Ensuring Data Integrity: A Comprehensive Guide to Quality Control Standards in Systems Biology
This article provides a comprehensive guide to quality control (QC) standards for researchers, scientists, and drug development professionals working with systems biology data.
Ensuring Data Integrity: A Comprehensive Guide to Quality Control Standards in Systems Biology
Abstract
This article provides a comprehensive guide to quality control (QC) standards for researchers, scientists, and drug development professionals working with systems biology data. It explores the foundational principles and critical need for robust QC frameworks to ensure data reproducibility and reliability. The content details practical, cross-platform methodologies for implementing QC in multi-omics workflows, including metabolomics and proteomics. It further addresses common troubleshooting scenarios and optimization strategies for pre-analytical, analytical, and post-analytical stages. Finally, the guide covers validation techniques, comparative performance assessment, and the establishment of community standards for longitudinal data quality, synthesizing key takeaways and future directions for biomedical and clinical research.
The Critical Role of Quality Control in Reproducible Systems Biology
Understanding the Reproducibility Challenge in Multi-Omics Data
Frequently Asked Questions (FAQs)
What is the core reproducibility problem in multi-omics research? The core problem stems from the heterogeneity of data sources. Multi-omics studies combine data from various technologies (e.g., genomics, proteomics, metabolomics), each with its own unique data structure, statistical distribution, noise profile, and batch effects. Integrating these disparate data types without standardized pre-processing protocols introduces variability that challenges the reproducibility of results [1].
Why is sample quality so crucial for reproducibility? The quality of the starting biological sample directly determines the fitness-for-purpose of all downstream omics data. Variations in sample collection, processing, and storage can introduce significant technical artifacts that obscure the true biological signal. Participating in Proficiency Testing (PT) programs is a critical step to ensure sample processing methods yield accurate, reliable, and trustworthy data [2].
How can I choose the right data integration method? There is no universal framework, and the choice depends on your data and biological question [1]. The table below summarizes key methods:
| Method Name | Type | Key Principle | Best For |
|---|---|---|---|
| MOFA [1] | Unsupervised | Identifies latent factors that capture shared and specific sources of variation across omics layers. | Exploring hidden structures without prior knowledge of sample groups. |
| DIABLO [1] | Supervised | Integrates datasets in relation to a known phenotype or category to identify biomarker panels. | Classifying patient groups or predicting clinical outcomes. |
| SNF [1] | Unsupervised | Fuses sample-similarity networks from each omics dataset into a single network. | Identifying disease subtypes based on multiple data types. |
| MCIA [1] | Unsupervised | Simultaneously projects multiple datasets into a shared dimensional space to find correlated patterns. | Jointly analyzing many omics datasets from the same samples. |
What are the key quality metrics for normalized multi-omics data? While standards are under development, quality control for normalized multi-omics profiles should assess the aggregated normalized data. This involves checking for batch effects, ensuring proper normalization across datasets, and confirming that the data quality reflects the overall proficiency of the study. The international standard ISO/TC 215/SC 1 is being developed to specify these procedures [3].
Troubleshooting Guides
Problem: Inconsistent Findings Between Omics Layers
Symptoms: A strong signal is detected at the RNA level (transcriptomics) but is absent or weak at the protein level (proteomics), leading to conflicting biological interpretations [1].
Solutions:
- Understand Biological Hierarchy and Timing: Recognize that different omics layers have distinct dynamics.
- The genome is largely static and foundational [4].
- The transcriptome is highly dynamic and can change rapidly in response to stimuli, sometimes requiring frequent assessment [4].
- The proteome is more stable due to longer protein half-lives and often requires a lower testing frequency [4].
- The metabolome provides a real-time snapshot of metabolic activity and can be highly variable [4].
- Implement Longitudinal Sampling: For dynamic processes, design experiments with multiple time points to capture the temporal relationship between molecular events (e.g., gene expression changes followed by protein abundance changes) [4].
- Use Vertical Integration Methods: Apply integration algorithms like DIABLO or MCIA that are designed for matched multi-omics data (data from the same samples). These methods are powerful for finding associations between non-linear molecular modalities [1].
Problem: Poor Technical Reproducibility Across Batches or Labs
Symptoms: The same analysis yields different results when performed at different times, by different personnel, or in different laboratories.
Solutions:
- Utilize Reference Materials: Incorporate well-characterized reference materials into every experimental run to monitor data quality over time and detect batch effects. The table below lists key resources:
- Participate in Proficiency Testing (PT): Engage in external quality assessment (EQA) schemes, such as those established by the Integrated BioBank of Luxembourg (IBBL), to compare your lab's sample processing performance against peers and drive continuous improvement [2].
- Adopt Standardized Pre-Processing: Develop and adhere to Standard Operating Procedures (SOPs) for each omics data type, from raw data processing to normalization, to minimize variability introduced by analytical choices [1] [2].
Problem: Difficulty Interpreting Integrated Results
Symptoms: Statistical models successfully integrate data and identify patterns, but translating these patterns into biologically meaningful insights is challenging.
Solutions:
- Conduct Multi-Omics Pathway and Network Analysis: Move beyond individual molecule lists. Use network-based approaches to visualize how genes, proteins, and metabolites from your integrated results interact within known biological pathways. This provides a systems-level context [5].
- Validate Findings with Functional Assays: Treat computational predictions as hypotheses. Use targeted experiments (e.g., siRNA knockdown, ELISA, or targeted mass spectrometry) to confirm the biological role of key molecules or pathways identified through integration.
- Leverage Multiple Integration Methods: Confirm the robustness of your findings by running your data through more than one integration algorithm (e.g., both MOFA and SNF). Consistent results across methods increase confidence in your conclusions [1].
Experimental Protocols for Quality Assessment
Protocol: External Quality Assessment via Proficiency Testing
Purpose: To ensure the fitness-for-purpose of biospecimen processing methods for downstream omics analysis and to benchmark laboratory performance against reference labs [2].
Methodology:
- Enrollment: Enroll the laboratory in a relevant PT program (e.g., the biospecimen processing scheme by IBBL).
- Sample Processing: Process the provided PT samples according to the laboratory's standard SOPs.
- Result Submission: Submit the processing results to the PT program organizers.
- Performance Analysis: Receive a z-score, which quantifies how much your lab's results deviate from the expected value or consensus of other laboratories.
- Corrective Action: If z-scores indicate significant deviation, implement corrective measures (e.g., refine SOPs, retrain staff, calibrate equipment) to improve performance in subsequent PT rounds.
The following workflow visualizes this cyclical process of continuous quality improvement:
Protocol: Intra-Laboratory Quality Control Using Reference Materials
Purpose: To monitor and control the quality of data generated from a specific omics platform over time, detecting batch effects and technical drift [2].
Methodology:
- Selection: Choose a commercially available or community-accepted reference material (see "Research Reagent Solutions" table above) relevant to your omics platform.
- Integration: Include the reference material in every batch of sample processing and data generation.
- Data Extraction: For each batch, analyze the reference material data and extract key quality metrics (e.g., number of features identified, accuracy of quantitation for known amounts, detection of expected variants).
- Trend Monitoring: Track these metrics over time using control charts. Gradual deterioration or sudden shifts in the metrics indicate that corrective measures are needed.
- Benchmarking: Compare the metrics obtained from your reference material data against established benchmarks or values from other labs to ensure inter-laboratory consistency.
The Multi-Omics Data Integration Workflow
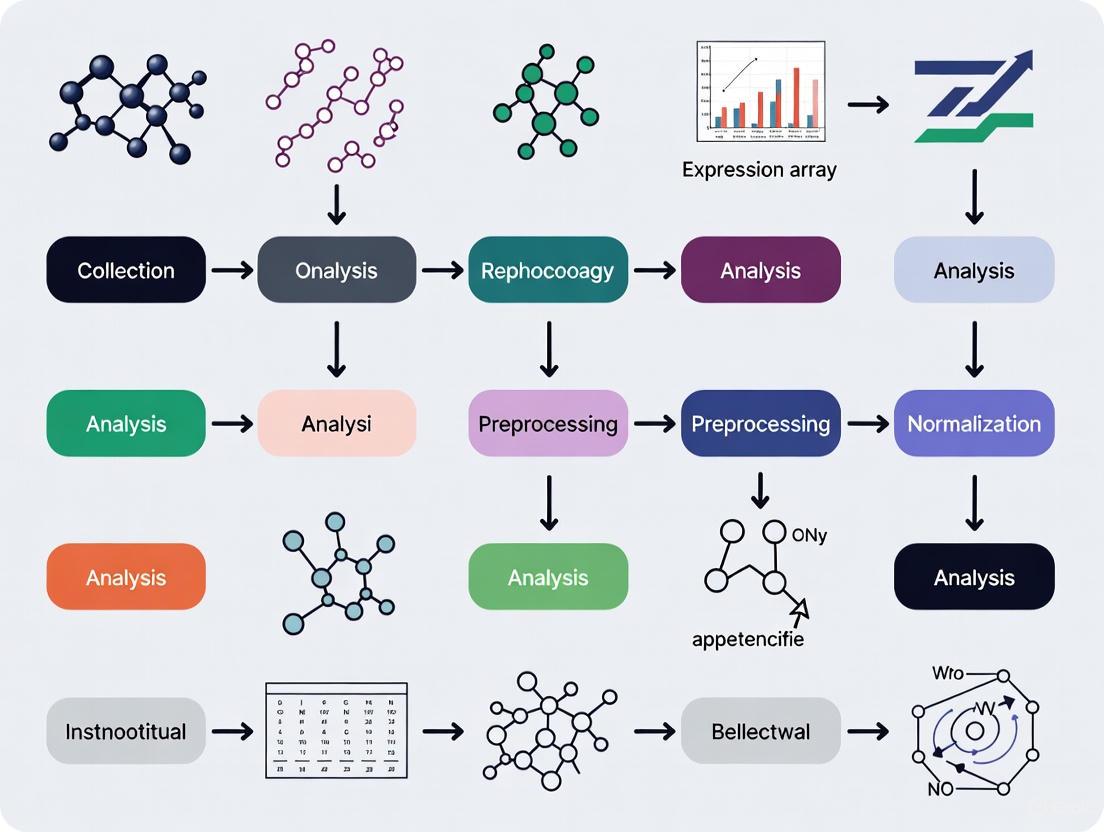
The diagram below outlines a generalized workflow for a reproducible multi-omics study, integrating the quality control measures and integration methods discussed. This workflow operates within the context of systems biology, aiming to understand the whole system rather than isolated parts [6].
Defining Quality Assurance (QA) vs. Quality Control (QC) in a Systems Context
In the data-intensive field of systems biology, where research relies on the integration of multiple heterogeneous datasets to model complex biological processes, a robust quality management system is not optional—it is essential for producing reliable, reproducible scientific insights [7]. Quality Assurance (QA) and Quality Control (QC) are two fundamental components of this system. Though often used interchangeably, they represent distinct concepts with different focuses and applications. Quality Assurance (QA) is a proactive, process-oriented approach focused on preventing defects by building quality into the entire research data lifecycle, from experimental design to data analysis. In contrast, Quality Control (QC) is a reactive, product-oriented process focused on identifying defects in specific data outputs, models, or results through testing and inspection [8] [9] [10]. For researchers, scientists, and drug development professionals, understanding and implementing both QA and QC is critical for ensuring data integrity, research reproducibility, and regulatory compliance in systems biology.
Core Concepts: Distinguishing QA from QC
The table below summarizes the key distinctions between Quality Assurance and Quality Control in the context of systems biology research.
Table 1: Key Differences Between Quality Assurance (QA) and Quality Control (QC)
| Feature | Quality Assurance (QA) | Quality Control (QC) |
|---|---|---|
| Focus | Processes and systems | Final products and outputs |
| Goal | Defect prevention | Defect identification and correction |
| Nature | Proactive | Reactive |
| Approach | Process-oriented | Product-oriented |
| Primary Activity | Planning, auditing, documentation, training | Inspection, testing, validation |
| Timeline | Throughout the entire data lifecycle | At specific checkpoints on raw or processed data |
The relationship between these functions can be visualized as a continuous cycle ensuring data quality from start to finish.
Figure 1: The Integrated QA/QC Workflow. This diagram illustrates how proactive Quality Assurance and reactive Quality Control function together within a research data lifecycle, forming a cycle of continuous quality improvement.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of systems biology experiments and subsequent quality control hinges on the use of specific reagents and materials. The following table details key resources and their functions in typical workflows.
Table 2: Key Research Reagent Solutions for Systems Biology Experiments
| Item | Primary Function & Application |
|---|---|
| Cultrex Basement Membrane Extract | Provides a 3D scaffold for culturing organoids (e.g., human intestinal, liver, lung) to better mimic in vivo conditions [11]. |
| Methylcellulose-based Media | A semi-solid medium used in Colony Forming Cell (CFC) assays to support the growth and differentiation of hematopoietic stem cells [11]. |
| DuoSet/Quantikine ELISA Kits | Tools for quantifying specific protein biomarkers (e.g., cytokines) in cell culture supernatants or patient samples with high specificity [11]. |
| Fluorogenic Peptide Substrates | Used in enzyme activity assays (e.g., for caspases or sulfotransferases); emission of fluorescence upon cleavage allows for kinetic measurement of enzyme activity [11]. |
| Flow Cytometry Antibody Panels | Antibody cocktails for immunophenotyping, allowing simultaneous characterization of multiple cell surface and intracellular markers (e.g., for T-cell subsets) [11]. |
| Luminex xMAP Assay Kits | Enable multiplexed quantification of dozens of analytes (e.g., cytokines, phosphorylated receptors) from a single small-volume sample [11]. |
Troubleshooting Guides: Addressing Common Data Quality Issues
Guide: Troubleshooting Poor Data Reproducibility
Problem: Inability to reproduce results from the same or similar datasets.
Question Flowchart:
Figure 2: Troubleshooting Poor Data Reproducibility
Guide: Troubleshooting Inconsistent Model Performance
Problem: Computational models yield inconsistent or unreliable predictions when applied to new data.
Question Flowchart:
Figure 3: Troubleshooting Inconsistent Model Performance
Frequently Asked Questions (FAQs)
Q1: What is the most significant challenge in bioinformatics QA today, and how can it be addressed? One of the most significant challenges is the volume and complexity of data, combined with the rapid evolution of technologies and methods [9]. High-throughput technologies can generate terabytes of data in a single experiment, making comprehensive QA time-consuming and computationally intensive. Furthermore, QA standards must continuously evolve to keep pace with new sequencing platforms and bioinformatics algorithms. Addressing this requires a focus on standardization and automation. Implementing standardized protocols and automated quality checks can significantly improve data reliability and reduce human error. The community is also moving toward AI-driven quality assessment and community-driven standards through initiatives like the Global Alliance for Genomics and Health (GA4GH) to establish common frameworks [9].
Q2: How can I convince my team to invest more time in documentation, a key QA activity? Emphasize that documentation is not bureaucratic, but a crucial tool for efficiency and reproducibility. Well-documented workflows [12]:
- Save time in the long run by preventing the need to reverse-engineer past analyses.
- Enable collaboration by allowing team members to understand and build upon each other's work.
- Are essential for regulatory compliance in drug development, providing the evidence required by bodies like the FDA [9].
- Directly address the "reproducibility crisis," where studies show over 50% of researchers have failed to reproduce their own experiments [9].
Q3: Our QC checks sometimes fail after a "successful" experiment. Is our QA process failing? Not necessarily. A robust QA process is designed to minimize the rate of QC failures, but it cannot eliminate them entirely. A QC failure provides critical feedback. This is when your QA system for investigation kicks in. A key QA activity is managing a Corrective and Preventive Action (CAPA) system [13]. When QC fails, the QA process should guide you to investigate the root cause of the deviation and implement actions to prevent its recurrence. Thus, a QC failure is a valuable opportunity for continuous improvement, triggered by QC but addressed by QA.
Q4: What are the minimum QA/QC steps I should implement for a new sequencing-based project? At a minimum, your workflow should include:
- Raw Data QA: Assess base call quality scores (e.g., Phred scores), read length distributions, GC content, and adapter contamination using tools like FastQC [9].
- Processing Validation: Check alignment rates, mapping quality, and coverage depth/uniformity after alignment [9].
- Metadata & Provenance Tracking: Ensure complete and accurate metadata describing experimental conditions, using community standards where possible (e.g., MIAME for microarray data) [7]. Document all data transformation steps.
- Analysis Verification: Apply statistical measures (e.g., p-values, confidence intervals) and validate results with independent methods or replicates where feasible [9].
Experimental Protocol: Implementing a QA/QC Workflow for Sequencing Data
Objective: To provide a detailed methodology for implementing a standardized Quality Assurance and Quality Control workflow for next-generation sequencing data within a systems biology project.
Background: Ensuring data integrity at the outset of a bioinformatics pipeline is critical for the validity of all downstream analyses and model building. This protocol outlines the key steps for QA and QC of raw and processed sequencing data.
Materials and Equipment:
- Raw sequencing data files (e.g., FASTQ format)
- High-performance computing (HPC) environment or server
- QA/QC software tools (e.g., FastQC, MultiQC)
- Reference genomes or transcripts (as required for the project)
- Data processing software (e.g., aligners like STAR or HISAT2)
Procedure:
Part A: Pre-analysis Quality Assurance (Proactive)
Define Quality Standards:
- Action: Prior to data generation, establish acceptance criteria for raw data. This includes minimum Phred quality scores (e.g., Q30), minimum read depth, maximum allowable adapter content, and maximum sequence duplication levels. Document these criteria in a Standard Operating Procedure (SOP).
- QA Rationale: This proactive step sets clear, objective benchmarks for data quality, preventing ambiguous judgments later [10].
Standardize Metadata:
- Action: Create a metadata spreadsheet using a structured format or controlled vocabulary (e.g., from the ISA-Tab framework or relevant minimum information checklist). Capture all experimental variables, sample information, and library preparation details.
- QA Rationale: Comprehensive and harmonized metadata is critical for data reuse, integration, and reproducibility, allowing others to understand the context of the data [7] [9].
Part B: Post-processing Quality Control (Reactive)
Assess Raw Data Quality:
- Action: Run FastQC on the raw FASTQ files from the sequencing run. Use MultiQC to aggregate and visualize results across all samples. Compare the results (e.g., per-base sequence quality, adapter contamination) against the pre-defined acceptance criteria from Part A.
- QC Rationale: This inspection identifies potential issues with the sequencing run or sample preparation that could compromise downstream analyses [9]. Data failing these criteria may need to be re-sequenced.
Validate Data Processing:
- Action: After alignment, collect and review key metrics. These include the overall alignment rate, the distribution of read mappings across genes/genome, and coverage uniformity. Compare these metrics across samples to identify outliers or batch effects.
- QC Rationale: These metrics verify the reliability of the alignment process and can reveal technical biases that need to be accounted for in the analysis [9].
Analysis and Interpretation:
- Any sample or dataset that fails to meet the pre-established quality thresholds must be flagged.
- The investigation into the root cause of the failure (e.g., sample degradation, library construction artifact) is a QA activity, often managed through a formal deviation or CAPA process [8].
- The final decision on whether to include, exclude, or re-process the data should be documented, providing an audit trail for the integrity of the research process.
The Impact of Pre-analytical Variables on Data Integrity
Troubleshooting Guides
A Systematic Approach to Pre-analytical Troubleshooting
Effective troubleshooting follows a logical progression from problem identification to solution implementation. This systematic approach minimizes experimental delays and preserves valuable samples [14].
Troubleshooting Steps Overview
| Step | Action | Key Questions to Ask |
|---|---|---|
| 1 | Identify the problem | What exactly is going wrong? Is the problem consistent? |
| 2 | List possible explanations | What are all potential causes? |
| 3 | Collect data | What do controls show? Were protocols followed? |
| 4 | Eliminate explanations | Which causes can be ruled out? |
| 5 | Experiment | How can remaining causes be tested? |
| 6 | Identify root cause | What is the definitive cause? |
Common Pre-analytical Scenarios and Solutions
Scenario 1: Inconsistent Biomarker Results in Multi-Site Trials
Problem: Variable results for the same analyte across different collection sites.
Troubleshooting Table
| Possible Cause | Investigation Method | Corrective Action |
|---|---|---|
| Different tourniquet application times | Review phlebotomy procedures | Standardize to <1 minute application [15] |
| Variable centrifugation speeds | Audit equipment calibration | Implement calibrated centrifuges with logs |
| Inconsistent sample processing delays | Track sample processing times | Establish ≤2 hour processing window |
| Improper storage temperatures | Monitor storage equipment | Use continuous temperature monitoring |
Scenario 2: Degraded Nucleic Acids in Biobanked Samples
Problem: Poor RNA/DNA quality despite proper freezing.
Troubleshooting Table
| Possible Cause | Investigation Method | Corrective Action |
|---|---|---|
| Multiple freeze-thaw cycles | Review sample access logs | Create single-use aliquots [16] |
| Slow freezing rate | Monitor freezing protocols | Implement controlled-rate freezing |
| Improper storage temperature | Validate freezer performance | Maintain consistent -80°C with backups |
| Contamination during handling | Review aseptic techniques | Implement UV workstation sanitation |
Frequently Asked Questions (FAQs)
Sample Collection & Handling
Q1: How does tourniquet application time affect potassium measurements?
Prolonged tourniquet application with fist clenching can cause pseudohyperkalemia, increasing potassium levels by 1-2 mmol/L. Case studies show values as high as 6.9 mmol/L in outpatient settings dropping to 3.9-4.5 mmol/L when blood was drawn via indwelling catheter without tourniquet [15].
Q2: What is the minimum blood volume required for common testing panels?
| Test Type | Recommended Volume | Notes |
|---|---|---|
| Clinical Chemistry (20 analytes) | 3-4 mL (heparin) 4-5 mL (serum) | Requires heparinized plasma or clotted blood [15] |
| Hematology | 2-3 mL (EDTA) | Adequate for complete blood count [15] |
| Coagulation | 2-3 mL (citrated) | Sufficient for standard coagulation tests [15] |
| Immunoassays | 1 mL | Can perform 3-4 different immunoassays [15] |
| Blood Gases (capillary) | 50 μL | Arterial blood for capillary sampling [15] |
Q3: Why do platelet counts affect potassium results?
During centrifugation and clotting, platelets can release potassium, causing falsely elevated serum levels. Whole blood potassium measurements provide accurate results, as demonstrated in a case where serum potassium was 8.0 mmol/L but whole blood was 2.7 mmol/L in a patient with thrombocytosis [15].
Sample Processing & Storage
Q4: How do multiple freeze-thaw cycles impact sample integrity?
Repeated freezing and thawing degrades proteins, nucleic acids, and labile metabolites. Each cycle causes:
- Protein denaturation and aggregation
- RNA fragmentation
- Loss of enzymatic activity
- Metabolic profile changes
Best practice: Create single-use aliquots during initial processing [16].
Q5: What quality indicators detect pre-analytical errors?
| Indicator | Target | Acceptable Rate |
|---|---|---|
| Sample hemolysis | <2% of samples | Varies by analyte [15] |
| Incorrect sample volume | <1% of samples | Per collection protocol [15] |
| Processing delays | <5% of samples | Within established windows [16] |
| Mislabeled samples | <0.1% of samples | Zero tolerance ideal [17] |
Data Integrity & Documentation
Q6: What documentation ensures pre-analytical data integrity?
The ALCOA+ framework provides comprehensive standards:
- Attributable: Who collected and processed the sample
- Legible: Permanent, readable records
- Contemporaneous: Recorded at time of activity
- Original: Primary records preserved
- Accurate: Error-free documentation
- Complete: All data including metadata
- Consistent: Sequential, dated records
- Enduring: Long-term preservation
- Available: Accessible for review [18]
Q7: How can I validate my pre-analytical workflow?
Implement these verification steps:
- Process Mapping: Document each step from collection to analysis
- Control Samples: Use standardized controls at each stage
- Periodic Audits: Review documentation and sample quality
- Equipment Monitoring: Log storage conditions and centrifuge calibration
- Staff Training: Regular competency assessments [19] [16]
The Scientist's Toolkit: Research Reagent Solutions
Essential Materials for Pre-analytical Quality Control
| Item | Function | Application Notes |
|---|---|---|
| EDTA Tubes | Preserves cell morphology for hematology | 2-3 mL volume adequate for hematology tests [15] |
| Sodium Citrate Tubes | Maintains coagulation factors | 2-3 mL sufficient for coagulation tests [15] |
| Heparin Tubes | Inhibits clotting for chemistry tests | 3-4 mL needed for 20 chemistry analytes [15] |
| Serum Separator Tubes | Provides clean serum for testing | 4-5 mL of clotted blood required [15] |
| PAXgene Tubes | Stabilizes RNA for molecular studies | Prevents RNA degradation during storage [16] |
| Temperature Loggers | Monitors storage conditions | Continuous monitoring with alarms [16] |
| Hemolysis Index Controls | Detects sample hemolysis | Visual assessment insufficient; quantitative needed [15] |
Data Integrity Framework Diagram
Frequently Asked Questions (FAQs)
Q1: What are the primary goals of the mQACC and the Metabolomics Society's Data Quality Task Group?
The Metabolomics Quality Assurance and Quality Control Consortium (mQACC) is a collaborative international effort dedicated to promoting the development, dissemination, and harmonization of best quality assurance (QA) and quality control (QC) practices in untargeted metabolomics. Its mission is to engage the metabolomics community to ensure data quality and reproducibility [20]. Key aims include identifying and cataloging QA/QC best practices, establishing mechanisms for the community to adopt them, promoting systematic training, and encouraging the development of applicable reference materials [20]. While the search results do not explicitly list a "Data Quality Task Group" (DQTG), the Metabolomics Society hosts several relevant Scientific Task Groups, such as the Data Standards Task Group and the Metabolite Identification Task Group, which focus on enabling efficient data formats, storage, and consensus on reporting standards to improve data quality and verification [21].
Q2: I am designing a large-scale LC-MS metabolomics study. What are the critical QA/QC steps I should integrate into my workflow?
For large-scale LC-MS studies, robust QA/QC is essential to manage technical variability and ensure data integrity. Key steps and considerations are detailed below.
- Pooled Quality Control (QC) Samples: Incorporate pooled QC samples throughout your analytical sequence. These are typically prepared by combining a small aliquot of all study samples and are injected repeatedly at the beginning for system conditioning and at regular intervals during the run. They are crucial for monitoring instrument stability, correcting for analytical drift, and assessing data quality [22] [23].
- Comprehensive Internal Standards (IS): Use a mixture of stable, isotopically labeled internal standards that cover a wide range of chemical classes and retention times. This helps monitor instrument performance and extraction efficiency. Note that in untargeted metabolomics, their use for direct signal correction may be limited due to potential matrix effects [22].
- Batch Design and Normalization: When analyzing hundreds of samples across multiple batches, careful batch design with randomized sample injection is critical. Systematic errors between batches must be corrected using post-acquisition normalization algorithms that rely on data from the pooled QC samples [22].
- Reference Materials (RMs): Utilize available reference materials (RMs) for process verification. These can include certified reference materials (CRMs), synthetic mixtures, or other standardized materials to help validate your analytical pipeline and enable cross-laboratory comparisons [23].
Q3: A reviewer has asked for evidence that our metabolomics data is of high quality. What should we report in our publication?
Engaging with journals to define reporting standards is a core objective of mQACC [24]. You should provide a detailed description of the QA/QC practices and procedures applied throughout your study. The Reporting Standards Working Group of mQACC is actively developing guidelines for this purpose. Key items to report include [24]:
- A clear description of the QC samples used (e.g., pooled QC, process blanks) and their preparation.
- The frequency and pattern of QC sample injection throughout the analytical sequence.
- The type and number of internal standards used.
- How the data derived from QC samples were analyzed, assessed, and interpreted to ensure acceptance criteria were met (e.g., intensity drift, retention time stability, missing data).
- The normalization and correction procedures applied to the data based on QC information.
Q4: Our laboratory is new to metabolomics. Where can we find established best practices for quality management?
The mQACC consortium is an excellent central resource. Its Best Practices Working Group is specifically tasked with identifying, cataloging, harmonizing, and disseminating QA/QC best practices for untargeted metabolomics [24]. This group conducts community workshops and literature surveys to define areas of common agreement and publishes living guidance documents [24]. Furthermore, the Metabolomics Society provides a hub for education and collaboration, with task groups focused on specific data quality challenges, such as metabolite identification and data standards [25] [21].
Troubleshooting Common Experimental Issues
Problem: Signal drift or drop in instrument response during a large-scale LC-MS sequence.
- Potential Causes: Gradual contamination of the ionization source, depletion of mobile phases, or column degradation over many injections [22].
- Solutions:
- Pre-sequence Preparation: Prepare large, single batches of mobile phase (e.g., 5L) to avoid variability during the run [22].
- Regular QC Monitoring: Use a sequence design that interlaces pooled QC samples every 5-10 experimental samples. Plot the feature intensities or total signal from these QCs to visualize and quantify drift [22] [26].
- Data Normalization: Apply post-acquisition correction algorithms (e.g., QC-SVRC, LOESS signal correction) using the data from the pooled QC samples to mathematically compensate for the observed signal drift [22].
Problem: High variability or failure of results in inter-laboratory comparisons.
- Potential Cause: A lack of standardized protocols and common reference materials leads to inconsistencies between platforms and laboratories [23].
- Solutions:
- Adopt Reference Materials (RMs): Integrate commercially available or community-developed RMs into your workflow. These materials act as a common benchmark to validate performance across different laboratories and instruments [23].
- Implement SOPs: Develop and adhere to detailed Standard Operating Procedures (SOPs) for sample preparation, instrumentation, and data processing to ensure consistency [9] [23].
- Community Engagement: Participate in interlaboratory studies and follow the guidelines being established by groups like the mQACC Reference Materials Working Group, which is actively working to define best-use practices for these materials [24] [23].
Problem: Difficulty in confidently identifying metabolites detected in an untargeted analysis.
- Potential Cause: Insufficient data or context provided in public repositories and publications to support metabolite annotation claims.
- Solutions:
- Follow Reporting Standards: Adhere to the metabolite identification reporting standards being developed by the Metabolite Identification Task Group of the Metabolomics Society. This ensures you report the necessary evidence (e.g., MS/MS spectrum, retention time) for different levels of confidence [21].
- Use Controlled Vocabularies: Engage with the MetFAIR Task Group, which focuses on improving the reproducible reporting of metabolite annotations using controlled vocabularies and structural identifiers, facilitating better data sharing and integration [21].
Experimental Protocol: Implementing a QC Framework for an LC-MS Metabolomics Study
The following protocol provides a detailed methodology for integrating a robust QA/QC system into a liquid chromatography-mass spectrometry (LC-MS) based untargeted metabolomics study, based on community best practices [24] [22] [23].
Sample Preparation and Experimental Design
- Sample Randomization: Randomize the injection order of all study samples to avoid confounding biological effects with batch effects.
- Pooled QC (PQC) Preparation: Create a pooled quality control sample by combining a small, equal volume from every individual sample in the study. If the cohort is extremely large, a representative subset of samples can be used to create the PQC [22].
- Internal Standard (IS) Mixture: Add a mixture of isotopically labeled internal standards to every sample (including blanks and QCs) prior to protein precipitation or extraction. Select standards to cover a broad range of chemical classes and retention times (e.g., labeled amino acids, carnitines, lipids, fatty acids) [22].
Instrumental Sequence Setup and Data Acquisition
- Sequence Structure: Structure the LC-MS sequence as follows:
- Conditioning: Start with several injections of the PQC to condition the system.
- Blank: Run a solvent blank to identify background signals.
- Balancing: Use a block-randomized design to balance sample groups across the sequence.
- QC Frequency: Inject the PQC sample repeatedly after every 5-10 experimental samples throughout the entire sequence to monitor performance [22].
- Reference Material: Include a well-characterized reference material (RM) at the beginning and end of the sequence, or in a separate quality audit run, to assess overall method and instrument performance against a known standard [23].
Data Processing and Quality Assessment
- Quality Metrics Calculation: After processing raw data, calculate the following metrics from the PQC samples:
- Feature-wise Relative Standard Deviation (RSD): Determine the percentage of metabolic features in the PQC with an RSD below 20% or 30%. A high number of low-RSD features indicates good analytical precision.
- Retention Time Drift: Measure the stability of retention times for internal standards and endogenous features in the PQC.
- Total Signal Intensity: Track the overall signal response in the PQC over the sequence to identify global drift.
- Data Normalization: Apply a quality control-based normalization method (e.g., using the
pqnmethod in R, or LOESS regression based on PQC samples) to correct for systematic signal drift identified in the sequence [22].
The logical workflow for this protocol, from preparation to assessment, is designed to systematically control for technical variability.
Research Reagent Solutions for Metabolomics QC
The table below details key materials essential for implementing a robust quality control system in metabolomics, as championed by mQACC and related initiatives.
| Item | Function & Application in QA/QC |
|---|---|
| Pooled Quality Control (PQC) Sample | A pooled aliquot of all study samples. Injected repeatedly throughout the analytical sequence to monitor instrument stability, correct for signal drift, and assess the precision of metabolic feature measurements [22] [23]. |
| Isotopically Labeled Internal Standards | Stable isotope-labeled compounds (e.g., with ²H, ¹³C) not naturally found in the sample. Added to all samples to monitor instrument performance, extraction efficiency, and matrix effects. They should cover a wide range of the metabolome [22]. |
| Certified Reference Materials (CRMs) | Highly characterized materials with a certificate of analysis. Used to validate analytical methods, assess accuracy, and enable cross-laboratory comparability of results [23]. |
| Long-Term Reference (LTR) QC | A stable, study-independent QC material (e.g., a commercial surrogate or a large pooled sample) analyzed over long periods across multiple studies to track laboratory performance and ensure consistency over time [23]. |
| Process Blanks | Samples containing only the extraction solvents and reagents. Used to identify and filter out background signals and contaminants originating from the sample preparation process or solvents [22]. |
The 'FAIR' Guiding Principles for Systems Biology Data Management
The FAIR Guiding Principles are a set of four foundational principles—Findability, Accessibility, Interoperability, and Reusability—designed to improve the management and stewardship of scientific data and other digital research objects, including algorithms, tools, and workflows [27]. Originally published in 2016 by a diverse group of stakeholders from academia, industry, funding agencies, and scholarly publishers, these principles provide a concise and measurable framework to enhance the reuse of data holdings [27] [28].
A key differentiator of the FAIR principles is their specific emphasis on enhancing the ability of machines to automatically find and use data, in addition to supporting its reuse by human researchers [27] [29]. This machine-actionability is critical in data-rich fields like systems biology, where the volume, complexity, and speed of data creation exceed human capacity for manual processing.
The following table summarizes the core objectives of each FAIR principle.
| FAIR Principle | Core Objective | Key Significance for Systems Biology |
|---|---|---|
| Findable | Data and metadata are easy to find for both humans and computers. | Enables discovery of datasets across departments and collaborators, laying the groundwork for efficient knowledge reuse [29] [28]. |
| Accessible | Data can be retrieved by users using standard protocols, with clear authentication and authorization where necessary. | Supports implementing infrastructure for controlled data access at scale, ensuring security and compliance [29] [28]. |
| Interoperable | Data can be integrated with other data and used with applications or workflows for analysis. | Vital for multi-modal research, allowing integration of diverse datasets (e.g., genomic, imaging, clinical) [29] [28]. |
| Reusable | Data and metadata are well-described so they can be replicated or combined in different settings. | Maximizes the utility and impact of datasets for future research, ensuring reproducibility [29] [28]. |
Experimental Protocols: Implementing FAIR in a Systems Biology Workflow
This section provides a detailed methodology for applying the FAIR principles to a typical systems biology experiment involving multi-omics data integration.
Protocol: FAIRification of a Multi-Omics Dataset
Aim: To manage a dataset comprising transcriptomic and proteomic profiles from a drug perturbation study in a FAIR manner to ensure its future discoverability and utility.
Materials and Reagents:
- Cell Line: HEK293 (or other relevant model system)
- Perturbation Agent: Small molecule drug candidate (e.g., a kinase inhibitor)
- RNA Extraction Kit: (e.g., Qiagen RNeasy Kit)
- Protein Lysis Buffer: RIPA buffer supplemented with protease and phosphatase inhibitors
- Next-Generation Sequencing Platform: (e.g., Illumina NovaSeq) for RNA-seq
- Mass Spectrometer: (e.g., Thermo Fisher Orbitrap Exploris) for quantitative proteomics
Methodology:
- Experimental Design and Metadata Planning:
- Before data generation, define the minimum reporting standards required for your data types (e.g., MIAME for transcriptomics, MIAPE for proteomics).
- Create a data dictionary using community-standard ontologies (e.g., EDAM for data types, UO for units, NCBI Taxonomy for organisms).
Data Generation and Curation:
- Generate raw data (e.g., FASTQ files for RNA-seq, .raw files for proteomics).
- Process raw data through established pipelines (e.g., RNA-seq alignment with STAR, proteomics identification with MaxQuant). Record all software versions and parameters.
- Derive processed data (e.g., gene count matrices, protein abundance values).
Assignment of Persistent Identifiers:
- Obtain a Digital Object Identifier (DOI) for the overall dataset from a repository like Zenodo or your institutional repository.
- For individual data files and components, use universally unique identifiers (UUIDs).
Metadata Annotation and Rich Description:
- Describe the dataset with rich metadata, including:
- Project Title, Description, and Funding Source.
- Creator and ORCID IDs.
- Keywords from ontologies like MeSH or EDAM.
- Detailed methodology linking to this protocol.
- Data Access and License Information (e.g., CCO 1.0 Universal for public domain, or a custom license for restricted access).
- Describe the dataset with rich metadata, including:
Data Deposition in a Public Repository:
- Deposit the data in a recognized, community-accepted repository.
- Recommended Repositories:
- Omics Discovery Index (OmicsDI): A cross-domain resource.
- ArrayExpress or GEO for transcriptomics data.
- PRIDE for proteomics data.
Provenance Tracking:
- Use a workflow management system (e.g., Nextflow, Snakemake) that automatically captures the provenance of all data transformations, from raw data to final results.
The Scientist's Toolkit: Essential Research Reagent Solutions
The table below details key materials and their functions in the context of generating and managing FAIR systems biology data.
| Research Reagent / Material | Function in Experiment | Role in FAIR Data Management |
|---|---|---|
| Sample Barcoding Kits | Enables multiplexing of samples during high-throughput sequencing or mass spectrometry. | Provides a traceable link between a physical sample and its digital data file, supporting Reusability through clear sample provenance [27]. |
| Stable Cell Lines | Provides a consistent and reproducible biological model for perturbation studies. | Reduces experimental variability, ensuring data is Reusable and reproducible by other researchers [28]. |
| Standardized Buffers & Kits | Ensures consistency in sample preparation (e.g., lysis, nucleic acid extraction) across experiments and labs. | Promotes Interoperability by minimizing technical artifacts that would prevent data integration from different batches or studies [28]. |
| Controlled Vocabularies & Ontologies | A set of standardized terms (e.g., Gene Ontology, Cell Ontology) for annotating data. | Critical for Findability and Interoperability, as it allows machines to accurately understand and link related data concepts [27] [28]. |
| Persistent Identifier Services | A service (e.g., DataCite, DOI) that assigns a permanent, globally unique identifier to a dataset. | The cornerstone of Findability, ensuring the dataset can always be located and cited, even if its web URL changes [29] [28]. |
FAIR Data Management: Troubleshooting Guides and FAQs
FAQ 1: Our data is confidential. Can it still be FAIR? Answer: Yes. FAIR is not synonymous with "open." Data can be Accessible only under specific conditions, such as behind a secure authentication and authorization layer [28]. The key is that the metadata should be openly findable, describing the data's existence and how to request access. The path to access should be clear, even if the data itself is restricted.
FAQ 2: We have legacy data from past projects that lacks rich metadata. Is it too late to make it FAIR? Answer: It is not too late, but it can be a challenge. A practical approach is to perform a "FAIRification" process [28]:
- Inventory: Catalog all existing datasets.
- Annotate: Manually or semi-automatically enrich the data with as much metadata as possible using current standards.
- Identify: Assign persistent identifiers (e.g., DOIs) to the curated datasets.
- Deposit: Store the enhanced datasets and metadata in a suitable repository. While time-consuming, this process maximizes the return on investment from past research [28].
FAQ 3: What is the most common mistake in trying to be FAIR? Answer: A common mistake is focusing only on the human-readable aspects of data and neglecting machine-actionability. This includes using PDFs for data tables (which are difficult for machines to parse), free-text fields without controlled vocabulary, or failing to use resolvable, persistent identifiers. The FAIR principles require data to be not just human-understandable, but also machine-processable [27] [29].
FAQ 4: How do FAIR principles support AI and machine learning in drug discovery? Answer: FAIR data provides the foundational layer required for effective AI. AI and ML models require large volumes of well-structured, high-quality data. By making data Interoperable and Reusable, FAIR principles allow for the harmonization of diverse data types (genomics, imaging, EHRs), creating the large, integrated datasets needed to train robust models. This accelerates target identification and biomarker discovery [28].
Visualization of FAIR Workflows and Relationships
Implementing Robust QC Frameworks Across Omics Technologies
In systems biology research, ensuring the integrity and reliability of data is paramount. Quality Control (QC) samples are essential tools that provide confidence in analytical results, from untargeted metabolomics to genomic studies. These samples help researchers distinguish true biological variation from technical noise, a critical consideration for drug development professionals who rely on this data for decision-making. The overarching goal of implementing a robust QC protocol is to ensure research reproducibility, a fundamental challenge in modern science where a significant percentage of researchers have reported difficulties in reproducing experiments [9].
Quality assurance (QA) and quality control (QC) represent complementary components of quality management. According to accepted definitions, quality assurance comprises the proactive processes and practices implemented before and during data acquisition to provide confidence that quality requirements will be fulfilled. In contrast, quality control refers to the specific measures applied during and after data acquisition to confirm that these quality requirements have been met [30]. For systems biology data research, this distinction is crucial in building a comprehensive framework for data quality.
Core QC Sample Types and Their Applications
Defining the Fundamental QC Samples
Effective QC strategies in systems biology incorporate several types of reference samples, each serving a distinct purpose in monitoring and validating analytical performance.
Pooled QC Samples: Created by combining equal aliquots from all study samples, pooled QCs represent the "average" sample composition in a study. When analyzed repeatedly throughout the analytical sequence, they monitor system stability and performance over time, helping to identify technical drift, batch effects, and variance among replicates [30] [9].
Blank Samples: These samples contain all components except the analyte of interest, typically using the same solvent as the sample reconstitution solution. Blanks are essential for identifying carryover from previous injections, contaminants in solvents or reagents, and system artifacts such as column bleed or plasticizer leaching [30] [31].
Standard Reference Materials (SRMs): These are well-characterized samples with known properties and concentrations, often obtained from certified sources like the National Institute of Standards and Technology (NIST). SRMs serve as validation tools for bioinformatics pipelines, allowing researchers to identify systematic errors or biases in data processing and analysis workflows [9].
Quantitative Metrics for QC Sample Assessment
Table 1: Key Quality Metrics for Different Analytical Platforms in Systems Biology
| Analytical Platform | QC Sample Type | Key Metrics | Acceptance Criteria Examples |
|---|---|---|---|
| Next-Generation Sequencing | Pooled QC, SRMs | Base call quality scores (Phred), read length distributions, alignment rates, coverage depth and uniformity | Phred score > Q30, alignment rates > 90%, coverage uniformity across targets |
| Mass Spectrometry-Based Metabolomics | Pooled QC, Blanks, SRMs | Retention time stability, peak intensity variance, mass accuracy, signal-to-noise ratio | <30% RSD for peak intensities in pooled QCs, mass accuracy < 5 ppm |
| Nuclear Magnetic Resonance (NMR) Spectroscopy | Pooled QC, SRMs | Spectral line width, signal-to-noise ratio, chemical shift stability, resolution | Line width consistency, chemical shift deviation < 0.01 ppm |
Table 2: Troubleshooting Common QC Sample Issues
| Problem | Potential Causes | Investigation Steps | Corrective Actions |
|---|---|---|---|
| Deteriorating Signal in Pooled QCs | Column degradation, source contamination, reagent instability | Check system suitability tests, analyze SRMs, review QC charts | Clean ion source, replace column, refresh mobile phases |
| Contamination in Blank Samples | Carryover, solvent impurities, vial contaminants | Run blank injections, check autosampler cleaning protocol, test different solvent batches | Implement rigorous wash protocols, use high-purity solvents, replace vial types |
| Shift in Reference Material Values | Calibration drift, method modification, instrumental variance | Compare with historical data, run independent validation, check calibration standards | Recalibrate system, verify method parameters, service instrument |
Implementation and Troubleshooting Guide
Frequently Asked Questions on QC Sample Implementation
Q1: How should pooled QC samples be prepared and implemented throughout an analytical sequence?
Pooled QC samples should be prepared by combining equal aliquots from a representative subset of all study samples (typically 10-50μL from each) to create a homogeneous pool that reflects the average composition of your sample set. This pooled QC should be analyzed at regular intervals throughout the analytical sequence—typically at the beginning, after every 4-10 experimental samples, and at the end of the batch. The frequency should be increased for less stable analytical platforms or longer sequences. The results from these repeated injections are used to monitor system stability and performance over time [30].
Q2: What is the most effective approach when QC results indicate an out-of-control situation?
The worst habits when encountering QC failures are automatically repeating the control or testing a new vial of control material without systematic investigation. These approaches often resolve the problem temporarily without identifying the root cause. Instead, implement a structured troubleshooting approach: first, clearly define the deviation by comparing current results with established acceptance criteria and historical data. Then, systematically investigate potential sources—check sample preparation steps, mobile phase composition, instrument performance, and column integrity. Make one change at a time while testing to identify the true cause. Frequent recalibration should also be avoided as it can introduce new systematic errors without addressing underlying issues [32] [31].
Q3: How can ghost peaks or unexpected signals in blank samples be resolved?
Ghost peaks in blanks typically originate from several sources: carryover from previous injections, contaminants in mobile phases or solvents, column bleed, or system hardware contamination. To resolve these issues: run blank injections to characterize the ghost peaks; perform intensive autosampler cleaning including the injection needle and loop; prepare fresh mobile phases with high-purity solvents; and consider replacing or cleaning the column if bleed is suspected. Using a guard column or in-line filter can help capture contaminants early and protect the analytical column [31].
Q4: What are the key considerations for incorporating Standard Reference Materials into QC protocols?
Standard Reference Materials should be selected to match the analytes of interest and matrix composition as closely as possible. They should be analyzed at the beginning of a study to validate analytical methods and periodically throughout to monitor long-term performance. When using SRMs, it's critical to: document the source and lot numbers; prepare SRMs according to certificate instructions; track performance against established tolerance limits; and investigate any deviations from expected values. SRMs are particularly valuable for technology transfer between laboratories and for verifying method performance when implementing new protocols [9].
Experimental Protocol: Implementing a Comprehensive QC Strategy for Untargeted Metabolomics
Objective: To establish a robust QC system for an untargeted metabolomics study using liquid chromatography-mass spectrometry.
Materials Needed:
- Test samples for analysis
- Appropriate solvents for extraction and reconstitution
- Vials for sample collection and storage
- Internal standards
- Certified reference materials for key metabolites
- Quality control materials
Procedure:
Sample Preparation:
- Prepare experimental samples using standardized extraction protocols.
- Create a pooled QC sample by combining equal aliquots (e.g., 10-20 μL) from each experimental sample.
- Prepare blank samples using the same solvent as for sample reconstitution.
- Prepare standard reference materials according to certificate instructions.
Sequence Design:
- Begin sequence with system equilibration injections (4-6 injections of pooled QC).
- Analyze blank samples to establish background signals.
- Analyze standard reference materials to validate method performance.
- Implement a randomized sample sequence with pooled QC samples inserted every 4-8 experimental samples.
- Include procedural blanks at regular intervals to monitor contamination.
- Conclude sequence with additional pooled QC and reference material analyses.
Data Acquisition and Monitoring:
- Monitor retention time stability for internal standards and reference materials.
- Track peak intensity variance in pooled QC samples (typically <20-30% RSD).
- Assess mass accuracy against theoretical values for reference compounds.
- Evaluate chromatographic peak shape and symmetry.
Quality Assessment:
- Calculate coefficient of variation for features detected in pooled QC samples.
- Perform principal component analysis on pooled QC samples to identify outliers.
- Compare measured values for reference materials against certified ranges.
- Document all quality metrics and any deviations from acceptance criteria.
Troubleshooting Note: If pooled QC samples show progressive deterioration in signal intensity or retention time shifts, consider column aging, source contamination, or mobile phase degradation as potential causes. Implement appropriate maintenance procedures before continuing with sample analysis [30] [31].
Workflow Visualization and Reagent Solutions
QC Sample Implementation Workflow
QC Troubleshooting Pathway
Essential Research Reagent Solutions for QC Protocols
Table 3: Key Reagents and Materials for Quality Control Implementation
| Reagent/Material | Function in QC Protocol | Application Examples |
|---|---|---|
| Certified Reference Materials | Provides ground truth for method validation and calibration | NIST Standard Reference Materials, certified metabolite standards |
| Internal Standard Mix | Corrects for instrument variability and sample preparation losses | Stable isotope-labeled analogs of target analytes |
| High-Purity Solvents | Minimize background interference and contamination | LC-MS grade water, acetonitrile, methanol |
| Quality Control Pooled Plasma | Assesses analytical performance across multiple batches | Commercially available human pooled plasma from certified vendors |
| System Suitability Test Mix | Verifies instrument performance before sample analysis | Compounds with known retention and response characteristics |
| Mobile Phase Additives | Maintains consistent chromatographic performance | Mass spectrometry-grade acids, buffers, and ion-pairing reagents |
Implementing robust QC samples aligns with the FAIR principles (Findable, Accessible, Interoperable, Reusable) that are increasingly important in systems biology research [33]. Proper documentation of QC protocols, including preparation methods, acceptance criteria, and results, ensures that data meets quality standards for regulatory submissions and collaborative research. As bioinformatics continues to evolve with AI-driven quality assessment and community-driven standards, the fundamental role of pooled QCs, blanks, and standard reference materials remains critical for producing trustworthy scientific insights in drug development and biological research [9]. By adhering to these best practices for QC sample design and implementation, researchers can significantly enhance the reliability and reproducibility of their systems biology data.
Frequently Asked Questions (FAQs)
Q1: My RNA-seq data fails the "sequence quality" check in the quality control report. The per-base sequence quality is low at the 3' end of the reads. What does this mean, and what should I do?
A1: Low quality at the 3' end of reads is a common issue often caused by degradation of RNA samples or issues with the sequencing chemistry. You should:
- Check RNA Integrity: Verify the RNA Integrity Number (RIN) of your original sample. A RIN below 7 may indicate degradation.
- Trimming: Use a quality control tool like FastQC to generate the report and a trimming tool like Trimmomatic or Cutadapt to remove low-quality bases from the ends of the sequences. This prevents errors in downstream analysis like alignment or transcript assembly [34].
Q2: After aligning my sequencing data to a reference genome, the alignment rate is unexpectedly low. What are the potential causes and solutions?
A2: A low alignment rate can stem from several factors. Follow this structured approach to isolate the issue [35] [36]:
- Verify Reference Genome: Ensure you are using the correct reference genome build and that it is not contaminated.
- Check Sample Identity: Confirm that your sequencing data is from the same species as the reference genome. Cross-species contamination can cause low alignment.
- Inspect Quality Scores: Re-examine your initial quality control metrics. High levels of adapter contamination or poor sequence quality will lower alignment rates. Trim the data if necessary.
- Try a Different Aligner: Test with a different alignment tool (e.g., if using STAR, try HISAT2) to rule out tool-specific issues [34].
Q3: During the variant calling workflow, my tool outputs an error about "incorrect file format." How can I troubleshoot this?
A3: Bioinformatics tools are often specific about their input file formats and versions.
- Validate File Format: Use a tool like SAMtools to check the integrity and format of your input file (e.g., BAM file) [34].
- Check File Versions: Ensure all files in your pipeline are from compatible versions. For example, an older version of a BAM file might not be compatible with a newer variant caller.
- Consult Documentation: Refer to the documentation of the specific tool generating the error. It will often list exact format requirements. Reproducible workflow platforms like nf-core provide version-controlled pipelines that help avoid these compatibility issues [34].
Troubleshooting Guides
Guide 1: Troubleshooting Poor Data Quality in Sequencing Experiments
Problem: Quality control tools (e.g., FastQC) report poor per-base sequence quality, high adapter contamination, or overrepresented sequences.
Resolution Process:
- Understand the Problem: Run FastQC on your raw FASTQ files to identify the specific quality issues [34].
- Isolate the Issue [35] [36]:
- Poor Quality Scores: If quality drops at the ends, it is likely a sequencing chemistry issue. If the drop is uniform, the sample may be degraded.
- Adapter Contamination: This indicates that the library preparation did not efficiently remove adapter sequences.
- Overrepresented Sequences: This can point to contamination (e.g., ribosomal RNA, vector sequence) or a low-diversity library.
- Find a Fix or Workaround:
- For poor quality and adapter contamination, use a trimming tool. The table below summarizes common QC metrics and their implications [34].
- For overrepresented sequences, you may need to remove the contaminated reads or, if the issue is severe, re-prepare the library.
Table 1: Common Sequencing Data Quality Issues and Solutions
| QC Metric | Problematic Output | Potential Cause | Recommended Solution |
|---|---|---|---|
| Per-base Sequence Quality | Low scores (Q<20) at read ends | Sequencing chemistry; degraded RNA | Trim reads using Trimmomatic or Cutadapt [34] |
| Adapter Content | High adapter sequence percentage | Inefficient adapter removal during library prep | Trim adapter sequences [34] |
| Overrepresented Sequences | A few sequences make up a large fraction of data | Sample contamination or low library complexity | Identify sequences via BLAST; redesign experiment if severe |
| Per-sequence GC Content | Abnormal distribution compared to reference | General contamination or PCR bias | Investigate sample purity and library preparation steps |
Guide 2: Resolving Workflow and Code Generation Errors
Problem: A bioinformatics pipeline (e.g., a Snakemake or Nextflow script) fails to execute, or a custom script for analysis does not produce the expected output.
Resolution Process:
- Understand the Problem [36]:
- Read the Error Message: Copy the exact error message from the terminal or log file.
- Check the Logs: Most workflow tools and scripts generate detailed logs. Look for warnings or errors that precede the final failure.
- Isolate the Issue [35]:
- Reproduce the Issue: Run the failing command or script in a minimal, clean environment (e.g., a new container) to rule out environment-specific problems.
- Simplify the Problem: If a complex script is failing, comment out sections and run it step-by-step to identify the exact failing command.
- Check Dependencies: Verify that all required software, packages, and libraries are installed and are the correct versions. Using containerized environments like Biocontainers can prevent dependency conflicts [34].
- Find a Fix or Workaround:
- Search for Similar Issues: Look up the error message in bioinformatics forums like Biostars or the software's GitHub repository [34].
- Consult Reproducible Workflows: Refer to established, version-controlled workflows from repositories like nf-core for examples of correctly implemented steps [34].
- Implement a Fix: Based on your research, apply the fix, which could involve updating a tool, changing a file path, or correcting a syntax error in your code.
Experimental Protocols
Protocol 1: Quality Control and Trimming of Raw Sequencing Reads
Objective: To assess the quality of raw sequencing data (FASTQ files) and remove low-quality bases and adapter sequences to ensure robust downstream analysis.
Methodology:
- Quality Assessment:
- Run FastQC on your raw FASTQ files to generate a comprehensive quality report.
- Examine the HTML output for issues detailed in Table 1.
- Trimming and Cleaning:
- Use Trimmomatic (for Illumina data) to perform the following:
- Remove Illumina adapter sequences.
- Trim leading and trailing low-quality bases (below quality score 3).
- Scan the read with a 4-base wide sliding window and cut when the average quality per base drops below 20.
- Drop reads that are shorter than 36 bases after trimming.
- Example command:
java -jar trimmomatic.jar PE -phred33 input_forward.fq.gz input_reverse.fq.gz output_forward_paired.fq.gz output_forward_unpaired.fq.gz output_reverse_paired.fq.gz output_reverse_unpaired.fq.gz ILLUMINACLIP:adapters.fa:2:30:10 LEADING:3 TRAILING:3 SLIDINGWINDOW:4:20 MINLEN:36
- Use Trimmomatic (for Illumina data) to perform the following:
- Post-Trimming Quality Assessment:
- Run FastQC again on the trimmed FASTQ files to confirm that quality issues have been resolved.
Protocol 2: Alignment of RNA-seq Data to a Reference Genome
Objective: To accurately map high-quality, trimmed RNA-seq reads to a reference genome for subsequent transcript assembly and quantification.
Methodology:
- Tool Selection: Select an appropriate aligner. For RNA-seq data, splice-aware aligners are required. STAR is recommended for its high accuracy and speed [34].
- Generate Genome Index:
- First, the reference genome must be indexed. This is a one-time step for each genome/annotation combination.
- Example STAR command for genome indexing:
STAR --runMode genomeGenerate --genomeDir /path/to/genomeDir --genomeFastaFiles reference_genome.fa --sjdbGTFfile annotation.gtf --sjdbOverhang 99
- Align Reads:
- Run the alignment using the indexed genome and the trimmed FASTQ files.
- Example STAR command for alignment:
STAR --genomeDir /path/to/genomeDir --readFilesIn output_forward_paired.fq.gz output_reverse_paired.fq.gz --readFilesCommand zcat --outFileNamePrefix aligned_output --outSAMtype BAM SortedByCoordinate --quantMode GeneCounts
- Post-Alignment QC:
- Use tools like SAMtools to index the resulting BAM file and generate alignment statistics.
- Use Qualimap to perform a more detailed RNA-seq QC on the BAM file, checking for genomic coverage and bias.
Workflow Visualization
Multi-Step QC Protocol
Troubleshooting Logic
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for a Sequencing QC Workflow
| Item Name | Function / Role in the Protocol |
|---|---|
| High-Quality RNA Sample | The starting material; its integrity (RIN > 7) is critical for generating high-quality sequencing libraries and avoiding 3' bias. |
| Library Preparation Kit | A commercial kit (e.g., Illumina TruSeq) containing enzymes and buffers to convert RNA into a sequenceable library, including adapter ligation. |
| Trimmomatic | A flexible software tool used to trim adapters and remove low-quality bases from raw FASTQ files, cleaning the data for downstream analysis [34]. |
| STAR Aligner | A splice-aware alignment software designed specifically for RNA-seq data that accurately maps reads to a reference genome, allowing for transcript discovery and quantification [34]. |
| Reference Genome FASTA | The canonical DNA sequence of the organism being studied, against which sequencing reads are aligned to determine their genomic origin. |
| Annotation File (GTF/GFF) | A file that describes the locations and structures of genomic features (genes, exons, etc.), used during alignment and for quantifying gene counts. |
| Biocontainer | A containerized version of a bioinformatics tool (e.g., as a Docker or Singularity image) that ensures a reproducible and conflict-free software environment [34]. |
Robust Quality Control (QC) is the foundation of reliable, reproducible data in systems biology. For metabolomics and proteomics, platform-specific QC strategies are essential to manage the complexity of the data and mitigate technical variability, ensuring that observed differences reflect true biology rather than analytical artifacts. This guide details best-practice QC protocols for both fields, providing researchers and drug development professionals with actionable troubleshooting frameworks to enhance data quality.
Metabolomics Quality Control (QC) Best Practices
The QComics Protocol
QComics is a robust, sequential workflow for monitoring and controlling data quality in metabolomics studies. Its multi-step process addresses common pitfalls, from background noise to preanalytical errors [37].
Core Steps of the QComics Workflow:
- Initial Data Exploration: Detect contaminants, batch drifts, and "out-of-control" observations.
- Handling Missing Data: Differentiate between missing values and truly absent biological signals to prevent loss of information.
- Outlier Removal: Identify and remove outlying samples that can skew results.
- Monitoring Quality Markers: Use specific chemical descriptors to address preanalytical errors from sample collection or storage.
- Final Data Quality Assessment: Evaluate overall data quality in terms of precision and accuracy.
Experimental Protocol for QComics Implementation:
Sample Preparation:
- Procedural Blanks: Prepare by replacing the biological sample with water during extraction, using the same chemicals and SOPs. Analyze five blanks at the start and end of the sequence to assess background noise and carryover [37].
- QC Samples: Prepare a pooled QC sample by mixing equal aliquots of all study samples. If pooling is not viable, use a surrogate bulk representative sample [37].
LC-MS Analysis Sequence:
- Inject five consecutive procedural blanks for system stabilization [37].
- Inject at least five consecutive QC samples to condition the system for the study matrix [37].
- Analyze real samples in a randomized order. Intercalate a QC sample after every 10 study samples (increase frequency for smaller studies) [37].
- Inject five procedural blanks at the end to assess carryover [37].
Chemical Descriptors for Quality Assessment: Select a set of metabolites that are reliably detected in the QC samples. These should represent diverse chemical classes, molecular weights, and chromatographic retention times to monitor method reproducibility comprehensively [37].
Real-Time QC Monitoring with QC4Metabolomics
For real-time monitoring, QC4Metabolomics is a software tool that tracks user-defined compounds during data acquisition. It extracts diagnostic information such as observed m/z, retention time, intensity, and peak shape, presenting results on a web dashboard. This allows for the immediate detection of issues like retention time drift or severe ion suppression, enabling corrective action during the analysis rather than after its completion [38].
Post-Acquisition Correction with PARSEC
For improving the comparability of separately acquired metabolomics datasets, the PARSEC (Post-Acquisition Standardization to Enhance Comparability) strategy offers a three-step workflow. This method involves data extraction, standardization, and filtering to correct for analytical bias without long-term quality controls, enhancing data interoperability across studies [39].
Proteomics Quality Control (QC) Best Practices
Addressing Core Proteomics Challenges
Proteomics faces unique hurdles, including the vast dynamic range of protein abundance and the introduction of batch effects. The following table summarizes common challenges and their mitigation strategies [40].
Table 1: Common Proteomics Challenges and Mitigation Strategies
| Challenge Area | Technical Issue | Recommended Mitigation Strategy |
|---|---|---|
| Sample Preparation | High dynamic range, ion suppression | Depletion of high-abundance proteins (e.g., albumin); multi-step peptide fractionation (e.g., high-pH reverse phase) [40]. |
| Batch Effects | Confounding technical variance | Employ randomized block design; inject pooled QC reference samples frequently (e.g., every 10-15 injections) across all batches [40]. |
| Data Quality | Missing values, undersampling | Utilize Data-Independent Acquisition (DIA); apply sophisticated imputation algorithms based on the nature of the missingness (MAR vs. MNAR) [40]. |
Automated QC in High-Throughput Proteomics
The π-Station represents an advanced, fully automated sample-to-data system designed for unmanned proteomics data generation. Its integrated QC framework, π-ProteomicInfo, is key to maintaining data quality [41].
The π-ProteomicInfo Automated QC Workflow:
- Monitor Module: A standalone program tracks instrument status and automatically transfers raw data files upon run completion [41].
- Analyzer Module: Triggered after data transfer, it generates qualitative and quantitative profiles for each run [41].
- QC Module: Extracts QC metrics for data quality assessments. If QC data is unqualified, it triggers the Controller Module [41].
- Controller Module: Immediately stops data acquisition to prevent the loss of precious samples and sends text notifications to specialists for maintenance [41].
Benchmarking Performance: In a long-term stability assessment over 63 days, the π-Station platform demonstrated a variation in protein identification below 3% (intra-day) and 6% (inter-day), with a maximum median CV of protein abundance under 8%, showcasing exceptional robustness [41].
Troubleshooting Guides and FAQs
Metabolomics Troubleshooting
Q: My QC samples do not cluster tightly in a PCA scores plot. What could be the cause? A: Poor clustering of QCs indicates high analytical variability. Potential causes include instrument sensitivity drift, column degradation, inconsistent sample preparation, or issues with the pooling of the QC sample itself. Check the reproducibility of your chemical descriptors' retention times and peak areas. Implementing a real-time monitor like QC4Metabolomics can help identify such issues as they occur [38].
Q: How should I handle missing values in my metabolomics dataset? A: QComics emphasizes the need to separately handle missing values (e.g., due to low abundance) from truly absent biological data. For values missing due to being below the limit of detection, imputation with a small value (e.g., drawn from the lower end of the detectable distribution) may be appropriate. Values missing at random might be addressed with more advanced imputation methods, but the strategy should be carefully chosen to avoid introducing bias [37].
Proteomics Troubleshooting
Q: What are the signs that sample preparation failed in a proteomics run? A: Key indicators include very low peptide yield after digestion, poor chromatographic peak shape, excessive baseline noise in the mass spectrometer (suggesting detergent or salt contamination), or a high coefficient of variation (CV > 20%) in protein quantification across technical replicates [40].
Q: How can I prevent batch effects from confounding my study during the experimental design phase? A: The most effective strategy is a randomized block design. This ensures that samples from all biological comparison groups (e.g., control vs. treated) are evenly and randomly distributed across all processing and analysis batches. This prevents a technical batch from being perfectly correlated with a biological group, which is a primary source of confounding [40].
Q: What is the best way to handle missing values in quantitative proteomics data? A: The best approach is to first determine if data is Missing at Random (MAR) or Missing Not at Random (MNAR). If MNAR (a protein is missing because its abundance is too low to detect), imputation should use small, low-intensity values drawn from the bottom of the quantitative distribution. If MAR, more robust methods like k-nearest neighbor or singular value decomposition are appropriate [40].
Essential Research Reagent Solutions
The following table details key reagents and materials critical for implementing robust QC in metabolomics and proteomics workflows.
Table 2: Key Research Reagents and Materials for QC
| Item | Function | Application Field |
|---|---|---|
| Pooled QC Sample | A quality control sample made by pooling aliquots of all study samples; used to monitor analytical stability and performance over the sequence run. | Metabolomics [37], Proteomics [40] |
| Procedural Blank | A sample prepared without the biological matrix; used to identify background noise, contaminants, and carryover from reagents and the preparation process. | Metabolomics [37], Proteomics |
| Chemical Descriptors | A predefined set of metabolites reliably detected in the QC samples; used as markers to assess method reproducibility, retention time stability, and signal intensity. | Metabolomics [37] |
| Isotopically Labeled Internal Standards | Synthetic standards with stable isotope labels; added to samples to correct for variability in extraction, ionization, and analysis. | Targeted Metabolomics [37], Proteomics [40] |
| SISPTOT Kit | A miniaturized, spin-tip-based kit for automated, low-input proteomic sample preparation, enabling high-throughput spatial proteomics. | Proteomics [41] |
Workflow Visualization
QComics Metabolomics QC Workflow
Automated Proteomics QC and Monitoring
Leveraging Instrument Performance Metrics and System Suitability Testing
Core Concepts and Importance
What is System Suitability Testing (SST) and why is it critical in systems biology research?
System Suitability Testing (SST) consists of verification procedures to ensure that an analytical method and the instrument system are suitable for their intended purpose on the day of analysis. It confirms that the entire analytical system—from instrumentation and reagents to data processing—is functioning correctly and can generate reliable, reproducible data. In systems biology, where models are built upon experimental data, SST provides the foundational assurance that this primary data is trustworthy. Robust SST protocols are a direct response to the reproducibility crisis in science, where studies indicate over 50% of researchers have failed to reproduce their own experiments [33] [9].
How do performance metrics and SST relate to the FAIR principles and model reproducibility?
SST is a practical implementation of the FAIR (Findable, Accessible, Interoperable, Reusable) principles for data. The performance metrics gathered during SST, such as mass accuracy and retention time stability, are critical metadata that make data Interoperable and Reusable by providing context on the experimental conditions and data quality. For mechanistic models in systems biology, a study is considered repeatable if one can run the author-provided code and obtain the same results, and reproducible if one can recreate the model and data de novo with the same results. High-quality data, verified by SST, is the bedrock of both [33].
Troubleshooting Guides
FAQ 1: My liquid chromatography (LC) method, which previously passed SST, is now failing repeatability requirements (for example, high %RSD). What should I investigate?
This is a common issue where a pharmacopeial method fails after a period of stable operation [42]. Follow a "divide and conquer" strategy to isolate the variable causing the failure.
- Step 1: Eliminate the sample preparation variable. Prepare a single, large volume of the system suitability sample. Inject this same sample multiple times (e.g., n=10). If the %RSD is now acceptable, the problem likely lies in the sample preparation process across multiple vials, not the instrument itself [42].
- Step 2: Investigate the injection process. If the problem persists with a single vial, the issue is likely in the analytical system. The most common culprit in such cases is the autosampler's injection mechanism. Check for:
- Air bubbles in the sample syringe or needle.
- Partial blockages in the sample path or injector rotor seal.
- Worn components in the autosampler that lead to variable injection volumes [42].
- Step 3: Check the chromatographic column. While less likely to cause sudden area changes, replace the column with a new one to definitively eliminate it as a source of the problem. This follows the "easy over powerful" troubleshooting rule [42].
- Step 4: Review data for patterns. Examine the sequence of peak areas. A gradual trend (up or down) may indicate a different issue (e.g., column degradation, mobile phase depletion), while random variation strongly points to the injection process [42].
FAQ 2: My mass spectrometer is no longer detecting low-abundance species in a bottom-up proteomics experiment, despite high sequence coverage for a standard protein digest. What key metrics should I check?
High sequence coverage of a standard protein like BSA is a common but insufficient metric for detecting low-abundance species, as it does not effectively identify settings that limit dynamic range [43]. You need metrics that focus on detection limit and sensitivity.
- Step 1: Use a more relevant standard. Employ a spiked sample, such as a BSA digest with synthetic peptides present at known low concentrations (e.g., 0.1% to 100% of the BSA peptide concentration) to simulate impurities [43].
- Step 2: Evaluate dynamic range and Limit of Detection (LOD). Using the spiked sample, calculate the signal-to-noise ratio (S/N) for the low-abundance peptides. The LOD is typically defined as S/N > 3. Also, assess the intra-scan dynamic range by analyzing the peak area ratio of co-eluting light and heavy isotopic peptide pairs at different concentration ratios [43].
- Step 3: Check critical MS parameters. Key instrument parameters that significantly impact the detection of low-abundance species include [43]:
- MS1 and MS2 scan times: Shorter times may prevent the instrument from accumulating enough ions from low-abundance species.
- MS2 precursor selection threshold: A threshold set too high will ignore low-intensity precursors.
- Source voltage and tuning parameters: Suboptimal settings can reduce ionization efficiency.
FAQ 3: My field instrument (e.g., temperature sensor, pressure gauge) is showing sudden, erratic readings. How do I begin diagnosis?
For field instruments in bioreactor or fermentation control systems, a systematic approach is key.
- Step 1: Perform a power and connection check. Verify that the power supply is stable and that the voltage is within normal limits. Inspect all cable connections for looseness, and check connectors for corrosion or damage [44] [45].
- Step 2: Isolate the fault. Use a multimeter to check the output signal of the sensor itself and compare it to the expected value. For a temperature sensor showing a sudden rise, check for an open circuit in the thermocouple or RTD. For a sudden drop, look for a short circuit [44].
- Step 3: Inspect the environment. Check for environmental factors such as electromagnetic interference, which can cause signal distortion, or external vibrations that may have damaged the sensor [44] [45].
Performance Metrics and Experimental Protocols
Standard Protocol for Establishing LC-MS System Suitability for Peptide Mapping
This protocol is adapted from best practices for characterizing therapeutic proteins and monoclonal antibodies [43] [46].
Sample Preparation:
- Obtain a commercially available peptide mixture (e.g., Pierce Peptide Retention Time Calibration Mixture) or create a custom standard.
- A robust approach is to use a BSA tryptic digest spiked with a set of synthetic "Intra-scan" peptide pairs (isotopically labeled) and "Inter-scan" peptides at known concentrations (e.g., 0.1%, 1%, 10%, 100%) to simulate low-abundance impurities [43].
- Dissolve the sample in an appropriate mobile phase compatible with the LC method.
LC-MS/MS Analysis:
- Chromatography: Use a defined LC system and column. Apply a linear gradient from aqueous to organic solvent over a set time (e.g., 10-60 minutes). Maintain a constant column temperature [43] [46].
- Mass Spectrometry: Operate the mass spectrometer in data-dependent acquisition (DDA) mode. Set the MS1 scan range (e.g., 300-1500 m/z) and resolution. Select the top N precursors for MS2 fragmentation. Critical parameters to define include MS1 and MS2 scan times, and the MS2 precursor intensity threshold [43].
Data Processing and Metric Calculation:
- Use a software platform (e.g., Byos, Skyline) to process the raw data. The software should identify peptides, extract ion chromatograms (XICs), and calculate key metrics [46].
- Input the sequences of the expected peptides and any fixed modifications (e.g., isotopic labels) for accurate identification [46].
- The software automatically generates a system suitability report, evaluating the metrics against predefined acceptance criteria.
Key Quantitative Metrics for LC-MS System Suitability
The table below summarizes essential metrics for evaluating an LC-MS system's fitness for peptide mapping in systems biology [43] [46].
Table 1: Key LC-MS System Suitability Metrics and Acceptance Criteria
| Metric Category | Specific Metric | Typical Acceptance Criteria | Significance in Systems Biology |
|---|---|---|---|
| Mass Accuracy | Precursor Mass Error | < 5-10 ppm | Ensures correct identification of model components (proteins, metabolites). |
| Retention Time Stability | Retention Time Shift | < 0.5 min (or %RSD < 1%) | Critical for aligning data across runs and for reproducible model building. |
| Chromatographic Performance | Peak Width (at half height) | < 0.3 min (or defined %RSD) | Indicates separation efficiency, impacting quantification accuracy. |
| Sensitivity & Dynamic Range | Limit of Detection (LOD) | S/N > 3 for 0.1% spiked peptide [43] | Determines ability to detect low-abundance species critical to network models. |
| Sensitivity & Dynamic Range | Intra-scan Dynamic Range | Accurate quantitation over 2-3 orders of magnitude [43] | Allows for correct quantification of species at vastly different concentrations. |
| Peptide Identification | Number of Peptides Identified | > 90% of expected peptides | Provides confidence in proteome coverage for the model. |
Workflow for System Suitability Testing and Data Integration
The following diagram illustrates the logical workflow for implementing SST and integrating the quality-assured data into systems biology research.
The Scientist's Toolkit: Essential Research Reagents and Materials
For establishing a robust LC-MS/MS system suitability protocol in a protein biochemistry or systems biology lab, the following reagents and materials are essential.
Table 2: Essential Research Reagents for LC-MS System Suitability
| Item | Function and Importance |
|---|---|
| Bovine Serum Albumin (BSA) Tryptic Digest | A well-characterized protein digest standard used as a baseline to evaluate instrument performance, particularly for generating sequence coverage and retention time stability [43]. |
| Synthetic Isotopically-Labeled Peptides | Peptides with heavy labels (e.g., C13, N15) spiked into a BSA digest to accurately evaluate intra-scan dynamic range, limit of detection, and quantitative accuracy by creating known concentration ratios [43] [46]. |
| Pierce Peptide Retention Time Calibration Mixture | A commercially available, predefined mixture of peptides used to standardize and monitor retention time stability and mass accuracy across instruments and laboratories [46]. |
| Standardized LC Columns | Columns from a consistent manufacturer and lot are critical for reproducing chromatographic separation and achieving the retention time stability required for reproducible data across studies. |
| Mass Calibration Standard | A solution with known ions (e.g., ESI Tuning Mix) used to calibrate the mass axis of the mass spectrometer, ensuring high mass accuracy for confident compound identification [43]. |
| FASTA File of Standard Sequences | A digital file containing the amino acid sequences of the proteins/peptides in the suitability standard. This is input into processing software to enable automated identification and metric calculation [46]. |
Integrating Cyberinfrastructure for End-to-End Data Provenance and Management
Within the framework of a thesis on establishing robust quality control (QC) and quality assurance (QA) standards for systems biology data research, this technical support center addresses the critical cyberinfrastructure needed to ensure data integrity from generation to reuse [47]. Systems biology projects are inherently transdisciplinary, generating vast, complex multi-OMICs datasets [48]. The primary goal of QA in this context is proactive, focusing on perfecting the data management process to prevent compromises in data quality, while QC is product-focused, reactively testing data outputs against specifications [49]. Effective integration of cyberinfrastructure for end-to-end data provenance—tracking the origin, transformations, and lifecycle of data—is foundational to both QA and QC, enabling secure, FAIR (Findable, Accessible, Interoperable, Reusable), and reproducible scientific discovery [50] [48] [47].
Technical Support Center: FAQs & Troubleshooting Guides
FAQ Category 1: Data Collection & Metadata Management
Q1: Our experimental team views detailed metadata collection as a burdensome "ephemera" task. How can we justify and streamline this process for QA purposes? A: Rich metadata is not ephemera; it is the essential context that makes data reusable and interpretable, directly supporting QC/QA goals of reliability and reproducibility [48]. To streamline:
- Automate Capture: Leverage instrumentation that automatically generates metadata summaries and result files. Integrate these data streams directly into your laboratory information management system (LIMS) to reduce manual entry [47].
- Adopt Standards: Utilize standardized metadata frameworks (e.g., those being developed by the OASIS Data Provenance Standards TC) to ensure interoperability and future-proofing [51].
- Demonstrate Value: Provide examples where metadata (e.g., equipment settings, reagent lots, animal handling logs) was crucial for interpreting anomalous results or integrating disparate datasets, turning a QC investigation into a QA process improvement [49] [47].
Q2: How do we define what metadata is "enough" for future reuse, especially for AI-ready data? A: Adopt the motto: "Investigate everywhere, trust nothing, test everything" [47]. For AI/ML readiness, provenance is key. The Integrity, Provenance, and Authenticity for AI Ready Data (IPAAI) program area within NSF's CICI framework explicitly targets this challenge [50]. As a rule, capture:
- Provenance: Unique identifiers for samples, derived data, and software versions [48] [51].
- Experimental Context: All technical and biological confounders (e.g., sample preparation details, instrument calibrations) [48].
- Transformations: A complete audit trail of all data processing, filtering, and analysis steps [51].
FAQ Category 2: Data Security, Sharing & Compliance
Q3: We need to share data collaboratively but are concerned about security and unauthorized access. What cyberinfrastructure solutions are available? A: The NSF Cybersecurity Innovation for Cyberinfrastructure (CICI) program supports solutions for this exact issue [50]. Key approaches include:
- Usable and Collaborative Security for Science (UCSS): Implement security tools integrated into the scientific workflow, such as encrypted data transfer portals and federated identity management, which facilitate secure collaboration without hindering scientists [50].
- Transition to Cyberinfrastructure Resilience (TCR): Harden your data repositories and sharing platforms through security testing and validation of existing cybersecurity research tailored for scientific CI [50].
- Policy Compliance: Ensure your data sharing and user training protocols comply with updated NSF research security policies, including requirements for malign foreign talent recruitment program certifications [50].
Q4: Our funding mandate requires FAIR data sharing, but our datasets are complex and multimodal. Where do we start? A: Begin by defining your internal and external user communities and their needs during the project planning phase [47].
- Plan for Release Early: Align internal data formats with the submission requirements of your target public repositories (e.g., GEO, PDB) from the start to avoid reformatting scrambles later [48] [47].
- Utilize Reference Datasets: Consider contributing to or using Reference Scientific Security Datasets (RSSD) to support reproducible security and data handling research [50].
- Implement Provenance Tracking: Use or develop tools that generate standardized provenance metadata, a core requirement for data to be truly interoperable and reusable, as emphasized by the Data & Trust Alliance and OASIS [51].
FAQ Category 3: System Integration & Workflow Issues
Q5: Our data management and analysis workflows are siloed, leading to provenance breakdowns and QC failures. How can cyberinfrastructure integrate these? A: An end-to-end cyberinfrastructure platform acts as a unifying framework. For example, the UCSB BisQue Deep Learning platform is designed to manage multimodal imaging data with a robust backend ensuring data integrity and provenance [52].
- Integration Strategy: Develop or adopt a platform that connects data capture, storage, computation, and analysis in a unified environment. This provides a single source of truth for data lineage [47] [52].
- Workflow Orchestration: Use workflow management systems (e.g., Nextflow, Snakemake) that automatically log all parameters, code versions, and execution environments, creating an immutable record for QC audits [47].
- The "Rosetta Stone": Create a project-wide data dictionary and SOP glossary to ensure all team members, from wet-lab biologists to modelers, have a common understanding of terms and processes, which is a critical sociological aspect of cyberinfrastructure [47].
Q6: We encountered an Out-of-Specification (OOS) result during in-process QC testing. What is the integrated QA/QC response protocol? A: This scenario highlights the synergy between reactive QC and reactive QA [49].
- QC Initiates Investigation: The QC lab first investigates for potential laboratory error (proactive QC) [49].
- QA Takes Over Process Review: If lab error is ruled out, QA immediately investigates the manufacturing or data generation process for deviations (reactive QA) [49].
- Cyberinfrastructure Provides Audit Trail: Your data provenance system should provide the complete history of the sample and its data, including all metadata (operator, instrument logs, reagent IDs), to expedite the root cause analysis [48] [51].
- CAPA Implementation: The findings lead to a Corrective and Preventive Action (CAPA), where QA updates SOPs or supplier oversight to prevent recurrence, demonstrating continuous process improvement [49].
Table 1: NSF CICI Program Areas for Cybersecurity & Data Integrity
| Program Area | Primary Focus | Relevance to Data Provenance & QC |
|---|---|---|
| Usable & Collaborative Security for Science (UCSS) | Integrating security into scientific workflows for safe collaboration. [50] | Ensures secure data provenance tracking in collaborative environments. |
| Reference Scientific Security Datasets (RSSD) | Creating reference metadata artifacts from scientific workloads. [50] | Provides standardized data for testing QC/QA and provenance tools. |
| Transition to Cyberinfrastructure Resilience (TCR) | Hardening CI through testing and validation of security research. [50] | Improves robustness and trustworthiness of data provenance systems. |
| Integrity, Provenance, Authenticity for AI (IPAAI) | Enhancing confidence in AI results via dataset integrity. [50] | Directly addresses provenance standards for AI/ML-ready data. |
Table 2: Color Contrast Requirements for Accessibility in Visualizations
| Element Type | Minimum Contrast Ratio (Background vs. Foreground) | Example Application in Diagrams |
|---|---|---|
| Normal Text | 4.5:1 [53] | Text inside nodes (labels, descriptors). |
| Large Text | 3:1 [53] | Main titles or headers within a diagram. |
| Graphical Objects (Icons) | 3:1 [53] | Arrowheads, symbols, or other non-text elements. |
| Note: Very high contrast (e.g., pure black on pure white) can be difficult for some users; consider off-white backgrounds. [53] |
Detailed Experimental Protocol: Implementing a FAIR Data Pipeline
This protocol outlines the methodology for establishing a QA-compliant, provenance-tracking data pipeline, as implemented in systems biology consortia like MaHPIC [47].
1. Planning & Design Phase:
- Community & Needs Assessment: Define all data producer and consumer roles within and outside the project. Document their required data formats, volumes, and analysis needs. [47]
- Provenance Model Selection: Adopt or define a metadata schema for data provenance (e.g., aligning with emerging OASIS standards) [51]. Create a project "Rosetta Stone" data dictionary. [47]
- Cyberinfrastructure Selection: Choose platforms (e.g., BisQue [52]) that support scalable data management, automated metadata capture, and have robust, secure APIs for tool integration.
2. Implementation & Data Generation Phase:
- Unique Identification: Assign persistent unique IDs to all biological samples, derived data files, and software versions. [48]
- Automated Metadata Capture: Configure instruments to output metadata logs. Use LIMS to capture manual experimental observations. [47]
- Secure Data Transfer: Use encrypted, auditable transfer protocols (e.g., SFTP, Globus) to move data from acquisition sites to central storage or cloud compute resources. [50] [47]
3. Processing, Analysis & Sharing Phase:
- Workflow Orchestration: Execute all data processing and analysis via versioned, containerized workflow scripts that automatically record parameters and environment. [47]
- Provenance Logging: The CI platform must aggregate sample IDs, raw data, processing logs, and analysis outputs into a queryable provenance graph. [51] [52]
- FAIR Curation & Deposition: Before publication, package datasets with rich metadata following community standards and deposit in appropriate public repositories (e.g., GEO for transcriptomics, PDB for structures). Mint DOIs for citation. [48]
Visualizations: Workflow and Relationship Diagrams
Title: End-to-End Data Provenance Workflow for Systems Biology
Title: QA, QC, and Cyberinfrastructure Relationship in Systems Biology
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item Category | Specific Tool/Solution | Function in Data Provenance & QC |
|---|---|---|
| Data Management Platform | BisQue, CyVerse, Terra | Provides unified environment for data storage, visualization, and analysis with built-in provenance tracking and scalability for multimodal data. [52] |
| Provenance & Metadata Standard | Data & Trust Alliance / OASIS Data Provenance Standard | Standardized metadata framework for tracking data lineage, transformations, and compliance, ensuring interoperability and trust. [51] |
| Workflow Management System | Nextflow, Snakemake, CWL | Orchestrates reproducible data analysis pipelines, automatically generating audit trails of all processing steps, crucial for QC reproducibility. [47] |
| Security & Collaboration Tool | NSF CICI UCSS-compliant tools (e.g., Globus, Open OnDemand) | Enables secure data transfer and collaborative analysis while integrating security into the scientific workflow, protecting data integrity. [50] |
| Reference Data & Databases | Protein Data Bank (PDB), NCBI repositories, RSSD artifacts | Provide essential, high-quality reference data for QC benchmarking, method validation, and training AI models (e.g., AlphaFold). [50] [48] |
| Unique Identifier Service | Digital Object Identifier (DOI), Research Resource Identifiers (RRID) | Provides persistent, citable identifiers for datasets, code, and samples, making them findable and trackable in the literature. [48] |
Identifying and Correcting Common QC Failures in Complex Workflows
Technical Support Center: Troubleshooting Guides and FAQs
This technical support center is designed within the context of establishing robust quality control (QC) standards for systems biology data research. It provides actionable guidance for diagnosing and mitigating key sources of variability that compromise the reproducibility and reliability of multi-omics data, which is fundamental for credible scientific discovery and drug development [33] [9].
Section 1: Sample Preparation Variability
Sample preparation is a primary source of technical variance, introducing bias and error that propagate through all downstream analyses [40] [54].
Troubleshooting Guide: Common NGS Library Prep Failures
Q: My sequencing run yielded poor coverage and high duplication rates, but the library looked fine on the BioAnalyzer. What went wrong? A: This is a classic sign of issues originating in library preparation. You need to systematically diagnose the failure [55].
Diagnostic Flow:
- Examine the Electropherogram: Look for a sharp peak at ~70-90 bp, indicating adapter-dimer contamination, or a broad/smeared distribution suggesting uneven fragmentation [55].
- Cross-Validate Quantification: Compare fluorometric (Qubit) and qPCR-based results. Relying solely on UV absorbance (NanoDrop) can overestimate usable material due to contaminant interference [55] [9].
- Trace Steps Backwards: Identify at which stage the failure likely occurred (e.g., ligation, fragmentation, input) [55].
Table 1: Troubleshooting Common NGS Sample Preparation Failures [55]
| Problem Category | Typical Failure Signals | Common Root Causes | Corrective Actions |
|---|---|---|---|
| Sample Input/Quality | Low yield; electropherogram smear; low complexity. | Degraded DNA/RNA; contaminants (phenol, salts); quantification error. | Re-purify input; use fluorometric quantitation (Qubit); check 260/230 & 260/280 ratios. |
| Fragmentation & Ligation | Unexpected fragment size; high adapter-dimer peak. | Over/under-shearing; poor ligase efficiency; incorrect adapter:insert ratio. | Optimize fragmentation time/energy; titrate adapter ratio; ensure fresh enzyme/buffer. |
| Amplification/PCR | High duplicate rate; amplification bias. | Too many PCR cycles; polymerase inhibitors; primer exhaustion. | Reduce cycle number; use master mixes; re-amplify from leftover ligation product. |
| Purification/Cleanup | Incomplete size selection; high sample loss. | Wrong bead:sample ratio; over-dried beads; pipetting error. | Precisely follow bead cleanup protocols; avoid pellet over-drying; implement operator checklists. |
FAQs: General Sample Preparation
Q: What are the signs of failed sample preparation in a proteomics experiment? A: Key indicators include very low peptide yield after digestion, poor chromatographic peak shape, excessive MS baseline noise (suggesting detergent/salt carryover), or a high coefficient of variation (CV > 20%) across technical replicates [40].
Q: How does sample preparation affect metabolomics accuracy? A: Improper handling leads to metabolite degradation, introduces matrix effects, and increases batch variability. This results in data bias, reduced reproducibility, and inaccurate quantification. Best practices include rapid freezing, using internal standards, and adhering to standardized SOPs [56].
Experimental Protocol: Implementing Process QC in Plasma Proteomics [54] Objective: To monitor variability at each stage of a complex sample preparation workflow. Methodology:
- QC Sample Design: Create five categories of QC samples (QCA to QCE) derived from a pooled plasma standard.
- Embedded Monitoring: Process these QC samples in parallel with experimental samples at critical points:
- QCA: Post-depletion of high-abundance proteins.
- QCB: Post-protein digestion.
- QCC: Post-peptide labeling (e.g., TMT).
- QCD: Post-fractionation.
- QC_E: A constant reference analyzed intermittently throughout the LC-MS/MS sequence.
- Metric Tracking: Quantify key parameters (e.g., protein yield, digestion efficiency, label efficiency) for each QC category. Maintain a CV of <10% for critical steps [40] [54].
Diagram: Sample Preparation QC Workflow
Title: Embedded QC Monitoring in Sample Prep Workflow
Section 2: Instrument Drift
Instrumental drift introduces systematic, non-biological variation over time, particularly detrimental in large-scale omics studies [57] [58].
Troubleshooting Guide: Correcting LC-MS Instrument Drift in Metabolomics/Proteomics
Q: My large cohort study shows strong batch effects. How can I diagnose and correct for instrument drift? A: Batch effects are often caused by sensitivity drifts over time. Correction requires a combination of experimental design and bioinformatic normalization [57] [40].
Diagnostic & Correction Flow:
- Use Intrastudy QC Samples: Inject pooled QC samples (made from a mix of all experimental samples) every 6-10 analytical runs [57] [54].
- Monitor QC Metrics: Track the Relative Standard Deviation (RSD) of features across QC injections. An RSD > 20-30% indicates problematic drift [57] [58].
- Apply Correction Algorithms: Use QC-based normalization methods to model and remove the drift signal from the experimental data.
Table 2: Comparison of Batch-Effect Correction Methods [57]
| Method | Complexity | Key Principle | Reported Performance |
|---|---|---|---|
| Median Normalization | Low | Normalizes each feature to the median of all QC samples. | Simple but may not capture non-linear drift. |
| QC-Robust Spline Correction (QC-RSC) | Medium | Uses a penalized cubic smoothing spline fitted to QC data to model drift. | Effectively reduces systematic variance in QC samples. |
| TIGER (Technical variation elimination with ensemble learning) | High | Employs an ensemble learning architecture to model complex drift patterns. | Demonstrated best overall performance in reducing QC RSD and improving biological classification accuracy [57]. |
FAQs: Managing Instrument Performance
Q: What are the key LC-MS system suitability tests to run before a large proteomics study? A: Run a standard sample (e.g., HeLa digest, BSA digest) and verify [54]:
- Retention Time Stability: CV < 5% for internal standard peptides (e.g., iRT).
- MS1 Mass Accuracy: < 5 ppm for Orbitrap systems.
- Peak Shape: Peak width of 4-8 seconds at baseline.
- Signal Intensity: Total Ion Current (TIC) variation < 30%.
- Dynamic Range: Ability to detect proteins across expected concentration range.
Q: How do I handle retention time (RT) shifts in untargeted metabolomics? A: RT alignment is critical. Strategies include [57]:
- Using external RT calibrants injected periodically.
- Applying alignment algorithms (e.g., in XCMS, MZmine) that match peaks across runs based on m/z and RT.
- Manually inspecting and correcting misalignments for critical features, especially in large studies where unexpected shifts can occur between calibrant runs.
Experimental Protocol: Implementing QC-Based Drift Correction with TIGER [57] Objective: To eliminate technical drift from an untargeted LC-MS metabolomics dataset. Methodology:
- Sequence Design: Analyze samples in randomized order. Inject a pooled QC sample at the beginning for system conditioning, then after every 8-10 experimental samples.
- Data Processing: Perform peak picking, alignment, and integration using standard software (e.g., XCMS, Compound Discoverer).
- Drift Modeling with TIGER: Input the matrix of feature intensities, with QC samples labeled. The TIGER algorithm uses an ensemble learning model to predict the "true" intensity of each feature in the QCs based on injection order, then generalizes this correction to the experimental samples.
- Validation: Assess performance by calculating the reduction in RSD for features in the QC samples post-correction. The dispersion-ratio (D-ratio) should also decrease significantly.
Diagram: Instrument Drift Monitoring & Correction Pathway
Title: Workflow for Correcting Analytical Instrument Drift
Section 3: Bioinformatics Variability
Computational pipelines introduce "computational variation," an often-overlooked source of quantitative uncertainty distinct from biological and analytical variation [58].
Troubleshooting Guide: Managing Data Processing & Analysis Variability
Q: My proteomics dataset has many missing values. How should I handle them without introducing bias? A: The strategy depends on the nature of the missingness [40] [54]:
- Missing Not At Random (MNAR): Values are missing because abundance is below detection. Use left-censored imputation (e.g., replace with a value drawn from a low-intensity distribution).
- Missing At Random (MAR): Values are missing randomly. Use more robust methods like k-nearest neighbor (KNN) or singular value decomposition (SVD) imputation.
- Avoid: Simple zero or mean imputation, which severely distorts the data structure and leads to false positives.
Q: My multi-batch omics data shows strong clustering by batch in PCA. How can I fix this? A: This indicates a strong batch effect. While randomization and QC correction (Section 2) are first-line defenses, post-hoc bioinformatic correction may be needed [40].
- Use Combat or Similar Tools: Apply statistical methods designed to remove batch effects while preserving biological variance.
- Re-run PCA: Verify that QC and experimental samples from different batches co-cluster after correction.
- Caution: Over-correction can remove true biological signal. Always validate findings with independent methods.
Table 3: Key Data Analysis QC Criteria for Omics [9] [54]
| Analysis Stage | QC Parameter | Target Threshold | Purpose |
|---|---|---|---|
| Identification | False Discovery Rate (FDR) | ≤ 1% (0.01) | Controls false positive peptide/protein IDs. |
| Quantification | Technical Replicate CV | Median CV < 20% | Assesses precision of measurement. |
| Data Completeness | Missing Value Rate | < 50% missing for >70% of proteins/features | Ensures sufficient data for robust stats. |
| Reproducibility | Replicate Correlation (Pearson r) | r > 0.9 | Indicates high consistency between replicates. |
| Batch Effect | PCA of QC Samples | Tight clustering of all QCs | Confirms absence of major technical batch effects. |
FAQs: Ensuring Reproducible Analysis
Q: What are the FAIR principles and why are they crucial for systems biology? A: FAIR stands for Findable, Accessible, Interoperable, and Reusable. Adhering to these principles ensures that models, data, and code can be discovered, understood, and reused by others, which is fundamental for reproducibility, collaboration, and building upon existing work in systems biology [33].
Q: What software engineering practices improve model reproducibility? A: Key practices include [33]:
- Version Control: Use Git for all code and scripts.
- Comprehensive Documentation: Include README files and in-line comments.
- Use of Standards: Employ community standards like SBML for models and SED-ML for simulation experiments.
- Containerization: Use Docker/Singularity to encapsulate the complete software environment.
- Public Repositories: Deposit code in GitHub/GitLab and models in BioModels or similar repositories.
The Scientist's Toolkit: Essential Reagents & Materials for QC
Table 4: Key Research Reagent Solutions for Quality Assurance
| Item | Primary Function | Application Field |
|---|---|---|
| Pooled Intrastudy QC Sample | Monitors and corrects for instrument drift and batch effects. | Metabolomics, Proteomics, Lipidomics [57] [54]. |
| iRT (Indexed Retention Time) Peptide Kit | Provides stable internal standards for LC retention time alignment and system suitability. | Proteomics (DDA/DIA) [54]. |
| Nucleic Acid Integrity Number (NAIN) Assay | Quantifies the degradation level of RNA/DNA input material. | Genomics, Transcriptomics (NGS) [55]. |
| UPS1/Sigma Dynamic Range Protein Standard | A defined mixture of proteins at known ratios to assess LC-MS/MS quantitative accuracy, precision, and dynamic range. | Proteomics [54]. |
| Solid Phase Extraction (SPE) Columns | Removes salts, lipids, and other contaminants during metabolite extraction, reducing matrix effects. | Metabolomics [56]. |
| Bead-Based Cleanup Kits (SPRI) | Performs size selection and purification of NGS libraries, critical for removing adapter dimers and short fragments. | Genomics (NGS Library Prep) [55]. |
| Stable Isotope-Labeled Internal Standards (SIL IS) | Enables absolute quantification and corrects for extraction efficiency and ion suppression for specific target analytes. | Targeted Metabolomics, Proteomics (SIS peptides) [58]. |
Context: This guide is part of a broader thesis on establishing robust quality control (QC) standards for systems biology data research. It addresses common data integrity challenges to ensure reproducible and regulatory-compliant analyses in drug development and basic research.
Foundational FAQs
Q1: What is the difference between "missing values" and "truly absent data" in biological datasets? A1: Missing values are data points that were intended to be collected but are unavailable due to errors (e.g., sensor failure, human error) or non-response [59] [60]. Truly absent data refers to measurements that are logically or biologically nonexistent for a given sample (e.g., a gene not expressed in a specific cell type, or a clinical test not administered because it was not indicated). Distinguishing between them is critical; imputing a "truly absent" value can introduce serious bias [59].
Q2: Why is handling missing/absent data a critical QC step in systems biology? A2: Ignoring these issues distorts statistical results (mean, variance), leads to inaccurate machine learning models, and influences data distribution [61]. In bioinformatics, poor handling compromises research reproducibility—a key pillar of the FAIR data principles—and can delay drug discovery or lead to failed clinical trials due to erroneous conclusions [9].
Q3: How are missing values typically represented in datasets? A3: Common representations include:
NaN(Not a Number) in Python/Pandas.NULLorNonein databases.- Empty strings (
""). - Special numeric placeholders like
-999or9999[60].
Troubleshooting Guides
Issue 1: My dataset has gaps. Should I delete the affected rows or columns? Diagnosis: This is a listwise or pairwise deletion strategy. Use it only after assessing the nature and extent of missingness. Solution:
- Apply Listwise Deletion only if the data is Missing Completely at Random (MCAR) and the amount of missing data is very small. Removing too much data reduces statistical power [60] [61].
- Avoid Deletion if data is Missing Not at Random (MNAR), as deletion will amplify bias [60].
- Consider Column Deletion only if a specific variable has an excessively high (>40-50%) proportion of missing values and is non-essential. Action: Always document the proportion of data removed and justify the assumption of MCAR.
Issue 2: I need to fill in missing values before analysis. What is the simplest imputation method? Diagnosis: You are considering single-value imputation, which is simple but can underestimate variance. Solution:
- For numerical data: Use mean or median imputation for MCAR data. The median is more robust to outliers [59] [61].
- For categorical data: Use the mode (most frequent category) [59]. Protocol:
- Calculate the mean/median/mode using only the observed values.
- Replace missing entries with this calculated value.
- Critical QC Step: Flag or create an indicator variable to mark which values were imputed, as this alters the data structure [60].
Issue 3: Simple imputation feels inadequate. What are more advanced, model-driven methods? Diagnosis: Your data likely has complex relationships, or the missingness may be at random (MAR). Solutions & Protocols:
k-Nearest Neighbors (KNN) Imputation:
- Method: For each sample with a missing value, find 'k' samples with the most similar observed values across other variables. Impute the missing value based on the average (for numeric) or mode (for categorical) of these neighbors [59].
- QC Consideration: Standardize variables before calculating distance. Choose 'k' via cross-validation.
Multiple Imputation by Chained Equations (MICE):
- Method: A state-of-the-art technique that creates multiple (
m) complete datasets. - Protocol: a) Each variable with missing data is imputed using a regression model based on other variables. b) This process cycles through all variables iteratively. c) After convergence, the cycle is repeated to produce
mdistinct datasets [59]. - Analysis: Perform your intended analysis (e.g., regression) separately on each of the
mdatasets. - QC Synthesis: Pool the
mresults using Rubin's rules to obtain final estimates and standard errors that account for imputation uncertainty [59].
- Method: A state-of-the-art technique that creates multiple (
Issue 4: How do I classify the type of missingness (MCAR, MAR, MNAR) in my data? Diagnosis: Classifying missingness is a detective process based on data patterns and domain knowledge. Guide:
- MCAR (Missing Completely at Random): No systematic difference between missing and observed data. Test statistically (e.g., Little's MCAR test) or by comparing summary statistics of complete vs. incomplete cases [60] [61].
- MAR (Missing at Random): The probability of missingness depends on observed data. E.g., older patients might be more likely to have missing lab values. This can be investigated by examining correlations between missingness patterns and other observed variables [59] [61].
- MNAR (Missing Not at Random): The probability of missingness depends on the unobserved value itself. E.g., patients with very high viral loads may drop out of a study. This is untestable from the data alone and requires domain knowledge [59] [9]. For example, in single-cell genomics, a zero count could be a true absence (MNAR) or a technical dropout (MAR).
Diagram: Decision Flow for Classifying and Addressing Missing Data Types
Advanced Protocol: QC for Single-Cell ATAC-seq Data (A Case Study)
Scenario: A researcher is processing single-cell ATAC-seq data, which is notoriously sparse (has many zeros). They need to distinguish technical dropouts (missing data) from biological absences (truly absent data) to filter high-quality cells.
Protocol: Using PEAKQC for Periodicity-Based Quality Assessment [62]
Objective: To identify high-quality cells by assessing the nucleosomal periodicity pattern in fragment length distribution (FLD), a hallmark of successful ATAC-seq assays.
Detailed Methodology:
- Input Data: A BAM file containing aligned sequencing fragments for each cell.
- Calculate Fragment Length Distribution: For each cell, compute a histogram of fragment lengths (e.g., from 0 to 500 bp).
- Wavelet Transformation: Apply a wavelet transform to the FLD. This mathematical tool is excellent for detecting periodic patterns (like the ~200bp spacing between nucleosomes).
- Convolution & Scoring: Convolve the transformed signal with a wavelet that matches the expected nucleosomal periodicity. The strength of the resulting signal provides a periodicity score per cell.
- Cell Filtering: Cells with scores above a defined threshold (often based on distribution quantiles or bimodality) are retained as high-quality. These cells show clear nucleosomal patterning, indicating successful library preparation and minimal technical noise.
- Downstream Impact: Using PEAKQC-filtered cells improves downstream analysis clarity, including cell clustering and identification of cell-type-specific regulatory elements [62].
Diagram: PEAKQC Workflow for Single-Cell ATAC-seq Quality Control
Research Reagent & Solutions Toolkit
| Item | Function in QC / Missing Data Handling | Example/Note |
|---|---|---|
| Python Pandas Library | Primary tool for identifying (isnull()), summarizing, and performing simple imputations (fillna()) on missing data in tabular data [60]. |
Enables mean, median, ffill, bfill imputation. |
Scikit-learn SimpleImputer |
Provides a consistent API for single-value imputation (mean, median, most_frequent, constant) within machine learning pipelines [60]. | Ensures imputation parameters are learned from training data and applied to test data. |
Scikit-learn KNNImputer |
Implements k-Nearest Neighbors imputation for multivariate data, considering relationships between features [59]. | Requires careful choice of n_neighbors and distance metric. |
Statsmodels / IterativeImputer |
Facilitates advanced multiple imputation techniques like MICE, allowing for different models per variable type [59]. | Critical for proper uncertainty estimation in final analyses. |
| PEAKQC Python Package | Provides a specialized QC metric for single-cell ATAC-seq data by quantifying nucleosomal periodicity from fragment length distributions [62]. | Addresses the "true zero vs. dropout" question in sparse genomics data. |
| FastQC | A standard tool for initial quality assessment of raw sequencing data, generating metrics on base quality, GC content, adapter contamination, etc. [9]. | Identifies issues at the data generation stage that could lead to systemic missingness. |
| Reference Standards | Well-characterized control samples (e.g., standardized cell lines, DNA mixtures) used to validate bioinformatics pipelines and identify batch effects [9]. | Essential for distinguishing technical artifacts (potentially correctable missingness) from biological truth. |
| Metric | Value / Prevalence | Context / Implication | Source |
|---|---|---|---|
| Color Vision Deficiency (CVD) | ~8% of men, ~0.5% of women | When creating QC dashboards or visualizations, avoid red-green color pairs to ensure accessibility for all team members. | [63] |
| Research Reproducibility Crisis | Up to 70% of researchers fail to reproduce others' experiments; >50% fail to reproduce their own. | Rigorous handling of missing data and comprehensive QA protocols are direct responses to this crisis. | [9] |
| Potential Cost Saving in Drug Dev. | Improving data quality could reduce costs by up to 25%. | Investing in robust QA and data cleaning pipelines has a high return on investment by reducing late-stage failures. | [9] |
| Common Missing Data Imputation Methods | 1. Mean/Median/Mode2. KNN Imputation3. Model-Based (MICE/Regression)4. Indicator Variable | Choice depends on missingness mechanism (MCAR/MAR/MNAR) and data type. Model-based methods are generally preferred for MAR data. | [59] [60] [61] |
| Acceptable Deletion Threshold | No universal rule; often <5% MCAR data may be listwise deleted. | Higher percentages require imputation. Column deletion considered only for very high (>40-50%) missingness in non-critical variables. | Best Practice Synthesis |
Monitoring Quality Markers to Identify Pre-analytical Errors
Core Concepts: The Pre-analytical Phase and Quality Indicators
What is the pre-analytical phase and why is it a major source of laboratory errors?
The pre-analytical phase encompasses all processes from test ordering up to the point where the sample is ready for analysis [64]. This includes test requesting, patient preparation, sample collection, identification, transportation, and preparation [65]. In clinical diagnostics, this phase has been identified as the most vulnerable to errors, accounting for 60-70% of all laboratory errors [65] [64] [66]. A significant challenge is that many pre-analytical procedures are performed outside the laboratory walls by healthcare personnel not under the direct control of the laboratory, making standardization and monitoring difficult [65].
What are Quality Indicators (QIs) and how are they used to monitor pre-analytical quality?
Quality Indicators (QIs) are objective measures that evaluate the quality of selected aspects of care by comparing performance against a defined criterion [65]. In laboratory medicine, a standardized model of QIs for the pre-analytical phase has been developed by the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) Working Group on Laboratory Errors and Patient Safety (WG-LEPS) [65]. These QIs allow laboratories to quantify, benchmark, and monitor their performance over time, providing data to drive quality improvement initiatives across all stages of the testing process [65] [67].
Troubleshooting Guides: Identifying and Resolving Common Pre-analytical Errors
How can I identify and prevent sample quality issues?
Problem: High rates of unsuitable samples due to hemolysis, clotting, or incorrect volume.
Troubleshooting Steps:
Monitor Key Quality Indicators: Systematically track and categorize all rejected samples using the IFCC WG-LEPS QIs, such as:
Investigate Root Causes:
- Clotted Samples: Often result from improper mixing of blood with anticoagulant immediately after collection, use of a fine-gauge needle, or difficult venipuncture [67] [68].
- Hemolyzed Samples: Typically caused by use of a small-bore needle, difficult venipuncture, vigorous mixing, or forcing syringe-collected blood through the needle into an evacuated tube [64].
- Incorrect Volume: Affects the blood-to-anticoagulant ratio, critical for coagulation tests. This is a common error, particularly in pediatric samples [68].
Implement Corrective Actions:
- Standardize and reinforce training for phlebotomists and nurses on proper venipuncture technique and sample handling.
- Use the correct vacuum tubes to ensure proper fill volume.
- Gently invert tubes with anticoagulant 5-10 times immediately after collection.
Experimental Protocol for Monitoring Sample Quality:
- Data Collection: Use the laboratory information system (LIS) to record every rejected sample and the specific rejection criterion [67] [68].
- Calculation: Calculate the percentage of each error type monthly (e.g., Number of clotted samples / Total number of samples with anticoagulant x 100) [67].
- Benchmarking: Compare your laboratory's rates against published quality specifications to gauge performance level (optimal, common, or unsatisfactory) [67].
How can I reduce errors in test requesting and patient identification?
Problem: Inappropriate test requests and patient misidentification errors.
Troubleshooting Steps:
Monitor Key Quality Indicators:
Investigate Root Causes:
- Inappropriate Requests: Can be due to overuse (unnecessary tests) or underuse (needed tests not ordered), often stemming from a lack of involvement of laboratory specialists in test selection [64].
- Identification Errors: Occur when patient identification procedures are not rigorously followed, such as failing to use two unique patient identifiers or not labeling tubes in the presence of the patient [64] [66].
Implement Corrective Actions:
- Implement electronic ordering systems with clinical decision support.
- Develop and disseminate test request guidelines for common clinical scenarios.
- Mandate the use of at least two patient identifiers and enforce a policy of labeling samples at the bedside in the patient's presence [64].
How can I prevent errors related to sample transportation and storage?
Problem: Samples damaged in transport, delayed, or improperly stored.
Troubleshooting Steps:
Monitor Key Quality Indicators:
Investigate Root Causes:
- Delayed Transport: Can lead to glycolysis and falsely decreased glucose levels, or degradation of bilirubin if exposed to light [66].
- Improper Storage: Failure to centrifuge and separate serum/plasma in a timely manner can cause potassium to leak out of cells and sodium to move into cells, invalidating electrolyte results [66].
Implement Corrective Actions:
- Establish and communicate clear maximum time limits for sample transportation from different collection sites.
- Define and implement standard operating procedures for sample handling and storage immediately upon receipt in the laboratory.
Frequently Asked Questions (FAQs)
What are the most common pre-analytical errors reported in hematology laboratories?
The most frequently reported pre-analytical errors in hematology include clotted specimens and samples not received, with studies showing these can account for over 38% of all pre-analytical errors in this department [67]. Insufficient sample volume is also a predominant issue, particularly for pediatric and coagulation testing [68]. The table below summarizes quantitative data from published studies.
Table 1: Frequency of Pre-analytical Errors in Hematology Laboratories
| Quality Indicator | Study A (3-year data, n=95,002) [67] | Study B (1-year data, n=67,892) [68] |
|---|---|---|
| Clotted Samples | 3.6% (38.6% of all errors) | 0.26% (20.09% of all errors) |
| Samples Not Received | 3.5% (38.0% of all errors) | - |
| Insufficient Sample Volume | 1.1% (of total errors) | 0.70% (54.17% of all errors) |
| Inappropriate Sample-Anticoagulant Ratio | 9.1% (of total errors) | - |
| Hemolyzed Samples | 6.7% (of total errors) | - |
| Wrong Container | 1.8% (of total errors) | - |
How can quality specifications and sigma metrics be used to evaluate pre-analytical performance?
Quality specifications (QS) define benchmark performance levels for each QI, typically categorized as High (optimal), Medium (common), or Low (unsatisfactory) [67]. For example, the QS for "Misidentification error" is <0% for high performance and ≥0.041% for low performance [67]. Sigma metrics provide another powerful tool, calculating the number of standard deviations between the process mean and the nearest specification limit. A higher sigma value indicates a more robust process. One study calculated sigma values for pre-analytical QIs, finding performance ranging from 3.18 to 4.76 sigma, which is between "minimum" and "good" [67].
What is the difference between Quality Assurance (QA) and Quality Control (QC) in this context?
These are two distinct but related concepts [13] [69]:
- Quality Assurance (QA) is proactive and process-oriented. It focuses on preventing errors before they occur by establishing robust systems, including documentation, standard operating procedures (SOPs), training, and audits [13] [69].
- Quality Control (QC) is reactive and product-oriented. It involves the operational techniques and activities used to fulfill quality requirements, such as testing and inspection, to identify errors or deviations after they have occurred [13] [69]. Monitoring QIs is a QC activity; using the data to improve the phlebotomy training program is a QA activity.
Workflow Visualization
Diagram 1: Pre-analytical Phase Workflow
Diagram 2: QI Monitoring and Improvement Cycle
Table 2: Key Research Reagent Solutions for Quality Monitoring
| Item / Solution | Function / Application |
|---|---|
| IFCC WG-LEPS QI Model | A standardized set of 16 pre-analytical QIs providing a framework for consistent data collection and international benchmarking [65]. |
| Standardized Sample Collection Tubes | Color-coded vacuum tubes with pre-measured anticoagulant to ensure correct sample type and volume, critical for maintaining blood-to-anticoagulant ratio [68]. |
| Laboratory Information System (LIS) | Software platform for tracking samples, logging rejections, and calculating QI rates. Essential for data collection and analysis [67]. |
| Electronic Ordering System with Decision Support | Technology to reduce inappropriate test requests by guiding clinicians toward evidence-based test selection [64]. |
| Quality Control (QC) Samples | Commercially available or internally prepared samples with known properties used to monitor analytical and, where possible, pre-analytical processes [70]. |
| Bar Code ID System | Automates patient and sample identification, reducing misidentification and mislabeling errors at collection and throughout the testing process [64] [71]. |
Correcting for Batch Effects and Signal Drift in Longitudinal Studies
What are batch effects and signal drift, and why are they problematic in longitudinal studies?
Batch effects are systematic technical variations introduced into data due to changes in experimental conditions, such as different reagent lots, personnel, sequencing machines, or processing days [72] [73]. Signal drift refers to the gradual change in instrument signal intensity over the course of a single run or between runs, commonly observed in mass spectrometry and liquid chromatography–mass spectrometry (LC/MS) platforms [74] [75].
In longitudinal studies, which measure the same subjects over time, these technical variations are particularly problematic. Batch effects and drift can be confounded with the time-varying exposure of interest, making it difficult or nearly impossible to distinguish whether observed changes are driven by the biological factor under investigation or by technical artifacts [72]. This can lead to misleading outcomes, reduced statistical power, and irreproducible research [72].
How can I detect batch effects and signal drift in my data?
Both visual and quantitative methods are essential for detecting these technical issues. The table below summarizes the primary diagnostic approaches.
Table 1: Methods for Detecting Batch Effects and Signal Drift
| Method | Description | What to Look For |
|---|---|---|
| Principal Component Analysis (PCA) / UMAP | Unsupervised dimensionality reduction for visualizing sample clustering [76]. | Samples group by batch or acquisition date instead of biological condition. |
| Sample Correlation Analysis | Heatmaps of correlation between samples [73]. | Higher correlation among samples from the same batch compared to other batches. |
| Trend Line Plots | Plotting sample intensity medians or internal standard intensities in run order [73]. | A systematic upward or downward drift in intensity over time. |
| Boxplots | Plotting distribution of intensities (e.g., for all proteins/genes) per sample [73]. | Differences in median intensity, variance, or distribution shape between batches. |
The following workflow outlines a step-by-step process for diagnosing these issues:
What are the main strategies to correct for batch effects and drift?
Correction strategies can be categorized based on their underlying approach. The choice of method often depends on the omics field and experimental design.
Table 2: Comparison of Batch Effect and Drift Correction Methods
| Method | Principle | Best For | Pros & Cons |
|---|---|---|---|
| Combat | Empirical Bayes framework to adjust for known batch variables [76]. | Bulk transcriptomics, proteomics. | PRO: Simple, widely used. CON: Requires known batch info; may not handle nonlinear drift [76]. |
| SVA (Surrogate Variable Analysis) | Estimates and removes hidden sources of variation (unobserved batch effects) [76]. | Studies where batch variables are unknown or complex. | PRO: Does not require pre-specified batch labels. CON: Risk of removing biological signal if not carefully modeled [76]. |
| QC-Sample Based (e.g., SVR, RSC) | Uses regularly spaced pooled Quality Control (QC) samples to model and correct signal drift [74] [77]. | Metabolomics, proteomics with QC samples. | PRO: Directly corrects instrument drift. CON: Requires QC samples throughout the run [77]. |
| Bead-Based Normalization | Uses spiked-in metal-labeled beads as an internal standard to track and correct for signal drift [75]. | Mass cytometry (CyTOF) data. | PRO: Highly effective for instrument-specific drift. CON: Specific to mass cytometry [75]. |
| Harmony/fastMNN | Integrates datasets by aligning cells in a shared embedding space [76]. | Single-cell RNA-seq data. | PRO: Preserves biological variation while integrating batches. CON: Computationally intensive for very large datasets [76]. |
The general workflow for applying these corrections, from raw data to adjusted data ready for analysis, is as follows:
How do I validate that the batch correction was successful?
After applying a correction method, it is critical to validate its performance to ensure technical artifacts were removed without erasing biological signal.
Table 3: Metrics for Validating Batch Correction Success
| Validation Method | Description | Interpretation of Success |
|---|---|---|
| Visual Inspection (PCA/UMAP) | Re-examine the pre-correction diagnostic plots [76]. | Samples should cluster by biological group, not by batch. |
| Average Silhouette Width (ASW) | Quantifies how well samples mix across batches after correction [76]. | Higher scores indicate better batch mixing (closer to 1). |
| kBET | k-nearest neighbor Batch Effect test assesses if local neighborhoods of samples are well-mixed with respect to batch [76]. | A high acceptance rate indicates successful mixing. |
| Replicate Correlation | Measures the correlation between technical replicates across different batches [77]. | Increased correlation after correction indicates reduced technical noise. |
What are the best practices in experimental design to prevent batch effects?
Prevention is the most effective strategy. A well-designed experiment significantly reduces the burden of computational correction.
Table 4: Best Practices in Experimental Design
| Practice | Implementation | Benefit |
|---|---|---|
| Randomization | Randomly assign samples from all biological groups across processing and analysis batches [76]. | Prevents complete confounding of batch and biological group. |
| Balanced Design | Ensure each batch contains a balanced number of samples from each condition or time point [72]. | Allows statistical models to separate batch from biological effects. |
| Use of QC Samples | Include pooled quality control (QC) samples at regular intervals throughout the run [74] [77]. | Enables monitoring and correction of signal drift. |
| Replication Across Batches | Process technical replicates or a reference sample in every batch [75]. | Provides a direct anchor for cross-batch alignment. |
| Standardization | Use consistent reagents, protocols, and personnel training throughout the study [76]. | Minimizes the introduction of technical variability at the source. |
The role of quality assurance in managing batch effects throughout the data lifecycle is summarized below:
The Scientist's Toolkit: Essential Reagents and Materials
Table 5: Key Research Reagent Solutions for Batch Effect Management
| Item | Function | Field of Application |
|---|---|---|
| Pooled QC Sample | A homogenous pool of all or a representative subset of study samples; used to monitor and correct for instrument drift [74] [77]. | Metabolomics, Proteomics. |
| Stable Isotope-Labeled Internal Standards | Chemically identical but heavy-isotope-labeled compounds spiked into each sample at known concentration; used for normalization [77]. | Metabolomics, Proteomics. |
| Reference Standards | Well-characterized samples with known properties; used to validate bioinformatics pipelines and identify systematic errors [9]. | All omics fields. |
| Barcoding Kits (e.g., Pd-based) | Kits for multiplexing samples, allowing multiple samples to be processed and acquired simultaneously, reducing batch variation [75]. | Mass Cytometry (CyTOF), Proteomics. |
| Lanthanide-Labeled Beads | Beads with embedded heavy metals are spiked into samples as an internal standard for signal drift correction in mass cytometry [75]. | Mass Cytometry (CyTOF). |
FAQs on Batch Effect Correction
Q1: What's the difference between normalization and batch effect correction?
- Normalization brings all samples to the same scale to make them comparable (e.g., correcting for total ion count differences).
- Batch effect correction specifically removes systematic technical variation associated with batch variables [73]. Normalization is typically done first.
Q2: Can batch correction remove true biological signal? Yes, overcorrection is a risk, particularly if batch effects are confounded with the biological effect of interest or if an inappropriate method is used. This is why validation is crucial [76].
Q3: For a longitudinal study, at which data level should I perform batch correction? It is generally recommended to perform correction at the lowest level of data aggregation. For proteomics, correct at the peptide or fragment ion level before protein inference. For transcriptomics, correct at the gene count level [73].
Q4: What is the single best batch correction method? There is no one-size-fits-all solution. The best method depends on your data type (e.g., bulk vs. single-cell), the strength and nature of the batch effect, and whether you have QC samples. It is advisable to test multiple methods and validate them thoroughly [72] [77].
Q5: How many batches or replicates are needed for reliable correction? A minimum of two replicates per biological group per batch is ideal. More batches allow for more robust statistical modeling of the batch effect [76].
Optimizing Chromatography and Mass Spectrometer Performance
In systems biology research, the integrity of scientific conclusions is fundamentally dependent on the quality of the raw analytical data. Chromatography and mass spectrometry (MS) instruments serve as primary data generators in omics disciplines (proteomics, metabolomics, lipidomics), making their performance a cornerstone for reproducible, high-quality data [9]. The integration of multiple heterogeneous datasets to model and predict biological processes requires that underlying instrumental data be reliable, consistent, and standardized to enable meaningful exchange and reuse [7]. Performance optimization directly addresses the reproducibility crisis, where studies indicate over 70% of researchers have failed to reproduce another scientist's experiments, and 50% have failed to reproduce their own [9].
Adherence to the FAIR (Findable, Accessible, Interoperable, Reusable) data principles is now a critical objective for the systems biology community [78] [47]. This guide provides targeted troubleshooting and best practices to maintain instrument performance at a level that supports these ambitious data quality standards, ensuring that research assets can be meaningfully integrated and reused to accelerate scientific discovery [7].
FAQs: Addressing Common Instrumental and Workflow Challenges
What are the initial steps if my mass spectrometer shows a sudden drop in signal intensity? Begin by checking for clogged electrospray ionization (ESI) sources, a common culprit often caused by non-volatile components in samples or mobile phases. Verify the instrument's vacuum status and recent power history, as power failures can cause system venting requiring bake-out procedures [79].
How can I improve the robustness of my LC-MS method for complex biological samples? Utilize modern instrumentation designed for extreme robustness. For high-throughput labs, newer tandem quadrupole instruments can deliver over 20,000 injections without performance degradation. Implement advanced ion guides that efficiently remove contaminants before they reach the mass analyzer [80].
My GC-MS data shows drift over a long-term study. How can I correct this? Establish a quality control (QC) sample-based correction protocol using algorithms like Random Forest, which has proven most stable for correcting long-term, highly variable data. Measure pooled QC samples at regular intervals and use the data to normalize actual sample runs, accounting for batch and injection order effects [81].
What is the most effective way to reduce downtime in a high-throughput analytical laboratory? Focus on preventive maintenance and robust system design. Instruments engineered with contamination-resistant ion optics and automated calibration features can significantly reduce unplanned downtime. Implementing cloud-based monitoring solutions enables remote instrument checks and faster troubleshooting response [82] [80].
How can I make advanced MS techniques more accessible to novice users in my team? Leverage standardized, pre-configured system setups and intelligent interfaces. New "plug-and-play" ion sources with memory capabilities document usage and automatically share metadata with instrument software, simplifying operation while ensuring data consistency [80].
What strategies best support data standardization in collaborative systems biology projects? Adopt community-developed standards such as Systems Biology Markup Language (SBML) and employ minimum information checklists (MIAME, MIASE) for describing data and models. Utilize bespoke data management platforms like SEEK that support functional linking for data and model integration, helping retain critical experimental context [7].
Troubleshooting Guides: Step-by-Step Problem Resolution
Empty or Abnormally Low Chromatogram Signals
Figure 1: Troubleshooting workflow for empty or abnormally low chromatogram signals.
Follow this logical path to diagnose and resolve issues causing absent or diminished signals [83]:
Sample Injection Verification
- Confirm the sample vial is not empty and contains sufficient volume for injection.
- Check for air bubbles in the sample syringe or injection loop.
- Verify autosampler operation and injection sequence programming.
Liquid Chromatography Flow Path Diagnosis
- Ensure mobile phase reservoirs contain adequate solvent and lines are submerged.
- Confirm LC pumps are generating stable pressure and flow.
- Check for leaks or blockages in the entire flow path, including guard columns, analytical columns, and connecting tubing.
Mass Spectrometer Ion Source and Detector Inspection
- Examine the electrospray ionization (ESI) spray needle for clogs, which are frequently caused by non-volatile components in samples [79]. Clean or replace the needle following manufacturer protocols.
- Inspect the ion transfer tube or capillary for obstruction.
- Verify detector settings, gains, and high voltage supplies are operational.
High Background Signal or Contamination in Blank Runs
Figure 2: Troubleshooting workflow for high background signal or contamination in blank runs.
Elevated signals in method blanks indicate system contamination that must be addressed for reliable data [83]:
Liquid Chromatography System Carryover
- Perform intensive washing of the entire LC flow path with strong solvents appropriate for the column chemistry.
- Include dedicated needle wash steps in the automated method to minimize sample-to-sample carryover.
- For sticky compounds like biopharmaceuticals, consider using specialized systems and consumables designed to reduce analyte interactions [82].
Mass Spectrometer Source and Optics Contamination
- Clean the ESI source assembly (including spray needle, ion cone, and lenses) according to the manufacturer-recommended schedule and procedures.
- If background persists, inspect and clean downstream ion optics, which may require qualified service personnel.
Reagent and Mobile Phase Purity
- Use MS-grade or higher purity solvents and additives to minimize chemical background.
- Prepare fresh mobile phases regularly and use clean glassware.
- Consider establishing separate LC lines dedicated for blank injections to prevent cross-contamination from high-abundance samples.
Inaccurate Mass Measurement or Calibration Drift
Table 1: Mass Accuracy Troubleshooting Guide
| Observation | Potential Cause | Corrective Action |
|---|---|---|
| Consistent mass offset across all peaks | Incorrect calibration | Recalibrate instrument using manufacturer-specified calibration solution |
| Mass drift over time in long sequences | Temperature fluctuation in mass analyzer | Allow sufficient instrument warm-up time; implement periodic lock mass or reference compound infusion |
| Mass errors specific to certain ( m/z ) ranges | Contaminated ion optics or detector aging | Clean ion path components; contact service engineer for detector assessment |
| Poor mass accuracy only in high-pressure LC-MS mode | Incompatibility between LC flow rate and ion source parameters | Re-optimize ion source settings (gas flows, temperatures) for current LC conditions |
Follow this systematic approach [83]:
Immediate Calibration Verification
- Run the manufacturer-recommended calibration solution and verify mass accuracy meets instrument specifications.
- If calibration fails, perform a full instrumental calibration following standard protocols.
Environmental and Operational Factor Assessment
- Ensure the mass spectrometer has achieved thermal equilibrium, as temperature fluctuations in the analyzer can cause mass drift.
- For long sequences, incorporate a continuous reference compound or use quality control samples measured at regular intervals to enable post-acquisition correction [81].
Instrument Component Evaluation
- Check ion optics for contamination requiring cleaning.
- If mass errors persist despite calibration, contact technical support for comprehensive diagnostic testing, which may detect underlying electronic or detector issues.
Experimental Protocols for Quality Assurance
Protocol: Long-Term GC-MS Signal Drift Correction Using Quality Control Samples
Purpose: To correct for instrumental signal drift in GC-MS data acquired over extended periods (e.g., 155 days), ensuring quantitative comparability across all measurements [81].
Principles: Periodic analysis of a pooled Quality Control (QC) sample establishes a correction model based on batch number and injection order. The Random Forest algorithm has demonstrated superior performance for this application compared to spline interpolation or support vector regression [81].
Table 2: Key Reagents and Materials for Drift Correction Protocol
| Item | Specification | Purpose |
|---|---|---|
| Pooled QC Sample | Aliquots combined from all experimental samples | Represents entire chemical space of study; correction standard |
| Internal Standards | Stable isotope-labeled analogs of target analytes | Monitor and correct for individual sample preparation variations |
| Calibration Mixture | Certified reference materials at known concentrations | Initial instrument calibration and performance verification |
| Random Forest Algorithm | Python scikit-learn implementation | Computational correction of peak areas using QC data |
Procedure:
QC Sample Preparation:
- Combine equal aliquots from all experimental samples to create a homogeneous pooled QC sample.
- Divide into multiple identical vials and store under conditions that preserve sample integrity.
Experimental Design and Data Acquisition:
- Analyze the QC sample repeatedly (e.g., 20 times over 155 days) interspersed with experimental samples in a randomized sequence.
- Record the batch number (incremented at each instrument restart) and injection order number for all QC and sample analyses.
Data Processing and Model Building:
- For each chemical component ( k ) in the QC samples, calculate the correction factor ( y{i,k} = X{i,k} / X{T,k} ), where ( X{i,k} ) is the peak area in measurement ( i ), and ( X_{T,k} ) is the median peak area across all QC measurements [81].
- Using the correction factors ( {y{i,k}} ) as the target dataset, train a Random Forest model to find the function ( yk = f_k(p, t) ), where ( p ) is batch number and ( t ) is injection order.
Sample Data Correction:
- For components present in both sample and QC, calculate the corrected peak area ( x'{S,k} = x{S,k} / y ), where ( y ) is predicted by the model [81].
- For sample components not in QC, apply correction using adjacent chromatographic peaks or average correction coefficients from all QC data.
Validation: Principal Component Analysis (PCA) and standard deviation analysis of corrected QC data should show tight clustering, confirming reduced technical variance.
Protocol: Automated LC-MS System Performance Monitoring
Purpose: To establish an automated workflow for continuous monitoring of LC-MS system performance, enabling proactive maintenance and ensuring consistent data quality.
Principles: Regular analysis of standardized samples tracks key performance indicators (sensitivity, retention time stability, mass accuracy) over time, with cloud-based data tracking facilitating trend analysis and alert generation [82].
Procedure:
Performance Standard Preparation:
- Prepare a mixture of known compounds covering the mass range and retention times relevant to your analyses.
- Store in single-use aliquots to minimize variation.
Scheduled Analysis:
- Program the automated sequence to inject the performance standard daily or between every set of experimental samples.
- Utilize scheduled instrument calibration and system suitability tests to maintain performance [80].
Data Analysis and Alert System:
- Automatically process performance standard data to extract metrics: signal intensity, peak area reproducibility, retention time stability, and mass accuracy.
- Implement control charts with upper and lower limits for each metric.
- Configure automated alerts for when metrics trend toward specification limits.
Corrective Action Triggers:
- Define specific actions for each performance metric deviation (e.g., source cleaning for sensitivity drop, column replacement for retention time shifts).
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for Chromatography-MS Optimization
| Category | Specific Examples | Function in Experiment |
|---|---|---|
| Quality Control Materials | Pooled study samples; Standard reference materials (NIST) | Monitor instrument performance; Enable quantitative correction and data normalization |
| System Suitability Standards | Vendor-provided tuning solutions; Custom analyte mixtures | Verify instrument meets sensitivity, resolution, and mass accuracy specifications before sample analysis |
| Internal Standards | Stable isotope-labeled analogs; Chemical class surrogates | Correct for sample preparation losses and matrix effects; Improve quantitative accuracy |
| Column Regeneration Solvents | MS-grade acetonitrile, methanol, water; High-purity acids and buffers | Clean and regenerate chromatographic columns; Remove contaminants and restore separation performance |
| Ion Source Cleaning Kits | Manufacturer-specific tools; Ultrasonic cleaning baths; Polishing compounds | Maintain optimal ionization efficiency; Reduce background noise and signal suppression |
| Data Processing Tools | SBML-compliant software [78]; FAIR data platforms [47]; Automated QC algorithms [81] | Standardize data formatting; Ensure reproducibility and reusability according to community standards |
Optimizing chromatography and mass spectrometer performance transcends routine maintenance—it is a fundamental requirement for producing the high-quality, reproducible data that underpins reliable systems biology research. By implementing the troubleshooting guides, experimental protocols, and quality assurance measures outlined herein, researchers can significantly enhance their analytical data's credibility, interoperability, and long-term reusability.
The convergence of well-maintained instrumentation, standardized data formats like SBML, and FAIR data management practices creates a powerful framework for accelerating discovery in systems biology [7] [78]. This integrated approach ensures that valuable research assets can be meaningfully shared, validated, and built upon by the broader scientific community, ultimately advancing our understanding of complex biological systems.
Benchmarking Performance and Establishing Community Standards
In systems biology and drug development, establishing robust acceptance criteria for analytical methods is not optional—it's a fundamental requirement for generating reliable and reproducible data. Proper criteria for precision, accuracy, and false discovery rates (FDR) act as a quality control framework, ensuring that your findings are trustworthy and that resources are not wasted pursuing false leads. This guide provides troubleshooting advice and definitive protocols to help you set and validate these critical parameters within your research workflows.
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between precision and accuracy in the context of bioinformatics data?
- Precision, often measured by metrics like repeatability standard deviation or %CV, refers to the closeness of agreement between independent measurements obtained under the same conditions. It is about consistency and random error [84].
- Accuracy, or bias, refers to the closeness of agreement between a measured value and its true accepted reference value. It is about systematic error [84].
- In a classification context, precision is the proportion of true positives among all positive predictions (Precision = TP / (TP + FP)), which is crucial when the cost of false positives is high [85].
Q2: How should I set acceptance criteria for precision and accuracy when I have product specification limits? Traditional metrics like %CV can be misleading. Instead, evaluate precision and accuracy relative to your product's specification tolerance or design margin [84].
- For Precision (Repeatability): Calculate
(Repeatability Standard Deviation * 5.15) / (USL - LSL). The recommended acceptance criterion for analytical methods is ≤ 25% of tolerance, and for bioassays, it is ≤ 50% of tolerance [84]. - For Accuracy (Bias): Calculate
Bias / (USL - LSL). The recommended acceptance criterion is ≤ 10% of tolerance for both analytical methods and bioassays [84].
Q3: What is the False Discovery Rate (FDR), and why is it a problem in high-throughput biology?
- The FDR is the expected proportion of false discoveries among all reported positive findings. Controlling the FDR is standard practice in omics studies (e.g., genomics, proteomics) to manage the deluge of statistical tests [86].
- A critical problem is that in datasets with highly correlated features (like gene expression or metabolomics data), standard FDR control methods like Benjamini-Hochberg (BH) can sometimes, and counter-intuitively, report a very high number of false positives, even when all null hypotheses are true. This can mislead researchers into believing they have found hundreds of significant results when, in fact, they have not [86].
Q4: My proteomics pipeline uses a target-decoy approach for FDR control. How can I be sure it's working correctly?
- Many proteomics software tools may not consistently control the FDR, especially in Data-Independent Acquisition (DIA) analyses and at the protein level [87].
- You can validate your pipeline using an entrapment experiment, where you expand the search database with peptides from a species not in your sample. However, a 2025 study highlights that many published studies use entrapment incorrectly. Use the validated "combined" method for estimation:
FDP = (N_e * (1 + 1/r)) / (N_t + N_e), whereN_eandN_tare the number of entrapment and target discoveries, andris the ratio of entrapment to target database size [87].
Q5: What should I do if my positive control shows acceptable accuracy and precision, but I'm still getting high FDRs in my discovery experiments?
- This discrepancy suggests that the error control specific to your high-dimensional testing regime is inadequate. High FDRs often stem from dependencies in the data or slight biases that break test assumptions [86]. It is recommended to use suited multiple testing strategies and approaches like synthetic null data (negative controls) to identify and minimize caveats related to false discoveries [86]. Furthermore, for data types like in eQTL studies, global FDR correction methods like BH are considered inappropriate, and LD-aware methods or permutation testing should be used instead [86].
Troubleshooting Guides
High False Discovery Rate (FDR) in Omics Analyses
Problem: A surprisingly large number of significant features (genes, proteins, metabolites) are reported after FDR correction, but validation experiments fail.
Diagnosis & Solution:
| Step | Action | Rationale & Reference |
|---|---|---|
| 1 | Check Feature Dependencies | Run your analysis on a synthetic null dataset (where no true effects exist) with shuffled labels. If many features are still significant, strong correlations between features are likely inflating your FDR [86]. |
| 2 | Validate FDR Control via Entrapment | For proteomics, perform an entrapment experiment. Use the correct "combined" formula to calculate the FDP and plot it against the tool's reported FDR. If the lower bound estimate is consistently above the y=x line, your tool is failing to control the FDR [87]. |
| 3 | Use a More Robust Correction Method | Avoid relying solely on the Benjamini-Hochberg method for data with known strong dependencies (e.g., genes in pathways, SNPs in LD). Switch to permutation-based testing or other dependency-aware methods that are considered the gold standard in fields like GWAS and eQTL mapping [86]. |
| 4 | Verify Raw Data Quality | Ensure that poor data quality is not introducing biases. Check standard QA metrics for your data type (e.g., Phred scores, alignment rates, batch effects), as these can create systematic patterns that mimic true signals and increase false positives [9]. |
Experimental Protocol: Entrapment for FDR Validation in Proteomics
- Database Expansion: Create a concatenated database containing the true target proteins (
T) and a set of "entrapment" proteins (E). The entrapment proteins should be from an organism not present in your sample (e.g., add S. cerevisiae proteins to a human sample analysis) [87]. - Analysis: Run your standard proteomics data analysis pipeline (e.g., DIA-NN, Spectronaut) using this expanded database. Keep the entrapment hidden from the tool's logic.
- Result Collection: After analysis at a specific FDR threshold (e.g., 1%), record:
N_t: The number of discovered target peptides/proteins.N_e: The number of discovered entrapment peptides/proteins.r: The ratio of the sizes of the entrapment and target databases (r = size(E) / size(T)).
- FDP Calculation: Use the validated combined method to estimate the actual False Discovery Proportion [87]:
Estimated FDP = [ N_e * (1 + 1/r) ] / (N_t + N_e) - Interpretation: Plot the estimated FDP against the tool's reported FDR for a range of thresholds. If the curve lies above the y=x line, it indicates a failure to control the FDR at the claimed level.
The workflow below visualizes this entrapment validation process.
Poor Method Precision or Accuracy
Problem: Reportable results show high variability (poor precision) or a consistent shift from the reference value (poor accuracy), leading to unreliable product quality assessments.
Diagnosis & Solution:
| Step | Action | Rationale & Reference |
|---|---|---|
| 1 | Define Tolerance/Margin | Calculate your specification tolerance (USL - LSL) for two-sided specs or the margin (USL - Mean or Mean - LSL) for one-sided specs. Your acceptance criteria must be relative to this [84]. |
| 2 | Quantify Errors Relatively | Express precision as a % of tolerance and accuracy (bias) as a % of tolerance, not just as %CV or %recovery. This directly links method performance to its impact on product acceptance and OOS rates [84]. |
| 3 | Benchmark Against Standards | Compare your calculated %Tolerance for precision and accuracy against recommended standards (e.g., ≤25% and ≤10% of tolerance, respectively). If your values exceed these, the method error is consuming too much of the product specification and needs optimization [84]. |
| 4 | Troubleshoot the Method | Investigate the analytical method itself. Issues could lie in sample preparation, instrument calibration, reagent stability, or data processing algorithms. Implement rigorous QA protocols to proactively prevent these errors [9]. |
The following diagram outlines the logical workflow for establishing and troubleshooting method acceptance criteria.
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key materials and computational tools essential for implementing the quality control measures discussed in this guide.
| Item Name | Function & Purpose in Quality Control |
|---|---|
| Reference Standards | Well-characterized samples with known properties used to validate bioinformatics pipelines, identify systematic errors, and establish accuracy (bias) [9]. |
| Entrapment Databases | Databases containing peptides or sequences from organisms not present in the sample. They are used in entrapment experiments to empirically evaluate the false discovery rate control of analytical pipelines [87]. |
| Synthetic Null Datasets | Datasets generated by shuffling labels or simulating data where no true effects exist. Used to diagnose issues with FDR control arising from data dependencies and correlations [86]. |
| Quality Assessment Software | Tools like FastQC for sequencing data, which generate raw data quality metrics (Phred scores, GC content, adapter contamination) essential for the initial QA step [9]. |
| FDR Evaluation Tools | Scripts or software packages that implement correct entrapment estimation methods (e.g., the "combined" method) to rigorously assess the validity of a tool's FDR claims [87]. |
Quantitative Acceptance Criteria Recommendations
| Validation Characteristic | Recommended Calculation | Recommended Acceptance Criterion (Analytical Method) | Recommended Acceptance Criterion (Bioassay) |
|---|---|---|---|
| Precision (Repeatability) | (Stdev * 5.15) / (USL - LSL) | ≤ 25% of Tolerance | ≤ 50% of Tolerance [84] |
| Accuracy (Bias) | Bias / (USL - LSL) | ≤ 10% of Tolerance | ≤ 10% of Tolerance [84] |
| LOD (Limit of Detection) | LOD / Tolerance * 100 | Excellent: ≤ 5%, Acceptable: ≤ 10% | Excellent: ≤ 5%, Acceptable: ≤ 10% [84] |
| LOQ (Limit of Quantitation) | LOQ / Tolerance * 100 | Excellent: ≤ 15%, Acceptable: ≤ 20% | Excellent: ≤ 15%, Acceptable: ≤ 20% [84] |
Comparison of FDR Evaluation Methods
| Estimation Method | Formula | Purpose & Interpretation |
|---|---|---|
| Combined (Valid Upper Bound) | FDP = (N_e * (1 + 1/r)) / (N_t + N_e) |
Provides an estimated upper bound on the FDP. If this curve falls below the y=x line, it is evidence that the tool successfully controls the FDR [87]. |
| Invalid Lower Bound | FDP = N_e / (N_t + N_e) |
Provides a lower bound on the FDP. If this curve falls above the y=x line, it is evidence that the tool fails to control the FDR. Using it to claim success is incorrect [87]. |
Longitudinal Performance Assessment and Inter-laboratory Harmonization
Troubleshooting Guides
Troubleshooting Longitudinal Performance Drift in LC-MS/MS Systems
Problem: Gradual decay in instrument performance over time, leading to decreased peptide identifications and quantitative variability.
| Observed Issue | Potential Root Cause | Corrective Action |
|---|---|---|
| Decreased number of peptide identifications over successive runs [88] | Contamination of ion source or chromatography column | Implement routine system suitability tests using stable isotope-coded peptides; perform instrument cleaning and column replacement as per SOP [88] |
| Increasing quantitative variability between replicate runs [88] | Degradation of chromatographic performance or mass calibrant | Assess chromatographic peak shape and retention time stability; verify mass calibration accuracy; use quality control metrics (e.g., QuaMeter) for continuous monitoring [88] |
| Inconsistent performance across multiple identical LC-MS/MS platforms [88] | Lack of standardized protocols and quality control metrics between instruments | Establish standardized operating procedures (SOPs) and implement centralized quality assessment metrics across all platforms [88] |
| Failure to detect minor performance decays [88] | Insufficient sensitivity of monitoring procedures | Deploy a longitudinal performance assessment system with a reasonably complex proteome sample to detect subtle system decays [88] |
Troubleshooting Inter-laboratory Assay Harmonization
Problem: Inconsistent results for the same sample across different laboratories or testing platforms.
| Observed Issue | Potential Root Cause | Corrective Action |
|---|---|---|
| Differing results from different analytical methods [89] | Methods not harmonized, potentially using different reporting units | Identify gaps in testing and harmonize methods; use commutable secondary reference materials to ensure comparability [89] |
| Poor inter-laboratory reproducibility in NGS assays [90] | Assay performance variability between laboratory-developed tests (LDTs) | Perform concordance testing with a central reference assay; require 80% concordance threshold for network participation [90] |
| Lack of comparability in PCR-based assays (e.g., EBV DNA quantitation) [90] | Limitations in clinical use and interpretation of assay results | Convene expert workshops to establish recommendations for assay harmonization, validation, and appropriate clinical use [90] |
| Misinterpretation of laboratory results by clinicians [89] | Lack of harmonized processes across the total testing process (TTP) | Apply a systematic approach to harmonization including test requesting, sample handling, analysis, and reporting phases [89] |
Frequently Asked Questions (FAQs)
Q1: What is the core objective of longitudinal performance assessment in proteomics? The primary goal is to evaluate and maintain the long-term qualitative and quantitative reproducibility of LC-MS/MS platforms. This involves routine performance assessment to detect minor system decays, promote standardization across laboratories, and ensure the reliability of proteomics data over time [88].
Q2: How does inter-laboratory harmonization differ from standardization? Harmonization aims to achieve the same clinical interpretation of a test result, within clinically acceptable limits, irrespective of the measurement procedure, unit, or location. It acknowledges that different methods may be used but seeks to make their results comparable. Standardization typically involves all laboratories using the identical method and procedures [89].
Q3: What are the critical steps for a successful harmonization project? A systematic approach is essential [89]:
- Awareness: Recognize the need for harmonization across all steps of the total testing process.
- Planning: Develop an organizational roadmap with a detailed problem definition, relevant working groups, and funding sources.
- Consensus: Communicate with all stakeholders (pathologists, clinicians, regulatory bodies) to reach a cooperative consensus.
- Implementation & Monitoring: Publish and promote recommendations, then actively survey their adoption and effectiveness.
Q4: What is a key resource for ensuring harmonization in Next-Generation Sequencing (NGS) assays? The use of external reference standards is critical. Initiatives like the SPOT/Dx Working Group provide reference samples and in silico files to evaluate the analytical performance of validated NGS platforms against a gold standard, thereby achieving inter-laboratory standardization [90].
Q5: Which key metrics are used for quality control in longitudinal LC-MS/MS performance? Long-term performance is assessed using metrics such as the number of confidently identified peptides, quantitative reproducibility over time, chromatographic retention time stability, and mass accuracy. Tools like QuaMeter and SIMPATIQCO can monitor these performance metrics on Orbitrap instruments [88].
| Performance Metric | Assessment Method/Tool | Goal / Benchmark |
|---|---|---|
| Peptide Identification | Number of peptides identified from a complex proteome sample in a single LC-MS/MS run | Maximize depth; monitor for decays over time |
| Qualitative Reproducibility | Consistency of peptide identifications across replicate runs and over time | Achieve high reproducibility |
| Quantitative Reproducibility | Consistency of peptide abundance measurements across replicate runs and over time | Achieve high reproducibility |
| System Performance Monitoring | QuaMeter, SIMPATIQCO, SprayQc, jqcML | Attain standardization across multiple laboratories |
| Harmonization Parameter | Stage | Activity / Stakeholder Example |
|---|---|---|
| Test Requesting & Profiles | Pre-analytical | Harmonize test profiles (e.g., EFLM WG-PRE) |
| Sample Collection & Handling | Pre-analytical | Guidelines for patient preparation and transport (e.g., CLSI, EFLM WG-PRE) |
| Traceability & Reference Materials | Analytical | Use JCTLM-listed reference materials (e.g., BIPM, JCTLM) |
| Commutable Reference Materials | Analytical | Development of secondary reference materials (e.g., NIST, IRMM) |
| Assay Concordance | Analytical | Inter-laboratory concordance testing (e.g., 80% threshold in NCI DL Network) [90] |
| Reporting Units & Terminology | Post-analytical | Standardize units and terminology (e.g., IFCC C-NPU, Pathology Harmony) |
| Reference Intervals | Post-analytical | Establish common intervals for traceable analytes (e.g., IFCC C-RIDL) |
Experimental Protocols
Principle: Regular analysis of a standardized, complex proteome sample to monitor the stability of LC-MS/MS platform performance over time, assessing both qualitative (identification) and quantitative (reproducibility) metrics.
Workflow:
Materials:
- Standardized Proteome Sample: A consistently prepared, reasonably complex proteome extract (e.g., yeast lysate) [88].
- LC-MS/MS System: nanoflow Liquid Chromatography system coupled to an Orbitrap mass spectrometer.
- Data Processing Software: Software capable of peptide identification and quantification (e.g., MaxQuant, Proteome Discoverer).
- Quality Control Monitoring Tools: Software for tracking performance metrics (e.g., QuaMeter, SIMPATIQCO, jqcML) [88].
Procedure:
- Sample Reconstitution: Reconstitute the aliquoted standardized proteome sample in a suitable LC-MS compatible buffer according to the established SOP.
- System Equilibration: Ensure the nLC system and Orbitrap mass spectrometer are fully equilibrated and calibrated according to manufacturer specifications and laboratory SOPs.
- Data Acquisition: Inject a predetermined amount of the standardized sample onto the nLC-MS/MS system. Perform the analysis using the standardized, validated LC-MS/MS method with data-dependent acquisition (DDA).
- Data Processing: Process the raw data files through the standardized bioinformatics pipeline for peptide and protein identification and quantification.
- Metric Calculation: Calculate key performance metrics from the processed data. These must include:
- Total number of confidently identified peptides.
- Total number of identified proteins.
- Chromatographic metrics (e.g., median peak width, retention time stability).
- Mass accuracy metrics.
- Trend Analysis & Comparison: Compare the calculated metrics against the laboratory's established historical baseline and control limits. Use statistical process control (SPC) charts to visualize trends and identify significant performance decays.
- Corrective Action: If metrics indicate performance decay outside acceptable limits, initiate troubleshooting procedures. This may involve cleaning the ion source, replacing the chromatography column, or re-calibrating the instrument.
Principle: Use of shared reference standards and concordance testing to ensure uniform analytical performance and result interpretation across multiple laboratories employing different NGS platforms and laboratory-developed tests (LDTs).
Workflow:
Materials:
- Reference Standards: Well-characterized, commutable reference samples (e.g., cell line-derived DNA with known variants) and in silico sequence files [90].
- Central Reference Assay: An FDA-approved companion diagnostic or a gold-standard assay serving as the benchmark for concordance [90].
- Data Exchange Platform: A secure system for centralized collection of raw data and variant call files (VCFs) from all participating labs.
- Bioinformatics Pipeline: Standardized pipeline for centralized data re-analysis to minimize pipeline-induced variability.
Procedure:
- Benchmark Definition: Establish clear analytical performance benchmarks for the harmonization effort. This includes defining the variant types of interest (SNVs, Indels, CNVs, etc.) and setting a minimum concordance threshold (e.g., ≥80% positive percent agreement with the central assay) [90].
- Reference Material Distribution: Procure and distribute identical aliquots of the reference standards to all laboratories participating in the network.
- Testing Phase: Each laboratory processes the reference standards through their own clinically validated NGS platform and bioinformatics pipeline, following their routine SOPs.
- Data Submission: Participating laboratories submit their final variant call files (VCFs) and, if required, raw sequencing data (BAM/FASTQ files) to the coordinating center.
- Concordance Analysis: The coordinating center performs a centralized comparison of each laboratory's results against the results from the central reference assay. The analysis focuses on the pre-defined variants and calculates concordance rates.
- Network Admission: Laboratories that meet or exceed the pre-defined concordance threshold are admitted into the harmonized network.
- Ongoing Proficiency Monitoring: Maintain harmonization through periodic proficiency testing, monitoring of CLIA certifications, and reporting of any ultimate adverse event reports (UADEs) or significant changes to the approved assay [90].
The Scientist's Toolkit: Research Reagent Solutions
| Item / Resource | Function / Application | Key Feature / Standard |
|---|---|---|
| Stable Isotope-Coded Peptides [88] | Internal standards for quality control of nano-LC-MS systems; monitoring instrument performance | Enables precise quantification and detection of performance drift |
| Commutable Secondary Reference Materials (RM) [89] [90] | Calibrate different measurement procedures to a common standard, enabling result comparability | Commutability ensures material behaves like a clinical sample across methods |
| Complex Proteome Standard (e.g., Yeast Lysate) [88] | Longitudinal performance assessment sample for LC-MS/MS platforms | Reasonably complex and consistent sample to detect minor system decays |
| Standardized NGS Reference Samples [90] | Harmonize NGS assay performance across multiple laboratories; used for concordance testing | Characterized DNA with known variants for benchmarking lab performance |
| qcML Format & Tools (e.g., jqcML) [88] | Open-source format and API for exchanging and processing mass spectrometry quality control metrics | Standardizes QC data sharing and analysis |
| QuaMeter [88] | Multivendor tool for calculating performance metrics from LC-MS/MS proteomics instrumentation raw files | Provides standardized metrics for cross-platform comparison |
Using Multivariate Statistics (e.g., PCA) for Outlier Detection and Data Quality Review
FAQs on Multivariate Outlier Detection
Q1: What are the primary advantages of using multivariate methods like Hotelling's T² over univariate control charts for quality control?
Multivariate control charts, such as those based on Hotelling's T² statistic, are superior when monitoring multiple correlated quality control (QC) levels simultaneously. In a multi-level QC (MLQC) system, these levels are often correlated because they are measured by the same analytical process. Using individual univariate charts for each level ignores these correlations, leading to an inflated false positive rate. Hotelling's T² creates a single control chart that accounts for the variance-covariance structure between all variables, ensuring the correct level of false alarms and providing a more accurate state of the analytical process [91].
Q2: In a clustering analysis, how can I determine which variables are most influential in the formation of the clusters?
Principal Component Analysis (PCA) is a powerful tool for this purpose. When performed before or in conjunction with clustering, PCA identifies the principal components that explain the most variance in the data. You can examine the loadings (or contributions) of each original variable on these key components. Variables with higher absolute loadings (e.g., above 0.70) on the first few principal components have a greater influence on the dataset's structure and, consequently, on the cluster separation. For example, one study found that waist circumference, visceral fat, and the LDL/HDL ratio were highly influential (loadings > 0.70), while exercise and height had minimal impact (loadings < 0.30) [92].
Q3: My dataset has missing values and suspected anomalies. What is a robust workflow to address these data quality issues?
A robust machine learning-based strategy involves a structured pipeline focusing on accuracy, completeness, and reusability:
- Step 1 - Address Missing Values: Use imputation techniques like k-nearest neighbors (KNN) to handle missing data, significantly improving data completeness [93].
- Step 2 - Detect Anomalies: Apply ensemble-based anomaly detection algorithms, such as Isolation Forest or Local Outlier Factor (LOF), to identify outliers in the dataset [93].
- Step 3 - Dimensionality Reduction and Analysis: Use PCA and correlation analysis to understand the underlying structure of the data and identify key variables [93]. This entire process should be fully documented with version control to ensure reproducibility [93].
Troubleshooting Guides
Problem: A high number of false alarms from univariate control charts when monitoring multi-level quality control materials.
| Diagnosis Step | Explanation | Solution |
|---|---|---|
| Check for Correlation | A high false alarm rate often occurs when the multiple QC levels are correlated, violating the independence assumption of individual univariate charts. | Calculate the correlation matrix for your QC levels. If significant correlations (e.g., r > 0.6) exist, implement a multivariate control chart using Hotelling's T² statistic [91]. |
| Phase I Analysis | The control limits for the multivariate chart must be stably estimated from a period of known in-control operation. | Collect a baseline dataset (e.g., 50-60 measurements per QC level). Use this data to estimate the vector of means and the variance-covariance matrix, which form the basis for the T² control limits [91]. |
| Phase II Monitoring | The ongoing monitoring phase uses the limits established in Phase I. | Plot the Hotelling's T² values for new QC measurements against the upper control limit (UCL). A point exceeding the UCL indicates a potential out-of-control state for the entire multi-level system [91]. |
Problem: Poor clustering results with high-dimensional health data, making it difficult to identify distinct patient risk groups.
| Diagnosis Step | Explanation | Solution |
|---|---|---|
| High-Dimensionality | In high-dimensional space, distance measures become less meaningful, and noise can obscure actual patterns, a phenomenon known as the "curse of dimensionality." | Integrate Principal Component Analysis (PCA) with a clustering algorithm like Fuzzy C-Means (FCM). Use PCA to reduce the data to its most informative principal components before clustering [92]. |
| Identify Key Variables | Not all variables contribute equally to defining meaningful clusters. Some may be redundant or irrelevant. | After performing PCA, analyze the variable loadings on the first two components. Focus on and interpret the clusters based on variables with high loadings (e.g., > 0.70), as these drive the separation [92]. |
| Validate Cluster Quality | The chosen number of clusters may not best represent the natural grouping in the data. | Use internal validation metrics, such as the Silhouette Score, to evaluate the cohesion and separation of clusters. A higher score (e.g., 0.62) indicates well-defined clusters [92]. |
Experimental Protocols & Data
Protocol 1: Implementing a Hotelling's T² Multivariate Control Chart
Objective: To effectively monitor the quality of an analytical process using multiple, correlated quality control levels.
- Data Collection: For a predetermined period, collect data on your multi-level QC materials. For example, collect 84 consecutive measurements for three levels of QC [91].
- Phase I - Model Building:
- Split the dataset, using the first ~70% of data (e.g., 59 measurements) as the in-control baseline [91].
- From this baseline data, calculate the mean vector (μ) and the variance-covariance matrix (Σ) for the QC levels.
- Calculate the Upper Control Limit (UCL) for the Hotelling's T² chart. The UCL can be derived using the F-distribution:
UCL = [p(m-1)/(m-p)] * F₁₋α, p, m₋p, wherepis the number of QC levels,mis the number of observations in the baseline, andαis the type I error rate [91].
- Phase II - Process Monitoring:
- For each new set of QC measurements (a vector x), calculate the Hotelling's T² statistic:
T² = (x - μ)' * Σ⁻¹ * (x - μ)[91]. - Plot the T² value on the control chart with the UCL. Any point exceeding the UCL signals that the analytical process may be out of control.
- For each new set of QC measurements (a vector x), calculate the Hotelling's T² statistic:
Protocol 2: Integrating PCA with Clustering for Patient Stratification
Objective: To identify distinct at-risk groups in a population using high-dimensional health data.
- Data Preprocessing: Clean the dataset by addressing missing values, for instance, using KNN imputation [93].
- Anomaly Detection: Run an anomaly detection algorithm, such as Isolation Forest, to identify and review potential outliers that could skew the analysis [93].
- Principal Component Analysis (PCA):
- Standardize the data (mean-center and scale to unit variance).
- Perform PCA to transform the original variables into a new set of uncorrelated principal components.
- Decide how many components to retain based on explained variance (e.g., retain components that cumulatively explain >80% of variance) or the scree plot.
- Fuzzy C-Means (FCM) Clustering: Apply the FCM clustering algorithm to the retained principal components, not the original data. FCM assigns each data point a probability of belonging to each cluster, which is useful for capturing ambiguity in health states [92].
- Validation and Interpretation: Evaluate the quality of the resulting clusters using the Silhouette Score. Interpret the clusters by examining the original variables and their PCA loadings to define the clinical profile of each group [92].
Table 1: Quantitative Results from a Multivariate QC Study on a Levetiracetam Immunoassay
| QC Level | Mean Concentration | Correlation (r) with Level 1 | Correlation (r) with Level 2 | Out-of-Control Signals (Univariate Chart) |
|---|---|---|---|---|
| Level 1 | Not Specified | - | - | 12 (Total across all levels) |
| Level 2 | Not Specified | > 0.6 | - | |
| Level 3 | Not Specified | > 0.6 | > 0.6 | |
| Multivariate Chart (Hotelling's T²) | - | - | - | 0 |
This table summarizes key findings from a study that implemented a Hotelling's T² chart for plasma levetiracetam monitoring. The significant correlations between QC levels explain why the multivariate chart, which accounts for these relationships, generated no false alarms compared to the 12 signals from the combined univariate charts [91].
Table 2: Variable Loadings on Principal Components from a Cardiovascular Health Study
| Health Variable | Loading on PC1 | Loading on PC2 | Influence on Clustering |
|---|---|---|---|
| Waist Circumference | > 0.70 | > 0.70 | High |
| Visceral Fat | > 0.70 | > 0.70 | High |
| LDL/HDL Ratio | > 0.70 | > 0.70 | High |
| Non-HDL Cholesterol | > 0.70 | > 0.70 | High |
| Waist-to-Height Ratio | > 0.70 | > 0.70 | High |
| Exercise | < 0.30 | < 0.30 | Minimal |
| Height | < 0.30 | < 0.30 | Minimal |
| HDL | < 0.30 | < 0.30 | Minimal |
This table displays the variable loadings from a PCA-FCM analysis on public health data. Variables with loadings above 0.70 were the most influential in separating the population into distinct risk clusters for cardiovascular disease and obesity [92].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Analysis |
|---|---|
| Hotelling's T² Statistic | A multivariate generalization of the Student's t-statistic used to calculate a unified value that represents the distance of a multi-parameter observation from its in-control mean, accounting for correlations between parameters [91]. |
| Principal Component Analysis (PCA) | A dimensionality reduction technique that transforms a large set of correlated variables into a smaller set of uncorrelated variables called principal components. This helps in visualization, noise reduction, and identifying key drivers of variance in the data [93] [92]. |
| Variance-Covariance Matrix (Σ) | A pivotal matrix in multivariate analysis that describes the structure of relationships between all variables. Its diagonal contains the variances of each variable, and the off-diagonals contain the covariances between variables, which are essential for calculating multivariate distances [91]. |
| Fuzzy C-Means (FCM) Clustering | A clustering algorithm that allows data points to belong to more than one cluster by assigning membership probabilities. This is particularly useful in biomedical contexts where health states or risk groups are not always mutually exclusive [92]. |
| Isolation Forest | An ensemble-based, unsupervised machine learning algorithm designed for efficient anomaly detection. It works by isolating observations in a dataset, making it effective for identifying outliers in high-dimensional data [93]. |
| k-Nearest Neighbors (KNN) Imputation | A method for handling missing data by replacing a missing value with the average value from the 'k' most similar data points (neighbors) in the dataset, thereby improving data completeness [93]. |
| Silhouette Score | An internal validation metric used to evaluate the quality of a clustering result. It measures how similar an object is to its own cluster compared to other clusters, with scores closer to 1 indicating better-defined clusters [92]. |
Workflow Diagrams
Multivariate Quality Control Workflow
PCA-Enhanced Clustering for Patient Stratification
Comparative Analysis of QC Metrics Across Platforms and Laboratories
In modern systems biology and drug development, ensuring the reproducibility, accuracy, and reliability of data across different experimental platforms and laboratories is a fundamental challenge. High-quality data is the cornerstone of valid biological insights and successful regulatory submissions for new therapies [94] [95]. Variability in instruments, reagents, protocols, and analytical pipelines can introduce significant noise, compromising cross-study comparisons and meta-analyses. This technical support center is designed within the broader context of establishing robust, cross-platform quality control (QC) standards for systems biology data. It provides actionable troubleshooting guidance, standardized protocols, and comparative metrics to help researchers and quality control professionals identify, diagnose, and rectify common issues, thereby enhancing data integrity and interoperability [96] [97].
Section 1: Core QC Metrics – A Cross-Platform Comparative Table
The following table summarizes key quantitative QC metrics relevant to common platforms in systems biology and analytical chemistry, highlighting their significance and typical target ranges. These metrics serve as the first line of defense in assessing data quality [94] [95] [96].
| Platform/Technique | Key QC Metric | Typical Target/Threshold | Purpose & Rationale |
|---|---|---|---|
| LC-MS/MS (Biopharmaceuticals) | Signal-to-Noise Ratio (S/N) | >10:1 for LLOQ | Ensures reliable detection and quantification of low-abundance analytes (e.g., host cell proteins) above background noise [94] [98]. |
| Mass Accuracy (ppm) | < 5 ppm (high-res MS) | Confirms correct identification of molecules based on precise mass-to-charge ratio measurement [94]. | |
| Chromatographic Peak Width & Symmetry | RSD < 2% across runs | Indicates consistent chromatographic performance and column integrity, critical for reproducible retention times [94]. | |
| CITE-Seq (Single-Cell Multiomics) | Median Genes per Cell | > 1,000 | Assesses library complexity and sequencing depth; low counts may indicate poor cell viability or cDNA synthesis [95]. |
| Mitochondrial Gene Percentage | < 20% (cell-type dependent) | High percentages often indicate apoptotic or stressed cells; used to filter out low-quality cells [95]. | |
| ADT (Antibody) Total Count | Platform-dependent | Ensures sufficient antibody-derived tag detection for reliable surface protein quantification [95]. | |
| RNA-ADT Correlation (Spearman's ρ) | Positive correlation expected | Evaluates the biological consistency between gene expression and corresponding protein abundance [95]. | |
| Cross-Platform General | Inter-Laboratory CV (Coefficient of Variation) | < 15% (ideally < 10%) | Measures the precision and reproducibility of an assay across different sites and operators [96]. |
| Limit of Detection (LOD) / Quantification (LOQ) | Defined via calibration curve | Establishes the sensitivity of the method for detecting/measuring trace impurities or low-level biomarkers [94]. |
Section 2: Standardized Experimental Protocols for Key QC Analyses
Protocol 2.1: Peptide Mapping with LC-MS/MS for Biotherapeutic Characterization
This method is critical for monitoring Critical Quality Attributes (CQAs) like post-translational modifications [94].
1. Sample Preparation:
- Reduction and Alkylation: Dilute the therapeutic protein to 1 mg/mL in a suitable buffer (e.g., 50 mM Tris-HCl, pH 8.0). Add dithiothreitol (DTT) to 10 mM and incubate at 56°C for 30 minutes to reduce disulfide bonds. Cool, then add iodoacetamide to 25 mM and incubate in the dark at room temperature for 30 minutes to alkylate cysteine residues.
- Digestion: Add a proteolytic enzyme (e.g., trypsin) at a 1:20 (w/w) enzyme-to-protein ratio. Incubate at 37°C for 4-18 hours. Quench the reaction by acidification with formic acid (final concentration ~1%).
- Desalting: Use C18 solid-phase extraction tips or columns to desalt and concentrate the peptide mixture. Elute peptides in 50-70% acetonitrile with 0.1% formic acid. Dry using a vacuum centrifuge and reconstitute in 0.1% formic acid for MS analysis.
2. LC-MS/MS Analysis:
- Chromatography: Inject the sample onto a reversed-phase C18 column (e.g., 75 µm x 250 mm, 2 µm particle size). Use a binary gradient from 2% to 35% mobile phase B (0.1% formic acid in acetonitrile) over 90 minutes at a flow rate of 300 nL/min.
- Mass Spectrometry: Operate the mass spectrometer in data-dependent acquisition (DDA) mode. Full MS scans (e.g., m/z 350-1600) are acquired at high resolution (60,000). The most intense ions are selected for fragmentation (HCD) and MS/MS analysis.
3. Data Processing:
- Use software (e.g., Proteome Discoverer, MaxQuant) to search MS/MS spectra against a database containing the protein sequence.
- Key parameters: Precursor mass tolerance 10 ppm, fragment mass tolerance 0.02 Da, static modification for carbamidomethylation (+57.021 Da on C), variable modifications for oxidation (+15.995 Da on M) and deamidation (+0.984 Da on N/Q).
- Quantify modified peptide abundances relative to their unmodified counterparts to calculate modification percentages [94].
Protocol 2.2: Systematic Quality Control for CITE-Seq Data using CITESeQC
This protocol provides a quantitative framework for assessing the quality of single-cell multiomics data [95].
1. Data Input and Preprocessing:
- Load the raw RNA count matrix and Antibody-Derived Tag (ADT) count matrix into R.
- Perform basic Seurat object creation and initial filtering (e.g., remove cells with <200 genes or >20% mitochondrial reads).
2. Running CITESeQC Diagnostic Modules:
- Execute sequential modules to generate a comprehensive QC report:
RNA_read_corr(): Check correlation between RNA molecule count and genes detected.ADT_read_corr(): Check correlation between ADT molecule count and ADTs detected.RNA_mt_read_corr(): Assess mitochondrial gene percentage.def_clust(): Perform clustering based on gene expression to define cell populations.RNA_dist()&ADT_dist(): Calculate and visualize the cell-type specificity of marker genes and ADTs using Shannon Entropy.multiRNA_hist()&multiADT_hist(): Generate histograms of entropy values to assess overall marker specificity across all clusters.RNA_ADT_read_corr(): Examine the global correlation between RNA library size and ADT library size per cell.
3. Interpretation and Action:
- Low entropy values indicate specific expression of a marker in one cluster, which is desirable.
- A histogram peak at high entropy values suggests poor marker specificity system-wide, which may indicate technical issues with the assay or poor clustering.
- A weak or negative correlation in
RNA_ADT_read_corr()may signal a global technical problem with one modality (e.g., poor antibody staining efficiency) [95].
Section 3: Technical Support Center – Troubleshooting Guides & FAQs
FAQ 1: Why do my QC metrics show high inter-laboratory variability for the same assay?
- Potential Causes & Solutions:
- Lack of Standardized Reagents: Different sources or lots of calibrators, enzymes, or antibodies. Solution: Implement the use of certified reference materials (CRMs) or reagent kits with traceability to higher-order standards [96].
- Protocol Deviations: Minor differences in sample preparation steps (e.g., incubation times, temperatures). Solution: Develop and adhere to a detailed, written Standard Operating Procedure (SOP). Use the "Ten Simple Rules" for SOP writing to ensure clarity and completeness [99].
- Instrument Calibration Differences: Mass spectrometers or sequencers are not calibrated to the same standard. Solution: Follow strict instrument qualification (IQ/OQ/PQ) and use system suitability tests (SST) before each batch run [94] [96].
FAQ 2: How can I troubleshoot inconsistent or failed peptide mapping results?
- Root Cause Analysis Steps:
- Check Sample Prep: Verify reagent concentrations (DTT, iodoacetamide), pH of buffers, and digestion enzyme activity. Run a positive control protein (e.g., BSA digest).
- Inspect Chromatography: Look for peak broadening, tailing, or shifting retention times. This indicates issues with the LC system (e.g., column degradation, pump leaks, gradient inconsistencies) [94].
- Review MS Performance: Check for low signal intensity, poor mass accuracy, or unstable spray in the source. Perform tuning and calibration with standard compounds.
- Examine Data Integrity: Ensure software settings are correct and raw data files are not corrupted. Maintain audit trails as per FDA 21 CFR Part 11 guidelines [94] [97].
FAQ 3: What should I do if my CITE-Seq data shows a poor correlation between RNA and protein (ADT) levels?
- Diagnostic Pathway:
- Step 1 - Segmented Analysis: Use the root cause analysis principle of segmenting data [97]. Check if the poor correlation is global or specific to certain cell clusters or protein targets.
- Step 2 - Investigate ADT Side: Poor correlation often stems from ADT issues. Check for: antibody lot variability, inadequate washing steps leading to high background, or antibody aggregates causing non-specific binding.
- Step 3 - Check Biological Expectations: Not all genes and proteins correlate linearly due to post-translational regulation. Consult literature for expected relationships for your targets [95].
- Step 4 - Validate with Orthogonal Method: Confirm key protein expression findings using an orthogonal technique like flow cytometry.
FAQ 4: How do I handle outliers in my QC dataset without introducing bias?
- Guidance: Do not automatically dismiss outliers. Follow a systematic approach:
- Determine if you care about the outlier's impact on downstream results [97].
- Investigate Cause: Use data lineage to trace the outlier's origin [97]. Was it a single sample preparation error? An instrument glitch during a specific run?
- Apply Consistent Rules: Pre-define statistically sound criteria (e.g., values beyond ±5 standard deviations from the mean) for exclusion in your SOP. Document every exclusion with a rationale [100].
- Consider the Signal: Some outliers may indicate a biologically or technically significant event worth exploring further, such as a novel impurity or a process deviation [100].
Section 4: Visualizing QC Workflows and Relationships
Diagram 1: Generalized QC and Troubleshooting Workflow for Systems Biology Data
Diagram 2: Pillars of Cross-Laboratory Data Comparability
Section 5: The Scientist's Toolkit – Essential Research Reagent Solutions
This table lists key materials and their roles in generating robust, QC-ready data.
| Item | Primary Function | Relevance to QC & Standardization |
|---|---|---|
| Certified Reference Materials (CRMs) | Provide a metrologically traceable standard with assigned target values and uncertainty. | Essential for calibrating instruments and validating methods across labs, reducing inter-laboratory variability [96]. |
| Stable Isotope-Labeled Internal Standards (SIL-IS) | Chemically identical to the analyte but with a heavier isotopic mass. | Used in LC-MS/MS for precise quantification, correcting for sample loss during preparation and ion suppression in the MS source [94] [98]. |
| Multiplexed Antibody Panels (CITE-Seq) | DNA-barcoded antibodies for simultaneous detection of surface proteins. | Must be validated for specificity and lot-to-lot consistency to ensure reliable protein measurement correlation with RNA data [95]. |
| System Suitability Test (SST) Mix | A cocktail of known analytes at defined concentrations. | Run at the start of each analytical batch to verify instrument sensitivity, chromatography, and mass accuracy are within predefined limits before sample analysis [94]. |
| Quality Control (QC) Pool | A homogeneous, characterized sample representing the test matrix. | Run at intervals alongside patient/experimental samples to monitor long-term assay precision, accuracy, and drift over time [96]. |
| Standard Operating Procedure (SOP) Document | A detailed, step-by-step written protocol for a specific process. | The foundation of reproducibility. A good SOP prevents deviations and ensures all technicians perform the assay identically, which is critical for GMP/GLP compliance [94] [99]. |
Establishing Community Reference Values for Key QC Parameters
Frequently Asked Questions
What are Community Reference Values (CRVs) and why are they critical in systems biology research? Community Reference Values are standardized, consensus-derived performance thresholds for quality control parameters that enable cross-laboratory reproducibility and data harmonization. They provide benchmark values for key analytical metrics such as imprecision, bias, and total error, allowing researchers to validate their experimental systems against community-accepted standards. Within systems biology, where computational models integrate diverse datasets, CRVs ensure that underlying experimental data meets minimum quality specifications, thereby enhancing model reliability and predictive accuracy [78].
How often should QC parameters be verified against Community Reference Values? Verification frequency should follow a risk-based approach considering several factors:
- Assay criticality: Clinically significant analytes require more frequent verification
- Method robustness: Methods with lower Sigma-metrics need more frequent monitoring
- Result turnaround time: Rapid-response tests may need shorter verification intervals
- Sample stability: Tests with strict pre-analytical requirements need careful scheduling
The 2025 IFCC recommendations advocate for a structured approach to IQC frequency planning, with considerations for both the number of tests in a series and the timing between QC assessments [101].
What corrective actions are required when QC results exceed Community Reference Values? When quality control results deviate beyond established CRVs, laboratories must implement a structured corrective action process:
- Immediate actions: Cease patient testing, quarantine affected results, and notify relevant stakeholders
- Investigation: Identify root causes through systematic evaluation of reagents, instrumentation, operator technique, and environmental conditions
- Remediation: Address identified issues through recalibration, maintenance, or retraining
- Documentation: Record all deviations, investigations, and corrective actions for audit trails
- Prevention: Implement process improvements to prevent recurrence
How do CLIA regulatory updates impact QC parameter establishment? The 2025 CLIA regulatory updates significantly strengthen proficiency testing requirements, particularly for common assays like hemoglobin A1C, where specific performance thresholds have been established (±8% for CMS, ±6% for CAP). These regulatory changes emphasize the importance of establishing CRVs that not only meet scientific standards but also satisfy evolving compliance requirements. Personnel qualification standards have also been updated, requiring more rigorous educational backgrounds for technical consultants overseeing QC programs [102].
Troubleshooting Guides
Inconsistent Inter-Laboratory QC Results
Problem: Significant variability in QC results across different laboratories using the same experimental protocols.
Investigation Steps:
- Verify all laboratories are using identical reagent lots and calibration materials
- Confirm instrumentation maintenance and calibration records are current and consistent
- Assess environmental conditions (temperature, humidity) across laboratory settings
- Review operator competency and training documentation
- Evaluate data transcription and calculation methods for human error
Resolution Actions:
- Implement standardized calibration procedures across all sites
- Establish centralized reagent procurement and distribution
- Create cross-laboratory proficiency testing programs
- Develop enhanced operator training with competency assessment
- Introduce automated data capture to reduce transcription errors
Prevention Strategies:
- Regular inter-laboratory comparison studies
- Clear documentation of all procedural details
- Ongoing training programs for technical staff
- Implementation of statistical process control monitoring
Computational Model Failures Despite Valid Experimental QC
Problem: Systems biology models generate unreliable predictions even when individual experimental components meet QC standards.
Investigation Steps:
- Verify model implementation using software engineering principles (testing, verification, validation)
- Check adherence to SBML (Systems Biology Markup Language) standards for model representation
- Assess parameter estimation methods and uncertainty quantification
- Evaluate data integration approaches from multiple experimental sources
- Review model documentation and version control practices
Resolution Actions:
- Recalibrate model parameters using standardized estimation techniques
- Implement model verification through iterative development and continuous integration
- Adopt container-based solutions to ensure computational reproducibility
- Enhance documentation following FAIR (Findable, Accessible, Interoperable, Reusable) principles
- Utilize established model repositories for version control and dissemination
Prevention Strategies:
- Implement robust software engineering practices for model development
- Adhere to community standards for model representation and annotation
- Establish comprehensive model documentation protocols
- Participate in model reproducibility initiatives and community benchmarking [78]
Signal-to-Noise Ratio Degradation in Longitudinal Studies
Problem: Progressive deterioration of assay performance metrics over extended experimental timelines.
Investigation Steps:
- Monitor reagent stability through accelerated degradation studies
- Assess instrument performance trends using statistical process control
- Evaluate environmental monitoring data for systematic changes
- Review sample processing and storage conditions
- Analyze operator performance metrics for technique drift
Resolution Actions:
- Establish revised reagent stability protocols and expiration timelines
- Enhance preventive maintenance schedules for critical instrumentation
- Implement environmental control system improvements
- Update standard operating procedures with additional controls
- Provide refresher training for technical staff
Prevention Strategies:
- Proactive reagent stability monitoring programs
- Enhanced instrument maintenance and calibration schedules
- Robust environmental monitoring systems
- Regular competency assessment for technical personnel
- Longitudinal performance trending and alert systems
Quantitative Reference Data Tables
Performance Specifications for Common Analytical Platforms
Table 1: Allowable Total Error Limits for Key Biomarkers
| Analyte | Minimum Performance Goal | Desirable Performance Goal | Optimal Performance Goal | Regulatory Requirement |
|---|---|---|---|---|
| Hemoglobin A1C | ±10% | ±8% | ±6% | ±8% (CMS), ±6% (CAP) [102] |
| Glucose | ±12% | ±10% | ±8% | ±10% |
| Cholesterol | ±12% | ±9% | ±8.5% | ±9% |
| ALT | ±20% | ±15% | ±12% | ±20% |
| Sodium | ±5% | ±4% | ±3% | ±4% |
Table 2: Sigma-Metrics for Analytical Performance Assessment
| Sigma Level | Quality Performance | Defect Rate (DPM) | Recommended QC Strategy |
|---|---|---|---|
| >6 | World-class | <3.4 | Minimal QC (1-2 rules) |
| 5-6 | Excellent | 3.4-233 | Moderate QC (2-3 rules) |
| 4-5 | Good | 233-6,210 | Multirule QC (3-4 rules) |
| 3-4 | Marginal | 6,210-66,807 | Extensive QC (4-6 rules) |
| <3 | Unacceptable | >66,807 | Method improvement required |
Statistical QC Decision Rules
Table 3: Westgard Rules Implementation Guide
| Rule Name | Rule Definition | Application Context | Interpretation |
|---|---|---|---|
| 1₂₈ | One control exceeds ±2SD | All methods | Warning rule - potential error |
| 1₃₈ | One control exceeds ±3SD | All methods | Random error detected |
| 2₂₈ | Two consecutive controls exceed same ±2SD | All methods | Systematic error detected |
| R₄₈ | Range between two controls exceeds 4SD | All methods | Random error detected |
| 4₁₈ | Four consecutive controls exceed same ±1SD | High Sigma methods | Systematic error detected |
| 10ₓ | Ten consecutive controls on same side of mean | High Sigma methods | Systematic error detected |
Experimental Protocols
Protocol 1: Establishing Precision Parameters
Purpose: To determine within-run and between-run imprecision for quality control materials.
Materials:
- Quality control materials at multiple concentrations
- Calibrated instrumentation
- Data recording system
Procedure:
- Analyze QC material in duplicate twice daily for 20 days
- Record all results in appropriate database
- Calculate mean, standard deviation, and coefficient of variation for within-run and between-run data
- Compare calculated imprecision to established CRVs
- Document any deviations from expected performance
Acceptance Criteria: Within-run CV ≤ 1/3 of total allowable error; Between-run CV ≤ 1/2 of total allowable error
Protocol 2: Method Comparison and Bias Estimation
Purpose: To evaluate systematic differences between test and comparative methods.
Materials:
- 40-100 patient samples spanning reportable range
- Reference method or materials
- Statistical analysis software
Procedure:
- Analyze patient samples using both test and reference methods
- Plot results using difference plots (Bland-Altman) and regression analysis
- Calculate mean difference (bias) and 95% limits of agreement
- Compare observed bias to allowable bias based on CRVs
- Establish correction factors if necessary
Acceptance Criteria: Observed bias ≤ 1/4 of total allowable error
Experimental Workflow Visualization
CRV Development Workflow
Data Quality Integration Pathway
Research Reagent Solutions
Table 4: Essential Materials for QC Parameter Establishment
| Reagent/Material | Function | Application Context | Quality Specifications |
|---|---|---|---|
| Certified Reference Materials | Calibration and accuracy verification | Method validation and standardization | Traceable to international standards |
| Third-Party Quality Controls | Independent performance assessment | Daily quality monitoring | Commutable with patient samples |
| Stabilized Biological Materials | Long-term precision assessment | Longitudinal performance monitoring | Stable at recommended storage conditions |
| Computational Standards (SBML) | Model representation and sharing | Systems biology model development | Level 3 Version 2 compliance [78] |
| Containerization Solutions | Computational reproducibility | Model verification and validation | Docker/Singularity compatibility |
| Enzyme Activity Assays | Metabolic pathway assessment | Signaling network studies | Linearity across physiological range |
| Protein Quantitation Kits | Biomarker measurement | Proteomic studies | CV ≤10% at lower limit of quantitation |
| Nucleic Acid Extraction Kits | Genetic material isolation | Genomic and transcriptomic studies | Yield ≥90%, purity A260/A280 1.8-2.0 |
Conclusion
The establishment and adherence to rigorous, standardized quality control standards are not optional but fundamental to the success and credibility of systems biology research. This guide has synthesized a path forward, moving from foundational awareness to practical application, troubleshooting, and validation. The key takeaway is that a proactive, integrated QC framework is essential for generating reliable, reproducible data that can power robust biological discoveries and accelerate translational medicine. Future progress hinges on widespread adoption of community-driven best practices, continued development of harmonized protocols as championed by groups like mQACC, and the strategic integration of advanced cyberinfrastructure to manage data complexity. Embracing these principles will enhance data comparability across studies, build confidence in systems biology models, and ultimately strengthen the bridge from foundational research to clinical application and personalized therapeutics.
References
- 1. Multi-Omics: Challenges and Solutions [https://bigomics.ch/blog/key-challenges-in-multi-omics-data-integration/]
- 2. Multi-omics Quality Assessment in Personalized Medicine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390891/]
- 3. Multi-Omics Quality Control and Data Integration [https://www.iso.org/standard/88532.html]
- 4. Navigating Challenges and Opportunities in Multi-Omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11274472/]
- 5. Integrating Multi-Omics Data: Methods and Applications in ... [https://www.sciencedirect.com/science/article/pii/S2215017X25000657]
- 6. What is Systems Biology? [https://isbscience.org/what-is-systems-biology/]
- 7. The evolution of standards and data management practices in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4704484/]
- 8. Quality Assurance vs Quality Control in Life Science ... [https://www.dotcompliance.com/blog/quality-4-0/quality-assurance-vs-quality-control-in-life-sciences-manufacturing/]
- 9. What Is Data Quality Assurance in Bioinformatics? [https://ranchobiosciences.com/2025/04/bioinformatics-and-quality-assurance-data/]
- 10. What is quality assurance vs. quality control? 5 key ... [https://www.qualio.com/blog/quality-assurance-vs-quality-control]
- 11. Protocols & Troubleshooting Guides [https://www.rndsystems.com/resources/protocols-troubleshooting-guides]
- 12. What Is a Troubleshooting Guide and 6 Steps to Create ... [https://clickhelp.com/clickhelp-technical-writing-blog/troubleshooting-guide-definition-importance-and-tips-for-creating/]
- 13. 11.5: Principles of Quality Assurance (QA) and ... [https://bio.libretexts.org/Courses/Cedar_Crest_College/Intro_to_Biotechnology/11%3A_Government_Oversight_of_Biotechnology/11.05%3A_Principles_of_Quality_Assurance_(QA)_and_Quality_Control_(QC)]
- 14. How to be a Better Troubleshooter in Your Laboratory [https://www.goldbio.com/blogs/articles/how-to-be-a-better-troubleshooter?srsltid=AfmBOoq84jhb_z64DjesQL_auOzk2Naq6KWzB762LZ2t_KW1uVerQ67-]
- 15. Preanalytical Variables and Their Influence on the Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6238383/]
- 16. Expert Pre-Analytical Work Processing - Sampled [https://sampled.com/the-critical-role-of-pre-analytical-work/]
- 17. Guidelines for Research Data Integrity (GRDI) - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11739391/]
- 18. What Is Data Integrity in Biomedical Research? [https://ranchobiosciences.com/2024/12/biomedical-research-and-data-integrity/]
- 19. Quality Management System Implementation Guide for ... [https://www.scispot.com/blog/quality-management-system-implementation-guide-for-biotech-and-life-science-labs]
- 20. mQACC [https://www.mqacc.org/]
- 21. Scientific Task Groups [https://metabolomicssociety.org/board-committees/scientific-task-groups/]
- 22. Troubleshooting in Large-Scale LC-ToF-MS Metabolomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6918290/]
- 23. Reference materials for MS-based untargeted metabolomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8994740/]
- 24. Working Groups [https://www.mqacc.org/wgs]
- 25. Metabolomics Society [https://metabolomicssociety.org/]
- 26. Tips and tricks for LC–MS-based metabolomics and ... [https://www.sciencedirect.com/science/article/pii/S0165993624004230]
- 27. The FAIR Guiding Principles for scientific data ... [https://www.nature.com/articles/sdata201618]
- 28. FAIR data principles: What you need to know [https://tiledb.com/blog/fair-data-principles-explained]
- 29. FAIR Principles [https://www.go-fair.org/fair-principles/]
- 30. Quality assurance and quality control reporting in untargeted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9420093/]
- 31. LC Troubleshooting Essentials: A Guide to Common ... [https://www.chromatographyonline.com/view/lc-troubleshooting-essentials-a-guide-to-common-problems-and-solutions-for-peak-tailing-ghost-peaks-and-pressure-spikes]
- 32. Troubleshoot QC Results [https://unityweb.qcnet.com/Documentation/Help/UnityWeb/1535.htm]
- 33. Standards, Dissemination, and Best Practices in Systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10435326/]
- 34. BioAgents: Bridging the gap in bioinformatics analysis with ... [https://www.nature.com/articles/s41598-025-25919-z]
- 35. The Art of Troubleshooting for Customer Support ... [https://www.helpscout.com/helpu/art-of-troubleshooting-support/]
- 36. The complete guide to customer service troubleshooting [https://devrev.ai/blog/customer-service-troubleshooting]
- 37. QComics: Recommendations and Guidelines for Robust ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10809278/]
- 38. QC4Metabolomics: Real-Time and Retrospective Quality ... [https://pubmed.ncbi.nlm.nih.gov/40858289/]
- 39. Improving metabolomics data comparability without long ... [https://www.sciencedirect.com/science/article/pii/S000326702501147X]
- 40. Overcoming Common Challenges in Proteomics Experiments [https://www.technologynetworks.com/proteomics/articles/addressing-proteomics-challenges-enhancing-sample-preparation-techniques-405806]
- 41. Towards unmanned proteomics data generation: a fully ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572148/]
- 42. Failed System Suitability Test: A Case Study [https://www.chromatographyonline.com/view/failed-system-suitability-test-case-study-0]
- 43. Performance metrics for evaluating system suitability in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4966392/]
- 44. Troubleshooting and Solutions for On-Site Instrumentation ... [https://zeroinstrument.com/troubleshooting-and-solutions-for-on-site-instrumentation-failures/]
- 45. Common Faults in Field Instruments and Troubleshooting Tips [https://jiweiauto.com/common-faults-troubleshooting-field-instruments.html]
- 46. System Suitability Reports in Byos and Dashboards ... [https://support.proteinmetrics.com/hc/en-us/articles/22329990477972-System-Suitability-Reports-in-Byos-and-Dashboards-for-Monitoring-Instrument-Performance-in-Byosphere]
- 47. Practical Recommendations for Supporting a Systems Biology ... [https://datascience.codata.org/articles/dsj-2020-024]
- 48. A practical guide to FAIR data management in the age of multi ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11788310/]
- 49. Frequently Asked Questions About Quality Control vs. ... [https://www.biopharminternational.com/view/frequently-asked-questions-about-quality-control-vs-quality-assurance]
- 50. Cybersecurity Innovation for Cyberinfrastructure (CICI) [https://www.nsf.gov/funding/opportunities/cici-cybersecurity-innovation-cyberinfrastructure]
- 51. OASIS to Advance Global Adoption of Data & Trust ... [https://www.oasis-open.org/2025/03/06/oasis-to-advance-data-provenance-standards/]
- 52. NSF grant supports advances in cyberinfrastructure for ... [https://news.ucsb.edu/2025/021931/nsf-grant-supports-advances-cyberinfrastructure-multimodal-imaging-data]
- 53. Use sufficient color contrast - Harvard's Digital Accessibility [https://accessibility.huit.harvard.edu/use-sufficient-color-contrast]
- 54. Proteomics Quality Control: A Practical Guide to Reliable ... [https://www.metwarebio.com/proteomics-quality-control-reproducible-data/]
- 55. How to Troubleshoot Sequencing Preparation Errors (NGS ... [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 56. Metabolomics Service FAQs [https://www.arome-science.com/metabolomics-service-faqs/]
- 57. Instrumental Drift in Untargeted Metabolomics: Optimizing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10222478/]
- 58. Quantitative challenges and their bioinformatic solutions in ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993623000961]
- 59. Strategies for Handling Missing Values in Data Analysis [https://www.dasca.org/world-of-data-science/article/strategies-for-handling-missing-values-in-data-analysis]
- 60. 5 Effective Strategies to Handle Missing Values in Data ... [https://www.analyticsvidhya.com/blog/2021/10/handling-missing-value/]
- 61. Addressing Absence: Handling Missing Values [https://letsdatascience.com/handling-missing-values/]
- 62. PEAKQC: periodicity evaluation in single-cell ATAC-seq ... [https://pubmed.ncbi.nlm.nih.gov/40966653/]
- 63. 5 Tips on Designing Colorblind-Friendly Visualizations [https://www.tableau.com/blog/examining-data-viz-rules-dont-use-red-green-together]
- 64. Preanalytical Errors in Clinical Laboratory Testing at a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10981510/]
- 65. Quality Indicators to Detect Pre-Analytical Errors in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3428256/]
- 66. THE PREANALYTICAL ERRORS: A CONTINUOUS… [https://ascls.org/the-preanalytical-errors/]
- 67. Detecting Preanalytical Errors Using Quality Indicators in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9208812/]
- 68. Preanalytical Errors in a Hematology Laboratory [https://www.mdpi.com/2075-4418/13/4/591]
- 69. QA/QC Requirements for Biotech Companies and the ... [https://qbench.com/blog/qa-qc-requirements-for-biotech-companies-and-the-benefits-of-a-lims]
- 70. Establishing a framework for best practices for quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10861687/]
- 71. Pre-Analytical, Analytical, & Post-Analytical Phases of Lab ... [https://genemod.net/blog/pre-analytical-lab-testing-phase]
- 72. Assessing and mitigating batch effects in large-scale omics ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-024-03401-9]
- 73. Diagnostics and correction of batch effects in large‐scale ... [https://link.springer.com/article/10.15252/msb.202110240]
- 74. Addressing the batch effect issue for LC/MS metabolomics ... [https://www.nature.com/articles/s41598-020-70850-0]
- 75. MCP Data Normalization: Techniques & Best Practices 2025 [https://www.byteplus.com/en/topic/542085]
- 76. Why You Must Correct Batch Effects in Transcriptomics Data? [https://www.metwarebio.com/transcriptomics-batch-effect-correction/]
- 77. Metabolomics Batch Effects [https://www.metwarebio.com/metabolomics-batch-effects/]
- 78. Standards, dissemination, and best practices in systems ... [https://www.sciencedirect.com/science/article/abs/pii/S0958166923000320]
- 79. Q Exactive BioPharma Platform Mass Spectrometer Support [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/mass-spectrometry-support-center/liquid-chromatography-mass-spectrometry-instruments-support/q-exactive-biopharma-platform-mass-spectrometer-support/q-exactive-biopharma-platform-mass-spectrometer-support-troubleshooting.html]
- 80. Powerful New Products from ASMS 2025 Drive Mass ... [https://www.labmanager.com/powerful-new-products-from-asms-drive-mass-spectrometry-performance-34073]
- 81. Correction of gas chromatography–mass spectrometry long ... [https://www.nature.com/articles/s41598-025-24794-y]
- 82. Chromatography 2025: The Trends Transforming ... [https://www.sepscience.com/chromatography-2025-the-trends-transforming-laboratories-11149]
- 83. Mass Spectrometer (MS) troubleshooting guide [https://alliancebioversityciat.org/publications-data/mass-spectrometer-ms-troubleshooting-guide]
- 84. Establishing Acceptance Criteria for Analytical Methods [https://www.biopharminternational.com/view/establishing-acceptance-criteria-analytical-methods]
- 85. Classification: Accuracy, recall, precision, and related metrics [https://developers.google.com/machine-learning/crash-course/classification/accuracy-precision-recall]
- 86. Beware of counter-intuitive levels of false discoveries in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359981/]
- 87. Assessment of false discovery rate control in tandem mass ... [https://www.nature.com/articles/s41592-025-02719-x]
- 88. (PDF) Multicenter experiment for quality control of peptide-centric... [https://www.academia.edu/98610702/Multicenter_experiment_for_quality_control_of_peptide_centric_LC_MS_MS_analysis_A_longitudinal_performance_assessment_with_nLC_coupled_to_orbitrap_MS_analyzers]
- 89. Harmonization of Clinical Laboratory Test Results - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4975212/]
- 90. Assay Harmonization Activities and Resources - NCI [https://dctd.cancer.gov/drug-discovery-development/assays/harmonization]
- 91. Use of Hoteling's T2 multivariate control chart for effective ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131413/]
- 92. Using Fuzzy C-Means clustering and PCA in public health [https://www.sciencedirect.com/science/article/pii/S2352914825000541]
- 93. Machine learning-based strategies for improving healthcare ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12319021/]
- 94. How Mass Spectrometry enhances GMP quality control ... [https://amsbiopharma.com/mass-spectrometry-gmp-qc/]
- 95. Quantitative measures to assess the quality of cellular ... [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2025.1630161/full]
- 96. Standardization of clinical mass spectrometry | LabLeaders [https://diagnostics.roche.com/global/en/article-listing/lab-leaders/article/mass-spectrometry-standards.html]
- 97. The Data Engineer's Guide To Root Cause Analysis ... [https://www.montecarlodata.com/blog-the-data-engineers-guide-to-root-cause-analysis-2/]
- 98. Advanced mass spectrometry techniques for monitoring ... [https://www.sciencedirect.com/science/article/pii/S0167779925003117]
- 99. Ten simple rules on how to write a standard operating procedure [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1008095]
- 100. How to Troubleshoot Common Data Analysis Mistakes [https://www.netsuite.com/portal/resource/articles/data-warehouse/data-mistakes.shtml]
- 101. 2025 IFCC Recommendations for IQC [https://www.westgard.com/essays/quality-requirements-and-standards/ifcc-iqc-2025.html]
- 102. 2025 Changes to Point-of-Care Testing Regulatory ... [https://myadlm.org/education/point-of-care-testing-professional-certification/the-point/articles/2025/may]