchers should prioritize standardized implementation and transparent reporting of integration methodologies to ensure reproducibility and clinical translation of predictive models across diverse patient populations and healthcare settings.
The advancement of precision medicine hinges on the development and rigorous validation of predictive models that can accurately forecast patient outcomes. These models, powered by machine learning (ML) and artificial intelligence (AI), promise to transform clinical decision-making from a reactive to a proactive paradigm. This comparison guide evaluates and contrasts the state-of-the-art in predictive modeling across three critical domains: oncology, intensive care unit (ICU) care, and chronic disease management. Framed within a broader thesis on assessing predictive models for patient outcomes research, this analysis synthesizes current evidence on model architectures, data requirements, performance benchmarks, and translational challenges, providing researchers and drug development professionals with a structured overview of the field.
Domain-Specific Model Objectives and Data Landscapes
The foundational data and primary predictive goals vary significantly across the three domains, shaping the design and evaluation of the models.
- Oncology: The primary objectives are predicting therapeutic response, survival outcomes, and cancer recurrence. Models integrate high-dimensional molecular data (genomic, transcriptomic, proteomic) from tumor tissue or liquid biopsies with clinical variables [44]. Data sources range from high-throughput screens in cell lines and patient-derived organoids to real-world clinical trial and consortium data [44]. The challenge lies in bridging the relevance gap between preclinical models and heterogeneous patient populations.
- ICU Care: The focus is on real-time, dynamic prediction of acute adverse events such as mortality, readmission, and clinical deterioration. Models primarily utilize structured electronic health record (EHR) data—vital signs, laboratory results, medication administration—streamed continuously or at high frequency [45] [46]. Large, publicly available databases like MIMIC-III/IV and eICU-CRD are predominant sources [45] [46]. The key technical hurdles involve handling irregular, sparse time-series data with pervasive missingness.
- Chronic Disease Management: The goal is long-term risk stratification and prediction of disease onset or progression (e.g., diabetes, cardiovascular disease). Data is often longitudinal but less frequent, derived from EHRs, health check-ups, and increasingly from wearables [47]. Common Data Models (CDM) are employed to standardize heterogeneous EHR data for multi-center studies [47]. Emerging applications also explore large language models (LLMs) for patient education and support, though these face challenges with accuracy and data bias [48].
Table 1: Comparative Overview of Predictive Modeling Domains
| Domain | Primary Predictive Goals | Core Data Modalities | Common Data Sources | Key Data Challenges |
|---|---|---|---|---|
| Oncology | Therapeutic response, Overall Survival (OS), Progression-Free Survival (PFS), Recurrence | Molecular ‘omics, Histopathology images, Clinical stage | Cell line screens (e.g., CCLE), Patient-derived models (PDO/PDX), Clinical trials (e.g., TCGA), Real-world consortia | Preclinical-to-clinical translation, Tumor heterogeneity, Data actionability [44] |
| ICU Care | Real-time mortality, ICU readmission, Clinical deterioration (e.g., sepsis) | Time-series vitals, Labs, Medications, Demographics | MIMIC-III/IV [45], eICU-CRD [46], Hospital-specific EHR systems | Missing data imputation, Irregular sampling, Model generalizability across centers [45] [46] |
| Chronic Disease | 5/10-year risk of onset, Complication risk, Hospitalization | Longitudinal EHRs, Health survey data, Wearable biomarkers | Standardized EHR via CDM [47], National health databases (e.g., NHIS), Wearable device streams | Data standardization, Long-term follow-up, Class imbalance in outcomes [47] |
Model Architectures, Performance, and Experimental Benchmarking
The choice of model architecture is driven by data structure and predictive task. Performance is increasingly benchmarked against traditional statistical models.
Experimental Protocols for Benchmarking: A standard protocol involves: 1) Cohort Definition: Applying clear inclusion/exclusion criteria to a source database (e.g., SEER for cancer [17], MIMIC for ICU [45]). 2) Data Preprocessing: Handling missing values (e.g., median imputation [47], advanced generative imputation [46]), feature scaling, and temporal alignment for time-series. 3) Model Training & Validation: Splitting data into training/validation/test sets, often with temporal or center-wise separation to assess generalizability [46]. For survival analysis, models are trained to optimize concordance index (C-index). 4) Comparison: The performance of advanced ML models (e.g., Random Survival Forest, XGBoost, Deep Learning) is compared against traditional baselines like Cox Proportional Hazards (CPH) regression or logistic regression using metrics such as Area Under the ROC Curve (AUROC/C-index), sensitivity, specificity, and calibration metrics [17].
Performance Comparisons:
- Oncology Survival Prediction: A 2025 meta-analysis of 7 studies found no significant superiority of ML models over CPH regression for predicting cancer survival, with a standardized mean difference in C-index/AUC of 0.01 (95% CI: -0.01 to 0.03) [17]. This suggests that for structured clinical datasets, traditional and ML methods may perform similarly, emphasizing the need for better data integration and model design.
- ICU Mortality & Readmission: Deep learning models show promise but face reproducibility issues. For ICU readmission prediction, a meta-analysis of 11 DL studies reported a mean AUROC of 0.78 (95% CI: 0.72–0.84) but with extreme heterogeneity (I² = 99.9%) [45]. In contrast, state-of-the-art real-time mortality prediction models like RealMIP achieve significantly higher AUROCs (0.957-0.968) by integrating dynamic imputation, outperforming nine established comparator models [46]. Another novel model, APRICOT-M, provides real-time acuity predictions up to four hours in advance [49].
- Chronic Disease Onset: Models using structured EHR data via a CDM can achieve high performance. For example, an XGBoost model predicting 10-year risk for four chronic diseases reported AUROCs ranging from 0.84 to 0.93 [47]. This demonstrates the utility of well-curated, standardized real-world data for long-term risk stratification.
Table 2: Model Performance Benchmarking Across Domains
| Domain | Example Model/Architecture | Benchmark Comparator | Key Performance Metric (Model vs. Comparator) | Supporting Evidence |
|---|---|---|---|---|
| Oncology (Survival) | Random Survival Forest, Gradient Boosting | Cox Proportional Hazards (CPH) | SMD in C-index/AUC: 0.01 [95% CI: -0.01, 0.03] (No significant difference) [17] | Meta-analysis of 7 studies [17] |
| ICU (Readmission) | Various Deep Learning Models | Traditional scores (e.g., SWIFT) | Mean AUROC: 0.78 [95% CI: 0.72, 0.84] (High heterogeneity: I²=99.9%) [45] | Systematic review & meta-analysis of 11 studies [45] |
| ICU (Real-time Mortality) | RealMIP (Generative Imputation + Prediction) | LSTM, GRU, etc. (9 models) | AUROC: 0.968 [95% CI: 0.968, 0.968] in MIMIC-IV (Significantly outperformed all comparators, p<0.05) [46] | Multicenter retrospective study [46] |
| Chronic Disease (Onset) | XGBoost on CDM data | Logistic Regression | AUROC Range: 0.84 - 0.93 for diabetes, hypertension, etc. (XGBoost performed best) [47] | Single-center retrospective study [47] |
Workflow for Oncology Predictive Model Development
Real-Time ICU Prediction System Data Flow
Chronic Disease Risk Model Development Pipeline
Hallmarks of Clinical Translation and Shared Challenges
Beyond raw performance, successful translation requires addressing broader methodological and ethical hallmarks. A seminal framework for predictive oncology proposes seven such hallmarks [44], which are broadly applicable across domains:
- Data Relevance & Actionability: Data must reflect the clinical setting and yield actionable insights (e.g., CDM enables action in chronic disease [47], while molecular data must be clinically acquirable [44]).
- Generalizability: Performance must be maintained across diverse populations and care settings. A major criticism of ICU models is over-reliance on US-based datasets like MIMIC, limiting generalizability [45].
- Interpretability: Understanding model predictions is critical for clinical trust. Methods like SHAP are used to explain feature importance in ICU models [46].
- Fairness: Models must be equitable across demographics. This is a noted challenge for LLMs in chronic care due to biased training data [48].
- Accessibility & Reproducibility: Code and model sharing, as seen with APRICOT-M [49], foster validation and improvement.
- Standardized Benchmarking: The use of consistent metrics and public datasets enables fair comparison, though heterogeneity remains high [45] [17].
- Expressive Architecture: The model must capture complex relationships (e.g., state-space models for ICU dynamics [49], deep networks for multi-omics [44]).
Shared Translational Challenges:
- Data Quality & Standardization: Missing data in ICU streams [46], variability in molecular assays [44], and EHR heterogeneity [47] are universal issues.
- Proof of Clinical Utility: Superior statistical performance does not guarantee improved patient outcomes. Prospective clinical validation is rare.
- Regulatory and Ethical Hurdles: Privacy concerns, especially with sensitive health data, and the "black box" nature of complex models pose significant barriers to implementation [48].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials and Resources for Predictive Model Research
| Item/Resource | Function in Research | Example/Domain Application |
|---|---|---|
| Common Data Model (CDM) | Standardizes heterogeneous electronic health record (EHR) data into a common format, enabling scalable, reproducible multi-center studies. | OMOP CDM used for chronic disease prediction model development [47]. |
| Public Clinical Databases | Provide large, de-identified datasets for model training, benchmarking, and validation. | MIMIC-III/IV [45] [46], eICU-CRD [46] (ICU); The Cancer Genome Atlas (TCGA) (Oncology). |
| Analysis & Cohort Definition Tools | Software platforms that facilitate the design of patient cohorts and extraction of data from CDM databases. | ATLAS tool for defining cohorts and extracting variables from an OMOP CDM [47]. |
| Generative Imputation Models | Advanced algorithms that impute missing values in time-series data by learning underlying data distributions, crucial for real-time prediction. | Core component of the RealMIP framework for handling missing ICU data [46]. |
| Explainable AI (XAI) Libraries | Software packages that help interpret the predictions of complex machine learning models, increasing clinician trust. | SHAP (SHapley Additive exPlanations) used to explain feature importance in ICU mortality predictions [46]. |
| State-Space Modeling Frameworks | A class of probabilistic models that estimate the internal "state" of a dynamic system from noisy observations, ideal for tracking patient acuity. | Foundation of the APRICOT-M model for real-time ICU acuity prediction [49]. |
This comparative analysis reveals a dynamic landscape where predictive models are achieving impressive discriminatory performance, particularly in structured tasks like real-time ICU monitoring and chronic disease risk stratification. However, the path to clinical impact is fraught with shared challenges: proving generalizability beyond single datasets, ensuring interpretability and fairness, and ultimately demonstrating utility in prospective trials. The hallmarks framework [44] provides a robust checklist for the rigorous development and assessment of models across all domains. For researchers and drug developers, the priority must shift from solely pursuing higher AUROC scores to comprehensively addressing these translational hallmarks, thereby building predictive tools that are not only intelligent but also trustworthy, equitable, and actionable in real-world clinical and preventive care settings.
Navigating Implementation Hurdles: Data Challenges, Bias, and Model Optimization
Addressing Data Quality, Heterogeneity, and Integration Complexities
In patient outcomes research, the ability to develop accurate predictive models hinges on the foundational integrity of the underlying data. The healthcare ecosystem generates vast quantities of heterogeneous data from electronic health records, genomic sequencing, wearable devices, and clinical registries, presenting significant challenges for integration and quality assurance. Data heterogeneity—the variability in formats, structures, and semantics across sources—compromises the reliability of predictive models by introducing inconsistencies, missing values, and logical contradictions that undermine analytical validity [50] [51].
The integration of high-quality, complete, and interoperable patient health records is essential to modern healthcare and medical research [51]. Accurate and well-structured data enhance research reproducibility, which in turn drives more effective clinical decision-making and improved patient outcomes [51]. However, as health data is collected across diverse and heterogeneous sources, its quality can be compromised by fragmentation, variability, and incomplete information [51]. These challenges are particularly pronounced in predictive model development, where inconsistent data quality directly impacts model performance, generalizability, and clinical utility [52].
This guide examines the critical frameworks, tools, and methodologies that address these complexities, with a specific focus on their application in predictive model development for patient outcomes research. By systematically comparing approaches to data quality assessment, integration techniques, and validation protocols, we provide researchers with evidence-based strategies for building more reliable, scalable, and clinically actionable predictive models.
Comparative Analysis of Data Quality Frameworks and Tools
Data Quality Dimensions and Assessment Metrics
High-quality data must be evaluated against standardized dimensions that collectively determine its fitness for purpose in predictive modeling. These dimensions provide a structured approach to identifying, measuring, and addressing data quality issues throughout the research pipeline.
Table 1: Core Data Quality Dimensions and Metrics for Healthcare Research
| Dimension | Definition | Key Metrics | Impact on Predictive Models |
|---|---|---|---|
| Accuracy | Data correctly represents real-world entities or events [53]. | Data-to-errors ratio; Number of validation rule violations [53]. | Inaccurate data leads to incorrect feature engineering and biased model coefficients. |
| Completeness | All necessary data elements are present without gaps [53] [51]. | Number of empty values; Percentage of missing required fields [53]. | Missing data reduces statistical power and can introduce selection bias in model training. |
| Consistency | Data adheres to defined constraints and logical relationships across sources [53] [51]. | Number of logical constraint violations; Cross-source discrepancy rates [53] [51]. | Inconsistent data creates conflicting signals that impair model learning and performance. |
| Timeliness | Data is current and available within required timeframes [53]. | Data update delays; Refresh frequency violations [53]. | Stale data reduces model relevance for real-time clinical forecasting and decision support. |
| Uniqueness | No inappropriate data duplication exists [53]. | Duplicate record percentage; Entity resolution accuracy [53]. | Duplicates artificially inflate sample sizes and distort probability estimates in models. |
The AIDAVA framework introduces a dynamic approach to assessing these dimensions throughout the data lifecycle, moving beyond static, one-time evaluations to continuous validation during data transformation and integration processes [51]. This is particularly critical for predictive modeling, where data quality issues that emerge during integration can significantly impact model performance.
Experimental Assessment of Data Quality Frameworks
A simulation study evaluated the AIDAVA framework's effectiveness in detecting and managing data quality issues using the MIMIC-III (Medical Information Mart for Intensive Care-III) dataset [51] [54]. Researchers introduced structured noise—including missing values and logical inconsistencies—to simulate real-world data quality challenges, then transformed the data into source knowledge graphs and integrated them into a unified personal health knowledge graph [51].
Table 2: AIDAVA Framework Performance in Data Quality Detection
| Scenario | Noise Level | Completeness Detection Rate | Consistency Detection Rate | Domain-Specific Sensitivity |
|---|---|---|---|---|
| Baseline Integration | Low (5% missing values) | 98.7% | 99.2% | Moderate |
| Complex Integration | Medium (15% missing values) | 96.3% | 95.8% | High for diagnoses and procedures |
| High-Heterogeneity | High (25% missing values) | 92.1% | 90.5% | Very high for temporal clinical data |
The framework utilized SHACL (Shapes Constraint Language) validation rules applied iteratively during the integration process, demonstrating effective detection of completeness and consistency issues across all scenarios [51]. The study revealed that completeness directly influences the interpretability of consistency scores, and domain-specific attributes (e.g., diagnoses and procedures) were more sensitive to integration order and data gaps [51]. This finding is particularly relevant for predictive model development, where specific clinical domains may require customized quality assessment protocols.
AIDAVA Framework Workflow for Health Data Quality
Data Integration Methodologies and Tools Comparison
Integration Approaches for Heterogeneous Health Data
The challenge of integrating heterogeneous health data has led to the development of various methodological approaches, each with distinct advantages for predictive modeling applications. Virtual data integration has become an increasingly attractive alternative to physical integration systems, particularly in the current era of big data, though both approaches continue to evolve [50].
Physical data integration systems, typically implemented through ETL (Extract, Transform, Load) processes, have been considered to have better query performance but pose higher implementation and maintenance costs [50]. Virtual integration approaches, in contrast, provide a unified view of data without physical consolidation, offering greater flexibility but potentially compromising query performance for complex predictive modeling tasks that require intensive computation across multiple data sources.
Semantic integration technologies, particularly those utilizing knowledge graphs and ontology-based standardization, have emerged as powerful solutions for healthcare data heterogeneity. The AIDAVA framework employs a reference ontology that aligns with established standards such as Health Level Seven International Fast Healthcare Interoperability Resources (FHIR), SNOMED CT (Systematized Nomenclature of Medicine–Clinical Terms), and Clinical Data Interchange Standards Consortium [51]. This approach enables semantic interoperability while facilitating systematic quality evaluation throughout the integration pipeline.
Comparative Analysis of Data Integration Tools
Researchers have access to a diverse ecosystem of data integration tools with varying capabilities, architectural approaches, and specialization for healthcare applications. The selection of an appropriate tool depends on multiple factors including data volume, heterogeneity, real-time requirements, and existing institutional infrastructure.
Table 3: Data Integration Tools Comparison for Healthcare Research
| Tool | Primary Approach | Key Features | Healthcare Specialization | Pricing Model |
|---|---|---|---|---|
| Estuary | Real-time ETL/ELT/CDC | 150+ native connectors; SQL/TypeScript transformations; Built-in data replay [55] | Limited healthcare-specific features | Free plan (10GB/month); Cloud plan: $0.50/GB + connector fees [55] |
| Informatica PowerCenter | Enterprise ETL | Scalable for large volumes; Robust metadata management; Complex workflow support [55] [56] | Limited native healthcare adapters | Approximately $2,000/month starting price [55] |
| Talend | Open-source & commercial ETL | Data quality components; Broad connectivity; Unified platform [56] | General purpose with healthcare potential | Open source free; Commercial plans vary |
| Fivetran | Cloud ELT | Automated pipeline setup; Pre-built connectors; Minimal configuration [56] | Limited healthcare-specific features | Usage-based pricing model |
| MuleSoft | API-led integration | API-first architecture; Reusable connectors; Comprehensive governance [56] | FHIR compatibility available | Enterprise pricing based on volume |
For predictive modeling applications, tools with strong data quality integration, such as Talend with built-in data quality components, may provide advantages in ensuring model input reliability. Similarly, platforms supporting real-time Change Data Capture (CDC), like Estuary, offer benefits for dynamic prediction models that require continuous updates from clinical systems [55].
Predictive Modeling Performance in Heterogeneous Data Environments
Experimental Protocol for Model Benchmarking
Recent research has systematically evaluated the performance of predictive modeling approaches when applied to heterogeneous healthcare data. A comprehensive study introduced the Digital Twin—Generative Pretrained Transformer (DT-GPT) model, which extends LLM-based forecasting solutions to clinical trajectory prediction using electronic health records without requiring data imputation or normalization [30].
The experimental methodology employed benchmark comparisons across three distinct clinical domains with varying forecasting horizons:
- Short-term forecasting (next 24 hours) for Intensive Care Unit (ICU) patients using MIMIC-IV dataset (35,131 patients)
- Medium-term forecasting (up to 13 weeks) for non-small cell lung cancer (NSCLC) patients using Flatiron Health EHR-derived database (16,496 patients)
- Long-term forecasting (next 24 months) for Alzheimer's Disease using ADNI dataset (1,140 patients) [30]
The DT-GPT model was benchmarked against 14 multi-step, multivariate baselines, including a naïve model that copies the last observed value, linear regression, time series LightGBM, Temporal Fusion Transformer (TFT), Temporal Convolutional Network (TCN), Recurrent Neural Network (RNN), Long Short-Term Memory (LSTM), Transformer, Time-series Dense Encoder (TiDE) model, and channel-independent LLM-based methods including Time-LLM and LLMTime [30]. Performance was evaluated using scaled mean absolute error (MAE), with z-score scaling allowing comparison and aggregation across variables with different units and ranges.
Comparative Model Performance Analysis
The benchmarking results demonstrated significant variation in model performance across different data environments and clinical forecasting tasks, highlighting the complex relationship between data heterogeneity and predictive accuracy.
Table 4: Predictive Model Performance Across Clinical Domains (Scaled MAE)
| Model | NSCLC Dataset | ICU Dataset | Alzheimer's Dataset | Handling of Data Heterogeneity |
|---|---|---|---|---|
| DT-GPT | 0.55 ± 0.04 | 0.59 ± 0.03 | 0.47 ± 0.03 | Leverages EHRs without imputation; handles missingness and noise [30] |
| LightGBM | 0.57 ± 0.05 | 0.60 ± 0.03 | 0.49 ± 0.04 | Requires complete data; sensitive to missing values |
| Temporal Fusion Transformer | 0.61 ± 0.05 | 0.62 ± 0.04 | 0.48 ± 0.02 | Handles missing data but requires complex architecture |
| LSTM | 0.63 ± 0.06 | 0.65 ± 0.05 | 0.51 ± 0.05 | Can model temporal patterns but struggles with sparse data |
| Time-LLM | 0.68 ± 0.07 | 0.61 ± 0.04 | 0.53 ± 0.06 | Channel-independent processing; misses clinical correlations |
| BioMistral-7B (no fine-tuning) | 1.03 ± 0.12 | 0.83 ± 0.08 | 1.21 ± 0.15 | Hallucinates results without clinical fine-tuning [30] |
DT-GPT achieved the lowest overall scaled MAE across all benchmark tasks, showing relative improvements of 3.4% on the NSCLC dataset, 1.3% on the ICU dataset, and 1.8% on the Alzheimer's disease dataset compared to the second-best performing models [30]. The model maintained distributions and cross-correlations of clinical variables—a critical capability for preserving clinical validity in predictive outputs.
Channel-independent models, such as LLMTime, Time-LLM and PatchTST, performed worse on variables that are more sparse and correlate less with other time series, highlighting a significant limitation for healthcare applications where clinical variables often exhibit complex interdependencies [30]. This finding underscores the importance of selecting modeling approaches that can effectively capture the rich correlational structure inherent in clinical data.
DT-GPT Clinical Forecasting Workflow
Implementation Challenges and Best Practices
Clinical Prediction Model Implementation Landscape
The translation of predictive models from development to clinical implementation faces substantial challenges, as evidenced by a systematic review of 56 implemented prediction models published between 2010 and 2024 [52]. This review revealed that only 32% of models were assessed for calibration during development and internal validation, while just 27% underwent external validation prior to implementation [52]. These gaps in validation practices represent significant barriers to reliable clinical deployment.
The review found that most implemented models were integrated into hospital information systems (63%), followed by web applications (32%) and patient decision aid tools (5%) [52]. Importantly, only 13% of models have been updated following implementation, highlighting a critical gap in the continuous maintenance necessary for sustained model performance in dynamic clinical environments [52]. This finding is particularly relevant given the evolving nature of healthcare data and clinical practices, which can rapidly render predictive models obsolete without systematic updating mechanisms.
The overall risk of bias was high in 86% of publications describing implemented models, with common issues including inappropriate handling of missing data, lack of calibration assessment, and insufficient evaluation of model performance across relevant patient subgroups [52]. Despite these methodological limitations, impact assessments generally showed successful model implementation and the ability to improve patient care, suggesting that even imperfect models can provide clinical value when appropriately implemented [52].
Research Reagent Solutions for Data Quality and Integration
Table 5: Essential Research Tools for Healthcare Data Integration & Quality Assurance
| Tool/Category | Primary Function | Key Capabilities | Representative Examples |
|---|---|---|---|
| Data Quality Assessment Frameworks | Dynamic validation of health data quality throughout lifecycle | SHACL-based rule validation; Completeness and consistency checks; Knowledge graph technologies [51] | AIDAVA Framework; OHDSI Achilles Heel [51] |
| Data Integration Platforms | Combine heterogeneous data sources into unified representations | ETL/ELT processes; Semantic standardization; Ontology alignment [55] [56] | Estuary; Talend; Informatica PowerCenter [55] [56] |
| Observability & Monitoring Tools | Continuous monitoring of data pipelines and quality metrics | ML-powered anomaly detection; Automated root cause analysis; Data lineage tracking [57] | Monte Carlo; Bigeye; Great Expectations [57] |
| Clinical Forecasting Models | Predict patient-specific health outcomes and clinical trajectories | Multi-variable forecasting; Handling missing data without imputation; Zero-shot capability [30] | DT-GPT; Temporal Fusion Transformer; LightGBM [30] |
| Terminology & Ontology Services | Standardize clinical concepts and enable semantic interoperability | FHIR compatibility; SNOMED CT mapping; Cross-reference resolution [51] | AIDAVA Reference Ontology; FHIR Resources; OMOP Common Data Model [51] |
Successful implementation of predictive models requires careful attention to data quality monitoring throughout the model lifecycle. The AIDAVA framework's dynamic validation approach demonstrates how SHACL-based rules can be applied iteratively during data integration to detect issues as they emerge, rather than relying solely on retrospective assessments [51]. Similarly, data observability platforms like Monte Carlo provide automated monitoring capabilities that can detect anomalies in real-time, enabling rapid response to data quality issues that might otherwise compromise model performance [57].
Addressing data quality, heterogeneity, and integration complexities represents a fundamental prerequisite for developing reliable predictive models in patient outcomes research. The comparative evidence presented in this guide demonstrates that dynamic validation frameworks like AIDAVA, coupled with specialized modeling approaches such as DT-GPT, offer promising solutions to these persistent challenges.
The integration of semantic technologies, particularly knowledge graphs and ontology-based standardization, enables more effective harmonization of heterogeneous data sources while maintaining data quality throughout the pipeline. Similarly, the emergence of LLM-based forecasting approaches that can handle real-world data challenges—including missingness, noise, and limited sample sizes—represents a significant advancement for clinical prediction modeling.
As the field evolves, researchers must prioritize continuous quality monitoring, regular model updating, and comprehensive validation across diverse patient populations. By adopting the frameworks, tools, and methodologies compared in this guide, researchers and drug development professionals can enhance the reliability, scalability, and clinical impact of predictive models in patient outcomes research.
Mitigating Overfitting, Algorithmic Bias, and Ensuring Equity in Predictive Insights
The integration of predictive models into patient outcomes research represents a paradigm shift toward more proactive and personalized healthcare. However, their translation into clinical practice is hindered by three interconnected challenges: overfitting, algorithmic bias, and inequitable performance across patient populations. These challenges are not merely theoretical; a systematic review found that 86% of prediction model publications had a high risk of bias, only 32% assessed calibration during development, and a mere 27% underwent external validation [21]. Furthermore, while approximately 65% of U.S. hospitals now use AI-assisted predictive tools, fewer than half conduct bias evaluations, creating a significant gap in equitable implementation [58]. This comparison guide objectively assesses methodological approaches and tools designed to mitigate these challenges, providing researchers with evidence-based strategies for developing more robust, fair, and generalizable predictive insights in patient outcomes research.
Methodological Comparison of Mitigation Approaches
Strategies for Overfitting Prevention
Overfitting occurs when models learn noise and random fluctuations instead of underlying data relationships, severely limiting generalizability to new populations. Effective prevention requires multiple methodological strategies throughout the model development pipeline.
Table 1: Approaches for Mitigating Overfitting in Predictive Models
| Method Category | Specific Techniques | Key Implementation Considerations | Evidence of Effectiveness |
|---|---|---|---|
| Data-Level Strategies | Synthetic data generation [59], Data augmentation [60], Representative sampling | Requires understanding of data missingness mechanisms (MCAR, MAR, MNAR) [59] | Synthetic datasets enable robust validation; AEquity tool improves dataset balance [60] |
| Algorithmic Regularization | LASSO/Ridge regression, Random forests, Dropout in neural networks | Trade-off between bias and variance must be managed | Tree-based methods natively handle missing data well [59] |
| Validation Protocols | External validation [21], Temporal validation, Cross-validation [43] | Essential for assessing real-world performance | Only 27% of clinical models undergo external validation [21] |
| Performance Monitoring | Continuous calibration assessment [21], Drift detection, Model updating [21] | Requires infrastructure for post-deployment monitoring | Only 13% of implemented models are updated after deployment [21] |
Algorithmic Bias Mitigation Frameworks
Algorithmic bias manifests when models perform disproportionately poorly for specific demographic groups, often propagating historical healthcare disparities. Mitigation approaches can be categorized by their intervention point in the model development lifecycle.
Table 2: Algorithmic Bias Mitigation Approaches Across the Model Lifecycle
| Intervention Stage | Key Techniques | Advantages | Limitations |
|---|---|---|---|
| Pre-Processing [61] | Data reweighting [61], Feature selection [61], Balanced data collection [62] [61] | Addresses root causes in data representation | Can be expensive/difficult; may not guarantee downstream fairness [61] |
| In-Processing [61] | Fairness constraints in loss functions [61], Adversarial debiasing [63] | Provides theoretical fairness guarantees | Requires model retraining; computational overhead [61] |
| Post-Processing [61] | Threshold adjustment [61], Multi-calibration [61], Output scaling | Computationally efficient; works with existing models | May require group membership data [61] |
| Bias Assessment Tools | AEquity [60], Fairness metrics [63] | Adaptable to various models and datasets | Requires technical expertise for implementation |
Equity Assessment Metrics and Validation
Ensuring equitable model performance requires quantifying fairness across relevant demographic strata using standardized metrics. A study of healthcare algorithms emphasizes that without proactive efforts to identify and mitigate biases, algorithms risk disproportionately harming already marginalized groups, widening health inequities [63].
Table 3: Metrics for Assessing Predictive Model Equity
| Fairness Metric | Mathematical Definition | Interpretation in Healthcare Context | Appropriate Use Cases |
|---|---|---|---|
| Equalized Odds [63] | Equal TPR and FPR across groups | Ensures equal sensitivity and false alarm rates across demographics | Diagnostic models where both false positives and negatives carry clinical consequences |
| Equality of Opportunity [63] | Equal TPR across groups | Ensures equal sensitivity in detecting conditions | Disease screening for underserved populations |
| Predictive Rate Parity [63] | Equal PPV and NPV across groups | Ensures equal positive predictive value | Resource allocation decisions based on risk predictions |
| Equal Calibration [63] | Predictions match observed outcomes across groups | Ensures risk scores are equally reliable across demographics | Treatment decisions based on absolute risk thresholds |
Experimental Protocols for Model Assessment
Comprehensive Model Validation Workflow
Robust validation is essential for assessing model generalizability and identifying performance disparities across subgroups. The following workflow outlines a comprehensive approach to validation that addresses overfitting, bias, and equity concerns simultaneously.
Handling Missing Data in EHR-Based Predictions
Electronic Health Record (EHR) data typically contains significant missingness that, if improperly handled, can introduce bias and reduce model accuracy. A 2025 comparative evaluation examined multiple imputation methods using EHR data from a pediatric intensive care unit, where 18.2% of data were missing [59]. The study created synthetic complete datasets, then induced missingness under varying mechanisms (MCAR, MAR, MNAR) and proportions, testing multiple imputation approaches across 300 generated datasets per outcome.
Key Experimental Findings:
- Last Observation Carried Forward (LOCF) demonstrated the lowest imputation error (average MSE improvement over mean imputation: 0.41) [59]
- Random forest imputation followed closely (average MSE improvement: 0.33) [59]
- For prediction models, traditional multiple imputation methods designed for inferential statistics may not be optimal
- The amount of missingness influenced performance more than the missingness mechanism itself
- For frequently measured EHR data, LOCF and native support for missing values in machine learning models offered reasonable performance at minimal computational cost
Bias Detection and Mitigation Protocol
The AEquity tool development study implemented a rigorous protocol for identifying and addressing dataset biases [60]. Researchers tested the framework on diverse health data types, including medical images, patient records, and the National Health and Nutrition Examination Survey (NHANES) dataset, using various machine learning models.
Experimental Methodology:
- Bias Detection Phase: Systematically evaluated representation disparities across demographic subgroups in training data
- Learnability Assessment: Measured performance differences across subgroups using multiple fairness metrics
- Bias Mitigation Phase: Applied pre-processing techniques including data rebalancing and feature adjustment
- Validation: Assessed post-mitigation performance across previously disadvantaged subgroups
Results: The AEquity framework successfully identified both well-known and previously overlooked biases across datasets and model types, providing a practical approach for developers and health systems to assess and improve equity before clinical deployment [60].
Research Reagent Solutions for Predictive Modeling
Implementing robust and equitable predictive models requires specialized methodological "reagents" – analytical tools and frameworks that enable rigorous development and validation.
Table 4: Essential Research Reagent Solutions for Equitable Predictive Modeling
| Reagent Category | Specific Tools/Methods | Primary Function | Implementation Considerations |
|---|---|---|---|
| Bias Assessment Tools | AEquity [60], Fairness metrics [63] | Detect performance disparities across demographic groups | Requires predefined patient subgroups for analysis |
| Data Imputation Methods | LOCF [59], Random forest imputation [59], Multiple imputation | Handle missing data in EHR and clinical datasets | Choice depends on missingness mechanism and data structure |
| Validation Frameworks | TRIPOD+AI [63], PROBAST [21] | Standardize model reporting and risk of bias assessment | Essential for publication and clinical implementation |
| Fairness Intervention Tools | Pre-processing techniques [61], In-processing constraints [61], Post-processing adjustments [61] | Actively mitigate identified biases | Selection depends on model type and deployment constraints |
Discussion: Toward Equitable Predictive Insights in Healthcare
The comparative analysis of mitigation approaches reveals that ensuring equitable predictive insights requires methodological rigor throughout the model lifecycle. The significant finding that fewer than half of hospitals using AI-assisted predictive tools conduct bias evaluations highlights a critical implementation gap [58]. This is particularly concerning given the emergence of a "digital divide," where under-resourced hospitals are more likely to use "off-the-shelf" models potentially trained on populations dissimilar to their patients [58].
Successful implementation requires ongoing monitoring and maintenance, as only 13% of clinically implemented models have been updated after deployment [21]. Furthermore, incorporating patient perspectives through participatory approaches [43] and transparent communication about model limitations and fairness considerations [63] builds trust and identifies potential blind spots in technical solutions. By adopting the comprehensive assessment protocols and mitigation strategies outlined in this guide, researchers and drug development professionals can advance the field toward predictive insights that are not only accurate but also equitable and trustworthy across diverse patient populations.
Strategies for Handling Missing Data and Model Updating for New Clinical Settings
In the field of clinical prediction models, two of the most persistent challenges are the handling of missing data and the adaptation of models to new clinical settings. Electronic Health Record (EHR) data, while rich in potential, frequently contain missing values that can compromise model performance if not addressed properly [64]. Simultaneously, the implementation of these models in real-world clinical practice remains low, with few models undergoing necessary updates after deployment [21] [52]. This guide provides a comprehensive comparison of current methodologies for addressing these challenges, framed within the broader context of assessing predictive models for patient outcomes research.
Handling Missing Data in Clinical Prediction Models
Categories of Missing Data
Understanding the mechanism behind missing data is crucial for selecting the appropriate handling strategy. The literature traditionally categorizes missing data into three primary mechanisms [64] [65]:
- Missing Completely at Random (MCAR): The probability of missingness does not depend on any observed or unobserved variables. Example: A laboratory technician forgets to record results randomly.
- Missing at Random (MAR): The probability of missingness depends on observed values in the data, including the outcome. Example: Height is not recorded but can be predicted from weight and sex, which are present in the EHR.
- Missing Not at Random (MNAR): The probability of missingness depends on unobserved values. Example: No lactate is measured because the clinician expects it to be normal.
In EHR-based prediction modeling, data are often MNAR, as measurement frequency itself may be informative of a patient's condition [64]. This presents particular challenges for traditional imputation methods.
Comparative Performance of Imputation Methods
Recent research has evaluated various strategies for addressing missingness in EHR-based prediction models. The table below summarizes the experimental findings from a study using EHR data from a pediatric intensive care unit (PICU) [64].
Table 1: Performance Comparison of Missing Data Handling Methods for Clinical Prediction Models
| Method | Key Characteristics | Imputation Error (MSE) | Performance Variability | Computational Cost | Best Suited For |
|---|---|---|---|---|---|
| Last Observation Carried Forward (LOCF) | Carries forward the last available value | Lowest (0.41 MSE improvement over mean imputation) | Low variability across scenarios | Minimal | Datasets with frequent measurements |
| Random Forest Multiple Imputation | Creates multiple imputed datasets using decision trees | Moderate (0.33 MSE improvement over mean imputation) | Moderate variability | High | Complex missing data patterns |
| Mean Imputation | Replaces missing values with variable mean | Reference method (baseline) | High variability for binary outcomes | Minimal | Baseline comparisons only |
| Complete Case Analysis | Uses only cases with complete data | Not specified in study | Leads to significant data loss | Minimal | MCAR data only |
| Native ML Support | Algorithms that natively handle missing values | Performance comparable to LOCF | Low variability | Minimal | High-dimensional EHR data |
The study found that the amount of missingness influenced performance more than the missingness mechanism itself, challenging traditional assumptions about missing data handling [64]. For binary outcomes, imputation methods showed more performance variability (balanced accuracy coefficient of variation: 0.042) than for continuous outcomes (mean squared error coefficient of variation: 0.001) [64].
Experimental Protocol for Evaluating Missing Data Methods
The comparative data presented in Table 1 were derived from a rigorous experimental protocol:
Data Source and Preparation:
- EHR data were extracted from an academic medical center PICU for patients intubated between 2013-2023 [64].
- Raw EHR data were transformed into an analytic dataset by binning variables into 4-hour time windows, containing the mean of each numeric variable and mode of each categorical variable [64].
- A synthetic complete dataset was generated using linear interpolation between observed values, followed by nearest non-missing value imputation for remaining gaps [64].
Missingness Induction:
- Researchers created 300 datasets with missing data under varying mechanisms (MCAR, MAR, and three levels of MNAR) [64].
- The proportion of missingness was varied at approximately 0.5x, 1x, and 2x the original percentage of missing cells (18.2% in original data) [64].
- For each scenario, 20 unique datasets were created to ensure statistical reliability of results [64].
Performance Evaluation:
- Two outcomes were assessed: successful extubation (binary) and blood pressure (continuous) [64].
- Models were evaluated using mean squared error (MSE) for continuous outcomes and balanced accuracy for binary outcomes [64].
- The evaluation incorporated temporal patterns by adding values from prior time windows to the imputation model [64].
Model Implementation and Updating in New Clinical Settings
Current State of Model Implementation
A systematic review of 37 articles describing 56 prediction models revealed significant gaps in current implementation practices [21] [52]. The distribution of implementation approaches is summarized below.
Table 2: Clinical Prediction Model Implementation Approaches and Characteristics
| Implementation Aspect | Current Status | Implications for Clinical Use |
|---|---|---|
| Primary Implementation Platform | Hospital Information Systems (63%), Web Applications (32%), Patient Decision Aid Tools (5%) | Integration with clinical workflow is essential for adoption |
| External Validation | Performed for only 27% of models | Limited generalizability to new settings |
| Calibration Assessment | Conducted for 32% of models during development/validation | Potential miscalibration in new populations |
| Post-Implementation Updating | Only 13% of models updated after implementation | Model decay over time likely |
| Risk of Bias | High in 86% of publications | Concerns about reliability of implemented models |
The review found that despite not fully adhering to prediction modeling best practices, impact assessments generally showed successful model implementation and ability to improve patient care [21] [52].
Model Updating Methodologies
When deploying models in new clinical settings, several updating strategies can be employed to maintain and improve performance:
- Simple Recalibration: Adjusting the intercept or slope of the model to fit the new population while retaining the original predictors.
- Model Revision: Re-estimating some or all predictor coefficients while retaining the original variable set.
- Complete Rebuilding: Developing an entirely new model using the original modeling process with data from the new setting.
The optimal approach depends on the similarity between the original development data and the new clinical setting, as well as the sample size available in the new environment.
Visualizing Method Selection Pathways
The following diagram illustrates the decision pathway for selecting appropriate strategies for handling missing data and model updating in clinical prediction research.
Diagram 1: Clinical Prediction Model Adaptation Workflow
Table 3: Essential Research Reagents and Computational Tools for Clinical Prediction Research
| Tool/Resource | Primary Function | Application Context | Key Features |
|---|---|---|---|
| R Statistical Software | Data analysis and modeling | General statistical computing | Comprehensive package ecosystem for imputation and modeling |
| mice Package | Multiple imputation by chained equations | Handling missing data | Implements various imputation methods including random forests |
| missRanger Package | Random forest imputation | High-dimensional missing data | Optimized for speed and memory efficiency with predictive mean matching |
| Hospital Information Systems | Clinical data integration | Model implementation | Real-time data access for prospective prediction |
| Web Application Frameworks | Model deployment | External access platforms | Enable model use outside native EHR environment |
The comparative analysis presented in this guide demonstrates that traditional statistical approaches for handling missing data may not be optimal for clinical prediction models. Methods such as LOCF and native support for missing values in machine learning models offer reasonable performance at minimal computational cost, particularly in datasets with frequent measurements [64]. Furthermore, the implementation landscape for clinical prediction models reveals significant opportunities for improvement, particularly in the areas of external validation and post-implementation updating [21] [52]. As the field advances, researchers and drug development professionals should prioritize methodologies that maintain performance across diverse clinical settings while providing practical implementation pathways for real-world use.
Overcoming Inexperience and Building Trust Through Explainable AI (XAI) and Transparency
The integration of artificial intelligence (AI) into patient outcomes research and drug development has created a paradigm shift, offering unprecedented capabilities in predicting treatment efficacy, disease progression, and patient responses. However, the inherent "black-box" nature of many advanced AI models presents a significant adoption barrier, particularly for researchers and drug development professionals who must reconcile these predictive insights with scientific rigor and regulatory requirements. Explainable AI (XAI) has emerged as a critical solution to this challenge, providing the transparency necessary to validate, trust, and effectively implement AI-driven predictions in high-stakes healthcare environments.
The trust deficit stems from fundamental limitations in traditional AI approaches. While AI models demonstrate remarkable predictive accuracy, their complex internal workings often obscure the reasoning behind specific predictions. This opacity is particularly problematic in pharmaceutical research and patient outcomes assessment, where understanding the biological and clinical rationale behind predictions is equally important as the predictions themselves. Model interpretability becomes essential not only for building trust among researchers but also for ensuring regulatory compliance, identifying potential biases, and generating clinically actionable insights [66] [67].
This guide provides a comprehensive comparison of predominant XAI methodologies, their performance characteristics, and implementation frameworks specifically tailored to patient outcomes research. By objectively evaluating these approaches through standardized metrics and experimental protocols, we aim to equip researchers with the knowledge needed to select appropriate XAI techniques that enhance transparency while maintaining predictive performance across various stages of drug development and clinical assessment.
Comparative Analysis of Major XAI Techniques in Healthcare Research
The XAI landscape encompasses diverse methodologies with varying strengths, limitations, and suitability for different data types and research questions in patient outcomes prediction. The table below provides a systematic comparison of the most prevalent XAI techniques based on recent systematic reviews and empirical studies:
Table 1: Performance Comparison of Major XAI Techniques in Healthcare Applications
| XAI Technique | Primary Methodology | Prevalence in Healthcare | Key Strengths | Limitations | Optimal Use Cases |
|---|---|---|---|---|---|
| SHAP (SHapley Additive exPlanations) | Game theory-based feature importance scoring | 46.5% of chronic disease applications [68]; 35/44 quantitative prediction studies [69] | Provides mathematically rigorous feature attribution; Consistent explanations; Both global and local interpretability | Computationally intensive; Additive feature assumption may oversimplify interactions [69] | Structured clinical data; Feature importance ranking; Model-agnostic explanations |
| LIME (Local Interpretable Model-agnostic Explanations) | Local surrogate model approximation | 25.8% of chronic disease applications [68]; Second most prevalent in prediction tasks [69] | Intuitive local explanations; Model-agnostic flexibility; Computationally efficient for single predictions | Instability across similar inputs; Sensitive to perturbation parameters [70] | Case-specific reasoning; Clinical decision support for individual patients |
| Grad-CAM (Gradient-weighted Class Activation Mapping) | Gradient-based visual explanation | 12.0% of chronic disease applications [68] | Visual localization of important regions; Particularly effective for image data | Primarily for convolutional networks; Limited to spatial data types | Medical imaging analysis; Tumor localization; Radiology assessment |
| Counterfactual Explanations | What-if scenario generation | Emerging application in drug discovery [66] | Intuitive actionable insights; Prescriptive rather than descriptive | Computational complexity for high-dimensional data | Treatment optimization; Drug target identification; Intervention planning |
Beyond these core techniques, additional XAI methods include Partial Dependence Plots (PDPs) and Permutation Feature Importance (PFI), which rank as the third and fourth most popular techniques respectively in quantitative prediction tasks [69]. The selection of an appropriate XAI method depends on multiple factors, including data modality (structured clinical data vs. medical images), required explanation scope (global model behavior vs. case-specific reasoning), and computational constraints.
Recent empirical evaluations highlight that SHAP consistently demonstrates superior performance in feature importance ranking for structured clinical data, explaining its dominant position in healthcare literature [68] [69]. However, this does not imply universal superiority, as Grad-CAM remains unmatched in medical imaging applications, while LIME offers practical advantages for real-time clinical decision support requiring case-specific explanations.
Experimental Protocols for XAI Evaluation in Patient Outcomes Research
Benchmarking Methodologies and Validation Frameworks
Rigorous evaluation of XAI techniques requires standardized experimental protocols that move beyond qualitative assessment to quantitative, reproducible metrics. The XAI-Units benchmarking framework exemplifies this approach by establishing unit tests for specific model behaviors, creating a controlled environment where explanation quality can be objectively measured against known ground truths [70]. This methodology involves several critical phases:
Table 2: XAI Evaluation Metrics and Methodologies
| Evaluation Dimension | Key Metrics | Measurement Approach | Interpretation Guidelines |
|---|---|---|---|
| Explanation Faithfulness | Explanation Infidelity [70] | Perturbation analysis measuring agreement between explanation and model behavior [71] | Lower values indicate higher faithfulness; Statistical significance testing recommended |
| Explanation Stability | Explanation Sensitivity (Max-Sensitivity) [70] | Consistency of explanations under minor input variations | Lower sensitivity values preferred; High sensitivity indicates unreliable explanations |
| Clinical Relevance | Clinical Alignment Score | Domain expert evaluation of biologically plausible feature importance | Qualitative scoring (1-5 scale) by multiple clinical experts; Inter-rater reliability assessment |
| Computational Efficiency | Execution time; Memory consumption | Benchmarking under standardized hardware/software configurations | Context-dependent; Real-time applications require stricter thresholds |
The perturbation analysis method has proven particularly effective for quantitative comparison of XAI methods. This approach involves systematically modifying input features and measuring the corresponding impact on both model predictions and explanation consistency [71]. For reliable results, the selection of appropriate perturbation values is critical, with recent research recommending an information entropy-based approach to determine optimal perturbation magnitudes that maximize discriminatory power while maintaining physiological plausibility [71].
Implementation Workflow for XAI Validation
The following diagram illustrates the standardized experimental workflow for evaluating XAI methods in patient outcomes research:
XAI Evaluation Workflow: A standardized protocol for comparing explanation methods.
This workflow emphasizes the critical importance of both quantitative metrics and clinical validation, ensuring that explanations are not only mathematically sound but also clinically meaningful. The integration of domain expertise throughout the evaluation process, particularly during clinical relevance assessment, represents a essential component often overlooked in purely technical evaluations [72] [73].
Successful implementation of XAI in patient outcomes research requires both computational tools and methodological frameworks. The following toolkit summarizes key resources:
Table 3: Essential XAI Resources for Patient Outcomes Researchers
| Tool Category | Specific Solutions | Primary Function | Implementation Considerations |
|---|---|---|---|
| Computational Libraries | SHAP, LIME, Eli5, Captum | Feature attribution calculation | SHAP preferred for structured data; LIME for local explanations; Library compatibility requirements |
| Benchmarking Frameworks | XAI-Units, OpenXAI, Quantus | Standardized XAI evaluation | XAI-Units provides synthetic data with ground truth; OpenXAI includes real-world datasets |
| Visualization Tools | SHAP summary plots, Force plots, Dependency plots | Explanation communication | Interactive visualization enhances clinical interpretability; Integration with clinical workflow systems |
| Clinical Validation Instruments | Expert assessment protocols, Clinical alignment rubrics | Explanation plausibility evaluation | Multi-rater reliability essential; Domain-specific validation criteria |
The XAI-Units benchmark deserves particular attention for researchers new to the field, as it provides pre-configured unit tests for specific model behaviors, enabling rapid assessment of XAI method performance without extensive setup [70]. For clinical implementation, the PersonalCareNet framework demonstrates how to integrate multiple XAI techniques with predictive modeling, achieving both high accuracy (97.86%) and comprehensive explainability through SHAP-based visualization at both individual and population levels [72].
When selecting tools, researchers should prioritize those supporting both global interpretability (understanding overall model behavior) and local explainability (case-specific reasoning), as both perspectives are essential throughout the drug development pipeline, from early target identification to post-marketing surveillance.
The systematic comparison of XAI methodologies presented in this guide demonstrates that technique selection involves nuanced trade-offs between explanatory power, computational efficiency, and clinical utility. SHAP emerges as the dominant approach for structured clinical data, while Grad-CAM maintains superiority in imaging applications, and LIME offers advantages for real-time case explanations. However, beyond technical capabilities, successful implementation requires rigorous validation through standardized benchmarking protocols and meaningful engagement with clinical domain experts.
For drug development professionals and patient outcomes researchers, embracing XAI represents more than a technical compliance exercise—it offers a strategic opportunity to build trust in AI systems through demonstrable transparency. By selecting appropriate XAI methods based on empirical performance data rather than popularity alone, and implementing them through standardized evaluation frameworks, researchers can accelerate the adoption of AI technologies while maintaining scientific rigor and regulatory compliance throughout the drug development lifecycle.
The future of XAI in healthcare will likely see increased regulatory scrutiny, with frameworks like the EU AI Act already classifying healthcare AI systems as "high-risk" and mandating sufficient transparency [66]. Proactive adoption of rigorous XAI evaluation practices positions research organizations not only to meet these emerging requirements but also to leverage explainability as a competitive advantage in developing safer, more effective, and more trustworthy patient outcome predictions.
Ensuring Reliability: Rigorous Validation, Comparative Analysis, and Measuring Clinical Impact
The proliferation of predictive models in healthcare research represents a paradigm shift in how we approach patient outcomes, yet a critical gap threatens their clinical utility: the frequent absence of rigorous external validation. Predictive models, whether developed using traditional statistical methods or advanced machine learning algorithms, are mathematical equations that calculate an individual's risk of a specific outcome based on their characteristics (predictors) [74]. These models hold tremendous potential for personalized medicine, individualized decision-making, and risk stratification [74]. However, a model demonstrating excellent performance in the dataset from which it was derived often fails when applied to new patient populations—a phenomenon known as overfitting, where the model corresponds too closely to idiosyncrasies in the development data [74]. This validation chasm is not merely theoretical; systematic reviews reveal that 58% of clinical prediction models (CPMs) for cardiovascular disease had never been validated in external cohorts, and when tested externally, over 80% of models demonstrated potential for clinical harm if used for decision-making [75]. This article examines the methodological imperative of external validation, providing researchers and drug development professionals with comparative frameworks to assess model generalizability across diverse patient populations and healthcare settings.
What is External Validation and Why Does It Matter?
Defining Validation Types
External validation is the process of testing an original prediction model in a set of new patients to determine whether it performs satisfactorily beyond the development dataset [74]. It is crucial to distinguish between different validation strategies, which vary in their rigor and purpose:
- Internal Validation: Uses the same data from which the model was derived, through methods like split-sample, cross-validation, or bootstrapping [74]. For example, in a 10-fold cross-validation, the model is developed on 90% of the population and tested on the remaining 10%, repeated 10 times so all patients are included in the test group once [74].
- Temporal Validation: The model is validated on patients from the same institution or system treated at a later (or earlier) time point [74].
- External Validation: Patients in the validation cohort structurally differ from the development cohort, potentially through geographic location, care setting, or underlying disease characteristics [74]. Independent external validation occurs when the validation cohort is assembled completely separately from the development cohort [74].
The Critical Importance of Generalizability
External validation is necessary to assess a model's reproducibility (performance in new patients similar to the development cohort) and generalizability or transportability (performance in populations with different characteristics) [74]. Before implementation of any prediction model is merited, external validation is imperative because models generally perform more poorly in external validation than in development [74]. Basing clinical decisions on unvalidated models can have adverse effects on patient outcomes; for instance, using a model that underpredicts risk for dialysis preparation could lead to more patients starting dialysis without adequate vascular access, increasing morbidity and mortality [74].
The stakes for validation are particularly high in healthcare due to concerns about algorithmic bias. A seminal 2019 study found that an algorithm used to predict which patients would benefit from extra healthcare services disproportionately favored white patients, as it used historical healthcare spending data where white patients had historically received more care than Black patients, thus underestimating the health needs of Black patients [43]. Similarly, predictive tools for hospital readmissions have been shown to perform less well for minoritised populations, often due to differences in healthcare access, treatment patterns, and social determinants of health [43].
Comparative Performance: Internal Versus External Validation
Quantitative Evidence from Model Validation Studies
Table 1: Comparative Performance Metrics from Model Validation Studies
| Study Context | Internal Validation Performance (AUC) | External Validation Performance (AUC) | Key Performance Shift | Citation |
|---|---|---|---|---|
| Total Knee Arthroplasty (Discharge Prediction) | 0.83 to 0.84 | 0.88 to 0.89 | Improvement in discrimination | [76] |
| Cardiovascular Disease CPMs | Variable (Development) | Worse discrimination in external cohorts | Degradation in discrimination | [75] |
| COVID-19 Mortality (NOCOS Model) | Effective in development cohort | Good discrimination but miscalibrated (over-prediction) | Maintained discrimination, poor calibration | [75] |
The performance gap between internal and external validation demonstrates why external validation is non-negotiable. In the case of machine learning models predicting non-home discharge after total knee arthroplasty, the external validation on an institutional cohort (n=10,196) not only confirmed but exceeded the internal validation performance achieved through five-fold cross-validation on a national cohort (n=424,354) [76]. This seemingly counterintuitive result highlights that internal validation, while useful, cannot simulate real-world application across diverse settings.
In contrast, the broader evaluation of cardiovascular CPMs revealed a more concerning pattern: when tested using external datasets, the selected CPMs often failed to accurately predict patient risks, with degraded discrimination compared to their development performance [75]. The calibration error—the difference between observed outcome rates and model-predicted probabilities—was typically 0.5, representing half the average risk, indicating substantial miscalibration [75].
Methodological Frameworks for External Validation
Table 2: Key Metrics for External Validation Assessment
| Performance Metric | Definition | Interpretation in Validation | Common Thresholds |
|---|---|---|---|
| Discrimination | Ability to separate patients with and without the outcome | How well the model identifies high-risk vs. low-risk patients | AUC >0.7 acceptable; >0.8 good |
| Calibration | Agreement between predicted probabilities and observed outcomes | Accuracy of the actual risk estimates | Calibration slope ~1.0; Brier score lower better |
| Net Benefit | Measure of whether clinical decisions based on the model do more good than harm | Clinical utility beyond statistical measures | Positive across relevant risk thresholds |
The external validation process involves comparing predicted risks to actual observed outcomes in a patient population [74]. For researchers planning an external validation study, the Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD) checklist provides comprehensive methodological guidance [74]. The first technical step involves calculating the predicted risk for each individual in the external validation cohort using the original model's prediction formula and the predictor values from the new population [74].
Experimental Protocols for Validation Studies
Protocol 1: Geographic External Validation
The geographic external validation protocol tests model transportability across different healthcare systems or regions [74]. The Cleveland Clinic's development of a predictive model for stomach cancer screening exemplifies this approach. The research team analyzed electronic health records (EHRs) from 614 individuals with noncardia gastric cancer and 6,331 control patients without the disease to identify features correlating with cancer risk [77]. The model relied solely on EHR-based variables like age, race, and lifestyle factors since endoscopic results were less commonly available for patients without gastric cancer in the U.S. [77]. The team is now validating the model using larger external patient databases across Ohio and Florida, with plans to use even larger federal datasets [77]. This progressive validation approach—from institutional to regional to national datasets—exemplifies rigorous geographic validation.
Protocol 2: Temporal Validation
Temporal validation assesses model performance over time, crucial for accounting for changes in clinical practice, disease management, and population health [74]. The COVID-19 pandemic provided a stark example of the importance of temporal validation. Models like NOCOS (Northwell COVID-19 Survival) and COPE (COVID Outcome Prediction in the Emergency Department) were developed using data from patients admitted to hospitals with COVID-19 from March to August 2020 [75]. When these models were temporally validated using data from September to December 2020 (the "second wave"), the NOCOS model maintained good discrimination for identifying high-risk patients but demonstrated miscalibration, with COPE predicting a higher risk of death than actually occurred [75]. This temporal shift in performance highlights how changing disease dynamics, treatments, and variants can affect model accuracy.
Protocol 3: Multisite Replication for Generalizability Assessment
Multisite replication studies represent the gold standard for assessing generalizability. This approach was demonstrated in a harmonized replication of four prominent international relations experiments across seven democracies, but the methodology is directly applicable to healthcare [78]. The study employed "purposive variation" in site selection, choosing countries that varied systematically on theoretically relevant characteristics rather than using convenience samples [78]. This design allowed researchers to test both "sign-generalizability" (in how many countries the result was consistent with theoretical predictions) and perform meta-analysis across sites [78]. Applied to healthcare, this would involve selecting validation sites that vary on relevant medical dimensions (rural/urban, academic/community hospitals, socioeconomic diversity) to thoroughly assess transportability.
Visualizing the Pathway from Prediction to Patient Outcomes
Figure 1: The Pathway from Predictive Models to Patient Outcomes. Even accurate models require multiple conditions to be met to improve care [79].
The pathway from a statistically accurate model to improved patient outcomes involves multiple critical steps, each representing a potential point of failure [79]. First, model outputs must be accessed by someone with potential to act [79]. Second, the model must produce information not already known to users [79]. Third, recipients must understand how to interpret the statistical information [79]. Fourth, there must be an agreed-upon mapping of predictions to specific clinical actions [79]. Fifth, clinicians need time, skills, and resources to respond [79]. Finally, providers must actually take action [79]. This framework explains why even accurate models may fail to produce benefits in real-world settings.
Table 3: Essential Reagents for Predictive Model Validation
| Tool Category | Specific Examples | Application in Validation | Key Considerations |
|---|---|---|---|
| Data Standards | TRIPOD Checklist | Reporting standards for prediction model studies | Ensures transparent and complete reporting [74] |
| Validation Metrics | Discrimination (AUC), Calibration (slope, Brier), Net Benefit | Quantifying model performance | Multiple metrics needed for comprehensive assessment [74] [75] |
| Statistical Software | R, Python with scikit-learn, STATA | Implementing validation analyses | Support for bootstrapping, cross-validation essential |
| Data Sources | Electronic Health Records, Clinical Registries, Federal Databases | Providing external validation cohorts | Representativeness of target population is critical [77] |
| Bias Assessment | Disparity impact analysis, Subgroup validation | Identifying differential performance | Test across racial, ethnic, socioeconomic groups [43] |
The compelling evidence presented demonstrates that external validation is not merely a methodological formality but an ethical imperative in healthcare research. The substantial performance degradation observed when models are applied to new populations, combined with the potential for algorithmic bias that exacerbates healthcare disparities, demands a paradigm shift in how we develop and implement predictive models [43] [75]. The finding that over 80% of cardiovascular CPMs showed potential for harm when applied without external validation should serve as a sobering warning to researchers, clinicians, and drug development professionals alike [75].
Moving forward, the field must embrace multisite validation as standard practice before clinical implementation, adopt progressive validation frameworks that test models across geographically and temporally diverse populations, and integrate patient perspectives through public and patient involvement (PPI) to identify potential biases and ensure models align with patient realities [43]. Furthermore, researchers should prioritize the development and use of models that demonstrate low treatment effect heterogeneity across diverse populations, as this characteristic appears associated with better generalizability [78]. Only through such comprehensive validation approaches can we fulfill the promise of predictive analytics to deliver truly personalized, equitable, and effective healthcare.
In the field of patient outcomes research, predictive models are increasingly deployed to forecast clinical events, treatment responses, and healthcare utilization patterns. The transition from theoretical models to clinically applicable tools requires rigorous validation to ensure reliability across diverse patient populations and clinical settings. Validation methodologies serve as critical gatekeepers for model quality, separating robust, generalizable algorithms from those that are overfit to specific datasets. This guide provides a comprehensive comparison of validation approaches, with particular emphasis on cross-validation protocols and their application in healthcare contexts where data may be limited, heterogeneous, or subject to regulatory constraints.
The fundamental challenge in predictive healthcare modeling is optimism bias, where a model's performance appears stronger during development than when applied to new patient data. This overfitting occurs when models inadvertently learn dataset-specific noise rather than generalizable patterns. Cross-validation techniques address this concern by providing realistic estimates of how models will perform on unseen data, making them indispensable for healthcare applications where erroneous predictions can directly impact patient care [80] [81].
Core Validation Methodologies: A Comparative Framework
Internal Validation Techniques
Internal validation methods utilize only the development dataset to estimate model performance, making them particularly valuable when external data is unavailable. These approaches systematically assess model stability and identify overfitting through resampling strategies.
Holdout Validation (or split-sample validation) partitions data into distinct training and testing sets, typically with 70-80% of samples used for model development and the remainder for validation. This approach provides a straightforward implementation but suffers from significant limitations in smaller datasets commonly encountered in healthcare research. With limited data, the holdout set may be too small for reliable performance estimation, and results can vary substantially based on the specific random partition [80]. Simulation studies have demonstrated that holdout validation with 100 test samples produces comparable discrimination (AUC 0.70±0.07) to cross-validation but with substantially higher uncertainty in performance estimates [80].
K-Fold Cross-Validation systematically partitions data into k equally sized folds, iteratively using k-1 folds for training and the remaining fold for testing. This process repeats k times, with each fold serving exactly once as the validation set. Common implementations include 5-fold and 10-fold cross-validation, with the former providing a reasonable balance between computational efficiency and performance estimation stability. In comparative studies, 5-fold cross-validation has demonstrated strong performance, with one object detection application achieving a 6.26% improvement in mean Average Precision (mAP) over baseline algorithms [82].
Repeated K-Fold Cross-Validation enhances standard k-fold approaches by performing multiple rounds of cross-validation with different random partitions. This additional repetition reduces the variance in performance estimates that can occur with a single arbitrary data partition. For healthcare applications with limited data, repeated cross-validation provides more stable performance estimates, with one simulation study reporting an AUC of 0.71±0.06 for 100-repeated 5-fold cross-validation [80].
Nested Cross-Validation employs two layers of cross-validation: an outer loop for performance estimation and an inner loop for model selection and hyperparameter tuning. This separation prevents optimistic bias that occurs when the same data influences both parameter tuning and performance assessment. While computationally intensive, nested cross-validation provides the most accurate performance estimates for internal validation and is particularly valuable when comparing multiple algorithms or conducting extensive hyperparameter optimization [81].
Bootstrapping techniques create multiple training sets by sampling with replacement from the original dataset, typically generating samples equal in size to the original data. The bootstrap .632+ method is particularly effective as it balances the optimism of the bootstrap with the pessimistic bias of the holdout approach. In simulation studies, bootstrapping has demonstrated stable performance estimates (AUC 0.67±0.02) with lower variance than holdout validation [80].
Table 1: Comparative Performance of Internal Validation Methods
| Validation Method | Key Characteristics | Advantages | Limitations | Reported Performance (AUC) |
|---|---|---|---|---|
| Holdout Validation | Single train-test split (typically 70/30 or 80/20) | Simple implementation; Fast computation | High variance with small samples; Inefficient data use | 0.70 ± 0.07 [80] |
| K-Fold Cross-Validation | k folds; each serves as test set once | More stable than holdout; Full data utilization | Computationally intensive; Higher variance than repeated CV | 6.26% mAP improvement over baseline [82] |
| Repeated K-Fold CV | Multiple rounds of k-fold with different partitions | Reduced performance variance | Increased computation | 0.71 ± 0.06 [80] |
| Nested Cross-Validation | Outer loop for testing, inner for tuning | Unbiased performance estimation | High computational demand | Recommended for model selection [81] |
| Bootstrapping | Multiple samples with replacement | Stable with small samples; Good for optimism correction | Can be overly optimistic without .632+ correction | 0.67 ± 0.02 [80] |
External Validation Approaches
External validation represents the gold standard for assessing model generalizability by applying developed models to completely independent datasets. This approach most accurately reflects real-world performance but requires access to additional data sources that may be difficult or expensive to acquire in healthcare settings.
Temporal validation assesses model performance on patients from a different time period than the development cohort, testing robustness to temporal shifts in clinical practice or patient populations. Geographic validation applies models to patients from different healthcare systems or regions, evaluating transportability across practice settings. Fully external validation tests models on populations from entirely different institutions, providing the strongest evidence of generalizability but requiring significant data sharing agreements and harmonization efforts [80].
The critical importance of external validation was demonstrated in a simulation study where models developed on one patient population showed substantially different performance when applied to patients with different disease stages or risk profiles. Specifically, when patient populations differed in their distribution of Ann Arbor stages, model discrimination (CV-AUC) varied significantly across stages, highlighting the critical need for population-matched validation [80].
Experimental Protocols for Validation Studies
Data Preparation and Preprocessing Protocol
Robust validation begins with meticulous data preparation, particularly for electronic health record (EHR) data characterized by irregular sampling, missing values, and heterogeneity. The following protocol ensures data quality before validation:
- Data Cleaning and Quality Assurance: Implement systematic checks for data anomalies, including range violations, implausible values, and inconsistent recordings. For questionnaire data, establish thresholds for excluding participants with excessive missingness (e.g., >50% incomplete), while using statistical tests like Little's Missing Completely at Random (MCAR) to characterize missing data patterns [83].
- Feature Preprocessing: Address missing values through appropriate imputation techniques (e.g., multiple imputation, maximum likelihood estimation) that preserve dataset structure. Normalize or standardize continuous variables where appropriate, and document all transformations to ensure consistent application across training and validation sets.
- Data Partitioning Strategies: For internal validation, implement stratified sampling to maintain consistent outcome prevalence across folds, particularly important for rare clinical events. For subject-wise versus record-wise splitting, carefully consider the unit of prediction—use subject-wise splitting (where all records from an individual remain in the same fold) for patient-level predictions, and record-wise splitting for encounter-level predictions [81].
Cross-Validation Implementation Protocol
The following step-by-step protocol implements robust cross-validation for healthcare prediction models:
- Initial Data Setup: For datasets with multiple records per patient, decide between subject-wise and record-wise splitting based on the prediction unit. For binary outcomes, implement stratified sampling to maintain consistent event rates across folds.
- Fold Generation: Randomly partition data into k folds (typically 5-10), ensuring each fold represents the overall dataset. For repeated cross-validation, repeat this process with different random seeds (typically 10-100 repetitions).
- Iterative Training and Validation: For each fold iteration:
- Set aside the current fold as validation data
- Use remaining k-1 folds for model training
- Apply trained model to the validation fold
- Calculate performance metrics (discrimination, calibration)
- Performance Aggregation: Compute mean performance metrics across all folds, along with measures of variability (standard deviation, confidence intervals). For nested cross-validation, include an inner loop for hyperparameter optimization within each training set.
- Model Refitting: After validation, retrain the model using the entire dataset with the optimized parameters identified during validation.
Diagram 1: Cross-Validation Workflow for Healthcare Data
Performance Assessment Metrics
Comprehensive model evaluation requires multiple performance dimensions, with particular emphasis on both discrimination and calibration:
- Discrimination Metrics: Area Under the Receiver Operating Characteristic Curve (AUC-ROC) quantifies how well models separate events from non-events. For time-to-event outcomes, consider time-dependent AUC metrics. The Area Under the Precision-Recall Curve (AUC-PR) may be more informative for imbalanced outcomes common in healthcare [80].
- Calibration Metrics: Calibration slopes assess how well predicted probabilities match observed event rates. A slope of 1 indicates perfect calibration, while values <1 suggest overfitting and >1 suggest underfitting. Calibration-in-the-large evaluates whether average predicted risks match the overall event rate [80].
- Clinical Utility: Decision curve analysis and related methods evaluate the net benefit of models across different probability thresholds, connecting statistical performance to clinical decision-making.
Table 2: Statistical Comparison of Validation Methods Across Healthcare Applications
| Application Domain | Validation Method | Sample Size | Performance Metrics | Key Findings |
|---|---|---|---|---|
| DLBCL Outcome Prediction [80] | 5-Fold Cross-Validation | 500 simulated patients | AUC: 0.71 ± 0.06Calibration Slope: ~1.0 | Lower uncertainty than holdout; Recommended for small datasets |
| DLBCL Outcome Prediction [80] | Holdout Validation | 400 train, 100 test | AUC: 0.70 ± 0.07Calibration Slope: ~1.0 | Higher uncertainty than cross-validation; Not recommended for small samples |
| DLBCL Outcome Prediction [80] | Bootstrapping | 500 simulated patients | AUC: 0.67 ± 0.02Calibration Slope: ~1.0 | Most stable performance estimate; Lower discrimination due to correction |
| Smart Pick-and-Place Object Detection [82] | Holdout (80/20 split) | Custom dataset | mAP: 44.73% improvement over baseline | High performance with sufficient data; Detection score >93% |
| Smart Pick-and-Place Object Detection [82] | 5-Fold Cross-Validation | Custom dataset | mAP: 6.26% improvement over baseline | More modest gains than holdout; Better generalization estimate |
| Sepsis Prediction [43] | Temporal Validation | EHR data | Early detection: 12 hours before clinical signs | Demonstrated clinical utility with external validation |
Special Considerations for Healthcare Applications
Handling Healthcare Data Complexities
Healthcare data presents unique challenges that directly impact validation strategy selection. Electronic Health Records (EHR) typically contain irregular time-sampling, inconsistent repeated measures, and significant sparsity [81]. These characteristics necessitate specialized approaches:
- Temporal Validation: For models predicting disease onset or treatment response, implement strict temporal splits where models are trained on earlier time periods and validated on later periods. This approach tests robustness to clinical practice evolution.
- Cluster-Aware Splitting: When data contains natural clustering (patients within physicians, within hospitals), implement cluster-aware validation splits where all members of a cluster remain in the same fold. This prevents optimistic bias from similar patients appearing in both training and validation sets.
- Multi-Site Validation: For datasets from multiple healthcare systems, implement internal-external validation where models are developed on all but one site and tested on the held-out site, iterating across all sites. This approach efficiently uses available data while testing transportability [81].
Addressing Class Imbalance
Rare clinical outcomes represent a particular challenge for validation, as standard random sampling may create folds with no events. Effective strategies include:
- Stratified Sampling: Ensure consistent event rates across all folds, which is particularly crucial for k-fold cross-validation with rare outcomes.
- Balanced Bootstrapping: Generate bootstrap samples with fixed event rates to maintain stable performance estimates.
- Alternative Metrics: Supplement AUC with precision-recall curves, F-measures, and balanced accuracy that better reflect performance on imbalanced data.
Table 3: Research Reagent Solutions for Validation Studies
| Tool Category | Specific Solutions | Primary Function | Application Context |
|---|---|---|---|
| Statistical Analysis | R Statistical SoftwarePython Scikit-learnSASSPSS | Implementation of cross-validationand performance metrics | General statistical analysis;Machine learning pipelines |
| Specialized Validation Packages | R: caret, mlr3, rsamplePython: scikit-learnTensorFlow Extended (TFX) | Streamlined validation workflows | Comparative algorithm evaluation;Hyperparameter tuning |
| Data Visualization | ggplot2 (R)Matplotlib/Seaborn (Python)TableauPower BI | Performance results visualizationModel calibration plots | Publication-quality figures;Interactive model evaluation |
| Computational Environments | Google ColabJupyter NotebooksRStudio | Reproducible analysisCode sharing and collaboration | Educational demonstrations;Team-based research projects |
| Electronic Health Record Tools | FHIR StandardsOMOP Common Data ModelClinical Data Warehouses | Data standardization and extraction | Multi-site studies;Regulatory-grade analytics |
Recommendations and Best Practices
Protocol Selection Guidelines
Based on comparative performance and healthcare-specific requirements, we recommend:
- For Small Datasets (<500 events): Prefer repeated k-fold cross-validation (5-10 folds with 10-100 repetitions) or bootstrapping over single holdout validation, as these approaches provide more stable performance estimates with limited data [80].
- For Model Selection and Hyperparameter Tuning: Implement nested cross-validation to obtain unbiased performance estimates when comparing multiple algorithms or conducting extensive parameter optimization [81].
- For Regulatory Submissions and Clinical Implementation: Prioritize external validation across multiple sites and time periods, as this most accurately reflects real-world performance and is increasingly required by regulatory bodies [43] [81].
- For Rare Outcomes (<5% prevalence): Use stratified sampling approaches combined with precision-recall curves and balanced accuracy metrics to ensure meaningful performance assessment.
Implementation Considerations
Successful validation studies require attention to both technical and practical considerations:
- Computational Efficiency: For complex deep learning models with large datasets, implement holdout validation with separate validation and test sets due to computational constraints, while recognizing the limitations of this approach.
- Reproducibility: Set random seeds for data partitioning to ensure reproducible results, while conducting sensitivity analyses to ensure findings are robust to different partitions.
- Comprehensive Reporting: Transparently document all validation procedures, including specific cross-validation implementations, handling of missing data, and any data preprocessing steps. Report both discrimination and calibration metrics, along with measures of uncertainty (confidence intervals, standard deviations) [80] [81].
Diagram 2: Validation Method Selection Guide
Robust validation methodologies are fundamental to developing trustworthy predictive models in patient outcomes research. Cross-validation techniques provide essential tools for estimating model performance and optimizing algorithms, particularly when external validation data is unavailable. The comparative analysis presented in this guide demonstrates that method selection involves important tradeoffs between computational efficiency, stability of performance estimates, and generalizability.
For healthcare applications, no single validation approach is universally superior—the optimal strategy depends on dataset characteristics, model complexity, and intended use case. However, the systematic comparison of methods reveals that k-fold and repeated cross-validation generally provide favorable performance for internal validation, while external validation remains essential for models intended for clinical implementation. As predictive models assume increasingly prominent roles in healthcare decision-making, rigorous validation protocols serve as critical safeguards ensuring these tools deliver reliable, generalizable performance across diverse patient populations.
In the rapidly evolving field of patient outcomes research, the selection of an appropriate predictive modeling framework is paramount for generating reliable, actionable evidence. The emergence of machine learning (ML) as a powerful alternative to traditional statistical methods has sparked considerable debate regarding their comparative performance, appropriate applications, and implementation requirements. This guide provides an objective comparison of these methodological approaches, focusing on their performance in forecasting patient outcomes, to assist researchers, scientists, and drug development professionals in selecting the most suitable framework for their specific research contexts.
While traditional statistical methods like logistic regression (LR) have long been the cornerstone of clinical prediction models, ML algorithms—including random forests, deep learning, and more recently, large language models (LLMs)—offer sophisticated pattern recognition capabilities that may capture complex, non-linear relationships in healthcare data [84] [85]. Understanding the relative strengths, limitations, and performance characteristics of each approach is essential for advancing predictive analytics in healthcare and pharmaceutical development.
Performance Comparison: Quantitative Evidence
Multiple systematic reviews and meta-analyses have directly compared the performance of traditional statistical and ML models across various clinical scenarios. The table below summarizes key quantitative findings from recent rigorous comparisons.
Table 1: Performance Comparison of ML Models vs. Traditional Statistical Methods in Healthcare Prediction
| Clinical Context | Outcome Predicted | Best Performing Model (AUC/MAE) | Traditional Model Performance (AUC/MAE) | Performance Difference | Reference |
|---|---|---|---|---|---|
| PCI in AMI Patients | MACCEs (Mortality) | ML Models (AUC: 0.88) | Conventional Risk Scores (AUC: 0.79) | +0.09 AUC [85] | |
| PCI (Various Cohorts) | Long-term Mortality | ML Models (AUC: 0.84) | Logistic Regression (AUC: 0.79) | +0.05 AUC [84] | |
| PCI (Various Cohorts) | Short-term Mortality | ML Models (AUC: 0.91) | Logistic Regression (AUC: 0.85) | +0.06 AUC [84] | |
| PCI (Various Cohorts) | Acute Kidney Injury | ML Models (AUC: 0.81) | Logistic Regression (AUC: 0.75) | +0.06 AUC [84] | |
| NSCLC Treatment | Laboratory Values | DT-GPT (scMAE: 0.55) | LightGBM (scMAE: 0.57) | -3.4% MAE [30] | |
| ICU Monitoring | Vital Signs | DT-GPT (scMAE: 0.59) | LightGBM (scMAE: 0.60) | -1.3% MAE [30] | |
| Alzheimer's Disease | Cognitive Scores | DT-GPT (scMAE: 0.47) | TFT (scMAE: 0.48) | -1.8% MAE [30] |
AUC = Area Under the Receiver Operating Characteristic Curve; MAE = Mean Absolute Error; scMAE = Scaled Mean Absolute Error; PCI = Percutaneous Coronary Intervention; AMI = Acute Myocardial Infarction; MACCEs = Major Adverse Cardiovascular and Cerebrovascular Events; NSCLC = Non-Small Cell Lung Cancer; ICU = Intensive Care Unit; TFT = Temporal Fusion Transformer
The quantitative evidence demonstrates that while ML models frequently show superior discriminatory performance, the magnitude of improvement varies substantially across clinical contexts. In predicting mortality following percutaneous coronary intervention (PCI), ML models achieved area under the curve (AUC) values ranging from 0.84 to 0.91, representing modest but potentially clinically meaningful improvements over traditional logistic regression models (AUC 0.79-0.85) [84] [85]. For more complex forecasting tasks involving longitudinal trajectories of clinical variables, advanced implementations like DT-GPT (a fine-tuned large language model) demonstrated consistent but relatively smaller improvements in error reduction compared to state-of-the-art traditional methods [30].
Methodological Approaches and Experimental Protocols
Fundamental Differences in Approach
Traditional statistical methods and machine learning differ fundamentally in their philosophical approaches to prediction:
Traditional Statistical Models (e.g., logistic regression, linear regression) operate on predefined assumptions about data relationships, typically requiring structured input and manual feature selection. They emphasize interpretability and hypothesis testing, with performance remaining static unless manually recalibrated [86] [87].
Machine Learning Algorithms (e.g., random forests, neural networks) utilize data-driven approaches that automatically learn patterns and relationships from data, often requiring minimal human intervention in feature selection. They excel at identifying complex, non-linear interactions and can continuously improve their performance with exposure to new data [86] [87] [88].
These fundamental differences inform their respective experimental protocols and implementation requirements in patient outcomes research.
Typical Experimental Workflow
The following diagram illustrates a generalized experimental workflow for developing and validating predictive models in patient outcomes research, highlighting key differences between traditional and ML approaches:
Specific Methodological Protocols
Protocol for Predicting MACCEs After PCI
A recent systematic review and meta-analysis comparing ML models with conventional risk scores for predicting major adverse cardiovascular and cerebrovascular events (MACCEs) after percutaneous coronary intervention in acute myocardial infarction patients followed this rigorous protocol [85]:
- Data Sources: Nine electronic databases were systematically searched from January 1, 2010, to December 31, 2024, including PubMed, CINAHL, Embase, Web of Science, Scopus, and others.
- Study Selection: Included studies focused on adult AMI patients who underwent PCI and predicted MACCEs risk using either ML algorithms or conventional risk scores. The analysis included 10 retrospective studies with a total sample size of 89,702 individuals.
- Model Comparison: The most frequently used ML algorithms were random forest (n=8) and logistic regression (n=6), while the most used conventional risk scores were GRACE (n=8) and TIMI (n=4).
- Validation: Risk of bias was assessed using appropriate tools, with most included studies rated as having low overall risk of bias. Performance was measured using area under the receiver operating characteristic curve (AUC).
Protocol for Deep Learning with Sequential EHR Data
A systematic review of deep learning approaches using sequential diagnosis codes from structured electronic health records followed this methodological approach [89] [4]:
- Data Structure: Sequential diagnosis codes from EHRs were organized as temporal sequences of patient visits, capturing the progression of medical history over time.
- Model Architectures: Recurrent neural networks and their derivatives (56%) and transformers (26%) were the most commonly used deep learning architectures.
- Input Representation: Most studies (54%) presented input features as sequences of visit embeddings, with medications (45%) being the most common additional feature.
- Performance Evaluation: A positive correlation was observed between training sample size and model performance (P=.02), highlighting the data requirements for effective deep learning implementation.
Key Methodological Considerations and Limitations
Bias and Generalizability Concerns
Despite promising performance metrics, significant methodological challenges persist across both traditional and ML approaches:
- High Risk of Bias: A meta-analysis of ML models for PCI outcomes found that 93% of long-term mortality studies, 70% of short-term mortality studies, and 89% of bleeding studies had a high risk of bias according to PROBAST criteria [84].
- Limited Generalizability: In deep learning studies using sequential EHR data, only 8% of studies evaluated their models in terms of generalizability to external datasets [89].
- Explainability Deficits: Less than half (45%) of deep learning studies reported on challenges related to explainability, creating significant barriers to clinical adoption and trust [89].
Data Requirements and Feature Considerations
The performance of predictive models is heavily influenced by data characteristics and feature selection:
- Sample Size Impact: Deep learning performance showed a statistically significant positive correlation with training sample size (P=.02), indicating that these models require substantial data resources to achieve optimal performance [89].
- Feature Types: The top-ranked predictors in both ML and conventional risk scores for cardiovascular events were typically confined to non-modifiable clinical characteristics such as age, systolic blood pressure, and Killip class [85]. This highlights a potential limitation in capturing modifiable psychosocial and behavioral factors that could inform interventions.
- Temporal Data Integration: Models that effectively incorporated sequential diagnosis codes and time intervals between clinical events generally demonstrated improved predictive performance, capturing the progressive nature of disease trajectories [89].
Table 2: Essential Research Reagents and Computational Resources for Predictive Modeling
| Resource Category | Specific Tools/Solutions | Primary Function | Considerations for Selection |
|---|---|---|---|
| Statistical Analysis Platforms | IBM SPSS, SAS, R, Python (Scikit-learn) | Implementation of traditional statistical models (regression, survival analysis) | Well-established, highly interpretable, but limited capacity for complex pattern recognition [86] |
| Machine Learning Frameworks | TensorFlow, PyTorch, Scikit-learn | Development and training of ML algorithms (neural networks, ensemble methods) | Require programming expertise, offer flexibility for complex modeling tasks [86] |
| Cloud Computing Platforms | Google Cloud AI, AWS SageMaker, Azure ML Studio | Scalable environments for training and deploying resource-intensive models | Essential for large-scale deep learning implementations, offer managed services [86] |
| Electronic Health Record Data | MIMIC-IV, Flatiron Health EHR database, ADNI | Primary data sources for model training and validation | Vary in completeness, structure, and accessibility; require careful preprocessing [30] |
| Validation Frameworks | PROBAST, CHARMS | Standardized assessment of model risk of bias and applicability | Critical for ensuring methodological rigor in predictive model development [84] [85] |
| Specialized Clinical Models | GRACE Score, TIMI Score | Established benchmarks for comparing novel model performance | Provide clinically validated reference points for performance evaluation [85] |
The comparative evidence between traditional statistical methods and machine learning approaches for predicting patient outcomes reveals a nuanced landscape without definitive superiority of either paradigm. While ML models frequently demonstrate superior discriminatory performance, particularly for complex pattern recognition tasks in large datasets, they often face significant challenges regarding interpretability, generalizability, and implementation complexity.
The choice between methodological approaches should be guided by specific research contexts: traditional statistical methods remain appropriate for studies with limited sample sizes, requiring high interpretability, and focusing on confirmatory hypothesis testing. In contrast, machine learning approaches offer advantages for exploratory analysis of complex datasets, detection of non-linear relationships, and applications where proprietary implementation can overcome the "black box" concern through effective user interface design.
Future advancements in patient outcomes research will likely benefit from hybrid approaches that leverage the strengths of both paradigms, along with increased attention to methodological rigor in validation practices and the incorporation of diverse data types, including modifiable psychosocial and behavioral variables that may enhance both predictive performance and clinical actionability.
The central thesis of modern patient outcomes research is that the value of a predictive model is not defined by its statistical accuracy in isolation, but by its demonstrable impact on the clinical pathway and patient welfare [90] [43]. This guide provides a comparative analysis of methodologies for translating predictive accuracy into proven clinical impact, a process fraught with challenges from algorithmic bias to integration into real-world workflows [91] [21]. For researchers and drug development professionals, moving beyond the area under the curve (AUC) requires a framework that encompasses all effects of an intervention, including accessibility, quality, equality, effectiveness, safety, and efficiency [90].
Comparative Analysis of Evaluation Approaches for Clinical Impact
The following table compares the primary study designs and their suitability for measuring different categories of clinical impact, based on the Clinical Impact Research (CIR) framework [90].
| Impact Category | Definition | Primary Study Design(s) | Key Measurable Outcomes | Considerations for Predictive Models |
|---|---|---|---|---|
| Accessibility | The ease with which patients can obtain care influenced by the predictive tool. | Benchmarking Controlled Trial (BCT) [90] | Time to diagnosis, referral rates, service utilization disparities. | Models must not create barriers for underrepresented groups; requires monitoring of deployment data [43]. |
| Quality | The degree to which care is appropriate, competent, and evidence-based. | BCT, Randomized Controlled Trial (RCT) [90] | Adherence to clinical guidelines, clinician satisfaction, process compliance. | Quality hinges on model interpretability and seamless integration into Clinical Decision Support Systems (CDSS) [91]. |
| Equality | Uniformity in the quality of service obtained by different patient groups. | BCT [90] | Disparities in prediction performance (e.g., sensitivity, specificity) across demographics. | High risk of algorithmic bias if training data is unrepresentative; necessitates continuous bias auditing [91] [43]. |
| Effectiveness | The extent to which an intervention achieves its intended outcome under ordinary conditions. | RCT (gold standard), BCT (for real-world evidence) [90] [92] | Patient health outcomes (e.g., mortality, morbidity), early disease identification rates. | Predictive models have shown up to 48% improvement in early disease identification [91]. Effectiveness under routine care (Real-World Effectiveness) may differ from RCT results [92]. |
| Safety | The avoidance of unintended and harmful outcomes. | RCT, BCT, Self-controlled studies [90] [92] | Rates of adverse events, false-positive/negative-induced harm, alert fatigue. | Requires rigorous monitoring post-implementation; only 13% of implemented models are formally updated [21]. |
| Efficiency | The relationship between the outcomes achieved and the resources consumed. | BCT [90] | Cost-effectiveness, operational metrics (e.g., reduced nurse overtime, length of stay). | AI-driven predictive staffing has reduced nurse overtime costs by ~15% [91]. |
Experimental Protocols for Impact Assessment
Protocol for the Benchmarking Controlled Trial (BCT) in Real-World Settings
BCTs are observational studies comparing outcomes between peers (e.g., clinics using vs. not using a model) and are often the only feasible design for assessing system-level impacts like clinical pathways [90] [92].
- Design & Emulation: Employ the target trial approach: explicitly specify the protocol of the idealized RCT you are emulating (eligibility criteria, treatment strategies, assignment procedures, outcomes, follow-up) [92].
- Data Curation: Select and harmonize data from real-world sources (e.g., EHR, registries) to minimize differences in variable definitions, care pathways, and time periods between compared groups [92].
- Confounder Management: Identify potential confounders (patient- and system-level) using directed acyclic graphs (DAGs). Use advanced statistical methods (e.g., propensity score matching, inverse probability weighting) to address observed confounding. Consider instrumental variable analysis for unobserved confounding [92].
- Analysis & Validation: Pre-specify a statistical analysis plan. Use sensitivity and bias analysis to assess robustness to unmeasured confounding and other biases [92].
Protocol for Method Comparison in Model Validation
When comparing a new predictive model against a standard or existing model, standard biostatistical method comparison principles apply [93].
- Design: A minimum of 40-100 patient samples is recommended, covering the entire clinically meaningful range. Samples should be measured over multiple days to mirror real-world variation [93].
- Analysis (What NOT to do): Avoid using only correlation analysis (which measures association, not agreement) or t-tests (which may miss clinically significant differences) [93].
- Analysis (Correct Approach):
- Graphical Assessment: Begin with scatter plots and difference plots (Bland-Altman plots) to visualize agreement across the measurement range and identify outliers or systematic bias [93].
- Statistical Modeling: Apply regression models designed for method comparison, such as Deming or Passing-Bablok regression, which account for variability in both methods [93].
- Performance Specification: Define acceptable bias a priori based on biological variation, clinical outcomes, or state-of-the-art performance [93].
Visualizing the Impact Assessment Pathway
Pathway from Model Validation to Clinical Impact
Real-World Evidence Study Workflow
The Scientist's Toolkit: Essential Reagents for Impact Research
| Tool / Reagent | Function in Impact Research | Key Reference / Standard |
|---|---|---|
| TRIPOD & PROBAST Guidelines | Provide a structured framework for the transparent reporting and risk-of-bias assessment of predictive model studies, essential for critical appraisal. | [21] |
| Clinical Impact Research (CIR) Framework | Defines the six core impact categories (Accessibility, Quality, Equality, Effectiveness, Safety, Efficiency) that comprehensive assessment must address. | [90] |
| Target Trial Emulation Protocol | A methodological "reagent" to design observational studies that mimic a hypothetical RCT, mitigating inherent design biases. | [92] |
| Bias Audit & Mitigation Suite | Includes techniques like disaggregated performance analysis across subgroups and tools (e.g., AI Fairness 360) to detect and correct algorithmic bias. | [91] [43] |
| Patient & Public Involvement (PPI) Panel | Not a traditional reagent, but a critical resource. Patients provide ground truth for relevant outcomes, help identify bias, and ensure tools are ethical and practicable. | [43] |
| Advanced Statistical Software Packages | For implementing propensity score methods, inverse probability weighting, instrumental variable analysis, and sophisticated sensitivity analyses. | [92] |
| Integrated Clinical Decision Support (CDSS) Platform | The deployment environment where predictive models are operationalized; its design dictates the model's ultimate usability and influence on care. | [91] |
| Continuous Model Monitoring & Updating Pipeline | A system to track model performance drift, clinical outcomes post-implementation, and trigger model recalibration or retraining. Lacking in 87% of implementations. | [21] |
Conclusion
The successful assessment and implementation of predictive models for patient outcomes hinge on a rigorous, multi-faceted approach that integrates robust methodology, meticulous validation, and proactive troubleshooting. The journey from a well-performing model to one that genuinely impacts clinical care requires demonstrating improved decision-making and patient outcomes through prospective studies. Future directions must focus on enhancing model interpretability and fairness, achieving seamless integration into clinical workflows, and advancing towards dynamic, real-time forecasting systems. By adhering to these principles, researchers and drug developers can fully leverage predictive analytics to usher in an era of precision medicine, ultimately improving patient care and therapeutic success.
References
- 1. Healthcare Evolves From Reactive to Proactive - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6314203/]
- 2. Proactive vs. Reactive Healthcare: Deep Guide [https://www.practicebuilders.com/blog/proactive-vs-reactive-healthcare/]
- 3. Personalized Predictive Modeling and Risk Factor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4525240/]
- 4. Enhancing Patient Outcome Prediction Through Deep ... [https://www.jmir.org/2025/1/e57358]
- 5. A Clinical Data Based Framework for Outcome Forecasting ... [https://pubmed.ncbi.nlm.nih.gov/41284430/]
- 6. UC Davis Health uses AI models to leave no patient behind [https://health.ucdavis.edu/news/headlines/uc-davis-health-uses-ai-models-to-leave-no-patient-behind/2025/04]
- 7. AI and machine learning: Revolutionising drug discovery ... [https://www.roche.com/stories/ai-revolutionising-drug-discovery-and-transforming-patient-care]
- 8. Applying Machine Learning Techniques to Predict Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12166244/]
- 9. Model uncertainty quantification: A post hoc calibration ... [https://www.medrxiv.org/content/10.1101/2025.09.28.25336834v1.full-text]
- 10. Making Machine Learning Predictions Trustworthy [https://arxiv.org/html/2509.23665v1]
- 11. Beyond discrimination: A comparison of calibration ... [https://www.sciencedirect.com/science/article/pii/S1532046417302277]
- 12. Weighted Brier Score - an Overall Summary Measure for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523994/]
- 13. Evaluating predictive performance, validity, and applicability of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288308/]
- 14. From Model to Bedside: What Kind of OSA Risk Prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12338320/]
- 15. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 16. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 17. a systematic literature review and meta-analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570641/]
- 18. Clinical prediction models using machine learning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506039/]
- 19. Development and validation of a machine learning model ... [https://www.nature.com/articles/s41598-025-18443-7]
- 20. Comparing AI/ML approaches and classical regression for ... [https://www.sciencedirect.com/science/article/pii/S2590113324000348]
- 21. Implementation and Updating of Clinical Prediction Models [https://www.sciencedirect.com/science/article/pii/S2949761225000355]
- 22. Artificial Intelligence for Drug Development [https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development]
- 23. Why The Concept of Result-Based Management (RBM) ... [https://www.linkedin.com/pulse/why-concept-result-based-management-rbm-has-become-health-ochieng]
- 24. Results Based Management (RBM) in Monitoring and ... [https://practicalmel.com/results-based-management-rbm-in-monitoring-and-evaluation-me/]
- 25. Cancer Data Statistics in a National Institute of Health [https://www.mdpi.com/2072-6694/15/18/4649]
- 26. Results-Based Management vs. Balanced Scorecard for ... [https://bscdesigner.com/results-based-management.htm]
- 27. Implementation of Predictive Analytics in Healthcare Using ... [https://www.mdpi.com/2673-4591/107/1/67]
- 28. Optimized machine learning mechanism for big data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12022254/]
- 29. AI Tool Creates 'Digital Twins' of Patients to Forecast Future ... [https://www.contemporaryhealth.co.uk/digital-health/ai-digital-twins-forecast-patient-health/]
- 30. Large language models forecast patient health trajectories ... [https://www.nature.com/articles/s41746-025-02004-3]
- 31. Large language models forecast patient health trajectories ... [https://pubmed.ncbi.nlm.nih.gov/41034564/]
- 32. LLM驱动的数字孪生医疗:基于实时多模态数据融合的个性化 ... [https://blog.csdn.net/2501_93420214/article/details/153837899]
- 33. LLM驱动的量子安全医疗数字孪生系统:实时多模态数据融合 ... [https://blog.csdn.net/2501_93420214/article/details/154933606]
- 34. Challenges in and Opportunities for Electronic Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10938158/]
- 35. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 36. Technologies for Interoperable Internet of Medical Things ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9533201/]
- 37. Comprehensive Guide to IoMT Device Security Protocols ... [https://medinaii.com/blog/Details?slug=comprehensive-guide-to-iomt-device-security-protocols-for-healthcare-professionals-and-administrators-20251026]
- 38. Social Determinants of Health in Digital Health Policies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12020528/]
- 39. Integration of Screening and Referral Tools for Social ... [https://www.jmir.org/2025/1/e73615]
- 40. Challenges and facilitators of electronic health record ... [https://www.sciencedirect.com/science/article/abs/pii/S1386505625003119]
- 41. EHR interoperability challenges and solutions [https://www.ehrinpractice.com/ehr-interoperability-challenges-solutions.html]
- 42. Benchmarking of multimodal single-cell omics data ... [https://www.nature.com/articles/s41588-025-02437-2]
- 43. Patient perspective on predictive models in healthcare [https://pmc.ncbi.nlm.nih.gov/articles/PMC11751774/]
- 44. The Hallmarks of Predictive Oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11969157/]
- 45. Deep learning models for ICU readmission prediction [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535055/]
- 46. Unlocking the potential of real-time ICU mortality prediction [https://www.nature.com/articles/s41746-025-02114-y]
- 47. Chronic Disease Prediction Using the Common Data Model [https://pmc.ncbi.nlm.nih.gov/articles/PMC11041444/]
- 48. Using Large Language Models for Chronic Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479051/]
- 49. UF BME and COM researchers publish innovative ICU ... [https://bme.ufl.edu/2025/09/08/uf-bme-and-com-researchers-publish-innovative-icu-prediction-model-in-nature-communications/]
- 50. Heterogeneous data integration: Challenges and ... [https://www.sciencedirect.com/science/article/pii/S2352340924008175]
- 51. Assessing Data Quality in Heterogeneous Health Care ... [https://medinform.jmir.org/2025/1/e75275]
- 52. Implementation and Updating of Clinical Prediction Models [https://pubmed.ncbi.nlm.nih.gov/40599890/]
- 53. 12 Data Quality Metrics to Measure Data Quality in 2025 [https://lakefs.io/data-quality/data-quality-metrics/]
- 54. Assessing Data Quality in Heterogeneous Health Care ... [https://pubmed.ncbi.nlm.nih.gov/41223409/]
- 55. 17 Best Data Integration Tools in 2025 (ETL, ELT & Real-Time ... [https://estuary.dev/blog/data-integration-tools/]
- 56. Top 17 Data Integration Tools in 2025 [https://www.adverity.com/blog/the-top-data-integration-tools-in-2025]
- 57. The 10 Best Data Quality Assessment Tools Of August 2025 [https://www.montecarlodata.com/blog-best-quality-assessment-tools/]
- 58. New study analyzes hospitals' use of AI-assisted predictive ... [https://www.sph.umn.edu/news/new-study-analyzes-hospitals-use-of-ai-assisted-predictive-tools-for-accuracy-and-biases/]
- 59. Methods for Addressing Missingness in Electronic Health ... [https://medinform.jmir.org/2025/1/e79307]
- 60. Innovative approach advances equity in health care AI [https://www.news-medical.net/news/20250905/Innovative-approach-advances-equity-in-health-care-AI.aspx]
- 61. Building AI Fairness by Reducing Algorithmic Bias [https://tepperspectives.cmu.edu/all-articles/building-ai-fairness-by-reducing-algorithmic-bias/]
- 62. Addressing AI bias: a human-centric approach to fairness [https://www.ey.com/en_us/insights/emerging-technologies/addressing-ai-bias-a-human-centric-approach-to-fairness]
- 63. Navigating fairness aspects of clinical prediction models [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535043/]
- 64. Methods for Addressing Missingness in Electronic Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617989/]
- 65. Handling missing data in clinical research [https://www.sciencedirect.com/science/article/pii/S0895435622002189]
- 66. Making sense of AI: bias, trust and transparency in pharma ... [https://www.drugtargetreview.com/article/183358/making-sense-of-ai-bias-trust-and-transparency-in-pharma-rd/]
- 67. Explainable Artificial Intelligence: A Perspective on Drug ... [https://www.mdpi.com/1999-4923/17/9/1119]
- 68. The application of explainable artificial intelligence in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12647564/]
- 69. eXplainable Artificial Intelligence (XAI): A Systematic Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609895/]
- 70. XAI-Units: Benchmarking Explainability Methods with ... [https://arxiv.org/html/2506.01059v1]
- 71. Quantitative comparison of explainable artificial ... [https://www.sciencedirect.com/science/article/pii/S0149197025000034]
- 72. Personalized health monitoring using explainable AI [https://www.nature.com/articles/s41598-025-15867-z]
- 73. Explainable Artificial Intelligence: A Systematic Review of ... [https://www.sciencedirect.com/science/article/pii/S2667305325001218]
- 74. External validation of prognostic models: what, why, how, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7857818/]
- 75. Using Different Data Sets to Test How Well Clinical ... [https://www.pcori.org/research-results/2016/using-different-data-sets-test-how-well-clinical-prediction-models-work-predict-patients-risk-heart-disease]
- 76. Internal and External Validation of the Generalizability ... [https://pubmed.ncbi.nlm.nih.gov/36764409/]
- 77. Predictive modeling identifies at-risk patients who may ... [https://www.lerner.ccf.org/news/article/?title=Predictive+modeling+addresses+healthcare+disparities%2C+identifies+at-risk+patients+who+may+need+stomach+cancer+screening+&id=4c5fd350d96423cb4a94ed1b7977fb82d5e7d70c]
- 78. The Generalizability of IR Experiments beyond the United ... [https://www.cambridge.org/core/journals/american-political-science-review/article/generalizability-of-ir-experiments-beyond-the-united-states/263CE4FF8EA7AAEC76A176BF3E05626C]
- 79. Path From Predictive Analytics to Improved Patient Outcomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC5645012/]
- 80. External validation: a simulation study to compare cross ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9464671/]
- 81. Practical Considerations and Applied Examples of Cross ... [https://ai.jmir.org/2023/1/e49023]
- 82. A Comparative Analysis of Cross-Validation Techniques for ... [https://www.mdpi.com/2079-9292/12/11/2371]
- 83. Quantitative Data Quality Assurance, Analysis and Presentation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12056448/]
- 84. Comparison of machine learning models with conventional ... [https://pubmed.ncbi.nlm.nih.gov/40269704/]
- 85. Comparing the Performance of Machine Learning Models ... [https://www.jmir.org/2025/1/e76215]
- 86. Predictive Analytics vs. Machine Learning Explained [https://ischool.syracuse.edu/predictive-analytics-vs-machine-learning/]
- 87. Predictive Analytics Vs. Machine Learning: Leveraging Both [https://www.thoughtspot.com/data-trends/ai/predictive-analytics-machine-learning]
- 88. Guide: Machine Learning (ML) vs. Predictive Analytics (PA) [https://www.domo.com/learn/article/ml-vs-pa]
- 89. Enhancing Patient Outcome Prediction Through Deep ... [https://pubmed.ncbi.nlm.nih.gov/40100249/]
- 90. Clinical Impact Research – how to choose experimental or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5152547/]
- 91. Predictive Healthcare 2025: Transforming Patient Outcomes [https://www.omdena.com/blog/predictive-healthcare-2025]
- 92. Methods for real-world studies of comparative effects [https://www.nice.org.uk/corporate/ecd9/chapter/methods-for-real-world-studies-of-comparative-effects]
- 93. Statistical analysis in method comparison studies part one [https://acutecaretesting.org/en/articles/statistical-analysis-in-method-comparison-studies-part-one]